Breast Cancer Surgery: What Are My Options?
By Liza O. Thalheimer, M.D., FACS, Texas Breast Specialist

When a woman is diagnosed with breast cancer, a million thoughts run through her head. What type of breast cancer do I have? How quickly is it growing? Has the cancer spread? Will I lose one or both of my breasts?
All of this can have a profound impact on the treatment decisions a woman makes – especially in cases where breast surgery may play a pivotal role in their overall treatment plan. In fact, surgery is one of the primary treatments for breast cancer and is used:
• As a diagnostic and treatment tool to determine the cancer’s growth and progression
• To relieve symptoms found in advanced stages
• To cosmetically reconstruct the breast(s) after cancer surgery








• To reduce breast cancer risk for those with higher risk, such as women with an immediate family member who has had breast cancer, or those whose genetic tests indicate a mutation that conveys a high risk of breast cancer

Excluding skin cancers, the World Health Organization reports that breast cancer is the most common form of cancer worldwide. In Texas, over 21,000 women are expected to face a new diagnosis of breast cancer in 2022, according to the American Cancer Society.


How to decide which breast surgery is right for you Surgery for breast cancer depends on several factors including the size and location of the tumor(s),
stage of cancer, treatment options, and individual goals and preferences. While surgery will not fully treat metastatic breast cancer, it can be helpful to treat one site with significant symptoms.
Common surgical procedures used to treat breast cancer include breast-conserving surgery and mastectomy.
• Breast-conserving surgery, also referred to as a lumpectomy, quadrantectomy, or partial mastectomy, removes the area of cancerous tissues from the breast without removing the entire breast.
• Mastectomy is the surgical removal of an entire breast. It is usually performed when a patient cannot be treated with lumpectomy. In some cases, mastectomy will be the most appropriate or only option due to the type of breast cancer, tumor size, location of the tumor in the breast, or previous radiation treatment in the area. Some women may have both breasts removed in what is called a double mastectomy. If the cancer does not involve the nipple, a nipple sparing mastectomy may be
performed. An oncoplastic partial mastectomy is another option, which removes the cancer and reconstructs the tissue and breast.
Additional procedures include sentinel lymph node biopsy, lymph node dissection also known as a lymphadenectomy, and breast reconstruction surgery, which can be part of treatment after breast-conserving surgery or mastectomy. Is breast reconstruction required after a mastectomy?
The impact of breast cancer and its treatment is an important part of every patient’s cancer experience. The loss of one or both breasts may change a woman’s self-perception or body image. This can be a factor for patients deciding if breast reconstruction surgery is right for them. Some women decide to not proceed with reconstruction.
Many women who have a mastectomy choose to have breast reconstruction to restore the breast’s appearance. This procedure rebuilds the shape and appearance of the breast using saline or silicone implants, or tissue moved from elsewhere in the body. In some cases, after a
Serving Harris, Brazoria, Fort Bend, Montgomery and Galveston Counties October Edition 2022Volume 12 | Issue 10 see Breast Cancer...page 14 HOUSTON
PRSRTSTD USPOSTAGE PAID PERMITNO1 HOUSTONTX Memorial Hermann Southwest Hospital Provides Specialty Care for Houston Seniors See pg. 9 Inside This Issue Culinary Medicine Programs Aim To Improve Nutrition Education for Doctors See pg. 10 INDEX Legal Matters pg.3 Mental Health pg.4 Healthy Heart pg.7 Financial Forecast pg.11
IS IT TIME TO EXAMINE your malpractice insurance?
Unlike other Texas medical liability insurers, which are investor-owned companies, The Doctors Company remains fiercely independent and dedicated to your interests. Ask yourself, “Do I want an insurer founded by and for physicians that’s guided by my peers? Or do I want a profit-focused insurer that’s directed by Wall Street?”
Join us and discover why delivering the best imaginable service and unrivaled rewards is at the core of who we are.
Houston Medical TimesPage 2 medicaltimesnews.comOctober 2022
7990_TX_HoustonMedTimes_NORCAL_Jun2021_v4.indd 1 5/13/21 3:10 PM
Legal Matters
CO-Location and The Provider-Based Rules –No News Is…Good News?




 Sarah Kocher, J.D. Polsinelli, PC
Sarah Kocher, J.D. Polsinelli, PC


Provider-Based rules. Further, although there is some overlap, the CoPs and Provider-Based rules have distinct sets of requirements for compliance, as well as distinct penalties for failure to comply.
CMS recently released the 2023 Outpatient Prospective Payment System proposed rule (“OPPS Proposed Rule”), with notable provisions such as enrollment and payment policies for the newly established “rural emergency hospital” provider type. Also notable is a topic that is not addressed in the OPPS Proposed Rule – co-location. The OPPS Proposed Rule does not include any discussion of, or even nod to, the status of co-location
The CoPs and Provider-Based rules do not directly address co-location, but for nearly a decade, CMS interpreted the CoPs and Provider-Based rules as prohibiting a hospital from sharing nearly any space with another health care provider. Then, in November 2021, CMS issued final updates to the Medicare State Operations Manual, laying out a pathway for co-location under the general acute care hospital CoPs. Despite this opening under the CoPs, there has been no counterpart CMS guidance regarding co-location under the Medicare Provider-Based
THE NEW OLD WAY
under the Medicare Provider-Based rules. For hospitals attempting to create an effective strategy around co-location, and that have been riding a rollercoaster of CMS guidance on this topic, the lack of concrete guidance is likely frustrating…but no news may ultimately be good news for hospitals. An Overview of Co-Location. Co-location can take a range of forms, but generally occurs when a Medicare provider such as a hospital shares space with another healthcare entity. CMS regulates co-location under two primary sets of rules and guidance: (1) Medicare Conditions of Participation (“CoPs”) and (2) Medicare Provider-Based rules.
The distinction between the CoPs and the Provider-based rules is important. CoP and Provider-Based guidance come from separate divisions within CMS – the CMS Quality, Safety & Oversight Group, for updates and guidance relating to the CoPs, and the CMS Payment Policy Group, for updates and guidance involving the
rules. And with the lack of any discussion around co-location in the OPPS Proposed Rule, CMS is not engaging in formal rulemaking regarding co-location under the Provider-Based rules at this time. But where does this leave hospitals? The Status of Co-Location and the Provider-Based Rules.
Although CMS has not issued any recent guidance regarding co-location under the Provider-Based rules, there have been adjacent developments at the federal level that will likely impact any position that CMS ultimately takes. First, in Azar v. Allina Health Services, the United States Supreme Court held that CMS must utilize notice-and-comment rulemaking when establishing a “substantive legal standard” that would govern the scope of Medicare benefits, payment conditions, or eligibility to furnish services. In follow-up to Allina, on December 3, 2020, the Office of the General



Houston Medical Times Page 3 medicaltimesnews.com October 2022
see Legal Matters...page 14 Distinguished By Design We believe that elegance should weave through your every day, carrying unexpected moments where you discover what living well means to you. 2511 WILLOWICK RD HOUSTON, TX 77027 713.597.5022 novelriveroaks.com
At NOVEL River Oaks, elegant traditions marry the modern under canopied live oaks and manicured hedges. You can embody old traditions and embrace your own at this enchanting place.
Mental Health
DBS Is an Increasingly Viable Option for Patients with Treatment-Resistant OCD, New Study Shows
In the fight against treatment-resistant obsessive-compulsive disorder (OCD), one option, deep brain stimulation (DBS), is slowly gaining popularity since its inception nearly 20 years ago. DBS works similarly to a pacemaker and is used to treat certain neurological and psychiatric disorders.

As the use of DBS to alleviate OCD continues to increase, a group of researchers led by a team at Baylor College of Medicine sought to understand the efficacy of the treatment by using data collected from earlier studies. The group’s research, recently published in the Journal of Neurology, Neurosurgery, and Psychiatry, provides evidence that DBS can improve OCD as well as other related depression symptoms in certain patients.
“This paper is what we call a systematic review and meta-analysis, which is a methodology that takes all of the literature that is available so far
and rigorously analyzes it,” explains contributing author Dr. Sameer Sheth, associate professor, Cullen Foundation Endowed Chair, McNair Scholar and vice chair of research in the Department of Neurosurgery at Baylor.
“The advantage to doing so is that while we perform more DBS cases for OCD than other places in the country, with meta-analysis, we are taking scores of cases from around the country and around the world and synthesizing all the information so we can have a better, more general understanding of what this therapy does in an even larger group of patients.”
By opening the pool of data surveyed in the study to include evidence from the world, the researchers were able to provide a zoomed-out view of DBS case results and also were able to account for potential biases from smaller studies.
Baylor medical student Ron
Gadot explains the methodology used by the group. “As many of the studies regarding this established but underutilized therapy have incorporated small samples with varying methodologies, we performed novel sensitivity analyses that show that the demonstrated outcomes are not biased by small study effects. Our rigorous risk of bias analyses provides a foundation for crucial discussions regarding the optimization of study methodology going forward.”
Of the 34 included studies, which included a total of 352 patients, 66% of patients fully responded to the DBS at last follow-up. Dr. Wayne Goodman,

Hip or knee pain?
Mako SmartRobotics™
professor and D.C. and Irene Ellwood Chair for the Menninger Department of Psychiatry and Behavioral Sciences, summarizes the group’s findings. “DBS is a viable option for treatment-resistant OCD that can be expected to produce significant clinical benefit in about two out of three cases. [This study] offers hope for patients with severe symptoms of OCD whose disorder did not respond to a range of conventional therapies.”
Though DBS for OCD has been an approved therapy by the U.S. Food and Drug Administration since 2009, very few individuals who could benefit
Houston Medical TimesPage 4 medicaltimesnews.comOctober 2022 IMPORTANT INFORMATION All surgery carries risk. Talk to your doctor to see if joint replacement is right for you. MKOSYM-PM-16_24378 Copyright © 2020 Stryker Learn more at houstonmako.com
for joint replacement helps you get back to the things you love, quicker.
see Mental Health...page 14
Our breast care experts all specialize in one thing:


Texas Breast Specialists provide leading edge surgical approaches and integrated care that includes a multidisciplinary team. From five dedicated breast surgeons in the Houston area to our experts in medical and radiation oncology, genetic risk evaluation, and supportive care, we compassionately collaborate with you to better understand your disease and develop a personalized surgical treatment plan.
Diana M. Hook, M.D. The Woodlands
Cinthya Yabar Lowder, M.D. Kingwood, The Woodlands
Stacia S. Pfost, M.D. Houston, Sugar Land
To learn more, please visit
Jennifer R. Sasaki, M.D., M.S. Houston, Webster
Jamie E. Terry, M.D., MHCE, FACS Houston, Katy, Pearland
Liza O. Thalheimer, M.D., FACS
Houston, Cypress, Tomball
Houston Medical Times Page 5 medicaltimesnews.com
TexasBreastSpecialists.com.
TXO-4723 TBS Houston Medical Times Oct 22_10x13.0405.indd 1 9/27/22 10:10 AM
UT Southwestern Geneticists Identify New Mechanism for Nonalcoholic Fatty Liver Disease Absent Obesity

Using a genetic screening platform developed by a UT Southwestern Nobel Laureate, scientists with the Center for the Genetics of Host Defense at UT Southwestern Medical Center have identified genetic mutations that contribute to nonalcoholic fatty liver disease (NAFLD), providing a potential future target for therapeutic interventions.
While obesity and diabetes are well-known risk factors for fatty liver disease, the UT Southwestern researchers were able to identify a new cause of fatty liver disease absent obesity – a reduction in the level of Predicted gene 4951 (Gm4951), which in turn leads to non-alcoholic fatty liver disease. Currently there are no approved medications or treatments for the disease, which is rapidly emerging as a major cause of chronic liver disease
in the United States. Identifying the role of this gene in development of the disease provides important new direction for those studying the disease to find potential treatments.
“We identified a rare non-obese mouse model of NAFLD caused by GM4951 deficiency. This study lays the groundwork for the future development of approaches to activate the human Gm4951 homolog to combat NAFLD,” said lead author Zhao Zhang, Ph.D., Assistant Professor in the Center for the Genetics of Host Defense and the Division of Endocrinology in Internal Medicine. The findings appear in Nature Communications.
The Center for the Genetics of Host Defense is directed by Bruce Beutler, Ph.D., a Regental Professor and one of four Nobel Laureates at UT Southwestern. Dr. Beutler received
JUSTOPENED!
PROUD TO SERVE HOUSTON’S MEDICAL CENTER




the 2011 Nobel Prize in Physiology or Medicine for discovering an important family of receptors that allow mammals to sense infections when they occur, triggering a powerful inflammatory response. Dr. Beutler also developed the largest mouse mutagenesis program in the world, along with a forward genetic screen platform that allows researchers in the Center to screen for more than half of all genes in the mouse genome. Along with a means of instantly identifying mutations responsible for both quantitative and qualitative phenotypes, the program
allows for rapid discovery of many new components of the immune system.
“This study identified a potential human homolog of mouse GM4951 and the interaction of GM4951 with another human NAFLD/NASH associated protein HSD17B13, suggesting the discovery is likely conserved in humans,” said Dr. Zhang, whose lab is working to understand the molecular mechanism of metabolic diseases, with the underlying aim of translating this knowledge into novel

Houston Medical TimesPage 6 medicaltimesnews.comOctober 2022
This dual-branded property is owned and operated by American Liberty Hospitality. The new dual-branded Hilton Garden Inn and Home2 Suites, located in the heart of the medical center, combines convenience with state-ofthe-art amenities. Designed to serve medical professionals and the surrounding community, we offer fully furnished extended-stay suites, over 3,000 square feet of flexible meeting space and complimentary shuttle service. • 500-car parking garage • Full-service bar and restaurant • State-of-the-art fitness center • 24-hour business center • On-site guest self-laundry facilities • Heated outdoor pool • Complimentary shuttle to the medical center • Nearby Houston’s medical center, Hermann Park, the Houston Zoo, Museum District and Downtown Houston • Hilton CleanStay program 6840 Almeda Road, Houston, Texas 77030 Located on the Michael E. DeBakey Veterans Affairs Medical Center’s campus. WE’RE AT YOUR SERVICE. hgimedicalcenter.com • 346.433.8200 home2medicalcenter.com • 346.433.8300
Zhao Zhang, Ph.D. (left) and Bruce Beutler, Ph.D. (right)
see Fatty Liver ...page 13
Healthy Heart
Routine Mammograms May Provide Key Insights for Cardiovascular Disease
 By The American Heart Association
By The American Heart Association


Detection of breast arterial calcifications on breast mammograms was associated with a higher risk of cardiovascular disease in postmenopausal women, according to research published in Circulation: Cardiovascular Imaging, a peer-reviewed journal of the American Heart Association journal. According to the study, this finding may be useful to help determine women’s risk for heart disease and stroke.
By screening for breast cancer, mammography has helped save hundreds of thousands of lives. Using the test to also screen for heart disease might someday help save many thousands more. The prospect of leveraging a test that already is so widely administered, without additional cost or radiation exposure, is tantalizing to researchers hoping to
find a new way to fight heart disease.
Cardiovascular disease is the number one killer of women, causing 1 in 3 deaths each year.
Besides revealing masses that may be tumors, digital mammography can reveal buildup of calcium in the arteries in the breast. About 13% of women are estimated to have this buildup, called breast arterial calcification, or BAC, including about 10% of women in their 40s and around half of women in their 80s.
Early studies so far have found BAC’s presence appears to signal an elevated risk for heart attack, stroke and other cardiovascular consequences. Research has begun to reveal a link between calcium buildup in the breast and coronary artery calcification, an established measure that helps predict cardiovascular disease risk.
The analysis found: • Women who had breast arterial
calcification present on their mammogram were 51% more likely to develop heart disease or have a stroke compared with women who did not have breast arterial calcification.
• Women with breast arterial calcification were 23% more likely to develop any type of cardiovascular disease, including heart disease, stroke, heart failure and diseases of the peripheral arteries.


Currently, it is not the standard of care for breast arterial calcification
visible on mammograms to be reported. Integrating this information in cardiovascular risk calculators and using this new information can help improve cardiovascular risk reduction strategies.
“Losing even one woman to heart disease, stroke or breast cancer is too many,” said Erin Asprec, Executive Vice President and Chief Operating Officer of Memorial Hermann Health System and the 2022 Houston Go Red for Women chair.
Houston Medical Times Page 7 medicaltimesnews.com October 2022
see Healthy Heart ...page 14
Medicaid Expansion May Reduce Emergency Department Visits for Non-Emergencies

Analysis Of 80 million Emergency Department Visits Shows a Decrease in Visits For States That Expanded Medicaid Compared To States That Did Not
By Rae Lynn Mitchell
Hospital emergency departments
(EDs) provide lifesaving care for millions of people each year. However, around one-third of ED visits are for conditions that are not emergencies or for conditions that are preventable.
Research has found that a lack of health insurance coverage plays a role in whether a person seeks ED care, and the expansions of state Medicaid programs through the Affordable Care Act could have affected ED visits. However, research has not been fully conclusive and the understanding of how Medicaid expansions affect
different types of ED visits remains unclear.
Results of a new study in the journal JAMA Network Open suggest that expanding Medicaid might reduce ED visits for conditions that could be treated in a doctor’s office. Benjamin Ukert, PhD, assistant professor at the Texas A&M University School of Public Health, and colleagues from the University of South Carolina studied outpatient ED visits between 2011 and 2017, focusing on two states that have expanded Medicaid (New York and Massachusetts) and two states that have not (Georgia and Florida). They analyzed data on more than 80 million
ED visits by 26 million people between the ages of 18 and 64 during the study period.
The researchers measured total ED visits and ED visits broken down into five categories of medical urgency: not preventable and injury-related, emergent but preventable, emergent but primary care treatable, not emergent, and mental health and substance use disorders. In addition, the study included data on gender, race and ethnicity, age, unemployment rate and percentage of the population under 200 percent of the federal poverty level.
Prior research on Medicaid expansions has found increases in
access to primary care and preventive medicine services and decreases in ED visits among those who had faced barriers to care before. However, other studies have found increased ED use following Medicaid expansions due to reduced cost barriers. These seemingly contradictory findings point to the complex relationship between Medicaid expansions and ED visits, which this study aims to clarify by looking into varying degrees of medical urgency.
Ukert and colleagues found that Medicaid expansion was associated
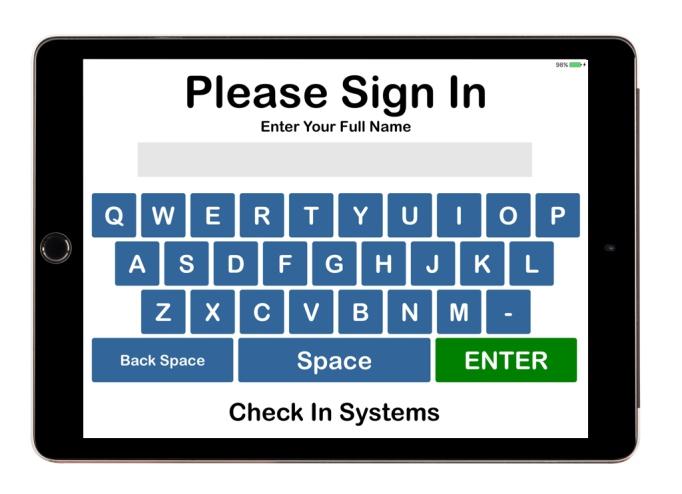
Medical Check In
Patient Sign In Process

Houston Medical TimesPage 8 medicaltimesnews.comOctober 2022
Improving customer service with technology As low as $34 / month 800-971-8871 www.medicalcheckin.com Fast
Organizes Patients by Reason HIPAA Compliant TX-RAMP Certified Unlimited Data Unlimited Support
see Emergency ...page 13
New Unit at Memorial Hermann Southwest Hospital Provides Personalized, Specialty Care for Houston Seniors
Memorial Hermann Southwest Hospital has opened a new acute care unit designed specifically to provide high-quality, holistic and person-centered care for the growing senior population in the Houston area.

The Acute Care for Elders (ACE) Unit is designed to address the challenges older adults often face during hospitalization. Every detail, from the specialized training for care teams to the design of the unit, has been developed to deliver personalized care. The ACE Unit represents a continuation of Memorial Hermann Health System’s commitment to serving older adults – a commitment that also includes a new inpatient hospice care offering at Memorial Hermann Southwest Hospital and
the Silver Trauma Unit at Memorial Hermann-Texas Medical Center
“The senior population is growing rapidly in southwest Houston and throughout the Greater Houston area, which is why the ACE Unit, and others like it, are so important to helping us achieve our vision to create healthier communities,” said Malisha Patel, Senior Vice President and CEO of Memorial Hermann Southwest Hospital and Memorial Hermann Sugar Land Hospital. “We are so pleased to be able to further personalize care for our older adult patients through this new unit.”
Patel says the ACE Unit helps patients and care teams:
• Maintain and improve patients’ health.
• Decrease the need for a transfer to another facility.
• Get patients home sooner.
• Decrease adverse events.
• Increase education about and connection to community resources.
• Reduce overall readmissions.
Recently, the Institute for Healthcare Improvement recognized Memorial Hermann Southwest
Hospital as an Age-Friendly Health System Participant. This honor reflects the hospital’s commitment to deliver on “the 4Ms” of age-friendly care: What Matters Most, Medication, Mentation and Mobility.
Memorial Hermann Southwest
Houston Medical Times Page 9 medicaltimesnews.com October 2022 Start a Healthcare Career in two years or less! Certified Nursing Assistant (CNA) Clinical Medical Assistant (CMA) CPR Dental Assistant Diagnostic Cardiovascular Sonography Adult Echocardiography Vascular Sonography Emergency Medical Services Emergency Medical Technician Emergency Medical Technician - Advanced Paramedic Health Information Management Health Science Medical Office Billing Coding Medication Administration for Nurse Aide Mental Health and Addiction Counseling Neurodiagnostic Technology Nursing Associate Degree Nursing Licensed Vocational Nursing (LVN) LVN – ADN Transition Pharmacy Technician Phlebotomy Technician Polysomnography (Sleep Medicine) Respiratory Care Sports & Human Performance Register today! alvincollege.edu | 281.756.3531 Alvin Community College is an Equal Opportunity Institution.
Photo from Left to Right: Dr. Murad Aslam MD - Clinical Lead Memorial Hermann Medical Group (MHMG); Teal Holden - Senior Vice President, Ambulatory and Primary Care Service Lines - Memorial Hermann Health System; Lavon Washington – Director Hospital Operations, Memorial Hermann Southwest Hospital; Malisha Patel – Senior Vice President and Chief Executive Officer, Memorial Hermann Southwest Hospital and Memorial Hermann Sugar Land Hospital; Toke Ogundiya MSN, RN, CMSRN, OCN, Clinical Manager; Gillian Alexander –Chief Nursing Officer, Memorial Hermann Southwest Hospital; Robert “Chase” Ogden, Jr., CPA - AVP, Finance, Community Hospitals; Cindy Garza, MSN, RN, NEA-BC - Administrative Director, Memorial Hermann Southwest Hospital; Dr. Kristel Poffinbarger MD - Vice President/Regional Chief Medical Officer Memorial Hermann Southwest Hospital & Memorial Hermann Sugar Land Hospital; Brian Kern, MBA, BSN, RN, NEA-BC - Director of Patient Care, Memorial Hermann Southwest Hospital
see Care for Seniors ...page 13
Culinary Medicine Programs Aim to Improve Nutrition Education for Doctors
UTSW Study Shows Medical School Programs Are Expanding but Underfunded
Culinary medicine programs are emerging at medical schools to meet a critical need to improve nutrition education in an era of unprecedented diet-related health problems including obesity and cardiovascular disease, according to a review of programs by UT Southwestern researchers published in Academic Medicine, the journal of the Association of American Medical Colleges.
The programs utilize teaching kitchens to give health professionals practical skills to help patients make evidence-based dietary changes while celebrating nourishing, accessible, affordable, and delicious food, said lead author Jaclyn Albin, M.D., Associate Professor of Internal Medicine and Pediatrics who leads the Culinary Medicine program at UT Southwestern.

“This work is the very first
scoping review of medical school-based Culinary Medicine programs in the U.S.,” Dr. Albin said. “We anticipate this to be a pivotal resource for the many medical schools seeking to launch programs and needing a collated literature base as well as information about funding, assessment strategies, and lessons learned.”
UT Southwestern has been an innovator in this field. Since starting its program in 2015, UTSW’s Culinary Medicine team has delivered interprofessional education in teaching kitchens across Dallas-Fort Worth to medical students, residents, fellows, other health professionals, and patients. More recently, the Culinary Medicine teams launched a clinical service line that delivers virtual consultations with other health care providers. One-on-one visits between
patients and registered dietitians and group cooking classes are expected to begin over the next several months.
To train the next generation of health professionals, Dr. Albin collaborates with dietitian Milette Siler, M.B.A., RD, LD, to lead classes for medical and graduate students, residents, and fellows across the UT Southwestern campus.
“I have always had a passion for teaching students and patients about nutrition, lifestyle, and other

environmental influences on health,” said Dr. Albin. “This has become increasingly complex as more patients face food allergies and intolerances, special dietary or nutritional needs, diseases like irritable bowel syndrome, and much more.”
The researchers identified 34 medical student-focused culinary medicine courses, utilizing a variety of curricular and assessment strategies that
see Culinary Medicine ...page 13
Houston Medical TimesPage 10 medicaltimesnews.comOctober 2022
UTSW’s Culinary Medicine team provides education in teaching kitchens for medical students, residents, fellows and other health professionals
Financial Forecast
Thinking About Starting a Family?
 By Grace S. Yung, CFP Midtown Financial Group, LLC
By Grace S. Yung, CFP Midtown Financial Group, LLC



Many individuals or couples want to build a family. But the process of getting started isn’t so simple. There are potential financial obstacles that you could face.

But the good news is that you have several options for having or adopting a child. So, it is essential to have a plan in place so you can navigate financial challenges.
Understanding Your Options
If you want to raise children – or
tried before in vitro.2
Adoption is another popular option for individuals and couples to start or grow a family. The cost of adoption can vary widely, with some alternatives being $20,000 or more.
The adoption laws can vary from state to state. For instance, in Texas, the birth mother must maintain parental rights for at least 48 hours after giving birth. During this time, she has full parental rights. But after the 48-hour time period has elapsed, the birth mother may place the baby for adoption.3
Some individuals and couples use a surrogate to help them have a baby. With a traditional surrogate, the woman who carries the baby is considered the biological mother
PLAN
PROOF
even have a baby – there are actually many potential options for you. These can include: The natural way, In vitro fertilization, Insemination, Adoption and Surrogacy.
In vitro fertilization typically involves taking eggs that are received via an ultrasound and then placing them in a petri dish with cells. If these become an embryo, it is transferred to a female. This process can be expensive as it runs between $12K -$15K on average and because this method is not usually covered by insurance.1
Insemination refers to the placement of gamete in a woman’s reproductive tract with the goal of pregnancy. Artificial insemination usually costs between $300 and $500 per cycle. Because it is less expensive than in vitro fertilization, it is often
because her egg is used.
The average cost of surrogacy can range from $90,000 to $130,000 depending on the arrangements that are made. The legal requirements and the cost(s) of other services can also vary from one state to another.4
Cost of Raising a Child(ren)
Having a child can change your life in many ways – including financially. So, it is essential to plan ahead. According to the U.S. Department of Agriculture, the average cost of raising a child to age 18 for middle-income parents was $233,610 in 2015. Today it is $272,049.6 the largest expense associated with raising a child is housing, followed by food.
Houston Medical Times Page 11 medicaltimesnews.com October 2022 PRT-00000-0000 Tracking #0-000000 (Exp. 00/00) The Financial Consultants at <DBA Name> are registered representatives with, and securities and advisory services are offered through LPL Financial (LPL), a registered investment advisor and broker-dealer (member FINRA/SIPC). Insurance products are offered through LPL or its licensed affiliates. [Credit Union name] and [DBA name] are not registered as a broker-dealer or investment advisor. Registered representatives of LPL offer products and services using [DBA name], and may also be employees of [credit union name]. These products and services are being offered through LPL or its affiliates, which are separate entities from, and not affiliates of, [credit union name] or [DBA name]. Securities and insurance offered through LPL or its affiliates are: DBA Name Located at Institution Name Agent Name, Desig 1, Desig 2, Desig 3, Desig 4 Title 1 Title 2 or Insurance Lic#xxxxxxxx Address line 1 Address line 2 City, State XXXXX (000) 000-0000 xExt or Description (000) 000-0000 xExt or Description (000) 000-0000 xExt or Description email.address@email.com www.webaddress.com Your Logo Here Not Insured by NCUA or Any Other Government AgencyNot Credit Union GuaranteedNot Credit Union Deposits or Obligations May Lose Value
LOCKUP A V2 MKT-06048-0122 Tracking #1-05228930 (Exp. A successful retirement in the future can often depend on having a solid plan now. If your money isn’t working as hard as you are, it may be time to act—there are no do-overs in retirement planning. Now is the time to consider developing a strategy that can help you work toward your financial goals. I specialize in providing comprehensive, personalized financial guidance with the goal of maximizing every remaining moment of the retirement countdown.
WISELY. YOU WON’T GET A DO-OVER. Call today to learn more or to schedule a consultation. S laicnaniFnwotdiMdnalaicnaniFLPL.CPIS/ARNIFrebmeM,rosivdatnemtsevnideretsigera,laicnaniFLPLhguorhtdereffosecivresyrosivdadnaseitiruce G.seititneetarapeseraCLL,puor nwotdilaicnaniF,puorGCLLM G.SecarYgnuC®PF MrotceriDgnigana 3081.etS,.tSamabalA553 Hnotsuo TX 7 8907 7 3389-553-31 O ecfif 1 9683-464-558- T eerF gmoc.lpl@gnuy.ecar wmoc.gfnwotdim.ww
see Financial Forecast ...page 13
Battling Cancer, 10-Year-Old Sworn In As Honorary VA Police Chief
By Maureen Dyman
The Houston VA got a new honorary police chief today, as Devarjaye “DJ” Daniel, 10, was sworn in at a special ceremony outside the Michael E. DeBakey VA Medical Center.

DJ, who is battling terminal spinal and brain cancer, has always dreamed of being a police officer. He is currently on a mission to be sworn in to as many law enforcement agencies as possible.
DJ’s ultimate goal is to increase awareness of childhood cancer while honoring the legacy of Abigail Arias, a 7-year old girl who dreamed of one day working in law enforcement. Abigail was sworn in as an honorary officer of the Freeport Police Department before she died of lung cancer. Her incredible courage and fight against cancer, inspired and touched thousands of people across the country.
DJ never got the chance to meet Abigail but wants to carry on her legacy.
“Abigail is always in my heart,” said DJ, proudly striking a pose in his new VA Police uniform. “At first my goal was to be sworn in by 100 law enforcement agencies, but I passed that a while ago….now I’m just having fun.”
Houston VA Medical Center Director Frank Vazquez and Police Chief Dwayne Barnes were thrilled to meet DJ and present him with a certificate making him honorary chief of the VA PD. “DJ’s courage is inspiring,” said Vazquez. “We
are honored to welcome him to our Houston VA family.”

The “swearing-in” ceremony was made even more special by the presence of DJ’s father, Theodis Daniel, a Navy Veteran, who has been coming to the Houston VA for care since Hurricane Harvey struck in 2017.
Upon being sworn in as honorary police chief, DJ gave Deputy Director Lindsey Crain a big hug and
asked, “Want to hear a joke?” He enjoyed telling jokes and giving firm handshakes and hugs to everyone present before stopping to pose for a photo with a group of Houston VA police officers gathered to welcome the newest and youngest officer into their ranks.
“Welcome aboard Chief,” Barnes told DJ. “It’s a true gift to have you join our VA family.”
Houston Medical TimesPage 12 medicaltimesnews.comOctober 2022 2319 N. GRAND BLVD., PEARLAND, TX. 77581 www.hmps.net | 281-485-2500 WHAT WE OFFER: • Integrating the Montessori method into the public school curriculum • Currently offering Pre-K thru 4th • Open enrollment until positions fill • Comprehension Stem Program • Character & Leadership Development • High Tech – 7 computers per classroom
Houston VA Deputy Director Lindsey Crain (left) and VA Police Chief Dwayne Barnes (right) present a certificate to DJ Daniel, making him an honorary police chief of the Houston VA.
Fatty Liver
therapeutic strategies.
The current study is built on the forward genetic screen platform, which allowed the researchers to identify two semi-dominant allelic missense mutations (Oily and Carboniferous) of Gm4951 and define a critical role for GTPase-mediated translocation in hepatic lipid metabolism. Among their findings, the researchers found that loss of GM4951 causes NAFLD without obesity, that GM4951
Emergency
Continued from page 8
with a decrease in ED usage of 4.7 visits per 1,000 people in the two states that expanded Medicaid programs. The analysis also found that most of the decreases were in less urgent conditions. This suggests that better access to preventive services and
Financial Forecast
Continued from page 11
The actual dollar figure can vary, though, based on your geographic area. Start Saving for College Expenses
Early
If you would like your child(ren) to attend college, it is recommended
Care for Seniors
Continued from page 9
Hospital is also a member of NICHE (Nurses Improving Care for Healthsystem Elders). As a member, ACE Unit nursing staff receive intensive training to support the development and delivery of age-friendly care that improves quality, experiences and outcomes.
“Collaboration among our physician, employee and community partners has made our ACE Unit possible, and we truly believe it
promotes lipid oxidation to prevent lipid from accumulation in the liver and that GM4951 functions as a GTPase to translocate HSD17B13 to lipid droplets.
GM4951 is a poorly characterized protein and this study defined the role of GM4951 as a GTPase involved in lipid oxidation, said Dr. Zhang. The GM4951-deficient mice developed nonalcoholic fatty liver disease on a high-fat diet with no changes in body weight or glucose metabolism, the researchers noted.
The research is supported by NIH grants R00DK115766 and
R01DK130959 to Dr. Zhang; NIH grants R01AI125581 and U19AI100627 to Dr. Beutler; funding from the Lyda Hill Foundation to Dr. Beutler, and partially through a sponsored research agreement from Pfizer, Inc. to Dr. Beutler.
An estimated one-quarter of adults in the U.S. have nonalcoholic fatty liver disease (NAFLD), an excess of fat in liver cells that can cause chronic inflammation and liver damage, increasing the risk of liver cancer, liver failure and need for transplant. NAFLD has become the most common cause of liver
disease worldwide. In recent decades, it has been suggested that changes in the lifestyles clearly drive the risk in the prevalence of NAFLD. However, hepatic fat content varies substantially among individuals with equivalent adiposity, indicating that genetic factors contribute to the development of NAFLD. Dr. Zhang’s lab is investigating more than 20 genes in which mutations affect liver triglyceride with no change in body weight to identify new mechanisms of NAFLD.
primary care providers through Medicaid coverage could have played a role. Possible mechanisms include substitution of primary care visits for ED visits and improved health leading to less need for ED visits. However, even after Medicaid expansions, more than 40 percent of ED visits were for non-emergent, preventable and primary care treatable conditions.
that you start saving early. In 2022, the average cost of attending any 4-year institution is $35,331. But this figure can vary, too, based on whether the school is public or private, and whether the student is from in-state or out-of-state.7
There are different ways you could set aside money for your child’s future education expenses, including some that offer tax-related incentives.
This points to the possibility of other social and economic factors that act as barriers to care.
These findings add to prior work by shedding light on ED visits of varying levels of medical urgency and by covering more post-expansion years. With this greater understanding, researchers and policy makers can better address Medicaid expansion
effectiveness and the possible role of other factors in access to quality medical care. Improving access to routine care promises to reduce the burden on EDs, which are expected to provide more emergency care as the country’s population continues to
will make a big difference in the lives of our senior population,” said Gillian Alexander, Vice President and Chief Nursing Officer for Memorial Hermann Southwest Hospital.
The ACE Unit is housed on the 10th floor of Memorial Hermann Southwest Hospital.
These include: 529 plans, Coverdell Education Savings Account, Personal savings account, Roth IRA, Cash value life insurance, etc.
Putting Your Financial Plan in Place as You Grow Your Family
Having children can involve many things, but it can be well worth it to make your family complete. When it comes to preparing financially – it is recommended that you talk
Culinary Medicine
Continued from page 10
lack standardization and measurement of competencies. While the programs have a positive impact on student wellness and nutrition knowledge, they struggle with adequate funding and faculty support.
Dr. Albin said the time is ripe for increased support. Suboptimal diets are well established as a driving force for increased morbidity in obesity, cardiovascular disease, and Type 2 diabetes, and the COVID-19 pandemic
with financial professionals. This includes working with a CERTIFIED FINANCIAL PROFESSIONAL™ who can advise you on planning for the short and long-term.
revealed the relevance of metabolic health in food insecure communities.
“Food is the top risk factor for early death in the U.S., and culinary medicine could transform the problem into the solution,” Dr. Albin said.
Other researchers who contributed to the review include first author Courtney Newman and Justin Yan, both UTSW medical students, and Sarah Messiah, University of Texas School of Public Health.
Houston Medical Times Page 13 medicaltimesnews.com October 2022
Continued from page 6
grow.
Breast Cancer
Continued from page 1
lumpectomy, reconstructive surgery can help restore breast symmetry and appearance.
Breast reconstruction can be performed at the same time as a mastectomy (immediate reconstruction), or after the
Legal Matters
Continued from page 3
Counsel of the Department of Health & Human Services (“OGC”) released Advisory Opinion 20-05 to clarify that a “substantive legal standard” subject to notice-and comment rulemaking is any requirement “not otherwise mandated by statute or regulation.” Because the Provider-Based regulations do not directly address co-location, and applying OGC’s own standards, any guidance regarding co-location under the Provider-Based regulations would arguably be subject to notice-and-comment rulemaking.
As an illustration of the impact of Allina on co-location, an Administrative Law Judge (ALJ) recently held that CMS’s restrictive
Mental Health
Continued from page 4
are able to receive it. Reasons for this gap include lack of awareness and challenges with insurance coverage. The group hopes that the results of their study will help increase awareness for DBS as a viable treatment for OCD and convince insurance companies to cover it more routinely.
“I think that is the biggest message to get across — this is an
completion of further treatment such as radiation and chemotherapy (delayed reconstruction). The timing of reconstruction depends on the type of breast surgery performed and individual patient factors.
As each person has a unique set of preferences and concerns related to the physical changes associated with surgery for breast cancer, patients should evaluate which surgical
procedures are right for them based on their own priorities and goals and address any questions or concerns with their physician.
For more information on breast cancer and breast surgery, visit TexasOncology.com or Texas Breast Specialists at texasbreastspecialists.
Healthy Heart
Continued from page 8
“We know that calcium build-up in the arteries of the breasts is visible in routine mammograms. That build-up may put postmenopausal women at a higher risk for cardiovascular disease,
interpretation of the Provider-Based regulations violated Allina. In this 2021 Department of Health & Human Services Departmental Appeals Board decision, the ALJ found that a Cleveland Clinic Foundation’s sleep study facility met Provider-Based requirements even though it was co-located with a Marriott hotel. The ALJ set aside CMS’s argument that the facility could not meet the Provider-Based regulatory definition for “Department of a Provider” if it did not have “separate space physically partitioned off by a door or wall” and an exclusive entrance; the ALJ acknowledged that this may be a “reasonable requirement,” but determined that she was “unable to impose such a specific requirement based on the text in the definition.” The ALJ went on to conclude that under Allina, she could not “implement CMS’s ad
hoc interpretations when there is ambiguity.” Importantly, CMS denied this particular attestation and argued the case pre-Allina and also prior to issuing updates to the State Operations Manual with respect to co-location under the CoPs. It is unclear whether CMS would continue with such a restrictive view of co-location today, but this case illustrates that CMS would face an uphill battle continuing such a view without first engaging in notice-and-comment rulemaking.
And to that point, the lack of any proposed rulemaking regarding co-location in the 2023 OPPS Proposed Rule is, if not outright good news for hospitals, not bad news either.
HOUSTON
Published by Texas Healthcare Media Group Inc.
Director of Media Sales Richard W DeLaRosa
Senior Designer Jamie Farquhar-Rizzo
Web Development Lorenzo Morales Distribution Robert Cox Brad Jander Accounting Liz Thachar
Office: 713-885-3808
Fax: 281-316-9403
For Advertising advertising@medicaltimesnews. com Editor editor@medicaltimesnews.com
effective method; it has been approved for a long time. It is underutilized,” said Sheth.
“The demonstrated effects of DBS in this report are even more impressive when one considers that these patients have failed numerous behavioral and pharmacological therapies. Having such a robust treatment when first- and second-line interventions are incomplete provides hope to those suffering,” said Dr. Eric Storch, professor and vice chair for the Department of Psychiatry and
Behavioral Sciences at Baylor.
The study was supported by the McNair Foundation, the Dana Foundation, the National Institute of Mental Health (1RF1MH121371), and the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (P50HD103555). See publication for a full list of disclosures.
which is the leading cause of death in women. I hope this study will encourage us to update the guidelines for reporting this information, so women can have all the information they need to make the best possible health decisions for themselves and live longer, healthier lives.”
Cardiovascular disease followed
by cancer are the top two causes of death among U.S. women. However, in the U.S., more women report worrying about their risk for breast cancer than heart disease, and only half of women are even aware that heart disease is the leading cause of death in women. Learn more at heart.org
Houston Medical Times is Published by Texas Healthcare Media Group, Inc. All content in this publication is copyrighted by Texas Healthcare Media Group, and should not be reproduced in part or at whole without written consent from the Editor. Houston Medical Times reserves the right to edit all submissions and assumes no responsibility for solicited or unsolicited manuscripts. All submissions sent to Houston Medical Times are considered property and are to distribute for publication and copyright purposes. Houston Medical Times is published every month
P.O. Box 57430
Webster, TX 77598 7430
Houston Medical TimesPage 14 medicaltimesnews.comOctober 2022
com.
Customized solutions for physicians and medical practices
Medical Specialty Group
Banking. Brokerage. Trusts. Practice finance. Those are table stakes. What sets Truist Wealth Medical Specialty Group apart are the trusted advisors who not only are skilled in their own profession, but also deeply knowledgeable and well-versed in the subtleties and complexities of physicians and their practice groups.
Together, we’ll partner with you to take on today’s challenges and seize tomorrow’s opportunities.
To learn more, contact:
Michael E. Smith
Senior Vice President Medical Relationship Manager
Truist Bank 713-265-6821 Mike.Smith3@truist.com
Michael E. Smith, Registered Adviser Representatives,
Investment and Insurance
not
Services,
Adviser Representatives, Truist Advisory Services, Inc.
Houston Medical Times Page 15 medicaltimesnews.com October 2022 Truist Wealth Medical Specialty Group is a marketing name used by Truist Financial Corporation. Services offered by the following affiliates of Truist Financial Corporation: Banking products and services, including loans and deposit accounts, are provided by SunTrust Bank and Branch Banking and Trust Company, both now Truist Bank, Member FDIC. Trust and investment management services are provided by SunTrust Bank and Branch Banking and Trust Company, both now Truist Bank, and Truist Delaware Trust Company. Securities, brokerage accounts and /or insurance (including annuities) are offered by Truist Investment Services, Inc., and P.J. Robb Variable Corp., which are each SEC registered broker-dealers, members FINRA, SIPC, and a licensed insurance agency where applicable. Life insurance products are offered through Truist Life Insurance Services, a division of Crump Life Insurance Services, Inc., AR license #100103477, a wholly owned subsidiary of Truist Insurance Holdings, Inc. Investment advisory services are offered by Truist Advisory Services, Inc., GFO Advisory Services, LLC, Sterling Capital Management, LLC, and Precept Advisory Group, LLC, each SEC registered investment advisers. Sterling Capital Funds are advised by Sterling Capital Management, LLC. ©2022 Truist Financial Corporation. Truist, Truist Purple, and the Truist logo are service marks of Truist Financial Corporation.
Truist Investment
Inc. Investment
Products: Are
FDIC or any other Government Agency Insured • Are not Bank Guaranteed • May Lose Value Truist.com/wealth
American Heart
Heart Challenge


HOUSTON November 19 TDECU Stadium
HEART WALK



The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic activity each week. You can knock that out in just 30 minutes a day, 5 days a week. Too much sitting and other sedentary activities can increase your risk of heart disease and stroke. Plus, regular activity can help you to think, feel and sleep better and perform daily tasks more easily.
JOIN US TO REINVIGORATE YOUR HEART HEALTHY LIFESTYLE AND MAKE AN IMPACT BY SAVING LIVES IN OUR COMMUNITY!
KELLY YOUNGBLOOD
EVP and CFO MRC Global


2022 Houston Heart Challenge Chair
American Heart Association
Thank you to Kelly for your support of our mission and commitment to the health of every Houstonian!
Board Member

October 2022 Houston Medical Times medicaltimesnews.com
Houston
Association®
TM







 Sarah Kocher, J.D. Polsinelli, PC
Sarah Kocher, J.D. Polsinelli, PC















 By The American Heart Association
By The American Heart Association









 By Grace S. Yung, CFP Midtown Financial Group, LLC
By Grace S. Yung, CFP Midtown Financial Group, LLC