TRANSFORMING TYPE 1 DIABETES
Learn about the first 20 members of our T1D Moonshot Community
THE DAWN OF EXPONENTIAL PROGRESS
THE DAWN OF EXPONENTIAL PROGRESS

Our Health Transformer community casts a vision for how AI will help solve the greatest health challenges of our time
MEET THE NEW HEALTH TRANSFORMERS
50+ founders tackling health moonshots –from addiction to women's health
Unlocking an Era of Exponential Progress
NNearly 13 years ago, we set out to unite a global army of Health Transformers – superhero innovators, doctorpreneurs, scientists – and inspire collaboration to achieve health moonshots. Our belief is that together we can solve the world’s biggest health challenges.
It’s easy to be discouraged when we look at health outcomes data from the past few years (especially after the global pandemic). But the reality is, we’ve never been more optimistic about many structural advancements being made – and the potential for transformative impact in the years ahead.
Something extraordinary is happening. A new foundation is being laid for an Era of Exponential Progress, and for the first time we not only believe that our health moonshot dreams are possible – we are starting to understand how they will be achieved.
A new species of innovation is evolving in the form of advanced AI as it merges with allied technologies like genomics, biologics, material science, advanced sensors, and nanotech, to create super tools that are just starting to embed into the fabric of our lives at work and home.
But tools alone do not bring forth much progress. Significant leaps forward are usually driven by the power of human imagination and fueled by purpose-driven collaboration.
While we're racing ahead with technological advancements, we must pause and ask: Are
we dreaming big enough? Are we working together, bridging divides and disciplines, to truly realize our human potential?
In this issue of StartUp Health Magazine, we've posed this challenge to a dynamic blend of game-changing Health Transformers –patients, creative minds, seasoned professionals, investors, and thought leaders – within the StartUp Health community. Their perspectives are not just eye-opening but a clarion call for all of us to expand our horizons and break the confines of traditional thinking. These often unheard voices paint a vision for an emerging health renaissance.
However, it's not enough to just envision. We need to act, and act collectively. If history has taught us anything, it's that collaboration inspired by purpose can produce wonders. Whether it's putting a man on the moon or eradicating a deadly disease, when humanity bands together with a shared dream, we make the impossible, possible.
2 StartUp Health Magazine / EXPONENTIAL PROGRESS
FOUNDERS’ LETTER
While we're racing ahead with technological advancements, we must pause and ask: Are we dreaming big enough?
About the Cover: Given our issue theme we decided to use AI to design our cover. We asked ChatGPT for three creative directions based on our feature story and then fed those prompts into three AI image generators. Then a few (very human) editors picked their favorite. What do you think?
Historically, humanity has been defined not just by its achievements but by its aspirations. The audacity to think bigger, to visualize what doesn't exist, and to carve a path towards it has always set us apart. Right now, in this era of exponential progress, we urge everyone to ignite their imagination. It’s not merely enough to have tools; we must also dream about the myriad ways they can redefine our reality.
And as you dream, remember that the greatest of visions can only be brought to life when shared. This brings us to the power of health moonshot collaboration. Throughout our journey with StartUp Health, we've realized that when passionate minds unite under a single purpose, magic happens. It's usually not the lone genius but the collective power of diverse minds that propel us forward.
So, what's still needed to unlock exponential (health moonshot) progress?
Firstly, a more profound infusion of bold, creative thinking is needed. It's the raw fuel that powers our ambitions. The limitations of the past shouldn't define our future aspirations. Our imagination has been the foundation upon which humanity has built wonders. Now, more

than ever, we need it to chart our next course for human health and wellbeing.
Secondly, the time is ripe for a renewed grand-scale, purpose-driven collaboration. In a world of increasing specialization, the melding of diverse minds brings about solutions that are greater than the sum of their parts. When a global community of Health Transformers rallies behind health moonshots – be it vanquishing Alzheimer’s, conquering diabetes, or extending a healthy lifespan universally – the combined might of shared purpose and innovative tools makes any challenge surmountable.
In essence, while we laud the astonishing progress of our era, we must remember that tools like AI, as potent as they are, need the guiding hand of human imagination and the binding force of collaboration.
This is our moment. An era where we're not just witnesses but active participants in crafting our own evolution and health. We possess both the means and the methods. What we now need is an amplified will – to think bigger, to dream bolder, and to come together in an unprecedented way to advance human health.
Steven Krein CEO & Co-founder

 Unity Stoakes President & Co-founder
Unity Stoakes President & Co-founder
startuphealth.com 3
MEET NEW HEALTH TRANSFORMERS 39 founders tackling moonshots addiction women's health TRANSFORMING TYPE 1 DIABETES Learn about the first 20 members of our T1D Moonshot Community THE DAWN OF EXPONENTIAL PROGRESS Our Health Transformer community casts a vision for how AI will help solve the greatest health challenges of our time





4 StartUp Health Magazine / EXPONENTIAL PROGRESS Founders' Letter 2 Health Transformers in the News 6 Feature: AI & Exponential Progress 12 Learn About the T1D Moonshot Community 24 Meet the Newest Health Transformers 34 INTHIS ISSUE 42 120 82 52 117 95
EDITOR-IN-CHIEF


Logan Plaster
DEPUTY EDITOR
Jennifer Hankin
CONTRIBUTING EDITORS


Nicole Kinsey, Lauren Schafer
WRITERS
Laura Plaster, Linda Morris, Susan Johnson, Abe Storer, Nicole Clark
startuphealth.com 5
104 74 62 36 56 46
HEALTH TRANSFORMERS IN THE NEWS
6 StartUp Health Magazine / EXPONENTIAL PROGRESS RECENT HEADLINES, AT A GLANCE NeuroSync Software Tracks Concussions, Cognition SPORTS BUSINESS JOURNEY 2/20/23 Cityblock Health is #29 on Fast Company’s List of the World’s 50 Most Innovative Companies of 2023 FAST COMPANY 3/2/22 Epicured Is One of the Best Gluten-Free Meal Kits and Delivery Services WOMEN'S HEALTH MAGAZINE 3/20/23
Healthcare Completes $6.75 Million Series A Funding Round MILWAUKEE BUSINESS NEWS 3/27/23 Adding VR Mindful Exposure Therapy to a Cancer Center’s Tobacco Treatment Offerings: An Acceptability Pilot Study of MindCotine JOURNAL OF THE NATIONAL COMPREHENSIVE CANCER NETWORK 3/30/23
Sift
daily health moonshot news,
StartUp Health on social media @startuphealth and subscribe to the StartUp Health Insider newsletter startuphealth.com/insider
For
follow
How

startuphealth.com 7 Colorado Health Startups That Will Change Your Life: HealthBook+ & Virta 5280 MAGAZINE 4/1/23 Our Favorite Startups from YC’s Winter 2023 Demo Day: Vitalize Care TECHCRUNCH 4/5/23 New Frontier Diagnoses Need, Expands Its Imaging Solution to Rural, Underserved Patients STARTLAND NEWS 4/7/23
$12M TECHCRUNCH 4/16/23
Scan.com, Which Gives Patients Direct Access to Private Medical Imaging Services, Raises
4/23/23
Top 50 in Digital Health: Troy Bannister, Particle Health; Kaitlin Christine, Gabbi ROCK HEALTH
4/28/23
Healthcare Leaders Such as Avanlee Care Are Leveraging Technology in a Tumultuous Economy FORTUNE
HEALTH TRANSFORMER NEWS // AT A GLANCE
Zeel’s New Program
Connects Massage Therapists to U.S. Military Veterans
MASSAGE MAGAZINE
5/1/23
Inbox Health Raises
$22.5M for Patient Billing Communications Platform
HIT CONSULTANT
5/4/23
AI Biotech Recursion Commits $88M to a Pair of Drug Discovery Acquisitions, Cyclica and Valence
MEDCITY NEWS
5/8/23
Top Digital Behavioral Health Companies Report: Arcade Therapeutics
AVIA MARKETPLACE
5/8/23
MedHaul Selected for the Verizon Forward for Good Accelerator Health Equity Cohort

VERIZON
5/8/23
CNBC Disruptor 50: Cityblock Health
CNBC
5/9/23
Goldfinch Health's Iowa Opioid Reduction Program Involves Rethinking Pain Treatment
RADIO IOWA
5/10/23
8 StartUp Health Magazine / EXPONENTIAL PROGRESS
Pear Suite Raises $2.5M for SDoH-Driven Care Navigation Platform to Empower AAPI Communities
HIT CONSULTANT
5/16/23
A Sweet Idea: Amy Cohn, Founder of Joydays, Shares Her Story


OPRAH DAILY
5/22/23
Scan.com Becomes Official Partner of the British & Irish Boxing Authority (BIBA)
BOXING NEWS
5/25/23
APA Launches Online Eating Disorder Assessment Tool in Collaboration with AvoMD
MEDSCAPE
5/30/23
InSilicoTrials, IBSA Group Partner to Expand AI Use in Drug Development
FIERCE BIOTECH
5/31/23
Sami, a Brazilian insurtech, gets $18 million
AXIOS
6/2/23
Leading Virtual Maternity Care Platform Babyscripts Announces Partnership with Memorial Hermann
MHEALTH TIMES
6/4/23
NEXT Life Sciences Raises $1.55M for Plan A, Its Male Contraceptive
FEMTECH INSIDER
6/5/23
startuphealth.com 9
Digital Health Startups, Including Babyscripts, Take Aim at Maternal-Health Crisis
THE WALL STREET JOURNEY
6/8/23
approved
UnaliWear Is One of the Three Best Medical Alert
Smartwatches
MIAMI HERALD
6/8/23
Cala Health Launches Wearable Device to Treat Hand Tremors
MEDCITYNEWS
6/14/23
Athelo Health and Gray OS Join White House Cancer Moonshot Program
Caregivers
NASHVILLE POST
6/20/23
BrainScanology Releases
Dementia Detecting App
SACRAMENTO INNO
6/20/23
Diatech Diabetes Receives
JDRF Award to Advance Novel Software Platform for Monitoring Insulin Pump Infusion Set Failure
JDRF
6/22/23
AvoMD Raises $5M Seed to Combat Doctor Burnout
AXIOS
6/23/23
Mount Sinai Pilots
Core Sound’s Studycast Integration Program Using Us2.ai
MEDICAL DEVICE NETWORK
6/29/23
How Startups Can Shape Their Corporate Culture Amid Global Turmoil, by Yishai Knobel of RxWare
FORBES
7/6/23
Valera Health Becomes

Humana in-Network Provider for Virtual Mental Health
MOBIHEALTH NEWS
7/6/23
10 StartUp Health Magazine / EXPONENTIAL PROGRESS
HEALTH TRANSFORMER NEWS // AT A GLANCE
AI-Enabled Senior Care Company CarePredict Scores $29M
MOBIHEALTH NEWS
7/12/23
Pelago (fka Quit Genius)
Rebrand Aims to Dump Substance Abuse Stigma
TRANSFORM MAGAZINE
7/13/23
Jade Kearney, CEO of She Matters, on Creating an App Helping to Reduce Disparities in Black Women’s Maternal Health

BLACK ENTERPRISE
7/14/23
LGBTQ+ Founders, Including Joseph Schneier of Trusty.care, Reflect on the Struggles of Fundraising, Seeking Allies, and Pleasing Investors
FIERCE HEALTHCARE
7/15/23
Why Troy Bannister, Founder of Particle Health, Decided to Replace Himself as CEO
TECHCRUNCH
7/16/23
NHS Fife Introduces Digital Pre-Op Pathway from Buddy Healthcare
DIGITAL HEALTH
7/21/23
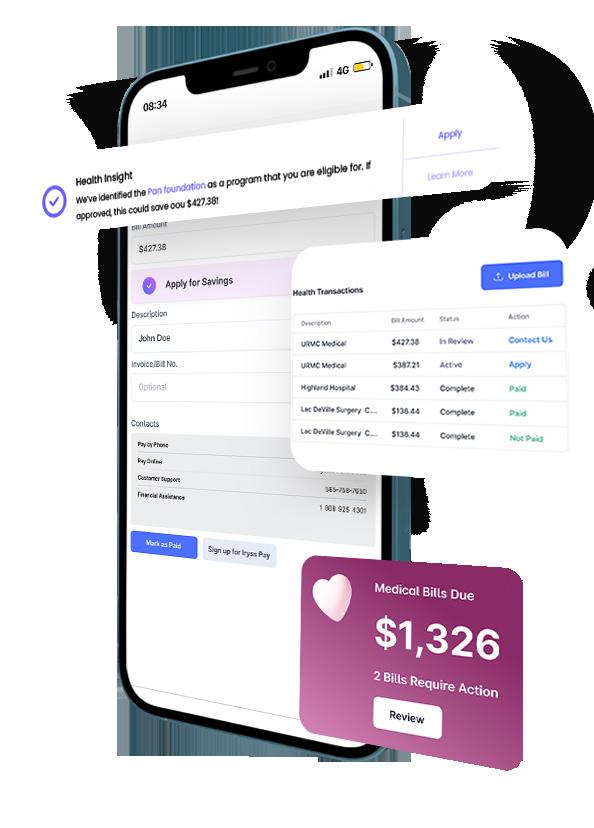
Iryss Is One of the 10 Most Promising Startups in Data Analytics Services for 2023
CIO REVIEW
8/1/23
M&T Bank Presents CEOs You Should Know: Yusuf
Henriques, CEO & Founder, IndyGeneUS AI
IHEART RADIO
8/1/23
startuphealth.com 11

Join our community of Health Transformers dedicated to achieving exponential progress in health at startuphealth.com
AI is Just the Beginning
Founders, doctors & industry-shapers cast a vision for exponential progress in health PREFACE BY UNITY STOAKES
There’s a palpable, pulsating energy coursing through StartUp Health’s community of Health Transformers today. As you flip the pages of this edition of StartUp Health Magazine, aptly themed “Exponential Progress”, we hope you’ll sense it too.
Historically, humanity has been defined not just by its achievements but by its aspirations. The audacity to think bigger, to visualize what doesn't exist, and to carve a path towards it has always set us apart. That’s one of our binding core values and the vision for health moonshots.
Right now, in this era of exponential progress, we urge everyone to ignite their imagination. It’s not merely enough to have powerful tools like AI, big data, and genomics; we must also dream about the myriad ways they can redefine our reality in ways that leap us forward and change health outcomes for all.
And as you dream, remember that the greatest of visions can only be brought to life when shared. Unlimited potential is powered by purpose-driven collaboration. Throughout our journey with
startuphealth.com 13
StartUp Health, we've realized that when passionate minds unite under a single purpose, magic happens. As our world pushes to reinvent the future, it's not the lone genius but the collective power of diverse minds that will propel us forward faster.
To that end, in this issue, we've curated a fascinating assembly of Health Transformers from the StartUp Health community that include patients, scientists, deep thinkers, industry pioneers, and entrepreneurs. We've posed to them a simple yet profound question: How can AI be leveraged in new and exciting ways to cure disease, treat illness, open up access to care, and increase equity? The answers, as you’ll discover, are as varied as they are visionary. They paint a vivid picture of a future where AI, harnessed with purpose and creativity, can leapfrog over legacy health problems.
However, just learning from these insights isn’t enough. As you peruse this collection, let it serve as an inspiration. Let it challenge you to think beyond what AI can do and ponder what it should do. Let's not just be witnesses to this era of exponential progress but be the catalysts who drive it.
Lastly, it's essential to underscore that technology, in its essence, is a tool. It’s our imagination that breathes life into it, and our collaborations that sculpt its impact. The intersection of these human attributes with exponential technologies presents an unparalleled opportunity –an opportunity to harness our very evolution.
To our readers, thinkers, dreamers, doers – we extend an invitation. Let's embark on this transformative journey together. Let’s harness our imagination, collaborate with purpose, and use these fantastic tools at our disposal to address the health challenges that have long seemed insurmountable.
It’s time to be audacious in our aspirations, bold in our visions, and relentless in our collaborations. Together, we can and will achieve our health moonshots.
Unity Stoakes Co-founder, StartUp Health
14 StartUp Health Magazine / EXPONENTIAL PROGRESS FEATURE / EXOPONENTIAL PROGRESS
“When it comes to global health innovation, language and communications can keep a great idea from coming to life. AI can help people from more diverse backgrounds to be able to communicate their business ideas concisely, and with the right audiences in mind.”
Ole Kjerkegaard Nielsen, CEO & Co-founder, GOPen
“Imagine AI as a vigilant ally to human caregivers, together reaching out to our youth in their times of need. In the realm of mental health, this partnership turns data into empathy, silent struggles into shared journeys. It's not about replacing human touch, but amplifying it.”
Daniel Penn, CEO & Cofounder, Tickit Health
“AI can potentially save payors millions of dollars by reducing injuries to patients during routine exams and surgery in women's health. Specifically, it can help physicians identify anatomy more quickly during surgery for conditions like endometriosis, and it can shorten surgery time.”
Adonica Shaw, CEO & Founder, Wingwomen
"Envision a future where your doctor visits centers more on your mental and emotional health rather than just your physical. With AI streamlining the review of a patient’s physical symptoms we provide more time for doctors to address the nuances of human emotions."
 Jeff McCormack, CEO & Co-founder, Iryss
Jeff McCormack, CEO & Co-founder, Iryss
"A patient awakens with a sharp pain in his shoulder. Rather than panicking, he reaches for his iPhone and opens an app that connects him to a virtual doctor for immediate triage. The AI-driven system quickly assesses his symptoms and connects him to the nearest ER doc. The ER doc evaluates the patient through a secure video call and decides that an in-person examination is necessary. With a simple command, the doctor dispatches a state-of-the-art Tesla ambulance equipped with cameras that continuously monitor and send vital signs in real time. As the patient is transported, the doctor orders an aspirin. A specialized printer in the ambulance prints the pill. At the ER, the LLM swiftly pulls all the patient's medical records,
startuphealth.com 15
How can AI be leveraged in new and exciting ways to cure disease, treat illness, open up access to care, and increase equity?
FEATURE / EXOPONENTIAL PROGRESS

displaying them in Virtual Reality (VR) for the doctor's comprehensive review. The doc, now interacting through a robot equipped with visionary technology, can determine the patient's Hemoglobin A1c and other vital labs merely by looking at him. The patient is thoroughly examined, treated, and sent home with the prescribed medications. As the patient goes about his daily routine the following day, an intelligent urinal
analyzes the metabolites in his urine and alerts the doctor to adjust the medication."
Harvey Castro, MD, ChatGPT Healthcare Advisor
“There are at least 90 nutrients and compounds found in our food supply for which there is substantial research on their impact on various illnesses. To establish helpfulness or harmfulness of a given food item as it relates to an
illness we have to execute sophisticated algorithms that will take into account all the relevant nutrients, their role in each illness, quality and quantity of research backing each role. There are hundreds of thousands of unique food-disease interactions. Advancements in AI will allow us to make that data actionable on a daily basis so that food will truly become medicine.”
Mory Bahar, CEO & Founder, Personal Remedies
"Generative AI represents a phase change in healthcare delivery and has the potential to revolutionize healthcare by enabling faster and more accurate diagnosis of disease through data analysis and pattern recognition. With the help of generative AI, healthcare providers can improve patient outcomes and reduce medical errors by predicting and preventing potential health issues before they become serious. The use of generative AI in healthcare can also lead to personalized treatment plans for patients based on their unique history and genetic makeup, ultimately improving overall quality of care."
Toby Cosgrove, MD
Former CEO & President, Cleveland Clinic Member, StartUp Health Board of Directors
16 StartUp Health Magazine / EXPONENTIAL PROGRESS
"In Africa and low GDP nations, healthcare access grapples with scarcity, compounded by few healthcare professionals amidst rapid population growth. Imagine AI-fueled telemedicine breaching remote care barriers, powered by predictive insights curbing disease and healthcare burdens. AI's synergy with healthcare holds the promise to level disparities, democratize access, and illuminate a path to health achievements—manifesting health moonshots into reality."
Ismail Badjie, CEO & Cofounder, Innovarx Global Health
"Perhaps the most riveting intersection between AI and healthcare is in the capacity of smart algorithms to mull through datasets at two or more greater orders of magnitude and

distill insights about the human condition that are otherwise currently still buried and unexamined, or on the other hand, misplaced and misunderstood. What the next generation of healthcarebased AI promises is in its generative power to see the forest for the trees and the trees for the forest, to understand us to such depths that it can anticipate our needs and prepare the ground with its prognosticative lens to perceive in years, if not decades, to steer us towards our optimum health."
Amir Bozorgzadeh, CEO & Founder, Virtuleap
"Generative AI is able to summarize important findings, draft notes, and rephrase. Take it a step further and imagine an app for patients to get interpretations of their labs,
with the ability to ask follow-up questions. No more barriers for everyone to access top care."
Yair Saperstein, MD, CEO and Co-founder, AvoMD
"Imagine a future where AI technology helps your doctor truly understand your diabetes in the context of your everyday life rather than in the context of glycaemic control."
Katharine BarnardKelly, PhD, Chief Science Officer & Co-founder, Spotlight-AQ
“AI-powered chatbots, designed for triage and pre-diagnosis, can effectively guide patients to the appropriate level of care. This not only streamlines the healthcare delivery process but also substantially enhances its efficiency and scalability.”
Cristian Pascual, CEO & Founder, Mediktor
startuphealth.com 17
exercise and diabetes: 1) preventing hypoglycemia during exercise by ensuring safe glucose range to start exercising; 2) predicting hypoglycemia during the post-exercise recovery period; 3) motivating individuals to start and maintain an exercise training program to reach their individual fitness goals."
Federico Fontana, PhD, CEO & Co-founder, Enhance-d
“AI is revolutionizing our capacity to harness massive datasets for personalized care. These models, trained on extensive DNA datasets without pre-set assumptions, unravel intricate patterns from base pairs to higher-order structures and functions. This learning fosters novel insights into DNA-trait associations and potential new

"One of the least talked about epidemics is loneliness among seniors. Large language models will be able to act as customized “virtual home health assistants” that will talk to thousands of patients a day in a customized, empathetic manner for less than twenty cents an hour! Similarly, what now exists at Amazon, Google, Netflix on the retail side, e.g. monitoring all your viewing and buying habits and immediately guiding you to the next TV show or book based on your history, personality and keystrokes, will now be utilized to keep you healthy! Next step is to make sure that we are selecting and educating humans to be better humans than the robots and not just memorizing formulas that AI will do much better than us."
Stephen Klasko, MD Former CEO, Jefferson Health
biological mechanisms. Generative AI can even synthesize new DNA sequences based on learned patterns, offering a tailored approach to meet the
urgent needs of rare disease patients globally.”
Joshua Resnikoff, CEO & Founder, TMA Precision Health
18 StartUp Health Magazine / EXPONENTIAL PROGRESS
“AI can drive precision health equity for the future by ensuring that greater diversity of clinical trials participants is included in the data aggregation, algorithms that are trained to identify diseases. This diversification of dataset is critical to the digital transformation that will help leapfrog legacy data and inherent biases that currently exist.”
Yusuf Henriques, CEO & Founder, IndyGeneUS AI
"AI in healthcare could lead to AI doctors that diagnose and treat patients remotely, using natural language processing, computer vision, and robotics; AI assistants that can generate personalized health plans, prescriptions, and reminders for patients, using reinforcement learning and data mining; AI researchers that can discover new drugs, therapies, and vaccines, using generative adversarial networks, deep learning, and bioinformatics."
Howard Rosen, Founder, LifeWire
"AI provides new opportunities to actively engage patients as valuable members of the disease research and development cycle. By using intelligent, personalized approaches to monitoring, data analyses, and targeted interventions in all areas of the health journey, we can partner with patients in ways that have never been done before."
Lynda Brown-Ganzert, CEO & Co-founder, RxPx
"As we delve into the realm of AI, it becomes our compass to navigate uncharted territories, unveiling the intricacies of its components and crafting a future where AI evolves from expert to mentor, nurturing a new generation of experts, human and machine alike."
Guilherme Berardo, CEO & Co-founder, Sami AI holds the promise of re-humanizing healthcare. By handling intricate tasks, it reduces administrative strains, letting providers deeply connect
with patients. AI's prowess in data analysis helps pinpoint health disparities, championing health equity by ensuring tailored care for all, regardless of background. Additionally, AI-driven solutions transcend geographical barriers, democratizing healthcare access."
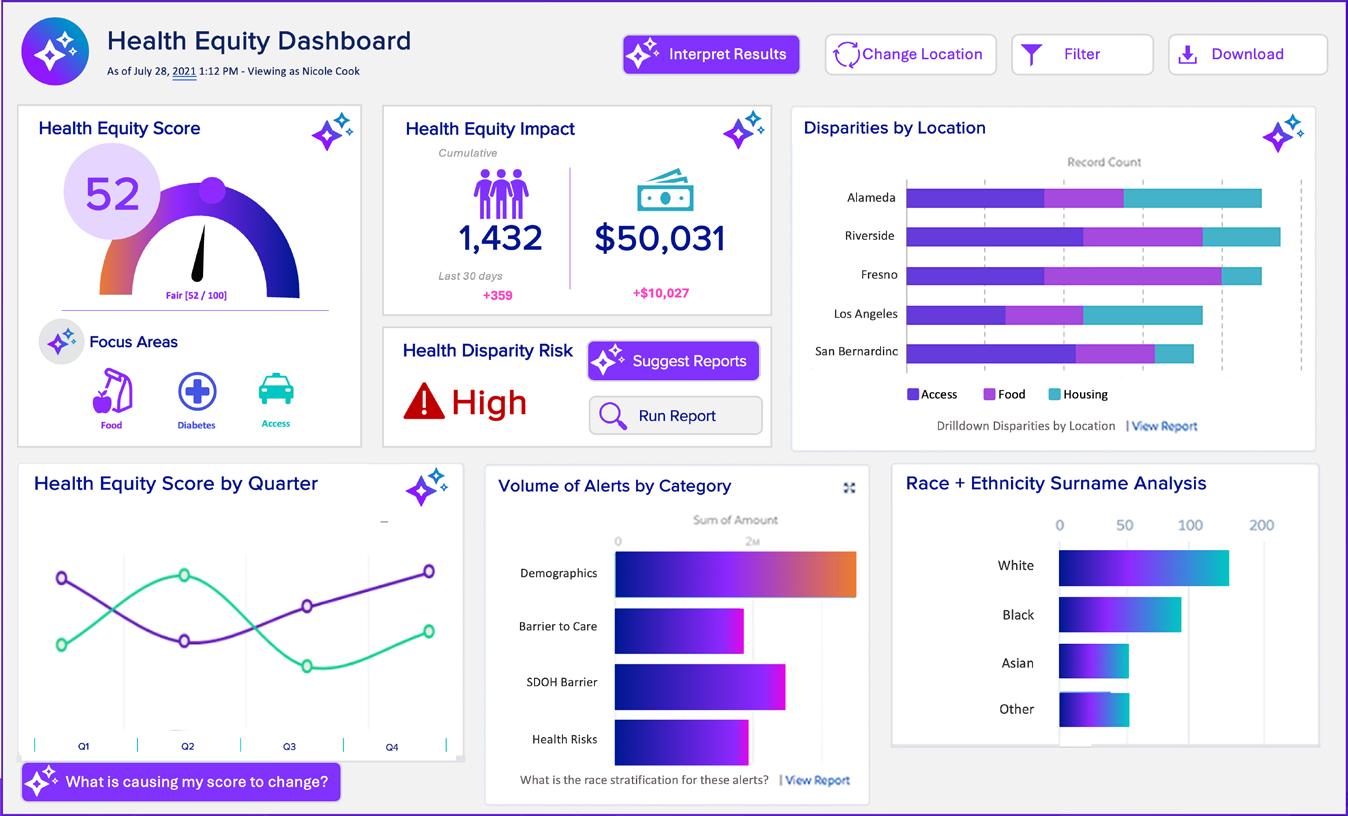
Nicole Cook, CEO & Founder, Alvee
"Generative AI chatbots can be used to assist patients in completing the risk assessments associated with their Annual Wellness Visit and providing 24/7 access to healthcare information and assistance. These chatbots will be key to enabling ease-of-use for the older population who we are serving."
Gail Port, CEO & Cofounder, GeroHealth
"Imagine a world where AI is being used to proactively scan sources like medical records, exercise, and sleep data, as well as information from your smart home and car to gain insights on your
startuphealth.com 19
health and provide early detection of health or neuro-developmental conditions. And not just for you, but for your children and others in your care."
Herman Lindvelt, CEO & Co-founder, Augmental Technologies
"AI will help identify the molecular dance of genes, proteins, and metabolites, rewriting the narrative of healthy longevity. AIpowered nanobots can restore health at the cellular level and offer real-time guidance for better health. Health equity research will benefit from predictive analytics regardless of ethnic background and provide the fullness of wellness to all."
Keshav K. Singh, PhD, Chief Scientific Officer, Yuva Biosciences
"AI can revolutionize cancer patient outcomes. By analyzing vast datasets, AI can uncover hidden patterns, enabling more accurate diagnoses and personalized treatment plans. It empowers
oncologists with predictive insights, anticipating disease progression and optimizing interventions. AI-driven algorithms can enhance decision-making, suggesting tailored therapies based on patients' unique profiles, genetics, and treatment responses."
Luis Santiago, CEO & Founder, Pegasi
"Imagine a world where individuals, residing in remote regions effortlessly access a “Genomic Guardian” app. With a simple DNA sample, AI-driven analysis swiftly unveils the individual’s genetic landscape, foreseeing risks, and empowering them with personalized recommendations. Health disparities dissolve as this democratized approach extends globally, offering everyone, regardless of location, a chance to proactively safeguard their well-being."
Dipu Patel, Vice Chair of Innovation, Department of PA Studies, University of Pittsburgh
"In addiction treatment we are beginning to see AIenabled wearable diagnostics that can predict craving episodes before they happen. By pairing this technology with intelligent drug delivery systems we can detect a craving before it occurs, notify the patient to use their inhaler, and in real-time optimize the dose of medicine delivered through the inhaler to match the severity of the craving we’ve detected."
Dalton Signor, CEO & Cofounder, Miist
"AI has the possibility of informing us about important relationships related to overall health and stands to completely revolutionize how we understand, care for, and even heal people. In terms of caring for loved ones, AI has the potential to correlate information from user interaction and alert us of potentially dangerous conditions that may previously have gone unnoticed for a longer period of time."
Avanlee Christine, Founder & CEO, Avanlee Care
20 StartUp Health Magazine / EXPONENTIAL PROGRESS FEATURE / EXOPONENTIAL PROGRESS
"The most obvious, immediate and pragmatic way we can use AI is to automate existing, well-defined processes, leaving the humans in the healthcare system free to fill the roles that only humans can perform: listening and empathizing, asking questions based on shared experiences, and responding to all the complexities and individual idiosyncrasies of the patient or their condition. Ideally, the money saved can be used to improve the pay of the clinicians and caregivers - and the time saved can give them more time to listen and respond.
Long run, AI can help us

"We are ushering in a new decade of transformation in health care, one that moves away from siloed data to radical interoperability. This future will be based on three Health IT pillars: digital
not just with diagnoses and treatments/cures, but it can help us create and analyze counterfactuals. With those, we can see not just the longterm impact of an intervention (whether a clinical treatment or something outside the healthcare system, such as better child care, housing, a cleaner, safer environment), but to compare it to what would happen otherwise. And that should help us, as a society, to start investing upfront in human health and well-being, rather than wait to fix it with expensive, imperfect healthcare that can never undo all the damage of waiting until it’s too late."
Esther Dyson, Angel Investor & StartUp Health Impact Board Member
identity, interoperability and continually-updated, person-centered health records."
Linda Van Horn, CEO & Founder, iShare Medical
"AI analyzes patient data, predicting disease risk and progression, enabling timely interventions. AI guides treatment decisions by forecasting individual responses to therapies, minimizing side
startuphealth.com 21
effects. Predictive modeling streamlines clinical trials by identifying ideal candidates, expediting drug development. AI integrates diverse data sources, offering a holistic view of patient health and disease evolution. AI anticipates drug-related risks, facilitating early risk management in personalized treatment plans."
Christian Dansereau, PhD, CEO & Co-founder, Perceiv AI
"Imagine that as a young adolescent all your personal data has been me-
thodically collected over time and that, presently, seems to have no relationship to any future concern whatsoever. Now imagine that data from millions of individuals whose data patterns are found to “correlate” tightly to yours is examined, with the only difference being they are older than you. Now for the magic of AI… which will engage in “time travel” and return with a prediction of when you might first present with the early symptoms of a disease or disorder – essentially a model of your “future self” – and best of
all, what to do and NOT to do to avoid it."
Kevin Rogers, CEO & Founder, MoodMD
"Mobile Medicine –which encompasses emergency medical services, fire services, nonemergency medical transportation, critical care transport, and community paramedicine -- is called "Safety Net Medicine" by those among us who support its professionals. The power of artificial intelligence in Mobile Medicine is to ensure that those who cannot speak
22 StartUp Health Magazine / EXPONENTIAL PROGRESS
for themselves -- due to injury, disability, cultural barrier, or even age -- are known by those who run toward the crisis and want to provide the most informed care possible. Imagine the impact of arriving at the scene of a crash and already knowing the special health needs of the children who may be in the vehicle, even if his or her parent has been injured and cannot describe their circumstances -- then knowing which facility is best suited to care for the child, what their healthcare wishes are (so they can be honored), and who else needs to know what the responders saw and did...and automatically starting the flow of information to the next link in the care continuum."
Jonathon Feit, CEO & Cofounder, Beyond Lucid Technologies
"The status quo is broken in speciality and primary care. AI can be leveraged to power technology solutions that positively
address burnout and turnover for physicians and staff. By promoting transparent pricing and eliminating repetitive tasks, redundant documentation, and overly complex billing, we are just starting to see the ways that AI is contributing to quality care, better access, and patient satisfaction. Imagine the impact when high value use cases are broadly deployed.
Darrell Atkin, VP Marketing, HealthMe
"AI can allow us to objectively assess brain phenomena that were previously only accessible via subjective measures. This advancement puts mental healthcare on even ground with the rest of medicine, and will allow for advancements in mental healthcare that were previously unimaginable."
Bechara Saab, PhD, CEO & Co-founder, Mobio Interactive
"AI can help address the needs of people 65 and
older with Alzheimer’s or other forms of dementia by helping us understand their stories and care preferences--without difficulty or delay. It can allow us to automatically interview patients and create a personal bio that helps providers understand the person holistically, beyond their physical medical needs. The person’s story belongs in their care."
Beth Sanders, CEO & Founder, LifeBio
"Medical imaging powered by AI enables swift and accurate diagnoses, bridging geographical gaps in specialized care. Telemedicine, driven by AI-driven chatbots and diagnostics, provides remote healthcare access to marginalized populations. Predictive analytics anticipate disease outbreaks and resource needs, aiding proactive intervention."
Alex Guastella, CEO & Founder, Quick’rCare
startuphealth.com 23
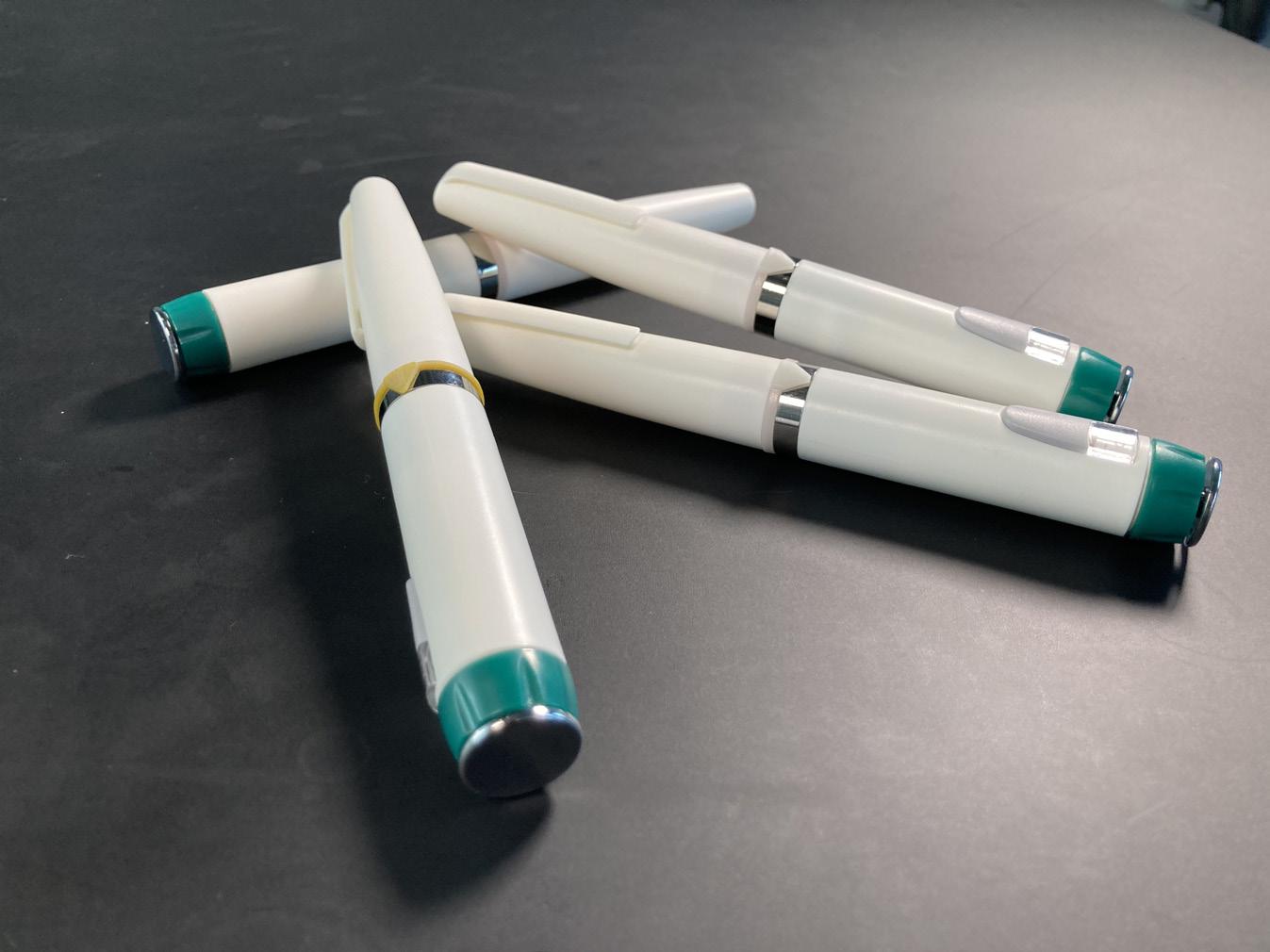
Meet the First Members of the T1D Moonshot Community













StartUp Health launched an entrepreneurial mastery program designed to help T1D innovators achieve their health moonshot.










The program, anchored by a program-related investment from The Helmsley Charitable Trust, has already welcomed more than 20 companies, with more joining every month. Learn more at startuphealth.com/t1d



24 StartUp Health Magazine / EXPONENTIAL PROGRESS
HEALTH MOONSHOT NEWS
Abvance Therapeutics
abvancetherapeutics.com
Abvance Therapeutics is dedicated to improving the lives of individuals with metabolic disease through innovative treatments. The company was founded in 2016 around breakthrough research exclusively licensed from Vanderbilt University and is led by CEO & Cofounder David Maggs, MD, an endocrinologist with 30+ years of experience in multiple pharmacological platforms and device programs targeting rare and common diseases. Co-founder & Scientific Advisor Alan Cherrington, PhD, a professor of diabetes research at Vanderbilt is a worldwide authority on liver glucose metabolism, and Steve Daly, COO, brings 30 years of experience in commercialization and product development, including 18 years in diabetes and metabolism. Their flagship product, ABV100, is a short-acting insulin and glucagon, which offers multiple product forms for both T1D and T2D. Notably, Abvance has completed a human study that validates the core concept, showing that co-administering insulin and glucagon provides protection against hypoglycemia without worsening hyperglycemia. The Abvance team was referred to StartUp Health by The Helmsley Charitable Trust.
Balance Health
balancehealthdiabetes.com
Pete Lomas, CEO & Founder of Balance
Health, is a Sydney-based serial entrepreneur. Living with Type 1 diabetes himself, Pete is driven to make a difference in the lives of people with diabetes through design-driven products and solutions. Balance Health is dedicated to unlocking expert diabetes clinical wisdom and making it easily accessible whenever and wherever it’s needed. Prior to launching Balance Health, Pete founded Not Just a Patch, a CGM patch business that now sells in 65 countries. Notably, it has become the sole CGM patch brand available in Walgreens and CVS pharmacies across the US. Pete’s commercial experience at Novartis, Janssen, and Abbott, spanning over a dozen years, further enriches his expertise. Craig Cooper of the Swiss Diabetes Fund referred Pete to StartUp Health.
Bulsai website coming soon
Bulsai, founded by Bill Ervin, a Type 1 diabetic with 30 years experience in sales and business development at Citibank and Keller Williams, utilizes ultrasound and AI to accurately ascertain the ideal placement and depth for insulin injections—akin to a body stud finder. The
startuphealth.com 25
LEARN MORE AT STARTUPHEALTH.COM/T1D
Bulsai technology guarantees precise insulin delivery, heightened absorption, and improved glycemic control, resulting in decreased risks of complications such as cysts, scar tissue, Lipohypertrophy (LH), and hospitalizations. The device will offer a cost-effective solution for insulin-dependent individuals, thereby minimizing expenditures on insulin and supplies. Following a comprehensive market analysis, Bulsai is actively advancing toward the development of its inaugural prototype.
Diatech Diabetes
diatechdiabetes.com
Diatech Diabetes, co-founded by John Wilcox and Luis Blanco during their senior year at Florida State University, is an AI-powered infusion monitoring company. Their flagship product, SmartFusion, is revolutionizing infusion set failure detection through an app and algorithm. John, the CEO and a Type 1 diabetes patient since his ninth birthday, conducted clinical research in pediatric endocrinology at Tallahassee Memorial HealthCare and contributed to diabetes technology research at FSU’s College of Medicine during his undergraduate studies. Luis Blanco, the CTO, has experience at Biosense Webster (a J&J Medtech company) on the clinical accounts team and conducted research at the joint FAMU-FSU College
of Engineering. Supported by advisors (currently or previously) affiliated with Stanford Medicine, Joslin Diabetes Center, Insulet, University of Houston, and T1D Exchange, Diatech Diabetes has achieved milestones including a preclinical animal study with 97% accuracy, a NIH/SBIR Phase 1 grant, and the granting of a US patent for their sensor system. The team was referred to StartUp Health by Craig Cooper of the Swiss Diabetes Fund.

26 StartUp Health Magazine / EXPONENTIAL PROGRESS
HEALTH MOONSHOT NEWS
Eran Atlas, Moshe Phillip, MD, and Revital Nimri, MD, the co-founders of DreaMed, based in Israel, are revolutionizing diabetes care with their AI Clinical Decision Support System (CDSS). Their clinically-proven and FDA-cleared technology enables a significant increase in the availability of personalized advice from expert endocrinologists for diabetes patients. DreaMed has received multiple grant awards from the Helmsley Charitable Trust. Eran, the CEO, brings over 13 years of leadership experience in diabetes-related technology, having served as the R&D Director for the MD-Logic Artificial Pancreas Project at Schneider Children’s Medical Center.
Dr. Phillip, Chairman & CSO, has over 25 years of expertise in endocrinology and pediatrics, currently leading the Institute of Endocrinology and Diabetes at Schneider Children’s Medical Center. Additionally, Moshe is the Vice Dean of R&D and Endocrinology Lecturer at Tel Aviv University and co-chairs the Advanced Technologies and Treatments for Diabetes Conference. Dr. Nimri, CMO of R&D, is a highly regarded pediatric endocrinologist and diabetes expert who has contributed to the development of automated insulin delivery systems, including the MD-Logic closed-loop system and other decision support systems.
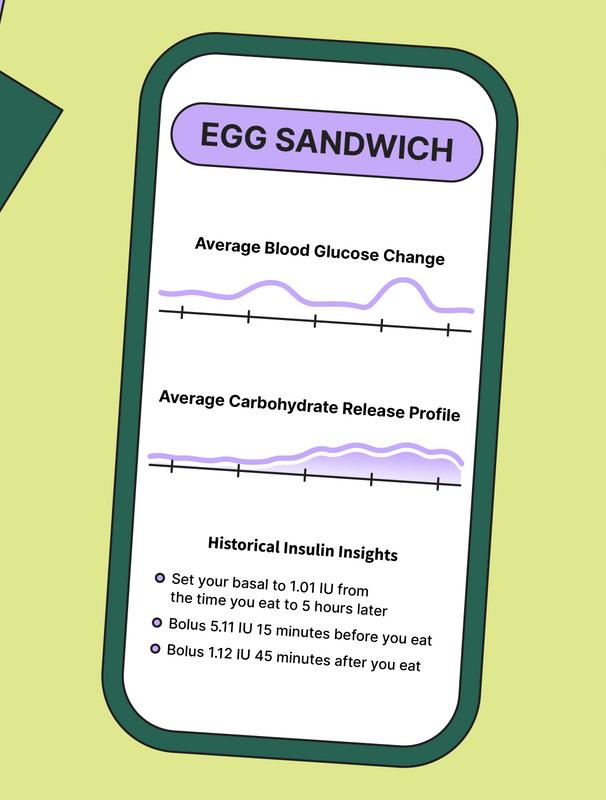
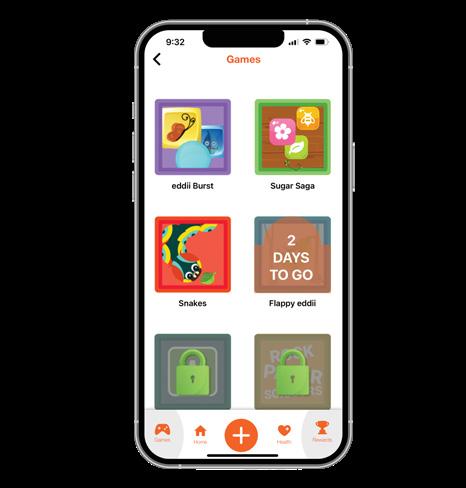
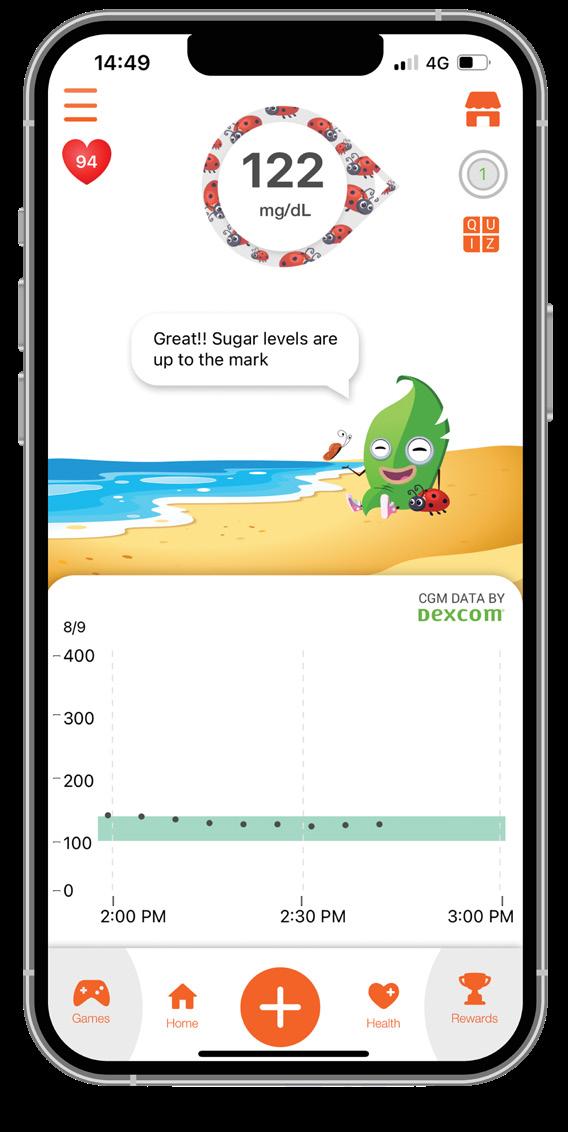
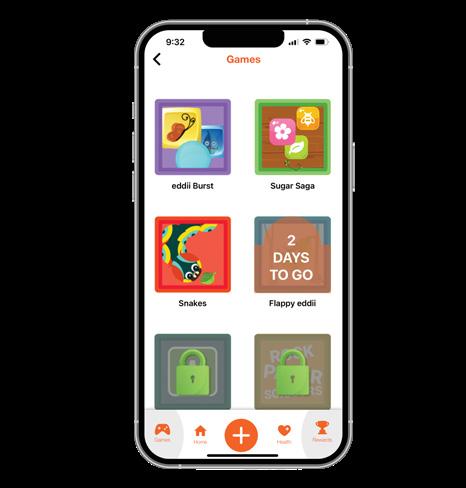
Farhaneh Ahmadi, PhD, co-founded Eddii, a personal health companion aimed at making diabetes management more fun and engaging in 2019. Drawing from her personal experience living with Type 1 diabetes, she teamed up with Alonso Lucero, who brings over a decade of healthcare operations expertise from Strategy& PwC and Monitor Deloitte. Eddii's innovative approach combines gamified real-
startuphealth.com 27
DreaMed dreamed.ai
Eddii eddiihealth.com
LEARN MORE AT STARTUPHEALTH.COM/T1D
time glucose monitoring, software-driven conversations, and clinical interventions to deliver a highly personalized diabetes management solution. The results so far have demonstrated a 5% improvement in children's time-in-range, along with enhancements in the emotional well-being of families. Eddii recently announced a strategic partnership with Dexcom, enabling real-time CGM readings to seamlessly integrate into their app.
Enhance-d enhance-d.com
Enhance-d co-founders Federico Fontana, PhD, Felipe Maturana, PhD, Fabio Saviozzi, and Sam Scott, PhD, are developing the ultimate digital hub for diabetes self-management. With a shared background at Supersapiens, a biowearable technology company offering real-time glucose insights, Federico, Felipe, and Fabio joined forces with Sam to launch Enhance-d in 2022. The company’s Scientific Advisory Board is comprised of top experts from academia, research, pharma, and former professional athletes with T1D. In recent years, Federico and Sam served as Head of Performance and Head of Research, respectively, for Team Novo Nordisk, the world’s first all-diabetes professional cycling team. Deniz Dalton, T1D Program Officer at the Helmsley Charitable Trust, referred Switzerland-based Enhance-d to StartUp Health.
Greens xplosionlive.com
Greens co-founders Isis Ashford and Kehlin Swain, engineers with user design experience from NASA and Intel, are on a mission to empower children with diabetes. Their flagship product is a mobile app that uses photovision analysis to help kids manage their glucose level. Supported by advisory board members from Children’s of Alabama and UTHealth Houston, the company has launched a paid pilot with Children's of Alabama and secured a funding award from the Air Force SBIR program. The team’s long-term vision is to impact the highly underserved market of Medicaid patients who struggle with chronic disease(s). GO-Pen
go-pen.com
GO-Pen co-founders Ole Nielsen, PhD, and Michael Hansen aim to enhance the lives of people with diabetes through an affordable and convenient insulin pen. Ole brings valuable expertise from Novo Nordisk and Coloplast, while Michael holds 18 patents related to insulin pen development along with an 18year tenure at Novo Nordisk. GO-Pen has secured a patent in Denmark with
28 StartUp Health Magazine / EXPONENTIAL PROGRESS
HEALTH MOONSHOT NEWS
patents submitted in 15 other markets and has raised over $6M from investors and grants, including funding from the European Innovation Council. The GOPen team was introduced to StartUp Health by the Diabetes Center Berne at the 2022 DiabetesMine Innovation Summit.

In-Range Animation inrangeanimation.com
In-Range Animation simplifies diabetes education with captivating microlearning animations, empowering patients to effectively manage their health. The platform provides instant access to both foundational and advanced diabetes concepts, allowing providers to prioritize personalized care. Through anima -
tion, In-Range transforms the diabetes journey, driving patient engagement, fortifying provider connections, and enhancing health outcomes. Co-founder Neil Israel, a Type 1 diabetic since 1980, leads project management and storytelling, complemented by his wife Suzie Israel's expertise in website development and design.

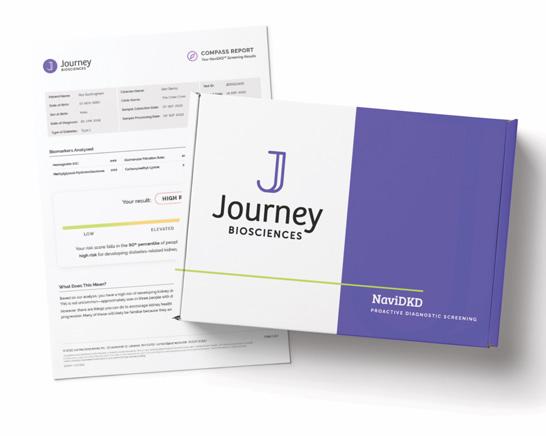
Journey Biosciences journeybio.life
Adam Graybill and Dr. Paul Beisswenger, the duo behind Journey Biosciences, have introduced an innovative predictive test called NaviDKD. This stateof-the-art test gauges the risk of kidney complications arising from diabetes. Gaining recognition for its unparalleled accuracy, the NaviDKD test has secured patents in both the US and Europe. Its credibility is further reinforced by the successful results from four longitudinal outcome studies.
Graybill comes from a background in sales and go-to-market roles at Cardinal Health, notably in the diabetes and medical device sectors, and has also held a significant position as a board member of the Northeast Ohio chapter of JDRF.
startuphealth.com 29
LEARN MORE AT STARTUPHEALTH.COM/T1D
Dr. Paul Beisswenger, a retired endocrinologist, boasts four decades at the Dartmouth Geisel School of Medicine. His expertise lies in researching the roots and genetic underpinnings of diabetic complications.
LovedBy
lovedby.com
LovedBy, founded in 2019 by Matthew and Victoria Farrar, introduces Nudg, an engagement platform aimed at enhancing the well-being of young individuals with diabetes. The platform seamlessly integrates with digital tools and wearables, eliminating manual tracking and the clinical workflow empowers pediatricians to prescribe tailored content, and social platform integration improves patient knowledge and adherence. Notably, LovedBy partners with hospitals including InterMountain Primary Children's, CHOC, and CHLA. Led by Matthew Farrar, a classically trained industrial designer with 25+ years in product design (at Apple Pay and Arrive Electric Vehicles),
LovedBy recently launched in the UK with Dexcom, and are set to launch in the US in early 2024, targeting 50k adolescents through Dexcom's network. The LovedBy team was introduced to us by Claudia Graham, a member of our T1D Moonshot Impact Board.
 Minutia minutia.co
Minutia minutia.co
Katy Digovich, CEO & Co-founder of Minutia, brings a personal connection to Type 1 diabetes (T1D), having lived with the condition for over 25 years. Minutia’s mission is to develop a nextgeneration cell therapy as a widely applicable cure for T1D. Minutia focuses on creating intracellular nucleic acid biosensors and regulators in stem cell-derived transplants, starting with insulinproducing cells, to pursue a cure. Before founding Minutia, Katy played a pivotal role in launching the Global Diabetes Program at the Clinton Health Access Initiative. With extensive experience in creating diagnostic tools across 40+ countries at the intersection of technology, health, and underserved communities, Katy and the Minutia team have demonstrated the efficacy of their robust insulin-producing cells and successfully de-risked their platform. Notably, they achieved a successful proof-ofconcept in a Phase 1/2 clinical trial, led by renowned researchers at UCSF. The
30 StartUp Health Magazine / EXPONENTIAL PROGRESS
HEALTH MOONSHOT NEWS
company has raised $4M+ in funding and received $3M in grant awards from esteemed organizations such as JDRF, CIRM, and NIH. Katy was referred to StartUp Health by JDRF.
Pramana Pharmaceuticals
pramanapharma.com
Pramana Pharmaceuticals brings together a scientific team with a wealth of experience in leadership roles at global pharma companies such as AstraZeneca, GSK, Janssen, Merck, and Shire and academic training and research experience at Health Canada, Mayo Clinic, Royal College of Physicians of Canada, University of British Columbia, University of Maryland School of Pharmacy, and University of Pittsburgh School of Medicine. With over 25 years of senior investment advisory and capital markets experience, CEO Diane Alexander leads Pramana in their development of a groundbreaking proprietary class of small molecules targeting diabetes and metabolic disorders. Tracy Sims, Executive Director at Eli Lilly, referred Diane to StartUp Health.
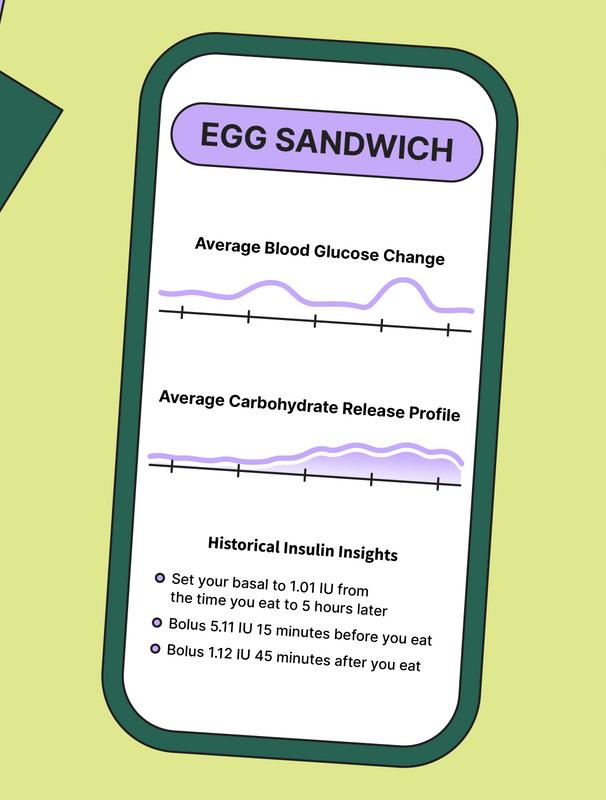
Replica Health replica.health
Sam Royston and Brad Jacobson are the co-founders of Replica Health, a search
and recommendation engine for metabolism, designed to address critical issues faced by Type 1 diabetics. Replica Health integrates previously unused data from CGMs, insulin pumps, Apple Health, and location data to develop a machine learning-driven model for understanding and analyzing metabolic history, with tools for providers to enhance treatment. Currently in prototype mode with ongoing beta testing, Replica Health will be launching to the public soon. Sam is a Type 1 diabetic, who deeply understands the disease, and a machine learning engineer with training from the Courant Institute at NYU, specializing in blood glucose prediction algorithms and data visualization. Brad studied Human Centered Design and Engineering at the University of
startuphealth.com 31
LEARN MORE AT STARTUPHEALTH.COM/T1D
Washington and has extensive experience leading product management, design, and research work streams for Fortune 500 companies.
Rezq Bio
rezq.bio
The founding team of Rezq Bio is on a mission to cure localized autoimmunity, beginning with Type 1 diabetes. CEO Arjun Hattiangadi brings 13 years of experience in investing, operating, and business development from UPMC’s commercialization and venture capital arm. David Finegold, MD, Chief Medical Officer and Professor of Human Genetics at the University of Pittsburgh, has overseen more than 20 clinical trials including a Phase 1a trial of Rezq’s cell therapy. Nick Giannoukakis, PhD, Acting Chief Scientific Officer and Lead Researcher at the Institute of Cellular Therapeutics at Allegheny General Hospital, is an expert in tolerogenic dendritic cell therapy for T1D. Scientific Advisor Massimo Trucco, MD, Head of the Institute of Cellular Therapeutics at Allegheny General Hospital, has received international recognition for his work on understanding and curing diabetes. Arjun was connected to StartUp Health during his time at UPMC.
SmartStart Health introduces an innovative patient education app tailored for individuals with diabetes using CGMs. CEO & Founder, Melissa Holloway, was diagnosed with Type 1 diabetes in 1994 and has two decades of healthcare industry expertise at Abbott Datamonitor. The platform personalizes content for patients based on specific CGM-related factors such as age, duration of diagnosis, and treatment approach, offering a convenient source of guidance accessible through handheld devices. Currently conducting a proof-of-concept study at an Ohio clinic, the company’s go-tomarket strategy is to significantly reduce the time commitment required from healthcare providers, enabling more effective and meaningful patient engagement. Melissa was referred to StartUp Health by a fellow Health Transformer.
Tribetic, founded by Suzanne Stites and Daniel Donlevie, is a platform focused on enhancing the metabolic health of Type 1 diabetics. Leveraging Daniel's background as a serial entrepreneur and a T1D patient himself, and Suzanne's
32 StartUp Health Magazine / EXPONENTIAL PROGRESS
SmartStart Health smartstart.health
TRIBETIC tribetic.com
HEALTH MOONSHOT NEWS
experience as a CPG marketer and consultant, Tribetic employs scientific principles to drive behavioral change in patients through personalized coaching. Their approach integrates live coaching, data-driven insights, and AI automation, supported by medical and metabolic experts, to holistically improve nutrition, sleep, exercise, and insulin control. By merging human coaching with AI, Tribetic aims to scale health outcomes and provide tailored guidance. Currently undergoing feasibility trials, Tribetic is refining its app and plans a direct-to-consumer launch to validate its innovative approach in the market. The Tribetic team was referred to StartUp Health by JDRF and David Dadick of Propeller.
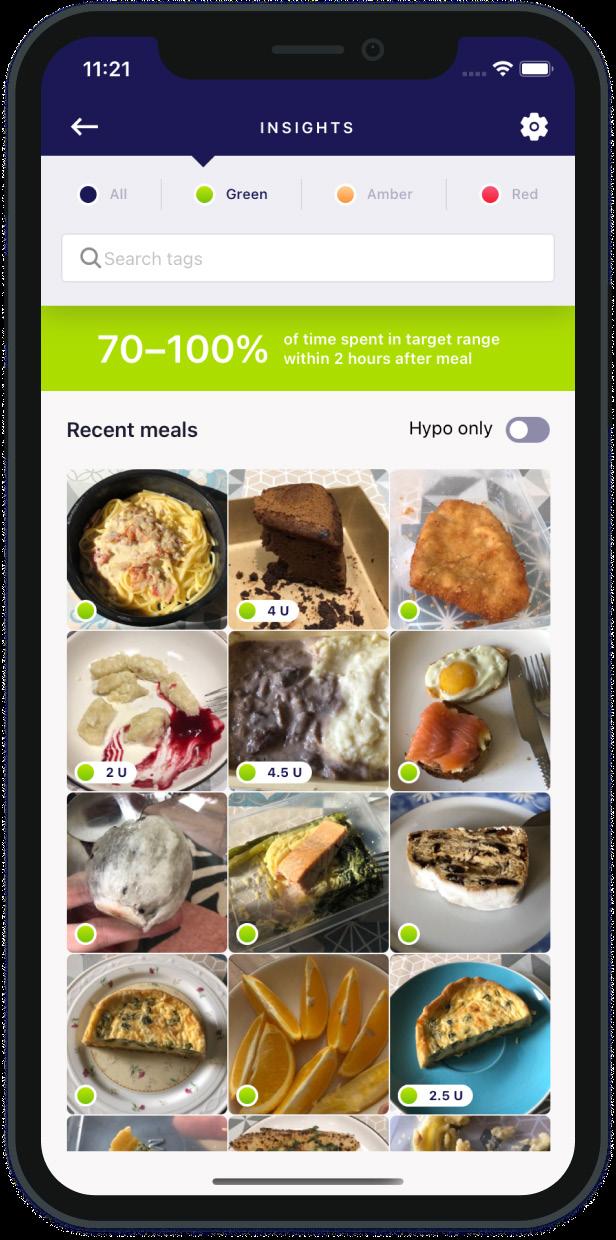
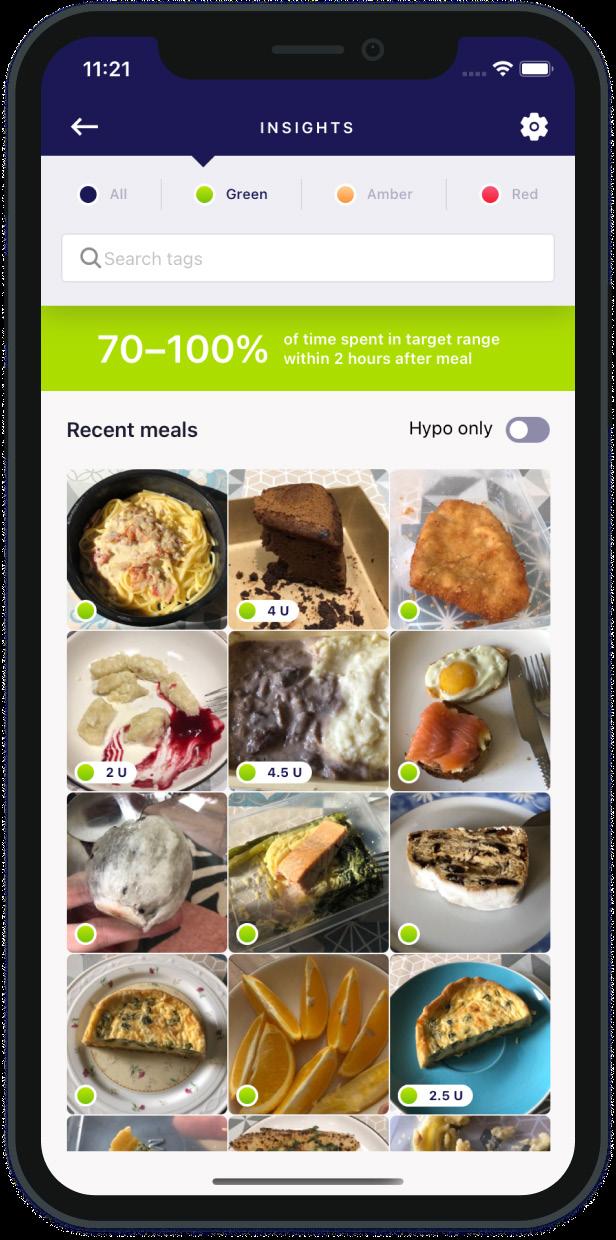
Undermyfork undermyfork.com
With a combined 30+ years of experience, Mike Ushakov and Eugene Molodkin are seasoned entrepreneurs in the tech industry. Their professional collaboration has spanned over a decade, and in 2018 they co-founded Undermyfork, a food diary mobile app catered to individuals with diabetes, using data from CGM sensors. Undermyfork is a Dexcom data partner and has received their CE mark, demonstrating its adherence to European standards of safety, health, and environmen-
tal protection. Rachel Stahl, a dietician at NYP/Weill Cornell Medicine and one of the company’s clinical advisors, referred Mike and Eugene to StartUp Health.
startuphealth.com 33 LEARN MORE AT STARTUPHEALTH.COM/T1D
MEET THE NEWEST HEALTH TRANSFORMERS
Each issue we introduce you to the inspiring founders we invested in recently. Their work addresses a range of health moonshots, from health equity to access to care.
Are you a passionate funder of health innovation? Learn how you can support the next generation of Health Transformers at startuphealth.com

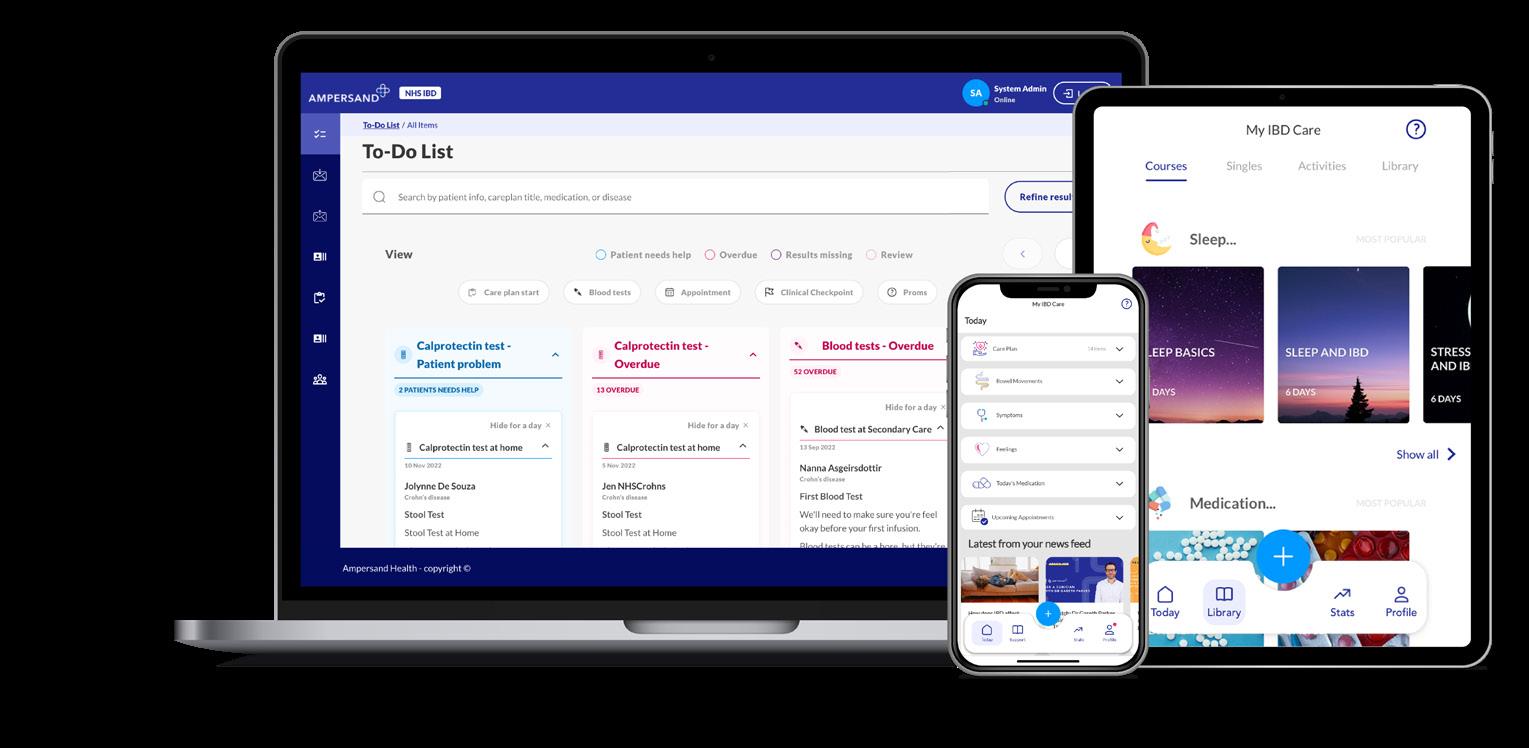
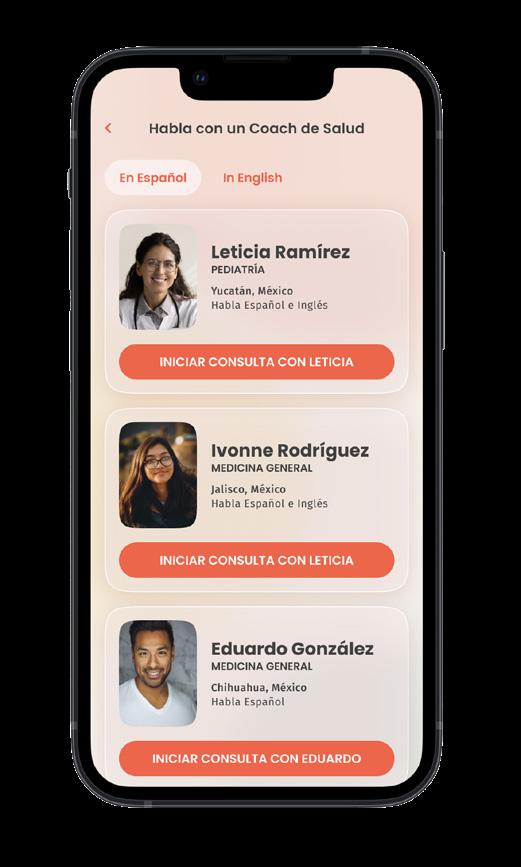
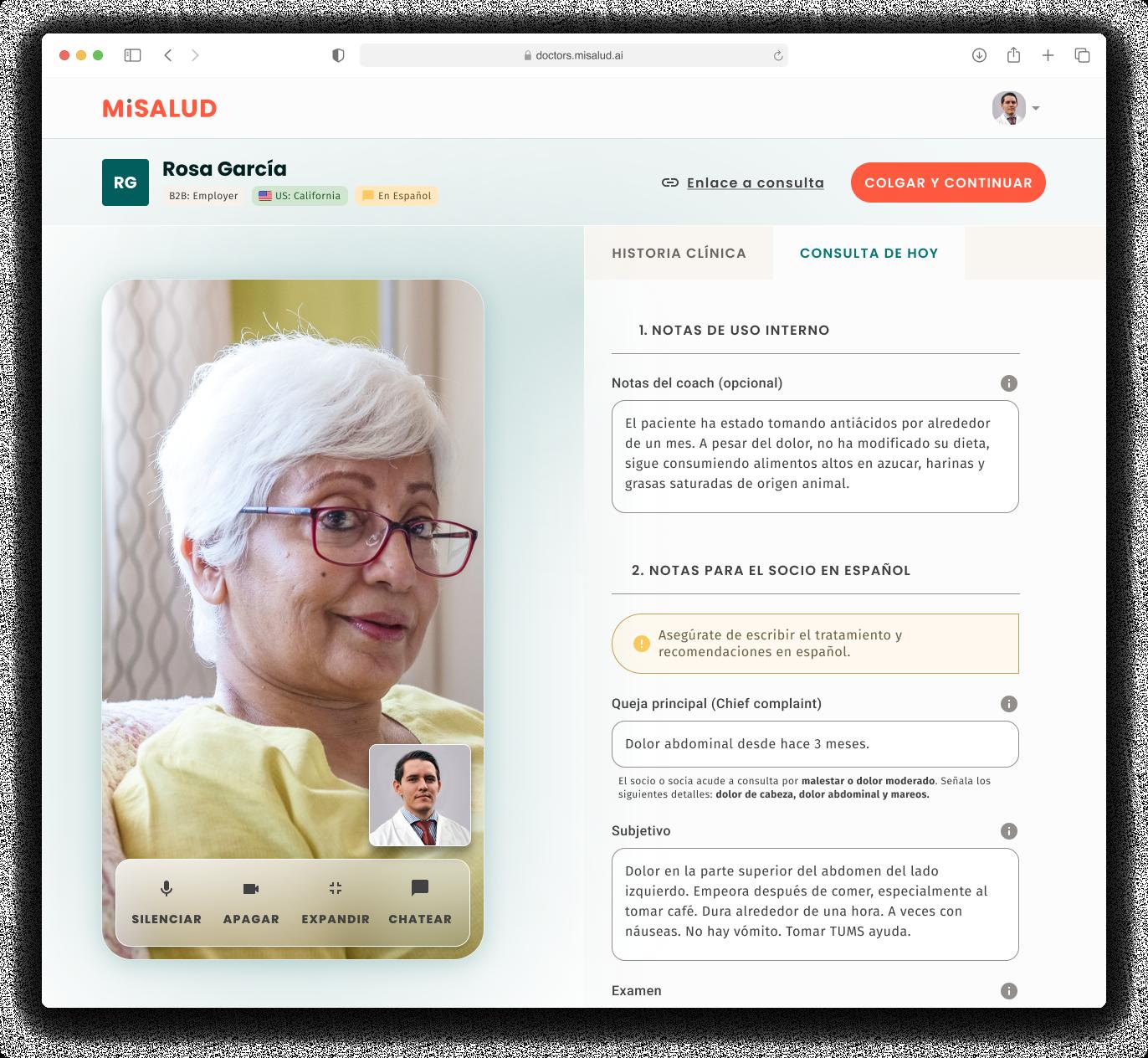
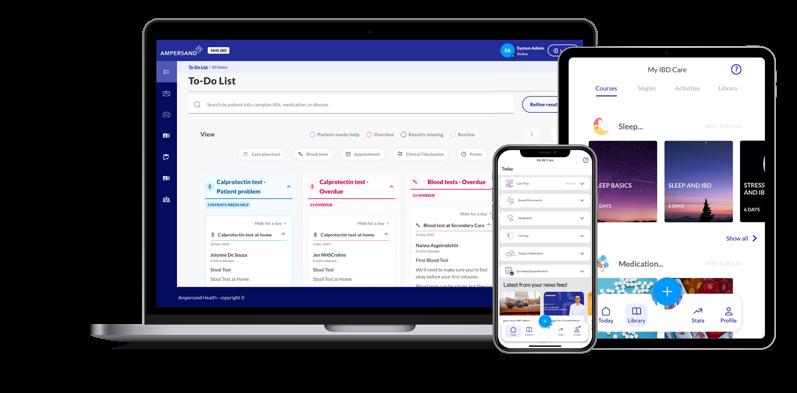
startuphealth.com 35 EDDII BETTERMEAL AI GREENS HANDL HEALTH JOURNEY BIOSCIENCES ALVEE HEALTH AMPERSAND HEALTH DREAMED SANITAS HEALTH INDYGENEUS AI MIIST THERAPEUTICS DIATECH DIABETES JOYDAYS DIFINITY SOLUTIONS MISALUD HEALTH AURASENSE KINOMETRIX EQUALITYMD LUMOS TECH REPLICA HEALTH ABVANCE THERAPEUTICS LASA HEALTH BALANCE HEALTH ENHANCE-D IRYSS GO-PEN HEALTHBOOK+ UNDERMYFORK REZQ BIO MOODMD PRAMANA PHARMACEUTICALS 36 39 42 46 49 52 56 59 62 66 70 73 76 79 82 86 89 92 95 98 101 104 107 110 114 117 120 123 126 129 132

Eddii Helps Children Manage Type 1 Diabetes
Farhaneh Ahmadi, PhD (right) has leveraged her experience as a Type 1 diabetes patient to build a fun, engaging app that empowers children to manage life with T1D.
IImagine for a moment that your child is one of the 64,000 people diagnosed each year in the US with Type 1 diabetes. All of a sudden their life (and yours) will never be the same again. There are hundreds of new things to learn and decide–how to monitor and track blood sugar changes, how to insulin dose, new vocabulary, all the factors besides food and insulin that affect blood glucose, how to interpret nutrition labels, what monitor to use, how to wear it correctly and deal with any chafing or discomfort, how to prepare for a school field trip or a sleepover, and on and on. Every day it’s something different. And every single day it must be managed.
Because managing a chronic health condition involves so much stress and strain, mental health issues often follow a diagnosis. For instance, people with Type 1 diabetes have a higher risk for anxiety and depression. People living with T1D often report how their condition makes them
feel isolated and lonely. Classmates or friends don’t know what it is really like to experience a blood sugar low or vigilantly monitor which snacks they consume at a birthday party. Diabetes distress can also lead to burnout, where a person gets overwhelmed by the constant disease management and stops taking care of themselves.
While medical device companies continually strive to offer better products for monitoring and managing T1D, they offer little support in terms of helping patients and their families navigate the questions, challenges, and emotional landscape of living with the condition. Parents end up constantly prompting and reminding their children to make sure they stay on top of their diabetes management, leading to friction–to children it feels like nagging, to parents it feels like perpetual worry. Either way, it doesn’t help motivate and support the young person as they live with diabetes and adds pressure to an already difficult situation.
ORIGIN STORY
“When you get diagnosed with T1D, you have to start dealing with it every day,” says Farhaneh Ahmadi, PhD. “It never goes away. During the best of your times and the worst of your times, it is right there in front of you.”
Ahmadi was diagnosed with T1D 14 years ago, during the first year of her PhD
startuphealth.com 37
T1D MOONSHOT
MEET THE HEALTH TRANSFORMERS
in biochemistry at Cambridge in the UK. She remembers the incredible challenge it was to learn how to manage the condition while monitoring cells in the middle of a lab experiment or out on the River Cam during rowing practice at 5AM. Once, she had to knock on a neighbor’s door at 1AM, asking for juice when she hit a low and found herself out of stock.
Ahmadi ended up taking a few months off from her PhD to focus on her health and learn how to be insulin dependent. Like many people diagnosed with a chronic illness, she also had to learn to combat the negative thoughts and find the right motivation and support system to take charge of her health. She joined Diabetes UK, found other people who understood the challenges of the condition, big and small, and started to feel a little less alone.
It was this experience, of finding voices that could educate her and guide her as well as validate her feelings and frustrations living with the condition, that led her to imagine an interface that could help provide the same thing to others–something that made living with a chronic illness
more manageable and less isolating.
“It really became the basis for what we created, which revolves around the user not feeling lonely and having a health buddy who is always there with you–who understands the effects of high and low glucose and who helps you manage it and manage your feelings about it.”

After finishing her PhD and spending years as a cancer researcher and then a healthcare consultant in the private sector, Ahmadi was ready to take on the challenge of building the tool she wished existed for herself all those years ago. Her vision was a platform that responded to real-time data, that was clinically-driven and outcomes-focused so that it had a real impact on users’ health, and that motivated its users to take ownership of their diabetes. Could you, she wondered, actually make it enjoyable for a child with T1D to engage with their blood glucose numbers and their health?
UNDER THE HOOD
Eddii is a next-generation diabetes app that helps people living with diabetes track their health. Eddii itself is a virtual in-app character that looks like a vibrant little leaf. Through games and amusing conversation, Eddii engages users in their health, giving them the information and confidence they need to take action...


Scan to read the full story or go to healthtransformer.co

38 StartUp Health Magazine / EXPONENTIAL PROGRESS MEET THE HEALTH TRANSFORMERS / EDDII
NUTRITION & FITNESS MOONSHOT
Founder Swathi Arulguppe Nagendra (pictured) combined her personal chronic disease journey with her love of data analysis to build a platform that delivers clinically-validated, hyper-functional nutritional recommendations to patients suffering from conditions like inflammatory bowel disease, celiac disease, Type 2 diabetes, thyroid disorders, and PCOS.

startuphealth.com 39 BetterMeal AI Delivers HyperPrecision Nutrition Through Better
of
Understanding
the Gut Biome
MEET THE HEALTH TRANSFORMERS
WWhen Hippocrates said “all disease begins in the gut” over 2000 years ago, he certainly didn’t know that one day researchers in the fields of heart disease, neurology, auto-immune disorders, diabetes, cancer, and others, would corroborate his statement. Gut health is exploding as a health area, with good reason: there’s a world of connections being made between the foods we eat (or don’t eat) and their impact on our gut microbiomes and overall health.
These connections are a gut check to healthcare as usual, which manages chronic disease symptoms but rarely gets to the root cause. More and more, doctors and patients are aware that the microbiome–the collection of microbes such as bacteria, fungia, and even viruses that naturally live in and on the body–is a critical part of overall health and wellbeing. What is less clear is how to actually improve and optimize a person’s microbiome in such a way to improve symptoms and even cure disease.
Most people end up taking a onesize-fits-all approach by incorporating probiotics and vitamins into their diet. Unfortunately, this often causes more harm than good. Participants in studies who consumed probiotics for longer time periods were more likely to end up with autoimmune issues. Not every person or health issue requires the amount or the type of bacteria present in these supplements. Without customized gut health recommendations, it’s easy to disrupt the delicate ecosystem that exists to protect
against pathogens, digest food, and develop immunities.
ORIGIN STORY
When Swathi Arulguppe Nagendra was a teenager, she did what most teenagers do: ate what she wanted without thinking about nutrients. By the age of 16, those habits caught up with her. She was pre-diabetic and suffered from polycystic ovarian syndrome (PCOS). She followed the recommendations of her doctors, managing the conditions through various medications and weight loss, but developed gastric conditions that necessitated multiple endoscopies.
“I felt like my life was over,” Nagendra explains. “I was surrounded by doctors, dependent on medication, and wasn’t getting better.”
While at university pursuing her degree in engineering and information science, her conditions flared up again. Nagendra went into research mode, looking for ways to improve her health. That’s when she came across the wealth of research on gut health and started to see the relationship between her diet and her symptoms. She followed a recovery process to calm her inflamed system and tweaked her diet to reduce irritation.
The results were eye opening. She reversed her pre-diabetes numbers and her PCOS symptoms abated. Nagendra began sharing her experience and what she learned about diet and gut health on a food blog, all while building her career as a data scientist. It was through that online nutrition space that she met Dr.
40 StartUp Health Magazine / EXPONENTIAL PROGRESS MEET THE HEALTH TRANSFORMERS / BETTERMEAL AI
Ramya Ram, an obstetrician researcher in Birmingham, England. The two shared a passion for helping people understand interactions between what they ate and their microbiomes.
In 2019, the pair started analyzing food to understand what compounds were present and how they interacted with the gut. Using a databank from over 500,000 patients, they cataloged many food compounds and analyzed unique biomarkers from basic blood and stool tests. From this analysis, they mapped biomarkers related to specific diseases and created a novel algorithm that connects these biomarkers to a precision nutrition plan to provide solutions for five specific health issues: diabetes, thyroid problems, PCOS, celiac disease, and irritable bowel disorders.
The team knew they were onto something big–biomarkers correlated with gut issues tested at 82% proof positive, meaning their solution could reach large numbers of people with greater results. Other gut health companies use their own at-home testing kits that have mixed success rates at detecting what’s happening within a patient’s microbiome. The success rate of their clinical studies meant that the solution they were creating could be applied just through looking at the standard blood panel that gets taken at a patient’s yearly physical, with no need to perform extra tests.
UNDER THE HOOD
“We had one user, a man in his late 70s, who was in constant joint pain due


to an autoimmune disorder. After he went through our program, his pain went down by 80% and he told us he was able to walk comfortably for the first time in years.”
To get started, new users simply upload their existing blood panels into the application, which then decodes and interprets overall gut health. The user begins their healing journey with a simple gut cleanse to repair and replace the protective mucus layer in the digestive system. Then the app acts like a nutritionist that goes with the user, making specific suggestions about meal choices, even when out at a restaurant. Using a comprehensive meal and ingredient database and natural language processing, BetterMeal AI can “read” menus and give the user a score to help choose the best option for them.
After an initial launch in 2020, the company gained traaction this past year in several hospital partnerships. For instance, a pilot program in the UK brought nutritionists and doctors together on their platform to support patients suffering with digestive issues. This collaboration produced an 11% increase in revenue for the hospital, mainly in patient retention. Nagendra attributes the better retention scores to the fact that patients felt truly cared for in their treatment plan...
startuphealth.com 41
Scan to read the full story or go to healthtransformer.co
T1D MOONSHOT
By providing an AIbased digital platform that offers culturallyfocused meal prediction, positive reinforcement, and an inclusive community of care, the Greens app by Xplosion Tech makes adhering to a treatment plan easier for young diabetes sufferers and their parents.
The Greens App Scales Diabetes Management with a Focus on Teens from Vulnerable Communities

42 StartUp Health Magazine / EXPONENTIAL PROGRESS
AA diabetes diagnosis comes with a necessary list of changes to lifestyle and eating habits. Overnight a person must begin thinking about checking their blood sugar levels, changing their diet, and taking insulin.
But changing health behaviors doesn’t happen overnight or after a single conversation with a doctor. In fact, changing habits may be the hardest part of a chronic disease diagnosis. There are a multitude of factors that come into play when it comes from translating clinical best practice into

startuphealth.com 43
a daily routine of disease management.
Some of these factors are cultural. While diabetes can affect anyone, it has hit the Black community the hardest in the United States. According to the American Diabetes Association (ADA) the prevalence of diabetes in non-Hispanic Blacks is 11.7%, versus 7.5% in non-Hispanic whites.
Within the BIPOC and economically-disadvantaged community in the American South, a chasm has opened between what doctors recommend for a patient with diabetes and what patients feel they can carry out on their own. When cultural norms around food run deep, it can be extremely difficult to reconcile “healthy foods” with “tasty foods.” These issues are compounded when the patient lives in a “food desert” where healthy foods aren’t readily available.
The result is a feeling of failure. If a patient can’t quit eating rich foods that have been cultural traditions for generations, they’re demonized. If they aren’t changing habits fast enough, they’re told they must not value their lives. Too often, medical professionals approach chronic disease with an attitude of, “you either want to eat healthy or you’re willing to die,” rather than acknowledging the need for baby steps in habit change. This leads to patients not being honest about the foods they’re eating for fear of recriminations, which then puts their health at further risk and erodes trust between them and their physicians.
Meal tracking apps take care of part of the problem, helping people with diabe-
tes track their food intake and stay on a healthy diet. But checking each piece of food independently is tedious and time consuming. This is particularly challenging when the patient is a teen, and parents end up doing a lot of guesswork.
So how can diet management and food tracking be made easy and accessible while also building a community of care that understands the cultural underpinnings of food and the challenges of behavior change? And for kids specifically, how could diabetes management be less overwhelming and parental concerns over their teen’s wellbeing be alleviated as they navigate this disease?
Founders of the Greens app pulled from their own experiences to solve these challenges.
ORIGIN STORY
Just before the pandemic, electrical engineer Isis Ashford’s father was diagnosed with Type 2 diabetes. He needed to completely change his diet and learn a variety of things he had never done before. It seemed simple enough when talking about it in the doctor’s office but putting these changes into real-life practice felt almost insurmountable, especially when part of this lifestyle change required remembering the nutritional information of the foods he was eating to understand how much insulin he needed to take and when to take it.
There was also a cultural disconnect from what the doctor was prescribing and what Ashford’s father was used to doing. Being from a small town in Alabama,
44 StartUp Health Magazine / EXPONENTIAL PROGRESS
THE HEALTH
/ GREENS
MEET
TRANSFORMERS
Ashford’s dad grew up eating and loving greens of all kinds: collard, mustard, turnip, etc. Kale, however, was not one of them. Doctors kept pushing Ashford’s father to eat kale, but no matter how many ways the family prepared it, he couldn’t get behind it. He wanted “his” greens and physicians couldn’t understand what difference it made.
The whole family rallied to help him, and they wanted to support his wellness journey, but the divide between his habits and lifestyle and what physicians were recommending was wide. Instead of taking his current diet and coming up with creative ways of improving it, medical professionals took an all-or-nothing approach: “Either stop eating that food or your diabetes gets worse.” He was demoralized.
At the time, Ashford was running Xplosion Technology with fellow cofounders, computer engineer Kehlin Swain and mechanical engineer Jaylen James, PhD. Operating in the biomechan-

ics space, this digital health platform focused on improving athlete performance using image detection on joints to lower sports injuries.

Faced with the challenges they were seeing in the life of Ashford’s father, and compounded by Swain’s experience growing up with a cousin with Type 1 diabetes, the trio figured out how to use their biomechanics experience to help people with diabetes. They began their research in collaboration with the National Science Foundation (NSF) and after speaking to 100 potential customers — diabetics ranging from gestational to Type 1, Type 2, and more — they began seeing an opportunity. There was a clear differentiation between those who had the tools and ability to manage their condition and those who didn’t.
Some interviewees were on government aided insurance, some were covered through private carriers. Those with access to insulin pumps and CGMs (continuous glucose monitors) had a better time managing their condition and food intake, while those who didn’t have access to the devices not only had difficulty but had no other systems or solutions available to them, causing them to fall through the cracks. Another realization was that of those interviewed, 90% were patients of color...
Scan to read the full story or go to healthtransformer.co

startuphealth.com 45
Handl Health Is Making Health Pricing Data Actionable, Powering a Wave of Innovators
COST TO ZERO MOONSHOT
Co-founders Ahmed Marmoush, Ria Shah, and Karthik Palaniappan have combined their experience in digital health consulting and big tech to build a single source of truth for accessing healthcare pricing information. Their API has the ability to drive down costs by offering transparent price comparisons for employers and benefits brokers.

HHealthcare has a cost transparency problem.
Imagine walking into a Best Buy and purchasing a TV with no knowledge of the cost, only later to receive a bill in the mail. Or what if you had to buy airline tickets without any visibility into sky high “airport facility fees”? As ridiculous as this sounds, it’s a fair picture of the US healthcare system in 2023.
Not only are healthcare expenses typically a surprise, they’re often exorbitant. Over the past 15 years, cost sharing has shifted to the consumer at a pace that
46 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS
has outstripped household income. In other words, the gap between income and healthcare costs is growing. One out of five families lack the savings needed to pay total out-of-pocket healthcare costs, so they either avoid necessary care or go into debt.
An answer to these two problems has come in the form of recent price transparency legislation like Transparency in Coverage. This law mandates that payers publish every single negotiated rate in a machine-readable format and give members an online tool to estimate out-ofpocket cost. Because of various new laws, every industry player including hospitals and insurance carriers must now publish their costs and provide the consumer with tools to shop.
These positive moves have created a new problem: data overload. More than 3000TB of healthcare pricing data is becoming available following the legislation, a volume and complexity virtually impossible to apply in real-world settings.
Pittsburgh-based Handl Health has stepped into the market to solve the problem, building a platform that powers an ecosystem of price transparency products by translating pricing data into actionable insights.
ORIGIN STORY
Ahmed Marmoush got his first real taste of the broken American healthcare system while working as a healthcare consultant at EY. Marmoush came from a family of pharmacists — who had immigrated to New Zealand from the Middle
East — so he thought he knew what to expect from the healthcare system when he came to the US. But when he got an impossibly expensive surprise bill in the mail after a routine blood test, he was taken aback.
He showed the bill to his EY colleague and friend Ria Shah. Her response was telling. She said, in essence, “It is what it is.” As the child of Indian immigrants, Shah had learned to simply adapt to the broken system. But as Marmoush stood in front of her, shaking his head about his medical bill, something clicked. They both saw the underlying issue beneath the bill. A lack of pricing transparency was forcing millions of people to find workarounds in healthcare just to survive. But healthcare regulations were shifting dramatically in favor of greater price transparency. At EY, they’d each gained the industry knowledge necessary to forge a solution, so they decided to step out and try.
The idea was elegantly simple: make healthcare pricing data accessible and actionable. With Marmoush’s clinical background and experience designing valuebased care models and cost containment strategies for health industries across the globe, and Shah’s extensive experience as a data strategist specializing in value-based contract design and big data management for major healthcare systems, they made a great team. Then they met Karthik Palaniappan and it took the team to a new level.
Palaniappan had put in years at Meta and Google Cloud as an engineer before
startuphealth.com 47
he was introduced to Marmoush and Shah. He knew he wanted more than big tech could offer — specifically to work on a greenfield project that would be a part of shaping healthcare delivery and policy. That opportunity came in Handl Health.
Handl Health received an accelerant when it was accepted into Techstars Healthcare in Los Angeles. That opportunity gave the team exposure to the mentors and clients necessary to scale their platform. Following the completion of the program in June 2023, they are well positioned to make the dream of healthcare price transparency a reality.
UNDER THE HOOD
Handl Health is a B2B platform focused on delivering accurate and actionable healthcare pricing data. It all comes down to one basic question: How much will a treatment or procedure cost?
“It might seem like a simple question,” says Marmoush, “but it’s incredibly complex to answer depending on who you are, what insurance you have, and what facility you use.”
The answer starts with data management. Handl Health has built better ways to ingest, aggregate, clean, and serve up healthcare pricing data. They’ve built algorithms that make sense of that data.
“Very few companies, even more than a year after this pricing data has come out, have successfully designed the right kind of pipeline to be able to use and deliver this data at scale,” says Shah.

That data can be personalized to the individual — “what will this procedure cost
me today?” — and is also tuned to be used at an enterprise-level, such as by an employer or benefits consultant looking to develop and fine tune healthcare benefits and budgets.
Their vision is to become the central healthcare pricing data platform.
“The beauty of a platform play is that there are so many use cases that we can service,” says Marmoush. An employer helping employees figure out which provider to go to based on cost and quality information. The CFO trying to analyze their claims between two different networks in order to make a decision on which is aligned with their budget. Or a provider trying to improve collections by giving patients upfront cost estimates.
And having accurate pricing data isn’t just about getting a better deal on care. It’s about mitigating risks. Thanks to recent regulatory changes, large employers have started to ask questions about how much their insurers are charging and if those rates are aligned with the payers’ fiduciary responsibilities.
In terms of their go-to-market strategy, Handl delivers their platform capabilities through APIs and low-code/nocode tools, starting with two offerings in market today. The first is a dashboard to help corporations compare insurance networks...
Scan to read the full story or go to healthtransformer.co

48 StartUp Health Magazine / EXPONENTIAL PROGRESS
/ HANDL HEALTH
MEET THE HEALTH TRANSFORMERS
Journey Biosciences Has Created a First-in-Class

Predictive Test for DiabetesRelated Kidney Disease
T1D MOONSHOT
KKidney disease can be a daunting and potentially life-changing complication for individuals living with diabetes. Sadly, one in three people with diabetes will develop kidney disease, and often, there are no warning signs or symptoms until significant damage has already occurred. Once diagnosed, the damage is often irreversible, and the only options for survival may be lifelong dialysis or a kidney transplant.
Imagine living life with diabetes, taking care of yourself, and following your doctor’s directions — only to discover that you have developed another life-altering condition. You’ve been caught off guard, with no indication that anything was wrong until it was too late. This is a
reality for millions of people around the world.
But, what if you could have been alerted to your risk of developing kidney disease years before you were diagnosed? An early warning could have prompted changes in your behavior and enabled you to take advantage of advanced technologies and clinical treatments that might have prevented or delayed a diagnosis, adding valuable years to your life.
The current lack of warning signs poses a significant challenge for preventing and intervening early in kidney disease. Most screening methods only report on current kidney function or the presence
startuphealth.com 49 MEET THE HEALTH TRANSFORMERS
Adam Graybill (right) and Dr. Paul Beisswenger have teamed up to bring to market a test that could potentially help millions of people with diabetes avoid kidney disease and dialysis.
of existing damage. The goal is to identify high-risk patients early, before the disease progresses and causes irreversible damage. This goal hasn’t been possible until now. This is where Journey Biosciences is making a difference with NaviDKD, a predictive test that could help millions of people avoid the life-altering effects of kidney disease. NaviDKD is designed to provide clinicians with the insights they need to take clinical actions that could prevent or delay the onset of kidney disease, helping patients live longer and healthier lives.
ORIGIN STORY
Paul Beisswenger, MD, (Dr. Paul) spent his career helping people living with diabetes as an endocrinologist, professor, and researcher at the Dartmouth School of Medicine. Over the years, he became frustrated by the serious complications his patients faced even when they worked hard to maintain blood sugar control. Driven by his passion to make a difference, he focused his research on finding solutions to reduce the burden of diabetes-related complications. His research led to the scientific foundation for a predictive test for kidney disease — one of the most devastating complications of diabetes.
In 2021, Dr. Paul teamed up with Adam Graybill, a seasoned business leader with a personal connection to the cause. Adam has witnessed firsthand how early diagnosis and risk awareness can greatly impact patient treatment, care, and outcomes. Inspired
by Dr. Paul’s research and recognizing the significant potential in the science, Adam worked alongside him to establish Journey Biosciences and NaviDKD. Over the past two years, they have successfully built a commercial lab and an operating model that works. NaviDKD has obtained patents in both the United States and Europe and has demonstrated in four landmark longitudinal outcome studies to accurately predict diabetesrelated kidney disease. As they continue to innovate and grow the company, Dr. Paul and Adam remain committed to reducing the burden of diabetes and other chronic conditions on patients and their families.
UNDER THE HOOD
NaviDKD is a blood test that measures key biomarkers to determine an individual’s risk of developing kidney disease related to diabetes. Using a proprietary algorithm, the test provides a personalized risk score in one of three profiles: high, elevated, and low. Since kidney disease is often asymptomatic, alerting high-risk individuals and providing clear mitigation pathways can save lives.
NaviDKD is an essential tool for establishing a kidney health baseline. For example, someone with a high risk score can take proactive steps to potentially decrease their risk score over time. On the other hand, someone with a low risk score may continue with their current care plan until they see an increase in their risk score, indicating the need for action. Even newly-diagnosed individu-
50 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / JOURNEY BIOSCIENCES
als with diabetes can use NaviDKD to determine their current risk level up to 12 years in advance of clinical signs and symptoms. This information can be used to collaborate with their physician in developing a personalized care plan. All patients can re-test annually to track any changes in their risk level and make adjustments to their care plan accordingly. By utilizing NaviDKD, individuals and their providers can take proactive steps to maintain kidney health and potentially avoid the devastating complications of diabetes-related kidney disease.
BIG PICTURE
Adam and the team at Journey Biosciences are the first members of a new cohort of Type 1 diabetes startups in the StartUp Health T1D Moonshot Fellowship. This Fellowship, supported by a program-related investment (PRI) by the Helmsley Charitable Trust, represents an exciting new way to create crossdisciplinary innovation in a specific disease area.
We’re proud to support the Journey Biosciences team in their groundbreaking work, as they have created a firstof-its-kind innovation with NaviDKD.
Journey Biosciences is the first to develop a predictive kidney disease screening for diabetes patients, which marks a significant leap forward in diabetes care. Their goal to screen at least 300,000 individuals within the next five years, equivalent to 4% penetration of the Type 1 diabetes community, will undoubtedly create opportunities for further innovation in di-
abetes treatment. Journey Biosciences is poised to lead the way in creating a better future for both the Type 1 and Type 2 diabetes population.
Journey Biosciences is also committed to improving health equity by prioritizing women and people of color, who are disproportionately affected by kidney disease. Originating from a renowned teaching hospital (Dartmouth), the company has a strategy to cater to underserved urban communities by targeting similar teaching institutions. This mission aligns well with our Health Equity Moonshot and our global goals of improving access to care.
From a business perspective, the potential impact of Journey Biosciences’ innovations is massive. By reducing kidney disease by just 20%, the healthcare system could save $8B, avoiding hundreds of thousands of dollars in yearly expenses per patient. This represents a significant opportunity for Journey Biosciences, with exponential growth projected from $3.4M in 2023 to $222.7M in 2027.
Through the development of NaviDKD, Journey Biosciences is giving those with diabetes proper warning signs of complications, potentially adding years of quality of life for millions.
Learn more & connect with founders at startuphealth.com/portfolio
startuphealth.com 51

Alvee’s AI Data Platform Gives Payors & Providers Tools to Advance Health Equity
HEALTH EQUITY MOONSHOT
Founder Nicole Cook (left) is building on 15 years of leadership experience at the intersection of health equity and EHR interoperability to create an AI data management tool that predicts patients’ social determinants of health.
Seamlessly integrated with EHRs and CRMs, it promises workflow automation and greater visibility for health disparities amongst vulnerable patient populations.
the cost of the prescribed pain meds.
But what if the doctor was able to intuit Maria’s potential barriers to care? In the physician’s hustle between tending to patients and required EHR documentation, what if they had immediate access to carefully mined data that painted a picture of Maria’s needs beyond the ER or doctor’s office? To take it a step further, what if the physician was equipped with recommendations for Maria based on her social determinants of health (SDOH) — her need for transportation or a Spanishspeaking medical assistant?
ORIGIN STORY
MMaria arrives in an emergency room with a bone fracture. After a quick examination and glance at her chart, a physician attends to Maria’s injury, rates her pain, and makes a treatment recommendation, sending her home with a prescription for painkillers.
What the physician doesn’t know is that English is Maria’s second language. Most of the treatment instructions were lost on the Spanish-speaking patient. Additionally, Maria doesn’t have a car to get to and from her follow-up doctor’s appointments or ample insurance to cover
While the scenario above is a blend of common SDOH case studies, the ‘what ifs’ are more than wishful thinking. With Alvee they are a reality. Founded and helmed by CEO Nicole Cook, Alvee equips payors and providers with an AIdriven workflow automation and data management tool that provides real-time patient-specific notifications about health disparities, SDOH, missing demographic information, and chronic conditions.
Cook is something of a native to the world of health data and interoperability. She spent seven years at Epic supporting the go-to EHR system’s early implementation in hospitals. She joined Epic on the
startuphealth.com 53
MEET THE HEALTH TRANSFORMERS
MEET THE HEALTH TRANSFORMERS /
heels of the passage of the HITECH Act in 2009, the Department of Health and Human Services legislation that pushed the medical community to adopt electronic health records. In her time there, she saw the healthcare software company grow from 3,000 employees to 10,000, an experience she likens to the often rapid evolutions of startups.
Cook was Epic’s boots on the ground, a conduit between the providers using the system and the software’s mothership. As such, she was often on the receiving end of the providers’ frustration with the system. It’s a common trope that Epic and large EHR systems like it introduced extra clicks and computer time, taking away from (rather than adding to) attentive patient care. She saw firsthand the physicians struggling to keep pace with the new requirements to document a patient’s health journey in the system.
From Epic, Cook pivoted and joined the startup world, serving as VP of Client Relations at SameSky Health. There, she worked closely with the company’s CEO & Founder Abner Mason, leader of multiple high-profile organizations committed to advancing health equity. It was at SameSky that Cook observed how disparate health databases and inconsistent measurement of health disparities created obstacles to stratifying health conditions by race, ethnicity, gender, or sex.
“It was frustrating to sit on the sidelines and see the lack of data keep payors and providers from taking action to improve health equity,” she said. “If you can’t measure health inequity, you can’t improve it.”
Cook envisioned a tool that would fill in data gaps when it came to demographic data collection and serve up health equity reports to keep healthcare organizations accountable for improving health equity amongst their patient population. In July 2021, she launched Alvee.
UNDER THE HOOD
Cook is a self-proclaimed data nerd, someone who has always loved all things magic and fantasy and was known to host Star Wars marathon parties as a kid. She nerds out over the “magic” of Alvee’s AI and machine learning technology in its ability to leverage APIs to pull in data from external sources like the US Census Bureau, CDC, FDA, and CMS.
“This is missing in EHR systems today,” Cook said. “We have a patient’s medical history and visit information but nothing that says based on where this person lives, this person may be at risk for having food insecurity or access to care issues.”
Alvee’s tool equips providers with a frictionless and discrete way to ask patients about possible barriers to care and offer recommendations. Alvee successfully completed their first platform integration with Salesforce Health Cloud at the beginning of the year. Without changing any part of a user’s workflow they can see health equity alerts specific to each patient for confirmed and possible barriers to care — such as food insecurity, lack of transit/transportation, disability, and language — all alongside the patient’s clinical appointment data and member plan details.
Take the scenario with Maria. In the
54 StartUp Health Magazine / EXPONENTIAL PROGRESS
ALVEE
brief few seconds that the ER physician would have to glance at her patient record, they might see “Possible Barriers to Care” alerts for “Food Insecurity” and “Transportation.” Drilling into the transportation barrier to care alert would yield resources to connect Maria to transportation benefits. What they wouldn’t see is Alvee’s backend data crunching — generative AI, predictive analytics, and machine learning models — to produce Maria’s realtime, patient-specific alerts.
Or, perhaps Maria speaks to a member service representative following her ER visit to inquire about billing. In that conversation, the representative would have the ability to conduct a social needs assessment with Maria to confirm information like her English proficiency, household size, or housing situation. The assessment is one more layer of Alvee’s tool. Responses
to this assessment would automatically update ICD-10 codes, the common language for recording health data in a consistent way between hospitals and countries.
“We integrate like a data fabric, weaving SDOH and health information together to provide insights,” Cook says. “Alvee makes the invisible barriers to care visible.”
Much of the tool’s wizardry is behind the scenes. Cook prefers it this way. For her, designing points of Alvee brand recognition into the EHR and CRM interfaces is not as important as seamlessly fitting into providers’ existing care workflows... Scan


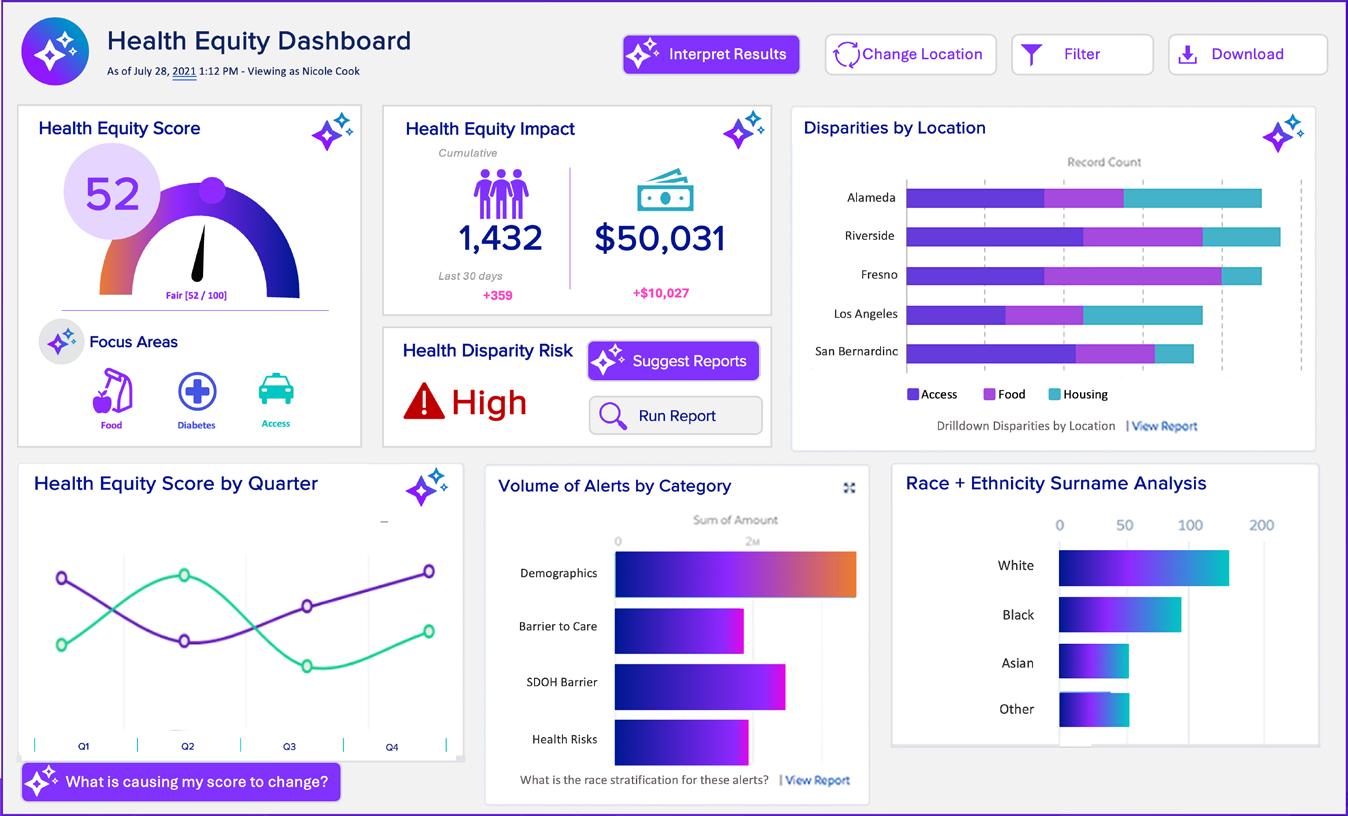
startuphealth.com 55
healthtransformer.co
to read the full story or go to
Ampersand Health Provides a Consistent Community of Care for At-Risk (and Frequently Overlooked) Patients
CURE DISEASE MOONSHOT
Backed by clinical validation and empathy, a team of doctorpreneurs created an app to empower and enhance the wellbeing of chronic inflammatory disease sufferers –giving them the tools to manage their own care and minimize the physical and mental challenges caused by fluctuating relapse and remission.

YYou cut your finger or scrape your knee, and your body sends inflammatory cells to heal the affected skin. This is an example of ‘acute inflammation.’
‘Chronic inflammation’ occurs when your immune system sends those same cells to various parts of your body even though no trauma or injury has necessarily triggered them. This form of inflammation can cause pain or discomfort and have a significant impact on your physical and mental health. It often presents in the form of “flare-ups,” where an individual
56 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS
experiences more distressing symptoms for a period of time followed by periods of “remission” when symptoms are non-existent or well-managed. This cycle of relapse and remission can be unpredictable, causing a great deal of stress for an individual and making them feel out of control at times. The unique bi-directional relationship between your mental and physical health is magnified during these episodes, because one can positively or negatively impact the other.
Crohn’s and ulcerative colitis, inflammatory arthritis, and eczema and psoriasis are examples of chronic inflammatory diseases. The uncertainty of when symptoms will arise can create anxiety. In addition, many patients find it hard to develop an understanding circle of care to support them through their condition journey out of fear of the physical and emotional burden these diseases can place on others as well as the stigma attached to them. The things patients do to stay one step ahead — i.e., track symptoms on their phone or in a notebook, chronicle eating and sleeping patterns, etc. — are frequently exhausting and overwhelming as they continue to wonder, “Will my body let me down when I need it most?”
The current apps meant to help patients are not clinically validated, making it difficult for attending physicians to trust they’re getting the right information to provide the best care. These digital solutions also don’t focus on helping patients self-manage both the physiological and emotional pain they face once away from a doctor’s care.
UK gastroenterologists, Dr. Bu Hayee and Dr. Gareth Parkes, recognized their patients’ ongoing challenges and feelings of powerlessness, and raised concerns about how those in their care were managing on their own. They began asking the questions: “How do we know you’re safe when you’re out of hospital? How can we be sure you’re not falling through the cracks, and if you have an episode of relapse, how are we making it easy for you to escalate yourself so we can see you when you need to be seen?”
Finally, they wondered, “How can we deliver not just a service but an optimum service for people living with these conditions?”
Ampersand Health offers an answer.
ORIGIN STORY
Dr. Bu Hayee, Consultant Gastroenterologist and Chief of Service for King’s College Hospital in the UK, and Dr. Gareth Parkes, Consultant Gastroenterologist and Clinical Lead for Gastroenterology at Royal London Hospital, were becoming increasingly aware of the physical and mental toll chronic inflammatory disease symptoms took on their patients. They each looked at the state of their own departments and wanted to provide patients with the best support to better self-manage their own disease to improve their lives, both physically and mentally.
The current slate of digital apps on the market — they researched more than 80 offerings — was not addressing the problem. Although they knew none were clini-
startuphealth.com 57
cally validated, there was a bigger issue: chronic inflammatory disease affects a lot of people — in the UK alone, one in 123 people suffer from either ulcerative colitis or Crohn’s disease and approximately 10 million people have arthritis — but the umbrella term of “chronic inflammatory disease” covers 40 or 50 manifestations of the same thing in different parts of the body under different names. This means, these varied disorders do not have the same perceived scale as something like diabetes or heart disease, and the tools available are not as advanced and immersive as those for other ailments.
Drs Hayee and Parkes not only wanted to focus on the “disease” itself — regardless of the manifestation — but the way it presents by building a business plan around the common experience of relapse and remission that develops in chronic inflammatory diseases. They shared their idea with Nader Alaghband — who would become the third co-founder and CEO — and the trio realized that by de-
veloping a platform supporting long-term remission while empowering patients to manage their own wellbeing even during a relapse, they could enhance and improve their physical and emotional wellness.
The team immediately involved national charities and conducted patient and clinician focus groups to inform the experience before their first UX/UI exercise. They developed a basic data collection and messaging tool, and as things progressed, they realized what they built could support a business, and Ampersand Health was formed.
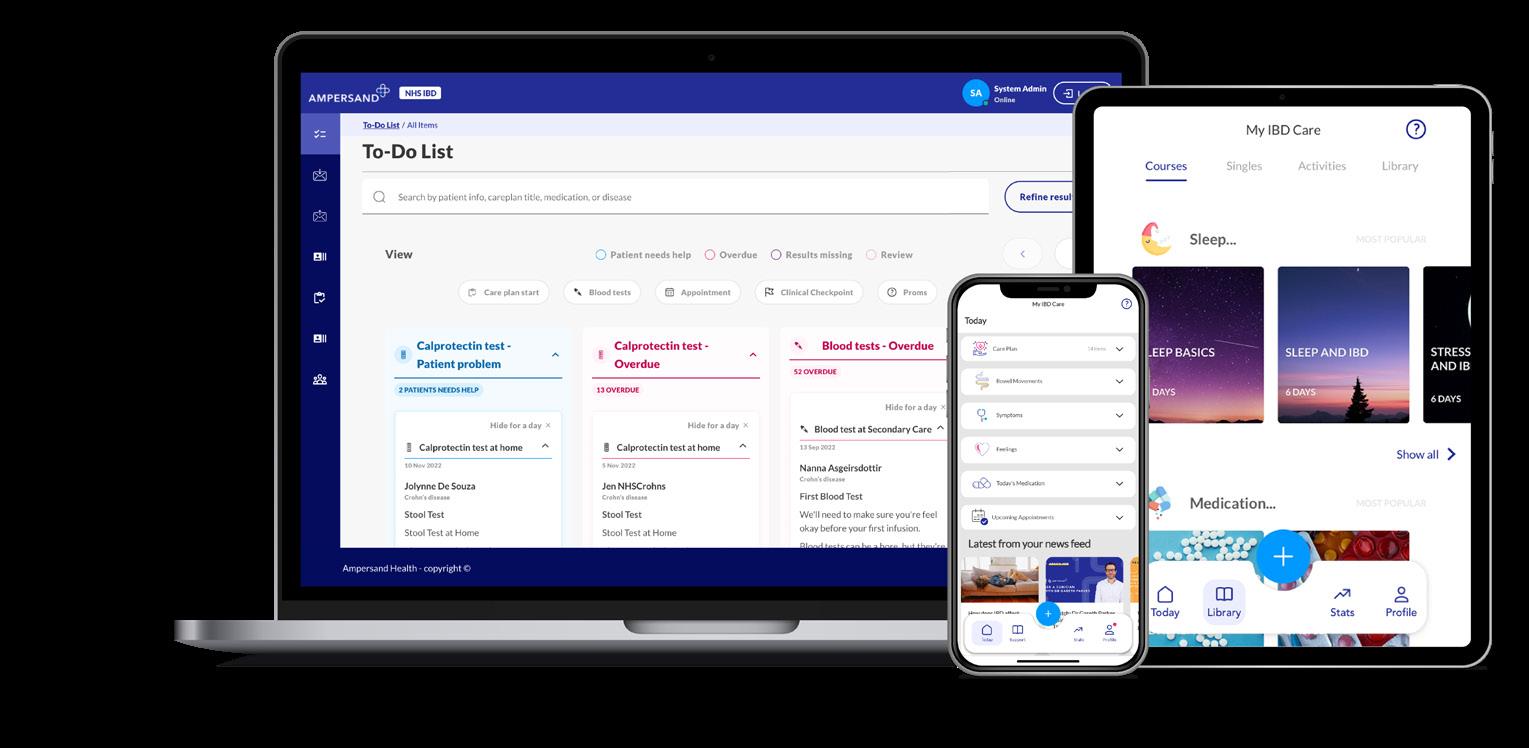
UNDER THE HOOD
“Monitor. Learn. Manage.” These are the three main tenets of the Ampersand Health app...

Scan to read the full story or go to healthtransformer.co

58 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / AMPERSAND HEALTH
DreaMed Simplifies Diabetes Care via AI-Driven Recommendations
T1D MOONSHOT
This Israeli-born startup is making significant clinical and regulatory headway in their effort to automate care recommendations for people with diabetes. Their platform endo. digital processes mountains of diabetes-related data, from new and emerging devices and sources, so physicians can focus on patient care.

OOver the last decade we’ve witnessed an explosion in the availability of personal health data. Whether it comes through wearable fitness trackers, remote patient monitoring devices or inhospital technology, the stream of data is getting deeper and wider by the day.
This increase in data volume opens up awesome opportunities for healthcare innovators to predict illness, diagnose disease and improve care. But it also creates new challenges. One place we’re seeing the two sides of this health data coin play out is in diabetes.
According to the IDF Diabetes Atlas, there are nearly 783 million people suffering from diabetes around the world. More and more of these individuals are gaining access to continuous glucose monitors
(CGMs) that track glucose levels throughout the day, without the need for a finger stick. Just recently, US Medicare has decided to expand reimbursement for CGMs for people with Type 2 that uses basal insulin. Last week, the authorities in France made a similar decision. This is life-saving, game-changing technology, but it brings with it a wave of health data that can be overwhelming for both patients and their physicians to manage. And that is just one device and data source of many in the diabetes space.
On the physician side, the tidal wave of diabetes health data causes endocrinologists and their staff to spend so much time combing through digital platforms and information that they experience information overload. They then can end up giving less attention to their patients, leading to
startuphealth.com 59
MEET THE HEALTH TRANSFORMERS
clinician burden, frustration, and concern for patient wellbeing.
As access to diabetes devices expands, data overload also becomes a problem for primary care physicians. These doctors aren’t diabetes specialists, so the web of new diabetes data sources is even more overwhelming. As a result, these doctors end up sending individuals back to an endocrinologist — of which there are too few — who now have a backlog of patients with data they need to wade through.
In the end, an incredibly valuable well of data can turn from an opportunity for healing to a burden. Thankfully, there are dedicated health innovators working on a solution. DreaMed, a team based in Israel and MN, is using artificial intelligence to make sense of disparate health data streams and offer care pathway recommendations at the click of a button.
ORIGIN STORY
Professor Moshe Phillip, MD, is the Director of the Institute of Endocrinology and Diabetes at the National Center for Juvenile Diabetes at Schneider Children’s in Israel. Over the years he noticed how innovative technology companies were collecting and disseminating so much digital diabetes data that it was becoming overwhelming for physicians and actually taking attention away from treatment and quality patient care.
Dr. Phillip knew what was good for his young patients, and that there had to be a better way to access and focus this data. He decided to create his own tech team and build a solution.
The professor reached out to Eran Atlas, a biomedical engineering student at Tel Aviv University, for help. The two, together with Revital Nimri, MD, from Schneider Children’s Institute and other team members, focused on the development of an artificial pancreas system suitable for people with Type 1 diabetes. Together with their partners, Prof Thomas Danne and Prof Tadej Battelino, their team was the first in the world to take a group of patients into a hotel, simultaneously in three different countries, give them laptops, and monitor the use of an algorithm to automate their insulin delivery while they slept. This initial study was published in the New England Journal of Medicine — the first such findings to be shared in the publication. Eventually this solution was sold to Medtronic and is part of MiniMed 780G.
Then they considered what more they could do for people with diabetes, knowing that the vast majority of the population would not be able to use artificial pancreas systems. Their vision was focused on how they could take that large amount of digital data and automate it to reflect how physicians actually think: treatment, recommendations, even a way to incorporate billing all in one place through the use of artificial intelligence.
In 2015, the team began work on an end-to-end automation of the care pathway with this mountain of diabetic data. They didn’t just want to collect information or even interpret it but develop a platform that did both in an accessible, manageable way and was also able to digitally share physician recommendations
60 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / DREAMED
and treatment plans between doctor and patient. If they could accomplish this, the team believed they could also incorporate automated billing to capture the appropriate codes for the different clinician services provided to make a seamless experience. They established DreaMed and hit two key milestones that prompted them to keep moving forward.
First, they published a multicenter study that proved they could achieve the same clinical results with their algorithm and digital platform as doctors in Joslin Diabetes Center and Yale New Haven Health System. This study was followed by additional clinical studies and real-world clinical data, showing the similarity between the recommendations of their platform — called endo.digital — and expert physicians. Next, they were the first in the world to receive FDA clearance to use continuous glucose sensor data and provide a recommendation for insulin therapy. This was new territory for the FDA, so DreaMed worked with the agency to create a new product code. Since that time, the company has received three more FDA clearances.
UNDER THE HOOD
The DreaMed product is called endo. digital, and on the website the first thing you read is, “We treat the data, you treat the person.” The goal of the digital experience is to “make the digitally complex simple” through the AI engine, and it works with the user in whatever way fits their needs.

The solution is elegantly simple to use.
The clinician opens their EMR user account and goes into the appropriate patient chart. There is a button that reads: “Give Me a Recommendation.” The provider clicks on the button, and a recommendation comes up based on the available data the AI has collected. The healthcare provider reviews the recommendation and edits as needed, then clicks “Approve.” The visit summary is auto populated, a notification is sent to the patient via mobile or email, and the app calculates their insulin needs.
DreaMed tells doctors they can decrease the number of process steps without having to engage with more technology or increase their data management. The company can cut a process from 30 steps down to 12. What once took 25 minutes to complete could now take nine minutes less — and it would include automating all billing.
Data is pulled two different ways: cloud to cloud if the patient device is set up for that, or old-school USB cable plug-in to a provided endo.digital device uploader that then sends the data to the cloud. The AI is agnostic as to how it gets the information.
On top of the randomized controlled study published in Nature Medicine, DreaMed conducted a study with a set of patients spread across 27 physicians across the world...
Scan to read the full story or go to healthtransformer.co

startuphealth.com 61
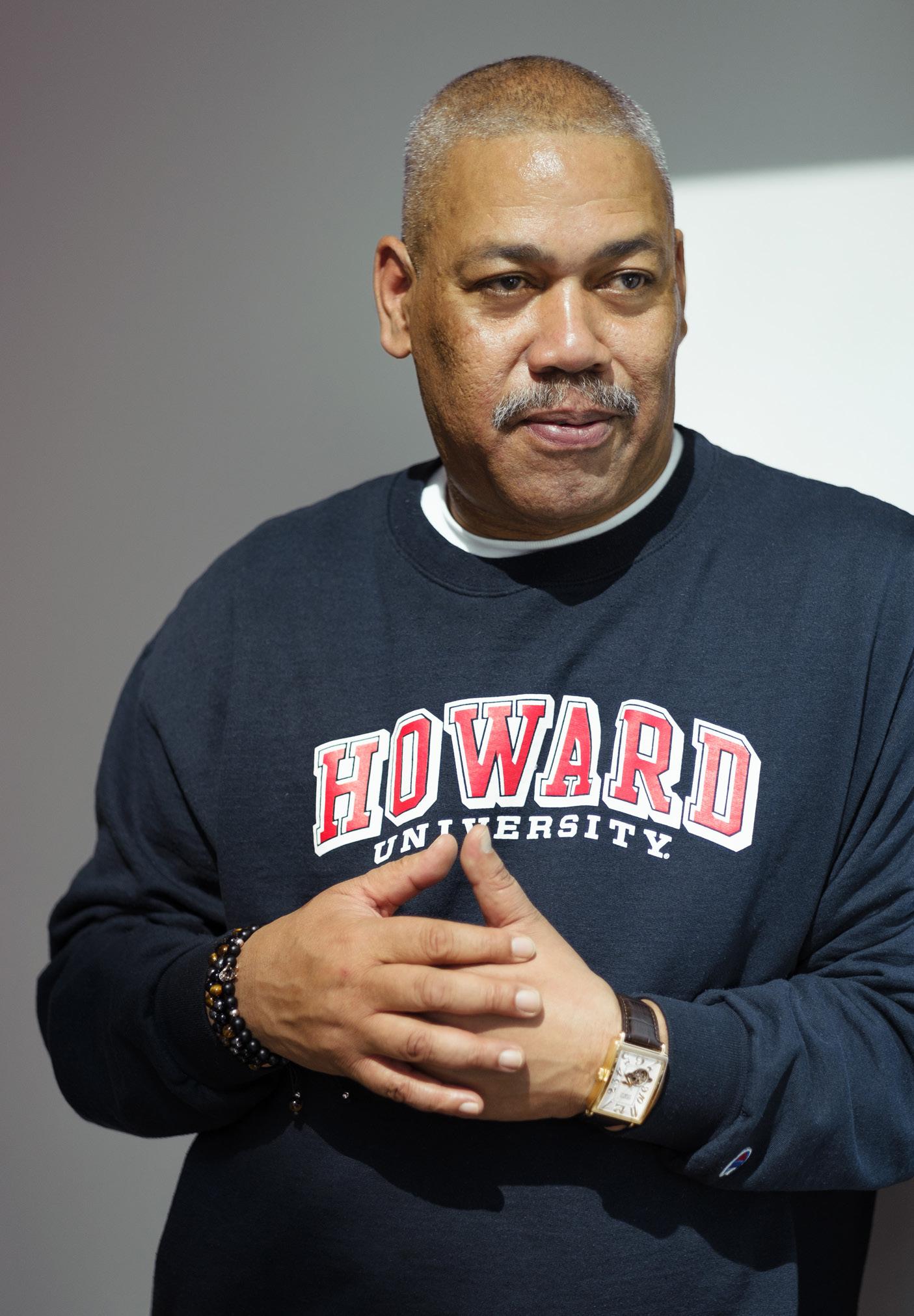
62 StartUp Health Magazine / EXPONENTIAL PROGRESS
Sanitas Health Offers CulturallyRelevant Mental Healthcare for Communities of Color
MENTAL HEALTH & HAPPINESS MOONSHOT
Through peer interaction, personal coaching, and data collection, the Baltimore-based digital platform founded by Rodney Bell (left) seeks to address the lack of therapists targeted to BIPOC populations — with the goal of catching those in need before they are in crisis.
FFor years, there has been a scarcity of psychiatrists and psychologists in the United States. The American Academy of Medical Colleges (AAMC) claims that 150 million Americans live in “federally designated mental health professional shortage areas.” By 2028, this deficit is estimated to widen by another 30% but the need for their services won’t. Notoriously left out when considering how to deal with this impending crisis are communities of color.
Without designated therapeutic support, BIPOC populations are faced with a few glaring issues. First there is the revolving door at emergency rooms. Many communities of color — including many in the Medicaid population — turn to the ER for mental healthcare. The ER often feels like
the last, best choice, the only open door in a closed-off healthcare system. But ER staff are generally unequipped to handle longterm mental health challenges, so they send these patients home to wait for an appointment with a therapist. Patients may wait up to six months for a visit with a specialist, creating anxiousness and bounceback visits to the ER. Finally, once an appointment is secured, not enough culturally-experienced therapists and support groups exist to appropriately address the mental health issues this overlooked community struggles with, leading to a sense of isolation and hopelessness.
To top it off, there is a great deal of stigma people of color face within their own communities, making it difficult to manage and get the mental health help they need. While there are many apps on the market focused on mental healthcare, few if any are geared specifically to minorities, and they do not promote peer interaction within those populations to help overcome feelings of loneliness. Many young people of color are at risk of falling through the cracks, leaving institutions committed to supporting the wellbeing of this fragile group desperate for an answer.
How to create an easily accessible, inclusive, and culturally-relevant solution that provides institutions with quality mental
startuphealth.com 63
MEET THE HEALTH TRANSFORMERS
health resources to offer those stuck in the public system? What are the ways to ensure the end user truly benefits by addressing them in ways that make them feel safe, heard, and understood?
The founders of Sanitas Health pulled from their own personal experience and rallied to the cause.
ORIGIN STORY
Originally from St. Louis, Missouri, Rodney Bell understands mental healthcare within communities of color. His fiancé’s twin daughters are bipolar and struggle with receiving the targeted care they need. The former co-founder of another StartUp Health company, Butterflly Health — a telehealth platform supporting women and vulnerable populations — noted that the two 20-somethings went to the ER when in crisis. Although they had private insurance, the care was culturally lacking, and the wait for an appointment was long, creating a void and a feeling of isolation that was difficult to manage, leading back to the ER once again. Bell knew from experience that most ER patients are on public insurance like Medicaid, and many were people of color. If his family was struggling, and he had specific mental health experience, what kind of care were these communities getting?
Bell has surveyed the macro challenge and concluded that what most people need is support from those who understand what they are going through. Within communities of color, there are very few therapists who are part of the BIPOC population and even fewer with cultural
experience. There is also a lack of safe spaces where a person can receive peer support. What people need is a “village,” focused on group therapy, coaching, and getting help before they are in crisis. What better way to do that than through telehealth?
Turning attention to the Medicaid community, Bell tapped into his digital health expertise and sought a solution for adults. He and his partners applied to Techstars for funding and resources to expand this vision of a telehealth platform that was peerfocused and offered coaching and therapy matching when necessary. He applied to programs in Los Angeles, Seattle, Atlanta, and Baltimore.
Once word got out in Baltimore that Sanitas was creating an inclusive digital mental health platform that focused on communities of color and that the goal was to work with Medicaid, doors began to open. The Boys & Girls Club of Metropolitan Baltimore approached him, clamoring for support for their youth. Crime in Baltimore is unique, and kids are exposed to it at a very young age, causing serious trauma to the city’s young people that puts them at immense mental and emotional risk.
Bell’s intention was to spend three months in Baltimore and then return to Los Angeles to take the next step with the platform. The city opened to them, however, and Sanitas received extraordinary support from the State of Maryland, Maryland Commerce Department, and more to bring their vision to life. What started out as a three-month fact-finding mission turned into a base of operations. Baltimore
64 StartUp Health Magazine / EXPONENTIAL PROGRESS
THE HEALTH
/ SANITAS HEALTH
MEET
TRANSFORMERS
is perfectly situated for the platform that requires cultural training for any social workers, coaches, or others who interface with the Sanitas community; and Sanitas is committed to hiring a diverse staff that is both BIPOC and has a living understanding of the populations they serve.
With this focus in mind, Sanitas distinguishes itself from other mental health apps that seem to focus on one of three things: therapy matching, tech-based coaching, and peer groups. The Sanitas platform provides all three with a specific expertise in targeting communities of color and the underserved.
UNDER THE HOOD
Sanitas Health is a subscription based, B2B2C platform. Organizations (hospital systems, university healthcare systems, community organizations, etc.) pay a negotiated monthly fee to Sanitas and provide the platform for free to their client/ patient population. When an organization identifies a person in need, they set them up on for onboarding to Sanitas’ platform. During onboarding, patients take standardized assessment tests:
The PHQ-9, which is used to screen, diagnose, monitor, and measure the severity of depression.
The GAD-7, which measures the severity of the four most common anxiety disorders: generalized anxiety disorder, panic disorder, social phobia, and post-traumatic stress disorder.
The adverse childhood experiences (ACEs) screening, used to look for common childhood traumas.
The scores from all three are combined to determine a baseline, which is then run through an algorithm. They use the subsequent scoring matrix to recommend which group or groups the patient should join. From there, the patient interfaces across three stages.
In Stage 1, patients are teamed with social worker-moderated peer groups composed of other individuals experiencing the same issue to create a sense of community. If it is determined that the user needs a higher level of care, they are escalated to Stage 2.
Stage 2 involves certified coaches available 24/7/365 via Zoom or text — in other words, one-on-one support.
If a therapist is required, Stage 3 is initiated for therapist matching and connection.

In general, roughly 21% of those on the platform have taken advantage of Stage 3, proving that peer engagement and coaching have been effective.
Every conversation conducted on the platform is stored in a database, fed through a natural language processing engine to determine if there are markers and indicators of stress and depression. By feeding this information through the database, the algorithm will learn triggers, key words, and markers, helping it become more preventative over time...
Scan to read the full story or go to
healthtransformer.co
startuphealth.com 65
HEALTH EQUITY
MOONSHOT
Founder Yusuf Henriques (pictured) and Chief Scientific Officer Bradford Wilson, PhD, have combined their experience at the FDA, in the military, and in academia to drive the development of therapeutics that are effective in underrepresented populations.

IndyGeneUS AI Is Bringing Genomic Medicine to Underrepresented Populations
66 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS
WWhile COVID-19 was devastating across the globe, it was particularly damaging for communities of color. African American, Latino, and Native American populations experienced disproportionately higher rates of infection and death than their European-American counterparts during the pandemic. This was in part due to underlying inequities in healthcare and increased exposure risks because of social and economic factors. While these disparities existed before COVID, the pandemic exacerbated them and made it painfully clear that healthcare reform was no longer a political debate, but a global necessity.
One of the roots of these health disparities lies in how and from whom data is gathered for research and new drug development. Historically DNA data banks, for genomics research, have overwhelmingly been made up of Caucasian males, which means that many populations from across the globe lack representation in genomics research. Currently, 87% of genomic data is of white, mostly male, origin. This means that the drugs and treatments being developed from this data do not have accurate biomarkers for the diverse patient population they are meant to treat.
Clinical trials face similar issues of lack of diversity. African Americans account for only 5% of clinical trial participants, which creates blind spots about the effectiveness of treatments. Every body metabolizes drugs at different rates based on a set of genetic variants and other factors including age, gender, medical history,
and other environmental factors. The biomedical community is aware of the lack of diversity in research and clinical trials, which is evidenced by the new FDA recommendation that 25% of clinical trial participants be from diverse populations.
“Even if you can get people to sign up for studies, there’s a huge dropout of minorities because they can’t afford the transportation cost or take off from work to attend follow-up visits,” explains Yusuf N. Henriques, an interdisciplinary scientist and former combat-medic in the US Army.
Access to healthcare has been another major factor in creating the disparities we see. Boundaries to healthcare include socioeconomic barriers including health insurance and physical barriers including distance for people in urban and rural communities respectively Federal agencies like the National Science Foundation have launched initiatives encouraging innovation in patient-centered, decentralized healthcare platforms to address the issue.
ORIGIN STORY
Henriques knows all about the challenges of gathering health data from diverse populations. As a former FDA regulator, he reviewed clinical data packages for medical devices and drug products up for approval. He remembers noticing how these trials lacked participation from a diverse patient population, even for medical products primarily aimed at minority patients.
“Because these trials end up using data that primarily comes from white males of
startuphealth.com 67
European descent, there ends up being a lot of trial and error to find the right effective dose for, say, a Black woman who metabolizes that blood pressure or diabetes medication differently.”
When the pandemic hit, Henriques was in NYC as part of the 2020 cohort of Apex, a nine-month incubator at NYU’s Veterans Future Lab. His focus during that time was on TruGenomix Health, Inc., the first Black-owned genomics company in the United States. He founded the company after his twin daughters’ summer camp counsellor, a US Marine, committed suicide. It was at TruGenomix that his current Chief Scientific Officer, Bradford Wilson, PhD, developed the PTSD gene expression assay (TruGen-1), after gaining exclusive rights to the patent from Henriques’ association with the Icahn School of Medicine at Mount Sinai (ISMMS) Psychiatry Department. Today, the gene expression assay helps identify individuals who might be at high risk for PTSD, anxiety, depression, and bipolar disorder.
During the peak of COVID, he left NYC to shelter in place with his family in Maryland and then quickly found himself on various task forces tackling COVID-19 logistical issues, like ventilator distribution and supply shortages. He did what he always did, first as a military combat medic and then in government service: respond to the pressing need in front of him. Then MIT offered him the opportunity to co-create a hackathon focused on dismantling racial injustice in healthcare systems.
The MIT Hacking Racism in Healthcare Challenge began in September of 2020. One of the verticals it addressed was lack of diversity in clinical trials, made more pressing by the sprint to develop COVID drugs that worked well for the people of color, who were most likely to contract and die from COVID-19. By that October, Henriques formed the idea for IndyGeneUS.
“MIT provided us with a platform and an initial network to leverage genomics to address these health disparities that COVID brought into focus. We came up with tangible ways to address the lack of representation in clinical trials, the barriers to access that exist, and to securely compile more diverse patient data, and create vaccines/drugs that work for more people.”
UNDER THE HOOD
IndyGeneUS (pronounced “indigenous”) is a precision medicine company using next-generation sequencing technologies to identify unique gene variants in diseases that affect underrepresented populations. By pairing a patient-centric approach and philosophy with a proprietary blockchain-encrypted precision health discovery platform, IndyGeneUS aims to become the trusted resource for delivering high-quality and reliable disease insights as well as molecular and cellular therapeutic development and bioprocessing that is inclusive of populations underrepresented in genetic research.
“We’re addressing the data issue for these communities and addressing the
68 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / INDYGENEUS AI
trust issue. This means we need to go where people are and not make this a burden for them to participate. We need labs in the ‘hood.’ We need health literacy communication to happen at the barbershop and on the street corners.”

To that end, IndyGeneUS established their first US lab on the historic campus of the old Walter Reed Medical Center, on Georgia Avenue in Washington, DC. This location helped establish their mission and model and holds sentimental value for Henriques, who used to walk the halls during his military days. By intentionally setting their services in an urban center, the company ensures that clinical trials and genetic testing take place in a comfortable, familiar setting for residents, and draw employees from the same community.
IndyGeneUS started with a focus on one of the largest underrepresented groups when it formed the Women’s Health Research Collaborative. In partnership with Endo Black, Inc., PCOS Challenge: The National Polycystic Ovary Syndrome Association, and The White Dress Project, IndyGeneUS is studying the genetics of endometriosis, PCOS, and uterine fibroids in diverse populations of affected women.
IndyGeneUS CSO Dr. Bradford Wilson explains, “This partnership gives us the potential to positively impact over 90% of women of all ethnicities who are affected by one or more of these conditions. Our advocacy partners tell us that there are women affected by all three of these conditions and there may be a ge-
netic explanation.”
On the global front, IndyGeneUS has already expanded their operation to the African continent. Last year, IndyGeneUS forged a public-private partnership with Global Health Innovations (GHI), which is a subsidiary of The Aurum Institute NPC (Aurum) with its headquarters in Johannesburg, South Africa. This collaboration is expected to accelerate IndyGeneUS’s ability to engage up to two million patients, enroll participants in research studies, and empower Africans to securely access, control, and manage their genomic and medical data within the IndyGeneUS Precision Health Discovery platform. IndyGeneUS’ second lab is located in the Woodstock area of Cape Town which is historically urban. By creating the world’s largest repository of indigenous and diasporic African clinical and genomic data, and applying their proprietary AI/ML algorithms that integrate multi-omics data, electronic health records, and the latest scientific literature to its analysis, IndyGeneUS plans to accelerate the discovery, development, and manufacturing of precision therapeutics for diverse populations. It’s health equity on a global scale, which addresses the disparities in access and information that African diaspora populations face around the world...
Scan to read the full story or go to healthtransformer.co

startuphealth.com 69

Miist Therapeutics Brings a Modern Approach to Fighting Nicotine Addiction
ADDICTION & OPIOID CRISIS MOONSHOT
After witnessing a wave of vaping addiction at college, Dalton Signor (left) partnered with an expert in inhaled medications to create a more effective nicotine cessation device, one that delivers relief quickly and titrates medication accurately.
OOne of the public health success stories we’ve witnessed in recent years has been the decline in youth cigarette smoking. According to recent data from the University of Michigan, youth smoking dropped to an all-time low of 2.3% in 2021 — down from nearly 23% in 2000. This is incredibly positive news, as we know smoking has a negative impact on nearly every bodily organ.
However, one of the tools used to curb youth smoking has spawned a new problem. E-cigarettes, first introduced in the 2000s as a smoking cessation tool, have risen in popularity among young people. Today, there are 11 million e-cigarette users, many of whom would never have considered cigarette smoking but found vaping as an easy on-ramp to nicotine use and are now addicted.
While vaping is less harmful than smoking cigarettes, experts — and a growing body of research — agree that vaping is bad for the body.
“Emerging data suggests links to chronic lung disease and asthma, as well as associations between dual use of e-cigarettes and smoking with cardiovascular disease,” writes Michael Blaha, MD, director of clinical research at the Johns Hopkins Ciccarone Center for the Prevention of Heart Disease.
One thing that appears unique about e-cigarette addiction among youth is that the majority of users would like to quit, but can’t. This problem caught the attention of Dalton Signor when he was going to college at Villanova University.
“From what I’ve seen personally I would say it would be typical for perhaps 40% of students to own an e-cigarette and up to 70% to use one on a weekly basis.” Signor said, who added that, anecdotally, he believes that many users would give up nicotine if there were an effective way to do so. “I started talking to these people and I said ‘Hey look, why are you smoking? Why are you using e-cigarettes?’ Pretty much across the board, the feedback that I got was, ‘Well, I’m hooked on this and there’s no easy way to quit, so I’m not even going to bother trying.’”
startuphealth.com 71
MEET THE HEALTH TRANSFORMERS
People have become so used to the idea that the pills, patches, and gums we have as treatments today don’t work that they’ve given up on trying to use them. Signor decided if he could come up with an effective treatment to curb nicotine addiction from cigarettes and e-cigarettes — one that takes into account the physical habits formed by smoking — he could do more than just make people physically healthier. He could help nicotine users regain control over their lives.
ORIGIN STORY
Dalton Signor was a freshman at Villanova University studying management consulting, when he started noticing how many of his friends were vaping.
“I had multiple close friends of mine who were heavily addicted to e-cigarettes, and I had a very clear line of sight into how that was undermining their life, their work, their school, all of that.” Signor said.

The tipping point for Signor wasn’t realizing how many of his college friends were vaping, but realizing how many of his younger sister’s 13-year-old friends were. “Currently we have a system where if you make one poor decision as a kid and start smoking cigarettes or e-cigarettes, as so many now are, you’re going to be addicted forever. That needs to change.” Signor said.
At the end of his freshman year, Signor began working to find a solution to treat nicotine addiction in a way that would be effective for young people.
For the treatment to work, it had to maintain the social and behavioral aspect of smoking. The treatment needed to be

something that cigarette and e-cigarette users could inhale to activate the same reward response that comes with smoking. This meant that one of the most important things would be nailing the development of a new inhalation technology.
Signor reached out to engineers at Aradigm, which was previously one of the leading inhaled drug delivery companies. Each engineer he spoke with pointed him to one person: Jeffrey Schuster, PhD, an astrophysicist renowned for his work in inhaled drug delivery. Schuster agreed to join the Miist team and help build a better inhalation device for smoking cessation.
During his junior year, Signor’s idea caught the eye of Entrepreneur First, a European talent investor, who wanted his team to move to London. Signor left school, and for four months operated out of London, raising more than $250,000...

72 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / MIIST THERAPEUTICS
Scan to read the full story or go to healthtransformer.co
Diatech Diabetes Upgrades Diabetes Care Through AI-Powered Infusion Monitoring
T1D MOONSHOT
Co-founders John Wilcox (R) and Luis Ernesto Blanco (L) are on a mission to transform diabetes management through their highly efficient AIpowered infusion monitoring software. This new technology will not just improve the lives of people with diabetes but also revolutionize the way insulin pump manufacturers approach diabetes care.

PPicture this: You are living with diabetes, and your pancreas either doesn’t produce enough insulin or cannot use it effectively. But you have found a convenient and precise way to provide your body with the insulin it needs, something that comes with fewer jabs than insulin injections – an insulin pump.
You learn that an insulin pump operates just like your pancreas, continuously delivering small amounts of insulin (the basal rate) to your body. You curiously study the nifty device’s parts–a compact pump that can be worn on a belt or placed in a pocket, a tube, and an infusion set with a cannula to be inserted under your skin. You are pleasantly surprised when you discover that the insulin pump also lets you deliver
bolus doses (extra amounts of insulin to cover meals or correct high blood sugar levels) to your body by pressing a few buttons.
With the insulin pump attached, you feel like you have a tiny superhero by your side that keeps your blood glucose (BG) levels in check as you go about your daily routine. Then one day, you suddenly feel extremely thirsty, overly tired, and nauseous (symptoms of hyperglycemia or high blood glucose). Your continuous glucose monitor (CGM) shows BG readings above 300 mg/dL. You panic and press the button to deliver a bolus of insulin to your body and wait for the BG level to return back to normal, only to watch it continue rising.
Insulin pump infusion failure occurs
startuphealth.com 73
MEET THE HEALTH TRANSFORMERS
when the insulin pump tries to infuse into the connected site, but the tissue is either too inflamed for the medication to successfully be delivered, the insulin leaks from the injection site, the cannula on the infusion set is bent, or there is an occlusion of the flow path causing insulin to build up in the line. These issues can cause disturbances to the flow of insulin and may prevent an accurate medication dose, resulting in an under or over delivery of insulin that can cause severe glucose levels. The scary truth is that it is very common, with over 250K incidents reported yearly.
The trickiest part is that sometimes these infusion failures can be so sneaky that they go undetected, making efficient diabetes management quite a roller coaster ride without the fun. But fear not because Diatech Diabetes’ SMARTFUSION™ app is here to get your pump back on track.
ORIGIN STORY
John Wilcox and Luis Ernesto Blanco met at Florida State University’s senior thesis research lab and found themselves on a journey that would change not just theirs but millions of people’s lives forever.
John, who was diagnosed with type 1 diabetes at the age of nine, had always seen the disease as an opportunity to make a difference rather than a disability. So, for his senior thesis, he chose to address a problem he was quite familiar with–insulin pump therapy and leak detection.
“I really wanted to do something for my insulin pump. You rely on it to give you medication, and sometimes it can just leak. And the only way you know is when it's too
late,” says John.
John’s innovative idea involved a colorimetric leak detection method, where leakage would cause a visible color change. When Luis, passionate about personalized medicine and having family members living with the disease, learned about John’s ideas and struggles, he felt an immediate connection.
Driven by their shared interests in diabetes technology and entrepreneurship, John and Luis wholeheartedly took up the challenge of developing biomedical engineering solutions that would reduce the impact of insulin pump infusion failures.
During their research, John and Luis recognized a handful of critical issues in the industry.
First, manufacturers weren’t incorporating better infusion failure sensors into CGMs and insulin pumps. Instead, they focused on hardware adjustments, like changing the infusion set adhesive and altering the cannula design to prevent infusion failure. Although reducing infusion failure is important, the risk of infusion failure remains with these improved systems.
The second was the dermatological nature of infusion failures and the lack of standardization in the infusion set technology. Infusion failures could happen anytime due to compromised attachment, improper insertion, or accidental bumping into a hard surface. The existing insulin pumps had occlusion systems that detected blockages, not issues like dislodgements or leakages. In addition, the detection time varied widely, ranging from a few seconds
74 StartUp Health Magazine / EXPONENTIAL PROGRESS
THE
/ DIATECH
MEET
HEALTH TRANSFORMERS
DIABETES
to a few days, making potential failures lifethreatening.
The third involved the industry’s shift towards automated insulin delivery (AID)–combining continuous glucose monitors with insulin pumps to regulate insulin delivery automatically. This made them realize the heightened need to make infusions monitored and safer by leveraging software solutions, which became the guiding principle behind the development of SMARTFUSION™.
In 2018, John and Luis established Diatech Diabetes as an LLC in Florida. They later joined a medical device accelerator in Memphis, Tennessee, and were incorporated as a Delaware C-Corp. Over the years, they have achieved significant milestones, including receiving a phase one SBIR grant from the NIH in 2021 and establishing R&D partnerships with two insulin pump companies for full software integration.
John and Luis’s ultimate goal is to integrate their software algorithm with existing on-market pumps through licensing or intellectual property acquisition. Recently, they secured fundingfrom JDRF, a momentous milestone for their work. With ongoing integration studies and future clinical trials, they are on track to bring SMARTFUSION™, their pre-FDA-approved algorithm, to fruition, representing a promising advancement in diabetes care.
UNDER
THE HOOD
SMARTFUSION™ is a software-based platform that monitors insulin infusion in real-time, providing critical benefits for

people with diabetes and insulin pump manufacturers. It ensures proper insulin delivery and alerts users to replace the pump's disposable part when needed to prevent potential hyperglycemia and even fatal outcomes.
In technical terms, SMARTFUSION™ integrates with existing on-market insulin pumps and accesses their onboard occlusion system sensors. Data from the sensors are then captured, processed, and analyzed to detect occlusions, leakages, failed insertion, and dislodgement. Once a failure is detected, the app sends instant personalized alerts to patients and caregivers. Preclinical trials have demonstrated an impressive 97% classification accuracy of the SMARTFUSION™ algorithm, establishing its reliability and effectiveness.
In an already saturated insulin pump market, manufacturers can leverage SMARTFUSION™ as a value-adding feature to differentiate themselves and be the preferred option for people with diabetes.
To underscore the importance of this technology, Luis extends the results of a survey involving more than 700 participants. It revealed that nearly 41% of the respondents experienced at least one infusion failure per month. “Patients usually receive a box of 10 infusion sets at the beginning of each month...
startuphealth.com 75
Scan to read the full story or go to healthtransformer.co
Joydays Offers a Line of Snacks that Provide 'All the Sweet without the Spike' for Patients with Chronic Conditions
CURE DISEASE MOONSHOT

YYou can’t sugarcoat the numbers: diabetes and other conditions related to chronic blood sugar imbalances are on the rise. Currently, 7.3 million people in the US have diabetes and 96 million people aged 18 or older have prediabetes. Besides diabetes, high blood sugar and metabolic dysfunction is strongly associated with heart disease, stroke, dementia, mood disorders, and the majority of cancers. A 2021 study estimates that 2.4 million deaths could be prevented just by reducing 20% of the sugar in processed foods. We are addicted to sugar, and this addiction is killing us.
Despite the clear and present danger excessive sugar consumption presents, it’s hard to cut it out of our diets. Some people lack access to healthier options because
of food deserts in rural and lower-income areas. For others, it’s hard to change habits, especially since our brains naturally see sugar as a reward, which gets reinforced from childhood. We treat ourselves to something sweet when we’re down, or need a pick-me-up, or are celebrating, or got through something hard. And then there’s the fact that added sugars hide in so many foods, even those we view as healthy.
Even when consumers are motivated to consume less sugar — say someone with Type 1 diabetes or a health enthusiast — the options are limited, particularly when it comes to ways to still enjoy favorite
76 StartUp Health Magazine / EXPONENTIAL PROGRESS
Founder Amy Cohn (right) — a media & tech exec and cancer survivor — has launched a next-gen food company that is redesigning our favorite snacks to help people manage diabetes and improve metabolic health.
MEET THE HEALTH TRANSFORMERS
foods without causing a blood sugar spike. Diabetes brands like Glucerna are ripe for disruption; they look and taste medicinal and don’t register as a treat. ‘Better for you’ brands of food might lower the sugar content, but are often high in saturated fat or low in the fiber your body needs to help balance blood sugar. Some protein bars come closer to achieving a low glycemic index, but don’t scratch the itch to eat a favorite snack, like a chocolate chip cookie.
ORIGIN STORY
Amy Cohn never thought she’d start a packaged food company. For years she thrived as a product manager, starting at Disney leading the product, social media, marketing, and community management team for ABCFamily.com. Her success there catapulted her to Head of Product & Digital Partnerships for the Oprah Winfrey Network (OWN), where she developed the product and social strategy for Oprah.com and the magazine, including the Emmy-winning Oprah’s Lifeclass. After OWN, Cohn moved from media to tech innovation and ultimately started a successful consulting company that worked with high-growth startups. Then, in 2020, she was diagnosed with colon cancer.
“My diagnosis changed everything. I had a deeper empathy for those with chronic conditions and discovered who is affected the most by certain diseases and why.”
This included learning about the link between metabolic health and colon cancer. People with Type 2 diabetes, for
instance, have a 27% greater chance of developing colon cancer. She also discovered that there’s a growing number of people in their 30s and 40s diagnosed with colon cancer and that it is linked to rising obesity numbers and unhealthy diets.
During her recovery, Cohn knew it was important to eat foods that kept her blood sugar stable, but found herself disappointed with the options, especially if she wanted a little treat. Products from the diabetes aisle at the drugstore didn’t satisfy, plus, “they felt ‘otherizing.’ When something like that is sitting on your desk at work, it feels like a signal that you’re sick, or something’s wrong with you,” Cohn explains.
Her product manager brain kept ruminating on the disconnect she saw between the communities most at risk for conditions related to high blood sugar and their access to and engagement with good options to mitigate that risk. She thought of where she was raised in West Texas, and the farmers in her family who worked hard growing crops for other people but lived in a food desert. How do you help someone to take the first step towards habit change when it comes to their sugar consumption? What’s the lowest barrier to engagement with more balanced food? What food do people have the hardest time giving up but might consider switching out for a better alternative?
She started exploring the market, and talking to people with diabetes about what they missed eating the most. Their answer: cookies. Good cookies. Chewy cookies. Cookies that were like their old standbys. Cookies whose packaging didn’t scream “I
startuphealth.com 77
have a chronic health condition!”


Cohn’s mission was clear: crack the better-for-you-cookie code. She brought together a team of experts, including Dr. Francine Kaufman, an endocrinologist and former president of the American Diabetes Association and Meg Moreta, MS, RDN, CDCES diabetes dietitian, to guide the nutritional balance; chef Aron Pobereskin, of Noma and Alinea, who oversaw the all important taste component; advisors such as Pat Turpin the founder of popchips and Roberto Pineda, a well-regarded R&D and baking innovation executive, among a group of other talented individuals who wanted to make the sweet dream of low-glycemic snacks that still taste like classic, familiar flavors a reality.
They tinkered, baked, tasted, and tinkered again. For many of these experts, it was the hardest project they’d ever worked on. It was one thing to get the nutritionals right and quite another to create a cookie that brought joy into someone’s day the
way a cookie ought to. But after more than 150 production trials, their hard work paid off in the form of soft, chewy, chocolate chip, double chocolate, and peanut butter cookies, made with 3 grams of sugar, 10 grams net carbs, and 5 grams of fiber.
UNDER THE HOOD
Joydays is a next-gen food company that creates blood-sugar-balanced snacks that taste like familiar favorites. Their first product offering is low-glycemic cookies that contain 70% less sugar than the leading chocolate chip cookie and 75% less saturated fat than the leading keto cookie, while providing a good source of fiber. These cookies are diabetes-friendly without looking or tasting pharmaceutical.
While their initial target audience is people with diabetes or other health concerns who are trying to cut back on sugar, Joydays also plans to capitalize on the growing awareness around the importance of keeping your blood sugar level stable. Biohackers, fitness bloggers, and the health conscious know it’s better to avoid glucose spikes and actively seek out products that balance blood sugar levels. In a 2021 survey, 72% of consumers said they were trying to reduce their sugar intake, which has a huge impact on the $24B sweet baked snacking category... Scan to read the full

78 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / JOYDAYS
story or go to healthtransformer.co
Difinity Solutions Introduces the First Modular, Multi-Dose Emergency Medication Delivery System
CURE DISEASE MOONSHOT
Co-founders and long-time friends Dr. David Kim (right) and Damien Tak describe their innovation as “EpiPen meets Coffee Pods.” Their new way to deliver life-saving rescue medications like naloxone and epinephrine could lower costs while increasing speed and accuracy to save lives.

IImagine you are enjoying a meal at your favorite restaurant with friends. A waiter shouts for help as a man has collapsed from an overdose. He’s not breathing. His skin is blue and you have a matter of seconds to save his life. You’re handed a naloxone kit, an overdose reversal medication. Fumbling with a syringe and needle, you break open the medication vial, carefully drawing up the medicine into the syringe. This takes time. Though you’re one of the few people who has actually been trained in delivering naloxone, you’re hesitant because you’ve never done it before and you know that errors can be deadly. You double check, making sure that you are giving the man the right drug. Then you check the dosage in the syringe. Wait,
now you need to tap on the syringe, pressing the plunger to remove bubbles. By the time you’re ready for injection, it’s too late. More than a million people have died since the opioid crisis began. More lives have been lost from opioids than from COVID-19. In 2020 alone, there were 90,000 drug overdoses. 250,000 lives are lost every year due to medication errors. Confusing and slow medication delivery modalities contribute to the crisis. It can take up to five minutes to draw up and deliver a medication like naloxone using the
startuphealth.com 79
MEET THE HEALTH TRANSFORMERS
MEET THE HEALTH TRANSFORMERS / DIFINITY SOLUTIONS
traditional needle and syringe model. In many cases, one has less than 60 seconds to save a life. “Five minutes later” is too late.
Furthermore, $19B is spent annually on medical errors due to the slow delivery of medication, wrong dosage, or wrong medication. The CDC estimates that the total economic burden of the opioid crisis in the US is $78B per year. People can’t get the rescue life-saving medicine they need on time, and when they do, errors practically bankrupt the system. It’s time for more innovative approaches.
Difinity is presenting a solution so seemingly simple you may be surprised it doesn’t exist yet.
ORIGIN STORY
David Kim, MD, and his best friend, Damien Tak, met in university. David went into pre-med as Damien went down the engineering path. After college, they had an idea as their independent experiences merged around the opioid crisis.
Damien was at a Vancouver restaurant with physician friends when a man collapsed. Frothing at the mouth, skin blue, and not breathing, he was dying from an overdose. Damien watched as his friends called 911. When the paramedics arrived, the first responder assured the bystanderphysicians that he knew what he was doing. Believing he was reaching for naloxone, the paramedic grabbed the wrong drug. Thankfully, Damien’s friend caught the potentially fatal mistake and alerted this paramedic. The experience made an impression on Damien: If a deadly misstep so easily entangled a trained professional,
how much more were well-meaning bystanders liable to make critical errors?
Around the same time, Dr. Kim saw the same problem from a medical professional’s point of view. He knew the power of delivering naloxone as an overdose rescue drug but was taken aback that the drug delivery system — the old method of drawing up the dose using needle and syringe — was so outdated. He witnessed first-hand the regularity of syringe and medication errors as well as how long this method took even for trained professionals.
Shortly after Damien’s experience in the restaurant, he and David imagined a plugand-play auto-injector inspired by coffeepod machines. It would be the “Swiss army knife” of auto-injectors. While drug manufacturers historically develop, sell, and make large returns from their own autoinjectors, such as the EpiPen, many medications are now generic. In addition to this, all emergency autoinjectors in the market are single use, disposable, and made only for a single drug indication. This allowed David and Damien to think outside of the box, taking the EpiPen idea and combining it with pre-filled pods which can be swapped in and out.
In 2019, the company launched. The early days were spent working on patenting and prototyping. In 2022, Difinity raised their first round of capital and improved the design. Their next step is to achieve a “design lock” and work on gaining FDA approval by 2026.
UNDER THE HOOD
David and Damien are designing the
80 StartUp Health Magazine / EXPONENTIAL PROGRESS
world’s first interchangeable, multi-dose, and modular emergency medication delivery system.
A few factors differentiate this auto-injector from the pack. One, the pods have preset doses of medication which eliminate room for error. Two, the pods are color-coded and bar-coded which improves accuracy. Three, a simple two-step process reduces delivery from a cumbersome five minutes with a traditional vial, syringe and needle to less than 30 seconds with their auto-injector. Four, while today’s autoinjectors, such as the EpiPen, are expensive and single use — the entire unit must be replaced when the drug expires every year — Difinity’s unused medication pods can be replaced much more cheaply instead of replacing the entire autoinjector. Lastly, the modular injector eliminates bulky kits and allows for multiple medications (pods) to be carried with one universal injector. As an example, the military currently carries eight or more different injectors as well as multiple drug vials, syringes, and needles in a kit. Difinity’s system can simplify their kit to one universal injector with a suite of pods.
Difinity is initially focusing on the opioid crisis and developing a naloxone pod for bystanders and first responders. Next, they plan to develop a pod solution for epinephrine. Difinity believes their autoinjector system can ultimately become a tool for all emergency medications.
FINAL WORD
Auto-injectors just make sense. Preloaded with the right amount of medica-
tion, even a child can use them safely and potentially save a life. But for too long these devices have been expensive, singleuse, and limited to very few medications. We’re proud to back Difinity because they’re changing this entire drug-delivery paradigm. Their elegantly simple system — modeled after the coffee pod phenomenon — has the potential to save lives and reduce costs on a grand scale. Military medical kits can be replaced and simplified. The widespread impact may include their injector packaged in every first aid kit, found with AEDs, sold for non-emergency use like supplements, outpatient use, and more.
We’re also proud to back Difinity because their founding team combines ingredients that are essential to a strong health moonshot company. Both Dr. David Kim and Damien Tak have witnessed the opioid epidemic, and the crisis of medication delivery, but from different angles. Dr. Kim works with patients daily as an emergency physician and sees the impact of medication errors on the broader healthcare system. As an engineer, Damien Tak has seen the power of disposable pod technology leveraged in other industries. And this experience is bound together by a decadeslong friendship that will help the team persist during the inevitably long road of FDA approval and commercialization.
Easy-to-use, interchangeable auto-injectors for rescue emergency medications is an idea whose time has come, and Difinity is bringing it to life.
Learn more & connect with founders at startuphealth.com/portfolio
startuphealth.com 81
MEET THE HEALTH TRANSFORMERS

82 StartUp Health Magazine / EXPONENTIAL PROGRESS
MiSalud Health Brings SpanishLanguage Virtual Care Rooted in Mexican Culture to the United States
ACCESS TO CARE MOONSHOT
A team of co-founders are building on their Silicon Valley experience and a tech surge in Guadalajara, Mexico, to create a new virtual care offering for Spanish-speakers in America. It’s a holistic, culturallyresponsive approach to health that’s a breath of fresh air for an often under-treated community.
IIt’s payday at a medium-sized onion farm in Southern California. The workers, the majority of whom are seasonal migrants from Mexico, gather in the break room waiting for their checks. The HR representative enters the room, hands out the paychecks and then attempts to tell the employees about some health benefits. The problem is, he speaks no Spanish. And even if he could, chances are that the healthcare providers available might not speak Spanish either — less than 5% of doctors and nurse practitioners in the US do.
Now, imagine instead that at this same payday, a team of Spanish-speaking doctors and healthcare providers are on site.
They give a presentation to the employees in Spanish and provide health screenings then and there. The employees have their blood pressure checked, height and weight recorded, and blood drawn for routine labs. As a result of these screenings, it’s discovered that more than 74% of employees have severe unmanaged chronic health conditions, like diabetes, hypertension, and high cholesterol.
But it doesn’t end there. Communication with the same healthcare provider continues using a mobile app. The workers get follow-up care and a health plan from someone they’ve met and trust. If they don’t respond to letters or notifications on the app, they get a phone call to walk them through what

startuphealth.com 83
steps they need to take for their health. It’s a relationship — a relationship with someone who understands their culture, who can, for example, talk someone with diabetes through lowering their carb intake while taking into account that a tortilla is a staple food of their diet.
ORIGIN STORY
The scenario above isn’t just an exercise in imagination. It’s a real case study from MiSalud Health, a fast-growing Spanishfirst bilingual digital health platform. It’s the brainchild of three co-founders
— Cindy Blanco, Wendy Johansson, and Bismarck Lepe — who’ve known and worked together on different companies for the past 15 years, brought together by a shared vision and passion to champion equity and access in tech for underrepresented people and communities.
For instance, over the past ten years or so, the trio has worked towards establishing a thriving tech hub in Guadalajara, Mexico. In 2016, Blanco co-founded StartupGDL, an organization dedicated to attracting global high-growth tech startups to the area, contributing to education, economic development, and equity in the IT ecosystem there. StartupGDL is a sister organization to Wizeline, a technology services provider of digital solutions, co-founded by Johansson and Lepe. Together with other innovators, they’ve created opportunities for growth in the region, connecting Mexican tech workers to the global economy and changing the lives of families through access to better paying jobs.
The impetus to address health concerns for Latinos in the US came when the pandemic exposed the dramatic healthcare inequalities for the population. For instance, Latinos in California were three times more likely to get COVID and then three times more likely to die from it. These statistics hit close to home for Lepe. His parents were migrant workers who spent May through December of each year while he grew up working on the Pacific Coast. He knew firsthand how difficult it was for them to access healthcare in these jobs.
The trio found themselves asking what impact they could make to create access to healthcare for the 42.5 million people in the US who speak Spanish as their native tongue, especially those with limited resources. They brought together some of the best technologists and thinkers they’d worked with before to problem solve on how to close the health equity gap in the Latino immigrant population, and create impact for their families back at home in Mexico. They envisioned a way to connect laborers and migrant workers to Spanish-speaking healthcare workers, using the same model they used to connect Mexican IT specialists and software engineers to the world. In 2021, they launched MiSalud Health.
UNDER THE HOOD
The MiSalud Health digital platform provides both physical and mental health services to the global Latinx population, starting with the states in the US with the highest Spanish speaking populations: California, Texas, and Florida. It’s
84 StartUp Health Magazine / EXPONENTIAL PROGRESS
THE HEALTH TRANSFORMERS / MISALUD HEALTH
MEET
Spanish-first, bilingual virtual care, so that families with varying fluencies can utilize the same app.
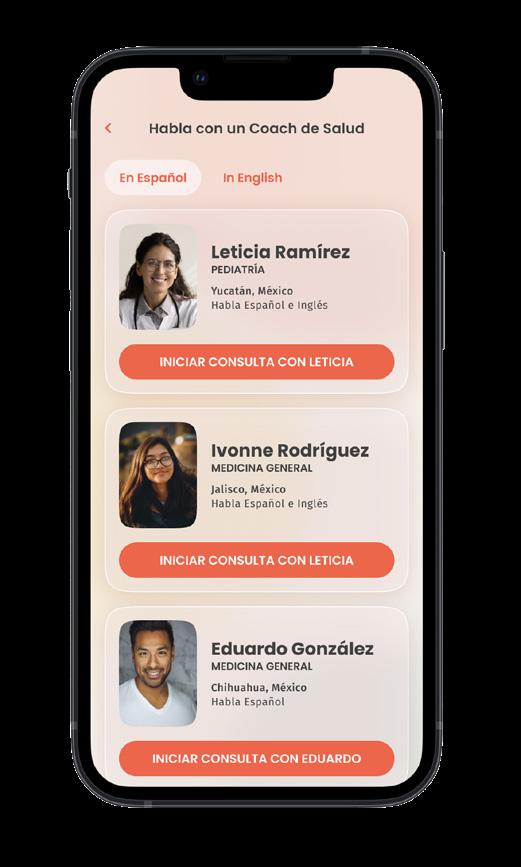
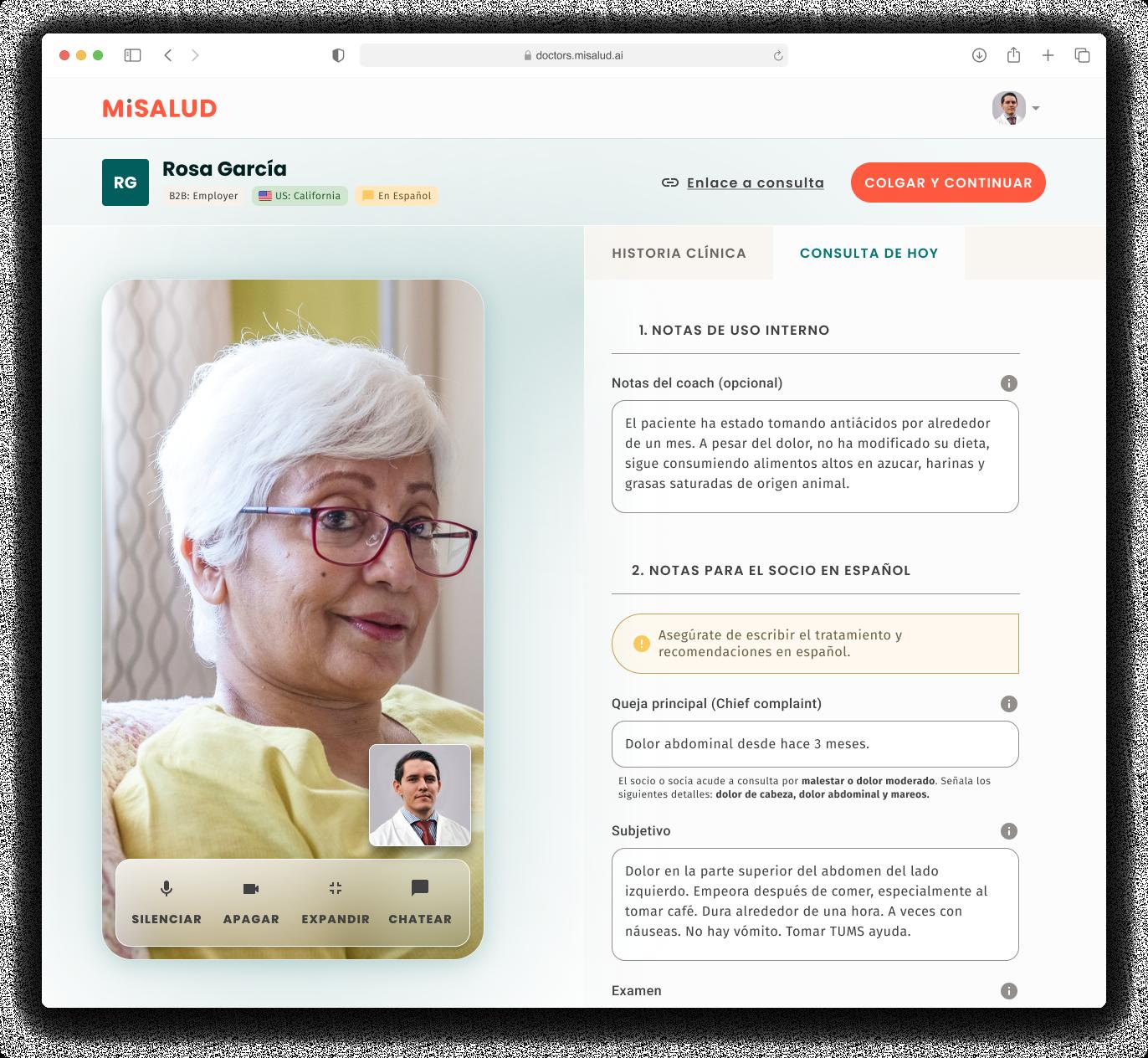
“Everyone on our team is fully bilingual and lives the same culture of our patients so they can deliver quality, culturally-appropriate care,” explains Johansson. “We know that when someone feels heard and understood, there are better health outcomes.”
While available directly to consumers as a subscription app, the majority of their business comes through employers who offer MiSalud Health to their Spanishspeaking employees. A key component and differentiator of the business is their handson approach to enrolling new users. As seen in the case study at the top, MiSalud Health comes to work sites, meets with the employees, and invests the time in establishing a relationship with them. It builds a level of trust that is necessary for real

health interventions to happen.
Once enrolled, employees can access a “health coach,” who is a fully licensed Latin American physician or psychologist. 80–85% of the consultations are focused on employees receiving preventive healthcare, managing chronic diseases or mental health issues, and preventing emergency department visits and unmet health needs. The other 15% or so of cases that require prescriptions, labs, or imaging, get passed onto Spanish-speaking US doctors. Either way, a core component of the care model is taking time with the patients and helping them navigate the healthcare system...
Scan to read the full story or go to healthtransformer.co

startuphealth.com 85
AuraSense Tech Uses Haptics to Help Physical Therapists Improve Hand Health
CURE DISEASE MOONSHOT

Recognizing a decrease in qualified healthcare professionals led this innovative “digiceuticals” company to develop better, more accessible care management for patients and providers through haptics and an immersive Metaverse experience.
TThere is a significant increase in demand for hand therapy care due to the aging population, pervasive technology utilization (i.e., video games, computers, cell phones), and work injuries. Despite this rise in demand, the number of physical therapists (PT) and occupational therapists (OT) who provide progressive treatment — exercises that work over a pe-
86 StartUp Health Magazine / EXPONENTIAL PROGRESS MEET THE HEALTH TRANSFORMERS
riod to heal, strengthen, and support better muscle and movement control — is on the decline. The International Society for Hand Therapy cites that there is one hand therapist for every 100,000 people in the United States. In addition, there are care deserts where the closest care provider is hours away from the patient. This makes providing care for those at-risk for worsening hand health in trouble and without a clear solution. Even beyond the demand and scarcity issues, care providers are underpaid, making it difficult to retain current clinicians or attract new ones. There is also limited access to actionable data that providers can use to improve outcomes. Both providers and patients are losing out in these scenarios, and the PT/OT system is suffering.
One critical question: How can clinicians gather better, more efficient hand movement data from patients in order to guide their care more effectively, and then present that data back to the patient in actionable ways?
The answer came from an unlikely source: a Portable Handheld Acoustic Speaker Disruptor invented for the US Navy.
ORIGIN STORY
Dr. David Charlot and Amber Ivey first met as kids. Both military brats, their parents were stationed in Stuttgart, Germany, where they became lifelong friends. Amber, whose background is in performance management and data, lives with multiple sclerosis (MS), enduring hand assessments with her doctor at every check-
up. She noticed little data collection other than her physician manually writing down observations that weren’t shared with her. Amber never knew whether she was doing the exercises correctly, if the way she performed the tasks meant she was getting weaker or stronger, or how the information gathered helped her condition.
David, an engineer with a PhD in bioengineering, has been involved with healthcare startups for the past 15 years, creating quantitative tools for better outcomes in the fields of cancer diagnostics, infectious disease, and drug discovery. He’s also the parent of a child with special needs who attends regular physical and occupational therapy appointments. When the pandemic hit and PT clinics shut down, in-home and Zoom sessions became the norm.
During one of these in-home sessions, David asked questions about the OT’s process. He explained he created digital healthcare solutions, and knowing his daughter’s needs he wondered if there might be a better way to approach her care. Perhaps it could be made easier for clinicians to use the information from these sessions to correlate certain activities to patient improvement and the therapist admitted they needed better tools for assessing progress and including their patients in their own care.
David’s initial thought was that immersive video game motion capture technology might work. After all, your entire body interacts with these activities. Why not use it for physical therapy and capture how the body is moving digitally rather than manually? Clinicians could then gather/process
startuphealth.com 87
data more efficiently, leading to more indepth analysis for optimum results.

To get started on this quest, David joined NSIN (National Security Innovation Network) Foundry, a Department of Defense technology startup incubator in March 2022. There he met Zavosh Zaboliyan, whose background was media, marketing, and advising companies on how to raise funds. Zavosh was living his own unsatisfying PT story due to a car accident and in speaking with David, he realized his experience was the norm and wanted to fix it for others.
At the incubator, David and Zavosh were paired with a team from NSWC CRANE working on a technology for peaceful crowd control and suppression. The team presented an acoustic speaker disruptor (a miniature sound gun) created to temporarily keep people from talking. Consisting of a “condenser shotgun” microphone with an ultrasonic transducer array pointed in the speaker’s direction,
within 200 milliseconds of speaking, your voice is projected back to you, causing you to stop talking. It’s based on the known psychophysics phenomenon that if you hear yourself speak out of sync, you’ll stop because you believe you’re talking to yourself (an experience common to those suffering from Schizophrenia). Intrigued, David jokingly asked if the technology could also create energy impulses that would make someone feel like they’re getting punched in the face. The team at CRANE explained how it could and David got a “eureka” moment thinking the solution can be adapted for use in physical therapy.
The final piece came together when Amber Ivey joined the duo, bringing her experience in data analysis and firsthand experience managing multiple sclerosis. The three formalized AuraSense Tech Corporation and completed the NSIN Foundry program, where they won a $20K prize on demo day, in the fall of 2022.

Through market discovery and business development conversations, the three discovered that about 20% of all US emergency room visits are hand-related injuries. The team spoke with veterans and other patients who mentioned still feeling lingering pain from years-old injuries and the inability to manipulate their hands efficiently because they never received optimal and complete care...
Scan to read the full story or go to healthtransformer.co

88 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / AURASENSE
Kinometrix Uses Predictive AI to Reduce Dangerous Falls in the Hospital
CEO Devina Desai (right) is leveraging her experience in patient safety, and close ties to health systems, to develop a fall risk platform that’s designed to reduce unnecessary injuries, curb physician burnout, and save hospitals millions.

FFalling down might not seem like a big health issue. But even for seemingly fit and healthy people, falls can lead to fractures, head injury, fear of falling, long-term disability, or death. You might think that patients already in the hospital would be protected from dangerous falls that could aggravate their condition or cause new health concerns. But counter-intuitively, in the one place where you hope you receive constant care, there is a risk of adding “injury to injury” from falls.
Falls are the most common preventable safety events in hospitals because facilities are often ill-equipped to predict and prevent them. Research shows that each year, about 700,000 to one million patient falls happen in hospitals in the United States.
These falls lead to about 250,000 injuries and 11,000 deaths.
Falls present a considerable cost for hospitals too. A 2023 study published in JAMA Health Forum estimates that each patient fall costs about $62,521.
Not to mention that treatment from a fall in the hospital doesn’t get reimbursed because associated injuries or harm are recognized as a “never event.” The Centers for Medicare and Medicaid Services (CMS) established the concept of “never events” to prevent “clearly identifiable, preventable, and serious” hospital-acquired conditions (HACs) and promote patient safety. And as of 2008, they
startuphealth.com 89 HEALTHY LONGEVITY
MOONSHOT
MEET THE HEALTH TRANSFORMERS
stopped reimbursing hospitals for caring for these conditions.
Human sitters — healthcare workers that stay with patients to ensure their safety — take up already limited resources, and more evidence is needed to show they work well at preventing falls. Camera or thermal bed monitors work precisely as intended; they monitor and alert clinicians when a fall occurs. They cannot predict falls and may even contribute to clinician fatigue. Manual fall risk assessment methods like Johns Hopkins Fall Risk Assessment Tool (JHFRAT), St Thomas’s Risk Assessment Tool in Falling elderly inpatients (STRATIFY), and Falls Risk Assessment Tool (FRAT) are subjective, undependable, and imprecise.
Addressing this persistent health challenge using predictive AI is Kinometrix President and CEO Devina Desai.
ORIGIN STORY
For many years Devina Desai worked in patient safety at Inova, a large healthcare system in Northern Virginia. Her interest in patient safety grew while doing clinical service and nursing research at Inova Fairfax. Her research role helped her better recognize the real and heavy cost of patient safety issues, particularly venous thromboembolic events (VTEs) at the hospital.
During her tenure at the hospital, she worked with a vendor called Kinometrix to validate their physical therapy device and data analytics platform. As part of her department’s validation process, Desai discovered the device did not significantly
impact outcomes. However she was impressed with the data analytics side of the platform. She and her team became curious if this could be used to address a more pressing concern — inpatient falls.
Kinometrix needed to pivot, and that meant identifying a leader who could guide a new vision. Innova and Kinometrix tapped Desai because of her deep understanding of patient safety, her work at a large health system, and her close working relationships with nurses and other providers.
Desai transitioned from Inova to Kinometrix and developed its first product, which now addresses the shortcomings of the traditional fall risk assessment systems and delivers a more accurate prediction of a person’s fall risk.
Today, Inova and Kinometrix have a collaborative relationship. The hospital has provided years of inpatient data to help the startup develop and validate its machine-learning platform and will likely be one of the first health systems to use the product.
UNDER THE HOOD
Hospitals gauge a person’s susceptibility to falls using manual assessment tools like the Johns Hopkins fall risk assessment, which uses a checklist to determine a patient’s fall risk score. This risk assessment method is subjective and timeconsuming, resulting in inaccuracy. It also cannot dynamically capture a person’s circumstances and risks as they change.
Kinometrix uses real-time data from a person’s electronic health record (EHR),
90 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / KINOMETRIX
with information like a person’s demographics and medications, to create an objective score of a person’s fall risk and risk drivers of the score. It also updates this risk score as information in a person’s EHR changes.
With the help of the Kinomterix fall risk assessment platform, clinicians can appropriately allocate fall prevention resources based on each patient’s personalized risk score.
Kinometrix operates on a machinelearning module. It’s constantly fed additional data to make it robust and more comprehensive. The more data that runs through it, the better it works.
Specifically, Kinometrix uses more variables than subjective assessment tools and about half a million patient records for its machine learning module for higher precision and accuracy than other risk assessment tools. Currently, it’s greater than 95% accurate at determining a person’s fall risk. For comparison, that’s about as accurate as a home pregnancy test. On the other hand, the accuracy of a manual fall risk assessment tool relies solely on the person using the tool. And that changes depending on how well the person uses it.
Plus, Kinometrix is easy to set up and runs instantly. It integrates seamlessly and works with any EHR vendor.
Fortunately, this fall-risk assessment platform is the first of the many patientsafety innovations the founders hope to build with Kinometrix.
Pressure injuries are another never event and a much more expensive problem than falls, costing healthcare systems
around $35 billion annually, compared to falls, which is $7 billion. Desai predicts that the next Kinometrix innovation will be a risk assessment platform that works better than and will replace subjective manual risk assessment methods like the Braden scale.
OUR TAKE
We’re proud to back Kinometrix because hospitals need a better way to predict and prevent falls. The toll of the status quo — in injury, death, and cost — is just too high. Falls and other areas of patient safety have plagued the healthcare system seemingly forever, and there’s been too little innovation applied to the sector.
But not just any startup could tackle such an entrenched problem. It’ll take a founder who intimately understands patient safety, hospital administration, and healthcare provider needs. We find that trifecta of experience in Devina Desai.
Finally, we’re excited to back the Kinometrix team because fall risk assessment is just the beginning. The founders’ goal is to develop a suite of products that promotes patient safety, reduces clinician workload, and conserves hospital resources and money.
Kinometrix protects lives, saves the healthcare system billions of dollars, prioritizes clinician needs and time, and lowers the burden of catering to never events.
Learn more & connect with founders at startuphealth.com/portfolio
startuphealth.com 91
EqualityMD’s Digital Health Platform Is Changing How the LGBTQ+ Community Perceives & Receives Care
HEALTH EQUITY MOONSHOT
Founder Justin Ayars (pictured) is building on more than a decade of LGBTQ+ advocacy, business development, and entrepreneurial work to create a virtual-first digital health platform that matches LGBTQ+ patients (and allies) with culturally-competent providers who are trained to create safe spaces where patients can be their authentic selves.

92 StartUp Health Magazine / EXPONENTIAL PROGRESS MEET THE HEALTH TRANSFORMERS
JJustin Ayars has a unique background. His godfather was Liberace, his father was a renowned musician who worked with Elvis and Barbra Streisand, and his grandfather worked for the CIA since the agency was created in 1947. Presented with these unusual paths, he instead chose to become a trial lawyer. As fate would have it, he ended up in the courtroom defending health insurance companies and large corporations throughout the DC region. His experience on the “dark side” of the healthcare litigation table showed him the imbalances of power and systemic inequities that plague the nation’s healthcare system. He wanted to fight for the oppressed but felt like there was nothing he could do as a corporate/insurance defense attorney. When layoffs trickled through law firms during the great recession, Ayars saw his as a blessing in disguise and vowed never to return to healthcare.
In the early years of the great recession, Ayars moved to Richmond, Virginia, and began a 13-year journey as a serial entrepreneur. He started a coffee business, a restaurant/nightclub, a marketing/media company, and a consumer behavioral data analytics company. The common thread through each endeavor was Ayars’ desire to create safe havens where the LGBTQ+ community could connect, be heard, and feel valued. Over time, Ayars became a highly sought-after educator/ speaker, influencer, and award-winning LGBTQ+ leader. In 2012, he established a LGBTQ+ chamber of commerce in
Richmond, and in 2019 he spoke about the economics of equality at the Lincoln Center in NYC during World Pride.
In 2019, Ayars created Equality Rewards, a consumer behavioral data analytics platform that helped consumers find LGBTQ+ inclusive companies and helped companies understand how to authentically engage the $1.4 trillion LGBTQ+ consumer market. But it turned out that this product was just a warm up. Ayars realized that general consumer behavior wasn’t the deeper problem he wanted to solve.
The one question he’d been asked by LGBTQ+ individuals throughout his years was, “Where can I find a doctor who makes me feel safe?” As healthcare became top-of-mind for everyone during the height of the pandemic, Ayars saw a business opportunity to create a new healthtech product that connected LGBTQ+ patients with inclusive providers on a secure platform where providers conducted telehealth sessions. Ayars’ hope was that this new product would bridge decades of health equity and data gaps which have prevented the LGBTQ+ community from experiencing inclusive healthcare.
In September of 2020, Ayars tested his theory by participating in a weekend hackathon sponsored by StartOut (a nonprofit supporting LGBTQ+ entrepreneurs) and created a fictitious company called “Pride Doctor” that matched LGBTQ+ patients with inclusive providers. Pride Doctor was a hit and created incredible buzz throughout Ayars’
startuphealth.com 93
MEET THE HEALTH TRANSFORMERS / EQUALITYMD

various networks. After swearing never to return to healthcare, in December 2020 he transformed Equality Rewards into equalityMD and began a new mission: Changing how the LGBTQ+ community perceives and receives healthcare.
CHALLENGE
In 2016, the NIH declared the LGBTQ+ community to be a “health disparity population” due to unique healthcare concerns and an historic lack of access to care. For Justin Ayars, while the NIH declaration was validating, it was something he already knew from experience.
This type of discrimination takes many forms, says Ayars. It exists from the waiting room to the emergency room and at every touchpoint in-between. A key factor, Ayars adds, is that discrimination can exist at the earliest interactions people have when seeking medical care: the intake form, the receptionist, even the layout and design of the waiting room. If a patient does not feel seen, heard, and accepted in a medical setting, they won’t feel comfortable, safe, or welcome to be their authentic self. When patients aren’t their authentic selves with medical providers, they will not get the full spectrum of care they may require. Seemingly small acts, omissions, and behaviors healthcare providers exhibit can be perceived as microaggressions that deter LGBTQ+ patients from coming out to their providers or even seeking the care they need.
That lack of care is a major problem. 56% of LGBTQ+ patients report expe-
riencing discrimination from within the healthcare system, ranging from providers and pharmacists to hospitals and insurance companies. It’s estimated that 28% of the LGBTQ+ community chooses not to seek care, even in dire circumstances, which causes health and wellness issues that affect entire communities and forces an undue economic burden on corporations, nonprofits, and families. This avoidance of care translates into a loss of 1% of the US GDP per year due to illness, absences, and even death.
Today, the LGBTQ+ community is forced to rely on word-of-mouth to find healthcare providers who understand and appreciate their intersectional identities and care for them with the dignity and respect every patient deserves. EqualityMD is changing that.
UNDER THE HOOD
EqualityMD is an online subscription service that utilizes a machine learning algorithm to match providers with patients. The platform calculates a patient’s personal preferences to create a custom list of providers tailored to their needs. Every provider on the platform has completed evidence-based LGBTQ+ cultural-competency training so they know how to create safe spaces where patients can be their authentic selves...
Scan to read the full story or go to healthtransformer.co

94 StartUp Health Magazine / EXPONENTIAL PROGRESS
LumosTech Provides Circadian Rhythm Misalignment Relief for Night Shift
Workers and JetLagged Travelers
HEALTHY LONGEVITY MOONSHOT
Working with renowned sleep disruption specialist Jamie Zeitzer, PhD, CEO & Founder Biquan Luo, PhD, pulled from her own experience suffering travelinduced fatigue to develop a noninvasive solution for the masses.

compasses travelers across multiple time zones and individuals working sliding shift schedules that include night hours. Several industries are affected by this unnatural sleep pattern, and the result — circadian rhythm misalignment or circadian clock disruption — impacts the lives of both the sufferer and those around them.
For those relying upon their physical and emotional wellness for their livelihood, being out of sync with nature’s internal clock puts their performance and overall quality of life at risk.
Circadian clock disruption can maniA
Approximately 95 million people in the US sleep at times against their body’s natural rhythm. This en-
startuphealth.com 95
MEET THE HEALTH TRANSFORMERS
fest through insomnia, irritability, excessive sleepiness while performing tasks, memory loss, and even long-term health disorders such as cancer and diabetes. The by-products are accidents, loss of income, self-esteem issues, debilitating health problems, and strained relationships. Employers face lower productivity, an increase in accidents and human errors, higher levels of burnout and churn rate, rising insurance costs, and lost revenue of $63.2B each year.
Jet-lagged travelers and night shift workers combat circadian rhythm misalignment with the usual suspects of solutions: caffeine, nicotine, and forcing oneself to stay awake to hopefully reset their internal clock; alcohol, marijuana, supplements, drugs, and naps to help them sleep. These, however, are temporary, build tolerance, create serious side-effects, or simply don’t work, leading to health issues. While attempts to shift slumber schedules by staying awake can accumulate enough homeostatic sleep drive — the process during the day that increases your desire to rest at night — the circadian rhythm remains unchanged, leading to sufferers waking earlier the next morning and unable to sleep at all the next day.
The current devices and apps designed to combat the issue by using light to boost the circadian rhythm are not sustainable. Bulky and not at all user-friendly, they are invasive and require a level of participation that may interrupt rather than support sleep. Night-shift workers and jet-lagged travelers need something that works with the body’s internal clock
to adjust its sleep schedule to unnatural routines without disrupting their lives and putting them at further health risk. They need a solution that enhances performance and wellness by incorporating seamlessly into the sufferer’s life.
Where would such a solution come from? As the saying goes, “experience is the teacher of all things,” and through shared, empathic experience, LumosTech created just such a solution.
ORIGIN STORY
Biquan Luo received her PhD in Genetics, Molecular and Cell Biology at USC then followed up with postdoctoral studies at Stanford. Originally from China, she flew across multiple time zones whenever she had a break. Dr. Luo discovered that as soon as she adjusted to local time, she had to return to the States, starting the process all over again. She suffered from serious jet lag, making it harder to get her mind and body back on track.
Around this time, Dr. Luo was exposed

96 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / LUMOS TECH
to Jamie Zeitzer, PhD, and his decades of research into how the human body’s circadian rhythm was regulated. She discovered she wasn’t just going through jet lag, but circadian rhythm misalignment or circadian clock disruption. The more Dr. Luo learned about the body’s internal clock and how it influenced not only sleep but overall health and wellness, she realized others must be experiencing the same issues and wanted to figure out a way to fix it for everyone. But how?
Focusing on jet lag, Dr. Luo worked with Dr. Zeitzer on tricking the body’s circadian rhythm into believing it was on a regular sleep and wake schedule even while shifting across time zones. They did this using light to reflect the circadian rhythm’s natural ebb and flow.
Our internal clock works on a 24-hour cycle, naturally tied to the rising and setting of the sun. Light influences its effectiveness, regenerating our body’s different systems and the chemicals that rejuvenate us. When that natural process is thrown off by pushing across various time zones where sunrise and sunset occur at drastically different times than what our bodies are used to, it takes a while to naturally adjust. While that happens, we’re physically and mentally out of sync, creating fatigue, exhaustion, and sleep deprivation even as we slumber because the act of sleeping isn’t the same as having a healthy, regulated circadian rhythm.
Dr. Zeitzer’s research revealed that short, gentle light pulses delivered during the night moved the circadian rhythm forward or backward, depending on the

need. Lab studies with human subjects in a tightly controlled, heavily regulated environment are one thing. Bringing it to life in the real world where people have far more distractions and unforeseen variables is quite another. Realizing a sophisticated algorithm could accommodate the dynamic actions and noise of real life, Dr. Luo and Dr. Zeitzer worked with a team of top scientists to develop algorithms — the true trade secret — then patented the entire experience.
Dr. Luo and her team sought and received funding from NASA to create a prototype to address circadian clock disruption for jet lag. They purchased an inexpensive, comfortable sleep mask and used Dr. Luo herself as the initial test subject. They wove electronic transmitters through the store-bought mask that communicated with the Bluetooth on her phone to receive the input gently and easily while she slept.
The goal was to have the algorithm work off the upcoming travel schedule then deliver the gentle light pulse during sleep in the days leading up to her trip without Dr. Luo changing her normal sleep/wake schedule. This naturally and gently adjusted her circadian rhythm to the local time of her travel before arriving and without disrupting her daily routine...
Scan to read the full story or go to healthtransformer.co

startuphealth.com 97
Replica Health Is Simplifying Type 1 Diabetes Management with Conversational AI


T1D MOONSHOT
Sam Royston (top) and Brad Jacobson are trailblazing a new era in Type 1 diabetes management with their platform. The Replica Health app will stand apart as an intuitive personal assistant, harnessing the power of conversational AI and natural language processing to offer actionable insight to users’ personalized queries in plain English.
IImagine walking on a tightrope, carefully balancing between two towering skyscrapers. You take each step with precision and unwavering focus. Now imagine doing the same blindfolded, unable to see where you’re going. All you can rely on are the numerous voices shouting contradictory directions. That’s what it feels like to be a Type 1 diabetic wearing continuous glucose monitors (CGMs) and insulin pumps. You get constantly bombarded with data but are starved for actionable insights.
As you stand atop the dizzying wire, you are handed a torrent of numbers, charts,
and alarms from the devices that help you keep your blood glucose levels in check.
Glucose readings, trend lines, insulin doses, carbohydrate intakes — it’s like drown-
98 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS
ing in an ocean of numbers, each representing your health. Suddenly, you realize that despite all the impressive technology at your disposal, you still lack the clarity and insights you desperately need.
Enter Replica Health, a wise personal assistant who analyzes all those data on your behalf and gives you answers in plain English.
ORIGIN STORY
Like so many founders in the diabetes market, Sam Royston’s desire to innovate came from a personal place. He was diagnosed with Type 1 diabetes at age 10 and then built a career as an expert in machine learning and data science. Year after year, as he grew in his knowledge, he sought ways to better manage his condition.
During his graduate studies at NYU’s Courant Institute in 2016, Sam began working on Type 1 diabetes directly. His work centered on predicting blood glucose levels and developing new algorithms to enhance these predictions. He also sought to leverage new data sources to improve the accuracy of blood glucose forecasts. This earlier research was the starting point for Replica’s technology.
Then, In 2017 Sam helped start an anomaly detection platform called VoteShield, which uses ML to make sense of civic datasets. That work brought his thinking to a new level, and introduced him to other collaborators with a similar passion for T1D.
What Sam came to realize was that while diabetes management had improved over the years, especially with the advent of
CGMs, it was still lacking in several critical areas. The most important of which was how people who wear insulin pumps and CGMs were creating tons of data but had a hard time correlating that with appropriate actions.
Unlike Type 2 diabetics, people with Type 1 diabetes generate a vast amount of data in their daily lives, as they have their blood sugar levels and insulin dosage constantly monitored. However, insulin pump data was often overlooked in retrospective analyses. The combination of insulin dosing and blood glucose data holds immense potential in understanding the carbohydrate release profile of various foods, the effects of various activities, and other metabolic questions.
The existing food-tracking software lacked the essential longitudinal analysis required to comprehend the full impact of a meal over time. A good understanding of the carbohydrate release profile demanded deeper insights into the timing and dynamic component of each individual’s data. And these picture-based apps, even with volumetric scanning, could only provide limited information, often reduced to scalar values like the number of carbs in a particular meal.
Sam and collaborator Brad Jacobson reached the conclusion that the key to better Type 1 diabetes management was to develop a method that incorporated all available time-based data, allowing for a comprehensive understanding of the metabolic responses to various meals, activities, and life events. In addition, they had to create a simple and intuitive solution, al-
startuphealth.com 99
lowing people with Type 1 diabetes to gain insights into their conditions and metabolic changes without having to constantly spend their time on data entry or finding their way around technical, confusing platforms.
A potential roadblock to developing the solution was the dynamic nature of data which had to be interpreted; often drawing from multiple sources. Using learnings from VoteShield, where a massive pipeline of evolving time-series data posed similar challenges, Replica overcame these issues quickly.
“When you have heterogeneous data sources like blood glucose and activity data from patients that should be brought into your platform, they should be constantly synchronized. The databases can shift under your feet, and it’s important to keep track of these changes to generate accurate outputs,” says Sam.

With every round of designing, Sam and Brad focused on making their platform’s interface simpler and simpler. They wanted to create a platform that would tell individuals using CGMs what they did right and where they went wrong. This way, they could leverage these insights to make informed decisions the next time they have a similar meal without excessively interacting with the app.
The result of their collaboration was Replica Health, an innovative platform that amalgamates data from multiple sources, including blood glucose readings and location information, to provide insightful reports and predictions. The app would fill a void in the market by offering

a unique natural language search interface, allowing users to query their data in plain English and receive detailed reports tailored to their questions.
Today, the duo is fine-tuning the app and working on numerous features to be added to the platform soon. They are also just weeks away from submitting their app to the app store.
UNDER THE HOOD
Replica Health is a user-friendly and intuitive app that utilizes data from CGMs and insulin pumps to create a feedback loop for users. It leverages conversational AI/natural language processing to decipher users’ complex and personalized questions about Type 1 diabetes and provide relevant answers...
Scan to read the full story or go to
healthtransformer.co

100 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / REPLICA HEALTH
Abvance’s Novel Coformulation of Insulin and Glucagon Could Revolutionize Diabetes Care
A team of scientists and physicians have discovered that insulin and glucagon, long thought solely to counteract one another as they lower or raise blood sugar levels, respectively, could actually work together for better and safer glycemic control. If their foundational work proves out, people suffering from diabetes who require insulin could have an easy and safe way to control their blood glucose levels more effectively without running the risk of hypoglycemia.
moment for Maggs, one that shaped his medical career.
I“It was like watching someone be resurrected.”
David Maggs, MD (pictured), recalls the first time he saw a patient with diabetes receive treatment with glucagon to counteract dangerously low blood sugar. At the time he was a junior doctor in Kent in the UK, working in the ER. Seeing patients wheeled in the door unconscious and seizing–basically on death’s doorstep–suddenly rally with a simple injection of glucagon was an amazing clinical
In the years to come, first as a trainee doctor, then as an endocrinologist, Maggs came to see the enormous burden type 1 diabetes (T1D) was for patients with the threat of hypoglycemia ever-present –”like a dark cloud hanging over their lives.” It’s a huge job balancing blood sugar on a daily basis. Too much insulin and you risk your blood sugar dropping low enough to cause a hypoglycemic event like the one above; too little and you risk long-term negative health effects. Besides the health challenges, it's a heavy emotional burden to live with diabetes, impacting spouses, children, how someone
startuphealth.com 101
T1D MOONSHOT
MEET THE HEALTH TRANSFORMERS
works and provides, and how someone lives a full life.
Medically speaking, two main peptides help people with T1D maintain their glycemic tightropewalk. Insulin brings blood sugar down when it is too high, and glucagon brings blood sugar back up when it drops too low. Because of their opposite functions, physicians and researchers have always considered them as adversaries, like two boxers duking it out in the ring. That’s certainly what Maggs thought, until one fateful evening in Boston when he was walking to a restaurant with Alan Cherrington, PhD, a world leader in understanding the roles of insulin and glucagon in the body.
On the way to dinner, Cherrington explained his recent animal studies to Maggs in which he put insulin and glucagon together, delivering the two peptides at the same time and at very specific molar ratios. Instead of the cage match the researchers anticipated, the two peptides actually responded dynamically to what the body needed: it wasn’t a fight, it was a dance, with each of the two peptides moving fluidly and intuitively to address rising and falling blood sugar levels. It was counter-intuitive thinking, but by the time dinner ended that night, Maggs knew he had to see what Cherrington’s research could mean for his patients with diabetes.
“THE DAMN THING WORKS”
Fast-forward to 2019, and travel south from Boston to Atlanta, and Maggs was doing just that–sitting in the back room of a clinical trial unit at Atlanta Diabetes
waiting to see how patients responded to receiving both peptides at once. As he sat with the clinical staff, Dr. Bruce Bode, a well-respected researcher in the insulin field and a founding partner at Atlanta Diabetes wherethe clinical trial was being conducted, walked into the room, stunned. “The damn thing works,” Bode said.
Even now, years later, after building a company around a planned coformulated offering of insulin and glucagon, Maggs seems incredulous at what they discovered in Atlanta. The glucose levels in the subjects in the Atlanta study behaved almost exactly as predicted. While the previous assumption was that delivering insulin and glucagon at the same time would be like simultaneously slamming on the brakes and accelerator in an automobile, it turned out that the two peptides, when delivered at a precise molar ratio, worked together to regulate blood glucose. When glucose rose, insulin dominated the actions of glucagon, and when glucose fell, glucagon dominated insulin in the opposing direction. The gas and the brakes responded as necessary, together making it a much smoother and predictable ride.
Together with Cherrington and peptide chemist Soumitra Ghosh, PhD, Maggs founded Abvance Therapeutics to develop a coformulation of short acting insulin and glucagon as a kind of “smart insulin” that responds in real time to blood sugar levels. The founders approached anotherbiotech company in 2019 for potential assistance in the coformulation work, and while thatcompany
102 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / ABVANCE
passed on the opportunity, the then US General Manager, Steve Daly, found the Abvance data incredibly compelling, so compelling that he eventually came on board as COO in 2023.
“I’ve worked in the insulin field for a large portion of my career and this really represents a holy grail type approach when it comes to insulin – better control, less hypoglycemia risk, and cost-effective, especially compared to therapeutic options coming down the road that are targeting the same clinical benefits and likely to carry a substantial pricing premium over today’s options,” says Daly.
Because the intervention utilizes two already FDA-approved treatments, ABV100’s target product profile for dosing and handling is one that’s barely a departure from the standard of care. For patients familiar with insulin dose determination and insulin delivery, their routine would hardly change, making adoption of ABV100 simple and straightforward. But the difference in results, in a product that unlocks an opportunity for improved glycemic control while reducing the risk and occurrence of hypoglycemia, could be enormous.
“Someone once described it as a ‘gentle insulin’ in conversation, and that really fits,” explains Daly.
ONWARDS AND UPWARDS
Abvance is on the cusp of having the necessary funding to advance their solution, called ABV100, into coformulation development, large animal work, and then IND (Investigational New Drug)

enablement with the FDA to move forward with testing in human subjects. Their proof of concept study in Atlanta, confirming that co-administering insulin and glucagon provided protection against hypoglycemia without worsening hyperglycemia, worked wonders in winning over skeptics who had long viewed the peptides as antagonists.
As they lay out the timeline and plan for eventual FDA submission, in the near term they will be refining the coformulation and experimenting with different types of insulins and glucagons in parallel. Once they have a candidate product, they plan to test it in different clinical product forms and insulin delivery modalities. Ultimately, the plan is that ABV100 will be available for patient use in vials, pens, and pumps wherever rapid acting insulin is used today.
Even as they get into the weeds of product development, the Abvance team keeps its eyes on the patients it hopes to serve; the millions of people with insulinrequiring diabetes worldwide who live in constant fear of hypoglycemic events, while simultaneously trying to prevent the long-term consequences of hyperglycemia. Daly recalls hearing a presentation from a man with T1D at a conference who had recently had his first child...
Scan to read the full story or go to healthtransformer.co
startuphealth.com 103

104 StartUp Health Magazine / EXPONENTIAL PROGRESS
Lasa Health Is Using AI to Diagnose Chronic Pelvic Pain
WOMEN'S HEALTH MOONSHOT
CEO and founder Margaret Melville (left) is leveraging her battle with endometriosis — and experience in global health innovation — to build an AI/ML platform that improves care for women with chronic pain. Their solution pushes back against a tide of gender inequity in care and provides relief for a burned out, shrinking physician workforce.
TTen years. 25 doctors. That is how long it took Margaret Melville to get diagnosed with endometriosis.
Sadly, her case is all too common. For patients with chronic pelvic pain conditions, like endometriosis, it takes an average of 10 years to get diagnosed. Chronic pelvic pain is notoriously one of the most complex and frustrating conditions for doctors. The majority of doctors do not feel equipped to care for this patient population, even clinicians specialized in women’s health. One OBGYN with 30 years of experience explains: “I still get squeamish and have a sense of dread when I see chronic pelvic pain on the chart.”
Women’s pain has been habitually and systematically underappreciated in health-
care. For years chronic pain in women has been dismissed as a mental health issue. Women with clearly defined conditions have been told “it’s all in their head.” When it comes to making diagnoses, this has a major negative impact. One study identified 770 diseases where women were diagnosed an average of four years later than men.
Health system challenges are also contributing to the problem. Physician shortages and staff burnout is at an all time high. Four out of five doctors feel like they do not have the time to properly diagnose patients, and women with complex chronic pain conditions are certainly no exception. As one women’s health nurse practitioner explained to Melville: “10 minutes is not enough time to understand 10 years of pain and come up with a sufficient plan.”
So how can a shrinking and overworked physician workforce provide women with more timely access to a needed diagnosis?
Enter Lasa Health and their AI clinical decision support system for precision women’s health.
ORIGIN STORY
Margaret Melville suffered with chronic pelvic pain for 10 years without answers. Ultimately, she visited 25 doctors before finally being diagnosed with endome-
startuphealth.com 105
MEET THE HEALTH TRANSFORMERS
triosis and celiac disease. Endometriosis is a chronic inflammatory disorder that impacts one in 10 women. Celiac disease is an autoimmune disorder where the immune system attacks its own tissues if the person eats gluten.
“I had a decade of despair, living in near constant pain,” says Melville. “After being told by dozens of medical professionals that I was fine, I started questioning my sanity. I finally have answers, but there are millions of women still suffering in silence. I knew I needed to build something that would change the way these patients are diagnosed.”
Melville wasn’t your average patient, however. She had deep experience working at the crossroads of gender, business, and health. As an undergraduate, she started a medical device company, designing affordable medical equipment for developing countries. She worked for USAID’s Global Health Center for Innovation where she had a front row seat to largescale tech-based healthcare solutions.
While pursuing her MBA from INSEAD, Melville decided to be the change that she personally needed in the world and started Lasa Health. She teamed up with technologist Christopher Fortuna who had been working on large language models “before it was cool.” Chris has leveraged machine learning expertise as a data scientist on exciting projects with healthtech unicorn, Owlet Baby Care, and the safety division of T.D. Williamson. Deeply motivated by Melville’s personal journey, Fortuna joined the team full time and has been building the Lasa Health’s
tech stack and ML research division.
“AI/ML is positioned to be the catalyst of a revolution in healthcare. It has the ability to bring incredible value to all parties involved at an accessible pricepoint,” says Melville. “Soon AI assistants will be an essential companion and force multiplier for all providers and physicians. We’re excited to press the cutting edge of this evolution.”
Since the company’s start, Lasa Health has built a large team of clinical advisors and participated in accelerators, including Springboard’s Digital Health Innovation program, Texas Tech University’s Accelerator, Rocky Venture Club’s HyperAccelerator, and National Science Foundation’s i Corps program.

UNDER THE HOOD
Lasa Health’s approach is to start with one of the most common reasons that women visit the doctor: pelvic pain. Approximately 25% of women suffer from chronic pelvic pain and are often left wondering if it is “normal” or if there is an underlying condition. Currently, it takes an average of 10 years from the onset of symptoms to a diagnosis. This is “the decade of despair,” says Melville.
Before an appointment, patients are sent a link to Lasa’s proprietary Pelvic Pain Assessment...

106 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / LASA HEALTH Scan to read the full story or go to healthtransformer.co
Balance Health Uses AI to Reimagine Diabetes Patient Engagement
T1D MOONSHOT
Serial entrepreneur Pete Lomas (right) built on his own struggle with Type 1 diabetes, and his extensive experience in the CGM market, to develop a platform that uses a unique manual ML knowledge management and acquisition technique to replicate expert diabetes clinicians’ decision making and give context-based guidance to patients with T1D.
PPete Lomas is a born entrepreneur. When he was diagnosed with diabetes, instead of slowing down, he kicked into a higher gear. He saw an unmet need in the continuous glucose monitor (CGM) market and built the company Not Just a Patch, which sells custom adhesive patches that protect CGM devices. Through that business he’s served 400,000 patients in 65 countries, giving him incredible exposure to the T1D community.
Business was booming, but something was missing in how Lomas managed his own condition. He realized that despite his insider knowledge of the diabetes

industry, he’d become gradually less engaged with his healthcare providers and his care overall. It dawned on him: if he felt disengaged, how much harder must it be for someone without his experience?
Patient disengagement is a widespread challenge in healthcare and particularly prevalent in chronic diseases like diabetes. Patients move from an initial hyperawareness of their condition and what it’s going to take to live and thrive, and then gradually drift away from physician communication and care plans. This devolving of the healthcare relationship leads to lower health plan adherence and worse outcomes.
We’ve known this to be a problem for
startuphealth.com 107
MEET THE HEALTH TRANSFORMERS
decades, yet most healthcare systems remain notoriously complex, bureaucratic, and functionally divided. Patients often report feeling overwhelmed by the amount of information provided — or lack thereof — and being unsure of how to approach wellness proactively. Treatment methodologies and tools are often one-size-fits all, rather than focusing on the patient’s unique challenges.
Creating a healthcare experience that engages patients, rather than leaving them confused on the sidelines, is critical to improving health because it’s the only thing that will lead to behavior change. And behavior change is often the key to taking control of a chronic condition.
Lomas considered these things and emerged with a question: How can the mundane T1D patient experience — consisting of the same questions and the same predictable approaches — be transformed or complimented to become more engaging, authentic, and personalized?
In the summer of 2022, Lomas began to have clarifying conversations with T1D experts and technologists on this topic. Market research confirmed the challenge he’d identified. What was less clear was the optimal technology to use to solve the problem. That is, until he reached out to Professor Byeong Kang.
Prof. Kang is the co-inventor of a unique alternative machine learning methodology focused on knowledge acquisition and management. This approach differentiates itself from traditional machine learning by actively
emphasizing the acquisition and utilization of domain-specific knowledge. He recruited Prof. Kang to his team and the framework for Balance Health began to take shape.
UNDER THE HOOD
Let’s step into the world of Balance Health and look at an example patient encounter with Bally, the conversational assistant powered by this machine learning approach.
Meet Sarah, a Type 1 diabetes patient who has been struggling with managing her condition. Frustrated with the traditional healthcare system, she turns to Balance Health in search of a more personalized and empowering experience.
Sarah opens the Balance Health app on her smartphone and initiates a conversation with Bally, the AI-powered assistant. “Hey Bally, I’m feeling overwhelmed with my diabetes management. Can you help me?”
Bally, equipped with an extensive knowledge base curated by real human experts, engages in a natural and empathetic conversation with Sarah. It starts by asking a series of insightful questions to understand her specific challenges, recent experiences, and goals.
Based on the data from patient-provider interactions and the expertise fed manually into the AI, Bally recognizes the context of Sarah’s situation and tailors its responses accordingly. It offers guidance, educates her on relevant topics, and provides actionable insights to address her concerns.
108 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / BALANCE HEALTH
For example, Bally might say, “Sarah, I understand managing diabetes can be overwhelming. Have you tried incorporating regular exercise into your routine? Studies have shown that physical activity can help improve blood glucose control. Let’s explore some exercise options that suit your lifestyle and preferences.”
Sarah feels a sense of relief as Bally’s conversational style and personalized recommendations resonate with her. She continues the dialogue, seeking advice on nutrition, medication management, and mental wellbeing.
As the conversation progresses, Bally draws upon its growing knowledge base, enriched by the expertise of endocrinologists, psychologists, diabetes educators, and other healthcare professionals. It seamlessly integrates their collective wisdom, delivering comprehensive guidance to Sarah in a Siri or Alexa style assistant.

Throughout the encounter, Bally provides ongoing support, reminding Sarah to check her blood glucose levels, take medications as prescribed, and offers encouragement to stay motivated on her journey. It also offers resources such as educational articles, videos, and access to support groups for further assistance.
Over time, as Sarah continues to engage with Bally, the AI learns from her experiences, gaining a deeper understanding of her unique needs and preferences. This iterative process allows Balance Health to continuously refine its recommendations and provide increasingly personalized and effective guidance.
Balance Health aspires to be a conver-
sational interface that leverages natural language processing to simulate meaningful conversations between patients and clinicians. While most machine learning models rely on fixed datasets, Balance Health takes a different approach. It harnesses the knowledge of real human experts in various fields by manually feeding their insights into the AI system. This is achieved by carefully listening to patient and provider interactions and incorporating the wisdom gained from those exchanges into the AI’s knowledge base for enhanced, optimized subsequent encounters with the patient.
The goal is to make health tech feel less like a machine and more like a real person, with the added benefit of being able to learn from past conversations. The interface records and saves conversations to this knowledge base, allowing the technology to adapt and improve over time evolving into a buddy system type app that uses that knowledge to uniquely support them.
Balance Health is currently working through the iteration of their MVP, adapting to the swift changes in ai adding capabilities such as the Bally app and evolving their knowledge capture capabilities to be sourced through conversations live as they happen rather than the current manual input...
Scan to read the full story or go to healthtransformer.co

startuphealth.com 109




110 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS
Enhance-d Delivers Digital Diabetes Management Tools Previously Reserved for Elite Athletes
This European co-founder team helps people with diabetes make daily health decisions with less stress through their integrated and user-friendly data platform.
EEvery day we wake up and a making decisions. A lot of them. A recent study out of Cornell estimates that we make more than 200 decisions each day on food alone. In a survey undertaken by Noom, responders indicated an average of three hours a day deciding what to wear, what to watch, what to eat, and what time to go to bed. Even once a decision was made, 87% of people admitted to changing their mind or not acting on the decision. Decision fatigue is a common complaint; when you’ve made so many choices already in a day your ability to make good decisions gets impaired.
If the burden of decisions is high for the average person, just imagine the number of decisions a person living with diabetes needs to make in their day. Those decisions about food aren’t just about preference but about what the potential impact will be
on their blood glucose. When you add in extra things like whether or not to exercise and what kind and for how long becomes a complicated calculus way beyond the typical questions of ‘do I feel like it?’ or ‘do I have time?’’ It’s a continuous tightwire act, a threading of the needle, to ensure that glucose numbers stay balanced and to avoid both hypo- and hyperglycemia.
To maintain this delicate balance, people with diabetes rely on things like continuous glucose monitors (CGM) and blood glucose meters and strips. They receive data about their blood sugar, but that data arrives independently of other health metrics like activity level, amount and quality of sleep, stress levels, and even information about what nutrition choices resulted in those sugar levels. It’s little wonder that cases of anxiety, stress, and diabetes burnout — feeling overwhelmed, exhausted and frustrated by the management of the condition — are widespread in the community. It’s decision fatigue on a grand scale, with serious consequences if you go on autopilot or stop paying attention to all the details.
ORIGIN STORY
Fede Fontana, PhD, and Sam Scott, PhD, first encountered the daily weight of
startuphealth.com 111
T1D MOONSHOT
decision making a person with diabetes carries under unusual circumstances. Fontana, a physiologist and data scientist, and Scott, a physiologist and researcher, met while working for Team Novo Nordisk, the world’s first all-diabetes professional cycling team. As Fontana worked with the athletes, first as a data interpreter and then as the head of performance, he quickly developed an enormous respect not just for them, but for anyone living with diabetes.
“It is a complex life and a complex job to manage glucose if you are living with Type 1 or Type 2 diabetes. It’s self management for the majority of the time.”
In their different roles supporting people living with Type 1 diabetes, Fontana and Scott realized that diabetes-related data was being presented in an overlycomplicated way and the different data streams rarely intersected. A diabetes specialist would look at CGM numbers and a different specialist would focus on heart rate, physical activity, sleep, and nutrition. There was no platform to bring the data together in one place to make sense of it all, or as Scott puts it, “there was no insightful conversation between the data.” This meant that the information wasn’t being leveraged to its full potential — both from the people living with diabetes and from their doctors.
“It can be just as hard for someone with Type 1 diabetes to manage glucose levels if they are exercising for 30 minutes three times a week as a cyclist with diabetes who spends three hours a day on a bike.”
The idea of creating a tool that they felt was missing had to be placed on the back-
burner for a number of years because the pair were busy on other projects. But that initial idea kept simmering in their minds. Then, through chance, after fruitful conversations with the Diabetes Center Bern (DCB), a foundation that supports startups in the diabetes space with expertise and financial support, they decided it was time to take the leap and strike out on their own.
By combining workflow and data streams with all available health metrics and bringing the data into the same hub and creating visuals for it, they could create better blood sugar outcomes for those that initially tested their platform and anticipate blood sugar changes before they arose. And they quickly realized that what they were doing had implications for a much broader audience.
To expand on the potential, they rounded out their own expertise in the physiology and science side by bringing on two additional founding team members: Fabio Saviozzi to lead the commercial side of the business as CCO and data scientist Felipe Mattioni Maturana, PhD, as CTO. All four co-founders knew or hed worked with each other before creating their team, so they hit the ground running with a cohesive working dynamics.
As Maturana describes his willingness to jump into the venture, “I knew Fede for about eight years. When he reached out to me with the idea, I thought, that’s a problem worth solving. It’s a big challenge, every day, but at the end of the day, we like what we do and working together is a joy.”
In October of 2022, they all quit their jobs and set out to create the tool they
112 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / ENHANCE-D
imagined that relieves the burden of daily decision making for anyone living with diabetes.
UNDER THE HOOD
Enhance-d is a digital diabetes management platform that integrates, analyzes, and presents data and decisions in a simple, user-friendly, and actionable manner to simplify decision making. It brings together all the available health data points to a single location for its user and provides personalized insights from the data, so that a person can make informed choices for their day. Enhance-d helps shoulder the burden of decision-making, relieving stress and confusion for a person living with diabetes, and supporting them in making choices that improve their health and overall wellbeing.
“We often hear from people living with diabetes that they wish they could live a normal life. ‘I want to dream as a person without diabetes. I want to go through emotions without always stressing and worrying about what I am going to do tonight as I approach my dinner.’ We want Enhance-d to provide a source of security for them so that they can know they’re making the right decisions,” Fontana emphasizes.
To that end, the platform is designed to learn about its users routines and habits, using AI and machine learning to predict what sort of glucose scenarios its users will face in a day. Someone can check the app almost like they check the weather, getting a sense of their diabetes forecast for the day and making plans accordingly. Enhance-d
also plans to speed up and improve decisions around diabetes management by establishing themselves as the first shared platform for patients and doctors, building common knowledge and insights to ensure the best possible approach to care.
The team is rolling out a beta version of its platform this spring and plans to upgrade to a full mobile app next year. They will start with a low-cost subscription model and then open up different options for reimbursement as they go along. With a multinational, multilingual team headquartered in Switzerland, Enhance-d’s initial market is DACH countries, with their eye on quick expansion across Europe and then on to the US.
“The business model changes from country to country, but regardless of location, the doctors and the patients have the same needs. We’re building a solution that focuses on the patient first, and then figuring out the business model to get it to them from there,” explains Saviozzi.
FINAL WORD
With its dynamic co-founding team and first-to-market comprehensive diabetes management platform, Enhance-d is poised to deliver clarity, ease, and confidence to the millions of people living with the condition, supporting informed decision making that leads to better physical and mental health.
Learn more & connect with founders at startuphealth.com/portfolio
startuphealth.com 113
Iryss Uses Predictive Analytics to Help Patients Manage the High Cost of Chronic Illness

COST TO ZERO MOONSHOT
WBy providing financial insights to “save before, pay now” for chronic illness sufferers, Iryss® hopes to eliminate the financial stress currently facing 133 million Americans. When someone is diagnosed with a chronic illness or disease, they often go through three stages of understanding. First is purely physical as the patient seeks to find out why they aren’t feeling well. The second phase is the emotional toll brought on by the diagnosis and what it now means to deal with a long-term, sometimes lifethreatening ailment. The third stage hits a few months later, after the patient has been presented with this new normal. That’s when the first bill for the diagnosis arrives and with it the financial reality of this journey.
The cost of long-term treatment, diagnostic services, and overall health management for people with chronic illness and disease is five times that of “preventative care” each year, and there are 133 million people dealing with life-changing ailments
throughout the US. General medical bills are hard enough to bear, and are a leading cause of bankruptcy in America, but disease management is much worse. Forty percent of cancer sufferers alone file for bankruptcy within four years of their initial diagnosis.
To date, planning for these kinds of crisis events has been nearly impossible. Financial planners don’t typically take health needs into consideration — or even how to consider them — when setting up
114 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS
retirement or savings plans for their clients. That’s in part because until recently, medical information was inaccessible and hard to analyze.
How can patients suffering from a chronic disease avoid going bankrupt so they can thrive mentally, physically, and financially? What resources are out there to help average people — who don’t have large amounts of disposable cash on hand for emergencies — be more financially prepared for long-term healthcare? What can be done to alleviate the economic burden in order for families to turn their focus to what matters most: the emotional and physical care and support of their stricken loved one?
Iryss has answers.
ORIGIN STORY
In 2008, buy-side healthcare equity analyst Jeff McCormack was sitting in his living room, holding his one-month-old son, when he felt numbness in his left leg. The master swimmer and triathlete was taken aback when it got bad enough that he couldn’t stand up. He saw his doctor and the diagnosis shocked him: multiple sclerosis. Suddenly, his whole world changed. He was first hit physically, then had to deal with the emotional strain. But, two months later, he received his first medical bill. He was stunned.
Jeff was a professional at the top of his career, familiar with both the medical and financial sectors, and yet nothing prepared him for the exorbitant costs associated with managing his chronic illness. While he was fortunate enough to be able to pay
the bills, he couldn’t help but think: What about people who couldn’t? What would he do, he wondered, if he were in the position to have to literally choose between feeding his family or getting his treatment? How would he handle that?
The research began and Jeff discovered some nasty truths in the chronic illness world. Medical issues are two-thirds of all bankruptcies in the US, making them the number one reason to file. The chronically ill spend five times more per year than healthy individuals — approximately $6,000. Healthcare is the number three line item for budgeting for the chronically ill but number 10 for healthy individuals. (For the chronically ill, first is lodging, then food, and then medical bills.) CNBC reports that 40% of people diagnosed with cancer are bankrupt within four years of diagnosis. In general, $500 billion of healthcare spending was on the shoulders of consumers last year (2022), growing at 9% per year and will be $800 billion in five years.
Jeff was astounded by these facts and wanted to find a way to help others not drown in debt simply because they were managing a chronic illness. First, he went to work for two AI companies to learn technology and how to scale businesses. Then he saw an opportunity to help others by using his financial expertise and became a financial advisor.
Jeff’s business grew and he was helping 75 families manage their finances, but it wasn’t scalable and making the impact he envisioned. So he made a leap of faith. His kids were now old enough that he wanted
startuphealth.com 115
them to see their father doing something that made a difference in people’s lives, something he recalled watching his own dad pursue when he was their age.
He combined what he learned with the AI companies and his experience in healthcare and finance to build something new. The vision was to create a virtual platform focused specifically on providing the tools and resources needed for chronically ill patients and their families to find financial relief through successful medical cost management.
Iryss was born during 2022, and Jeff and his team began the long road to building a program to support financial wellness for the chronically ill.
UNDER THE HOOD
Iryss is a SaaS platform available to chronically ill patients and their families. It’s split into two main components: a payment intelligence solution and a databased future healthcare cost estimator.

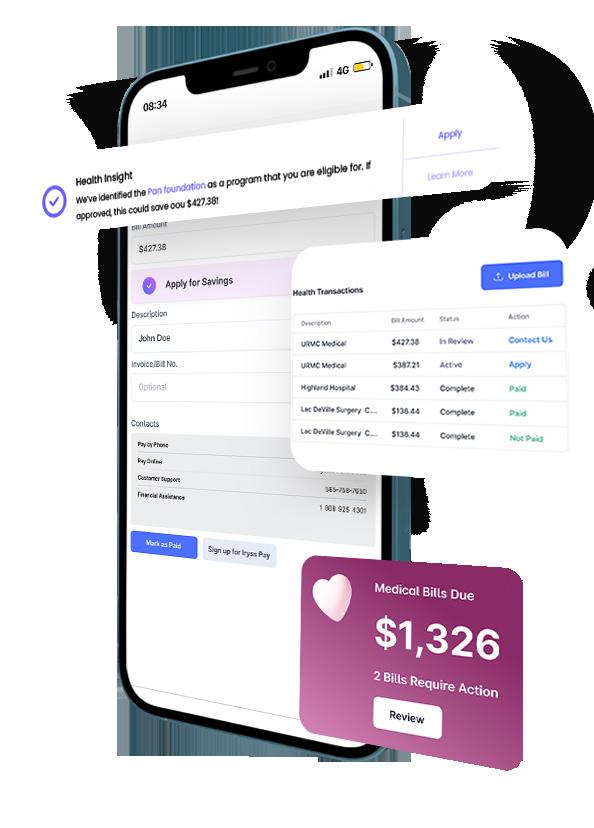
The first component analyzes bills and identifies opportunities to help chronically ill patients reduce them. Resources are provided to support lowering healthcare costs, including financial assistance programs and information on where to find more affordable diagnostic services, such as less expensive MRIs or blood draws, and pharmaceutical discounts and co-pays — all of which are options many chronically ill patients are unaware are available to them. Additionally, Iryss reviews the patient’s capacity to pay and recommends a payment strategy that’s in the patient’s financial best-interest.
The second component helps chronically ill patients plan for future healthcare costs utilizing data analytics. Iryss comes at this from a modeling perspective on a disease-specific basis. The platform takes the user’s medical data, pairs it with their financial information, and identifies which patients are at risk of not being able to pay their bill and will require assistance in managing the cost of their disease journey. This makes it possible for Iryss to work with users and their families to begin saving in preparation for what is to come. He calls it “save before, pay now”...
Scan to read the full story or go to healthtransformer.co

116 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / IRYSS
GO-Pen Is Designing Safe, Reusable Insulin Pens That Are Accessible for All
T1D MOONSHOT
Ole Nielsen, PhD, and Michael Hansen have built on their work at Novo Nordisk to create a new kind of insulin pen, one that does away with the need for syringe injections and makes diabetes care cheaper, safer, and even better for the environment.
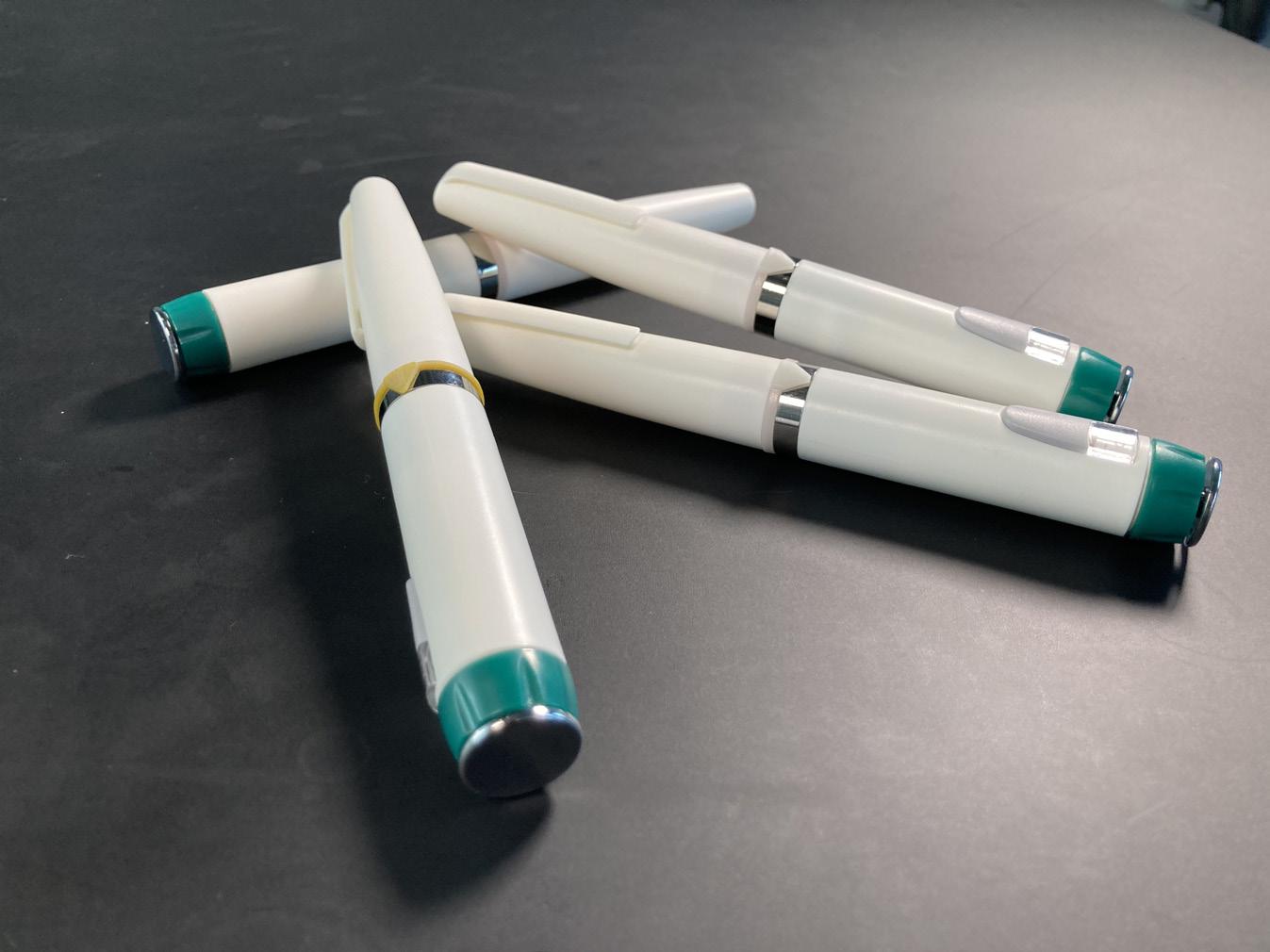
PPak Waslo lives in a kampung — or shanty town — outside the city of Jakarta
in Indonesia. At the age of 80, despite suffering from vision loss, he has to take a bus every day to a health center to get an insulin injection to manage his diabetes. He buys his insulin by the shot, but in the end, spends just as much on transportation as he does on his dose. His days pass in the same routine: bus, injection, bus ride home. It’s not how he wants to spend his remaining days, but at least it gives him more days to live.
Pak is not alone. In communities across the world, people dependent on insulin injections come up against inefficient sys-
startuphealth.com 117
tems of medicine delivery that take up resources, energy, and the patients’ precious time.
To the west, in Denmark, Ole Kjerkegaard Nielsen, PhD, encountered this global challenge in his role as the global director of Novo Nordisk’s TBL Value & Impact division. He wondered if there might be a cost-effective way to give people like Pak the ability to dose themselves with insulin at home. And he knew just the right person to answer that question: Michael Hansen.
Hansen was a close friend of Nielsen’s and colleague at Novo Nordisk. More importantly for the question at hand, he’d co-authored 29 insulin injection device patents and was one of the lead designers of insulin pens for Novo Nordisk.
When Nielsen approached him with a question about a better, cheaper at-home insulin pen, Hansen quickly conceived of a design that converts insulin in a syringe to a reservoir on a pen, allowing for affordable, accurate at-home dosing from a reusable device. An insulin pen like this would replace the use of syringes for injection, resulting in fewer skipped doses, greater dose accuracy, better quality of life, and a huge cost-savings.
“It was elegantly simple,” says Nielsen. “Michael knew how to do it and I knew there were a lot of people who needed it.”
WHAT THEY BUILT
There are three main ways of injecting insulin: dosing with a syringe, using an insulin pen that is pre-filled or comes with cartridges, and insulin pumps.
Approximately 46 million people use traditional insulin pens, two million use pumps, and 11 million people use syringe or vial injections. The GO-Pen bridges the gap between syringe injection and the more expensive insulin pens by converting the syringe dose to a reservoir on an affordable, reusable pen. The GO-Pen carries a three-day dose, is refillable, lasts up to three years, and provides more accurate dosing than a syringe.
That dosing accuracy is incredibly important with insulin. Too little, too much, or skipped or mistimed doses result in serious hypo- and hyperglycemia or even diabetic ketoacidosis — a serious complication that indicates your body is not breaking down sugars. To ensure proper dosing, the GO-Pen measures insulin with each click as you turn the dosing dial representing one unit. They’ve demonstrated its precision over time, so that even three years later, one click still equals one unit. Compare that to dosing by syringe which introduces human error with every injection.
“Basically no one should be using syringes,” Nielsen emphasizes. “Insulin injection by syringe is more complicated and leads to poorer health outcomes, not to mention more waste. We want to take that group of 11 million people today using syringes and provide them with the same health equity opportunities as everybody else.”
The simplicity and usefulness of the design begs the question of why did it take a startup to come up with it? Why didn’t someone else in the diabetes space jump
118 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / GO-PEN
at the chance? In some ways, the answer turns out to be a failure in the market: an annual €50M EBITDA opportunity simply isn’t enough of an incentive to address the problems of syringe injection for a company operating at large scale, says Nielsen. But for a startup, it’s well worth it, especially considering the other applications of an affordable, accurate injection pen.
For instance, GO-Pen could work for a variety of treatments or conditions that require in-home precision dosing, such as IVF and other hormone therapies, obesity, chronic inflammatory conditions like rheumatoid arthritis and Crohn’s disease, among others.
“We have established IP for the product, and once we get our product approved for diabetes and then for other in-home injectables, there are a number of larger companies looking to collaborate with us.”

WHERE THEY ARE IN THE PROCESS
Hansen and Nielsen launched GO-Pen in 2019 and received a patent for the device in Denmark in 2020. They hope to receive FDA approval around the end of 2023, which would allow them to launch in the US as soon as spring of 2024. In the meantime, GO-Pen is building their manufacturing capabilities and the structures necessary to get the product to people quickly when it is approved.
To that end, GO-Pen is raising money necessary to ensure production capacity. They’ve already raised €5.5M, €2.5M of which coming from an undiluted grant from the European Innovation Council
(EIC). The EIC exists to “identify, develop, and scale up breakthrough technologies and game-changing innovations.” It’s a grueling application process and only half a percent (.5%) of companies that apply get it. Besides the €2.5, the EIC will provide a €4M matching investment if the company obtains an investor of that size.
“We are in a strong position,” says Nielsen. “We are considering the best way to launch and setting ourselves up to deliver.”
While they prepare for launch, their design continues to rack up awards, building anticipation within the diabetes community. In 2022, they won top prize for diabetes devices from the Diabetes Center Berne, from a jury of industry experts and people with diabetes. And just this June 2023, they won the American Diabetes Association first ever Innovation Challenge at their annual convention in San Diego.
As gratifying as these wins are, for Nielsen it is all about the people their product will impact. He thinks of Pak taking the bus daily in Jakarta for his dose, and can’t wait to get the device in his hands. It’s a labor of love, resulting from years studying impact and sustainability across the globe. It’s also a testament to the long friendship between him and Hansen and the support of his family...
Scan to read the full story or go to healthtransformer.co

startuphealth.com 119

120 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS
HealthBook+ Empowers Patients with Personalized Health Data and Predictive Analytics
ACCESS TO CARE MOONSHOT
This “digital-first early identification and guidance platform” seeks to give patients greater ownership of their health and wellbeing. By combining comprehensive data consolidation with AI-driven predictive analytics, this startup helps patients better identify potential conditions and then suggests appropriate healthcare next steps.
WWhile electronic health records (EHR) are becoming more the norm in the United States, medical information for an individual is still scattered across numerous systems. This results in healthcare providers having access to an inaccurate and incomplete picture of a patient’s state of health when they seek treatment. Many care components are not taken into consideration, leading to unnecessary emergency room or urgent care visits, higher costs, and even reticence to seek medical care — 50% of consumers avoid it because of how complex healthcare has become.
In the US alone, one in 20 people are misdiagnosed due to incomplete data, leading to major morbidity and mortal-
ity. Unnecessary medical visits are costing patients upwards of $750 billion annually with employers losing approximately $225 billion due to absenteeism from physical and mental maladies.
While niche healthcare platforms have been created to great effect — such as those for musculoskeletal, diabetes, cancer, etc. — there has been no comprehensive digital system that presents individuals with a way to manage their entire health and wellness journey. That journey begins with understanding simple preventative measures, addressing acute needs, and management of chronic disease. Without a comprehensive record of an individual’s health history and status, care approaches can be mismanaged and conditions are either overlooked or overtreated.
HealthBook+ is working to change that paradigm.
ORIGIN STORY
It started in Greece — 35-year shipping veteran Stathis Topouzoglou had always been concerned with the health of his company’s seafarers. Providing medical care in the middle of the sea has always been a challenge. The process is difficult and over the years has resulted in misdiagnosis, bad health outcomes, and very high costs.
startuphealth.com 121
Obviously, timely remote care could help. Virtual health visits from the ship could avoid disastrous health situations in case of a serious emergency and also keep non-emergent situations from escalating to a costly diversion or transport. About 10 years ago, his determination to optimize the process drove Stathis to create a group of healthcare providers led by a very experienced physician. The team would perform pre-board history and physicals and keep information in a manual way for each seafarer. They provided remote healthcare before telemedicine was really on the scene more broadly. And they soon noticed that outcomes greatly improved. The key difference was being able to act on detailed knowledge of the patient’s medical history.
Stathis discussed the amazing results with his friend Panos Sechopoulos, MD, and they decided to build a digital health record owned by the patient. Dr. Sechopoulos is a practicing gastroenterologist who focuses on providing individualized recommendations. In his practice he integrates clinical gastroenterology with functional medicine and genetics. Review of all past records and obtaining detailed history of the patient’s health concerns are essential components he uses in providing personalized advice.
The two men believed digitizing entire health records and making them accessible on people’s phones, tablets, or computers would resolve the problem. For Stathis, this meant when someone got sick on ship, their detailed health record was there for the healthcare provider to
view regardless of location, leading to better quality care and less money lost. For Dr. Sechopoulos, it meant better health outcomes for his patients.
The vision was to empower the patients to become owners of their health information and provide some basic features such as a symptom checker.

In 2018 they created a rough digital health record with some basic AI features. Stathis suggested the name HealthBook and the journey started.
They reached out to Chris Turner, who had years of success working with health companies. Instrumental in taking Healthgrades from an early startup to a 900 employee/$250 million company in just eight years and transforming WhatsApp in Healthcare from $800K in revenue to more than $5 million in 18 months by leading its commercial teams, Chris was working with a company in Poland that had an AI symptom tracker that Stathis and Dr. Sechopoulos thought would be good to add on top of the initial HealthBook.
As the three got to work, Chris pointed out that many companies attempted building EHR capability with a personalized health record but failed, and having someone own their health was more powerful if they had all the data...
122 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / HEALTHBOOK+
healthtransformer.co
Scan to read the full story or go to
Undermyfork Uses an Instagram-Like Interface to Unlock the Potential of Continuous Glucose Monitoring for People with Diabetes

Co-founders Mike Ushakov, Eugene Molodkin, and Nikita Shulaev are helping ease the burden of diabetes by combining meal tracking and CGM data in an elegantly-designed, clinically-validated app experience.
WWhen a person has Type 1 diabetes (T1D), they live in a cycle of constant healthcare decision making. They’re constantly dealing with insulin while taking into account current blood glucose levels and recent and upcoming physical activity. And every few hours of their day, they have to make important decisions about what to eat and how much insulin to use with their meals.
Thanks to technology like continuous glucose monitors (CGMs), it’s now easier than ever for people with diabetes to keep track of their blood sugar levels throughout the day. CGM devices have a key metric to help patients estimate the quality of their diabetes management: time in
startuphealth.com 123
T1D MOONSHOT
MEET THE HEALTH TRANSFORMERS
range, the amount of time in a day they spent in their target blood glucose range. Included in ADA’s Standards of Care in 2019, time in range (TIR) is the second most important metric of diabetes wellbeing after A1C.
Yet, even with all the advantages that CGM provides, it is still incredibly difficult for its users to accurately get a clear picture of how insulin doses, blood glucose, and activity correlate with the food they consumed. The Undermyfork team decided to focus their efforts on exactly this problem.
“We asked ourselves: Can we unlock the full potential of CGM devices?” says Mike Ushakov, CEO of Undermyfork. “Can we help CGM users not only watch their blood glucose graph change but actually make lifestyle choices based on this graph?”
ORIGIN STORY
Mike Ushakov, Eugene Molodkin, and Nikita Shulaev are unlikely health tech founders. Serial entrepreneurs, they previously worked together on a browser extension company called Metabar that helped shoppers save money and find online deals. They sold their first company to Yandex, a European tech giant. From there, they were one of the world’s first experimenters in the currently overheated chatbot space, developing Forksy, a natural language engine and an AI-powered nutritionist that helps people log and track their food in a conversational form. The user could text their AI with a message like, “I had a burger and Coke, how
many calories did I just eat?” and the AI persona would reply with a calorie estimate and also provide some basic nutrition advice.
As a team with a consumer tech background, Ushakov, Molodkin, and Shulaev were always driven by the goal of product simplicity: how to design tools that could be adopted easily by millions (or, as they say, even hundreds of millions) of users.
“We call it a ‘grandmother’s test’,” says Ushakov. “The product is good enough only when your 80-year-old grandmother can start using it in several minutes. There’s usually a huge gap between an ordinary user of technology and an ordinary developer of technology, a gap in their ability to understand the tech products from the first glance. In a lot of situations normal people tend not to grasp product details that might just seem so obvious and straightforward for those who develop these products. That gap creates an unnecessary and an unjustifiable burden on those who are supposed to use the technology every day, and the gap should be crossed before the product reaches the mass market.”
As they worked on their AI nutrition coaching platform, they quickly realized that there is one particular group of their users who really needs and utilizes food logging on a daily basis: people with diabetes. Digging deeper, they saw a striking disconnect between their meal log and the ability to easily evaluate the effect of those meals on their blood glucose levels. Doing further research, they discovered — to their surprise — that there were two
124 StartUp Health Magazine / EXPONENTIAL PROGRESS MEET THE HEALTH TRANSFORMERS / UNDERMYFORK
dominant ways of informing the diabetes patient about their wellbeing. The typical software either just showed the user several diabetes management parameters, without further explanation and actionable advice on how to deal with these data. Or, on the other side of the spectrum, the products looked like they were designed for NASA’s mission control room. There seemed to be nothing in the middle. In short, they saw nothing on the market for T1D that passed their grandmother test.
“Imagine, when four years ago we checked 100+ different diabetes apps, either made by well respected manufacturers, or by independent developers, we only saw one or two apps overall that were allowing the user to do a supposed-to-besimple operation: scroll the blood glucose graph back to the data from a week or month ago,” says Molodkin, CTO of Undermyfork.
They set out to change the status quo and quickly recognized the common time, labor, and accuracy challenges of food logging. How could they make it elegantly simple for people to correlate what they ate to their CGM data? In this case, a picture turned out to be truly worth a thousand words. They realized that instead of manually entering data for each bite of food — a laborious and confusing process — people could upload photos of their meals, tag the food on the plate, and then this meal photo could be classified by its impact on blood glucose and whether it achieved time in range.
By creating a personal library of meals for each individual user, with those meals
color coded by their impact on blood sugar, someone could understand at a glance the impact of their choices — which meals brought them out of range and which meals kept them in it.
UNDER THE HOOD
Undermyfork is a diabetes management app that automatically combines glucose data from CGMs or BGMs with meal photos and calculates postprandial (after a meal) time in range (TIR). People with diabetes can compare their glycemic response to various meals and situations to quickly make informed decisions about what to eat. The app also allows endocrinologists and diabetes educators access to the same data, providing both a big picture overview — highlighting, for example, hypoglycemic events — and the ability to zoom into the data and examine meal details, insulin data, and glucose measurements.

Undermyfork is an official digital health partner of Dexcom, which means they’re able to seamlessly integrate data from the Dexcom API. By partnering with the leading CGM manufacturer in the world, they have a strategic advantage as the mass adoption of CGMs for diabetes care continues...

startuphealth.com 125
Scan to read the full story or go to healthtransformer.co
Rezq Bio’s Dendritic Cell Therapy Offers Hope in the Fight Against Autoimmune Disorders

Arjun Hattiangadi (right), Dr. David Finegold, and their research team have shown promising early results using innovative cell therapy to stop autoimmune attacks at the source. Their growing body of work offers new possibilities for the treatment of Type 1 diabetes and other autoimmune conditions.
AA house divided against itself cannot stand.
How do you cure the body when it is the body itself that is the problem? That is the complicated challenge immunologists and geneticists have to solve when it comes to autoimmune disease. Whether it’s Type 1 diabetes, IBD, multiple sclerosis, or any of a host of other conditions, the body’s immune cells receive false signals to attack its own healthy tissue, instead of protecting against invading organisms and infectious agents.
Autoimmune disorders are on the rise, with an estimated growth of between 3–9% each year. For Type 1 diabetes in
the United States, the numbers are even more startling — the CDC released a report indicating an almost 30% increase in Type 1 diabetes (T1D) in the US in just the past two years, with the highest rate of growth in the youth population. Environmental factors such as diet, exposure to certain chemicals and substances, and smoking are considered to blame for the rising numbers, although researchers and scientists are still trying to unravel the causes.
Whatever the origin, once the immune cells begin to attack healthy tissue, it becomes a self-perpetuating cycle. Take Type 1 diabetes, for example: something
126 StartUp Health Magazine / EXPONENTIAL PROGRESS
T1D MOONSHOT
MEET THE HEALTH TRANSFORMERS
triggers the body’s T-cells to attack the insulin-producing beta cells in the pancreas which then trains other cells in the body, specifically young dendritic cells, to continue this attack. Dendritic cells act as the captain of the immune systems — they tell the white blood cells what to fight. When immature dendritic cells are exposed to an attack on insulin production, they then mature into captains that tell the immune system to continue the assault on insulin production.
The question is, how do you keep the switch from flipping in these cells that tell them to attack? Or, once those switches have been activated, how do you reprogram them and turn them off?
ORIGIN STORY
Arjun Hattiangadi is used to explaining complicated scientific enterprises. For several years, he served as the director of healthcare portfolio development and management at UPMC (University of Pittsburgh Medical Center), evaluating and overseeing investments in emerging medical technologies and interventions. An entrepreneur and investor with both biotech and software experience, Hattiangadi has seen the gamut when it comes to new ventures. He has a good read on the shortcomings and adversities many well-intentioned efforts face and is accordingly discerning.
But when colleague David Finegold, MD, pediatrician and professor of genetics at the University of Pittsburgh, approached him with a life-changing therapy for Type 1 diabetics, it was hard not
to get involved. Dr. Finegold had overseen the successful phase 1A trial with his collaborators Drs. Massimo Trucco and Nick Giannoukakis, Head and Lead Researcher of the Institute of Cellular Genetics at Allegheny General respectively. The trio’s decades of pioneering work in the study of tolerogenic dendritic cell therapy for autoimmunity, put them further along than anyone else in answering the question of how to retrain those dendritic “captain” cells so they no longer signaled the T-cell troops to attack.
“This is what made it exciting; brilliant people with novel science backed by very promising trial results.”
The preclinical and phase 1A testing results not only established the safety of the procedure (the goal for such trials), but even saw some promising signals. Mice with diabetes involved in preclinical trials saw their diabetes reversed and needed no insulin. Even more striking, in the phase 1A safety trial, some patients who started with zero insulin production began secreting C peptide (a marker of insulin production) and one persistently for the year-long duration of the trial; all from just one course of treatment. This was significant as the patients in the safety trial were long standing Type 1 diabetes patients, and no insulin production was even hoped for.
“We hadn’t seen that elsewhere,” says Hattiangadi. “Everything about the study was incredibly positive, especially when compared to other therapies. We saw insulin production and minimal side effects.”
startuphealth.com 127
UNDER THE HOOD
Rezq Bio’s lead asset is a phase 1B/2A ready dendritic cell therapy intervention for the treatment of early-onset T1D. Built on the work of Drs. Trucco, Giannoukakis, and Finegold, Rezq Bio looks to arrest or reverse T1D and other localized autoimmune conditions, by stopping required signals in dendritic cells that tell the immune system to attack healthy parts of the body. In turning off this autoimmune attack, it is also hoped the treatment could be used for T1D prevention as well as combined with cellreplacement therapies for those with long established diabetes.
Here’s how it works: first the patient’s own dendritic cells are removed through a process called leukapheresis that extracts white blood cells while returning blood and plasma to the patient. Then these dendritic cells are modified to become tolerogenic, meaning they no longer promote T-cells to attack insulin producing cells. Then, these modified dendritic cells are injected near the pancreas, where they have a localized effect and avoid systemic complications.
For Dr. Finegold, the project offers his patients something he’s wanted to give them his entire career: hope. There are no approved therapies that exist that can reverse or stop the progression of T1D. Even when managed with insulin, complications like heart disease, kidney issues, and vascular problems are common. Dendritic cell therapy represents a chance to stop T-cells from attacking insulin production for good.
Although the founders are starting with T1D, the intervention could work with other localized autoimmune disorders and they’ve already completed strong preclinical studies for colitis. As they build investment partnerships, they plan to attack their laundry list of other conditions. For now, the priority is determining the efficacy of their intervention for patients. To that end, Rezq Bio is set up for rapid trial initiation, with their phase 1B/2A trial design previously approved by the FDA with the University of Pittsburgh as their manufacturing partner.
“It’s not a sprint,” Hattiangadi emphasizes. “It’s never as quick or easy as one would like, but we have the science, results, and growing team to get us where we need to go.”
OUR THOUGHTS
Rezq Bio has the research bonafides and the dedication to their mission to see their revolutionary intervention through to the end. Their early clinical results are incredibly promising and they have a time and tech advantage over their competition. They also have a clear idea of how to build out their team to walk the road ahead, recently rounding out their team of scientists and academic advisors with people experienced navigating the pharmaceutical industry and the FDA. We’re proud to support this work that has the chance to reverse or stop T1D in its tracks.
Learn more & connect with founders at startuphealth.com/portfolio
128 StartUp Health Magazine / EXPONENTIAL PROGRESS
MEET THE HEALTH TRANSFORMERS / REZQ BIO
MoodMD Analyzes Biomarkers to Address Mood Disorders at the Source
MENTAL HEALTH & HAPPINESS MOONSHOT
While helping fellow vets suffering with PTSD, founder Kevin Rogers (right) discovered critical flaws in how we treat mental health problems. Years of research led to the discovery of a set of biological contributors to mood issues prompting Rogers to create a platform that marries medical and psychological factors into one treatment paradigm.

IIn a recent poll conducted by CNN and Kaiser Health, nine out of 10 people think we are in the midst of a mental health crisis in America. More than one in five adults describe their own mental state as only “fair,” at best. The World Health Organization reports that the global prevalence of anxiety and depression increased by 25% in the first year of the COVID-19 pandemic, and suicide is now a top ten leading cause of death in every developed country.
Mood disorders — the category of mental health dysfunctions that include chronic stress, anxiety, including the most
devastating and accelerating form of anxiety, post-traumatic stress disorder (PTSD), and depression — account for a clear majority of mental health diagnoses in the United States. These disorders are comprised of a combination of body, brain, and mind anomalies, but today’s treatment, now decades old, involves only drug therapy and psychotherapy, dubbed “treatment as usual.”
The unfortunate reality in the 21st century is that treatment as usual isn’t working well. The success rate for drug therapy is about one in three, primarily because MDs are “guessing” at which prescription to write, in the absence of the mood chemistry testing that MoodMD conducts. And psychotherapy interventions vary widely
startuphealth.com 129
MEET THE HEALTH TRANSFORMERS
between therapists who most often use outdated modalities that lag far behind new scientific data and the new levels of disorder severity now a new normal part of the 21st century mental health landscape. Thus, the success rate for therapy, the other half of treatment as usual, is only one out of two — like flipping of a coin — where half the patients are often labeled as “treatment resistant” and sidelined or sent back to their GP for a replacement medication that is still a “guess.”
This two-factor, treatment-as-usual approach doesn’t account for the myriad of other factors that impact mood — things like neuro-hormonal brain chemistry including DNA analysis; lifestyle factors like sleep, diet, exercise; and the brain’s protected pockets of neural networks — requiring “depth psychology” to access to the subconscious where traumas like PTSD / PTSS find refuge or AI to process this new volume of data into precise treatment recommendations.
ORIGIN STORY
For years Kevin Rogers witnessed, as a psychotherapist, that treatment as usual was failing more than it was helping. As a young man, he served in military intelligence in “forward areas” and witnessed the frustrating shortcomings of PTSD treatment where poor results often lead to suicide of his comrades in arms. This experience caused him to pursue a bachelor’s degree in psychology that created his desire to devote his life addressing mood disorders, particularly in the veteran community. A lifelong learner, Rogers spent
years adding three graduate degrees to his educational collection following the bachelors, delving deep into every aspect of the psychological sciences. His conclusion: we needed to expand patient assessment and treatment to include a six-factor assessment set vs. the existing two-factor set that only partially assessed mood disorders.
“After all the thousands of hours spent as a psychotherapist, and years of study devoted to psychology, it was clear we weren’t doing enough to improve treatment success rates. A new, expanded paradigm needed to be architected,” explains Rogers.
Once he conceptualized the model, Rogers embarked on four years of R&D, guided by his mentor at Harvard. Prior to this, Rogers had founded and sold a unicorn-status business, affording him the time and capital to devote full attention to the mood disorder project. His obsession to assess everything and anything that could impact mood demanded a way to quickly aggregate and assess all of the relevant data points never conducted before. He worked with developer and engineer Brian Vanyo to create a sophisticated data collection and an AI model to process and distill the captured data into precision treatment recommendations. Rebecca Gleason developed the user interface and user experience model to guide patients easily through gathering the disparate mass of data and a graphical method to present recommendation results to all MoodMD patients.
Rogers asserted that the resulting site showed that “the whole really is greater than the sum of its parts. There are people
130 StartUp Health Magazine / EXPONENTIAL PROGRESS
THE HEALTH
/ MOODMD
MEET
TRANSFORMERS
who know certain aspects of the mood disorder spectrum, but no one had pieced together an entire, all-factors assessment and treatment model until MoodMD took shape.”

UNDER THE HOOD
MoodMD is a platform that delivers precision treatment for mood disorders through a comprehensive mood assessment and treatment plan that closely examines all relevant factors that can impact mood issues. The platform works as a one stop shop for patients offering a four-tiered subscription plan that provides everything from an initial, AI-driven, CBT stepwise program, to weekly or daily online access to behavioral health coaching and psychotherapists, to the ultimate combination of a full neurohormonal and genetics testing, coupled to coaching and therapy access — not offered by any other mental health treatment provider.
From a user perspective, the web program is easy to navigate starting with an allfactors, simple online data collection. The simple bio/neurochemistry data collection process comes from a patent-pending kit sent to a patient for saliva and urine collection then returned. Once all the data is received from patients, a personalized recommendations plan is presented to them online where they can view and proceed on their AI-rendered personal treatment pathway from any mobile device. They can upgrade their plan at any time to access more features, or the complete complement of services. They can also purchase from the site’s store additional testing, supplements,
or additional online therapy / coaching sessions at any time.
It’s been incredibly rewarding for Rogers to see MoodMD help patients in ways the outmoded status quo could not. Take “Joe,” for example. Joe came to Rogers looking for help with his lifelong struggle with anxiety. Joe felt unfairly handicapped in life via the way his mind and body handled its often-debilitating reaction to anxiety. Rogers tested Joe in all of the ways unique to MoodMD and discovered that Joe was one of those people whose GABA (the brain’s calming agent) production-engine enzyme was misfiring because of a lack of the proper nutrients in his diet. After diet therapy and adaptogens (special supplements for the brain) Joe got a brain “reboot” and was back into balance. From there depth therapy for his subconscious-embedded faulty thinking vault finally proved effective at helping Joe neutralize the negative belief systems he had built over the years.
MoodMD is live in North America and is looking to expand into Europe in the near future. They’ve partnered with Amazon Web Services (AWS) who have provided over $2M in services to assist with website hosting, security, and the most sophisticated AI tools in the industry, which helps assemble a precise, targeted set of recommendations that are AI-improved as each week’s progress is analyzed...
startuphealth.com 131
to
to healthtransformer.co
Scan
read the full story or go
MEET THE HEALTH TRANSFORMERS

132 StartUp Health Magazine / EXPONENTIAL PROGRESS
Pramana’s Biotech Discoveries Promise Revolutionary Type 1 Diabetes Management

Founder Diane Alexander (left) is revolutionizing drug discovery and development for diabetes from the inside out. At her biopharmaceutical company, she gives scientists freedom to operate with financial equity in their discoveries. She encourages new takes on previous research. The result? Breakthrough possibilities for T1D management.
to exercise, whether to go out with friends, what bedtime rituals are practiced–– decisions in the form of manual course corrections are constantly required to curb people living with Type 1 diabetes’’ episodes of high and low blood sugar levels.
Each health decision is like slicing the rudder of a boat through choppy waters, attempting to course correct a wayward direction. Redirect too much and you end up with too much insulin in your body, risking low blood sugar, or hypoglycemia. When this happens, individuals can experience symptoms like rapid heartbeat, shaking, and sweating. As hypoglycemia worsens, symptoms can include confusion, slurred speech, and even a loss of consciousness or seizures.
OOne hundred eighty decisions. On average, people living with Type 1 Diabetes (T1D) make 180 more decisions about their health each day than someone without diabetes. That’s equivalent to around one decision every five waking minutes. How much and when to inject insulin, what to eat, how and when
As one of the most common emergencies for people with T1D, the average person living with Type 1 diabetes experiences about two episodes of hypoglycemia per week, a figure that has not changed substantially in the last 20 years. Additionally, 25 percent of people living with Type 2 Diabetes develop recurring Hypoglycemia within 4-5 years of their diagnosis. Combined, that’s roughly 100 million people living at risk of hypoglycemia. Because of the innumerable combinations of their 180+ health decisions, there are as many different regimens for treating hypoglycemia in people living with Diabetes..
But what if there was a safe oral once daily medication that could prevent blood sugar dips and spikes for every person living with diabetes who suffers from hypoglycemia? Something that could eliminate
startuphealth.com 133
T1D MOONSHOT
MEET THE HEALTH TRANSFORMERS / PRAMANA PHARMACEUTICALS
all or most of those 180 extra decisions each day…something that could truly enable the achievement of glycemic control when taken with insulin?
Enter Pramana Pharmaceuticals Inc. and its boundary-pushing biotechnology. As a part of the company’s impressive portfolio of biological drug candidates, Pramana has driven a molecular innovation that has the potential to give the 100 million individuals who suffer from hypoglycemia back control of their lives.
ORIGIN STORY
Pramana’s origin story starts simply –“three senior scientists and a couple of investment advisors meet over coffee..” – but with an outcome that could save lives. In 2015, Diane Alexander, Co-founder and CEO of Canada-based Pramana, met with three medicinal biochemists over a cup of coffee to propose a deal. A serial entrepreneur, and senior investment advisor with over 25 years of capital markets experience, Alexander had gathered the accomplished scientists to discuss one of her favorite investment arenas–– biotechnology. She says she’s always had a penchant for the field, drawn to the positive impact that biotech innovation can have on health outcomes.
“Along the way, I’ve met some fascinating scientists,” Alexander says. “Particularly, scientists who’ve led medicinal chemistry programs that produced valuable drugs. Drugs that helped millions of people.”
When she met with three such scientists in late 2015, there were several targets of interest including some low-hanging fruit
to be had in molecular research surrounding Type 2 Diabetes (T2D). Big pharma had expressed interest in a particular protein receptor that could be developed into a therapeutic to address large, unmet needs in diabetes treatment. The protein, or target, was GPR119. Substantial investment was made advancing studies that could prove GPR119’s role in managing T2D. While the target proved to be a safe and well-tolerated conduit for T2D management – with some therapeutics advancing to Phase II clinical trials – nothing seemed to catch the eye of big pharma.
“There’s a lot of competition in T2D,” explains Alexander. “It’s more difficult for solutions to go to market, and in the case of GPR119 the historical efficacy data was just not robust enough”.
Sitting across from the scientists at the table, Alexander posed the question, “Why? Why wasn’t GPR119 successful, given it showed such therapeutic promise?” To get to the bottom of it, she proposed a partnership with the scientists. She sketched out a roadmap on the back of a napkin, detailing a timeline and resources to develop a proof of concept for GPR119’s use in managing T2D, along with other indications for the target in metabolic disorders.The goal was to discover and develop better molecules than had been previously interrogated. In addition, she offered them equity in the company.
“There was an urgency to our conversation, but I didn’t want them to have scientific boundaries” Alexander says. “I wanted to enable them to be in an open environment to go after whatever health targets
134 StartUp Health Magazine / EXPONENTIAL PROGRESS
they were interested in.”
Her theory was that if the scientists were given the freedom to research outside of the biases inadvertently introduced in legacy T2D studies, and they were given equity along with capital in the company that was backing them, she could spur a new level of innovation.
In 2016, the scientists began their research under the Pramana banner. By 2017, they’d filed a provisional patent for GPR119 to advance their pre-clinical research. Then, in 2019, Alexander was introduced to a body of work that suggested GPR119 had been misinterpreted. Further discovery of new therapeutics with that molecule would require a significant change of direction— from T2D therapy , to an indication prevalent as to 90% of people living with T1D and 25% of people living with T2D.
It was the kind of pivot that large corporate research teams struggled to make, but that Pramana was designed for. The team shifted directions, leading them to a breakthrough that would not only secure the company’s future but chart a new course of discovery in T1D management and hypoglycemia prevention.
UNDER THE HOOD
In her early conversations with big pharma clients to gauge interest in Pramana’s research, Alexander recalls being told two things: “You’re crazy to go after GPR119 again.” And, “Go talk to David E. Kelley, MD.” Kelley was a senior leader of Merck Research Laboratories, a renowned multinational pharmaceutical company dat-
ing back to 1668. He was known for his novel approaches in drug discovery and early clinical development for diabetes and obesity. Alexander listened to the latter bit of advice. In 2020, she invited Kelley into Pramana’s fold. She dismissed the naysayers who felt GPR119 research had run its course. In fact, she embraced the notion that perhaps GPR119 was misinterpreted.
Kelley’s legacy research in GPCRs and insulin ultimately inspired Pramana’s fresh look into the otherwise tired space of T2D molecular inquiry. While other biopharmaceutical labs’ T2D research stated that GPR119 was predominately expressed in beta cells – the producers of insulin –Kelley’s studies suggested something very different. By 2021, Pramana’s growing team of medicinal biochemists was able to prove Kelley’s hypothesis: It wasn’t the beta cell where GPR119 was mostly expressed. It was the alpha cell.
“It was new information in the world of metabolic disease research,” Alexander says. “Proving that GPR119 is mostly expressed in the alpha cell shifted our focus from Type 2 to Type 1 Diabetes. It opened the doors for hypoglycemia prevention and potentially to other novel therapies for us”

As a “g protein,” the GPR119 acts as a molecular switch inside cells, transmitting signals from outside a cell to its interior...
Scan to read the full story or go to healthtransformer.co

startuphealth.com 135
DEMIS HASSABIS was the CEO and co-founder of DeepMind and now leads Google DeepMind. His team developed AlphaFold, which revolutionized nearly every field of biology by using AI to accurately predict 3D models of protein structures.


Dream Impossible
We solve big health challenges by collaborating with mission-aligned organizations, families, and non-profits to transform once-siloed projects into powerful health moonshot communities. Learn more at startuphealth.com




 Unity Stoakes President & Co-founder
Unity Stoakes President & Co-founder







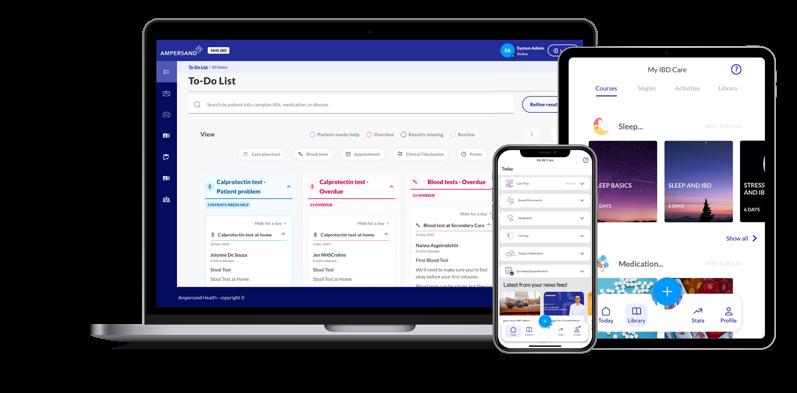









 Jeff McCormack, CEO & Co-founder, Iryss
Jeff McCormack, CEO & Co-founder, Iryss































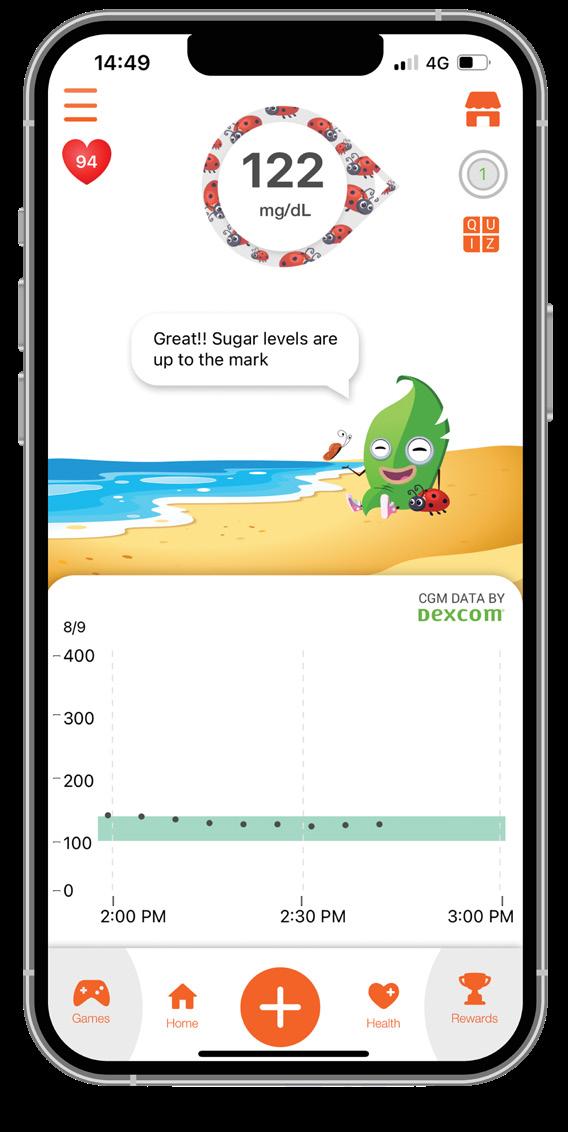


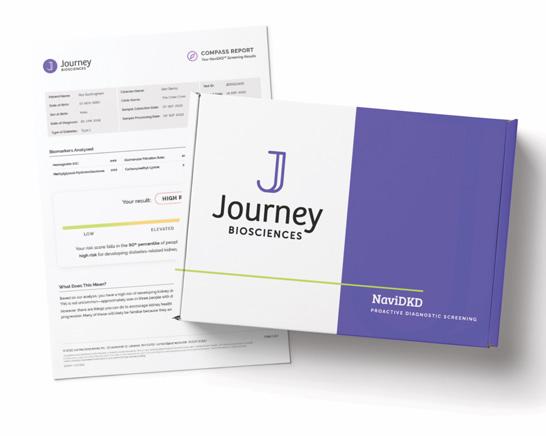 Minutia minutia.co
Minutia minutia.co