

OB-GYN expertise for your patients.
When your patients need the best possible specialty care, AHN has physicians with the right expertise — like our new OB-GYN.
Dr. Simons offers personalized, high-quality gynecological and obstetrical care to meet each patient’s individual needs.
To refer your patient, call (412) DOCTORS.
Kathryn M. Simons, MD
OB-GYN
Locations:
AHN North Fayette Health + Wellness Pavilion
Western Pennsylvania
OB/GYN Associates — Brentwood
Western Pennsylvania
OB/GYN Associates — Green Tree
Specialties : Skilled at surgical management of pelvic organ prolapse and minimally invasive surgery
Focuses on menopause, menstrual disorders, incontinence, contraception, and obstetrics
Allegheny County MediCAl SoCiety
Opinion Departments
Editorial....................................5
• The Future is Here
Deval (Reshma) Paranjpe, MD, MBA, FACS
Perspective ..............................8
• Physician Wellness Beyond Words— Advocating Wellness in Practice
Prerna Mewawalla, MD
Editorial ..................................10
• Crocks Die Too Richard H. Daffner, MD, FACR
Editorial .................................12
• New Relic Discovered in Troy Hill
Anthony L. Kovatch, MD
ACMS Photo Contest ............15

Perspective ............................16
• A Visit From Dr. Stead
Michael Lamb, MD
Society News..........................25
• Pittsburgh Ophthalmology Society announces new President Pamela P. Rath, MD
Society News..........................26
• Pittsburgh Ophthalmology Society Announces 2023-2024 Monthly and Annual Meetings Dates and New Monthly Meeting Location!
Society News..........................27
• Pittsburgh Ophthalmology Society Annual Meetings Guest Faculty
ACMS News ...........................32
• Women in Healthcare Committee Kickoff Event
Articles
In Memoriam ...........................19
H. Lee Dameshek, MD
Materia Medica ......................20
• Auvelity®: Shortening the Onset of Action in Major Depressive Disorder Ashley N. Rodgers and Karen M. Fancher, PharmD, BCOP
Legal Summary................ ......23
• Supreme Court May Force Providers to Take Deliberate Steps to Avoid a False Claims Act Lawsuit
Lourdes Sanchez Ridge
ACMS Meeting Schedule ......36
2023
Executive Committee and Board of Directors
President
Matthew B. Straka, MD
President-elect
Raymond E. Pontzer, MD
Secretary
Keith T. Kanel, MD
Treasurer
William Coppula, MD
Board Chair
Peter G. Ellis, MD
DIRECTORS
Term Expires 2023
Michael M. Aziz, MD
Micah A. Jacobs, MD
Bruce A. MacLeod, MD
Amelia A. Paré, MD
Adele L. Towers, MD
Term Expires 2024
Douglas F. Clough, MD
Kirsten D. Lin, MD
Jan B. Madison, MD
Raymond J. Pan, MD
G. Alan Yeasted, MD
Term Expires 2025
Anuradha Anand, MD
Amber Elway, DO
Mark Goodman, MD
Elizabeth Ungerman, MD
Alexander Yu, MD
PAMED DISTRICT TRUSTEE
G. Alan Yeasted
COMMITTEES
Bylaws
Raymond E. Pontzer
Finance
William Coppula, MD
Nominating
Raymond E. Pontzer, MD
Medical Editor Deval (Reshma) Paranjpe (reshma_paranjpe@hotmail.com)
Associate Editors
Douglas F. Clough
Richard H. Daffner (rhdaffner@netscape.net)
Kristen M. Ehrenberger (kricket_04@yahoo.com)
Anthony L. Kovatch (kovatcha42@gmail.com)
Joseph C. Paviglianiti (jcpmd@pedstrab.com)
Andrea G. Witlin (agwmfm@gmail.com)
ADMINISTRATIVE STAFF
Executive Director
Sara Hussey (shussey@acms.org)
Vice President - Member and Association Services
Nadine M. Popovich (npopovich@acms.org)
Manager - Member and Association Services
Eileen Taylor (etaylor@acms.org)
Co-Presidents
Patty Barnett Barbara Wible
Recording Secretary Justina Purpura
Administrative & Marketing Assistant Melanie Mayer (mmayer@acms.org)
Director of Publications Cindy Warren (cwarren@pamedsoc.org)
Part-Time Controller
Elizabeth Yurkovich (eyurkovich@acms.org)
ACMS ALLIANCE
Corresponding Secretary
Doris Delserone Treasurer
Sandra Da Costa
EDITORIAL/ADVERTISING
OFFICES: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212; (412) 321-5030; fax (412) 321-5323.
USPS #072920. PUBLISHER: Allegheny County Medical Society at above address.
The Bulletin of the Allegheny County Medical Society is presented as a report in accordance with ACMS Bylaws.
The Bulletin of the Allegheny County Medical Society welcomes contributions from readers, physicians, medical students, members of allied professions, spouses, etc. Items may be letters, informal clinical reports, editorials, or articles. Contributions are received with the understanding that they are not under simultaneous consideration by another publication. Issued the third Saturday of each month. Deadline for submission of copy is the SECOND Monday preceding publication date. Periodical postage paid at Pittsburgh, PA.
Bulletin of the Allegheny County Medical Society reserves the right to edit all reader contributions for brevity, clarity and length as well as to reject any subject material submitted. The opinions expressed in the Editorials and other opinion pieces are those of the writer and do not necessarily reflect the official policy of the Allegheny County Medical Society, the institution with which the author is affiliated, or the opinion of the Editorial Board. Advertisements do not imply sponsorship by or endorsement of the ACMS, except where noted.
Publisher reserves the right to exclude any advertisement which in its opinion does not conform to the standards of the publication. The acceptance of advertising in this publication in no way constitutes approval or endorsement of products or services by the Allegheny County Medical Society of any company or its products.
Annual subscriptions: $60
Advertising rates and information available by calling (412) 321-5030 or online at www.acms.org.
Assistant Treasurer
Liz Blume
COPYRIGHT 2023: ALLEGHENY COUNTY
MEDICAL SOCIETY
POSTMASTER—Send address changes to: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212.

The Future is Here
Deval (Reshma) PaRanjPe, mD, mBa, FaCs

Unfortunately, this may become a Hobson’s choice sooner than later. Artificial intelligence has limits and is, at least not yet sentient, according to Silicon Valley insiders. However it is about to change the way we live, much as the introduction of the fax machine, cellular telephones, and computers did in decades past. AI is like Eli Whitney’s new cotton gin, and it will power the new industrial revolution.
A recent report by Europol (the EU version of Interpol) warns that up to 90 percent of internet content could be generated or edited by AI by 2026. Think of what that means. Content websites will depend on an admittedly imperfect AI system to generate nearly everything you read on the internet. The tone, accuracy, and motive behind the content will be moderated by humans— who have not been doing a great job of late, as anyone who has witnessed the devolution of editorial standards on television, radio, web, and print news can attest. Editorializing, previously the ultimate faux pas, is now seemingly de rigeur in broadcast journalism.

More troubling still, AI may become the sole or prevalent editor of AIgenerated content. We have seen lately that AI can be problematic in that it has no EQ and no inherent moral compass. The New York Times story of the writer
whose Microsoft Chatbot made a pass at him and asked him to leave his wife is but one example. Aggressively racist and sexist behavior from other chatbots has also been well-documented. “It’s all in how you train the algorithm,” people may say, along the lines of “guns don’t kill people; people kill people.” Perhaps, but both guns and AI make it a lot easier to achieve nefarious ends on a grand scale.
AI is sweeping the television industry as well. An Indian news channel has employed an AI news presenter named Lisa, who can speak multiple languages flawlessly and still maintain
the studied cadence of a BBC reporter. She is attractive, well-rated by the audience, and could be programmed to tell you the weather report or that nuclear destruction is imminent and mass suicide is a reasonable option. If you watch her, she does not have six fingers or any of the classic AI “tells”. She looks like an attractive, well-spoken young woman in her twenties. The article interviewed viewers, most of whom did not mind an AI presenter and enthusiastically found her pretty; however one cynical taxi driver was rightly concerned that he could now REALLY not trust anything he was told on the news.
“Who ya gonna believe, me or your own eyes?”
—Groucho Marx
From Page 5
AI is already in the hands of cybercriminals who are running a scam in which they grab a snippet of speech from a real person and extrapolate that using AI into a scam phone call. Typically, grandparents or parents are called by an AI chatbot purporting to be the grandchild, who is in jail after a car accident or other mishap and needs bail money. Think this is farfetched? This happened to the parents of a good friend in Pittsburgh last year; they nearly fell for it because the voice sounded exactly like their grandchild and responded to them conversationally.
Actors are currently on strike, and one of their grievances is their lack of rights and protection against AI hijacking of their image, voice, and work. But the privacy and ownership issues extend beyond actors and celebrities to the average citizen. If you cannot protect and maintain ownership of the rights to your own image and voice, and if anyone can make video or audio of you that can’t be distinguished from the real thing, and this video or audio has you doing or saying terrible things---what and who can you really trust anymore? And how can you clear your name from allegations that you did or said something wrong? Look for the legal system to change as well.
Think of the implications for politics—if you thought you couldn’t trust politicians before, now they can claim AI as an excuse for misbehavior.
Good people could be falsely accused of heinous things, and bad people could be falsely exonerated. Whoever controls the media will have an incredibly powerful tool---if you thought there was “fake news” before, sit back, because the real “fake news” will now be possible. Imagine the chaos and discord that foreign governments and enemy agents will be able to sow using AI generated fake video and audio using social media. The American people (indeed any people—it’s human nature) have already proved in the last few years to be emotionally labile, intellectually lazy, and liable to quickly turn on one another along manufactured divisions under stress.
AI will cause upheaval in the labor market and force job retraining. If retraining is not possible, this, in itself, will cause a fundamental change in the economy. Many white-collar jobs will be eliminated—writers, editors, lower, and middle management, and even some upper management positions will no longer be necessary. Businesses will become more efficient, but large swaths of the populace will become unemployed and discontent leading to upheaval.
Skilled trades may not be so replaceable until AI-powered robots advance further and are more accessible.
AI will affect the practice of medicine profoundly. Health insurance companies and hospital systems will undergo the same slash-and-burn of lower and middle management seen in other industries, no doubt to the delight of upper management but also clinicians. AI will reach into diagnostic, therapeutic, and genetic realms at the expense of patient privacy, particularly if the information is integrated with health insurance companies. AI will also change clinical medicine for the better by outsourcing scutwork, streamlining care, improving efficiency, helping patients with preventive medicine, and aiding procedures with AI-powered robots. Can AI replace physicians? Not yet. But our job descriptions may change profoundly.
Our job as humans and physicians is to ensure that the AI set in place to help us operates under an ethical moral compass and has EQ and heart. Otherwise, it is a fine line between heaven and hell.
Buckle up; the future is here.

OUR SYSTEM or YOUR SYSTEM?
• Physician Billing Services for All Specialties

We would use OUR billing system or YOUR billing system based on YOUR preference.




• Credentialing Services for All Specialties

• Accounts Receivable Follow-Up for Practice Support
We would work your accounts on your system to maximize cash flow.


NEW Billing Client Example: A new client (a 6-physician family medicine group) liked their EHR, so the group asked us to bill using their billing system. Besides the benefit of keeping their EHR, the group is now experiencing greater efficiency and stability in their office by eliminating problems caused by biller turnover, vacations, diversion, and other time off.
Contact Ruby Marcocelli, Vice President at 412-788-8007 or rmarcocelli@fennercorp.com




Three Penn Center West Pittsburgh, PA 15276 fennercorp.com

“Calm and “Unparalleled market knowledge”566 Dorseyville - O’Hara Twp $780,000 400 Morewood - Shadyside $875,000 1521 Wightman - Squirrel Hill $920,000 409 Fox Chapel Rd - Fox Chapel $3,995,000
Physician Wellness Beyond Words— Advocating Wellness in Practice
PReRna mewawalla, mD
Physicians serve as the backbone of our communities and are responsible for treating people and helping them feel better every day. However, the immense pressure of treating patients, making life changing decisions, managing heavy workloads, all while trying to balance family life can lead to extreme burnout. The World Health Organization (WHO) defines burnout as a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by three dimensions: (1) feelings of energy depletion or exhaustion; (2) increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job; and (3) reduced professional efficacy .
Physicians experiencing burn-out and feeling depleted in their personal and professional lives is not just their individual or family problem. This is a broader societal issue, given that physician burnout is linked to worse patient outcomes. A study published in JAMA Internal Medicine found that burned out clinicians were twice as likely to report a recent medical error compared with those who were not burned out . Burnout has also been linked to a higher risk of medication errors, detachment from patients
leading to reduced patient satisfaction, lower productivity, and increased healthcare costs.
Physician burnout is very common across the board. Women physicians are even more likely to experience burnout compared to their male counterparts. 63% of women and 46% of men physicians reported being burnt out in 2022 . Factors such as being a primary caregiver, having more responsibilities on the personal front, gender discrimination in the workplace, pay disparities and disproportionate job demands may contribute to this. Additionally, women physicians may also experience bias and scrutiny related to their appearance, personality, and communication style, which can contribute to feelings of isolation and dissatisfaction with their work. Some physicians may also be subject to unconscious or sub-conscious bias due to their gender, ethnicity, age, sexual orientation, etc. which further creates a negative environment and exacerbates burn-out.
It is imperative to identify factors that fuel burnout among physicians leading to deteriorating well-being and wellness. It is important to not only address the symptoms of burnout but also focus on prevention and addressing the root causes. Burnout is a psychological syndrome that is
caused by chronic workplace stress. One of the primary reasons for physician burnout is the excessive workload they face daily. Physicians have to manage large patient populations and they are making life altering decisions every day. Additionally, significant time is also spent on documentation, reviewing patient results, responding to patient messages via EHR, coordinating with other healthcare professionals, and dealing with administrative tasks outside of patient care. Most employers do not give physicians enough time to do all the tasks they need to do aside from seeing patients so they can maximize their billing time. In the current environment, many hospital systems across the nation have experienced financial losses due to increases expenses, lower elective patient volume, etc. This is creating even more pressure on physicians to see additional patients and increase billing revenue.
We often hear of hospitals or employers trying to initiate programs to help physicians who are already burnt out. But organizations do little to take precautionary measures to prevent burnout from occurring in the first place or to at least make meaningful interventions when there
are early signs of burnout. So, what can be done to decrease physician burnout? One of the most important resolution areas that always comes up in physician surveys is having work flexibility. Being a physician requires long hours at work, leaving limited time for family or hobbies. Therefore, healthcare institutions can implement flexible working hours, remote working options for telehealth days and provide sufficient autonomy and empowerment for physicians to manage their own schedules, without being constantly micro-managed.
In addition, hospitals should provide adequate support staff. This could entail shifting the focus of administrative staff to nonvalue added activities to supporting physicians in the service of a patient. For instance, providing scribes to decrease the workload of documentation would go a long way. Having support staff to screen all results and bringing only the results which need to be acted upon to the physician’s attention. Adequate time should be allotted during regular working hours for other tasks that physicians need to do and not expect that to be an after-hour commitment. It is important to streamline administrative tasks and paperwork to reduce the burden on physicians. Identifying when one is burnt out and ensuring they can rest and take a break. It is essential to distribute the workload among the workforce, hire additional support staff, and delegate tasks to free up time for physicians to focus on patient care.
It is so important to have an efficient EHR that is easy to use. In the age of the iPhone and tablets, we still have EHRs that look like they are from the Stone Age. It is also vital to demonstrate frequent meaningful recognition and appreciation for physicians and treating them with respect.
In conclusion, physician wellness is a multi-faceted problem that needs addressing through a holistic approach. It is crucial to create a positive and supportive work environment that values compassion, empathy, and open communication. By promoting self-care practices, work-life balance, cultural change, and sharing the workload, healthcare institutions can reduce the risk of burnout amongst medical professionals. Ensuring physician wellness is critical not only for the physicians themselves but also for the patients’ safety and quality of care. Therefore, it is essential to prioritize the well-being of medical professionals to ensure a healthy and sustainable healthcare industry.
References
i https://www.who.int/news/item/2805-2019-burn-out-an-occupationalphenomenon-internationalclassification-of-diseases
ii Panagioti, M., Geraghty, K., Johnson, J., Zhou, A., Panagopoulou, E., Chew-Graham, C., ... & Esmail, A. (2018). Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA internal medicine, 178(10), 1317-1331.
iii https://www.forbes.com/sites/ corinnepost/2023/02/09/womenphysicians-face-burnout-crisisamid-lack-of-support-fromstaff/?sh=7bfa3e5b5d99

RiChaRD h. DaFFneR, mD, FaCR

Mary was a pleasant 82-year old woman, who, in the autumn of 1967, became a patient of mine in the Medical Clinic of the old E.J. Meyer Memorial Hospital (now Erie County Medical Center) in Buffalo during my internship. Mary had a history of severe abdominal pain radiating to her back for several years, and her frequent visits to the hospital had generated several pounds and multiple volumes of medical records. Repeated physical examinations as well as abdominal x-rays, upper GI exams, barium enemas, and intravenous urograms were all reported as being normal. She was labeled a “crock”. In March of 1968, she was admitted to my ward, after being found unresponsive at home by her daughter. The presumptive diagnosis was a stroke. A few hours after admission, she died. Fortunately (for us), her daughter consented to a post-mortem examination.
The autopsy revealed the cause of death, as well as the cause of her years of abdominal pain that had not only plagued her, but also had led to her being labeled a “crock”. Surprisingly, Mary had not suffered a stroke, nor a terminal cardiac event. Examination of the abdominal cavity revealed a large, non-calcified abdominal aortic aneurysm that was eroding into her third lumbar vertebra.
Crocks Die Too
The aneurysm had ruptured. These findings explained her longstanding symptoms perfectly. (Abdominal CT and ultrasound, both of which would have shown the aneurysm, were not available until years later). As we watched the autopsy, Andy, my resident turned to the rest of us and said in his Southern drawl, “Well gahs, crocks dah too.” It was a lesson we would not soon forget.
All physicians have experienced having to deal with symptomatic patients for whom they are unable to establish a diagnosis of the cause of those symptoms, despite using all our available modern diagnostic tools. By default, these patients are given a diagnosis of psychosomatic disease. Unfortunately, these patients are likely to return and challenge us again and again. When this occurs, we often label them a “crock”. Indeed, many times during my medical school training and internship when presenting such a patient on morning rounds, we would tell the attending physician that among the lab results, the patient’s “serum porcelain level” was elevated.
The diagnosis of a psychosomatic disorder is one of exclusion, after we have exhausted all possibilities of finding any pathology. And the key words here are the last seven words of the previous sentence. My late father serves as an example. In July 1992,
he began having vague abdominal pain radiating to his back, similar to Mary. He had been an otherwise healthy 86-year-old man, who seldom complained. GI barium studies, abdominal ultrasound, and abdominal CT studies were normal. (My partners who specialized in abdominal imaging confirmed this.) His gastroenterologist was considering labeling him a ”crock” but was disturbed by my father’s visible weight loss, and told me, “I think your dad has cancer. We’/re just not smart enough to find it.” In October he repeated the CT. The new exam showed a large carcinoma of the tail of the pancreas that was eroding into an adjacent lumbar vertebra. Unfortunately, in 1992 PET scanning combined with CT, that might have made an earlier diagnosis had not yet been developed. My dad died in February 1993.
I encountered similar patients when I was a General Medical Officer in the Air Force. One of the most common chief complaints I witnessed was, “I’m tired all the time,” in women in their early to mid 30’s. Multiple laboratory tests were all normal. Interestingly, I noticed a correlation between their complaints and their husbands’ ranks. On the enlisted man’s side, the rank was Technical Sergeant; on the officer’s side, the rank was Lt Colonel. The next higher rank for each
was Master Sergeant and Colonel, respectively. In both instances the husbands were likely to finish their military careers at the lower rank, which would affect their pensions in retirement. Their wives were understandably frustrated as they saw their husbands’ peers promoted while their husbands remained at a virtual dead end. Psychosomatic symptoms were a cover for their disappointment.
When all possibilities of disease have been ruled out, physicians faced with declaring the patient a “crock” or having “Mishugosi Syndrome” (from the Yiddish, mishigas [craziness] or mishugener [crazy person]) should look for a reason why the patient is exhibiting their symptoms. John, a 74-year-old “frequent flier” who visited the ER at Allegheny General on a

shortness of breath, chest pain, and abdominal pain to severe headaches. These complaints ordinarily result in the patient being admitted for observation and testing. John’s visits always coincided with whatever shift a particular attending physician, who incidentally had earned a degree in social work prior to going to medical school, was working. After several visits ended without any abnormalities being found, the attending put on her social worker’s hat and investigated John’s current living conditions. John lived alone with his dog on Pittsburgh’s North Side. His wife had died many years before and he was estranged from his children, all of whom lived far away. His frequent visits to the ER began when his dog died. John was lonely and the ER was one place where he could come for some interaction with caring people.
Sometimes technology, or the lack thereof contributes to a patient being labeled a “crock”. In Mary’s case CT and ultrasound had not yet been developed; in my father’s case PET CT had not been developed. In both of their cases, an early diagnosis was hampered by the fact that with bone destruction, approximately 50% of the bone structure must be destroyed before it is visible on a radiograph1 Today, MRI can show these elusive lesions early enough to affect the outcome. The paradox, however, may be that although we can make a diagnosis, we may not be able to cure the patient. In Mary’s case (in 1967) abdominal aortic surgery was in its infancy; in my father’s case (in 1992) an earlier diagnosis would not have changed the outcome. However, being able to establish a physical cause for the patient’s symptoms eliminates the diagnosis of “Crock”. As my resident Andy said over 50 years ago, “Crocks die too!”
Reference
For information contact John Fenner Email: fenner@fennercorp.com


1. Roberts CC, Daffner RH, Weissman BN, et al. ACR Appropriateness Criteria on metastatic bone disease. J Am Coll Radiol 2010; 7:400-9.
Dr. Daffner is a retired radiologist, who practiced at Allegheny General Hospital for over 30 years. He is Emeritus Clinical Professor of Radiology at Temple University School of Medicine.

The neighborhood of Troy Hill rests on a plateau overlooking the Allegheny River on Pittsburgh’s Northside; it is approximately 3 kilometers long and only 1 kilometer wide. In the center of this quaint village sits the Chapel of Saint Anthony of Padua which purportedly contains sacred relics, including the complete skeletal remains of a saint named Demetrius, a tooth of the chapel’s patron Saint Anthony, and a thorn from the true Crown of Thorns of the crucifixion of the Christ. All of the 4,000 to 5,000 relics in the chapel have original certificates of authenticity from the Vatican (the oldest of which dates from Aug. 12, 1716), except for one which mysteriously appeared on the evening of March 10 2023, — 102 and a half years following the birth of the village’s lifelong denizen, Lillian Abel Rausch.
“My mom Lillian and all of the Rauches love you!” I was told by a family member named Bobbie, who had married into my dear wife’s 12-sibling family from the North Hills suburbs several years after I had moved to the Steel City from the East Coast. “They all heard you say at the wedding at St. Anthony’s Chapel and afterward at the reception that you thought that Troy Hill was a wonderful, quaint old town and a
New Relic Discovered in Troy Hill
great place to live. Folks who grew up there or now live in Troy Hill must be very proud of the place and deserve to be there!”

home on a row-house-lined narrow street that terminated with a “tail” of downhill steps disappearing into the woods.

Having been a sports writer in my younger days, I may have been guilty of some measure of exaggeration in my comments (or more likely had taken too many toasts of champagne to the newlyweds at the reception); however, I was working at Allegheny General Hospital at that time and realized that Providence had assigned the would-be saints of the 20th century to the “Hilltop Heaven” of Troy Hill and left the devil to do his own thing in the Northside. Some blessed people look more beautiful in death than they or anybody else ever dared to in life, as if their inner being could no longer be airtightly concealed and emanates out of the body. I was absolutely convinced of this at Lillian’s wake at the funeral parlor just several blocks from her lifelong earthly

Here, Lillian spent most of her 102 and a half years raising a family of 5 daughters with her husband “Buck,” working tirelessly for the People Concerned for the Unborn Child and the Respect Life Foundation when the nest was empty, and spending her final years between reading voraciously in her living room parlor using a magnifying glass, praying daily among the relics of St. Anthony’s (a 1 mile walk) … and hobnobbing with yours truly at joint family events about the art of staying on top of things during the long life of serenity I coveted.
Far from the madding crowd’s ignoble strife, Their sober wishes never learn’d to stray;
Along the cool sequester’d vale of life They kept the noiseless tenor of their way.
— From “Elegy Written in a Country Churchyard” by English poet Thomas Gray.
Actually, my interaction with Troy Hill over the past 40 years has been largely vicarious through joint get togethers between the Lyons and Rausch clans at my in-laws Aunt Bobbie (Rausch) and Uncle Eddie’s unpretentious little home on “Good Lane,” where every possible family event and holiday was celebrated, no matter how trivial the occasion. The highpoint of birthday parties was the singing of the Lyons birthday medley which featured the entreaty:
“We hope you live to be 100/ We hope you live to be 100/ We hope you live to be 100/ And then 100 more!! The decades of this tradition were to reveal that Lillian alone had this wish granted!
Part of the allure for the children was the 3-foot high above-ground swimming pool which infringed upon much of the correspondingly little backyard. Hanging in the living room was a plaque stating the family’s institutional motto derived from Bobbie’s Troy Hill connection:

“He who knows he has enough is rich!”
…as well as the “mission statement” that was adopted by our children and our grandchildren:
Lillian never failed to attend a family gathering; likewise, it was unthinkable that she would ever fail to attend morning Mass at St Anthony’s, even in the final days when her vision and hearing were failing. She had the mistaken belief, in spite of the devotion and admiration of her many grandchildren and great grandchildren (which for an outsider like me were becoming too numerous to count), that if she was not seen or heard at the parties, surely she would immediately be forgotten. The saintly woman stoically bore the deep inner sorrow of having outlived several of her offspring and their spouses.
Time it was
And what a time it was
It was a time of innocence
A time of confidences
Long ago, it must be I have a photograph Preserve your memories
They’re all that’s left you
“Bookends” by Simon and Garfunkel
She was dogged in her advocacy for the disadvantaged and was connected with four generations of inhabitants of Troy Hill, visiting by foot the densely connected row houses of her neighbors throughout the village. It was said that she knew the whereabouts of all those resting in peace in the indigenous Voegtly Cemetery — even when the inscriptions on their tombstones had been worn away by the elements over two centuries.

connectedness was responsible for her grand longevity and for the prolonged duration of her keen memory and sharp cognitive powers, and I have scientific research to back up my claim! The wellknown “Roseto Effect”, first described in 1961 by Dr. Stewart Wolf and reported in JAMA in 1964, documents that the Italian villagers who emigrated to the small town of Roseto, Pennsylvania in the early 1900s and duplicated their small town Italian lifestyle, prioritizing close-knit living quarters and frequent socialization, experienced an overwhelming health benefit. This culture of inclusiveness seemed to be directly responsible for a comparatively lower rate of heart disease and better overall health than those neighboring nationalities who had adopted the “American way of life.” There was an incredibly low prevalence of myocardial infarction (ie. heart attacks) in the otherwise high-risk age group of men greater than 54 years of age, in spite of the fact that they continued to smoke unfiltered stogies, drink wine, and eat meatball and sausage fried in lard and cheese with reckless abandon.
Continued on Page 14
From Page 13
Researcher Wolf had this explanation: “The community was very cohesive. There was no keeping up with the Joneses. Houses were very close together, and everyone lived more or less alike. Elders were revered and incorporated into community life. Housewives were respected and fathers ran the families. There was very little crime.”
Regardless of their nationalities (Germans predominated), I suspect this same communal style of living contributed to a “Troy Hill Effect.” Lillian refused to move out of her diminutive home to the wealthier suburbs despite the supplications of her vast network of offspring. She died as she had lived: a peaceful dove.
Regardless of the lack of authenticity by the Vatican, I am certain that a piece of the heart and soul of the humble 102-and-a-half-year-old saintly woman will remain among the collection of relics in the chapel until the end of days. However, just in case I am mistaken, I wrote this story to dispel her fears that she could ever be forgotten!
You were meant for me!
I was meant for you!
I’m content, the angels must have sent you
And they meant you just for me!
—“Penny Serenade” (1929)
The author wishes to thank the Rausch Family for the information they provided and the permission to publicly reveal Lillian’s life of love of her faith, her family and of Troy Hill.
This story was originally published in the column OUT OF THE OLD BLACK BAG in the Pediablog (https://pediablog. com/2023/05/24/out-of-the-old-blackbag-45/ ). Under the editorship of Dr Ned Ketyer, the Pediablog was recently

2023 ACMS Bulletin Photo Contest
Please note instructions below for participating in the 2023 ACMS Bulletin Photo Contest:

1 Email your VERTICAL jpg photos with a resolution of 300 dpi or higher to ACMSBulletin@acms.org. Photos should be 8”W x 10”H. No more than three photos may be submitted.
2 You must be an ACMS member physician to submit photos.
3 Please save the photo file as the name of the photo. Also, please provide your name, specialty, email address and phone number in the email.
4 You will receive verification that your photo has been received and is eligible to be entered in the contest.
a) Horizontal photos will not be considered.
b) Photos with low resolution will not be considered.
c) Panoramic shots or photos featuring specifically identifiable individuals relatives will not be considered.
d) Be aware top third of image will be obstructed by Masthead.
5 5 The deadline for submission is Monday, October 3rd, 2023. After this date, a group of individuals selected by the ACMS Board of Directors and ACMS Editorial Board will vote on the top 12 photos.
6 Winners will be announced on the ACMS website, in the Bulletin and via email. The 1st-place winner’s photo will appear on the January 2024 cover; the remaining winning photos will appear on Bulletin covers throughout the year.
7 Please continue to check the ACMS website and future issues of the Bulletin for further updates and reminders.
8 If you have any questions, please contact Contact Cindy Warren at ACMSBulletin@acms.org.


Dr. Eugene A. Stead Jr., famed Chairman of Medicine at Duke University was the greatest medical educator of the last half of the 20th century. The following story about Dr. Stead was essentially a recollection of former Allegheny Health Department Director, Dr. Bruce Dixon. Stead had built Duke into what many considered to be the finest department of medicine in the country. More of his trainees and faculty became Internal Medicine Department Chiefs, Division Heads or Residency Directors than any other educator in the history of American Medicine with the possible exception of Sir William Osler. Additionally, the profession of “physician assistants” was invented by and nurtured by Dr. Stead. There were many Stead trained physicians at the University of Pittsburgh Medical Center (UPMC) in the era from 1960 to 2000, including the legendary Chief of Medicine, Dr. Jack Meyers; Residency Director, Dr. Bruce W. Dixon; Cardiology Division Head, Dr. James Leonard; and Rheumatology Division Head Dr. Gerald Rodnan. This gave the department of Medicine in Pittsburgh a real “Steadian flavor.”
It was therefore with a great deal of excitement that the medical residents at Presbyterian University Hospital were informed that Dr. Stead would
A VISIT FROM DR. STEAD
“What This Patient Needs is a Doctor”
be coming to the hospital as a visiting professor. Stead’s time was limited and so he chose to confine himself to simply making teaching rounds with one of the medical teams. This was somewhat disappointing to those who expected a lecture focused on one of Stead’s many areas of expertise such as congestive heart failure, syncope, shock, peripheral vascular disease, or sarcoidosis. Nevertheless, they also knew that Stead was a renowned bedside teacher. Teaching rounds were always patient centered at the bedside at Duke as well as at UPMC and so an entourage of residents, interns and medical students proceeded out of the medical conference room with Dr. Stead and down the hall towards the patient’s bedside.
At this point, Dr. Stead (in typical Steadian fashion) turned around and asked in his mellow Southern drawl, “Fellows, what are we going to talk about this morning?” That of course meant what was the patient’s tentative diagnosis or admitting problem. The senior resident on the team had chosen a patient with sarcoidosis and hypercalcemia. He naturally thought this would be a very interesting case to discuss. “Dr. Stead, we are going to have the intern present a patient with sarcoidosis and an elevated blood calcium level.” “Well, that sounds very interesting,” said Dr. Stead, “Always
liked sarcoidosis, very interesting systemic disease. There is still a whole lot to learn about that disease, but I don’t think I want to talk about that today. What else ya got?” At this the residents, interns, and students stared in disbelief. Had they heard him right? He didn’t want to talk about that! Was he serious? Stead looked around at the shocked crowd and then focused his gaze at the senior resident. “What else ya got?” “Well. we are also prepared to present a case of streptococcus viridans endocarditis.”
“That’s very interesting too” Stead replied. “My colleague, Dr. Paul Beeson was one of the first persons to use penicillin to successfully treat streptococcus viridans endocarditis and my famous mentor, Dr.
Soma Weiss wrote the best description of the natural history of endocarditis. That case involved a medical student by the name of Alfred Reinhart who died from streptococcus viridans endocarditis. Mr. Reinhart died in 1931. Dr. Weiss reported his case about 10 years later. That paper is a medical classic. I recommend it to all of you. But except for this, I really don’t wish to discuss endocarditis. What else do you have?” At that, the resident went through a litany of cases, hesitating now and then to see if the great Dr. Stead was interested. Stead gave a negative reply to all of them and then asked, “Who is your least interesting patient?” The senior resident looking surprised and confused said haltingly, “That would be Bessie. She’s at the far end of the hall and is waiting for nursing home placement. She has an ankle ulcer, a decubitus ulcer, and some cognitive issues.” “Dementia?” “Yes, sir, we think it is a senile form of dementia.” “Well, let’s go see this lady” and then Dr. Stead quickly led the team to the room at the end of the unit and the bedside of a lady we will call “Bessie Jones.”
After the intern presented the patient’s history and physical examination, Dr. Stead commented that “you must know this lady pretty well to be calling her by her first name.” Stead then asked the intern several questions regarding Bessie’s social history; where did she live, what was that neighborhood like, where was she born, was she married, did she have children or relatives and if so where did they live, did she get visitors, did she choose a nursing home or is it being assigned? Her team of doctors knew that she had never married; her only local relative was her niece. Her niece visited Miss Jones occasionally. Her nurse was in the room

at the time and she replied to Dr. Stead that there was an older man that visited her almost every day from 3 pm to 6 pm. “It would appear then that this man is a close and loyal friend of Miss Jones.” He then looked at the intern and in a very kind and mannerly drawl asked, “don’t you think we should know who this man is and wouldn’t it be nice if the nursing home is easily accessible to him?” “I don’t think you know Miss Jones as well as you should. Let’s see if we can get to know her better.” With that Stead began his own superlative history and bedside examination. Stead first established that her cognitive dysfunction was minimal. She had a bilateral cerumen impaction and couldn’t hear or understand the intern’s “big words”. She replied to Stead’s questions and comments perfectly well as he leaned towards her and spoke into the least blocked ear canal in easily understood language. Stead then commented on how common hearing problems and especially undiagnosed cerumen impaction were mistaken in the elderly for cognitive
dysfunction. He established that she was fairly poor and lived in a dangerous neighborhood. The man who visited her was the widower of Bessie’s best friend. They had, sort of, become companions. He lived in a better neighborhood close to the hospital and a few nursing homes. She had to leave school in the 6th grade and had worked for decades as a cleaning lady and she had other nieces and nephews in Virginia where she was born. For years she had visited Virginia every summer but she preferred Pittsburgh.
Then Stead demonstrated his observations on the sacral and ankle ulcers and whether these were purely pressure related or whether venous or arterial ischemia played a role. If arterial ischemia was a factor, a vasodilator might help. If venous stasis was the culprit and arterial circulation was still good, elevating the extremity would help. His conclusion was that venous stasis was a major cause. He then went into a question-and-answer discussion
Continued on Page 18
From Page 17
of the autonomic nervous system in the elderly and how it affects elderly blood vessels and blood flow. Stead gently elevated the legs and noted slight pallor in the nail beds that recovered fairly promptly. The arterial pulses at multiple levels in the lower extremities were normal. He discussed the vascular anatomy of the lower extremities and where the vulnerable sites were located for venous or arterial insufficiency. It was an educational tour de force. More importantly, it directly benefited Miss Jones. She understood the situation better, became more involved in her care, and complied better with frequent turning to alleviate pressure on the ulcers. Elevation of the leg and pressure dressings helped to improve the venous circulation without impairing arterial inflow. An ENT specialist removed all the cerumen from her ear canals. Her family in Virginia was willing to contribute some money towards a short nursing home
stay. She was placed in a facility that was on a bus route easily accessible to her friend. Her ulcers eventually healed. The house staff was in awe of what Stead had just done. One of the interns asked him, “Dr. Stead, why did you do that? Why did you want to see the least interesting patient?” Stead smiled and in his easy North Carolina country style replied, “You fellas are all over that sarcoidosis case, same thing with that fellow with endocarditis. Those folks will get good care because you boys are all up to snuff on that stuff. Me, I’m worried about the old lady at the end of the hall. Plus, just say for me I think you will find that when you get to know the patient well and think deeply about their clinical problems all patients are interesting and deserve the best attention we can give them.” This ended the most important educational experience of my medical career.
“There are lots of M.D.s, but there are too few doctors!”
—Dr. Eugene A. SteadReferences
Lazlo, John M.D., Neelon, Francis A. M.D., “The Doctor’s Doctor, A Biography of Eugene A.Stead Jr., M.D.”, Carolina Academic Press, Durham, North Carolina, 2006.
Stead, E.A. Jr. M.D., “What This Patient Needs is a Doctor”, Duke University Medical Center Press, Durham, North Carolina, 1978.
Tischler, Peter V, “Soma Weiss, Alfred Reinhart, and the care of the patient”, Perspect Biol Med 2010 Winter;53(1):75-86.

Lamb, Michael G. M.D., Personal Recollections and Notes.

In Memorium

H. Lee Dameshek, MD Former ACMS President (1984)

H. Lee Dameshek, M.D., age 86, of Pittsburgh, passed away peacefully at home on Saturday, July 1. Dad, Lor, Pop-Pop was born in Baltimore on March 16, 1937, and was raised in Harrisburg, Pennsylvania by his late parents, Sam and Rose. He loved growing up with his brothers, Allan (Nancy) and the late Fred (Jackie). He graduated from Franklin & Marshall College and the Tufts University School of Medicine. He completed his internship and residency at Presbyterian University Hospital and was a hematology fellow at Ohio State University Hospital. He practiced hematology and oncology at Presbyterian University Hospital in Pittsburgh from 1969 to 1997. He was clinical instructor and professor for many great physicians through the years. He served as staff president at Presby and as president of the Allegheny County Medical Society,
as well as on the board of directors for the Leukemia & Lymphoma Society of Western PA and as vice president for the American Cancer Society. He was a force in the Pittsburgh medical community. Caring for hundreds of patients over the years was his superpower. He saved many lives and helped those he could not, to die with dignity. The countless letters he received from these patients and their families upon his retirement are a testament to his legacy. His greatest joy came from his four children and 13 grandchildren — and when the Red Sox won the World Series. He shared his pride of his family’s accomplishments, big and small, with anyone who would listen. Throughout his life, Lee was an avid sports fan — enjoying (sometimes suffering with) the Red Sox and Celtics, Pitt, the Penguins and Steelers. He served as team doctor to Pitt football and Penguins hockey for many years — and passed his love of the teams onto his children and grandchildren. Lee was lucky to spend retirement between Pittsburgh and Scottsdale, Arizona, as well as frequently visiting his children and grandchildren. For someone who adored eating so much, it is funny that he never knew how to read a menu. You could always find him watching the latest game or MSNBC, which is ironic since he could never figure out how to operate the TV remote. He served as the faithful Tooth Fairy Witch and family birthday card artist and author. Among his favorite people were Ted Williams, Frank Sinatra, Mario Lemieux and Bill Russell. He enjoyed many golf matches, including seven holes-in-one, with good friends at Green Oaks CC, Westmoreland CC and around Scottsdale. The ultimate gift to Lee was to marry funny, caring, loving Michelle (Zubasic). Over the years, they shared
cruises, trips to Barcelona, England, and Italy — and treasured family holidays and trips to Hilton Head, Cape Cod and Bethany Beach. They loved the simple pleasure of taking in a movie and grabbing an early dinner. They are luckier than most to have had 57 years together. He is survived by Michelle, brother Allan (Nancy), and loving children, Lynne (Brian) Shine of Buffalo, New York; Amy (Mark) Brumbaugh of Oakmont, Pennsylvania; David (Beth) Dameshek of Encino, California; and Debbi (Eddie) Francl of Elgin, Illinois. His 13 grandchildren all had the wonderful opportunity to know and love their Pop-Pop, singing and skipping with him. His favorite job was to dance and sing them to sleep as babies. As they grew, he loved playing games and watching movies and sports with them. Pop-Pop was much loved, and his memory will be a blessing — he will be sorely missed. We hope wherever he is now, there is a full cup of hot decaf coffee — and no cinnamon in sight. Services were held privately with his family. Donations in Lee’s memory may be made to the Leukemia & Lymphoma Society of Western Pennsylvania (givenow.lls.org/ give/HLD). Arrangements entrusted to Ralph Schugar Chapel, Inc., family owned and operated. schugar.com PJC https://jewishchronicle.timesofisrael. com/h-lee-dameshek-m-d/
Auvelity®: Shortening the Onset of Action in Major Depressive Disorder
ashley n. RoDgeRs anD KaRen m. FanCheR, PhaRmD, BCoPMajor depressive disorder (MDD) is a leading cause of disability worldwide, and significantly contributes to the overall global burden of disease.1,2 This disease state is biologically based and can impair a patient’s social, occupational, and everyday functioning.3 The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) requires that a formal diagnosis of major depressive disorder must include five or more symptoms over a two-week period, with at least one of the symptoms of depressed mood or anhedonia. Other symptoms include insomnia, changes in eating habits, loss of interest in daily activities, fatigue, psychomotor changes, sense of worthlessness, impaired ability to concentrate, excessive guilt, and suicidal ideations.4 A patient can be diagnosed with major depression disorder at any time in life depending on differeces in one’s social, personal, or environmental factors. In 2020, 17% of those who struggled with major depressive disorder were between the ages of 18-25 years.5
Currently available medications to treat major depressive disorder center around the mechanism of increasing neurotransmitters within the brain, including serotonin, norepinephrine, and/ or dopamine. A common first line agent class that is used to treat major depressive disorder is the selective serotonin reuptake inhibitors (SSRIs).6 These medications block the serotonin transporter, SERT, from the reuptake of serotonin back into pre-synaptic terminal within the central nervous system (CNS). This results in an increase in the amount of serotonin present within the synaptic cleft, leading to improvement of depression symptoms. Another common medication class used in the treatment of this disease state is serotonin/norepinephrine
reuptake inhibitors (SNRIs). These medications work on the serotonin transporter, SERT, and the norepinephrine transporter, NAT, blocking the reuptake of serotonin and norepinephrine into the presynaptic terminal.6 This allows for both serotonin and norepinephrine to be available at increased levels within the synaptic cleft. Other common medications used to treat depression include atypical antidepressants, serotonin modulators, tricyclic antidepressants (TCAs), monoamine oxidase inhibitors (MAOIs), and N-methyl-D-aspartate (NMDA) receptor antagonists.6
Although the currently available antidepressants have shown efficacy in lessening the symptoms of depression, these medications often take several weeks to produce clinically meaningful effects.2 Not only do these medications take time to reshape the receptors within the brain, but they also have varying effects on patients. Hence, an agent that may work for one patient may not produce the same results in another. In the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial, two-thirds of patients with depression failed to achieve remission of their depression symptoms with the first-line treatment.2 This illustrates that major depression disorder is different for everyone that experiences this disease state. Depending on a patient’s circumstances, waiting six to eight weeks to derive meaningful benefit from a medication may not be feasible.
Within the last two decades, it has been found that subanesthetic doses of the glutamatergic drug ketamine, an NMDA receptor antagonist, had rapid antidepressant effects in treatment resistant patients with depression, leading to an investigation of other agents in this class.1
Accordingly, one agent that has been considered is dextromethorphan. When taken orally in humans, this medication is rapidly metabolized by the CYP2D6 enzyme, making it difficult to achieve potential therapeutic plasma levels of substrate compound.7 To achieve therapeutic plasma concentrations of dextromethorphan, a CYP2D6 inhibitor must be utilized to block the metabolism of this medication. Bupropion, with distinct centrally acting mechanisms of action, was a strong choice as a metabolic inhibitor of dextromethorphan and has potential for pharmacological synergy and clinical use across of neuropsychiatric conditions.7 This led to the creation of dextromethorphan/bupropion, also known as AXS-05 and marketed under the brand name Auvelity®, which was approved by the United States Food and Drug Administration (FDA) for the treatment of major depressive disorder in August 2022.1 With this combination, the aim is to shorten the time it takes to achieve clinical improvement of depression symptoms.
Dextromethorphan-Bupropion (Auvelity®)
This medication has a unique mechanism of action in that it uses bupropion, a common antidepressant and tobacco cessation agent, to block the metabolism of dextromethorphan. This allows dextromethorphan to reach clinically significant plasma levels. Alone, dextromethorphan acts as an uncompetitive NMDA receptor antagonist and a sigma-1 receptor agonist, stimulating the central nervous system.3
As an NMDA receptor antagonist, dextromethorphan blocks the inhibitory neurotransmitter gamma-aminobutyric acid (GABA) from binding to the NMDA receptor, decreasing the release of GABA into the central nervous system. This allows for a decrease in the inhibition of the ex-
Materia Medica
citatory neuron glutamate.8 Dextromethorphan then acts to increase serotonin levels in the brain by acting as a serotonin reuptake inhibitor and sigma-1 agonist to increase serotonin levels in the dorsal raphe of the brain.7 Together, both these medications act as norepinephrine reuptake inhibitors and alpha-4-beta-2 nicotinic (nACh) antagonists.7 Bupropion also acts as a dopamine reuptake inhibitor. Between dextromethorphan and bupropion, these two medications combine the mechanisms of action of distinct antidepressant therapeutic agents into one therapeutic agent.7 After repeat administration of dextromethorphan-bupropion, steady state plasma concentrations of the individual agents are reached within eight days.1
The GEMINI Study
The GEMINI study was a phase 3 trial that assessed the efficacy and safety of dextromethorphan-bupropion compared to placebo in the treatment of patients with MDD.3 This trial was double-blinded and placebo-controlled over a six week period across 40 different centers in the United States from June 2019 – December 2019. Patients were selected for this study based upon their scores on the Montgomery-Asberg Depression Rating Scale (MADRS) and the Clinician Global Impression-Severity scale (CGI-S). Men and women between the ages of 18-65 that had a total MARDS score of 25 or higher, signifying moderate or greater severity of depression, a CGI-S score of 4 or higher, and a diagnosis of depression according to the DSM-5 criteria without psychotic features were considered to be appropriate candidates for the study.3 As part of the screening process of each patient, an independent assessor confirmed the eligibility and symptom severity of each patient through a clinical review of patient medical history and clinician- and patient-reported outcome measures. Key exclusion criteria for this study included those who had diagnosed bipolar disorder, psychotic disorder, panic disorder, obsessive-compulsive disorder, treatment resistant depression (defined as 2 or more adequate failed antidepressant treat-
ments), alcohol/substance use disorder within the last year, clinically significant risk of suicide, and history of seizure disorder.3
Patients were randomly assigned in a 1:1 ratio to receive either dextromethorphan-bupropion (45mg-105 mg) or placebo orally for 6 weeks. The randomization of the treatment was performed by a central interactive web response system.3 Patients received their medication once daily for the first three days, and then twice daily for the remainder of the trial period. Study visits occurred at 1, 2, 3, 4, and 6 weeks after the baseline visit. The primary endpoint for this study was the change from baseline to week 6 in the MARDS total score. The key secondary endpoints included remission, defined as MADRS total score of less than or equal to 10, at week 2, and clinical response, defined as greater than or equal to 50% reduction in MADRS total score at week 6.3
Dextromethorphan-bupropion significantly reduced MADRS total scores compared to placebo at all time points that were accessed.3 The least-squares mean change from baseline to week 6 in MADRS total score was -15.9 points in the dextromethorphan-bupropion and -12.0 points in the placebo group (least squares mean difference of -3.87; 95% CI, -1.39 to -6.36; p = 0.002). Remission, defined as a MADRS total score of less than or equal to 10, was achieved by a significantly greater percentage of patients in the dextromethorphan-bupropion group than in the placebo group at week 2 (16.9% and 7.5% respectively; p = 0.013) and at every time point thereafter. Clinical response, defined as greater than or equal to 50% reduction in MADRS total score at week 6, was achieved by 54% of patients in the dextromethorphan-bupropion group and 34% in the placebo group (p < 0.001). The authors concluded that dextromethorphan-bupropion treatment resulted in early and substantial achievement of remission on the MADRS total score, with statistically significant separation from placebo demonstrated at week 2 and at every subsequent time point.3
Adverse Effects
In the GEMINI trial, the percentage of patients who experienced an adverse event was 61.7% in the dextromethorphan-bupropion group and 45.1% in the placebo group. The most common adverse events in the dextromethorphan-bupropion group included dizziness, nausea, headache, somnolence, and dry mouth.3 Other adverse effects of this medication include excessive sweating and sexual dysfunction.9 The COMET study was a Phase III, multicenter, open-label long-term safety study assessing dextromethorphan-bupropion for up to one year.9 In this study, 876 patients with MDD were included; patients could be rolled over from prior studies of the agent or newly enrolled. Long-term safety in this study was consistent with the results observed in other clinical studies, including GEMINI.9
Administration Considerations
The recommended starting dose is one tablet taken once daily in the morning for three days, then increased to one tablet twice daily (taken at least eight hours apart). Doses may be taken with or without food.1,9 A dosage reduction to one tablet once daily in the morning is recommended for patients with moderate renal impairment, patients who are known to be poor CYP2D6 metabolizers, and when co-administered with strong CYP2D6 inhibitors. Co-administration with strong CYP2B6 inducers should be avoided.9 Due to the risk of serotonin syndrome, dextromethorphan-bupropion should not be administered with a monoamine oxidase inhibitor (MAOI) or within fourteen days of stopping treatment with an MAOI; similarly, and MAOI should not be used within fourteen days of stopping dextromethorphan-bupropion.1
The patient’s baseline blood pressure should be assessed prior to the initiation of dextromethorphan-bupropion and periodically during treatment.9 Patients should also be screened
Continued on Page 22
Materia Medica
From
for a history of bipolar disorder, mania, or hypomania prior to initiating therapy, as these disorders may be activated by treatment with an antidepressant.1
Dextromethorphan-bupropion is contraindicated in patients with seizure disorders and in those with disorders that have an increased risk of seizure, including a current or prior diagnosis of bulimia or anorexia nervosa, or where there is abrupt discontinuation of alcohol, benzodiazepines, barbiturates, or anticonvulsant drugs.1 As with any antidepressant, this medication may increase suicidal thoughts and actions in young adults, especially in the first month of treatment or when the dose is changed.9 The prescribing information contains a Black Box Warning regarding an increased risk of suicidal thoughts and behaviors in pediatric and young adult patients.9
Use in Other Disease States
Treatment with dextromethorphan-bupropion was effective in reducing symptoms of agitation in patients with Alzheimer’s disease in a phase 2/3 study known as ADVANCE-1.1 A significantly greater change from baseline was observed in 357 patients with a probable diagnosis of Alzheimer’s compared to placebo at three weeks and five weeks. Two other studies that assess the efficacy and safety of in patients with Alzheimer’s disease-related agitation are ongoing.10
Dextromethorphan-bupropion was significantly more effective than bupropion alone when used for smoking cessation treatment in a phase 2, double-blind trial of 58 smokers.1 Those in the dextromethorphan-bupropion arm had a 25% greater reduction in the number of cigarettes smoked per day over the three-week treatment period than those in the extended-release bupropion arm.1
Implications for Practice
While the reported data for the use of dextromethorphan-bupropion is intriguing, it only includes short-term data on efficacy and adverse effects. Longer-term follow-up is needed to determine if the impressive response rates are sustainable, and whether there are any long-term safety concerns.3 Likewise, currently published studies excluded patients with psychosis or other psychiatric disorders, alcohol and/or substance abuse disorders, a clinically significant suicide risk, and significant medical co-morbidities; therefore, the application of the study findings may not reflect clinical practice.3 Dextromethorphan-bupropion has not been evaluated in pediatric patients or patients who are over 65 years of age with MDD.1 Finally, there is limited data on the use of dextromethorphan-bupropion in patients with treatment-resistant depression.11
A further concern is abuse potential with longterm use of dextromethorphan.11 The populations included in published studies were not considered to be at risk for abuse; more data is needed to determine whether the use of this agent would confer an additional liability in patients with a history of addiction, or conversely, whether it could be a potential treatment option for patients with opioid use disorder.11
The landscape of treatment options for MDD continues to evolve. Treatment strategies will always need to be individualized, and should consider the currently available agents, anticipated adverse effects, onset of action, and clinical practice recommendations. The GEMINI trial data supports the consideration of dextromethorphan-bupropion for the treatment of MDD. However, the specific place in therapy of this agent remains undefined, and long-term outcomes are yet to be reported. Further information and extended follow-up data are eagerly awaited.
Ms. Rodgers is a Doctor of Pharmacy candidate at Duquesne University School of Pharmacy. Dr. Fancher is an Associate Professor of Pharmacy Practice at Duquesne University School of Pharmacy. She also serves as a Clinical Pharmacy Specialist in Oncology at the University of Pittsburgh Medical Center at Passavant Hospital. She can be reached at fancherk@duq.edu or (412) 396-5485.
REFERENCES
1. Keam SJ. Dextromethorphan/Bupropion: First Approval. CNS Drugs. Nov 2022;36(11):1229-1238. doi:10.1007/ s40263-022-00968-4
2. Tabuteau H, Jones A, Anderson A, Jacobson M, Iosifescu DV. Effect of AXS-05 (Dextromethorphan-Bupropion) in Major Depressive Disorder: A Randomized Double-Blind Controlled Trial. Am J Psychiatry. Jul 2022;179(7):490-499. doi:10.1176/ appi.ajp.21080800
3. Iosifescu DV, Jones A, O’Gorman C, et al. Efficacy and Safety of AXS-05 (Dextromethorphan-Bupropion) in Patients With Major Depressive Disorder: A Phase 3 Randomized Clinical Trial (GEMINI). J Clin Psychiatry. May 30 2022;83(4) doi:10.4088/JCP.21m14345
4. DSM-5 Changes: Implications for Child Serious Emotional Disturbance. 2016. CBHSQ Methodology Report.
5. National Institute of Mental Health. Major Depression. Available at https://www.nimh.nih.gov/health/statistics/major-depression. Accessed May 15, 2023.
6. Sheffler ZM, Patel P, Abdijadid S. Antidepressants. StatPearls. 2023.
7. Stahl SM. Dextromethorphan/Bupropion: A Novel Oral NMDA (N-methyl-d-aspartate) Receptor Antagonist with Multimodal Activity. CNS Spectr. Oct 2019;24(5):461-466. doi:10.1017/ S1092852919001470
8. Krystal JH, D’Souza DC, Mathalon D, Perry E, Belger A, Hoffman R. NMDA receptor antagonist effects, cortical glutamatergic function, and schizophrenia: toward a paradigm shift in medication development. Psychopharmacology (Berl). Sep 2003;169(3-4):215-33. doi:10.1007/s00213-003-1582-z
9. Auvelity [prescribing information]. New York, New York: Axsome Therapeutics, Inc., 2022.
10. ClinicalTrials.gov. United States National Library of Medicine. Available at www.clinicaltrials.gov . Accessed May 15, 2023.
Supreme Court May Force Providers to Take Deliberate Steps to Avoid a False Claims Act Lawsuit
louRDes sanChez RiDgeOn June 1, 2023 the U.S. Supreme Court unanimously decided a pivotal issue related to the False Claims Act (FCA)i that will make it more difficult for health care providers to assert a defense. The Supreme Court held that a defendant who knowingly submits a false claim to a government agency seeking reimbursement is liable under the FCA even if the regulation pertinent to the claim is ambiguous and subject to different reasonable interpretations. No longer can a provider argue that the regulation is ambiguous. As long as the government can prove that the provider knew the claim was false, the regulation’s ambiguity is irrelevant. As a consequence, providers will need to take steps to document their basis and beliefs of the truthfulness of their claims submitted to Medicare, Medicaid and other government programs to avoid an FCA lawsuit. It is important for health care providers to understand the FCA, know its ramifications and potential liability because it is one of the statutes most often used against health care providers. The FCA was enacted in 1863 in response to massive frauds on the federal government by large contractors during the Civil War. Today, the FCA is used largely in cases involving health care fraud and defense contracting. The FCA is a federal statute that prohibits anyone to knowingly present or cause the presentation of a false or fraudulent claim for payment or approval to a government agency. For health care providers, the submission of claims to Medicare, Medicaid or any government health care program is most often the basis of an FCA lawsuit. The FCA allows private parties, called “relators” to step into the shoes of the Federal government, who is the victim of the fraud, and bring a civil lawsuit against a party whom they
claim has defrauded the Federal Government. In health care, it is often brought because of allegations of upcoding, double billing, phantom billing, kickbacks and other frauds. Once a relator files a complaint, usually under seal, the Government investigates the complaint and decides whether to intervene in the lawsuit. If it intervenes, it proceeds to prosecute the case. If the Government declines to intervene the relators are still able to continue with the lawsuit. The relator’s compensation, however, is significantly higher if the Government declines to intervene and the relator wins the lawsuit. Many times, the provider’s knowledge of falsity is at issue. The FCA requires the relator or the Government to prove two essential elements:
(1) the falsity of the claim and (2) the provider’s knowledge of the claim’s falsity. The provider’s knowledge that a conduct is wrongful is called “scienter”. The FCA defines the term “knowingly” as the defendant 1) having actual knowledge of the falsity 2) acting in deliberate ignorance of the truth (meaning, purposely avoiding taking steps to confirm the veracity or falsity of the information) or 3) acting in reckless disregard of the truth (meaning, being conscious of the risk of falsity but submitting the claim anyways). In U.S. ex rel. Schutte v. Supervalu Inc,ii Supreme Court faced the issue of whether the FCA is violated when there is an ambiguous regulation subject to different reasonable interpretations but where the provider, nonetheless, knew that the claim submitted was false. In Supervalu, the relator alleged that Supervalu and Safeway (the “pharmacies”), submitted false claims to Medicare and Medicaid when it charged its retail prices for medications as their “usual and customary” prices instead of their discounted
prices, even though the pharmacies charged their discounted prices a majority of thetime. Medicare and Medicaid state plans offer outpatient prescription drug coverage to its patients but the reimbursement to the pharmacies is limited to the lowest of different amounts including the provider’s usual and customary charges to the general public. The relator argued that claims seeking reimbursement for their retail prices instead of the discounted prices were false claims. The Pharmacies argued that the term “usual and customary” was ambiguous and that other pharmacies may have reasonably interpreted the term to be the retail prices. They argued that this, by itself, should be enough to dismiss the FCA case. The Court held that whether the term was ambiguous is irrelevant. The issue is whether the provider knew the invoices were false or at least knew that there was a high probability that it was false at the time of submission. This ruling substantially limits a provider’s defense to an FCA suit.
Burden of an FCA lawsuit
FCA lawsuits are filed in Federal Court under seal until the court unseals it. Many times, a target is unaware that they are under investigation. Most often the first inkling of an investigation is the Government’s issuance of a Civil Investigative Demand (CID). A CID is a strong tool used by theGovernment where it demands documents, answers and oral testimony from the health care provider. The return of these documents and testimony often leads to an FCA lawsuit and/or criminal indictment. It is very important to engage an attorney to respond to the CID. If a lawsuit ensues, the burden on the provider is enormous. An FCA lawsuit is not only expensive but it disrupts the practice,
Continued on Page 24
Legal Summary
From Page 23
causes mental anxiety and a loss of reputation. Therefore, health care providers should avoid the possibility of a lawsuit.
Avoiding a lawsuit
Because the Government or relator must prove that the health care provider knew that the claim was false or was deliberately ignorant of the truth or recklessly disregarded the truth, health care providers must document their decision-making process relating to statements or claims submitted to government agencies such as CMS. If there is clear guidance from the government agency on a particular regulation then the health care provider should document the guidance. For those ambiguous situations where there is little or no guidance, providers should document how they interpreted the regulations and attach any supporting documents. Providers may request written clarification from CMS or pertinent government agency, which, as a practical matter is often impossible. But
even if CMS fails to respond, the fact that the provider sought clarification is a strong indicator that the provider intended to comply. Providers may also request legal advice. However, any communication seeking legal advice from an attorney is privileged and confidential. This means that if the provider decides to disclose the privileged communications to the Government and/or relators, he/she would have to waive the attorney-client privilege. Therefore, attorney-client communications should be drafted knowing that its disclosure to the Government and/or relator is a strong possibility. If the defendant sought legal advice giving the lawyer truthful and complete information so that the lawyer can give a valid opinion as to theambiguous regulation, and the provider complies with the advice, the provider may assert that he/she relied on the legal advice which will significantly weaken the government or relator’s proof of scienter. In addition, having a strong and effective compliance plan fortifies the defense.


These steps build a strong wall against FCA attacks by the Government and/or relator. If these walls are raised, it will be an uphill battle for the Government or relator to successfully prove the provider’s scienter as required by the FCA.
DISCLAIMER: This article is for information only and should not be considered legal advice. To obtain legal advice on this matter, please contact an attorney experienced in this area of law.
Lourdes Sanchez Ridge practices law at Pietragallo Gordon Alfano Bosick & Raspanti LLP. She focuses on white-collar criminal defense. She is licensed in Pennsylvania, Washington, D.C. and Florida. Her bio can be found at https://www.pietragallo.com/lawyers.
i 31 U.S.C. §§ 3729 – 3733
ii 598 U. S. ____ (2023). The Supreme Court consolidated two cases: United States ex rel. Schutte v. SuperValu Inc., No. 21-1326, and United States ex rel. Proctor v. Safeway, Inc., No. 22-111.
Pittsburgh Ophthalmology Society announces new President Pamela P. Rath, MD

Pamela P. Rath, MD, was installed as president of the Pittsburgh Ophthalmology Society (POS) during the annual banquet held March 9, 2023 at the Hotel Monaco in Pittsburgh, PA. She has been an active member of the POS since 2006, serving as a Board member since 2016 and Course Director of the Ophthalmic Personnel Meeting from 2016 through 2023. Dr. Rath will serve a two-year term, which ends March 2025.
Dr. Rath is a Pittsburgh native who received her medical degree from the State University of New York at Buffalo where she was elected to Alpha Omega Alpha honor medical society. She completed her residency at the University of Minnesota where she received multiple awards including for research, teaching and patient care and compassion. She completed a fellowship in medical retina, inherited retinal diseases, electrophysiology as well as ocular oncology at Moorfields Eye Hospital in London, England.
Board certified by the American Board of Ophthalmology, she is a retina specialist at Everett and Hurite Ophthalmic Association. She has 20 years of experience specializing in the treatment of medical retinal diseases. She is also trained in the diagnosis and treatment of intraocular tumors and hereditary diseases of the retina.

She looks forward to working with the POS board of directors to continue the tradition of excellence in offering high level educational programming to POS members for both the monthly meeting series and the annual meeting.
The Society would also like to congratulate Laurie A. Roba, MD who was elected as President-Elect.
Dr. Roba will serve a two-year term and succeed Dr. Rath as President in 2025.
Society News
Pittsburgh Ophthalmology Society Announces 2023-2024 Monthly and Annual Meetings Dates and New Monthly Meeting Location!

Pamela P. Rath, MD, President of the Pittsburgh Ophthalmology Society (POS), is pleased to announce the 2023-2024 POS Monthly Meeting Series and Annual Meeting dates. A total of six meetings are scheduled, beginning September, and concluding with the Annual meeting on March 8, 2024.

The Society will host the monthly meetings as in person events at their new monthly meeting location, the PNC Champions Club at Acrisure Stadium (100 Art Rooney Ave, Pittsburgh, PA 15212). The venue is centrally located on the North Side with parking available in several lots that are within walking distance of the stadium. Please visit the POS website for additional details.

Registration begins at 4:00 pm with the first lecture beginning at 4:30 pm. The Agenda includes a Resident Case Presentation. This year’s second-year Resident presenters from the UPMC Vision Institute include: Doowon Huh, MD; Saloni Kapoor, MD; Patricia Campos, MD; Raven Diacou, MD; and Gideon Nkrumah, MD.
Members will receive registration information, including the link to register, 1 month prior from the date of each meeting. Registration is required (no walk-ins, please) and will be managed on-line only.
NEW Monthly Meeting Location
PNC CHAMPIONS CLUB at ACRISURE STADIUM
Society News
POS Monthly Meeting Guest Faculty
Dr. Shields completed her ophthalmology training at Wills Eye in 1987 and subsequently did fellowship training in ocular oncology, oculoplastic surgery, and ophthalmic pathology.
She has authored or coauthored 12 textbooks, over 1400 articles in major journals, over 300 textbook chapters, given over 700 lectureships, and many awards. The 5 most prestigious honors include:
The monthly meeting series begins September 14th with guest speaker Hajirah Saeed, MD, Associate Visiting Professor University of Illinois College of Medicine Department of Ophthalmology, Chicago IL; Lecturer on Ophthalmology (part-time); Harvard Medical School, Boston, MA. Thank you to Srinivas Kondapalli, MD for inviting Dr. Saeed.
Dr. Saeed joined the Department of Ophthalmology and Visual Sciences in 2022 as a Visiting Associate Professor, with a specialty in Cornea and Refractive Surgery and a focus on the pediatric population. She is internationally recognized as an expert on Stevens Johnson syndrome (SJS) and has an NIH grant focusing on the genetics and epidemiology of SJS. In addition, she and her team of researchers are working on novel diagnostic methods for various corneal pathology through machine learning, corneal collagen crosslinking in pediatric patients, and sustainable eye banking in the developing world.

• The Donders Award (2003) given by the Netherlands Ophthalmological Society every 5 years to an ophthalmologist worldwide who has contributed to the field of ophthalmology. She was the first woman to receive this award.
• The American Academy of Ophthalmology Life Achievement Honor Award (2011) for contributions to the field of ophthalmology.
There is no meeting in November as the American Academy of Ophthalmology’s national meeting will take place November 3-6, 2023.
Dr. Kolomeyer is the author of numerous book chapters and 35+ peer-reviewed publications and serves on committees for the American Glaucoma Society, American Academy of Ophthalmology, Association for Research in Vision and Ophthalmology, and the Pennsylvania Academy of Ophthalmology. Thank you to Sharon Taylor, MD, FACS for extending the invitation to Dr. Kolomeyer to present to members.
The Society welcomes Carol L. Shields, MD Chief, Ocular Oncology Service, Wills Eye Hospital Professor of Ophthalmology, Thomas Jefferson University of Philadelphia as guest faculty for the October 5 meeting. Thank you to Pamela Rath, MD, for inviting Dr. Shields.

Closing out 2023, the December 14 meeting features Natasha Nayak Kolomeyer, MD, Board-certified ophthalmologist and Fellowship-trained Glaucoma Specialist—Wills Eye Hospital, Assistant Professor of Ophthalmology; Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA

Dr. Kolomeyer has been the recipient of numerous awards and grants throughout her career. These include the Achievement Award from the American Academy of Ophthalmology; the Mentoring for the Advancement of Physician Scientists grant as well as the Healthcare Policy Leadership Development grant from the American Glaucoma Society; the Resident Excellence Award and Resident Research grant from the American Society of Cataract and Refractive Surgery; and The Chairman’s Award for Academic Honors and Distinction from the New York Eye and Ear Infirmary.
To welcome in the new year, the January 11, 2024 meeting features Tarek Hassan, MD, Professor of Ophthalmology at Oakland University William Beaumont School of Medicine; Senior Partner and previous Director, Vitreoretinal Fellows Training Program at Associated Retinal Consultants; President, American Society of Retina Specialists (ASRS), Royal Oak, MI.
Dr. Hassan has an active clinical and academic practice. He is involved in a wide array of both basic science and clinical vitreoretinal research studies and has served as principal investigator or co-investigator in more than 100 national trials, notably in the areas of macular degeneration, diabetic retinopathy, retinal vein occlusion, and vitreoretinal surgery. He has authored and co-authored more than 160 papers in peer-reviewed journals and 8 books or book chapters for medical texts. He is a scientific reviewer for all the leading journals within ophthalmology and retina, and on the editorial board of several.

He has been a leader in the areas of retinal detachment repair, diabetic retinopathy, and macular degeneration, and has lectured extensively nationally and internationally for many years, giving more than 450 presentations
Continued on Page 28
Society News
From Page 27
on these topics. He was awarded the AAO Achievement Award in 2003, the ASRS Senior Honor Award in 2004, and the AAO Senior Achievement Award in 2013. He has also been named to the “Best Doctors in America” listing every year since 2000. He has been very committed to retina fellow education, and in the past twenty years, he has had the distinct honor to train 34 clinical vitreoretinal fellows and over 20 international research fellows. Thank you to Thierry Verstraeten, MD, for inviting Dr. Hassan to present.


An internationally renowned expert in orbital and ophthalmic plastic surgery, Dr. Kahana is a sought-after lecturer and a respected leader in our field. He is a Program Director for an ASOPRS-approved fellowship in oculofacial plastic surgery, and teaches ophthalmology residents from Beaumont, Ascension and Kresge/Wayne State University.
He has authored over 80 peer-reviewed publications, multiple book chapters and reviews, and has given >100 lectures throughout the United States and internationally, including several endowed lectures and visiting professorships. In 2020, Dr. Kahana was given the honor of delivering the annual Ralph E. Wesley ASOPRS Foundation Lecture. Dr. Kahana has served in numerous leadership positions, including as President of the North American Society of Academic Orbital Surgeons (NASAOS) and Chair of the Thesis Committee and the Scientific Advisory Committee for ASOPRS. He is also a Program Director for his own ASOPRS fellowship.
Wrapping up the 2023-2024 monthly meeting series, the February 8, 2024 speaker is Alon Kahana, MD, PhD with Kahana Oculoplastic & Orbital Surgery. Dr. Kahana is a Professor & Vice Chair of Ophthalmology; Oakland University William Beaumont School of Medicine; Rochester, MI. Thank you to David Buerger, MD, FACS and Cari Lyle, MD for inviting Dr. Kahana.
Contact Nadine Popovich, administrator, to confirm the status of your membership, registration, or to inquire about an upcoming program. She can be reached by email: npopovich@acms.org or by phone: 412.321.5030 x110.

The Great Renaissance: Generative AI’s Moment is Now, But Do New Solutions Really Deliver?
Giving and getting healthcare will always require conversations. How those conversations are documented and recalled by patients or clinicians is intriguing, because medical documentation hasn’t significantly changed much over the last 100 years. Until now.

Today, AI companies are very much in the business of disrupting the status quo of how clinicians document medical encounters. Big benefits are touted: lower clinician burnout, greater job satisfaction, and more time to spend with patients. But do they deliver on these promises? According to Hugh Sims, an individual Abridge user and ENT specialist, the answer is a responding yes: “I can’t tell you how much this program has changed my life! The lack of mental exertion to remember patients is at a 30 year low. I can concentrate on the patient. I can enjoy the charting. I’m a better listener with patients. Overall, my happiness has increased!”
Abridge is building a solution for providers by providers. Through his experience as a cardiologist, Abridge’s co-founder and CEO, Shiv Rao, saw opportunities to improve the gap between medical conversations and what happens next.


Shiv Rao, a Pittsburgh-based cardiologist, and CEO and co-founder of Abridge, a Pittsburgh-based company, was never driven by AI hype, but rather aimed to address the pervasive problem he saw in his own clinic: physician burnout. Every clinician understands the ways in which patient conversations can be overshadowed by the mountain of notes they have to take during, or after, the visit. Founded on Carnegie Mellon University roots, Abridge’s research and proprietary data set of 1.5 million medical encounters culminated in the firstpublished and first-to-market AI system for generating SOAP note drafts. Today, Abridge’s AI accurately summarizes conversations between doctors and patients, saving clinicians

over 2 hours per day on documentation and giving them the autonomy to focus more on the practice of medicine.

Because medical conversations are high-
Final Thoughts
We barely go a day without seeing new stories about clinician mental health woes or leaving the sector altogether as a result

MISSION

Founded in 1960, the Allegheny County Medical Society Foundation has extended the reach of physicians into the community through grant giving to local organizations.


The mission of the Foundation is: A Advancing Wellness by confronting Social Determinants and Health Disparities. This mission works to fulfill an overall vision of a healthy and safe Allegheny County.

Throughout the ups and downs of the past few years, the Foundation’s work has become even more important in supporting local non-profits.
The desire to give back to the community is an inherent trait of those who become physicians. Please consider how you can personally help support the Foundation and, in turn, continue to support a healthy region.
Contact the ACMS team to learn more about how your organization can help support the ACMS Foundation.
As physicians, you know that it takes a village to keep the community healthy and safe. Please consider a donation to the Allegheny County Medical Society Foundation.
Your donation will help the Foundation fund local non-profits in future grant cycles, and will help further the mission of the ACMS Foundation.

Donations can be mailed to: ACMS Foundation
850 Ridge Avenue Pittsburgh, PA 15212
Scan this QR Code to Donate via Qgiv:
2023 ACMS Foundation Grant Applications are OPEN:
Deadline: September 15, 2023
As the 501(c)3 philanthropic arm of the Allegheny County Medical Society, the foundation awards grants to support home and community environments that nurture and develop healthy children and families for a healthy Allegheny County.
The Foundation believes that all people have the inherent capacity to effect change in their lives and in their communities. The Foundation will support programs that respect and value individuals and their collaborative work to improve healthcare in our community.
T The following is a list of criteria that will be considered in the review process:
• Project will create an impact on communities in Allegheny County, PA.
• Project addresses a pressing need or timely issue OR presents a unique approach to addressing an “every day,” ongoing challenge.
• Project has potential for broader impact or replication
• Project will respond to the ACMS Foundation Mission: Advancing Wellness by confronting Social Determinants & Health Disparities.
Grant Application & Details:
www.acms.org/acms -foundation/acmsgrants
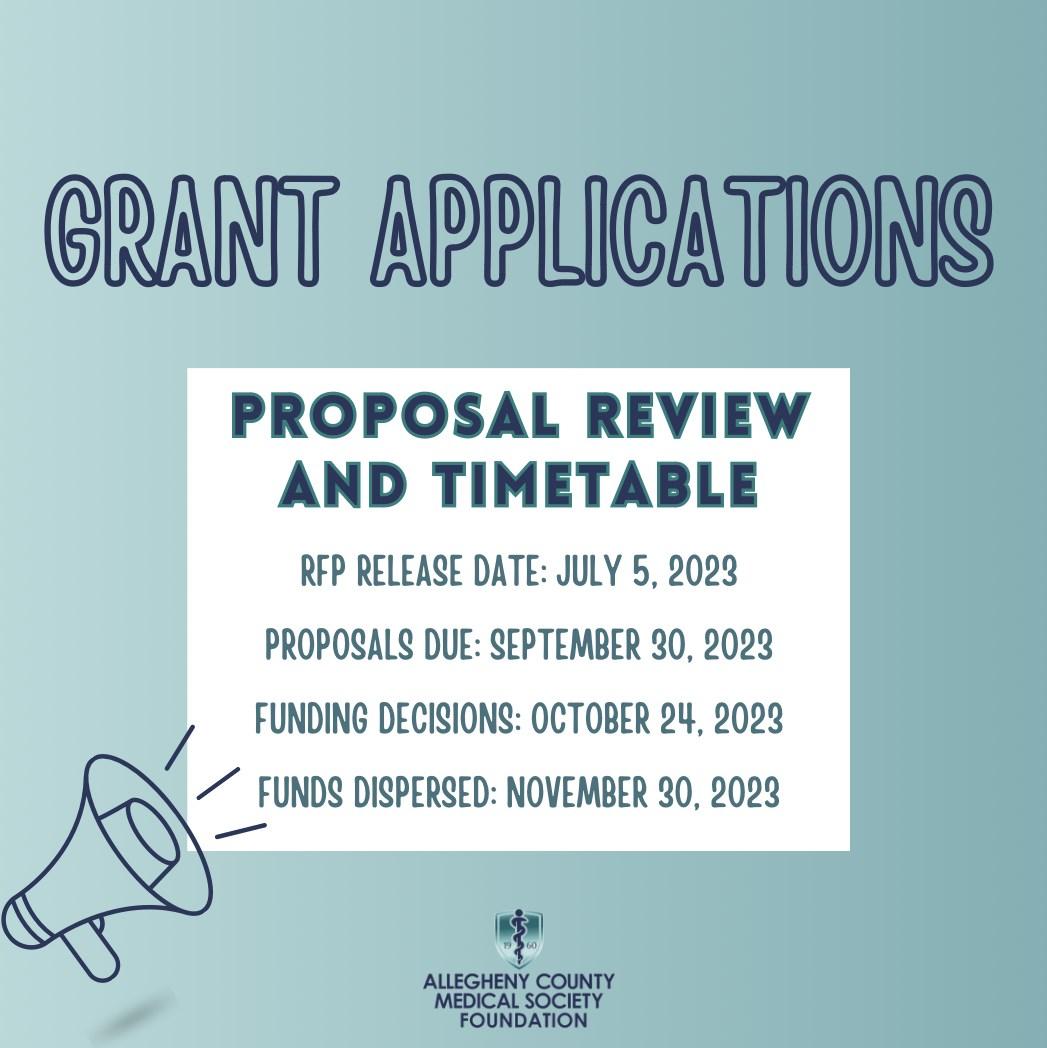
The Allegheny County Medical Society (ACMS), led by Matthew Straka, MD, President is pleased announce the following Co-Chairs for the newly created ACMS Women in Healthcare Committee.


In recognition of the continued growth in the number of female physicians – both in practice and in leadership roles – the Allegheny County Medical Society established the Women in Healthcare Committee. The objectives and goals are well-defined and includes a space dedicated to inspiring all ACMS members to: support, mentor, and empower women physicians; encourage their interest and active participation in organized medicine; foster mentorship and networking among women physicians; advance women physicians role in political and legislative advocacy and promote women physicians as leaders.
We are looking for Committee Members! Your responsibility is important, but your time involved is minimal! By coming together, supporting each other, and advocating for change, you can create a meaningful impact on the medical profession, gender equality, and the overall well-being of women physicians! Contact Nadine Popovich, Vice President, Member and Association Services at 412.321.5030 x110 or email to npopovich@ acms.org to become involved.

Anuradha Anand, MD, Physical Medicine & Rehabilitation Specialist, Advanced Pain and Rehab Specialists and Tiffany DuMont, DO, Pulmonary Critical Care Physician, Program Director, Pulmonary and Critical Care Fellowship, Allegheny Health Network, Medical Director of the Intensive Care Unit Allegheny General Hospital.
This is a wonderful platform to highlight the accomplishments of women, promote career success and development and help pave the way for future generations of women in medicine, says Tiffany Dumont, DO. Both Dr. Anand and Dr. Dumont are enthusiastic to work alongside committee members to identify meaningful programs and networking opportunities and to achieve the group’s goals.
Anuradha Anand, MD Tiffany DuMont, DO

The co-chairs invite you to attend the August 9 kick-off event at the Longue Vue Club. ACMS members and non-member are welcome to attend this social event.
The evening begins at 6:00 pm with open bar and appetizers on the patio, followed by an inspiring presentation by Margaret Larkins-Pettigrew, MD, MEd, MPPM, FACOG. Visit the ACMS website, click on the events tab and scroll to the August 9 Women in Healthcare Event to register.

Women in Healthcare Committee Kickoff Event


Come CeleBRate women in healthCaRe with us on national women’s Day!
august 9, 2023 | 6:00 Pm - 8:00 Pm
This summer, the ACMS is officially launching the Women in Healthcare Committee, co-chaired by Anuradha Anand, MD, and Tiffany Dumont, DO. To commemorate this exciting new addition to our lineup of member engagement opportunities, we invite all ACMS members and their non-member colleagues to attend a casual networking event on National Women’s Day, August 9th, 2023!

The ACMS Women in Healthcare Committee is pleased to welcome honored guest speaker Margaret Larkins-Pettigrew, MD, MEd, MPPM, FACOG. Dr. Larkins-Pettigrew is an international diversity, inclusion and equity expert, healthcare strategist and maternal/infant health care equity advocate. She is the Senior Vice President and Enterprise Chief Diversity, Equity, and Inclusion Officer for Allegheny Health Network/Highmark Health. As a practicing physician, she cares for women in her general OB/GYN practice, with a special interest in providing care for women living with HIV and those in under-resourced communities. Her passion for health equity and building programs that improve outcomes for women, people of color, vulnerable and marginalized communities has been a common thread throughout her highly respected career and commitment to service.



Join us at Longue Vue Club for a night of networking on the patio overlooking the city, while enjoying appetizers and a complimentary bar. In addition to our honored guest speaker, attendees will have the opportunity to connect with colleagues and learn more about the goals of the new Women in Healthcare Committee. You are not obligated to join, but your feedback on the programming and initiatives you wish to see from this group is greatly appreciated.


If you are interested in learning more about serving on this new committee, please contact Nadine Popovich (npopovich@acms.org). We look forward to welcoming members and non-members for an evening of camaraderie on August 9th.
HONORED GUEST
Margaret
Member Spotlight



Congratulations to John Williams, MD, as he accepts an award for his eight years of outstanding service on the AMA Council on Medical Education in his final year as Chair. John is a past President and Chair of the Allegheny County Medical Society and a past ACMS Foundation Trustee! Thank you, Dr. Williams, for your wisdom in advancing medical education!

Let’s welcome our newest ACMS staff member, our summer intern, Isabella Lin! A fun fact about Isabella is she plays both field hockey and judo. Our association is benefiting greatly from her enthusiasm, innovative ideas, and valuable contributions.”

Call for Nominations – 2024 Leadership Positions

BoaRD oF DiReCtoRs anD aCms house oF Delegates nominations aRe Due By august 15, 2023






The ACMS Nominating Committee is accepting nominations for six open positions on the 2024 Board of Directors, including (5) three-year term board seats, and (1) 1-year term board seat that has become vacant. The ACMS Election will take place during the first week of November and the new board members will be announced following certification at the December 5, 2023, Board of Directors meeting. The terms of the new Board members will begin on January 1, 2024.
Serving on the ACMS Board of Directors requires participation in four meetings per year (held quarterly), with in-person attendance preferred at all meetings. There may, from time to time, be special meetings of the Board of Directors should the need for a meeting arise. Board positions are open to all ACMS physician members.
The ACMS Delegation will also elect several members to serve as Delegates or Alternate Delegates for the PAMED House of Delegates. The 2024 dates for the House of Delegates are October 25-26, 2024. ACMS Delegates are elected for a term of two-years (and may not serve more than 3 consecutive terms). Alternate Delegates are elected for a oneyear term and there is no limit to consecutive terms for Alternate Delegates. Applicants for a Delegate or Alternate Delegate position should be considerate that the ability and willingness to attend the House of Delegates in-person will be considered during the vetting process. In-person attendance will be encouraged.
Joining the Allegheny County Medical Society board of directors and/or Delegation


can provide a multitude of benefits, including professional development, networking opportunities, the ability to influence and impact the medical profession, and personal fulfillment. It can be an excellent platform to contribute to the medical community and advance one’s career in healthcare. We hope you will consider nominating yourself or a colleague for these important roles.
To nominate yourself or a colleague please use the online submission portal by visiting https://www.acms.org/2023-acms-leadership/ nominations. If you have any questions, please reach out to ACMS Executive Director, Sara Hussey (shussey@acms.org) or Dr. Raymond Pontzer, ACMS Nominating Committee Chair.
ALLEGHENY COUNTY MEDICAL SOCIETY — 2023 MEETING SCHEDULE

ALL MEETINGS BEGIN AT 6:00 PM
Upcoming Events
No upcoming events Executive Committee*
Tuesday Evenings—2nd Tuesday at the start of each new quarter.
October 10, 2023
Finance Committee
Tuesday Evenings
August 29, 2023
November 14, 2023
Delegation April, June, August, October
Nominating May, August
ACMS Foundation
October 24 Grant Proposal Review
Board of Directors*
Tuesday Evenings
September 12, 2023
December 5, 2023
PAMED BOARD
May 4
August 3
PAMED HOUSE OF DELEGATES / HERSHEY
October 27-28, 2023
October 26-27, 2024
AMA HOUSE OF DELEGATES
November 11-14 National Harbor, MD AMA Annual Meeting June 2024 Chicago, IL
AMA Interim Meeting
July 4—Independence Day
ACMS HOLIDAYS – OFFICE CLOSED

