



you
makes a difference. And you have to decide what kind of difference you want to make.”





you
makes a difference. And you have to decide what kind of difference you want to make.”
The National Health Service (NHS) has been in the news a lot of late, not just because of the obvious pressure created through the pandemic, putting staff and resources under severe pressure and leading to all sorts of knock-on consequences in the availability of wider health services, but also because of the ageing population, austerity, staff shortages, stress, increasing incidents of violence against staff, and the costs of new treatments and technology.
According to the UK Health Secretary Sajid Javid, one in nine of the population in England is on a waiting list for hospital care, and despite a two-year recovery plan this is likely to grow before it gets better. In Scotland this figure is slightly better, at closer to one in ten (just over 400,000). Additionally, Shadow Health Secretary Wes Streeting claimed there were 93,000 staff vacancies. In Scotland, the Royal College of Nursing reported in November 2021 that there was a record high shortfall of 3,400 nurses (which rises to 5,000 if you count all vacancies for registered nurses, midwives, and healthcare support workers).
I have friends and family in the health-service, and every one of them talks of low morale, burnout and, for far too many, a desperate urgency to retire as soon as possible. I know the health service isn’t alone in all of this, but it does not feel healthy, and an unhealthy health service is surely in nobody’s interest.
So, is the health service healthy and happy? Are the claims of its demise or creeping privatisation exaggerated? Are there trends we should be more conscious of, or issues we need to raise awareness around? And how does our health service compare with other countries?
The health service, alongside freedom of speech and a free press, is one of the values people hold most dearly about the UK. So much so that an homage to the NHS formed the centrepiece of the opening ceremony of the London Olympics in 2012. And during the early part of the pandemic, many of us took to the streets to clap health workers (and other front-line workers) for their invaluable contribution to society. This edition of The Geographer, then, is in a small way our thanks to the NHS for all it has done over the past two years and all it continues to do.
Mike Robinson, Chief Executive, RSGS
RSGS, Lord John Murray House, 15-19 North Port, Perth, PH1 5LU tel: 01738 455050 email: enquiries@rsgs.org www.rsgs.org
Charity registered in Scotland no SC015599
The views expressed in this newsletter are not necessarily those of the RSGS.
Cover image: 2012 London Olympic Games Opening Ceremony. Julian Simmonds / Shutterstock
Masthead: A beautiful winter’s morning at Lake Camp, Hakatere Conservation Reserve, Canterbury. South Island. © Rach Stewart
RSGS:
Almost 800,000 trees, including Scots pine, birch, aspen, holly, rowan and oak, have been planted at Beinn Eighe National Nature Reserve near Kinlochewe since it was established in 1951. Woodland cover has increased by over 40%, creating ‘corridors’ that connect fragments of ancient woodland, allowing animals to move more freely, helping to combat climate change, and increasing local biodiversity.

This year, the main planting phase will end with the last 20,000 trees. In future years, natural regeneration will help expand the woodland further, and NatureScot will only use targeted planting for under-represented species in areas where there is no seed source.
Due to the local oceanic climate, the woodlands at Beinn Eighe are classed as temperate rainforest. Many such forests around Europe are degraded due to pollution or mismanagement, but Scotland has some of the best examples of the habitat anywhere in the world.

Dutch engineers have solved one of the biggest hurdles towards a sustainable future – how to store excess renewable energy generated when weather conditions are favourable, and release it on demand. Developed by Ocean Grazer (oceangrazer. com), the Ocean Battery is an energy storage solution for offshore wind farms. Installed at the seabed at the source of power generation, and based on hydro dam technology that has proven itself for over a century as highly reliable and efficient, Ocean Battery provides eco-friendly utilityscale energy storage up to GWh scale.
To store energy, the system pumps water from the rigid reservoirs into the flexible bladders on the seabed. The energy is stored as potential energy in the form of water under high pressure. When there is demand for power, water flows back from the flexible bladders to the low-pressure rigid reservoirs, driving multiple hydro turbines to generate electricity.
a better way to see the world
“Bound by paperwork, short on hands, sleep, and energy… nurses are rarely short on caring.”
Sharon Hudacek, nurse educator
In November, we were pleased to present Keith Anderson, Chief Executive of Scottish Power since 2018, with RSGS Honorary Fellowship, in recognition of his role as a leading representative of industry in the climate discussion, and for leading the transition of Scottish Power to 100% renewables, helping in Scotland’s journey towards becoming net zero by 2045. Recently, he was behind the demolition of Scotland’s last coal power station, Longannet (see page 27).
2021 was an incredibly busy year, but we have plans to ensure 2022 is successful too. We get opportunities to input to all sorts of policy work and discussions, and it is difficult not to, when we get so excited about the universality of geography and the need to problemsolve and engender action on so many complex issues and wicked problems. So we will continue to embrace opportunities that pop up. However, our main focus for 2022, beyond the usual talks, magazines, medals, various advisory roles, conferences and events, will be around two key priorities: education and climate change.
On education, we will continue to support young people and teachers, build online and CPD activity, input to curricular discussions with Government, represent views in national fora and with education bodies, work with other scientific societies to develop collaborative thinking, push for more choice and a higher profile for all things geographical, and look at how we can drive the profile of Geography in early school years and the uptake of Geography in senior phase and university. In addition, we will always work to push scientists and geographers into direct policy discussions and consultations.
On climate change, our Climate Solutions course is still growing, we are seeing a lot of interest in offering more to businesses and organisations trying to put plans in place, and we hope we will see more internationalisation of this over the coming months. In addition, we will continue to work in a number of other key climate areas, the most obvious being the three other topics where action is so essential – agriculture, transport and cities. To find out more please check out our website under ‘What We Do’.
Because of growing success and workload, we are now advertising for an additional member of staff to fill a new post of Deputy Chief Executive. This person will support our Chief Executive, Mike Robinson, particularly in expanding RSGS’s public-focused and policy-related work, and in fundraising and financial management. The person appointed will focus initially on helping us to significantly increase uptake of our major Climate Solutions training programme, and then increasingly transition into the many broader aspects of RSGS’s work at a senior level.
Antimicrobial resistance (AMR) poses a major threat to human health around the world. A comprehensive assessment of the global burden of AMR, published in The Lancet at doi.org/10.1016/S0140-6736(21)02724-0, found an estimated 4·95 million deaths associated with bacterial AMR in 2019, including 1·27 million deaths attributable to bacterial AMR. In the global study of 204 countries, the team of international researchers estimated the allage death rate attributable to resistance to be highest in western sub-Saharan Africa (27·3 deaths per 100,000) and lowest in Australasia (6·5 deaths per 100,000). Lower respiratory infections accounted for more than 1·5 million deaths associated with resistance in 2019, making it the most burdensome infectious syndrome. For comparison, researchers estimate that, in the same year, AIDS caused 860,000 deaths and malaria caused 640,000.
In November, we were pleased to present RSGS Honorary Fellowship to Lee Craigie, Active Nation Commissioner for Scotland. Working closely with the Scottish Government and leading NGOs to champion active travel and the outdoors in a wide range of policy fora, Lee has helped ensure that walking and cycling are accessible and inclusive for all, and as a figurehead and policy lead she has helped increase the budget for active travel in Scotland. She has demonstrated support for the promotion of physical activity for marginalised young people and girls, and has advocated for the environment and decreasing carbon emissions.
Covid has caused huge disruption in schools, particularly around the potential for outdoor and experiential learning. As restrictions start to be lifted, having the courage to start planning these activities again is a judgement being made in schools across the country. The importance of residential trips cannot be underestimated and, as always, Geography teachers are at the vanguard of developing these opportunities.
It looks like formal examinations will also run this May for the first time in two years. It is with some relief that the pressure of making these judgements has been removed from teachers, but there is still some uncertainty. The Scottish Qualifications Authority is providing a range of different support measures and guidance, but the details of these will not be released until early March. Geography is one of the earliest exams this year, taking place on 27 April, and for many pupils this will be the first formal exam they have ever sat. The RSGS-produced Chalk Talk summary videos are being well used for revision and to fill any gaps in learning, and continue to be a resource valued by teachers, parents and pupils, being viewed over 18,000 times.


According to research by campaigning organisation Climate Emergency UK, more than one in five of all councils in the UK have no climate action plan. Out of 409 local authorities, 84 had no climate action plans, while 139 had not committed to achieve net zero emissions by a specific date. Climate Emergency UK scored 325 plans according to 28 questions based on how well councils’ plans would help mitigate climate change locally, the extent to which climate was integrated into existing policies, community engagement, climate education, scale of emissions targets, and commitments to tackle the ecological emergency. High scores included 91% for Somerset West and Taunton, 89% for West Midlands, and 87% for Manchester City.
The Scottish explorer and plant-collector Isobel Wylie Hutchison is attracting a lot of attention just lately, particularly with documentary-makers. I have been asked to give some background information on her travels and experiences by three separate film-making teams, who intend to produce documentaries for television. These documentaries will either focus entirely on Isobel, or include her as part of a wider theme. I believe that filming on all these projects will take place this year.
Isobel is one of Scotland’s most underappreciated explorers, and her expeditions in the 1920s and 30s to Greenland, Alaska and Arctic Canada deserve much wider recognition. I’m very glad that her story is going to be shared with wider audiences.

Since 1890, RSGS’s prestigious Medals have allowed us to celebrate outstanding contributions made by individuals in a wide range of geographical fields. And among learned societies, RSGS is unusual in that our Fellowships are honorary, bestowed solely in appreciation of achievement. These awards help us publicly recognise some of the best in humanity, project the importance of geographical endeavour, build our connections with some of the most influential minds of our day, and thank those who push the boundaries, promote kindness, and provide inspirational role models.
We have been able to carry out this work in large part thanks to a fund established by Agnes Livingstone-Bruce, who endowed the very first medal back in 1901 in memory of her father, the explorer David Livingstone. This led to the establishment of the Inspiring People Fund, which supports the costs of administering today’s programme of awarding Fellowships and Medals.
But after 120 years, we need to replenish this fund to ensure that we can keep making these important awards. And so we are launching a fundraising appeal which will be sent to our members and posted on our website. Please look out for this appeal, and please support us if you can.

In January, Tropical Cyclone Ana caused extensive disruption across Southern Africa as torrential rains and heavy flooding resulted in more than 80 deaths and left tens of thousands of people homeless. The storm formed over western Madagascar and then hit northern and central Mozambique and Malawi. Heavy rains caused overflowing rivers, floods and landslides, which resulted in casualties and widespread damage.
Malawi experienced copious amounts of infrastructural damage, with roads destroyed by rapidly flowing floodwater. President Lazarus Chakwera declared a state of disaster in areas affected by the cyclone, and appealed for humanitarian assistance for essential items such as tents and food.
A spokeswoman for the World Food Programme highlighted some of the impacts, including damage to agricultural land, key infrastructure and houses, causing loss of life and livelihoods, adding, “Southern African countries have been repeatedly struck by severe storms and cyclones in recent years that have impacted food security, destroyed livelihoods and displaced large numbers of people.”
Several parts of Africa have experienced destructive flooding over the past year, as they deal with the twin issues of prolonged drought and increases in rainfall intensity, which together create prime flooding conditions. The continent is projected to experience a greater frequency of heavy rain according to the latest IPCC report, meaning that the region impacted by Cyclone Ana is projected to see an increase in such events as global temperatures continue to rise.
Nadia Whittome MP is sponsor of a Private Members’ Bill going through the UK Parliament, to require matters relating to climate change and sustainability to be integrated throughout the curriculum in primary and secondary schools and included in vocational training courses. She said, “the education system should be helping young people get informed on the impacts of climate change.”
Some students have voiced their frustration at the lack of opportunities to discuss climate change in classes and the lack of resources available, and teachers have described feeling like they are pressured to be cautious when talking about the climate crisis and unequipped to teach what can be considered a controversial subject.
A spokesperson from the Department of Education said that “by 2023 all teachers in all phases and subjects will have access to high-quality curriculum resources so that they can confidently choose those that will support the teaching of sustainability and climate change.”
please support us© RSGS Collections
We continue to make weekly additions to our blog (www.rsgs. org/blog), covering a range of interesting topics and news. Recent posts include:
Sir Fitzroy Maclean: Escape to Adventure – the legendary Scottish soldier considered to be one of the inspirations for Ian Fleming’s James Bond undertook a hair-raising mission in Benghazi.
A Sleigh Ride in the Snow – when the weather outside was frightful, Captain Fred Burnaby was pole-vaulting across the Volga and battling across the frozen Kazakh steppe in a sleigh drawn by three camels.
A Fruitful 2021 at RSGS – as we entered into a new year we reflected on some of RSGS’s activities and achievements during 2021.
Isobel Wylie Hutchison: Toasting Rabbie Burns in Greenland –“It is Burns Night! Can one be the only Scot in Greenland and forget to celebrate such a festival? One cannot!” said Isobel Wylie Hutchinson as she celebrated the famous poet in Greenland in 1929.
Following the decision to postpone face-to-face talks for the second half of the season due to ongoing Covid-19 restrictions and limitations, our revised online programme got underway in early January, with the first talk – Tim Marshall speaking on The Power of Geography – attracting over 500 households! We are delighted with the general numbers joining us every week.
The revised online programme will continue until the end of March and, with relaxing conditions, we are hopeful of returning to faceto-face talks in September. As always, we are grateful to all of our members and others who have continued to support us throughout these times. We look forward to your continuing support and to welcoming you back to in-person events when it is safe to do so. Please visit rsgs.org/events for details and to reserve tickets for forthcoming talks in the online programme.
Tens of thousands of tonnes of extra medical waste from the response to Covid-19 has put tremendous strain on health care waste management systems around the world, threatening human and environmental health and exposing a dire need to improve waste management practices.
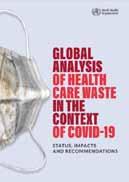
A new report (www.who.int/publications/i/ item/9789240039612) from the World Health Organization (WHO) bases its estimates on the c87,000 tonnes of personal protective equipment that was procured between March 2020 and November 2021 and shipped to support countries’ urgent Covid-19 response needs through a joint UN emergency initiative. Most of this equipment is expected to have ended up as waste. The authors note that this just provides an initial indication of the scale of the problem; the report does not take into account any of the Covid-19 commodities procured outside of the initiative, nor waste generated by the public, like disposable masks. “Covid-19 has forced the world to reckon with the gaps and neglected aspects of the waste stream and how we produce, use and discard our health care resources, from cradle to grave,” said Dr Maria Neira, Director, Environment, Climate Change and Health at WHO.

In November, a scientific research mission supported by UNESCO discovered one of the largest coral reefs in the world off the coast of Tahiti. The pristine condition of, and extensive area covered by, the rose-shaped corals make this a highly valuable discovery. “It was magical to witness giant, beautiful rose corals which stretch for as far as the eye can see. It was like a work of art,” said French underwater photographer Alexis Rosenfeld.
“To date, we know the surface of the moon better than the deep ocean. Only 20% of the entire seabed has been mapped. This remarkable discovery in Tahiti demonstrates the incredible work of scientists who, with the support of UNESCO, further the extent of our knowledge about what lies beneath,” said UNESCO Director-General Audrey Azoulay. See ioc.unesco.org/news/rare-coral-reef-discovered-near-tahitiunesco-mission for more information.
The Geography world lost a champion with the death last summer of Leslie Hunter FRSGS. Born in Glasgow, Leslie started teaching at Alloa Academy on 1 April 1961. That year he also married Val, his wife for almost 60 years. After further spells of teaching in Wick and Edinburgh, he became a lecturer at Moray House College of Education, training young Geography teachers.
In 1975, Leslie was appointed Geography specialist HMI, a post which offered him further challenge and satisfaction in his beloved subject. He oversaw the introduction of Standard Grade and Revised Higher, and produced the excellent Effective Learning and Teaching in Geography
Leslie was well respected by Geography teachers because he’d experienced Geography at all levels. He understood the subject, and the quirks and limitations imposed by individual schools and local authorities. Subject inspectors help drive up standards by encouraging and building confidence in teachers of all ages and experience. Leslie was the very best exemplar. The idea that school inspections are dreadful things filled with angst was certainly not the case with Leslie. His kindness in setting teachers at their ease during inspections was impressive. For example, he didn’t expect a teacher to continue teaching the prepared lesson when a helicopter landed outside and provided a different interest!
Apart from his trusty HMI briefcase, Leslie had two other essentials, especially on inspections in the Highlands, Western Isles or Northern Isles: his collapsible fishing rod, and his binoculars for bird watching.
Leslie actively supported teachers through the Scottish Association of Geography Teachers, and he served on RSGS’s Education Committee and as Chair of RSGS’s Dundee Group. Leslie didn’t consider himself an important man, but those of us who had the pleasure of knowing him, knew different!
Things have calmed down a bit since COP26 in Glasgow and the follow-up to that; it feels a long time ago that we were bouncing between coordinating and chairing events, media interviews, extra publications and hosting various visitors. And although it is not as hectic, we are still very active. We have given talks to external bodies, including the International Development Alliance, Scottish Enterprise, and several Chambers of Commerce. In January, we were delighted to address the staff conference for Sistema, an organisation for which we have a high regard. We look forward to working closely with all of them as the year progresses.
We gave evidence to the Scottish Parliament’s Net Zero, Energy and Transport Committee, to debrief them postCOP26. We met with the Historic Towns Trust, looking at developing historical atlases of Scottish towns and cities. We continue to be represented on the Scottish Government’s Agriculture Reform Oversight Implementation Board. And we are talking to the Explorers Club of New York about future joint working. So there is lots to get our teeth into over the course of 2022.
If you would like to know more about any of these work areas, or to get involved, please drop us an email on enquiries@rsgs.org

Within the crises of climate change and biodiversity loss, the role of cities is becoming ever more prominent. According to the World Bank, some 55% of the world’s population currently live in cities and this is expected to increase to 70% by 2050. In their 2020 report on urban development, they say, “Once a city is built, its physical form and land use patterns can be locked in for generations, leading to unsustainable sprawl. The expansion of urban land consumption outpaces population growth by as much as 50%, which is expected to add 1.2 million km² of new urban built-up area to the world in the next three decades. Such sprawl puts pressure on land and natural resources; cities consume two-thirds of global energy consumption and account for more than 70% of greenhouse gas emissions.”
This increased emphasis globally on the role of cities is a vital area of future sustainable development. RSGS has been working through Perth City Leadership Forum to convene discussion about how a smaller city like Perth, with advantages of scale and good environmental integrity, can play more of a role. We hope to help deliver projects which can make Perth more resilient, prosperous and net zero; and, by doing so at city and area scale, provide example and experience to inspire other cities to develop too.
In January, we ran a biodiversity conference featuring the Mayor of Lahti in Finland, European Green Capital of 2021, Elizabeth Mrema, Executive Secretary of the Convention on Biological Diversity, and an array of other speakers from around the world. Over 200 people and organisations attended, and we hope good things will follow. As Elizabeth Mrema said, “your work will be an inspiration for other cities.” See mostsustainablecity.com for more information and to watch the speeches.
Rivers have captivated wildlife writer Keith Broomfield since childhood: special serene places where nature abounds and surprises unfold at every turn. If Rivers Could Sing is his personal Scottish river wildlife journey, in which he delves deeper into his own local river – the River Devon as it flows through the counties of Perthshire, Kinross-shire and Clackmannanshire – to explore its abundant wildlife and to get closer to its beating heart.

 Jo Woolf FRSGS, RSGS Writer-in-Residence
Jo Woolf FRSGS, RSGS Writer-in-Residence
The Shackleton Museum in County Kildare, Ireland, has established an annual event called the Ernest Shackleton Autumn School. For the last couple of years this event has been held online in the form of live-streamed presentations by guest speakers on all aspects of Shackleton’s story. I was invited to take part in last year’s event, called Virtually Shackleton 21, on 30 October. My talk, entitled Sir Ernest Shackleton at the Royal Scottish Geographical Society, focused on Shackleton’s time as Secretary of RSGS and was illustrated with some of our much-loved artefacts, such as his CV and photographs of the Endurance before it set sail. All the talks are available to view online, on the Shackleton Museum’s YouTube channel, ’Shackleton Museum Athy’, at www.youtube.com/ watch?v=Q2jc4t6STTY
We were delighted to participate in the Royal Society of Edinburgh’s inquiry panel which ran during late December and early January, responding to the UK Parliament consultation on ‘Aligning the UK’s economic goals with environmental sustainability’. There is broad consensus on the need to find more suitable economic indicators than GDP, and the need to begin to cost current externalities, but there still remains a good deal of debate about how best to do that, which measures to back, and how to begin challenging the primacy of GDP in government thinking and public discourse.

The Scottish Government Climate Assembly, a group of over 100 citizens from all backgrounds tasked with outlining recommendations on how Scotland should change to tackle the climate crisis effectively and fairly, will soon be coming to an end. The Assembly has commended the Scottish Parliament for bringing the Assembly together, and for taking its 81 recommendations into consideration. Just some of the recommendations highlight the importance of shared goals and targets, prioritising the most pressing climate issues, fair access to public transport, and the necessity of climate education to succeed in our collective mission in Scotland towards net zero.
In November, we were delighted to present RSGS Honorary Fellowship to Professor Ed Hawkins, a leading climatologist from the National Centre for Atmospheric Research at the University of Reading, a lead author for the IPCC’s Sixth Assessment Report on the physical science of climate change, and designer of the climate ‘warming stripes’ graphics. Ed received his Fellowship certificate at one of our Meet the Experts events, monthly online Q&A sessions with sustainability experts.

In January, RSGS Chief Executive Mike Robinson spoke with The Herald for its Climate Conversations podcast, discussing a wide range of topics, from Scotland’s position as a leader in climate change to the importance of political will globally. Together with podcast host Marc Strathie, he considered the industries that have a significant impact on the feasibility of achieving net zero by 2030, and how RSGS is helping to bring people up to speed on climate change as quickly as possible. The hour-long podcast can be found at shows.acast.com/climate-conversations
In February 2020, First Nations representatives from British Columbia joined more than 500 participants from 50 countries in Mexico City to discuss a roadmap for the Decade of Indigenous Languages which officially began at the start of 2022. The resulting Los Pinos Declaration places Indigenous peoples at the centre of its recommendations, under the slogan ‘Nothing for us without us’. In its strategic recommendations for the Decade, the Los Pinos Declaration emphasises Indigenous peoples’ rights to freedom of expression, to an education in their mother tongue, and to participation in public life using their languages, as prerequisites for the survival of Indigenous languages, many of which are currently on the verge of extinction.
See en.unesco.org/news/pinos-declaration-chapoltepek-lays-foundationsglobal-planning-international-decade-indigenous for more information.

Uptake of our Climate Solutions course continues to go well. It has been great to see that a large number of staff from all three enterprise networks (Scottish Enterprise, South of Scotland Enterprise, and Highlands and Islands Enterprise) have now completed the course. We have more interest from overseas, with Outward Bound Oman adopting both the Climate Solutions Accelerator course and the Scotland: Our Climate Journey film for training young people in Oman about all things climate-related. We have had a lot of interest from existing participant companies in rolling out access to the course to their entire supply and customer chains. And each Wednesday, The Herald newspaper has featured an article with testimonials and experiences of participants in the course, and some of the wider issues surrounding climate solutions adoption. Here is a sample of recent feedback: “I have been really struck with the impact the course has had on quite a number of participants. While we hoped the course would help raise understanding across the board, it’s gone well beyond these expectations – so thank you to the whole team once again.” And another piece of (too?) honest feedback: “I thought the course was very good indeed; frankly, much better than I expected it to be! I’m no climate change denier but I find a lot of the material on climate change to be annoyingly preachy and self-righteous. This wasn’t; it was interesting and informative and it made me think.”
We want anyone and everyone to undertake the course in order to encourage a universal understanding of this critical issue. Please visit rsgs.org/climate-solutions to learn more.
visit rsgs.org/climate-solutions
Geographers should be interested in what is happening to the NHS because it is through making geographical comparisons with other countries that we can see that its current decimation is unnecessary. The claim that there is no alternative but to spend less can be disproved by considering how other very nearby countries manage to spend more. Furthermore, there is a geography to the cuts that have taken place in the UK which reveals where is prioritised and where is not. Finally, very local geographical stories, such as two briefly told here from Oxford and Glasgow, can also help reveal what is going on.
On 9 January 2020, the BBC published a news story entitled ‘11 charts on the problems facing the NHS’. The second of those charts (Figure 1) shows how cuts in spending increases for the NHS began in earnest in the late 1970s, were briefly reversed for 13 years after 1996, but then began again after 2009. All of these changes were political choices, as the labelling of the graph makes clear, although there had been something of a political consensus between 1955 and 1978 when spending increases were usually above 4% a year regardless of the political party in power in the UK.
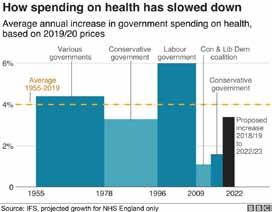
A spending increase of 4% a year does not mean an actual improvement in service; it often means just holding the line. This is especially so today when the population is ageing far faster than it was in the 1960s or 1970s. That BBC article went on to show that spending on health care in the UK is much lower as a proportion of GDP than it is in France and Germany, and that is even the case when private health spending is included. It also showed that there was little difference in outcomes in the different countries of the UK, almost certainly because spending across them varies so little as compared to spending across Europe. In 2017, health spending in the UK as a whole, including all the spending on private hospitals, was almost identical to the EU average. Today it will almost certainly be less than that average, not least as other countries in Europe have responded with a larger increase in emergency spending due to the pandemic. This is alongside the now usually higher increases in health spending that most other European countries are making as they bolster up their health services more widely. In contrast, the UK government plans to reduce public spending overall once the pandemic has subsided, as illustrated by the submissions it has made to the International Monetary Fund on planned future public spending.
The final graph the BBC published in their series of 11
illustrates one theory as to why these choices have been made. That graph (Figure 2) shows that patient satisfaction with the NHS was falling until 1997, then rose as public spending rose, to a high of 70% being ‘very or quite satisfied’ in 2009, before falling again afterwards. Satisfaction with the NHS tends to track how well the NHS is able to cope, which in turn is largely determined by how well it is funded and organised.

Why would some politicians instigate changes in funding that inevitably result in a fall in satisfaction with the NHS? These politicians often say that a continuation of funding increases could not be maintained. That clearly was not the case as other countries in Europe chose differently despite suffering similar economic shocks at particular times. Geographical comparisons are a key way in which you can determine if the politicians are lying to you about what is possible, as compared to what they are choosing to do.
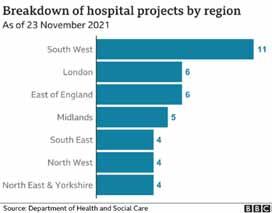
Of course, there is always some part of the UK that is receiving a greater increase in health funding, or less of a decrease, at any one time. Politicians tend to point to the increases to say that they are doing something substantial. It is well known that the UK government has promised “40 new hospitals” in England. What is less well known is that hardly any of these hospitals are new; most are extensions to (or rebuilding on) existing sites, but even here there is a clear geographical pattern to what is planned as yet another graph
“A spending increase of 4% a year does not mean an actual improvement in service.”
(Figure 3), published by the BBC on 1 December 2021, makes clear. The 40 planned projects are concentrated in the South West of England; although as the BBC story that accompanied that graphic made clear, there are now doubts as to whether most of those will happen on time. More importantly, even if the planned projects were to all be completed, they would not reverse the decimation that has been occurring more widely, or even begin to address the increase in need that comes as we age and become more frail overall. Neither would they begin to cope with the health legacy of a pandemic and a disease which is becoming endemic, resulting in greater levels of illness than before for an as-yet-unknown number of years to come. What is going on? I grew up in the city of Oxford in England at a time when the NHS was well funded and in a city with a surfeit of public hospitals. I left the city when I was aged 18 and returned nine years ago. One of many shocks on returning was discovering what had happened to the old ‘Manor’ ground where Oxford United used to play. It now housed a brand-new private hospital, built walking distance from the old public hospitals so that consultants who chose to do part private work could walk over with ease. Before the private hospital had been built, there had been much less opportunity to expand the private health sector in the city. Later I discovered that some Oxford colleges offer to fund private health insurance for their academic and other staff. Something dystopic was happening, however slowly and gradually, so that each of us can tell a story of the dismantling of public health care, but few of us can see the overall orchestration underlying this.
In January 2020, it was quietly announced that a new £20 million private hospital had been opened just off the Old Govan road in Glasgow. The ‘Ross Hall Clinic Braehead’ was described as “state-of-the-art” by the Daily Record. Nestled on an industrial estate between an accountancy firm and a computer shop, and opposite a new charging station for electric cars, “The new hospital includes 17 new consulting rooms, a new MRI scanner alongside new respiratory, colposcopy and urodynamic departments. The inclusion of these key additions will mean that an extra 200 outpatients a day will be able to receive care from clinical specialists.” But of course only a few people will be able to afford to use these services, and others will rely on the NHS sending them there, if it is able to do so.
The pandemic could have begun a sea-change in the direction of health care and healthcare spending across the UK. Many private hospitals would not have survived it had they not been supported by state contracts and emergency funding to keep them solvent. We could have nationalised most of

the new private facilities, at almost no cost – given that they were no longer solvent. Instead they were supported, kept alive for when they could begin could begin fully operating; and new private facilities were built during the pandemic.
In relation to the growth in need, healthcare spending has been decimated across the UK. One reason this is allowed to happen is because a small but growing proportion of the population can afford to bypass the ever-lengthening waiting lists; they do not have to worry about what will happen to them if and when they fall ill. They receive an increasingly better level of service as compared to what most people can access. And the politicians who have presided over this growing social and health divide are not unaware of this. In fact, they are often lobbied by private healthcare companies or have even more direct involvement than that.
Why should British geographers care about any of this? One reason, perhaps the most trivial, is that it will affect the maps of health outcomes for many years to come, to the extent that differential health and social care is part of the reason as to why people live shorter lives in some areas rather than others. A less trivial reason is that even if they are not worried about the direction their society is travelling in generally, they could worry about themselves. A recent RGS-IBG survey found that 51% of students who go on to study Geography at university do so because they rank “earning a good salary” as important (while only 19% said they ranked “doing ‘good’ through my job” as important). However, only a minority, even of that 51%, will ever earn enough to be able to afford private health care.
“Each of us can tell a story of the dismantling of public health care.”
 University of Birmingham
University of Birmingham
The state of the National Health Service (NHS) in the UK has always been the subject of debate, which often generates more heat than light. Two elements have often been linked: ‘privatisation of the NHS’ (over 933,000 Google hits) and ‘end of the NHS’ (a mere 203,000 Google hits). However, both of these debates have long histories. For example, Aneurin Bevan, the Minister of Health who created the NHS in 1948, wrote in his book In Place of Fear (1952) that recently announced legislation would ‘mutilate’ the service. More recently, government critics have ‘cried wolf’ at almost every NHS reorganisation since 1989. This article explores privatisation in health and social care, with reference to differences within the UK.
The definition of privatisation is contested, with the term used in many different ways along a continuum. The ‘minimal definition’ tends to be used by Government, and is largely concerned with ‘finance’, with services free at the point of use: we are not privatising the NHS because treatment remains (largely) free. The ‘maximal’ definition tends to be used by critics, and refers to any movement from public to private in provision, finance or regulation. In terms of provision or ownership, it is often considered that the NHS is fully public. However, it has always contained some private elements. For example, GPs, dentists and opticians are independent contractors (or small businesses). Put another way, it was only the hospitals that were nationalised.
In terms of provision, the term ‘creeping privatisation’ has been used since the 1980s, but it is creeping fairly slowly, currently amounting to some 10% of the NHS budget. However, this varies by sector. For example, while acute hospitals still remain public, areas such as general practice, mental health and hospice provision have always been less public.
Turning to finance, some regard the NHS as being (largely) free at the point of use because the most important and costly element – hospital treatment – is free. However, there have been some charges almost throughout the period of the NHS, such as charges for prescriptions, and optical and dental treatment. Bevan resigned from the Labour Cabinet in 1951 in protest about charges. Charging has broadly increased over time. There is some variation between the UK
nations. For example, Wales has free prescriptions. Scotland has free dental examinations for all, but requires payment up to 80% of cost to a maximum of £384 (with free treatment for particular groups such as those aged up to 26).
The final criterion of regulation is more difficult to assess. Regulation can act as a counterweight to provision: that if (a big if) properly regulated, then ownership does not matter. However, it could be said that we have more regulators (eg, Care Inspectorate in Scotland) but insufficient regulation.
The main problem of crying wolf with the NHS is that few took much notice when the wolf appeared for Long Term Care (LTC) which has now been significantly privatised. Unlike the NHS, LTC has always relied on significant amounts of ‘informal’ (unpaid, and often female) care, and has been subject to means testing, but originally in 1948 charges were set at similar levels to pensions. There has been a huge explosion in private provision since the 1990s. There have also been huge levels of debt for ‘self-payers’, which has led to people selling their homes to pay for care.
LTC exhibits perhaps the most obvious differentiation linked to political devolution. The Royal Commission into LTC, set up by Tony Blair, recommended free ‘personal care’ in 1999, which was rejected in England, but taken up by Scotland to provide free ‘personal care’ (but ‘hotel charges’ remain). In England, the Conservative government’s promise to ‘fix’ social care has resulted in a cap on lifetime costs on personal care, which will mean that some people will still have to sell homes. In Wales, a Labour / Plaid Cymru alliance has promised a ‘National Care Service’ (NCS) to provide ‘free’ social care within three years. In Scotland, the First Minister wished to build a “social care legacy equal in stature and impact to the creation of the NHS after World War 2.” The Feeley Review (2021) recommended an ‘NCS’ within a ‘human rights approach’. However, unlike the NHS, nationalisation or public ownership was ruled out. An NCS is clearly meant to be compared with the NHS. Bevan was very clear what an NHS meant. The term NCS should not be used if it is not free at the point of use (minimal definition, above) or publicly owned (maximal definition), and is not ‘in place of fear’.
Professor Martin Powell, Professor of Health and Social Policy,
“It is often considered that the NHS is fully public. However, it has always contained some private elements.”© Luke Jones
 , Pro-Vice-Chancellor and Dean, Otago Business School; Co-Director, Centre for Health Systems and Technology, University of Otago, Dunedin, New Zealand
, Pro-Vice-Chancellor and Dean, Otago Business School; Co-Director, Centre for Health Systems and Technology, University of Otago, Dunedin, New Zealand
Readers familiar with the UK NHS (the NHS) will find much in common with New Zealand’s health system. There are also some important points of difference. The two both have so-called national health systems, largely funded by general taxes and delivered through government-owned public hospitals and related facilities. Both also feature private provision, which delivers some public services. New Zealand was the first country in the world to pursue creation of a national health service. This was through the Social Security Act 1938, some ten years ahead of NHS establishment. This Act sought to create comprehensive social services including education, housing and retirement support, along with health care. Health care services were to be nationalised, with all professionals becoming government employees. Instead, in a historic compromise with the then British Medical Association NZ branch, resistant to nationalisation, the foundations of the New Zealand health system today were laid. This permitted general practitioners to retain private ownership and to generate income through patient service fees. It was agreed that the government would subsidise fees which were consequently brought down to a low level. Public hospitals would be free of charge with all professionals on salary fully funded by the government. Public specialists would be permitted to maintain a parallel private practice. Expenditure is today just over 9% of GDP; government provides around 80% of total funding, with the remainder from private sources. The social-insurance-style Accident Compensation Corporation covers injuries.
Over the years, government subsidies for general practice have not kept up with costs, and patient fees have increased to the point they are often prohibitive and a major access barrier. Nonetheless, New Zealand has a strong system of general practice. Those unable to pay often have their fees waived or will attend a public hospital emergency department where services are free. Around 40% of public hospital specialists also retain a private practice. There are no private emergency or intensive care facilities, so private specialty work is dominated by routine procedures such as hip replacements and cataract removal. Like the NHS, waiting lists prevail in public hospitals which are underfunded and face perpetual pressure to improve efficiency. Those with private insurance or ability to pay often seek private treatment where waiting lists are virtually non-existent. Interestingly, the same specialists unable to provide treatment in a timely fashion in the public sector can do so
privately. A significant proportion of elective work is privately provided. Critical backup and support for private patients with complications is provided in the public sector, taxpayerfunded. Patients are also not able to see a private specialist without a publicly-subsidised GP referral.
In contrast with the NHS, New Zealand’s services were built in the context of strong regionalisation which has persisted over time. Decision making and services vary hugely by district, exacerbated by a system of 20 local District Health Boards (DHBs) established in 2000. These have responsibility for service planning and delivery for a geographic area, and fund public hospitals, primary care and disability support services. Some 30 Primary Health Organisations (PHOs), established in 2003, channel government funding into various services and work with general practices for delivery. PHOs in areas with higher populations of Maori, Pacific or lower socio-economic status receive more government funding, which is used to reduce patient fees and improve services for these groups which are more likely to suffer ill health. From 2013, in an effort to integrate care planning and delivery, the government required each PHO to enter into an alliance with the local DHB.
The current arrangements will cease in July 2022 when significant reforms take effect. Guided by the Pae Ora (Healthy Futures) Act, a new national entity, Health NZ, will take over all DHB responsibilities and centrally plan and fund public hospitals and primary care services. In a first for the country, a new Maori Health Authority will do the same for Maori people. The two new entities will work in partnership, giving effect to core principles of the Treaty of Waitangi signed in 1840 between Maori and the Crown. Public hospitals will be funded separately from primary care. Considerable work is going into building new primary care locality networks, aimed at integrating a range of providers, including social services. A core goal of the reforms is equity and population health through national planning. An obstacle to this, which the reforms will not address, is the underlying institutions of parallel public and private systems, the latter of which does not serve the less well-off.
Gauld R, ‘New Zealand’, in R Tikkanen, R Osborn, E Mossialos, A Djordjevic, G Wharton (eds), International Health Care System Profiles, New York, Commonwealth Fund, 2020 (www.commonwealthfund.org/international-healthpolicy-center/countries/new-zealand)
Professor Robin Gauld
“New Zealand was the first country in the world to pursue creation of a national health service.”
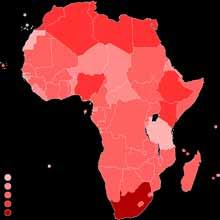
The Covid pandemic has had serious health and economic consequences right across the globe, and no country, it would seem, has been spared. African countries are no exception. Even in some quite remote rural areas in the continent, there have been Covid outbreaks, mainly attributed to migrants returning to villages from work in the urban areas. However, the available data suggest that the direct clinical effects of Covid in Africa may have been less severe than elsewhere. Just over 17% of the world’s population is located in Africa, but Africa has experienced only about 3% of the world’s recorded Covid cases and just over 4% of global deaths. Quite why this is the case is still being debated and researched, but there are two possible explanations being explored. The first is that there has been a significant under-reporting of both positive cases and deaths in many countries. There has been a well-reported shortage of testing kits in Africa, so it would not be unreasonable therefore for there to be an under-reporting. Secondly, there is a view that the relative youth of the African population may be a factor. It is well-established that elderly people are more vulnerable to Covid than younger people, and the median age of the population in Africa is 19.7 years, compared to 40.2 years in the UK. In Africa, only just over 3% of the population is over the age of 65 years; in the UK the equivalent figure is 18%. However, the same cannot be said for the indirect consequences. Many clinics have reported a rise in the incidence of nonCovid diseases as access to primary health care has been impacted. This has been because of lockdowns which have resulted in the reduced availability of transport for people to attend clinics, as well as staff shortages at clinics themselves through staff illness. People in pre-Covid days would have regularly attended clinics when needed, and been tested for malaria, tuberculosis and HIV, among other things, but during the pandemic, testing for these diseases has been much reduced, leading to more serious cases of all three conditions developing before being able to be treated.
Children’s education has also been badly affected. Schools in most African countries have been closed for varying periods of time during the pandemic. In Uganda, schools were closed for over 18 months, for example. Unlike in the UK and other high-income countries, online learning from home has been largely unavailable, except for a very few wealthy, mainly urban families. For the majority, lack of ownership of computers, tablets and smartphones, lack of access to the internet, and, in all too many cases, lack of electricity precluded this as a means of continuing learning outside school. One of the more successful Millennium Development Goals was focused on providing access to universal primary education, with 91% of children in Africa by 2015 receiving a full programme of primary education. Sadly, these gains have been set back by the pandemic, but the full impact is yet to be evaluated, although there is evidence already from some areas that fewer girls than boys are returning to schools when they re-open.
Economic gains over the last couple of decades have also been damaged by the pandemic. The reduction in global demand, especially during 2020, has had a serious impact, especially on those African economies which are more interconnected with the global economy. Reduced global demand for copper, which typically provides about 30% of Zambian government revenues annually, has had a major negative impact on that country’s economy. An important export for Kenya is cut flowers, being Kenya’s third largest earner of foreign exchange in a typical year. In 2020, as the pandemic started to grip the world, exports of cut flowers, most of which are to Europe (mainly to the Netherlands and the UK) declined precipitously from 17,600 tonnes in February 2020 to only 8,000 tonnes in April of that same year. This very much reflected both the cancellation of flights out of Kenya to Europe, the expense of chartering cargo aircraft, and the reduction in consumer demand as weddings and other events and celebrations were curtailed as a result of lockdowns in Europe and elsewhere. As lockdowns eased, the market built up again, but it was not until August 2021 that the volume of exports had recovered to pre-Covid levels. It is estimated that up to one million people depend either directly or indirectly on the cut flower industry in Kenya, and a great many of these lost their jobs and their income.
For those countries where tourism represents a significant element of economic activity, notably South Africa, Kenya, Tanzania, Botswana, and increasingly Mozambique and Namibia, the decline in tourist arrivals, and the drop in tourist income, has been calamitous. In South Africa, pre-Covid tourism generated about R130 billion annually (about £6.3 billion), and contributed about 8% of Gross Domestic Product, as well as about 4.5% of employment. In 2019, international arrivals amounted to 10.2 million people, but this dropped to 2.8 million in 2020. In Kenya, where tourism makes up about 8% of GDP, international arrivals dropped from just over two million in 2019 to 568,000 in 2020. Tanzania saw its tourist revenues drop from US$2.6 billion in 2019 to less than US$1 billion in 2020. The impact on national economies, local employment and household incomes, without social security or furlough safety nets, has been severe, and countries are still counting the cost.
Whereas these macro-level impacts have been challenging in the extreme, smallholder farmers at the local level have not been immune from the economic impacts of Covid either. Markets have been closed for periods of time, and transport for inputs has been badly affected, which, in turn, has impacted agricultural production and household incomes in different ways. Experiences from Malawi are very instructive. Although Malawi did not experience a complete lockdown in response to the Covid pandemic, nonetheless there were school closures, restricted opening of marketplaces, gatherings restricted to fewer than 100 people per group,
Dr Boyson Moyo, Lilongwe University of Agriculture and Natural Resources; Professor John Briggs, University of Glasgow
“Many clinics have reported a rise in the incidence of non-Covid diseases.”
and vehicle capacities reduced to 60%. This had a significant impact on smallholder farmers, sometimes in unexpected ways.

For the majority of small-scale farmers, particularly those who rely on grain production, especially maize, marketing opportunities were severely curtailed as many markets were closed and the movement of those buying agricultural products on sale in towns was also severely restricted. Because of the reductions in the seating capacity of passenger vehicles, and limited sizes of gatherings for mobile markets where major crop produce sales often take place, demand necessarily declined and smallholder farmers’ incomes and livelihoods were badly hit. The Government of Malawi estimated that the country’s agri-food system suffered a loss of 10.4% over the first two months of the pandemic, and although it stabilised after that, it did so at lower than pre-pandemic levels.
Although grain producers were hard hit, ironically a small minority of other smallholder farmers fared quite well. There was a widespread belief among many in the population that crops such as ginger, lemon and green leafy vegetables were key in keeping people healthy and resistant to Covid. Hence, these crops have seen an increase in demand during the pandemic. The challenge, however, for producers was that ginger and lemon production can only come from mature plants, so the increased demand did not directly result in immediate increased production. But for those farmers who were already producing lemons and ginger there was a small and unexpected windfall increase of incomes. Happily, the production of vegetables offered more flexibility as these could be sown and grown quickly, and as restrictions relaxed on marketplaces, those farmers who were able to produce such crops benefitted. An unexpected consequence of school closures was that students who were out of school became useful in agricultural production, not least for the production of vegetables which were in high demand. Labour shortages which in the past might have negatively impacted production were not now, by and large, an issue.
A further unexpected consequence is that there is a view that with people spending more time on their farms instead of in school or in their other jobs because of the pandemic restrictions, this may have had an impact on reducing the spread of the virus. Indeed, with social distancing and the requirement to keep away from crowds in place as part of the government’s response to the pandemic, farms and vegetable gardens provided spaces for safe isolation and social distancing without the need for putting on a mask.
Africa has not escaped the pandemic and the consequences have been significant. How Africa recovers economically is going to be an interesting challenge over the next few years.

“The impact on national economies, local employment and household incomes has been severe.”
 Dr Julia Grace Patterson, Chief Executive, EveryDoctor
Dr Julia Grace Patterson, Chief Executive, EveryDoctor
The NHS has just experienced the most extraordinary challenge in its history. The pandemic has heaped enormous pressure upon a service which was already struggling to cope after a decade of government underfunding (during the 2010s, the real terms growth in health spending was the lowest since the NHS’s inception). As a result, both of cumulative underfunding and of treatment delays because of Covid-19, the NHS in England currently has waiting lists of 6.1 million patients. These are the longest ever on record.
One might expect that in the face of such an extraordinary national healthcare crisis, the response from our politicians would also be extraordinary. Extraordinary funding increases. Extraordinary measures to support current staff and recruit new ones. Extraordinary efforts to transform the NHS into a service which truly fits the healthcare needs of the public in 2022. We might expect that having lived through a pandemic which has claimed the lives of over 150,000 people in the UK, healthcare would (finally) be put front and centre of this government’s agenda. Sadly, this does not appear to be the case.
There is much fanfare currently about proposed NHS funding increases, which the government plans to implement until 2024 2025. And yet this increase (which will amount to a 3.5% spending increase in real terms) is lower than funding increases in the 1960s, 1970s, 1990s and 2000s. In short, it’s a much more paltry investment than the government is letting on.
As well as this lukewarm investment in the health of the nation, there is a Bill travelling through the UK Parliament at present called the Health and Care Bill. It is causing enormous concern to NHS campaigners, who believe that the Bill will accelerate NHS privatisation. The Bill involves fragmenting the NHS in England into 42 ‘Integrated Care Systems’, governed by Boards, which look as though they’ll be allowed to give seats to private healthcare providers. There is much discussion about Bill amendments at present, with campaigners and many politicians alike trying to remove the ability of private healthcare providers to occupy these Board seats. Whether or not this is achieved, the Bill has broader and deeper consequences for the NHS. It contains elements which will allow the Secretary of State for Health and Social Care to intervene in local services. It contains a worrying policy called “discharge to assess” which means that a patient can be discharged from a hospital before having an assessment from the services which will provide continuing care for that person in the community. And
it’s bound up in difficult-to-decipher rhetoric which sounds progressive, but has seemingly little in the way of practical detail (the government’s Integration and Innovation White Paper which preceded the Bill talks of putting “pragmatism at the heart of the system” and claims it will “set aside bureaucratic rules”). The thing is, every NHS shake-up contains a great deal of bureaucracy. Old rules will simply be replaced with new rules. And it seems that this particular shake-up will remove some power from experienced local healthcare providers, and transfer it to the Secretary of State. Our current Secretary of State for Health and Social Care has no background in health. Neither did his two predecessors. It is unclear to many of us why a politician in Whitehall would presume to make better decisions for patients than a local clinician.
The Bill is winding its way through Parliament, and at the time of writing (February 2022) is awaiting its third reading and a vote in the House of Lords. It may be voted down, and if so will then have to return to the House of Commons. But quite frankly, even with successive ping-pongs back and forth, tweaking amendments here and there, this Bill is simply the wrong Bill. It does not prioritise the welfare and support of staff who have endured the trauma of the pandemic and the incredible strain of working in an understaffed and underfunded workforce for a decade. It does not consider how that workforce can be buoyed up, grown and nurtured, to provide fantastic care to NHS patients in the decades to come. And it does not appear to tackle the enormous problems of inequitable care across the NHS, which disadvantage many patient groups.
We desperately need a national conversation about the future of public healthcare in the UK. We need politicians to admit to the existence of NHS privatisation (which is embedded, and takes up around 7% of the annual budget in England). We need to think hard about the kind of NHS we want. And it is time, as we emerge from the acute phase of this pandemic, to think radically. The government needs to listen; listen to patients, listen to experts, listen to healthcare providers. It needs to scrap this Bill, and write a better one.
“We desperately need a national conversation about the future of public healthcare in the UK.”
No one I know has set New Year resolutions for 2022 that do not include making Covid history. The latest scourge of Omicron takes us into the third year of seemingly endless disease and death. Yet we now know Covid-cycles of destruction can be broken by vaccination and testing. But vaccination and testing have to happen everywhere if the virus is to be contained. And to bring Covid under control, Boris Johnson and President Joe Biden should appoint a global coordinator. Their task: to urgently transfer the vaccines and testing equipment, that the richest countries currently monopolise, to the poorest countries still without them. Only then, by backing up the work of the World Health Organisation (WHO) and the global vaccines agency, COVAX, can we halt the threat from new variants.
For even as the West has reached 70% adult vaccination, 90 countries have yet to meet the worldwide (end of 2021) target of 40%. In low-income countries the figure is still only 4%. Even now, three in four African health workers, who are risking their lives to save lives, remain unvaccinated. In Africa’s biggest country, Nigeria, which has a population of over 200 million, only one in 50 people (2%) are fully vaccinated. And another huge country, Ethiopia, with over 100 million people, remains frighteningly unprotected, with only 1.2% fully vaccinated. But in some countries, immunisation rates are even below 1%: Chad 0.5%, DR Congo 0.1%. Worse still, in Burundi, the vaccinated account for just 0.04%, just one in every 2,500. With the low coverage, it is not surprising that these countries are fertile grounds for the disease to spread.
It also puts next year’s WHO global vaccination target, of 70% by July, in jeopardy. We’re failing because the richest countries continue to stockpile vaccine and equipment supplies with the result that, even after all of us have boosters, there is a surplus in the richest countries and a shortage in the poorest. Cooperation between rich and poor countries failed so badly in 2021 that 60 million vaccines, that could have been sent from the global north to the global south, passed their ‘use by’ date and, instead of being sent southwards to prevent the spread and mutation of Covid, had to be destroyed. I hate waste. So does the British public. Lives could have been saved by sending Africa the unused vaccines before they expired.
Quite simply we are having to recreate Nightingale wards in the United Kingdom to cope with possible emergency admissions here because we have failed to halt the emergence and spread of the Omicron virus abroad. And it seems we have also inexcusably sat on over-ordered PPE surpluses, letting medical equipment like masks and
gowns also pass their ‘use by’ date instead of being sent to countries in desperate need of them – because of a predetermined cap imposed on the overseas aid budget.
And as long as we waste vaccines and can’t offer unused equipment to people in Africa and elsewhere, global medical experts are predicting 200 million further Covid cases for 2022. Almost 5.5 million lives have now been lost to Covid.

Unless we get vaccines and testing equipment to the global unvaccinated, they anticipate it could lay waste to five million more lives in the months to come.
The longer we delay vaccinating the unprotected, the more likely the virus will keep mutating. But with 1.4 billion vaccines being produced every month, and nearly 20 billion by June (in total), we have the capacity to vaccinate everyone in the world. To control the disease also requires testing – and again, we have failed to honour our promises. Only one in 250 of the Covid tests administered worldwide have been administered in low-income countries. So, in 2022, to end the pandemic, we must stop the underfunding of vaccinations, testing and medical equipment needed in low-income countries.
President Biden will recall his Vaccine Summit in the first weeks of 2022. On the agenda should be a ‘fair shares’ agreement, with America and Europe guaranteeing more than half the $23.4bn cost of getting vaccines, testing and other medical equipment to the poorest countries. Big international financial institutions, like the World Bank and the IMF, should be asked to come up with the cash needed to build in-country capacity to administer the vaccines, staff the makeshift vaccination clinics and help prevent future pandemics. And if we need more cash to save lives, let’s try some innovative ideas. France has raised $1.25bn for global health since 2006 through its tax on airlines. $100bn of the $650bn in special drawing rights (new international money created by the IMF) could be quickly deployed to provide resources for poorer countries to buy the necessary medical supplies. The richer countries could leverage $2bn of loan guarantees into $10bn of additional resources for poorer countries. During the financial crisis of 2009, we underpinned the world economy with $1.1tn of support. The medical price tag for 2022 is $60bn, only a fraction of what was spent in 2009 and certainly a fragment of what it’s costing us now in lost output and lost trade. It’s the best investment the world can make, and the best ever insurance policy to stop the agony of lost lives.
This article is extracted with permission from an article written for the Daily Mirror, available at www.mirror.co.uk/ news/politics/five-million-more-lives-could-25843975
“Vaccination and testing have to happen everywhere if the virus is to be contained.”
 Axel Heitmueller, Senior Associate Fellow, Tony Blair Institute for Global Change
Axel Heitmueller, Senior Associate Fellow, Tony Blair Institute for Global Change
I look back at the early days of the pandemic with a mix of cold sweat and wonderment. Those early months in spring 2020 were filled with great anxieties about the ability of the NHS to cope with the rapidly rising numbers of hospitalisations. There was no cure, there was no vaccination, and there was a great sense of uncertainty. The spectre of people dying in corridors in Italian hospitals loomed large. No one knew when cases would peak.
At the same time, up and down the country, something extraordinary was happening. NHS organisations that had been in fierce competition for years found ways to collaborate. Innovation was adopted in days not years. Stifling bureaucracy was suspended. For the first time in my decade in the NHS, action preceded planning. There was no playbook, no business case template. A burning hot platform instilled purpose that couldn’t be served by postponing action until tomorrow.
Maybe naively many of us felt that this might be the beginning of a new chapter in the provision of health and care, allowing us to hang on to the momentum, the collaboration, and focus on transformation. A strong collective purpose, an existential threat leading to rapid change as opposed to plans for change. That sentiment didn’t last very long. Midway through April the Covid case numbers finally started to turn and with them the elastic band of change snapped back fast.
On 29 April 2020 the NHS London regional leadership issued a letter asking all London designated Integrated Care Systems (ICS) to produce a transformation plan within ten days. This was to address 12 specific expectations including a high-level financial summary. To all intents and purposes, an impossible ask not least because everyone locally was exhausted, many were recovering from Covid themselves.
The muscle memory of NHSE [NHS England] kicked in with a vengeance.

By 10 May, we did submit a plan; the NHS always does. I’ve not counted the opportunity and real costs of those ten days and nights, but it will have been considerable.
It will come as no surprise to those who have gone through the motions many times before in the NHS that this plan was never
delivered. It was never written to be deliverable. In the months that followed, it was simply superseded by new plans and instructions.
Schrödinger’s NHS cat is the illusion of top-down change –always present, never to be seen. If half the plans for change published in the past decade had actually been implemented, the NHS would be a beacon of transformation. They weren’t and as a consequence it ranks towards the bottom of international league tables for health outcomes. This is increasingly impossible to sustain. Unprecedented sums of money are flowing towards health and with that come public and political expectations. At the same time, the first major health legislation in a decade is going through Parliament and Covid has demonstrated that accelerated change is possible.
Forthcoming White Papers, which will set out the detailed policy underpinning the legislative reforms in the coming weeks and months, are an opportunity to think harder about a change model that delivers on these expectations. There is much to learn from recent decades about the role of different policy levers. The evidence is increasingly strong: healthcare as a complex ecosystem can’t be meaningfully controlled top-down. A command-and-control style may provide the illusion of being in charge, but it most certainly does not foster innovation and
“Unprecedented sums of money are flowing towards health and with that come public and political expectations.”
change of the nature that is required. Market forces have also had limited impact. Reaching for structural change on its own also avoids the real work; form should follow function. Instead, implementable change requires local energy, aligned policy levers, collaboration, and a level of autonomy.
Less top-down and more local freedoms will run against the deep instincts of the Treasury which rightly seeks accountability for public spending. A central question for the reform agenda is therefore how to ensure accountability while moving towards greater local autonomy.
I see five potential areas worth considering for a progressive public management playbook to achieve meaningful change:
1 Empower and trust citizens to hold local systems to account: local autonomy may come with local variation in care. Therefore, a necessary feature of a more devolved system should be a transfer of trust and power to citizens to hold their local healthcare system to account. Currently it is very hard for patients to understand what good care should look like. Addressing this will not only support direct accountability between a patient and caregiver but also accelerate the adoption of best practice innovation.
2 Rely on local democracy: the governance of Integrated Care Systems offers an opportunity to include local government. This opens the door to a progressive version


of Local Area Agreements between different public sector organisations and citizens through their elected representatives. Regions differ in their health needs. Trading off resources and needs within local preferences and democratic structures will provide a different quality of legitimacy compared to traditional NHS plans.
3 Reward learning as part of accountability: making integrated care happen will require systems leadership. Compared to organisational leadership, this is a fundamentally different style. Part of systems leadership is acknowledging and becoming comfortable with not having all the answers. Systematic and continuous learning will be essential in driving change and should be explicitly rewarded and nurtured.
4 Focus on fewer, essential measures: with more accountability concentrated locally, central control and regulation can retreat to functions that truly benefit from a national perspective and scale. This includes setting a small set of non-negotiable baseline safety and operational measures. Healthcare is evidence based and closing the gap between what we know and what we do is essential. Healthcare is also a high-risk business, and the NHS does not always get it right.
5 Move towards dynamic, outcome focused measures: whether for national or local purposes, we should reduce the burden of data collection. Real World Evidence from electronic patient records and app-enabled, patient-led data collection are increasingly routinely available. This offers opportunities to compare a broader and increasingly outcome-based set of measures across ICSs and providers in more timely and agile ways. It may also safeguard against the gaming of data collected specifically for performance management.
Sharing power with local organisations, citizens, and elected politicians requires a significant cultural and behavioural shift in NHS England and the centre of government. The pandemic offered us a glimpse of a much more innovative and dynamic health and care system, and the technological leap it created makes radical reform a realistic prospect. Seizing that opportunity will require political courage. But then, insanity is doing the same thing over and over and expecting a different result.
“Healthcare as a complex ecosystem can’t be meaningfully controlled topdown.”
We are surrounded by feedback. From hotels to holidays, meals to music, we now provide or seek out feedback about almost every kind of product or service you can imagine. But what about healthcare? In most countries, including the UK, it isn’t common for clinics and hospitals to ask for or display patient feedback, and even if it were, what would be the purpose? Healthcare, especially in emergencies, is not usually something people look forward to choosing and using.
At Care Opinion, a non-profit social enterprise, we’ve been sharing online patient feedback for over 15 years now. We’ve learned that feedback, and particularly online feedback, can be complex, multi-layered and highly relational, with a range of powerful and surprising impacts for both patients and healthcare staff.
At careopinion.org.uk many thousands of people have shared their specific experiences of health and care: childbirth, emergencies, operations, mental health issues, addictions, end of life. These stories are by turns heart-warming or angry, grateful or desperate, routine or life-changing. But all are about things that mattered to the person experiencing care, and sometimes about services that could have been better. We link these stories to the local services which provided the care, and aim to alert staff (by email) to their feedback. And then staff respond: around 75% of stories receive a response on average, rising to over 97% in Scotland and Northern Ireland. That’s because in those jurisdictions Care Opinion is now the online platform of choice for feedback across the healthcare system, used by all hospital, ambulance, mental health and many other services. In addition, feedback flows upwards to regulators, policymakers and politicians, and outwards to medical and nursing schools, analysts and researchers.
To give a simple but significant example: ‘Caryn’ shared feedback about visiting her new baby in the neonatal care unit. She arrived to find her baby smelled “like one of the nurses’ very overpowering perfume.” Nicole, the nurse manager for the service, responded quickly with an apology and a policy change: “clinical staff will no longer wear any perfume to work.”
Since we started doing this, in 2005, a body of research evidence has slowly accumulated to describe the motivations of feedback authors, the perceptions of staff hearing these stories, and the wider impacts on care.
There are three leading reasons why people post their feedback: to praise services, to inform other patients, and to improve standards of care. People don’t see the feedback they give as ‘data’ (the prevalent health system perspective) but instead as ‘care’ for the health services they use and rely on even when their feedback is critical. So perhaps unsurprisingly, it matters to authors that their feedback reaches the people it is about.
But many staff are wary of online feedback, perhaps expecting the negative onslaught common on unmoderated social media. So it is remarkable that, over time, staff reading and responding to online feedback report positive effects on morale, confidence and pride. One nurse told us, “When I read this feedback, I remember why I became a nurse.”
Having established Care Opinion as a sustainable, effective platform for individual services, we’re now becoming

interested in wider, system-wide issues such as safety and team culture. For example, some evidence suggests that expressed patient gratitude can improve the performance of medical teams, and witnessed gratitude may increase prosocial behaviours in onlookers. Could we somehow channel the steady flow of gratitude expressed through Care Opinion in ways which directly improve organisational culture and performance?
The stories shared on Care Opinion form a unique resource of experience narratives for health professional education and training. And text mining techniques are being used to analyse this narrative data at scale, identifying patient safety concerns and indicators of poor culture which may warrant the attention of regulators. So what have we learned over the past 15 or more years?
First, that despite the fears of healthcare staff, the overwhelming majority of patients are giving feedback because they want to help both staff and future patients. Second, that by sharing experiences of care safely and openly, we can foster trust and understanding between those proving care and those using it. And third, that change in healthcare may be glacially slow, but is not impossible. In many parts of the UK, patient feedback has now become ‘the new normal’.
“Many thousands of people have shared their specific experiences of health and care.”
 Professor D Robin Taylor
Professor D Robin Taylor
I have known Wayne* since he was a medical student. He is conscientious and caring, but maintaining these qualities as a young doctor is being challenged – not by shift work or long hours but by his experience of ‘the system’. I met him unexpectedly leaving the hospital on a dark evening last November. He was not his usual self. He was angry. “I have spent half the day at loggerheads with my seniors. I was told to set a patient up for non-invasive ventilation [NIV]. But the man is dying. It was going to achieve nothing. The patient himself didn’t want it. I stupidly did his blood gases [a test that measures oxygen and carbon dioxide in the blood] and fed the results back over the phone. All I got was the order to start NIV. It was terrible.”
In fact, Wayne decided not to start the NIV. It was the right decision, but it came at a cost. Mercifully there were good outcomes. The patient received palliative treatments and died peacefully. The case was openly discussed at a multidisciplinary team meeting. Wayne was supported in his decision to step back from delivering treatment that was futile and contrary to the patient’s wishes.
Wayne’s experience is common. In the delivery of acute services in hospitals, the ‘system’ is driven by the idea that when a patient deteriorates, more is better. More investigations. More treatments. Regrettably it is often only when all else fails that it is acceptable to think differently. This matters. Nearly 30% of patients admitted to Scottish hospitals are in the last year of life. In many instances, saving life is the right thing to do. But in some it is not. There comes a point when ‘doing everything possible’ is simply wrong. This is not just because the medical treatments may be ineffective, but because they are so often harmful.
Trying to fix a pathological process – even if it is reversible –is not necessarily right for all of the people all of the time. Likewise, mitigating risk via standardised once-size-fits-all protocols has unintended consequences. In the ‘system’, protocols can morph into laws that must not be broken regardless of consequences. Junior doctors in particular often stick rigidly to a protocol rather than risk criticism. Worse, they then experience moral distress; defined as discordance between what is the right thing to do and what they feel required to do.
Can we escape from the tyranny of ‘fix it’ medicine and from the harms that patients suffer when treatments are at odds with their best interests and even against their (often ignored) wishes? Yes, we can. Societally, we need to agree that modern medicine has limits and that being reconciled to human mortality doesn’t mean failure. Atul Gawande made the point in his book Being Mortal.
There are also practical ways forward. First, the context of a patient’s acute deterioration needs to be considered. Wayne’s patient had had multiple admissions and progressively declining health over two years. Giving him ‘the benefit of the doubt’ one more time would have been a deceitful cop-out. Treatment goals that are realistic rather than falsely hopeful
are what was needed. These goals need to be explicit and well communicated. Palliative treatments should be sooner and not later.
Second, there is shared decision-making. Wayne discussed the patient’s situation with him, including his personal priorities, and these were honoured. This approach goes a long way to avoiding inappropriate medical interventions. Third, harm avoidance should be a priority especially in the frail and vulnerable. There is an old maxim in medicine that says “primum non nocere.” First, do no harm. But what about the patient who, after briefly responding to treatment, deteriorates further? When should we let go rather than cling on? Nurses often know instinctively when clinging on is the wrong thing to do. But letting go is counter-intuitive to many doctors. When the dilemma is pushed aside and isn’t openly addressed, bad things happen. In some, the dying process is unnecessarily prolonged.
As a clinician I know all too well that in the circumstances of severe illness, everyone is stressed and anxious. That makes it difficult to process complex information about an illness and its treatment. Fear and urgency take over. For some sons and daughters, the news that their parent is dying comes as a shock and they want to put up a fight. But sometimes it’s the wrong fight. Relatives’ expectations can be unrealistic.
‘Never say die’ and ‘do everything possible’ have become more and more demanding for all of us as technological advances have increasingly incentivised the ‘fix it’ mentality. By all means let us emphasise the power in medicine to save and sustain life. But let’s also avoid the problems that come from insisting that endless attempts to fix things are always the priority in urgent medical care. Setting aside one-sizefits-all curative intent when it’s not appropriate needs to be legitimised and openly embraced in the system that is the NHS.
* His name has been changed to protect his identity. Professor Taylor is a consultant respiratory physician and lives in Edinburgh.
“There comes a point when ‘doing everything possible’ is simply wrong.”





1. A sperm whale and dusky dolphins, photographed from a doorsoff helicopter flight in Kaikoura, South Island. | 2. A beautiful show of colours just before sunrise at Lake Matheson, Fox Glacier, South Island. To the left stands Mount Tasman, and to the right Aoraki Mount Cook, New Zealand’s tallest mountain. | 3. Sunset through the pōhutukawa trees at the rugged west coast Piha Beach, Waitākere, Auckland, North Island. | 4. Sunrise at Te WhanganuiA-Hei (Cathedral Cove Marine Reserve) in the southern part of Mercury Bay on the Coromandel Peninsula, North Island. | 5. A winter sunset at the foot of New Zealand’s tallest mountain, Aoraki / Mount Cook, at Hooker Lake, Aoraki / Mount Cook National Park, South Island. | 6. Cape Reinga, the most spiritually significant place in New Zealand for Maori, where the Tasman and Pacific Oceans meet, the northernmost point in New Zealand. | 7. Autumn sunrise at Lake Wānaka, South Island; the famous Wanaka Tree started life as a farmer’s fencepost over 100 years ago. | 8. Sunrise at Tititea / Mount Aspiring, Mount Aspiring National Park, South Island; the Māori name ‘Tititea’ translates to ‘Glistening Peak’. | 9. Sunrise from Te Mata Peak, Hawkes Bay, North Island; seashell fossils over two million years old were part of the sea floor which tilted and shifted to create this mountain. | 10. Sunset along the foreshore to Milford Sound, Fiordland, South Island, carved by glaciers during the ice ages, and dubbed by Rudyard Kipling as the ‘eighth wonder of the world’. | 11. Sunrise at Cape Egmont Lighthouse and Mount Taranaki, Taranaki coastline, North Island. All images © Rach Stewart, www.rachstewartphotography.com Rach is a professional New Zealand landscape photographer and workshop leader who is inspired by landscapes and loves to travel to new places finding the all-important elements that connect humans with nature. She lives for travel and adventure and capturing the beauty created by our natural world.






This time last year we featured an article on Covid-19, to help understand the statistics behind the pandemic and how the UK and Scotland were performing compared to other countries around the world. At the time, the UK had one of the worst per capita Covid death rates in the world, after a slow and incoherent early response, whereas a small number of countries who reacted more definitively saw many fewer deaths. Another year on, much has changed, not least the wide rollout of the vaccine, but it can still be difficult getting clear information, so we thought it would be helpful to look again at the statistics.
Globally the virus is still prevalent, now surpassing 5.68 million deaths compared to 2.19 million this time last year, an increase of 160% year on year. The number of daily new infections globally has risen to around three million new cases per day, so the chance of further mutations remains high. At the height of the pandemic last year this figure was around one million.
The UK death rate (per capita) is still relatively high, though several countries, especially around eastern Europe, have seen deterioration in their success in limiting the virus, so the UK’s position is less stark than it was. The biggest change of the last 12 months has been the successful introduction of vaccines. This has undoubtedly helped reduce mortality but as infection levels have increased so substantially, the number of deaths is still increasing.
This time last year there had been 100,162 deaths from Covid in the UK. When I wrote this article (in January 2022), according to UK government statistics there were 151,987 deaths within 28 days of a positive Covid test (or 174,233 deaths if you count those which state Covid as the cause of death). Both figures help evidence that the rate of people dying after becoming infected has fallen over this period, from 2.7% of infections across the UK to around 1% currently. It is
likely that this is in part at least a result of more testing, but it is most likely a testament to the success of the vaccines.
In Russia, where vaccination levels sit at only 47.8%, the number of deaths in this second year have increased from 71,076 in January 2021 to 321,990 in January 2022. The USA, India and Brazil have all seen at least double the deaths of the first year of Covid too.
In the UK as a whole, 71.7% of people are ‘fully vaccinated’ (at least two jags). This compares favourably with the global average (51.7%) and with the US (63.5%), and is comparable with many other western countries. France and Italy have vaccination rates of around 76.3%, and Portugal has 90.5%. In the developing world, access to vaccines has been much more restricted. In Egypt, vaccination levels are sitting at 25.2% and in Bangladesh 35.9%, but countries like Nigeria and Ethiopia are only sitting at 2.5% and 1.4% respectively. The problem with any virus, of course, is that it will mutate anywhere, so this level of global non-vaccination remains a risk for all of us, and risks ever more variants.
According to the Office for National Statistics, in England at least, over the period 1 January to 31 October 2021, the age-adjusted risk of deaths involving Covid-19 was 96% lower in people who had received a second dose compared with unvaccinated people.
In Scotland, we have the highest rate of vaccination in the UK (74.4%), the lowest infection rate, and the second-lowest death rate (after Northern Ireland). Although we have lost over 10,000 people to Covid since the beginning of this crisis, the measures taken appear to have been more effective than those in England, which has had a consistently higher death rate per capita. By contrast, New Zealand, which has a similar-sized population, has seen only 52 deaths over the same period, and now the vaccines are available, hopefully will not ever have to face the same toll that many in Europe have paid.
UK statistics are available from the Office for National Statistics (ons.gov.uk), and the UK Coronavirus Dashboard (coronavirus. data.gov.uk/details/cases). International data is available from Johns Hopkins University COVID-19 Dashboard (coronavirus.jhu.edu/ map.html), the World Health Organization Coronavirus (COVID-19) Dashboard (covid19. who.int), ourworldindata.org/covid-vaccinations, and www.worldometers.info/coronavirus.
Mike Robinson, Chief Executive, RSGS
“This level of global nonvaccination remains a risk for all of us.”
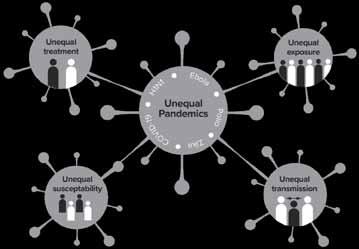 Health Sciences Institute,
University
Health Sciences Institute,
University
There are significant geographical inequalities in health. For example, there is a nine-year gap in male life expectancy and a seven-year gap in female life expectancy between the most and least deprived neighbourhoods of the UK. These geographical patterns in health are also evident in Europe, North America and globally. Covid-19 provides a key example of these geographical inequalities in health: Covid-19 death rates are twice as high in the most deprived areas of the UK. This article examines these inequalities in Covid-19 in more detail and explores how Covid-19 and inequality have combined to produce a syndemic pandemic.
Even in the first stage of the pandemic (March to June 2020) clear evidence was already emerging from a variety of countries of geographical inequalities in Covid-19. USA analysis found that socio-spatial gradients were found in terms of infection levels in New York City, with dramatically increased risk of death observed among residents of the most disadvantaged counties. In Canada, a higher percentage of cases was observed in the neighbourhoods with the lowest average income levels compared to the highest. Large-scale analysis of the impact of deprivation on Covid-19 mortality in Scotland during the first year of the pandemic (March to May 2021) found that the risk of death was more than twice as high in the most (86.5 per 100,000) compared to the least (38.2 per 100,000) deprived neighbourhoods. What explains these stark geographical inequalities in the Covid-19 pandemic? The pathways linking deprivation to Covid-19 are multiple: Covid-19 is a syndemic pandemic. It acts synergistically with – and exacerbates – existing social, economic, and geographical inequalities. The concept of a syndemic was originally developed by the anthropologist Merrell Singer when he examined the relationships between HIV/AIDS, substance use, and violence in inner-city areas of the USA in the 1990s. A syndemic exists when risk factors or co-morbidities are intertwined, interactive and cumulative –adversely exacerbating the disease burden and additively
increasing its negative effects. For the most disadvantaged communities, Covid-19 is being experienced in this way: a syndemic pandemic.
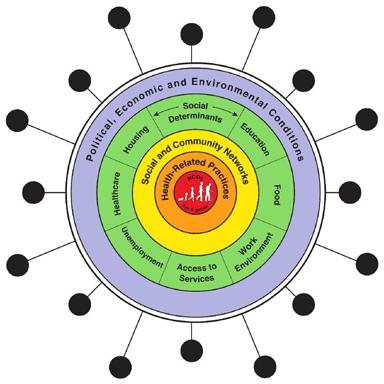
Existing inequality thereby increases adverse Covid-19 outcomes (as with other pandemics) through four pathways: increased vulnerability, due to a higher burden of chronic conditions (such as diabetes, respiratory conditions, heart disease) that increase the severity and mortality of Covid-19. increased susceptibility: immune systems weakened by long-term exposures to adverse living and environmental conditions make people from deprived communities more vulnerable to infection from Covid-19. increased exposure as a result of inequalities in working conditions; lower-paid workers are much less likely to be able to work from home and are more reliant on public transport. increased transmission: inequalities in housing conditions contribute to inequalities in Covid-19, as deprived neighbourhoods are more likely to contain houses of multiple occupation, and smaller houses with a lack of outside space, as well as to have higher population densities.
Covid-19 struck within a context in which there were already extreme, and rising, health inequalities in most countries. Now the pandemic is also being experienced unequally. What does the post-Covid future hold for health inequalities? And what can be done to reduce them? This all depends on how policy makers in different countries choose to react. Research into previous periods of crisis suggests that governments can mitigate the longer-term health inequalities impacts by improving public health and healthcare services, increasing access to public services to support those with social or health needs, and maintaining and enhancing social security safety nets. The longer-term effects of Covid-19 on inequalities depend on public policy choices.
Professor Clare Bambra, Professor of Public Heath, Population
Newcastle
“A syndemic exists when risk factors or co-morbidities are intertwined, interactive and cumulative.”
Thesyndemic of Covid-19 (reproduced from Bambra et al, 2020, with permission from BMJ Publishing). Pathways to pandemic inequalities.

Health care services are not free at the point of delivery in Nigeria and have to be paid for by users. Unfortunately, about 70% of the Nigerian population live below the poverty line and are too poor to pay for good medical care. Consequently, most of the poor have resorted to self-treatment by using local herbs, many of which are of doubtful quality and poor efficacy, and which can have unknown side effects. Others patronise ‘quack’ doctors or unofficial medicine stores to purchase relatively cheap drugs, which are frequently found to be fake and ineffective, and which can often result in serious side effects or even death. The standard of hygiene is very low in many areas, as the majority of people do not have access to treated, safe water. Sanitation is poor, with trash and refuse littering human environments. Many houses lack latrines or toilet facilities, which can result in high levels of environmental contamination with human waste. All these factors encourage the proliferation of disease agents and vectors, and the transmission of many infections. Consequently, people are exposed to various health hazards. Communicable diseases such as malaria, cholera, typhoid fever, dysentery, intestinal helminthiases, gastroenteritis, schistosomiasis and respiratory tract infections are common in most parts of the country. The people who are most exposed to these infections are the poor, who reside in those poor housing and unhygienic environments where transmission of these diseases is rampant. Children and infants suffer most because of continuous exposure to infections, as well as the inability of their parents to provide good housing or to access appropriate health care for them. Against this background, St Andrew’s Clinics for Children Ile-Ife (STACC Ile-Ife) was established in September 1998
with the remit to treat children under the age of five years in Osun State, Southwest Nigeria. STACC Ile-Ife was located within Obafemi Awolowo University in the city of Ile-Ife, with approval from the University authorities, and it was funded, and remains funded, by St Andrew’s Clinics for Children (www.standrewsclinics.org.uk), a charity registered in Scotland. As many of the people targeted for health care service reside in communities located at some distance from Ile-Ife, with some of them approachable only by poor, unsurfaced roads, the health care service was designed as a mobile clinic operation so as to take health care to children in their communities. The company constituted a clinic medical team to visit each clinic community roughly fortnightly to examine and treat the sick children for their various ailments. The medical team includes a qualified medical doctor, a trained midwife, a technical assistant and a field assistant. The medical personnel are sourced from among the staff of the Health Centre at Obafemi Awolowo University. Starting with visiting three communities in the region, the service has now expanded to take in ten different communities.
On a clinic day, the medical team travels to the community with the drugs and other facilities required for the day’s work in the company’s vehicle. The clinic is usually held at a convenient venue within the community provided by the people. The children that need care are brought to the clinic venue by their mothers or guardians. Each child attending the clinic for care is issued an identity card with an identification number. At the commencement of the day’s clinic work, the
Samuel O Asaolu, Director of STACC Ile-Ife, Nigeria
“Children and infants suffer most because of continuous exposure to infections.”© St Andrew’s Clinics for Children Ile-Ife (STACC Ile-Ife)
doctor and the nurse give talks to the mothers for about 1520 minutes on the importance of hygiene and other issues affecting child health. The doctor then attends to each child, listening to the mother for the health problem of the child, and then examining the child thoroughly to diagnose the type of illness affecting the child. Thereafter, with the assistance of the nurse, the child is given appropriate treatment and medication, making use of the drugs and other facilities taken to the field. Records of all the diseases diagnosed and care given to each child are made. When the ailments of a child are such that the team cannot handle at the community level, the parents or guardians are usually advised to seek care for the child in the hospital in Ile-Ife. All the treatments by STACC Ile-Ife are given free of charge and the parents do not pay for the care.
The team typically targets seeing and treating up to a maximum of 60 children on each clinic day. In the five months from July to November 2021, the average number of clinics held per month was 20, the average number of children treated per month was 820 and the number of various diseases treated was 30. In the early period of running the mobile clinics, there used to be a much longer list of diseases encountered among the children, sometimes up to 70, but over time, and as a result of the care we have been giving the children, there has been an improvement generally in the health status of the children. Currently, the two most frequently encountered diseases among the children are malaria and upper respiratory tract infections (URTI).
Malaria cases represent 35 40% of all cases, while URTI accounts for about 30 35% of the cases. In order to reduce the prevalence of malaria among the children, long-lasting insecticide-treated nets are distributed to the mothers from time to time, to be used by the children when in bed so as to

prevent mosquito bites and reduce malaria transmission. The recent announcement by the World Health Organisation that a vaccine has been developed against malaria is welcome news, as it is hoped that this might be made available to help reduce the burden of malaria among the children in our clinic communities in the not-too-distant future.
In order to promote understanding and ensure good quality of service delivery, staff meetings are held twice a year, where staff members can discuss the progress of the work and share their views on problems they encounter in the running of the clinics. STACC Ile-Ife prepares a report monthly to record details of the work of the mobile clinics.
There is little doubt that the regular mobile clinics to the ten communities in Osun State have had a significant impact on the health of the children in that area. STACC Ile-Ife has been providing this care for almost a quarter of a century now and hopes to continue this care for at least another quarter of a century.
Babies and children who sleep under bed nets impregnated with insecticide are far less likely to die young from malaria. But some scientists have worried that those who avoid malaria in their early years might not develop immunity, resulting in increased risk later. Now, an ambitious study in Tanzania has found that thousands of people who slept under bed nets 20 years ago, as children, have a 40% survival advantage compared with those who did not. See www.science.org/ content/article/malaria-preventing-bed-nets-save-children-s-livesimpacts-last-decades for more information.
“Currently, the two most frequently encountered diseases among the children are malaria and upper respiratory tract infections.”
 Maggie’s
Maggie’s
Cancer support charity Maggie’s is helping to give people the best possible start to treatment with a revolutionary new course. The new 90-minute Pre-habilitation Workshops are specifically designed for people newly diagnosed with cancer to take an active role in their emotional, nutritional and physical health. Pre-habilitation is about helping people ‘get ready’ for what’s ahead. Maggie’s expert staff will help people to self-manage, recognise and respond to any lifestyle changes they might like to make.
Evidence suggests that providing people with dietary, exercise and psychological support at this early stage gives people the best chance of treatment success, and helps people to feel better about themselves, increase a sense of being in control, and reduce stress. This pilot project, funded by the Scottish Government, is being rolled out at all eight of Maggie’s Scottish centres and will run until 2023.
Maggie’s Chief Executive, Dame Laura Lee, said, “We know that pre-habilitation, effectively preparing people for what to expect, has so many benefits, including reducing the length of stay in hospital and post-treatment complications. As well as improving recovery, fitness, nutritional status and neurocognitive function, and helping people to have a better quality of life.
“Our new pre-habilitation programme encourages people to take an active role in their emotional, nutritional and physical health. Gentle exercise, eating well and emotional and psychological support are already aspects of the Maggie’s core programme of support, but this usually comes after the person has started treatment. This new project will ensure people newly diagnosed with cancer find the support they need sooner. And we will deliver this support in partnership with the NHS, as part of people’s overall care package. We are already obtaining feedback to ensure the sessions are as impactful as possible, and aim to establish whether outcomes are improved for those who use the programme.”
The new Pre-habilitation Workshops will be delivered in addition to Maggie’s core programme of practical and psychological support designed to help people live well with cancer. There are 24 Maggie’s centres across the UK, all built in the grounds of NHS cancer hospitals. They are designed to be warm and welcoming and are run by expert staff who offer bespoke support to people at any stage of treatment and beyond, as well as family and friends.
 Alison Allan, Centre Head for Maggie’s
Alison Allan, Centre Head for Maggie’s
Fife, explains the importance of the Pre-habilitation Workshops as part of Maggie’s wider programme of support. She says, “Challenges can arise for families at any point, and we are here for people throughout, but we want people to know that Maggie’s is here to help them right at the start, and we can help people prepare for what’s ahead. We want to introduce our expert support at the earliest stage possible so people can learn how to maintain a sense of control at a time they might feel adrift, when they are likely to worry and have lots of things to consider about what, or if, treatment is available.
“Our new pre-habilitation programme helps them to physically and emotionally prepare by highlighting small changes they can make and adopting healthy behaviours, and our workshops also help support people who may not be offered any treatment, by helping individuals to maintain control and feel better in themselves. In essence, we help people to ‘get prepared’ and we help people choose a pathway to suit their individual needs; introducing them to other support services available locally to help them throughout their cancer experience. Of course, this is also an introduction to Maggie’s and all of the other evidenced-based bespoke support we offer.”
To deliver the Pre-habilitation Workshops, Maggie’s will work very closely with NHS clinical teams, as well as our cancer support specialists, clinical psychologists and dietitians. Maggie’s also offers specialist exercise support and access to advice and support on rarer cancers too. With eight centres across Scotland, including Glasgow, Lanarkshire, Dundee, Edinburgh, Forth Valley, Fife, Aberdeen and the Highlands, Maggie’s aims to meet the needs of cancer patients in locations close to home. Please visit Maggies.org for more information.
Maasai and their livestock. © Alicia Davis“Pre-habilitation is about helping people ‘get ready’ for what’s ahead.”

Two global emergencies are simultaneously affecting people and our planet. One is the climate crisis, and the other is a pandemic. To some these are competing priorities for our time and resources, but they are intricately linked. We must combine resources and tackle both as one issue.
Pandemics are not unusual, but increasing anthropogenic pressure on biodiversity will increase the likelihood of more frequent pandemics. However, health and the environment are still considered separate issues, with health an immediate and personal crisis, while climate change is an issue seen by many as beyond individual control.
The initial response to the current pandemic, which involved preventing infection spread though lockdowns, had a positive impact on infection spread, air quality, and to some extent biodiversity. However, the economic impact has been one of the worst on record and, as such, has had an adverse bearing on climate mitigation measures and conservation efforts. The pandemic has also placed immense pressure on health and social care services, to a point where staff are exhausted and waiting lists for treatments are increasing.
In the UK the NHS is seen as a significant contributor to the climate crisis, through the emission of greenhouse gases both directly through energy consumption and indirectly through procurement. The NHS has therefore been investing in measures to reduce the carbon footprint through changes within estates and service delivery models. Yet despite our determination to deliver more climate-friendly services, achieving this is viewed as a costly exercise at a time when funding is inadequate to provide sufficient services to meet demand as waiting lists grow. Furthermore, there is still as yet no long-term plan to address the shortfall and support NHS recovery as we emerge from the pandemic.
There are, however, opportunities to implement with greater vigour many of the initiatives to prevent ill-health and support rehabilitation that were taking root before the pandemic. Policies on cleaner transport, biodiversity improvements, green exercise and sustainable agriculture are more important than ever. The ‘green push’ to recovery is estimated to significantly reduce carbon emissions through a combination of individual behaviour changes learned through the experiences of Covid-19 lockdown, underpinned by policy to address climate change.

Health and environmental protection are now much better understood in our communities and in our homes as Covid-19 has changed the way we live our lives.
Social distancing, mask wearing, enhanced cleaning, increased ventilation, and vaccination to reduce severe illness underpin every aspect of social, educational, and economic engagement. There have been positive consequences in the reduction of other infectious diseases, reviews of building standards to improve ventilation, and greater social engagement outdoors. We are realising the physical and mental health benefits of good quality, accessible greenspace. We are seeing changes to working practice as we increase the use of technology to support health and commercial services. We are recognising global interdependencies as we face restrictions in travel and shortages of goods but, in turn, we are looking to increase local production. We are facing unprecedented changes in our lives and have experienced significant pain and loss. However, we are learning that by working together and being creative we can adapt. We need to build on hard-earned successes to address the climate crisis and the impact of the pandemic. By combining efforts, we will be more successful in achieving a healthier greener planet.
Dr Jackie Hyland, Consultant in Public Health Medicine
“Policies on cleaner transport, biodiversity improvements, green exercise and sustainable agriculture are more important than ever.”© Raul Baz
The ScotWind Leasing announcement is an exciting and significant milestone in Scotland’s renewable energy story. The first offshore wind leasing in Scottish waters for a decade is something our industry has been working towards for several years, and will enable the next generation of offshore wind farms to be developed.
To date, offshore wind in Scotland has lagged behind the rest of the UK, with 1.9GW operational and another 8.4GW in construction or advanced development. But the possibility of these 17 new lease offers will add greatly to our existing project pipeline, creating huge ambition for our sector to deliver on.
In many ways, while this is the start of a long road ahead, just getting to this point has required our members to dedicate huge resources to put forward the strongest possible proposals for new offshore wind projects. Engagement with Scottish supply chain companies and a wide range of marine stakeholders has been happening for some time, as well as government and industry collaboration on identifying key strategic investments that will create world-class facilities. This will continue to be vital if these projects are to progress to construction later in the decade.
It is hard to illustrate the scale of the opportunity by discussing gigawatts alone, but the numbers are remarkable. Just before Christmas, the Longannet power station chimney in Fife was finally demolished, with the First Minister and Scottish Power highlighting the symbolism of ‘making coal history’. For almost 50 years, Longannet generated around a quarter of Scotland’s electricity, with 2.4GW of capacity. In contrast, this offshore leasing round has the potential to deliver more than 24GW of clean renewable electricity, ten times as much as Longannet and more than double what is currently installed around the entire UK coast. Scottish Power is one of the biggest winners of offshore sites from ScotWind, along with around 11 other consortiums and companies who will now begin to firm up their plans as they go through the regulatory permissions process in the coming years.
But while Scotland is the windiest country in Europe, with a quarter of Europe’s offshore wind resource, not everything blows our way. There are three big areas that will challenge the industry, and lots of work ahead to ensure that maximum environment and economic benefit is secured from this exciting development, a keystone of Scotland’s blue economy. The first will be the task of ensuring that Scotland’s grid network has the capacity to deliver clean electricity where it is needed. With significant expansion expected in onshore wind as well, an unprecedented scale of upgrade will be crucial. Upgrading transmission infrastructure is a process just as lengthy and complex as developing an offshore wind farm, so there is no time to lose. On the flipside, projects like these are also huge industrial opportunities, delivering jobs and economic benefit for years to come.
Some of the winning projects may have plans to convert their electricity into green hydrogen, or supply local industry, but we should also be ambitious about the formation of a North Sea grid to trade clean energy with our European neighbours, as well as the cables needed to supply the rest of the UK. For the wind farms themselves, a huge programme of work is already under way to make offshore transmission cabling more strategic, with the potential for some projects to share cables to shore. The second challenge will be for this huge expansion in the offshore built environment to be done in a way that supports the overall ambitions of the Scottish Government and stakeholders for our marine ecosystem. We know that across the globe there is both a climate crisis and a biodiversity crisis, and we must ensure that offshore wind makes a positive contribution in response.
As an industry we now have a great deal of experience in delivering offshore wind projects that have the confidence of regulators and deliver huge amounts of clean electricity to decarbonise our society. The much larger size of turbines possible offshore, expected to reach 20MW within a few years, makes these

Claire Mack, Chief Executive, Scottish Renewables
“This offshore leasing round has the potential to deliver more than 24GW of clean renewable electricity.”© Nicholas Doherty
sites a very efficient renewable resource. We also know very much more about potential impacts on birds, marine mammals and fish, and there are a plethora of industry research initiatives and projects exploring all aspects of the science. We will need to continue to work closely with all those with a stake in the blue economy as the offshore wind sector grows to be a major sustainable industry.
Collaboration is the third challenge facing the sector moving forward. It is essential that all these companies and projects, often forced to compete, collaborate to maximise the supply chain commitments that have been set out in their bids.
Despite the scale of the opportunity ahead, Scotland is still in competition with many other offshore wind markets demanding supply chain investment from those with the expertise. So, it’s imperative that we focus on Scotland’s strengths.

We now have the most seabed dedicated to commercial floating wind development of anywhere in the world. These 11 floating wind projects give Scotland a clear opportunity to create a major new sector to drive the blue economy, drawing on our deep-water expertise and making a just energy transition a reality in the North Sea.
The announcement in the autumn of a £110m tower manufacturing factory at Nigg was an extremely welcome boost to the sector, and now we are in an even stronger position to work with our excellent ports and suppliers to map out the needs of the sector stretching many years ahead. The work led by Sir Jim McDonald last year on strategic investment has set in train a framework for developers to work together in the interests of the Scottish economy, and the hard work to deliver this begins now. Continued close working between government and industry can deliver an exciting future for offshore wind in Scotland –and an exciting future for Scotland on the global stage.
An historic event took place in December 2021 as Scotland’s last remaining coal-fired power station chimney was demolished, marking the “definite end of coal power” in the country in the same year that COP26 was held in Glasgow. Longannet in Fife, owned by Scottish Power, was the largest plant of its kind in Europe at the time that it began producing energy for Scottish homes in 1970, and continued to be the largest freestanding structure in the country until its demolition.

Scotland has been ‘coal-free’ since Scottish Power closed the station in 2016; the energy company now only generates 100% green electricity through its wind and solar farms. Keith Anderson, chief executive of Scottish Power, said: “At COP26 in Glasgow, we were proud to show the world that Scotland has already made coal history. As a 100% renewable energy company, we are committed to helping the UK end its reliance on fossil fuels. For half a century, Longannet’s chimney has dominated the Firth of Forth skyline. We bade farewell to that landmark today –however, this is a landmark day for Scotland too.”
The night before the demolition, Scottish Power projected the environmental slogan ‘Make Coal History’ onto the chimney, along with the multi-coloured ‘global warming stripes’ created by Professor Ed Hawkins of Reading University, showing the change in global average temperature from 1850 to 2020.
Scotland’s First Minister, Nicola Sturgeon, who pushed the ignition button on the controlled implosion, described the demolition as “a symbolic reminder that we have ended coal-fired power generation in Scotland, as we work in a fair and just way towards becoming a net zero nation by 2045. Our goal is to generate 50% of overall energy consumption from renewable sources by 2030, and Scotland’s energy sector is well placed to deliver on the key investments in renewables, hydrogen and energy storage required to achieve this.”

It was October 2017. I was sitting in a microbus heading towards Kutupalong Rohingya refugee camps in Cox’s Bazar. I noticed signposts at the streets: “Warning! Wild Elephants Migration Route.” The camps were a reserve forest, habitat for the endangered Asian elephant along a migration route for elephants travelling between Myanmar and Bangladesh. Many trees have been chopped down to make more space for refugee shelters for the massive influx of ethnic Rohingya escaping violence in Myanmar. Later that day I found a young boy admitted into a camp hospital critically injured by a wild elephant attack. The elephants trampled his mother and three other siblings a few days back. Elephants always follow their traditional routes and corridors for regular movement, and if they find any obstacle within it, they try to break it. The elephant habitat was under threat and the passages have been encroached by human settlements. This was a tragic example of how deforestation and the refugee crisis have created a complex situation for vulnerable people and endangered wild animals.
Bangladesh has just celebrated her golden jubilee anniversary of independence in December 2021. Fifty years into its independence, what are the transformative milestones of health? The fledgling country was beset by disease and poverty in 1971. However, Bangladesh has made a remarkable turnaround by implementing the Millennium Development Goals in the areas of poverty alleviation, food security, primary education, mortality ratio, immunization coverage, and tackling communicable diseases. Life expectancy has gone from 46 years to 73. Infant mortality has declined from 167 to 22 deaths per 1,000 live births. The country’s literacy rate has risen from 26.8% to 74.7%. In 2015, Bangladesh became a lower-middle income country, from being a low-income country.
Let us look at some challenges into this journey of Bangladesh at 50 through the lens of climate change, planetary health and palliative care. When we talk about climate change, we prefer just to concentrate on greenhouse gases, fossil fuels or net zero. How about looking at the root causes behind these? In the past 50 years, the proportion of the Bangladeshi population living in cities has grown
offrom 8% to 39.4% and is projected to be 61.2% in 2050. Along with demographic transition, Bangladesh has also been going through a rapid epidemiologic transition in which non-communicable diseases now account for two-thirds of all deaths. Bangladesh ranks 15th among 33 countries where children are at extremely high risk of the impacts of the climate crisis.
In 2015, the Economist Intelligence Unit ranked Dhaka 139 out of 140 cities by the liveability index, and ranked Bangladesh 79 out of 80 countries by the quality of death index. Climate change has internally displaced millions of people into urban slums. Malaria and dengue fever are climate-sensitive diseases and significant problems of Bangladesh. Here is a little secret. Mosquitoes have no regulatory system; thus, their body temperature is the same as the air temperature. Higher temperatures reduce the time for virus replication and dissemination in the mosquito. A hot humid environment, pollution everywhere and water accumulation in Bangladesh are important for the reproduction and spread of mosquitoes.
Perhaps the threat now facing our country is not just different diseases or climate change. The real risk lies within the society we have created, and inside ourselves. Planetary health may give more insight, which is the health of human civilization and the state of the political, economic, and social systems. It will take time to address underlying political, economic, and social forces that created and perpetuate slums or refugee settlements. Palliative care can improve quality of life of our patients with life-threatening and lifelimiting diseases.
So, there is scientific evidence. What we have to do over the next 50 years is much more dramatic and more exciting than what we did when we moved into the situation we’re in today. We need more individual consciousness and connection with others. There is a huge urgent need of integrated action at both local and global levels in keeping up Sustainable Developmental Goals and the Paris Agreement based on the latest solidarity at COP 26 in Glasgow.
We do not want to be climate refugees that no one wants to host. Together we can move from understanding to action and emerge stronger. The countdown has begun.
Dr Farzana Khan MA MPH MBBS, Global Health Academy, University
Edinburgh
“Bangladesh has made a remarkable turnaround by implementing the Millennium Development Goals.”
 Roger Crofts FRSGS
Roger Crofts FRSGS
It is all too easy to be pessimistic following the failure of the Framework Convention on Climate Change parties at COP26 to agree a deal on emissions reduction to achieve net zero, and the failure of the Convention on Biological Diversity to meet the key targets on biodiversity. If this is not bad enough, remember the increasing inequality of access to environmental resources through commercial exploitation and global trade patterns. The prescient words of HM The Queen, reinforced by Sir David Attenborough and Barack Obama, to put national interests to one side and play statesmen’s roles are, unfortunately, not heeded by national political leaders. What needs to be done? Sackcloth and ashes will not do. We need to rise to the challenges: experts, businesses, citizens and government. Here are some ideas to stimulate debate. For the scientists and technical experts there are many challenges. We hear so much about the need to stop use of fossil fuels immediately. But, do the alternatives to hydrocarbons exist, for example to replace plastics which all households and commercial organisations use in abundance? And how is the transition from fossil use for heating and transport to be delivered quickly and affordably? Targets by governments act as a stimulus, but are there sufficient incentives and investment to develop and implement the replacement technologies at the pace needed? And, we need improved decision support mechanisms, including transparent and independent verifiable ways of calculating and communicating the whole lifetime costs and benefits of existing and new technologies.
We also need greater honesty in communication. Nuclear energy is a good example. To categorically state that electricity produced by nuclear fission is carbon-free is not accurate, given the carbon intensity of construction of reactor vessel and containment vessel. Nuclear fusion holds out hope, and the technological advances now being made need political encouragement and massive financial investment.
The learned societies, like the RSGS and the Royal Society of Edinburgh, have important roles to play in facilitating communication and improving the discourse within society about what we know, what we don’t know, and what are the levels of uncertainty.
Second, the business community needs to take its environmental and societal responsibilities more seriously. There are many good initiatives, such as the World Business Forum on Sustainable Development and the appointment of Mark Carney FRSGS as the UN Special Envoy for Climate Action and Finance. But, shareholder value remains a core principle, and avoids the wider responsibilities that businesses have of adopting the circular economy and using triple bottom line accounting mechanisms, both of which imbue a broader-based ethical approach into business.
More fundamental is the wise use of the world’s natural resources, especially its soil, water and minerals. The 20th-century exploitative approach is no longer tenable, yet bad practice remains in all parts of the world according to official UN agency statistics, meaning that soil erosion and loss continue
to increase, and productivity continues to decline, and the world’s oceans are overfished. Incentives, codes of practice and regulations all need to be refreshed, and new mindsets to rid entrenched approaches adopted.
Third, citizens cannot avoid the challenges. The headline changes needed are very difficult, but essential: changing behaviours and reducing impact on the environment and on poorer societies. Personal consumption patterns need to recognise that short lifespans and throwaway approaches are outmoded. Purchasing local products, challenging the purchase of products reliant on global supply chains, and using packaging from non-renewable resources are all issues which citizens as consumers should continue to argue for, while demonstrating their changing behaviour.
The two elephants in the room are increasing levels of consumption globally and increasing population. Measured debate is essential, despite how contentious these issues, especially population control, are. The voice of women in these debates is most crucial, as shown in Africa when they have a leadership role.
The final challenge is for governments to move from rhetoric to realistic delivery. The ask is simple: to deliver more effective, integrated policy and resources based on a long-term vision. The operative word is delivery. It is easy to announce new targets. All too often the path to full achievement in practice is neither thought through nor are all of the elements needed set out in a deliverable action plan. For the environment, the essential element is for ethical requirements to be embedded in all policies, programmes and funding schemes. The prime Scottish requirement is the radical revision of agricultural support. One example is the current failure to implement integrated programmes for flood protection founded in nature-based solutions and whole catchment management, rather than allowing engineering-led projects to build more barriers without working with nature, as in the recent flood protection schemes in Selkirk, Hawick and Musselburgh.
Engaging all generations is vital. Education in the formal primary, secondary and tertiary sectors is crucial. Why is every child and every student not taught the basics of how the environment works, what humans have done and are doing to it, and what type of behaviours and ethics are needed for the future?
Geography is at the core of this, so surely should be a compulsory subject at all primary and secondary levels with urgent changes to the out-dated curriculum put in place as a matter of urgency.
“We need to rise to the challenges: experts, businesses, citizens and government.”
Tonga in the Southwest Pacific Ocean is used to experiencing a range of natural hazards from tropical cyclones, earthquakes and tsunamis. On 15 January 2022, the eruption of a little-studied volcano known as Hunga-TongaHunga Ha’apai led to a massive underwater eruption and coupled tsunami that travelled across the Pacific Ocean with a trans-oceanic impact. This is known as a far-field tsunami, as the source is many thousands of kilometres away from the coastal areas that experienced flooding. In the immediate vicinity of the volcano, the explosive eruption produced a tsunami felt throughout Tonga and the neighbouring Pacific islands.
The word tsunami literally means ‘harbour wave’ in Japanese, and comprises a series of waves as a huge mass of water travelling at speed across the ocean. Tsunamis are generated when a mass of water moves suddenly and with great force, such as the seafloor elevating quickly, or an earthquake, a submarine landslide or caldera collapse associated with underwater volcanic eruption. The shock waves generated by the eruption traversed many thousands of kilometres, were seen from space, and were recorded in New Zealand, almost 2,000km away. Soon after the eruption started, huge volumes of volcanic ash entered the atmosphere and covered coastal communities in a blanket of ash.
The Pacific has a sophisticated Tsunami Warning System, capable of sending simultaneous alerts across to Hawaii, Alaska, British Columbia, Japan, South America and Polynesia. It was put in place following the major earthquake and tsunami generated off Chile in May 1960. These tsunami warnings are issued even if the eruption or earthquake occurs on the other side of the world, and are recorded on a global network of ocean buoys. The waves produced following the Tonga eruption travelled across the ocean with wavelengths of tens of kilometres, at speeds of commercial jet aircraft. Such tsunamis have clearly-defined travel times across ocean basins, thus allowing time for the tsunami warnings or tsunami watch to be enforced in coastal communities around the Pacific.
Tsunami waves generated by the eruption in Tonga travelled across the whole Pacific Ocean to Fiji, the Cook Islands, New Caledonia, New Zealand, along both the North and

South American coastlines, and to Japan. Some of these places reported flooding and localised inundation. A onemetre-high wave was recorded in Hilo, Hawaii, no stranger to catastrophic tsunamis, and waves were up to two metres in Japan. Along the Australian east coast, tsunami waves of 0.8m were seen and recorded on tide gauges up to three days after the eruption. The waves that inundated Tonga, although modest at 1.2m, led to significant inundation of low-lying coastal landscapes, which damaged roads, buildings, and coastal defence infrastructure such as seawalls.
The combination of volcanic eruption, submarine landslide and tsunami led to catastrophic damage to an undersea telecommunications fibre optic cable c800km long, severing Tonga’s connection to the rest of the world. The rest of the world was unable to reach Tonga for a period of days following the cascade of natural hazards. This also made it very difficult for the emergency services to communicate with each other, as well as for the Tongan authorities to ask for emergency aid and support. This disaster highlighted the vulnerability of essential infrastructure, and the wider impacts beyond the local and regional scale, in the wake of the eruption.
Tsunamis produced by volcanic eruptions are relatively rare, at around 5% of all recorded events. However, they can be some of the most destructive and wide-reaching. In historical times, the eruption of Krakatoa, Indonesia in 1883 generated a 30m tsunami in the Sunda Strait which led to the deaths of 36,000 people across Java and Sumatra. The tsunami in Tonga was also relatively rare since it caused atmospheric pressure disturbances, transferring energy into the ocean, resulting in additional sea-level disturbances known as meteotsunami. These are driven by fast-moving weather events, such as severe thunderstorms and storms. Such storms generate waves that move towards the shore, where ocean and atmospheric waves travel at similar speeds across the ocean. Recordings of these pressure waves were felt in multiple gauges around the world, including Europe and the UK, with weather stations able to detect the pressure waves, reflecting the enormous energy released following the volcanic eruption. In this way, the event in the Southwest Pacific had a truly global impact.
“Tsunami waves generated by the eruption in Tonga travelled across the whole Pacific Ocean.”
Tonga’s volcanic eruption, tsunami and ashfall has caused an estimated US$90.4M of damages in the country – the equivalent of approximately 18.5% of Tonga’s Gross Domestic Product – a World Bank assessment for the Government of Tonga has found. Earthquakes continue to shake the region, and the volcanic danger might not be over.


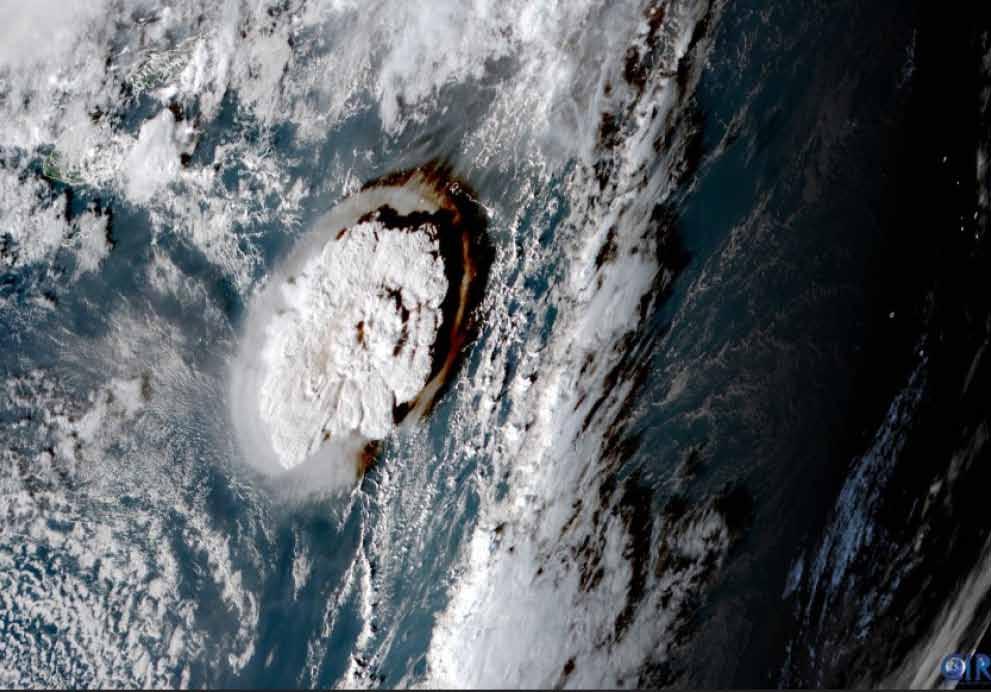

Tonga lies in the Pacific, around 1,100 miles northnortheast of New Zealand. The volcano erupted about 40 miles north of the capital Nuku’alofa, and triggered a tsunami which flooded parts of the archipelago, rippling out much further, even causing an oil spill in Peru. According to Nature, the extraordinary power of the blast of Hunga-Tonga-Hunga Ha’apai is forcing scientists to rethink their ideas on the hazards posed by the many submarine volcanoes that lurk beneath the waves of the Pacific Ocean.
Communications with Tonga have remained very limited since the volcanic eruption and tsunami, after the main undersea cable connecting the island nation to the rest of the world broke in at least two places. Even as we go to print (February 2022) there are reports that progress has been slow in the search for Tonga’s submarine telecommunications cable. Bad weather and rough seas persist in the area; it took until 7 February for the cable repair ship Reliance to recover and fix the Tonga end of the international cable, but the Fiji end remains elusive. Latest updates from Tonga confirm that at least three people have died and many are still struggling with the fallout of the eruption, with severe flooding and damage to buildings and property affecting almost every one of the 106,000 inhabitants in some way. It is believed that several small settlements in outlying islands have been wiped out completely, and a thick layer of ash blankets the main island, tainting drinking water, possibly damaging crops, and resulting in the need for large clean-up efforts. Most people in Tonga are involved in farming and agriculture, meaning that the long-term destruction to lives and livelihoods could be massive. Due to the need for critical international aid deliveries, Tonga, which had previously seen only one case of Covid-19, has now seen its first community outbreak since the start of the pandemic, prompting warnings that, with the natural disaster and virus, Tonga’s fragile health care system could quickly become overwhelmed.
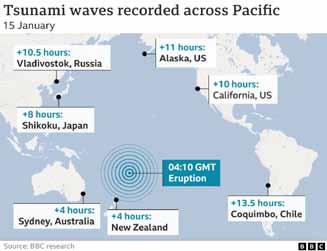
 of Nursing Scotland
of Nursing Scotland
Our members are tired, emotionally and physically drained from the relentlessness of the past two years. But many were feeling this way even before the pandemic hit. They were already responding to the consequences of an ageing population with increasingly complex health needs, of being short-staffed with high levels of vacancies, of being unable to have their breaks or have time for professional development, of going home at night carrying the guilt of care left undone and the impact this has on patients and their colleagues.
There is no doubt the pandemic shone a light on just how critical the role of nursing staff is in providing safe and effective care, their 24/7 presence and their willingness to step up in challenging times. Our members appreciated the clapping. The rainbows brought many smiles, and the goodwill of the public was a help through those initial months in lockdown. Nursing staff felt that at last their role was being recognised.
The public gaze has moved on. The vaccination programme, largely delivered by nursing teams, has had a significant impact and the nation is beginning to learn to live with this deadly virus.
For nursing staff, the work hasn’t changed but the spotlight has once again gone out.
The Royal College of Nursing is looking for the Scottish Government to show it values our nurses and nursing support workers in hospitals, community teams and care homes, and to invest in the workforce now and for the future.
Nursing and midwifery vacancies in the NHS in Scotland are at a record high, and there are similarly high levels within Scotland’s care homes. There are simply not enough nursing staff to run existing services, let alone seek to improve or expand these services.
The link between low pay, staff shortages and safe staffing is clear. Nursing must be seen as an attractive and rewarding career across NHS and social care services. There must be opportunities for career development and progression, and fair pay which recognises the job they do.
Measures need to include ongoing investment in nursing student numbers across the four fields of nursing (adult, child, mental health and learning disability). But equally important is a focus on retaining our experienced nursing staff, giving them the opportunity to work flexibly, to continue to contribute to nursing teams and share their skills and expertise. Over 20% of Scotland’s nursing and midwifery workforce is aged over 55.
We’ve seen a sharp rise in the proportion of nursing staff considering leaving their job. In an RCN survey last year, over 60% of those who responded said they were thinking about this. Of those, three-quarters said this was because they felt undervalued, with 65% citing that understaffing was a key issue. In the same survey, two-thirds of nursing staff said they were too busy to provide the level of care they would like.
The public too are recognising the impact of workforce pressures. In polling carried out in October 2021, 84% of Scots agreed that nurses do not get to spend long enough with their patients, and over three-quarters said there are not enough nursing staff to provide safe and effective care. Addressing the current staffing shortages is vital to stabilise our health and social care services as we move towards recovery.
Over two years ago, our members supported the Scottish Government’s proposal to introduce legislation to secure safe staffing. We campaigned hard to make this legislation work for patients and our members, so it is extremely frustrating that the Health and Care (Staffing) (Scotland) Act 2019 is still to be implemented. The reasons for passing this Act have been made even clearer by the Covid-19 crisis. Safe and effective staffing is a fundamental element of remobilising the NHS and helping to ensure that Scotland’s care homes can deliver care to residents with increasingly complex health needs. The Scottish Government needs to set out a clear timetable for implementation of this important legislation. Recognising the impact of the job and working under such sustained pressure is also key to retaining the current nursing workforce. Over 89% of the Scottish public said more should be done to protect the well-being of nursing staff. Government and employers have taken steps to fund and provide services to help staff with practical and emotional needs, and aid rest and recuperation. However, we are still hearing from members that they simply don’t have the time to take advantage of the services that have been set up.
A new approach to workforce planning is needed that takes account of all these factors. Planning that is based on what services need now and in the future, rather than on what is affordable. That takes account of the well-being of staff and the need for learning and development. Planning that truly values the role of nursing in delivering Scotland’s health and care services, and builds a workforce that has the skills and capacity to provide the safe and effective care the people of Scotland expect and deserve.
Colin Poolman, Interim Director, Royal College
“There are simply not enough nursing staff to run existing services.”
I began my independent life in debt. This isn’t unexpected for many American teenagers, higher education requiring the loans that it does. But the third-party debt collectors were more unusual.
By my last year of high school, I had to abandon plans to go to college. What I did have was outstanding medical debts, and a crummy job paying $9.25 an hour (my state’s minimum wage) washing dishes at a local restaurant.
Over that summer, I’d noticed the nerves in my hands and feet weren’t working quite right, and my doctor had ordered an MRI. This meant a trip to the local hospital, my mom and my Blue Cross insurance in tow.
My insurance was provided by my father’s position cleaning at a local factory, its coverage less than ideal. Like insurance on a car, the low monthly premium meant a lot had to be paid out-of-pocket before the insurers would begin to cover anything. It also meant higher co-payments, which is the amount you pay towards each service even after you’ve paid the initial fee.
I left the hospital feeling worse than when I arrived, and $800 in debt at the age of 18. Eight hundred dollars, or so I thought. The hundreds more in blood testing hadn’t been mailed to me yet.
The grand total would eventually shake out to be closer to $1,500 – as much as the car I’d need to work, two months of rent if I ever hoped to move away from home, or a semester’s tuition at the local community college. That’s the American experience even for our youth. A trail of debt, alongside faltering credit and daily calls to remind you of what you owe. A thousand dollars for four sessions of therapy. Two thousand for wisdom teeth removal, unless of course, as you’re so helpfully reminded, you choose to forgo any anaesthetics in order to save the money. Seven hundred dollars for a month’s supply of
insulin, where the only option other than payment is death. Many insurance companies require a certain amount of payment from the insured before they will begin to cover the costs of care.
While there have been strides made by federal initiatives, such as the Affordable Care Act, to improve access to government health insurance for the poorest of America’s citizens, there is still a long way to go, with healthcare providers still entitled to refuse care to Medicaid patients except in life-threatening circumstances, and little protection for those who are not yet, but are at risk of, falling into poverty.
The American experience is also immediate access. I’ve never known a queue for healthcare, nor have I suffered with a few mandated options that don’t fit my needs. But is it worth the dread of seeking medical care, of accepting help even in an emergency, when a journey in an ambulance can cost more than a thousand dollars?
In 2018, The New York Times reported on the case of a woman severely injured by a passing train while waiting on a platform in New York, who was witnessed pleading with bystanders not to call an ambulance for fear of financial ruin. The story exploded on social media, as thousands of others shared their own similar experiences.

Years of financial progress lost in a single visit to the emergency room. People forced to crowdfund for life-saving surgeries, their struggles repackaged as feel-good news stories about charity rather than a failure of our system to take care of its own. The bitter truth that, sometimes, it’s easier just to hope that ankle will stop clicking on its own.
I am fortunate that I have always been able to wait to see a doctor, to drive myself to the hospital, to get the care that I have needed, and to get by in spite of my debts with the support of a caring family. But is it worth the cost to those living paycheck to paycheck, day to day? You’ll have to ask over half the country, which says an unexpected expense would prevent them from affording their next due rent. For many, healthcare ends up being that expense.
“Years of financial progress lost in a single visit to the emergency room.”

Unable to do my regular stints at the Fair Maid’s House, yet still very keen on the subject of Geography, I got thinking about those whom I had met over the years as they visited. One such was a short, elderly gentleman with his son. They were from Dublin and had been in touch with RSGS prior to their visit. Barely over the threshold, he pointed a finger into my chest and demanded to know what I knew about the fate of Scotia! Thinking as quickly as I was able, I remembered that one of the display cases in the Explorers’ Room contained material about the vessel and its voyage, so I conducted both visitors upstairs to show them what was there. The senior of the two was interested, but not too enthusiastic, since it was the fate of Scotia which was his interest.
Scotia was a barque, a three-masted vessel with the fore and main masts being square-sailed and the mizzenmast rigged fore and aft. Today they are used as ‘sailing school’ ships –indeed, coincidence number one, I was once taught the rudiments of sailing on just such a vessel.
Scotia was built in 1872 as the Norwegian whaler Hekla. The ship was 42.5m (139’ 6”) in length, with a beam of 8.8m (28’ 9”) and a draught of 4.7m (15’ 6”). After a series of different Norwegian owners and use as a whaler and sealer, she was purchased by William Speirs Bruce for 45,000 Kroner (£2,650) in 1902 and renamed Scotia. The costs of the purchase were undertaken by the Coats family from Paisley, which hits another coincidence – for a couple of years after I left school I was employed by J & P Coats, thread makers to the world!
She was rebuilt by the Ailsa Shipbuilding Company in Troon, for use as a research vessel by the Scottish National Antarctic Expedition. The ship was strengthened internally, with beams 640mm (25”) thick added to resist the pressure of ice whilst in the Antarctic. A new steam engine was fitted, which drove a single-screw propeller; it could propel the vessel at 13km per hour (7 knots). The work was supervised by Fridtjof Nansen, the Norwegian explorer, scientist, diplomat, humanitarian, polymath and Nobel Peace Prize laureate. When the conversion of the ship was complete, she was inspected by Colin Archer, who had prepared Fram for Nansen’s 1893 expedition to the Arctic. Thomas Robertson, who had 20 years’ experience of sailing in the Arctic and Antarctic on board the whalers Active and Balaena, was appointed captain of Scotia. Sea trials of the rebuilt ship were conducted in August 1902.
Scotia sailed on 2 November 1902 for the Antarctic, with a crew of six scientists, five officers and 26 crewmen. She arrived at the Falkland Islands on 6 January 1903, and then sailed to Laurie Island, South Orkney Islands where she arrived on 25 March. Scotia overwintered in Scotia Bay, where she was frozen in for eight months. She departed for the Falkland Islands on 27 November, en route for Buenos Aires, Argentina where she underwent a refit. Scotia returned to Laurie Island on 14 February
1904, sailing eight days later for the Weddell Sea. She departed from the Antarctic on 21 March. Calling at Saint Helena in June, she arrived at Millport, Cumbrae, Ayrshire on 21 July 1904 (20 years after RSGS’s unofficial birthday), and was met by the Marine Station’s yacht Mermaid, the Coats’ Triton and Gleniffer, and the steamer Marchioness of Lorne, and escorted to Millport. Bruce, Robertson and their scientists took to Scotia’s launch and landed at the Marine Station’s slip. They were met by Sir John Murray, Lieutenant Shackleton, Dr Sommerville, David Robertson, Mr J G Bartholomew, Mr Henry Coates, Mrs W S Bruce, Mrs Robertson and others. Bruce received the Gold Medal of the Royal Scottish Geographical Society, Robertson the Silver, and the other scientists Bronze. During the proceedings, a telegram from King Edward was received congratulating Bruce. After lunch, purveyed by Messrs White and Smith, Gordon Street, Glasgow, Scotia set off at six o’clock for Gourock, her final destination. You can read more about Scotia’s adventures and William Speirs Bruce in Jo Woolf’s excellent book, The Great Horizon The coincidences are not yet done, for W S Bruce and his family lived at various addresses in the
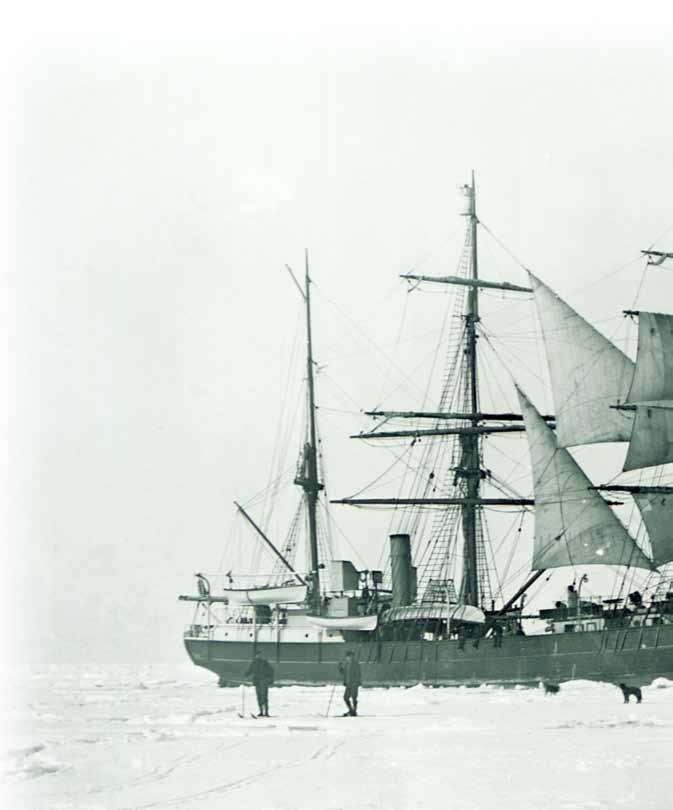
John Lewington FRSGS, RSGS volunteer
“Scotia sailed on 2 November 1902 for the Antarctic, with a crew of six scientists, five officers and 26 crewmen.”William Speirs Bruce. © RSGS Collections
Edinburgh suburb of Portobello, just as I had done too! Following the expedition, it was planned that Scotia would see further use by the universities of Scotland as a research vessel. However, in an effort to recoup some of the costs of the expedition, she was sold by auction. She served as a sealer and whaler until 1913, operating off the coast of Greenland. Following the loss of Titanic in April 1912, Scotia was chartered by the Board of Trade for use as a weather ship on the Grand Banks of Newfoundland, warning shipping of icebergs. A Marconi wireless was installed to enable her to communicate with stations on the coast of Labrador and Newfoundland. Following this she became a collier, sailing between South Wales and France. On 18 January 1916, she caught fire and was burnt out off Sully Island, Glamorgan, in the Bristol Channel. Her crew survived. And thus Scotia came to a watery end; fitting, I suppose, after her life at sea. I don’t know whether my elderly visitor or his son will ever read this, but I am sorry to have to report that Scotia did not receive a more significant end. William Speirs Bruce died on 28 October 1921, his body cremated and his ashes scattered in the South Atlantic Ocean off the southern shores of South Georgia.
At the end of their visit, I asked Mike Robinson to look out the Visitors Book from late 1904 or early 1905, when the RSGS was addressed by the crew of Scotia, and, of course, he was able to find where this visitor’s ancestor had signed in, allowing my visitors to leave with the hop, skip and jump of the delighted!
Back in 2002, an unusual collaboration took place between the Royal Scottish Geographical Society (RSGS) and the Royal Scottish Country Dance Society (RSCDS). Plans to celebrate the centenary of the Scottish National Antarctic Expedition included a book of Scottish country dances with music: The Scotia Suite. The seven dances were named to reflect the journey of the research vessel SY Scotia and her crew, led by polar scientist William Spiers Bruce. They continue to be danced to this day by many of the 10,000 RSCDS members worldwide.



In October 2021, as Chairman of the RSCDS and a Board member of the RSGS, I couldn’t resist the challenge from a former RSGS Trustee to commemorate 100 years since Speirs Bruce’s death by linking the two Societies once more. The resultant short video (www.rscds.org/blog/dance-scotia) includes Speirs Bruce artefacts from RSGS collections held in the Fair Maid’s House, and RSCDS dancers filmed in Edinburgh and Antarctica. The fun of dance, and our shared history, is clear as an RSCDS Board member leads international travellers to Antarctica in dancing The Piper and the Penguin on board ship, and on the snow!
In her foreword to The Scotia Suite, HRH The Princess Royal, a Vice-President of RSGS, reflected that “geographers and dancers each know the value of working as a team” and that “the voyage of the Scotia can inspire creative art as much as it stimulates scientific endeavour.” This recent joint celebration is testament to these sentiments.
“Plans to celebrate the centenary of the Scottish National Antarctic Expedition included a book of Scottish country dances with music.”
 Chris Fleet FRSGS, Map Curator, National Library of Scotland
Chris Fleet FRSGS, Map Curator, National Library of Scotland
In 1860, the year when this map was published, Joseph Lister became Professor of Surgery at Glasgow. In his role as visiting surgeon at Glasgow Royal Infirmary over the following decade, Lister conducted experiments on the use of antiseptic techniques which revolutionized the craft of surgery, and would go on to save millions of lives worldwide. This map allows us to see inside Lister’s Infirmary like no other. By this time, the original Infirmary building, at the southern end of the complex shown here, was over 60 years old. Designed by Robert Adam and constructed on the site of the former Bishop’s Palace adjacent to the Cathedral, it had a magnificent facade, and separate stairs at each end to access the wards above. This allowed for appropriate separation of male and female patients, as well as multiple access routes to its “splendid and commodious” operating theatre on the upper floor. Situated beneath a huge central dome, with five ranges of stacked wooden benches, the theatre allowed seating for over 200.
The central wing projecting north was added in 181415, containing a staff dining-room, accommodation, and additional wards for about 80 patients. A detached fever block, constructed in 1828-29 to the north-east, became attached to the main building in 1842 by constructing a large Clinical Lecture Room, Waiting Room, Dispensary, Inspection Room and a Pathological Museum. The western wing, built around 1839, included the Superintendent’s House, Boiler House, and washing and drying rooms.
The Ordnance Survey’s Town Plans allow us to scrutinize both the interior and exterior of Victorian urban buildings like the Infirmary in incredible detail. Never before nor since would Ordnance Survey map Glasgow or other urban areas in Britain in such detail. One of the primary motivations behind this mapping was to promote sanitary and other public health improvements. Whilst mapping initiatives at less detailed scales at this time also showed the close links between sources of disease, poverty and population, these more detailed maps provided an essential basis for planning improvements to water supply, sewerage, lighting, housing and the wider urban infrastructure.

“The Ordnance Survey’s Town Plans allow us to scrutinize both the interior and exterior of Victorian urban buildings like the Infirmary in incredible detail.”Ordnance Survey, Town Plan of Glasgow, 1:500, Sheet VI.11.3 and VI.11.8. Surveyed 1857, published 1860. Image courtesy of the National Library of Scotland. View online at maps.nls.uk/view/74416228 and maps.nls.uk/view/74416223

Colin Thubron (Chatto & Windus, September 2021)
The Amur River is almost unknown. Yet it is the tenth longest river in the world, rising in the Mongolian mountains and flowing through Siberia to the Pacific to form the tense, highly-fortified border between Russia and China. In his 80th year, Thubron took a dramatic 3,000-mile long journey from the Amur’s secret source to its giant mouth. Harassed by injury and by police arrest, he made his way along the Russian and Chinese shores on horseback, on foot, by boat and via the Trans-Siberian Railway, talking to everyone he met. By the time he reached the river’s desolate end, where Russia’s 19th-century imperial dream petered out, a whole, pivotal world had come alive.
Rachel Clarke (Little, Brown, January 2021)
How does it feel to confront a pandemic from the inside, one patient at a time? Clarke is a palliative care doctor who looked after some of the most gravely unwell patients on the Covid-19 wards of her hospital. Amid the tensions, fatigue and rising death toll, she witnessed the courage of patients and NHS staff in conditions of unprecedented adversity. Drawing on testimony from nursing, acute and intensive care colleagues, and her patients, Clarke argues that this age of contagion has inspired a profound attentiveness to, and gratitude for, what matters most in life.
Simon Reeve (Hodder & Stoughton, October 2021)
Best-selling author and presenter Reeve takes us on epic and thrilling adventures, in beautiful, tricky and downright dangerous corners of the world, as he travelled through the Tropics, to remote paradise islands, jungles dripping with heat and life, and on nerve-wracking secret missions. He shares what his unique experiences and encounters have taught him, and the deeper lessons he draws from joy and raw grief in his personal life, from desperate struggles with his own fertility and head health, from wise friends, fatherhood, inspiring villagers, brave fighters, his beloved dogs, and a thoughtful Indian sadhu.

Readers of The Geographer can buy Journeys to Impossible Places for only £15.00 (RRP £20.00) plus £3.10 UK P&P. To order, please contact hukdcustomerservice@hachette. co.uk
Nicholas P Money (Reaktion Books, April 2021)
A vision of biology set within the entire timescale of the universe, told with poetry, social commentary and humour, this is about the timing of life, from microsecond movements to evolutionary changes over millions of years. Human consciousness is riveted to seconds, but a split-second time delay in perception means that we are unaware of anything until it has already happened. We live in the very recent past. Over longer timescales, Money examines the lifespans of the oldest organisms, prospects for human life extension, the evolution of whales and turtles, and the explosive beginning of life four billion years ago.
Stuart Blume (Reaktion Books, April 2021)
At a time when vaccines are a vital tool in the fight against Covid-19, Blume, Emeritus Professor of Science and Technology Studies at the University of Amsterdam, takes a longer historical perspective. He argues that globalization and cuts to healthcare have been eroding faith in the institutions producing and providing vaccines for more than 30 years. He tells the history of immunization from the work of early pioneers such as Louis Pasteur and Robert Koch, through the eradication of smallpox in 1980, to the recent introduction of genetically engineered vaccines, exposing the limits of public health authorities while suggesting how they can restore our confidence.
Stefana Sabin (author) and Nick Somers (translator) (Reaktion Books, July 2021) Sabin examines those who wore glasses through history, art and literature, from the green emerald through which Emperor Nero watched gladiator fights to Benjamin Franklin’s homemade bifocals and the famed four-eyes of Emma Bovary and Harry Potter. Spectacles are objects that seem commonplace, but Sabin shows that because they fundamentally changed people’s lives, glasses were the wellspring of a quiet social, cultural and economic revolution. She argues that modernity itself began with the paradigm shift that transformed poor eyesight from a severely limiting disease into a minor impairment that can be remedied with mechanisms constructed from lenses and wire.
Printed by www.jtcp.co.uk on Claro Silk 115gsm paper. 100% FSC certified using vegetable-based inks in a 100% chemistry-free process.