14 minute read
RESEARCH & INNOVATION
Research shows exercise improves overall well-being and quality of life for cancer survivors
By Cynthia McMurray
Advertisement
Decades of research show “taking it easy” is not always the best prescription for healing. While there are obvious contraindications, a new research study is looking at how exercise impacts the overall well-being of cancer patients and survivors. Activating Cancer Communities through an Exercise Strategy for Survivors (ACCESS) is a free exercise program designed to lessen the impact of a cancer diagnosis and its treatments on the health and well-being of individuals confronted with the disease. Launched in September 2018, ACCESS is already having a huge impact, according to Dr. Melanie Keats, a professor with the School of Health and Human Performance at Dalhousie University, affiliate scientist in the Department of Medical Oncology, and a three-time cancer survivor. As one of the principal investigators for ACCESS, Dr. Keats works closely with co-investigator, Dr. Scott Grandy, an associate professor at Dalhousie and affiliate scientist in the Department of Cardiology at the QEII Health Sciences Centre. Together they hope to not only support the current research that irrefutably shows regular exercise is a vital, yet often neglected, piece of the cancer treatment and care journey, but also how it can be feasibly implemented into real-world situations. “ACCESS will help us translate the exercise evidence into care to ensure exercise becomes part of the standard treatment for all cancer patients and survivors,” says Dr. Grandy. One of those patients is
Living with colon cancer since 2015, Andrea Davidson joined the new ACCESS program at the QEII in October 2018. ACCESS will help researchers translate exercise evidence into care to ensure physical activity becomes part of the standard treatment and care for all cancer patients and survivors. QEII Foundation
Andrea Davidson, a Halifax native originally diagnosed with colon cancer in July 2015. Referred by her oncologist, Andrea joined ACCESS in late October 2018. “In December 2017, I fell in the bathtub and broke my arm. That arm healed, but my other arm took up all the phantom pain,” she explains. Andrea also broke her pelvis. “I was in a lot of pain, but exercise got rid of it,” she says. Andrea’s results are not surprising according to both Dr. Keats and Dr. Grandy, which is why they are so passionate about ACCESS. The ACCESS program received funding from the QEII Foundation through Dragon’s Den, part of the Nova Scotia Health Authority Central Zone’s Perioperative Education Day. When the Dragon’s Den opportunity presented itself, they rose to the challenge much like contestants in the TV show. “There was a short proposal sent in advance that included a financial impact statement showing how this would affect cost and patient care and they selected the top four who were invited to pitch to the Dragons,” says Dr. Grandy. Ultimately ACCESS won first place, receiving $50,000 over two years.
Since launching ACCESS, Dr. Keats says they have had more than 160 referrals — 78 per cent from clinicians with the remainder being self-referrals. Participants attend one of three locations: the QEII’s Victoria General site, the Rath Eastlink Community Centre in Truro, or the Canada Games site in Clayton Park, where they typically attend 24 free sessions over 12 weeks, most coming twice per week. “This trial is different than a standard clinical trial where you say, ‘here is an exercise program. Does it improve fitness markers in this patient population?’ We are still looking at patient outcomes, such as quality of life and reduced fatigue, but with a typical research study, everyone would get the same exercise regimen,” explains Dr. Keats. “Here, every individual works on the same components of the exercise program — cardiovascular fitness, strength, balance, flexibility — but one person might be running on the treadmill, whereas another may be on the bike pedalling slowly or going for a short walk.” “They are at very different levels that depend on what they are able to do on any given day,” she says. Dr. Keats says participants use the Green-Yellow-Red Light Program. “Green light — great day — let’s go for it. Yellow light? Not quite as good as a green-light day, so we bring it back a bit. Red light doesn’t mean stop, it just means let’s move and do something but at a very low level,” she says. Andrea comes to the QEII at least once per week where she is guided through her personal fitness program that includes the treadmill, exercise bike, free weights, exercise tubing and core strength-building exercises. “I already have more energy. I don’t have hip or arm pain anymore and I can really tell if I haven’t been here. I get wobbly.” Andrea says. “It has given me a real sense of balance again — it makes me feel younger.” “We have 30 years of evidence that says exercise is safe, feasible and we should be doing it. Yet very few places offer exercise programs for cancer survivors,” Dr. Grandy explains. “We need to make the leap between what we know and what we are doing, and this trial makes that leap.” Participants range from people who believe in exercise, to those that think it is a waste of time but their doctor told them to try it. Dr. Grandy says that no matter where you may fall on that spectrum, the bottom line is that doing anything is better than nothing. “The number of cancer diagnoses in the next 15 years is going to increase by 78 per cent, so the impact on the healthcare system will be astronomical,” says Dr. Keats. “If we can help patients better cope with their treatment, prevent or manage other health conditions, and reduce their time in the hospital, maybe we can help mitigate some of that burden for everyone.” “Exercise really is tremendous. I may have no control over this cancer — it just does what it wants — but I can help fight it the stronger I am and exercise does that,” says Andrea. For more information about ACCESS, look for them on Facebook, Instagram or Twitter @ACCESSforWellness, contact 902 473 2035 or access.wellness@nshealth.ca.
Accessing MRI when it matters most
QEII first to have new technology
By David Pretty
In March 2019, the QEII Health Sciences Centre received delivery of the Evry* MRI machine, a unique instrument designed to provide point-of-care diagnostic information for patients in the emergency department. Funding for this project includes $700,000 from Atlantic Canada Opportunities Agency, $1.26 million from the Research Nova Scotia Trust and $1.4 million of in-kind contributions from Synaptive Medical, Evry’s manufacturer. Currently, due to safety and design restrictions, MRIs are often housed far away from emergency departments. But according to Dr. Steven Beyea, scientific director for the Biomedical Translational Imaging Centre (BIOTIC) at the QEII, these same limitations are precisely what inspired Synaptive Medical to design the Evry device. “They’ve attempted to re-engineer what an MRI looks like,” he says. “For example, they’ve gotten rid of the requirement for thousands of litres of liquefied helium, a limitation requiring expensive and specialized building ventilation, improving the ability for the machine to sit within the point of care.”
This collaborative research partnership with Synaptive Medical will allow Dr. Beyea’s

team to be the first in the world to evaluate the potential impact this new technology could have on emergency medicine patients at the QEII, and beyond. “This partnership is about being the first to access this technology,” he says. “Synaptive Medical is seeking a collaborative partnership with our healthcare system, and in doing so they’re investing in Nova Scotia.” While giving local healthcare professionals an opportunity to work hands-on with leading-edge technology, as well as the economic development opportunities, Dr. Beyea believes the province could see a broad spectrum of benefits. Evry is expected to be up and running by early fall. After the installation, BIOTIC will begin research to evaluate the value the instrument could have to physicians and patients at the A collaborative research partnership with Synaptive Medical, including Michelle MacPherson (left), director of MRI Product Development, Synaptive Medical, and Alex Panther (right), director of MRI Research & Development, Synaptive Medical, will allow Dr. Steven Beyea (centre) and his team at BIOTIC to be the first in the world to evaluate the potential impact this new technology could have on emergency medicine patients at the QEII, and beyond. Contributed
QEII’s Charles V. Keating Emergency and Trauma Centre, and to the healthcare system more broadly. “Given that this is a brand new form of MRI, the goal is to make evidence-informed decisions about whether this should or should not someday become a standard of care within the emergency medicine department,” Dr. Beyea says. This will involve working in close conjunction with Synaptive Medical.
“We’ve worked with the company and various clinical partners to develop a four-year collaborative research program specifically aimed at evaluating whether, or if, this new technology provides value to the healthcare system in a variety of different ways,” Dr. Beyea explains. For Dr. Matthias Schmidt, a neuroradiologist at the QEII, the potential advancement of MRI technology is an exciting prospect. “MRI gives me an opportunity to learn about tissue structure detail and function,” Dr. Schmidt says. “It’s a very versatile procedure that can get into anatomy, physiology and biochemistry and be very sensitive for subtle diseases.” This in turn, makes MRI an ideal point-of-care device. “When a patient comes in with an acute neurological symptom the question is: Is this because of a stroke or an inner ear problem?” says Dr. Schmidt. “If it’s a stroke, the patient should be admitted and treated by neurology, but if it’s an inner ear problem then they can be treated
MRI - Page 15
Jennifer’s Mobile Hair Services Hair Services in Your Home
starting at $ 25 Cuts
Big data and artificial intelligence to drive health care forward
By Cynthia McMurray
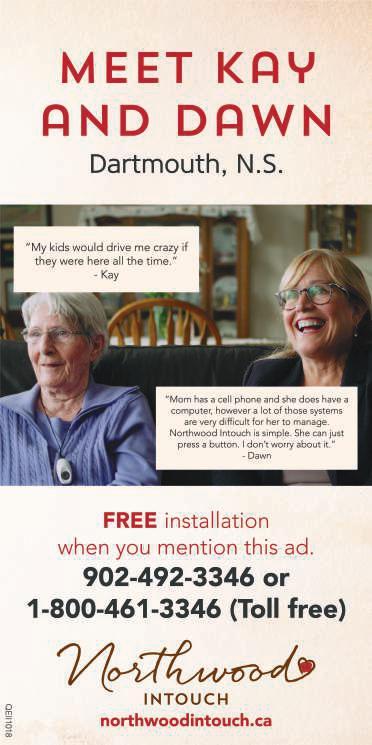
When most people hear the term artificial intelligence (AI), they have a futuristic image ripped straight from the latest action/sci-fi movie in which robots take over the world. But nothing is farther from the truth, according to Dr. Leonard D’Avolio, an assistant professor at Brigham and Women’s Hospital at Harvard Medical School. Dr. D’Avolio was invited to be a keynote speaker at the Dalhousie Medical Research Day in April 2019 by Dr. Michael Dunbar, an orthopaedic surgeon at the QEII Health Sciences Centre, director of Dalhousie University’s Department of Surgery Research and QEII Foundation Endowed Chair in Arthroplasty Outcomes. Sponsored by the QEII Foundation, Dr. D’Avolio spoke about big data and building the machine learning system. Dr. D’Avolio is a software engineer and the co-founder of a performance improvement organization called Cyft, which uses data and AI to improve clinical care and operations. He says there is nothing to fear with AI and big data. In fact, if anything is to change and improve in today’s healthcare system, we will need to fully embrace this inevitable shift in technology. “Unfortunately, the way it is positioned now, it is sort of ‘robot versus man’ and the stage is set for AI to go to war against doctors to revolutionize health care,” he says. “But AI is neither artificial, nor is it intelligent. It’s just math.”


Dr. Leonard D’Avolio (left), an assistant professor at Brigham and Women’s Hospital at Harvard Medical School, was invited to be a keynote speaker at the Dalhousie Medical Research Day in April 2019 by Dr. Michael Dunbar, a QEII orthopaedic surgeon, director of Dalhousie University’s Department of Surgery Research, and QEII Foundation Endowed Chair in Arthroplasty Outcomes. Dr. D’Avolio spoke about big data and building the machine learning system. QEII Foundation
Dr. D’Avolio, who has family connections in Nova Scotia, offers the example of maps.
“In the past, we had paper maps. You could pull it out of your pocket to understand the lay of the land,” he says. “Now we have Google Maps. We still have maps — the underlying data — but when AI and big data come together, they give us new abilities.” This data goes beyond simply



allowing us to see which roads connect. We can now see what the traffic is like in real time and if you take route A versus route B, which route will you get there faster. “This is a really profound opportunity. It’s a new capability — not a new tool, not a new technology,” he explains. “The super power that we now have access to, and we are now just beginning to scratch the surface of, is that we can learn in ways that were never before possible.” “What area of health care wouldn’t be affected by the opportunity to learn faster, better, in real time?” And that is really what it boils down to, according to Dr. Dunbar.
BETTER - Page 15



QEII Foundation raises $4 million to bring Atlantic Canada’s first hybrid OR to the QEII
Equipment and technology within surgical suite completely donor-funded
By Nicole Topple
Within one year, the QEII Foundation – in collaboration with the Maritime Heart Centre – has raised $4 million towards Atlantic Canada’s first hybrid operating room (OR) at the QEII Health Sciences Centre. The announcement, which was unveiled at the QEII Foundation’s Heart Heroes event on May 15, 2019, revealed that all of the technology and equipment within the new leading-edge operating suite will be completely donor-funded. At Heart Heroes, Danny Chedrawe, who is a longtime supporter of the QEII Foundation and Honorary Trustee, and Stewart E. Allen, who made a $1-million gift in support of the hybrid OR, were both honoured with Heart of Gold awards for their visionary support of heart health care. A hybrid OR is one of the most technologically-advanced operating suites available today –allowing surgical care teams to perform diagnostic imaging, minimally invasive procedures, and complex, open surgeries all in the same room, at the same time. This is especially important when treating trauma patients like car accident victims or if an emergency situation arises in the OR, as patients will no longer need to be transferred to other units or care teams for imaging procedures. “By establishing Atlantic’s Canada first hybrid operating room, the QEII will be a leader in eliminating the physical divide between the operating room and essential diagnostic imaging,” says Dr. Gerald MacKean, the QEII’s division head of vascular surgery. “The technology funded by QEII Foundation donors will be paramount to delivering the most innovative and effective care for patients.” Thanks to donors, the region’s first hybrid OR will be fully outfitted with state-of-the-art surgical and imaging technology, which will ultimately drive more complex and cutting-edge procedures, smaller incisions, less stress on the heart, and shorter recovery times for patients. “Ensuring Atlantic Canadians have the most innovative and advanced care in our region is what inspires our donors to support projects, like the hybrid OR,” says Lydia Bugden, vice chair of the QEII Foundation’s Stewart E. Allen, who made a $1-million gift in support of the QEII’s hybrid OR, was honoured at the QEII Foundation’s Heart Heroes event on May 15, 2019. The Heart of Gold award recognizes his visionary support of heart health care. QEII Foundation
Board of Trustees and chair of the heart campaign. The QEII is one of the top 20 health centres in Canada and one of 17 academic teaching hospitals across the country. According to Lydia, access to a hybrid OR will allow the QEII and its world-class teams to continue to elevate heart health care and help set standards from coast-to-coast. Government has approved $32.2 million for the construction and renovation of the third and fifth floors at the QEII’s Halifax Infirmary, which includes the addition of the new hybrid OR. With the QEII Foundation contributing $4 million to fund all of the advanced technology to bring the surgical suite to life, the impact for QEII patients and their families will be significant. Construction is currently underway on the new hybrid OR, which is slated to open and treat its first patients in fall 2020.