ACMS is Taking Action on Physician Wellness

Congress Pushes
Value-Based Medicare
Reimbursement

ACMS is Taking Action on Physician Wellness

Congress Pushes
Value-Based Medicare
Reimbursement
When your patients need specialty care, AHN has physicians with the right expertise — like our new surgical oncologist.
Dr. Chalikonda uses the most advanced minimally invasive surgical techniques to remove cancer, and to ensure the fastest and best possible outcomes.

To refer your patient, call 412-359-3115
Most major insurance plans are accepted.
Surgical Oncology
Location: AHN Allegheny General
Specialties : Expertise in diagnosing and treating patients with cancerous conditions of the pancreas and stomach
Performs minimally invasive surgical procedures and HIPEC cancer treatment
Editorial....................................5
• Fall Nourishment

Deval (Reshma) Paranjpe, MD, MBA, FACS
Editorial ..................................8
• War Stories
Richard H. Daffner, MD, FACR
ACMS Photo Contest ............11
Perspective............................12
• Imposter Syndrome
Timothy Lesaca, MD
Perspective ............................14
• Baseball and Old Lace: The Hope Which Springs Eternal
Social and Legislative
In Memoriam...........................27
Materia Medica ......................18
• Terlipressin (Terlivaz®): The First Medication to be FDA Approved for the Treatment of Hepatorenal Syndrome (HRS)
Foundation..................29
Bylaws
Lauren Maurer, Doctor of Pharmacy Candidate, University of Pittsburgh School of Pharmacy, Pittsburgh, PA
Legal Summary....................22
• Congress Pushes Value-Based Medicare Reimbursement
William H. Maruca, Esquire ACMS Meeting Schedule ......32
2023
Executive Committee and Board of Directors
President
Matthew B. Straka, MD
President-elect
Raymond E. Pontzer, MD
Secretary
Keith T. Kanel, MD
Treasurer
William Coppula, MD
Board Chair
Peter G. Ellis, MD
Term Expires 2023
Michael M. Aziz, MD
Micah A. Jacobs, MD
Bruce A. MacLeod, MD
Amelia A. Paré, MD
Adele L. Towers, MD
Term Expires 2024
Douglas F. Clough, MD
Kirsten D. Lin, MD
Jan B. Madison, MD
Raymond J. Pan, MD
G. Alan Yeasted, MD
Term Expires 2025
Anuradha Anand, MD
Amber Elway, DO
Mark Goodman, MD
Elizabeth Ungerman, MD
Alexander Yu, MD
G. Alan Yeasted
Bylaws
Keith .T. Kanel, MD
Finance
William Coppula, MD
Nominating
Raymond E. Pontzer, MD
Medical Editor Deval (Reshma) Paranjpe (reshma_paranjpe@hotmail.com)
Associate Editors
Douglas F. Clough
Richard H. Daffner (rhdaffner@netscape.net)
Kristen M. Ehrenberger (kricket_04@yahoo.com)
Anthony L. Kovatch (kovatcha42@gmail.com)
Joseph C. Paviglianiti (jcpmd@pedstrab.com)
Andrea G. Witlin (agwmfm@gmail.com)
ADMINISTRATIVE STAFF
Executive Director
Sara Hussey (shussey@acms.org)
Vice President - Member and Association Services
Nadine M. Popovich (npopovich@acms.org)
Manager - Member and Association Services
Eileen Taylor (etaylor@acms.org)
Co-Presidents
Patty Barnett
Barbara Wible
Recording Secretary Justina Purpura
Administrative & Marketing Assistant Melanie Mayer (mmayer@acms.org)
Director of Publications Cindy Warren (cwarren@pamedsoc.org)
Part-Time Controller
Elizabeth Yurkovich (eyurkovich@acms.org)
Corresponding Secretary
Doris Delserone Treasurer
Sandra Da Costa
OFFICES: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212; (412) 321-5030; fax (412) 321-5323. USPS #072920. PUBLISHER: Allegheny County Medical Society at above address.
The Bulletin of the Allegheny County Medical Society is presented as a report in accordance with ACMS Bylaws.
The Bulletin of the Allegheny County Medical Society welcomes contributions from readers, physicians, medical students, members of allied professions, spouses, etc. Items may be letters, informal clinical reports, editorials, or articles. Contributions are received with the understanding that they are not under simultaneous consideration by another publication. Issued the third Saturday of each month. Deadline for submission of copy is the SECOND Monday preceding publication date. Periodical postage paid at Pittsburgh, PA.
Bulletin of the Allegheny County Medical Society reserves the right to edit all reader contributions for brevity, clarity and length as well as to reject any subject material submitted. The opinions expressed in the Editorials and other opinion pieces are those of the writer and do not necessarily reflect the official policy of the Allegheny County Medical Society, the institution with which the author is affiliated, or the opinion of the Editorial Board. Advertisements do not imply sponsorship by or endorsement of the ACMS, except where noted.
Publisher reserves the right to exclude any advertisement which in its opinion does not conform to the standards of the publication. The acceptance of advertising in this publication in no way constitutes approval or endorsement of products or services by the Allegheny County Medical Society of any company or its products.
Annual subscriptions: $60
Advertising rates and information available by calling (412) 321-5030 or online at www.acms.org.
Assistant Treasurer
Liz Blume
COPYRIGHT 2023: ALLEGHENY COUNTY MEDICAL SOCIETY
POSTMASTER—Send address changes to: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212.


The weather’s turning, but that means good things for your palate. New and exciting restaurants are popping up all over Pittsburgh—take advantage of the cool weather to check out some new and almost-new hotspots.
Ross Township boasts the greatest number of new openings of late:
Hong BBQ & Hot Pot
4801 McKnight Road, Ross Township
Coming soon---an all-you-can-eat chain Korean Barbecue/Chinese Hot Pot restaurant with multiple Florida locations. For $30.99 for adults and $15.99 for kids, you can pick either BBQ or Hot Pot, or for an extra fee you can try both. You are the chef and get to flash cook your food. Don’t waste food though---they’re serious about that warning and will charge you $13.99/ lb for wasted food. Beer and wine are inexpensive and you can get an impressive array of proteins, vegetables, noodle and bubble teas.
Ross Cafe
4846 McKnight Road, RossTownship
Turkish breakfast in Pittsburgh! This alone should get you to try this café featuring traditional Turkish favorites (think kebabs and grilled chicken, lamb and seafood dishes) as well as standard American fare. Try the pistachio cream waffles, the sigara boregi (fried phyllo stuffed with cheese and parsley), or one of the many enticing combo plates. Delivery available!

Barrio Tacos + Tequila + Whiskey Ross Park Mall, Ross Township
Barrio Tacos + Tequila + Whiskey is an Ohio-based chain whose Pittsburgh outpost is located inside Ross Park Mall, between L.L. Bean and The Cheesecake Factory. Featuring “build your own tacos in six steps” with a dizzying array of proteins ranging from Coca-Cola marinated steak to chorizo to jalapeno lime shrimp and bbq gochujang tofu-- and shells, sauces and toppings to match. Enjoy specials on the dog-friendly patio as you gaze up at Frida Kahlo.
Eiwa Japanese Ramen & Bar 4860 McKnight Road, Ross Township
Authentic Japanese fare including hakata tonkatsu ramen, spicy miso ramen, pork gyoza, and donburi/rice bowls, as well as pan-Asian cuisine. Soft opening in progress.

From Page 5
City Kitchen
145 Bakery Square Boulevard, Larimer
A change in management for the Galley food hall at Bakery Square has renamed it City Kitchen. The concept remains the same—multiple culinary options with a communal bar. Options include Elevate, SOMI, Bahnmilicious, Al Dente and Pisco and Lime (Peruvian fusion). Look for a gourmet burger bar and Hawaiian smoked meats via on-site smoker and charbroiler.
1627 Smallman Street, Strip District (Terminal Building)
The NYC-based winery, restaurant and performance space chain now has a spot in The Terminal. The venue has more than a dozen house wines on tap and features a globally influenced menu focused on small, shareable plates that are meant to complement the vino. The concert hall includes a balcony and seats about 250 spectators.
Essence Cafe
1924 East Carson Street, South Side
Check out this stylish vegan eatery open Thurs-Sun 12-10pm for a vegan world tour, featuring a selection of Middle Eastern, African, Indian and American dishes masterminded by Chef Ojok Grichang.
520 E. Ohio Street, North Side
Now this you need to try. The owners of the stellar Fig and Ash turned the space next door into a nostalgia-laced eatery that will make you feel like you stepped back in time to a 1970s and 1980s childhood. The fare is both reasonably priced and Fig and Ash quality, which will also blow your mind. Live events such as Wednesday Bluegrass nights, cornhole, awards and mocktails add to a sense of childlike fun alongside seriously good food.
KPOT
1816 Murray Avenue, Squirrel Hill
This national all-you-can-eat Korean barbecue chain restaurant will be opening a Squirrel Hill location shortly. .
Jackworth Ginger Beer Brewery
6615 Hamilton Avenue, Larimer
Oh great, you say: yet another brewery opening up!. Before you yawn, not so fast---this one brews both alcoholic and non-alcoholic GINGER beers. A full bar serving a wide array of drinks is on site, and I’d bet that the Dark and Stormy (ginger beer, Bermudian black rum) will be a de rigeur cocktail.

CoNectar
411 Grant Ave, Millvale
Put this on your honey-do list. This is a nectar bar (you heard that right) that will be serving small plates curated to accompany local honies.
Balvanera
1600 Smallman Street, Strip District
Something to look forward to indeed—this large Argentinian brasserie, whose first location is in Manhattan, will feature traditional Argentinian food, South American wines, and craft cocktails. Brought to you by a native Pittsburgher teamed up with Buenos Aires native; this will make your taste buds tango.
Go forth, and eat well.

Earlier this year, the PAMED Board of Trustees created a task force to address the issue of emergency department (ED) overcrowding in Pennsylvania. Led by PAMED President -Elect, Kristen Sandel, MD, the task force issued a letter to Governor Shapiro , urging him to address this issue at a state level. The ACMS was pleased to sign on to the final version of this letter that was submitted to the Governor on August 9.

PAMED has launched a webpage dedicate to this initiative, with resources available for Physicians and the Public:
www.pamedsoc.org/laws -advocacy/pamed-priorities/ed -overcrowding
The breadth of this issue is dauntingan issue that has taken decades to develop, only to be exacerbated by the COVID-19 pandemic. We ask you to share your personal story of being affected by emergency department overcrowding and ask your legislators to urge the Governor to address the root causes and ensure Pennsylvania citizens have better access to care, lower mortality rates and increased quality of care.

Iremember that when I was a child, I often heard my father and many of his friends talking about their military service during World War II. Most of these men had seen combat in Europe. My father had tried to enlist but found that he was too old for active duty. Instead, he joined the New York National Guard. My father was a pharmacist, and consequently, he was assigned to a medical unit. (He often said that he had fought in the “Second Battle of Saratoga”.)
I served for two years as a member of the United States Air Force1. During my residency and subsequent practice positions I encountered many colleagues who had also been in the military. It was not unusual, therefore, that sometimes the lunchtime chatter would include our own war stories. Although the men of my father’s generation and ours had done our military service at different times, the contents of the stories that we told one another were very similar. Specifically, at no time, with one exception, did any of my father’s friends talk about their combat experiences. (The one exception was an incident where, during an air raid, my father’s friend dove under a wagon to shelter himself and landed in a fresh steaming pile of horse manure. That explained why he had the nickname of “Stinky”.) Post
traumatic stress disorder (PTSD) as it is now called today, was unknown to that generation. The medical personnel of the time referred to PTSD as “combat fatigue”. Instead, virtually all the stories that were told were humorous2,3. For example, one of my father’s favorite stories was about the night that he and a friend decided to raid the mess hall for a few snacks. Unfortunately, a sentry had been posted in the area and when he saw the two soldiers approaching, he gave out a challenge. Instead of saying “Who goes there?”, He said, in his Brooklyn accent, “Who dat?” My father’s friend replied, “Who dat”? The befuddled sentry responded to this by shouting “Who dat what say “Who dat’?” I recall the laughter in the room whenever my father told that story.
And so, I’d like to share a few of my own war stories.
I was fortunate that, as a physician, I did my service as an officer, with the rank of Captain. Basic training was performed at Sheppard Air Force Base in Wichita Falls, Texas, along the Oklahoma border (fig. 1). During the three-week course my class of physicians, dentists, nurses and one optometrist learned the military protocols that transformed us from civilian to military life. One aspect they emphasized was the separation of officers from enlisted men. I will admit now that the instructors at OBMTM (Officer Basic Military Training Medical) did a fantastic job of making a group of mostly reluctant participants (the physicians) “rah-rah” Air Force by the time we left.
I arrived at my permanent assignment, Wright-Patterson Medical Center, near Dayton, Ohio, with two other physicians from my basic training class. The first thing we did was an orientation session with our supervisor, Dr. Joe Clift. Joe had been there for a year and was the senior physician in the General Medical Clinic, where we were assigned. Among the many things Joe told us was to ignore all the “BS” we had been given at Sheppard about the relations between the officers and enlisted personnel. “Here the sergeants run everything,” he said. “They may

ask you to do some things you think are strange. I’m not going to tell you what to do. You can decide on your own. However, my advice is that if you play ball with the sergeants, they will make your stay here as comfortable as possible.” And with that, we were dismissed to set up our offices.
Within ten minutes of entering my office, there was a knock on the door, announcing the arrival of Master Sergeant Hogue. He, like all the senior non-commissioned officers (NCOs) was carrying a clipboard. After the introductions and welcomes were made, he asked me if there was anything I needed. I thanked him and said that I thought I was set. He turned to leave, and just as he was getting ready to go through the door he turned, and like a scene out of an episode of the TV show “Columbo”, he said, “Just one more thing, sir. Would you mind signing this requisition for me?”
I looked at the requisition and replied, “But Sarge, it’s blank.”
“Oh, I wouldn’t worry yourself over that, sir. We’ll fill it in later”.
I gave him a questioning look but took out my pen and signed the requisition. He gave me a crisp salute and said “Thank you, sir. Welcome aboard.” I passed the test. I later learned that the sergeants engaged in extensive bartering with each other, much like what was portrayed in the movie and on the TV show MASH.
Six weeks after my arrival at Wright-Patterson, I was on duty in the emergency room and spotted a fresh face approaching the registration desk.
He was in his dress blue uniform and was wearing medical insignia. His hair was regulation length, and his shoes were shined.
“Welcome to Wright-Pat,” I said. “You must be coming from Sheppard.”
“How did you know?” he asked.
“Six weeks ago, I looked just like you,” I replied.
He looked at my crumpled uniform, scuffed shoes, “Frito Bandito” moustache and long sideburns (I didn’t grow my beard until 1974), and said, “You mean I’ll look like you in six weeks?”
“Probably, if not sooner. Welcome aboard,” I said.
The sergeants and some of the career officers referred to the two-year medical officers as “The Boys from M*A*S*H” after the irreverent 1970 movie, for our unmilitary attitudes. I remember once a group of us were standing outside the base theater following a mandatory “Commander’s Call”. We were approached by a full colonel who told us, “You’re a disgrace to the uniform of the U.S. Air Force. Your hair is too long, and your shoes aren’t shined.”
“Schmuck, who asked your opinion,” Joel, a pediatrician from New York, known by the nickname “The Mouth”, replied.
The colonel saw our medical insignia, realized he was getting nowhere and muttered one of my favorite quotes from the MASH movie, “Goddam doctors” and left. We would hear that appellation many times during our tours of duty.
We were all obligated to the “Doctor Draft” since we had been granted education deferrals to complete our basic medical training. We were, like the doctors in the movie and later the
TV series, reluctant participants in the military but doing our “patriotic duty” nonetheless. Although we resisted the military “spit and polish” we worked well together as a team. Unlike the hostility between medical and surgical specialties we frequently encountered in academic life, we quickly bonded as a true band of brothers. If I called a surgeon in the middle of the night to see a patient, he would come in without making any excuses. The system worked so well that eight of our staff who wanted to practice in Southern California formed a multispecialty group following their discharge.
Members of the armed services are entitled to a significant discount on air fares when flying in uniform. Once, I was waiting at Chicago’s O’Hare airport for a connecting flight back to Dayton, when I encountered Barry, one of my medical school classmates. Barry was stationed at an Indian reservation in Arizona, serving in the U.S. Public Health Service (USPHS)2. The USPHS has a uniform that is virtually identical to that of the Navy, except for different emblems. Both of us were in our “summer tan” uniforms. Barry, however, had shoulder-length hair and a full beard. He was also wearing cowboy boots. While we were talking, I noticed a young Marine staring at us. He looked like he had just stepped off a recruiting poster. His hair was closecropped, the creases in his uniform were perfect, and you could see your reflection in his highly polished shoes. I approached him and said, “Can I help you, Lance Corporal?”
Continued on Page 10
From Page 9
“Yes, sir. What outfit is your buddy in?”
Without a moment of hesitation, Barry said, “The Indians.”
“Is that some sort of special ops?” the Marine asked.
“Oh, yes,” Barry replied. “Very hush-hush.”
The marine saluted us and went on his way. Barry and I chuckled, knowing the stories our newfound friend would tell his buddies.
The birth of one’s first child is always a special occasion. Marc, my oldest son was born several weeks after my arrival at Wright-Patterson, ironically on Labor Day. We were living in Fairborn, Ohio, a suburb of Dayton, literally across the highway from the air base. My wife awoke with her first labor pains around 6 a.m., within an hour the pains were coming every five minutes. On a good day, the house we were renting was a mere seven minutes from the base hospital. The problem was that we had to cross railroad tracks to get to the base and frequently we had to stop and wait for a (long) freight train to pass. As we approached the crossing, I began thinking that there
was a possibility I’d have to deliver the baby myself. Fortunately, there was no train and we made it to the hospital without incident and were directed immediately to the obstetric floor.
I was a General Medical Officer (GMO), ordinarily on the lowest rung of the hospital hierarchy having just completed my medical internship. However, our hospital had several interns, one of whom was rotating on OB. He admitted my wife and took her to a labor room to check the progress of her labor, while I waited in the hallway. Five minutes later he came out, white as a sheet. I knew that was a bad sign.

“What’s the matter?” I asked, with trepidation.
“She’s crowning.”
“So, it looks like you’re going to do the delivery,” I replied.
“Do you know how to deliver a baby?” he asked.
“Of course. Don’t you?”
“No. I only watched a couple of deliveries in medical school.”
“Well, let’s get her to the delivery room and scrub up.” (Thank God for the good clinical training I had at Buffalo.)
While we were scrubbing up, I was
thinking of what an honor it would be to deliver my first child. However, as we were gowning up, in walked “Bud” Carlson, a big teddy bear of a man, the obstetrician. “I had a feeling you’d be here today, so I took a little detour from going to the golf course,” he said. “Go get some coffee, I’ve got this,” he added. And then, he whispered to me, “I’ll show ‘Numbnuts’ here how it’s done.”
And the rest, as they say, is history. I have many more war stories to share. Perhaps I will in a future Editorial.
1. Daffner RH. Remembering the Berry Plan. ACMS Bulletin, May 2020, pp 136 – 138.
2. Strosberg JM. Two Years on the Cheyenne River Sioux Tribe Reservation. Troy, NY, The Troy Book Makers, 2022
3. Daffner RH. “Meatball Medicine”. ACMS Bulletin, Apr 2023, pp 12 – 14.
Dr. Daffner is a retired radiologist, who practiced at Allegheny General Hospital for over 30 years. He is Emeritus Clinical Professor of Radiology at Temple University School of Medicine. He served in the US Air Force from 1968 to 1970.

1 Email your VERTICAL jpg photos with a resolution of 300 dpi or higher to ACMSBulletin@acms.org. Photos should be 8”W x 10”H. No more than three photos may be submitted.
2 You must be an ACMS member physician to submit photos.
3 Include the name of the photo (please keep file names short) as well as your name, specialty, address and phone number in the email.
4 You will receive verification that your photo has been received and is eligible to be entered in the contest.
a) Horizontal photos will not be considered.
b) Photos with low resolution will not be considered.
c) Panoramic shots or photos featuring specifically identifiable individuals relatives will not be considered.
d) Be aware top third of image will be obstructed by Masthead.
5 5 The deadline for submission is Monday, October 3rd, 2023. After this date, a group of individuals selected by the ACMS Board of Directors and ACMS Editorial Board will vote on the top 12 photos.
6 Winners will be announced on the ACMS website, in the Bulletin and via email. The 1st-place winner’s photo will appear on the January 2024 cover; the remaining winning photos will appear on Bulletin covers throughout the year.
7 Please continue to check the ACMS website and future issues of the Bulletin for further updates and reminders.
8 If you have any questions, please contact Contact Cindy Warren at ACMSBulletin@acms.org.
Why do people sometimes feel like frauds despite the abundant evidence of their accomplishments? Rather than internalizing their capabilities and efforts, they attribute their successes to transient and external causes, such as good luck or random chance.
Impostor syndrome is a psychological phenomenon referring to a pattern of behaviors in which people feel unworthy of their accomplishments and have a persistent and internalized fear of being exposed as inferior and undeserving. Antithetical to the concept that realizing your dreams is the pathway to happiness and fulfillment, those with Impostor Syndrome experience insecurity in direct proportion to their achievements.
While early research focused on women, this syndrome has been found to impact adults in equal proportion. Research also suggests that approximately 70% of adults may experience characteristics of this syndrome at least once in their lifetime. Imposter Syndrome was initially described by psychologists Pauline Clance and Suzanne Imes in the 1978 article titled “The Imposter Syndrome in High Achieving Women: Dynamics and Therapeutics.” (1) Clance and Imes observed that those in their study did not experience an internal sense of
satisfaction despite being validated as measured by awards and promotions. These individuals instead described an ongoing internal experience of selfdoubt, accompanied by emotions of guilt and fear.
In 2018, Joel Bothello and Thomas Roulet further elaborated upon the definition of Imposter Syndrome by studying the phenomenon of students who had recently achieved advanced academic degrees and yet credited their accomplishments to luck and contingencies rather than skill and merit, and deemed their professional accomplishments as having minimal societal value. (2)

Dr. Valerie Young, in her 2011 book, “The Secret Thoughts of Successful Women: Why Capable People Suffer from Imposter Syndrome and How to Thrive in Spite of It”, quantified the syndrome into five interrelated subgroups (3). These subgroups are described as follows:
The Perfectionists: Those who set extraordinarily ambitious self-imposed goals and suffered emotionally when not achieving them. The perfectionists were seldom satisfied and seemed unable to have compassion toward themselves.
The Overachiever: Compensating for an internal perception of inadequacy by
working longer and harder at the expense of outside interests and obligations.
The Natural Geniuses: This group experienced a childhood environment in which they were reinforced to believe that they were superior to others and were expected to excel regularly and effortlessly.
The Soloists: Believing that asking for help would reveal personal deficiencies thereby validating their sense of inadequacy.
The Experts: Basing their sense of competence and self-esteem on what they know and accomplish and driven not by the pleasure of learning but rather by fear of being described as inferior.
Theories regarding the etiology of Imposter Syndrome are multiple and include the typical nature verses nurture arguments such as biologic risk factors versus early family dynamics, as well as the introjection of problematic societal stereotypes regarding gender, ethnicity, and financial success. A common denominator for most of these theories, however, involves three pathways of etiology. First is the minimizing of one’s field of productivity, manifested by devaluing one’s work and profession, and negating its influence upon society. Second is the questioning of the intrinsic value of the basic knowledge gained in
one’s occupation, deeming it superfluous and unnecessary. Third is actually experiencing feedback from others who depict your accomplishments as being insignificant. The academic quandary of publish-versus-perish syndrome is a common example in which highly qualified professionals feel invalidated. There is a plethora of articles written on treatment recommendations for Imposter Syndrome. As expected, there is focus on cognitive behavioral therapy techniques, meant to clarify the extent of the difficulties, exploring what interventions have been tried in the past, differentiating the experience of feeling incompetent as opposed to objectively demonstrating ineptitude, and identifying misconceived attributions and perceptions. Common to most treatment approaches, however, are several basic axioms. One must attempt to learn to live within a reasonable expectation of
proficiency. It is impossible to know all things. Similarly, it can be a challenge to take pride in the knowledge one already possesses. Rather than being selfdefined by external parameters such as income or public recognition, there exists the possibility of greater contentment in taking pride in the expression of your natural abilities. Comparing oneself to others is a frustrating journey.
Overcoming Imposter Syndrome is not just a process of challenging the internal mindset but should also incorporate opportunities in which expertise and accomplishments are recognized, particularly in academic and professional environments. Seritan and Mehta, in their publication, “Thorney Laurels: The Imposter Phenomenon in Academic Psychiatry” (4) suggested specific supportive strategies for academic institutions. They involve providing educational workshops on
When joining or leaving a health system.
For information contact John Fenner
Cell: 412-638-1846
Email: fenner@fennercorp.com
Imposter Phenomenon for faculty and staff, greater emphasis on professional mentorship programs, acknowledging aspects of Imposter Syndrome in the academic processes of promotion and remediation, and greater recognition of the syndrome within employment assistance programs.
Imposter Syndrome is a curious paradox. Even though others believe in you, you fail to believe in yourself, and inadvertently invalidate those who seek to validate you. If in doubt, perhaps some useful advice would be when multiple people believe in you, trust them.
(1) Clance, P. R., & Imes, S. A. (1978). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention. Psychotherapy: Theory, Research & Practice, 15(3), 241–247.
(2) Bothello J and Roulet TJ (2019) The imposter syndrome, or the misrepresentation of self in academic life. Journal of Management Studies 56: 854–861.
(3) Young, V. (2011). The Secret Thoughts of Successful Women: And Men: Why Capable People Suffer from Impostor Syndrome and How to Thrive in Spite Of It. United Kingdom: Crown.
Three Penn Center West Pittsburgh, PA 15276 fennercorp.com
Specializing in Hospital and Physician Consulting and Billing Since 1991
(4) (4) Seritan, A.L., Mehta, M.M. (2016) Thorny Laurels: The Impostor Phenomenon in Academic Psychiatry. Acad Psychiatry 40, 418–421.
However, when Doctor Bill Coppula’s family and myself left the stadium after the seventh inning stretch, we worried less about the final score (the home team won big) and more about finding an ideal background with enough light to take the perfect picture to preserve the memory, especially for the grandchildren!

A straggling few got up to go in deep despair.
The rest clung to the hope which springs eternal in the human breast; They thought, “If only Casey could but get a whack at that— We’d put up even money now, with Casey at the bat.”
from “Casey at the Bat” by American poet Ernest Lawrence Thayer (1863-1940)
During the dog days of the summer of 2013, the Andrew McCutchen-led Pittsburgh Pirates were vying for first place in the Central Division of the National League; they were to finish the season 3 games behind the St. Louis Cardinals and ultimately lose to them in the playoffs. Now 10 years later in the dog days of the summer of 2023, the McCutchen-led Pirates are mired in the nether regions of the division, battling the same Cardinals for the basement. However, on July 15, 2023, those of us who attended the ACMS-sponsored night game at PNC Park -- to forget about life and burnout for a while -- did so with the same “hope that springs eternal within the human breast” that made the above poem an iconic treasure of Americana.
Three generations of Pirate fans making a memory at the ACMS-sponsored Pirate game on July 15, 2023. “I have a photograph/ Preserve your memories/ They’re all that’s left you”---from the song “Bookends” by Simon and Garfunkel

We all learn the hard way that whether you win or lose the game, whether you are fighting for first place or last place, the most important thing---perhaps the only thing---is whether the memories made are preserved for posterity. Therefore, in a “lean time” of Pittsburgh baseball 7 years ago, I wrote this story about “Aunt Dorothy,” a distant relative of the family who loved baseball like no other human being was capable. She joined our young family at corporate-sponsored outings (like the ACMS event) to the old Three Rivers Stadium by invitation and taught me “everything I really need to know” about baseball—and about life. The original story, simply entitled “Baseball and Old Lace” was published in the Pediablog on September 1, 2016.
Here is the link to that blog https://www.thepediablog. com/2016/09/01/mind-on-the-run-28
My grandson Miles posing as Shoeless Joe from Hannibal, MO

You’ve gotta have heart
All you really need is heart
When the odds are sayin
You’ll never win
That’s when the grin should start from the 1958 musical comedy “Damn Yankees”
For much of the twentieth century three things were a fixture in the baseball culture of America: the New York Yankees winning the pennant, the venerable Harry Carey singing “Take Me Out to the Ballgame” at the seventh inning stretch of Chicago Cubs games, and the Washington Senators firmly entrenched in the basement of the American League standings. The team’s pitiable lack of success, even lack of mediocrity, inspired a heart-warming play/movie, “Damn Yankees,” featuring the team’s potential savior, “Shoeless Joe from Hannibal Mo.”
But a fictional character could not save the ailing franchise, and eventually the Senators escaped from the wrath of the D.C. patrons by moving across the
border to Canada and becoming the Montreal Expos. Ironically, the new team escaped from the basement but not from bankruptcy, and the team executives made a second effort to win the hearts of Washingtonians. The reprise was highly successful, and the reincarnated Washington Nationals are currently competing with the “Damn Cubs” of Chicago for the National League crown. Maybe it was just getting out of the same league as the Yanks.
The fortunes of the Pittsburgh Pirates took a different trajectory. Blessed with a host of young talent and a future Hall of Fame manager named Leland, the team came within one out of making it to the World Series in 1992 when Barry Bonds, then just a “puppy,” could not throw a lumbering Sid Bream out at the plate. The name of the utility player for the Atlanta Braves who pinch hit and drove in the winning run in the bottom of the ninth inning has been long erased from our civic consciousness.
At any rate, this imbroglio seemed to break the heart and spirit of Pittsburgh baseball for 20 years, as the team nosedived into record-setting losing seasons and became a basement-dweller of the

same ilk as the Senators. But for me and an old woman named Dorothy these were the best years of our lives.
There are no greater baseball fans than widowed, silver-haired old ladies whose children are grown, whose grandchildren live outside the state, and who get connected by fate with a distant relative in his middle age who needs a haircut. This middle-aged man “lived too far from the city to learn baseball” when he was just a kid. More accurately, he stank so much at baseball that, instead of always batting ninth and playing right field, he had become a diehard fan by default.
“Aunt Dorothy” precisely fit this phenotype. A brother-in-law of mine highly recommended that Dorothy cut my hair when she was not busy cutting that of her life-long elderly friends, neighbors, and nursing home inmates.

Cutting my straight, limp hair in the parlor of her Northside home was a no-brainer, so we concentrated on our strategies to return the Pirates to competitiveness as if we were the board of directors, the general managers, or the agents of a phenomenon like “Shoeless Joe.” She listened on her radio to every
inning of every game of the west coast road trips — more diligently than any Pirate fan had in the past or ever would — without falling asleep as I had done with the Yankees as a kid growing up in New Jersey.
Dorothy loved the young, clean-cut, humble players, and I think she dreamed that shortstop Jay Bell was her grandson. During those 20 lean years she was our family’s guest at company-sponsored outings to Three Rivers Stadium and, since my kids weren’t all that excited about family bonding experiences, she was my sidekick. Although Dorothy frenetically moved around her salon, at the ballgames she sat smiling quietly for the duration — neither eating stadium
Continued on Page 16
From Page 15
junk food, drinking beer, nor even going to the restroom. Sometimes I wondered if she was privy to some private replay of her entire life being shown to her alone on the Jumbotron between innings.
I cannot remember whether her dear Pirates won or lost any of the games we attended and in those seasons of the doldrums it was generally thumbs-down; only one dreary ballgame we attended alone stands out in my weakening, constipated memory. It was during the “dog days” of late August when my wife sent me to the ballpark as a distraction — a third consecutive miscarriage seemed to be in progress. I confided the heaviness of my heart to Dorothy, subconsciously seeking sympathy. “Don’t worry needlessly” she consoled. “These troubles have a way of working themselves out.” Now I realize that what she really was saying was, “Have heart, young man — you gotta have heart!”
About a week later something seemed incongruous with the seemingly terminating pregnancy: the hormone levels were rising rather than falling. A fetal sonogram was performed. In previous situations the radiologist had personally disclosed the sad reality that the sac was empty. This time he strolled into the room and pointed to the screen. “There is the heart — you can see it beating.” We knew that the baby was a fighter.
The rest is history. The miracle child — known to his close friends as “Hobo Joe” — would become a long-distance runner and run a half marathon before he was a teenager. Dorothy died before she could ever see Hobo Joe run, or play baseball, or even “play catch” with his old man. As irony would have it, the kid never got into baseball; maybe he just could not resist the loneliness and ecstasy of the long-distance runner.
When Dorothy was playing out the bottom of the ninth in a nursing home, reminiscing as she faded in and out of consciousness, I ran a marathon in her honor. I hung the finisher’s medal in her room; after her death, it could never be located, and I just gave up hope of ever seeing it again.
“It breaks your heart. It is designed to break your heart. The game begins in the spring when everything else begins again, and it blossoms in the summer, filling the afternoons and evenings, and then as soon as the chill rains come, it stops and leaves you to face the fall alone — just when you need it the most.”
— H. Bartlett Giamotti, former commissioner of baseball, renowned for his insatiable love of the game. He died of a heart attack at the age of 51 while still in office.
Now our Pirates are in the wild card running. It would be quite a twist of fate if our resurrected team faces the reborn Washington Senators in the playoffs. It would be a confrontation of perennial losers that would ignite the spirit of any old diehard fan. I imagine that Aunt Dorothy would be granted a front row seat in that big ballpark in the sky reserved for those who followed west coast road trip games on the radio when the teams were down and out. I can see
her before the games signing autographs with Roberto and Willie — and maybe wearing an old lost marathon medal over her heart.
Although beautifully written, I believe Bart Giamotti’s postulate is erroneous. For the true-blue baseball fan, even the chill rains of old age and the bitter frost of dying cannot deprive us of the sport’s memories. When our minds become near empty and we need them the most, the memories of baseball endure within our hearts.

PS: Correction: The Pirates lost the game on July 15th in the last inning 3-1. That lie printed above was a scheme forged by artificial intelligence of which I only learned about from Aunt Dorothy in a dream. As before, she continues to teach me everything about baseball and about courageously living the simple life with which we have been gifted.
PPS: I apologize for misleading the readers about the outcome of the game! But as Jim Bouton stated in his iconoclastic narrative on professional baseball “Ball Four”:“It never hurts to apologize, especially if you don’t mean it.”
As for the miracle-child “Hobo Joe,” he practices medicine now near Williamsport, PA---the venue for the annual Little League World Series---as ““the hope which springs eternal” within me never strikes out!












Hepatorenal Syndrome (HRS) is a lifethreatening condition that can occur in patients with advanced liver disease, most commonly in patients with cirrhosis and ascites.1,2 This condition is characterized by decreased kidney function in the absence of intrinsic kidney disease, such as proteinuria, hematuria, or abnormal findings on ultrasound.3 In HRS, a decline in renal function is seen secondary to a decline in liver function and its effects on the body: sodium retention, ascites, intrahepatic vascular resistance, and splanchnic vasodilation (due to increased production of vasodilators).3 It is suspected that portal hypertension, cirrhosis, spontaneous bacterial peritonitis (SBP), and nephrotoxic agents (NSAIDs, aminoglycosides, contrast media) could be also be triggers.2 According to the American Liver Foundation, one in ten individuals who are hospitalized with liver failure are estimated to have HRS,2 and the incidence of HRS in patients who develop decompensated liver disease is 18% within 1 year of diagnosis and up to 40% at 5 years.1 Moreover, delays in starting specific therapy to treat HRS is very detrimental to patients with this condition.
Most often, patients present with symptoms of fatigue, edema, and dramatically decreased urine production. Signs of cirrhosis can also be seen, such as jaundice, ascites, and hepatic encephalopathy.1
Historically, HRS has been stratified into two types, Type 1 HRS (HRS-1) and Type 2 HRS (HRS-2). HRS-1 is more severe and defined by a rapid reduction of renal function—baseline serum creatinine (sCr) doubles to at least 2.5mg/dL or there is an observed 50% decline in creatinine clearance to below 20mL/min in two weeks’ time.3 HRS-1 can also result in multiorgan failure.1 On the other hand, HRS-2 is characterized by a more progressive decline in renal function (that does not fit into the criteria above) and it is associated with a longer median survival time compared to HRS-1.1 More recently, the diagnosis of HRS has been defined in the 2021 International Club of Ascites (ICA) guidelines that coincides with three stages of acute kidney injury (AKI) .3,4 In this particular guideline, HRS-1 is now termed HRS-AKI. It is important to note that in the literature HRS Types 1 and 2, as well as AKI-HRS, are both commonly used to define the condition; however, HRS-AKI has a sCr cutoff of >1.5mg/dL to encourage earlier and more rapid interventions.5
n Cirrhosis, acute liver failure, acute-on-chronic liver failure (ACLF)
n Increase in sCr, ≥0.3 mg/dL within 48 hours or ≥50% from baseline value and/or urinary output ≤0.5 mL/kg of body weight for ≥6 hours (requires use of a urinary catheter)
n No full or partial response for ≥2 days of diuretic withdrawal and volume expansion with albumin (dosed at 1 g/kg of body weight/ day; maximum 100g/day)
n Absence of shock
n No current or recent treatment with nephrotoxic drugs
n In the absence of CKD, assess for parenchymal disease, as indicated by proteinuria >500 mg/day, microhematuria (>50 red blood cells per high power field), urinary injury biomarkers (if available) and/or abnormal renal ultrasonography
n Suggestion of renal vasoconstriction, with FENa <0.2% (levels <0.1% are considered highly predictive)
* All criteria must be met for the diagnosis of HRS-AKI
Liver transplantation is considered the optimal treatment for patients with HRS-AKI, however, these patients often have contraindications to transplantation. The scoring system used in liver transplantation (Model for End-Stage
lauRen mauReR, DoCToR oF PhaRmaCy CanDiDaTe, univeRsiTy oF PiTTsBuRgh sChool oF PhaRmaCy, PiTTsBuRgh, Pa
Liver Disease, MELD) does not correlate to a favorable outcome for these HRS patients due to their elevated sCr levels and worse prognosis due to renal failure.5 A temporary option to bridge HRS patients to transplantation is renal replacement therapy (RRT). A drawback of RRT in HRS is its risks of acute complications, such as infections, bleeding, hemodynamic instability, and disruptions in volume management.5
While liver transplantation and renal replacement therapy are more long-term solutions, there are ways to acutely manage HRS patients. In the setting of volume depletion, administration of albumin maintains cardiac output and can be beneficial in fluid management.3,5 Additionally, vasoconstrictors, such as midodrine, octreotide, and vasopressin, can be used to reverse splanchnic vasodilation.5 In the setting of ascites, diuretics may be used to decrease fluid overload, spontaneous bacterial peritonitis (SBP) prophylaxis or treatment can be initiated, and paracentesis may be utilized.3 Moreover, if a patient develops hepatic encephalopathy, lactulose and rifaximin can be used.
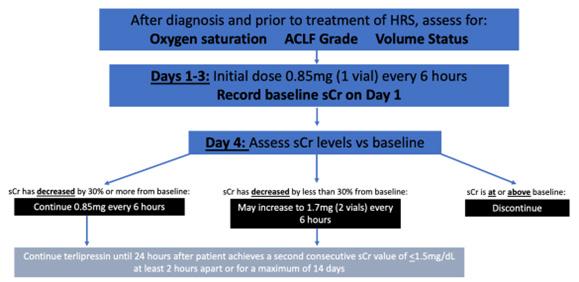
There has been an unmet need for the treatment of HRS-AKI in the United States; current management is either not favorable for patients (liver transplantation and/or RRT) or only acutely controls symptoms or secondary complications (restoring hemodynamic stability, removing excess fluid, reversing hepatic encephalopathy, and others). Up until recently, patients did not have many options and faced challenges managing this condition. However, in September 2022 the FDA approved terlipressin (Terlivaz®), a synthetic vasopressin analogue, for the use in HRS.
Interestingly, terlipressin is not a new drug. This vasopressin analogue has been the standard of care for HRS in many European and Asian countries for years.3 The FDA only recently approved the medication (made by Mallinckrodt Pharmaceuticals) due to previous concerns that its benefit did not outweigh the risks it posed.6 The phase 3 CONFIRM trial established terlipressin’s approval.
Terlipressin has predominant vasopressin 1A receptor effects and acts as a splanchnic vasoconstrictor.3,7 It acts as both a prodrug for lysine-vasopressin and has pharmacologic action on its own.7 Moreover, the drug activates vasopressin 1B receptors, which can counteract adrenal insufficiency (often seen in patients with decompensated cirrhosis) by stimulating the release of adrenocorticotropic hormone and cortisol.3 Prior to using terlipressin, patients must be assessed for Acute-on-Chronic Liver Failure (ACLF) grade and adequate baseline oxygenation saturation level.7 Patients with volume overload, hypoxia (as defined as SpO2< 90%), or ACLF grade 3 status are at increased risk of fatal respiratory failure. Of note, this medication is contraindicated in patients experiencing hypoxia, worsening respiratory symptoms, and in the setting of ongoing coronary, peripheral, or mesenteric ischemia. Terlipressin does not need to be adjusted for hepatic or renal impairment.
While a patient is receiving terlipressin, their oxygen needs to be continuously monitored via pulse oximetry. If hypoxia occurs, treatment must be discontinued. In the setting of intravascular volume overload, any albumin or other fluids being used must also be discontinued and diuretics must be used judiciously. It is possible to temporarily interrupt, reduce, or discontinue treatment until a patient’s volume status has improved.7 Other adverse events to be aware of are abdominal pain (19.5%), nausea (32%), respiratory failure (31%), diarrhea (26%), and dyspnea (25%), as well as pleural effusion, sepsis, bradycardia, and signs of ischemia.8

The CONFIRM trial, as briefly mentioned earlier, was a phase 3, randomized, 2:1, multi-center, double-blind, placebo- controlled study that aimed to confirm the efficacy and safety of terlipressin in patients with HRS Type 1 (or HRS-AKI). A total of 300 patients (from July 2016- July 2019) were randomized to receive either terlipressin (n=199) or placebo (n=101). These subjects had HRS Type 1, cirrhosis, ascites, and rapidly progressive kidney failure (sCr doubled to at least 2.25mg/ dL) within 14 days before randomization.8 The following patient characteristics excluded trial participation: sCr >7 mg/dL , one or more large-volume paracenteses of 4L or more within 2 days before randomization, sepsis or uncontrolled bacterial infection (or both) with antibiotic treatment less than 2 days, or severe cardiovascular disease within 4 weeks before randomization. In the trial, 1 mg of terlipressin or placebo was administered intravenously over 2 minutes every 5.5-6.5 hours. Of note, it was strongly recommended that all patients (treatment and placebo groups) receive albumin (max 100g on day 1 and 20-40g/day thereafter). A total of 165 patients (83%) in the terlipressin group and 92 patients (91%) in the placebo group received albumin; a total of 121
patients (61%) in the terlipressin group and 61 patients (60%) in the placebo group had previously received midodrine and octreotide.8
The primary endpoint in the CONFIRM trial was verified reversal of HRS (two consecutive sCr measurements of <1.5mg/dL at least 2 hours apart up to day 14 and survival without RRT for at least an additional 10 days). Secondary endpoints included HRS reversal (sCr <1.5mg/ dL), durability of HRS reversal (without RRT to day 30), HRS reversal among patients with inflammatory response syndrome, and verified reversal of HRS without recurrence by day 30. Overall, 32% of patients in the terlipressin group had verified reversal of HRS compared to 17% of patients in the placebo group (P=0.006). Additionally, at day 14, 23% of patients in the terlipressin group required RRT compared to 35% in the placebo group. All of the secondary outcomes were statistically significant between the groups (P<0.001) except for verified reversal of HRS with no recurrence through day 30 (P=0.08).8
While 176/200 patients (88%) in the terlipressin group and 88/99 (89%) of patients in the placebo group reported adverse events, the benefit versus risks should be weighed carefully. Serious side effects (abdominal pain, skin discoloration, cardiac ischemia, cyanosis, internal ischemia, and respiratory failure) were noted in the terlipressin group and must be monitored.8
HRS-AKI carries a high mortality in end stage liver disease and current management options are limited. Early diagnosis and intervention are essential to improving outcomes. In adult patients with HRS-AKI, the addition of terlipressin to albumin was more effective than addition of placebo in reversing HRS. Serious respiratory failure can occur with terlipressin but it has the potential to be another treatment option in the management of HRS. Future trials could further investigate populations that optimize benefit while minimizing toxicity.
1. American Liver Foundation. Hepatorenal syndrome. Updated March 16, 2023. Accessed June 5, 2023. https:// liverfoundation.org/liver-diseases/ complications-of-liver-disease/hepatorenalsyndrome/.
2. Mukhtar NA, Khalili M. Liver disease. In: Hammer GD, McPhee SJ. eds. Pathophysiology of Disease: An Introduction to Clinical Medicine, 8e. McGraw Hill; 2019. Accessed June 05, 2023.
3. Simonetto DA, Gines P, Kamath PS. Hepatorenal syndrome: pathophysiology, diagnosis, and management. BMJ. 2020;370:m2687.
4. Biggins, S.W., Angeli, P., Garcia-Tsao, G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021; 74(2):1014-1048.
5. Flamm SL, Brown K, Wadei HM, et al. The current management of hepatorenal syndrome-acute kidney injury in the United States and the potential of terlipressin [published correction appears in Liver Transpl. 2022 Jan;28(1):144]. Liver Transpl. 2021;27(8):1191-1202.
6. Dunleavy, K. Mallinckrodt scores longawaited FDA not to treat life-threatening liver condition. Fierce Pharma. September 15, 2022. Accessed June 5, 2023. https://www. fiercepharma.com/pharma/mallinckrodtscores-long-awaited-fda-nod-treat-lifethreatening-liver-condition#:~:text=A%20 phase%203%20trial%20had,uncertainty%20 of%20benefit%20over%20risk.
7. Terlipressin (Terlivaz®) [package insert]. Bedminster, NJ. Mallinckrodt Pharmaceuticals, Inc.; 2022
8. Wong F, Pappas SC, Curry MP, et al. Terlipressin plus albumin for the treatment of type 1 hepatorenal syndrome. N Engl J Med. 2021;384(9):818-828.
Ms. Maurer is a Doctor of Pharmacy candidate at the University of Pittsburgh School of Pharmacy. At the time of this writing, Ms. Maurer was on a clinical rotation at Allegheny Health Network, Allegheny General Hospital. For any questions concerning this article, please contact the Center for Pharmaceutical Care, Allegheny Health Network, Allegheny General Hospital, Pittsburgh, PA at (412) 3593192 or email tucker.freedy@ahn.org

When
Email: fenner@fennercorp.com
“Quality—you know what it is, yet you don’t know what it is.”
Association of ACOs, the National Rural Health Association, and Premier, Inc.
In this best-selling 1974 novel, Pirsig’s narrator (and alter ego) suffered a debilitating breakdown triggered by his obsession with the elusive nature of quality. Arguably, the same problem has hamstrung the American healthcare system’s reimbursement methodologies for many years.
In these divisive times, it’s rare to see Republicans and Democrats agree on anything, but a bipartisan bill that may provide critical support to practices eager to transition from fee-for-service to quality-based care may be gaining traction in Congress.
The Value in Health Care Act of 2023 was sponsored by Representatives Darin LaHood (R-IL), Brad Wenstrup, D.P.M. (R-OH), Larry Bucshon, M.D. (R-IN), Suzan DelBene (D-WA), Earl Blumenauer (D-OR), and Kim Schrier, M.D. (D-WA). The presence of three physicians among this group of lawmakers is no coincidence.
Equally impressive is the list of organizations that co-signed an American Hospital Association letter supporting the bill: Accountable for Health, the American Academy of Family Physicians, the American Academy of Orthopaedic Surgeons, the American College of Physicians, the American Medical Association, America’s Essential Hospitals, America’s Physician Groups, AMGA, the Association of American Medical Colleges, the Federation of American Hospitals, the Healthcare Leadership Council, the Health Care Transformation Task Force, the Medical Group Management Association, the National
Despite decades of efforts to break the stranglehold of fee-for-service payment in the healthcare industry, value-based methodologies continue to face obstacles. Payors have long contended that the incentives inherent in FFS payments reward quantity of care over quality. A full bowl of alphabet-soup alternatives have been adopted (and abandoned) since the earliest days of HMOs and capitation, with mixed results. The very name “health maintenance organization” signaled an attempt to reward results, i.e. maintenance of health, over quantity of treatment. But capitation and preauthorization, two of the primary tools in the HMO kit, have fallen out of favor as symbols of healthcare rationing. Instead, payors including Medicare have turned to various financial incentives for managing costs while ensuring quality.
First, some history: the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) offered incentive payments of 5% over standard rates for physicians and other clinicians who participate in Advanced Alternative Payment Models (APMs). APMs must require participants to use certified electronic health record (EHR) technology, provide payment for covered professional services based on quality measures; and either: (1) be a Medical Home Model expanded under CMS Innovation Center authority; or (2) require participating APM Entities to bear more than a nominal amount of financial risk for monetary losses. Eligible clinicians must receive at least 50 percent of Medicare Part B payments or see at least 35 percent of Medicare patients through an Advanced APM Entity, and 75 percent of practices in the APM need to use certified EHR Technology. The AMA notes
that development and availability of APMs for physicians, especially specialists, to participate in has been extremely limited. The 5% incentive was to expire, but in late 2022, Congress reauthorized it for another performance year, with the payments reduced to 3.5% but using an increased conversion factor.
A second track, the Merit-Based Incentive Payment System (MIPS) provided Medicare payment adjustments, up or down, based on a composite performance score. It requires providers to report certain statistics to CMS, with a penalty of a 9% reduction in Medicare payment rates for not reporting. (Advanced APM participants under MACRA are excluded from MIPS reporting as an additional incentive). Newly enrolled Medicare eligible clinicians who enroll in Medicare for the first time during the performance year and those who are below the low-volume threshold (annual Medicare Part B allowed charges ≤ $90,000 OR who provide care to 200 or fewer Medicare Part B patients; OR provide fewer than 200 covered professional services to Part B patients) are exempt from reporting as well. The MIPS incentives are increasing while the MACRA incentives have been cut and may expire without Congressional action. In 2026, MIPS clinicians will receive a 0.25 percent conversion factor update in addition to any quality adjustments. The average MIPS adjustment is typically 3 percent, resulting in potential payment adjustment of 3.25%. The National Association of Accountable Care Organizations (NAACO) has stated that incentives will not favor clinicians in advanced APMs again until 2032.
Additionally, the Affordable Care Act established the Medicare Shared Savings Program which provides incentive payments to Accountable Care Organizations (ACOs) and their members
—Robert Pirsig, Zen and the Art of Motorcycle Maintenance.
if the ACOs meet certain cost targets and quality measures while managing populations of traditional Medicare beneficiaries. The Department of Health and Human Services reports that the Shared Savings Program has grown into one of the largest value-based purchasing programs in the country. As of January 2023, Shared Savings Program ACOs include over 573,000 participating clinicians who provide care to almost 11 million people with Medicare. CMS has set a goal that 100 percent of people with Traditional Medicare will be part of an accountable care relationship by 2030.
adjacent lumbar vertebra, explaining her pain. My resident, from Georgia, upon seeing the findings said, in his deep southern drawl, “Fellahs, there’s a lesson here. Crocks daah (die), too.” Unfortunately for the patient, CT scanning and ultrasound exams had not been developed. The important lesson is that for most patients with a diagnosis of psychosomatic illness, the symptoms are real, and in fact a small number of these patients indeed have real abnormalities accounting for their symptoms.
Enter the proposed Value in Health Care Act of 2023. If enacted, it would strengthen and expand the existing quality-based programs to bring more providers and Medicare patients under their coverage.
The Act would continue the 5% APM incentive payments for at least two years and freeze
Sigmund Freud’s view of humor was that it was a conscious expression of thoughts that society usually suppressed or was forbidden.2 As long as the humor, in this case name-
the 50% revenue threshold that physicians in value-based care models must meet to qualify for these bonuses, opening up the MACRA program to a wider group of physicians. It would also give the Health and Human Services (HHS) secretary the authority to further increase the revenue threshold by no more than 5% in any single year.
HHS would also be directed to provide additional technical support to ACOs, small practices, physicians, and other providers that serve rural or medically underserved populations.
calling, is meant in a benign fashion, it is considered harmless.
The Act would also allow for expanded participation by lowering thresholds for episode models that would otherwise not meet the current APM criteria.
Under the Act, revenue-based distinctions in the ACO Shared Savings Program would be removed, improving certain rural and safety net providers’ share in the savings they earn without forcing them to accept greater risk. The Act would increase benchmark transparency to ensure that CMS does not penalize ACOs for their own success, and create an optional full-risk model for ACOs.
However, in today’s politically divisive atmosphere, it is best to use humor only when you truly know your audience. As a good example, I remember the not so “good old days,” when it was expected that a speaker at a conference or a refresher course would tell jokes. Many of the “old timers” were very colorful characters. Today, fortunately, speakers are business-like and jokes are tacitly forbidden, since they are bound to offend someone. Finally, we should always remember that no matter how unpleasant some of our patients are to us, they are still our fellow human beings.
Dr. Daffner, associate editor of the ACMS Bulletin, is a retired radiologist who practiced at Allegheny General Hospital for more than 30 years. He is emeritus clinical professor of Radiology at Temple University School of Medicine and is the author of nine textbooks. He can be reached at bulletin@acms.org.
The Value in Health Care Act of 2023 has united such traditional adversaries as the AMA and the AHA (not to mention the two major parties) in an effort to support and expand existing alternatives to the fee-for-service approach to Medicare payments. The new law would accomplish this goal by tweaking the rulebook for participation and payment, not by changing the methodology for measuring the elusive concept of “quality.” Its passage would be a win/win scenario for providers, patients, and taxpayers.
1. Shem S. The House of God. Richard Marek Publishers 1978.
2. Freud S, (Strachey J, Trans.). Jokes and their relation to the unconscious New York: W. W. Norton, 1960 (Original work published 1905).
William H. Maruca, Esquire is a healthcare partner in the Pittsburgh office of the national law firm Fox Rothschild LLP. He can be reached at wmaruca@foxrothschild.com or 4312.394.5575
• Physician Billing Services for All Specialties
We would use OUR billing system or YOUR billing system based on YOUR preference.
• Credentialing Services for All Specialties
• Accounts Receivable Follow-Up for Practice Support
We would work your accounts on your system to maximize cash flow.
NEW Billing Client Example: A new client (a 6-physician family medicine group) liked their EHR, so the group asked us to bill using their billing system. Besides the benefit of keeping their EHR, the group is now experiencing greater efficiency and stability in their office by eliminating problems caused by biller turnover, vacations, diversion, and other time off.
Contact Ruby Marcocelli, Vice President at 412-788-8007 or rmarcocelli@fennercorp.com
Three Penn Center West Pittsburgh, PA 15276 fennercorp.com
On August 17th, the ACMS hosted a Legislative Update and Leadership Social at the Kimpton Hotel Monaco. This event was held for all ACMS members who serve in elected leadership roles on the ACMS Board of Directors, the ACMS Foundation Board, the ACMS Delegation, and leaders from the Pennsylvania Medical Society. Attendees received a legislative update from the Pennsylvania Medical Society team, followed by remarks and a Q&A session with ACMS Member and State Representative Arvind Venkat, MD. Rep. Nick Pisciottano was also in attendance.
One of the perks of serving in a leadership role at the ACMS is the opportunity to attend exclusive events like this one. While the nomination window for elected positions has closed for the 2024 year, please feel free to reach out to Sara Hussey, Executive Director, to learn more about getting involved in 2025.




We extend our gratitude to all our elected volunteers who attended the event. For more photos, visit the photo gallery at www.acms.org.

Module 6: Approaches to Addressing Patient's Substance Use Disorder
Module 7: Effective Opioid Tapering Practices
Tuesday, October 17 / 6:00 pm to 8:00 pm
VIRTUAL MEETING (Link will be sent once registered.)
ACMS Members Free | NonMembers $50.00


Agenda: 6:00 pm – Module 6 Begins (1 hour)
7:00 pm – Module 7 Begins (1 hour)
Expert Presenters | Rabecca Dase, MHA and Denise Vanacore Chase, PhD, ANP-BC, FNP-BC, PMHNP-BC
Join us on Tuesday, October 17 from 6:00 pm to 8:00 pm to learn about using the Prescription Drug Monitoring Program (PDMP) to address substance use with a patient and effective opioid tapering practices. Both modules are part of the Evidence-Based Prescribing: Tools You Can Use to Fight the Opioid Epidemic educational series.
Each module in this training series can be applied to the NEW required eight training hours on the treatment and management of patients with opioid or other substance use disorders, as mandated under the Consolidated Appropriations Act of 2023 for all Drug Enforcement Administration (DEA)-registered practitioners.

The Pennsylvania Department of Health and Quality Insights have partnered to provide live and virtual opioid education sessions at no cost to you. This program qualifies for ACT 124 Prescribing Practices for Opioids CME or Patient Safety/Risk Management Credit (but not both).


The University of Pittsburgh School of Medicine has designated each module for a minimum of 1 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Attendees are required to complete the individual pre-event questionnaires for Modules 6 and 7 before the start of the program. Both links will be sent in your program confirmation email.
Module 6
Learn how to integrate the PDMP with other screening tools to identify those who may require substance use disorder treatment or increased monitoring;
Define Screening, Brief Intervention, and Referral to Treatment (SBIT), its main goals, and its main components

Learn how to screen a patient for a potential substance use disorder, conduct a brief intervention, and refer a patient to treatment;
Learn how to discuss a substance use disorder with a patient and handle patient resistance;
Learn how to incorporate SBIRT into clinical practice
Module 7
Discuss how to use the PDMP to determine if a provider should consider tapering his/her patient;
Discuss several indicators that prescribers can look for when considering a taper;
Inform prescribers on how to discuss tapering with patients using patient-centered techniques;
Present a general opioid tapering protocol and how to adapt this protocol to the needs of any patient
Present information on how to manage withdrawal and how to use tools to measure withdrawal symptoms in patients.
Questions? Contact Eileen Taylor at etaylor@acms.org or to (412) 321-5030 x105.
& Cybersecurity
Mergers & Acquisitions
Peer Review and Credentialing for Physicians Employment Contracts and Restrictive Covenants

& Employment Benefits
Mike Cassidy - Compliance; Contracts, Peer Review, Stark/AKS
Jeremy Farrell - Labor & Employment
Ryan James - Commercial Litigation
Rebecca Moran - Mergers & Acquisitions and Physician Contracts
Jerry Russo - Criminal Defense and Investigations

Paul Welk - Mergers & Acquisitions
Recently, the Allegheny County Health Department (ACHD) created a dashboard containing data on reportable diseases in the county. The ACHD uses reports of disease to identify clusters, determine at risk populations, assess burden of disease, monitor trends and recommend measures to prevent transmission.

The dashboard was developed so residents and other stakeholders can explore information about many reported infectious diseases. The dashboard includes data from 2012 to 2021 and provides information on trends, hospitalizations, deaths, demographic characteristics and information on associated risk factors.
A link to the dashboard can be found here: https://tableau.alleghenycounty.us/t/PublicSite/views/IDEDashboard2012-2021/InfectiousDiseaseDashboard2012-2021?%3AshowAppBanner=false&%3Adisplay_count=n&%3AshowVizHome=n&%3Aorigin=viz_ share_link&%3AisGuestRedirectFromVizportal=y&%3Aembed=y#1
Tucker Arensberg lawyers have experience in all major healthcare law issues including:
George was born in Verona where his father served as the Burger or Mayor of the town for 16 years. He and his younger sister, Jane Garboden, MD, both became physicians, George graduating from the University of Pittsburgh and Jane from the Woman’s Medical College in Philadelphia. George chose medicine believing that it would be an honorable way of contributing to society.
After graduating from the University of Pittsburgh School of Medicine in 1953, George completed his internship in 1954 at St. Francis General Hospital in Bloomfield. The Korean War had just ended, and George volunteered to join the U.S. Air force. George was stationed in Japan and served as a flight surgeon for three years and served as the commanding officer of the medical facility on base.
Following completion of his military experience, he decided to specialize in ophthalmology and completed a three-year ophthalmology residency at the Veteran’s Hospital in Pittsburgh.
Following residency, he entered clinical practice, initially with Dr. Jay Linn, Jr. for 3-4 months and then joined Phil Grana, MD.in Braddock. When Dr. Grana retired, George moved his practice to Forest Hills with Art Fleming, MD, joining him in practice.

When Art relocated his practice nearby, they parted business on amicable terms. Art practiced in Forest Hills in the same neighborhood and George and Art and George often had lunch together. George then recruited John Mikulla, MD in 1978. John retired from the practice in 2016. Jean Harwick, MD joined the practice and worked with George for about 9 years. Joel Brown, MD joined the practice and remains as the senior partner at Forest Hills location. During George’s retirement George stayed in touch with the practice, communicating with Joel frequently. George enjoyed teaching residents in ophthalmology and volunteered to oversee the glaucoma clinic at Falk clinic for many years. He was a surgical tutor both at the Eye and Ear Hospital and the Oakland VA hospital and had an appointment as Clinical Associate Professor at the University of Pittsburgh School of Medicine.
Dr. Gerneth was passionate regarding the ethical practice of medicine and appropriate utilization of medical services. He chaired the Quality Assurance Committee at the Eye & Ear Hospital and served a consultant for provider relations for the Pennsylvania Ophthalmology Society, working with advocate, Norman Edelstein, MD resolving reimbursement issues.
George was a leader in organized medicine and served as President of the Allegheny County Medical Society in 1993. George also served as President of the Pennsylvania Academy of Ophthalmology and Otolaryngology in 1982 and received their Distinguished Service award in 1987.
Following the national trend to separate the two subspecialties, in 1990, George served on the incorporation and reorganization committee that separated the Ophthalmologists and the Otorhinolaryngologists into two different academies in Pennsylvania. George served as President of the Pittsburgh Ophthalmology Society from 1981 - 1983 He was a member of the Medical Eye Care Foundation.
George relaxed at Laural Mountain Park near Ligonier, PA. There he cultivated a friendship with fellow ophthalmologist Dorothy C. Scott, MD and her husband Glenn. Both George and Dorothy inspired many young ophthalmologists to become involved with local and state societies to help oversee the delivery of cost effective and ethical ophthalmologic care.
George’s wife, Eileen, pre-deceased him by seven months. Both lived at Longwood in Verona-Oakmont. George is survived by 2 daughters and 6 grandchildren.
—Al Biglan, M.D
I would like to thank many who have helped to construct this obituary. Norman Edelstein, Joel Brown, Jane Garboden, Nadine Popovich, and Shara Taylor who inspired this effort.
At the June 13, 2023 ACMS Foundation Board Meeting, the Foundation Board of Trustees approved a Bylaws revision that would add TWO (2) additional Community Board Members to the ACMS Foundation Board of Trustees, for a total of Four (4) Community Board Members, starting with the 2024 Year (Jan. 1, 2024). The suggested Bylaws changes below will be presented at the September 12, 2023, ACMS Board Meeting. The changes will be printed in the September and October ACMS Bulletin for comments by membership. Final changes and approval will be made at the December 5, 2023, Board Meeting.
Trustees and Officers
1. Trustees
The Trustees shall be nine (9) eleven (11) in number consisting of five (5) members representing the Allegheny County Medical Society: the President, President-Elect, Secretary and the Treasurer; the most recent past president of the Allegheny County Medical Soci ety, two (2) four (4) community members who are not physicians, one (1) member who shall have previously served as a physician Trustee and who shall serve as Secretary of this Foundation; and one (1) member who shall have previously served as a physician Trustee and who shall serve as Treasurer of this Foundation. All members shall have an equal vote.
2. Election
A. The two four (4) community members shall be elected, in alternate years, for a two-year term on nomination by the Board of Directors of the Allegheny County Medical Society. These members may be elected for two successive terms and shall take offic e January first following their election.
B. The five (5) members who serve representing the Allegheny County Medical Society, shall serve for a term of one year, beginni ng January first, and their terms of office shall coincide with the terms of the Allegheny County Medical Society office held.

C. The Secretary shall be elected by this Board of Trustees for a term of two years and may serve two successive terms.
D. The Treasurer shall be elected by this Board of Trustees for a term of two years and may serve two successive terms.
3. Organization
E. Meetings of the Trustees shall be held at least twice a year at the call of the presiding officer. Five Six members present shall constitute a quorum with full power to act.
The ACMS Foundation Bylaws can be found on the website at: www.acms.org/acms -foundation/about -the-foundation/
Comments on these changes can be submitted to: ACMS Executive Director Sara Hussey at shussey@acms.org
Respectfully Submitted, 2023 Bylaws Committee
Keith T. Kanel, MD (Chair), Peter G. Ellis, MD & Raymond E. Pontzer, MDAt their October Board Meeting, the ACMS Foundation Board of Trustees will award $200,000+ in grant dollars to local non-profits. As we prepare to distribute these funds to the community, we want to acknowledge the physician members and community members who have provided support to the ACMS Foundation in 2023.

Scan this QR Code to Donate via Qgiv or visit acms.org/acms-foundation/donate/
Qgiv allows donors to setup monthly donations. Consider setting up a recurring donation!
To learn more about the ACMS Foundation visit: acms.org/acmsfoundation
Physician suicide is a profoundly distressing and often underreported issue within the healthcare industry. Physicians, who dedicate their lives to serving others, are disproportionately affected by mental health issues and burnout. According to a study published in JAMA Surgery, physicians have a 1.4 to 2.3 times higher risk of suicide compared to the general population. This alarming statistic serves as a wake-up call, urging us to confront the hidden crisis within the medical community.
The ACMS’s annual “Putting Self-care in Healthcare” campaign, which runs throughout the month of September each year, is not merely about providing discounts and prizes to our members. Our larger goal is to raise public awareness of the pressing mental health issues facing physicians, as well as provide tools and resources to help physicians create and maintain physician wellness to deliver high-quality healthcare. We are ready to take the next steps in this campaign.
The ACMS, alongside our Foundation arm, the ACMS Foundation, has been awarded a $10,000 grant from “The Physicians Foundation” to implement a physician wellness toolkit and wellness program. Over the next year, the ACMS Foundation will work alongside 10 other State and County Medical Societies to develop a toolkit and wellness program to combat physician burnout. We look forward to sharing this work with our members and hope to solicit feedback and guidance from our members as we move along in this process.
If you are passionate about this issue, please reach out (shussey@acms.org) so that we can contact you as information and guidance are needed.
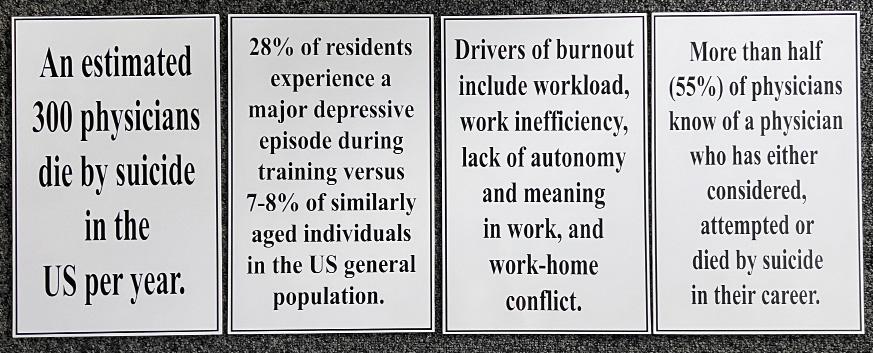
We understand that changing deeply ingrained cultures, systems, and policies in healthcare takes time, legislation, and a shift in mindset. However, we also recognize that every physician matters. Through our “Putting Self-care in Healthcare” campaign, we aim to offer simple ways to decompress, help alleviate smaller burdens, and encourage physicians to draw motivation from their families. And by taking this next step in creating a wellness toolkit and physician burnout resources, we hope to provide a means for a tangible change.
The Physicians Foundation is a nonprofit 501(c)(3) organization that seeks to advance the work of practicing physicians and help facilitate the delivery of healthcare to patients. It pursues its mission through a variety of activities, including grantmaking, research, white papers, and policy studies. Since 2005, The Foundation has awarded numerous multi-year grants totaling more than $40 million. In addition, The Foundation focuses on the following core areas: physician leadership, physician practice trends, physician shortage issues, and the impact of healthcare reform on physicians and patients. As the healthcare system in America continues to evolve, The Physicians Foundation is steadfast in its determination to strengthen the physician-patient relationship and assist physicians in sustaining their medical practices. For more information, visit www. PhysiciansFoundation.org.
On September 12, the ACMS Board of Directors had their fall meeting to update ACMS Board members on recent developments. As we head into a busy fall season and the official start of ACMS/ PAMED membership renewals, the ACMS team wanted to keep all our members informed about the work the ACMS Board of Directors and staff have been doing.
The Board of Directors hear updates from all the standing committee chairs:
• The Finance Committee, led by Chair William Coppula, MD, reported that both the ACMS and ACMS Foundation are in good financial shape, partly due to a favorable stock market in 2023. Both the ACMS and the ACMS Foundation have shifted their investment management to Hirtle Callaghan, a specialized firm for non-profits and foundations. This transition has been successful.
• The Bylaws Committee, chaired by Keith Kanel, MD, proposed adding two community board members to the ACMS Foundation Board of Trustees in 2024. The ACMS Board of Directors initiated this change process, with final approval expected in December 2023.
• The Nominating Committee, led by Raymond Pontzer, MD, presented a slate of candidates for the 2024 election to the ACMS Board, which has been approved. Members will receive their digital ballots between October 31 and November 11.
• In the President’s Update, Matthew Straka, MD, announced the return of ACMS Honors in April 2024 as a fundraiser and awareness event for the ACMS Foundation. The ACMS also plans to reintroduce the Distinguished ACMS Awards in a late fall 2024 event, honoring county physicians and acknowledging board members. Volunteers are being sought for the ACMS Awards Committee, and interested individuals can contact Sara Hussey, Executive Director, for consideration.
We had a great summer of events. We tried for a well-rounded balance of professional education (AI Town Hall with Abridge), family friendly (Pirates Game), targeting a specific need (Women in Healthcare Committee), and Advocacy/Leadership connections (Legislative Update + Social). All these events were well attended, had strong engagement, and resulted in either brand new members or reengagement of members who hadn’t been involved.
ACMS Member Benefits
Our team relaunched our benefits page (https://www.acms.org/resources/member-benefitsdiscounts/). Some of these benefits provide ACMS with non-dues revenue kickbacks and some are partnerships that simply provide value to our members and fill a need. We look forward to continuing to build these resources. Recommendations are welcome.
The ACMS relaunched our Putting Self-Care in Healthcare campaign in support of Physician Suicide Awareness Day. This month our press opportunities include: Yinz are Good podcast with Dr. Arvind Venkat (speaking on physician burnout), interview with Rick Dayton (Sara Hussey), Live segment on Talk Pittsburgh (9/15, Sara Hussey & Dr. Anu Anand), and Ya Jagoff Podcast later this month.
Sara Hussey, ACMS Executive Director, provided an update that included Mission Moments from the summer, operational updates, organizational successes and challenges, and membership updates. The ACMS now boasts 2450 members, which is an increase of 357 members since May 2023. Membership renewal is open for the 2024 membership year, expiring on December 31, 2024.
To conclude the meeting, the 2023 ACMS Delegation Vice Chair, Dr. Bruce MacLeod, and PAMED Board of Directors Trustee, Dr. G. Alan Yeasted, jointly updated members on matters from the Pennsylvania Medical Society and issues that will be discussed at the 2023 House of Delegates. These updates included significant conversations about delegate allocation and representation, particularly concerning student member delegation allocation. Several proposed resolutions aim to provide adjustments to the allocation. ACMS Members are encouraged to review the proposed resolutions at www.pamedsoc.org/house-ofdelegates/resolutions and reach out to the 2023 ACMS Delegation Chair, Dr. Richard Hoffmaster (hoffmasterrb@upmc.edu), with any comments.
On behalf ACMS President Matthew B. Straka, MD, as well as the entire Board of Directors, we’d like to thank every single member for their support over this last year. We continue to see our organization grow and engagement has been up significantly. We hope you are feeling excited to renew your ACMS membership for 2024. Please reach out with any questions, comments, or concerns.
850
COUNTY MEDICAL SOCIETY — 2023 MEETING SCHEDULE

ALL MEETINGS BEGIN AT 6:00 PM
Upcoming Events
No upcoming events Executive Committee*
Tuesday Evenings—2nd Tuesday at the start of each new quarter.
October 10, 2023
Finance Committee
Tuesday Evenings
November 14, 2023
Board of Directors*
Tuesday Evenings
December 5, 2023
Committees
Delegation
Nominating
ACMS Foundation
Dates to be announced
September 28, 2023 6:30 PM
October 24 Grant Proposal Review
PAMED BOARD
August 3
AMA Interim Meeting
AMA Annual Meeting
PAMED HOUSE OF DELEGATES / HERSHEY
October 27-28, 2023
October 26-27, 2024
AMA HOUSE OF DELEGATES
November 11-14
June 2024
ACMS HOLIDAYS – OFFICE CLOSED
January 2 New Year’s Day (Monday)
January 16 Martin Luther King (Monday)
February 20—President’s Day (Monday)
May 29—Memorial Day (Monday)
June 19—Juneteenth Day (Monday)
July 4—Independence Day (Tuesday)
National Harbor, MD
Chicago, IL
September 4 Labor Day (Monday)
November 10 Veteran’s Day (Friday)
November 23 Thanksgiving Day (Thursday)
November 24 Thanksgiving Friday (Friday)
December 25 Christmas (Monday)
Ridge Avenue, Pittsburgh, PA 15212