Sexual Harassment Allegations in Healthcare: Rising Risks
 By Richard Cahill, JD, Vice President and Associate General Counsel The Doctors Company
By Richard Cahill, JD, Vice President and Associate General Counsel The Doctors Company


Consider the following scenario: A successful and highly respected pediatrician with an unblemished record over decades of practice learns of a HIPAA breach by a member of his administrative staff. The employee is terminated after an investigation reveals that the employee had been responsible for multiple breaches. Imagine the physician’s reaction when the former employee’s attorney not only initiates a wrongful termination suit, but also alleges retaliation, claiming the employee rebuffed sexual advances from the physician.
To gain additional leverage, the former employee’s attorney submits a complaint of sexual harassment with the medical board and files a criminal complaint for sexual battery. In addition, the attorney sends a letter to the medical executive committee of the principal hospital where the physician admits patients, resulting in a peer review investigation. Finally, the former employee blankets social media with an aggressive smear campaign.
This example demonstrates that no healthcare practitioner is immune from the growing number of reported incidents of alleged sexual harassment in the workplace and that the ramifications are widespread. Accusers could be employees, independent contractors, patients, third-party vendors, or visitors. Individuals alleged to have acted inappropriately could include coworkers, supervisors, subordinates, professional staff—and even patients.
Repercussions of Harassment Claims
Shortly after a complaint is filed, costly and potentially embarrassing investigations may be conducted by law enforcement, human resources departments, and administrative agencies. Depending on the nature and
scope of the findings, serious adverse consequences and irreparable harm to a practitioner’s reputation may follow. The consequences could include the following actions:
• Criminal prosecution.
• Civil litigation with the potential for substantial monetary damages, which may not be covered by professional liability policies.
• Licensing board actions that may impose limitations on an individual’s ability to continue practicing.
• Exclusion from third-party payer networks, which can have a significant impact on a practitioner’s financial stability.
• Adverse decisions by the medical executive committees of the facilities where the practitioner works, resulting in a limitation of privileges.
Risk Mitigation Strategies
Given the risks, heightened awareness, and increased scrutiny of sexual harassment claims, healthcare practitioners and facilities are strongly encouraged to develop, implement, and consistently enforce a zero-tolerance policy. Consider developing written protocols that are periodically reviewed,
audited, and updated as necessary. Include the following details:
• The types of conduct that will not be tolerated, regardless of the identity of the alleged perpetrator.
• A clear methodology for reporting claimed instances of wrongdoing.
• The process to be followed in investigating complaints and rules to help ensure that confidentiality and due process are appropriately protected.
• The documentation to be completed and maintained.
• The range of sanctions (up to and including termination) for both employees and patients, should the allegations ultimately be determined to be true.
Train new staff as part of the onboarding process, and provide ongoing training for all staff. Develop and retain attendance sheets as proof of the training. In the event of a subsequent problem, proof of training demonstrates good faith and diligence in continuing efforts to comply with federal and state requirements.
Institute a process of publishing
PRSRT STD US POSTAGE PAID PERMIT NO 1 HOUSTON TX PERMIT # 1149 AUSTIN TX May Edition 2023 Volume 6 | Issue 5 St. David’s Georgetown Hospital Names New Chief Executive Officer See pg. 8 Inside This Issue AI Can Spot Early Signs of Alzheimer’s in Speech See pg. 10 INDEX Legal Matters pg.3 Oncology Research ........ pg.4 Healthy Heart pg.6 Hospital News pg.8 seeRising Risks ...page 14
Equals make THE BEST PARTNERS.
Austin Medical Times Page 2 May 2023 austinmedtimes.com
We’re taking the mal out of malpractice insurance. As a company founded and led by doctors, we know what keeps you up at night. It’s why we partner with practices of all sizes to help manage the complexities of today’s healthcare environment and reward the practice of good medicine. Because when you have a partner who’s also a peer, you have malpractice insurance without the mal. Join us at thedoctors.com 7588_TX_HoustonMedTimes_BP_Oct2020_0920_v1.indd 1 9/17/20 1:45 PM
Legal Matters
Mitigating Your Greatest Data Privacy Risk
 By
By
Third-party vendors pose a significant risk
The greatest data privacy threat to companies is commonly thought to be that company’s employees. While employees can be a threat, the majority of data breaches and intrusions (63%) are tied to or directly caused by third-party vendors.
II. The concept of vendor management
Companies can effectively manage their vendor risk if they follow a comprehensive vendor management
program. Many companies rely on their procurement department to gather information on vendors and/ or to establish a risk profile through vendor assessments. But as more and more vendors have cloud-based or Internet-of-Things components, it is time to pull vendor management away from the procurement team and implement different measures.
III. The information security agreement
The company must be the party establishing parameters for its risk tolerance and legal and regulatory obligations. A written document, whether a stand-alone agreement or an exhibit or addendum to the underlying relationship agreement, that sets forth specific physical and technical standards as well as ongoing obligations by your vendors is commonly referred to as an information security agreement (“ISA”).
At a minimum, an ISA should address the following:
• Certifications. Certain industries have required certifications (e.g., the Health Information Technology for Economic and Clinical Health Act), while others follow industry standards (e.g., SOC2). Vendors should provide copies of their certifications.
• Data breach notification. How will the vendor notify you if your data is breached? When must the vendor notify you of a breach? What does the vendor have to do for you and the data subjects post-breach?



• Employee/subcontractor management. Do vendor employees need background checks? Can the
vendor engage subcontractors without your approval?
• Data encryption, storage/ destruction. Where can and can’t the vendor store your data? What happens to your data when your agreement with the vendor is over?
• Malware. What internal processes does the vendor have in place to detect malware and prevent cyberattacks? Does the vendor regularly scan its systems (and make the results of those scans available to you upon request)? What happens if the vendor passes a virus on to you?
Austin Medical Times Page 3 May 2023 austinmedtimes.com Medical Check In Improving customer service with technology As low as $34 / month 800-971-8871 www.medicalcheckin.com Fast Patient Sign In Process Organizes Patients by Reason HIPAA Compliant TX-RAMP Certified Unlimited Data Unlimited Support
see Data Risk ...page 14
Kathryn T. Allen, J.D.
Kelsey L. Brandes, J.D. Polsinelli, PC
Liver Transplant Survivor’s Recovery Linked to Sociodemographic Factors, UTSW Study Shows
Positive Coping, Resiliency, Post-Traumatic Growth, And Psychiatric Symptoms Vary at Different Stages After Surgery
Theresilience and coping abilities of patients who’ve had liver transplants vary and change over time and are often linked to sociodemographic factors including income, race, and education, a study led by UT Southwestern Medical Center researchers shows. The findings could lead to tailored interventions to optimize clinical and patient-centered outcomes among liver transplant recipients.
“When we take care of patients who have gone through this life-changing surgery, recovery really evolves over time,” said transplant hepatologist Sarah R. Lieber, M.D., M.S.C.R., Assistant Professor of Internal Medicine and a member of the Division of Digestive and Liver

Diseases. “We don’t fully understand or capture that with current metrics that focus on mainly clinical outcomes such as survival. The aim of this project was to get a more in-depth view of novel patient-reported concepts at different stages of survivorship.”
Dr. Lieber led the study published in Liver Transplantation, working with UTSW mentor Amit G. Singal, M.D., M.S., Professor of Internal Medicine, a member of the Division of Digestive and Liver Diseases and the Harold C. Simmons Comprehensive Cancer Center, Medical Director of the Liver Tumor Program, and Chief of Hepatology.
Transplantation offers the chance for a cure for thousands of patients in the
Postdoctoral Certificate in
U.S. every year with diseases or trauma that affect the liver. Although more than 70% who receive this surgery survive at least five years, Dr. Lieber said, their recovery can be filled with physical, emotional, and psychological challenges. Liver transplant survivors must adapt to a new life that includes strict medication adherence, frequent clinical monitoring, and unanticipated complications.
To better understand what factors influence survivorship, Dr. Lieber and colleagues emailed surveys to hundreds of patients who received liver transplants between January 1990 and November 2019 and were followed at the University of North Carolina Liver Transplant Center.
The surveys collected sociodemographic information such as age, sex, race, ethnicity, education level, and income; pre-transplant characteristics such as reason for transplantation, waitlist time, and psychiatric history; and post-transplant characteristics including length of hospital stay, employment status, and whether patients had a caregiver. They also included survey questions validated for other chronic conditions to assess
the patients’ abilities to positively cope as well as their level of post-traumatic growth (the ability to adapt and grow after a traumatic event), resiliency, and symptoms of anxiety and depression. The researchers received 191 completed surveys from patients with a broad span of survival periods ranging from less than a year post-transplant to more than 10 years. A majority of respondents were male (about 64%) and Caucasian (about 84%) and ranged from 28 to 83 years old.
see Liver Transplant ...page 13
Infant & Early Childhood Development
The online and hybrid PhD and Master’s programs in Infant and Early Childhood Development (IECD) with emphases in mental health and developmental disorders is a multidisciplinary degree that includes mental health, education, occupational therapy, physical therapy, speech and language development, and the neurosciences.
For 45 years, Fielding has been educating scholars and leaders in pursuit of a more just and sustainable world.

Austin Medical Times Page 4 May 2023 austinmedtimes.com
Fielding.edu/IECD Online & Hybrid PHD and MASTER’S DEGREES
Sarah R. Lieber, M.D., M.S.C.R., Assistant Professor of Internal Medicine, is a member of the Division of Digestive and Liver Diseases
Oncology Research

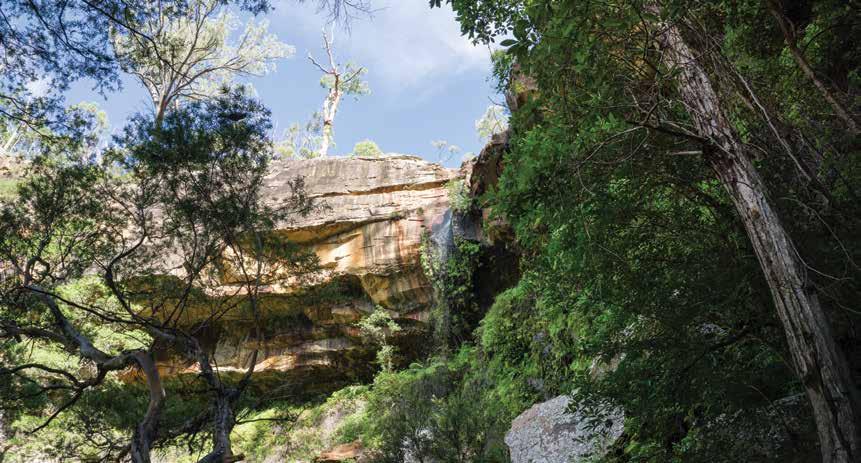
Spending Time in The Great Outdoors When You Have Cancer
By Shubhada Shrikhande, M.D., Texas Oncology Austin North

Think about the last time you were outdoors. Did you feel happier, calmer, a sense of peace? Studies have shown being outside can benefit one’s health and well-being, offering opportunities for physical activity while also reducing stress and improving mental health.
For cancer patients, a compromised immune system often requires them to be more cautious of where they are spending their time. For many, it means staying indoors, which can lead to feelings of isolation and depression.
However, spending time outside and feeling the sun on your skin or
taking a few deep breaths of fresh air may provide a brief and comforting escape from the daily stresses of cancer for both patients and caregivers. Benefits of spending time outside
In a recent poll, current and former cancer patients were asked about the impact of cancer on self-perception, body image, and mental and emotional health. 70% of respondents said they experienced one or more symptoms of depression during cancer treatment.
Research has shown that spending time outdoors reduces symptoms of depression and anxiety and helps the mind to rest. One study found that contact with nature decreased mental distress and increased feelings of happiness, positive social interactions, and a sense of meaning and purpose in life.
Feelings of stress are also common among cancer patients. Adding time outside can be beneficial in helping
patients cope with a cancer diagnosis or while going through treatment. According to the National Recreation and Park Association, as little as 20 minutes a day spent outdoors can reduce stress.
Other notable benefits of spending time outside include:
• Better breathing
• Improved sleep
• Motivation to exercise
• Escape from over stimulating technology and sounds
• Boosted immunity
Outdoor activities suitable for cancer patients
Adding outdoor time doesn’t
require hours of commitment. Activities may vary based on treatments, side effects, and how patients feel on any given day. Sometimes just a few minutes outside each day is all that is needed to improve one’s mood.
Exercise releases hormones called endorphins which reduce feelings of stress and pain. Easy, low-impact outdoor activities like walking or hiking through one of over 80 state parks across Texas, swimming, riding a bike, yoga, or gentle stretching can improve blood circulation, appetite, and muscle strength. It see Oncology Research...page 14
Austin Medical Times Page 5 May 2023 austinmedtimes.com
you can get the Austin Medical Times delivered straight to your inbox. Never miss an Issue of Austin’s Leading Local Healthcare News Online. Subscribe to Our Digital
austinmedtimes.com
Now
Issue
FEEL GOOD AGAIN
Healthy Heart
A Heart-Healthy Life Begins with Good Prenatal Care

The American Heart Association Says Healthy Hearts Are A Key To Healthy Pregnancies.
By Megan Jameson The American Heart Association
Poorheart health puts both mothersto-be and their children at risk. Heart disease is the leading cause of pregnancy-related death causing more than 1 in 4 pregnancy-related deaths
What’s good for mom is also good for baby. The study found that children are more likely to have good cardiovascular health during adolescence and beyond if their mothers had good heart health during pregnancy.
“The role of a healthy lifestyle
GIVE
centraltexasfoodbank.org
Presented by
(26.5%), according to the American Heart Association Heart Disease and Stroke Statistics 2022 Update. A study published in 2022 in the Association’s flagship journal, Circulation, found that only about 40% of women in the U.S. who give birth have good heart health prior to their pregnancy with excess weight being the major driver of poor pre-pregnancy health.
According to Michelle A. Albert, M.D., M.P.H., FAHA, volunteer president of the American Heart Association, even if a woman isn’t at her healthiest before becoming pregnant, it’s never too late to work on getting healthier for her baby and herself.
“Pregnancy is often a pivotal time in a woman’s life from both short and long term perspectives. For some, it may be their first experience with a major medical condition, for most, it’s a natural time to be more forward-thinking about their own health, as well as that of their baby,” said Albert. “Getting regular prenatal care as well as post-pregnancy cardiovascular risk factor management if appropriate along with making healthy lifestyle changes can improve the pregnancy and birth experience.”
during pregnancy cannot be emphasized enough.” Albert said. “Healthy diet, moderate exercise including walking, smoking cessation and other healthy behaviors are important tools for a healthy pregnancy for both mother and child.”
Women who have heart disease or who experience cardiovascular complications during pregnancy should work closely with their health care clinician to monitor their health and take medications as prescribed to treat and reduce cardiovascular risk factors that could follow them through life.
“There is still much to learn about the special risks of maternal and infant health related to cardiovascular health. This is an area the American Heart Association continues to follow closely, devoting research dollars and other resources to ensuring the healthiest outcomes for parents and babies throughout their lifetime,” Albert said.
Learn more about having a healthy pregnancy at heart.org.
Austin Medical Times Page 6 May 2023 austinmedtimes.com
We’re all ready to feel good again, but for our food insecure neighbors there’s no vaccine to fight hunger.
The 1 in 5 Central Texas children at risk of hunger deserve a shot at a happy summer.
UT Austin Research Initiative Focuses on Unique Needs, Hardships of Military Spouses

For 41-year-old mother of four Melissa Megoulloa, taking on the challenges as the spouse of an Army sergeant was familiar territory, dating back to her childhood.
“I’m a Navy brat. I saw what a hard time my mother had when we were kids. I swore if I married a military man, I’d make sure no one goes through what we did,” said Megoulloa. “Every [military] base I’ve moved to, I’ve asked, ‘How can we do this better?’”
The nation’s more than 700,000 spouses of active-duty military personnel like Megoulloa face myriad practical and emotionally taxing obstacles in supporting their partners. As part of its multifaceted work to address the social support and behavioral health needs of military and veteran families, the Institute for Military and Veteran Family Wellness at The University of Texas at Austin is launching a new research initiative focused on supporting military spouses. The institute is a joint effort
of Dell Medical School’s Department of Health Social Work and the Steve Hicks School of Social Work.
Supported by a $1.4 million award from the Congressionally Directed Medical Research Program (CDMRP), the UT team will adapt and test an existing curriculum-based peer support group model called the Military Spouse Resiliency Group Program. The program trains military spouses to become peer leaders who facilitate supportive discussions with other active-duty spouses and connects participants to local and national support resources. The Unique Challenges of Military Spouses
Frequent relocation to brand new surroundings has placed the Megoulloa household of six in constant upheaval. For the past twenty years, her husband has been moved through his job in active military service every 18 months to three years. When he gets a new assignment, all his arrangements
Empathy-Focused Phone Calls May Improve Depression
Aseries of simple phone calls holds promise in helping to curb symptoms of depression, according to a study from Dell Medical School at The University of Texas at Austin, published today in the journal Psychiatric Services.

Known as “Sunshine Calls,” the four-week program was conducted as a randomized controlled trial of 240 mostly homebound, older adults. Participants who suffered from depressive symptoms at the beginning of the program experienced improvements in loneliness and depression. Researchers used a standardized measurement scale for depression to show that depressive symptoms dropped from an average of 13 points down to 9. A score of 10 points and above signifies symptoms of clinical depression.
The study adds to a growing area of research and innovation focused on alternate models for delivering
mental health support. It further underscores the need to expand the workforce while advancing existing health systems to pay for new kinds of effective solutions.
“The high incidence of depression and loneliness in the U.S., combined with an extraordinary shortage of mental health professionals, means we need effective, affordable solutions to care in America,” said study author Maninder “Mini” Kahlon, Ph.D., Associate Professor of Population Health at Dell Med.
A 2016 U.S. Department of Health and Human Services report projects the workforce will need 10,000 mental health professionals by 2025.
“This is a low cost, minimally invasive method that builds on our essential need for human connection. It’s as simple as that,” said Kahlon. Study participants were Meals
are given with detailed instructions from the Army. In contrast, spouses often don’t receive any guidance, said Megoulloa.
“The families are expected to just figure it out. Things like, how do we get to the new location? Can I find a job? How will I set up play dates for my kids? We have to create a whole new support system for ourselves to survive.”
A recent study indicated that nearly a quarter (24%) of active-duty family members say that “military family quality of life” is a top concern, pointing to instability and
inconsistency of daily life as the key reason. Spending enough time with children and family, the frequency and difficulty of relocating, and limited communication from the military command are common issues cited.
Initial results from the current study show that participants of the peer support group model experience improvements in quality of life, depression and anxiety, self-care behaviors and perceived social support.
on Wheels America clients, about half of whom lived alone, and 58 who suffered from depression. The phone calls were made by people who were not health care professionals but had undergone a brief training about how to listen and ask questions and learn as much as they could about the person they were calling. The researchers measured depression levels using a standardized questionnaire, the PHQ-9. Participants received one call each weekday during the first week and were given the choice to cut back
the phone call frequency to two or three times weekly thereafter. The Sunshine Calls program was developed by Factor Health, an initiative of Dell Med and the Episcopal Health Foundation, in collaboration with Meals on Wheels Central Texas. Factor Health tests and builds programs at scale to deliver health outside of traditional settings such as clinics and hospitals.
Austin Medical Times Page 7 May 2023 austinmedtimes.com
see Military Spouses ...page 13
Hospital News
St. David’s Georgetown Hospital Names
New Chief Executive Officer
St.David’s Georgetown Hospital has named Kyle Landry as its
new chief executive officer, replacing Hugh Brown who retired on April 7, 2023. Landry assumed his new role on April 17, 2023.
Since 2015, Landry has served in various leadership positions within St. David’s HealthCare, most recently serving as chief operating officer at St. David’s South Austin Medical Center. In this role, Landry oversaw the hospital’s Level II Trauma Center and emergency department. He also helped launch the hospital’s breast cancer, robotic bronchoscopy, structural heart and transcatheter aortic valve replacement (TAVR) programs, as well as expanded surgical services.
“Kyle’s knowledge of our healthcare system, combined
with his demonstrated success in managing hospital operations and building positive relationships with physicians, make him well equipped to take on this new role,” David Huffstutler, president and chief executive officer of St. David’s HealthCare, said. “I look forward to the many contributions he will make to further advance the great work at St. David’s Georgetown Hospital.”
Prior to his time at St. David’s South Austin Medical Center, Landry served as vice president of operations at St. David’s Medical Center, where he successfully led multiple service lines, grew the comprehensive stroke center (the highest level of certification for stroke care) and neuroscience program, and served as the facility’s chief staffing officer. He started his career with St. David’s HealthCare as an executive resident, completing rotations with
the healthcare system’s hospital executive teams.
Landry received a bachelor’s degree in sociology from the University of Michigan and earned his master’s degree in health care administration from Trinity University in San Antonio.
Texas Oncology Adds Physicians from Central Texas Colon and Rectal Surgeons to its Colon and Rectal Specialty Division
Eight Physicians Added to Texas Colon & Rectal Specialists, Texas Oncology’s Growing Colon And Rectal Specialty Practice

Texas Oncology announced today that the physicians who practice with Central Texas Colon and Rectal Surgeons will join Texas Colon & Rectal Specialists, the colon and rectal specialty division within Texas Oncology, effective May 1. With the addition of these eight physicians, Texas Colon & Rectal Specialists now has 39 total physicians serving patients at 38 locations in the Austin, Dallas-Fort Worth, San Antonio, Houston, and Amarillo metropolitan areas.
Established in 2008, Central Texas Colon and Rectal Surgeons is the largest group of colon and rectal surgeons in central Texas who are certified by the American Board of Colon and Rectal Surgery, the leading national standards body. Texas Oncology will assume
responsibility for operations at the three current Central Texas Colon and Rectal Surgeons locations, in south, central, and north Austin.
“We are committed to expanding our practice to deliver better colon and rectal care to patients in central Texas by connecting them to our broad network of expert physicians and clinicians,” said Steven Paulson, M.D., president and chairman of the board, Texas Oncology. “High-quality, evidence-based colon and rectal care, including cancer treatment, is a vital healthcare service that we are prioritizing as part of our comprehensive care plan.”
Colorectal cancer is the second leading cause of cancer deaths among men and women combined in the U.S., with more than 12,400 cases diagnosed last
year in Texas.
“Central Texas patients will benefit from our joining Texas Colon & Rectal Specialists by giving them access to even more resources, expertise, and opportunities for enhanced care,” said Thiru Lakshman, M.D., president, Central Texas Colon and Rectal Surgeons. “We will continue to provide the same high level of comprehensive care for all types of colorectal diseases, both benign and malignant. We are proud to join an established, innovative provider of high-quality colon and rectal care that includes leading edge oncology care.”
The addition of the Central Texas Colon and Rectal Surgeons physicians to Texas Colon & Rectal Specialists provides patients more opportunities to participate in groundbreaking clinical trials
and research, with a physician team that is active in research, as well as ongoing training in advancements in the treatment of complex colon and rectal diseases and disorders.
Texas Colon & Rectal Specialists is part of Texas Oncology’s surgical group, which includes more than 130 surgeons with specialties in breast, gynecologic oncology, urology, colon and rectal, neuro-oncology, thoracic, and surgical oncology. Texas Oncology surgeons performed more than 152,000 procedures last year.

Austin Medical Times Page 8 May 2023 austinmedtimes.com
Kyle Landry



















Austin Medical Times Page 9 May 2023 austinmedtimes.com
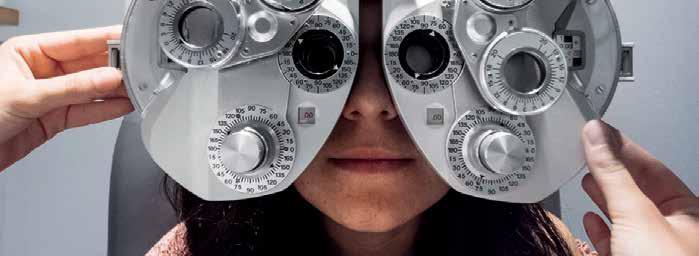
AI Can Spot Early Signs of Alzheimer’s in Speech Patterns, Study Shows
O’Donnell Brain Institute Researcher Says Findings May Lead to A Simple Screening Test for Early Detection of Cognitive Impairment

New technologies that can capture subtle changes in a patient’s voice may help physicians diagnose cognitive impairment and Alzheimer’s disease before symptoms begin to show, according to a UT Southwestern Medical Center researcher who led a study published in the Alzheimer’s Association publication Diagnosis, Assessment & Disease Monitoring.
“Our focus was on identifying subtle language and audio changes that are present in the very early stages of Alzheimer’s disease but not easily recognizable by family members or an individual’s primary care physician,” said Ihab Hajjar, M.D., Professor of Neurology at UT Southwestern’s Peter O’Donnell Jr. Brain Institute.

Researchers used advanced

machine learning and natural language processing (NLP) tools to assess speech patterns in 206 people – 114 who met the criteria for mild cognitive decline and 92 who were unimpaired. The team then mapped those findings to commonly used biomarkers to determine their efficacy in measuring impairment.
Study participants, who were enrolled in a research program at Emory University in Atlanta, were given several standard cognitive assessments before being asked to record a spontaneous 1- to 2-minute description of artwork.
“The recorded descriptions of the picture provided us with an approximation of conversational abilities that we could study via artificial intelligence to determine
speech motor control, idea density, grammatical complexity, and other speech features,” Dr. Hajjar said. The research team compared the participants’ speech analytics to their cerebral spinal fluid samples and MRI scans to determine how accurately the digital voice biomarkers detected both mild cognitive impairment and Alzheimer’s disease status and progression.
“Prior to the development of machine learning and NLP, the detailed study of speech patterns in patients was extremely labor intensive and often not successful because the changes in the early stages are frequently undetectable to the human ear,” Dr. Hajjar said. “This novel method of testing performed well in detecting those with mild cognitive impairment and more specifically in identifying patients with evidence of Alzheimer’s disease – even when it cannot be easily detected using standard cognitive assessments.”
During the study, researchers spent fewer than 10 minutes capturing a patient’s voice recording. Traditional neuropsychological tests typically
take several hours to administer. “If confirmed with larger studies, the use of artificial intelligence and machine learning to study vocal recordings could provide primary care providers with an easy-to-perform screening tool for at-risk individuals,” Dr. Hajjar said. “Earlier diagnoses would give patients and families more time to plan for the future and give
see Alzheimer ...page 13
Austin Medical Times Page 10
cookie delivery cookie delivery
cookies,
cookiedelivery.com
Warm
delivered.
Dr. Ihab Hajjar holds the Pogue Family Distinguished University Chair in Alzheimer’s Disease Clinical Research and Care, in Memory of Maurine and David Weigers McMullan.

Austin Medical Times Page 11 May 2023 austinmedtimes.com
Single-Dose Nasal Spray Could Soon Treat Traumatic Brain Injury
 By Ann M. McKelvey
By Ann M. McKelvey
Researchers at the Texas A&M University School of Medicine are working to combat the severe outcomes of traumatic brain injury, also called TBI, with a non-invasive therapeutic they believe could prevent the cycle of neuroinflammation that leads to long-lasting complications.
TBI has been at the forefront of public attention in recent years. More than 50 million TBI cases occur annually, creating a global financial burden of $70 billion and making TBI a major health problem. In America, more than 611 TBI-related hospitalizations occur per day. The hallmarks of mild to moderate TBI are progressive cognitive decline and changes in mood resulting in long-term behavioral impairments, including the development of mental disorders in surviving patients. These devastating outcomes have fueled
researchers’ investigations into how to resolve the long-lasting issues that follow TBI.
Chronic neuroinflammation and long-term TBI symptoms
The devastating outcomes of TBI have been linked to a condition that develops in the brain after TBI called chronic neuroinflammation. Prior work has identified the actors in this inflammatory process, which include a specific type of central nervous system cell called microglia, or resident immune cells of the brain. After a person sustains a TBI, these cells become activated as a response to neuron death. While such activation is beneficial for removing cellular debris in the acute phase after TBI, their unrelenting activation, called chronic neuroinflammation, adversely affects brain function. These cells begin a mechanism that works through the signaling system p38/MAPK, known for communicating external stimuli into the
Age Well, Live Well Aging Unbound –Celebrating Older Americans Month
By Chelsea Couch HHSC Texercise Coordinator
May is Older Americans Month
and the 2023 theme, “Aging Unbound,” highlights diverse aging experiences, combats ageist stereotypes and showcases how we all benefit when older adults are supported to remain engaged, independent and included.
Texas has one of the fastest-growing populations of older adults, and older Texans are a vital
element in what makes Texas the diverse, strong state it is. According to the 2018 Texas Population Projections Data Tool, Texas has the third largest population of adults age 50 and older. In 2020, Texas had 9 million adults age 50 and older, and that population is projected to grow 82% to 16.4 million by 2050.
The Texas Health and Human Services Commission (HHSC) Age Well Live Well (AWLW) campaign assists older adults, their caregivers

body. Hyperactivation of this pathway in microglia leads to a continuous release of multiple pro-inflammatory molecules, which then affect and degrade neuronal function, leading to brain tissue loss and myriad symptoms.
Previous work has explored using mesenchymal stem cells (MSCs) as a means for modulating the responses of the immune system. These cells can self-renew and are capable of developing into various types of cells. Beyond this capacity, MSCs can also secrete anti-inflammatory cytokines and other molecules that directly modulate the inflammatory response of the immune system through receptors on their cell surfaces that sense the presence of pro-inflammatory molecules. Using stem cell-derived extracellular vesicles to combat chronic neuroinflammation
Researchers in the laboratory of Ashok K. Shetty, PhD, professor and associate director of the Institute for Regenerative Medicine and professor in the Department of Cell Biology and Genetics at the Texas A&M School of Medicine, capitalized on research into the field of extracellular vesicles (EVs) as a means of solving the question of how to prevent the cycle of neuroinflammation from the beginning.
Shetty said using stem cell-derived EVs to combat neuroinflammation
after TBI stems from their potent anti-inflammatory effects noted in cell culture assays and other disease models. EVs are nanosized vesicles, essentially a means of transporting cellular cargo, such as proteins, lipids, microRNAs (miRNAs), and DNA, to targeted cells. To understand the capabilities of EVs, Shetty’s group used small RNA sequencing on EVs shed from MSCs. The findings from the sequencing showed at least eight miRNAs capable of specifically inhibiting the inflammatory processes that have neuroprotective or brain repair capabilities. These miRNA molecules within EVs are released when they come in contact with target cells.
“Remarkably, EVs shed by MSCs are naturally enriched with miRNAs capable of inhibiting the various processes that lead to chronic neuroinflammation after TBI,” said Maheedhar Kodali, research scientist at
see Brain Injury ...page 13
and their communities to prepare for aging. This statewide healthy aging campaign promotes easy pathways to available resources and emphasizes how to make healthy changes using three core message areas: Be Healthy, Be Connected and Be Informed. Explore AWLW and other aging resources by visiting the Aging Well Resources Order Form. Texas HHSC has a variety of resources to support healthy aging. These include:
• Aging Texas Well is a strategic planning effort that reviews policies impacting older Texans, assesses local and state readiness to meet the needs of older adults, and helps communities build their service capacity. The Aging Texas Well strategic plan uses the Older Americans Act impact areas as a foundation to plan for aging needs and identifies aging specific priorities for the state.
• Texercise is a health promotions initiative that provides free physical activity and nutrition resources to educate, motivate and engage adults age 45 and
older in healthy behaviors. To learn more, visit the Texercise website.
• The Supplemental Nutrition Assistance Program assists people with buying the food they need for good health. To learn more, visit the SNAP website.
• Area Agencies on Aging provide older adults, their families and caregivers with nutrition services, including home and congregate meals as well as evidence-based fitness programs. To connect with the nearest AAA, call Texas HHS at 800-252-9240.
• Aging and Disability Resource Centers are part of the No Wrong Door System and help streamline access to long-term services and support for the whole family. To learn more, call Texas HHS at 855-937-2372.
When older Texans are engaged in healthy behaviors, have opportunities to stay socially connected and are informed of aging resources, they can age unbound and live well.
Austin Medical Times Page 12 May 2023 austinmedtimes.com
A Single Intranasal Dose of Anti-Inflammatory Stem Cell-Derived Extracellular Vesicles Is A Promising Means of Treating Traumatic Brain Injury
Liver Transplant
Continued from page 4
The surveys showed that although 85% in the early survival period (one year or less) had high post-traumatic growth, only about 15% of late survivors (between five and 10 years) had the same characteristic. High resilience was reported in only about 33% of survivors and was associated with relatively high income.
Military Spouses
Continued from page 7
“The ultimate goal is to improve spouses’ sense of social and community support, self-care practices, mental health and quality of life,” said study principal investigator Elisa Borah, director of the institute and research associate professor at the Steve Hicks School of Social Work. “This research will examine the extent to which group-based peer support led by trained, peer military spouse leaders gets us closer to that goal.”
“In addition to extended
Alzheimer
Continued from page 10
clinicians greater flexibility in recommending promising lifestyle interventions.”
Dr. Hajjar collaborated
Brain Injury
Continued from page 7
the Institute for Regenerative Medicine and the first author of the research article. Their work was published in the February 2023 issue of the journal Brain Behavior and Immunity.
Developing a single-dose nasal spray for TBI patients
Using an animal model of moderate TBI to explore the therapeutic relevance of the miRNA component of the EVs in the acute phase of injury, the laboratory non-invasively administered the EVs by choosing the intranasal route. Within six hours of delivery, the EVs had already been incorporated within neurons and microglia throughout the entirety of the brain. Of particular note is that the
Lower resilience was seen among patients with longer hospital stays and later survival stages. Patients who reported a lower ability to cope after transplant were more likely to be 65 or older, non-Caucasian, have less education, or needed a transplant for nonviral liver disease. Dr. Lieber said about 25% of liver transplant survivors had clinically significant anxiety and depression, more frequent among early survivors and women with pre-transplant mental health disorders.
separation, numerous moves, single parenting, relationship strains and challenges in caring for their spouse’s health concerns, military spouses may also struggle to establish careers or finish educational degrees due to the unpredictable nature of military life,” said Borah, whose research is focused on developing, testing and effectively implementing mental health treatments and social supports for military-connected adults.
Potential to Scale Across the Armed Forces
This year, UT’s new three-year study will begin recruiting Army spouse participants at Fort Hood, Texas – the largest active-duty armed post in the U.S. Armed Forces – with
on this study with a team of researchers at Emory, where he previously served as Director of the Clinical Trial Unit of the Goizueta Alzheimer’s Disease Research Center before joining UTSW in 2022. He is continuing to collect
various components of the microglial cell’s inflammasome—a multi-protein complex formation facilitating robust inflammatory response—were significantly reduced by treatment. As Shetty describes, “Inflammasomes are the mediators of neuroinflammation, and their persistence leads to chronic neuroinflammation through unrelenting hyperactivation of p38/ MAPK signaling.”
A major component of moderate TBI, however, is the chronic and ongoing symptoms that follow the injury itself. Using a similar animal model, the group used behavioral analyses to study animal models 63 days after brain injury. They observed that the activity of the inflammasome was linked to higher levels of anxious and depressive-like behavior, as well as more difficulty in cognitive processes such as discerning
These characteristics could help predict clinical outcomes, she said. For example, anxiety and depression, the ability to cope, and resilience have been shown to predict how well a patient can self-manage care and interact effectively with the health system for other chronic diseases, and are important predictors for quality of life and functioning, such as the ability to return to work and engage in daily activities. Dr. Lieber and her colleagues plan to continue to study other facets of survivorship in
the goal to support 150 spouses. If this group support intervention proves effective, Borah expects to scale the model across other Army locations, with the potential to affect the lives of many thousands of spouses.
“Being a part of a program like this helps you create an instant family,” said Megoulloa. You’ve got people telling you what to be careful about and how to prepare in a new place where you don’t even know what you need to be worried about.”
The Military Spouse Resiliency Group Program was adapted from the Veteran Spouse Resiliency Group, a support model operating within the university’s Veteran Spouse Network. The newer program is tailored
voice recordings in Dallas as part of a follow-up study at UTSW being funded with a National Institutes of Health grant.
This study’s research was supported by grants from the National Institutes of Health/
minor changes in the environment required for encoding location memory, and pattern separation, a process by which a region of the brain called the hippocampus transforms similar inputs into distinct patterns or representations for encoding memories. Yet, treating TBI animal models with intranasal EVs prevented chronic activation of the inflammatory response that occurs through the p38/MAPK system.
“Notably, such EV treatment in the acute phase of TBI maintained better long-term cognitive function and alleviated anhedonia, a depressive condition in which individuals with TBI find it difficult to experience pleasure from activities that were pleasurable before suffering from TBI,” Shetty said.
As most clinical trials testing the efficacy of anti-inflammatory drugs have shown either no or limited
liver transplant patients, such as how these variables change over time, which could help researchers develop tailored interventions to improve clinical outcomes and quality of life.
“High-quality care of patients after liver transplant includes treating the whole person,” Dr. Lieber said. “Survivorship research informs how we develop and implement interventions to help our transplant community.”
specifically to active-duty spouses, whose experiences during and after military life can be vastly different.
As part of Dell Med and the Steve Hicks School of Social Work, the Institute for Military and Veteran Family Wellness serves as a hub for researchers and community members to work together to develop programs and practices needed by service members, veterans and their family members. The institute partners with local and national providers, researchers, and military and veteran community members who are committed to ensuring that military communities have access to effective care for their mental health and community-based needs.
National Institute on Aging (AG051633, AG057470-01, AG042127) and the Alzheimer’s Drug Discovery Foundation (20150603).
effectiveness in preventing long-lasting cognitive and mood problems after mild to moderate TBI, an intranasal spray of stem cell-derived EVs could provide a new avenue for treating TBI in the near future, Shetty said.
The scientific strategy employed in this work highlighted the importance of not only preventing acute inflammation, but also stopping chronic inflammatory cascades. The single-dosage treatments may indeed point the TBI research field in an exciting new direction. Shetty envisions a future where civilian and military personnel who incur a mild to moderate TBI due to contact sports, motor vehicle accidents, and combat get a nasal spray of stem cell derived EVs as soon as they are taken to the emergency room.
Austin Medical Times Page 13 May 2023 austinmedtimes.com
Rising Risks
Continued from page 1
the zero-tolerance harassment policy. This can be achieved in employee onboarding documentation, professional employment contracts, conditions of treatment or admission, third-party vendor agreements, website notices, and office signage.
Be Sure You’re Covered
Consult with your personal or corporate attorney to understand the potential financial risks of claims involving allegations of sexual harassment or misconduct. Confer with your insurance agent or broker to determine proactively what coverages might be available in your state in the event of such a claim.
Policy language and state regulatory requirements can vary among jurisdictions. Although most
Data Risk
Continued from page 3
• Disaster recovery/business continuity. If the vendor experiences a major interruption in business, how long will it need to recover? This is particularly important to infrastructure vendors
• Insurance. Does the vendor have sufficient insurance in place that will make you whole in the event the vendor experiences a data breach? Is the vendor properly capitalized to stand behind its liability?
• Liability. What is the minimum liability your company will be comfortable with accepting in the event of a vendor’s data breach or breach of the ISA? The vendor’s liability for breaches must be higher or uncapped for regulated
Oncology Research
Continued from page 5
is recommended to consult with a physician before starting an exercise program during or after cancer treatment.
Gardening is another great activity to enjoy outside. Not only does it add beauty to one’s surroundings, but it enables people to commune with nature, work out frustrations, and grow fresh food to nourish their bodies. Gardening improves mood and increases self-esteem, and when
practitioners carry professional liability coverage in the event of a malpractice claim, it is not uncommon for professional liability policies to specifically exclude coverage for acts of sexual misconduct committed by a practitioner against a patient. Depending on the professional liability carrier, the practitioner may be provided with a courtesy defense covering the costs of legal fees and expenses, but no payment for any indemnity incurred would be paid in the event of an adverse jury verdict or arbitration award.
It is also prudent to consult with insurance brokers and agents about the availability of employment practices liability insurance (EPLI). EPLI may provide coverage for certain types of workplace harassment, including sexual misconduct involving the policyholder and an employee.
And finally, as noted above,
businesses.
IV. The vendor management process
A. Prework.
1. Establish written criteria that define when vendors will be required to sign an ISA (i.e., when the vendor will have access to your data, infrastructure or network).
2. Work with the legal and information security teams to draft a form ISA.
3. Establish written parameters for tolerance on vendor-requested changes to the ISA.
B. Internal rollout.
1. Educate internal stakeholders about the ISA, its purpose and its effectiveness.
2. Modify the company’s internal process so that an ISA is now provided to any new vendor that meets the established criteria.
3. Establish who has authority within the organization to approve
people spend time in a garden, anxiety levels can drop and feelings of depression lessen.
Protecting your skin from the sun
As spring turns to summer and people venture outside more, it is important to protect your skin from the sun’s ultraviolet (UV) rays, which is the number one cause of skin cancer. Also, many treatments for cancer can increase the sensitivity of skin to sunburn. The American Cancer Society suggests the following tips to stay “sun safe”:
• Stay in the shade and limit your direct exposure to the sun between 10 a.m. and 4 p.m.
claims of inappropriate sexual behavior against a licensed healthcare practitioner may result in administrative proceedings by a state licensing board or the privileges committee of a healthcare facility. Endorsements to pay legal defense costs are widely available as part of professional liability policies in the event of an administrative investigation or subsequent disciplinary hearing. Contact your agent or broker to explore your coverage options.

The guidelines suggested here are not rules, do not constitute legal advice, and do not ensure a successful outcome. The ultimate decision regarding the appropriateness of any treatment must be made by each healthcare provider considering the circumstances of the individual situation and in accordance with the laws of the jurisdiction in which the care is rendered.
vendor-requested deviations to the ISA.
C. External rollout.
1. Send the ISA to vendors with clear messaging that explains the ISA’s purpose and relationship to other legal documents.
2. Create a process for the receipt of vendor changes and establish who will negotiate with the vendor.
3. Establish a repository of ISAs that can be called on easily when there is an issue with the vendor.
V. Conclusion
Facing a regulatory body or your customers after you experience a data breach will be less painful when you can point to a comprehensive, all-encompassing vendor management process. And the process will be even less painful when you can get relief from the vendor that is responsible for the breach instead of paying out of your own pocket.
• Wear protective clothing, sunglasses, and a wide-brimmed hat to cover as much skin as possible. Use a broad-spectrum sunscreen with an SPF of at least 30, reapplying at least every two hours Being outdoors can make cancer patients and caregivers feel freer, more grounded, and connected to nature. Taking the time to spend just a few moments outside each day with a thoughtful presence helps the body refuel and diminish stress, bringing a sense of calm to a whirlwind of emotions and feelings while navigating cancer.
Austin Medical Times Page 14 May 2023 austinmedtimes.com Published by Texas Healthcare Media Group Inc. Director of Media Sales Richard W DeLaRosa Senior Designer Jamie Farquhar-Rizzo Web Development Lorenzo Morales Distribution Brad Jander Accounting Liz Thachar Office: 512-203-3987 For Advertising advertising@ medicaltimesnews.com Editor editor@medicaltimesnews.com Austin Medical Times is Published by Texas Healthcare Media Group, Inc. All content in this publication is copyrighted by Texas Healthcare Media Group, and should not be reproduced in part or at whole without written consent from the Editor. Austin Medical Times reserves the right to edit all submissions and assumes no responsibility for solicited or unsolicited manuscripts. All submissions sent to Austin Medical Times are considered property and are to distribute for publication and copyright purposes. Austin Medical Times is published every month P.O. Box 57430 Webster, TX 77598-7430
KEEPING NEW MOMS AND MOMS-TO-BE SAFE AND HEALTHY
A healthy pregnancy is best for both mom and baby. Pregnancy and childbirth can put a woman’s health at risk, but many pregnancy-associated deaths can be avoided.
BEFORE GETTING PREGNANT
It’s important to understand your medical risks and to get as healthy as possible before pregnancy. Talk to your health care team about:
• Whether you have any signs of heart disease
• Your family health history
DURING PREGNANCY
• Visit a health care provider regularly
• Take medication as prescribed
IN AND AROUND DELIVERY
• Watch for changes and take action
• If you have concerns about your health or the health of your baby, consult your health care provider
AFTER DELIVERY
• Make your health a priority
• Get continued medical care
• Inform new health care
• Your blood pressure
• Whether you should lose or gain weight, and if so, how Getting 150 minutes of physical activity per week
• Healthy eating
• Sodium in your diet
• Whether prenatal vitamins
• Reduce stress and manage anxiety
• Monitor weight gain
• Avoid unhealthy habits such as smoking, alcohol and
immediately
• Some complications show up days after delivery
• Heart Rate and blood pressure normally decrease within 48 hours postpartum
• Blood pressure may increase
providers about the pregnancy
• Monitor your mental health
• Find ways to be active
are recommended
• Quitting any unhealthy substances, such as tobacco, alcohol, and
• marijuana or other drugs
• Safety in your home environment
illegal drugs
• Follow extra precautions if you’re older than 35
again 3-6 days later due to fluid shifts.
• During this period, you should be monitored for complications.
• Find time to sleep
• Eat nutritious food
• Rely on a support network







LEARN THE WARNING SIGNS
It’s important for you to stay on top of your own health. Many heart-related problems can happen in the days and weeks after delivery — even up to a year later. Some symptoms, such as fatigue and mild pain, are expected after childbirth. But strange or sudden changes may be a sign of stroke, heart problems or other dangerous conditions. Seek medical care right away if you have any worrisome symptoms during or after pregnancy, including:
• Severe or worsening headache
• Blurred vision or other vision changes

• Feeling dizzy, faint or disoriented
• A fever over 100.4 F
• Extreme weakness or fatigue
• Vaginal bleeding or foul discharge
• Abdominal pain
• Chest pain or racing heart

• Rapid or labored breathing
• Severe nausea or vomiting
• Unusual swelling of hands or face
• Redness, pain or swelling in arms or legs
• A slowing or stopping of fetal movement
• Severe anxiety or depression


• Thoughts of harming yourself or your child
• General ill feeling
Austin Medical Times Page 15 May 2023 austinmedtimes.com
©2023 American Heart Association, Inc., a 501(c)(3) not-for-profit. All rights reserved. Go Red for Women is a registered trademark of AHA. The Red Dress Design is a trademark of U.S. DHHS. Unauthorized use prohibited.
Austin Medical Times austinmedtimes.com
 By Richard Cahill, JD, Vice President and Associate General Counsel The Doctors Company
By Richard Cahill, JD, Vice President and Associate General Counsel The Doctors Company



 By
By






























 By Ann M. McKelvey
By Ann M. McKelvey