






Chief Executive Officer
Megan N. Schagrin, MBA, CAE, CFRE mschagrin@saem.org
Director, Finance & Operations
Doug Ray, MSA, dray@saem.org
Manager, Accounting Edwina Zaccardo, ezaccardo@saem.org
Director, IT
Anthony "Tony" Macalindong, amacalindong@saem.org
IT AMS Database Specialist
Dometrise "Dom" Hairston, dhairston@saem.org
Specialist, IT Support Dawud Lawson, dlawson@saem.org
Director, Governance
Erin Campo, ecampo@saem.org
Manager, Governance
Juana Vazquez, jvazquez@saem.org
Coordinator, Governance
Demetrius Pritchett, dpritchett@saem.org
Director, Communications & Publications
Laura Giblin, lgiblin@saem.org
Sr. Manager, Communications & Publications
Stacey Roseen, sroseen@saem.org
Manager, Digital Marketing & Communications, Alison “Ali” Mistretta amistretta@saem.org
Specialist, Web and Digital Content Alex Gorny, agorny@saem.org
Sr. Director, Foundation and Business Development
Melissa McMillian, CAE, CNP mmcmillian@saem.org
Sr. Manager, Development for the SAEM Foundation
Julie Wolfe, jwolfe@saem.org Manager, Educational Course Development
Kayla Belec Roseen, kroseen@saem.org Manager, Exhibits and Sponsorships David Perez, MSMC, dperez@saem.org
Director, Membership & Meetings
Holly Byrd-Duncan, MBA, hbyrdduncan@saem.org
Sr. Manager, Membership George Greaves, ggreaves@saem.org
Sr. Manager, Education
Andrea Ray, aray@saem.org
Sr. Coordinator, Membership & Meetings
Monica Bell, CMP, mbell@saem.org
Specialist, Membership Recruitment
Krystle Ansay, kansay@saem.org
Meeting Planner
Kar Corlew, kcorlew@saem.org
AEM Editor in Chief
Jeffrey Kline, MD, AEMEditor@saem.org
AEM E&T Editor in Chief
Susan Promes, MD, AEMETeditor@saem.org
AEM/AEM E&T Peer Review Coordinator Taylor Bowen, tbowen@saem.org aem@saem.org, aemet@saem.org
Monday - Thursday: 8 a.m. to 5 p.m. CT; Friday: 8 a.m. to 3 p.m. CT Phone: (847) 257-SAEM (7236) or email: saem@saem.org
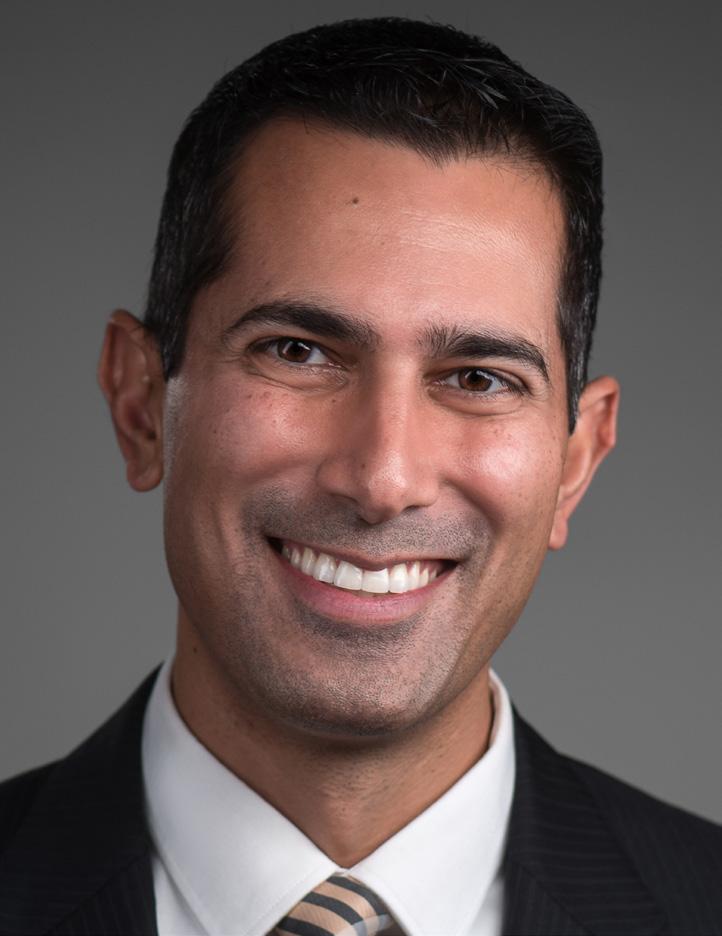
Ali S. Raja, MD, DBA, MPH President Massachusetts General Hospital/ Harvard Medical School
Michelle D. Lall, MD, MHS President-Elect Emory University
Pooja Agrawal, MD, MPH
Jody A. Vogel, MD, MSc, MSW Secretary-Treasurer Stanford University
Wendy C. Coates, MD Immediate Past President
UCLA Department of Emergency Medicine, David Geffen School of Medicine at UCLA
Members at Large
Yale Department of Emergency Medicine
Jeffrey P. Druck, MD
University of Utah School of Medicine
Ryan LaFollette, MD
University of Cincinnati
Julianna J. Jung, MD , MEd Johns Hopkins University School of Medicine
Nicholas M. Mohr, MD, MS University of Iowa Carver College of Medicine Ava Pierce, MD UT Southwestern Medical Center,
Thriving
The Growing Impact of Asynchronous Care in
A Traditional EM Career Path Not the Best Fit? Consider a Telehealth Fellowship!
88 Toxicology
Navigating the Rise of GLP-1 RA Exposures: What Emergency Physicians Need to Know
92 Understanding the Pharmacology, Treatment Challenges, and Aftermath of the Ghouta, Syria Sarin Attack
94 Voices & Viewpoints
The Legacy of Eugenics in Standardized Testing and Its Impact on Diversity in Emergency Medicine 96 The Pass/Fail Step 1 Shift: Implications for Underrepresented Emergency Medicine Bound Medical Students 98 Wellness Addressing Workplace Violence in Emergency Medicine: Bridging the Gap Between Reporting and Reality
Wellness Reflection Burnout in Emergency Medicine: Observations From a Future Physician
104 Wilderness Medicine Rising Search and Rescue Incidents Highlight Need for Enhanced Wilderness Medical Training 106 Women In Academic EM Careers by Design: Achieving Self-Promotion Without Being Seen as a Self-Promoter 108 Discover What You Might Have Missed: Top Publications From AWAEM

“Your support and camaraderie have been invaluable to me, and I am deeply grateful for it.”

Harvard Medical School/Massachusetts General Hospital 2024-2025 President, SAEM
SAEM has always felt like a family to me. I’ve met some of my best friends within our organization and have relied on them through thick and thin, seeking advice on everything from COVID-19 protocols to parenting. It’s always seemed so mindboggling to me that all of you — amazing academics focused on emergency medicine — also make time to build strong relationships and do so many remarkable things outside of the hospital. Your support and camaraderie have been invaluable to me, and I am deeply grateful for it. Connecting with everyone — from our most senior leaders to our medical students and residents – has meant the world to me and been my favorite part of SAEM.
So it was with a heavy heart that I recently learned of my dear friend Dr. Amy Kaji’s passing. I had known Amy for a couple of decades, but we really got to spend time together when we both joined the SAEM Board about ten years ago. She was impossible not to love. Somehow, she had done all the things in academic emergency medicine — from serving as SAEM President to editing Rosen's Emergency Medicine and achieving the rank of professor at UCLA, among too many other achievements to list here — and yet still found time to support her friends and family. Conversations with her were never superficial; she wanted to know what was happening outside of work, took the time to know Danielle and our boys, and shared her own struggles with a vulnerability that I’ve tried to emulate. Even when I last spoke to her a few weeks before her death, she found a way to focus the conversation on me instead of everything she was going through. Amy had a huge heart, and I
know many of us will always miss her immensely.
Amy was known for many things, including her leadership abilities and research skills. She was also an awardwinning educator and mentor, and one of the things she enjoyed most about being on the SAEM Board was our connection with the RAMS (Resident and Medical Student) Board. So, I know she’d be just as excited as I am to read this month’s profile on our RAMS President, Dr. Emily “Ly” Cloessner. She’s another fantastic leader, and she and the RAMS Board will have an amazing year, building off all their successes from last year.
Finally, I wanted to briefly mention the great meeting that we recently had with the National Institute on Minority Health and Health Disparities last month in Bethesda. Megan Schagrin, Melissa McMillian, Jody Vogel, MD, and I met with them and Jeremy Brown, MD from the National Institutes of Health Office of Emergency Care Research. We discussed several potential collaborative opportunities, and I am excited about the possibilities that lie ahead. I hope to share more details with you soon.
In the meantime, please enjoy this month’s Pulse – I know Amy would have loved reading about the fantastic work being done by everyone in this organization that she loved so much!
ABOUT DR. RAJA: Ali Raja, MD, DBA, MPH, is a professor of emergency medicine at Harvard Medical School and the deputy chair of the department of emergency medicine at Massachusetts General Hospital.
Member-at-Large, 2024-2025 SAEM Board of Directors
Associate Professor, Assistant Program Director, Department of Emergency Medicine, University of Cincinnati
Dr. LaFollette is SAEM Board Liaison for the following SAEM Groups:
President: Petra Duran-Gehring, MD Overview
AEUS, the largest community of educators and researchers in emergency ultrasound, is dedicated to the education and development of the emergency medicine ultrasound network.
• Provided scholarship funding for the ARMED program (Arthur Broadstock, MD, University of Cincinnati, and Jacob Schoeneck, MD, Wake Forest University) and ARMED MedEd (Rebecca Theophanous, MD, Duke University).
• Presented several awards, including the AEUS Innovation Award, which supports pioneering advancements in emergency ultrasound, and the AEUS Medical Student Ultrasound Enthusiast Award, which funds attendance at the SAEM annual meeting. AEUS also sponsors multiple SAEMF AEUS Research Grants.
• AEUS facilitated a highly successful Grant Writing Mentorship Program, led by Dr. Frances Russell, offering grant writing support and instruction to AEUS members. In the 2023-2024 cohort, nine mentees participated, with one receiving a SAEMF grant, two securing foundational grants, and two others funded by EMF.
• SonoGames24 was the largest event yet, with 105 resident teams participating!
Special thanks to the SonoGames Organizing Committee and the 90+ member volunteers for making it a success. We look forward to an even bigger event in Philadelphia in 2025!
• The AEUS Narrated Lecture Series has been updated with five new courses, including four on regional anesthesia and one on traumatic pneumothorax, along with eight updated courses.
• Probing the Literature is a monthly ACEP/ SAEM National Ultrasound Journal Club available to academy members, covering two articles each month.
Chair: Nancy Kwon, MD, MPA
The Faculty Development Committee is charged with creating resources and education to further the career opportunities of academic emergency physicians and to act as a central resource for academic career advancement.
• Presented seven didactics at SAEM24, in collaboration with AACEM, AWAEM, the Simulation Academy, and the Education Committee.
• The updated Academic Career Guide will soon be available on the SAEM website.
• Developing a toolkit and pathway for junior and mid-career faculty.
• Planning a webinar on the diverse career options in and beyond emergency medicine, covering topics such as career transitions, retirement, and alternative job opportunities.
• Collaborating with AWAEM to support faculty with promotion letters and guidance through the promotions process.
• Continuing the development of the Who’s Who in Academic Emergency Medicine podcast.
Chair: Joshua Joseph, MD, MS, MBA
Overview
The ED Administration and Operations Committee has the task of advancing the unique operations and administrative challenges of the academic emergency department. It does this by monitoring trends and new opportunities in the space and providing educational resources and
community in several outputs online and through the annual meeting.
• Updated the Asynchronous Operations Curriculum on SOAR
• Sponsored an SAEM24 didactic on operationalizing an operations curriculum in conjunction with the education committee
• Working on an educational series about artificial intelligence and its applicability to administration and operations
• Developing a webinar on the impact of boarding in the emergency department
Chair: Dustin Williams, MD
Overview
The Membership Committee is tasked with helping recruit and engage the SAEM membership. Through a regular survey, the committee makes recommendations responding to the trends and directions of the membership and encourages member involvement through communications and onboarding.
• Created a membership survey, to launch in September 2024, which will be used to change SAEM programming in the years to come
• Achieved record membership and attendance at the SAEM Annual Meeting
• Analyzation and implementation of the 2024 Membership Survey findings
• Engagement of residents and medical students through regional and national meetings
Chair: Erin Kane, MD, MHPE
The Emergency Medical Services Interest Group was established to identify and address the educational needs of EMS providers and their learners by offering educational sessions at the annual meeting and updating ongoing EMS curricula.
• Identifying positions for section membership to have a greater involvement in SAEM EMS IG development and works
• Unifying the EMS fellowship list offerings between societies for more consistently up to date information
• Working with the National Association of EMS Physicians (NAEMSP) Education Committee to develop EMS curricular development updates, scholarly activity offerings, and mentorship opportunities for EMS-bound learners
• Working with RAMS to develop an annual EMS Fellowship webinar for interested applicants to receive updates and explore opportunities in EMS scholarly activity
• Exploring opportunities for further collaboration across national societies and institutions for broader EMS exposure for non-fellowship trained providers to participate in work that improves prehospital care in critical access and underserved communities
Chair: Raghu Seethala, MD
Overview
The Critical Care Interest Group aims to promote emergency medicine-critical care (EM-CC) physicians at the local and national levels by recognition and engagement in leadership development activities. The Critical Care IG also creates a forum and community for mentorship, education and operations in the varied environments of EM-CC.
• The group sponsored two didactics at SAEM 24 on the topic of critical care in the era of boarding and co-sponsored a didactic with GEMA on resuscitation education in resource-limited settings
Works in Progress
• The interest group is exploring crowdsourcing methods to gather comprehensive data sets on critical care boarding across member institutions, with a focus on better quantifying its impact.
Chair: Jennifer Mitzman, MD
Overview
The Pediatric Emergency Medicine Interest Group is tasked with promoting pediatric emergency medicine as a career path within emergency medicine. This is achieved through didactic presentations, enhanced research integration, and increased fellowship support.
Notable Accomplishments
• Sponsored a didactic on the complexities of managing pediatric behavioral health crises in the era of boarding
Works in Progress
• The Pediatric Interest Group and its growing membership is striving for Tier
III interest group status through rigorous education and mentorship structure
• Increasing research visibility by permitting the concurrent acceptance of abstracts at adjacent conferences, thereby enhancing the presence of Pediatric Emergency Medicine at our annual meeting

Daniel N. Jourdan, MD, NRP
Resident Member, 2024-2025 SAEM Board of Directors
Chief Emergency Medicine/Internal Medicine
Resident, Henry Ford Hospital, Detroit
Dr. Jourdan is the SAEM Board Liaison for the following SAEM groups:
Chair: Amanda J. Deutsch, MD
Overview
The Wellness Committee is actively engaged in addressing emergency physician wellness and resilience, primarily by building a knowledge hub of resources, tools, and models focused at both the individual and organizational levels.
• Organizing the 3rd Annual Stop the Stigma EM Month this October. Focused on addressing the stigma surrounding mental health and accessing support, the event last year included collaboration with 14 national and international EM organizations.
• Significant contributor to SAEM24, including 6 didactics, the annual storytelling evening, and a workshop on wellness tools that drive change.
• Piloted the first-ever Wellness Consultation in collaboration with the SAEM Consultation Services Committee.
Next meeting: September 12, 3 p.m. CT
Co-chairs: Alyssa Valentyne, MD, Gayle Kouklis, MD
Overview
The Climate Change and Health Interest
Group focuses on the impact of climate change on public health, specifically within emergency medicine. Group efforts include research, advocacy, and education regarding the impacts of climate change and opportunities to mitigate its effects within the house of medicine.
• Over the past year, published multiple SAEM Pulse articles in addition to multiple presentations and didactics at SAEM24.
• Currently collaborating with ABEM to create board (re)certification questions based on the latest climate health research.
• Focused on publishing multiple SAEM Pulse articles and submitting didactics to SAEM25.
Next meeting: September 26 at noon, CT
Co-chairs: Nicholas Stark, MD, Zaid Altawil, MD, and Jonathan Oskvarek, MD, MBA
Overview
The Innovation Interest Group seeks to inspire and foster collaboration among innovation-minded emergency physicians to share ideas on applying design thinking and emerging technologies to help solve the challenges of today and the future in the health care system.
• Increased membership to 200+
• Hosted a didactic at SAEM24 focused on utilizing design thinking to find solutions to challenges in psychiatric emergency medicine.
• Collaborating with other SAEM Interest Groups on webinars: “AI in the ED” and “Telehealth in EM”
Chair: Katherine Dickerson Mayes, MD, PhD
Overview
The Neurologic Emergency Medicine Interest Group seeks to enhance research, education, and patient care in all areas of acute neurological emergencies, including traumatic brain injuries, stroke, epilepsy, and intracranial hemorrhages.
• Interest group members actively participate in multiple trials, including ICECAPS and BOOST.
• Planning for multiple didactic submissions for SAEM25, including new guidelines for the care of traumatic brain injuries and intracranial hemorrhages.

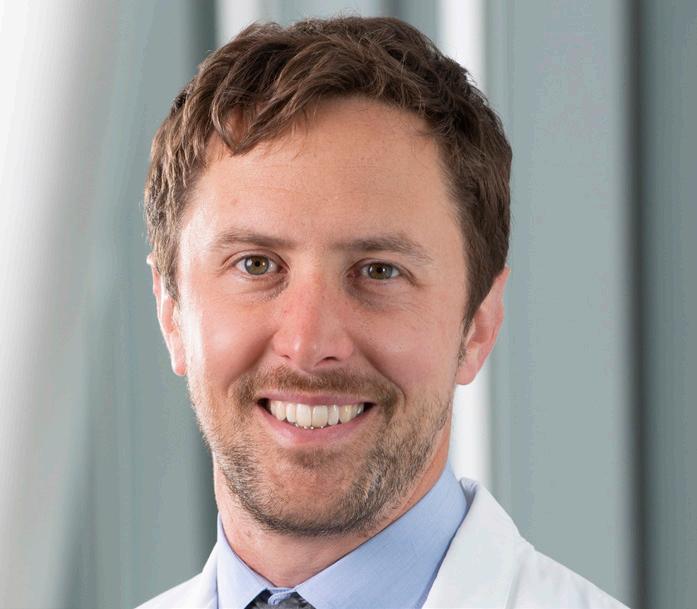
Emily “Ly” Anne Cloessner, MD, MSPH, is a current PGY-4 and chief resident at Washington University in Saint Louis. Her path to emergency medicine (EM) began with a career in public health and public service, driven by a commitment to community service. As a fellow at the Centers for Disease Control and Prevention (CDC), she developed domestic vaccine policy, contributed to the Global Ebola Vaccine Implementation Team’s guidance on Ebola vaccine use, and supported CDC international offices during infectious disease outbreaks. Her work earned her multiple awards from agencies within the U.S. Department of Health and Human Services.
Dr. Cloessner earned her medical degree from the Medical University of South Carolina and completed her undergraduate studies at the College of Charleston. She received her master's from Johns Hopkins Bloomberg School of Public Health. In her work with SAEM, she has served as a member-at-large on the RAMS board from 2023 to 2024, as the RAMS board liaison to the research committee since 2023, published several Pulse articles with the research committee, and currently chairs the nominating committee. She is also active in the SAEM Global Emergency Medicine Academy and has helped organize the World Health Organization Basic Emergency Care Training of Trainers course at the SAEM Annual Meeting for the last two years. Dr. Cloessner is the 2024-2025 president of the SAEM RAMS board.

Congratulations on your election as the new president of RAMS. What are your primary goals for RAMS during your term?
Thank you! I’m so excited to be leading our RAMS Board this year. I couldn’t ask for a more talented group of people to be working with.
My primary goal is to help RAMS engage fully with their membership. RAMS has experienced tremendous growth over the past two years and, with over 5,200 members, now makes up more than half of SAEM’s total membership. Given this influx of new members, I want to ensure that all RAMS are empowered to become active members of SAEM. I believe that engaging with SAEM academies and committees and using our SAEM Career Roadmaps can connect any RAMS member to the experiences they need to advance their career in emergency medicine. Our RAMS board is working hard to make these connections possible.
What issues do you feel are most relevant to current and future emergency medicine trainees? What steps do you hope to take toward addressing these issues during your tenure as RAMS president?
Emergency medicine trainees have faced several challenges in recent years. The job report of 2021 and the subsequent SOAP of 2022 have changed the perceptions of our specialty among EM-interested medical students. For residents committed to EM, the influence of private equity in our job market and upcoming changes to how residents will be evaluated in residency and boarded thereafter are sources of ongoing anxiety.
These issues have fundamentally changed what it means to be a trainee in EM. EM residents and EM-interested students now come from a broader application pool. Additionally, recent Match and SOAP data show that many current trainees may not have originally planned on EM as their specialty. As RAMS president, I see it as my job to help all RAMS, especially those struggling to find their niche, connect with experiences that will help them build fulfilling careers. To this end, the RAMS board will continue revising our career roadmaps, engaging with our workforce committee, and stepping up our membership engagement efforts to assist all our RAMS in creating successful careers in emergency medicine.
When, why, and how did you first become involved with RAMS?
I attended my first SAEM meeting in my first year of residency. My program did not have a strong presence in global health, so my program director sent me to the annual meeting and told me not to return without a research mentor. Together, we put together a list of sessions for me to attend, including the Global Emergency Medicine Academy’s (GEMA) World Health Organization (WHO) Basic Emergency Care Training of Trainers course (which I have since helped organize), the GEMA meeting, and several research presentations. At the annual meeting, I not only found a research mentor, I discovered a whole community of academic emergency physicians who were just like me. I knew I had found my academic “home” with these physicians, who remain my mentors. I can’t speak highly enough about the
continued on Page 8
people in GEMA: Dr. Torben Becker, who has been endlessly available to me; Dr. Kyle Martin, who has helped me prepare for fellowship applications; and the fine folks who have let me help organize the WHO course the past few years. It’s a wonderful group to grow with and learn from.
My positive experiences with GEMA led me to seek further involvement with SAEM. As a resident, RAMS seemed like the logical place to start. With the encouragement of my mentors, I ran for the board in the 2022-2023 year and served as a member-at-large on the RAMS board last year. This past year, I was encouraged to run for the presidency and was successful in that election.
Why should EM residents and medical students become involved with RAMS? What needs does the group meet or concerns does it address?
The beauty of working in a specialty that sees any patient, for any reason, at any time, is that there is also a place in emergency medicine for any academic interest you can imagine. Through its academies and committees, SAEM offers myriad experiences for RAMS members seeking mentorship or career-building opportunities. Particularly for those in residency programs or schools with smaller research communities, engagement with SAEM can help fill gaps in resumes and prepare members for the next stage of their careers. I found the mentorship and research opportunities I needed for my fellowship application through SAEM, and I believe other RAMS can find the same.
What upcoming RAMS initiatives excite you?
More than any single initiative, I’m excited about the overall growth in our RAMS membership and the expansion of activities from the RAMS board. This year, our board is operationalizing its strategic plan and working to build greater connections between our board and SAEM academies, as well as developing partnerships with other national EM organizations. We have increased our involvement with the workforce committee, continued our work with #StopTheStigmaEM, and are updating the RAMS career roadmaps. These efforts have already yielded promising results. I get immense joy from hearing how RAMS members have become more involved at the national level, connected with new research mentors, or published research with colleagues they met through SAEM. These are the fundamental experiences that build community in our specialty. I’m proud of the work the board has done to facilitate these experiences for our members.
Who or what influenced your decision to choose the academic/EM specialty and if you were not doing what you do, what would you be doing instead?
I came to medicine after a career in public health, which directly influenced my choice of emergency medicine as my specialty. EM physicians are at the forefront of every epidemic and public health issue facing America. On any given day I might treat patients who are victims of gun violence, COVID, traffic accidents, or the opioid crisis. It therefore probably comes as no surprise that if I were not in medicine, I would likely still be at the CDC, working to reduce the risk of people experiencing health-related emergencies.


Any tips on surviving, perhaps even thriving, during residency?
I have two tips:
First, embrace wherever you find yourself. I’m in Saint Louis, and I love it here. Where else can one find this caliber of training, along with a local Taco Bell Fitness Course? (I’m not kidding.) Keeping a sense of curiosity about your new home can make residency more enjoyable.
Second, pare down. Training significantly limits your free time. Being honest with yourself about what is important academically and personally will ensure that valuable time is well spent. For me, this has meant saying yes only to research that aligns with my goals and makes sense for me and focusing my external commitments within SAEM, while allowing other opportunities to pass by.
Tell us about your dream workday.
My dream workday involves being in our trauma and critical care pod, where our sickest patients are treated. I get in a few thought-provoking and successful resuscitations. Drinks and sandwiches at the Gramophone, our usual hangout, follow afterward.
What are your research and/or academic interests?
I am interested in the intersection of larger public health issues and the emergency department, both in the United States and globally. I am particularly concerned with infectious disease cases, especially vaccine-preventable ones, that result in emergency room visits. My overall career goal is to maximize community-level interventions to prevent the progression of these diseases to epidemic levels and create emergency room protocols for outbreaks if these preventative measures fail.
I am also engaged in work with point-of-care ultrasound (POCUS), particularly its application in settings with limited resources. I’m a member of GEMA’s new POCUS subcommittee and work with the Global Health Coalition Corporation, teaching POCUS globally. Much of my current work that is nearing publication is related to my POCUS interests.
October is #StopTheStigmaEM month. Stigma is a leading barrier to mental health care for emergency physicians. Many fear that treatment for mental illness could jeopardize their careers or licenses to practice.
What do you consider the key challenges to addressing this stigma?
This can be a sensitive area for trainees, and I’m proud of RAMS’ ongoing involvement with the #StopTheStigmaEM campaign to reduce stigma around seeking mental health care within our community. Overall, there are positive signs of change within the medical community regarding this issue. While many jokes have been made about mandatory wellness modules, the fact that ACGME now has requirements for trainee wellness was a crucial institutional step in acknowledging the mental health needs of physicians. Many programs, including mine, now provide multiple mental health resources beyond what ACGME mandates.
However, addressing stigma within our community is not enough. As negative perceptions around mental health issues change within the medical field, we find ourselves in a situation where the culture of medicine is ahead of its licensing entities. For example, in Missouri, my licensing application asks, “Do you currently have any condition or impairment which in any way affects your ability to practice in a professional, competent, and safe manner, including but not limited to: (1) a mental, emotional, [or] nervous…. disorder?” As long as licensing applications continue to include such questions, physicians will worry that seeking necessary health care may negatively impact their career trajectory. Ultimately, resolving the stigma around mental health care requires all parties to be on the same page regarding physicians seeking care.
What can be done to create a sense of safety for EM physicians and medical trainees that would encourage them to ask for help or self-report when they’re struggling with their mental health.
As mentioned, creating a sense of safety for physicians to seek mental health care will come from acceptance, both inside and outside the medical community, that physicians have the same health care needs as everyone else. More immediately, I encourage trainees who are struggling to reach out to a trusted mentor if they are unsure how to access the confidential resources available at their institution.
What is one thing you can't do without while on shift?
Snacks. I’m infamous for needing a constant supply of food on shift.
What is your “go to” work/on-shift hack?
I learned this tip for caring for trauma patients from my co-resident, Emilie Lothet: if you need to irrigate a head laceration and don’t want to make a mess, cut down a side of a basin and rest the patient’s head through the opening. The basin will catch the irrigation fluid, and you can use a Yankauer to prevent any overflow.
What is a favorite FOAMed resource?
Derangedphysiology.com
What would most people be surprised to learn about you?
I triple majored in college. I have a bachelor of science in psychology and in chemistry, along with a bachelor of arts in art history. I put serious thought into whether I would pursue a career in art preservation.
Who would play you in the film of your life and what would that film be called?
The medical classic, “The House of God” needs a sequel. Let’s call it “Take Your Own Pulse” (rule 3 in the original book) and put in an ensemble cast from everyone’s favorite medical TV shows. Can Katherine Heigl play me?
What is your guilty pleasure?
I never feel guilty about taking time for myself or for the health of my mind and body. I’m currently enjoying caring for my summer garden and catching concerts in town.
What is at the top of your bucket list?
Easy! Refreshing my SCUBA certification before my elective rotation in Hawaii. It turns out there are several places you can dive around Missouri, so I should get this done before the year’s end!
Who would you invite to your dream dinner party?
An unfortunate consequence of medical training is that residency and then fellowship matching have dispersed my friends across the country. My dream dinner party brings all of us back together for an amazing home cooked meal.

SAEM mourns the loss of our former President Amy H. Kaji, MD, PhD, a compassionate leader, cherished colleague, and beloved friend. Dr. Kaji passed away on August 1, 2024 at the age of 56. She touched countless lives through her unwavering dedication to emergency medicine and her deep commitment to SAEM.
At the time of her passing, Dr. Kaji was Senior Advisor for Academic Development at Harbor-UCLA Medical Center and a Professor of Clinical Emergency Medicine at the David Geffen School of Medicine at UCLA. SAEM extends its deepest condolences to her family, friends, trainees,
colleagues, and all those who had the privilege of working with and learning from her.
Dr. Kaji's medical career was marked by exceptional brilliance and dedication. A Harvard College graduate, she earned her medical degree from Thomas Jefferson Medical College. Her extensive training included an emergency medicine residency and research/disaster medicine fellowship at Harbor-UCLA, where she also completed an MPH and a doctorate in epidemiology from UCLA School of Public Health.
Dr. Kaji authored hundreds of published works and was a methodological
and statistical editor for Annals of Emergency Medicine and JAMA Surgery. In addition, she edited the 9th edition of Rosen's Emergency Medicine and co-authored the first edition of the study guide, Emergency Medicine Board Review. Her three-book series, The Kaji Review, remains a valuable educational resource for emergency medicine students, residents, and attending physicians.
A renowned and respected educator, Dr. Kaji was the recipient of the ACEP National Faculty Teaching Award and the UCLA Distinguished Lecturer Award.
Beyond her professional achievements, Dr. Kaji was a cornerstone of SAEM,
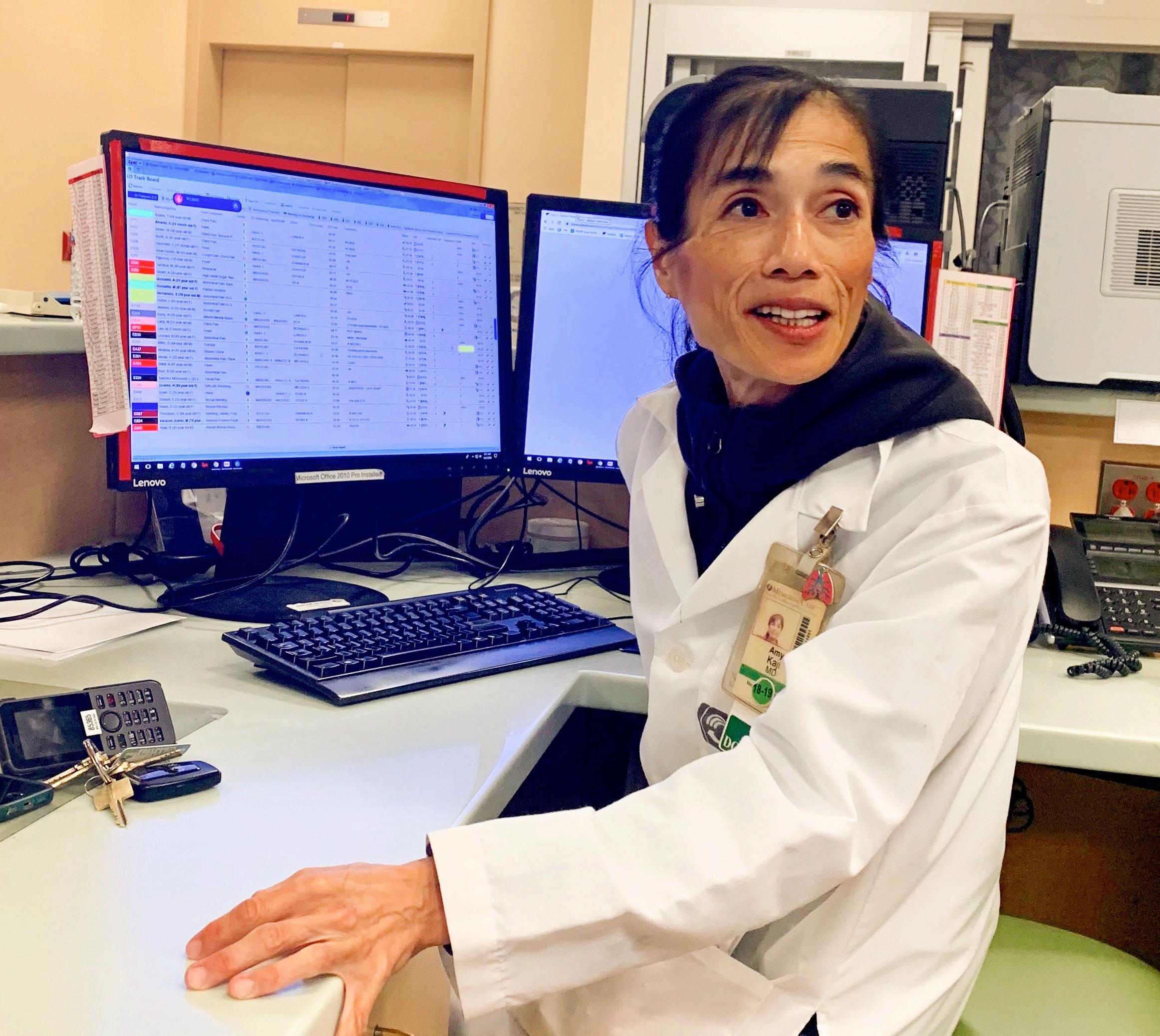
exemplifying selflessness and dedication throughout her 22 years as a member. In addition to chairing several committees, Dr. Kaji was a devoted member of the SAEM Foundation Board of Trustees from 2014 to 2023 and served on the SAEM Board of Directors from 2013 to 2023. As the 2021-2022 Board President, she guided the organization with vision and resilience through the challenges of the post-COVID world, helping to shape its future and strengthen its mission.
Dr. Kaji’s unwavering belief in the power of collaboration and teamwork for the greater good was evident in every aspect of her life. Whether mentoring
young physicians, chairing committees, leading SAEM, or providing care during the pandemic, she fostered a spirit of unity and cooperation, always prioritizing the recognition and promotion of others over herself. Her humility and modesty were hallmarks of her character, and she touched countless lives through her kindness.
Dr. Kaji’s beautiful soul, warm smile, and enormous heart will be deeply missed by all who knew her. As we remember Dr. Kaji, we find solace in her own words, which encapsulate her character and the legacy she leaves behind: “[At the end of my career] I would like to be remembered
as being a thoughtful, dedicated emergency physician, teacher, and team player.”
Amy, you will be remembered for all this and so much more. Your legacy is woven into the fabric of our organization and the hearts of all fortunate enough to have known you. Rest in peace.
SAEM Foundation is accepting donations to support a special award in honor of Dr. Kaji. Donations can be made at saem.org/donate
By Hannah Mishkin, MD, MS; Lindsay MacConaghy, MD; Neha Raukar, MD, MS; Laura Walker, MD, MBA; and Wan-Tsu Wendy Chang, MD, on behalf of the SAEM Academy of Women in Academic Emergency Medicine
Artificial intelligence (AI) is rapidly evolving and increasingly integrated into various aspects of our professional lives. In this series, we will explore how AI, particularly large language models (LLMs), can enhance efficiency in academic work within emergency medicine.
Introduction
AI enables computer systems to perform tasks that typically require human intelligence, such as problemsolving, learning, and reasoning. Essentially, AI uses advanced statistical methods to predict outcomes based on patterns in large datasets. This predictive capability is enhanced through neural networks — computer systems inspired by the human brain,
where data is processed through interconnected layers of "neurons" that adjust based on recognized patterns.
A specific type of neural network called transformers excels at handling sequences, such as sentences, by focusing on different parts of the data simultaneously. This allows them to understand context and generate coherent responses. These models are trained on vast bodies of text, known as corpora, which may include books, articles, and even social media posts, enabling them to process and generate natural language.
Among the most advanced AI tools available are LLMs such as ChatGPT, Copilot, and BERT. These models are
designed to understand and generate human language, making them valuable tools for both personal and professional applications in emergency medicine.
This article series will delve into various applications of LLMs in academic emergency medicine. We encourage you to explore using an LLM available through your institution or consider utilizing the free version of OpenAI’s ChatGPT 3.5, accessible at www.chatgpt.com
Getting
To begin using an LLM like ChatGPT, you’ll need to create a free account. Once your account is set up, you can interact with the model by asking it to perform tasks using everyday language.
For effective use, follow this three-step process:
1. Prompting: Clearly state what you want to create, including context about who you are and your intended audience.
2. Detailing: Provide a thorough description of the desired output. The more details you give, the closer the result will be to your expectations.
3. Revising: Review and provide feedback on the output. You might ask the LLM to shorten a speech, adjust the tone of an email, or refine the language used.
When interacting with LLMs, think of them as a helpful administrative assistant. Use conversational language, similar to how you would talk to a colleague, rather than a string of keywords. However, be mindful that LLMs operate in the public domain, so avoid including sensitive or private information.
Feedback is a crucial element of the learning process, especially in emergency medicine education. Delivering difficult feedback effectively requires careful attention to tone, timing, and context — areas where LLMs can offer valuable assistance. Consider this example of feedback:
“Learner X really needs to work on their attitude. They arrived five minutes late, missed some key findings on the physical exam, and when I provided feedback, they were defensive.”
Now, let's use ChatGPT to reframe this feedback to be more empathetic and constructive.
Step-by-Step Guide:
1. Open ChatGPT. Start by opening your ChatGPT interface.
2. Enter the Prompt. Input a clear and specific prompt, such as: "I have received some difficult feedback on a learner's performance. Please help me rephrase this feedback in a supportive way and suggest the best time and method for delivering it."
3. Input the Feedback. Copy and paste the feedback you received, ensuring that any identifying details are removed for privacy.
Here’s an example of a response generated by ChatGPT:
Supportive Feedback:
"Hi [Learner X], I’d like to discuss some observations from our recent shift together. First, I want to acknowledge the effort you’ve been putting into your learning and the progress you’ve made. It’s clear you’re committed to becoming a skilled clinician, which I greatly appreciate.
I noticed a few areas where there might be room for growth. For example, during our shift, you arrived slightly late and missed some key findings on a physical exam. I understand that shifts can be hectic, and these things happen to all of us at times.
When I provided feedback afterward, I sensed some defensiveness, which is completely understandable. Receiving feedback can be challenging, especially when we’re striving to do our best. My goal is to support your development and help you grow as a clinician. Feedback is a tool for growth, and I’m here to work with you through any challenges you might face.
Let’s discuss strategies to improve in these areas together, such as ensuring timely arrival, enhancing physical exam skills, and making feedback sessions more constructive. I’m here to support you every step of the way."
Refining the Output:
While this response is well-crafted, always review AI-generated content for accuracy and relevance. Adjust as needed to ensure it aligns with your intent. Additionally, consider how this feedback might be delivered — whether in person, via email, or as part of a remediation plan. The flexibility of LLMs allows for continuous refinement of communication strategies.
Conclusion
AI tools like ChatGPT enhance academic
“Artificial intelligence (AI) is rapidly evolving and becoming increasingly integrated into various aspects of our professional lives.”
emergency medicine by streamlining feedback, improving communication, and optimizing workflows. By integrating these technologies thoughtfully, we can elevate the quality of education and care we provide.
The authors would like to acknowledge the use of GPT-4, an AI language model developed by OpenAI, for providing editorial assistance and refining the manuscript.

Dr. Mishkin is the emergency medicine residency program director at Reading Hospital, Tower Health, in West Reading, Pennsylvania. Her academic areas of focus include innovation in medical education and administration, and diversity, equity, and inclusion.

Dr. MacConaghy is an assistant professor of emergency medicine at Geisinger Commonwealth School of Medicine and serves as the assistant residency program director at Guthrie Robert Packer Hospital in Sayre, Pennsylvania. Her professional focus includes advancing medical education and residency training.

Dr. Raukar is an associate professor and vice chair for academic advancement and faculty development at Mayo Clinic Rochester. Her research emphasizes life-threatening injuries in athletes, innovations in emergency medicine, and faculty and leadership development. She leads initiatives to cultivate the leadership skills of the next generation of physicians.

Dr. Walker is an assistant professor of emergency medicine at Mayo Clinic. She is a leader in emergency medicine and hospital operations, focusing on health systems, equity, and quality improvement. Her research aims to improve healthcare systems and promote effective management practices within emergency medicine.

Dr. Chang is an associate professor of emergency medicine at the University of Maryland. Her professional focus is on medical education and the management of neurologic emergencies.

By McRae Wood, Kristy Jones, and Cole Ettingoff, MPH, on behalf of the SAEM Behavioral Health Interest Group
Emergency departments (EDs) play a critical role by providing immediate care for psychiatric patients during crises. However, ensuring continuity of care post-discharge remains a significant challenge. Patients frequently revisiting the ED for behavioral health complaints add strain to patient loads and are at risk of bias. Effective strategies are essential to bridge the gap between acute ED care and ongoing communitybased mental health support. Several interventions and models have been studied and implemented to address this issue, aiming to reduce readmissions, improve patient
outcomes, and ensure a seamless transition to community care.
Critical Time Intervention (CTI) is a widely researched model designed to support psychiatric patients during the critical period following discharge from the hospital. This intervention is characterized by its time-limited, community-based approach involving three phases: Transition, Try-out, and Transfer of Care. In the Transition phase, intensive support is provided as patients leave the hospital, helping them adjust to life outside the institutional setting. During the Try-out phase, patients
begin to test their ability to manage independently while still receiving support. The final Transfer of Care phase involves gradually connecting patients to long-term community resources and services. (BioMed Central) CTIs have shown an overall improvement in patient outcomes by ensuring continuous care during the vulnerable transition period. Despite the challenge of maintaining caseworkers with small caseloads, local analyses of readmission costs and unreimbursed care demonstrate the financial value of such a model. Implementing CTI requires an initial investment in training

“Effective strategies are essential to bridge the gap between acute ED care and ongoing community-based mental health support.”
and resources yet offers a structured method to ensure psychiatric patients do not fall through the cracks during the critical post-discharge period, thereby decreasing readmission costs over time.
Various transitional care programs have been developed to enhance the continuity of care for psychiatric patients and reduce ED readmissions. These include the High Alert Program (HAP), which specifically targets patients at high risk of readmission by providing intensive follow-up and assistance with coordination of care. The PatientCentered Medical Home (PCMH) model focuses on a holistic approach to patient care, integrating mental health services within primary care settings. Lastly, the Collaborative Care (CC) Program involves
a team-based approach where primary care providers, care managers, and psychiatric consultants work together to manage patients’ mental health conditions. These models emphasize comprehensive, multidisciplinary services that incorporate behavioral and pharmacological strategies, case management, and coordination between inpatient and outpatient services. (MDPI) Robust partnerships with such programs may facilitate “warm” referrals, exchange health records, and open channels for patient information flow back to the ED, improving overall continuity of care.
Effective continuity of care often involves a multidisciplinary approach that includes a range of health care professionals.
Studies highlight the importance of involving case managers, social workers, pharmacists, and peer support volunteers in the care process. For example, case managers can ensure that patients attend follow-up appointments and adhere to treatment plans, while social workers can help patients navigate social services and access community resources. Pharmacists play a key role in medication management, ensuring patients understand their prescriptions and avoid adverse drug interactions. Peer support volunteers, who have lived experience with mental health conditions, can offer unique insights and emotional support to patients. This collaborative approach helps manage medication compliance,
continued on Page 17

continued from Page 15
provide emotional support, and connect patients with community resources, thereby reducing the likelihood of readmissions. Although multidisciplinary discharge planning is common in traditional inpatient settings, it is less common in EDs. Hospitals experiencing frequent prolonged ED boarding may need to create similar discharge planning processes to aid ED psychiatric patients.
EmPATH units offer a proven model of care delivery for acute psychiatric needs, helping keep ED beds open for medical emergencies by providing designated spaces for mental health crises. These units take medically cleared patients out of the chaotic ED and into community-styled open spaces, immersing them with psychiatrists or advanced practice providers who draft treatment plans. These units create a therapeutic environment that reduces the stress and chaos often associated with EDs, allowing patients to receive more focused and specialized care. They have also been shown to significantly improve patient satisfaction and outcomes by providing a bridge between the ED and long-term psychiatric care. If prolonged treatment is required, patients are transferred to inpatient psychiatry units. The success of EmPATH units underscores the importance of creating dedicated spaces for psychiatric care within hospitals, ensuring that patients receive the appropriate level of care without overwhelming the ED. Additionally, EmPATH units decrease ED boarding times, hospital length of stay, and psychiatric admission rates while improving outpatient follow-up visits and enhancing continuity of care following a mental health emergency. Initial funding for such units can be daunting, but public-private partnerships have made them possible in several states, improving ED revenue
Small changes in practice can significantly impact the delivery of care for patients with acute psychiatric concerns. Safety planning for the time immediately following discharge is crucial. The Coalition on Psychiatric Emergencies offers an ICARE2E toolkit for improving
care delivery, including tools for lethal means counseling, safety planning, and post-discharge caring contracts. Providing practical patient education on coping techniques, resources like the suicide and crisis hotline (988), and community crisis centers should be comparable to education provided for other common conditions, such as exercises for musculoskeletal injuries. Culturally sensitive patient education focused on specific, attainable tactics should be part of the overall discharge strategy to improve patient outcomes and lower the likelihood of behavioral health ED readmissions.
EDs often serve as the final safety net for patients who have fallen through other systems. While many impactful interventions for preventing acute psychiatric stabilization or ED revisits are upstream, EDs are uniquely positioned to offer invaluable data on unmet community needs related to psychiatric care. Such data can be valuable to public health and community partners, allowing ED leaders to advocate for patients beyond their walls. Establishing consistent primary care for psychiatric patients has been shown to improve continuity of care and reduce acute ED visits. By analyzing data on ED visits, hospitals can identify trends and gaps in community mental health services. This information can be used to advocate for increased funding, improved mental health services, and policy changes that address the root causes of frequent ED visits. EDs can also collaborate with local health authorities and community organizations to develop targeted interventions that address the specific needs of their patient populations.
EDs routinely provide patient education upon discharge for various diagnoses, yet behavioral health presentations may receive less support. Although chronic behavioral health conditions cannot be cured in the ED, the unique perspective and training of ED staff can greatly impact patients and their families. Acute crises present prime opportunities to educate patients on coping techniques and available resources like crisis hotlines and community centers. Culturally sensitive patient education focusing on specific, attainable strategies should be part of the discharge plan to improve outcomes
and reduce readmissions. For example, patients presenting with suicidal ideation may be provided with information on safety planning, coping strategies, and local mental health resources. ED staff can also offer guidance on recognizing warning signs of a mental health crisis and steps to take if those signs appear. By providing comprehensive discharge education, EDs can empower patients to take control of their mental health and reduce the likelihood of future crises.
(Cureus)
Ensuring continuity of care for psychiatric patients discharged from emergency departments is necessary for improving patient outcomes and reducing the burden on healthcare systems. Strategies such as Critical Time Intervention, transitional care programs, multidisciplinary approaches, EmPATH units, improved care delivery, and reinforced patient education have all proven effective in bridging the gap between acute care and ongoing assistance. Through collaborative efforts and the implementation of innovative care models, the healthcare system can better serve psychiatric patients, ultimately improving public health while reducing the strain on emergency services.


McRae Wood is an MD candidate at Trinity School of Medicine, Georgia, pursuing her passion for emergency medicine. She enjoys soccer, traveling, and spending time with her husband and new baby boy.
Kristy Jones is a fourth-year medical student at Mercer School of Medicine and aspiring psychiatrist with an interest in acute care. She was vice chair of the planning committee for the recent Symposium on Responding to Behavioral Health Emergencies.

Cole Ettingoff, MPH is a thirdyear medical student at Trinity School of Medicine in Georgia. He has a deep passion for all things EM, EMS, and public health and, among other roles, is a leader in the SAEM Behavioral Health Interest Group.

Ronny Otero, MD, MSHA; Neha P. Raukar, MD, MS; and Anthony Rosania, MD, MHA, MSHI on behalf of the SAEM Vice chairs Interest Group
Stepping into the role of vice chair presents an exciting opportunity that promises both challenges and rewards. It's a position that not only offers the opportunity to significantly influence your department but also provides a unique perspective on academic administration. As clinical chairs increasingly handle issues beyond the emergency department, including roles within medical schools, the expansion of emergency departments, and service on hospital committees, the vice chair’s role in managing modern academic emergency medicine departments has become increasingly crucial.
To fill these roles, a chair depends on the expertise of senior faculty members to advise on the increasingly complex landscape of departmental missions. A vice chair is usually appointed when an academic department has expanded in size and complexity to the extent that the chair needs additional support from senior faculty members with specialized expertise. These vice chairs might focus on specific areas such as research, operations, education, or clinical services, depending on the department's needs. Each vice chair brings a distinct skill set to the department, contributing to its overall
success. However, responsibilities and job descriptions can vary widely between institutions. Even if two vice chairs hold the same title, such as vice chair of research, their duties and expectations might differ based on the institution's priorities, resources, and structure. This diversity in roles means that your responsibilities as a vice chair can vary greatly from those of vice chairs in other departments or specialties. For example, while you might focus on advancing research initiatives, a vice chair in another department might be more involved in managing clinical operations or

“The vice chair role is fundamentally about supporting the chair and the department in achieving their goals.”
developing educational programs. Understanding these differences is crucial for effective collaboration across the institution and achieving departmental goals.
Vice chairs hold various specific titles, each focusing on different domains within an academic department. The SAEM Vice Chair Interest Group recently cataloged these roles, finding the most common titles to include:
1. Education: Oversees educational programs, including undergraduate, graduate, and continuing education. Responsibilities include curriculum development, ensuring teaching quality, and meeting accreditation standards.
2. Faculty Development/Academic Affairs: Focuses on faculty professional growth, including mentoring, organizing professional development workshops, and creating career advancement pathways. This role sometimes overlaps with education.
3. Clinical Operations/Clinical Affairs: Manages day-to-day clinical activities, including staff management, practice policies, and patient care quality and safety.
4. Diversity and Inclusion: Promotes a diverse and inclusive environment by developing strategies and programs to enhance diversity among students, faculty, and staff. This role may also include ensuring that care provided to various patient groups meets the
highest quality standards, measuring health outcomes for these populations, and offering education to faculty on caring for diverse patients. Additionally, this role might involve collaborating with recruitment committees to ensure that diversity is a key factor in hiring decisions.
5. Patient Safety and Quality: Dedicated to improving patient safety and care quality. Responsibilities include developing quality improvement initiatives, monitoring patient outcomes, and ensuring compliance with safety standards. This role is sometimes linked with the clinical operations role.

continued from Page 19
6. Research and Scholarship: Supports research activities by helping faculty secure funding, overseeing research projects, and ensuring high-quality research output. Unique among the roles, some departments find this role particularly challenging to fill.
While many believe that serving as a vice chair is a direct path to becoming a department chair, this isn't always the case. Some vice chairs are content with their current roles, focusing on their specific skill sets and supporting the chair. Additionally, with departments often having 5-10 vice chairs, it's not feasible for all to eventually become chairs. In some instances, a department may appoint an executive vice chair, who advocates for the chair, mentors other vice chairs or division heads, and occasionally acts as an intermediary when the chair is unavailable. The career progression from a vice chair role might lead to other domain-specific positions within the medical school or health system, rather than to a chair position.
The duties of a vice chair vary based on their area of expertise, but generally include supporting the chair in managing specific functions within the department. This can involve administrative tasks, vision setting, strategic planning, and representing the department in various capacities.
For example, a vice chair for education might be responsible for developing new training programs, overseeing the accreditation process, liaising between residency programs and midlevel residency or fellowship programs, distributing educational resources, and ensuring that that the educational needs of students and residents are met. They may also take part in faculty evaluations, curriculum reviews, and fostering partnerships with other educational institutions.
Conversely, a vice chair for clinical operations would focus on the logistics of running the department’s clinical services. This could include scheduling staff, managing budgets, ensuring compliance with health care regulations, and enhancing patient care processes.
A vice chair for diversity and inclusion might focus on recruiting a diverse faculty, creating mentorship programs for underrepresented groups, and leading workshops on cultural competency. They would also monitor the department’s progress on diversity goals and report on these to the chair and stakeholders.
While each domain is distinct and “triple threats” are uncommon, it is essential for each domain-specific vice chair to have a basic understanding of the roles and responsibilities of the other vice chairs within the department. Communication is key, especially where domains overlap, such as in clinical operations and quality. Clearly defining roles is important, but it cannot fully substitute for effective communication.
Most vice chair positions are found in academic departments with residencies and fellowships, though this is not always the case. The path to becoming a vice chair typically involves demonstrating excellence in your area of expertise, whether in education, research, clinical practice, or another
domain. Candidates are typically senior faculty members who have demonstrated leadership skills and a strong commitment to the department's goals. They often have a proven track record of achievements, such as published research, successful teaching programs, or enhancements in clinical practices.
Medical directors and other leaders aspiring to vice chair roles can benefit from mentorship, both from their chair and other vice chairs. Transitioning from a director to a vice chair presents unique challenges and opportunities, making understanding these differences crucial for success and for feeling valued in the role.
The role of vice chair is demanding and time-consuming, requiring a careful balance between administrative duties and clinical, educational, or research responsibilities. It also involves collaborating with a wide range of stakeholders, including faculty, students, staff, and external partners.
A major challenge is effective time management. vice chairs often juggle multiple projects and responsibilities, which demands strong organizational skills and the ability to delegate tasks when necessary. Balancing daily role-specific tasks with pursuing growth opportunities can be particularly challenging, especially for those aspiring to future chair positions. In this context, mentorship from the chair and other senior members of the institution is crucial.
Another challenge is navigating departmental politics. As a vice chair, you may need to mediate conflicts, build consensus, and advocate for resources. This requires strong interpersonal skills, along with the ability to negotiate and compromise. You might oversee multiple director-level reports with overlapping responsibilities, and it's essential to help them understand their roles and expectations in relation to both the vice chair and, more importantly, the chair and the department. Despite the challenges, these mentorship and coaching opportunities can be among the most rewarding aspects of the position.
The role of vice chair is distinct in both culture and responsibility compared to that of directors in similar domains. While a director may enjoy greater autonomy in their day-to-day tasks, the vice chair often explicitly represents the chair. Therefore, alignment and constant communication with the chair are critical.
Despite the challenges, the role of vice chair is highly rewarding. It offers the opportunity to shape the future of your department, influence policy, and drive improvements. It also provides a platform for professional growth and the chance to work closely with other leaders in your field. As a vice chair, you have the unique opportunity to develop and implement strategies that can significantly impact patient outcomes, faculty development, and departmental efficiency. On a personal level, you can enhance your leadership skills, expand your professional network, and gain deeper insights into the administrative and strategic aspects of running a department. Collaborating with other leaders, both within your institution and in the broader field, allows you to work on innovative projects, share best practices, and contribute to the advancement of the specialty.
Before pursuing a vice chair position, it's important to evaluate whether the role aligns with your career goals and personal strengths. Reflect on what you currently enjoy in your role and what you hope to achieve in the future. The position of vice chair is more than just a meritbased promotion; it carries a significant responsibility for the overall success of the department. In many ways, it is a position of service — service to the chair in representing the department, and service to your direct reports through mentorship, coaching, and creating growth opportunities. This means that being "on mission" becomes vital, as your personal growth becomes more closely tied to the success of the department.
Consider whether you are prepared for the increased responsibilities and if you possess the necessary skills to excel in a leadership position. It may be helpful to seek advice from current or former vice chairs and chairs to gain a deeper understanding of the role and its demands. Additionally, consider applying for the SAEM Chair Development Program (CDP), a comprehensive leadership training initiative specifically designed to enhance the capabilities and effectiveness of new and aspiring academic emergency medicine department chairs. Through skill development, advising, and mentorship, the CDP prepares participants for the multifaceted responsibilities of departmental leadership.
Becoming a vice chair is a pivotal step in an academic career, offering a unique opportunity to significantly impact your department and advance your professional goals. However, the role comes with its own set of challenges and demands that require careful consideration
Understanding the specific duties and responsibilities associated with the vice chair role in your area of expertise is essential. Whether your focus is on education, clinical operations, diversity and inclusion, or another domain, being wellprepared and informed about what the position entails will set you up for success.
The vice chair role is fundamentally about supporting the chair and the department in achieving their goals. It involves leadership, collaboration, and building strong relationships — with the chair, partners and stakeholders, and your reports and faculty. Serving as a vice chair can be both fulfilling and enriching, offering personal and professional rewards while allowing you to play a key role in shaping the direction and success of your department.

Dr. Otero is the vice chair for clinical operations at Froedtert & MCW Department of Emergency Medicine, overseeing eight emergency departments throughout the enterprise. He is involved in strategic initiatives related to emergency care and improving the interface of admissions into the health system. He is also the co-director of the Health Executive and Administrative Leadership (HEAL) Fellowship for MCW Emergency Medicine.

Dr. Raukar is a clinician, researcher, and educator, serving as vice chair for academic advancement and faculty development at Mayo Clinic. She leads initiatives to cultivate the leadership skills of the next generation of physicians.

Dr. Rosania is the vice chair for clinical operations, associate professor of emergency medicine, and chief of the Division of Operations, Quality & Informatics in the Department of Emergency Medicine at Rutgers Health – New Jersey Medical School.

By Elizabeth Leenellett, MD, and Caroline Freiermuth, MD, on behalf of the SAEM Academy
for
Women
in Academic
Emergency Medicine, the SAEM Awards committee, and the SAEM Faculty Development Committee
The Emergency Medicine Program of Women in Leadership (EMPOWER) at the University of Cincinnati identified a critical issue among faculty members: Despite their impressive accomplishments and expertise, many women were reluctant to self-promote or advocate for recognition. This collective hesitation highlighted a broader challenge within academic medicine: navigating the complexities of career advancement in a competitive field where service, rather than visibility, is often the primary motivation. To address this, EMPOWER created an awards committee, which was later expanded to
include the entire department, aiming to foster a culture where achievements are celebrated, recognized, and leveraged for professional growth.
The awards committee was created to address three key objectives:
1. Building Internal and External Recognition: Enhance faculty visibility within the institution and in professional circles, thereby boosting their professional reputation and that of the department.
2. Facilitating Promotion and Career Advancement: Acknowledge the critical role of visibility and recognition in career progression, leadership opportunities, and overall professional development. Receiving awards builds credibility as an expert and can lead to invitations for collaborations or speaking engagements.
3. Teaching Self-Promotion Skills: Equip faculty with the skills to confidently articulate their accomplishments. Award nominations serve as an opportunity for faculty to practice. Rather than having the committee

“The establishment of an awards committee has proven instrumental in addressing the challenges associated with self-promotion and recognition among faculty.”
produce nomination letters, having faculty draft their own letters has proven more effective for self-advocacy.
Founded in 2019
EMPOWER established an awards committee to identify relevant awards and deserving nominees within its membership. A list of awards with nomination deadlines was compiled, including those from SAEM and the Academy for Women in Academic Emergency Medicine (AWAEM), American College of Emergency Physicians’ (ACEP) and the American Association of Women Emergency Physicians, Association of American Medical Colleges and the Group on Women in Medicine and Science (GWIMS), and institutional awards. Group discussions proactively identify women faculty and residents who meet the award criteria, selecting one candidate per award cycle. A champion is also
identified to contact the nominee, obtain their CV, and write a draft nomination letter based on the award criteria. The letter is then shared with the group, including the nominee, for edits. Success of this approach led to the committee’s expansion into an EM Departmental Awards Committee later that year.
An email is sent to the entire department to solicit interested members for the awards committee, aiming for broad representation. The committee currently has approximately 12 active members, including assistant, associate, and full professors, with an equal gender distribution. They meet for an hour each quarter to review upcoming awards and suggest nominees.
The committee is deliberate in evaluating all upcoming awards for potential candidates and ensures diversity
and inclusivity in nominations, fostering a supportive environment for all faculty members. When multiple candidates meet the award criteria, special consideration is given to those who identify as women or are underrepresented in medicine, prioritizing them for nomination. Those not chosen are prioritized for future cycles.
The committee also considers how many awards each person has been nominated for and works to ensure that new names are proposed. Experience has shown that awards often lead to more awards, as it is easier to adjust a winning nomination letter to meet an award criteria than to create a new one. Nearly half of our award winners have received multiple awards. Award nominations are tracked and have grown to include many subspecialty societies, incorporating the vast interests of the faculty group.

“By creating a supportive environment and providing structured guidance, the committee has significantly improved the visibility, recognition, and career advancement opportunities for the entire department.”
CASE IN POINT
continued from Page 23
One lesson learned was that the champions often wrote multiple letters for candidates they did not know well, resulting in considerable time and effort. Understanding the importance of creating compelling letters, combined with the short turnaround times needed to meet deadlines, led to some burnout. After consideration, it was recognized that no one knew their accomplishments better than the nominees. Additionally, reflecting on their journey and recognizing their achievements is an important process. Now, nominees are encouraged to draft initial letters highlighting their achievements and qualifications, tailored to the award criteria. To aid this process, a drive with prior submissions was created to serve as templates. Drafts are then refined collaboratively within the committee to ensure comprehensive and compelling submissions that align with award criteria and resonate with selection committees.
The committee has facilitated nominations for more than 200 awards at local, regional, and national levels across various categories. These efforts have resulted in faculty, residents, and advanced practice providers receiving over 100 prestigious awards, underscoring the effectiveness of the committee's success in highlighting talent, recognizing achievements, and enhancing professional visibility.
Public announcements of awards have increased both internal and external recognition of achievements. The nomination itself, regardless of the outcome, has often improved the individual’s sense of value and departmental recognition, which is key for job satisfaction and reducing burnout. Furthermore, adding awards and nominations to resumes has strengthened dossiers when being considered for
promotion, leadership positions, and job searches.
The culmination of these efforts aids in retention and recruitment, as a satisfied faculty speak volumes. Additionally, the nominations increase departmental academic stature. As other colleagues become more aware of expertise and prior accomplishments, they are more likely to serve as sponsors and promote other faculty members for opportunities such as invited speaking engagements and committees. Notably, the department’s commitment for promoting diversity, equity, and wellness within emergency medicine was recognized with the 2023 AWAEM Outstanding Department Award and the 2023 ACEP Wellness Center of Excellence Award, both of which were identified, and letters drafted, by the awards committee.
Through its journey, the awards committee has gleaned valuable insights:
While being nominated by the committee is affirming, he passive process did not significantly develop self-promotion skills. Encouraging faculty members to take ownership of their achievements and effectively communicate their qualifications has been pivotal. It is an opportunity to reflect on their career, recognize their achievements and boost confidence. Reviewing award criteria also helps them understand what success in that category looks like, which may help guide future career decisions. Self-nomination is more effective for developing self-promotion skills.
The committee refines the draft nomination letter from the candidate, changing language to active voice, adding superlatives, and highlighting the impact of the nominee’s achievements to maximize their chance of success. The result is an authentic, more targeted nomination, ultimately increasing the likelihood of a winning letter.
Nominees gain recognition from the award nomination, while committee members experience enhanced job satisfaction by contributing to their colleagues’ and the department’s success. This mutual benefit fosters a sense of community and well-being among both nominees and committee members.
The establishment of an awards committee has proven instrumental in addressing the challenges associated with self-promotion and recognition among faculty. By creating a supportive environment and providing structured guidance, the committee has significantly improved the visibility, recognition, and career advancement opportunities for the entire department. Moving forward, the committee remains dedicated to continuing its impactful work, empowering faculty members to confidently celebrate and share their achievements, thereby reinforcing a culture where excellence is celebrated, diversity is embraced, and professional growth is nurtured.

Dr. Leenellett serves as professor and vice chair of faculty affairs and inclusive excellence at the University of Cincinnati Department of Emergency Medicine, the W. Brian Gibler, MD, Endowed Chair for Education in Emergency Medicine, and chief of staff for UC Health-West Chester Hospital.

Dr. Freiermuth is an associate professor of emergency medicine at the University of Cincinnati, where she holds the Shawn Ryan Endowed Chair to Benefit the Acute Treatment of Mental Health and Substance Use Disorders.

By Spencer Lord, MD, and Gregory P. Wu, MD, on behalf of the SAEM Critical Care Interest Group
Refractory shock includes both refractory cardiogenic shock and refractory distributive shock, often in the form of refractory septic shock. Refractory cardiogenic shock involves ongoing systemic hypoperfusion and end-organ dysfunction despite the use of two vasopressor/inotrope therapies and addressing the underlying cause. Refractory septic shock is characterized by persistently low mean arterial pressure despite adequate fluid resuscitation and high doses of vasopressors, typically norepinephrine ≥1 μg/kg/min. This condition may also involve septic cardiomyopathy with or without vasoplegia. This discussion will review the mechanisms, patient identification, risk stratification,
contributing factors, treatment monitoring, and briefly, patient selection for mechanical support devices.
Refractory septic shock occurs through multiple pathways. First sepsis-induced myocardial dysfunction is driven by depressed TNF-α and IL-1β, leading to impaired cardiac contractility via nitric oxide and cyclic GMP suppression. Second, microcirculatory dysfunction causes dissociative shock due to mitochondrial damage, resulting in persistent vasoplegia. Third, systemic inflammatory shock involves widespread endothelial activation, coagulopathy, and blood flow dysregulation, leading
to further tissue hypoperfusion and persistent vasoplegia with disseminated intravascular coagulation. Finally, neurohormonal dysregulation occurs when there is a deficient response to vasopressin or impaired reninangiotensin-aldosterone system which exacerbates vasoplegia.
Refractory cardiogenic shock can perpetuate due to several causes. First is ischemia and myocardial dysfunction, a vicious cycle where worsening ischemia leads to less efficient myocardial function, increased oxygen demand, and continued worsening myocardial necrosis. This is the most common cause and becomes selfperpetuating. Second is the systemic
“Refractory cardiogenic shock involves ongoing systemic hypoperfusion and end-organ dysfunction despite the use of two vasopressor/inotrope therapies and addressing the underlying cause.”
inflammatory response, analogous to events in septic shock, with systemic proinflammatory response, coagulopathy, combined with microcirculatory dysfunction, and dissociative shock. Lastly is failure of oxygen utilization, where despite increasing oxygen delivery, the myocardium and peripheral tissues are unable to utilize oxygen.
Emergency medicine is focused on risk stratification, early identification of critical illness, and initiating management in this patient population. Therefore, we will discuss easy-to-use risk assessment scores to help tailor medical management or identify those who need mechanical cardiac support or transfer to an ECMO center.
A combination of a bedside severity score (bSS) and computed severity score (cSS) in children (≤18 years old) is predictive of mortality when the bSS is ≥2 and the cSS >20.5. These scores are based on the presence of myocardial dysfunction (US EF <25% or CI <2.2), lactic acid >4 mmol/L, and vasopressorinotrope score (VIS) (mcg/kg/min). Scores were most predictive of mortality after 12 hours of management and were designed to evaluate their association with mortality and the composite endpoint of mortality/ need for extracorporeal life support. Similar results have been demonstrated in adults, where elevated VIS and lactic acid levels, cardiac indices, ejection fraction predict mortality at the time of ICU admission. For patients in cardiogenic shock, the Survival After Veno-Arterial ECMO (SAVE) score predicts survival on ECMO to hospital discharge. The Simplified acute physiology score II (SAPS II) and Sequential Organ Failure Assessment (SOFA) are also able to predict both short- and long-term survival on ECMO.
Use of Rapid Bedside Analyzers or Blood Gas Analysis
Refractory shock is often associated with metabolic derangements. Identification
of reversible causes — think of all your “hypos” (e.g., hypoglycemia, hypocalcemia, hypothermia, hypothyroidism/hyperthyroidism), acidosis, blood loss, adrenal insufficiency, toxicological causes, and secondary shocks — whenever your patient does not respond to initial treatment. Consider dissociative shock in your undifferentiated patient with severe lactic acidosis. Dissociative shock is caused by dysfunction of respiration at the cellular level, leading to cell death. Rapid beside blood analyzer systems and blood gas analysis have been used effectively to measure potassium, sodium, glucose, and hemoglobin.
Resuscitation and Titration of Vasopressors and Inotropes
There is significant variability in fluid resuscitation practices before initiating vasopressors, indicating that clinical exams, vitals, and provider experience alone are insufficient for consistent care. Point-of-care ultrasound significantly improves diagnostic accuracy in undifferentiated shock and should be frequently used in the resuscitation bay. For vasopressor and inotrope support, start every adult with norepinephrine. Then use mean arterial pressure, labs, point-of-care echocardiograms, and, if available, SvO2 from a central line in the SVC to guide the timing of vasopressin and inotropes like epinephrine or dobutamine. Additionally, ΔPCO2 from both central venous and arterial sites, combined with lactic acid, can help guide fluid responsiveness.
Unfortunately, patients with refractory septic shock fare far worse than those with refractory cardiogenic shock when placed on mechanical cardiac support such as veno-arterial ECMO. In a recent retrospective study, refractory septic shock was associated with a lower likelihood of successfully weaning from VA ECMO (15.5% vs. 45.5%) and survival to hospital discharge (7.0% vs. 28.9%).
A systematic review and meta-analysis
of patients with septic shock on VA ECMO showed a pooled survival rate of 36.4% (CI: 23.6%-50.1%). Patients with an EF <20% had a survival rate of 62%, but only 45.5% (CI: 16.7%-75.8%) in North America. Those with septic shock and an EF >35% had a survival rate of only 32.1% (CI: 8.69%-60.7%) (Ling 2021). For refractory shock with persistent vasoplegia, angiotensin II, hydroxocobalamin, and methylene blue can be effective, but timing and patient selection require further research. Thus, routine consideration of mechanical cardiac support should be limited to patients with refractory cardiogenic shock until further research helps guide management in refractory septic shock.
To manage and appropriately discharge patients with suspected refractory shock, use rapid bedside laboratory analysis, point-of-care echocardiogram, and arterial and SvO2 or ScvO2 measurements to guide fluid resuscitation and tailor vasopressor administration. Utilize the SAVE score to identify patients for ECMO center referral and consider dissociative shock in your assessment.


Dr. Lord is an instructor of surgery at Massachusetts General Hospital, NewtonWellesley Hospital, and Wentworth-Douglass Hospital. He is an emergency physician and surgical intensivist.
Dr. Wu is an associate professor of emergency medicine and internal medicine at Albany Medical College. He is an emergency physician and medical intensivist. He also is the clerkship director for critical care and the associate fellowship director for resuscitation and emergency critical care.

By Jacob Landis; Nancy Kwon, MD, MPA; and Annabella Salvador-Kelly, MD, on behalf of
the SAEM Faculty Development Committee and the SAEM Equity and Inclusion Committee.
Dr. Annabella Salvador-Kelly is a distinguished physician leader serving as senior vice president of medical affairs and deputy chief medical officer for Northwell Health, New York’s largest health care provider and system. Her journey began at New York University (NYU) and continued with medical school at SUNY Downstate Health Sciences University. She completed her emergency medicine residency at NYU Medical Center/Bellevue Hospital Center in New York City.
Dr. Salvador-Kelly’s career has been deeply influenced by her parents, who
immigrated to the United States from Portugal seeking a better quality of life, economic opportunities, and access to education for their children. Her parents came from modest backgrounds and, having received only a primary school education in Portugal, entered the workforce during their teenage years. As the first in her family to attend college and medical school, Dr. Salvador-Kelly embodies natural drive, resilience, and optimism. She describes herself as extroverted and hands-on, with a passion for helping others. “I am one of those individuals that never wants to sit still,” she says. “I enjoy being
involved in a wide range of activities and was drawn to a fast-paced career with variety and the opportunity to make a real difference in the lives of others, especially in times of acute need.”
The loss of her grandfather to an acute myocardial infarction on a farm in Portugal, due to a lack of available medical care, solidified her desire to pursue medicine. Emergency medicine, with its fast-paced environment and diverse medical cases, offered the perfect opportunity for her to make a significant impact on patient care and health care delivery.

“I enjoy being involved in a wide range of activities and was drawn to a fast-paced career with variety and the opportunity to make a real difference in the lives of others, especially in times of acute need.”
After completing her residency in 1999, Dr. Salvador-Kelly joined North Shore University Hospital’s Emergency Department, part of what is now known as Northwell Health. Starting as a frontline physician in the emergency department (ED), she quickly gravitated toward performance improvement initiatives. “I really enjoyed this type of work, which involved identifying challenges that hindered our ability to deliver exceptional patient care and making improvements that positively impacted patient outcomes and satisfaction.”
Her dedication led her to become the director of performance improvement for the ED at North Shore University Hospital, a role she held for 12 years. In 2013, she transitioned to Long Island
Jewish Medical Center (LIJMC), another Northwell Health facility, as associate chair, spearheading performance improvement efforts. Her success in this role led to her appointment as associate medical director, overseeing performance improvement for the entire hospital. Two years later, she was promoted to associate chief medical officer for Northwell Health, a testament to her performance improvement, leadership, and team-building skills.
Dr. Salvador-Kelly’s career trajectory was not without challenges but was shaped by her experiences, choices, and opportunities. As a woman in medicine, she encountered unconscious biases and a lack of female mentors and role models. She often found herself addressed by
her first name while male colleagues were referred to as “doctor.” Early in her leadership journey, female physicians were underrepresented in leadership roles and key committees.
A staunch advocate for diversity in medicine, Dr. Salvador-Kelly took it upon herself to enact change. She actively invited female physicians to participate in committees, ensuring diverse representation in key roles. As chair of Northwell’s Diversity and Health Equity Physician Council, she championed culturally appropriate health care delivery to eliminate health care disparities. As a member of the Chairs Search

“It is important to be intentional about empowering women and providing access to leadership development opportunities.”
DEI FACULTY PROFILE
continued from Page 29
Committee, she ensures a diverse group of applicants are interviewed. She has witnessed positive changes over the years, attributing the increase in female physician leadership at Northwell Health to mentorship programs, allyship, and faculty development programs like the CALLS (Career Advancement, Learning, Leadership, and Strategy) program. CALLS is a leadership program dedicated to early-career female physicians. Northwell Health also offers several other leadership programs dedicated to team members at different career stages, including the Physician Executive Leadership Development Program (PELDP) and the Executive Leadership Development Program (ELDP). Dr. Salvador-Kelly serves as a faculty member for both programs. “It is important to be intentional about empowering women and providing access to leadership development opportunities,” she says. Her

commitment extends beyond Northwell Health, as she actively participates in SAEM’s Equity and Inclusion Committee.
The COVID-19 pandemic brought unprecedented challenges. In addition to her existing responsibilities, Dr. Salvador-Kelly co-chaired Northwell
Health’s Clinical Advisory Group, playing a crucial role in implementing clinical workflows, creating clinical policies and guidelines, operationalizing loadbalancing solutions, and facilitating disaster privileges to onboard new physicians and providers. “I think the biggest setback was dealing with an
“If it’s something you really want to do, keep pushing forward and don’t give up. Don’t let anybody tell you it can’t be done.”

unknown illness,” she reflects. “We were making daily changes, attempting to keep up with the evolving changes at the federal and state levels. It was important to ensure that our team members felt safe and we had enough resources available.” During this time, she collaborated with the New York State Department of Health on vaccine prioritization and dissemination plans.
Following the pandemic, Dr. SalvadorKelly was promoted to deputy chief medical officer for Northwell Health. “With every role, I enjoyed the experience and learned a great deal. Continuous learning is critical in leadership,” she commented. Her current role encompasses a wide range of responsibilities, including leading medical affairs, credentialing, developing system policies, standardizing hospital bylaws, and collaborating with various departments on medication selection, procedural products, and sustainability initiatives. She attributes part of her success to her involvement in national
committees, including the previously mentioned SAEM Equity and Inclusion Committee, as well as the SAEM Faculty Development Committee, the American College of Emergency Physicians’ (ACEP) Bylaws Committee, ACEP’s Quality and Patient Safety Committee, and NYACEP’s Practice Management Committee.
Dr. Salvador-Kelly finds immense fulfillment in faculty development, educational endeavors, and wellness initiatives. As a faculty member at the Zucker School of Medicine at Hofstra/ Northwell and Northwell Health’s Center for Learning and Innovation, she has the opportunity to inspire and educate future health care leaders. She believes her background in emergency medicine has been instrumental in her administrative success. “As emergency medicine physicians,” she explains, “we gain experience across various specialties, learn to work effectively in teams, make difficult decisions under pressure, utilize limited resources efficiently,
and navigate conflict within a highly stressful environment.” She believes this experience is why emergency medicine physicians are exceptionally well-suited for administrative roles.
Dr. Salvador-Kelly’s advice to aspiring professionals pursuing a career in medicine is simple yet powerful: “If it’s something you really want to do, keep pushing forward and don’t give up. Don’t let anybody tell you it can’t be done. You have to be passionate, and you have to want it.”
To women pursuing leadership roles, she emphasizes the importance of perseverance and passion, despite the inevitable “bumps in the road.” Dr. Salvador-Kelly’s journey is an inspiring testament to her unwavering commitment to medicine, education, leadership, and championing diversity in health care.



Jacob Landis is a high school senior interning in the emergency department at Long Island Jewish Medical Center. He plans to pursue a career in medicine.
Dr. Kwon is a professor and vice chair of emergency medicine at Long Island Jewish Medical Center. She is also the Central Region medical director of diversity and health equity for Northwell Health.
Dr. Salvador-Kelly is Northwell Health’s senior vice president of medical affairs, deputy chief medical officer, and associate professor of emergency medicine at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell. She leads medical affairs throughout Northwell Health, including credentialing, policies and procedures, and curating talented physicians and team members. She is also responsible for standardizing pharmacologic and therapeutic interventions and procedural products across the entire clinical enterprise.

By Alaa Aldalati, MBBS and Suzanne Bentley, MD on behalf of the SAEM Simulation Academy
In an era where diversity, equity, and inclusion (DEI) are at the forefront of educational reform, a new national initiative aims to revolutionize DEI training for emergency medicine residents. Spearheaded by a group of 26 dedicated educators and simulation experts from the SAEM Simulation Academy, in collaboration with the SAEM AIDEM, this initiative draws inspiration from a groundbreaking study that identifies 14 critical areas of need for DEI teaching, best delivered through simulation. This initiative will be presented at the CORD Virtual DEI Conference in September 2024.
Simulation-based education has long been recognized as a powerful tool in medical training, offering a safe and controlled environment where residents, attendings, and health care teams can hone their skills. For DEI training, its importance is even more pronounced. Simulation allows residents to practice and improve their communication skills, particularly when interacting with patients from underrepresented minorities. Through carefully crafted scenarios, participants can engage in
experiential learning experiences with feedback across a wide range of patient interactions, helping them to develop empathy, cultural competence, and the ability to navigate complex social dynamics.
The study underscores the need for comprehensive DEI training in emergency medicine, highlighting 14 areas of focus. These include:
• Recognizing and addressing implicit bias
• Effective communication with patients from diverse backgrounds

“Simulation allows residents to practice and improve their communication skills, particularly when interacting with patients from underrepresented minorities.”
• Understanding social determinants of health
• Providing culturally competent care
• Managing language barriers
• Building trust with underrepresented communities
• Identifying and addressing health disparities
• Enhancing teamwork and collaboration in diverse groups
• Developing advocacy skills for DEI issues
• Implementing inclusive policies and practices
• Addressing microaggressions in the clinical setting
• Understanding the impact of systemic racism on health
• Fostering an inclusive learning environment
• Continuously evaluating and improving DEI initiatives
One of the remarkable aspects of this DEI curriculum is its adaptability. While simulation centers and standardized patients offer an ideal setting for this
training, the curriculum is designed to be flexible enough to be implemented in any residency program, regardless of available resources. Virtual simulations, role-playing exercises, and peer-to-peer interactions can effectively supplement traditional simulation techniques, ensuring that all residents receive comprehensive DEI training. Simulation allows residents to practice and receive feedback on both common and rare cases they may not frequently encounter.
The national initiative to promote DEI teaching in emergency medicine residencies, supported by the SAEM Simulation Academy, marks a significant step forward in medical education. By leveraging the power of simulation, this curriculum not only equips residents and staff with essential communication skills but also fosters a deeper understanding of the unique challenges faced by underrepresented minorities. This initiative embodies a commitment to creating a more inclusive and equitable health care system, where every patient receives the highest standard of care.

Dr. Aldalati earned her MBBS from Alfaisal University in Saudi Arabia. She completed an emergency medicine residency at the Mayo Clinic, where she served as chief resident, and a simulation fellowship at Brown University. She is currently pursuing a master’s degree in health professions education at Johns Hopkins University. Her interests include telesimulation and diversity, equity, and inclusion.

Dr. Bentley is an emergency medicine physician, director of simulation innovation and research, and chief wellness officer at NYC Health + Hospitals/Elmhurst. She is also a professor of emergency medicine and medical education at the Icahn School of Medicine at Mount Sinai and the current president of the SAEM Simulation Academy. Dr. Bentley has a broad background in medical education, simulation, wellness, safety science, and research, with specific training and expertise in debriefing, teamwork and communication training, and in-situ simulation.

By Cindy Bitter, MD, MA, MPH; Andrew Wong, MD; and P. Logan Weygandt on behalf of the SAEM Wellness Committee
In May 2024, Iowa joined a growing list of states enacting anti-DEI laws, including Alabama, Florida, Idaho, Kansas, North Dakota, South Dakota, Tennessee, and Utah. Although bills are proposed in additional states, they have yet to pass, and state universities in Arizona, Georgia, and Texas have reduced DEI efforts in response to proposed legislation. A national bill that would prohibit federal funding for medical schools implementing DEI policies has also been proposed.
While the specifics and prohibited activities vary by bill, the implications for academic medicine are significant.
Despite mixed evidence, there are indications that diversity within health care teams enhances patient-centered outcomes. Consider this:
• Patients with code teams led by female physicians experience higher rates of return of spontaneous circulation and survival to hospital discharge.
• Female patients have lower mortality rates when surgeries are performed by female surgeons.
• Outcomes for all surgical patients improve with a higher number of female surgeons and anesthesiologists on staff
• Hospitalized Medicare patients, hospitalized under female physicians have lower mortality rates
• Female patients with congestive heart failure receive more guideline-

“Patients with code teams led by female physicians experience higher rates of return of spontaneous circulation and survival to hospital discharge.”
concordant care when treated by female physicians
• Race concordance between patients and physicians can reduce infant mortality rates among black infants
• In a video simulations, Black patients were more likely to consent to cardiac surgery if recommended by a Black physician rather than a white one.
• Language concordance is linked to better control of hypertension and diabetes
• At a population level, counties with more Black primary care physicians have lower all-cause mortality rates and reduced health disparities among Black patients.
These trends mirror evidence that companies with greater board diversity tend to perform better.
Anti-DEI initiatives are impacting the health care workforce. Beyond patient
care, students, residents, attending physicians, and other health care staff may experience moral injury from witnessing persistent health disparities, a situation likely worsened by the COVID-19 pandemic. Some physicians have relocated from states where they feel targeted due to their identity, and U.S. medical students are avoiding residencies in states with reproductive health care restrictions. This trend may result in future physician shortages, as many residents tend to remain in the regions where they trained after graduation
Promoting diversity in medicine is crucial because patients achieve better health outcomes when the health care team reflects their own backgrounds. This fundamental truth should motivate all providers to support DEI efforts to ensure the health and well-being of ourselves, our trainees, and the diverse patients we serve.



Dr. Wong is a professor in the department of emergency medicine at the University of California, Davis. He is a member of the health system’s Department Wellness Champion Committee.
Dr. Weygandt is an assistant professor at Johns Hopkins Emergency Medicine.
Dr. Bitter is an associate professor in the division of emergency medicine at Saint Louis University. She is co-champion of wellness initiatives for her residents and serves on the Wellness Task Force for SSMSaint Louis University Hospital.

By Yanina Purim-Shem-Tov, MD, MS
Resident education is a cornerstone of academic emergency medicine, shaping the future of our field. Ensuring high-quality training requires substantial time and effort from faculty, whose expertise and mentorship are crucial. However, motivating faculty to invest their time can be challenging. Drawing from the latest literature, we explore effective strategies to incentivize faculty involvement in resident education.
Formal recognition and rewards are among the most effective strategies. According to a study in The American Journal of Medicine, faculty members highly value public acknowledgment of their teaching efforts. Awards such as
"Educator of the Year" and certificates of excellence can significantly boost morale and incentivize participation. Including educational contributions in annual performance reviews and promotion criteria further emphasizes their importance.
Providing opportunities for professional growth also serves as a strong incentive. Faculty development programs that focus on teaching skills, curriculum design, and educational research not only enhance the quality of resident education but also help faculty members advance their own careers. Workshops, seminars, and courses that offer Continuing Medical Education
(CME) credits can be particularly appealing. As highlighted in Academic Medicine, CME credits are a tangible benefit that faculty members appreciate and actively seek.
Allocating protected time for educational activities is crucial. The literature consistently shows that lack of time is a major barrier to faculty involvement in teaching. Institutions can address this by adjusting workloads to include dedicated time for educational responsibilities. Financial compensation, whether through direct stipends or salary adjustments, is another powerful motivator. The International Journal of Emergency Medicine suggests that

“Incentivizing faculty to contribute their time to resident education requires a multifaceted approach.”
financial incentives can significantly increase faculty engagement in educational activities.
Fostering a culture that values education is fundamental. Leadership must actively promote and support educational initiatives, creating an environment where teaching is seen as a core mission. Peer recognition programs and regular faculty meetings focused on educational achievements can help build this culture. Encouraging collaboration and mentorship among faculty members can also enhance the overall educational experience for residents.
Utilizing technology can streamline the teaching process and reduce the burden on faculty. Online platforms for curriculum delivery, virtual simulations, and digital assessment tools can make education more efficient and accessible. The American Journal of Medicine highlights that technology not only enhances learning but also provides
flexibility for faculty to contribute without the constraints of traditional classroom settings.
Aligning the goals of resident education with the broader priorities of the institution can also drive faculty engagement. When educational initiatives are linked to institutional missions, such as improving patient care or advancing research, they gain more support and visibility. Faculty members are more likely to invest their time if they see their efforts contributing to the institution's overall success.
Incentivizing faculty to contribute their time to resident education requires a multifaceted approach. Recognition and rewards, professional development opportunities, protected time, financial compensation, a collaborative culture, technological support, and alignment with institutional priorities are all key strategies supported by current literature. By implementing these best practices,
academic emergency medicine programs can ensure that resident education remains a priority, ultimately leading to better-prepared and more competent emergency physicians.
The commitment to fostering an enriching educational environment will not only benefit residents but also contribute to the professional satisfaction and development of faculty members, ensuring a robust future for academic emergency medicine.

Dr. Purim-Shem-Tovis the executive vice chair of faculty affairs at Rush University Medical Center and a professor of emergency medicine at Rush Medical College. She is a graduate of the Executive Leadership in Academic Medicine (ELAM) program at Drexel University and has received numerous awards for her contributions to medicine and leadership.

By Anita G. Subbarao, MD; Brandon Allen, MD; and Joe Gannett, MD, on behalf of the SAEM Operations Interest Group
Artificial Intelligence (AI) is set to revolutionize many aspects of health care, including emergency medicine. For emergency physicians, understanding AI’s foundational concepts and its applications in operations is crucial. This article series aims to provide a comprehensive introduction to AI, highlighting its transformative potential in the context of emergency department operations.
AI refers to the simulation of human intelligence in machines that are
programmed to think and learn. This includes data analysis, decisionmaking, and process optimization. AI technologies have the potential to integrate smoothly into each stage of a patient’s journey through the emergency department. By streamlining operations from initial triage to discharge or admission, AI can significantly enhance the efficiency and effectiveness of healthcare delivery. These technologies encompass machine learning (ML), large language models (LLMs), and natural
language processing (NLP).
One primary benefit of AI is its potential to process and analyze vast amounts of data quickly and accurately. This capability enables predictive modeling, which could forecast patient influxes and optimize staffing levels to efficiently meet demand. AI-powered triage systems could also rapidly assess patient symptoms, analyze medical images with high accuracy, and prioritize cases based on severity, allowing physicians to make more timely

“AI technologies have the potential to integrate smoothly into each stage of a patient’s journey through the emergency department, significantly enhancing the efficiency and effectiveness of healthcare delivery.”
and informed decisions. If successfully implemented, such advancements could improve patient outcomes, reduce overcrowding, and enhance workflow efficiency within the emergency department.
However, the implementation of AI tools in emergency medicine also presents several challenges and potential drawbacks. AI algorithms must be based on reliable data. Incomplete data or biases in training data could result in disparities in care that might disadvantage certain patient groups. Additionally, there is a risk of over-reliance on AI systems, which could undermine the clinical judgment of health care professionals. The integration of AI also raises ethical and legal questions regarding patient privacy and data security, as well as accountability in the case of diagnostic errors. Moreover, the initial cost of implementing AI technologies and the need for ongoing
maintenance and training pose a substantial financial burden on health care institutions. These challenges underscore the importance of careful consideration, robust governance, and continuous evaluation to ensure that AI tools are effectively and ethically integrated into emergency medicine operations.
Consider whether integrating AI is a step your department should take. With promising results from recent studies and significant potential for enhancing patient flow and triage accuracy, the decision to adopt AI could be transformative for your emergency department. Implementing AI technologies could streamline operations, optimize resource allocation, and improve decision-making processes. Therefore, evaluating the potential benefits and aligning them with your department’s needs and goals is crucial to making an informed and strategic decision

Dr. Subbarao is a second-year emergency medicine resident at the University of Washington. She earned her MD at the UC Davis School of Medicine. Her academic interests include clinical informatics, operations, and healthcare administration, with a focus on improving patient care and operational efficiency.

Dr. Allen is an associate professor in the department of emergency medicine at the University of Florida College of Medicine UF Health. He serves as the administrative fellowship director, medical director of the clinical decision unit (CDU), and UF Health chest pain center medical director. Dr. Allen also holds the position of affiliate associate professor in the department of psychiatry and is the UF Health rehab quality medical director. His academic and clinical interests focus on emergency medicine, clinical decision-making, and quality improvement in patient care.

Dr. Gannett is an assistant professor in the department of emergency medicine at UT Southwestern. He earned his MD at Cooper Medical School and completed his residency at LSU-NOLA. His health systems leadership fellowship at Los Angeles General Medical Center emphasized patient flow and quality improvement. He is dedicated to improving care for underserved communities.

By Allison Spice and Michael Zdradzinski, MD on behalf of the SAEM Education Committee and SAEM RAMS
Starting my four-week emergency medicine rotation was an exhilarating experience, filled with learning opportunities and inspirational moments. I was eager and excited to soak up as much knowledge and experience as possible. However, when I arrived for my eighth shift, I encountered a challenge that would test my adaptability: most of the patients were "boarding," a term that refers to patients who are admitted but still waiting for an inpatient bed. With nine out of twelve patients in the pod in this situation, my opportunities to engage with and learn from new, active patients were significantly limited.
My brief experience with boarding was just a glimpse of a complex problem plaguing emergency departments (EDs) nationwide. The issue, which worsened during the COVID-19 pandemic, continues to affect both patient care and medical education. As students, we enter emergency medicine rotations with specific goals: learning about the specialty and its fit with our career aspirations, gaining valuable clinical experience, and securing positive standardized letters of evaluation (SLOEs). So how can a medical student stand out and make the most of the limited patient interactions during a rotation in an era of frequent boarding?
Fortunately students can follow the guidance provided in SAEM's M3 curriculum chapter, "How to Get the Most Out of Your Emergency Medicine Clerkship." This chapter offers valuable strategies for ensuring a positive and enriching learning experience despite the challenges posed by boarding. Below are a few suggestions to consider.
1. Utilize Downtime: Take advantage of quieter moments to dive into clinical resources and deepen your medical knowledge. This time is invaluable for self-study and preparation

“Most of the patients were 'boarding,' a term that refers to patients who are admitted but still waiting for an inpatient bed.”
2. Seek Feedback: Ask for input from attendings, residents, and nurses during your shifts. Receiving input in real-time allows students to make immediate adjustments and apply recommendations to improve their skills.
3. Set Personal Goals: Use downtime establish individual goals for your rotation, such as improving procedural skills, refining examination techniques, documentation, or enhancing your presentation abilities. By identifying specific areas for growth, you can engage in “feed-forward” teaching by asking for advice on achieving these goals and then implementing the feedback with your next patient and then ask for feedback and additional guidance.
4. Practice Patient Presentations: During department “lulls,” practice formulating
and presenting patient assessments and management plans. This skill, essential in the ED, requires consistent practice to master.
5. Maintain a Positive Attitude: Despite the frustration of limited patient care opportunities, remain proactive and willing to help. Check on patients, distribute blankets, or assist with procedures like IV urinary catheter insertions. Not only does this support patient comfort, it moves patient care forward and allows you to and contribute to the team.
Many students are drawn to the fastpaced nature of emergency medicine, so it can be frustrating when boarding slows down the department’s flow. However, even during these slower periods, there are always opportunities to maximize learning and make a meaningful impact. When faced with such challenges,
consider implementing these strategies to navigate your rotation effectively and make the most of every opportunity.

Alison Spice is a recent graduate of Saint James School of Medicine. She has been involved with the SAEM education committee since 2022 and will be applying for residency in emergency medicine during the upcoming 2025 Match cycle. Dr. Zdradzinski is an assistant professor at Emory University School of Medicine. His primary interests include curricular development, and he serves in various educational and physician wellness leadership roles.


By Marissa Millard and Nicklaus P. Ashburn, MD, MS
In the high-stakes environment of prehospital care, where decisions are made in seconds and can mean the difference between life and death, the realities of frontline health care come sharply into focus. For many aspiring physicians, emergency medical services (EMS) experience provides an unparalleled foundation for medical school, offering a unique blend of practical skills, mental resilience, and a deep understanding of patient care. However, this intense environment also presents challenges that can complicate the transition to a more structured, academic setting.
The high-stress, fast-paced nature of EMS work can sometimes
foster a preference for immediate action over thorough deliberation, which may clash with the slower, more methodical pace of medical education. Additionally, the emotional toll of frontline prehospital health care can lead to burnout, potentially affecting academic performance and personal well-being. Thus, while EMS experience certainly enriches the path to becoming a physician, it also introduces complexities that require careful navigation. In this piece, we explore these complexities with medical students who have EMS experience.
The benefits of EMS experience are clear. One student highlighted how it improved their communication skills,
stating, “The number one thing it taught me: how to interact and talk to patients, how to establish rapport in such a short amount of time.” Another student emphasized the clinical advantages, explaining, “When you actually see something, it’s so different than when you read about it… Coming in with that knowledge already was so nice, because it took a big burden off.”
This hands-on experience in emergency care can significantly ease the academic load and enhance practical skills. A third student reflected on the confidence gained through EMS, sharing, “The thing I see the most now… things that would scare or intimidate a lot of people coming into

medical school, you know, high-acuity patients, were not scary to me because the fear of the unknown was taken away and I already have a framework of how I would approach them.” This insight shows how EMS experience reduces the initial fears and uncertainties common among new medical students.
However, the intense nature of EMS work can also have significant downsides. One student confided, “Mental health in EMS is not great; morale in EMS is really poor, and my understanding is that it’s gotten worse since COVID.” This highlights a critical issue: the emotional and psychological toll that can accumulate from working in such high-pressure environments. Another student reinforced this point, sharing their struggle with PTSD: “I’ve
seen young people being shot or having car accidents... It made it hard to transition... cadaver lab was triggering because it reminded me of certain calls where we had to do CPR and run codes.”
A final student shared how in school, “It’s very weird to talk about these chaotic scenes [like traumatic falls or accidents] in a sterile environment,” noting that classroom lectures often bring him back to disturbing patient-specific memories.
In conclusion, EMS experience offers a rich, albeit challenging, preparation for medical school. It equips future physicians with critical practical skills, resilience, and a profound understanding of patient care. However, the psychological toll and emotional challenges cannot be overlooked, requiring support and resources for those
“For many aspiring physicians, emergency medical services experience provides an unparalleled foundation for medical school, offering a unique blend of practical skills, mental resilience, and a deep understanding of patient care.”
making the transition. As these students' experiences show, the impact of EMS on medical education is multifaceted, providing both valuable benefits and significant challenges.

Marissa Millard is a secondyear medical student at Wake Forest University School of Medicine in North Carolina. She is passionate about integrating clinical practice with innovative research and is committed to improving patient care. Her special interests include community health initiatives and preventive medicine, with a focus on making health care accessible to all.

Dr. Ashburn is an NIH-funded investigator and assistant professor of emergency medicine at Wake Forest University School of Medicine. He completed a Master of Science in translational and health system sciences and an NIH T32 mentored training program in cardiovascular disease epidemiology and prevention. He is supported by an NHLBI K23 grant focused on emergency department-initiated preventive care. His research interests include chest pain risk stratification and novel cardiac biomarkers.

By Marta AW Rowh, MD, on behalf of the SAEM Academy of Geriatric Emergency Medicine
If you haven’t yet experienced a medical student referring to a patient younger than yourself as “old,” just wait — it’s coming. This situation raises the question of when a patient should be considered an “older adult” and whether this designation should influence the care they receive. Teaching this nuanced understanding to (usually) young medical students, who are still learning the fundamentals of medicine, presents an additional challenge.
Many medical curricula lack a focus on geriatrics, and while highlighting topics relevant to older populations is important, it can inadvertently
perpetuate counterproductive stereotypes. Before you think you’re immune to ageist bias, know that ageist biases are prevalent across various medical fields, including oncology and cardiology, and are found globally, from the United States to Iran. Pervasive ageist beliefs portray older adults as frail, weak, “cute,” or helpless. Such perceptions lead to assumptions that older adults are incapable of caring for themselves or making informed decisions, which can influence the recommendations we make. Extensive research shows that attitudes toward aging can impact both longevity and overall health. Our own views and biases about aging also significantly affect our patients’ health outcomes.
The first step is to review and update our educational materials to ensure they accurately represent older adults. Next, we need to distinguish between common challenges associated with aging — such as falls, changes in vision or hearing, cognitive decline, and social isolation — and what constitutes normal aging. We should address or refer these common, potentially modifiable conditions, as they significantly impact quality of life. Our clinical examples should model this commitment to accurate representation. However, if our didactic teachings do not align with departmental practices, the socalled “hidden curriculum” will prevail, undermining our educational goals.

“Pervasive ageist beliefs portray older adults as frail, weak, ‘cute,’ or helpless, leading to assumptions that they are incapable of making informed decisions.”
Combating ageism involves more than just using PowerPoint presentations. It starts with having frank discussions about the experience of aging within our specialty. For example, I share personal stories about the effort required to maintain muscle mass as I age, not to have trainees mimic my exercise routines, but to convey my lived experience of growing older. Recovery from night shifts now takes days instead of hours. However, it’s not all bad. I worry less and have gained a contentment that has enriched my life and reduced my patient load per hour. This perspective allows me to better identify what’s important to my patients and to be more flexible in creating care plans
aligned with their goals. Additionally, my experience with end-of-life discussions has improved through supporting several family members through this process.
Research suggests that personal interaction is the most effective way to combat bias. Getting to know individuals who are different from our own social group helps to humanize “the other.” We have a responsibility to represent the “older other” in ourselves. By modeling the questions we want to be asked by our health care providers, we can demonstrate the importance of treating older adult patients with dignity. We should also teach our learners to recognize and respect different stages of life by noting when patients are of similar age to ourselves or our parents. While
I currently feel middle-aged enough to connect my trainees with my geriatric patients, I will soon become part of the older population myself, God willing. As a specialty, we must ensure our learners develop a balanced perspective on health and aging. Otherwise, we will receive the care we have created.

Dr. Rowh is an assistant professor at Emory University, where she studies structural drivers of health for vulnerable populations. Her recent research focuses on sports injuries in older adult populations.

By Chang Woo Park, MD and Shaza Aouthmany, MD
The unearthly mountain peaks of the Himalayas stretch over 1,550 miles, piercing through the white pillow clouds above Nepal. As the descent into the region begins, it is almost unimaginable that such beauty exists.
Our group of three residents was honored to participate in simulation training at Dhulikhel Hospital in Nepal. Located just 1-3 hours outside of the capital city, Kathmandu, the up-andcoming city of Dhulikhel has only one hospital in the entire region. Access to even basic health care services is a luxury for many. Remote villages lack proper medical facilities, forcing patients to travel long distances, sometimes up to 24 hours, to receive health care. Yet, amidst these challenges, the sense of
community and solidarity is palpable. Local healers and community health workers play a vital role in bridging the gap, offering traditional remedies and essential health care services.
Visiting the health care system in Nepal was an eye-opening and humbling experience. From the bustling streets of Kathmandu to the remote villages nestled in the Himalayas, the disparities in access to health care were starkly evident.
The emergency department (ED) at Dhulikhel Hospital is housed in a separate building. The ED system divides patients into different zones based on their triage level: green, yellow, and red. It has a separate procedure room for minor procedures such as
laceration repairs and dislocation reductions. There is one dedicated shock trauma room that serves only one bed. The department itself is very open, with no security checks, allowing anyone to enter and exit as they wish. Despite the lack of advanced technology, they do have portable X-ray and ultrasound machines. However, X-ray images still need to be physically printed and examined with a light to read the image. Unlike Western health care, which emphasizes HIPAA and patient privacy, patient beds in this ED are side by side, making individual privacy virtually impossible.
The main goal of the visit was to teach and evaluate the simulation training at Dhulikhel Hospital. The
“From the bustling streets of Kathmandu to the remote villages nestled in the Himalayas, the disparities in access to health care were starkly evident.”
team was fortunate enough to donate a simulator to the deserving medical staff to further enrich their training and learning. The staff's enthusiasm and interest in simulation were uplifting, with their eyes lighting up with amazement as they physically interacted with the simulator. The philosophy of "see one, do one, teach one" was the main objective, helping the faculty members become effective trainers and facilitators for future learners of medicine. Although there were rough patches in the beginning, as they ran more simulations and even created their own scenarios, they became more proficient, ready to pioneer their own simulation training within their medical education.
The experience in Nepal was profoundly humbling. It is easy to lose sight of the medical privileges enjoyed in other parts of the world. Despite the lack of resources and funds, the dedication of the medical providers in Nepal to their patients is impressive and inspiring. The camaraderie among the medical staff, seen in their shared meals, jokes, dancing in the middle of a restaurant, and singing freestyle karaoke together, was heartwarming. There is hope to return one day to witness the growth of their simulation training and its impact on their medical education.


Dr. Park is a recent graduate of the University of Toledo emergency medicine residency. He will be starting his new career with Vituity in Chicago.
Dr. Aouthmany is associate dean of graduate and continuing medical education, designated institutional official, and associate professor of emergency medicine at the University of Toledo College of Medicine and Life Sciences.




By Susan Owens, MD, MPH; Mallika Manyapu, MD, MPH; Tania Ahluwalia, MD, MPH; Shweta Gidwani, MBBS, MRCEM, FRCEM; and Kate Douglass, MD, MPH, on behalf of the SAEM Global Emergency Medicine Academy
In India, a trauma-related death occurs every 1.9 minutes, and the mortality rate for severe trauma — defined by an Injury Severity Score (ISS) greater than 16 — is six times higher than in high-income countries. Given the multifactorial burden of trauma in India, effective trauma training for emergency medicine (EM) providers is crucial. The Ronald Reagan Institute of International Emergency Medicine (RRIEM) at George Washington University has significantly contributed to the development of EM and system strengthening in India through a structured three-year hybrid modular EM training program. RRIEM
partners with 18 hospitals across India to train EM physicians. To bolster learner engagement, we designed and implemented a month-long virtual training module aligned with trauma education and based on Knowles' principles of andragogy
In the context of regular virtual teaching sessions, we selected important, locally relevant topics and created interactive sessions that built upon existing tools and knowledge. For PGY-1 trainees, we augmented traditional case-based discussions with a site-based trauma procedure
demonstration challenge. Each site was assigned a trauma procedure to demonstrate via live or video submission. Procedure topics included hemorrhage control, cervical spine immobilization, pelvic binders, chest tubes, and venous access. Teams from different sites shared their local protocols and supplies, leading to robust discussions on indications, contraindications, and case-based interactions to reinforce learning. Demonstrations were adjudicated using a rubric (see Figure 1), and certificates were awarded to the winning sites for each challenge.
CRITERIA POINT VALUE
Demonstrates storage location in ED 10
Demonstrates materials needed for procedure 15
Discuss checklist or department protocol 10
State steps of procedure 15
Correctly demonstrate procedure 20
Discuss common complications 10
For PGY-2 and PGY-3 trainees, the virtual sessions included an evidencebased medicine (EBM) presentation challenge framed around various trauma clinical decision rules and local practice patterns, such as the Canadian Head Computed Tomography rule, National Emergency X-Radiography Utilization Study (NEXUS) criteria for cervical spine imaging, and fluid resuscitation strategies
for severe burns. Teams presented evidence in front of their peers, leading to robust discussions on contextually appropriate care representing different sites across various cities in India.
For the entire group of learners, weekly Grand Round sessions were part of the points accumulation. Full group activities included the Trauma Quiz Bowl and a multisite virtual trauma telesimulation competition. More details are shared below, focusing on incorporating games and contests with contextually relevant content to increase engagement and learning for this critical clinical topic. In addition, we hosted special guest lectures given by a pediatric EM specialist and a health policy and systems researcher from an Indian health systems think tank.
Activities Overview
• Bleed Box Challenge. Trainees evaluated available hemorrhage control supplies in their emergency departments (EDs). They could demonstrate their available kit or "bleed box," or, as an opportunity for quality improvement, assemble
a theoretical bleed box, considering where it would be stored, its contents, and indications for use. The winning site was awarded a certificate.

GLOBAL EM
continued from Page 49
• Trauma Quiz Bowl. Trainees competed in a two-hour live, site-specific, team-based multiple-choice question competition on a virtual video conferencing platform regarding trauma management for ED patients. Questions were adapted from the commercial resource Rosh Review, and the challenge was implemented using PollEV.com, which allowed sites to compete easily using a smartphone as an answering device. The three sites with the highest scores were awarded certificates.
• Virtual Trauma Telesimulation Competition. Using our program experience with telesimulation, we organized a multisite trauma simulation broadcast on a virtual platform, allowing for adjudication and debriefing across our entire program. Four teams of five participants were fielded from geographically distinct sites (see Figures 3a and 3b). The first round involved a pediatric head trauma case that decompensated,
“Interactive activities allowed trainees to demonstrate various trauma-related skills and share information about local resources, fostering active, reflective learning and peerto-peer knowledge exchange.”
requiring recognition of Cushing’s triad, placement of an intraosseous line after failed intravenous access, medication management, and emergent intubation. The two winning teams then competed in the championship round, which involved a polytrauma case resulting from a fall from a human pyramid during the Janmashtami festival. This required massive transfusion for hemorrhagic shock, application of a pelvic binder, a positive FAST exam, and emergent placement of an internal chest drain. The two top-scoring teams were awarded certificates.
• Rosh Review Assessment Challenge. Trainees had access to Rosh Review for study purposes and were assigned assessments to complete at the end of each module to reinforce key concepts in EM. For the trauma month, sites were incentivized to complete the module assessment, with certificates awarded to the first site with full trainee completion and the site with the highest average score among trainees.
Planning and orchestrating multiple learning activities with a competitive element over one month required
“Gamification of learning through competitive activities not only added excitement but also provided opportunities for site recognition and praise, further motivating students to actively participate.”
significant organizational effort before implementation. This included planning documents, curated reminder emails, and collaborative efforts to ensure fair challenge adjudication. Both trainees and site directors submitted unsolicited positive feedback throughout the month. The success of this module can be attributed to several key factors: the substantial variety of activities compared to conventional content delivery methods, the relevance of the module content to the daily trauma burden in India, and the knowledge exchange fostered among peers. Gamification of learning through competitive activities not only
added excitement but also provided opportunities for site recognition and praise, further motivating students to actively participate.
The challenges of the COVID-19 pandemic have led to increased use of virtual and hybrid medical education, which has become a cornerstone of medical education. Since the onset of the COVID-19 pandemic in May 2020, the RRIEM partnership program has delivered nearly 1,000 hours of virtual emergency medicine education, including 28 hours specifically during this trauma month. This education has been in addition to bedside learning, practice questions, and reading.

We strive to continually improve content delivery by piloting educational activities that captivate learners and encourage multidirectional exchange of ideas among medical professionals. The format of this trauma module successfully created a dynamic and interactive learning environment for our trainees, which can be extended to other core topics in EM and easily adapted to local resource availability.

Dr. Owens is an assistant professor of emergency medicine at the University of Kentucky and core faculty for the master's in emergency medicine program through the Ronald Reagan Institute of Emergency Medicine at George Washington University.



Dr. Manyapu is a global emergency medicine fellow at George Washington University.
Dr. Ahluwalia is an assistant professor of pediatrics and emergency medicine at George Washington University and the director of global pediatrics at the Ronald Reagan Institute of Emergency Medicine.
Dr. Gidwani is part of the senior leadership at the Ronald Reagan Institute of Emergency Medicine at George Washington University, an adjunct associate professor at George Washington University, and a senior consultant at Chelsea and Westminster NHS Trust in London, United Kingdom.

Dr. Douglass is an associate professor of emergency medicine at George Washington University and the director of the Ronald Reagan Institute of Emergency Medicine at George Washington University.

By David Rudolph, MD, and Bhakti Hansoti, MBCHB, PhD, MPH
Introduction
In 2022, mpox (formerly known as monkeypox) was declared a Public Health Emergency of International Concern. While the majority of the approximately 32,000 U.S. cases peaked in August 2022, a resurgence in early 2024 and the international spread of a more lethal clade of mpox have prompted warnings from the Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) about potential future epidemic surges. Emergency medicine physicians, often the first point of contact for patients during emerging infectious disease outbreaks, must remain informed about the latest developments, tools, and strategies to manage mpox effectively while addressing the associated stigma of the
disease. At Johns Hopkins, over 55% of mpox patients in our health system presented to the emergency department (ED).
This article synthesizes information from two review articles, Huang et al. (2022) and Soheili et al. (2022) and presents considerations from studies conducted at both the Johns Hopkins ED and across eight EDs within the EMTIDE (Emergency Medicine Transmissible Infectious Diseases and Epidemics) network.
Mpox, an orthopoxvirus similar to smallpox, presents with a characteristic rash that evolves from papules to pustules, vesicles, and eventually ulcerating lesions and scabs.
Approximately two-thirds of patients
experience a flu-like prodrome with fever, lymphadenopathy, myalgias, and sore throat. Rectal pain from mpox proctitis can occasionally be the sole symptom — some mpox-positive patients may not have a rash at the time of presentation. Both men and women can contract mpox, and if a patient reports potential exposure and presents with rectal pain, a rectal sample should be collected for testing even in the absence of a rash.
Mpox transmission is primarily associated with close contact, particularly sexual contact, with higher rates observed among men who have sex with men (MSM). A thorough sexual history should be obtained for all patients being evaluated for mpox, along with routine screening for HIV, syphilis, and gonorrhea/chlamydia.
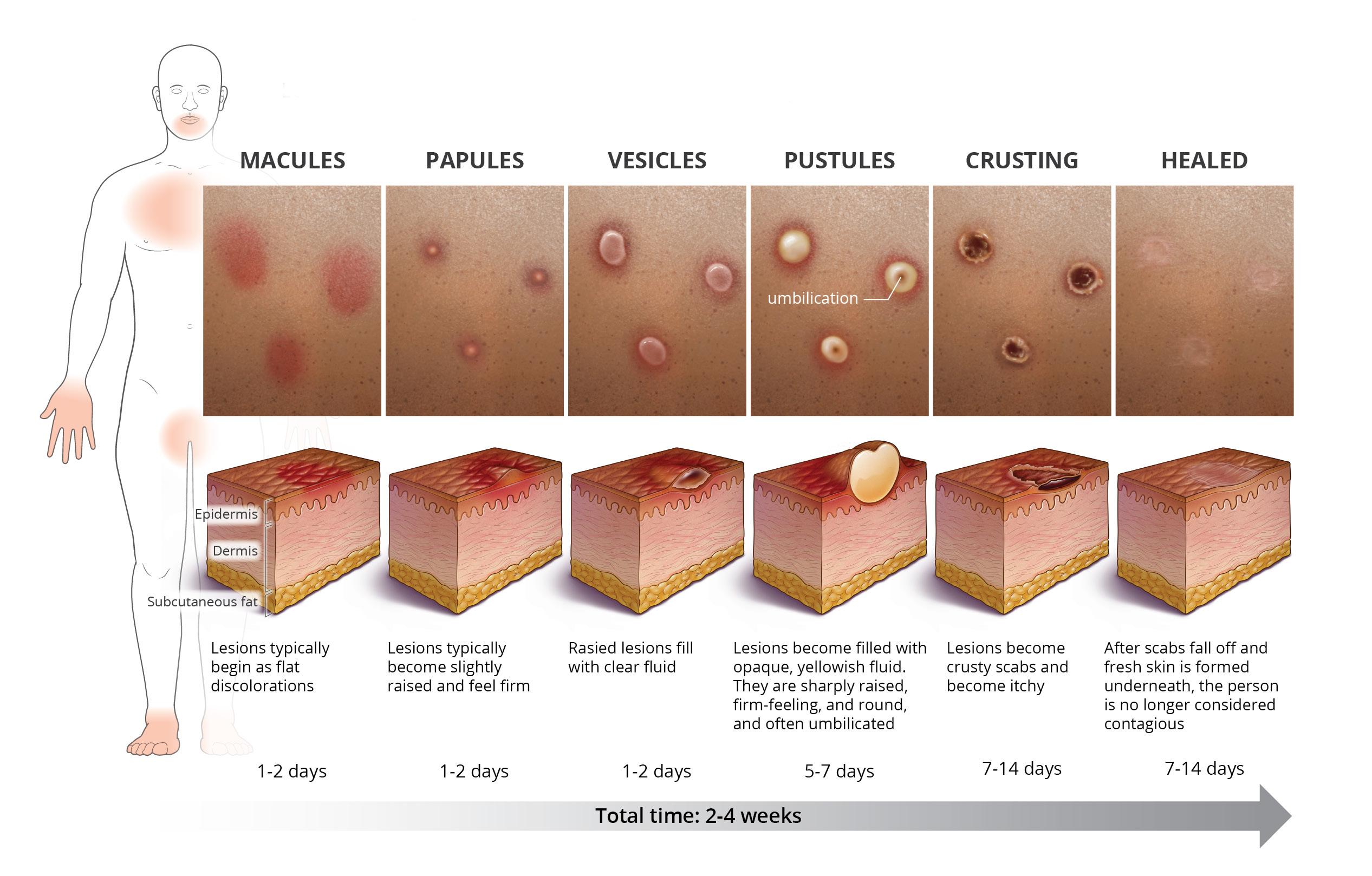
Mpox cutaneous Lesions: Description and Progression. Reprinted with permission from the National STD curriculum. Credit: Cognition Studio, Inc. and David H. Spach, MD.
“Emergency Medicine physicians are often the first point of contact during emerging infectious disease outbreaks, making it crucial to stay current on the latest knowledge to efficiently manage mpox.”
Consider triple-site testing (throat, rectal, and vaginal swabs or urine) based on the sexual history. Since herpes simplex virus (HSV) can mimic mpox, testing for HSV should also be considered.
An unpublished review from eight academic ED sites showed high coinfection rates with other STIs: 36% of mpox patients had syphilis, and 14% had either gonorrhea or chlamydia. Alarmingly, only about 50% of these patients were tested for other sexually transmitted infections (STIs), highlighting the need for more comprehensive STI screening, especially for diseases with high sexual transmission rates and the increased incidence of syphilis in the United States.
We recommend that ED patients with suspected mpox be routinely tested for HIV, chlamydia, gonorrhea, and syphilis co-infection during the ED encounter.
The initial practice of unroofing skin lesions for specimen collection is no longer recommended. The CDC now advises collecting two separate swabs from each suspected lesion, using a sterile, dry, non-cotton swab to vigorously rub the surface. Personal protective equipment, including an N95 mask, gown, gloves, and eye protection, should be used during patient care and specimen collection.
Patients should be counseled on quarantine measures while awaiting mpox
test results. A patient can end quarantine once skin lesions scab over and new skin forms beneath. The average duration of symptoms is 2–4 weeks.
Tecoviromat (TPOXX) is a 14-day oral antiviral initially approved for smallpox but now available as an investigational new drug (IND) for mpox. Eligible patients include those with:
• Severe disease (e.g., multiple organ involvement, hemorrhagic/necrotizing complications, or hospitalization for mpox)
continued on Page 55

“As a safety net care venue, it is essential for facilities to have a dedicated team responsible for staying current on mpox-related best practices to prevent delays in diagnosis, treatment, and follow-up care.”
INFECTIOUS DISEASES
continued from Page 53
• Lesions in areas prone to severe scarring or complications (e.g., oral lesions causing dysphagia, anorectal lesions causing pain and constipation, or extensive skin lesions requiring debridement)
• Risk factors for severe disease (e.g., immunocompromised status, children, pregnant or breastfeeding individuals, or underlying skin conditions like eczema or psoriasis)
If a patient meets these criteria, contact the local or state public health department to check TPOXX availability. Alternatively, patients can access TPOXX through the STOMP (Study of Tecovirimat for Mpox) trial, regardless of whether they meet IND criteria. Patients meeting IND criteria are enrolled directly through the open-label arm of the trial, guaranteeing receipt of TPOXX if eligible. Patients not meeting IND criteria are randomized, with a two-thirds chance of receiving the drug and a one-third chance of receiving a placebo. To start the STOMP process, call 1-855-876-9997.
JYNNEOS is a two-dose intradermal or subcutaneous live attenuated vaccine for mpox prevention. Partial vaccination (one dose) is 36–75% effective, while full vaccination (both doses) is 66–89% effective. It is recommended over the older ACAM2000 vaccine due to better efficacy and safety for immunocompromised individuals and those with certain skin conditions. The two doses are administered 28 days apart and are now more widely available than in 2022.
According to the Advisory Committee on Immunization Practices (ACIP), the JYNNEOS vaccine is recommended for:
• Patients exposed to mpox as postexposure prophylaxis, including those attending large public events where there is local mpox transmission
• Individuals at high occupational risk for orthopoxvirus transmission, such as laboratory technicians working with orthopoxviruses (currently, it is not recommended for health care personnel without individual sexual risk factors or exposure to mpox patients without proper PPE)
• Individuals at high risk of acquiring mpox, including MSM, transgender, or nonbinary individuals (and their sexual partners) with high-risk behaviors in the past six months (e.g., multiple partners, sex in exchange for pay, or an STI diagnosis)
All patients who present to the ED should be counseled on vaccination as a future prevention strategy. Refer to local health department guidance for JYNNEOS availability in your region to better advise patients who test negative for mpox but are eligible for the vaccine to prevent community outbreaks.
In our quality improvement project for ED patients with mpox, we found that patients often have lingering questions about their diagnosis after their ED visit. Like other sexually transmitted infections, mpox carries stigma and historical trauma, particularly for sexual orientation and gender identity minorities. It is essential to ensure patients have access to ongoing care and support beyond the ED visit (ideally with the health department or a local infectious diseases clinic) to avoid repeated presentations for TPOXX information or quarantine management. Telehealth appointments are recommended, and involving social work and case management may be necessary for additional resources and support.
Mpox cases, though currently rare, are still circulating, and many of these patients may present to the ED for diagnosis and treatment. Providers need to maintain a high index of suspicion in
patients with a plausible transmission history, even if no rash is present. All patients should be tested for HIV, chlamydia, gonorrhea, and syphilis co-infection, and an established linkageto-care strategy should be in place, as quarantine periods may vary based on symptom resolution. As a safety net care venue, it is challenging to stay up to date on therapeutic availability, so facilities should identify a person or team responsible for maintaining current best practices, serving as a centralized resource for mpox-related questions to prevent delays in diagnosis, treatment, and follow-up care.
By the time of this publication, mpox epidemiology may have evolved. To stay updated on current trends, refer to the CDC for biweekly or monthly trends. This article was submitted on behalf of the mpox working group at the Johns Hopkins University Center For AIDS Research.

Dr. Rudolph is an instructor in emergency medicine at Johns Hopkins University. He completed his MD at the University of Iowa, his emergency medicine residency at Johns Hopkins, and is an international emergency medicine and public health fellow at Johns Hopkins. His research includes the delivery of ED-based HIV PrEP and STI services.

Dr. Hansoti is an associate professor in emergency medicine at Johns Hopkins University. She completed her MBChB at the University of Edinburgh, her emergency medicine residency at the University of Chicago, her MPH from Johns Hopkins, and her Ph.D. from the University of Cape Town. Her research focuses on the intersection of global health, HIV, and implementation science.
By Mack Sheraton, MD, MS, MHA; Arwen Declan, MD, PhD; and Christian Rose, MD, on behalf of the SAEM Informatics, Data Sciences, and Artificial Intelligence Interest Group
Introduction
Imagine a typical night in your emergency department (ED): boarding patients fill hallway beds, a lone physician juggles the board and the waiting room, and an overhead page calls attention to the ambulance bay for a 70-year-old patient with a ground-level fall. Amid this chaos, the potential of artificial intelligence (AI) to bring order is enticing. However, the question arises: Would an AI algorithm managing patient flow prioritize this elderly fall victim, or might its computed prognostications delay her care in favor of those with
a higher survival probability? What evidence would underlie such a decision? Is this ethical? Ultimately, who makes the decision—the physician, the system, or the machine?
These ethical quandaries are not new in emergency medicine, but integrating AI presents unique challenges. The guiding principles of medical ethics — beneficence, autonomy, nonmalfeasance, and justice — help navigate these decisions, but how can we ensure ethical AI integration? This article explores AI from the perspectives of beneficence and autonomy, with
respect for the classic challenge of balancing the needs of individual patients with those of the population. In Part 2 of this article, our colleagues will examine nonmalfeasance and fairness.
Beneficence, the duty to prioritize patient well-being, is a core principle of medicine. Emergency physicians pride themselves on doing what’s best for their patients. However, practical beneficence can become a tug-of-war between individual care and population health.
“We must remain the final arbiters of patient care, using AI as a tool to inform and support medical management strategies rather than as a surrogate decision-maker.”
of-life preferences is essential, and we must ensure these factors are not overlooked in favor of optimization.
Respecting an individual's freedom to make their own decisions
Acting in the best interest of the individual; providing benefit
Consider an AI system that optimizes resource allocation in overcrowded EDs. While increased efficiency is appealing, potential consequences must be considered. What if the system deprioritizes care for the most vulnerable patients, like our 70-year-old fall victim, in favor of those with statistically better outcomes? Physicians play a crucial role in protecting the human element against the relentless pursuit of efficiency.
As we integrate AI, physicians must critically evaluate AI recommendations and advocate for systems that incorporate individualized patient care. We must remain the final arbiters of patient care, using AI as a tool to inform and support medical management strategies rather than as a surrogate decision-maker. Our understanding of a patient’s personal values, cultural background, and quality-
Autonomy, the right to make informed decisions about one’s care, faces new challenges as AI is integrated. AI-assisted decision-making complicates the process of informed consent. Ensuring that patients understand the implications of AI involvement and can make truly informed choices requires careful consideration and clear communication.
Moreover, the ethical implications of using patient data to train AI systems cannot be ignored. Although data anonymization is standard, patients may not be fully aware that their information could be used to train AI systems. As physicians, we must advocate for transparency and ensure patients have a say in how their data is used.
AI recommendations may also inadvertently influence both physician and patient decision-making. Physicians must be vigilant in ensuring AI recommendations do not overshadow patient preferences and values. We must become "technology translators" who can explain complex AI processes in simple, comprehensible terms and who champion AI systems that adapt to individual patient needs.
As emergency medicine stands on the brink of a technological revolution, we must maintain our primary mission: to provide compassionate, patient-centered care. We must responsibly guide the integration of AI in clinical practice with strong ethical principles. By actively engaging with the ethical dilemmas posed by AI, we can help shape a future where technology enhances our ability to deliver high-quality care. This requires multidisciplinary collaboration among health care providers, patients, ethicists,
policymakers, and AI researchers to ensure innovation aligns with ethical values. We must be strong advocates for our patients, working to safeguard the physician-patient relationship and protect the integrity of our practice.
The ED of tomorrow is being shaped today. We must ensure it is built on a solid ethical foundation. By embracing this opportunity to guide the evolution of our field, always keeping the best interests of our patients at the forefront, we can create a future where human compassion and AI synergistically support exceptional emergency care

Dr. Sheraton is an assistant professor of emergency medicine at UT Houston Health Science Center. He focuses on responsible generative AI use in medical education and the automation of healthcare administration through digitalization.

Dr. Declan is the assistant research director at Prisma Health Upstate and clinical assistant professor at the University of South Carolina School of Medicine –Greenville and Clemson University. She applies informatics methods to improve patient care and support the clinician workforce.

Dr. Rose is an assistant professor of emergency medicine at Stanford University, focusing on the intersection of clinical practice and informatics to elevate patient care and promote a human-centered approach. Dual-boarded in emergency medicine and clinical informatics, his work leverages technology within healthcare to transform health outcomes through information systems.

By Diane Kuhn, MD, PhD; Marta Rowh, MD, PhD, MPH; Emily Binstadt, MD, MPH; Arwen Declan, MD, PhD; and Christian Rose, MD, on behalf of the SAEM Informatics, Data Sciences, and Artificial Intelligence Interest Group
Introduction
It is early Sunday afternoon, and the 70-year-old female patient from Part 1 of this article has undergone a full workup, with no injuries identified. As you finalize her discharge paperwork, the artificial intelligence (AI) algorithm in your EHR alerts you that the patient might need a skilled nursing facility referral. When you check with your patient, she assures you that she is comfortable living at home and has adequate social support: she states that she is highly independent and not in need of assistance, and she asks why you were concerned. Was it because of her age? As you explain that you were following computer-guided clinical recommendations, you wonder
whether the AI algorithm was biased in its assessment of her resource needs.
The conclusion of the case scenario, much like the concerns highlighted by our colleagues in Part 1, raises concerns about the ethical implications of AI’s evolving role in emergency medicine.
In this article, we focus on nonmalfeasance and justice.
It's early Sunday afternoon, and the 70-year-old female patient from Part 1 of this article has undergone a full workup, with no injuries identified. As you finalize her discharge paperwork, the artificial intelligence (AI) algorithm in your electronic health record (EHR) alerts you that the patient might need a referral to a skilled nursing facility. When you
check with the patient, she assures you that she is comfortable living at home and has adequate social support. She states that she is highly independent, does not need assistance, and asks why you were concerned — was it because of her age? As you explain that you were following computer-guided clinical recommendations, you wonder whether the AI algorithm was biased in its assessment of her resource needs. This scenario, much like the concerns highlighted by our colleagues in Part 1, raises ethical questions about AI’s evolving role in emergency medicine. In Part 2, we focus on the principles of nonmaleficence and justice.
Avoiding and doing no harm to the individual
Treating all individuals with fairness, equality, and impartiality
Nonmalfeasance
We’re all familiar with the dictum “do no harm,” a concept deeply entrenched in the practice of medicine. "Do no harm," which summarizes the rule of thumb approach to nonmaleficence, seems straightforward enough. However, current AI health care algorithms fail to consistently meet this fundamental standard.
First, AI requires the sharing and use of sensitive patient data. Since sharing personal data introduces risks to patients, they should be informed about these potential risks and should always have the ability to opt in (consent) or opt out of AI data sharing. Second, the accuracy and helpfulness of health recommendations by AI algorithms is unclear. We do not know to what extent these algorithms can integrate empathy, the desire for social interaction, or other complex human
needs, such as feeling heard. Without incorporating these complex human variables, AI-generated medical advice risks introducing harm by recommending overtreatment, undertreatment, or inappropriate treatment. Furthermore, we do not know how these algorithms will impact the essential human interactions between physicians and patients. Physicians who have sworn an oath to “do no harm” will have to grapple with nonmaleficence as they review and interpret the recommendations AI systems generate.
In addition to nonmaleficence, physicians must ensure that the benefits of treatment and health care resources are equitably offered to all patients. Many hope that integrating AI into clinical decision-making will eliminate the well-documented human biases in health care. However, since AI systems are trained on large datasets that reflect existing societal biases, AI can inadvertently perpetuate and even exacerbate these inequities. Such biases can manifest at multiple stages: preprocessing, when data is cleaned and prepared; in-processing, when the algorithms are developed and trained; and postprocessing, when the AI outputs are implemented in clinical settings.
In addition to perpetuating health inequities, AI algorithms can prioritize resource optimization and efficiency, potentially at the expense of individual patient care. For instance, an AI system designed to reduce hospital costs might recommend treatment plans based on cost benefits to the system rather than health benefits to the patient. Consequently, a patient’s care may be standardized without considering the nuances of individual circumstances that human physicians typically navigate with a more personalized focus. While several comprehensive frameworks and checklists have been developed to address these risks, the lack of transparency in AI decision-making processes can obscure discriminatory practices. Ensuring that AI contributes to health care justice requires continuous investment in research, transparent practices, and the inclusion of diverse patient populations in the development and deployment of AI systems.
AI algorithms are increasingly being implemented in health care. These algorithms are typically designed to
maximize efficiency, and substantial human oversight and advocacy will be necessary to ensure that they treat patients fairly and avoid causing harm. Change in emergency medicine is inevitable, particularly as it relates to AI. Engaged clinicians and physician researchers can help guide AI development to ensure its use aligns with the principles of nonmaleficence and justice, avoiding patient harm and inequitable treatment

Dr. Kuhn is an assistant professor of emergency medicine at Indiana University, with research interests in patient-centered care, informatics, and health equity. Her focus is on the utilization of health information technology to enhance the value of emergency care to patients.

Dr. Rowh is an assistant professor of emergency medicine at Emory School of Medicine and a former Air National Guard chemical, biological, radiological, and nuclear (CBRN) unit emergency physician. Her academic interests focus on bias in medical education and sports injuries in the older adult population.

Dr. Binstadt is an associate professor of emergency medicine at University of Minnesota Medical School and a core faculty member at Regions Hospital Emergency Medicine Residency. Her academic interests include simulation, ethics, wilderness medicine, and issues of justice, equity, diversity, and inclusion in medicine.

Dr. Declan is the assistant research director at Prisma Health Upstate and a clinical assistant professor at the University of South Carolina School of Medicine-Greenville and Clemson University. She applies informatics methods to improve patient care and support the clinician workforce.

Dr. Rose is an assistant professor of emergency medicine at Stanford University, focusing on the intersection of clinical practice and informatics to elevate patient care and promote a human-centered approach. Dual-boarded in emergency medicine and clinical informatics, his work leverages technology within healthcare to transform health outcomes through information systems.

By Jeremy Brown, MD
The National Institutes of Health (NIH) is composed of numerous institutes, each with a distinct focus. Some, such as the National Eye Institute and the National Heart, Lung, and Blood Institute, concentrate on specific organs. Others, like the National Cancer Institute and the National Institute of Neurological Disorders and Stroke, focus on diseases. Still, others, including the National Institute of Child Health and Human Development and the National Institute on Aging, center their work on specific populations.
Earlier this year, representatives of the Society for Academic Emergency Medicine (SAEM) met with several program officials from the National Institute on Minority Health and Health
Disparities (NIMHD), another populationfocused institute.
NIMHD began as a modest office in 1990 and was designated an official institute in 2010. As its name suggests, its mission is to lead scientific research to improve minority health and eliminate health disparities. It offers opportunities common to other institutes, such as the K23 Mentored Patient-Oriented Research Career Development Award and the R01 Research Project Grant. Additionally, NIMHD provides targeted opportunities, such as funding for research into health care interventions in immigrant populations
Several emergency care physicians and researchers have received funding from NIMHD. For instance, Dr. Colleen
Gutman from the Department of Emergency Medicine at the University of Florida in Gainesville recently received a K23 award to study how implicit bias affects physician behavior in pediatric emergency departments.
Other emergency care researchers are supported by R01 grants. Dr. Lesli Skolarus from Northwestern University and Dr. William Meurer from the University of Michigan are studying hypertension control in underserved populations that use safety-net hospitals. They have recruited patients with hypertension from emergency departments and are comparing two groups: one group is instructed to follow up with a primary care provider after emergency department discharge, while the second group receives prompted self-monitored blood pressure monitoring and tailored feedback, along with facilitated primary care

appointments and transportation.
Another R01 grant from NIMHD supports Dr. John McConnell, a health economist and professor in the Department of Emergency Medicine at Oregon Health & Science University, who studies the impact of changes in Medicare policy on transgender beneficiaries.
Dr. Marina del Rios from the Department of Emergency Medicine at the University of Iowa is using NIMHD support to identify and debunk misinformation about vaccines in predominantly Hispanic communities in Chicago. Dr. Jennifer Newberry from the Department of Emergency Medicine at Stanford
University is using her R01 support from NIMHD to explore ways to increase culturally specific knowledge of mental health, trauma, and support services in the Latinx population of East San José, California. Additionally, Dr. Phil Levy, who holds the Edward S. Thomas Chair in the Department of Emergency Medicine at Wayne State University, is using a P50 from NIMHD to address cardiometabolic health disparities and improve Black-White lifespan inequality in Detroit and Cleveland.
For more information on NIMHD opportunities, you can sign up for the NIMHD External newsletter or attend their five-day Summer Institute

Dr. Brown is the director of the Office of Emergency Care Research (OECR) where he leads efforts to coordinate emergency care research funding opportunities across NIH. Additionally, Jeremy is the primary contact for the NINDS Exploratory and Efficacy FOAs and serves as NIH's representative in government-wide efforts to improve emergency care throughout the country. He is also the medical officer for the SIREN emergency care research network which is supported by both NINDS and NHLBI. Jeremy.brown@nih.gov

By Dina Wallin, MD; Ana Acevedo, and Wendi Wendt, MD, on behalf of the SAEM Pediatric Emergency Medicine Interest Group
Three family members involved in a rollover motor vehicle collision arrive at the emergency department (ED): two adults and a 20-month-old toddler. The toddler was properly restrained in a car seat, had no loss of consciousness, and has normal vital signs in the ED, except for tachycardia while crying. He soothes easily with a toy, and the team finds an overall normal exam, except for scattered superficial abrasions on both hands and a contusion on his forehead. Does this child need imaging to evaluate for cervical spine injury (CSI)?
Consider an 8-year-old who was struck by a car traveling approximately 15 miles per hour and then thrown five
feet. She had no loss of consciousness and is awake, alert, and reporting only a mild headache and posterior neck pain. Her exam is normal, except for a few bruises on her arms and legs. Does she need imaging to evaluate for CSI? If so, what modality?
CSI is rare in pediatrics, found in fewer than 1-3% of patients with blunt trauma, compared to 5-10% of older adults with blunt trauma. However, children younger than 8 years old tend to develop higher-level (C1-C2) CSI compared to older children and adults, creating an opportunity for missed injuries that can lead to significant morbidity. (See this review for more basics on pediatric CSI.)
Diagnosing CSI in pediatric patients can be challenging for several reasons: pediatric cervical spines have different biomechanics than those of adults, leading to different injury patterns; pediatric patients can be difficult to examine and may require anxiolysis to obtain axial imaging; and, most significantly, children have an increased risk of future malignancy after radiation exposure compared to adults, motivating providers to minimize ionizing radiation exposure in CSI workups.
What a perfect storm — a highmorbidity but rare condition, for which diagnosis is especially challenging. If only emergency providers had an
evidence-based, easy-to-use instrument to support decision-making! Fortunately, researchers from the Pediatric Emergency Care Applied Research Network (PECARN) came to the rescue with their pediatric CSI prediction rule, which helps providers triage injured children into high, lower, and low-risk categories for CSI, with recommendations for each.
First, assess for high-risk features: Glasgow Coma Scale (GCS) ≤ 8; unresponsive on the Awake, Verbal, Painful, Unresponsive (AVPU) scale; abnormal findings in airway, breathing, or circulation; or focal neurologic findings. If a pediatric patient has any of these, CT is recommended to evaluate for CSI. (For top-tier care, consider the use of low-dose CT for pediatric patients. Using low-dose rather than conventional CT nearly halves the risk of developing future malignancy.) If the patient has none of these high-risk features, then screen for other features that increase the risk of CSI: report of neck pain; substantial head injury; substantial torso injury; or posterior neck midline tenderness to palpation ("substantial" was defined as an injury requiring inpatient admission or surgical intervention). If the child has any of these, plain films are recommended to screen for CSI. (Many centers use AP, lateral, and odontoid views for children aged five years and older, and AP and lateral views for children younger than five, with the lateral view providing the most useful information.) What if a patient has no risk factors for CSI? A provider can clinically clear them. No imaging needed, no collar required.
This rule is particularly helpful because it does not rely on the history or mechanism of injury, many aspects of which may not be present at the initial ED evaluation of a minimally verbal child. This study also includes patients suspected of nonaccidental trauma, which is unusual in pediatric trauma literature. A few important points about these findings: first, in the PECARN study, children with "high" risk features had a CSI prevalence of 12.1%, and those with lower risk features had a CSI rate of 2.8%. These injuries are present in a minority of patients, even among the sickest. Second, this tool does not provide specific recommendations for pediatric patients with anatomic variants with increased risk of CSI, such as children with trisomy 21, who have a higher prevalence of atlantoaxial instability.
• GCS score 3-8 or unresponsive on the AVPU scale
• Abnormal airway, breathing, or circulation
• Focal neurological deficits on examination
CART-DERIVED RISK FACTORS
• Altered mental status†
• Self-reported neck pain or neck tenderness on examination
• Substantial‡ head or torso injury
Although a "predisposing condition" was a risk factor for CSI in PECARN’s previous retrospective work, neither medical conditions nor mechanisms of injury (such as diving) emerged as significant predictors of CSI in this cohort, likely because this tool focuses on signs and symptoms present in the trauma bay rather than remote history. Lastly, this tool does not address the utility of MRI or how to approach a child with persistent neck pain after a negative CT. Nonetheless, most children will fall into the PECARN high, lower, and low-risk categories, and this new tool presents an incredible opportunity to improve the care we deliver.
Revisiting the cases: First, the 20-month-old with a forehead contusion and no other findings after a concerning mechanism of injury. Applying the PECARN decision instrument, there are no identified high-risk factors. The child also has no lower risk factors (a forehead contusion is not considered a "substantial" head injury), so clinical clearance is appropriate. Yes, clinical clearance after a rollover motor vehicle collision! For the 8-year-old with a mild headache and neck pain after being struck by a vehicle, she meets no highrisk criteria but does report neck pain. Therefore, she should receive AP, lateral, and odontoid plain films of her cervical spine. CT is not warranted unless these films are abnormal.
In summary, the PECARN pediatric CSI prediction rule offers a valuable framework for assessing cervical
RISK OF CERVICAL SPINE INJURY
187/1549 (12.1%)
Consider CT
RISK OF CERVICAL SPINE INJURY
217/7676 (2.8%)
Consider plain x-ray
RISK OF CERVICAL SPINE INJURY
29/13205 (0.2%)
Consider clinical clearance 12.1% 2.8% 0.2%
spine injury risk in children, helping to guide imaging decisions effectively. By focusing on clinical indicators rather than historical or mechanism-based factors, it ensures that appropriate care is provided while minimizing unnecessary radiation exposure. Applying this rule can significantly enhance patient safety and outcomes in pediatric trauma cases

Dr. Wallin is an associate clinical professor at UCSF-San Francisco General Hospital and an emergency medicinepediatric emergency medicine physician at UCSF, where she focuses on medical education, bioethics, and diversity, equity, and inclusion in health.

Dr. Wendt is an assistant professor of pediatric emergency medicine in the Department of Pediatrics at the Medical College of Wisconsin and a pediatric emergency medicine physician at MCW, where she focuses on injury prevention, pointof-care ultrasound, and sedation.

Ana Acevedo is a fourthyear medical student at the Perelman School of Medicine at the University of Pennsylvania, applying into emergency medicine. Ana’s interests include global health, pediatric EM, and DEI in medical education.

By Megan Musselman, PharmD, MS, and Maria Rudis, PharmD, on behalf of the SAEM Toxicology/Addiction Medicine Interest Group and the SAEM Academic Emergency Medicine Pharmacists Interest Group
Patients with acetaminophen overdose frequently present to the emergency department. According to the 2022 National Poison Data System annual report, acetaminophen remains the second most common substance linked to fatalities.
Acetaminophen poisoning occurs when the liver's ability to detoxify acetaminophen is overwhelmed, leading to the accumulation of the toxic metabolite N-acetyl-p-benzoquinone imine (NAPQI). Normally, NAPQI is detoxified by glutathione. In cases of overdose, glutathione stores are depleted, causing hepatocellular damage and potential liver failure. N-acetylcysteine (NAC) is a highly effective antidote; when administered
within the first eight hours, it prevents most liver injuries and reduces mortality.
For decades, dosing IV NAC has followed a "one size fits all" approach. The FDA-approved IV NAC regimen involves administering 300 mg/kg over 21 hours using three separate IV infusion bags, each with its own concentration and infusion rate. However, recent efforts have aimed at more individualized dosing regimens. These include optimizing the delivery of the standard 21-hour protocol, increasing the dose and duration of NAC in massive (“high risk”) ingestions, and shortening NAC administration when liver function tests return to baseline.
The traditional 21-hour NAC IV regimen, administered in three sequential doses with differing doses and concentrations, can lead to interruptions in antidote infusion and is associated with dosing errors. Additionally, non-allergic anaphylactoid reactions (NAAR) frequently occur due to the large initial NAC dose (150 mg/kg) in the first bag.
A simplified two-dose regimen is appealing as it may reduce interruptions in care, medication errors, and the incidence of dose-related NAARs. Two-dose regimens generally extend the initial bolus over several hours. Since NAARs are typically dose-related, reducing the infusion rate from the
“N-acetylcysteine (NAC) is a highly effective antidote; when administered within the first 8 hours, it prevents most liver injuries and reduces mortality.”
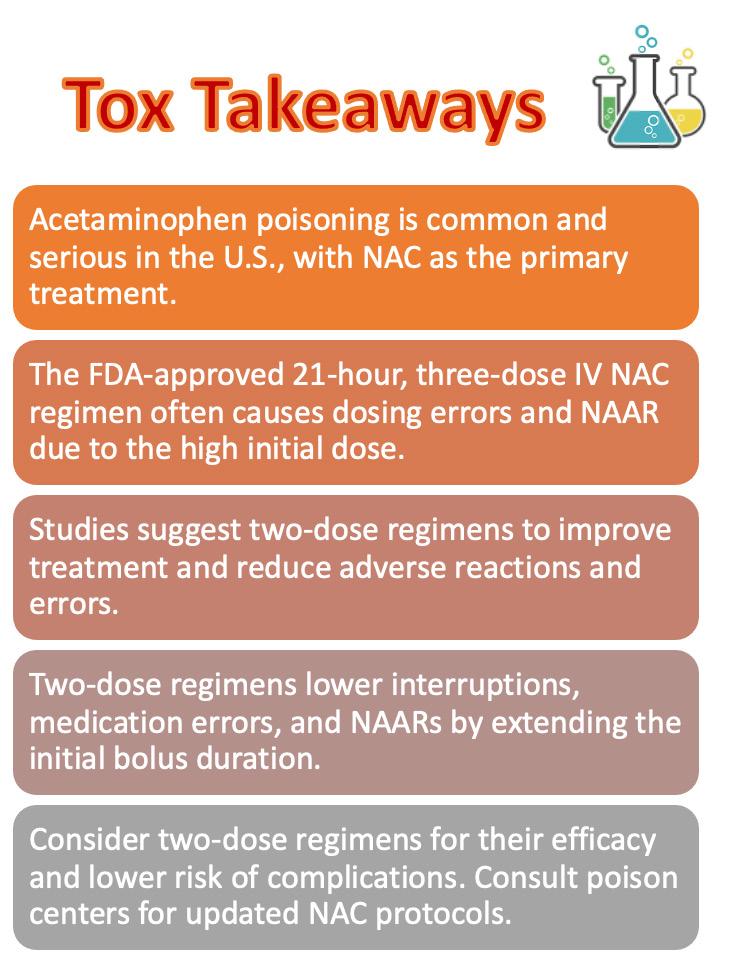
initial 150 mg/kg bolus over one hour in the traditional three-dose protocol to 50 mg/kg/hour over four hours may help decrease NAARs.
Recent evidence and a systematic review suggest that a simplified twodose IV NAC regimen is both safe and effective. The two-dose NAC regimens have similar, and in some studies, noninferior outcomes compared to the traditional three-dose regimen in terms of liver injury. They also result in fewer adverse reactions, including cutaneous reactions (e.g., flushing, itching),
systemic reactions (e.g., bronchospasm, hypotension, angioedema), fewer treatments for adverse reactions, and fewer delays or interruptions in NAC infusions. Additionally, two-dose NAC infusion regimens result in fewer medication errors.
While the two-bag regimen shows clear advantages over the traditional three-bag regimen, some have proposed that a single-bag system might be even better. However, one-dose systems involve significantly larger total doses (e.g., 430 mg/kg, 450 mg/kg) and still administer the same large initial dose (150 mg/ kg) in the first hour as the traditional three-dose regimen. This approach does not seem to reduce adverse events or medication errors. Moreover, these larger total doses exceed the amount of NAC typically required for a standard single acute ingestion, which is not classified as a “massive” ingestion. Therefore, the single-dose regimen does not offer an advantage in reducing adverse events or medication errors.
The advantages of the two-dose/20hour regimen are particularly relevant for emergency medicine practice. The changes from the traditional three-dose regimen occur in the first four hours of infusion, when the patient is likely still
in the emergency department. Effective and efficient resource utilization and minimization of unnecessary treatments and interventions are increasingly important to maintain throughput and flow in the era of ever-increasing ED boarding.
For patients requiring antidotal therapy following acetaminophen overdose, a two-dose NAC regimen appears to have similar outcomes to the traditional threedose regimen in terms of liver injury while resulting in fewer adverse reactions, fewer treatments for adverse reactions, fewer delays or interruptions in NAC infusions, and fewer medication errors.
Poison centers are available 24/7 at 1-800-222-1222 to provide guidance on NAC protocols, including modifications for complicated and high-risk acetaminophen ingestions. Consulting with a local toxicologist for the most appropriate dosing regimen is recommended. Stay connected with your local poison center to ensure your NAC protocols remain current with the latest research.

3-dose FDA approved regimen (“Prescott protocol”)
Table 1. Comparison of Traditional Three-Dose and Simplified Two-Dose NAC Regimens
*IV: intravenous; NAC: N-acetylcysteine; FDA: US Food and Drug Administration; mL: milliliter; D5W: dextrose 5% in sterile water; mg: milligram; kg: kilogram; SNAP: Scottish and Newcastle Antiemetic Pre-treatment for Paracetamol Poisoning, used in the United Kingdom with a unique treatment threshold (four-hour [APAP] = 100 mcg/mL nomogram line) compared to the United States (four-hour [APAP] = 150 mcg/mL nomogram line).
Dr. Musselman is a clinical pharmacy specialist in emergency medicine and the clinical emergency department pharmacist coordinator at North Kansas City Hospital. She also serves as the PGY-2 emergency medicine pharmacy residency program director.

Dr. Rudis is a clinical pharmacy specialist in emergency medicine at Mayo Clinic in Rochester, Minnesota. She is also an associate professor of emergency medicine and pharmacy at the Mayo Clinic College of Medicine. She is a board-certified clinical toxicologist (DABAT) and a fellow of the College of Critical Care Medicine. She co-chairs the Mayo Clinic Pharmacy Formulary Subcommittee on Emergency Medicine and Toxicology and the Emergency Medicine Enterprise Pharmacy Leadership Group.

By Joseph Ciano, DO, MPH, MS
Medical training is a challenging journey. It involves countless clinical hours, competency exams, fluctuating between day and night shifts, sleep dysregulation, difficult patient conversations, witnessing births and deaths, deciding on subspecialty training, finding the right job after graduation, and, of course, managing the ups and downs of personal life while learning to be a great doctor.
When I graduated from emergency medicine residency in 2019, I was excited to begin a new chapter. I was ready to make my own decisions without the required approval of a supervising physician. I looked forward
to a higher salary, fewer shifts, and a new level of respect from patients and nursing staff. I could practice medicine the way I believed was best for my patients.
It was a well-earned, happy moment.
At the same time, there was a whisper — a persistent internal dialogue that had been playing in my head since college. Though I tried to ignore it, it always resurfaced. As I reflected on what graduating from residency meant for my life, career, and future patients, the whisper said, “You’re not ready.” I found myself comparing my abilities to those I perceived as more competent — those who seemed to have a broader medical knowledge base, better bedside manner, superior procedural
skills, or more natural talent. They had something I felt I lacked.
Imposter syndrome: that was the whisper.
The completion of each step of medical training is a milestone worth celebrating, but it can also be unsettling, as each new step comes with new responsibilities and expectations. While I didn’t feel this way on my graduation day, conversations with some of the most senior and confident doctors in my circle revealed that many medical professionals, even if only briefly, experience feelings of self-doubt and inadequacy.
The truth is, the whisper does quiet down at times, but it’s always lurking in
im·pos·tor syn·drome (noun) the persistent inability to believe that one's success is deserved or has been legitimately achieved as a result of one's own efforts or skills.

the background. A career in emergency medicine has taught me to be prepared and proactive. With that in mind, I’ve compiled three tips that have helped me over the years in dealing with imposter syndrome and work-related anxiety:
Trust in the process.
You’ve been given a seat at the table because others chose to believe in you. Trust that you deserve this. Your skills and experiences have proven you competent. You’ve taken numerous exams and met standardized assessments established by experts in your field. Trust the process and all those who have believed in your abilities and potential. Trust your employer who hired you, your mentor who believed in you, and the part of you that once believed this journey was possible.
Many of us in medicine are adept at this skill. This tip is particularly helpful if you’re experiencing anxiety or self-doubt during high-stakes moments, such as a time-sensitive procedure, a presentation, or an important conversation you can’t cancel or reschedule. Compartmentalize your feelings and save them for later
processing. Just don’t forget to process them.
Find a healthy way to manage your feelings.
There are many ways to deal with selfdoubt, anxiety, and stress. This might include confiding in trusted people, seeking a counselor, connecting with a mentor, or talking to someone who will listen without judgment. Other methods might involve physical exercise, time in nature, meditation, mindful breathing, worship, prayer, or social time with friends or family. There’s no single way to process feelings, so don’t assume a method won’t work for you, or rely exclusively on just one.
These tools will help you build a sustainable career in medicine and prevent you from missing the personal and professional opportunities that will shape your future. You know more than you’re consciously aware of. The years spent charting, studying late, researching difficult cases, preparing presentations, and spending extra time with patients all contribute to a lived experience of learning. Over time, you’ve internalized
countless snippets of knowledge and developed pattern recognition skills that will serve you well.
Trust the process that brought you to where you are today, compartmentalize your feelings during high-stakes moments, and most importantly, find a healthy and sustainable way to manage those feelings. Your patients, friends, family, and mind will thank you.

Dr. Ciano is the associate course director of the Master’s in Emergency Medicine Certificate Program in Durgapur, India, and a clinical assistant professor at the Perelman School of Medicine at the University of Pennsylvania. He also works as an emergency medicine physician at the Hospital of the University of Pennsylvania. His professional interests include medical education and global health. This article was inspired by a keynote speech Dr. Ciano delivered at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell emergency medicine residency graduation ceremony in New York.

Interviewed by Sara Schulwolf on behalf of the SAEM Research Committee
Cameron Gettel, MD, MHS is an assistant professor in the department of emergency medicine at the Yale School of Medicine, a clinical investigator at the Yale Center for Outcomes Research and Evaluation, and co-director of the Yale Emergency Scholars (YES) Program. He is an active member on the executive committee of SAEM's Academy of Geriatric Emergency Medicine (AGEM). Dr. Gettel was a 2024 recipient of the SAEM Early Investigator Award.
Congratulations on your recent SAEM early investigator award! What factors do you think contribute to being a successful clinician-scientist at your career stage? What have been the biggest challenges that you have encountered so far in your career? Several factors contribute to being a successful clinician-scientist in the early stages of a career. The most important of these is mentorship. It is critical to have mentors in your corner who have navigated this path before, are willing to invest time and energy in you, and will advocate for you, ensuring that your
time is adequately protected to grow your research portfolio.
The biggest challenge has been securing long-term funding. However, I have found that staying persistent, as advised by many prior successful mentors, and adopting the strategy of submitting numerous grant applications increases the likelihood of success.
How did you become interested in a career in emergency medicine (EM) research, and specifically in the area of geriatric EM?
While I loved the ability to influence people’s lives on a one-to-one basis at the bedside, I valued the opportunity research offered to ask and answer important questions that had the potential to influence outcomes for a larger population.
Geriatric EM research drew me in for several reasons, both personally and professionally. Personally, while I was in medical school, several older adult family members experienced suboptimal care transitions among the
community setting, the emergency department (ED), the hospital, and skilled nursing facilities, ultimately resulting in decreased mobility and quality of life. Professionally, in my early years of residency, I consistently saw older adults from nursing homes come to the ED with incomplete paperwork that failed to detail the clinical question to be evaluated. Often, the patient had cognitive impairment and couldn’t provide adequate details, the family members were unaware the patient was in the ED, the ambulance providers were uncertain, and the nursing home staff had changed shifts by the time I contacted them. Many times, we ended up conducting large and costly workups and potentially admitting these patients to the hospital unnecessarily, which may have been misaligned with their goals of care. This was a pain point for me, and I remember an early mentor telling me to run towards those pain points and address them head-on.
I’m sure that many EM providers can relate to encountering pain points in
our health care system, but it’s much less common for people to turn their frustration into action, as you did. Can you speak to how you made that happen within the space of improving transitions of care for older adults?
In my case, it definitely took a team to move the needle — primarily my mentor Dr. Elizabeth Goldberg and motivated stakeholders across the state of Rhode Island. It came down to a group of people unwilling to settle for the status quo. We first assessed nursing home-to-ED care form documentation and found that the vast majority neglected to share the older adult’s usual mental status, usual functional status, and reason for transfer— all crucial information for the ED clinician. I was excited that the end of the research project was not just identifying the deficiencies in nursing home-to-ED documentation for older adults. Instead, we took the next step and thought through how to improve the current situation by standardizing communication forms statewide. Since then, we’ve implemented the standardized forms we developed and found that critical element documentation has improved. Research can sometimes feel abstract or removed from the work once it’s accepted into a journal, but these efforts, when directly translated to the patient, are gratifying and worth celebrating.
Especially as an early career physician-scientists, is it difficult to create dedicated time for grant writing or other research pursuits?
How do you negotiate time with your department chair?
Looking back, I’ve realized it’s a twoway street. I came to the table having shown that I was invested in a career in EM research by completing a rigorous two-year fellowship. Having done my fellowship at Yale, departmental leadership at the time knew who I was, my skills, productivity, and work ethic, and where I was likely to pursue and obtain funding on the path to independence. My department came to the table with a deep commitment to research and afforded me a runway for a few years of protected time to seek out and obtain that funding, as well as access to resources, support services, and the infrastructure critical to achieving those goals. I have no novel advice on negotiating with your department chair, but I think framing the conversation around the benefits to both
sides is a good starting point. Leadership understands that you are not superhuman and can’t work 14 shifts a month and have R-level grants.
What advice would you give to medical students or residents interested in pursuing a career as a physicianscientist?
My primary advice would be to pursue advanced training. Twenty years ago, you might have been able to obtain an academic EM job without fellowship training. It’s becoming increasingly difficult nowadays. If you want to do it right, I strongly suggest getting the methodologic training needed to answer the questions you find important. After residency, I completed the two-year National Clinical Scholars Program, a health policy and health services research fellowship. Currently, I also serve as codirector of the Yale Emergency Scholars (YES) Program, which condenses a fouryear residency and a two-year SAEMcertified fellowship track into five years. These opportunities, and several others within the specialty, serve as excellent launching pads for motivated trainees.
You have had research grants funded by agencies such as the Centers for Medicare and Medicaid Services (CMS) and the National Institute on Aging (NIA) and have received multiple R03 awards from the National Institutes of Health (NIH). What advice would you give to EM researchers interested in pursuing federal research grants?
My first piece of advice is that it’s a numbers game. It’s unlikely you will succeed on your first grant. Stay persistent. If you are fortunate to hit early, there will likely be lulls later on where you will need to continue finding funding opportunities and throwing things at the wall to see what sticks. Second, and more logistically, spend the majority of your time on the Specific Aims page — make it as clear and concise as possible, as the majority of the study section reviewers will look solely at that. Third, on a more macroscopic level, work smarter, not harder. Don’t reinvent the wheel and forge your own path. Instead, do your homework by looking up people in your topic area of interest and look at their website profiles and NIH Reporter to see their funding trajectories.
How has SAEM impacted your path as a clinician-scientist?
SAEM has impacted my path as a clinician-scientist as it has been my academic home. The SAEM Annual Meeting is, without a doubt my favorite conference of the year, as I get to reconnect with old friends at different institutions and meet new folks at various stages of their careers. As a few specific examples, I have benefited immensely from the brain power within SAEM’s Academy of Geriatric Emergency Medicine (AGEM), the SAEMF GEMSSTAR funding, and serving on SAEM committees that have advanced emergency care research and provided opportunities for networking and collaborations.
What upcoming projects are you most excited about? Any upcoming publications we should keep an eye out for? I’m trying to juggle a few plates without dropping any. In the pipeline, I have a few bread-and-butter health services research projects looking at outcomes of older adults (particularly those living with dementia), in the vulnerable time period after emergency care. I am wrapping up a few projects where we developed new patient- and caregiver-reported outcome measures assessing ED-to-community care transitions. Some of the work I’ve really enjoyed over the last few years has addressed the dynamics of the EM workforce.
What is one thing you wish all EM physicians would take away from your work and apply to their practice? Spend a little extra time with older adult patients when discharging them. Understand their concerns, as well as the concerns of family members, and ensure they are addressed. With primary care access being limited, the days following emergency care represent a vulnerable period. Ensure they have a good understanding of what you expect to happen in the coming days and what specific red flags should prompt a return ED visit.

Sara Schulwolf is a fourth-year medical student and MPH student at the University of Connecticut. She is currently serving as the medical student representative for the RAMS Board and liaison to the SAEM research committee.

By Rebecca G. Theophanous, MD, MHSc on behalf of SAEM Educational Research Interest Group
Simulation-based medical education is a critical component of emergency medicine resident training. By incorporating simulation models into medical training, physicians can practice clinical skills such as psychomotor hand-eye coordination for procedures, engage in deliberate practice for recognizing and optimizing pointof-care ultrasound (POCUS) views, and encounter pathology that is less common in patient populations. Studies have shown high efficacy for simulation models in medical training, as they strive to replicate realistic patient scenarios or facilitate the practice of specific skills in a safe, controlled environment. For POCUS specifically, various simulation experiences exist, ranging from low to
high fidelity and low to high cost. These POCUS simulations enable residents to practice not only image acquisition and interpretation but also higher levels on Miller’s pyramid of clinical competence, such as clinical integration and medical decision-making. Below, we provide an overview of different types of simulation training models available.
POCUS training is time- and resourceintensive, often requiring in-person training with low student-to-teacher ratios and a comprehensive curriculum that includes diagnostic examinations and procedural applications. Some of the educational burden has shifted toward e-learning with online modules, especially after the COVID-19
pandemic, with studies showing comparable efficacy between online and in-person learning. However, certain skills and competencies cannot be assessed remotely or in a classroom setting, leading to the development of low-fidelity simulators by POCUS faculty to mitigate high costs and resource limitations.
Partial task-trainers are designed to test specific tasks, typically procedures, and can be used repeatedly to practice the psychomotor skills necessary to successfully complete a procedure without risk to the patient. Partial task trainers or phantom models can be
continued on Page 73
VISUAL REPRESENTATION OF ULTRASOUND SIMULATION MODELS





Table 1: Different types of medical
Phantom (homemade) low low
Specific procedural skill, low cost
Partial-task trainer low low
Specific procedural skill, lower cost
Model does not preserve, wears down with repeat use, no patient aspect
Standardized patient moderate low
Wears down with repeat use, no patient aspect
Human model, normal anatomy, patient interaction No pathology
Mannequin high high
Computer-based simulator high high
Pathology, psychomotor ultrasound skills, anatomy
High cost
E-learning modules with probe moderate high
Pathology, psychomotor ultrasound skills, anatomy
Incorporates cases with pathology, learner assessments, probe spatial orientation but no anatomy
High cost
High cost
and their characteristics. The author is not supported or employed by any of the companies or products mentioned in this article nor are they promoting any product or company, only citing them as examples.
“Simulation-based medical education component of emergency medicine resident allowing physicians to practice clinical less common pathologies in a controlled

is a critical resident training, skills and encounter controlled environment.”

continued
from Page 70
homemade or inexpensive models. Several POCUS experts have published “recipes” for creating homemade models using ballistics gel or gelatin with molds, including models ocular ultrasound, lung ultrasound, thoracentesis or pericardiocentesis, abscess drainage, and more Other homemade models using meats such as chicken or pork can be used for nerve block simulators, allowing for the injection of saline or lidocaine with realistic hydrodissection around nerves or fascial planes. The disadvantage is that these models wear out over time with repeated use and usually simulate only one level of difficulty and one procedure. Blue Phantom and Simulab offer vascular access models for peripheral IV and central line training, allowing learners to practice adjusting image depth and gain, and visualizing the needle in both transverse and longitudinal views to optimize their technique.
Standardized patients provide a more realistic human model, enabling learners to practice obtaining correct images, visualizing actual anatomy and spatial orientation, and troubleshooting when faced with obstructing artifacts. Although this model is somewhat limited by the use of healthy volunteers without pathology, it is more realistic for the clinical setting and also requires communication with the patient. Learners should be attentive to patient comfort with probe pressure and manipulation.
High fidelity simulators, though costly, offer significant advantages in realistic real-time image display, improved image quality, varying difficulty levels, and built-in user feedback for improvement. These simulators are particularly effective for testing and deliberate practice of higher-level skills. The most common method used is interpolative, deriving 2D images from pre-acquired, rendered 3D ultrasound volumes. Examples such as the CAE Vimedix or Sonosim mannequin simulators can teach learners using a three-dimensional view of the anatomical structures alongside projected ultrasound images on the computer screen.
Mannequins equipped with radiofrequency identification devices (RFID) allow the transmission of images from the ultrasound probe to the computer screen. This technology
supports cases with pathologic findings, enabling the learner to practice navigating clinical scenarios as they would in real life. The RFID tags on the mannequin’s body also simulate real anatomic locations, which is an advantage over task trainers and standardized patients that lack pathology or spatial orientation. This model is ideal for thoracic and abdominal POCUS applications.
Generative image-based methods use computed tomography or magnetic resonance imaging to create ultrasound image slices, though these require an offline preprocessing phase to create the simulation algorithm inputs. Generative model-based methods can be used for dynamic models, such as a beating heart or sliding lungs, although creating these images is complex.
Finally, screen-based computer simulators with extensive e-learning platforms, such as SonoSim, incorporate computer-generated cases of normal and pathology images, facilitate knowledge and skill assessments through questions and probe manipulation, and more. Some research studies have shown these simulators perform as well as traditional teaching methods
Summary
Simulation-based medical education continues to evolve and improve, with innovative technologies including computer-based, probe-based, and phantom model training. Virtual reality is being explored in early studies for medical education and clinician training, and artificial intelligence is continuously expanding current knowledge. It is exciting to see how the field is growing, augmenting ultrasound education for learners at all levels of training.

Dr. Theophanous is an ultrasound-fellowship trained emergency medicine physician at Duke University Hospital and the emergency ultrasound director at the Durham VA. She teaches clinical point-of-care ultrasound (POCUS) and has presented POCUS didactics locally and nationally. Her research involves implementing a POCUS curriculum for EM physicians, creating a standardized POCUS nerve block training model, and developing innovative 3D ultrasound technology.
@rbectheo, @dukeemergency, @duke_eus

By Alana Moore; Orly Morgan; Juhi Varshney, MD; and Mark Supino, MD, on behalf of the SAEM Social Emergency Medicine and Population Health Interest Group
Introduction
People experiencing homelessness (PEH) represent a highly vulnerable segment of the population frequently confronted with numerous mental health challenges. Extensive research indicates a significant overlap between PEH and those with severe psychiatric conditions, including schizophrenia, schizoaffective disorder, bipolar disorder, depression, post-traumatic stress disorder, substance use disorder, and acute psychotic episodes. The link between
housing insecurity and mental illness arises from various complex sociological and physiological factors, with the chronic stress of housing insecurity exacerbating pre-existing psychiatric conditions prevalent among PEH. Both housing instability and mental illness profoundly impact long-term health outcomes, with studies suggesting a 17.5-year reduction in life for PEH compared to the national average. Individuals with schizophrenia face a threefold decrease in life expectancy regardless of their housing status.
When PEH engage with psychiatric care, it is predominantly in acute care and inpatient settings. National surveys estimate that 34% of PEH Emergency Department (ED) admisssions are due to acute psychiatric issues, compared to 4% of ED visits in the general population. Despite the critical need for access to mental health services, outpatient psychiatric care utilization and psychiatric medication

prescription rates are lower for PEH than for the general population. Housing insecurity is a longitudinal risk factor for poor health outcomes and impacts emergency psychiatric service outcomes immediately post-discharge. A cohort study by Laliberté et al. found significantly increased hazard ratios for mental healthrelated ED and hospital readmission within 30 days post-discharge among PEH compared to patients with stable housing. Unfortunately, very few existing studies document the perspectives of PEH regarding their follow-up experiences immediately post-discharge from psychiatric acute care services.
Our study at Jackson Memorial Hospital in Miami-Dade County, Florida, aims to address this gap. We have been surveying PEH presenting to our countylevel safety-net ED about their attitudes and obstacles regarding obtaining outpatient follow-up care after discharge. The overall goal of the project is to learn from PEH perspectives and experiences
in obtaining follow-up care in the immediate post-discharge period. The patient-centered information generated from this study will help contextualize existing literature documenting low outpatient follow-up rates in the immediate period post-discharge from acute care services, informed by PEH knowledge and experiences. This information is critical, as we cannot appropriately address existing disparities in outpatient care use without insight into why rates are low to begin with.
Among those who discussed barriers to following up with outpatient psychiatric care post-discharge, the qualitative component of the survey found that the ability for PEH to adhere to medication treatment post-discharge was considerably complicated by their housing status. Participants described numerous ways in which their housing status posed direct challenges to medication retention, thus impeding their ability to adhere to treatment.
Many participants reported lacking a secure space to store their prescribed medications. Several participants described instances of medication loss and/or theft occurring either on the street or while staying in a shelter. One participant shared, “I know I need to take Keppra, but it either got stolen, I lost it, or I sold it to get my next meal.” A few participants in the study expressed relief after being prescribed long-acting injectables (LAIs), as they were no longer burdened by the issues they experienced while taking oral formulations. Another participant shared, “If it rains or gets too hot out… well, I’m getting older, so it’s hard to be on the street when it’s like that, but then also my meds would get stolen in shelters. Things are easier now, though. Just gotta get a Depot [LAI] about every two weeks.” These participant perspectives highlight some important potential benefits of LAIs on medication adherence in PEH populations.

“The patient-centered information generated from this study will help contextualize existing literature documenting low outpatient follow-up rates, informed by PEH knowledge and experiences.”
continued from Page 75
The survey also includes a section where participants can select barriers they have experienced while trying to access outpatient care from a dropdown list of suggestions. The most common answers included travel/mobility barriers, not having a phone, prohibitive copays, lack of adequate insurance coverage, medication side effects, miseducation/ lack of identification, lost insurance card, and having a bad experience in the ED. Notably, participants who were navigated to a shelter post-discharge reported significantly fewer barriers from the dropdown list on average compared to those whose shelter arrangements were not coordinated prior to discharge. This likely occurs because predischarge planning and coordination of shelter placement help mitigate barriers and facilitate care for PEH post-discharge.
It is important to acknowledge the limitations of our study. The findings are based on a small sample size and are geographically limited, which may affect the generalizability of the results. Additionally, our reliance on selfreported data introduces the potential for bias, especially when discussing the results of survey participants with severe psychiatric comorbidities, as their histories may be complicated by a low level of insight. Despite these limitations, our study provides critical insights into the perspectives of PEH regarding their experiences with postdischarge psychiatric follow-up care. These insights offer a valuable viewpoint for understanding potential risk factors for loss to follow-up in the immediate postdischarge period.
Directions
Study findings may be useful for
developing community-tailored discharge planning interventions informed by the lived experiences of PEH. Further research is necessary to build and pilot those interventions to help address systemic barriers to care. Screening for housing instability, particularly in emergency settings, and the widespread adoption of targeted screening tools, like the two-item questionnaire piloted in New York City, can significantly enhance the identification and subsequent care of unhoused patients. Our results show that follow-up barriers are reduced when PEH are discharged to shelters. Efforts should be made to support strategies that bridge patients to shelters, including funding for social work, navigation programs, and other hospital-to-shelter discharge initiatives. To those developing these initiatives, our study findings underscore the importance of seeking and incorporating patient input when forming discharge plans. Doing so will help build a robust set of strategies and more comprehensive care plans, as patient perspectives will provide detail to the complexity of real-world experiences and may uncover factors and variables not previously considered.
Conclusion
The incentive of our project is to generate preliminary materials that can be built upon to develop more comprehensive and empathetic approaches to postdischarge care for PEH. There is an urgent need in this population, and more work is necessary to help PEH access care after leaving acute care settings. This is especially true for PEH postdischarge from acute psychiatric care settings, where interventions cannot only occur at the time of crisis. Efforts must be made to facilitate continued psychiatric follow-up care post-discharge for PEH to maintain treatment adherence. Doing so will impact an individual’s health, quality of life, and acute care utilization patterns. By prioritizing patient input and addressing systemic barriers, health care providers can better support this vulnerable population, improving
both immediate and long-term health outcomes. This holistic approach is essential for fostering a more equitable and effective health care system that truly meets the needs of those experiencing homelessness and severe mental health challenges

Alana Moore is a fourth-year medical student at the University of Miami Miller School of Medicine, where she is also completing a Master of Public Health degree. As a member of her campus street medicine team, Alana initiated a research project that integrates her clinical interest in emergency medicine with her dedication to improving health access for unhoused individuals.

Orly Morgan is a fourth-year medical student at the University of Miami Miller School of Medicine, pursuing a Master of Public Health degree concurrently. Orly, an active member of the campus street medicine team, is conducting research that merges her emergency medicine interests with her commitment to enhancing healthcare access for the unhoused population.

Dr. Varshney is a medical education fellow at Emory School of Medicine. In 2024, she graduated from the Jackson Health System/University of Miami emergency medicine residency program, where she served as chief resident. During her residency, Varshney was involved in study design and implementation, and continues to assist with project data analysis and outcomes reporting.

Dr. Supino is the faculty lead and principal investigator for the research project. He holds two roles within Jackson Health System: assistant medical director of the emergency medicine department and associate director of the emergency medicine residency program.

By Al’ai Alvarez, MD and Amanda J. Deutsch, MD, on behalf of the SAEM Wellness Committee and the Stop the Stigma EM Subcommittee
In the high-stakes world of emergency medicine, the mental health of physicians often takes a backseat to patient or department needs. The emergency department epitomizes a VUCA (volatile, uncertain, complex, and ambiguous) environment where rapid decision-making under pressure is the norm. This challenging backdrop makes mental health support crucial, yet it's often overlooked. A paradigm shift is now challenging the notion that seeking mental health support signifies weakness or should only occur during crises. As we kick off #StopTheStigmaEM Month this October, it's time to reframe mental health care as an essential component of organizational culture in our specialty.
Traditionally, our approach to mental health has been reactive, with physicians often suffering in silence or seeking help only when it becomes unbearable. This not only stigmatizes mental health care but also fails to harness its potential for optimizing performance and well-being in our VUCA environment. Just as we don't wait for a cavity before visiting a dentist, we shouldn't wait for a mental health crisis before seeking support.
The Dual Mental Health Continuum is a powerful tool for understanding the spectrum of mental health states, ranging from flourishing to languishing.
This model recognizes that mental health is dynamic and separate from the spectrum of mental illness. Individuals can move along this continuum based on various factors, including workrelated stressors. By adopting this framework, our departments and institutions can create environments that support optimal functioning across the entire spectrum, even amidst the unpredictability of our specialty.
A significant challenge in our field is the prevalence of the imposter phenomenon, particularly during career transitions. Many professionals experience self-doubt and feelings of inadequacy, believing they're not as competent as others perceive them to
“Residency training places high-achieving individuals into a demanding environment marked by long work hours, sleep deprivation, and repeated exposure to traumatic events, all while expecting them to maintain high-quality performance.”
be. These feelings intensify during pivotal moments such as starting residency, becoming an attending physician, or taking on leadership roles. These isolating experiences also occur when we are involved in adverse events. The complex and ambiguous nature of emergency medicine can exacerbate these feelings. Historically, these struggles have been rarely discussed, leaving individuals to grapple with them in isolation.
Forward-thinking emergency departments can recognize that addressing these challenges is an organizational imperative, no longer just an individual responsibility. By creating supportive structures and fostering open dialogues, departments can cultivate a culture where vulnerability is seen as a strength and essential for navigating our VUCA environment.
Integrating proactive mental health care into routine operations is crucial. This could involve regular check-ins, peer support programs, or dedicated mental health days. Other ideas include incorporating self-compassion practices into daily routines or offering on-site counseling services, providing tools to manage the volatility and uncertainty inherent in emergency medicine.
Reducing stigma at an institutional level begins with leadership openly discussing mental health and demonstrating a commitment to staff well-being. It also involves creating policies that protect the privacy of those seeking help, including removing mental health-related questions from credentialing questionnaires. We're just as human as our patients, and practicing good mental hygiene should not negatively impact career progression,
In emergency medicine, the mental health of physicians is often overlooked, despite the high-pressure and unpredictable nature of their work. Traditionally reactive, mental health care must evolve towards proactive support, acknowledging that mental well-being is essential for both individual and organizational success. Addressing challenges such as the imposter phenomenon and reducing stigma are crucial steps in this transformation. By fostering an organizational culture where mental health care is integral, emergency departments can enhance job satisfaction, reduce burnout, and improve patient outcomes.
This October, during #StopTheStigmaEM Month, we call on the emergency medicine community to embed mental health support as a core component of our organizational culture. Visit our Stop the Stigma EM webpage starting October 1 for updated resources and a full calendar of events. Follow SAEM's social media channels throughout the month as we spotlight initiatives that foster education and raise awareness. Together, we can break the stigma and build stronger, more resilient teams.
especially given the demands of our specialty.
By prioritizing mental health organizationally, emergency medicine can create environments where all team members thrive personally and professionally, despite the VUCA nature of our work. This approach not only benefits individual emergency physicians but also enhances patient care by ensuring frontline staff operate at their best in highpressure situations.
Creating a culture that truly supports mental health requires ongoing effort and a willingness to evaluate and improve strategies continuously. The potential benefits — including improved job satisfaction, reduced burnout, enhanced resilience to VUCA stressors, and improved patient outcomes — make this investment worthwhile.
This #StopTheStigmaEM Month, let's commit to redefining mental health care in emergency medicine. By viewing it as an essential aspect of organizational culture rather than an individual burden, we can build stronger, more resilient departments capable of meeting the complex challenges of modern healthcare while supporting the well-being of those dedicated to helping others in times of crisis.


Dr. Alvarez is director of well-being at Stanford Emergency Medicine and chair of the SAEM Wellness Committee Stop the Stigma EM Subcommittee. @alvarezzzy
Dr. Deutsch is director of well-being at Thomas Jefferson Emergency Medicine and chair of the SAEM Wellness Committee. @amandajdeutsch

By Kyra Reed, MD and Amanda J. Deutsch, MD on behalf of the SAEM Wellness Committee
Residency training is crucial for developing habits that impact careers in the long term. It is imperative to shift the culture around mental health and cultivate proactive habits for managing it, starting in residency. During residency training, we place high-achieving, successful individuals into a demanding environment marked by long work hours, sleep deprivation, and repeated exposure to traumatic events. Despite these challenges, we expect them to maintain high-quality performance while navigating a steep learning curve in clinical settings. This environment takes a significant emotional and physical toll, with resident burnout rates alarmingly high — 76% nationwide in emergency medicine (EM).
Despite awareness of these issues, residents often navigate mental health resources independently, encountering numerous barriers, with stigma
being a major impediment. When the Indiana University School of Medicine Emergency Medicine (IUSM EM) surveyed residents about these barriers, residents expressed concerns about how seeking mental health support might affect others' perceptions of their competence and their future employment prospects. One resident shared, “I thought I would be perceived as weak or incompetent for seeking help.” Another expressed, “I was worried that seeing a counselor or being on medication would impact my future employment.” Similar concerns persist among attendings considering new positions or locations.
This stigma is unacceptable in our profession, given its tangible associated consequences. Each year, between 300 and 400 physicians die by suicide, and trainees are not exempt. Suicide is the second leading cause of death
among residents, linked to depression, emotional exhaustion, sleep deprivation, loneliness, and strained relationships — all exacerbated during residency.
EM prides itself on serving as a safety net for society, yet we fall short in providing a similar safety net for our resident trainees who are learning to navigate tremendous job stress while managing the factors contributing to it. One challenge in addressing trainee mental health needs is the current reactive framework. The common message to residents is, “If you need help, here are resources.” This phrasing can unintentionally stigmatize seeking assistance, as it may suggest that asking for help is a sign of failure or a burden. We need to change this culture to make seeking help a normal and accepted part of residency.
To address this, the Indiana University School of Medicine (IUSM) Emergency
Medicine Residency Program has implemented a pioneering wellness and mental health curriculum that normalizes mental health needs through proactive standardization starting on day one of intern year. This approach preemptively removes barriers to resources, normalizes challenging experiences during training, creates built-in support systems, and addresses inequities in the current wellness and mental health paradigm — all aimed at turning stigma on its head.
Auto-enrollment, or “opting out” is effective in increasing the use of medical and non-medical programs by making participation the default option. This approach normalizes the intervention and integrates it into standard practice. In contrast, “opting in” requires individuals to actively seek out the intervention, which can make it seem non-standard and reactive.
At IUSM EM, therapy sessions are automatically scheduled for incoming interns through the Department of Mental Health Services during their orientation month. These sessions are integrated into the orientation schedule alongside advanced trauma life support, simulation sessions, educational lectures, and other activities, helping to normalize their use. The sessions are virtual and free, eliminating financial, logistical, and confidentiality concerns. Since implementing opt-out counseling (n=63 residents), utilization rates have surged from 3% to as high as 62%, demonstrating the effectiveness of this approach. One resident noted, "Optouts made me address my anxiety and depression that I had put on the back burner for more than a decade."
Addressing concerns about stigmatizing employment application questions is also crucial. The IUSM EM Residency PD team has crafted a standardized statement advocating for the removal of such questions from credentialing forms. This proactive measure empowers residents to seek care without fearing professional repercussions. Residents are informed that if an employer asks about mental health on credential forms, they will receive the following statement. This statement aims to protect residents who use mental health resources, alleviate fears about future hiring, and educate employers about the negative impact of stigmatizing questions and the need for supportive changes.
At SAEM, we recognize that wellness is critical to the success of medical leadership, impacting patient care, clinician health, and trainee education. Fulfilled clinicians are more motivated, compassionate, and dedicated, leading to improved team performance. From a business standpoint, addressing wellness can reduce costly turnover and enhance productivity. A culture focused on wellbeing fosters lower attrition rates, greater clinical and academic output, and overall institutional efficiency. Investing in wellbeing ensures a stable, efficient, and innovative healthcare organization, supporting long-term sustainability and success.
Just in time for Stop the Stigma EM Month, we are excited to introduce the SAEM Well-Being Consultation Program, designed to enhance the well-being of emergency medicine professionals and their departments. This program offers tailored support and practical solutions rooted in proven well-being frameworks.
Key Focus Areas Include:
• Incorporation of national well-being frameworks
• Workload management
• Workplace environment
• Engagement incentivization
• Leadership collaboration
• Mentorship and advising
• Departmental policies and practices
Leverage the expertise of SAEM’s accomplished committee and academy members to develop, evaluate, and improve your department’s practices. Our consultations aim to provide valuable insights and strategies to foster a thriving, resilient, and effective emergency medicine environment.
For more information or to schedule a consultation, please contact us at ConsultationServices@saem.org.
IUSM EM Program Director Team Statement To Employers:
"The IUSM EM residency program integrates preventative mental health counseling and peer support sessions into our curriculum for ALL residents. Standardization of mental health resource utilization is a preventative strategy aimed to improve overall well-being and to reduce stigma that often creates barriers to seeking care prior to a mental health crisis. IU Health Physicians has removed questions related to mental health on employment applications because such inquiries potentially prevent physicians from seeking care that ultimately promotes positive coping skills, deepens empathy, and improves resilience. These are all viewed as assets in the physicians we train at IUSM EM. We encourage your leadership to consider removing or editing this question for the same reasons."
Bottom line: it is time for our specialty to extend the same safety net of care and support to our resident trainees and colleagues as we provide to the communities we serve. By standardizing mental health support, adopting proactive measures, and advocating for systemic changes, we can pave the way for healthy and fulfilling careers for all.


Dr. Reed is assistant program director of the Indiana University School of Medicine Emergency Medicine Residency. Twitter: @silver_liningKR, @IUSM_EM Instagram: @iusm_em
Dr. Deutsch is director of well-being at Thomas Jefferson Emergency Medicine and chair of the SAEM Wellness Committee. @amandajdeutsch

By Ronny Otero, MD; Peter Hou, MD; and Michael Gottlieb on behalf of the SAEM Bylaws Committee
Published in the European Journal of Emergency Medicine (2022; 29: 389-390), the SAEM-supported Policy Statement on Minimal Standards for Safe Working Conditions in Emergency Medicine outlines essential conditions for which emergency physicians should advocate. As members of the Society for Academic Emergency Medicine (SAEM), it is vital to stay informed and proactive in supporting these standards to ensure the safety, wellbeing, and efficiency of our emergency departments (EDs).
Key Components of the Policy Statement
Adequate Number of Staff: Ensuring that there is an adequate number of physicians, nurses, paramedics, and other essential staff is fundamental to providing high-quality patient
care. Overburdened staff can lead to errors, increased stress, and burnout, compromising patient safety and care quality.
Adequate Competence of Staff: Staff should be adequately trained and competent in their respective roles. Continuous professional development and training programs are vital to maintaining high standards of care and adapt to the evolving medical landscape.
Adequate Recognition from Other Specialists: Emergency physicians should receive appropriate recognition and support from other medical specialists. Collaboration and mutual respect among health care professionals enhance patient outcomes and foster a positive working environment.
Adequate Contingency System and Organizational Plan: In the event of a mass casualty incident, a well-designed contingency plan is essential. This includes having a clear organizational structure and protocols to manage such crises efficiently.
Adequate Design of Working Hours: Working hours should be designed to minimize fatigue and burnout. Shift schedules should consider the physical and mental well-being of the staff, promoting life balance and reducing the risk of errors.
Adequate Physical Design of the ED: The physical layout of the ED should facilitate efficient workflow and patient care. This includes having sufficient space, appropriate equipment, and a design that supports both staff and patient needs.

Adequate Equipment: Ensuring that the ED is equipped with the necessary tools and technology is crucial for effective patient care. This includes everything from medical instruments to advanced diagnostic equipment.
Adequate Supporting Infrastructures: Supporting infrastructures, including information technology systems, are vital in reducing administrative and bureaucratic burdens. Efficient IT systems can streamline processes, allowing health care professionals to focus more on patient care. Health systems should support robust cybersecurity systems to protect patient’s personal information and health.
Adequate Space for Rest and Refreshment: Providing adequate space for staff to rest and refresh during shifts is important for maintaining their well-being. Breaks are essential for reducing stress and preventing burnout.
SAVE THE DATE!
Join us on Wednesday, October 16, 2024 for an SAEM Bylaws Webinar. Learn about the work and duties of the SAEM Bylaws Committee and consider self-nominating or nominating a peer for a position on the Bylaws Committee. Register today!
With Babies: Facilities should be available to support professionals with young children, such as spaces for breastfeeding and pumping. This promotes a family-friendly work environment and supports the retention of valuable staff.
Adequate Equal Opportunity Hospital Policies: Hospitals should have policies that promote equal opportunities and do not discriminate based on race, religion, or sex. A respectful and inclusive work environment is fundamental to staff morale and patient care.
Adequate Psychological and Emotional Support: Providing psychological and emotional support to health care professionals is critical. This includes access to counseling services and stress management programs to help staff cope with the demanding nature of their work.
While SAEM supported this policy statement in 2022, many issues addressed remain pressing. The high level of burnout within our specialty underscores the need for continued advocacy and implementation of these standards. By promoting these conditions, we can enhance the safety, effectiveness, and sustainability of emergency medicine.
As SAEM members, staying informed about these policies and advocating for their adoption in our workplaces is crucial. By doing so, we support our colleagues, patients, and the future of our specialty.

Dr. Otero is the Vice-Chair for Clinical Operations for Froedtert & Medical College of Wisconsin Department of Emergency Medicine. His role is to oversee eight emergency departments throughout the enterprise. He is involved in strategic initiatives related to Emergency care and improving the interface of admissions into the health system. He is also the Director of the Health Executive and Administrative Leadership (HEAL) Fellowship for MCW Emergency Medicine.

Dr. Hou is assistant professor of emergency medicine at Harvard Medical School and an emergency physician and critical care specialist practicing in both the emergency department and surgical and mixed intensive care units at Brigham and Women’s Hospital. He currently serves SAEM on the Bylaws Committee, Research Committee, Workforce Committee, SAEM Telehealth, Informatics, Data Science, and Artificial Intelligence Interest Group, Critical Care Interest Group, and as a member of the SAEM Academy for Diversity and Inclusion in Emergency Medicine.

Dr. Gottlieb is the vice chair of research, ultrasound division director, and a professor of emergency medicine at Rush University Medical Center. He also currently serves as the director of learner assessment and program evaluation for the SAEM ARMED MedEd Program and a member of the SAEM Bylaws Committee. He is a nationally recognized speaker, educator, and researcher.

By Shivam Shah, MD, MS
As emergency department wait times continue to make headlines, patients are increasingly utilizing telehealth for their care. Although telehealth saw a surge during the COVID-19 pandemic, it has been around for decades. Innovations in technology have expanded the realm of asynchronous care. Growing in popularity, asynchronous care, or "store-and-forward" care, is a form of telemedicine where health information is captured by the patient and transmitted to a provider who renders care without real-time interaction.
Asynchronous care offers numerous benefits. Patients can access care conveniently on their own time, avoiding the need to miss work or attend a clinic
“Patients can access care conveniently on their own time, avoiding the need to miss work or attend a clinic appointment.”
appointment. Besides convenience and geographic benefits, wait times are reduced as most asynchronous care visits are completed quickly. Additionally, asynchronous care often incurs lower costs compared to many in-person visits. For providers, asynchronous care visits are much quicker since all the information is provided at once. According to the Department of Health and Human Services, most
asynchronous care visits take about three to five minutes. Providers also have greater flexibility to complete asynchronous visits—whether before a shift, from home, or during clinical time. With these advantages, it is no surprise that asynchronous care is growing in popularity among both patients and providers.
However, challenges arise when a complaint is too severe for an

“Since the differential diagnosis for eye pain is broad and serious conditions may cause lasting harm if not addressed promptly, it is crucial to track these patients and ensure timely care.”
asynchronous visit or when red flag symptoms appear in a seemingly benign chief complaint, such as "eye pain." Many companies offering asynchronous care products will advise patients to see their primary care provider or go to the emergency department. However, it is unclear how many patients follow these recommendations. Since the differential diagnosis for eye pain is broad and serious conditions may cause lasting harm if not addressed promptly, it is crucial to track these patients and ensure timely care. One solution is for health systems to manage asynchronous care directly.
By creating an in-house asynchronous platform or integrating a third-party product, health systems can innovate across their entire health care delivery system. Patients can receive asynchronous care through their health system’s app or an EMR patient portal.
These records remain within the health system, providing the patient’s primary care provider and specialists with essential information. If a complaint is concerning or if the patient reports red flags symptoms, the visit can be automatically converted to a video visit within the system. Additionally, if there is significant concern, the provider can recommend that the patient visit an emergency department, ideally within the same system. By flagging asynchronous visits in the electronic health record (HER), emergency department providers will have additional information about the patient, and primary care providers and specialists can follow up after the emergency visit. The benefits are manifold: health systems can extend their care throughout the patient’s health continuum, from wellness to illness. Treating providers will have quick access to a patient’s medical chart for a quick and comprehensive view of the patient’s
health. Patients will receive consistent, high-quality care from a trusted source.
As asynchronous care continues to gain traction, health systems are ideally positioned to lead the next generation of health care delivery. By leveraging their infrastructure and integrating new technologies, they can ensure that patients receive seamless, coordinated care, while also driving innovation and efficiency in the health care system.

Dr. Shah is a fourth-year emergency medicine resident at Mount Sinai Hospital in New York City. He is passionate about increasing access to care through digital health and innovation. Follow him on Twitter @ShivamSShah

By Tony Fabiano, MD
When starting residency, many believe they have a clear career path, only to realize halfway through that traditional routes may not be the best fit. For those, like me, who find full-time community practice or conventional academic fellowships aren’t the right match, exploring alternative options can be challenging. Opting for a telehealth fellowship might be the answer. I opted for a telehealth fellowship, not to shift to full-time telemedicine, but to influence the future of health care. This decision was about more than just diversifying my skill set; it was about positioning
myself at the forefront of a significant transformation in medicine. For those contemplating their next steps, here’s why this path is worth exploring.
Fellowships can be crucial in achieving both career and personal goals. For me, a telehealth fellowship has provided the chance to master virtual care nuances and understand its integration into hospital systems and the broader U.S. health care landscape. It has allowed me to establish myself as a leader in this evolving field while developing administrative skills — from project selection and vendor contracting to managing large-scale telehealth
programs. This choice has enhanced my job market competitiveness, ensured career and income flexibility, and helped me build relationships with industry leaders.
Telehealth represents the future of health care, yet it’s not always top of mind for emergency physicians. This innovative model is poised to disrupt traditional health care delivery and is already affecting emergency medicine. Gaining expertise in telehealth not only mitigates career risk but also positions one to shape the future of the specialty, stay at the cutting edge of change, and embrace leadership challenges and

“Opting for a telehealth fellowship might be the answer. I opted for a telehealth fellowship, not to shift to full-time telemedicine, but to influence the future of health care.”
rewards. Telehealth is high-tech, fastpaced, and involves systems thinking. It offers opportunities for both independent and collaborative problem-solving on various scales. Systemically, it improves access to care, reduces costs, enhances health outcomes, and helps alleviate provider burnout.
The flexibility offered by telehealth can mean fewer emergency department hours, though it doesn’t replace that work. After intense shifts in the resuscitation bay, it can be refreshing to handle low-acuity calls from home. Telehealth skills are locationagnostic and applicable across different practice environments, providing job and income flexibility. As administrative skills are developed, there are opportunities to influence hospital systems or explore entrepreneurship, consulting, or medical directorships. Importantly, one can retain their identity as an emergency physician while exploring new opportunities or transitioning as desired.
Emergency physicians are wellsuited to lead in the telehealth domain. Our adaptability, innovative mindset, and comfort with uncertainty make us ideal candidates for shaping this field. Telehealth offers a chance to extend expertise beyond the emergency department, proactively address health care access, and shape a more efficient and equitable system. A telehealth fellowship is not just about practicing medicine virtually; it’s about understanding and implementing virtual care within hospital systems and the broader health care landscape. It provides experience in working with vendors, navigating projects, and managing large-scale telehealth operations. These experiences prepare one to lead at the health system level or pursue entrepreneurial ventures, creating both career and life flexibility.
For those interested in exploring this path, reaching out via email could be
the first step. Engaging in conversations with those who have taken this path can provide deeper insights into how it might align with personal career goals and aspirations. If this sounds like a journey you want to embark on, don’t hesitate to reach out via email. Together, we can advance patient care, improve health outcomes, and shape the future of emergency medicine.

Dr. Fabiano is a telehealth fellow at Jefferson Health in Philadelphia and a recent graduate of the University of Cincinnati emergency medicine residency. He is passionate about leveraging telehealth to drive innovations in patient care. You may contact him at tonyfabianomd@gmail.com

By Helena Kons, MD; Jessica Rivera Pescatore, PharmD; Stacy Marshall, MD; and Sukhshant Kaur Atti (Sukhi), MD
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are approved by the Food and Drug Administration (FDA) for treating type 2 diabetes mellitus. They work by activating pancreatic GLP-1 receptors, which stimulates glucose-dependent insulin release. Recently, the use of GLP-1 RAs has expanded due to their additional benefits such as cardioprotection, stroke reduction, and prevention of chronic kidney disease progression, especially in individuals with obesity. Beyond their role in managing obesity, there has been a surge in the use of injectable GLP-1 RA preparations for routine weight loss, driven by
sensationalized testimonials. Several of these drugs have recently received FDA approval specifically for weight loss. Consequently, prescriptions for GLP-1 RAs have skyrocketed over the past decade. A recent infodemiolgocial study reported a 221% increase in GLP-1 RA prescriptions from January 2016 to December 2021. As the demand for agents like semaglutide (Ozempic, Wegovy), liraglutide (Saxenda), exenatide (Byetta), and tirzepatide (Mounjaro) has grown, supply has struggled to keep up, leading to national shortages. These shortages have led to an emergence of compounded products, further
contributing to therapeutic errors due to varying concentrations, multi-dose preparations, and instructions or education on proper use The rise in therapeutic use and related errors has led to increased calls to poison centers and visits to emergency departments (EDs) nationwide. Between January 2017 and December 202, U.S. poison centers reported over 5,700 singlesubstance exposures to GLP-1 RAs. While most cases had minimal effects requiring no medical treatment, many patients presented to the ED, and a small number required hospitalization.
Despite the increase in exposures, often from supratherapeutic dosing,
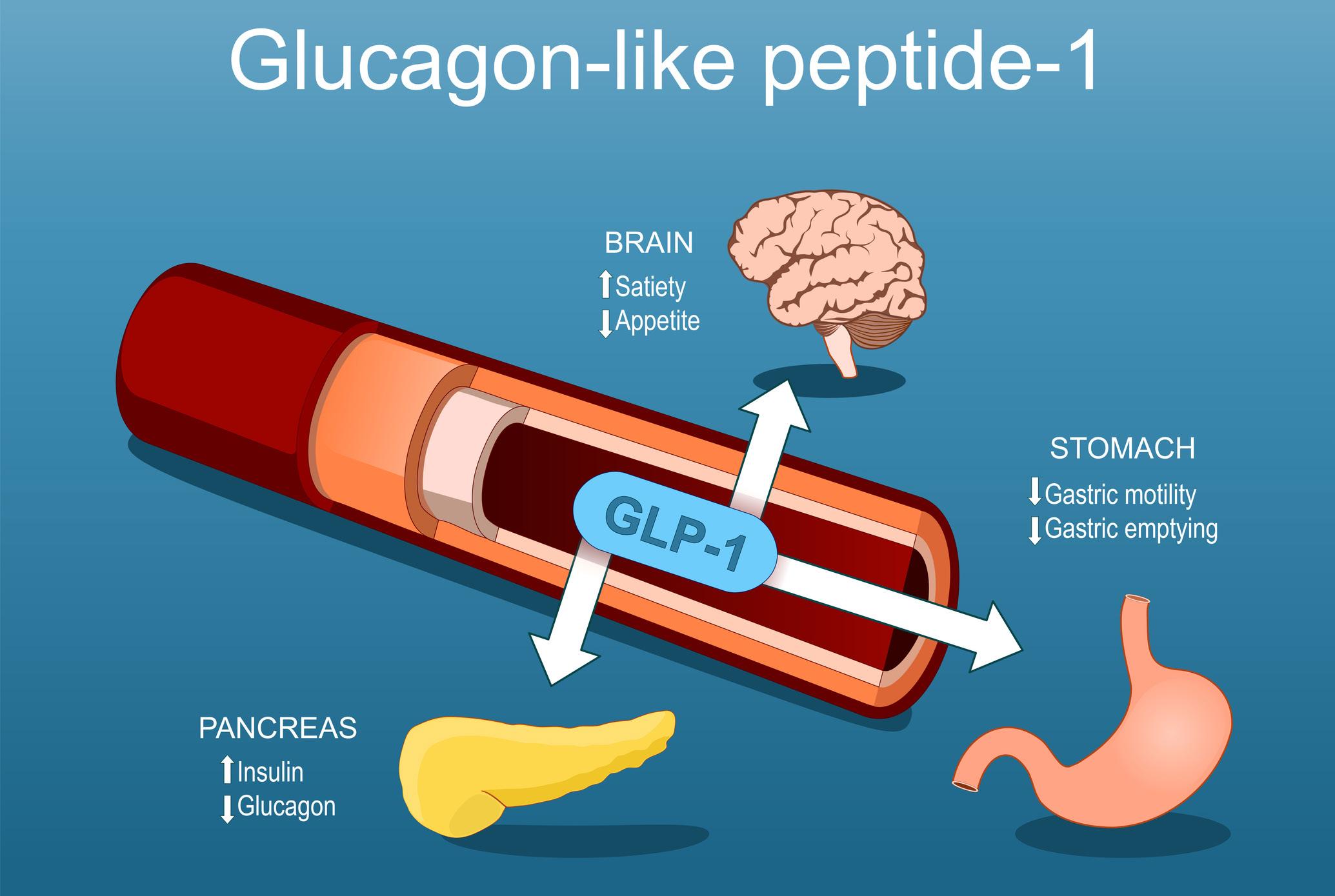
“Despite the increase in exposures, often from supratherapeutic dosing, there is limited information available to emergency physicians regarding triage, management, and disposition strategies.”
there is limited information available to emergency physicians regarding triage, management, and disposition strategies. The current situation is further complicated by the lack of information on adverse effects beyond clinical trials and the pharmacokinetic properties that can affect exposures.
One mechanism behind GLP-1 RA efficacy in weight loss is their ability to slow gastric emptying, which can cause early satiety. As a result, many patients experience nausea and vomiting, leading some to discontinue use when symptoms become intolerable. Slowed gastric emptying may also affect the absorption and bioavailability of other medications, particularly those with extended-release
mechanisms. Additionally, the elimination half-lives of GLP-1 RA medications vary significantly, ranging from two hours to one week, leading to prolonged effects and persistent symptoms (see Table 1). Many GLP-1 RAs exhibit extensive protein binding, creating the potential for drug interactions through displacement from plasma proteins. Be aware of potential drug interactions in patients taking medications with narrow therapeutic indices if they show signs or symptoms of toxicity.
A recent study from a single poison center indicates that most exposures to GLP-1 RAs resulted from therapeutic
errors. Common issues include patients taking doses too early, due to perceived pen malfunctions, confusion about daily versus weekly administration, incorrect amounts drawn from multidose vials, or forgetting previous doses.
As with all clinical assessments, evaluating a patient with potential GLP-1 RA toxicity in the ED starts with a comprehensive history and physical examination. Key information includes the exact product involved, details about the injectable device (single-use pen, multidose pen or vial, syringe size, amount withdrawn,
continued on Page 90

TOXICOLOGY
continued from Page 89
compounded or commercial product, concentration, dose administered), and any concomitant use of antidiabetic or hypoglycemic agents.
Gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal pain are common, even with therapeutic doses. More severe presentations, like gastroparesis, bowel obstruction, or stercoral colitis, may occur and should be considered in the evaluation. A thorough abdominal examination can help determine if further evaluation for intra-abdominal pathology is needed.
Laboratory assessments should include point-of-care glucose, a basic metabolic panel, and a complete blood count. Depending on the patient’s condition — such as extensive comorbidities, abdominal tenderness, or persistent nausea and vomiting — additional tests like a hepatic function panel, serum lipase level, and abdominal
“Gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal pain are common, even with therapeutic doses.”
imaging (e.g., computed tomography) may be warranted.
It is important to include GLP-1 RA use in the differential diagnosis for intractable abdominal pain or persistent nausea and vomiting. Supportive care with intravenous fluids (IVF), antiemetic therapy, and possibly dopamine antagonists, like metoclopramide or droperidol, to enhance gastric emptying and motility, is reasonable.
Gastrointestinal fluid losses from persistent vomiting and/or diarrhea can lead to prerenal acute kidney injury. For patients experiencing severe acute kidney injury, signs of dehydration, or an inability to tolerate oral intake, inpatient admission may be necessary.
While the risk of pancreatitis in GLP1 RA toxicity is not well established, there have been isolated case reports linking GLP-1 RAs to pancreatitis. This has led to an FDA black box warning for necrotizing and hemorrhagic pancreatitis, particularly associated with exenatide.
Severe hypoglycemia (blood sugar less than 56mg/dL per clinical trials) secondary to GLP-1 RA administration alone is extremely rare, even in large overdoses. A recent study by Marshall et al, based on a single poison center’s experience, reported a low incidence of hypoglycemia associated ith GLP-1 Ras. In cases of therapeutic errors, the likelihood of hypoglycemia developing is low. However, the risk of
severe hypoglycemia increases when patients are also taking insulin or other hypoglycemic agents for diabetes management. It is advisable to admit for observation patients who have overdosed on GLP-1 RAs and are concurrently taking hypoglycemics, such as insulin or sulfonylureas. In such cases, dextrose supplementation may be provided as needed, along with food, if tolerated.
For patients who experience unintentional exposures due to therapeutic errors and are not taking other hypoglycemic medications, discharge from the ED should be considered if their laboratory results and physical examination are reassuring, gastrointestinal symptoms are well controlled, and they can tolerate oral intake. However, even if initial symptoms are managed in the ED and the patient appears stable, they should be informed that symptoms may persist for several days depending on the specific agent involved. Patients should be instructed to return to the ED if they experience worsening symptoms, such as severe abdominal pain, persistent nausea or vomiting, inability to tolerate oral intake, hypoglycemia, altered mental status, extreme lethargy, or signs of dehydration. All exposures should be reported to your local poison center by calling 1-800-222-1222. Poison centers are available 24/7, 365 days a year, to provide accurate and timely information on common exposures, including those involving GLP-1 RAs. They can support emergency physicians by offering important details on history,
product differentiation, pharmacokinetic properties, triage, risk assessment, management, and disposition strategies. Additionally, poison centers are uniquely equipped to provide follow-up calls to patients. If a patient is deemed appropriate for ED discharge and agrees to poison center follow-up, emergency medicine providers can collaborate with poison center staff to arrange routine check-ins over several days. This helps monitor symptom progression and ensures patients return to the ED if necessary. Many poison center protocols include follow-up for GLP-1 RA exposures over 48-72 hours due to the anticipated prolonged effects.

Dr. Kons is a second-year emergency medicine resident at the University of Alabama at Birmingham. She is a graduate of the Anne Burnett School of

When managing a patient exposed to an injectable GLP-1 RA in your ED, keep these key points in mind:
1. Obtain a thorough history, including detailed information about the patient’s medications.
2. The risk of severe hypoglycemia (glucose < 56 mg/dL) is low with single-substance therapeutic errors and is rarely reported, even with large overdoses.
3. Gastrointestinal symptoms are common and may persist for several days.
4. Contact your local poison center at 1-800-222-1222. Collaborate with them to establish post-ED follow-up for patients suitable for discharge.
Dr. Rivera Pescatore is the clinical director of the Alabama Poison Information Center and an assistant professor of emergency medicine at the University of Alabama at Birmingham. Her research and clinical interests include snake envenomation and antidote stewardship.

Dr. Marshall is an assistant professor of emergency medicine at the University of Alabama at Birmingham and a medical toxicologist for the Alabama Poison Information Center. Her interests include substance use in adolescents, identification of novel drugs of abuse, and research using poison center-based data.

Dr. Atti is an assistant professor who practices emergency medicine and medical toxicology at the University of Alabama at Birmingham. She works with the emergency medicine residency and medical toxicology programs at UAB, along with the Alabama Poison Information Center. Her research and clinical interests include

By Aaron Oates, MD
On the early morning of Aug. 21, 2013, missiles struck the suburban area of Ghouta, Syria. Located northeast of the capital, Damascus, the area had already faced severe food and medical shortages due to the ongoing war. Missiles first hit the eastern part of Ghouta at approximately 3 a.m. local time. Two hours later, a second, nearly identical attack occurred in western Ghouta.
It was immediately apparent that the weapons used were chemical. Hundreds of civilians began experiencing similar symptoms: eye irritation, vomiting, diarrhea, hallucinations, altered mental status, and significant airway secretions. Social media videos showed dead and dying
livestock, as well as symptomatic civilians. People sought refuge on rooftops to escape the nerve agent, but to little effect. Already overwhelmed by the ongoing warfare, makeshift hospitals in the region were ill-prepared for the influx of patients. Hundreds of men, women, and children died from sarin exposure. According to Ameenah Sawaan, a volunteer and eyewitness, the medical response was largely ineffective in preventing severe toxicity and death. Reports indicated inadequate airway equipment and few medical personnel trained in airway management. Atropine, a medication used to treat sarin exposure, was not available in sufficient quantities and was used intermittently as a last resort for patients in critical condition. Decontamination efforts included removing clothing and hosing patients
down with water. However, due to the large number of victims and limited resources, these efforts were not standardized. First responders and volunteers also lacked adequate personal protective equipment and began experiencing symptoms themselves.
In the days and weeks following the attack, a chemical weapons watchdog identified sarin, also known as GB, as the deployed weapon. Sarin was originally developed by German scientists in the 1930s and received its GB designation from the North Atlantic Treaty Organization (NATO).
Sarin acts by irreversibly binding to acetylcholinesterase, an enzyme responsible for breaking down acetylcholine. This inhibits acetylcholine

metabolism, leading to a buildup of acetylcholine in the synapse and resulting in cholinergic excess. Unregulated acetylcholine activation of both nicotinic and muscarinic receptors results in a rapid acute cholinergic crisis.
Acetylcholine-sensitive receptors are widespread and control the release of secretions and neurological functions. The acronym DUMBBBELLS describes the physiological effects of muscarinic receptor overactivation: diarrhea, urination, miosis, bronchospasm, bradycardia, bronchorrhea, lacrimation, lethargy, sweating, and salivation. Nicotinic effects may also be observed, including mydriasis, tachycardia, weakness, hypertension, and fasciculations. These symptoms can be paradoxical to muscarinic signs, complicating clinical assessment. Medical teaching traditionally emphasizes muscarinic signs due to their greater life-threatening potential. The most dangerous signs, known as the "killer B’s," are bradycardia, bronchospasm, and bronchorrhea. Reports from Ghouta indicated the presence of these symptoms in victims.
Chemical attacks in resource-limited areas pose significant challenges, as many guidelines are not feasible in these settings. According to the Centers for Disease Control and Prevention (CDC), during nerve agent mass casualty events, airway, breathing, circulation, and decontamination (ABCD) should be addressed first. In both hospital and prehospital settings, patients should undergo a rapid primary assessment of
“Hundreds of civilians began experiencing similar symptoms: eye irritation, vomiting, diarrhea, hallucinations, altered mental status, and significant airway secretions.”
their airway, breathing, and circulation. Additionally, decontamination should involve the removal of all clothing and thorough full-body washing with soap and water, conducted concurrently with the primary survey. Proper personal protective equipment (PPE) for staff and decontamination of individuals is critical. The CDC recommends Level C PPE, including air-purifying respirators, nitrile or butyl gloves, chemical-resistant clothing, and eye protection. Such equipment was scarce during the 2013 attack.
Atropine, a reversible muscarinic receptor antagonist, can be administered intramuscularly every 5 to 10 minutes, with doses up to 6 mg in adults with severe symptoms. Children and infants may receive atropine in smaller, weight-based doses. Atropine works by competitively binding to muscarinic receptors, displacing excessive acetylcholine and mitigating its effects. It should be administered repeatedly until airway secretions are reduced and the patient is breathing comfortably or can be ventilated without resistance.
Pralidoxime (2-PAM), a secondary agent, may also be used. While 2-PAM is recommended in the U.S. for sarin and organophosphate exposure, its efficacy lacks international consensus. 2-PAM directly blocks the cholinesterase inhibitor, such as sarin, from binding, allowing acetylcholinesterase to resume its normal function.
In addition to atropine and pralidoxime, benzodiazepines are recommended for treating seizures resulting from sarin gas and organophosphate exposure.
The U.S. State Department estimates that up to 1,400 people died as a result of the attack. This event has been described as the most significant confirmed use of chemical weapons since 1988. The attack prompted international reactions, with various organizations attributing responsibility to the Syrian government
under President Assad. In response, the Syrian government agreed in September 2013 to dismantle its chemical weapons program to avert potential military intervention. The United Nations later classified this dismantling as incomplete because it did not include all potential chemical agents, such as chlorine gas. In 2017, another sarin gas attack occurred in Khan Shaykhun, leading to U.S. military action targeting the Shayrat airbase, which was believed to be the source of the attack.
The immense loss of life from these attacks underscores the destructive nature of nerve agents. The deployment of such weapons in underresourced areas contributed to the high casualty rate. Ensuring these weapons are never used again and preparing for similar disasters is critical. Future preparations must also account for resource-limited areas and their capabilities. As seen in this attack, nerve agent deployment in conflict zones poses a significant challenge for managing large numbers of patients.
The long-term effects of sarin exposure remain unknown. Like other organophosphates, sarin is lipophilic and can cross the blood-brain and placental barriers, potentially leading to neurological and reproductive consequences. For the thousands directly affected and their families, the attack has left an indelible mark. As a medical community, we must strive not only to prepare for such attacks but also to work toward preventing them.

Dr. Oates is a second-year emergency medicine resident at Baylor College of Medicine in Houston, Texas. A double Bison, Oates earned both a Bachelor of Science in biology with a chemistry minor and his medical degree at Howard University in Washington, D.C.
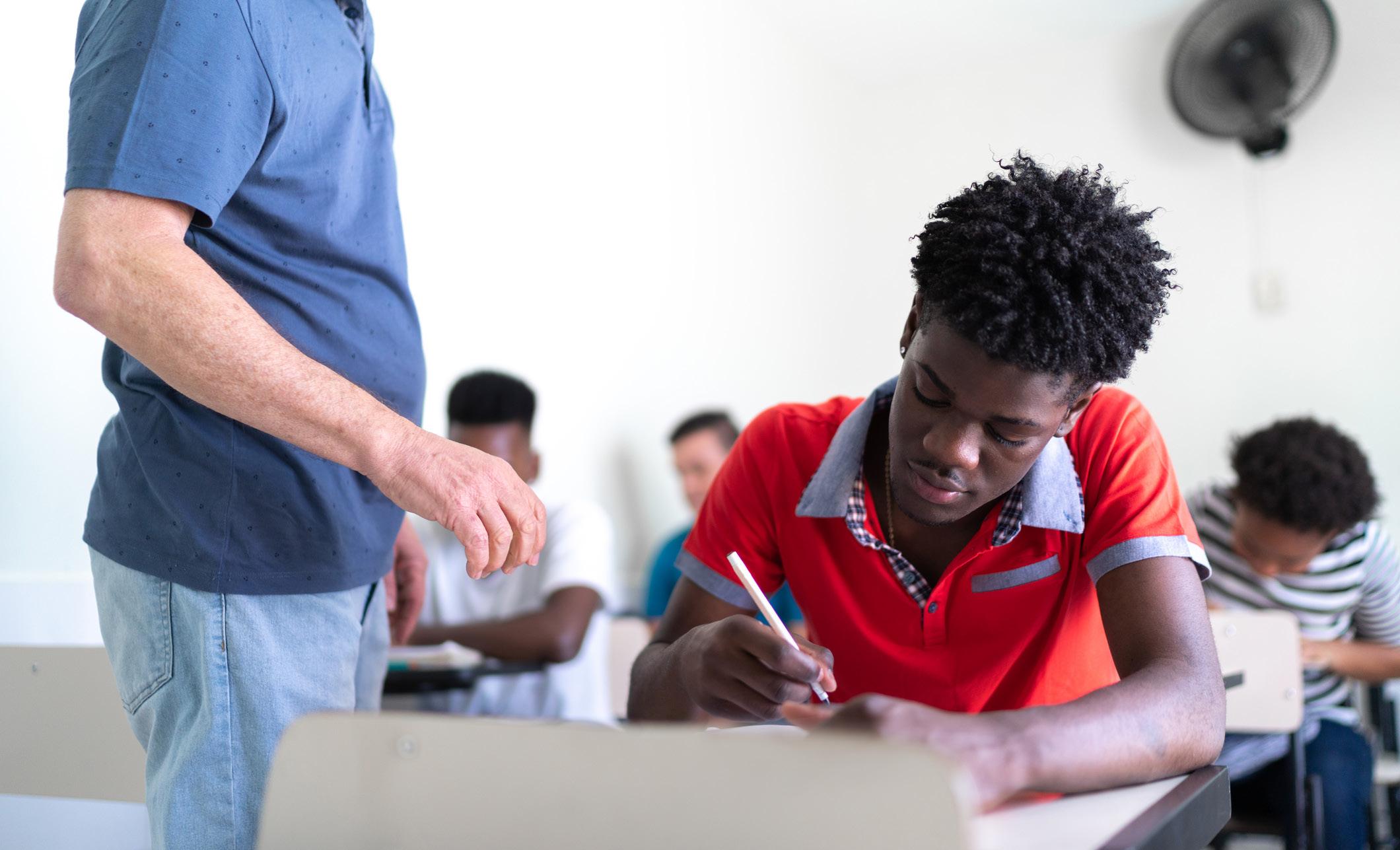
By Ashlea Winfield, MD, MSPH, on behalf of the SAEM Academy for Diversity and Inclusion in Emergency Medicine
Meritocracy is based on the idea that success in life is determined solely by effort and ability. Those who struggle do so because they do not work hard enough or are not smart enough. Admission to medical schools and residency programs should be based solely on merit, as this is considered the fairest approach. However, many argue that meritocracy is a myth or that we need to redefine what we mean by merit, reexamining the factors that demonstrate "fit" for a career in medicine. This article aims to highlight how one of the most cherished measures of merit, standardized testing, is rooted in racist practices that widen the racial achievement gap.
What if I told you that standardized testing is rooted in eugenics?
Carl Brigham, a eugenicist and psychologist, developed the first standardized tests to measure intelligence for the U.S. Army during World War I. Although he later reversed his views on eugenics, his initial theories posited that races could be ranked based on innate intelligence. His overarching goal was to prevent the decline of the education system due to the intermingling of races. He subsequently developed the SAT using the same race-based intelligence testing practices. The SAT and many of these practices formed the basis for many standardized tests used today.
The reality is that the racial achievement gap in standardized testing, including the MCAT, NBMEs, and USMLE exams, is well-documented. Underrepresented minorities (URiMs) consistently report worse scores than their white counterparts. Although the transition to pass/fail testing for Step 1 has occurred, underrepresented minorities continue to account for more than 50% of failures. Given that standardized exams are rooted in stratifying intelligence along racial lines, it is unsurprising that underrepresented minorities do not perform as well. These tests are doing what they were originally intended to do: excluding ethnic and racial minority groups.
“Given that standardized exams are rooted in stratifying intelligence along racial lines, it is unsurprising that underrepresented minorities do not perform as well.”
In medicine, we seem to cling to standardized testing as a fair measure of intelligence, using it to quickly screen the numerous applications we receive each year, despite the fact that the exams have been known for decades to carry a clear bias against minoritized candidates and are closely linked to parental resources and income. If we are serious about improving representation of marginalized groups in medicine, we cannot continue to uphold a system that is both rooted in and perpetuates racist practices. Any refusal to move away from reliance on standardized testing directly
acknowledges that we value a system rooted in eugenics more than we care about advancing diversity and equity in medicine. The notion that we have no alternative methods for evaluating candidates is false. Convenience and tradition should not outweigh the imperative of eliminating racism from our evaluative systems.
The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policies, positions, opinions, or views of the Society for Academic Emergency Medicine or its members.

Dr. Winfield is an assistant professor of emergency medicine and associate director of the Cook County Health Simulation Center in Chicago where she leads simulation-based education, emphasizing procedural competency and diversity. She completed her residency at Cook County Health, where she served as chief resident and received the Robert Simon Leadership Award. In 2022, she was named Cook County Health Physician of the Year and recognized in the National Minority Quality Forum’s 40 under 40. Dedicated to increasing diversity in medicine, she has developed initiatives and lectures on topics including gender-expansive care, traumainformed care, and implicit bias. She serves on the executive committee of the SAEM Academy for Diversity and Inclusion in Emergency Medicine.

By Melissa Fornagiel
In early 2022, USMLE Step 1 transitioned from a numerical three-digit score to a pass/fail model. According to the National Board of Medical Examiners (NBME), this change was designed to reduce student stress, enhance well-being, and foster a more holistic and diverse residency application review.
Reactions from the medical community have been mixed, and ongoing uncertainty remains regarding the impact on undergraduate medical education. Two years later, how has the pass/fail Step 1 altered the medical school experience for emergency medicine (EM) hopefuls, and how does it affect the recruitment of diverse EM residency candidates?
Proponents argue that a pass/fail model allows students to shift their focus from memorizing extraneous details irrelevant to clinical medicine to pursuing passion projects and clinical interests. A 2021 study notes that students underrepresented in medicine (URiM) specifically favor the change because it promotes a holistic residency application review, addressing inequities in standardized testing.
This change may be particularly beneficial for emergency medicine, where dedicated rotations are often only offered close to the residency application deadline, deterring many from applying to the specialty. The reduced pressure to excel on Step 1 should free up time for students to gain earlier exposure to EM. Given that EM has lower rates of racially diverse
physicians compared to many other specialties, this change has the potential to attract more URiM applicants. Additionally, Step 2, which remains graded, continues to evaluate clinical knowledge.
Historically, Step 1 scores were used by residency programs to screen candidates. Poor scores often precluded students from competitive specialties or programs within a specialty. However, Step 1 scores, like many standardized tests, are not as objective as they may seem, as they are affected by underlying socioeconomic disparities, such as the ability to afford expensive preparatory materials. Due to these arbitrary cutoffs, a 2001 study found that Black students were 3 to 6 times less likely to be offered a residency interview compared to other students.
“Proponents argue that a Pass/Fail model allows students to shift their focus from memorizing extraneous details irrelevant to clinical medicine to pursuing passion projects and clinical interests.”
Critics of binary Step 1 scoring argue that de-emphasizing standardized test scores creates uncertainty among students and may perpetuate the very disparities it aimed to address. Since the transition, overall national Step 1 pass rates among U.S. medical students have decreased from 97% in 2020 to 90% in 2023, disproportionately affecting URiM students who, on average, score lower due to inequities in standardized testing.
While the transition has undoubtedly reduced the stress of studying for Step 1, this stress may shift to how students perceive other aspects of their application will be weighted, such as Step 2 and extracurricular activities. Many worry that an even heavier emphasis will be placed on Step 2 to determine residency outcomes and that it will simply replace Step 1 as a screening tool. Since Step 2 is taken late in the third year, students may have only a limited timeframe to gauge their competitiveness for programs before application season.
Another concern is that “holistic” application reviews that value extracurricular experiences may inherently favor students from well-connected backgrounds, such as those with parents in medicine, from well-resourced high schools or colleges, or attending more prestigious medical schools. This has farreaching implications, as the same wellconnected students holding prestigious research positions are also most likely to pass Step 1 due to broader access to resources. In this way, the pass/fail model addresses only one link in the chain of a broader systemic issue: one that begins with a student’s socioeconomic status and geography, which impacts undergraduate college acceptances, MCAT scores, medical school prestige, strength of extracurricular activities, and ultimately Step 1 and 2 scores. While the pass/fail model is a step in the right direction, residency directors must ensure that new metrics used as substitutes for scores are truly holistic and inclusive,
taking into account all aspects of students’ backgrounds.
The shift to pass/fail may incentivize students to study just enough to pass Step 1 and dedicate more time to enhancing their CVs through shadowing, research, and other extracurricular activities. Unfortunately, this may inadvertently shift the stress from Step 1 studying to an added pressure to build strong extracurricular activities. For URiM candidates, who are more likely to struggle with imposter syndrome, this adds pressure to work even harder compared to peers to prove their worthiness and belonging. Throughout medical school, many URiM students grapple with the question: Am I doing enough to stand out on applications, given that the cards are stacked against me? Residency program directors should ensure that opportunities are available to expose URiM candidates to EM early and connect them with opportunities that can bolster their CVs.
With less quantifiable data to evaluate candidates, residency programs must avoid subconsciously relying on heuristics and implicit biases. This is similar to the “Ban the Box” initiative, which removed questions about prior criminal history from employment applications but led to adverse effects for Black male applicants, as employers sometimes assumed a criminal history even if none existed. Similarly, the removal of Step 1 scores may lead to implicit assumptions of incompetence in URiM applicants. This underscores the importance of continuous implicit bias training in a pass/ fail Step 1 world.
It is too early to evaluate the impact of pass/fail Step 1 on diversity within EM residency programs beyond conjecture. The 2024 resident matriculants were the first class under this system to match, and more URiM students did match into EM in 2024 compared to 2023 However, among the applicant pool, 6.9% were
Black, yet they disproportionately represented 20% of the unmatched candidates. White students made up 64.7% of the applicants but were only 41.4% of the unmatched candidates. More data is needed over the coming years to fully assess the long-term effects on residency selection.
Despite these challenges, the pass/ fail model presents an unprecedented opportunity for increased diversity in EM, but only if implemented thoughtfully. As the emergency department is a critical safety net and point of care for many marginalized patients, it is essential that EM physicians represent their populations to foster positive patient care and advocate for at-risk patients. During interview season, residency program directors should be intentional in their approach, being mindful of internal biases and understanding that even holistic review processes are not immune to bias. With a novel emphasis on experiential learning and extracurricular activities, EM programs should work to expose URiM students to EM early and ensure that connections and extracurricular opportunities within the department are accessible to them. In this way, EM programs can actively support URiM medical students, fostering an inclusive physician workforce that reflects and advocates for the communities it serves.
The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policies, positions, opinions, or views of the Society for Academic Emergency Medicine or its members

Melissa Fornagiel is a secondyear medical student at T.H. Chan School of Medicine at the University of Massachusetts. She is a former EMT from Holliston, Massachusetts.

By Suzanne (Suzi) Bentley, MD, MPH; Bryant Tufino Flores; and Amanda J. Deutsch, MD, on behalf of the SAEM Wellness Committee
It comes as no surprise to emergency physicians that studies identify emergency departments (EDs) as high-risk settings for violence against health care workers. According to a 2024 poll by the American College of Emergency Physicians (ACEP), more than 9 out of 10 emergency physician respondents reported being threatened or attacked in the past year. Additionally, 71% of respondents believe that violence in the ED has worsened over the past year. The reasons are multifactorial, including high patient volume, the acuity of
illness, the presence of intoxicated or mentally ill patients, and the often unrestricted, 24/7 visitation policies — all of which contribute to making ED staff particularly vulnerable to violence
The National Institute for Occupational Safety and Health defines workplace violence (WPV) as behavior ranging from offensive or threatening language to homicide.
The level of violence in EDs is alarming and continues to grow. It is crucial to recognize that numerous studies show current incidence rates
of WPV are grossly underreported, and officially reported numbers often fail to reflect the lived experiences of staff. It remains impossible to truly quantify or document WPV due to the lack of standard measurement instruments or institutional reporting policies, compounded by stigma and personal reasons for underreporting. Literature also varies in defining what constitutes WPV, with similar variability in research studies. Notably, staff perceptions of what constitutes “violence” vary, which can significantly affect reporting rates. This variation stems from the fact that
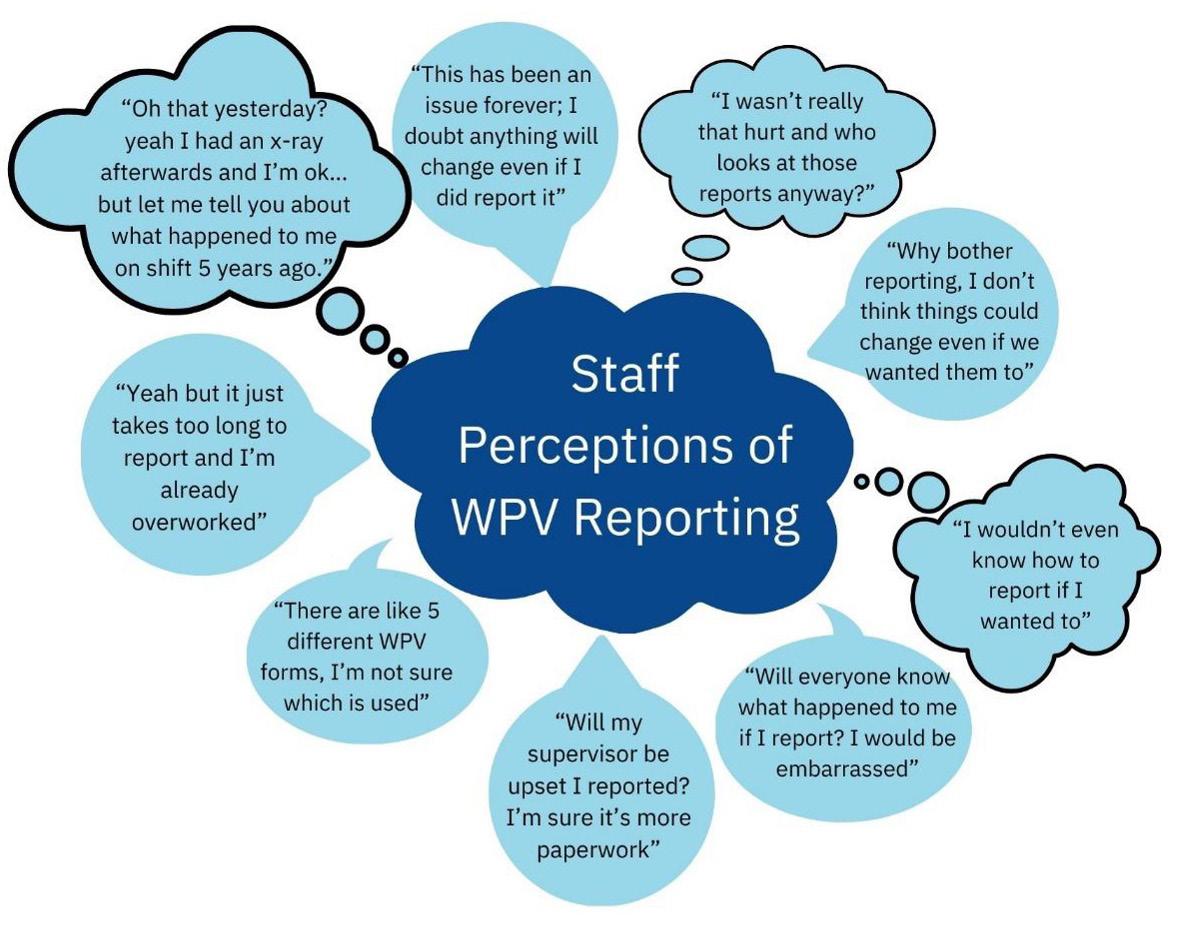
“The level of violence in emergency departments is alarming and continues to grow, with workplace violence against healthcare workers accounting for 73% of all nonfatal workplace injuries.”
most frameworks focus on the term “violence” rather than “aggression.” Some staff members define violence as a form of aggression that is intended to cause serious harm, such as injury or death. Under this definition, all violent acts are considered aggressive, but not all aggressive acts are classified as violent. This distinction is important because it influences whether certain behaviors are reported, depending on whether staff perceive them as violent or merely aggressive
Although these distinctions may hold legal or police significance, it is essential to change the culture and mindset to include both aggression and violence as serious threats to the safety and wellbeing of health care workers. Health care workers have a 20% higher chance of experiencing WPV than other employees and face at least a fourfold increase in risk compared to other professions. According to the most recent data from the U.S. Bureau of Labor Statistics, WPV against health care workers accounts for 73% of all nonfatal workplace injuries.
Neither violence nor aggression should be tolerated. Improving the reporting of WPV and aggression against staff presents a significant opportunity. While addressing WPV may often seem hopeless, we can control what happens after incidents and take action in areas within our control. High-quality patient care is impossible without staff safety and wellbeing, which in turn requires systems that protect and support caregivers. Enhanced
continued on Page 101

“Improving the reporting of workplace violence and aggression against staff is essential not only to improve the accuracy of incidence rates but also to inform better prevention, crisis response, and post-incident support.”
continued from Page 99
reporting of WPV and aggression against staff is essential not only to improve the accuracy of incidence rates but also to inform better prevention, crisis response, and post-incident support. WPV may never be fully preventable, but we can control how we respond to our staff after incidents. We can educate our trainees and staff on what WPV is, emphasize that it is never acceptable, teach them how to take meaningful action, highlight the importance of improving reporting, guide them on how to report incidents, and explain what happens afterward in the process. Figure 1 highlights real staff comments about WPV reporting
“How” to Report
“Why” to Report
“Am I Safe?” to Report
Across all drivers
and reflects common themes in staff perceptions of reporting.
Through synthesizing trends from available literature, focus group data, debriefing themes, survey data, and staff feedback during a deeper dive at our institution, several major, interconnected drivers of reporting were elucidated: “How,” “Why,” and “Am I ‘safe’ to report?”
Staff need to understand the impact of reporting to feel empowered to do so (“Why?”). Reporting must be easy and straightforward (“How?”). The options for reporting must make staff feel psychologically safe and comfortable speaking up (“Am I safe?”). For example, staff buy-in regarding the “why” to report involves the belief that their voices are
Streamline and simplify reporting pathways. Provide education on reporting procedures through quick, "just-in-time" training rather than annual modules.
Launch an educational campaign explaining the importance of reporting, the improvements made from reporting, and what to expect after reporting. Host town halls or open forums to emphasize the reasons for reporting and outline the post-reporting process, while also providing opportunities to gather insights, ideas, and questions from frontline staff.
Address and normalize feelings of reluctance to report. Partner with existing workforce wellness supports, such as peer support programs, to dispel myths about reporting. Create open staff forums to provide emotional support after workplace violence incidents and help staff understand that reporting is a tool for speaking up, being heard, and contributing to future improvements.
Develop policies to standardize responses to WPV reporting, including investigation protocols and resources for staff support. Establish a standardized escalation pathway for WPV incidents, ensuring that hospital leadership is informed. Create a dashboard to track WPV incidents, increase awareness, and analyze trends for targeted interventions. Form a dedicated WPV Against Staff Committee to coordinate WPV data, responses, and the initiation and execution of interventions.
heard, that speaking up is valid, and that resulting changes justify reporting. Improvements in this area also contribute to creating an overall culture of safety and support, which further reinforces the “Am I safe?” driver. Ultimately, all three main drivers must be addressed to lead to meaningful changes in reporting behaviors: Staff must feel safe to report, know how to report, and believe that reporting is worthwhile and that they will be supported during and after the process.
These drivers can guide interventions targeting WPV reporting, a first step in combating workplace violence in the ED. We recommend iteratively expanding initiatives to address reporting hesitancy, socializing the “why” of reporting with an emphasis on resulting changes, and fostering ongoing interdisciplinary collaboration to support staff with a united front. We must all heed the call to action to partner, speak up, support one another after WPV incidents, work to heal from past experiences, and actively fight against the concerning “normalization” of WPV in the ED.



Dr. Bentley is chief wellness officer at New York City Health + Hospitals/Elmhurst. @SuziBentleyMD
Bryant Tufino Flores is assistant coordinating manager at NYC Health + Hospitals/Elmhurst.
Dr. Deutsch is director of well-being at Thomas Jefferson Emergency Medicine. @amandajdeutsch

By Priya Iyengar
“Emergency medicine, really?! Keep an open mind!” This was the common reaction when I expressed my growing interest in the specialty during my first year of medical school.
I understand this apprehension given the delicate ecosystem of emergency medicine, which is constantly threatened by the larger chaos in the health care system. This chaos can erode the passion of those entering the field, who are initially drawn to the high acuity needs of EM and their own curious, adaptable dispositions. Moral injuries from a broken system can leave them feeling disheartened
The discussion about burnout in emergency medicine is particularly
relevant in the context of the pandemic, with troubling headlines about burnout periodically making the rounds. In conversations with an EM mentor, we noted some statistical nuances behind these headlines that often get lost in public opinion. For example the 2021 U.K. study on physician life span by specialty had a very small sample size of EM physicians vs the other specialties, and the authors made a note of EM’s recency as a specialty and the large standard deviation.
I feel pure enthusiasm every shift as I witness the satisfying management of diverse cases and enjoy the blend of procedures and medicine in a culture that fosters hospital leaders However, I reluctantly admit that ongoing public discourse tempers my enthusiasm.
Like many students, I believe that how the specialty addresses burnout will be key to maintaining the interest of future physicians.
There is a dissonance between EM’s foundational spirit — caring for anyone, anywhere, anytime — and the avoidable factors leading physicians to emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. Recently, I saw social media posts listing EM as having the highest burnout rates, the secondhighest depression symptoms, and the shortest life spans among specialties, with comments offering personal stories in corroboration. While every specialty faces troubling statistics, EM is often seen as the poster child for burnout, a grave concern that demands attention.

“There is a dissonance between EM’s foundational spirit—caring for anyone, anywhere, anytime—and the avoidable factors leading physicians to emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment.”
These striking numbers influence students’ decision-making and are a significant factor in the recent decline in applications to EM training programs post-pandemic.
At my institution, I learned about strategies endorsed by EM physicians to combat burnout. Circadian shifts for residents stood out for their potential to prevent working against their physiology more than necessary. A systemic, conscious effort is noteworthy for going beyond simply promoting better personal wellness habits. I realized that fellowship training in areas like education, disaster medicine, or toxicology provides intellectual outlets for physicians, helping
them keep the learning spirit alive alongside clinical care. During a Schwartz Round, I witnessed an EM physician processing a difficult experience with colleagues, creating a better path forward rather than internalizing failure and guilt. I was moved by this space to explore human emotions without unwarranted punishment or judgment. Regarding burnout contributors like tedious tasks such as EHR documentation, I learned from my hospital’s EM leaders about the potential of leveraging artificial intelligence to free up more time for clinical work.
Organizational change, resources, and opportunities for physician wellness are not just theoretical recommendations but
also personally convincing. As I continue my medical education, I am eager to see how the specialty embraces bold changes in addressing systemic burnout to welcome future physicians and promise a sustainable career.

Iyengar is a second-year medical student at UMass Chan Medical School in Worcester. The motivation for this article stemmed from her reflections during her participation in the 2024 BOLD EM program

By Natalie Bonthius, MD, on behalf of the SAEM Wilderness Medicine Interest Group
Recent years have seen a notable increase in search and rescue (SAR) missions and outdoor injuries in the United States. A striking example of this trend occurred in Zion National Park, Utah, where a single weekend in 2021 saw over ten separate SAR incidents, straining the park's resources. Rangers were called to rescue hikers trapped in treacherous slot canyons by rising floodwaters, assist rock climbers who had fallen and sustained serious injuries (e.g. broken bones and head trauma), and search for lost visitors who had wandered off established trails and were found dehydrated and disoriented with heat exhaustion. This surge in emergencies underscores the growing number of SAR missions and the strain on resources, highlighting the urgent
need for increased public awareness and education in wilderness medical skills.
The rise in SAR missions strongly correlates with the increased popularity of outdoor activities. The COVID-19 pandemic significantly contributed to this trend, as people sought safe and socially distanced recreational opportunities. National parks, forests, and other outdoor areas experienced record visitation numbers. For instance, Yellowstone National Park had its busiest July ever in 2021, with over a million visitors, while Grand Teton National Park saw a 20% increase in visitors compared to 2019.
This surge in outdoor activity has brought more people into nature and highlighted the unpreparedness of many new visitors. According to the National Park Service, several parks have seen a significant increase in SAR missions. Acadia National Park in Maine experienced a one-third increase in SAR operations in 2021 compared to 2019. Zion National Park, Arches National Park, and Canyonlands National Park in Utah also reported record numbers of SAR missions.
Several factors contribute to the increase in SAR missions. One major factor is the influx of inexperienced visitors. Many newcomers to outdoor
activities often underestimate the challenges and risks associated with wilderness environments. Inadequate preparation, lack of proper gear, and overreliance on technology for navigation are common issues. For example, at Acadia National Park, rangers frequently receive calls from hikers who venture onto trails without sufficient planning or equipment, often finding themselves stranded or lost.
Unpredictable weather conditions have also exacerbated the situation. Sudden changes in weather can catch even experienced hikers off guard, leading to dangerous situations that require rescue. Climate change has made weather patterns more erratic, increasing the likelihood of such incidents.
Increased accessibility of cellphones and other communication devices has made it easier for people to call for help, even in minor situations. While this accessibility can be life-saving, it also means that SAR teams are called out for incidents that might not have required intervention in the past.
The rising number of SAR missions has placed considerable strain on SAR teams, many of which are volunteer-based and operate with limited resources. Staffing shortages, partly due to the COVID-19 pandemic, have further complicated the situation. National parks have struggled to hire and retain enough rangers to meet the growing demand for SAR services.
For example, Acadia National Park relies on a partnership with a local volunteer SAR group and agreements with local fire and emergency services to manage the increased workload. Despite these efforts, low staffing levels and the physically demanding nature of SAR operations have made it challenging to keep up with the rising number of calls.
The increase in SAR missions and outdoor injuries underscores the need for enhanced wilderness medical education. Proper training and preparation can significantly reduce the number of incidents requiring rescue and improve outcomes for those who do need assistance.
One key component of wilderness medical education is learning first aid and CPR. In remote settings where
professional medical help may be hours or even days away, knowing how to perform basic first aid and CPR can be lifesaving. For instance, a hiker who knows how to treat a severe cut or stabilize a broken limb can prevent a situation from worsening while waiting for rescue. In the case of cardiac arrest in a remote area, CPR performed by a companion can mean the difference between life and death before professional help arrives.
Navigation and survival skills are also crucial aspects of wilderness medical education. Many SAR missions are initiated because individuals become lost or disoriented in the wilderness. Understanding how to use a map and compass, read the terrain, and navigate without relying solely on electronic devices can prevent many of these incidents. For example, during the weekend in Zion National Park with over ten SAR missions, many lost hikers could have avoided trouble with better navigation skills. Additionally, knowing how to build a shelter, find and purify water, and create a fire can help individuals survive unexpected situations, such as being stranded overnight due to injury or getting lost.
Risk assessment and planning are essential skills that can help prevent accidents and injuries. Educating people on how to assess risks, plan their trips, and prepare adequately for different scenarios is vital. This includes checking weather forecasts, understanding the terrain, and knowing one's physical limits. For instance, many SAR missions in national parks involve hikers who overestimate their abilities and underestimate the difficulty of trails. By teaching individuals how to properly assess and prepare for their adventures, many of these incidents can be avoided.
Proper use of outdoor gear is another critical element of wilderness medical education. Many SAR incidents involve individuals who are inadequately equipped for their outdoor activities. A surprising number of rescue calls come down to two simple issues: wearing inappropriate footwear, such as sandals on rugged trails, and not carrying enough water. Understanding what gear is necessary for different activities and conditions, and knowing how to use it properly, can prevent many common injuries and emergencies.
Implementing education programs to address these needs can be highly effective. Public awareness campaigns by
national parks and outdoor organizations can educate the public on the importance of preparation and safety. For example, using social media, brochures, and workshops can reach a broad audience and provide valuable information on how to stay safe outdoors. Additionally, mandatory training programs for certain activities or permits can ensure that participants have the necessary skills and knowledge. For instance, requiring hikers to complete a safety course before obtaining a backcountry permit can reduce the likelihood of SAR incidents.
Partnerships with educational institutions can also play a significant role. Collaborating with schools, universities, and outdoor education centers can help integrate wilderness medical education into broader curricula. Offering courses and certifications can attract a diverse group of learners, ensuring that more people are prepared for outdoor activities. Enhanced volunteer training for SAR teams and ensuring they have the necessary resources can improve response capabilities and reduce the strain on these teams.
Community involvement is another important aspect. Encouraging local communities to get involved in SAR operations and outdoor education can foster a culture of safety and preparedness. Community-led initiatives, such as local hiking clubs and outdoor skill workshops, can effectively spread knowledge and skills.
By implementing comprehensive education programs and raising public awareness, we can reduce the strain on SAR teams and ensure that outdoor recreation remains a safe and enjoyable activity for all. Wilderness medical education is not just about responding to emergencies but also about preventing them through proper preparation and knowledge.

Dr. Bonthius is a third-year emergency medicine resident at UHS Southern California. She is the founder of Survival Med, a wilderness medicine education company with more than 25,000 students globally since 2021. She provides medical education for the National Park Service, National Association for Search and Rescue, U.S. military, medical schools, universities, physicians, and more.

By Yanina Purim-Shem-Tov, MD, MS on behalf of the SAEM Academy for Women in Academic Emergency Medicine
Navigating the delicate balance between self-promotion and being perceived as a self-promoter can be particularly challenging for women physicians in academic medicine. The dual demands of advancing one’s career while maintaining collegial relationships require strategic thinking and a nuanced approach. Here are key strategies to help women physicians promote their accomplishments effectively without coming across as self-promoters.
One of the most effective ways to highlight achievements is through
third-party endorsements. Peer recommendations, letters of support, and nominations for awards serve as powerful tools. Encouraging colleagues, mentors, and department heads to acknowledge your contributions can validate your accomplishments in a manner that feels more objective and less self-serving. Cultivating a network of advocates who can speak to your skills and successes can amplify your professional reputation without you having to directly assert your worth.
See Women Don’t Self Promote, but May Be They Should by Pamela Reynolds
Instead of merely listing accomplishments, sharing stories that highlight the impact of your work can resonate more with your audience. Narratives that illustrate how your contributions have improved patient care, advanced research, or enhanced educational outcomes can make your achievements more relatable and memorable. For example, detailing how a particular research project led to improved clinical guidelines or how your teaching methods resulted in higher exam scores can provide context and demonstrate real-world impact.
“Cultivating a network of advocates who can speak to your skills and successes can amplify your professional reputation without you having to directly assert your worth.”
See Graceful Self-Promotion–It’s Essential by Page S. Morahan, PhD
Professional platforms like LinkedIn, academic blogs, and medical journals provide spaces where you can share your work within the context of industry-wide discussions. Publishing articles, presenting at conferences, and participating in panels allow you to showcase your expertise in a manner that is consistent with professional development and knowledge sharing. Highlighting your work in these forums positions you as a thought leader rather than someone who is simply self-promoting.
See Description of the Novel Networking, Open Discussion, Engagement, and Self-Promotion (NODES) Framework for the Advancement of Women Physicians on Social Media by Tricia Pendergrast
Engaging in collaborative projects can also enhance your visibility. Leading or participating in multi-disciplinary teams or research collaborations allows your contributions to be recognized within the framework of a collective effort. When your role in a successful project is acknowledged by peers and collaborators, it underscores your abilities while distributing the focus across the team. This approach not only helps in promoting your work but also builds valuable professional relationships.
See Women Don’t Self Promote, but Maybe They Should by Pamela Reynolds
Mentorship and sponsorship play crucial roles in career advancement. Mentors can provide guidance, while sponsors actively advocate for your advancement. By investing time in mentoring junior colleagues and fostering professional development, you can build a reputation as a supportive leader. This not only highlights your own achievements but also positions you as

someone committed to the growth of others in the field. Mentors and sponsors can also be instrumental in endorsing your capabilities and contributions to broader audiences.
See Mentorship and Sponsorship: The Power of Female Role Models
When discussing your achievements, it’s important to strike a balance between confidence and humility. Acknowledging the support of your team, the mentorship you received, and the collaborative nature of your projects can help convey that your successes are part of a collective effort. Using language that emphasizes “we” over “I” can also shift the focus from self-promotion to team success. This approach helps in portraying you as a competent professional who values and recognizes the contributions of others.
See Humble leadership: A review and synthesis of leader expressed humility by Thomas Keleman, et al.
For women physicians in academic medicine, self-promotion is a critical
aspect of career advancement. By leveraging third-party endorsements, sharing impactful stories, utilizing professional platforms, engaging in collaborative projects, seeking mentorship and sponsorship, and communicating with confidence and humility, it is possible to highlight accomplishments effectively without being perceived as a selfpromoter. These strategies ensure that your contributions are recognized and valued within the broader context of your professional community.

Dr. Purim-Shem-Tov is the executive vice chair of faculty affairs at Rush University Medical Center and a professor of emergency medicine at Rush Medical College. She is a graduate of the Executive Leadership in Academic Medicine program at Drexel University and a recipient of numerous awards for her contributions to medicine and leadership.

By Jane M. Hayes, MD, MPH; Lindsay V. Walsh, MD; Margaret E. Samuels-Kalow, MD, MPhil, MSHP; and Richelle J. Cooper, MD, MSHS,
on behalf
of
the
SAEM Academy for Women in Academic Emergency Medicine
In the rapidly evolving field of emergency medicine, the scholarly contributions of women physicians are increasingly critical to shaping the future of patient care and advancing the discipline. The Academy for Women in Academic Emergency Medicine (AWAEM) celebrates these impactful contributions through its annual publication awards, which highlight the exceptional research and insights from women in the field. The top publications from AWAEM members in 2023 reflect a wide range of crucial topics, from addressing health disparities to advancing career development for women physicians.
These studies not only enhance our understanding of pressing issues but also offer actionable solutions that can transform practice and policy in emergency medicine.
This literature review sheds light on the groundbreaking work recognized by AWAEM, underscoring the significance of these contributions to both individual practitioners and the broader medical community. By examining the work of the winners and finalists of the AWAEM publication awards, we gain valuable insights into the challenges and innovations that are shaping the future
of emergency medicine. These findings are particularly relevant for emergency medicine physicians, especially women, who are at the forefront of delivering equitable, high-quality care in often challenging environments. As we delve into these top publications, we see a compelling reflection of the dedication, expertise, and leadership that drive progress in our field.
Colleen Gutman, MD
Race, Ethnicity, Language, and the Treatment of Low-Risk Febrile Infants

This study found that caregivers using a language other than English were more likely to experience nonindicated interventions for febrile infants meeting low-risk criteria for invasive bacterial infection, suggesting that communication barriers may impact care equity.
Moon Lee, MD, MPH
Career Advancement Among Women Physicians in Nine Academic Medicine Specialties
This study reveals that gender parity in academic advancement is lost at the assistant professor-to-associate professor level across nine specialties, highlighting barriers to the early career advancement of women faculty.
Kathleen Li, MD, MS
Standard Nurse Phone Triage Versus Tele-Emergency Care Pilot on Veteran use of In-person Acute Care: An instrumental Variable Analysis
This pilot study shows that 60% of veterans using tele-emergency care resolved their issues without an emergency department (ED) visit, suggesting potential improvements in veterans’ access to prompt care.
Brittany Punches, PhD, RN
Patient Perceptions of Microaggressions and Discrimination Toward Patients During Emergency Department Care
Nearly half of participants in this mixedmethods study reported discrimination during their ED visits, often attributing it to prior health care encounters, emphasizing the lasting impact of previous discrimination on care perceptions.
Caitlin Ryus, MD, MPH
Emergency Department Use Among Recently Homeless Adults in a Nationally Representative Sample
This study found no link between homelessness and ED use after adjusting for physical and mental health conditions and social disadvantages, highlighting the need for programs addressing intersecting social and medical issues for undomiciled patients.
Senior Author Research
Winner
Michelle Lin, MD, MPH
Patient Sociodemographics and Comorbidities and Birth Hospital Characteristics Associated With Postpartum Emergency Department Care
This study reported higher odds of postpartum ED visits among Black and Hispanic patients across all hospital types, suggesting a need for improved care coordination and efforts to mitigate structural racism in obstetric care.
Finalists
Anita Chary, MD, PhD
“I’d Rather See Action”: Application
and Recruitment Experiences of Underrepresented in Emergency Medicine Trainees
This qualitative study examined DEI perspectives in the EM residency application process among racial and ethnic minorities. Key themes included the need for genuine DEI commitment, better racial representation, and prioritizing applicants as learners.
The findings highligh the need for a comprehensive DEI recruitment strategy.
Marianne Gausche-Hill, MD
Racial and Ethnic Disparities in the Provision of Bystander CPR after Witnessed Out-of-Hospital Cardiac Arrest in the United States
This research found that Black and Hispanic patients were less likely to receive bystander CPR compared to White patients, stressing the need for community-focused initiatives to reduce racial disparities in out-of-hospital cardiac arrest care.
Tracy Madsen, MD, PhD
Association of Prior Stroke With Health Care Perceptions of Adequate Emergency Care in Women
Women with a history of stroke reported feeling less likely to receive adequate

continued from Page 109
emergency care based on gender, race, and ethnicity, underlining the importance of addressing negative health care perceptions to avoid care delays for timesensitive conditions.
Catherine Staton, MD, MScGH “A Man Never Cries”: A Mixed-Methods Analysis of Gender Differences in Depression and Alcohol Use in Moshi, Tanzania
This study of gender differences in depression and alcohol use disorder in Tanzania found that men’s lack of social support may contribute to alcohol use disorder, suggesting a need for genderdifferentiated treatment programs for substance use.
Sarah Perman, MD, MSCE
Dissecting the Complex Association Between Age and Sex in Cardiac Arrest Outcomes-Age Disparity, Sex Disparity, or All of the Above?
This commentary discusses gender disparities in out-of-hospital cardiac arrest (OHCA) care, highlighting that reproductive-aged women received less bystander CPR but had better neurological outcomes, calling for targeted interventions to reduce disparities in OHCA care.
Richelle Cooper, MD, MSHS No More Useless Band-aids that Fail to Solve America’s Emergency Department Boarding Crisis
This editorial addresses ineffective solutions to ED boarding, citing barriers like prioritizing elective admissions, undervaluing emergency care, and structural discrimination. The authors call for government intervention, a shift in priorities, and more equitable care.
Almaz Dessie, MD
Reporting Race and Ethnicity in Medical Research: You Can’t Fix What You Don’t Know
This editorial urges thoughtful reporting of race and ethnicity data in health care research, recommending adherence to recent guidelines from the Journal of the American Medical Association, Canadian Medical Association Journal, and leading health equity researchers that emphasize
transparent data collection and category definition.
Colleen Gutman, MD
Patient Centered or Provider Centered?
The Inclusion of Social Determinants of Health in Emergency Department Billing and Coding
This editorial warns that including social determinants of health in emergency department coding could lead to stigmatization in the medical recored and calls for a patient-centered approach using objective screening tools.
Ellen Weber, MD
After 50+ Years, Emergency Medicine (and Our Patients) Remain Undervalued
This reflective editorial examines the undervaluation of emergency medicine and the challenges faced by ED patients, including overcrowding and long wait times, and warns of the potential consequences of worsening conditions.
Monica Saxena, MD, JD
Reworking Emergency Medicine Resident Education Post-Dobbs v Jackson Women’s Health Organization
This article reviews the US Supreme Court’s decision to overturn the federal right to an abortion and examines the increasing clinical challenges faced by EM physicians. It underscores the need for EM training programs nationwide to uphold the core principles of clinical practice and evidence-based care.
Emily Cleveland Manchanda, MD, MPH Training to Build Antiracist, Equitable Health Care Systems
This article discusses how educators can identify segregated healthdcare practices, develop skills to address inequities, and implement new practices within and between institutions. They emphasize starting with practical first steps at the institutional level.
Cherri Hobgood, MD
Resilience Building Practices for Women Physicians
This article highlights evidence-based interventions to enhance resilience and reduce burnout among women physicians, emphasizing the importance of role-modeling for improving the retention of women physicians.
Dana Im, MD, MPP
A Quality Measurement Framework
for Emergency Department Care of Psychiatric Emergencies
This literature review gathered an expert panel to assess existing quality measures for psychiatric care in the ED. They created a framework to guide quality improvement initiatives for adult psychiatric care in the ED.
Ynhi Thomas, MD, MPH, MSc
The Development of an Educational Workshop to Reframe and Manage Professional Conflict via a Sex and Gender Lens
This article details a workshop on communication skills for difficult conversations, focusing on sex and gender perspectives. It addresses challenges faced by women EM physicians and offers tools to increase self-efficacy in handling conflicts.

Dr. Hayes is a third-year emergency medicine resident at the Harvard Affiliated Emergency Medicine Residency (HAEMR) at Mass General Brigham. She attended medical school at Washington University in St. Louis and earned an MPH from the Harvard T.H. Chan School of Public Health.

Dr. Walsh is a third-year emergency medicine resident at the Harvard Affiliated Emergency Medicine Residency (HAEMR) at Mass General Brigham. She attended medical school at the University of Massachusetts Chan Medical School in Worcester, Massachusetts, and is a member of the SAEM Wellness Committee.


Dr. Cooper is a professor of emergency medicine and research director at the UCLA Department of Emergency Medicine.
Dr. Samuels-Kalow is an associate professor at Harvard Medical School (HMS), an attending physician in emergency medicine and pediatric emergency medicine at Massachusetts General Hospital (MGH), and the vice-chair for research in the Department of Emergency Medicine at Mass General Brigham (MGB).
Your contributions to SAEMF Foundation (SAEMF) and dedication have helped shape today's emergency medicine (EM) care, leaving a lasting impact on the field. Through your involvement in SAEM and SAEMF and your generous giving, you have supported education, research, and training that benefits SAEM member researchers and enhances emergency care.
Today, we invite you to consider becoming a part of the SAEMF Legacy Society by making a planned gift to support our mission. The SAEMF Legacy Society is our way of expressing gratitude to visionary donors like you who commit to supporting SAEMF beyond their lifetimes.
By including SAEMF in your estate plans or planned giving, you ensure that future generations of SAEM members can continue to enjoy the same opportunities and support that have been vital to your career.
If you are ready to make a legacy gift decision now, a simple bequest is often the easiest, and the language to include in your bequest and/or trust is as follows:
"I give, devise, and bequeath to The SAEMF, a 501(c) (3) charitable organization having its principal offices in Des Plaines, Illinois: the sum of $_____ or _____ percent of my estate. [or all (or _____ percentage of) the rest, residue, and remainder of my estate.] This gift is to
be used to further the charitable purposes of The SAEMF, the philanthropic arm of the Society for Academic Emergency Medicine, at the discretion of the foundation's board of trustees. (The SAEMF Taxpayer Identification Number is 26-2371803.)"
Or, take some time to browse SAEMF’s legacy giving resources. We just added several new legacy videos that you may find helpful as you consider opportunities. We recommend consulting with your financial advisor to identify a planned gift that aligns with your intentions.
If you have already remembered SAEMF in your estate, please let us know using the SAEMF Legacy Society Letter of Declaration. We would like to welcome you into the SAEMF Legacy Society! We will be honored to recognize your status as a Legacy Society donor in our communications and at events.
Your legacy gift will ensure that the SAEMF continues to be a driving force in advancing emergency medicine education and research, benefiting countless future generations of SAEM members and their patients. Take the next step by contacting our development team to discuss your interests with a member of SAEMF’s Legacy Gifts Committee.
How do I become a Legacy Society donor? • When is the right time to consider legacy giving? • What options are there for planned gifts?

















SAEMF Legacy Society Donor
SAEMF Annual Alliance Enduring Donor
“When I earned my credentials over 40 years ago, emergency medicine was a young specialty, and there were only a couple dozen emergency medicine residencies in the entire country. No one knew what an emergency physician was, as most “ER docs” were residents or interns in academic hospitals, or, rotating staff physicians covering the ER in private hospitals.
It was emergency medicine research that defined our place in the House of Medicine, and it continues to refine our practice today. I started contributing to emergency medicine research in 1982 when I completed my emergency medicine residency and started my first academic faculty position. I gave annually, and I gradually increased my contribution as my income increased.
In 2000, we established our estate plan, and I specifically created a charitable trust to continue my giving to emergency medicine research in perpetuity. In 2008, when the Society for Academic Emergency Medicine (SAEM) started our SAEM Foundation (SAEMF), I was there, serving on the SAEMF Development Committee, and I soon added my legacy gift in perpetuity for SAEMF to my estate plan charitable trust.
We all have had assistance and mentors along the way, and it is only fitting that we should give back, and pay it forward to those who will follow. I am asking you to join me in giving annually to your SAEMF, to increase your contribution as your income increases, and to establish your legacy in perpetuity through your will or estate plan to continue to enhance your specialty in the future.
Together, we can assure a bright future for our specialty. I appreciate your understanding of the importance of emergency medicine research, and I thank you for your consideration in joining me to fund our specialty's future in perpetuity!”
We're Grateful to Dr. Wilcox for his longtime support through the SAEMF's Annual Alliance and as an SAEMF Legacy Society donor. He has endowed a new scholarship that recognizes excellence in research by RAMS Residents and Medical Students. This scholarship will elevate funding available for residents and medical students interested in careers in academic emergency medicine research and education. Are you interested in creating new pathways to encourage bright minds of tomorrow to pursue a career in academic emergency medicine research and education? Please let us know what you would like to explore – email us at foundation@saem.org.

Sign Up for an SAEM Committee: Drive Change, Elevate Your Impact, Expand Your Network!
A valuable benefit of SAEM membership is the opportunity to serve on an SAEM committee. Committee involvement nurtures leadership and teamwork skills, provides opportunities to collaborate with diverse individuals; connects you with like-minded professionals; and expands your network. Through committee participation, you’ll enrich your knowledge and expertise while gaining insights into the latest innovations and best practices. Moreover, committee membership serves as a platform to drive positive change within the association and the academic EM specialty, allowing you to leave a lasting impact. Your unique committee signup link was sent to your SAEM membership email on August 28, 2024. Didn’t receive it? Got questions? Reach out to us at governance@saem.org Signups close October 11, 2023. Visit our SAEM Committees page to learn more!
Step Up for Leadership in 2024-2025!
Nominations Open September 23
Nominations open for soon for key leadership positions on the SAEM Board of Directors, RAMS Board, SAEM Nominating and Bylaws committees, AACEM and SAEM academy executive committees, and the SAEM Foundation Board of Trustees. We’re looking for dynamic leaders who are not just committed but truly passionate about fostering growth and innovation within our community. If you or someone you know bring diverse perspectives, exceptional skills, and the experience
to lead effectively, this is the perfect opportunity to step forward. This is your opportunity to make a lasting impact. Do you have what it takes? Or do you know someone who does? Visit our nominations webpage for more details on the nomination process. The deadline for submissions is November 1, 2024. Don’t miss this chance to lead and inspire!
Celebrate Excellence: Submit Your Nominations for SAEM and RAMS Awards
SAEM awards season opens October 1, and we invite you to join us in recognizing excellence in emergency medicine by nominating a colleague, mentor, or yourself for an SAEM or RAMS award. SAEM Awards celebrate excellence, honor achievements, and acknowledge the very best in academic emergency medicine research, education, and leadership. Check out the award categories and the nomination process and plan to submit your nomination by December 9! Your involvement is the key to making this season of recognition truly special.
Seeking Participants for New URiM Academic EM Program — Apply by Sept. 15
Co-sponsored by the SAEM Academy for Diversity and Inclusion in Emergency Medicine and the SAEM Equity and Inclusion Committee, the Leadership, Engagement, and Academic Pathway (LEAP) offers mentorship and development opportunities to support students from historically marginalized groups to achieve their academic and professional goals in emergency medicine. Apply by September 15, 2024. Questions? Contact adiem@ saem.org.
Mentees: M3 students from historically marginalized groups are invited to apply.
Mentors: EM physicians with a strong scholarly track record are needed for a one-year co-mentorship.
Mark Your Calendars With These SAEM25 Submission Dates!
The SAEM Annual Meeting is a premier platform for showcasing cutting-edge
research in academic emergency medicine. Submitting your work allows you to present to a knowledgeable audience, receive expert feedback, and advance your research. The meeting’s focus on original education, research, knowledge sharing, and career development makes it an ideal venue for gaining recognition and advancing your career. Mark your calendars and plan to submit your work to SAEM25!
Closing Sept. 17: Advance EM Workshop submissions
Due Oct. 2: Didactic submissions
Due Nov. 6: Dr. Peter Rosen Memorial Keynote submissions
Unlock Exclusive SAEM24 Educational Content Now on SOAR!
Exciting news for SAEM members! The SAEM Online Academic Resources (SOAR) platform has been updated with exclusive SAEM24 content. Enjoy unlimited access to hundreds of topnotch SAEM24 educational sessions from leading experts in academic emergency medicine. This valuable resource is free for all SAEM members. Explore SOAR anytime, anywhere to enhance your knowledge and skills.

Emergency Medicine faculty currently represent just 0.3% of NIH study sections. We need to change that! In addition to the Early Career Reviewer (ECR) program, the NIH is now inviting scientific societies to recommend expert reviewers from all career stages for study sections through its new Scientific Society
continued from Page 115
– Reviewer Recommendations program. Let’s increase emergency medicine representation by nominating yourself or another expert for a study section by September 30. More EM investigators on study sections mean more opportunities for success in emergency care research. Learn More
Apply by October 1 for the Neuro-EM Scholars National a K12 Program
The Neuro-EM Scholars National K12 Program is currently accepting applications for its inaugural scholar cohort as well as nominations for its Pipeline Program. Created with the National Institute of Neurological Disorders and Stroke (NINDS) at the NIH, this innovative program aims to recruit, mentor, and train early-career emergency medicine faculty in neurological disorder research. It also supports early career investigators, promoting diversity and participation from underrepresented backgrounds. Scholar applications and Pipeline nominations are due October 1, 2024. Interested candidates and nominators can learn more and register for updates via the official program website.
Accepting Applications for eLead and ARMED MedEd!
SAEM educational courses are designed to support and advance the careers of professionals in emergency medicine. Whether you’re looking to deepen your expertise in medical education research or enhance your leadership skills, these programs offer tailored experiences to help you achieve your goals.
• Advanced Research Methodology Evaluation and Design: Medical Education (ARMED MedEd): builds on foundational knowledge to help health professions education researchers design high-quality medical education research projects and grant proposals. Scholarships are available. Deadline: October 31.
• Emerging Leader Development
Program (eLEAD): aimed at developing foundational leadership skills in emerging leaders within academic emergency medicine. Offers a structured, longitudinal experience to help participants build a meaningful career network and open new opportunities in their field. Deadline: October 31.
September 30, 2024 Is the Deadline to Apply for A NIDA Mentor-Facilitated Training Award, Sponsored by SAEMF
The SAEMF-sponsored NIDA Mentor Facilitated Training Award offers a $10,000 stipend for awardees and a $2,000 stipend for mentors. This program supports early career investigators in substance use disorder (SUD) research, particularly opioid use disorder (OUD), through a mentor supervised project. Learn more and apply by September 30, 2024.
SAEMF Emergency Medicine Interest Group Grant (EMIG) Applications Open October 15, 2024
As champions of medical student education, we understand the pivotal role EMIGs play in fostering excellence. SAEMF EMIG Grants fuel the growth of established and/or developing EMIGs, fostering innovative approaches in undergraduate emergency medicine education. From essential supplies to insightful consultations, SAEMF EMIG Grants provide the crucial seed money your group needs to flourish. Apply by 5 pm CT on January 31!
Add These Upcoming Webinars to Your Watch List!
Our growing SAEM Webinar Library offers a full range of live and recorded webinars on various emergency medicine topics, offering a fantastic opportunity to stay ahead in the field, learn from experts, and connect with peers. Don't miss out — register for these upcoming webinars today!
• Landing Your Dream Job: Current Perspectives on the Emergency Medicine Job Landscape, Sept. 10
• Biostats Made Simple: Session 3, Sept. 18
• Leadership Unlocked: SAEM Nominations and Opportunities, Sept. 24
• Biostats Made Simple: Session 4, Oct. 15
• SAEM Bylaws Committee, Oct. 16
• Highlighting Career Pathways & Leaders in Geriatric Emergency Medicine, Oct. 24
Showcase Your Research at the 2024 SAEM Great Plains Regional Meeting! Join us for the 2024 SAEM Great Plains Regional Meeting, "Adapting to a Changing Landscape," on Saturday, November 9, at the Hyatt Regency Coralville Hotel & Conference Center in Iowa City, Iowa. Hosted by the University of Iowa Department of Medicine, this event provides a platform for emergency medicine residents and faculty to showcase their research. Highlights include poster sessions, top abstracts presentations, plenary speakers, and a Quiz Bowl for medical students and residents. Don't miss the opportunity to contribute—submit your abstracts by October 1, 2024, for a chance to present!
Submission Deadline for the AEM E&T Proceedings Issue is Sept. 15
AEM Education and Training (AEM E&T) is now accepting submissions for a special SAEM24 Proceedings issue, set to be published in early 2025. We welcome manuscripts and conceptually driven white papers from SAEM academies, committees, and interest groups. Submissions should spotlight innovative ideas and concepts that reflect your unique expertise, with a focus on advancing education and training in emergency medicine. The deadline to submit is September 15, 2024—don't miss out!
SAEM membership provides exceptional benefits, granting you access to a wealth of resources designed to advance your career in emergency medicine. Enjoy exclusive opportunities for professional development and connect with a vibrant community of peers and leaders. Leverage these invaluable resources to unlock your full potential.
Fellowship Directories
Access SAEM’s comprehensive, searchable directories to find the ideal emergency medicine fellowship. These essential tools help elevate your career. Start your search today!
• Fellowship Directory
• Global EM Fellowships Consortium (GEMFC) Directory
Residency Directory
SAEM’s Residency Directory offers a comprehensive, searchable listing of EM residencies. Users can compare institutions, save favorites, and access program websites directly. Email us at SAEM Directories to list your institution.
LGBTQIA+ Mentorship Program
Join EM medical students and residents in a supportive program with faculty-
led mentorship, Zoom meetings, panel discussions, and in-person events at the SAEM Annual Meeting. Sign up today to advance your career.
Enhance your ED’s cultural competence with our customizable DEI curriculum Tailored for diverse learners, it fosters inclusivity, improves patient outcomes, and sparks vital discussions. Engage your department today.
Featured Chapters:
• Health and Social Inequities of Sex and Gender Minority Patients and Providers
• Understanding and Combating Ableism in Medicine: Promoting Access and Inclusion for Individuals with Disabilities Through Systemic Change
• What Should I Say? Understanding Person- vs. Identity-First Language
Academic Career Guide
The Academic Career Guide provides essential strategies for students and early-career physicians pursuing academic emergency medicine roles like department chair or residency program director. Unlock your potential in academic EM.





This toolkit guides aspiring EM researchers, offering insights and strategies for medical students, residents, and junior faculty. Learn from experts and navigate your research career with confidence. Access The Reason for Research anytime, anywhere!
AEUS
Access a comprehensive ultrasound curriculum for emergency physicians in training. AEUS faculty can manage learners and administer exams online. Non-members can view lectures on AEUS YouTube and AEUS Vimeo channels.


Shape the Future of SAEM—Your Feedback Matters!
We value your insights and experiences! By completing our 2024 Member Survey, you'll help us enhance the services, resources, and programs that matter most to you. Your participation is essential to understanding your needs, preferences, and concerns, and will help shape SAEM’s future to better serve the academic emergency medicine community. Help us ensure that SAEM continues to provide a membership that meets your needs and exceeds your expectations. Take the survey today!
Why Your Input Matters:
• Enhancing Member Experience: Your feedback helps us tailor our offerings, including educational resources, meetings, networking opportunities, and committees, to better meet your needs.
• Driving Positive Changes: Your opinions influence our decisions, ensuring we focus on initiatives that matter most to you.
• Strengthening Community Engagement: Participating in the survey strengthens our community, fostering collaboration and camaraderie among members.
Recent Actions Based on Your Feedback:
• Instagram Account: We’ve launched the official SAEM Instagram account @SAEMonline for updates and behind-thescenes content.
• Website Improvements: Enhanced usability and functionality based on your feedback make the SAEM website more userfriendly.
• Record High Annual Meeting and Membership Numbers: Thanks to your feedback and support, we’ve achieved record attendance at SAEM24 and record membership numbers. Incentives:
As a thank you, complete the survey and provide your email for a chance to win free registration to SAEM25 in Philadelphia (May 13-16, 2025). Residents and medical students are also eligible to win an electronic stethoscope.
Submitted by Dustin Williams, MD, and Ramana Feeser, MD on behalf of the SAEM Membership Committee
Applying for or nominating someone for an award showcases exceptional achievements and boosts visibility within your department or on a national level. It can also support your case for promotion or tenure. Here are some tips for a successful nomination.
Step 1: Check for Calls for Awards. Monitor your email and the SAEM website for award announcements. When you see a call for nominations, identify potential candidates and mark the due date on your calendar. Some awards permit self-nominations, while others require nominations from active SAEM members. If you’re a strong candidate, consider discussing your nomination with a colleague.
Step 2: Review Eligibility. Ensure that you or your nominee meets the award’s criteria. Some awards are for junior faculty with less than eight years post-residency, while others target fellows or distinguished leaders in SAEM.
Step 3: Update the CV. Verify that the candidate’s CV is current, as most SAEM awards require an updated CV. Key details relevant to the award should be easy to find. If nominating, provide your CV to your letter writer to aid in preparing a strong recommendation.
Step 4: Gather Supporting Documents. In addition to the CV, awards may require a cover letter, nominee photo, additional letters of support, or media contact information. Collect these documents in advance for submission.
Step 5: Review the Standardized Letter Format. Download and complete the standardized letter for each award. This form guides the awards committee in evaluating nominees and highlights key aspects of the candidate's work.
Step 6: Submit Your Application. Ensure all documents, including letters and CV, are ready to upload. Avoid last-minute submissions by applying well before the deadline.
For questions about the nomination process, the SAEM Awards Committee is available to assist. Though the process may seem daunting initially, it becomes easier with experience. Departments with award committees are familiar with the process; if your department lacks one, consider establishing it with your chair or vice chair. Happy nominating!
Submitted by Cassandra Mackey, MD, and Jennifer Carey, MD, on behalf of the SAEM Awards Committee.
Looking to contribute more to academic emergency medicine? Consider becoming a leader within the Society for Academic Emergency Medicine (SAEM)! We’re seeking individuals who bring diverse ideas and can listen to the ideas of others. And guess what? You’re more prepared than you think!
SAEM is a dynamic organization full of potential. Leadership here isn’t about pushing one viewpoint but about balancing the
needs of all members, prioritizing ideas, and making thoughtful decisions. If you’re committed to the SAEM mission, willing to listen, collaborate, and put in the effort, you’re ready to lead. We all experience self-doubt—it’s the classic impostor syndrome. This feeling is completely natural, especially when stepping into new roles. But let’s dispel that notion: why expect to know everything about leadership from the start? With guidance, humility, and practice, you’ll grow into it. So, take the leap into SAEM leadership and discover the exciting opportunities SAEM offers!
Opportunities to Get Involved
• Nominating Committee (2-year commitment): Play a critical role in shaping the future of SAEM by selecting candidates to fill vacancies on the Board of Directors and standing committees. Identify and nominate rising stars who will help lead emergency medicine forward.
• Bylaws Committee (3-year commitment): Help ensure SAEM’s rules remain relevant by updating the Bylaws as the organization and its environment evolve. Your work will help guide how decisions are made and ensure respectful dialogue during disagreements.
• SAEM Board of Directors Members-at-Large (3-year term): As a member of the board, you will set priorities for the organization, provide oversight for SAEM’s various committees, sections, and interest groups, and evaluate the CEO. You can also be re-elected for a second term to continue shaping SAEM’s direction.
• Resident Representative (1-year term): Provide the resident perspective on the SAEM Board and represent the voice of the next generation. This is a great opportunity to develop leadership skills alongside more experienced leaders. To be eligible, residents must be endorsed by their program leadership and enrolled in an ACGME-accredited EM residency program.
• Additional Leadership Roles: There are many other leadership opportunities in SAEM’s RAMS, AACEM, SAEM Foundation, and its various academies, interest groups, committees, and task forces. These positions offer you a chance to lead more focused efforts, collaborate with peers, and hone skills like listening, networking, and setting priorities.
Key Dates:
• September 23, 2024: Nominations open.
• September 24, 2024: Join the “Leadership Unlocked” webinar at 1 p.m. CT to learn about the nomination process and open positions. Get your questions answered live—register today!
• November 1, 2024: Nominations close—be sure to submit yours on time.
Helpful Tips
• Start When It Feels Right: But remember, in the words of Winnie the Pooh, “You are better than you think you are!”
• Learn by Doing: Get involved by joining an SAEM academy, committee, or interest group to expand your connections and gain valuable experience.
• Become a Leader: Move from being a member to leading a group— It’s like going from fan to rockstar.
• Seek Advice: Reach out to former leaders for tips and insights. They’ve been in your shoes and can offer guidance on navigating your new role.
• Community Support: Remember, you’re not alone! The SAEM community is one of the greatest benefits of membership. You’ve got a network behind you!
You’re standing at a crossroads, with leadership opportunities right in front of you. Now’s the time to seize them, bring your best effort, uplift those around you, and join the team that’s advancing academic emergency medicine. For more details, watch this video by SAEM’s Past President, Dr. Wendy Coates.
Submitted on behalf of the SAEM Nominating Committee.
Academy of Administrators in Academic Emergency Medicine
AAAEM Collecting Data for FY24 Benchmark Survey
The Academy of Administrators in Academic Emergency Medicine (AAAEM) Benchmark Committee is collecting data for the FY24 academic year for the annual benchmark surveys. These surveys are used to benchmark academic emergency medicine department’s/division’s clinical, education, and research missions. If you have any questions or need assistance submitting your organization’s data, contact Alyssa Tyransky (alyssa.tyransky@osumc.edu).
AAAEM will share some of the results of the FY24 data collection at the AAAEM booth at SAEM25 so stop by and learn more about the surveys and AAAEM.

If you’re struggling, tell someone.


Nicklaus P. Ashburn, MD, MS, assistant professor of emergency medicine at the Wake Forest University School of Medicine, has been awarded a K23 grant from the National Institutes of Health/National Heart, Lung, and Blood Institute (NIH/NHLBI) for conducting a five-year randomized control trial focused on providing preventive cardiovascular care for at-risk patients in the emergency department. He will evaluate a novel, protocolized intervention known as EMERALD (Emergency Medicine Cardiovascular Risk Assessment for Lipid Disorders), the first of its kind in the country. Dr. Ashburn and his team of experts in emergency medicine, cardiology, social sciences, and biostatistics designed this patient-centered intervention to improve the health of patients with unmitigated cardiovascular disease risk factors.

Prashant Mahajan, MD, MPH, MBA, has been named chair of the Department of Emergency Medicine and the William G. Barsan Collegiate Professor of Emergency Medicine in the University of Michigan (U-M) Medical School. Dr. Mahajan was the previous vice chair of the U-M Department of Emergency Medicine, and a tenured professor and section chief of pediatric emergency medicine. Dr. Mahajan is founding chair of the Emergency Medicine Research and Education network by Global Experts (EMERGE) a global network of 20 academic emergency departments in more than 15 countries. He also is director of Research and Education in Acute Care with Advanced Technology (REACT), and past chair of the American Academy of Pediatrics Section of Emergency Medicine. Dr. Mahajan's research focuses on clinical decision-making in austere circumstances.

David Kim, MD, PhD, has received an R01 grant from the National Institutes of Health (NIH) for “Integrating Acute and Ambulatory Care with Post-Discharge Monitoring and Machine Learning." This project aims to monitor high-risk emergency department patients after hospital discharge to better understand how patient physiology evolves after discharge and to identify remote monitoring signals that may represent important changes in health status. Dr. Kim is an assistant professor of emergency medicine at Stanford University School of Medicine.

Samuel Yang, MD, was awarded an R01 grant from the National Institutes of Health (NIH) as a Multiple Principal Investigator. The award is for “Single-cell based diagnostic platform with single-molecular transcriptional response profiling for rapid phenotypic antimicrobial susceptibility testing of gonorrhea,” which will strive to develop novel diagnostic technologies that not only provide clinically actionable information with unprecedented performances in sensitivity, specificity, speed, multiplexity, and resolution but are also affordable and accessible to the public. The grant is awarded jointly to both Johns Hopkins and Stanford universities with a total $3.88 million over five years. Dr. Yang is a professor of emergency medicine at Stanford University School of Medicine.

Tehreem Rehman, MD, MPH, MBA, was one of two fellows selected from a national pool for a Bedside Medicine Fellowship. The Society of Bedside Medicine, in partnership with Gordon and Betty Moore Foundation and Johns Hopkins Medicine, established the Bedside Medicine Fellowship to foster a community of clinician-educators and researchers dedicated to upholding the value of the bedside encounter in improving patient outcomes. Dr. Rehman’s project, entitled “Clinical Pathways: Advancing Health Equity in Clinical Reasoning,” aims to empower trainees to identify areas of significant variation in their bedside patient care and subsequently apply quality improvement methodology to achieve evidence-based structure and equity in their clinical reasoning. Dr. Rehman is on faculty at the Icahn School of Medicine at Mount Sinai and an attending physician at The Mount Sinai Hospital.

Rebecca Theophanous, MD, MHSc, has been promoted to associate professor of emergency medicine at the Duke University School of Medicine. Dr. Theophanous is emergency ultrasound faculty at Duke University Hospital and the Durham Veterans Affairs Healthcare System. Her grant-funded research involves identifying facilitators and barriers to ultrasound program implementation and clinician training. She also has published on 3DUS technology as an innovative bedside tool.

Carly Eastin, MD, was promoted to professor of emergency medicine at the University of Arkansas for Medical Sciences, effective July 1. On September 1 she will be transitioning to the University of Iowa Carver College of Medicine as a clinical professor of emergency medicine. Dr. Eastin is the immediate past chair of SAEM’s Evidence Based Medicine Interest Group.

Nikhil Goyal, MBBS, has been named senior vice president, accreditation, for the Accreditation Council for Graduate Medical Education (ACGME). Dr. Goyal will oversee the activities of the accreditation staff members responsible for 17 medical and hospital-based specialty review committees and those supporting the programmatic accreditation of graduate medical education (GME) programs. As a member of the ACGME Senior Leadership Team, he will act as a liaison to other GME organizations and agencies. He will also provide support to the review committees to help ensure fair reviews of GME programs, drive improvement in the use of accreditation data, and communicate accreditation-related matters to the medical education community. Prior to joining the ACGME, Dr. Goyal was the associate designated institutional official (DIO) at Henry Ford Health and a practicing emergency physician at Henry Ford Hospital in Detroit, Michigan.

Steven L. Bernstein, MD, has received a 7-year, $27.7 million award from the National Institutes of Health's National Center for Advancing Translational Sciences (NIH NCATS) to found SYNERGY: The Dartmouth Clinical and Translational Science Institute (CTSI). Dr. Bernstein is the senior associate dean for clinical and translational research at the Geisel School of Medicine, chief research officer at Dartmouth-Hitchcock Medical Center, and director of the C. Everett Koop Institute at Dartmouth.

Morgan Wilbanks, MD, has been promoted to associate professor of emergency medicine at the Medical College of Wisconsin Medical School. Dr. Wilbanks was previously an assistant professor in the department of emergency medicine.
Dr. Ian B. K. Martin Appointed Interim Senior Associate Dean for Faculty Affairs and Associate Provost for Faculty Affairs at MCW

Ian B. K. Martin, MD, MBA, has been appointed interim senior associate dean for faculty affairs and associate provost for faculty affairs, effective September 9, 2024. Dr. Martin is professor with tenure, and system chairman of the Medical College of Wisconsin Department of Emergency Medicine. He also serves as professor of medicine, professor in the Institute of Health and Equity, and emergency physician-in-chief for the Froedtert & the Medical College of Wisconsin health network. He will continue in his current leadership roles in the Department of Emergency Medicine and the health network.
Gregory Faris

Gregory W. Faris, MD, has been promoted to associate professor of clinical emergency medicine and clinical pediatrics at Indiana University School of Medicine. Dr. Faris is medical director for Marion County Dispatch and medical director for the Indianapolis Fire Department with the Division of Out-ofHospital-Care. He has been recognized for his teaching excellence with numerous awards including the Kevin G. Rodgers Excellence in Clinical Teaching Award and Indiana University School of Medicine Trustees Teaching Award.

Alicia Pilarski, DO, has been promoted to professor of emergency medicine at the Medical College of Wisconsin Medical School. Dr. Pilarski was previously an associate professor in the department of emergency medicine.

Amy Zosel, MD, MSCS, has been promoted to professor of emergency medicine and medical toxicology at the Medical College of Wisconsin Medical School. Dr. Zosel was previously an associate professor in the department of emergency medicine.
continued from Page 121
Dr. Frances Russell Promoted to Professor of Clinical Emergency Medicine, IU School of Medicine

Frances Russell, MD, has been promoted to professor of clinical emergency medicine at Indiana University School of Medicine. Dr. Russell is co-director of Ultrasound in Medical Education. She has received multiple national and local awards, including the Indiana University School of Medicine Trustees Teaching Award and SAEM Academy of Ultrasound Academic Excellence Award.
Dr. Sara Damewood Promoted to Professor and Vice Chair of Education, University of Wisconsin School of Medicine

Sara Damewood, MD, has been promoted to professor and vice chair of education within the BerbeeWalsh Department of Emergency Medicine, University of Wisconsin School of Medicine and Public Health.
Dr. Andrew Farkas Promoted to Associate Professor of EM and Medical Toxicology, Medical College of Wisconsin Medical School
Andrew Farkas, MD, has been promoted to associate professor of emergency medicine and medical toxicology at the Medical College of Wisconsin Medical School. Dr. Farkas was previously an assistant professor in the department of emergency medicine.
Cory Showalter Promoted to Associate Professor of Clinical Emergency Medicine and Clinical Pediatrics, IU School of Medicine

Cory Showalter, MD, has been promoted to associate professor of clinical emergency medicine and clinical pediatrics at Indiana University School of Medicine. Dr. Showalter is interim pediatric emergency medicine division chief at Riley Hospital for Children and regional medical director for Pediatric Emergency Medicine. He has been recognized for his exceptional teaching, including the Indiana University School of Medicine Trustees Teaching Award and the Department of Emergency Medicine Residency Impact Award.
Dr. Roxanna Lefort Promoted to Associate Professor of Clinical Emergency Medicine and Clinical Pediatrics, IU School of Medicine

Roxanna Lefort, MD, MPH, has been promoted to associate professor of clinical emergency medicine and clinical pediatrics at Indiana University School of Medicine. Dr. Lefort is the program director for the disaster medicine fellowship within the Division of Out-of-HospitalCare. She has been recognized by the Riley Physicians Living Our Values Excellence Award and Indiana University School of Medicine Faculty Teaching and Mentorship Award.

Brian Patterson, MD, MPH, has been named the inaugural physician administrative director for Clinical AI for UW Health. In this role, Dr. Patterson will lead the application of advanced algorithms and machine learning techniques to find insights in large medical datasets to improve medical diagnosis, treatment, and disease prevention. Dr. Patterson is an associate professor with tenure at the BerbeeWalsh Department of Emergency Medicine, UW School of Medicine and Public Health.


Michael Ward, MD, PhD, MBA, and Alan Storrow, MD, of Vanderbilt University Medical Center's Department of Emergency Medicine, are the investigators of a new NHLBI-funded T32 postdoctoral training program called the Vanderbilt Interdisciplinary Hospital-based Systems of Care Research Training Program. This program marks a novel collaboration between emergency medicine and hospital medicine, creating the third adult emergency medicine T32 training program and the first hospital medicine program.
Dr. Ward is vice chair for research in the Division of Emergency Medicine Research and an associate professor in the departments of emergency medicine and biomedical informatics at Vanderbilt University Medical Center. Dr. Storrow is an associate professor and associate director for research in the Department of Emergency Medicine at Vanderbilt University Medical Center.



The Department of Emergency Medicine, Division of EMS Medicine at the Medical College of Wisconsin played a pivotal role in the planning and execution of the health and medical response for the recent Republican National Convention (RNC) in Milwaukee. Division of EMS Medicine members: M. Riccardo Colella, DO, professor; J. M. Liu, MD, professor; Ben Weston, MD, associate professor; Matthew Chinn, MD, associate professor; Tom Grawey, DO, assistant professor, Department of Emergency Medicine, Medical College of Wisconsin, and colleagues engaged in over a year of planning leading to a safe and successful event. Engaging with and supporting 19 different subcommittees, their extensive collaboration and leadership led to the development of

Gregory Fermann, MD, has been named chair of the Department of Emergency Medicine and the Richard C. Levy Professor at the University of Cincinnati College of Medicine. Dr. Fermann has served the Department of Emergency Medicine in various capacities, including medical director of the Center for Emergency Care, vice chair for strategic planning, director of the Clinical Trials Center, vice chair for research, and most recently, as executive vice chair. He has earned numerous accolades, including the 2023 Ohio ACEP Physician Leadership Award, the 2023 Timothy D. Freeman Sustained Excellence Award, and the UC Clinical Trialist of the Year award.
The SAEM Pulse Academic Announcements section publishes academic appointments, promotions, retirements, grant awards, research announcements, published papers, etc. Send your content (50-75 words max) to newsletter@saem.org. The next content deadline is October 1, 2024 for the November-December 2024 issue.
hundreds of pages of documents, engaging health system leadership and national medical assets, and spearheading the creation of a highly effective Patient Movement Process, which the United States Secret Service plans to use as a national model for future National Special Security Events (NSSEs). Additionally, the team innovated with the creation of a new RNC-specific online patient care record and a real-time patient tracking dashboard for monitoring concerning trends such as food poisoning and chemical irritants. The comprehensive and forward-thinking work of the MCW EMS team has established a robust framework that will enhance emergency preparedness and response for major events nationwide.

Accepting ads for our “Now Hiring” section!
Deadline for the next issue of SAEM Pulse is October 1.
For specs and pricing, visit the SAEM Pulse advertising webpage.



The University of California San Francisco, Department of Emergency Medicine is recruiting for a full-time faculty member at the Associate Professor or Professor level to serve as the Director of Quality Improvement at our UCSF Hellen Diller Medical Center at Parnassus Heights campus. We seek individuals who meet the following criteria: emergency medicine faculty with a track record of successfully developing and maintaining rigorous, data-driven quality and safety programs, establishing a culture of safety, improving the identification and review of cases, and ultimately, optimizing the quality of patient care. Rank, step and series will be commensurate with qualifications.
The Department of Emergency Medicine provides comprehensive emergency services to a large local and referral population at multiple academic hospitals across the San Francisco Bay Area, including UCSF Hellen Diller Medical Center, Zuckerberg San Francisco General Hospital and Trauma Center, and the UCSF Benioff Children’s Hospitals in San Francsico and Oakland. The Department of Emergency Medicine hosts a fully accredited 4-year Emergency Medicine residency program and multiple fellowship programs. There are opportunities for leadership and growth within the Department and UCSF School of Medicine.
Board certification in Emergency Medicine is required. All applicants should excel in bedside teaching and have a strong ethic of service to their patients and profession.
The University of California, San Francisco (UCSF) is one of the nation’s top five medical schools and demonstrates excellence in basic science and clinical research, global health sciences, policy, advocacy, and medical education scholarship. The San Francisco Bay Area is well-known for its great food, mild climate, beautiful scenery, vibrant cultural environment, and its outdoor recreational activities.
PLEASE APPLY ONLINE AT: https://aprecruit.ucsf.edu/apply/JPF05030
Applicants’ materials must list current and/or pending qualifications upon submission. The posted UC salary scales set the minimum pay determined by rank and step at appointment. See [Table 5] (https://www.ucop.edu/academic-personnel-programs/_files/2023-24/oct-2023-acad-salary-scales/t5-summary.pdf). The minimum base salary range for this position is $177,100-$377,200. This position includes membership in the [health sciences compensation plan] (https://ucop.edu/academic-personnelprograms/_files/apm/apm-670.pdf) which provides for eligibility for additional compensation.
UCSF seeks candidates whose experience, teaching, research, and community service has prepared them to contribute to our commitment to diversity and excellence. UCSF is an Equal Opportunity/Affirmative Action Employer. The University undertakes affirmative action to assure equal employment opportunity for underrepresented minorities and women, for persons with disabilities, and for covered veterans. All qualified applicants are encouraged to apply, including minorities and women. For additional information, please visit our website at http://emergency.ucsf.edu/










Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.

Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pa.




The University of California, San Francisco (UCSF) Department of Emergency Medicine is recruiting for a highly experienced investigator to join our dynamic team. The ideal candidate will have a proven track record of securing federal funding and conducting groundbreaking research. We seek an individual who can lead large-scale projects and drive forward our research agenda, contributing significantly to our department's objectives.
Required qualifications include: 1) board certification in emergency medicine or pediatric emergency medicine, and 2) experience obtaining and managing federal research grants. Candidates having at least 5 years of experience in a research leadership role are preferred. The successful candidate will have excellent leadership, communication and organizational skills, as well as a proven ability to work collaboratively in a multidisciplinary team environment.
The Department of Emergency Medicine provides comprehensive emergency and trauma services to large local and referral populations at multiple academic hospitals across the San Francisco Bay Area, including UCSF Hellen Diller Medical Center, Zuckerberg San Francisco General, and the UCSF Benioff Children’s Hospitals in San Francisco and Oakland. Our department serves as the primary teaching site for a fully accredited, 4-year Emergency Medicine residency program and offers 10 fellowship programs, including multiple research training programs. Research is a major priority of the department with over 100 peer-reviewed publications each year. We have a highly successful health services research group, participate in multiple clinical research networks (i.e., PECARN, SIREN), and have research expertise in several other disciplines within EM. There are substantial opportunities for leadership and growth within the Department and UCSF School of Medicine.
The University of California, San Francisco (UCSF) is one of the nation’s top five medical schools and demonstrates excellence in basic science and clinical research, global health sciences, policy, advocacy, and medical education scholarship. The San Francisco Bay Area is well-known for its great food, mild climate, beautiful scenery, vibrant cultural environment, and its outdoor recreational activities.
PLEASE APPLY ONLINE AT: https://aprecruit.ucsf.edu/apply/JPF05161
UCSF seeks candidates whose experience, teaching, research, and community service has prepared them to contribute to our commitment to diversity and excellence. UCSF is an Equal Opportunity/Affirmative Action Employer. The University undertakes affirmative action to assure equal employment opportunity for underrepresented minorities and women, for persons with disabilities, and for covered veterans. All qualified applicants are encouraged to apply, including minorities and women. For additional information, please visit our website at http://emergency.ucsf.edu/
Check companies advertising jobs on SAEM’s EM Job Link against your LinkedIn contacts. Leverage professional connections for more information about the company or request a referral.

Whether
GREGG MOJARES, DO, FACEP Vice Chairman, Emergency Department

We offer leadership and staff positions at leading children’s hospitals, academic medical centers and teaching hospitals nationwide.
Rewarding and sustainable careers begin with caring for ourselves and each other. We foster collegial environments where physicians can find the perfect fit for their professional development, personal well-being and scheduling needs.
Medical City Children’s Hospital at Medical City Dallas
PEM fellowship or 4-year dual EM residency
K. Hovnanian Children’s Hospital at Jersey Shore University Medical Center, Neptune

May 13-16, 2025 | Philadelphia Marriott Downtown