
8 minute read
Uncommon conditions: Cushing’s disease
At age 25, Amy Stracey was diagnosed with Cushing’s disease, a very serious but hard to diagnose disease. Following treatment and surgery from the QEII’s endocrinology care team, Amy returned to school and is now a registered nurse. QEII Foundation
Uncommon conditions
Advertisement
QEII’s collaborative response to treating Cushing’s disease
By Allison Lawlor
Amy Stracey was a fit young woman in the Canadian Forces when a rare disease turned her life upside down. Thanks to her strong determination to recover, coupled with the expertise of her medical team at the QEII Health Sciences Centre, she not only made a full recovery, but also returned to school motivated to help others living with health conditions. Having successfully completed basic training and posted to CFB Shearwater, Amy started noticing she was losing significant muscle tone and gaining weight. “I thought I should be getting stronger, but I was getting weaker,” she says. Her muscles ached, she had swelling in her body and her face became moon-shaped. She went to see her doctor and he recommended a weight loss program. She persisted, knowing something wasn’t right in her body. She was eventually referred to Dr. Ali Imran, an endocrinologist at the QEII’s Halifax Neuropituitary Clinic. In 2010, at age 25, she was diagnosed with Cushing’s disease. She was 240 pounds, more than 100 pounds above her normal weight. Until now, she had always been healthy and fit. “Cushing’s is a very serious disease,” says Dr. Imran. “But in the early stages, it is hard to diagnose.” It is not a common disease. In Nova Scotia, QEII specialists see between three and five new cases each year. In people with Cushing’s disease, a non-cancerous tumour in the pituitary gland produces too much ACTH, a hormone that causes the adrenal glands to make cortisol. Cortisol is often called the body’s stress hormone. The disease can go undiagnosed for years and if left untreated, can lead to other health conditions such as bone fractures, diabetes, high blood pressure and even death. “There are people walking around with this condition who don’t even know they have it,” says Lisa Tramble, a registered nurse in the QEII’s Halifax Neuropituitary Clinic. Five days after Amy was diagnosed, she went in for surgery. Dr. David Clarke, the QEII’s chief of neurosurgery, and Dr. Emad Massoud, an otolaryngologist at the QEII, performed the surgery endoscopically with an illuminated optical, tubular instrument used to look into the body. Accessing the tumour through the nose, no incisions were needed. During the surgery, a hole was drilled into the base of the skull to gain access to the pituitary gland. Using a small scalpel, Dr. Clarke removed the small tumour. Given the nature of Cushing’s, tumours can be as small as two millimetres in diameter and hard to detect. The surgery was a success. Two months later, Amy ran a five-kilometre race in the Scotiabank Blue Nose Marathon wearing a t-shirt with a photo of herself and the words, “Running for Cushing’s.” Amy was medically released from the military. She lost the weight she had gained and returned to school with the dream of becoming a nurse. “I knew I wanted a career where I could give back,” she says. Last year, Amy graduated from Dalhousie University and is now a registered nurse at the QEII’s hemodialysis unit. Grateful for the care she received from the endocrinology clinic, she thinks she might like to work there one day. “I know I would have to learn a lot,” she says.
Close to 20 years ago, Drs. Imran and Clarke started working closely together, knowing that by combining their expertise they could better serve patients. “We wanted to provide them with one-stop care,” says Dr. Imran. Dr. Clarke agrees. Instead of having multiple appointments on various days to different specialists, patients, like Amy, have their diagnosis and medical care coordinated and streamlined to reduce the number of visits and tests required. As many as 1,800 pituitary patients are followed, providing the doctors with a valuable resource for their research and ability to continually improve the care they provide. “Our clinic really has become a model for other clinics across the country,” says Dr. Clarke, who co-chairs the Halifax Neuropituitary Program with Dr. Imran. “We have been a leading centre in pituitary disease in the country over the last decade.”
Thankful for her recovery from Cushing’s disease, Amy is equally thankful for the care she continues to receive from the team at the QEII. “I feel like I am my old self,” she says.


Continued from Page 2
committed to improving patient care, research and advocacy of thyroid cancer across the country. Currently, CANNECT has 12 centres in eight provinces and they collect data on patients from across the country including 1,400 patients in Atlantic Canada, 3,000 in Winnipeg and another 3,000 in London, Ont., to create one large database that has become an invaluable resource. The Blue Butterfly Evening and Carol are a big part of that. “The event would not exist if it weren’t for Carol,” Dr. Rajaraman explains. Because thyroid cancer is not a high-profile cancer, and it is very survivable in most cases, it tends to be left behind when it comes to awareness and funding. Dr. Rajaraman says this is why the yearly event is so crucial. All of those funds stay within the community and go directly to helping Atlantic Canadians. Donations and sponsorship for the event are on the rise and include contributions from community members, local businesses, large corporations and Saint Mary’s University, who has donated the venue space since the event began. The Blue Butterfly Evening is much more than a fundraiser. It is one of the most unique wine tasting events in Atlantic Canada, according to Carol. And Dr. Rajaraman says the event and the ITOC team have become a family. “It is really an acknowledgement for the healthcare team and patients, all of whom rarely get acknowledged for the vital work they do to bring awareness to the issue and

Dr. Mal Rajaraman (left), QEII radiation oncologist, and Dr. Ali Imran (right), QEII endocrinologist, are part of the QEII’s Interdisciplinary Thyroid Oncology Clinic (ITOC). The ITOC partnered with Carol Dodds (centre), thyroid cancer survivor, to raise awareness and funds for vital research and thyroid cancer care at the QEII through the Blue Butterfly Evening event. QEII Foundation
improve care and treatment,” he adds.
The ITOC, which has quickly become a recognized centre for excellence in thyroid cancer care and treatment, includes Dr. Rajaraman; Dr. Ali Imran, an endocrinologist; Dr. Steve Burrell, a nuclear medicine physician and Dr. Jonathan Trites, a surgeon — each of whom are thyroid cancer clinical leads in their departments at the QEII. The ITOC also includes dedicated nurses, pathologists and other clinicians that create a one-of-a-kind clinic where patients can see all of the key team members in one visit instead of having to travel numerous times for appointments over what can be many months. Since it began, the Blue Butterfly Evening event has helped raise $383,257 net. Apart from the database, plans for the funds include improving the reliability of ultrasound reports for thyroid nodule evaluation, as well as several smaller projects designed to advance thyroid cancer treatment and care.
THE NEW ALL-ELECTRIC I-PACE
SEE A JAGUAR CHARGE.

Sail into your new adventure.

THE 2019 VOLVO XC60

S TA R T I N G F R O M


$46,700 *
Banking blood
QEII hematopathologists create world-leading blood bank algorithm
By Allison Lawlor
Dr. Calvino Cheng and Dr. Jason Quinn have developed an innovative method to dramatically reduce red blood cell product waste at the QEII Health Sciences Centre. Without an adequate supply of the precious resource, patients couldn’t receive surgeries, chemotherapy or blood transfusions.
The QEII hematopathologists found a way to optimize blood ordering for the red blood cell inventory by using data from inpatients at the health centre in a more innovative way. “We wanted to find a way to help save blood,” says Dr. Cheng, the outgoing medical director of the blood transfusion services at the Nova Scotia Health Authority’s Central Zone in Halifax and medical director of the Pathology Informatics Group. After noticing that the blood bank was still expiring around two per cent of its red blood cell products, Dr. Cheng and his collaborators developed an algorithm that looks at hemoglobin levels of all admitted patients. It then determines the probability for transfusions in the centre within the next 48 hours, calculates what blood was historically used and then projects what will be needed. All of this
BLOOD - Page 15
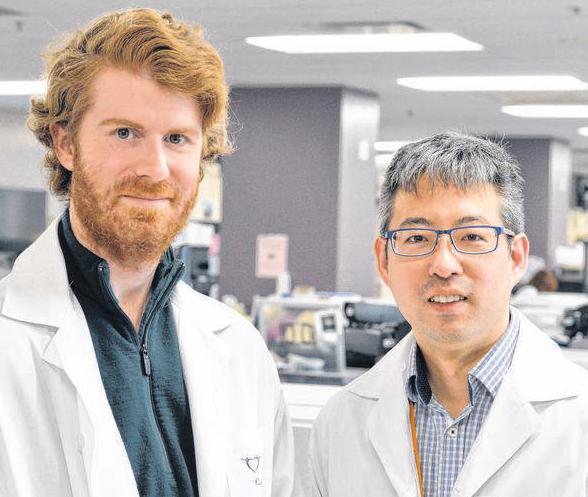
Dr. Jason Quinn (left) and Dr. Calvino Cheng (right), QEII hematopathologists, have developed a way to optimize blood used for transfusions by using data from inpatients at the QEII in a more efficient way. QEII Foundation
THE WORLD’S FIRST LUXURY COMPACT SUV – REDEFINED



2020 Range Rover Evoque
$ 47,000 * Starting from





