POLST Legislation Introduced in PA Senate: What’s in the Bill?
Burnout: The Milk of “Humankindness”


POLST Legislation Introduced in PA Senate: What’s in the Bill?
Burnout: The Milk of “Humankindness”

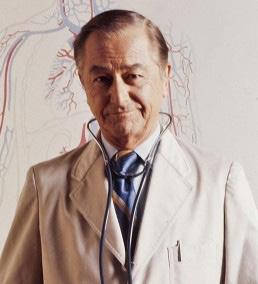
When your patients need the best possible specialty care, AHN has physicians like Dr. Lally and his team of cardiovascular experts as a part of our nationally recognized heart program.
Dr. Lally provides patients with customized treatments for optimal outcomes. He sees patients at North Fayette and Sewickley.
Francis Lally, MD, FACC
Cardiologist
Locations: North Fayette 200 Quinn Drive, Suite 210
Pittsburgh, PA 15275
Sewickley 301 Ohio River Boulevard Suite 301
Sewickley, PA 15143
Specialties : Coronary artery disease, structural heart disease, and cardiovascular disease prevention
To refer your patient, call (412) DOCTORS.
Most major insurance plans are accepted.
Editorial....................................5
• Garden of Eden
Deval (Reshma) Paranjpe, MD, MBA, FACS
Letter to the Editor ..................7
Associate Editorial ..................8
• Preventing HIGH Myopia in 2023
Joseph Paviglianiti, MD
Editorial ..................................12
• Med-Mal 101—A Primer Part V: Communication and Incidental Findings
Richard H. Daffner, MD, FACR
Perspective ............................16
• Burnout: The Milk of “Humankindness”
Anthony L Kovatch, MD
Perspective ............................20

• QUID EST VERITAS
Michael G. Lamb, MD
Reportable Diseases..............15
ACMS News ...........................31
• Top Physicians Under 40
ACMS News ...........................32
• Everyday Hero Award—Dr. Louis Heyl Jessica Merolillo
ACMS News ...........................33
• House of Delegates Update Foundation..............................34
• ACMS Honors Awards
ACMS News ...........................36
• POLST Legislation Introduced in PA Senate: What’s in the bill?
Lisa George, MPH, CHES
Materia Medica ......................25
• Vonoprazan (VOQUEZNA™)
Abigail Reigh, PharmD
Grace Kim, PharmD
Legal Summary......................28
• Data Trackers: A New Compliance
Concern Under HIPAA
William H. Maruca, Esq.
Gene Therapy .......................30
Jerry Vockley, MD, PhD
Cancer Coalition Letter.......38
ACMS Meeting Schedule ......40
2023
Executive Committee and Board of Directors
President
Matthew B. Straka, MD
President-elect
Raymond E. Pontzer, MD
Secretary
Keith T. Kanel, MD
Treasurer
William Coppula, MD
Board Chair
Peter G. Ellis, MD
Term Expires 2023
Michael M. Aziz, MD
Micah A. Jacobs, MD
Bruce A. MacLeod, MD
Amelia A. Paré, MD
Adele L. Towers, MD
Term Expires 2024
Douglas F. Clough, MD
Kirsten D. Lin, MD
Jan B. Madison, MD
Raymond J. Pan, MD
G. Alan Yeasted, MD
Term Expires 2025
Anuradha Anand, MD
Amber Elway, DO
Mark Goodman, MD
Elizabeth Ungerman, MD
Alexander Yu, MD
G. Alan Yeasted
Bylaws
Raymond E. Pontzer
Finance
William Coppula, MD
Nominating
Raymond E. Pontzer, MD
Medical Editor Deval (Reshma) Paranjpe (reshma_paranjpe@hotmail.com)
Associate Editors
Douglas F. Clough (dclough@acms.org)
Richard H. Daffner (rdaffner@acms.org)
Kristen M. Ehrenberger (kehrenberger@acms.org)
Anthony L. Kovatch (kovatcha42@gmail.com)
Joseph C. Paviglianiti (jcpmd@pedstrab.com)
Andrea G. Witlin (agwmfm@gmail.com)
ADMINISTRATIVE STAFF
Executive Director
Sara Hussey (shussey@acms.org)
Vice President - Member and Association Services
Nadine M. Popovich (npopovich@acms.org)
Manager - Member and Association Services
Eileen Taylor (etaylor@acms.org)
Co-Presidents
Patty Barnett Barbara Wible
Recording Secretary Justina Purpura
Administrative & Marketing Assistant Melanie Mayer (mmayer@acms.org)
Director of Publications Cindy Warren (cwarren@pamedsoc.org)
Part-Time Controller
Elizabeth Yurkovich (eyurkovich@acms.org)
Corresponding Secretary
Doris Delserone Treasurer
Sandra Da Costa
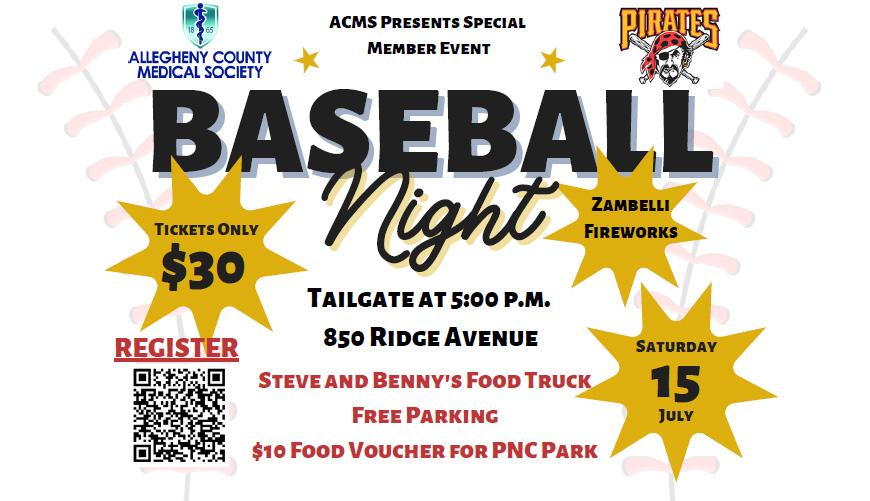
OFFICES: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212; (412) 321-5030; fax (412) 321-5323.
USPS #072920. PUBLISHER: Allegheny County Medical Society at above address.
The Bulletin of the Allegheny County Medical Society is presented as a report in accordance with ACMS Bylaws.
The Bulletin of the Allegheny County Medical Society welcomes contributions from readers, physicians, medical students, members of allied professions, spouses, etc. Items may be letters, informal clinical reports, editorials, or articles. Contributions are received with the understanding that they are not under simultaneous consideration by another publication. Issued the third Saturday of each month. Deadline for submission of copy is the SECOND Monday preceding publication date. Periodical postage paid at Pittsburgh, PA.
Bulletin of the Allegheny County Medical Society reserves the right to edit all reader contributions for brevity, clarity and length as well as to reject any subject material submitted. The opinions expressed in the Editorials and other opinion pieces are those of the writer and do not necessarily reflect the official policy of the Allegheny County Medical Society, the institution with which the author is affiliated, or the opinion of the Editorial Board. Advertisements do not imply sponsorship by or endorsement of the ACMS, except where noted.
Publisher reserves the right to exclude any advertisement which in its opinion does not conform to the standards of the publication. The acceptance of advertising in this publication in no way constitutes approval or endorsement of products or services by the Allegheny County Medical Society of any company or its products.
Annual subscriptions: $60
Advertising rates and information available by calling (412) 321-5030 or online at www.acms.org.
Assistant Treasurer
Liz Blume
COPYRIGHT 2023: ALLEGHENY COUNTY
MEDICAL SOCIETY
POSTMASTER—Send address changes to: Bulletin of the Allegheny County Medical Society, 850 Ridge Avenue, Pittsburgh, PA 15212.


Never put your plants outside before Mother’s Day, they warn. This year, I listened (as I’ve done ruefully every year since the year I disobeyed). On Mother’s Day, I moved the whole brood outdoors after this long winter—pink and yellow plumeria, Meyer lemons, red and coral hibiscus, star jasmines and button jasmines, neem tree, curry leaf plants, the fig, the banana…..only the orchids remain indoors, being the delicate creatures that they are.
Putting your hands in the earth, making space for a young plant in a freshly filled pot or a freshly made garden bed, gently teasing apart the root ball and setting the whole thing in the soil, packing it tenderly and watering it down, gently tying stem to stake with the twist-tie from last week’s loaf of bread…..is this not a form of parenthood?


I love watching the young plants grow strong and tall in the sunshine and rain, marvel at each blossom and bloom, and cheer on the fruit as it grows day by day. The Meyer lemon trees are budding and will soon explode into fragrant bloom. Hummingbirds will hover, sipping from the hibiscus and
grazing their velvet-tipped stamens. The peonies are springing back to life in balls of pink and white suddenly emerging on long stalks from their ancient beds, and the neighbor’s lilacs are flooding the air with extravagant perfume. The double cherry blossoms haven’t blossomed yet, but maybe they’re late bloomers this year.
This year, I’ve planted four types of peppers, oregano, mint, basil, tarragon, and a glorious giant heirloom tomato whose name I have forgotten but whose fruit is sure to grace a Caprese salad or two this summer if all goes well. I can’t forget the lavender, and pink hydrangeas, and three bright red geraniums to honor a dear friend who loved them.
Every gardener whether expert or dilettante knows the profound satisfaction of even the smallest harvest of flowers and fruit. Every gardener knows the joy of watching living things grow and thrive and be productive and beautiful. It is the primal thrill of new life, of new beginnings, of new hope. The miracle of new life never ceases to astonish, whether it is my dinnerplate dahlia growing new shoots from beside the old dead wooden plant from last year, or a birth announcement and picture of a beautiful infant after a long winter of death and disease.
Continued on Page 6
From Page 5
I was recently given the honor of writing a medical school recommendation letter for a bright and beautiful young woman who I’ve known since she was a year old. I’ve watched her grow from baby to toddler to little girl to a kind, confident, mature, caring, and capable adult. I’ve watched her loving parents raise her well and beam with quiet pride at her many accomplishments over the years. I’ve egged her on to apply to medical school for years and am incredibly happy that she is doing so because it is her dream, one she is working hard to achieve. I am also joyful and relieved because she is exactly the kind of human that I hope one day will take care of me as a physician when it is my turn to be a patient. (“We’re all pre-op; it’s just a matter of when” -- if I recall correctly from my General Surgery rotation). By
the way, she has nerves of steel and steady hands, and my personal sorting hat sends her to Surgery, although who knows where her heart will lead her in the Match.
I have another mentee I’ve adopted, a hyper-responsible, bright, and caring college student who is also determined to be a physician. Recently she texted me to share her excitement at shadowing neurosurgeons and attending a surgery simulation with residents—as well as the befuddlement of a premed student thrust into a busy surgery rotation with no idea about medical traditions or institutions. Every serious and urgent question she asked (do I wear scrubs or professional attire to Grand Rounds? People told me different things; I don’t want to mess up. Is the Grand Rounds an awards ceremony?) was adorable and achingly sweet because I suddenly remembered
being at that tender stage. Watching her become excited about our calling has been really life-affirming for me, as corny as it sounds.
Growing heirloom tomatoes is one thing; I’m convinced that watching a young person put down strong roots, grow up wisely and well, and turn into a kind, capable and caring physician is the ultimate joy another physician can have.
Find yourself a garden of young would-be physicians to nurture and grow, even if they are not your own children—perhaps especially if they are not your own children, because then they will look at you without filial bias and take you more seriously and let down their guard. (That’s the one joy of being the cool aunt). It is most rewarding to the soul and helps offset the stress of your own professional life. What greater joy is there than helping someone else bloom?

Sigmund Freud’s view of humor was that it was a conscious expression of thoughts that society usually suppressed or was forbidden.2 As long as the humor, in this case name-
offend someone. Finally, we should always remember that no matter how unpleasant some of our patients are to us, they are still our fellow human beings.
References
1. Shem S. The House of God. Richard Marek Publishers 1978.
2. Freud S, (Strachey J, Trans.). Jokes and their relation to the unconscious New York: W. W. Norton, 1960 (Original work published 1905).
• Physician Billing Services for All Specialties
We would use OUR billing system or YOUR billing system based on YOUR preference.
• Credentialing Services for All Specialties
• Accounts Receivable Follow-Up for Practice Support
We would work your accounts on your system to maximize cash flow.
NEW Billing Client Example: A new client (a 6-physician family medicine group) liked their EHR, so the group asked us to bill using their billing system. Besides the benefit of keeping their EHR, the group is now experiencing greater efficiency and stability in their office by eliminating problems caused by biller turnover, vacations, diversion, and other time off.
Contact Ruby Marcocelli, Vice President at 412-788-8007 or rmarcocelli@fennercorp.com
Three Penn Center West Pittsburgh, PA 15276 fennercorp.com
229 ACMS Bulletin / August 2021

Letter to the Editor
I was relieved to know that Dr. Paranjpe did not write “An Unexpected Perspective” in the April Bulletin, even though I don’t disagree with much of what was said in that particular article. But ChatGPT and similar A-I products are only in their infancy and, as Yogi Berra (or was it Niels Bohr?) said, “It’s hard to make predictions, especially about the future,” and I am sure we are in for a bumpy ride.
A major challenge will be how to recognize false information generated by A-I if A-I and/or its creators can’t tell if information that it relies on is false.
Bruce Wilder MD
412-636-3541
 josePh
josePh
If your kids or grandkids are nearsighted, you might want to read this…
Many physicians are mild to moderately nearsighted and it’s just something we deal with via glasses/ contacts/refractive surgery. What many physicians don’t realize is that HIGH myopia (defined as myopia “worse” than -5 diopters) is an important and common cause of blindness and/or low vision in the world. Even here in the USA, many physicians have had their careers ended because of a myopic retina detachment, particularly in surgical professions that require some stereovision/depth perception. We have several of them in our practice and adult eye practices have many more. Unfortunately, while the world has been consumed by the coronavirus pandemic, another pandemic has been quietly happening, exacerbated by technology, architecture, and the coronavirus pandemic itself: the pandemic of acutely worsening pathologic HIGH myopia globally. It’s a real issue and one that is acutely worsening. The time to tackle it is now.
Some brief housekeeping: Think of the diopter measurements of eyeballs like shoe sizes for feet. A person wearing a size 9 shoe has a shorter
foot than someone with a size 12 shoe. Shoe manufacturers also used to put the width of shoes (A,B,C,D,E from narrow to wide) on shoeboxes, but they don’t anymore. Similarly, eyes have an axial length (from front to back) and a width (from top to bottom). So, feet have a length and a width, and so do eyeballs. Forgive the simplistic analogy. If your eye measures too short from front to back, you are called “farsighted” and your diopter measurements are in the “plus” range: +1,+2 +3, etc. If your eye grew too long, you are called “nearsighted” and your diopter measurements are in the “minus” range: -1,-2,-3-4, etc. If your eyes are perfectly sized from front to back, you have a “zero” or “plano” eyeball and usually, no glasses needed. Pour yourself some wine and celebrate! My most myopic patient has a -27.00 refraction (that’s a really long eyeball from front to back!) and wears -20.00 contacts (highest available) with -7.00 glasses overtop). Just to finish the shoe analogy… if farsightedness/nearsightedness represent the “length” of your eyeball, astigmatism can be viewed as the “width” of your eyeball. Yes, that’s oversimplified, but the analogy works for our discussion and helps our young patients grasp the idea of some very confusing terminology.
In the past, most “American” nearsightedness tended to start in the 4th grade, and progress through the teenage years (as their eyes grow), and then level off in late high school/ early college. In the USA, we were blessed with a relatively low average “rate” of myopia, and American myopia was of a low average “amount” (-2.75 diopters was the most common contact lens (CTL) power when I was in training 25 years ago). Myopia of that amount tends to be more of an annoyance, but doesn’t usually progress to cause vision threatening issues. HIGH myopia, though, which is caused when the eye grows a lot longer in childhood than it’s supposed to, can lead to serious eye issues later on in adulthood.
Adult myopia/nearsightedness is mostly caused by the axial lengthening of the eye that occurred during childhood. As the eye elongates, spectacle lenses are needed to focus the light “further back” onto the retina of the now elongating eye. If your eye grows by 0.4mm (that’s not very much!), it makes you approximately -1.00 diopter more nearsighted. Another study found that if your eye grew by 1mm, it made your refraction -2.50 diopters more myopic. Contrary to the popular belief
that the eye does not grow after birth (we hear this multiple times daily in our office), the eye actually does grow quite a bit after birth. Newborns have an eye axial length (distance from front of eye to back of eye) of approximately 16-18mm, which reaches approximately 23.5-24mm by adulthood for emmetropic (no refractive error) eyes. Highly myopic eyes can measure 26mm or longer, though there are a wide range of adult axial lengths depending on the study one reads. But in general, the longer your eye grows, the more nearsighted you are. Furthermore, and more importantly, the longer your eye grows, the more stretched everything inside the globe (i.e. your retina) is. The more stretched your retina is, the greater the lifetime risk of retina issues, most of them quite serious. A longer stretched retina, over time, predisposes one to myopic macular changes, which can result in breaks in the retina and subsequent choroidal neovascularization, treated by the dreaded “shots into the eyeball” (anti-VEGF meds such as Avastin, Lucentis, or Eylea…and yes, you are awake for that and no, it’s not pleasant). Furthermore, a stretched retina can tear or rip; these are myopic retina detachments and need an immediate retina procedure or surgery to reattach the retina, or you are permanently blind in that eye. Ouch.
Given the choice, most of us would prefer to own an eyeball with an axial length of approximately 23.5 mm. No glasses. Low risk for retina issues. Life is good. If your eye grows by 2 mm longer during childhood, that likely makes you a -5.00 high myope (high myopia is loosely defined as anything worse than -5.00). Two stinking
millimeters in the comparative length of an eyeball is the difference between “no glasses” and “coke bottles” (sorry for the vernacular). While there are certainly more factors that play into developing myopia, axial lengthening of the eye during childhood is the MAIN cause of high myopia and the subsequent pathology that can derive from it in adulthood.
The rate of “myopia” (includes mild to severe) among all Americans across all ages was 25% in 1971. Now it is 41.6% according to National Eye Institute (NEI) statistics. Let’s face it, your kids and grandkids are becoming more myopic than previously before. Many factors may be at play here. Changes in educational methods (8 hours on an IPAD in school, followed by 4 hours of homework on

a Chromebook at night), with spare time almost 100% spent on iPhones, tablets, or computers are a big generational change. Also driving this increased myopia prevalence is that our kids spend less time outdoors than former generations. Sunlight causes the retina to release dopamine, which reduces axial elongation of the eye. Plus, being outside allows the eyes to “relax and defocus” on the horizon, which is impossible in a small cramped windowless classroom. American architectural choices in school construction in the late 1960s through the 1980’s didn’t help. Look at Peabody/Obama High School in East Liberty. When they remodeled it in the 70’s, scores of windows were bricked up.

In the 1970s, the energy embargoes and “avoiding all outside distractions for students” were the drivers for these schools being built/ remodeled bereft of windows. My middle school in Lancaster was built in the energy/oil embargo years of the 70s as well: air conditioned, with very few windows. We didn’t care back then; we were just so happy to be in a brand-spanking-new air-conditioned building; we were more entranced by the little blue light domes in the hallways which meant the A/C was on. Windows? Who needed them? Contrast this to new schools being built in Asia: very few walls, lots of windows and walls of glass that let the eye “defocus” on the horizon.
Eastern Asia is the hotbed of myopia and always has been. If we think back to how Asians were unfortunately portrayed in 1970s TV shows (and even Asian cartoon characters of the time), they were always stereotypically portrayed with small thickish glasses. Indeed, in Taiwan, 36.4% of 8-year-old school children are myopic. Similarly, the rate of myopia in 8-year-olds is 34.7% in Singapore and 30.8% in Shanghai. In California, only 14.8% of 8-year-olds are myopic (and that is in a state that has a disproportionately higher amount of Asian-Americans than the rest of America). If we look at 15-year-olds, 78.4% of 15-year-olds in Guangzhou, China are myopic, 56% in California (again, perhaps demographically skewed versus the rest of America), 29.4% in England, 17.4% in Northern Ireland, 18.9% in Australia, and only 3.4% in Ghana. Africa by far has the lowest per capita rate of myopia
in the world.
More importantly, though, is the RATE at which myopia and HIGH myopia is increasing lately. In Taiwan, 8-year-olds had a 5.8% rate of myopia in 1983, 21% by the year 2000, and the aforementioned 36.4% in early 2020. Note that this was BEFORE the coronavirus pandemic, which has only sped the rate of myopia up further…more school computers, more iPhones, less outdoor time. Studies of myopia in 8-year-olds in Shanghai and Guangzhou, China mimic this trend. Not only are the rates of standard myopia (less than -5.00 diopters) increasing, but the rates of HIGH myopia (worse than -5.00 diopters) are increasing in huge numbers. Currently, there are 277 million HIGH myopes in the world. By 2050, that number is projected to be 938 million, representing 10% of the projected 2050 world population. Myopia, and more importantly, HIGH myopia, is increasing worldwide, and precipitously in East Asia, but very quickly here in the USA as well. More glasses now. Many more retina detachments later. It is a big problem on the horizon.
Back to our shoe analogy: Shaquille O’Neal’s size 22 feet served him well in childhood/young adulthood. No one would debate that. But he is 51 years old now, and it’s not far-fetched to predict that he may be more predisposed to problems with the 28 bones in his foot (I had to look that up) and foot arch issues than a person with a more “standard” sized foot. His foot size was NOT a problem in childhood for him (except in shoe procurement…how did his mom find him shoes before the era of the internet?), but likely may be a problem as he gets older. Same, too,
for eyeballs: Childhood high myopia isn’t a problem for kids; there are glasses and contacts to make them see 20/20. It’s what happens 30 years later when they reach later adulthood and the eye has been “stretched” for 40 years: retina macula issues, retina detachments, esotropia of myopia, etc., and these can be devastating to their careers and their lives.
Fortunately, there is much ongoing research into the “prevention,” or at least “slowing down” of myopia over the last 10 years or so, especially over the last few years. Not surprisingly, most of the studies are being done in Asia, where high myopia and the blindness secondary to it are major concerns. The basic premise is that if we can keep children’s eyes from growing too long, they will have fewer retina/blindness issues as older adults. Unfortunately, this article suffered from axial lengthening (over-wordiness of the author) so we will have to wait until next month to find out how to prevent (or at least slow down) eyes from growing too long. Stay tuned!

Sources:
He, M, et al. Refractive Error and Visual Impairment in Urban Children in Southern China. Invest Ophth Vis Sci. 2004: 45(3)793-9.
Hsu, CC, et al. Prevalence and Risk Factors for Myopia in Second Grade Primary School Children in Taipei: a Population-Based Study. J Chin Med Assoc. 2016: 79(11): 625-32.

Matsumura, S, et al. Global Epidemiology of Myopia. 2020. In Ang, M and Wong, T (editors): Updates on Myopia. Springer.
Theophanous, C, et al. Myopia Prevalence and Risk Factors in Children. Clin Ophthal. 2018: (12):15811587.
Sun J, et al. High Prevalence of Myopia and High Myopia in 5060 Chinese University Students in Shanghai. Invest. Ophth Vis Sci. 2012: 53(12):7504-9.
World Society of Paediatric Ophthalmology and Strabismus: Myopia consensus Statement 2023.

For information contact John Fenner
Email: fenner@fennercorp.com
Fenner Consulting
Three Penn Center West Pittsburgh, PA 15276 412-788-8007
fennercorp.com
Specializing in Hospital and Physician
Consulting and Billing Since 1991

“If you perform enough studies, you will eventually find something you cannot explain.
“If you perform enough studies, you will eventually find something you will wish you had not found.”1
In 2019, I published four editorials on medical malpractice, describing some of my experiences as an expert witness in diagnostic radiology over the course of 35 years 2-5. In this editorial, I’d like to comment on two common issues that may result in medical malpractice suits: communication issues and the challenges posed by the discovery of incidental findings. These two areas become prime targets for such suits when one considers that since the 1980s, virtually every patient has undergone some sort of imaging or laboratory study as part of their medical or surgical workup. (In the 1940s the ratio was one patient in twelve). With the incidence of medical malpractice rising in the 1980s, the American College of Radiology (ACR) introduced their ACR Practice Parameter for Communication of Diagnostic Imaging Findings in 19916. Since then, this, the most controversial of the Practice Parameters has been revised no fewer than seven times.
This Practice Parameter touches on five areas: The components of a final
imaging report; preliminary reports; non-routine communications; informal communications, and self-referred patients.
The final imaging report is a definitive and legal document. It should be transmitted in a timely manner to the ordering physician. In turn, the ordering physician shares responsibility to obtain the report, to read it, and to follow any recommendations made in it. In addition, in Pennsylvania, Act 112-2018, the Patient Result Information Act mandates that whenever a significant abnormality is found on a diagnostic imaging exam, the individual providing that service shall directly notify the patient or the patient’s designee. The Act suggests the following “preamble” to the notification: “You are receiving this notice as a result of a determination by your diagnostic imaging service that further discussions of your test results are warranted and would be beneficial to you.”
The following case is illustrative. A 32-year-old man was thrown from his trail bike and struck his right foot on a boulder. He was seen in the Emergency Room of his local hospital where he complained of foot and ankle pain. Ankle x-rays (only)
were obtained and were interpreted by the emergency physician and the radiologist as normal. He was sent home with an elastic wrap, told to take acetaminophen and ibuprofen for pain, and was advised to follow up with his primary care physician (PCP). Two weeks later, the patient saw his PCP, complaining of increasing pain and swelling in his foot. The PCP sent him for new x-rays of his ankle and foot, which were obtained in an imaging center in the same building as the PCP’s office was in. The requisition gave the indications for the study as “Pain and swelling”. There was no mention of a previous traumatic event. The radiologist reported the foot x-rays as showing dislocation at the talonavicular joint, multiple fractures of the tarsal navicular bone, and disruption of the calcaneo-cuboid joint. The findings were typical of a Charcot (neuropathic) joint. The radiologist asked if the patient was diabetic. The radiologist had his receptionist hand carry the final report to the PCP’s office in the same building. The PCP never contacted the radiologist to discuss the findings. Two weeks later, with still no improvement, the PCP referred the patient to an orthopedic surgeon who made a diagnosis of fractures and dislocations of the hindfoot and performed a fusion.
The patient sued the hospital, the emergency physician, both radiologists, and the PCP. All, except the second radiologist, settled. At that radiologist’s trial, I pointed out to the jury that the defendant radiologist had not violated the Standard of Care. Even though his diagnosis was erroneous, he did not call the study normal. His report had many alarm bells attached that should have prompted the PCP to call and inform him (the radiologist) that there had been trauma to the foot. In this case, it had been the PCP who was in error for failure to communicate (and probably for never reading the x-ray report). The jury returned a verdict for the defense.
Preliminary reports may be written, sent electronically, or given verbally. Whenever a preliminary report is generated, there should be documentation in the final report as to whom it was sent as well as the date and time of the transmission. (“Findings reported to Dr. X by telephone at 2:30 PM on January 18, 2023”, e.g.)
The following case is illustrative. A 52-year-old man had a chest x-ray prior to undergoing surgery for a herniated lumbar disc. The x-ray showed a 3 cm chest mass in the left upper lobe. The interpreting radiologist identified the mass and reported it not only in his final report, but also on a hand-written form that was sent immediately to the surgeon’s office. The final radiology report noted that a preliminary report was also sent. Two years after successful disc surgery, the patient complained of left-sided chest pain. A subsequent chest x-ray showed the mass was now double
in size from before and was eroding the adjacent two ribs. There were multiple metastatic lung nodules. A malpractice suit was filed against the neurosurgeon, the hospital, and the radiologist after the patient died. The neurosurgeon later admitted that he had not read either report, saying in his deposition, “I’m a spine doctor, not a chest doctor.” The radiologist and the hospital were dismissed as defendants; the neurosurgeon settled the case for $600,000.
Non-routine communications are those necessitated by findings that suggest a need for immediate or urgent intervention. In an emergency, radiologists should make every effort to directly communicate the findings to the ordering physician. The ordering physician also has an obligation to obtain the results of any test(s) ordered. Leaving a message with a nurse, an aide, or an answering service does not guarantee the report will be delivered. When all else fails, the patient should be contacted directly. There were many times when I diagnosed a subtle fracture that I called the attending physician in our Emergency Department to make sure (s)he saw it. Furthermore, there were also several times when I saw significant findings on a study ordered on an outpatient and was unable to directly contact the ordering physician. In those instances, I called the patient, identified myself as the radiologist who had read their study, explained the findings to them, and recommended they go to the nearest emergency room for treatment. (If they wanted to come to Allegheny General, I would
notify the ED to expect the patient.) All such communications should be documented in the final report.
The following case is illustrative. A 65-year-old woman saw her PCP on a Friday afternoon because of fever and productive cough. The PCP ordered a chest x-ray that showed extensive bilateral pneumonia. The radiologist who interpreted the study called the PCP’s office only to be informed by the answering service that he had left for the weekend. The radiologist left a message for a call-back when the PCP had been reached. The PCP never called the radiologist, who subsequently forgot about the case. The patient was found dead at home Monday morning. The postmortem exam showed diffuse pneumonia that had worsened since the x-ray was taken. The family sued the PCP and the radiologist. In his deposition, the radiologist stated that he had documented his attempts to contact the PCP. However, because he was unable to communicate with the PCP, he had an obligation to give his report directly to the patient (and recommend she seek immediate medical care). The family was awarded $600,000 from the PCP and the radiologist.
Informal communications are those that occur outside of the normal reporting mechanism. Such “curbside consultations” often occur in a hallway, or a physician’s lounge. In many instances, one member of our hospital staff would show me images taken either in another institution or, in the case of orthopedics, in their offices. All such informal consultations should be
Continued on Page 14
From Page 13
documented, listing the patient’s name, date, and time of the consultation as well as the “interpretation” given. This is self-preservation.
Many patients, particularly health professionals, refer themselves for imaging studies, such as mammograms. In these instances, the results should be given directly to the patient, stating not only the findings, but also any recommendations. Furthermore, these communications should be documented in the final report, and the patient should be told to communicate with their PCP or another specialist, if for no other reason than to notify him/her that such a study had been performed.
for acute abdominal pain. The scan showed appendicitis. However, on the uppermost image, a 3 cm mass was present in the left lower lobe. This was duly reported, and, after an appendectomy, a biopsy of the lung lesion showed a small cell carcinoma.
Modern imaging (CT, MRI) is very sensitive to finding incidental abnormalities. Some, such as calcified granulomas are considered classic “Leave me alone” lesions, to be followed periodically. Others show typical findings of a malignancy, such as a spiculated border. And then there are those lesions that are indeterminate and need further evaluation, usually including a biopsy. Table 1 shows the recommendations for dealing with incidental findings. The key things when encountering any incidental finding are that the report should mention the finding, should speculate about the possible nature of the finding, and, most importantly, should contain recommendations for additional studies, including biopsy. It is incumbent on the ordering physician to consult the radiologist to inquire about the next step(s) for dealing with such “incidentalomas”.
Communication is a vital part of medical practice. All communications —formal or informal should be duly recorded and documented to not only protect the physicians involved, but more importantly, to protect our patients.
1. Daffner RH. Diagnostic Pearls 18 and 19, in Clinical Radiology: The Essentials 3rd ed. Philadelphia, Walters Kluwer, 2007, p 527.
2. Daffner RH. Medical Malpractice
101: A primer. ACMS Bulletin Jun 2019, pp 164 – 167.
3. Daffner RH. Medical Malpractice
101: A primer Part II: The road to the courtroom. ACMS Bulletin Jul 2019, pp 204 – 207.
4. Daffner RH. Medical Malpractice
101: A primer: Part III: Elements of a malpractice suit. ACMS Bulletin Aug 2019, pp 242 – 245.
Finding Recommendation(s)
Definitely benign Follow-up 6 months to 2 years
Definitely malignant (I think) Biopsy for confirmation
Finally, with so many imaging and lab studies being performed, what does one do when an abnormality is found incidental to the original indication for the study. A good example was in the case of a colleague of mine who underwent an abdominal CT scan The
5. Daffner RH. Medical Malpractice
101: A primer: Part IV: The expert witness. ACMS Bulletin Sep 2019, pp 286 – 290.
6. American College of Radiology. ACR Practice Parameter for Communication of Diagnostic Imaging Findings. Reston, VA, 2020.
Dr. Daffner is a retired radiologist, who practiced at Allegheny General Hospital for over 30 years. He is Emeritus Clinical Professor of Radiology at Temple University School of Medicine
Indeterminate Biopsy for diagnosis
* Case classifications reflect definitions utilized by CDC Morbidity and Mortality Weekly Report.
** These counts do not reflect official case counts, as current year numbers are not yet finalized. Inaccuracies in working case counts may be due to reporting/investigation lag.
NOTE: Disease reports may be filed electronically via PA-NEDSS. To register for PA-NEDSS, go to https://www.nedss.state.pa.us/NEDSS
To report outbreaks or diseases reportable within 24 hours, please call the Health Department’s 24-hour telephone line at 412-687-2243. For more complete surveillance information, see ACHD’s 10-year summary of reportable diseases: https://www.alleghenycounty.us/Health-Department/Resources/Data-and-Reporting/Infectious-Disease-Epidemiology/Epidemiology-Re-

‘Yet do I fear thy nature; it is too full o’ the milk of human kindness to catch the nearest way.’
—Addressed by Lady Macbeth to her husband in William Shakespeare’s play “Macbeth” (1606), criticizing his attribute of kindness, which would prevent the ruthlessness necessary to seize the throne. Or is it actually her husband’s “humankindness” that is paralyzing his ambition? Only Shakespeare knows for sure!
You never give me your money
You only give me your funny paper
And in the middle of negotiations
You break down
I never give you my number
I only give you my situation
And in the middle of investigation
I break down ……
Boy, you’re gonna carry that weight
Carry that weight a long time!
As he exited the confessional that Saturday afternoon feeling the profound relief of self-disclosure to his God and to the world, the young doctor suddenly became enlightened that it would take many years to perform the necessary
penance for lasting self-forgiveness. This was only accomplished in full when he revealed his story to this writer and granted him permission to be his narrator. I reconstruct the young doctor’s dilemma as he related it to me in the first person:
I was down and out and tormented by profound anxiety about the future, repeating to myself the malediction: “You have destroyed your life, you have destroyed your wife, you have destroyed your family!” In reality, all six members of my nuclear family were in excellent health, we had paid off our home mortgage, and I was professionally “at the top of my game.” Unfortunately, the medical network that I had worked for at 110% capacity for the 12 previous years was financially moribund and grooming itself for a buyout by laying off the “less profitable” physicians, who in those dire circumstances were the “lucky ones.”
I was thanklessly forced to expand my duties, increasing my time pressure and guilt about stealing time and effort from my young family. After one highly stressful workday and the stark realization that the pressure of being a “good soldier” was damaging my physical and mental well-being, I just ”snapped,” abruptly wrote a letter of resignation I would painfully regret for years to come, and released my professional aspirations into the winds of a tornado of uncertainty. I realize now, a quarter of a century later, that I had been brainwashed by a power
that was not yet fully defined: BURNOUT.
Fortunately, I landed a new job with a large, distinguished private practice, knowing that it carried a reputation for rapid turnover of its providers and a grueling work schedule---sometimes into the late hours of the evening. When I realized that I had with full awareness, and despite this awareness, jumped from the proverbial “frying pan into the fire,” I allowed my every waking moment to be hijacked by an even more severe anticipatory anxiety of irrational self-destruction.
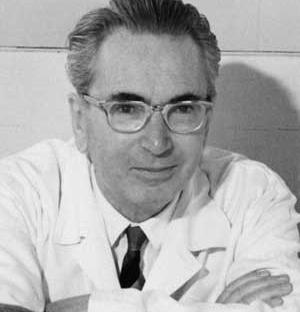
Ironically and even more to my detriment, I had successfully included during my years of tough-minded medical training the art of concealing my suffering---in fact, I brandished any suffering internally as the means to an end. I was a disciple of Holocaust survivor and Austrian existentialist and psychotherapist, the founder of Logotherapy, Viktor Frankl ---was I not? After all, had not commitment to his basic premise---“Those who have a ‘why’ to live, can bear with almost any ‘how’--sustained me through the rigors of premed and medical school and residency without a breach of my ambition? Was I not a survivor of prolonged late childhood Post-Traumatic Stress Disorder due to parental terminal illness? I symbolically wore an inscription of Frankl’s basic tenet over my heart like a tattoo: “In some ways suffering ceases to be suffering at the moment it finds a meaning, such as
the meaning of a sacrifice.”
However, my past robust philosophies could not prevent the spiraling anticipatory anxiety from propelling me into a previously unexperienced emotion---intractable depression. Intense cognitive behavioral therapy, meditation, prayer, and selfhelp measures (including reading the iconic best-seller “I’m OK---You’re OK” by psychiatrist Thomas Anthony Harris) produced no freedom from the fetters I had forged for myself, until…
It was the evening I first learned to “drink the milk of humankindness.” “What does your wife think about all this?” asked the therapist, an older woman who I had been referred to because the psychiatrist claimed she was “excellent;” I must admit that I had a skepticism colored by hopelessness.
“She has been very supportive,” I glumly responded. “But I am afraid she will no longer love me because I am so weak.” (I had reached rock bottom.)
“You mean because you are HUMAN?” she shot back at me.
She needed to say no more; in the long pause that followed while I cried tears for the first time since my childhood, all the irrationality, self-destructive ego with its Superman complex, and selfloathing had been suddenly and rightfully exterminated. I realized that I was little more than a victim of the human condition like all the rest of us and not exempt from its unwelcome vicissitudes. One word would break the horrible, self-imposed spell and spearhead the restoration. It was not a gesture of human kindness from an all-understanding professional but the decision to remind a physician that he is little more than a card-carrying member of humankind--and should be grateful for that simple privilege. I think that one word sustained me throughout the next 30 years of practice.
The story having been disclosed, we jump back to the present. I will never forget the lessons I learned after digesting the young doctor’s revelations. As a retiree and a narrator who has spent a lifetime performing penance for sins for which I may or may not have been guilty, I likely have a jaded perspective on the 60+ percent of physicians, veterinarians (1), dentists, and those of all other walks of life who are currently victims of burnout. I believe that any life change can precipitate burnout, including and especially, retirement. Who isn’t busy being created, is busy burning out. We must recreate ourselves every day by acknowledging our simple humanity. It is this “change of heart” that must be first and foremost in combating this modernday demon. We are the only ones who are capable of changing our own DNA!
Accomplishing the necessary change of heart will involve rooting out and providing lifelong freedom from the many different “complexes” that hold the mind hostage. Here are a few of these that I have foolishly and steadfastly embraced over my own lifetime:
Toxic-masculinity or Supermom complex
—Toxic Imposter complex
—Toxic Everybody’s Everything complex
—Toxic Wounded Veteran complex
Toxic Martyrdom or Silent Sufferer complex
—Toxic Fear of Failure complex and last but not least, for the medical profession---the Toxic Marcus Welby complex (Doctor Marcus Welby was the fictional television character who was the ultimately wise but humble, avuncular general practitioner who could do not do wrong and made more exotic diagnoses than the irascible, but more true-to-life, Doctor Gregory House).
Continued on Page 18
From Page 17
I think that many of us carry an entire “garbage bag” of these deleterious complexes throughout our careers; in retrospect, I think they were the principal component of the “Old Black Bag” I considered my sidekick for the forty-plus years I carried it around in practice. The beloved companion was more like an albatross, hermetically concealed from my inside and outside world. From out of these personal garbage bags, the fallacious scare-tactics of our psyches emanate: You know you’re strong and brave enough, but your brain wants to tell you that you’re NOT!
These distortions in self-perception, especially the toxic martyrdom/silent sufferer complex, did not dissipate with the final episode of “Marcus Welby, MD:
“The irony of my profession is that while learning deep truths about the bodies of strangers, I have ignored my own” acknowledges writer and young ENT surgeon Dr Allessandra Colainni in her self-reflective essay “Insensible Loss.”(2) “I have stood for hours in the operating room, forcing hunger to extinguish itself, willing my hands to stop aching while holding a dissector or a retractor. I have choked down food when I was not hungry, not knowing whether I would have time to eat again on shift. To avoid scrubbing out to urinate, I have kept myself dehydrated before surgeries that I knew would run long. I have worked through migraines, through pneumonia, and after fainting in a patient’s room during a procedure. I have forgotten to take my birth control about a hundred times. I have laughed when I was sad and frowned when I was happy. I have learned that the adrenaline generated from a beeping pager can transform me
from a wilting mess in a call-room bunk to a calm professional wielding a scalpel, so what does it really mean to be tired?”
She concludes with the insight that many of us physicians who suffer these same privations lack:
“Perhaps extremism is my pathology and surgery its latest incarnation.”

I think it is commonplace to fall prey to these fallacies, and even more so, to substitute “compassion fatigue” for frank burnout. The art of medicine with its emphasis on empathy and advocacy can drain the humanistic resources of an individual more completely than it can drain the will to power. We must never relent on the practices of self -help. Could anybody warn us better than the venerable Sir William Osler, MD?
“Mercy and consideration for the other man, but none for yourself, upon whom you have to keep an incessant watch.”
realized that satisfactory provider functioning is only possible under the umbrella of “psychological safety.”(3) Widely-recognized expert Dr. Amy C. Edmondson defines psychological safety as a “climate of trust and respect in which people are comfortable expressing and being themselves, and share the belief that teammates will not embarrass, reject, or punish a colleague for speaking up.” Medical administrators are taking the lead from the experience and knowledge of other industries.
At least anecdotally, the shortages in manpower wrought by the COVID pandemic appear to be easing up in some areas. The demand to master too many new skills, especially technical skills, at the same time (which sometimes is tantamount to a career change) has reached the point of equilibrium. “Going the extra mile” with toxic regularity has been deemed an occupational hazard. The medical profession has acquired the courage and willingness to implement the changes requisite for us to provide the level of personal care demanded by its clients---the patients; it is finally embracing the profound wisdom of the Serenity Prayer recited at every Alcoholics Anonymous meeting:
“God, grant me the serenity to accept the things I cannot change, The courage to change the things I can, And the wisdom to know the difference.”
I believe that the new wave of administrators has finally concluded that, while the self-esteem of employees is boosted by hard work and collaboration, it can be destroyed by lack of a voice. The medical team has finally
It is time for all member of the medical profession—armed with a sense of humor--- to accept the fact that, as the external obstacles in their working environment are in the process of being corrected, they must prevail in the more challenging and critical area: resetting the expectations of the heart and soul. In this way, restoration of the individual and healing of a wounded (but not yet
crippled) profession can be expedited. As in the story by American author Ernest Hemingway “The Big Two-Hearted River” about a young man psychologically devastated by war, we know why the grasshoppers have turned black; we must know for the sake of our society, how long it will take for this blackness to go away!
“As he smoked his legs stretched out in front of him, he noticed a grasshopper walk along the ground and up onto his woolen sock. The grasshopper was black. They were all black. They were not the big grasshoppers with yellow and black or red and black wings…These were just ordinary hoppers, but all a sooty black in color.
Now, as he watched the black hopper that was nibbling at the wool of his sock with its fourway lip he realized that they had all turned black from living in the burned over land. He realized that the fire must have come the year before, but the grasshoppers were all black now. He wondered how long they would stay that way.”
How much longer will we the medical profession have to “carry that weight”?
As my old spiritual advisor Viktor Frankl forwarned us:
“When we are no longer able to change a situation, we are challenged to change ourselves.”
1. Kovatch, MD, Anthony L: Burnout: Save the Beasts and the Children. // www.thepediablog.com/2022/05/19/ out-of-the-old-black-bag-21/


2. Colainni, MD, Allessandra: Insensible Loss. Gurnica, November 29, 2022
3. Hanrahan, MD, MPH, Rosemary: Psychological Safety in Healthcare. Allegheny County Medical Society Bulletin, November, 2022, pages 8-11

On a recent Oprah Winfrey show, Oprah encouraged her guests to tell “their truth” and that she in turn needed to speak “her truth”. The suggestion here is that there are many truths that are valid. In contrast, a witness in a courtroom swears an oath to tell “the truth”, not “my truth”. In history’s most famous court case, Jesus of Nazareth emphasized to Pontius Pilate that “I am here to testify to the truth”. Pilate’s curious reply was “what is truth?” This question has echoed across centuries of human history. Most recently in a New York Times interview covering the subject of artificial intelligence, I.T. guru Geoffrey Hinton spoke of a future with so much fake imagery and text that “nobody will be able to tell what is true anymore”. Jean Paul Sartre and other existentialist philosophers of the post-World War II era have argued that the only absolute truth is one’s existence. All other truths are created by men and women, and each is free to create their own versions of truth and their own ideas of what is correct and incorrect, right and wrong. Sartre’s mantra in this regard was “existence precedes essence”. It’s essentially a philosophy of “me” that centers on “me”. Modern narcissistic youth culture, secular media, and academia have embraced this philosophy (albeit with some modification) in an attempt to create “a
dictatorship of me”. What has become especially popular is the idea that truth is relative. With very little serious questioning postmodern educators and the media have touted that there is not “a truth”, there is my truth, your truth, and their truth.
In medical science, just as in the courtroom, we have preferred to work with “the truth” rather than my truth or your truth. We call such examples of truth; scientific laws, medical facts, and medical-scientific truths. These laws and facts are based on theories, observations, experimentation, and objective analysis, the often acclaimed scientific method. This format for the pursuit of scientific certainty assures us that what we know is indeed true and a consensus is thus formed based on such objective analysis and experimental data. Centuries ago, William Harvey proved beyond a doubt that the heart functions as a muscular pump pushing the blood through a vascular network. This is a medical fact. It is the truth, not just my truth or your truth. It’s not something one can deny or attempt to censor. This is because it has been objectively verified by experiment, analysis, and experience. Like most scientific laws it is also rational; it makes sense.

Existentialism deals with self-created truth. There is no objective truth or standard by which we can examine the veracity of your truth or my truth.
If objective truth does not exist, then examining tools, debate, and rational analysis become meaningless. In such a system when two “truths” stand in opposition to each other, there is no objective reference or guide to determine what side is right. Disputes then end up being settled violently by whoever has power and force on their side. This may mean political power, monetary power or simply a powerful control over the discourse (as in for example professional or media censorship). This has happened in the past (even before existentialism had any prominence) and it is happening even more so today with a post-modern existentialistic rationale. It’s a very concerning trend in regard to medical science.
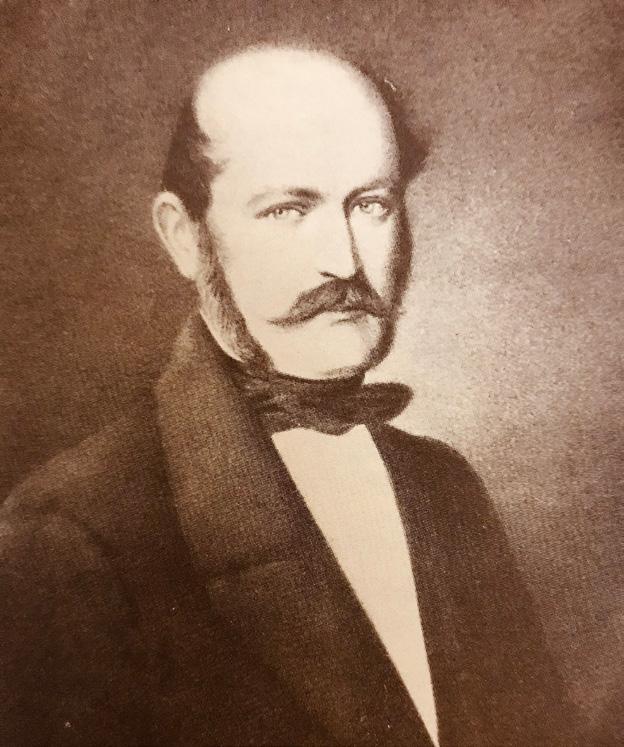
A classic example of how this becomes problematic occurred around 1850. Ignaz Semmelweis, a junior faculty obstetrician in Vienna, of Hungarian Jewish ethnicity, discovered a way to prevent “childbed fever”. This disease was the scourge of European obstetric wards with a mortality rate of 12 to 25%. After persistently studying the situation, Semmelweis concluded that the disease was spread by physicians with unclean hands examining women in labor. He recommended a regimen of handwashing with chlorinated lime solution to prevent the disease. The results of this practice were dramatically successful, a better than 90% reduction
in the incidence of childbed fever on that hospital ward. His Austrian superior, Johann Klein was unimpressed and preferred to believe, as everyone knew, that the disease was caused by a “miasma” in the air. Semmelweis had a prickly personality, and was an outsider, a political liberal who praised republicanism. There was also a degree of audacity seen in his suggestion that physicians were involved in causing the disease. This, plus his being a Jewish Hungarian junior faculty member in a Viennese medical profession dominated by Austrians, doomed the acceptance of the “Semmelweis Doctrine” until decades later. Klein had temporarily crushed the “hand washing” intervention by using political power and dogmatic authority. His truth ruled. In modern terms Semmelweis was “cancelled”. He died in an insane asylum and women continued to die from “childbed fever”.
A similar situation arose regarding “pink disease” in the first half of the 20th century. This condition caused encephalopathy, painful peripheral neuritis, severe anemia, poor feeding, and sometimes even death in infants
from 6 months to 2 years of age. Its cause was obscure until 1948 when Dr. Josef Warkany (a Jewish refugee from Vienna) reported high levels of mercury associated with the disease. Warkany was then on the faculty at Cincinnati Children’s Hospital. In Europe he had been a world famous teratologist. In America he was a post-World War II foreigner with a German accent. Mercury was a common ingredient in “teething powder” and diaper rinses. The idea of mercury being at the root of this was unfashionable and contrary to conventional pediatric teaching (teething was felt to be a dangerous condition and mercury in small amounts had been used medicinally for centuries). In a 1951 follow up study, Warkany and Hubbard reported on 41 children with pink disease and 92% of them had mercury in their urine. Yet, in Conybeare’s 1954 Textbook of Pediatrics, the etiology of the disease was still considered “uncertain”. Older pediatricians, manufacturers of teething powder, and those in positions of power continued to resist Warkany’s tenet. In the late 1950s and early 1960s mercury was finally withdrawn from teething powder and pink disease essentially disappeared. The pediatric hierarchy and the teething powder manufacturers had been all too content with “their truth” rather than contend with facts that were challenging and “inconvenient”.
In the 1920s a different type of disease was being discussed in Germany. The German state was said to be “inwardly sick and rotten”. The cause of this statewide disease was multifactorial and it included the mentally ill, the feeble minded, homosexuals, drug addicts, and the physically deformed. It would also eventually include Jews,
who were identified as “race polluters, parasites, germ carriers, maggots, and agents of racial tuberculosis”. The cure for this social epidemic was outlined in 1920 by Karl Binding and Alfred Hoche in a now infamous text, “The Permission to Destroy Life Unworthy of Life”. In this they advocated for eugenics and medicalized killing as a “healing work”. This preceded Hitler’s rise to power by more than a decade. Slowly but surely the German medical profession bought into these ideas. The euphemistic terms “healing work” are interesting to compare with the modern terms for abortion on demand up to the time of delivery, “reproductive health care”. In both cases killing is involved but disguised as a medical treatment, as a form of health care. In his book on the history of Nazi racial principles and their influence, “Racial Hygiene, Medicine under the Nazis”, Robert Proctor states “Biology and Medicine were commonly presented as providing the foundations for Hitler’s National Socialism”. In effect, German physicians who supported these ideas were “just following the science”. The National Socialist’s Physicians League announced as one of their maxims “the primacy of national biology over national economy”. The physical health of the state as determined by biological science was to trump any economic considerations. A similar disregard for the economy took place during the Covid-19 epidemic in the United States when draconian mandates closed so many businesses in the name of medical science. Truly there is nothing new under the sun. Academics in every field gave
Continued on Page 22
From Page 21
support to the Nazi regime. Those who resisted were forced to leave the country or taken to concentration camps.
In Russia during the 1930s, biologist Trofim Lysenko waged a political campaign with the aid of communist dictator Joseph Stalin against Mendelian Genetics which they labeled “bourgeois pseudoscience”. In its place they promoted a form of Lamarckism that decades of experimentation had proven wrong. But that didn’t matter, Lysenkoism was taught in schools as the only acceptable theory. Biologists who spoke out against Lyysenkoism were imprisoned (as in the case of Nicola Vavilov) or executed. Eventually, scientists throughout the entire Soviet Bloc (including Poland, Czechoslovakia, Hungary, and East Germany) were forced to accept this discredited theory that promised to turn Siberia into a land filled with orchards and gardens. Only with the death of Stalin in 1952 did things begin to change. Medical Genetics was set back decades in these countries.

In the United States during the last quarter of the 20th century, the specter of mercury toxicity rose again. Some pediatricians and parents noted autism occurring in children apparently in relation to the timing of vaccinations. A mercury compound, thimerosal, was being used then as a preservative in certain vaccines. This led to a movement among some parents to refuse having their children vaccinated. The pediatric establishment and the companies producing the vaccines argued vigorously that the vaccines had nothing to do with triggering autism. After all, millions of children were vaccinated and the overwhelming majority of children tolerated the immunizations quite well. That same argument had been used in regard to teething powder and pink disease. Unfortunately, the pediatricians had not learned an important lesson regarding pink disease. Renal excretion of mercury can vary quite a bit and that likely plays a role in the susceptibility to mercury toxicity. Recently, it’s been documented that pink disease survivors were more likely to have grandchildren with autism. It is becoming increasingly clear that the mercury in the vaccines probably played a role in at least some
cases of autism. Mothers who were opposed to the routine childhood vaccination regimen during this controversy were often labeled as “nutty women” by the medical community. Some pediatricians even refused to accept unvaccinated children as patients.
In the early years of the 21st century there were attempts to discredit evolutionary biology and mandate the parallel teaching of creationism as part of a religious and political agenda. A very small group of scientists supported these ideas and proposed a “new scientific theory” which they named “intelligent design”. Conservative lawmakers, primarily in the Midwest, attempted unsuccessfully to legislate the teaching of “intelligent design” into the biology curricula. This new theory could be neither proven nor disproven as it was more of a religious or philosophic argument than a new scientific paradigm. The whole situation rekindled memories of the 1920s when in some states teaching the “theory of evolution” was a crime.
These historical events show how medical scientific non-truths can be presented as the only true scientific option (as with Nazi eugenics, and

Stalin’s Lysenkoism) by powerful agenda driven elites. There is also a history of the drug industry, organized medicine and powerful medical academics refusing to accept medical scientific truths that are inconvenient or imply an iatrogenic etiology. In these cases my truth and our truth replaces the truth.
In the past few years this has all been repeated. During the Covid-19 pandemic, national health experts salaried by the federal government as well as political leaders of the Democratic party assured the American people that the pandemic arose in the Wuhan marketplace from infected bats. This, they said, had been scientifically proven. And yet the first three cases in Wuhan had no known connection to the market. Add to this the fact that a laboratory experimenting with coronavirus was in Wuhan and you have circumstances that suggest a possible laboratory origin. Plus, they could not demonstrate the entire Covid-19 genome in any bats or in any intermediate host such as pangolins. In 2021, eighteen preeminent virologists wrote in science’s most prestigious journal “Nature” that the origins of Covid-19 needed to be further investigated. It was not all a “done deal”. Still the folks from the NIH and the government pundits maintained it came from bats. Most importantly, people (including scientists) who dissented from this viewpoint were censored and removed from social media. Medical schools (dependent on federal funding) also mainly towed the party line.
The point here is not which side is right in this debate. The point is that the question has not been answered and more debate and data are needed.
Silencing descent is not the way science should be done. This should be obvious from the previous historical examples. There were similar debates regarding the ability of standard surgical masks to prevent infection and whether the new coronavirus vaccines were safe for children. These were legitimate questions, but again social media moguls and political leaders tried to silence those who didn’t agree with their truth. Most ridiculous of all was how wearing or not wearing a mask became a badge of political loyalty. The scientific community needs to abhor silencing debate.
That is not happening. There is currently a group of academics that believe there are more than two biological sexes. There are at least as many scientists and physicians (probably more) who think this is nonsense. No biologist has ever demonstrated in humans more than two types of gametes, male and female, spermatozoa and ovum. Some exponents of the new gender theories claim there are three sexes, others seven, others eleven. The number of possible genders and their corresponding pronouns seems to increase every few months. A biologic man can claim to really be a woman just by saying so. A “gender fluid” person can claim to be a man one day and a woman the next day and sometimes they claim to be both simultaneously. Surgical interventions to change the sex characteristics of minors are being accepted as legitimate effective therapeutic procedures without much supportive research. Transsexual women are claiming to be able to have menstrual cycles and this claim is supported by some academics. In this regard it may be good to recall the words of Voltaire “those who can make
you believe absurdities, can make you commit atrocities”.
A political agenda is driving this debate more than a scientific one. Dissenters are called transphobic, homophobic, fascists, or Nazis. The challenges that dissenters offer are labeled as disinformation or hate speech. One wonders when such things will labeled as Orwellian “thought crimes”. Once again we are seeing an attempt to silence discussion on a topic that has vast medical and social repercussions. Promoting “queerness” is a part of the LGBTQ agenda for some LGBTQ activists. Gender confusion and the idea of gender fluidity (an absurdity until recently) serve that purpose well. Medical centers treating these problems make more and more money as gender dysphoria becomes increasingly common (in teenage girls the increase has been exponential). Picking one’s own gender has for some persons become the ultimate existentialistic choice. We are no longer confined by our biological sex. We determine if we are men or women and we can do it whenever we want. Each person’s “truth” trumps any other “truth” and dissenters must be shouted down or silenced. There are adults and children who legitimately suffer from gender dysphoria and they need good rational scientifically proven treatments that truly work and do no harm. There are others that are simply pursuing a fetish or fad and they need help too. What works best in these circumstances should not be determined by politicians or agenda driven activists.
It is really not completely clear at this time how to accurately identify the
Continued on Page 24
From Page 23
persons with true gender dysphoria, what is its’ biologic cause, what are all the psychosocial factors involved, and what is the best way to treat these persons so that a good outcome is achieved. There is still considerable debate among medical and psychological professionals on these issues. In a 2015 position paper on gender dysphoria the Spanish Society of Endocrinology and Nutrition noted the need for concern “that any clinical intervention should follow the principles of scientific rigor, experience, ethical, and deontological principles and the necessary caution in front of chronic, aggressive, and irreversible treatments”. The LGBTQ community and some professionals have taken the stand that any treatment other than gender affirmation should be outlawed and some states are attempting to do this. One size fits all usually doesn’t work well in medicine. Many medical conditions have subgroups that require different forms of therapy. It is reasonable to assume that more detailed studies and analysis will reveal various subgroups of persons with gender dysphoria (this is already occurring to some extent) and that these subgroups will not all respond to or even desire gender affirmation to attain a good outcome. Some studies in the pediatric population suggest that many children respond well to just psychological counseling without gender affirmation. But when sociopolitical agendas determine what is true in science and medicine serious problems can arise. Silencing debate and discourse is not the way science should be pursued in a free society. That’s a truth that even Jean Paul Sartre would concur with and that medical history should have taught us.
1) Stewardson A, Didier P, “Ignaz Semmelweis-Celebrating a Pioneer of Patient Safety”, Lancet, vol.75 Issue 9785, pages 22-24, July2011.
2) Dally A, “The Rise and Fall of Pink Disease”, Social History of Medicine vol. 10 issue 2, pages 291-304 August 1997.
3) Lifton, R.J., “The Nazi Doctors, Medical Killing and the Psychology of Genocide”, Basic Books Inc. New York, N.Y., pages22-125, 1986.
4) Proctor R, “Racial Hygiene, Medicine Under the Nazis”, Harvard University Press, Cambridge, Mass. pages 62-83, 1988.
5) Mutter J et al, “Mercury and Autism: Accelerating Evidence”, Neuro Endocrinology Letters, 2005 Oct; 26(5):439-46.
6) Kern J et al, “The Relationship Between Mercury and Autism: A Comprehensive Review and Discussion”, J Trace Elem Med Biol. 2016 Sep;37-8-24;doi 10.
7) Shandley K et al, “Ancestry of Pink Disease (Infantile Acrodynia Identified as a Risk Factor for Autism Spectrum Disorders)”, J Toxicol. Environ Health 2011;74(18):1185-94
8) Zapatera Gaviria A et al, “What Do We Know About the Origin of Covid-19 Three Years Years Later”, Revista Clinica Espanola 223 (2023)240-291.
9) Bloom, JD al, “Investigate the Origins of Covid 19”, Science 2021; 372:694.
10) De Vries, A, Klink D, et al, “What the Primary Care Pediatrician Needs to Know about About Gender Incongruence and Gender Dysphoria in Children and Adolescents” Ped Clinic of North Am. 2016 Dec; 63(6):1121—1136.
11) Wallien, Madeline et al. “Psychological Outcome of GenderDysphoric Children”, J Am Acad Child Adolesc Psychiatry. 2008 Dec; 47(12):PP. 1413-1423-
12) De Antonio, I E et al, “Position Statement: Gender Dysphoria in Childhood and Adolescence, Working Group on Gender Identity and Sexual Development of the Spanish Society of Endocrinology and Nutrition”, Endocrine Nutrition 2015 Oct; 62(8):380-3.
VOQUEZNA™ contains vonoprazan, a novel potassium-competitive acid blocker (PCAB), co-packaged with amoxicillin and/or clarithromycin tablets as an FDA approved treatment of Helicobacter pylori (H. pylori) infection in adults. VOQUEZNA™ is supplied as VOQUEZNA™ Triple Pak™ (vonoprazan 20 mg tablets; amoxicillin 500 mg capsules; clarithromycin 500 mg tablets) and VOQUEZNA™ Dual Pak™ (vonoprazan 20 mg tablets; amoxicillin 500 mg capsules). Both packs contain a 14-day supply of co-packaged medication, dosed twice-daily (vonoprazan triple pack) or three times daily (vonoprazan dual pack).1 Vonoprazan is marketed by Phathom Pharmaceutical and is predicted to be available for prescribing in the first quarter of 2023.2
Triple therapy with a PPI, clarithromycin, and amoxicillin (or metronidazole) is the treatment standard for eradication of H. pylori in the United States. However, increasing resistance to commonly used antibiotics, including clarithromycin and metronidazole, has led to a decline in H. pylori eradication rates with PPI-based triple therapy.3
Vonoprazan is the first FDA approved drug that inhibits the gastric acid secretion pathway in a reversible manner. The final step in the gastric acid secretion pathway is catalyzed by the enzyme gastric H+/K+-ATPase. Proton pump inhibitors (PPIs) and PCABs (vonoprazan) both inhibit the H+/K+-ATPase enzyme and prevent the final step of gastric acid production. PPIs do so in an irreversible manner while PCABs in a reversible manner via competitively blocking potassium channels.4 Preclinical studies showed that vonoprazan is stable at a low pH
and produces a more potent, longer lasting acid-blocking activity than PPIs. Because they are stable at low pH, PCABs do not require a gastroprotective formulation, which results in a faster and less variable onset of effect.5
In a phase III randomized controlled trial in Japanese patients with H. pylori gastroduodenal ulcers treated with either vonoprazan 20 mg (with amoxicillin 750 mg and clarithromycin 200 mg or 400 mg) or lansoprazole 30 mg (with amoxicillin 750 mg and clarithromycin 200 mg or 400 mg), the overall incidence of adverse effects (diarrhea, nasopharyngitis, and dysgeusia) was 34.0% in the vonoprazan group and 41.1% in the lansoprazole group. Adverse effects that occurred in greater than 2% of patients included diarrhea (12.5% vs 15.3%), nasopharyngitis (5.5% vs 4.7%), and dysgeusia (4.0% vs 3.1%) in the vonoprazan group and lansoprazole group, respectively. Drug-related adverse effects occurred in 20.4% of patients in the vonoprazan group compared to 24.6% in the lansoprazole group. Serious adverse effects occurred in 4 versus 2 patients in the vonoprazan and lansoprazole groups, however the specific adverse effects were not reported. Adverse effects leading to study drug discontinuation occurred in 3 versus 2 patients in the vonoprazan and lansoprazole groups respectively.6
Another randomized controlled trial that compared twice daily vonoprazan dual pack to twice daily vonoprazan triple pack observed similar rates of adverse events between groups (27.5% versus 30.5%, p=0.524). Four participants (three in the dual therapy and 1 in the triple therapy group) discontinued the treatment
due to skin rash or diarrhea and nausea. No severe adverse events occurred and 91.4% of adverse events were mild. The most common adverse events were diarrhea, bloating, and constipation.7
Vonoprazan in dual and triple packs have both been shown to be tolerable in clinical trials. Two phase I studies conducted in Japan and the UK found single doses of vonoprazan up to 120 mg (Japanese study) and single doses up to 40 mg (UK study) were well tolerated in healthy volunteers.8 A phase II study of patients with erosive esophagitis showed that vonoprazan was well tolerated at doses of 5, 10, 20, and 40 mg daily.9
In a randomized, controlled trial in the United States and Europe, adverse effects occurred in 2.3% of H. pylori-positive, adult patients receiving vonoprazan triple pack or vonoprazan dual pack twice daily for 14 days. The most common adverse reactions that occurred in the vonoprazan triple therapy and vonoprazan dual therapy groups respectively included diarrhea (5.2% and 4.0%), dysgeusia (0.6% and 4.6%), vulvovaginal candidiasis (2.0% and 3.2%), abdominal pain (2.6% and 2.3%), headache (1.4% and 2.6%), hypertension (1.1% and 2.0%), and nasopharyngitis (2.0% and 0.3%). Adverse reactions leading to treatment discontinuation occurred in 1.2% of patients treated with vonoprazan dual therapy, the most common being rash, which occurred in 0.6% of patients. Adverse reactions leading to treatment discontinuation occurred in 2.3% of patients treated with vonoprazan triple therapy, the most common being diarrhea (0.6%) and hypertension (0.6%).1
Continued on Page 26
From Page 25
A phase III, randomized, double-blind, multicenter, parallel-group comparative study was designed to verify the non-inferiority of vonoprazan to lansoprazole for the eradication of H. pylori in patients with gastroduodenal ulcers. The vonoprazan group received vonoprazan 20 mg, amoxicillin 750 mg, and clarithromycin 200 mg or 400 mg, twice daily for 7 days. The lansoprazole group received lansoprazole 30 mg, amoxicillin 750 mg, and clarithromycin 200 mg or 400 mg, twice daily for 7 days. This trial found a first-line eradication rate of 92.6% (95% CI, 89.2% to 95.2%) in the vonoprazan group versus 75.9% (95% CI, 70.9% to 80.5%) in the lansoprazole group. The difference between treatment groups was 16.7% (95% CI, 11.2% to 22.1%) confirming non-inferiority of vonoprazan to lansoprazole with a non-inferiority margin of 10% (p<0.0001).6
A prospective, multicenter, randomized controlled trial in Japan compared twice daily vonoprazan dual therapy to twice daily vonoprazan triple therapy. Patients with an H. pylori-positive culture test who were naïve to treatment were randomly assigned to receive either dual or triple vonoprazan therapy for a duration of 7 days, with stratification by age, sex, H. pylori antimicrobial resistance, and institutions. Patients were tested for eradication of H. pylori at least 4 weeks after treatment. The H. pylori eradication rates after treatment were similar between the vonoprazan dual and triple therapy groups by both the intention-to-treat analysis (84.5% and 89.2%, p=0.203) and by the per-protocol analysis (87.1% and 90.2%, p=0.372). Patients who were positive for clarithromycin-resistant H. pylori had a higher eradication rate if they received vonoprazan dual therapy compared to triple therapy (92.3% versus 76.9%, p=0.048).7
Finally, a meta-analysis of 5 studies found that eradication rate of clarithromycin-susceptible H. pylori infections was not significantly different with vonoprazan-based treatment compared to PPI-based treatment (pooled eradication rates, 95.4% versus 92.8%, p=0.225). However, for clarithromycin-resistant H. pylori infections, vonoprazan-based triple therapy was superior to PPI-based therapy in randomized controlled trials (pooled eradication rates, 82.0% versus 40.0%, p<0.0001) and in non-randomized controlled trials (80.8% versus 41.8%, p<0.0001).10
The average wholesale price (AWP) for each tablet/capsule supplied in both vonoprazan dual and triple packs is around $8.70. Each pack contains 112 tablets/capsules and costs $975 for one 14-day package.11,12 In comparison, the AWP for a 14-day kit of lansoprazole, amox-
icillin, and, clarithromycin costs about $360.13 If prescribed separately, a 14-day supply of lansoprazole 30 mg (28 capsules, $13.24 each), amoxicillin 500 mg (56 capsules, $0.39 each), and clarithromycin 500 mg (28 tablets, $6.02 each) would cost $561.12.14,15,16
Discount cards are available through GoodRx. com, with prices varying by pharmacy. The current discounted price with coupon is $807.41 for both vonoprazan dual pack and vonoprazan triple pack, $265.05 for lansoprazole, amoxicillin, and clarithromycin 30-500-500 mg kit, or a total of $46.49 for three separate prescriptions of lansoprazole capsules, amoxicillin capsules, and clarithromycin tablets.17
Vonoprazan is not specifically formulated to reduce pill burden, instead, the co-packaged tablets and capsules in blister packaging increase ease of dispensing and administration.1
Vonoprazan does not require renal or hepatic dosage adjustment but both regimens should be avoided in patients with severe renal impairment (eGFR < 30 mL/min) and in patient with moderate to severe hepatic impairment (Child-Pugh B or C). Two components of the vonoprazan co-packaged therapy (vonoprazan and clarithromycin) are substrates for CYP3A. Clarithromycin is also a strong CYP3A inhibitor and P-glycoprotein inhibitor. Concomitant use of vonoprazan with CYP3A inducers and inhibitors, as well as P-glycoprotein substrates, should be avoided. Both vonoprazan dual and triple pack regimens can be taken with or without food.1
Vonoprazan is a novel potassium-competitive acid blocker that can be used for the treatment of H. pylori infection. Clinical trials have shown that vonoprazan dual pack and vonoprazan triple pack are safe and tolerable with mild side effects including gastrointestinal upset (diarrhea, constipation, and nausea), nasopharyngitis, vulvovaginal candidiasis, and dysgeusia.1 In clinical trials, serious adverse effects or adverse effects leading to drug discontinuation occurred in less than 2% of study participants. Vonoprazan has demonstrated non-inferiority to the current standard H. pylori treatment with a PPI, clarithromycin, and amoxicillin, for non-clarithromycin resistant infections, and is superior to standard H. pylori treatment for clarithromycin-resistant infections.6,7 The cost of vonoprazan is the largest barrier to its accessibility.11,12 Even with discount cards accepted at most retail pharmacies, the cost is over $800 for a complete 14-day course of therapy.17
Given the cost and non-inferiority to the current standard of care for clarithromycin-susceptible H. pylori infections, vonoprazan may be most beneficial if reserved for treatment of clarithromycin-resistant H. pylori infections.
1. VOQUEZNA TRIPLE PAK (vonoprazan tablets; amoxicillin capsules; clarithromycin tablets) and VOQUEZNA DUAL PAK (vonoprazan tablets; amoxicillin capsules) [package insert]. Buffalo Grove, IL: Phathom Pharmaceuticals; 2022.
2. Phathom Pharmaceuticals Announces FDA Approval of VOQUEZNATM. GlobalNewsWire. March 5, 2022. Accessed October 21, 2022. https://www.globenewswire.com/news-release/2022/05/03/2435147/0/en/ Phathom-Pharmaceuticals-Announces-FDA-Approval-of-VOQUEZNA-TRIPLE-PAK-vonoprazan-amoxicillin-clarithromycin-and-VOQUEZNA-DUAL-PAK-vonoprazan-amoxicillin-for-the-Treatment-of-H-pylo.html
3. Chey WD, Wong BCY, Practice Parameters Committee of the American College of Gastroenterology. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102(8):1808-1825. doi:10.1111/ j.1572-0241.2007.01393.x
4. Shin JM, Inatomi N, Munson K, et al. Characterization of a novel potassium-competitive acid blocker of the gastric H,K-ATPase, 1-[5-(2-fluorophenyl)-1-(pyridin-3-ylsulfonyl)-1H-pyrrol-3-yl]-N-methylmethanamine monofumarate (TAK-438). J Pharmacol Exp Ther. 2011;339(2):412-420. doi:10.1124/jpet.111.185314
5. Hori Y, Imanishi A, Matsukawa J, et al. 1-[5-(2-Fluorophenyl)-1-(pyridin-3-ylsulfonyl)-1H-pyrrol-3-yl]-N-methylmethanamine monofumarate (TAK-438), a novel and potent potassium-competitive acid blocker for the treatment of acid-related diseases. J Pharmacol Exp Ther. 2010;335(1):231-238. doi:10.1124/jpet.110.170274
6. Murakami K, Sakurai Y, Shiino M, Funao N, Nishimura A, Asaka M. Vonoprazan, a novel potassium-competitive acid blocker, as a component of first-line and second-line triple therapy for Helicobacter pylori eradication: a phase III, randomised, double-blind study. Gut. 2016;65(9):1439-1446. doi:10.1136/gutjnl-2015-311304
7. Suzuki S, Gotoda T, Kusano C, et al. Seven-day vonoprazan and low-dose amoxicillin dual therapy as first-line Helicobacter pylori treatment: a multicentre randomised trial in Japan. Gut. 2020;69(6):1019-1026. doi:10.1136/gutjnl-2019-319954
8. Sakurai Y, Nishimura A, Kennedy G, et al. Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of Single Rising TAK-438 (Vonoprazan) Doses in Healthy Male Japanese/non-Japanese Subjects. Clin Transl Gastroenterol. 2015;6:e94. doi:10.1038/ ctg.2015.18
9. Ashida K, Sakurai Y, Nishimura A, et al. Randomised
clinical trial: a dose-ranging study of vonoprazan, a novel potassium-competitive acid blocker, vs. lansoprazole for the treatment of erosive oesophagitis. Aliment Pharmacol Ther. 2015;42(6):685-695. doi:10.1111/apt.13331
10. Li M, Oshima T, Horikawa T, et al. Systematic review with meta-analysis: Vonoprazan, a potent acid blocker, is superior to proton-pump inhibitors for eradication of clarithromycin-resistant strains of Helicobacter pylori. Helicobacter. 2018;23(4):e12495. doi:10.1111/hel.12495
11. Vonoprazan, amoxicillin, and clarithromycin (co-packaged): Drug information. Lexicomp. Accessed October 20, 2022. https://www.uptodate. com/contents/vonoprazan-amoxicillin-and-clarithromycin-co-packaged-drug-information?search=vonoprazan&selectedTitle=1~4&usage_type=panel&display_rank=1&kp_tab=drug_general&source=panel_search_result#F57055664
12. Vonoprazan and amoxicillin (co-packaged): Drug information. Lexicomp. Accessed October 20, 2022. https://www.uptodate.com/contents/ vonoprazan-and-amoxicillin-co-packaged-drug-information?search=vonoprazan&selectedTitle=1~4&usage_type=panel&display_rank=1&kp_ tab=drug_general&source=panel_search_result
13. Lansoprazole, amoxicillin, and clarithromycin (co-packaged): Drug information. Lexicomp. Accessed October 21, 2022. https://www.uptodate.com/ contents/lansoprazole-amoxicillin-and-clarithromycin-copackaged-drug-information?search=prevpac&source=panel_search_result&selectedTitle=1~1&usage_type=panel&kp_tab=drug_general&display_rank=1
14. Lansoprazole: Drug information. Accessed October 21, 2022. https://www.uptodate.com/contents/ lansoprazole-drug-information?search=lansoprazole&source=panel_search_result&selectedTitle=1~85&usage_type=panel&kp_tab=drug_general&display_rank=1
15. Amoxicillin: Drug information. Lexicomp. Accessed October 21, 2022. https://www.uptodate.com/ contents/amoxicillin-drug-information?search=amoxicillin&source=panel_search_result&selectedTitle=1~148&usage_type=panel&kp_tab=drug_general&display_rank=1
16. Clarithromycin: Drug information. Lexicomp. Accessed October 20, 2022. https://www.uptodate.com/ contents/clarithromycin-drug-information?source=auto_suggest&selectedTitle=1~2---1~2---clarithro&search=clarithromycin
17. GoodRx. goodrx.com. Accessed October 20, 2022. https://www.goodrx.com/
Nearly all physician practices and healthcare providers maintain a digital presence today. Few independent practices design their own websites, instead contracting out to professionals. Recently, a common feature incorporated into many website and mobile app designs that gathers user data for analytical purposes has caught the attention of the federal agency that interprets and enforces the HIPAA privacy and security rule. If you have a website for your practice, you should determine if it includes one or more of these “data trackers” and take appropriate steps to remain in compliance with HIPAA.
Data trackers (such as cookies, tracking pixels, beacons, and session replay scripts) are elements encoded into a website that capture and analyze the activities of those who access the website and report that tracking data for advertising and analytical purposes. “Pixels,” one common form of trackers, are snippets of HTML or JavaScript code or tiny invisible 1×1 pixel images that are placed on web pages, usually
in the footer, and are used to gather information about website visitors and track their activity. “Cookies” are HTML code that interact with web browsers to track, personalize, and save information about each user’s session. The web server embeds identifying data to the user’s web browser, which remembers when the user lands on that site in the future. If you ever wondered why your social media feed fills up with ads for the very product you were just searching for on Google, thank a tracker. (No, your phone is not eavesdropping on you).
An adage about the Internet holds that if you are not paying for a product, you are the product. In fact, that principle has applied to many traditional media including radio and broadcast (pre-cable) TV. As always, advertisers want to reach eyeballs, and not just any eyeballs. Today’s advertisers want to narrowcast their messages to specific audiences and carefully quantify their return on investment for each ad. They can’t tell who reads a billboard or magazine ad, but increasingly tracker technology can reveal a great amount of information about anyone who clicks on a website or online ad.
So, how does HIPAA figure in? In December, the U.S. Department of Health and Human Services (HHS)
Office for Civil Rights (OCR) published a Bulletin warning HIPAA-covered entities and business associates about the use of tracking technologies that may collect protected health information (PHI) in violation of HIPAA. OCR stated:
The HIPAA Rules apply when the information that regulated entities collect through tracking technologies or disclose to tracking technology vendors includes protected health information (PHI). Some regulated entities may share sensitive information with online tracking technology vendors and such sharing may be unauthorized disclosures of PHI with such vendors. Regulated entities are not permitted to use tracking technologies in a manner that would result in impermissible disclosures of PHI to tracking technology vendors or any other violations of the HIPAA Rules. For example, disclosures of PHI to tracking technology vendors for marketing purposes, without individuals’ HIPAAcompliant authorizations, would constitute impermissible disclosures.

OCR warned that although data gathered by trackers could be used in beneficial ways to help improve care or the patient experience, it could also be misused to promote misinformation, identity theft, stalking, and harassment.
Trackers may capture individually identifiable health information (IIHI) that the individual provides when they use HIPAA covered entities’ websites or mobile apps, including medical record numbers, home or email addresses,
or dates of appointments, geographic location, medical device IDs, or other unique identifying code. IP addresses, which identify a computer or device but not the user, are frequently captured by trackers. OCR considers all these items to generally be PHI, even if it relates to individuals who have not been treated by or even scheduled treatment by the covered entity. This is because such information relates to the individual’s past, present, or future health or health care or payment for care. For example, if an individual searched the term “oncologists in Allegheny County,” that search could suggest that the individual may have cancer or suspect that they do.
Covered entities may have userauthenticated webpages, which require a user to log in, such as a patient or health plan beneficiary portal or a telehealth platform, and/ or unauthenticated webpages, that do not require users to log in, i.e., the general information portions of a public-facing website. As expected, the authenticated pages capture more identifiable information and OCR requires them to meet all HIPAA requirements even if an individual is not yet a patient of the entity. Patient portals and other authenticated pages frequently contain sensitive PHI, such as an individual’s IP address, medical record number, home or email addresses, dates of appointments, etc.
With respect to unauthenticated webpages, which generally do not collect PHI, tracking technology could capture information about visitors to a webpage that addresses specific symptoms or health conditions, or that permits individuals to search for doctors or schedule appointments
without entering credentials. For example, tracking technologies could collect an individual’s email address and/or IP address when the individual visits a regulated entity’s webpage to search for available appointments with a health care provider.
Any time a covered entity is disclosing PHI to the tracking technology vendor, OCR considers that vendor to be a HIPAA Business Associate and requires the covered entity to obtain a Business Associate Agreement. Some of the more prominent tracker companies including Google Analytics and Meta (Facebook’s parent company) have refused to sign BAAs. These companies claim to be able to identify, filter and “scrub” potentially sensitive health-related data from the data stream they collect so that it is never ingested into their ads ranking and optimization systems. Not good enough, according to OCR, who stated “it is insufficient for a tracking technology vendor to agree to remove PHI from the information it receives or de-identify the PHI before the vendor saves the information. Any disclosure of PHI to the vendor without individuals’ authorizations requires the vendor to have a signed BAA in place and requires that there is an applicable Privacy Rule permission for disclosure.”
So, can you just have visitors click through a box to grant permission? Not so fast – OCR says HIPAA does not permit PHI disclosures to tracking technology vendors “based solely on a regulated entity informing individuals in its privacy policy, notice, or terms and conditions of use” of such disclosures. OCR further states that website
banners that ask users to accept or reject a website’s use of tracking technologies, such as cookies, do not constitute a valid HIPAA authorization.
Several vendors have emerged in recent months who claim to offer a solution to this dilemma by signing BAAs with covered entities, interposing their technology between the covered entity and the tracker company, and scrubbing PHI from the data so that it never reaches a destination that is not covered by a BAA. This may prove to be a valid approach but requires careful review.
Several large lawsuits are working their way through the courts targeting tracking service vendors and the webpage owners who used them, sometimes without fully understanding what their web vendors had installed. As a precaution, many healthcare providers have chosen to remove the trackers from their websites, but that may prove insufficient depending on how the courts rule. Others have limited the trackers to the unauthenticated, general portions of their websites, and/or limited the kinds of information that the trackers can gather.
If you have a website, your first step should be to determine if any trackers are installed and if so, what information they are gathering and from what portions of your website. Then, consult qualified counsel for guidance on the best way to remedy any noncompliance.
across the age spare in time for treatments to be effective. The result is that nearly every rare genetic disorder becomes a candidate for therapy as its cause becomes discovered.
jeRRy voCKley, mD, PhD
Dr. Vockley is Chief of Genetic and Genomic Medicine and Director of the Center for Rare Disease Therapy at the UPMC Children’s Hospital of Pittsburgh, and the Cleveland Family Endowed Chair for Pediatric Research in the Department of Pediatrics at the University of Pittsburgh School of Medicine. He is a Founding Fellow of the American College of Medical Genetics and Genomics (ACMG) and currently serves on its board of directors. He is an ACMG delegate to the AMA House of Delegates.
Rare genetic disorders affect as many as 3-5% of all babies born in the United States, accounting for 40% of neonatal and childhood mortality. They also represent a significant burden of chronic hospitalization and medical care utilization for adults as well as children. Approximately 10,000 such disorders have been identified or hypothesized to exist. Treatment is supportive except in a limited number of instances where specific treatments exist. Development of new therapies has been hampered by at least two major factors: difficulty in diagnosing diseases early enough to enable treatment before irreversible damage occurs, and the high cost of developing new drugs and getting them approved by regulatory agencies. Whole genome sequencing techniques have become exponentially less expensive and more rapid since the completion of the human genome project, such that return of clinical data can now be achieved in days rather than years and at a cost that is comparable to other less expansive techniques. This data can be reanalyzed on a regular basis, allowing for identification of genetic disease
Gene therapy has often been heralded as being “just around the corner” for nearly 25 years. However, ethical, and technical hurdles have slowed its development. Recent advances suggest we may indeed now be turning that corner. At least 334 potentially durable, nononcology gene therapies are in development, including 40 in phase 2 trials or later, and ClinicalTrials.gov listed over 2,000 gene therapy trials as of mid-2022. Several such therapies for rare diseases have already been approved by the FDA, and by
2030, it is estimated that at least 30 nononcology gene therapies will be approved in the United States alone. These therapies could be used to treat up to 50,000 patients annually and have the potential to result in major shifts in disease management pathways. The clinical implications of gene therapy are profound but highlight the bottlenecks in drug development that still limit transition to treatments. Movement from the basic science laboratory to clinical trials is hampered by a regulatory system rooted in traditional trial design for common disorders, with a focus on double blind, placebo control trials as the gold standard. Not only are such trials not necessarily the best model to study efficacy in rare diseases, but they can also be unethical in diseases with early onset or a rapidly progressive course. This reality requires a fresh assessment of safe ways to obtain approval for new drugs for rare diseases. Simply put, development of new therapies one disease at a time is not tenable in an era when the cause of dozens, if not hundreds of new diseases is uncovered each year.
Clinical trial design for rare diseases often requires special consideration compared to those of larger trials for common disorders. Traditional randomized controlled trials with small sample size may not be appropriate or even adequately powered for statistical significance especially given a potentially large number of known and unknown risk factors. Platform options that allow application of a
repetitive technology would accelerate trials in many instances. For example, considering gene therapy vectors with different gene inserts as fundamentally the same “medication” would reduce the need for entry level toxicology studies and shorten the time to phase 1 trials in patients. At the other end of the spectrum, “N of 1 trials” by definition test one drug, potentially designed for one patient, and cannot be either blinded or broad based. Finally, drug development and testing are an incredibly expensive and high risk proposition that is most likely to be successful through public, industrial and academic collaboration. Here, public funding of basic science research (largely via the National Institutes of Health) can provide sufficient insight into the pathophysiology of a rare disease and identify appropriate targets for clinical drug development, while industry can benefit from more targeted clinical trials that require less pre-clinical expense on their part. Finally, novel trial design as defined by the FDA can minimize expense while safeguarding patient safety. Legislation will likely be necessary to adress some of these issues.
Given the limited implementation of gene therapy to date, and the relative lack of data on the long-term efficacy and safety of treatments, the practical clinical implementation of potentially single-treatment in vivo gene therapy can be modeled on care pathways for other single-treatment, clinically high-value but complex procedures such as solid organ transplantation or stem cell transplantation, where healthcare systems have developed hub-and-spoke models of care to accommodate the unique needs of these patients. Selection of patients must ensure that the right therapy is used for the right gene, and sometimes even the correct specific gene mutation. Long term follow- up of patients to demonstrate efficacy will be critical to direct cost-effective implementation of gene therapies. Ultimately, there are multiple stakeholders in the process of gene therapies for rare genetic disorders including patients, academic scientists, government funders, and pharmaceutical companies, all of whom will need to collaborate in the development process to guarantee safe, effective, and equitable treatments.


Tiffany DuMont, DO - AHN - Pulmonology

Dillon Stein, DO - Butler Memorial Hospital - Hospice & Palliative Care
Elizabeth Ungerman, MD, MS - UPMC - Anesthesiology and Perioperative Medicine
Ravi Ved, DO - AHN - Primary Care - Sports Medic ine
Meilin Young, MD - AHN - Pulmonology
 By: jessiCa meRolillo—Business oPeRations manageR—heyl Family PRaCtiCe
By: jessiCa meRolillo—Business oPeRations manageR—heyl Family PRaCtiCe
member who through the eyes of colleagues and patients goes above and beyond in providing patient care. His nomination outlined his ability to connect with patients on a deeper level, his dedication to promoting a healthy lifestyle, and his authenticity.

For Dr. Louis Heyl, the field of medicine has been an integral part of his life; some might even say it’s deeply personal. As a second-generation physician, so much of what Dr. Heyl learned about medicine came as a direct result of his shared experiences with his father, Dr. Frank Heyl. When Dr. Heyl’s father started practicing medicine out of his home in West View over 75 years ago, quality patient care and accessibility built a strong foundation for a practice that would soon pave the way for healthcare in the Pittsburgh area.
Not many practices in the Pittsburgh area, if any, span three generations, with two of those generations caring for patients in the original building where it all began. More than that, not many practices can grow to the extent Heyl Family Practice has grown and remain accessible and personal with their patients. To achieve that feat, it takes something special. It takes an Everyday Hero like Dr. Louis Heyl.
Dr. Heyl was recently nominated for the Pennsylvania Medical Society’s Everyday Hero award, an award that recognizes a PAMED

If you ask him, though, what he does isn’t “special”, it is what he signed up to do as a physician. “It’s something I love to do. You hear all these [great things said about you] and you just think, ‘Of course, why wouldn’t I do those things?’” The truth of the matter is, there are qualities that separate a good doctor from a great doctor, and Dr. Heyl embodies many of those – just ask his patients, his staff, and his family. He has carried on the legacy of his father with grace and high regard.
Sandra, 74, and Bob Guckert, 80, have been patients of the practice since Dr. Frank Heyl walked the halls of the West View Office. As original patients of his, and now patients of Dr. Lou Heyl, they can’t say enough great things about the continued support over the years. Sandra recalled a time when her husband, Bob, was hospitalized due to some health complications. Dr. Heyl eased their uncertainty.
“You know when [you’re at the hospital] the doctor comes to check on you and they are out of the door before they even get in? Well, when Dr. Heyl comes in, he pulls up a chair, sits down and gives you his full attention. He makes sure every box is checked off. That made us feel so good,” said Sandra.
Sandra and Bob are one of the many couples that have stayed committed to Dr. Heyl and the family practice across three generations of care.
In true Dr. Heyl fashion, he was very appreciative to be awarded this designation, but gave credit to his team for making his job so enjoyable. “To be successful in patient care today, it’s a huge team process. I think when I started there were 8 employees in our little practice here and now we have 44. It takes that many people to do what we do and to make it look [easy].”
Leadership such as this is exactly why Dr. Heyl and his family practice will continue to thrive and attract new patients in the Pittsburgh area. It is also why Dr. Heyl is truly an Everyday Hero. His passion, his dedication and his love for the profession help him exceed the standards of quality patient care. He doesn’t let other things get in the way of providing a high-quality experience, and that’s what brings people back.
He states, “Once you close that [exam room] door, nothing has changed. Maybe the things around it have changed - the insurance, - but once you close that door, you get to sit there with the patient and ask them how they are doing, what’s going on... It’s great.”
To learn more about Dr. Heyl and his longstanding practice, Heyl Family Practice, in West View and McCandless, visit their website at: https://www.genesismedical.org/location/ West-View-Office.



On Thursday, May 11, the ACMS Delegation met virtually for a Kickoff call. Dr. Richard Hoffmaster was introduced as the 2023 Chair and Dr. Bruce MacLeod was introduced as the 2023 Vice-Chair. Dr. Todd Hertzberg, Speaker of the House at the Pennsylvania Medical Society, provided an overview of the House of Delegates program and timeline, as well as some tips on the resolution process, comment periods, and parliamentary process. As a general note for all ACMS Members, resolutions are due by June 1, 2023. If you wish to put forth a resolution for the 2023 House of Delegates, please draft a resolution and submit that resolution to an elected Delegate who will submit it on your behalf. If you have any questions, please reach out to (shussey@acms.org)
Sara Hussey, ACMS Executive Director.
Are you interested in learning more about serving as a Delegate or Alternate Delegate? The Nominating Committee will be accepting nominations for Delegates and Alternates over the summer. To learn more about the requirements and time commitment, please reach out to Sara Hussey.


On April 27, 2023, the ACMS and the ACMS Foundation hosted ACMS Honors at the Heinz History Center. Over 125 ACMS members and community partners gathered to celebrate the achievements of many of our members, including the Top Physicians Under 40 from 2022 and 2023, as well as the 2023 Allegheny County Everyday Hero award winner, Dr. Louis Heyl.

We also heard from three of the local non -profit organizations who were awarded grant money from the ACMS Foundation in 2022. These organizations: Jeremiah’s Place, Beverly’s Birthdays, and Family House, shared the impact that grants from organizations, like the ACMS Foundation, can have on their ability to operate and run programs to support the community members.
Through the Qgiv donation site at the event, and donations received after the event, we raised over $9,000 for the ACMS Foundation. Those donations will help to fund at least one grant project in the 2023 year.
Thank you to all who attended and donated. If you were unable to attend but are interested in supporting the ACMS Foundation, please donate by scanning the QR code.

We are already looking forward to next year ’s event and we hope to see many more of our members and community partners in attendance in 2023.
To view pictures from the event visit the ACMS Facebook Page!
As physicians, you know that it takes a village to keep the community healthy and safe. Please consider a donation to the Allegheny County Medical Society Foundation.
Your donation will help the Foundation fund local non-profits in future grant cycles, and will help further the mission of the ACMS Foundation.
Donations can be mailed to: ACMS Foundation
850 Ridge Avenue Pittsburgh, PA 15212
Scan this QR Code to Donate via Qgiv:
 lisa geoRge, mPh, Ches—jeWish healthCaRe FounDation
lisa geoRge, mPh, Ches—jeWish healthCaRe FounDation
A significant step has been made toward establishing Pennsylvania Orders for Life-Sustaining Treatment (POLST) as law in the Commonwealth. On April 19, Senator Gene Yaw (R-23rd District) introduced Senate Bill 631, which would codify POLST for use by medical professionals across all health care settings to document treatment wishes for patients who voluntarily wish to execute a POLST order.
Although the bright pink POLST form has been used in Pennsylvania for decades to translate patients’ wishes for care into actionable medical orders, the lack of legislation on POLST has led to confusion and inconsistent use among providers. This bill aims to enhance clarity for providers regarding POLST usage and bolsters the protections for seriously ill patients to receive care that aligns with their care preferences regardless of the setting.
SB 631 amends Title 20 (Decedents, Estates, and Fiduciaries) of the Pennsylvania Consolidated Statutes, providing a legal basis for POLST forms to be used across care settings. It defines the appropriate population for POLST as “patients who are considered to be at risk for a life-threatening clinical event because they have a serious life-limiting medical condition, which may include advanced
frailty.” It also clarifies for whom POLST is not appropriate and describes the elements of a properly executed POLST order. The lack of existing legislation poses particular challenges to EMS providers, who are presently only legally authorized to honor the state’s Out-of-Hospital Do Not Resuscitate order and must call Medical Command for authorization to follow a POLST. This can lead to patients having to endure medical interventions at the end of life that do not align with their wishes. SB 631 would allow POLST to be recognized and acted upon across care settings, inside and outside the hospital, and grants emergency medicine personnel the authorization to honor patients’ documented preferences for care without the need for Medical Command Physician authorization.
Further, this bill emphasizes the importance of POLST as part of a shared decision-making process involving a discussion of current clinical status and care preferences between a patient or surrogate and health care provider. The POLST conversation provides patients with an opportunity to speak with their loved ones and their providers about their preferences for care they wish to receive and not to receive. It gives providers clear direction
regarding medical interventions, regardless of the care setting. Voluntary consent is essential, and patients have the right to refuse to execute a POLST, without consequences from a provider or insurer.
This bill also establishes a multistakeholder POLST Advisory Committee to advise the Pennsylvania Department of Health on POLST form revisions and POLST education.
POLST legislation is critical to ensure the appropriate use of POLST across the Commonwealth, in the appropriate populations, as part of a conversation about wishes for endof-life medical care. It will benefit providers by contributing greater clarity and guidance on the POLST process.
Read the full text of SB 631 here. To voice your support for SB 631, contact your state senator. The Pennsylvania Medical Society supports this legislation and has launched an easy-to-use online form that allows you to contact your senator with just a few clicks.
If you haven’t checked out the PA POLST Learning Center a library of on-demand trainings on POLST—all of which offer free continuing medical education and continuing nursing education credits. Please consider sharing with your staff to ensure they are educated on proper POLST use.
To stay up to date on POLST legislation, education, and resources, subscribe to the POLST Notes newsletter. Visit www.papolst.org to sign up. For more information or answers to your questions about POLST, contact info@papolst.org.
Lisa George, MPH, CHES PA POLST Coordinator Senior Communications and Program Specialist Jewish Healthcare Foundation













The Allegheny County Medical Society and the PA Medical Society are both endorsing the recent letter from The Pennsylvania Cancer Coalition on HPV Prevention.



February 22, 2023
Dear Pennsylvania Health Providers, Nationally, the Human Papillomavirus (HPV) is estimated to cause about 37,300 new cases of cancer each year.1
February 22, 2023
Dear Pennsylvania Health Providers,
Nationally, the Human Papillomavirus (HPV) is estimated to cause about 37,300 new cases of cancer each year.1
We have an opportunity to eradicate HPV-associated cancers, and yet too many people are not getting this safe and effective vaccine that prevents six different cancers associated with HPV which include oropharyngeal cancers and approximately 91% of cervical cancers.2 In Pennsylvania (PA) oral pharyngeal cancer incidence has been trending up since 2005 for males and females of all races. It is now the 8th most diagnosed cancer in PA males and 11th for females.3
We have an opportunity to eradicate HPV-associated cancers, and yet too many people are not getting this safe and effective vaccine that prevents six different cancers associated with HPV which include oropharyngeal cancers and approximately 91% of cervical cancers.2 In Pennsylvania (PA) oral pharyngeal cancer incidence has been trending up since 2005 for males and females of all races. It is now the 8th most diagnosed cancer in PA males and 11th for females.3
A nine-valent HPV vaccine (HPV9) is available to protect against multiple strains, including HPV 16, 18, 31, and 33, the types that cause most cervical and other anogenital cancers, as well as some oropharyngeal cancers. The HPV vaccine is approved for ages 9 years through 45 years for ALL GENDERS. The American Cancer Society (ACS) and American Academy of Pediatrics (AAP) recommend vaccination at age 9, and many Pennsylvania’s vaccine advocates are leading this charge, including the Pennsylvania Chapter of the AAP.
A nine-valent HPV vaccine (HPV9) is available to protect against multiple strains, including HPV 16, 18, 31, and 33, the types that cause most cervical and other anogenital cancers, as well as some oropharyngeal cancers. The HPV vaccine is approved for ages 9 years through 45 years for ALL GENDERS. The American Cancer Society (ACS) and American Academy of Pediatrics (AAP) recommend vaccination at age 9, and many Pennsylvania’s vaccine advocates are leading this charge, including the Pennsylvania Chapter of the AAP.
In Pennsylvania, only 68.7% of adolescents age 13-17 are fully vaccinated against HPVassociated cancers.4 Nationally, approximately 27% of men and 53.6% of women between the ages of 18–26 are vaccinated.5 In rural communities, HPV vaccination rates are low, yet incidence and mortality rates of HPV-associated cancers are high.6 The HPV vaccination rate for Pennsylvania adolescents living in non-urban geographic locations drops to an alarmingly low rate of 48.7% compared to the 95.75 rate for ≥ 1 dose MenACWY.7
In Pennsylvania, only 68.7% of adolescents age 13-17 are fully vaccinated against HPVassociated cancers.4 Nationally, approximately 27% of men and 53.6% of women between the ages of 18–26 are vaccinated.5 In rural communities, HPV vaccination rates are low, yet incidence and mortality rates of HPV-associated cancers are high.6 The HPV vaccination rate for Pennsylvania adolescents living in non-urban geographic locations drops to an alarmingly low rate of 48.7% compared to the 95.75 rate for ≥ 1 dose MenACWY.7
We need to address the public health issue and the burden of cancer related to the low HPV vaccination rates of Pennsylvania adolescents and adults. Provider recommendation for the HPV vaccine is considered the most effective determinant of vaccine uptake compared to other interventions such as parent education.
We need to address the public health issue and the burden of cancer related to the low HPV vaccination rates of Pennsylvania adolescents and adults. Provider recommendation for the HPV vaccine is considered the most effective determinant of vaccine uptake compared to other interventions such as parent education.

PA has partnered with our neighbors, MD, WV, OH, VA, DC and DE in a multi-state Callto Action to increase HPV vaccination by strong and consistent provider recommendations and initiation of HPV vaccination starting at age 9. HPV vaccination is cancer prevention!
PA has partnered with our neighbors, MD, WV, OH, VA, DC and DE in a multi-state Callto Action to increase HPV vaccination by strong and consistent provider recommendations and initiation of HPV vaccination starting at age 9. HPV vaccination is cancer prevention!
1 https://www.cdc.gov/cancer/hpv/statistics/cases.htm https://www.cdc.gov/cancer/hpv/statistics/cases.htm
2 https://www.cdc.gov/cancer/hpv/statistics/cases.htm
3 Pennsylvania Cancer Registry. 2019 Data Set
4 https://www.cdc.gov/vaccines/imz‐managers/coverage/teenvaxview/data‐reports/index.html
1 https://www.cdc.gov/cancer/hpv/statistics/cases.htm
https://www.cdc.gov/cancer/hpv/statistics/cases.htm
5 McElfish PA, Narcisse MR, Felix HC, Cascante DC, Nagarsheth N, Teeter B, Faramawi MF. Race, Nativity, and Sex Disparities in Human Papillomavirus Vaccination among Young Adults in the USA. J Racial Ethn Health Disparities. 2021 Oct;8(5):1260‐1266. doi: 10.1007/s40615‐
2 https://www.cdc.gov/cancer/hpv/statistics/cases.htm
3 Pennsylvania Cancer Registry. 2019 Data Set
020‐00886‐5. Epub 2020 Oct 8. PMID: 33033889; PMCID: PMC9753349.
4 https://www.cdc.gov/vaccines/imz‐managers/coverage/teenvaxview/data‐reports/index.html
6 Brandt HM, Vanderpool RC, Pilar M, Zubizarreta M, Stradtman LR. A narrative review of HPV vaccination interventions in rural U.S. communities. Prev Med. 2021 Apr;145:106407. doi: 10.1016/j.ypmed.2020.106407. Epub 2021 Jan 1. PMID: 33388323.
7 https://www.cdc.gov/vaccines/imz‐managers/coverage/teenvaxview/data‐reports/index.html
5 McElfish PA, Narcisse MR, Felix HC, Cascante DC, Nagarsheth N, Teeter B, Faramawi MF. Race, Nativity, and Sex Disparities in Human Papillomavirus Vaccination among Young Adults in the USA. J Racial Ethn Health Disparities. 2021 Oct;8(5):1260‐1266. doi: 10.1007/s40615‐
020‐00886‐5. Epub 2020 Oct 8. PMID: 33033889; PMCID: PMC9753349.
6 Brandt HM, Vanderpool RC, Pilar M, Zubizarreta M, Stradtman LR. A narrative review of HPV vaccination interventions in rural U.S. communities. Prev Med. 2021 Apr;145:106407. doi: 10.1016/j.ypmed.2020.106407. Epub 2021 Jan 1. PMID: 33388323.
7 https://www.cdc.gov/vaccines/imz‐managers/coverage/teenvaxview/data‐reports/index.html
Set your electronic health record notifications from age 9 years through 45 years for men and women. Initiating the HPV vaccination at age 9 has been shown to increase vaccine completion by 22 times.8
Make a strong recommendation for HPV vaccines for all patients ages 9 years through 26 years. Data shows that your recommendation may improve vaccinations by up to 5 times.9
For adults age 27 years through 45 years, engage in shared decision to help determine the benefits of vaccination.
Vaccination recommendation should be made in all healthcare settings to include acute, non-acute, GYN, and dental locations.
Encourage same day vaccination in your facility.
Review your patients who have not completed their 2 or 3 dose series and proactively recall patients to your facility.
Review vaccination status at every visit- not just well checks.
Check adult patients through age 45 to ensure they have completed their HPV series.
Identify an immunization champion at your facility.
Implement standing orders which can be found at Vaccine Standing Orders for Healthcare Providers (immunize.org).
Vaccines for Children Program (VFC), provides free HPV vaccines for all kids enrolled in Pennsylvania Medicaid or who have no insurance. The HPV vaccine is a covered benefit for insurances through age 26. Over 95% of insurance cover ages 26 years through 45 years with share decision making which can be documented with an e-prescription / prescription.
Please review the resources and links at the end of the letter. Thank you for all that you do to improve the health of your patients and for your participation in this important effort to prevent cancer by increasing the uptake of HPV vaccination in Pennsylvania.
Sincerely,


ALL MEETINGS BEGIN AT 6:00 PM
No upcoming events Executive Committee*
Tuesday Evenings—2nd Tuesday at the start of each new quarter.
July 11, 2023
October 10, 2023
Committees
Delegation
Nominating
ACMS Foundation
Finance Committee
Tuesday Evenings
August 29, 2023
November 14, 2023
Board of Directors*
Tuesday Evenings
September 12, 2023
December 5, 2023
Dates to be announced
June & August
May, August
June 13, 2023 Prep for Grant Proposals
October 24 Grant Proposal Review
PAMED BOARD
May 4
August 3
AMA Interim Meeting
AMA Annual Meeting
PAMED HOUSE OF DELEGATES / HERSHEY
October 27-28, 2023
October 26-27, 2024
AMA HOUSE OF DELEGATES
June 10-14 Chicago, IL
November 11-14 National Harbor, MD
June 2024 Chicago, IL
ACMS
February
June
July 4—Independence Day