DIALOGUE DERM
m
Editor: Norma White-Weithers, MS, DVM, DACVD • Veterinary Allergy & Dematology Consultant, Baldwin, NY 11510

Work: 646-329-4719 • Fax: 631-694-3401 • E-mail: nweithers@yahoo.com
Assistant Editor: Tim Strauss, DVM • Frederick,CO 80516 | E-mail: drtim@comcast.net

FROM THE PRESIDENT
Dear Colleagues,
It is hard to believe that this was our first meeting back in person in New Orleans. After a 2 year hiatus from our Annual Meeting, I enjoyed seeing all of my fellow members of AAVD, ACVD and NAVDF speaking about hot topics, trends and tacks withing the veterinary scope. Walking the exhibit hall was interactive with enthusiastic exhibitors who were equally excited to move back to in person, while continuing to do our best to remain safe while navigating the pandemic.
Many thanks to the NAVDF organizing and programming committees for making this event a success. I would also like to welcome the members of the executive committee into their new positions and thank them for their efforts on behalf of the AAVD. I am excited to serve as president of the Academy and follow in the footsteps of my mentor, Dr. Klaus Loft. At the executive meeting, we brainstormed about how to grow the Academy including the development of student groups at veterinary schools and a membership option for students and technicians. We also discussed utilizing the AAVD social media to continue to engage with the membership. I encourage the membership to reach out to me, or any member of the executive board, with your ideas. Our e-mail is info@aavd.org. This is your organization, and we welcome any ideas you would like to see from the board.
Recipients for 2020-2022 will were recognized at Saturday’s Annual General Business Meeting. Dr. Outerbridge presented the award to 2020 recipient Dr. Stephen White. Dr. Scott presented the award to 2021 recipient Dr. Patrick McKeever. Dr. Amanda Burrows is the recipient for 2022, though she is not in attendance at NAVDF. Dr. Outerbridge made the announcement regarding Dr. Burrows’s award. Board members were encouraged to share any photos they may have of past award presentations or general photos of past award recipients for inclusion on the AAVD website.
Last, I would like to take this time to dedicate this Derm Dialogue to the late Dr. Dunbar Gram. Dr Gram was a special member of our community, and he was always pushing to make all the veterinary dermatology great. He was an accomplished clinician and professor, and he will continue to be greatly missed.

Sincerely,
Rose Miller, DVM, DACVD
AAVD President 2022-2023
Dr. Dunbar Gram
Rose Miller, DVM, DACVD
FALL 2022
AAVD Executive Board
President Dr. Rose Miller Coeur d’Alene, ID Immediate Past-President Dr. Klaus Loft Boston, MA
Vice President Dr. Verena Affolter Davis, CA
Treasurer Dr. Anna Jenstead Madison, WI
Members-at-large
Dr. Brian Scott Largo, Florida
Dr. Natalie Theus Columbus, Ohio
Dr. Jennifer Thomas Stillwater, OK
WAVD Representative Dr. Jeanne Budgin New York, NY
Editor, Derm Dialogue
Dr. Norma White-Weithers Baldwin, NY
Executive Secretary
Amy Blankenhorn Association Coordinator II
Meeting Planner
ktravitz@pamedsoc.org
Administrative Assistant Jill Bennish, jbennish@pamedsoc.org
NAVDF Program Committee
NAVDF-OC Committee
Positions
Program Chair
Dr. Sandra Koch Co-Chair
Dr. Klaus Loft
Dr. Petra Bizikova Dr. Alberto Cordero Dr. Gram Dunbar Dr. Brian Scott
WAVD Committee
AAVD Representative to the WAVD Dr. Jeanne Budgin
Term Name Affiliation Email
Chair 2021-2023 Dr. Rose Miller AAVD RMillerdvm@gmail.com Co-Chair 2021-2023 Dr. Kristin Holm ACVD Kshdvm@yahoo.com
Treasurer 2021-2023 Dr. Allison Kirby ACVD Alliekirby@yahoo.com
Social & 2021-2023 Dr. Dana Liska ACVD Danaliskadermvet@gmail.com Sponsorship Chair
Social & Sponsorship 2018-2023 Dr. Klaus Loft AAVD Klausloft@gmail.com Co-Chair
OC Mbr AAVD 2019-2023 Dr. Norma White Weithers AAVD Nweithers@yahoo.com
OC Mbr AAVD 2021-2024 Dr. Anna Jenstead AAVD A Jenstead@gmail.com
OC Mbr ACVD 2020-2024 Dr. Lindsay McKay ACVD Lindsay.mckay@vca.com
OC Mbr ACVD 2021-2025 Dr. Melissa Eisenschenk ACVD melderm@gmail.com
3 7
2 DERM DIALOGUE
Overview of Staff and Leadership
ROUNDTABLE SUMMARIES
ROUND TABLE: EQUINE SARCOIDS
Moderator: Sandra Koch, DVM, MS, DACVD
OBJECTIVE: Discuss knowledge and experiences with the diagnosis and treatment of equine sarcoids.
Participants: there were a total of 6 people present (including the moderator): 3 veterinary dermatologists from academia, one veterinary dermatologist from a private institution and 2 veterinary dermatology residents,
Introduction: There was consensus among the participants that equine sarcoids should be taken more seriously among the veterinary and horse owner communities. Equine sarcoid is cancer! Even though not metastatic, it can be locally aggressive. Unfortunately, there are very few good randomized controlled studies to support treatment decisions.
Types - What type of sarcoids do you see more commonly in your practice?
• Mixed
• Nodular (more donkeys and mules)
• Occult and mixed
Diagnosis - How do you diagnose sarcoids? Clinical diagnosis only? Other tests?
• Based on clinical signs in some cases
• Occult: fungal culture, biopsy for alopecia areata
• Rule out other diseases fist according to each case (skin scrapings, trichogram/fungal culture, fine needle aspirate/cytology and biopsy
Biopsy - There are controversies regarding biopsy of sarcoids due to some belief that biopsy will make sarcoid worse or more aggressive. Do you recommend biopsy? Regardless of the type?
• Not always – does not think it always become a problem
• No. Worried that may get worse in some cases
• Biopsy sometimes
• One occult that got worse but not really bad
• Yes. Earlier better as chronicity can affect biopsy results
Age - Do you believe that older horses generally have more problematic sarcoids than younger horses?
• I do not know
• No
• No
Body location - Do you believe that sarcoids in different body locations behave differently?
If so, what locations are the most problematic in your experience?
• Yes. Areas that can be traumatized, saddle, limb, flank, and neck.
• Yes. Genitalia
DERM DIALOGUE
Continued on page 4 3
ROUNDTABLE SUMMARIES
Do you always treat? Benign neglect for flat or occult sarcoids?
• One person does not always treat
• Other two people treat based on each case client’s interest/decision
Size - Do you believe that small sarcoids are more likely to respond to “appropriate” therapy than large sarcoids?
• Smaller are easier to treat but may not necessarily respond better
• Very thick, nodular and fibroblastic sarcoids may not respond well to topical therapies
Chronicity - Do you believe that chronicity affects response to therapy? In other words, “new” sarcoids (ones that have not been in place very long) are more likely to respond to “appropriate” therapy than those that have been there for extended periods of time?
• For fibroblasts perhaps
• New sarcoid may respond better because they may have not been treated before
• It may also matter what may have been tried before as far as treatment
• Treatment may make the tumors look worse
How much consideration do you give to the following when selecting therapy? Animal
compliance, owner compliance, costs, duration of treatment, other
factors/logistics
It seems like all these factors play a role in sarcoid management. Horses that are trailed to hospitals might be different to manage compared to horses that veterinarians attend to at the barn/farm, which would involve all aspects above.
What are the most common types of sarcoid treatment you use in your practice and which ones you have most success with?
• Imiquimod on occasions and surgical excision followed by cisplatin or just cisplatin
• Imiquimod first choice, surgical removal, or electrochemotherapy with injectable cisplatin or cisplatin – mostly for nodular and fibroblastic, some cases of autologous implantation
• “SMART surgery” technique important – change everything in between removal and closure
• 5FU – one good positive experience in a mixed sarcoid
• Acyclovir – positive response in one case with occult sarcoid
• Retinoid - vitamin A?
• BCG not in US?
What treatment has not worked based on your experience?
• One person does not like 5FU or X-terra
• One person sends cases to oncologist for treatment so no experience with therapies
DERM DIALOGUE
Continued from page 3 4
ROUNDTABLE SUMMARIES
CANINE SOLAR DERMATITIS/ ACTINIC KERATOSIS ROUNDTABLE
Moderator: Jacqueline Gimmler, DVM, MS, DACVD
1. Attendees included board-certified dermatologists from multiple countries, general practitioners, residents, and veterinary technicians.
2. What is Solar Dermatitis = inflammation of skin from sunlight
a. Actinic reaction on white/ light/ damaged skin not sufficiently covered by hairs is exposed to chronic sunlight.
b. Actinic = exhibiting chemical changes produced by radiant energy especially in the visible and ultraviolet parts of the spectrum
3. Pathogenesis
a. Background on UV light
i. UVB (290-320 nm wavelength) is sunburn/ erythema spectrum (“phototoxicity”). UVA (320-400 nm) penetrates deeper, cause of photosensitivity reactions
b. UV light that penetrates natural barriers is absorbed by chromophores (light-absorbing molecules) in the skin = melanin, keratin, blood, hemoglobin, porphyrin, carotene, nucleic acids, lipoproteins, peptide bonds, and aromatic amino acids (tyrosine, tryptophan, histidine)
c. Absorbing UV light raises energy level of chromophores; beyond a certain point of prolonged repeated sun exposure, chromophores are no longer able to scavenge free radicals, and ends up releasing free radicals: superoxide radical (O2-), hydrogen peroxide (H2O2), and hydroxyl radical (OH) i. results in biochemical processes that damage cell components. Causes hyperproliferation, mutagenesis, alteration of cell surface markers, and toxicity.
ii. Cellular changes: Vacuolated keratinocytes in superficial epidermis (sunburn cells), Apoptotic keratinocytes (w/in 4 hours from direct damage of cell membrane; after 24h from DNA alteration), vascular dilatation and leakage, depletion of Langerhans & mast cells
iii. Increase in tissue histamine, prostaglandins, leukotrienes, inflammatory cytokines, adhesion molecules, and reactive oxygen species = PROINFLAMMATORY STATE OF SKIN
d. Factors that influence
i. Natural barriers: length and thickness of fur ii. Amount of melanin in skin iii. Length of daily sun exposure
iv. Time of day: light most intense 11am-2pm
v. Sunny climate
vi. Altitude: for every 300m increase in elevation, sun intensity increases by 4%
4. Which Breeds are mostly affected:
a. White, short-haired, big dogs (outside more): PitBull, American Bulldog, Dogo Argentino, Bull Terrier, English Bulldog, Boxer, Chihuahua
b. Canine Nasal Solar Dermatitis: Australian Shepherd, any dog with depigmentation/ scarring of nasal area
i. No attendees have actually seen this presentation. There were some attendees wondering whether this presentation was a presentation of dermatomyositis, DLE, or Pemphigus Erythematosus that had been misclassified as nasal solar dermatitis.
DERM DIALOGUE 6
5
Continued on page 6
ROUNDTABLE SUMMARIES
c. Others: Dalmatians, Hound dogs, GSP, whippet, beagle
d. Not usually seen in thick-coated white dogs, even ones that live 100% outside: Great Pyrenes, herding dogs
i. One attendee has seen solar lesions on the more sparsely haired regions of the face of thick-coated dogs with a dermatoscope
ii. Solar glossitis has been reported in sled dogs!
5. Lesion distribution:
a. Canine Nasal Solar Dermatitis:
i. erythema & alopecia on bridge of nose, depigmentation, ulceration, crust on dorsal nasal planum
b. Canine Solar Dermatitis of Trunk & Extremities
i. Alopecia, erythema, scale, thick white-pink scars (burn victim), comedones, papules, purple furuncles, draining tracts, ulcerations
ii. Only white skin affected (if black/brown spotted breed, that skin is normal)
iii. Body site: flank & abdomen, or sometimes primarily right or left side of body (preference for side laying when sunbathing)
iv. Often concurrent hemangiomas or cutaneous hemangiosarcoma
c. Sometimes concurrent non-healing ulcerations (concern for squamous cell carcinoma)
6. How to diagnose
a. Biopsy & Histopathology
i. Early depigmented nose: fewer melanocytes, less melanin pigment
ii. Epidermal hyperplasia w/ intraepidermal edema; vacuolated (sunburn cells) apoptotic keratinocytes; superficial perivascular dermatitis; deep vascular dilatation; solar elastosis (basophilic degeneration of elastin) needs special stains (periodic acid-Schiff, PAS); bandlike superficial dermal fibrosis; ulceration
iii. Actinic folliculitis, actinic follicular cyst formation, dermal fibrosis
b. Presumptive diagnosis based on consistent lesions on white skin
i. Many attendees use this option, only biopsy non-healing lesions, or biopsy for histopathology only if they’re also performing biopsy for a deep tissue culture.
7. How to treat
a. Sunlight avoidance: stay inside, build shade cover, body suit
i. Sunscreen: many attendees use
1. Sport spray for humans
2. Sunscreen Stick for babies with less fragrance
3. Dermoscent spf 40, mineral; pH for dog skin
ii. Nose cover
1. Dog nose protectors (best for after topicals) or sun shade
iii. Skin 2 is a paint-on pigment, doesn’t stick to mucosa, comes in pink and black. You wait until it dries them powder it. Total opaque spf 1200, can last 1-7 days. Popular in Australia.
1. Previously utilized tattoo ink does not actually provide UV protection because it’s too deep; not recommended any longer.
iv. If patient sunbathes by windows, put a 3M filter on the screens to filter out UVB
v. Body suits for UV protection
1. Made to fit body suits- custom tailoring (Gremelie?)
2. K9 topcoat
9 DERM DIALOGUE 9
6
Continued from page 5 Continued on page 7
ROUNDTABLE SUMMARIES
3. Latin America has body suits made of fabric with copper fibers that are also antimicrobial
b. Culture & antibiotics for deep pyoderma
i. Biopsy of macerated deep tissue for cultures, then a biopsy for histopathology is more justified
c. Steroids for furunculosis
i. Many use steroids
ii. Many use NSAIDs instead and see a good response
d. Vitamin A to normalize epithelial turnover, 8,000-10,000 per dog per day.
i. Concern for dry eye (Keratoconjunctivitis sicca, KCS)
1. Rare but many monitor for it (monthly)
2. Pet owners can do it themselves if trained, give them the package (for good dogs)
ii. Start daily, can taper to 3x weekly
iii. Iams study, almost impossible to overdose Vit A and get hepatotoxicity like humans
iv. Beta carotene (30mg BY MOUTH TWICE DAILY) mentioned in textbook as precursor to Vit A; no one has used this
e. Imiquimod (Aldara)- most reserve for cancerous lesions
f. Surgical excision
g. Phovia?
i. Not advised since increases skin growth and this is already a disease of increased epidermal turnover
ii. Successful in perianal fistulas and even dermatophyte in dogs!
8. Actinic Keratosis
a. Caused by UV light, occur in lightly haired/ lightly pigmented areas
b. Single or multiple, ill-defined erythema, hyperkeratosis, and crusting, to indurated, and hyperkeratotic plaques from 0.3-5cm diameter
c. Breeds: Dalmation, American Staffordshire terrier, beagle, basset hounds, bull terriers
d. Histopathology: atypia and dysplasia of epidermis and superficial follicular epithelium, hyperkeratosis (para), and occasionally solar elastosis of underlying dermis.
e. Premalignant lesions, capable of transforming to invasive SSC
f. Treatment
i. Early lesions regress w/ sunlight avoidance & photoprotection
ii. Topical/ oral steroids help w/ pruritus/ pain
iii. More advanced lesions: topical imiquimod, systemic retinoids, cryosurgery, or surgical excision
9. Other thoughts
a. DermLite- human dermatoscope is great for seeing smaller or more subtle lesions b. Kitoscell cream- good for fibrosis, keloid scars cuts down, topical, very cheap
c. Eryfotona AK-NMSC- from lab in Spain, cell regenerator to help DNA recover, lotion/cream
d. Cryosurgery
i. Can use acne aperture to spray larger areas
ii. For small lesions, really fast so no numbing or sedation needed
iii. If big area, send nsaid afterward
e. 5-fluorocil (5-FU)- call antimetabolite, causes inflammation that destroys bad cells; expensive; toxic if ingested
f. NSAID
9 DERM DIALOGUE 9
7 Continued on page 8 Continued from page 6
ROUNDTABLE SUMMARIES
i. Solaraze (diclofenac)- topical nsaid
ii. Previcoxx or others
g. Evan likes a combo of Vit A, Vit E, Meloxicam, sometimes pentoxifylline
i. Very cost effective
h. CO2 laser- for pinpoint hemangiomas, need for anesthesia
i. Topical lidocaine jelly, put on 3-4 times every 15min before procedure with no sedation in good dog
ii. Some do a broad spray to vaporize and thin out large areas
i. Topical timolol TWICE DAILY gel or drops (cheap)- shrinks small hemangiomas (may decreased heart rate in cats with less effect on glaucoma)
i. Also, ultrasound the spleen because maybe skin hemangiomas are mets from spleen
ii. Steroids & cyclosporine
iii. Pentoxifylline helps too
j. Zinc for very scaly dogs
k. Cold Plasma can help too
l. Systemic retinoids- hard to find i. Bloodwork to start, recheck 1 month later; lots of problems not seen.
ii. Isotretinoin, cheap in Australia
iii. Can get compounded in US, must have pharmacist, doctor, and person saying you won’t get pregnant
iv. Differin gel- schnauzer comedones, 3x weekly
10. So often damage is already done in early life and now we’re dealing with it years later a. When seeing younger white dogs, we need to warn them about sun damage
11. Also talked about white dogs with furunculosis of face, legs, etc.
a. Related to atopic dermatitis or short-coated folliculitis?
9 DERM DIALOGUE 9
8 Continued from page 7
ROUNDTABLE SUMMARIES
CANINE PEDAL FURUNCULOSIS
Moderator: Amelia G. White, DVM, MS, DACVD®
What are the etiologies that you have seen that contributed the most?
Allergy Conformation
Breed Hair coat
Trauma
Exercise Obesity
Musculoskeletal disease
How to work through this:
Set appropriate client expectations. Recommend surgery and orthopedic evaluations. Diet. Establish routine hygiene plan. Use steroids for maintenance at least topically.
Many people agree this condition probably starts as a sterile process progressing to secondary bacterial infection, which explains why it responds so well to steroid therapy
When working these up, how many people rely on FNA/cytology vs culture? How do you decide? Depends on what stage of disease they are in.
In early cases it is important to set client expectations early, especially communicating that they will need to keep the paws clean for life.
Some participants agreed that biopsy for aerobic culture and histopathology to establish a clear diagnosis at the onset of disease/referral can be useful to rule out other conditions and direct antibiotic selection (when appropriate).
Many dermatologists agree that these cases are chronic when they arrive for initial evaluation and systemic antibiotics to treat secondary deep infection may be warranted. However, when the disease flares down the road, most people do not repeat culture or histopathology and instead use topical therapy approaches and systemic anti-inflammatory medications, particularly glucocorticoids, to stop the flare.
Sometimes clients prefer to focus on wanting pet to just feel better acutely, so veterinarians need to: -Understand and work with client expectations along with setting clear, realistic client expectations that long-term care plan need to be established as soon as possible (e.g., workup underlying disease and conditions, paw cleaning, etc.)
-Helping clients understand what is considered “improvement” especially long-term since these dogs’ paw will never be “normal” and flare ups are common
It seems that some dogs have generalized furunculosis (all digits, all paws) vs localized disease (e.g., dogs with musculoskeletal disease).
9 DERM DIALOGUE 9
9 Continued on page 10 Continued from page 9
ROUNDTABLE SUMMARIES
How do you prefer to manage these cases?
Is your approach different based on severity and extent of disease, and how often do you use antibiotics?
Depends on history, but most of cases veterinary dermatologists agreed they are not using systemic antibiotics since these lesions always seem to get better with steroid or other anti-inflammatory therapy
Culture - some prefer FNA collection technique unless planning to biopsy for histopathology (worried here about wound healing in these lesions anyway, and unnecessary trauma to the history).
Histopathology - some veterinary dermatologists only biopsy if they think it is something other than furunculosis (e.g., neoplasia) - example of a ruptured sebaceous gland deep in dermis leading to clinical furuncle; nodular form of cutaneous lymphoma; nodular fungal pododermatitis; etc.)
Medications to be most effective? Topical and systemic?
Nutritional modification: Metabolic Mobility due to high level of omega fatty acids, limited ingredient diets even when it clearly is atopy (role of anti-inflammatory, low allergen diets to reduce food associated atopy flares)
Steroids: the group agreed that steroids are most effective to make lesions resolve quickly and prevent recurrence. Many people discussed the need to transition to lower systemic doses of steroids over time and rely more heavily on routine hygiene therapy with topical steroids or topical tacrolimus
Modified cyclosporine (Atopica®) - group feels this is highly effective treatment option, but it does not work acutely to provide relief. This is a good long-term plan option along with topical hygiene therapy. The group speculated this may be because it is similar in some aspects of SGPS, and cyclosporine is an effective treatment option for nodular immune-mediated dermatoses.
Oclacitinib (Apoquel®) - group feels it has varied efficacy and does not feel that it causes or contributes to the development of this disease; group does not feel it is as effective for this condition as compared to steroids and Atopica®. The group speculated that it may be more effective with off-label use (higher dose), early and/or mild disease, and in dogs with atopy as etiological component. The group mentioned that Apoquel® may have better outcomes when combined with topical steroids or tacrolimus, especially in allergic dogs.
Lokivetmab (Cytopoint®) – the group unanimously agreed this is not an effective treatment option.
Topical therapy
0.1% tacrolimus – overall the group reported limited success with this therapy. One member reported better successes as a long-term management tool after getting disease under control or in cases with focal/localized disease (e.g. maintain hygiene and use topical tacrolimus).
Frequency of application of tacrolimus use: start it at twice daily, then reduce to once daily to EOD therapy long term
Care giver burden was discussed. Specifically, many people reported that owners experience fatigue with continuing topical treatments/hygiene long-term and let treatments and hygiene lapse, resulting in disease flare.
Pentoxifylline – some reported it may be beneficial adjunctively, especially in scarred cases, bulldog breeds, as well as cases requiring antibiotics.
9 DERM DIALOGUE 9
10 Continued on page 11 Continued from page 9
ROUNDTABLE SUMMARIES
Steroids – many veterinary dermatologists reported that they used topical steroids during acute flares and as maintenance care. These commonly include Synotic and mometasone. Steroids are used daily initially and then reduced in frequency. Creams were preferred (not as messy and clients can see the drug going onto the skin). Many people educate clients on the maximum amount per week as maintenance, which is safe to use, and many report that skin atrophy is not likely when, don’t see a lot of issues with thinning probably because clients with use 2-3x/week long-term (compliance improved with less frequent administration).
Cleaning therapy - wipes, Dawn dish soap to degrease and remove keratinous debris as pre-shampoo, medicated shampoos (chlorhexidine-based products preferred)
Mupirocin and use of topical ear medications were mentioned and many report that they use these as well. Several veterinary dermatologists commented that chronic use of topical antibiotics should be limited due to the concern about resistance to antibiotics.
Managing Pain
The group agreed that steroids seem to be the most effective to acutely relieve pain and discomfort from the inflammation.
Gabapentin as an adjunct therapy is recommended, which may be more impactful in cases with underlying musculoskeletal or neurologic etiologies.
Nocita® (bupivacaine liposome injectable suspension) may be useful to promote complete analgesia of the paw as compared to short-acting 2% lidocaine blocks (expense of Nocita® in large dog may be limiting factor).
This could be additionally beneficial when performing biopsy of the paw lesions for histopathology or culture, or in cases of CO2 laser removal.
Laser therapy: therapeutic lasers vs CO2 lasers vs Phovia
Some people report using CO2 surgical laser for single lesions that will not resolve with medical therapy, or in cases that need fusion podoplasty
Therapeutic lasers were thought to have little to no effect
Experience with the use of Phovia was limited in the group, but some reported it to be beneficial in addition to traditional therapeutic approaches.
Surgical fusion podoplasty - how do you feel about this and what do your surgeons typical advice?
Many veterinary dermatologists reported that veterinary surgeons do not typically like to perform this procedure as a treatment for this condition. Instead, they prefer to wait until a false paw pad develops and covers the area, or they simply refer them back to the veterinary dermatologist to manage medically.
9 DERM DIALOGUE 9
11 Continued from page 10
OTITIS
Moderator: Paul Bloom. DVM. DACVD
Nine people were present. 2 from GP, 1 from the university, 1 from industry, 5 from referral practice We first discussed an article in Vet Record that 1 of the participants had published concerning the use of compounded burrows w/betamethasone .1%. He compared using the burrows with Surolan. The cure rate was 65% for burrows and 59% for Surolan with the conclusion that burrows was non inferior to Surolan. We next discussed how people had owners instill medication into the ears. All but 1 participant uses a 1 cc syringe for owners to measure out medication to put in the ear. Volume was dependent on the size of the animal ranging from 0.2- 1.0 cc usually bid. 1 participant only uses ointment so has the owner instill enough medication to hear it squish when the ear canal is massaged.
We then discussed ear cleaning. 2/3 of the participants have owners use ear cleaner at home- some during the treatment phase and others only during maintenance. Some used products that were “ceruminolytic” and others used cleaners that also contained steroids.
We then discussed the difference between ear cleaner and ear flush. We determined that the difference was the ingredients, with the former used for supposed ceruminolytic activity while the latter was to deliver active drug (EDTA, antibiotic, steroid) in large volume. During this discussion a couple participants reported reaction to pHnotix while used in the clinic. One said that dogs developed pinna erythema and another reported that some dogs hypersalivated (thought it may be from the lemon smell from the product).
We then discussed the requirement of determining the status of the tympanic membrane before dispensing medication or before discontinuing treatment. It was agreed that the status of the TM didn’t prevent or alter the medication that was dispensed. It was also agreed that status of the TM at the end of the treatment was unimportant as long as the dog was clinically normal.
Discussion of myringotomy was then discussed. 4 participants only did myringotomies if otitis media was confirmed based on CT while 1 participant only does a myringotomy if the tympanic membrane was unhealthy enough that it would rupture when touched with a red rubber tube. It was next discussed how to culture the middle ear. Most of the participants who culture the middle ear used a red rubber tube w/a small amount of saline to help collect material.
We then discussed using systemic antibiotics for OM. All but 1 participant used it, usually based on culture for 4-8 weeks. It was discussed that the length of time used was arbitrary and unless a repeat CT was performed +/- myringotomy you could not be certain that the OM had resolved. One participant reported resolving OM with aggressive tympanic cavity flushing and then instilling a mixture that contains 4 oz of TrizEDTA/ Dex SP (120 mg= 0.1%) with either gentocin (360 mg), amikacin (1200 mg) or baytril (12 cc of LA baytril – 100 mg/ml). The ear is then treated with the triz mixtue bid and some otic ointment depending on which antibiotic is being used in the triz mixture. Note that in the past this person would infuse under sedation w/a red rubber tube the triz mixture q 3 d x 4 weeks but then went to q 7 d x 4 weeks and now does not repeat the infusion.
Lastly a participant from Brazil reports that she has over 100 cases of cholesteatomas primarily in pugs and frenchies (and 5 cats) and will be writing it up
Three participants routinely do CT on all ears or on all ears before deciding to do a myringotomy. The remaining people usually did not do one unless the TM looked very abnormal (like it was ready to rupture)
As a comment I found it very interesting the large variation on how ears are treated yet everyone seems to have the same success rate!
9 DERM DIALOGUE 9
12
ROUNDTABLE SUMMARIES
ROUNDTABLE SUMMARIES
RETIREMENT FROM PRACTICE…WHAT’S IT LIKE? WILL I STILL BE RELEVANT?
HOW DO I KEEP UP TO DATE?
Moderator: Candace Sousa. DVM, DACVD
Participants
1. Kidney, Carolyn
2. Lewis, Diane
3. Meadows, Richard
4. Nagle, Terry
5. Preziosi, Diane
6. Rothstein, Emily
7. Lewis, Tom
8. Schmeitzel, Lynn
The session was conducted as a traditional roundtable discussion, rather than a workshop. Participants related their current professional status – still working (as employees in practice or at a university, sole proprietors, consultants) or retirees. A common theme was how the decision was made that it was the right time to retire or how will the decision be made. Concerns were somewhat about income but more so on health insurance. There were no conclusions but the agreement that this sort of group would be beneficial in the future, particularly as a repository for documents that some have used prior to and at retirement.
The other “big” discussion was how to keep up to date and relevant. Proposals briefly discussed were:
1. Creation of an abbreviated “Listserv” for those no longer in practice.
• This could be open also to these who work alone to keep in contact in between the annual meetings
• A Facebook groups? Microsoft teams/
2. A journal Club, that might include a monthly discussion group, of current dermatology articles to encourage keeping up to date.
We also discussed the option for this group to offer mentoring to those interested in dermatology, either as students, GPs, technicians, or prospective dermatology residents. A conclusion from this small group is that this kind of roundtable discussion should be a part of future NAVDF and even WCVD meetings and should not be charged for, unless there is a specific fee for food. We want to go back to traditional breakfast discussion groups. I (Candace Sousa) am volunteering to lead this group and discussion going forward.
Recommended book – Surviving the Baby Boomer Exodus, published in 2010
Thank
From Daryl Leu
After 42 to years in practice, it’s difficult to go from all out “balls to the wall” to “what do I do with all this free time and oodles of medical knowledge?”
Personally, I was going stair crazy.
9 DERM DIALOGUE 9 13 Continued on page 14
you to Drs. Lou Gotthelf, Alice Jeromin, Karen Kuhl, Daryl Leu, Guille Manigot, Helen Power, Rob Schick, Brett Wildermuth for providing their thoughts prior to the NAVDF
ROUNDTABLE SUMMARIES
1. The most obvious option is to continue working at a relaxed pace, 1 - 2 days a week (maybe just do all the rechecks), at your clinic if that is possible. It’s a win-win situation for a retired dermatologist and a new budding dermatologist.
2. Write a book, your memoirs, an atlas or a manual; or make instructional videos. Writing exercises the mind (brain plasticity).
3. Teach at a university or community college.
4. Lecture tour.
5. Start an informational website (blog).
6. Stay connected by sharing information on multiple listserve(s).
7. Consult on an app, like VIN.
8. Consult on a telemedicine app. (I found this to be very invigorating, but a lot of night and weekend work).
9. Go back to school (I’ve applied to law school)
10. Volunteer (Fish and wildlife, Zoo, human hospital, veterinary school, dog/cat show circuit, State Fair, etc.)
11. Take up a hobby (taxidermy, art, illustration, photography, cinematography, etc.)
Retirement is great, but it’s challenging to keep your mind active, and your refrigerator door closed.
From Lou Gotthelf
I sold my practice 2 years ago and I am working part time at the vet school at Tuskegee University. I did not want all of my acquired knowledge and experience to go to waste, so I am in the outpatient clinic with three or four senior students who rotate clinical services every 3 weeks. I work 2 days a week doing mostly annual physicals and vaccinations. The pressure of private practice is off, which allows me to just practice medicine. I have lots of free time for my family and for my many hobbies.
Seeing preventative medicine patients gives me the opportunity to diagnose and treat a lot of skin and ear cases with the students. I do my ear lecture every rotation and we are doing a “skills lab” with the video otoscope. The students really love the idea of having a “seasoned” vet to teach them the nuances of practice. I can tell that the 4th year students have brains brimming to overflow with facts, but recognizing diseases is the difficult part. Once we identify a disease, most of them can spout off facts concerning the condition. If not, then I can provide them references to go to and then we can discuss them. (We had a DLE case last week that led to a discussion of autoimmune skin diseases). It is gratifying to be able to help them make diagnoses that they would not think of during their physical exams. Because they are all studying for the NAVLE, we discuss things that they might not understand or need clarification on.
9 DERM DIALOGUE 9
14 Continued on page 15 Continued from page 13
ROUNDTABLE SUMMARIES
We also get rotating undergraduate pre-vet students that need to experience clinical medicine. They mostly observe and hold animals, but they are full of questions, and I can help them with their journey into our profession.
I would recommend that any retiring veterinarian can give back as a mentor to students at a vet school or to vet techs/assistants at a local college.
From Rob Schick
Biggest concerns since leaving BP primarily insurance. Health insurance is insanely expensive. We are still being covered under Cobra but when that runs out, we will be faced with even higher increased premiums.
I think advice I would have to younger derms would include to invest wisely so financial concerns won’t be an issue. Meet with a financial planner early on. Enjoy your practice but develop other interests and hobbies. You want to enjoy your retirement after all the hard work.
From
Helen Power
1. Retire to something, not from (I think you might have told me this and it is important).
2. Staying working part time is really a good idea; wind it down slowly.
3. Make sure there is a new community out there for you.
4. Exercise
5. Lastly, start thinking about, not necessarily planning for, but thinking about how you want the next chapter to be.
A book that I have gotten so much from about all aspects of retired life and wish I had read about 2 years before I would be making those big decisions:
How to Make your Money Last, 2nd edition. Jane Bryant Quinn; and it’s about a lot more than money. have the same success rate!
9 DERM DIALOGUE 9
15 Continued from page 14
ROUNDTABLE SUMMARIES
PYTHIOSIS, LAGENIDIOSIS AND PARALAGENIDIOSIS IN DOGS AND CATS.
Moderator: Tina Brown, DVM, MS, DACVD.
There were 12 attendees in total, eight were practicing veterinary dermatologists, four were dermatology residents and one was a practicing dermatohistopathologist.
Presentation of pythiosis, lagenidiosis, paralagenidiosis
The discussion opened by asking if anyone had seen cases with atypical presentations in dogs and cats. One person noted a feline cutaneous case of pythiosis with no draining tracts and the patient did well with surgical resection. Another mentioned that they have an active case of canine paralagenidium with subcutaneous swelling but no draining tracts. One clinician mentioned a pythiosis case in a dog where multiple areas were affected on the body, including two of the limbs. However most agreed that cutaneous cases were usually a single site on the body with distal limbs being the most common site and occasionally seeing lesions on the trunk of the body.
When asked if anyone had seen a case of Lagenidium gigantium, or type of lagenidium, one person mentioned one case that was fatal due to systemic spread to lymph nodes even after surgical resection and antifungal therapy.
One dermatologist mentioned a case of canine cutaneous pythiosis involving one distal front leg. The patient had a front limb amputation with clean margins and pythium serology significantly decreased one month post op. The pet had recurrence if pythiosis in the prescapular lymph node months but responded well to a combination of itraconazole, terbinafine and mefenoxam.
Diagnosis and treatment options
In regard to pythium serology, most clinicians send samples to Auburn University, and it was noted that the serum must be kept cold and transported on ice.
One practicing dermatologist mentioned success with a pythium vaccine obtained from a lab in Oklahoma through Dr Richard Hansen.
When asked if anyone had seen nonsurgical cases that responded to antifungal therapy alone, most agreed that traditional antifungal therapy with terbinafine and itraconazole were usually ineffective without surgery. However, a few dermatologists have used mefenoxam in the form of Subdue Maxx and felt it was effective in a few non-surgical cases. One dermatologist mentioned a case of distal limb pythiosis in which the owner was hesitant to amputate, and the lesion resolved with a combination of terbinafine, itraconazole, mefenoxam, and prednisone. In this case, the serology levels submitted to Auburn University decreased one month after starting this protocol and eventually the serology was reported to be in the negative range. The dose of mefenoxam was 4 mg per kg once or twice a day. One clinician noted that they had used full strength (22 percent) mefenoxam in the form of Subdue Maxx for topical application. When asked if any pets had any side effects or bloodwork changes with oral mefenoxam, one person noted they had used it in over 10 cases with no adverse effects or CBC/chemistry changes. Another noted that they had treated a dog with the same combination and while no changes were noted on bloodwork, the pet was lethargic and reluctant to eat on this protocol.
9 DERM DIALOGUE 9
16 Continued on page 17
ROUNDTABLE SUMMARIES
Minocycline was discussed as adjunctive therapy and a few dermatologists have incorporated minocycline in the treatment plan. Another clinician noted the use of hyperbaric oxygen at Auburn University where a case of pythiosis in which hyperbaric oxygen was used to reduce the size of the lesion before surgical resection. One clinician asked if anyone had used interferon or topical imiquimod in these cases, however no one had tried either of these therapies.
Overall, most medical treatment plans included a combination of prednisone, terbinafine, itraconazole, minocycline, and mefenoxam in some cases. One clinician asked when and how to withdraw medications once the patient has improved. Most agreed that the prednisone was usually tapered first due to side effects. One person mentioned a case of paralagenidium where the owner abruptly discontinued medications and the lesions recurred but then responded when terbinafine, itraconazole and mefenoxam was initiated again. Additionally, the dose of terbinafine was discussed and all agreed that their target dose had increased over time, one person mentioned that they were using 40mg per kg of terbinafine in dogs, divided twice a day.
9 DERM DIALOGUE 9
17 Continued from page 16
ROUNDTABLE SUMMARIES
ROUNDTABLE: CONTROVERSIES ON THE USE OF TELEMEDICINE IN VETERINARY DERMATOLOGY
Moderator: Dr. Lori Teller, DVM, DABVP (canine/feline)
Attendees: 18 individuals from academia, private practice and industry with various background including dermatology, ophthalmology and general (or primary) practice.
Objective: Discuss the risks and benefits of using telehealth/telemedicine in veterinary dermatology, the role of the VCPR, and how to advance the use of veterinary teledermatology.
General Notes:
• Telehealth/Tele-education/Teleadvice and Teletriage are approved for veterinarians to utilize outside of an existing VCPR
• can provide general information on a referral for a procedure such as imaging, video-otoscope exam, or other dermatologic diagnostic or therapeutic
• procedures.
• Some states (currently 5 states) have statutory or regulatory language that allows the creation of a VCPR virtually.
Do you currently use teledermatology in your practice?
Yes. About 50% of those present have been using teledermatology in their practices.
What are your current views on teledermatology? How are you using it?
• Use of telemedicine increased with the onset of the COVID pandemic o some noted that its utilization has decreased as things have normalized
• Generally, some attendees have been using teledermatology since before the pandemic o others are ready to implement teledermatology in their practices
• Dermatologists have been practicing telemedicine for decades, but not calling it telemedicine and not charging for services rendered
• We can help clients with different needs, particularly determining if/when they need to come in, measure compliance with and response to treatment, and providing follow-up or education on a variety of issues
• Some people are concerned teledermatology will not be effective
o discussed that teledermatology is not intended to replace the in-person visits or the need for diagnostic tests and procedures, but to be used in cases to complement and augment in-person visits
• Triage is a very important use of telehealth
• Tele-education/Teleadvice plays a role in supporting referring veterinarians as well as animal owner
• It can be used initially to start a conversation about what the patient will need, and clients can be charged for your time and knowledge
• Furthermore, the patient can then be brought into the office to perform procedures and provide appropriate care, ultimately generating more income to the practice
• The entire team should be educated about telemedicine and involved in its implementation and utilization
o Involving your team makes a difference to the implementation and utilization of a successful teledermatology practice
• It can be difficult to establish new clients and patients through teledermatology because of legal and regulatory issues, as well as the inability to bond with the client and put hands on the animal
9 DERM DIALOGUE 9
18 Continued from page 17
Continued on page 19
ROUNDTABLE SUMMARIES
• A few people using it to communicate with referring DVM (rDVM) for new clients/consults
o Dermatologist can communicate with client directly and a report with differential diagnoses and recommended diagnostic tests and/or therapeutics can be sent to the rDVM
o The rDVM can follow the recommendations: perform the diagnostics and/or prescribe as deemed appropriate
o The dermatologist can charge the client (or the rDVM, who then passes the charge to the client)
o The dermatologist can also have a consult with the rDVM and not speak directly to the client. The dermatologist charges the rDVM, who then passes the charge to the client.
• Teledermatology is suitable for follow-ups regarding stable patients and can be helpful with prescription refills.
What are the benefits of teledermatology:
• To you and your practice?
• People using it are having positive experiences.
• Some people involve their technicians in telehealth and schedule technician telehealth appointments for a fee
• Many clients and veterinarians are willing and happy to have the telemedicine services
• Allow dermatologist set boundaries and capture charges for services otherwise given away for free, such as existing clients emailing with pictures and questions and asking for recommendations
What about your referral (or potential) referral base?
• Some dermatologists are using telemedicine to provide paid consultations to referring veterinarians.
Your clients and patients?
• Benefit to clients from distant locations without access to care or specialty care
o Can help a client determine if should accept a referral and drive long distances to do so
• May be used as telehealth/tele-education outside an established VCPR
What do you see as barriers to implementation of teledermatology in your practice?
• Scheduling teledermatology appointment between in-person appointments can be challenging if you run late for the telemedicine appointment.
o There is not a staff person to let them know dermatologist is running behind
o Clients may get anxious or upset if they think the dermatologist forgot them
• Some clients get upset with the fee associated with a teledermatology visit
o Staff can be instrumental in explaining the shift to telemedicine
• May have a teleconsultation with a new client who was sent by the rDVM, especially if a dermatologic procedure is not needed
o Consult can also be done with rDVM with or without the client present
o There are several start-up companies creating panels of specialists to handle rDVM-todermatologist consults
What are some of the controversies surrounding teledermatology?
• They can be challenging because of the need for a hands-on exam and procedures
• Changing the in-person VCPR to a virtual VCPR requires each state/territory and federal agencies to change their definition, either in statute or regulation.
9 DERM DIALOGUE 9
19 Continued on page 20
Continued from page 18
ROUNDTABLE SUMMARIES
Type of telemedicine platform being used:
• People mentioned using Teams, Zoom, VetNOW or Google Duo
• 3rd-party telemedicine platforms have some advantages (takes payment, scheduling, reminders, upload history and pictures, can transfer/upload pdf files into the computer program people use)
How are teledermatology visits being scheduled?
• Some people incorporate them into their normal appointment schedule
• Having history collected in advance and using technicians or students for the history-taking can help
• Time: 30-60 min
o We need to value and charge for our time
• Perhaps have one dermatologist doing only telehealth/tele-education/teledermatology for a scheduled block of time
• Create guidelines/notes to give to clients prior to the telemedicine visits, so that they understand how to be prepared and have reasonable expectations.
• Have client submit pictures ahead of time
o Client can also answer brief survey with specific questions related to skin problem before the appointment
How are people charging?
• Fee can be charged and paid for through the 3rd-party platform or a staff person can collect the fee when scheduling the appointment
o Fee is paid in advance!
• Charges vary – some people charge the same fee as the in-person exam while others charge less
• For clients and rDVMs –
o Fee may include a limited number of free follow-up telederm visits after the initial visit.
- Determine initial fee accordingly
9 DERM DIALOGUE 9
20 Continued from page 19
THE DERMATOLOGISTS ROLE IN FELINE ASTHMA AND FELINE CHRONIC RHINITIS
Moderator: Christina Gentry DVM, DACVD
Participants: There were a total of 16 people, 15 in private practice and 1 in academia/private practice.
Discussion Points
1. How does the recent renaming/reclassifying of Feline Atopic Syndrome (FAS) change our perspective/ role with diseases that are usually treated by general practitioners and internal medicine specialists?
The group overall agrees that the naming change better reflects the clinical presentation of allergic skin and allergic respiratory disease in the cat. The participants also felt that the name change is more in line with human medicine where the human allergist treats components of respiratory disease as well as performs skin testing.
There was a general agreement that we should be involved in cases of respiratory driven otitis media. This may be primary complaint of the patient OR is found incidentally on CT for in-patients with chronic rhinitis. There was not a consensus on whether treating the otitis media (OM) in asymptomatic patients provided clinical benefit.
There is concern that dermatologists have minimal training in the clinical management of feline chronic rhinitis and feline asthma compared to internists. There is agreement that we do have the immunologic background since there is significant cross over with feline atopic skin syndrome (FASS).
2. Who should see these patients first?
There is consensus that feline chronic rhinitis and feline asthma should be seen by internist prior to dermatology referral. We may begin a relationship with these patients during the diagnostic phase if OM is seen on CT imaging. Only 2 participants work in clinics that are multispecialty and have a good working relationship with the internists to allow for this dual work up.
A participant mentioned that they see referrals from Veterinary Dentists when OM and rhinitis are seen on CT.
There is concern that once a dermatologist takes responsibility for these patients it will be harder to transfer them back to an internist for care. This presents an issue for a poorly controlled asthmatic cat that has a crisis that we are not trained to manage and typically do not offer in-patient care (unless part of a multispecialty hospital with a 24 ER/ICU).
One participant has serum and skin tested many cats with feline asthma. The group felt that many of these patients are already on steroids making skin testing difficult.
1. How well do these patients respond to immunotherapy?
One participant performed a research study in which transtracheal washes were presumed on presumed feline asthma and 1/3 would have other diseases that was not just asthma and rhinitis (mainly infectious disease).
9 DERM DIALOGUE 9
21 Continued on page 22
ROUNDTABLE SUMMARIES
ROUNDTABLE SUMMARIES
There is not much experience in treating these cats with rhinitis or asthma only, but the group is treating patients with both skin and respiratory disease
Immunotherapy does seem to help in these patients, but we do feel that clients need to have the expectation of 18-24 months prior to seeing full effect. This allows them to go through two allergy seasons prior to deciding on success of immunotherapy.
The general consensus was that higher dosing of steroids chronically could affect the response to immunotherapy in cats that have feline atopic syndrome. Secondary viral or bacterial respiratory infections can make a response to immunotherapy more difficult to interpret.
Those that have treated feline asthma feel that they do respond well with immunotherapy. However, the participants that have treated feline chronic rhinitis with immunotherapy have seen a more variable response rate. One participant mentioned that they have done immunotherapy for feline chronic rhinitis and the patient has done well.
A comment was made that this may occur because they may have more unknown environmental triggers (litter, scents, pollutants) that are not treated.
2. What therapies have you as a dermatologist prescribed patients with feline asthma and chronic rhinitis? Did these patients have concurrent skin disease?
Prednisolone
Prednisolone is the most common therapy the participants have seen prescribed.
Cerenia
Cerenia has been used for chronic rhinitis by several participants along with steroids and immunotherapy. Cerenia based drops- 1 part injectable Cerenia to 9 parts saline and a drop is applied to each nose daily. One participant mentioned that this seemed to be irritating to the cats.
Hyperbaric oxygen therapy
One participant said that the internist at their hospital has treated feline chronic rhinitis with hyperbaric oxygen chamber.
Suction and flushing of nasal passages
One participant feels that suction and flushing of nasal passages can lead to significant improvement. This is done daily to every other day during the allergy season depending on the severity of the clinical signs. Little Noses® saline spray and bulb syringe is used for this purpose.
Steroid nasal sprays
Steroid nasal sprays have also been tried in dogs and cats, but patients do not like this. One participant stressed the importance of managing viral diseases such as herpes virus as a way to limit flares of rhinitis and asthma. Respiratory viral panels and FIV/FeLV were also recommended.
Apoquel ®
- For asthma, a few participants have used it and found it helpful. The dosing recommendation varied from the standard canine dosing of 0.4-0.6mg/kg per day as well as ¼ of a 16mg tablet once to twice daily for average
9 DERM DIALOGUE 9
22 Continued on page 23 Continued from page 21
ROUNDTABLE SUMMARIES
cats. For very large cats some are using 8mg once to twice daily. The moderator is using 3.6mg tablets for smaller cats and 5.4mg for larger cats once to twice daily. Participants preferred the ¼ of 16mg tablet over the 3.6/5.4mg tablet due to client financial concerns.
Potential adverse events for off label use of Apoquel were also discussed. Several participants have seen neutropenia after starting, but the clinical significance is unclear. No feline patients became ill even with mild to moderate neutropenia. Most participants discontinued Apoquel if there was moderate neutropenia. One patient had a significant increase in ALT and Alk Phos that resolved with Apoquel discontinuation. Several participants have seen increased ALk Phos increase in canine patients and the drug was discontinued. Blood work monitoring recommendations by practitioners were also varied. There was agreement that performing a CBC/Chemistry panel when initiating therapy was ideal. One participant recommends CBC/Chemistry 2 months after initiating therapy, while others may wait 4-6 months.
There was a discussion on the participants comfort level on prescribing Apoquel at the current off label status. Almost all participants are prescribing Apoquel in feline patients and will inform clients that this is an off label/ non-FDA approved treatment.
Some participants would stop prescribing Apoquel for feline patients if black box labeling similar to Claro would occur.
3. If we are getting more involved in feline rhinitis and feline asthma, should we also assist in treatment of more canine lymphoplasmacytic rhinitis and canine presumed allergic lower airway disease?
Generally, the group recommends similar therapy with allergy medications and immunotherapy like they do in feline patients. Additionally, several participants found Cytopoint helpful in rhinitis and conjunctivitis. One participant found that chronic antibiotic use can be reduced with immunotherapy caused by postnasal drip in patients that get recurrent pneumonia. Immunotherapy is based on skin or serum testing. Another participant had a similar experience that immunotherapy allowed reduction of pulse antibiotics in a GSP and allowed for a decrease in chronic triamcinolone in Husky. Participants felt that rhinitis dogs may respond better/faster to immunotherapy than dogs with atopic dermatitis.
4. How do we get the word out there that we are here to help both internists and the general practitioner with these diseases?
- Consensus statement from us and the internists on treatment of feline chronic rhinitis and feline asthma (more research needed)
- Getting case series on treatment published.
- Inviting internists to the meeting and visa-versa to get the word out
9 DERM DIALOGUE 9
23 Continued from page 22
Continued on page 24
ROUNDTABLE SUMMARIES
5. How do we get to these patients early enough prior to start immunotherapy to prevent scaring, prevent progression of lymphoma and improve chance of success?
We agree that dermatologist management of immunotherapy may still be better than in GP management and we want to encourage referral to a dermatologist early in the disease course.
GPs that refer want to know how they can streamline to referral. Telemedicine consultations with GP may be helpful in discussing referral as well as discussing GP performed serum allergy tests. Medical record review may help GPs in areas where dermatology referral is geographically difficult.
There is a recommendation to discuss with local dermatologist on which serum testing company they prefer. There are a variety of companies, and the participants have different opinions on which company is better.
9 DERM DIALOGUE 9
24 Continued from page 23
Elisabeth Churchward
1.Why perform a neurological exam? We’re starting with the real basic stuff. This may sound self-explanatory, but occasionally it helps to remind ourselves about the reasons we do things. The aims of the neurological evaluation of any companion animal are to answer the following questions:
1. Do the clinical signs observed refer to a nervous system lesion? AKA Is the animal neurological?
2. What is the location of this lesion within the nervous system? AKA Where is the disease?
3. How severe is the problem?
4. What types of disease process might explain the clinical signs?
The first three questions are answered by performing a general physical and neurological examination and aim to determine the anatomical diagnosis (location and distribution of the lesion within the nervous system). This sounds straightforward enough, but remember that many other conditions, such as orthopaedic disease, can mimic neurological conditions. Examples of that would be dog with bilateral cranial cruciate ligament rupture or cat with pelvic fracture mimicking spinal disease causing paraparesis. For each of the presenting complaints we will consider during this course, the first question when approaching such cases will be to think of what non-neurological disease could cause a similar presentation and make sure they are ruled out first.
For this reason, it is always important to keep your mind open and your eyes peeled when performing the neurological examination. The last question is then answered by compiling the information on the patient signalment and history of the problem with the anatomic diagnosis to determine the differential diagnosis. As we will see further, using information about timing of onset, progression of signs (or lack of it/regression) and lesion localisation (where in the nervous system but also how it is distributed - focal/multifocal/diffuse) will be fundamental to narrowing down your differential list.
At the end of this process, when you know where you are looking (lesion localisation) and what you are looking for (having narrowed down the differential list), diagnostic tests are then carried out to investigate the differential diagnoses and rule them in or out. The choice and interpretation of these tests relies on having a clear understanding of the anatomical diagnosis and the most likely disease processes – in addition to an understanding of owner issues such as finances and commitment.
2. Do the clinical signs refer to a lesion in the nervous system?
A number of non-neurological conditions may mimic a nervous system lesion. Orthopaedic problems, cardiorespiratory diseases or metabolic disturbances, to name a few, can easily mimic some common neurological presentations such as gait abnormalities, neuromuscular weakness or collapse. Furthermore, some inflammatory, infectious or neoplastic diseases of the nervous system may also affect other body systems. A detailed clinical examination should therefore be performed before embarking on the neurological examination. Orthopaedic examination and evaluation of femoral pulses are particularly important when evaluating animals with abnormal gaits. Ophthalmic (and in particular retinal) examination can be particularly useful when evaluating a cat suspected of neurological form of feline infectious peritonitis, lymphoma, systemic arterial hypertension or Toxoplasmosis or a dog with distemper, fungal disease, systemic hypertension or Toxoplasmosis.
9 DERM DIALOGUE 9 The
Localisation 25
Neurological Examination & Lesion
Continued on page 26
The Neurological Examination & Lesion Localisation
3. Why should we bother to localise the problem?
Localising lesions is probably more important in neurology than with any other specialty. Since the nervous system is one of the few body systems that (with some exceptions) can’t be seen or palpated from the outside surface of the patient; the only way we can evaluate it is by assessing whether it is functioning normally or abnormally. And when things start to function abnormally, the neurological examination is there to tell us which part to start investigating to get to the root of the problem. The location of the source(s) of dysfunction in the nervous system is the anatomic diagnosis (we often use the term ‘neuroanatomic localisation’). Narrowing down the particular part of the nervous system that is affected is important for several reasons:
1. From a diagnostic point of view, the differential diagnosis list is almost entirely dependent on the anatomic diagnosis. Aside from determining which part of the nervous system is affected, localising the lesion also involves determining whether the problem is focal, multifocal (i.e., affecting multiple parts of the nervous system) or diffuse (i.e., affecting globally and symmetrically one or more parts of the nervous system). Such information can then be used to narrow down the differential list (see section how to establish a differential diagnosis list).
2. A number of disease processes may only be diagnosed by excluding other causes mimicking a similar clinical history and presentation. This process of exclusion relies on evaluating the correct part of the nervous system to confidently rule-out these mimics. If we haven’t localised the lesion when we start performing our investigation, the interpretation of any diagnostic test results can be a very challenging task for the clinician when they are presented with negative findings (as seen with some vascular or degenerative diseases of the central nervous system) or findings that do not match the clinical history).
3. Finally, running a limited number of investigations results in less cost for the owners, less time spent to reach a diagnosis for the clinician, and less risk for the patient (performing a 45-minute MRI scan on one region, with a short anaesthetic, is less risky than performing a 3-hour scan of the whole spine). And of course, this is made much easier if you’ve already narrowed down the area to be investigated.
4. What are the principles of lesion localisation?
Before rushing into the specifics of the neurological examination, it’s worth remembering a couple of points. In particular, when we do the neurological exam, we should be focusing on the questions we are trying to answer:
1. Is the patient neurologically abnormal or not?
2. Which part(s) of the nervous system may be involved to explain these abnormalities?
3. Is the lesion localisation focal, multifocal or diffuse?
The first question doesn’t require any detailed knowledge of neuroanatomy or neuroanatomic pathways, but it does require familiarity with the normal neurological examination. By simple observation and testing a number of reflexes and responses, the clinician should be able to determine if the patient is neurologically normal or not. We will cover the finer points of the neurological examination later, but it is important to remember that the only way to get familiar with normal variations of the neurological examination, is to practice as much as possible on normal patients as well as abnormal ones.
The neurological examination aims to test the integrity of these various components of the nervous system
9 DERM DIALOGUE 9 26 Continued on page 27 Continued from page 25
and, if present, detect any functional deficits. One of the most crucial things to remember is that normal findings are as important as abnormal ones in localising the lesion - it is the combination of both that helps confirm where the problem lies. Neurological abnormalities detected on examination should be added to the list of abnormal findings collected from the history. Each of these abnormal findings should then be correlated to a specific region or to specific pathways within the peripheral and/or central nervous system.
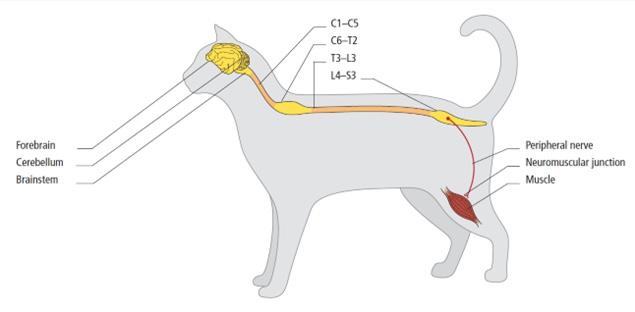
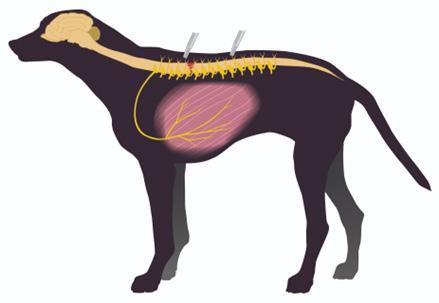
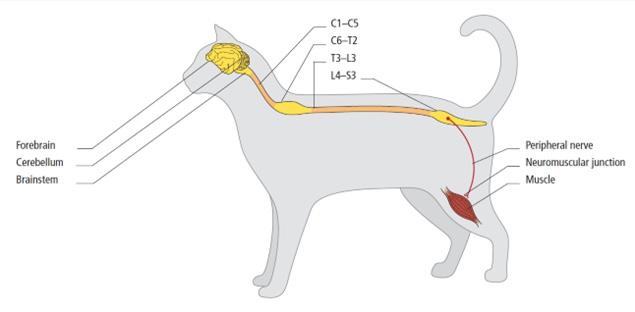
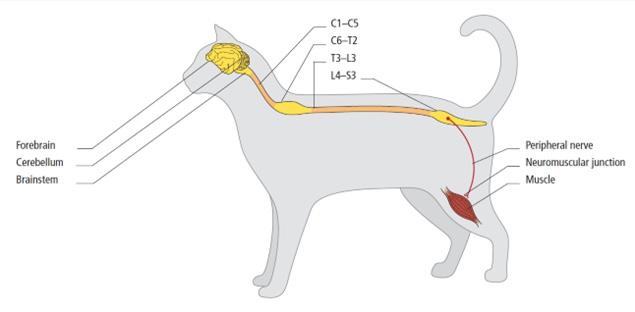
Attempts should then be made to explain all the abnormal findings by a single lesion within one of the following regions of the nervous system:
• forebrain
• brainstem
• cerebellum
• C1 – C5 spinal cord segments
• C6 – T2 spinal cord segments
• T3 – L3 spinal cord segments
• L4 – S3 spinal cord segments
• peripheral nerves / neuromuscular junctions / muscles
Lesions within these regions result in predictable and specific neurological signs (see later). It should be noted that in localizing a lesion, it is not necessary that all of the clinical signs referable to one localisation are present. If a single lesion cannot explain all the listed abnormal findings, the anatomical diagnosis is considered as multifocal or diffuse.
5. Functional anatomy of the main regions of the nervous system
Forebrain
The forebrain includes the cerebrum and diencephalon and is the area of the brain located rostral to the tentorium cerebelli.
The cerebrum is composed of the cerebral cortex, white matter and basal nuclei. The cerebral cortex is important for behaviour, vision, hearing, fine motor activity and conscious awareness of touch, pain, temperature and body position. The cerebral white matter mainly conveys ascending and descending sensory and motor activities within and between cerebral hemisphere as well as from and to the rest of the central nervous system. The basal nuclei are involved in muscle tone, and initiation and control of voluntary motor activity. The cell bodies of upper motor neurons are located in the motor cortex (pyramidal system), the diencephalon (thalamus) as well as motor centres of the brainstem (extrapyramidal system).
The diencephalon is involved in autonomic and endocrine functions, sleep and wakefulness, olfactory function, vision and pupillary light reflex (optic nerve = cranial nerve II) and emotional behavioural patterns via connections with the limbic system. It also acts as a sensory relay system to the cerebral cortex for the functions of vision, hearing, conscious awareness of pain (nociception) and body position (proprioception).
9 DERM DIALOGUE 9 27 Continued on page 28 Continued from page 26
The
Neurological Examination & Lesion Localisation
Brainstem
Embryologically, the brainstem consists of all of the brain apart from the forebrain and cerebellum. It includes the midbrain (mesencephalon), pons (metencephalon), the medulla oblongata (myelencephalon) and the cerebellar peduncles.
The brainstem contains the regulatory centres for consciousness (ascending reticular activating system), cardiovascular system and breathing (medullary reticular formation). It links the cerebral cortex to the spinal cord through ascending sensory and descending motor pathways often known as the long tracts. Finally, the brainstem has ten pairs of cranial nerves (cranial nerves III to XII) involved in a variety of motor and sensory functions including facial expression, prehending food, swallowing, equilibrium and hearing.
Cerebellum
The basic role of the cerebellum is to control the rate, range and force of movements without actually initiating any motor activity. It coordinates muscle activity and “smoothes” movements once they have been induced by the upper motor neurons. Because of its close association with the brainstem vestibular nuclei, it also functions in the maintenance of posture and the regulation of muscle tone when the body is at rest or during motion. Finally, the cerebellum normally has an inhibitory influence on urination.
Spinal Cord
The spinal cord lies within the vertebral canal. It is divided into functional segments (eight cervical, thirteen thoracic, seven lumbar, three sacral and variable number of caudal) which can be organised into four regions:
• Cranial cervical [C1-C5]
• Cervico-thoracic [C6-T2]
• Thoraco-lumbar [T3-L3]
• Lumbo-sacral [L4-S3]
These segments contain the cell bodies of the lower motor neuron (LMN). The segments C6 - T2 and L4 - S3 contain the cell bodies of the LMN innervating the thoracic and pelvic limbs. Lesions at the level of these intumescences results in LMN signs in the corresponding limb(s). Some spinal cord segments lie in the vertebra of the same annotation while others do not.
Neuromuscular System
The neuromuscular system is composed of motor units that consist of a neuron cell body, its axon, the neuromuscular junction, and muscle fibers. Consequently, an abnormality in any portion of this motor unit can result in clinical signs of neuromuscular disease. The lower motor neuron (LMN) is an integral part of this unit and is an efferent neuron connecting the central nervous system to a target muscle. Its cell body lies within the ventral horn of the spinal cord grey matter or within the cranial nerve nucleus of the brainstem. Its axon leaves the central nervous system by the ventral nerve roots to join successively a spinal nerve and a peripheral nerve before it synapses via a cholinergic (nicotinic) neuromuscular junction with a muscle. The motor unit composed of the LMN, the neuromuscular junction and the muscle fibres innervated is the final common pathway for motor activity.
9 DERM DIALOGUE 9 28 Continued on page 29 Continued from page 27
The Neurological Examination & Lesion Localisation
Overview of the central and peripheral nervous system (Small Animal Neurological Emergencies, Platt & Garosi editors, Copyright 2012, Manson Publishing, reproduced with permission of Taylor & Francis Books UK)
Principles of lesion localisation
Before rushing into the specifics of the neurological examination, it’s worth remembering a couple of points. In particular, when we do the neurological exam, we should be focusing on the questions we are trying to answer:
1. Is the patient neurologically abnormal or not?
2. Which part(s) of the nervous system may be involved to explain these abnormalities?
3. Is the lesion localisation focal, multifocal or diffuse?
The first question does not require any detailed knowledge of neuroanatomy or neuroanatomic pathways. By simple observation and testing a number of reflexes and responses (see hands-on and hands-off approach sections), the clinician should be able to determine if a cat or a dog is neurologically sound or not. It is important to note though that an animal may have a normal neurological examination yet still be neurological e.g., a dog with idiopathic epilepsy.
The neurological examination aims to test the integrity of these various components of the nervous system and, if present, detect any functional deficits. One of the most crucial things to remember is that normal findings are as important as the abnormal ones in localising the lesion. Neurological abnormalities detected on examination should be listed and added to the list of abnormal findings collected from the history. Each of these abnormal findings should then be correlated to a specific region or to specific pathways within the peripheral and/or central nervous system.
By making a list of neurological deficits (including presenting complaint - see table below) and considering
9 DERM DIALOGUE 9 29 Continued on page 30 Continued from page 28
The Neurological Examination & Lesion Localisation
The Neurological Examination & Lesion Localisation
where they could arise in the nervous system, we can try to localise the lesion (i.e. make an anatomic diagnosis). The table below provides a few examples of classic clinical presentations and their anatomic diagnoses:
Clinical signs Anatomic diagnosis
Epileptic seizures
Narcolepsy-cataplexy
Abnormal behaviour
Head pressing
Head tilt, nystagmus, falling and leaning Depression, stupor, coma
Dropped jaw
Paralysis of eyelids, lips, nostrils and/or ears
Circling: With loss of balance
Without loss of balance
Forebrain
Diencephalon Forebrain Forebrain
Vestibular apparatus Brainstem or forebrain Bilateral CN V (trigeminal nerve) CN VII (facial nerve)
Vestibular apparatus Forebrain
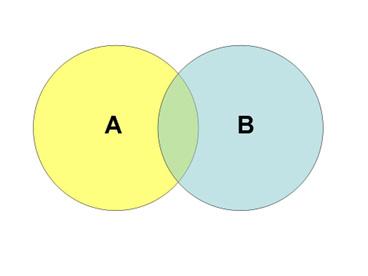
However, a deficit on its own is rarely diagnostic and localising the lesion often requires cross referencing the abnormal and normal findings. Each sign and portion of the neurological examination should be considered a piece of a jigsaw. This concept is illustrated with the principle of the Venn diagram below.
A Venn diagram is a diagram that shows all possible logical relations between a finite collection of sets. This example involves two sets, A and B, represented here as coloured circles.
The yellow circle, set A, represents vestibular disorder which could be related to a peripheral problem (disorder of the balance receptors in the inner ear) or a central problem (disorder of the balance ‘control box’ in the brainstem = central vestibular nuclei). As we will see in the next module, proprioception is intact with peripheral vestibular disorders while with central vestibular disorders it is commonly affected and therefore this finding can be used to distinguish between peripheral and central vestibular disorder. The blue circle, set B, represents abnormal proprioception on the front and hind limbs on the same side as the
9 DERM DIALOGUE 9 30 Continued on page 31 Continued from page 29
The Neurological Examination & Lesion Localisation
vestibular signs. On its own, abnormal proprioception on limbs on the same side could indicate a lesion in the cervical spinal cord, brainstem or forebrain on the opposite side.
The lesion localisation represented in this case, are the points in the area where the blue and yellow circles overlap. In this example, it corresponds to the brainstem which is the common denominator between these two neurological findings (vestibular disorder and abnormal proprioception).
On that basis, attempts should then be made to explain all the abnormal findings by a single lesion within one of the following regions of the nervous system: focal forebrain – brainstem – cerebellum - [C1 – C5 spinal cord segments] – [C6 – T2 spinal cord segments] – [T3 – L3 spinal cord segments] - [L4 – L6 spinal cord segments] –[L7 – S3 spinal cord segments], peripheral nerve - neuromuscular junction – muscle. We will go through each of these during the different modules of this course.
Overview of the central and peripheral nervous system (Small Animal Neurological Emergencies, Platt & Garosi editors, Copyright 2012, Manson Publishing, reproduced with permission of Taylor & Francis Books UK)
Lesions within these regions of the nervous system result in predictable and specific neurological signs. As we have previously discussed, remember again that in localizing a lesion, it is not necessary that all the clinical signs referable to one location or syndrome be present. If a single lesion cannot explain all the listed abnormal findings, the lesion localisation is considered as multifocal (affecting multiple parts of the nervous system) or diffuse (affecting globally and symmetrically one or more parts of the nervous system).
9 DERM DIALOGUE 9 31 Continued on page 32 Continued from page 30
How to practically localise the problem within The Nervous System?
The Neurological Examination & Lesion Localisation
The neurological examination can be divided into two main parts:
1. Hands-off examination – (i) state of consciousness, awareness and behaviour, (ii) posture and body position at rest, and (iii) gait evaluation
2. Hands-on examination – (i) postural reactions testing, (ii) muscle tone and size, (iii) spinal reflexes, (iv) nociceptive testing, (v) cranial nerve evaluation
It is often too tempting in the face of a neurological presentation to rush into testing an animal’s spinal reflexes, postural reactions or cranial nerves and neglect the hands-off part of the examination which can provide a lot of useful information.
Part I – Observation
Part II – Hands-on examination
Cranial nerves Behaviour
Mental status / Consciousness
Postural reactions
Posture and body position at rest Spinal reflexes
Gait Muscle tone and size
Identification of abnormal involuntary Sensory evaluation movements
The neurological examination: Hands-off
Now that we have worked out exactly why we’re doing a neurological examination we can talk about how to do it. In the attachment, we have given you a fairly typical neurological exam form.
There are lots of different variations of this out in practice and it is very good idea to have some of these forms printed out and readily available whenever you are doing your exam.
As with clinical examinations, the most important thing to remember when performing a neurological exam is to follow the same routine every time, and this is where having the form in front of you is an enormous help. Remember that each portion of the examination provides you with a small but vital role in answering the questions about being neurologically abnormal or not and where the disease may be located. Try not to do one of the tests written on these forms without knowing what it should help you determine.
Typically, the neurological exam form starts with observations that can be made with the patient walking or moving around the consultation room. This allows assessment of level of consciousness and interaction with surroundings, as well as the presence or absence of circling, head tilt, vision, and head pressing. It also allows for the observation of gait, including whether hypermetria (increased in stride length) or ataxia (incoordination) are present and in which limbs, and whether the patient is weak or has tremors. With very close observation of the issues listed below it is also possible to evaluate most of the cranial nerves:
• Most dogs lick their nose as a response to smell stimuli, allowing evaluation of both cranial nerve I and XII.
• Blinking usually occurs as a response to tactile stimuli from the cornea (drying of the tear film) which allows evaluation of cranial nerves V and VII
• Pupil size and symmetry, as well as close observation of eye tracking movements assess cranial nerves II, III, IV
9 DERM DIALOGUE 9 32 Continued on page 33 Continued from page 31
and VI.
• Facial asymmetry (drooping on one side, excess salivation on one side of the mouth) can suggest a problem with cranial nerve VII
• Loss of temporal muscles on one side of the head might suggest a problem with cranial nerve V
• A head tilt, nystagmus and vestibular ataxia are usually present in animals with a lesion affecting cranial nerve VIII
• If an animal can bear weight while standing (even if they are ataxic) then weakness is probably not a major feature of the disease. Lower motor neuron and neuromuscular junction problems should drop down the list.
All of this can be enormously helpful, especially in patients who may be difficult to evaluate for reasons of aggression.
(A) Mental Status
Assessing mental status relates to an assessment of forebrain and brainstem function – what we are doing is evaluating levels of awareness, consciousness and appropriateness of response to surrounding environment, all of which are functions that are carried out by the front part of the brain. A reduced but appropriate response to the surrounding however, can be due to brainstem disease but would often be accompanied by cranial nerve dysfunction.
The forebrain takes all of the information from other parts of the body (vision, hearing, olfactory, tactile stimulation), integrates it, and makes decisions on what to do with that information.
Disturbances of awareness include:
• Dysphoria – an inappropriate reaction to the surrounding environment which may include hyperexcitability or vocalizing inappropriately
• Disorientation – being confused by the surrounding environment. The video below demonstrates a dog with severe obtundation (see below) and confusion.
Changes in levels of consciousness that might be seen include:
• Obtundation – reduced responsiveness to normal stimuli
• Stupor – lack of response to all but noxious stimuli
• Coma – no response to any stimuli. Generally speaking, this usually goes with more caudal lesions (within the brainstem) but can be caused by bilateral cerebral disease.
(B) Posture and Body Position at Rest
Evaluate abnormal postures such as:
• Head tilt (associated with vestibular disorder)
• Head turn (associated with ipsilateral forebrain lesion)
• Ventroflexion of the neck (associated with neuromuscular disorder (e.g. hypokalaemia, myasthenia gravis, thiamine deficiency, polymyopathy etc.) or severe cervical spinal cord grey matter lesion)
• Spinal curvature (kyphosis, scoliosis or lordosis).
Attention should also be given to the position of joints, limb stance, tail posture and presence of voluntary tail
9 DERM DIALOGUE 9 33 Continued on page 34 Continued from page 32
Neurological Examination
The
& Lesion Localisation
The Neurological Examination & Lesion Localisation
movement. Cats often carry their tails elevated straight dorsally when they have a significant balance loss.
(C) Gait Evaluation
Gait evaluation may reveal whether a lesion(s) is localized within the brain, spinal cord or neuromuscular system. Normal gait requires intact function of the brainstem, cerebellum, spinal cord and sensory and motor peripheral nerves, neuromuscular junctions and muscles.
• With forebrain disease, the gait may be relatively normal
• Circling may occur either with forebrain disease (towards the side of the lesion usually) or vestibular disease (look for a corresponding head tilt and nystagmus)
• Pacing and head pressing are signs of forebrain disease. However, it does not imply that a structural forebrain lesion is present and such forebrain dysfunction can be secondary to metabolic disease (e.g. hepatic encephalopathy) or toxicity.
• Hypermetria and truncal sway may indicate cerebellar disease (as shown on the video below), or occasionally cranial cervical spinal cord disease.
• Paresis – this describes weakness affecting one (mono) or more (hemi-/para-/tetra-) limbs. It can occur with problems in the spinal cord, brainstem or peripheral nervous system.
• Plegia: complete paralysis of one (mono) or more limbs. Essentially plegia is a more severe form of paresis, in which the motor pathways to the affected region have been completely disrupted.
• If the gait is abnormal, is it abnormal in all limbs? Both limbs on one side of the body? Or hindlimbs only? Answering these questions will help localise the lesion usually to a single area of the nervous system.
Ataxia is defined as an uncoordinated gait and can arise from a peripheral nerve or spinal cord lesion (general proprioceptive ataxia), a vestibular lesion (vestibular ataxia) or a cerebellar lesion (cerebellar ataxia). Clinical approach to ataxia is discussed in more details in the next module.
As we will see further in this course, two qualities of paresis can be distinguished: upper motor neuron (UMN) and lower motor neuron (LMN) paresis. Detection of one of these qualities will help localise the lesion to either the UMN (brainstem and spinal cord) or LMN (predominantly peripheral nerve and neuromuscular junction) anatomy.
UMN paresis causes a delay in the onset of protraction, which is the swing phase of the gait.
LMN paresis reflects degrees of difficulty in supporting weight and varies from a short stride to complete inability to support weight, causing collapse of the limb whenever weight is placed on it. Care must also be taken as many cats can have an apparent plantigrade stance (crouched posture) in a perceived hostile environment such as a consultation room. Compared to UMN paresis, disorders affecting the LMN only cause paresis and not ataxia.
Once the observational tests are done, we can begin examining the patient in a more hands-on fashion. Generally, we start with tests of proprioception – the general approach is that evaluating proprioception is the most useful way to tell which limbs of the patient are normal and which are abnormal. This is the first step to evaluating which region(s) the lesion is likely to be located within.
Once proprioception has been evaluated it’s time to move on to the reflexes and assessment of muscle tone –
9 DERM DIALOGUE 9 34 Continued on page 35 Continued from page 33
The Neurological Examination & Lesion Localisation
evaluating whether the lesion is affecting upper motor neurons or lower motor neurons (and which ones).
The neurological examination: Hands-on The hands-on part of the neurological examination is divided into:
• Postural reaction testing
• Spinal reflexes including muscle tone and mass
• Nociception testing
• Cranial nerve testing
Postural Reactions Testing
The postural reactions are testing proprioception which is the ability to sense stimuli arising within the body regarding position and equilibrium. There are two types of proprioception: general (position sense; see below) and special (balance; vestibular apparatus).
General proprioception is mediated via proprioceptive receptors in joints and muscles. As the movement takes place, these receptors send messages to the brain via sensory peripheral nerves and spinal cord proprioceptive pathways. Some of these messages will reach the cerebral cortex on the opposite side (conscious proprioception) while the rest will reach the cerebellum (unconscious proprioception).
The main aim of postural reaction testing is to detect subtle deficits that were not obvious on gait evaluation, i.e. if a dog is paralysed, postural reaction testing in the affected limb(s) is not worthwhile as it would have to be affected in conjunction with the motor dysfunction. Commonly used postural reactions include paw positioning, hopping, hemiwalking and wheelbarrowing. Each test evaluates the same components of the nervous system, so it is not essential to perform them all, especially when an abnormality has been detected. All the components of the peripheral nervous system and CNS that affect the limb tested are needed in order for the animal to perform postural reactions:

• Afferent = joint proprioreceptor, peripheral sensory nerve, ascending proprioceptive pathway in the spinal cord (spinothalamic pathways), brainstem and contralateral forebrain
• Efferent = contralateral forebrain, brainstem, descending motor pathways in the spinal cord, peripheral motor nerve and skeletal muscles
A lesion anywhere along these components can result in abnormal postural reactions. Therefore, on its own, an absent postural reaction does not provide specific information for lesion localisation. It is just a small piece of the jigsaw!
9 DERM DIALOGUE 9 35 Continued on page 36 Continued from page 34
Proprioceptive (paw) positioning response in the hindlimbs (Small Animal Neurological Emergencies, Platt & Garosi editors, Copyright 2012, Manson Publishing, reproduced with permission of Taylor & Francis Books UK)
(i) Paw positioning test
With the animal in standing position, pick up each paw and replace it on the floor in a ‘knuckled’ position. Normal animals should replace their paw properly almost immediately. When performing this test, the animal should be standing squarely on all four limbs. It is fundamental that the majority of the animal’s body weight is supported in order to improve test sensitivity as shown on the video below. Failure to do so causes flexion of the limb, which results in the stimulation of proprioceptors within the flexed joints.
Sometimes this is not possible to perform, especially in small dogs and cats which tend to lift their legs off the floor as soon as they are touched. In this case another postural reaction (often hopping response) should be evaluated instead.
This test requires proprioceptive sensory input via the peripheral nerve and spinal cord (afferent and efferent), plus intact forebrain, lower motor neurons and skeletal musculature (efferent). Note that animals that are weak from other conditions affecting the skeletal musculature may have delayed positioning response – to counter this it is important to support either the pelvis or thorax whilst performing this test.
(ii) Hopping response
With the animal in standing position, pick up the limb opposite that being tested (either fore- or hind) and allow some weight bearing on the limb being tested. Then move the animal laterally (in the direction of the limb being tested). Normal animals should recognize the change in centre of balance almost instantly and correct by hopping sideways. A variation on this test in the hindlimbs is to allow the animal to stand on both hindlimbs and push laterally (gently at first) on the quadriceps femoris of each limb alternately. You should feel a change in extensor tone in each limb as it resists the sideways force, and as you increase the strength of the push a sideways step should be elicited. Hopping requires similar pathways to paw position testing, but proprioceptive fibres in the spinal cord carrying these signals travel in the lateral funiculi rather than the dorsal funiculi (which carry paw position information). Vestibular and cerebellar nuclei are more involved in this test.
In cat paw position testing (or “knuckling” response) can be very difficult to assess. It is best to replace it by hopping response as illustrated on the video above.
In combination with gait evaluation, postural reaction testing helps derive a conclusion as to how many limbs are involved and therefore narrow down the lesion localisation:
• If all four limbs are abnormal on gait evaluation and/or postural reaction testing, then the lesion is likely to be (a) cranial to T3 spinal cord segments (brainstem, C1 to C5 spinal cord segment or C6 to T2 spinal cord segments) or (b) a generalised polyneuropathy, junctionopathy or polymyopathy (=neuromuscular lesion localisation). Aside from lesions caused by peracute disease processes (i.e. stroke or head trauma), lesions affecting the forebrain result in such a mild contralateral paresis that it is usually not apparent in the gait.
• If only pelvic limbs are involved on gait evaluation and/or postural reaction testing, then the lesion is likely to be affecting either the T3 to L3 spinal cord segments, L4 to S1 spinal cord segments, or peripheral nerve roots/ nerve of the pelvic limbs.
9 DERM DIALOGUE 9 36 Continued on page 37 Continued from page 35
The Neurological Examination & Lesion Localisation
Spinal Reflexes - Muscle Tone and Size
Spinal reflex evaluation helps to narrow down further the lesion localisation by testing the integrity of the cervicothoracic intumescence (C6 – T2 segments) and lumbosacral intumescence (L4 – S3 segments) as well as respective segmental sensory and motor nerve, that form the peripheral nerve, and the muscles innervated.
Lesions at the level of these intumescences or affecting the peripheral nervous system result in LMN signs in the muscles innervated i.e. loss of segmental spinal reflexes as well as reduced muscle tone and size. Lesions cranial to the intumescence (UMN dysfunction) will result in normal to increased segmental spinal reflexes (due to release of the inhibitory modulatory effect of the UMN on the LMN). Spinal reflexes are best performed with the dog in lateral recumbency and with the cat in dorsal recumbency between the thighs of the examiner.
Withdrawal reflex and the patellar reflex are the most reliable ones in cats and dogs. Other spinal reflexes (triceps, biceps, extensor carpal radialis and gastrocnemius) are more difficult to perform and too subjective to reliably interpret, especially in small dogs and cats.
Passive movement of the limb helps to assess muscle tone. The extensor carpi radialis reflex is tested by hitting the proximal region of the antebrachium and observing a slight extension of the carpus. The triceps reflex is also shown and as you can see, is very difficult to elicit (and interpret!). The triceps tendon proximal to it insertion on the olecranon is struck. The desired reaction is extension of the elbow or carpus. This tests the integrity of the C7 - T1 spinal cord segments – radius nerve and triceps muscle. Finally, the withdrawal reflex is assessed by pinching the nail bed or digit and observing reflex contraction of the flexor muscles and withdrawal of the tested limb. Sensory input is through the median, ulnar and radial nerves while motor input is through C6 - T2 spinal cord segments, axillary, musculocutaneous, median and ulnar nerves (see below section on withdrawal reflex for more details).
Again, passive movement of the limb helps to assess muscle tone. The patellar reflex is assessed by striking the patellar tendon (see below section on patellar reflex for more details). The cranial tibial and gastrocnemius reflexes are less reliable than the patellar reflex. The cranial tibial is elicited by striking the proximal part of the cranial tibial muscle and observing for flexion of the tarsus while the gastrocnemius reflex is elicited by placing a finger over the gastrocnemius muscle and striking it with a hammer. The normal reaction is extension of the hock. These reflexes test the integrity of spinal cord segments L6 - S1 (cranial tibial) and L7 - S1 (gastrocnemius) as well as peroneal (cranial tibial) and tibial (gastrocnemius) peripheral nerves. Finally, the flexor withdrawal reflex is evaluated (see below section withdrawal reflex for more details).
Withdrawal reflex: apply a noxious stimulus by pinching the nail bed or digit with the fingers or haemostat. It is essential to ensure that the animal is physically capable of fully flexing all of its joints and that orthopaedic disease, for instance, does not confound the interpretation of this reflex. This stimulus causes a reflex contraction of the flexor muscles and withdrawal of the tested limb. Sensory input is through the median, ulnar and radial nerves, and motor output is through C6 - T2 spinal cord segments and the nerve roots of the axillary, musculocutaneous, median and ulnar nerves. If this withdrawal reflex is absent, individual toes can be tested to detect if specific nerve deficits are present. Reduced/absent withdrawal reflexes are consistent with a LMN (i.e. C6 – T2 spinal cord segments for thoracic limb and L6 – S1 spinal cord segments on the pelvic limb, associated spinal and peripheral nerves, muscle innervated – see below) disorder. The withdrawal reflex is a segmental spinal cord reflex that only depends on the function of the local spinal cord segments. In the thoracic limbs it evaluates the integrity of the spinal cord segments C6 – T2, the brachial plexus, the peripheral nerves (radial, axillary, musculocutaneous, median and ulnar nerves) and the muscle innervated.
9 DERM DIALOGUE 9 37 Continued on page 38 Continued from page 36
Neurological Examination
Lesion
The
&
Localisation
In the pelvic limbs, it evaluates the integrity of spinal cord segments L4 – S1, the femoral and sciatic nerves and the muscles innervated. A normal withdrawal reflex constitutes flexion of the hip (femoral nerve function), stifle and hock (sciatic nerve function). Sensory input is through the tibial and peroneal branches of the sciatic nerve (lateral, dorsal and ventral aspect of the foot) and the saphenous branch of the femoral nerve (medial aspect of the foot including the second digit). Motor output is through L4 - S1 spinal cord segments and nerve roots, femoral nerves, sciatic nerves and associated tibial and peroneal branches.
Two important points to remember when testing the withdrawal reflex:
1. When testing the withdrawal reflex, remember that you are testing the STRENGTH of the withdrawal. It is therefore fundamental to (i) observe flexion of all the joints of the limb tested when pinching the nail bed or digit, but also after that you apply more pressure and try to pull the limb toward you, to (ii) properly test the strength of the withdrawal.
2. The withdrawal reflex is a segmental spinal cord reflex that only depends on the function of the local spinal cord segments. Therefore, it should be stressed that the withdrawal reflex in the thoracic and pelvic limbs does NOT depend on the animal’s conscious perception of the noxious stimuli (nociceptive function - see below).

Withdrawal (flexor) reflex. When a noxious stimulus is applied to a digit, the limb should be withdrawn towards the body. Sensory input enters the spinal cord through the dorsal root to activate ipsilateral flexor motor neurons via interneurons and simultaneously inhibit the antagonistic extensor muscles. Contralateral stimulation of extensor muscles is inhibited by the descending UMN influence on the contralateral LMNs.
Patellar reflex: hit the patellar ligament and observe a reflex contraction of the quadriceps muscle and extension of the stifle joint. The patellar reflex tests the integrity of spinal cord segments L4 – L6 (and associated nerve roots) as well as femoral nerve (which all control quadriceps function). Evaluation of the extensor tone in the pelvic limb can be used as a control in dogs or cats with an ambiguous patellar reflex as it involves the same neuro-anatomical components (femoral nerve and quadriceps muscle). A reduced/absent patellar reflex is consistent with a lesion of the L4 – L6 spinal cord segments, the femoral nerve or quadriceps muscle. A lesion cranial to the L4 spinal cord segment can cause a normal or exaggerated patellar reflex. In the absence of other neurological deficits, an exaggerated patellar reflex means little and can be observed in an excited or nervous animal. The patellar reflex can also appear hyper-reflexive with a sciatic nerve or L6 – S1
9 DERM DIALOGUE 9 38 Continued on page 39 Continued from page 37
The Neurological Examination & Lesion Localisation
spinal cord segment lesion. This pseudo-hyperreflexia is caused by a decreased tone in the antagonist muscles that flex the stifle.
Evaluation of the cutaneous trunci (panniculus) reflex
This reflex is elicited by pinching the skin of the dorsal trunk between vertebral level T2 and L4–L5 and observing a contraction of the cutaneous trunci muscles bilaterally, producing a twitch of the overlying skin.
This reflex is present in the thoracolumbar region and is absent in the neck and sacral region. From the dermatome tested, the sensory nerve from the skin enters the spinal cord at the level of the segments corresponding to that dermatome (approximately two vertebrae cranial to the level tested). Afferent sensory information ascends the spinal cord and synapses bilaterally at the C8–T1 spinal cord segments with the motor neurons of the lateral thoracic nerve, which courses through the brachial plexus and innervates the cutaneous trunci muscle. The cutaneous trunci reflex can be decreased or lost caudal to a lesion anywhere in this pathway.
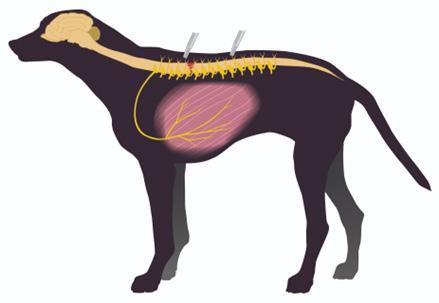
Testing is started at the level of the ilial wings as can be seen in this video below.
If the reflex is present at this level the entire pathway is intact and further testing is not necessary. With spinal cord lesions, this reflex is lost caudal to the spinal cord segment affected, indicating the presence of a transverse myelopathy. Pinching the skin cranial to the lesion results in a normal reflex, while stimulation of the skin caudal to the lesion does not elicit any reflex. Such findings help to further localize lesions between T3 and L3. This reflex can also be lost ipsilaterally (with a normal contralateral reflex) with disease affecting the brachial plexus (and hence the motor lateral thoracic nerve) regardless of the level at which the skin is stimulated. In the absence of other neurological deficits, a lack of the cutaneous trunci reflex means very little.
Cutaneous trunci (panniculus) reflex – illustration depicts a focal spinal cord lesion in the thoraco-lumbar region: stimulation caudal to the lesion will not elicit a response while stimulation cranial to a lesion up to C8-T1 dermatomes will elicit a response.
9 DERM DIALOGUE 9 39 Continued on page 40 Continued from page 38
The Neurological Examination & Lesion Localisation
Nociception Testing
Tested by pinching the digits with the fingers or with haemostats. Only a behavioural response to noxious stimulus (turning of the head, attempt to bite, vocalising) indicates conscious pain perception. If no response is elicited when using fingers, the test should be repeated with haemostats to ensure that the response if absent. Withdrawal of the limb is only the withdrawal (flexor) reflex and should NOT be taken as evidence of pain sensation.
Although it only defines the degree of dysfunction and not the degree of structural damage, nociceptive testing has significant prognostic value in cases of spinal cord or peripheral nerve lesions. Therefore, its only usually a test that needs to be performed when there has been complete loss of motor function in the limb. Lateral and medial digits of affected limbs, the perineal region and the tail should all be tested.
Cranial Nerve Testing
There are 12 pairs of cranial nerves. Cranial nerves (CN) I and II are associated with the forebrain. CN III is associated with the mesencephalon, and CN IV-XII are associated with the pons and medulla oblongata (myelencephalon). Not all of them are clinically relevant in terms of neurological examination. Anatomy, physiology and signs of dysfunction of clinically relevant cranial nerves are discussed in a separate module. Here below we are briefly reviewing cranial nerve testing and findings which are relevant to your clinical activity:
• Menace response and visual placing
• Pupil size, symmetry and responsiveness
• Trigeminal and facial nerve function
• Response to nasal stimulation
• Oculocephalic reflex and pathological nystagmus
Menace response
The menace response is elicited by making a threatening gesture at the eye tested while the other eye is blindfolded with the other hand. Prior to menace response testing, you must ensure that facial nerve (CN VII) function, which mediates closure of the eyelids (efferent part of the response), is intact by testing the palpebral reflex (CN V = trigeminal sensory and CN VII = facial motor) as shown on the video below.
Expected response is a closure of the eyelid (CN VII = facial) and retraction of the globe (CN VI = abducens), which in turn causes passive retraction of the third eyelid. This response is absent in very young animals (<1012 weeks).
This response tests the ipsilateral retina, optic nerve (CN II), contralateral optic tract and contralateral forebrain, ipsilateral cerebellum and facial nerve (CN VII).
Visual placing response
The visual placing response of the thoracic limb requires intact visual and motor pathways and can be useful in assessing visual function in a cat or small dog, where the menace response is ambiguous. It is tested as shown on the video below by carrying the animal towards a tabletop. On approaching the surface the animal will reach out to support itself on the table before the paw touches the table.
9 DERM DIALOGUE 9 40 Continued on page 41 Continued from page 39
The Neurological Examination & Lesion Localisation
Each eye can be evaluated separately by ‘blindfolding’ the contralateral eye as shown on the video above.
Evaluation of pupil size and symmetry
The pupillary size and symmetry should be assessed in ambient light as well as in darkness.
Normal pupils should be symmetrically shaped and equal to each other in size.
This test the parasympathetic (mediates constriction of pupil) and sympathetic (mediates dilation of pupil) supply to the eye.
It is important to rule-out primary or secondary anatomic or mechanical abnormalities (iris atrophy, uveitis or glaucoma) before consideration is given to a neurologic dysfunction in cats with pupils of unequal size (anisocoria) or shape (dyscoria).
Which pupil is abnormal can be determined by checking the pupillary light reflex and determining if the asymmetry in pupil size increases in bright light (larger pupil is the abnormal one) or in complete darkness (dark adaptation test), (smaller pupil is the abnormal one).
Trigeminal and Facial nerve function
Trigeminal nerve (CN V) provides sensory innervation of the face (cutaneous elements of the face as well as the cornea, mucosa of the nasal septum and mucosa of the oral cavity) and motor innervation to the masticatory muscles (temporalis, masseter, medial and lateral pterygoid and rostral part of the digastric muscles).
Motor function of CN V is assessed by evaluating the size and symmetry of the masticatory muscles and testing the resistance of the jaw to opening.
Sensory function (sensation of the face) can be individually tested by the corneal reflex (ophthalmic branch), the palpebral reflex (ophthalmic or maxillary branch when touching the medial or lateral canthus of the eye respectively), the response to nasal stimulation (ophthalmic branch) (see below), and by pinching the skin of the face with a haemostat or forceps and observing an ipsilateral blink or facial ‘twitch’ if normal.
The corneal reflex (shown on the video below) tests the ophthalmic branch of the trigeminal nerve (CN V = afferent part of the reflex) and facial nerve (CN VII mediating eyelid closure) as well as abducens nerve (CN VI mediating retraction of the eyeball by orbicularis muscle).
The pinching of the skin of the face and response to nasal stimulation are other useful cranial nerve tests and they are shown on the video below. Pinching of the skin of the face such as the upper lip with haemostat forceps should result in an observable curl of the lips. The presence of this reflex indicates that the afferent arm (CN V) and efferent arm (CN VII) of this reflex are intact. Depending on the intensity of the stimulation, a behavioural response (turning of the head) may also be observed (due to a cortically mediated response). Occasionally decreased perception of facial sensation (facial hypoalgesia) can be observed in animals with contralateral forebrain disease. In such cases, the animal curls its lip (normal reflex arc) but fails to show a behavioural response after stimulation of the lip contralateral to the lesion (abnormal response).
9 DERM DIALOGUE 9 41 Continued on page 42 Continued from page 40
The Neurological Examination & Lesion Localisation
A reflex response is best distinguished from a conscious response by stimulating the nasal mucosa, also shown on this video: the normal animal will pull its head away, whilst the animal with forebrain disease may blink or show a facial twitch, but not show a conscious reaction.
The facial nerve (CN VII) supplies motor function to the muscles of facial expression.
Its function is assessed by observation of the face for movement and symmetry of the ears, eyelids, lips and nostrils. The facial nerve is also responsible for the motor response (efferent part) of the following tests:
• palpebral reflex (CN V & VII)
• corneal reflex (CN V & VII)
• menace response (CN II & VII)
• pinching of the face (CN V & VII).
A Schirmer tear test (STT) can evaluate the parasympathetic supply of the lacrimal gland associated with CN VII. STTs are quite variable in normal cats but a value of <10mm wetting per minute is considered abnormal. The palpebral reflex (which is shown at the beginning of the video of the menace response) is elicited by touching the medial canthus of the eye and observing a reflex closure of the eyelids. The afferent arm of the reflex is mediated by the trigeminal nerve (CN V sensory) while the efferent arm is mediated by the facial nerve (CN VII motor).
Oculovestibular reflex and pathological nystagmus
Physiological nystagmus, which is normal, is evaluated by rotating the head from side to side (oculovestibular reflex). It is best performed by holding the cat or small dog at arm’s length and rotating it from side to side. Moving the head of a larger dog from side to side should be easy to perform.
This type of nystagmus consists of a slow phase in the direction opposite to that of the head rotation and a fast phase in the same direction as the head rotation.
It tests the vestibular receptors in the inner ear, vestibulocochlear nerve (CN VIII), medial longitudinal fasciculus in brainstem, and cranial nerves involved in movement of the globe (CN III, IV and VI). Loss of physiological nystagmus indicates a lesion in one of these areas.
In the absence of any head movement, nystagmus should never be present in a normal animal.
Pathologic nystagmus can be either spontaneous (observed when the head is in a normal position at rest) and/or positional (observed when the head is held in different positions [e.g. to either side, dorsally or ventrally or by placing the animal upside down on its back]).
Nystagmus is usually classified on the basis of its direction (the fast movement) and may be horizontal, vertical or rotatory; the fast movement occurs away from the side of the lesion. Central vestibular disease may cause any of these, while peripheral vestibular disease can only cause horizontal or rotatory nystagmus. Nystagmus will be discussed in more detail in the module on ataxia.
9 DERM DIALOGUE 9 42 Continued on page 43 Continued from page 41
The Neurological Examination & Lesion Localisation
Eye position and strabismus
While examining the eyes, the eyeballs should be assessed as to whether they are normally positioned in the orbits. The normal position of the eyeball is dependent on the innervation of the extraocular muscles by the oculomotor (CN III), trochlear (CN IV) and abducens (CNVI) nerves. The function of these cranial nerves can be tested by performing vestibular eye movements (see above), evaluating the degree of abduction (CN VI) and adduction (CN III).
The oculomotor nerve (CN III) innervates the ipsilateral dorsal, ventral, medial recti muscles as well as the ventral oblique muscle. This nerve also controls pupillary constriction and is involved in the retraction of the upper eyelid (levator palpebrae superioris) via its parasympathetic component. It therefore plays an important role in the efferent arm of the PLR and eyelid movement. The oculomotor nuclei are located in the rostral mesencephalon. Their axons exit the brainstem and traverse the cavernous sinus lateral to the hypophysis before exiting the skull through the orbital fissure.
The trochlear nerve (CN IV) innervates the contralateral dorsal oblique muscle. This muscle is responsible for inward turning of the eye. The trochlear nucleus is located in the caudal mesencephalon. After leaving the brainstem, its axons decussate on the dorsal surface of the brainstem and course rostrally through the cavernous sinus before exiting the skull via the orbital fissure.
The abducens nerve (CN VI) innervates the ipsilateral lateral rectus and retractor bulbi muscles. Its nucleus is located in the rostral medulla oblongata and its axons follow the same pathway as the axons of CN III and CN VI.
Strabismus refers to a deviation of the eyeball within the orbit that the patient cannot overcome. The strabismus may be present at rest (resting strabismus) or may only be evident on provocation by moving the head into an abnormal position (positional strabismus). Resting strabismus can be the result of a lesion within the nuclei or cranial nerves innervating the extraocular muscles (CN III, IV and VI) or a lesion of the extraocular muscles themselves. It can also be associated with non-neurological conditions causing mass effect on the orbit (retrobulbar tumour or abscess). Positional strabismus results from a loss of vestibular control over maintenance of the normal eye position within the orbit. Vestibular information is projected through the medial longitudinal fasciculus to cranial nerves III, IV, and VI. If this input is abnormal, then a strabismus may be seen when the head position is perturbed. A ventral or ventrolateral strabismus is most commonly observed.
The gag reflex
The glossopharyngeal and vagus nerves share sensory (nucleus solitarius) and motor (nucleus ambiguous) nuclei. CN IX innervate the musculature of the pharynx and palatine structures. CN X controls motor function of the larynx (recurrent laryngeal branch), pharynx and oesophagus. It also provides sensory function to the larynx, pharynx and thoracic and abdominal viscera.
The pharyngeal (swallowing or gag) reflex can assess the function of CN IX and CN X. It is evaluated by applying digital pressure to the hyoid bones to stimulate swallowing or by stimulating the pharynx with a finger to elicit a gag reflex as shown on this video.
9 DERM DIALOGUE 9 43 Continued on page 44 Continued from page 42
The Neurological Examination & Lesion
Localisation
The Neurological Examination & Lesion Localisation
Differential diagnosis
The differential diagnosis list is entirely dependent on the anatomic diagnosis. Determination of a differential diagnosis list is essential in choosing and interpreting any diagnostic test however sophisticated they may be. The aim of performing diagnostic tests should only be to confirm or exclude the differentials in the list and not replace the clinical evaluation!
A list of differential diagnoses is made based on the history (onset and progression of the condition) and result of neurolocalisation. The latter defines the lesion localisation (forebrain, brainstem, cerebellum, spinal cord segments, peripheral nerves, neuromuscular junction and muscles) and distribution of the disease (focal, multifocal, diffuse) within the nervous system. The manner in which the onset and progression of the differentials distinguish them from each other is displayed in the figure and the table below. To aid consideration of what type of disease processes could explain the neurological signs, neurologists use the mnemonic ‘VITAMIN D’ (Vascular, Inflammatory/Infectious, Traumatic/Toxic, Anomalous, Metabolic, Idiopathic, Neoplastic/Nutritional, Degenerative).
Each disease process has a typical onset and progression as well as distribution within the nervous system. As an example, vascular (e.g. stroke, ischaemic myelopathy) or traumatic diseases (disc herniation, spinal fracture/luxation, head trauma) have a sudden onset and are non-progressive or regressive in terms of pattern of development of the neurological signs. Neurological signs relating to metabolic diseases often wax and wane with time and are bilaterally symmetrical. With neoplastic disease, the signs are usually progressive and often focal while with inflammatory/infectious diseases they are also progressive but more often multifocal. Consequently, you should often be able to narrow down the differential (VITAMIN D) to two or three possibilities, utilising information from the owner about the mode of onset and pattern of disease development as well as considering the neurolocalisation.

9 DERM DIALOGUE 9 44 Continued on page 45 Continued from page 43
neoplastic
inflammatory/infectious diseases they are also progressive but more often multifocal. Consequently, you should often be able to narrow down the differential (VITAMIN D) to two or three possibilities, utilising information from the owner about the mode of onset and pattern of disease development as well as considering the neurolocalisation.
The Neurological Examination & Lesion Localisation
PATHOLOGICAL PROCESS MODE OF ONSET EVOLUTION DISTRIBUTION
Vascular
Peracute or acute (haemorrhage may cause subacute onset)
Non-progressive or regressive (haemorrhage may cause progression over a very short period)
Inflammatory/infectious Acute, subacute or insidious Progressive (wax and wane in some cases early after onset)
Focal and often asymmetrical
Focal or multifocal Asymmetrical or symmetrical
Traumatic
Peracute or acute Static or improve over time Often focal Asymmetrical or symmetrical
Toxic Acute Variable Diffuse and bilaterally symmetrical
Anomalous Chronic (occasionally acute)
Metabolic Variable (often acute)
Non-progressive or slowly progressive usually early in life
Variable
Wax and wane or progressive Diffuse and bilaterally symmetrical
Idiopathic Acute
Neoplastic
Chronic
Non-progressive or regressive Specific to each syndrome
Progressive Often focal Asymmetrical or symmetrical
Nutritional Variable (acute or insidious) Progressive Diffuse and bilaterally symmetrical
9 DERM DIALOGUE 9 45 Continued on page 46 Continued
page
from
44
disease, the signs are usually progressive and often focal
regressive
syndrome
inflammatory/infectious diseases they are also progressive but more often multifocal. Consequently, you should often be able to narrow down the differential (VITAMIN D) to two or three possibilities, utilising information from the owner about the mode of onset and pattern of disease development as well as considering the neurolocalisation.
Neoplastic Chronic Progressive Often focal Asymmetrical or symmetrical
PATHOLOGICAL PROCESS MODE OF ONSET EVOLUTION DISTRIBUTION
Vascular Peracute or acute (haemorrhage may cause subacute onset)
Non-progressive or regressive (haemorrhage may cause progression over a very short period)
Focal and often asymmetrical
Nutritional Variable (acute or insidious) Progressive Diffuse and bilaterally symmetrical
Degenerative Chronic Progressive Often diffuse and symmetrical
Inflammatory/infectious Acute, subacute or insidious Progressive (wax and wane in some cases early after onset)
Focal or multifocal Asymmetrical or symmetrical
Disease processes that can affect the nervous system and their respective mode of onset, evolution in time and expected distribution within the nervous system
Disease processes that can affect the nervous system and their respective mode of onset, evolution in time and expected distribution within the nervous system
Having evaluated where the problem is within the nervous system and created a short list of potential disease processes which could be the cause, you can then choose which diagnostic tests will help you to explore this list.
Localisation of Disease within the Central Nervous System
Having evaluated where the problem is within the nervous system and created a short list of potential disease processes which could be the cause, you can then choose which diagnostic tests will help you to explore this list.
Spinal Cord
The examination of the motor system should enable localisation of spinal disease to one of five segments of the spinal cord. It is essential to note that the divisions of the spinal cord listed below refer to spinal cord segments, which do not correspond exactly with vertebrae of the same number. Motor dysfunction can also occur with brainstem disease but there will be an association with cranial nerve dysfunction in this situation; this is considered separately below.
The most common signs of spinal cord dysfunction are ataxia or incoordination, weakness caudal to the lesion and spinal pain. Ataxia can also be a feature of vestibular and cerebellar diseases (see below). The presence of focal spinal pain is localising and suggests a compressive lesion such as disc extrusion or neoplasia (extradural or intradural-extramedullary lesions). Non-painful spinal diseases are usually lesions that affect the spinal cord parenchyma only (intramedullary lesions), such as degenerative and vascular disorders. The degree of weakness of the patient often parallels the severity of the lesion. Proprioceptive deficits are an early indicator of compressive spinal cord lesions. In severe cases, superficial and deep pain perception are absent caudal to the lesion. In all cases of focal spinal cord disease, whatever the location, there are no mentation changes or signs of cranial nerve dysfunction.
9 DERM DIALOGUE 9 46 Continued on page 47 Continued from page 45 Idiopathic progressive or
Specific to each
The
Neurological Examination & Lesion Localisation
Spinal Segments Cervical 1-Cervical 5
Lesions affecting the spinal cord segments C1-C5 can cause weakness or paralysis in all four limbs (tetraparesis / tetraplegia) or in the limbs on just one side (hemiparesis). Lesions in the center of the spinal cord in this region can cause weakness in the thoracic limbs with minimal deficits in the pelvic limbs (central cord syndrome). Segmental spinal reflexes are not affected by lesions in this region of the spinal cord and therefore remain intact. Severe lesions can cause respiratory weakness or apnea.
Spinal Segments Cervical 6 – Thoracic 2
Lesions affecting spinal cord segments C6-T2 can result in the same pattern of motor dysfunction in the thoracic and pelvic limbs as that seen with C1-C5 lesions, with the addition of weak or absent spinal reflexes in the thoracic limbs. Segmental spinal reflexes are intact in the pelvic limbs. With mild extradural lesions, the pelvic limbs can be more severely affected than the thoracic limbs.
Spinal Segments Thoracic 3 – Lumbar 3
Lesions affecting the T3 through L3 spinal segments may cause varying degrees of ataxia and weakness in the pelvic limbs with normal motor function in the thoracic limbs. The segmental spinal reflexes in all limbs remain intact with lesions in this region. Acute lesions in this region may cause a Schiff-Sherrington posture but this does not have prognostic significance. The cutaneous trunci reflex (panniculus) may be absent two vertebral levels caudal to the site of the lesion.
Spinal Segments Lumbar 4 – Sacral 2
Lesions affecting the L4 through the second sacral spinal segments cause weakness in the pelvic limbs with limited ataxia and reduced spinal reflexes (patella reflex /femoral nerve L4-L5; flexor withdrawal reflex / sciatic nerve L6-S2).
Spinal Segments
Sacral
1 – Sacral 3
Lesions affecting the sacral spinal segments can cause mild pelvic limb weakness with reduced or absent flexor withdrawal reflexes but may predominantly cause urinary and fecal incontinence with reduced or absent perineal or anal reflex, in addition to reduced motor function in the tail.
Brain Stem
The brain stem includes the midbrain, pons and medulla oblongata with cranial nerves III through XII. Severe brain stem lesions can cause severe depression, stupor or coma, but the animal’s personality and behavior are appropriate unless there is concurrent cerebral disease. Tetraparesis or tetraplegia with decerebrate rigidity, conscious proprioception deficits and intact spinal reflexes are often seen with brain stem disease. Ipsilateral cranial nerve deficits are possible in isolation or in conjunction with central motor and sensory dysfunction, depending on whether the cranial nerve is affected after it has exited the brainstem or before respectively. In addition to the above signs, there is the potential for cardiac and respiratory abnormalities, including apnea and cardiac arrest.
Vestibular System
The function of the vestibular system is to send messages to the brain about the gravitational forces acting on the head and any movement that the head experiences. The brain can then determine the position of the head in space and can coordinate subsequent movements of the eyes and limbs.
(i) PERIPHERAL COMPONENT
9 DERM DIALOGUE 9 47 Continued on page 48 Continued from page 46
The Neurological Examination & Lesion Localisation
The peripheral component of the vestibular system is located in the inner ear and is made up of a membranous labyrinth and the vestibular portion of cranial nerve VIII. This system is intricately associated with the auditory system and is enclosed in the petrous temporal bone close to cranial nerve VII and the sympathetic supply to the eye and face.
(ii) CENTRAL COMPONENT
The central component of the vestibular system consists of vestibular nuclei in the caudal brainstem (medulla oblongata) and the flocculonodular lobe of the cerebellum. These nuclei are connected to the nuclei of cranial nerves III, IV, and VI to control the movement of the eyes so that the eyes move in a coordinated fashion with the head. The vestibular nuclei are also connected via the vestibulospinal tract to the extensor muscles of the neck and the limbs; they are responsible for extensor tone in the ipsilateral limbs and cause contralateral extensor inhibition.
Clinical Signs of Vestibular Disease
Damage to either the peripheral or the central components of the vestibular system will cause vestibular dysfunction. It is most common to see unilateral lesions and therefore asymmetric signs, but bilateral lesions are possible. The signs exhibited by the patient depend upon the portion of the vestibular system affected. Indeed, it is important to use these differences in lesion localization, as peripheral and central vestibular diseases have several different differentials to be considered as well as different prognoses. Head Tilt – this is the most common sign of unilateral vestibular disease and occurs because of the loss of muscle tone on one side of the neck. The head tilt is towards the side of the lesion in peripheral disease whereas it can be to any side if there is a central lesion. Often, there is no head tilt if there is bilateral disease and instead there are wide excursions of the head and neck from side to side.
Ataxia & Dysequilibrium – the loss of general balance that is experienced by the animal with vestibular disease is manifested by a base-wide stance and swaying of the head and trunk. This can progress to rolling, leaning or falling to one side with unilateral lesions. Peripheral vestibular disease occurs without any deficits in conscious proprioception or strength, whereas a central lesion may cause these abnormalities.
Nystagmus – this is rhythmic movement of the eyes with a fast and a slow phase. The direction of the nystagmus is often described as the direction of the fast phase but can be horizontal, rotational or vertical in its direction. In normal animals, a physiologic nystagmus should be induced by rotation of the head, with the direction being in the plane of the head movement and the fast phase being towards the side of rotation (this may also be termed the occulocephalic reflex). This may be altered or absent in animals with vestibular disease. Nystagmus can be spontaneous which means that it occurs when the head is stationary in a normal position. With unilateral peripheral lesions, the fast phase is away from the side of the disease and the direction can be horizontal or rotational. With central lesions, the fast phase is usually away from the side of the disease, but the direction can be vertical as well as horizontal or rotatory. If the nystagmus is detected only when the head is placed in an unusual position, this is called positional nystagmus and can occur with both peripheral and central lesions but may be more common with the latter. Animals with bilateral disease usually do not have spontaneous or positional nystagmus.
Strabismus – Vestibular disease may cause one eye to be deviated ventrally or ventrolaterally when the neck is
9 DERM DIALOGUE 9 48 Continued on page 49 Continued from page 47
The Neurological Examination & Lesion Localisation
The Neurological Examination & Lesion Localisation
extended – positional strabismus. The ventrally deviated eye is usually on the side of the lesion. Occasionally, a constant ventral strabismus is present with vestibular disease.
Cranial Nerve Abnormalities - Peripheral vestibular lesions may be accompanied by ipsilateral facial nerve paresis and, or Horner’s syndrome due to the anatomical proximity of these two nerve supplies. It is possible that multiple cranial nerve defects be present with central vestibular disease.
Cerebellum
Cerebellar disease is one of the most readily recognizable syndromes in veterinary practice. The cerebellum coordinates movements. It controls the rate and range of movements but not the initiation of the movement itself. Cerebellar disease results in an inability to regulate the rate, range, and force of a movement (i.e., dysmetria). Clinical signs include an exaggerated limb response when a movement is initiated, such as “goose-stepping” (hypermetria) when walking. Limb movements are typically spastic and clumsy. Initiation of movement is delayed and often accompanied by tremors (i.e., intention tremors). Tremors are especially noticeable involving the head. Intention tremors disappear at rest. Fine, pendular, or oscillatory eye movements also may be present. A bilateral menace deficit may be noted, although vision is not affected. If the lesion involves only one side of the cerebellum, the menace deficit will be ipsilateral.
Infrequently observed signs associated with specific areas of the cerebellum include opisthotonus (e.g., when a lesion involves the rostral lobe of the cerebellum), and vestibular signs (e.g., when a lesion occurs in the flocculonodular lobe or fastigial nuclear area of the cerebellum).
Thalamus and Hypothalamus (Diencephalon)
The hypothalamus is intimately involved in autonomic visceral body functions, including appetite, sexual activity, sleep-wake cycle, body temperature, blood pressure regulation, heart rate, and emotions. It also regulates much of the body’s endocrine activity. Animals with the hypothalamic syndrome may show signs of altered mental status (e.g., disorientation, lethargy, or coma); and / or behavior changes (e.g., aggression, hyperexcitability, pacing, wandering, hiding, tight circling, head pressing, and trembling). Gait is usually normal. Abnormal temperature regulation may be manifested as hyperthermia, hypothermia, or poikilothermia. Abnormalities in appetite are seen as polyphagia and obesity, or anorexia and cachexia. Vision is frequently impaired if the lesion extends to involve the optic chiasm, in which case pupils may be dilated and weakly or non-responsive to light stimulation. Endocrine disturbances most often include diabetes insipidus or hyperadrenocorticism (clinical signs include polydypsia, polyuria, polyphagia, alopecia, pendulous abdomen, and muscular weakness).
Pure thalamic lesions are infrequently reported in dogs and cats; however, signs might include postural reaction deficits (contralateral), mild ataxia, visual deficits (contralateral), hypalgesia (contralateral and especially involving the head), an “adversive” syndrome (propulsive circling and head/eye deviation toward the side of the lesion) with rostral thalamic lesions, and possible disturbances in consciousness (depression, semi-coma) or seizures.
Cerebrum
9 DERM DIALOGUE 9 49 Continued from page 48
Continued on page 50
Diseases of the cerebrum usually cause alterations in behavior and / or mental status, seizures, blindness with normal pupillary reactivity, and contralateral proprioception deficits. Many animals will present with just one of these signs representing a lesion in a focal area of the brain.
Behavioral changes include those seen with lesions of the thalamus and hypothalamus in addition to circling (usually to the side of the lesion), compulsive pacing, head pressing, standing in corners, and getting trapped under furniture. Circling however, can also be seen with lesions of the brain stem, so is not a definitively localising sign. With cerebral disease, the animal’s gait is reasonably normal in most cases although with severe lesions, there may be a moderate ataxia. Depression, stupor or coma represent decreasing levels of consciousness seen with disease of the cerebrum. These signs can also be seen with brain stem disease, so the clinician should attempt to discern whether there is an inappropriate mentation (dementia) in addition to the altered consciousness, which would confirm the cerebral origin of the disease.
9 DERM DIALOGUE 9 50 Continued from page 49
The Neurological Examination
Lesion Localisation
&
North American Veterinary Dermatological Forum


www.navdf.org









52
Our Sponsors! Gold Silver Bronze
Thank You —to