A health moonshot program for ambitious founders and funders


"Education is the most powerful weapon you can use to change the world."
-Nelson Mandela



A health moonshot program for ambitious founders and funders


"Education is the most powerful weapon you can use to change the world."
-Nelson Mandela


AAfter deep reflection on what we have learned over the past five decades as artists and instigators, entrepreneurs and technologists, and as patients and citizens of the world, we keep realizing that our life’s work is only just beginning. With StartUp Health we started a magnum opus that many skeptics say is an impossible mission: to grow a global army of Health Transformers to solve the world’s biggest health challenges. The skepticism has been enlightening, sometimes maddening, and ultimately a helpful driver to keep us moving forward.
Nelson Mandela inspired us long ago with his great words and we are believers: "It always seems impossible until it's done."
Our masterplan, now in its second decade of development, is to leverage the power of community and collaboration and to inspire and educate a world of like-minded people to work together to achieve health moonshots.
We believe the cumulative result of this global force for good will become clear over time in the form of improved health and happiness for billions of people. We are aware this sounds dreamy and the reality is we are seemingly far away from driving transformational change anytime soon.
So we are doing something about it.
We are embarking on our next chapter to expand what we started 12 years ago with StartUp Health Academy. We are building Health Transformer University, with the sole purpose of helping grow generations of Health Transformers who collaborate to solve big health challenges (read about it on page 94). We are seeking passionate founders and funders who want to build and back health moonshot companies. To join our mission, contact us at moonshots@startuphealth.com.
Steven Krein CEO & Co-founder Unity Stoakes President & Co-founder"Education is the most powerful weapon which you can use to change the world."
- Nelson Mandela
TThe other day my nine-year-old son brought home a school assignment in which he’d been asked to write down 100 things he was thankful for. Among such gems as “cozy fireplace” and “a full stomach” was #11: “AI”. I asked him about it, and he said, “I love ChatGPT!”
To my son, AI is just a game, a way to get the computer to write funny stories and answer questions about Marvel supervillains. But his answer got me thinking about the nature of intelligence, and how our minds are shaped by mountains of data.
When schools are at their best, they teach people how to learn, not what to think. They layer wisdom over data so that we can confront the challenges of the future, not merely analyze the past. That’s a particularly important skill in entrepreneurship, and our world of health innovation, because we’re always solving for an unknown future.
At StartUp Health, we’ve been working for more than a decade on our own futureoriented intelligence framework. It’s a unifying principle that says that founders matter more than companies and that a founder’s mindset matters more than their momentary performance. In other words, “who” beats “what” and how you think can mean the difference between success and failure, between impact and irrelevance.
That mindset is on display in nearly every one of these pages, from the story of how Wendy Powell helps women thrive after pregnancy (read about MUTU on page 26) to how Sunny Liang is bringing clinically-validated sleep therapy to the masses (read about Zen Sleep on page 86).
Which founders, companies and ideas will transform health in the long run, surviving long sales cycles, regulatory hurdles and medical complexities? It’s not just the ones with the largest data sets for training their algorithm. It’s the ones that have cultivated mindsets of collaboration and commitment. And it’s the Health Transformers who pause to recalibrate that mindset quarter after quarter and year after year.
It’s clear my son’s generation will have a different relationship with AI than mine. But my hope, for him as with the entire StartUp Health ecosystem, is that new AI-driven wellsprings of data will drive us further into the deep wisdom questions of HOW we make decisions and WHO can ultimately benefit.
Logan Plaster Editor-in-Chief




follow
Kevin Dedner of Hurdle Selected for Fierce Healthcare's 2022 List of Most Influential Minority Executives in Healthcare
FIERCE HEALTHCARE
9/26/22
Virta Health Reverses Diabetes with Diet and Exercise
NPR 9/26/22
Sanguine Biosciences Selected for Fortune's Top Ten Best Small and Medium Workplaces in Biotechnology and Pharmaceuticals
FORTUNE
9/29/22
Particle Health Launches EHR Data Sharing Tool
BECKER'S HEALTH IT
10/4/22
Discover (DFS) and TYDEi to Digitize Healthcare Purchases
NASDAQ 10/6/22
The Hottest Startups in Lisbon: Virtuleap

WIRED
10/7/22
D.C.’s Rose Health Acquired by Californian Behavioral Health Company
WASHINGTON BUSINESS JOURNAL
10/10/22
Lifestores Healthcare
Raises $3M to Expand Its Pharmaceutical Marketplace Across Nigeria
TECHCRUNCH
10/12/22
Toyin Ajayi, MD, of Cityblock Selected for the Female Founders 100: The Top Women Entrepreneurs of the Year
INC. 10/15/22
Gabbi Is One of the Most Promising Women's Health Startups of 2022, According to VCs

BUSINESS INSIDER
10/17/22
Unified Women's Healthcare Buys Digital Menopause Startup Gennev
AXIOS
10/20/22
Aidoc Partners with Us2.ai on Echocardiogram Analysis Tool
MOBIHEALTHNEWS
10/24/22
Valera Health Selected as a Brand That Matters in 2022
FAST COMPANY
10/25/22
Medical Device Company
Lazzaro Medical Secures
$1M from Northwell Health
BECKER'S HOSPITAL REVIEW
10/28/22
10 Innovators Shaping the Future of Health: Toyin
Ajayi, MD, CEO & Cofounder of Cityblock
FORTUNE
11/16/22
$1.8M TO DISCOVER NON-HORMONAL CONTRECEPTIVES
Cyclica Awarded $1.8M Grant from Bill & Melinda Gates Foundation to Discover Non-Hormonal Contraceptive
HIT CONSULTANT
11/15/22
12 StartUp Health Companies Named to the Digital Health 150: 9amHealth, Babyscripts, Buddy Healthcare, Cala Health, MindTrace, Mobio Interactive, Neolth, Particle Health, Renalis, Salvo Health, Sami, and Spect
CB INSIGHTS
12/7/22
Mammha Helps Tackle the Leading Cause of Postpartum-Related Deaths: Mental Health
MSNBC 12/20/22
SoCal-Based Quantgene Uses Gene Sequencing to Track COVID Variants
SPECTRUM NEWS 1
1/4/23
The Patient Journey Tech Stack: Yishai Knobel of RxWare Makes 10 Pharma Predictions for 2023

HIT CONSULTANT
1/5/23
Dr. Yusuf Sherwani of Quit Genius Shares His Behavioral Health Predictions for 2023
Healthcare Founders at Salvo Health and Other Startups That Raised Money in 2022 Share Their Best Pitch-Deck Advice
BUSINESS INSIDER
12/27/22
HIT CONSULTANT 1/10/23
Arrive Health Acquires Medication Adherence Tech from UPMC
MEDCITYNEWS
1/18/23
Avanlee Care Joins Forces with Walmart, Uses Technology to Support Millions of Unpaid Caregivers
FIERCE HEALTHCARE
1/13/23
NexStride from De Oro Devices Helps Clovis Veteran with Parkinson's Walk Again
ABC30 FRESNO
1/23/23
Technology from Babyscripts Could Improve Pregnancy Care for LowIncome Patients
STAT NEWS
1/24/23
Why Some Anxiety Is Good, Even Though It Feels Bad, Featuring Dr. Tracy Dennis-Tiwary of Arcade Therapeutics

NPR ON POINT PODCAST
1/26/23
BrainScanology: Refining Shape Measurements at the Biological Level
DIGITAL FIRST MAGAZINE
1/31/23
UCSF, Cedars-Sinai Partner with Biome Analytics on Researching EHR Interventions for Kidney Injuries
BECKER'S HOSPITAL REVIEW
2/1/23
Valera Health Is One of the Companies Cigna Is Investing In


BECKER'S HOSPITAL REVIEW
2/7/23
Wingwomen Pivots from Peer Support to Coaching Platform for Women with Preexisting Conditions

Trying to Conceive
FEMTECH INSIDER
2/13/23
Extending the Human Life Span by a Decade Within a Decade: An Interview with Jo Bhakdi, CEO & Founder of Quantgene
FORBES 2/15/23
'BrightPay Health Is One to Watch in a New Wave of Startups Tackling Financial Issues Within the Healthcare Space' BUSINESS INSIDER
2/13/23
Colby Takeda of Pear
Suite Selected as a Tech Entrepreneur of the Year
Finalist for the Hawaii Entrepreneur Awards 2023
HAWAII BUSINESS MAGAZINE
2/16/23
Vous Vitamin Is One of the Best Personalized Vitamin Subscription Services, According to a Certified Nutrition Coach
SPORTS ILLUSTRATED
2/16/23
Each issue we introduce you to the inspiring founders we invested in recently. Their work addresses a range of health moonshots, from Women's Health to Access to Care.
Learn how you can back the next generation of Health Transformers at startuphealth.com

When Jade Kearney had her first child, she came face to face with the staggering healthcare crisis facing Black women in America. Now she’s built a maternal health platform that provides community support for under-represented women and cultural competency coaching for physicians.
AAmerica has a maternal health crisis. More specifically, America has a Black maternal health crisis. More women die in childbirth in America than in any other high-income country and if you are a Black woman in America, the mortality rate is twice as high as the average and three times higher than that of a white woman.
These statistics are widely known and yet the problem keeps getting worse. From 2018 to 2020, the maternal mortality rate for Black women increased from 37 deaths per 100,000 live births to 55.3 deaths. COVID-19 only exacerbated the problem; pregnant women
with COVID-19 were more likely to experience complications and people of color were at greatest risk in the pandemic because of health inequities. If you are a Black woman in the United States, you are more likely to take public transportation, have no or limited paid time off when you are sick, lack access to healthcare, and have pre-existing conditions that increase the risks if you contract COVID-19.
Jade Kearney knew these statistics when she became pregnant with her first child. At the time, she was pursuing a master’s degree in digital media at NYU, intending to use her background as an academic director to create tools for teachers. She never thought she’d create a digital health platform for Black mothers. Then her daughter was born.
“I made it through pregnancy, through preeclampsia. I hemorrhaged during delivery. I made it through all of that. I thought the hard work was done. But really for me, the hard work started postpartum,” says Kearney.
When Kearney experienced postpartum anxiety OCD, she struggled to find the support and medical care she needed. A healthcare provider prescribed her Zoloft and told her to check in after
six weeks, not understanding the stigma around antidepressants in the Black community and the hesitations a Black mother might have to start such a drug. Even friends and family failed to understand what she was going through.
“Black women do not talk about pain,” says Kearney. “We try to fit the strong Black woman stereotype. Suffering is expected as part of the journey and we suffer in silence.”
This stigma partially explains why Black women are twice as likely as white women to experience maternal mental health (MMH) conditions — like anxiety, depression, OCD — but half as likely to receive any type of care. And it’s a vicious cycle: when doctors fail Black women in maternal care, it becomes harder for these women to turn to them when they need help after the baby comes.
“There’s a distrust of the medical system,” explains Kearney. “It’s rooted in all sorts of things historically, even not being fully transparent about mental illness because of fear your children might be taken away.”
Kearney wanted more for herself and other Black women experiencing postpartum mental health challenges. She wanted community. She wanted a culturally competent healthcare provider who understood the particular challenges she experienced in the medical system. She wanted better outcomes for women like her in America.
“Sometimes with all the statistics, you
say the word ‘Black’ so much that you forget that this is an American problem,” says Kearney. “We are American, and the American healthcare system is failing us.”
Kearney decided to bring Black mothers together at the table to discuss the challenges of mental health in their community. She put together a brunch event and didn’t know if anyone would come. The brunch sold out in two hours. The moms ranged in age from 20 to 65 but all shared the same desire to connect over their experiences navigating maternal care.
A few themes emerged from this brunch, themes that helped shape the initial idea for She Matters. First, these moms wanted better words and terminology to describe what they were going through. They wanted a resource that helped them frame their experience in such a way that they got the care they needed. On the flip side, they felt like therapists, psychologists, and other mental health professionals needed to make the effort to understand them better so they could provide more help.
Galvanized by the conversations she was having with other mothers, Kearney conceived of an app that would provide the tools women like her needed and the tools providers needed to provide better care to their patients. She developed the first iteration of She Matters as her digital media thesis project at NYU. The project took off from there, landing in NYU’s accelerator program and raising its first pre-seed funding, before making into the Techstars program in 2021.
In the beginning, She Matters focused on postpartum mental healthcare for Black women, working to connect them to culturally sensitive therapists and training mental health professionals to better understand the nuances of working with this population. Over the course of their time in Techstars, the model expanded to other aspects of Black maternal care, like the two biggest comorbidities Black women experience: preeclampsia and hemorrhaging. They now offer coaching to entire healthcare networks and hospitals, to ensure culturally competent care for Black women before, during, and after delivery.
She Matters is a digital health platform that supports Black mothers by providing access to community, culturally relevant resources, and culturally competent healthcare providers. Additionally, it operates as a learning management system (LMS) for physicians and healthcare
systems through its coaching platform that provides certification and continuing medical education (CME) credit. It’s an enterprise solution, working with whole hospital networks to make sure their labor and delivery departments are culturally competent.
She Matters is also a telehealth platform that connects women to certified therapists and culturally competent healthcare providers for appointments. Women can log in, find a provider, make an appointment, and do a video visit, all on the app. It takes health insurance and Medicaid and also has more than 2000 hours of volunteer hours from mental health professionals it can offer to those without insurance. They are building out the telehealth capabilities of the app and have other features, like a symptom tracker, in the pipeline.
“These features will help us with our goal of improving communication between those with lived experience and healthcare providers.”
To that end, She Matters provides feedback to hospitals via survey responses from their Black patients, improving practices by tracking patient outcomes. Their surveys have an 86% response rate on average, and this high rate makes for a big impact in regards to patient safety, patient experience, and addressing health equity gaps.
As Kearney explains, “Being a Black woman in the healthcare system is lonely and scary. The surveys help validate this experience. And then we can bring this feedback to hospitals and hold their feet
Black women with pregnancy complications are 2x as likely to develop stroke and heart attack and 4x as likely to experience high blood pressure.
to the fire to do better for their patients.”
Doing better for these patients represents huge possible savings for insurance companies and hospitals. Maternal mental health conditions represent $18.1B in readmission costs, not to mention the $7.5B in readmission cost for hypertension or the $4.8B in costs associated with gestational diabetes. It’s a relatively untapped market with few existing solutions.
“Raising [funds for She Matters] is very personal to me,” says Kearney. “I can connect this to an ROI. There’s money here and it’s lucrative and it’s a good business decision, but it’s also just the right thing to do. Black women are dying and we can change that.”
She Matters closed a $1.5M pre-seed round in August 2022 and is growing out their team to expand their user community and physician training. Their goal is to be in 80% of US hospitals in the next five years, beginning with areas where there are currently legislative mandates for Black maternal mental healthcare training and maternal care deserts with limited access to care.
“When a Black woman sees the She Matters shield on a hospital, I want her to know that there is someone in that place who understands her experience and will do everything possible for her to come out. The shield means safety.”
StartUp Health is proud to back the She Matters platform because its co-founders, Jade Kearney and Marguerite Pierce, have the knowledge, education, vision, and
lived experience to bring better maternal healthcare to America, saving lives and preventing costly hospital readmissions. By approaching the problem from both the patient side and the physician side, they form a bridge of communication and trust from which real change can happen.
We’re also excited to back this team because the She Matters cultural competency course was developed in-house, drawing on Kearney’s background in intercultural/multicultural and diversity studies at Georgetown University. Not only is she an educator who understands how people learn, but she is a Black mother who understands how the system fails women like her. She and Pierce, her COO, have walked through maternal mental health issues and come out the other side and know personally what the medical community needs to understand about treating Black women.
Though rooted in their own experience, the She Matters team has an expansive vision to provide culturally competent care to all types of people. In the near future, they plan to launch ‘We Matter,’ a health platform that offers cultural competency courses and resources for the LGBTQ+ community, as well as products that address the needs of Latina women and Native women. As Kearney says, “We all deserve to experience motherhood from a place of safety without shame.”
contact: shematters@startuphealth.com
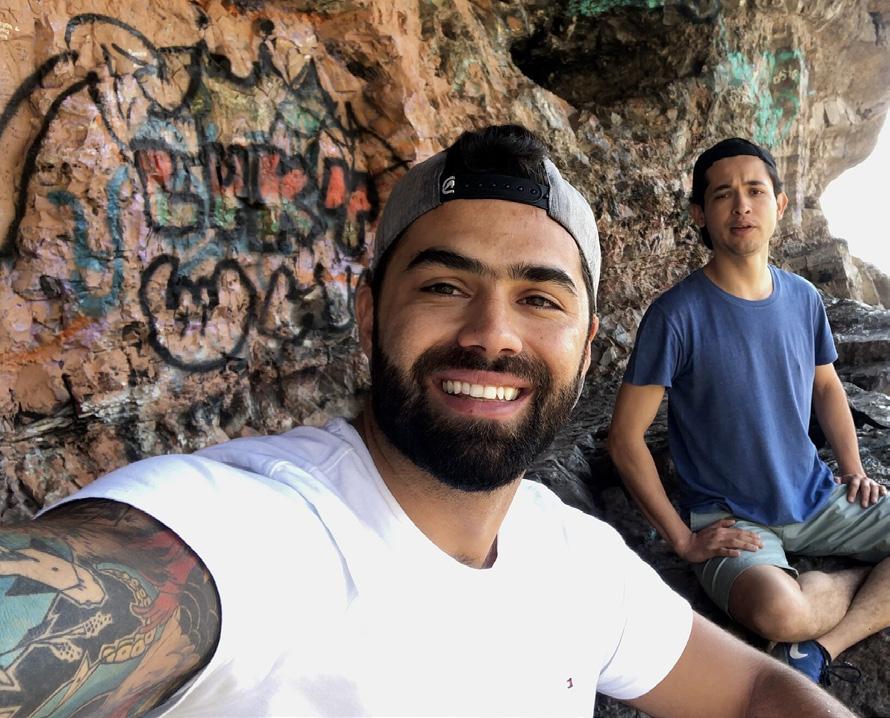
L.R. Fox likes to solve big problems. He helped bring order to the chaos of the drone industry, now he’s working to change how the world sees male birth control with a safe, reversible Vasalgel procedure.
GGlobally, nearly half of all pregnancies are unplanned. Yes, half. One of the most important decisions of someone’s life–whether or not to have a child–is often the result of chance. There are big picture health equity issues that contribute to unplanned pregnancies: things like education levels, access to birth control and healthcare, and gender inequality. Then there’s the human error side of it: old

condoms, forgotten pills, miscalculated fertility cycles.
Historically, women have shouldered the burden of pregnancy prevention, often turning to hormonal birth control methods to ensure they don’t have a child. For most of their adult life, women using these methods endure side effects that can range from annoying (weight gain, unusual hair growth, breast tenderness) to concerning (nausea, mood changes, blood pressure risks) to harmful (migraines, cardiovascular disease and blood clots, and breast cancer).
As reproductive health issues play out in the headlines, there’s been growing press around the idea of better male birth control, something that would help couples share the onus of responsibility for unplanned pregnancies. The two current main options for men–condoms and vasectomies–don’t get the job done. Condoms have a 18% failure rate and a 57% dissatisfaction rate, making compliance difficult to achieve across the population. The pain and discomfort associated with vasectomy make it less popular with men. But more significantly, vasectomy is considered permanent contraception since the ability to reverse the vasectomy by reattachment of the vas deferens requires expensive microsurgery and restabilizing patency of the vas deferens is unpredictable, making it an unappealing option for younger men who might want to have a child sometime down the road.
In recent years, researchers have worked on cracking the code for hormone-based birth control for men. The news of the
trial phases of “the male pill” produced a fair bit of understandable glee and ribbing from the half of the population who have suffered the side effects of hormonal birth control for years. While they are still under development, the fact of the matter is that hormonal contraception for men comes with the same laundry list of problems as hormonal contraception for women–physical and emotional side effects, difficulty adhering to a schedule, issues of access and supply.
There needs to be a better way. No one, whether they have testes or ovaries, should have to suffer the side effects of hormonal birth control. No one should have to choose between having an unplanned pregnancy or increasing their risk of certain cancers. The decision to have a child shouldn’t be a game of chance. Whether someone works in tech in downtown Seattle or raises cattle in the Paraguayan Chaco, they need a longlasting, safe, and practical solution to preventing pregnancy.
Growing up in the foster care system of California, L.R. Fox saw firsthand the consequences of unintended pregnancies. He remembers a particular moment as a teenager when he looked around his group home and saw the chaos around him–things like abuse, poverty, domestic violence–and thought so much of it could have been prevented if people got to choose when they had a child.
“It’s a systemic problem that affects every class of society. People should be able
to effectively choose when to bring a child into the world.”
Fox is not the type to ignore a problem. At age 19, he launched WhiteFox Defense Technologies, when he recognized the security and safety issues the booming drone industry created. He worked with Congress to pass legislation that guided safe integration of drone usage into society and grew the company into one of the most influential thought leaders in the counter-drone and airspace management arena, earning him a spot on the Forbes list of 30 under 30 in 2019 at the age of 23.
Moving from aerospace to male birth control might seem like a leap, but as Fox explains, he’s drawn to “solving big problems that everyone recognizes and yet no one is doing anything about.” As he worked with Congress to solve airspace issues around future potentialities like flying taxis, it struck him as ridiculous to be thinking about flying taxis as a nation when we haven’t even cracked the code on how to reliably prevent unplanned pregnancies, particularly when it comes to the man’s role.
Fox started exploring solutions for effective male birth control and came across the work of Parsemus Foundation and its founder Elaine Lissner, known as the “Mother of Male Birth Control.” After decades of experimentation with various potential methods, Lissner and her team discovered a safe and effective method of non-hormonal male contraception known as RISUG (Reversible Inhibition of Sperm Under Guidance). Developed in India and initiated in 1979, RISUG
involves injecting a polymer gel into the vas deferens which allow fluids, but not sperm, to pass through the channel. After successful use in around 1,000 patients, RISUG was shown to be a safe and effective solution. Parsemus expanded on those learnings and optimized the formula and procedure to increase accessibility, naming the new product Vasalgel.
Vasalgel solves the major problems of other male birth control options. It takes 10 minutes to implement; it does not involve removing, cutting, cauterizing, or crimping tissue; it lasts for 10 years; and it is designed to be completely reversible at any time by another simple injection which dissolves the gel. There’s no need to remember to take a pill every day or have a
"Vasalgel solves the major problems of other male birth control options. It takes 10 minutes to implement; it does not involve removing, cutting, cauterizing, or crimping tissue; it lasts for 10 year; and it is designed to be completely reversible at any time."
condom on hand, making it a more practical option for rural communities or those lacking access to regular medical care. It is easily reversible, unlike a vasectomy, so when a person wants to start a family they can. It can be reinstated at any time after removal, and it is non-hormonal, making it safe to use without fearing the side effects.
As a non-profit, the Parsemus Foundation focused its efforts on proving Vasalgel safe and effective through trials and studies, as well as proving the demand and need for it. They were looking for a commercialization partner, someone to create the market for such a product and dispel some of the cartoonish misconceptions about male birth control, someone with experience shaping a nascent industry through legislation and messaging. In short, they were looking for someone exactly like Fox at the very same time Fox was looking for an answer to the global issue of family planning.
NEXT Life Sciences exists to develop and distribute Vasalgel technology, a nonhormonal, long-lasting, reversible form of male birth control that empowers its users to choose if and when they bring a child into this world. In short, NEXT Life is creating a scalable and accessible global solution to the 85 million unintended pregnancies that occur each year.
Through preclinical studies, NEXT Life zeroed in on the optimized formula of Vasalgel that combines maximum efficacy for both contraception and reversal.
13%
The failure rate of condoms because of user error
85M
Number of unintended pregnancies that occur each year globally
They’re conducting one final study of this formula before moving into clinical trials in 2023. Currently over 50,000 people across the world are on the interest list for the product.
“We have the proof of concept. Now we are working to make this the standard of care,” says Fox.
To that end, NEXT Life is about to announce its medical advisory team, composed of some of the world’s foremost vasectomists. Fox says the physicians have greeted the news of Vasalgel technology with enthusiasm. “They love it because it is faster, easier, and in review of its use in India, has been demonstrated to be safe. It also has pragmatic value to a doctor because of the vastly bigger market size it offers.” Most vasectomies are performed
on men over the age of 45; Vasalgel has the potential to work for nearly every sexually active man.
A large part of the task ahead for NEXT Life is changing some of the norms and expectations regarding contraception. It’s a messaging challenge, one the company’s Chief Marketing Officer, Dan Connolly, is meeting head on.
“It really is a cultural opportunity, the starting point of a revolution,” Connolly explains. “We want to shift the narrative to the idea of freedom–Vasalgel is about the freedom of deciding when to have a child. It’s about setting people and families up for success.”
NEXT Life is fundraising to build out its research and development and communications teams as they head towards FDA approval. They plan to implement a phased launch in 2024, rolling out different delivery methods that capitalize on their current demand before growing to private and public insurance funding and government grants.
“The question is how to introduce a brand new technology into the lives of people some would say are adverse,” says Fox. “We plan to show them the value of getting to exercise the right to not have a child if you don’t want to have a child. Men should have a choice, and it should be a shared opportunity to make that choice.”
Sometimes a company comes along that dares to disrupt not only the method in which healthcare is delivered but a society’s fundamental way of thinking about
healthcare. NEXT Life is one of those companies. StartUpHealth is proud to invest in NEXT Life’s innovative, patented male contraceptive technology that is turning birth control on its head.
Part of our enthusiasm stems from Fox’s successful track record at creating scalable, accessible solutions in highly-regulated industries. Through his work at WhiteFox in the aerospace industry and as a Vice Chair of the Chamber of Commerce, Fox proved himself able to navigate legislative and cultural minefields to create deliverables that work on different scales in different contexts. We can’t wait to see how he does the same in the contraceptive care space.
NEXT Life is also poised to capitalize on the current cultural moment, when there’s a groundswell of interest in male contraception. It’s well positioned in the growing marketplace of solutions as something that works for most men, at any stage of life. Part of this marketplace revolution comes from the recent Supreme Court decision to limit abortion access. As Fox put it, “no matter which side of the aisle you are on, both sides can agree that the less you are putting a woman in the position of needing an abortion, the better it is for society.” Vasalgel technology does just that.
contact:
next@startuphealth.com

Wendy Powell has helped more than 90,000 women get back to living their lives with strength and confidence after pregnancy through her purpose-built fitness program. Now she’s scaling the platform with new offerings around functional health and mental wellness.
PPostpartum pelvic floor issues are a common problem. One estimate says more than one in three new mothers will experience urinary incontinence while one in five will experience severe pelvic floor muscle injury. It’s so common that it almost seems normal; mothers at the playground may joke about wetting themselves when they sneeze or laugh — diminishing the real shame, discomfort, or even pain they experience.
But common does not mean normal. Just because something happens frequently doesn’t mean it should be acceptable. And when it comes to the pelvic floor, there are widespread ramifications to ignoring a problem. The pelvic floor is
essentially a support system, holding the uterus, bladder, bowel, and other pelvic organs in place so that they can work properly. When it is weak, it can contribute to chronic back pain, pain during sex, core weakness and diastasis recti, a prolapsed uterus, as well as the aforementioned incontinence.
These consequences aren’t just physical. Women with urinary incontinence after giving birth are almost twice as likely to develop postpartum depression, and a recent survey by MUTU found that 87% of women said that pelvic floor issues affected their mental health at some point. The emotional impact can be subtle: a dip in confidence or capability. As one mother puts it, “It’s hard to be present and effective at work or in your community when you’re worried you’ll wet yourself or you can’t lift something you used to.”
Many women turn to exercise as the answer to their pelvic floor issues, but don’t understand why the traditional fitness paradigm — “if something is weak, work out harder or longer” — doesn’t get them results. In fact, some forms of exercise increase the strain on these muscles and the risk of prolapse. Without proper engagement and a systematic plan, postpartum
pelvic floor issues leave women feeling like something is irrevocably changed or broken about their body, affecting mood, intimate relationships, and lifestyle.
Enter MUTU.
When Wendy Powell was pregnant with her first child about 17 years ago, she figured her body was prepared for the challenge of pregnancy, delivery, and recovery. She was a highly-certified personal trainer who specialized in pre- and postnatal fitness.
“In theory, I knew my stuff. Then my body didn’t do what I thought it was supposed to do.”
Powell discovered that the strategies she had learned were not enough. As she struggled through her own core and pelvic issues following the birth of her first child, then, two years later, her second, she came to face a hard truth: the expertise she had trained in was not sufficient to fully recover from childbirth.
“The core and pelvic floor issues I was having — the ones I had heard from my training clients and now was learning for myself — the tools I had to deal with them simply were not good enough.”
She knew the knowledge and expertise to deal with pelvic floor issues must exist somewhere. Powell broadened her focus of study beyond the fitness world and began working with biomechanists, physical therapists, sex therapists, and midwives to understand how the muscles, ligaments, nervous, and skeletal system functioned together to support pelvic floor function-
ing. From there, it was a matter of translating what she learned into solutions that women could understand and follow.
“Part of the challenge is that we are so disengaged with our pelvic floor that we don’t even know what it’s supposed to feel like when you are engaging it correctly,” Powell explains. “My goal was to develop strategies and exercises with the language for someone to know they are getting it right or wrong.”
Powell launched the first iteration of her program over ten years ago. At the time it was her filming herself in her backyard doing the series of pelvic floor exercises she designed with input from specialists. From the start, the focus was on medical credibility and functionality — the questions “is it safe?” and “does it work?” fueled everything she created. Sure, the exercises might help a woman tone up after pregnancy, but as Powell says, “it was driven by dignity and confidence and function, not aesthetics.”
The program worked. And after a few celebrity endorsements (Pink’s trainer posted about using it and the Daily Mail reported that Kate Middleton did MUTU after the birth of Prince Louis), it snowballed. At this point, 90,000 women have been through MUTU System’s 12step course, and it doesn’t show signs of slowing down.
“The ongoing feedback we receive is women saying, ‘I thought I was just buying an exercise program but you’ve given me back myself.’ Women are told that they just have to put up with certain problems after having a baby, that they are
normal, but that’s simply not the case.”
The MUTU System is a postpartum recovery app and community that provides evidence-based techniques to improve pelvic and abdominal function. The MUTU digital platform guides users through a 12-module program that rebuilds a sense of connection with their bodies, helping them understand how it works and how to best engage and release it. The goal is to restore dignity, function, and confidence in a medically-recommended, body-positive way.
MUTU currently operates as a D2C
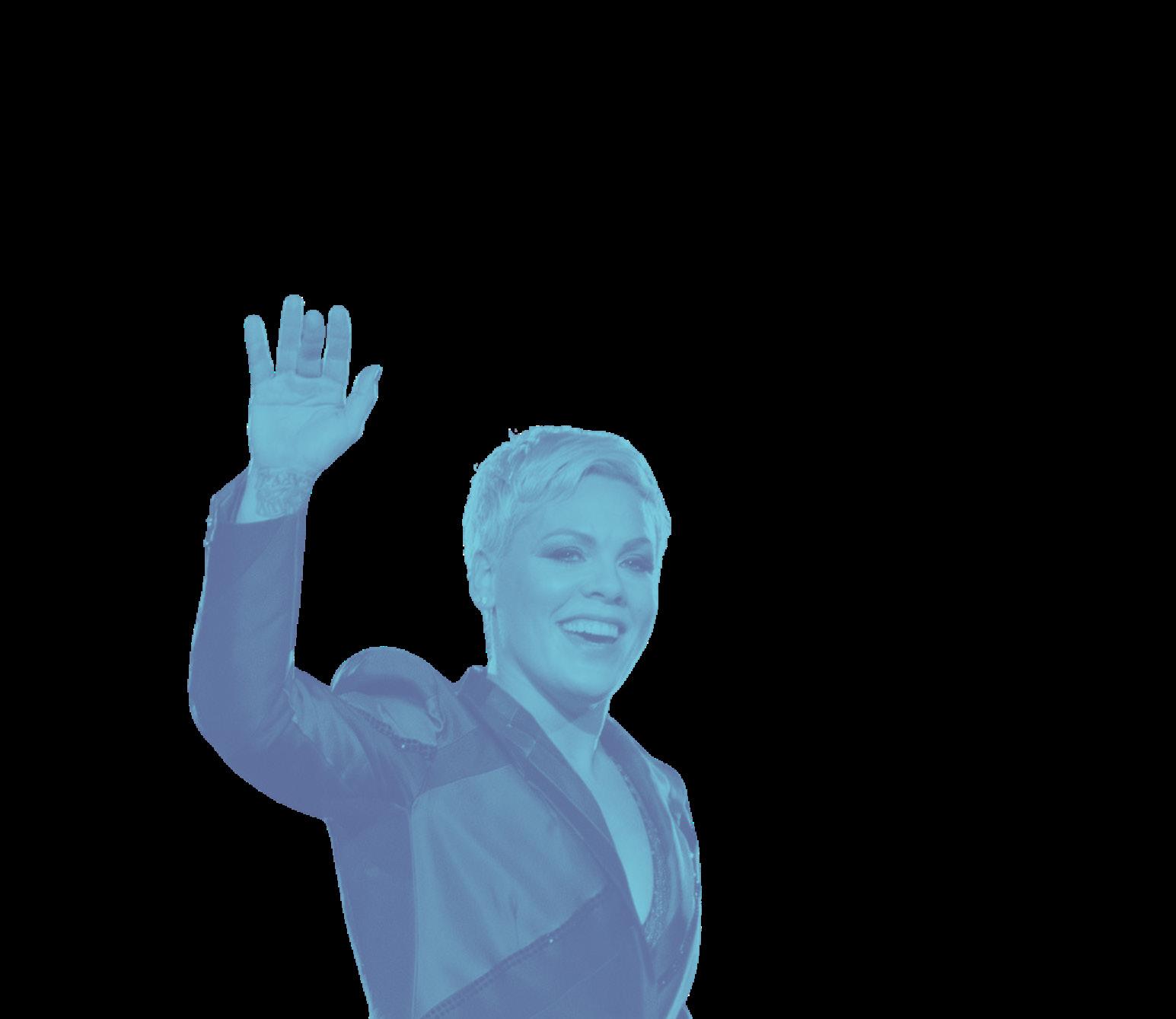
with a majority of women hearing about it from a pregnancy care provider or through word of mouth. Most of their users come to the program three to 12 months after giving birth, realizing that their body isn’t going to just “bounce back” to normal. They can sign up for a year’s membership or go month to month.
The workouts are brief, ranging from 12–20 minutes a day, but the results speak for themselves. For example, 92% of women who experienced bladder symptoms saw improvement after using the MUTU System, 89% of women who experienced pain or discomfort during or after sexual intercourse reported an improvement,

The program worked. And after a few celebrity endorsements (Pink’s trainer posted about using it and the Daily Mail reported that Kate Middleton did MUTU after the birth of Prince Louis), it snowballed. At this point, 90,000 women have been through MUTU System’s 12-step course.
and 88% of women suffering from symptoms of prolapse reported improvement. These results led to a partnership with the NHS in the UK during the pandemic when physiotherapists couldn’t see patients in person, paving the way for future opportunities to care for patients at scale and prevent costly pelvic health problems.
“The average time it takes for someone to go to the doctor with incontinence is seven years. Then there’s physiotherapy, and if that doesn’t work, surgery. In the meantime, there are mental health implications and healthcare costs all along the way.”
Powell and her team look to expand MUTU in two strategic directions in the year to come. First, they plan to develop their offerings beyond postpartum into other life stages, supporting women with pelvic floor issues during menopause, perimenopause, and before and during pregnancy. They also intend to offer more pathways for women into the MUTU System by integrating themselves with public and private insurance and partnering with larger corporate entities and health services.
“We’ve proved it works and now want to empower more women to understand their bodies and its signals so they can live with confidence. MUTU is as much a foundation for life and mothering as it is a work out,” says Powell.
MUTU combines a proven track record and reputation as the go-to trusted authority on postpartum recovery with a highly
scalable product that is poised to serve a significantly larger sector of the population. Their focus on functional health, mental wellness, and bodily confidence sets them apart from their aestheticallyminded competitors, and it allows them to easily integrate themselves with health services and employee benefits. They stand poised to change the way the healthcare community talks about pelvic health, so it recognizes that common problems don’t have to be normal or acceptable.
Wendy Powell’s passionate leadership comes from her life experience both as a fitness expert and a mother. It’s easy to become just another exercise routine to choose from, but Powell ensured that the MUTU System stands the test of time (and results). She pursued evidence-based solutions so that women could trust what they were doing was safe and effective. Thanks to this focus on real, corroborated results, MUTU was selected as an Innovation Accelerator Fellow with the NHS in the UK, and they are currently partnered with the NHS in research studies that further validate the program.
The pelvic floor is the support system to so many bodily functions, and MUTU is the support system that helps it function as it should. We’re proud to back this system that gives women the strength to live full lives, with confidence that their body works.
contact:
mutu@startuphealth.com

Scott Kaiser, MD, and Katherine Steinberg, MPP, health innovators with deep expertise in geriatrics and care transformation, have developed a new platform to address loneliness and other critical social determinants of health. Their approach leverages digital technology to deliver datadriven and scalable solutions while keeping authentic human connection front and center.
WWithin the Healthy Longevity & Aging
Moonshot, we often write about the simplebut-profound math of changing demographics and our aging population. By 2030, a quarter of the US population will be over 65, approaching the first time in history that there will be more people over the age of 65 than under 18. Meanwhile, something on the order of 40% of healthcare dollars are spent on people over 65.
As a physician specializing in geriatric medicine, and through a career leading
care innovation efforts, these demographic realities have always been front of mind for Determined Health co-founder, Dr. Scott Kaiser. Anticipating the needs of an aging population, Dr. Kaiser points out that “if you consider the many things that influence how people age, social connectivity stands out as one of the most profoundly impactful, and potentially modifiable, factors.”
Not only do loneliness and social isolation have devastating impacts upon health and wellbeing — with research indicating adverse health effects equivalent to smoking 15 cigarettes per day — but they are key cost drivers as well. Social isolation is associated with increased risks of emergency department visits, hospitalization, nursing home placement, and conditions such as dementia (50% increased risk) that bear a devastating human and economic toll. By one AARP analysis, $6.7B in annual Medicare spending alone is attributable to isolation.
What this all amounts to is the somewhat shocking realization that one of the greatest predictors of poor health, functional decline, and even premature mortality for older adults is something clinical teams may be overlooking all together. Loneliness and social isolation aren’t tangential to health; social connection is primary.
To quote US Surgeon General Dr. Vivek Murthy, “It is more important than ever that we rethink and harness the power of relationships and recognize that they are not just nice to have but they are necessary to have.” Kaiser, along with Determined
25% Percentage of the US population that will be over 65 years old by the year 2030
40% Percentage of US healthcare dollars spent on people over 65 years old
Health co-founder Katherine Steinberg, MPP, MBA — a seasoned healthcare transformation and innovation specialist — heeded this call, setting out to create new tools to combat the loneliness epidemic across diverse communities and bringing social connection into the core of high-quality care.
Incubated within a 100-year-old nonprofit, the Motion Picture & Television Fund (MPTF) — which supports members of the entertainment community, including 60,000+ entertainment industry retirees — Determined Health was born out of a community of storytellers. And in true Hollywood form, the Determined
Health origin story brings together a passionate cast of characters, introducing a steady flow of existential threats (a global pandemic, for example), as they set out on a quest to overcome seemingly insurmountable challenges. Enter Kaiser and Steinberg, healthcare innovators, determined to reimagine aging and transform care.
Appreciating the degree to which healthcare all too often may be “shooting at the wrong target, overlooking the nonclinical factors that so profoundly drive outcomes,” Kaiser and Steinberg aligned to found Determined Health, with the conviction that “everyone deserves access to personalized, high-quality, well-coordinated care — supported by a team that understands them and their values.”
Eager to develop and scale the impact of the most promising innovations in geriatric care and population health, the duo drew key insights from their work at MPTF that they believed could provide the seeds of such transformation. In particular, seeing the profound impact of MPTF’s nationally recognized social call program — developed under Kaiser’s leadership with the support of AARP — they set out to better understand what made this approach so successful. The key differentiator of the approach was prioritizing human-to-human connection first and foremost. The calls weren’t automated, the volunteers weren’t running down a checklist or doing surveys to determine healthcare needs. Instead the goal was to have a friendly, engaging conversation, with the person on the receiving end of
the call driving that conversation.
Kaiser and Steinberg leveraged a grant from The Eisner Foundation to build a prototype for a social connection platform. Their Connection1st CallHub platform was designed to facilitate connections between people, safely and easily. Those two priorities — ease and safety — meant they wanted the platform to meet the users where they were in terms of technology by using ordinary phone calls, and it meant de-risking the platform by protecting people’s privacy and routing all calls through a trusted phone number. This was especially important for the older population with whom they were working, often the target of phone scams and fraud.
Fueled by an urgent need to combat isolation exacerbated by the pandemic, Kaiser and Steinberg were approached by organizations across the country to use their platform. This beta testing fueled the iterative development of a platform forged by real-world demand and directly meeting the needs of key end-users. Through this process, the Determined Health team not only found an effective solution to reduce social isolation, loneliness, anxiety, and depression, but recognized that these calls could prove to be the key entry point to influence overall health and wellbeing. Once again, the secret ingredient: creating genuine connections and building trust.
The driving insight, and in a way an ode to their Hollywood heritage, Steinberg points out, “when you’re able to connect with someone and build trust, getting to know their unique story, understanding
them and appreciating what really moves them, you can develop meaningful engagement as a powerful force to positively influence health and wellbeing” This type of engagement is often the missing ingredient, especially when it comes to identifying and addressing unmet needs and filling critical care gaps. As Kaiser explains, “We’ve seen countless examples where, despite robust screenings, real needs are still going undetected. Then, through friendly calls with simple conversations about sports, movies, etc. people begin to confide, sharing their deepest concerns, like ‘I just don’t know what to do, it’s the end of the month and I’m going to have to choose where to cut back, food or medicine.’ With this, the full picture begins to emerge and we’re able to route this critical information back to the care team to intervene.”
At its core, Determined Health exists to form meaningful connections between people and between organizations to create the best possible care for older adults. They leverage community-partnered networks to drive engagement and reach high-risk, high-need populations.
“There are just too many gaps people are getting lost in,” says Steinberg. “We work with Community Based Organizations (CBOs), health systems, and health plans to bridge these gaps and provide a stronger ecosystem of care.”
Let’s say a health plan wants to address more social determinants of health (SDoH) among its members. Health
plans don’t tend to have established volunteer networks that can reach out to their populations, but by partnering with Determined Health, they can create and train a network of volunteers through CBOs who can then reach out to folks, make calls, collect data, and most importantly, create trusted points of connection that identify needs all while reducing loneliness and its related health issues.
This partnership approach helps leverage new resources for a community. For example, one of Determined Health’s initial partners is Meals on Wheels. If a health plan partnered with the MoW volunteer network for these calls, they might identify people in need of regular meal services. Thanks to Determined Health’s safe, HIPAA-compliant platform, these different types of organizations can be married together to meet the needs of a shared population.
The person behind the technology to make this all possible is Charles Johnson II, Determined Health’s third co-founder. Johnson came from a more consumerfocused space but was won over by the mission-driven culture and determination to take on the biggest challenges in healthcare and solve them.
Johnson shaped the tech driving Determined Health to be almost invisible to the end user receiving the phone call, keeping the focus on the connection with another person. It’s a backwards-compatible approach, so that anyone comfortable using a phone can have the same access to resources as someone more comfortable with digital apps. This layered method
lets them reach more people, particularly those at highest risk of isolation.
Their approach to technology mirrors their approach to care. Start with a simple phone call and build out analytic systems and interventions from there. Start with the connection first, and then as trust builds, the opportunities to assess health, coordinate care, and provide specialized medical help emerge. Determined Health flips the stack so that the person receiving care remains the focal point. It’s person-centered care born out of a real relationship, with a real person, and not just tacked on to an existing care model.
This past year, Determined Health built out its version 2 platform, signed deals with health plans and systems, and was awarded a Phase 1 SBIR grant to develop tools for people with dementia. As they head into autumn, they are looking to raise funds for commercial expansion in 2023 and to create virtual tools for the $39B dementia care space.
“We are going to have more people over the age of 65 than under the age of 18 for the first time in history,” says Kaiser. “This presents a great opportunity but we have to be aware of the challenges. We’re thinking big about how to meet the needs of this aging population, but starting small, with the individual. We want to know each person well with a broad base of connectivity and then layer on care so that people can live better and age better.”
StartUp Health is thrilled to welcome Determined Health to our family of
global entrepreneurs for several reasons. By combining Dr. Kaiser and Steinberg’s deep health innovation expertise with Johnson’s consumer-focused tech experience, Determined Health is poised to meet the problem of loneliness with know-how and agility.
We’re also proud to invest because the solution Determined Health offers has already proven itself nimble, able to adapt to the needs of different populations across varied environments. Whether being utilized by community-based organizations, health systems, or health plans — from Hawaii to Maine — its emphasis on community partnerships means it maximizes resources that already exist in a community, instead of having to build from the ground up every time. It easily scales up or down so it’s as useful to a small community as it is to a large health system.
Finally, we’re proud to back Determined Health because of how they put people front and center. This is authentic, personcentered care that understands the power of relationship. From its simple design that allows anyone who can answer a phone call to participate, to the time spent building trust, to the customized care solutions it provides, Determined Health always comes back to the simple and transformative idea of building human connections.
contact:
determined@startuphealth.com

Co-founders Joachim Ehis Okojie, BDS, and Chukwuebuka
Anyaeji, BDS, have built an “infrastructure-as-a-service” company that helps newly-minted dentists get their careers launched while providing high-quality, lower-cost care to patients.

Five years ago, Joachim Ehis Okojie and Chukwuebuka
Anyaeji were freshly-minted dentists, graduates of the prestigious University of Lagos in Nigeria. Like any new dentists, they were eager to get their practices up and running. After their years of study and training, it was time to get to work.
Easier said than done. Setting up a dental practice is a huge cost, no matter where in the world you do it. Between X-ray machines, administrative staff, equipment, dental chairs, and the like, even a small practice sets a dentist back a formidable sum of money. In Nigeria, there is limited access to financing so a new dentist ends up joining an established practice or working in a government facility because they can’t secure a loan for their own practice.
And then there’s a matter of gaining patients. Although the dental industry in Nigeria is majorly understaffed (one estimate puts it at one dentist to 148,000 Nigerians), dental facilities struggle to fill their appointments.
“In this part of the world,” Dr. Okojie explains, “people don’t see the value in attending dental clinics. When you look deeper at the issue, you see that part of the reason is cost.”
The average cost of a routine dental appointment in Lagos, with X-rays, cleaning, and checkup, comes to the equivalent of about $150. Compared to the average income for someone in Lagos, this cost sits higher than many people can afford. Even if they can afford it, there’s also an educational aspect to getting a population on
board with regular dental care.
“Understanding the need is a huge part of the equation as well,” Dr. Okojie says.
Not only does regular dental care save huge costs down the road in terms of preventing cavities and the need for emergency treatments, but research suggests strong connections between oral health and overall health. Gum disease, for example, is associated with heart disease, diabetes, respiratory conditions, and more recently, Alzheimer’s disease. Changing a population’s view of dentistry and increasing their access to care impacts far more than their smiles.
In the beginning of 2020, Drs. Anyaeji and Okojie started to discuss how to improve access to regular dental care in Nigeria. What do you do when you have a grossly underserved population, dentists who can’t afford to set up their own practices, and existing dental practices who can’t fill up their appointment slots because of cost issues?
They came to a beautifully simple answer: if you can leverage the facilities that already exist, a new dentist could rent space in an established practice to build up his or her own practice. It’s tapping into the gig economy for dentists. It drives costs down for the patients because the dentist isn’t paying off the entire cost of setting up a space, allowing the dentists to attract clients who might otherwise wait to see a dentist until a serious problem arises.
The partners scraped together enough funds to set up an initial branch to test
Although the dental industry in Nigeria is understaffed (about one dentist to 148,000 Nigerians), dental facilities struggle to fill their appointments.

their idea. In 2021, they opened Yanga — a one-chair facility with X-ray capacity and a front desk administrator. Dentists simply booked a time slot, walked in, and had everything they needed to care for their patients. In exchange, the dentists paid a percentage of what they earned.
The experiment worked. The Yanga Dental Clinic grew from one chair to three chairs, with 53 dentists regularly using the facility to see patients. On any given day, six to eight dentists come into Yanga, building their clientele and establishing their own practices.
“We built it into a full service one-stop shop. In the past 17 months, the clinic has seen 1,600 patients.”
To get started at Yanga, a dentist signs
up to join on their website and pays a very low annual fee (the equivalent of about $10). They then receive access to a personalized booking page where they can list the services they offer and the cost. Patients book through the website and come to the Yanga facility for treatment. Patients pay at the Yanga front desk, or Yanga bills their insurance, and Yanga pays the dentists at the end of each business day after taking a small percentage of the bill.
A few factors are fueling Yanga’s success and shaping their roadmap for the future. First, while they don’t set the fees for the dentists using the space, they strongly encourage them to charge within certain ranges to keep the price accessible to patients. Yanga keeps the annual subscription fee they charge the dentists low, to help them pass on the savings to clients.
Additionally, they’ve focused on marketing to help Yanga dentists acquire new patients. Their Instagram feed, for example, educates consumers on the benefits of regular dental care with vibrant, culturallyrelevant posts. Part of their aim with these posts is to alleviate people’s dread of going to the dentist, even make it fun. The term “yanga” is the equivalent of strutting your stuff, and they encourage their clientele to enjoy flaunting their smiles.
In the past year, Yanga established partnerships with several major HMOs, including Reliance, Leadway Health, and Hygeia. Not only does this help the dentists with patient acquisition, but the Yanga administrator also takes on the headache of filing and settling claims for the dentists, further simplifying the process of getting a new practice up and running. They’ve also built relationships with pharmacies in the city, so that pharmacists can refer people with tooth complaints to Yanga for affordable care.
Currently, the Yanga team is building out the tech side of the business so it becomes an end-to-end solution for both dentists and patients. The Yanga app allows patients to schedule appointments and pay bills and dentists to set up their schedule and a virtual wallet to receive payments. It also will enable Yanga to expand its services across Lagos, the biggest city in Africa, and beyond to more remote parts of the country, as well as across West Africa.
“We’re optimistic about the model. We’ve seen that it works. And now we have a lot of requests from different cities. We want to increase access to dental care for
all of Nigeria, starting in Lagos and going everywhere.”
Yanga has created a healthcare infrastructure service that taps into existing resources to provide affordable dental care. We’re proud to back this smart approach that harnesses the gig economy to drive down costs for the consumer, while providing dentists the space and tools they need to work. They’ve proven that it works, and they’ve set themselves up well with a vision and team to expand their approach.
If the eyes are windows to the soul, the mouth is a window into the overall health and wellbeing of a body. We believe that prioritizing dental health has far-reaching effects, and Yanga is doing amazing work to normalize routine dental care and oral hygiene in West Africa. Their marketing and messaging communicates the benefits of taking care of teeth clearly and respectfully. It’s a thoughtful and effective approach that is helping them create a new consumer base in Lagos.
We’re excited to see how the app they’re developing allows their dentistry model to travel to other parts of Nigeria and West Africa, especially remote areas that are underserved. As they continue to build partnerships with HMOs and health insurance companies, they can expand their reach and set up clinics where they are needed most. It’s a big challenge but one Yanga is ready to sink its teeth into.
contact:
yanga@startuphealth.com
By focusing on the specific mental and emotional needs of healthcare professionals, Vitalize Care creates a more equitable and positive experience for both healer and patient.
RRecent surveys suggest that 60% of healthcare workers feel burnt out, making it three times more likely that critical errors will occur when treating patients. Because of this paradigm, greater than 30% of healthcare workers currently on the job plan to leave in two to three years, costing the US healthcare system over $60B annually. A good deal of that financial investment goes into replacing staff, training, and other ancillary costs.

But there is more than money being lost with the revolving door of medical professionals due to mental health concerns. A successful healthcare system relies on having the staff to provide appropriate care to patients. As turnover rates rise and experienced, trained professionals continue leaving due to burnout, there aren’t enough clinicians to address patient needs. Workloads haven’t lessened; the number of staff available to deal with it has. That means fewer trained professionals bearing an already overwhelming workload.
While most hospitals offer employee assistance programs, their engagement rates are less than 5% for a few key reasons: 1) They are understaffed, resulting in long wait-times and complicated onboarding processes; 2) they are highly stigmatized as participating can jeopardize their careers; and 3) they are focused solely on one-onone therapy and lack peer support.
On the other hand, existing digital solutions such as mindfulness apps don’t address the unique experiences clinicians face on a daily basis — loss of a patient, medical errors, traumatic emergency room experiences, etc.
Overworked and overburdened medical professionals are experiencing life-altering mental health challenges that are proving fatal. There is a critical shortage of clinicians due to emotional distress; creating a more equitable way to address the specific and unique stressors healthcare workers face every day is key.
Vitalize Care plans to unlock that muchneeded, targeted access.
30%
Percentage of US healthcare workers who plan to leave their jobs in the next 2-3 years
$60B
Added cost to the US healthcare system created by rapid workforce turnover
During his freshman year at the University of Maryland, Vitalize Care cofounder Veeraj Shah discovered he and his peers had no idea how to find on-campus healthcare information, so he created Chat Health, a chatbot system that provided students everything they needed to navigate the university-based healthcare system.
As Chat Health grew, Veeraj became more interested in the intersection of health and technology so he joined a startup incubator. There he met Sanketh Andhavarapu, founder of a tutoring program geared to a student’s specific needs. Sanketh aspired to be a patient caregiver,
spending hundreds of hours working as a volunteer and medical assistant in a variety of clinical settings during school. The two immediately found themselves standing in front of a whiteboard together, coming up with ideas on how to heal an ailing healthcare system, building upon the concept of lived-experience engagement.
Veeraj and Sanketh had both witnessed how healthcare providers were emotionally exhausted, increasingly disconnected from their patients, and losing their sense of purpose. So they dived into the clinician mental health space. Veeraj collaborated with the US Surgeon General on mental health initiatives for the healthcare workforce and led research in behavioral health funded by the Bill & Melinda Gates Foundation. Sanketh conducted research on how burnout leads to more medical errors and published the largest study on PTSD rates among healthcare workers during the COVID-19 pandemic. This led them to the mutual finding that mental wellness options available to clinicians in need of mental health support were not proving very effective.
They started talking to as many healthcare workers as they could to better understand the disconnect between the kind of help providers needed and the mental healthcare available. From talking to over 200 healthcare workers, Veeraj and Sanketh landed on several key insights. Seeking help within a peer-group environment — openly sharing what they were feeling and facing with coworkers — was proving uncomfortable and difficult
for many healthcare professionals who already carried shame from the situations that led to their mental and emotional difficulties. Engaging in programs led by mental health professionals also left clinicians wanting as the care physicians were not experienced in dealing with their specific needs, therefore making it difficult to address them properly. Similarly, digital mindfulness and mental wellness solutions — while anonymous and easily accessible — dealt with issues on a broader level, once again not getting to the crux of the problems clinicians face on a daily basis, and creating a mental wellness void in the process.
Healthcare workers were seeking accessible mental health support led by those who had been through the same experiences but without it putting them at risk, shaming them, or making them feel overlooked. With a panel of 50 clinicians, the two began co-designing a digital platform that provided specifically-targeted mental health support from different healthcare workers. Users could choose anonymity while dealing with topics and situations that resonated with them, by working with someone who knew what they were going through and had been in the trenches.
As Veeraj says, “Technology works when it meets the users where they are, and they can use it without fundamentally changing their behavior.”
The two co-founders knew they had to build a user-friendly solution to bring mental wellbeing to healthcare workers on a platform that is easily accessible,
engages them in a way that makes them feel they are being heard and their unique needs are recognized, and gets them the mental health support they need when they need it. Fall of 2021 saw the Vitalize Care platform ideated and designed, and the first hospitals approached them to pilot the project. To do that, they knew they needed a strong development mind to bring it to fruition.
In February 2022, Nikhil D’Souza joined the duo and the three co-founders started fully developing Vitalize into a functioning business. Nikhil was part of the team that created Vincere Health — a “quit smoking and get paid” digital platform that successfully completed the United Healthcare Techstars accelerator and raised a seed round — and was entrenched in researching clinical trial effectiveness at Eli Lilly and Company, among other things. Already steeped in bringing new medicines to market and providing quality healthcare to all via the digital space, Nikhil’s know-how and expertise in utilizing technology to bridge the healthcare gap provided an opportunity to better understand and address how to take Vitalize from design to a functioning website and mobile application. By the spring of 2022, the interface was built, and the first pilot hospital was onboarded.
The core feature of Vitalize Care is group coaching for healthcare workers. Through the mobile app, healthcare workers connect via a live coaching session with peers who share their experi-
ences. The coaches are clinicians who have been in the shoes of those seeking support — they are physicians and nurses who became health coaches because they were passionate about holistic care. Each has a certificate in health and wellness coaching in addition to their personal experience as healthcare workers.
Conducted like a Zoom session, coaches keep their cameras on but those seeking assistance can protect their identity by changing their username, turning off their camera, and even altering their voice. Coaching is geared specifically to the needs of the healthcare professional, and those seeking assistance can choose from sessions that resonate with what they are going through at any given time. There are several opportunities to engage throughout the day for easy access at a clinician’s convenience.
The live group coaching is complemented by other features to ensure a comprehensive and holistic mental health journey. The app offers text-based peer support, which allows healthcare workers to connect with others dealing with their same issues, again anonymously with their identity protected. Healthcare workers can also access on-demand content such as guided meditation and tools to build mindfulness and positive psychology skills to complement the live features. The holistic approach assists with grief management and to help build resilience when faced with unexpected situations and mental health challenges.
For healthcare employers, Vitalize offers data and analytics on staff mental
health and app engagement to help organizational leadership better understand how to support their staff. This can reduce burnout that will lower attrition rates and keep the cost of replacing, training, and acclimating staff down while also supporting a healthy, happy workforce.
Vitalize Care is a young company with young founders, which we see as a distinct advantage in this category. They bring a fresh perspective to what has long been a stigmatized and overlooked category: mental health for healthcare workers. In their experience developing Vitalize, Veeraj and Sanketh have discovered that there is a generational divide. Younger physicians and nurses are deeply aware that the stigma attached to the label of poor mental wellness simply means it’s necessary to discuss it openly to remove the shame and get people the help they need. This awareness is slowly having what they view as a ripple effect on how hospitals and healthcare systems react and even how funding is allocated to mental health. The traditional mindset that physicians and care workers should be able to handle anything because they have been trained to do so is not seen as viable by the younger generation coming in. The standard of self-maintenance is only attainable by a few people and it’s not realistic.
Vitalize Care recognizes this and is getting in front of it to support a space for more holistic and equitable care for those who are given the job of caring for
all of us. The Vitalize team is committed to building something that clinicians can trust. They already have products in the pipeline that will engage thousands of healthcare workers through selling to hospitals and health systems, healthcare staffing and digital health companies, and state and national medical societies. They foresee a complete overhaul of the healthcare system within a decade or two because the clinicians who are young now — those leading the charge for such things as making COVID-19 vaccines available to all — will soon be the ones making decisions in the medical industry. Vitalize intends to be there at the forefront. They have already brought on board their first paying health system and have several more in the pipeline for the upcoming months.
We’re proud to back Vitalize because they plan to not only focus on the individual drivers of burnout and mental unrest but the roots and causes of both; they will continue developing solutions for the systemic changes needed. That deep dive has the potential of creating avenues for care that will boost the wellbeing of current medical workers while also energizing and attracting the new generation of clinicians.
contact:
vitalize@startuphealth.com
MENTAL HEALTH & HAPPINESS
CEO & Founder Rob Stephenson funneled his mental health journey into an app and platform that’s helping people articulate their wellbeing, so they can get support from their employer and friends when they need it.

We’ve become accustomed to answering this all-too-familiar question. Our responses might vary from a superficial “good,” to a slightly more honest “tired,” but if we’re being completely transparent, we rarely answer the greeting with the whole truth. Why?
We’ve made checking in with how we feel too casual. We’ve become desensitized to the question “How are you?” We flip through our leaflet of socially acceptable
responses, pick one, and move on, rarely taking stock of our mental wellbeing.
Sometimes it’s difficult to come to terms with our mental state and even more difficult to share it with the people around us. Without oversharing in a casual conversation, how do we communicate the truth about how we are feeling?
How powerful would it be if our daily “how are you” check-ins were honest? What if there were a simple way to communicate our daily wellbeing with the people we hang out with or work with–and even ourselves–without having to unpack our latest therapy session?
It might seem like a micro solution to the massive mental health crisis in the United States, but according to Rob Stephenson, the practice of checking in about our mental state has huge ramifications for our workplaces, our homes, and our lives.
Rob Stephenson founded FormScore after receiving advice from his physiotherapist on how to manage his challenges with bipolar disorder.
“Alongside therapy and medication, a particular therapist gave me the idea of tracking my mood using a score out of ten,” says Stephenson. “I found this really helpful because what it did was help me build up the awareness of what proactively, positively drives my wellness.”
For years Stephenson tracked his daily wellness in his head, a diary, or a spreadsheet, never sharing with anyone outside of his close circle of family and friends
how he was working on his mental health. It wasn’t until 2017 when he noticed a change in the social stigma of mental health that he decided to share his story with others about struggling with bipolar.
“When I shared my story, I got a huge number of people sharing their stories back,” says Stephenson. “I started to understand how many people experience a mental health challenge but do so in silence because of the stigma.”
This realization that people had a real desire to share how they were feeling with others inspired Stephenson to become a campaigner for improving mental health in workplaces and communities. Stephenson’s initial effort was to create a nonprofit dedicated to eliminating mental health stigma in the workplace. He delivered keynotes and TED Talks on the subject for years before deciding to share his personal “mental health score” with an audience.
The reaction was overwhelmingly positive. Audience members jumped at the opportunity to score themselves on a scale of one to ten and share it as well. This led Stephenson to sharing his daily score in his email signature and in LinkedIn posts.
“I’d get comments like, ‘I really like getting an email from you Rob because I want to know what your score is today.’”
Stephenson began getting email responses and comments from people sharing their daily scores as well. It was then that he realized that people want to share how they’re feeling, they just needed a simple, effective way to do so. Thus, FormScore was born.
FormScore is a workplace wellbeing platform that helps individuals better manage their own wellbeing and support their loved ones and provides employers with anonymized wellbeing insights and analytics.
Employees can engage with FormScore via an app, a browser plug-in, and forthcoming MS Teams and Slack integrations. The methodology is designed to get to the root of how users are actually feeling. The platform is designed around a simple, daily question: “How are you feeling?” Users answer with a number system — 10 being the best form and 1 being the lowest.
FormScore encourages users to reflect on a number of specific questions to provide a deeper understanding of their general wellbeing. “Have I slept well recently?” “How purposeful do I feel?” Mulling over one’s healthy habits, sense of purpose, community connection, and stressors help users determine their daily score.
Once a person determines their daily score, it can be shared with friends, family, and trusted colleagues who also use the app. The goal is not only to get the user to check in with themselves daily, but to provide them with a support system.
“We’re not trying to be big social media here,” Stephenson says. “We’re trying to facilitate a small group of connections of networks of support with people that care about each other.”
When a user’s score is low, the hope is that their selected FormScore community will reach out and check in. This check-in might look like sending a song or an en-
couraging word to lift their spirits. On the opposite end of the spectrum, when someone’s FormScore is super high, the hope is still the same: that an acknowledgement of how someone feels will create greater connections.
FormScore has taken this community support between friends and family members and stretched honesty about mental wellbeing into the workplace.
At the employer level, the FormScore solution is all about providing anonymous wellbeing data, giving line managers and wellbeing leaders real-time actionable insights into how their people are doing in aggregate terms. For example, if a team’s score is trending down compared to the organization due to “work” and “stress” then it could give managers the inspiration to look at workloads and resource allocation to see if unrealistic deadlines are affecting the wellbeing of the team.
The FormScore team have exciting plans to cross reference wellbeing data with productivity and employee engagement whilst overlaying company events and ways of working. This will then create valuable insights for both the employee and the employer and demonstrate the link between performance and investment in wellbeing. For example, suppose a business is going through a merger. It will be possible to demonstrate the impact of the transaction on wellbeing, how engaged employees are, and how productive they are.
At the heart of FormScore is an intentionality born from Rob’s own experience.
His openness with sharing his personal journey with bipolar disorder and healing has equipped him to lead a movement about intentional sharing when it comes to mental health. StartUp Health is proud to back FormScore, because Rob’s leadership is breaking down decades of stigma.
We’re also proud to invest in FormScore because while the concept of performing a daily wellness check-in might seem simple, its results can be profound. We all know that behind that “how are you feeling?” is an honest answer that wants to be expressed. FormScore’s simple premise has
the ability to strip away the excess and focus on what’s most essential.
Finally, StartUp Health is proud to back FormScore because of its success to date. Not only has FormScore secured pre-seed funding to grow its team, it’s also proven to have an impact on wellness over time. In a study conducted with Amey Consulting, FormScore improved workplace wellbeing by 7% over the course of 12 weeks.
contact: formscore@startuphealth.com
SOMOS Is Expanding Genetic Data in Latin America While Serving Indigenous Populations in an Equitable Way
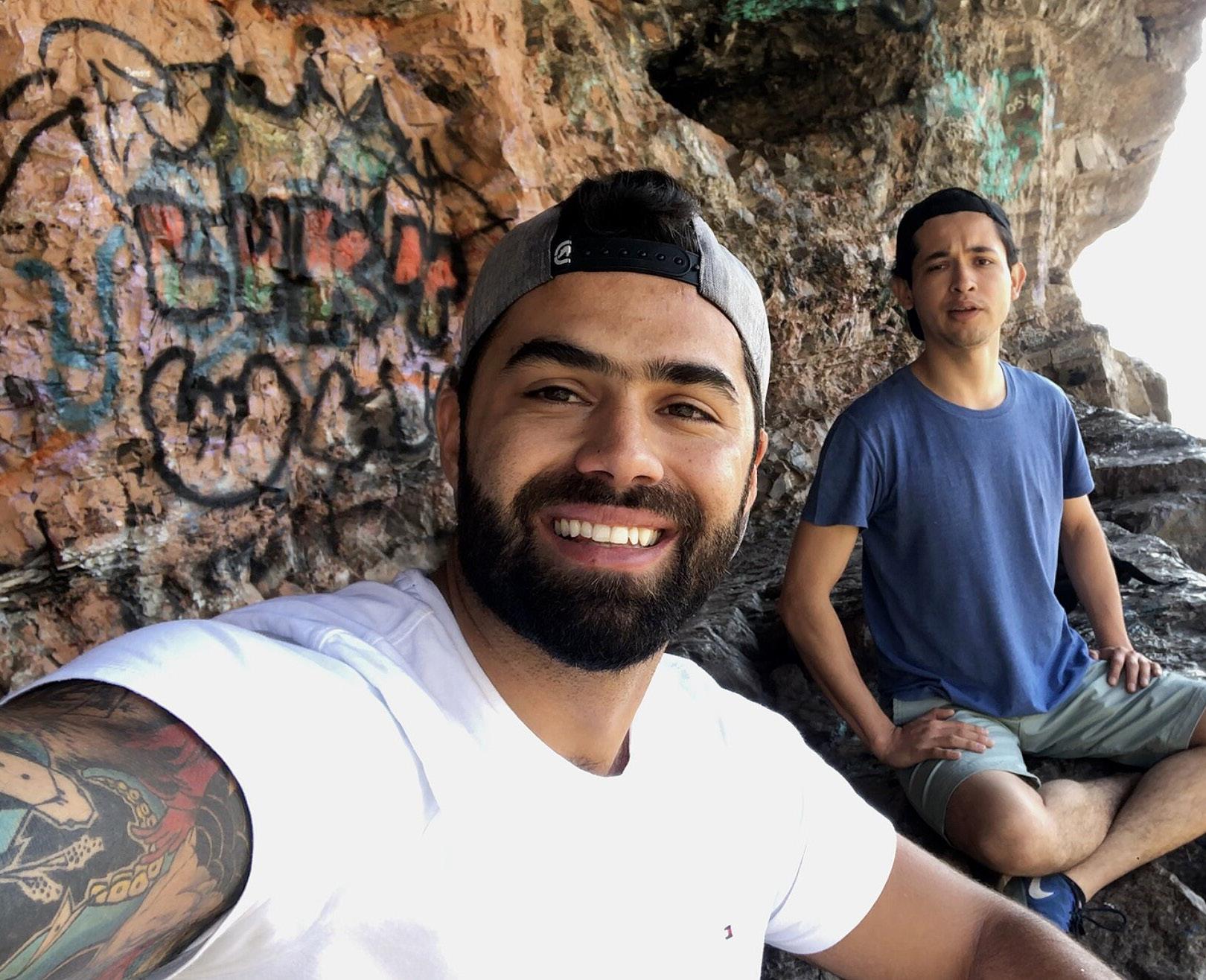
Co-founders Federico von Son and Christian Rodriguez – both medical doctors trained in Mexico – are building “23andMe for Latin America” with a twist. They’re putting boots on the ground to make sure that native communities across Latin America are represented, and then fairly compensated for their participation in the biobank.
FFor years we’ve heard about the promise of precision medicine, driven by a revolution in genetic data. This year Wired magazine declared that “the era of fast, cheap genome sequencing is here,” thanks in part to technology companies driving the cost well below $500. Companies like 23andMe and Ancestry. com brought this world to consumers by the tens of millions, normalizing conversation about genetic health risks.
However, genetic testing has a diversity problem. It’s well documented that when researchers study large populations to connect genetics with disease prevalence, they primarily look at populations of European ancestry. It’s not surprising: it’s cheaper and faster to work with the genetic data that’s readily available.
One prime example of this is the lack of detailed genetic data available within the Latin American population. This lack of diversity isn’t a political or social issue so much as a medical problem. When a pharmaceutical company creates a drug or
dosing regimen based on one population’s genetic data, they run the risk of over or under prescribing that drug for millions of people. Whether its blood thinners or cancer treatments, examples abound of specific Latin American populations metabolizing drugs faster or slower than the general population, putting people at unnecessary risk.
Genetic testing opened up the world to precision medicine. Now it’s time to see the world as diverse as it is, and create drugs and therapies suited to unique populations. In Latin America, that’s going to require a targeted, concerted effort to bring new communities into the fold. It’s going to require a company to see Latin America as its own ultra-diverse patchwork of communities, not a genetic monolith.
This is precisely where SOMOS has placed itself in the market. It offers genetic testing geared towards the Latin American market, with a specific eye on cultivating diverse biobank data from indigenous populations in a culturally responsible way.
While Federico von Son was training as a physician in Mexico, he noticed a problem. He was being asked to care for Mexican patients based on research that had little to do with the patient population in front of him.
“I really got very concerned because I identified that the genetic markers that were over-represented in other regions, like Europe or Asia, weren’t represented in
Latinos,” says Dr. von Son. “So how could it make sense to continue giving a drug that’s not metabolized the right way in the Mexican population?”
So Dr. von Son decided to improve the amount of available genetic data in Mexico. He started a direct-to-consumer genetic testing company and he and his team trained more than 500 healthcare professionals to conduct and utilize genetic testing in their practices. That process unearthed a deeper problem, and sparked Federico’s next endeavor. Genetic testing was simply too expensive to get the necessary diversity across Latin America. And without that diversity, patients would continue to be benchmarked against populations on other continents.
To solve this issue, Dr. von Son teamed up with fellow physician Dr. Christian Rodriquez and founded SOMOS. They’re taking a two-prong approach to improve genetic testing in Latin America. The first is to do the labor intensive field work of gathering genetic data from indigenous communities in Mexico and across Latin America. The second is to market in-depth Latin American genetic data to consumers in the United States.
“We started to tell people about their percentage of Aztec or Mayan heritage,” says Dr. von Son, who has an eye towards the Los Angeles market. “People get really excited about this information.”
SOMOS launched in the United States in September 2020. They invested in building their algorithm and the platform, and then COVID-19 hit and put a lot of projects on hold. But their direct-to-
consumer product met an eager market in the United States and helped them stay on track. Their next goal is to hit 50,000 users and then begin meaningful conversations with the pharma industry.
SOMOS is currently raising a round to collect data first from Mexico (which represents about 25% of the genetic diversity of the continent). The money will be used to collect 7,000 genetic samples from 70 indigenous groups, creating “the largest indigenous biobank in history.” More importantly, says Dr. von Son, it’ll be a centralized biobank, since SOMOS is working off of blockchain technology.
In order to gather genetic data that’s never been collected before, SOMOS is collaborating with the Mexican government to reach often-isolated indigenous communities. They’re also establishing methods for making sure these communities are remunerated for their participation.
“When I started collecting samples from indigenous communities, I realized how easy it would be for unethical organizations in the same space to take advantage of people’s trust,” says Dr. von Son. “I realized that we needed to use technology to build a strong, transparent relationship with these communities. We started using blockchain technology so that we could invite them to participate in the biobank, but at the same time establish a transparent line of communicating and remunerating the community.”
“We don’t own the data,” adds Dr. von
Son. “We want to be the AirBnB or the Uber of genetic data. We want to be the highway for accessing the data. We don’t need to own it.”
Building that trusted line of communication starts with coming into the community with humility, sharing a meal with someone and getting permission from the right community leaders. It means understanding that particular community’s needs. Sometimes those needs are acute, says Dr. von Son, like a lack of clean water or medicine, and SOMOS has been able to serve in these critical ways while also partnering on genetic testing.
The work that SOMOS is doing gathering genetic data from hard-to-reach Mexican communities has given them a deeper understanding of Latin American genetics, which they’ve turned into a consumer product targeted towards Latin Americans in the United States. To date they’ve analyzed genetic data for around 6,000 people, including folks who have taken a 23andMe or Ancestry.com test but want deeper data on their Latin American heritage.
SOMOS currently operates in Mexico and the United States, with plans to replicate their model in other Latin American countries. With five additional countries after Mexico, Dr. von Son estimates that SOMOS would cover 80% of indigenous groups in Latin America.
While there are certainly other companies hoping to be the “23andMe for Latin America” — not the least of which
is 23andMe itself — we’re proud to back Dr. Fererico von son, Dr. Christian Rogriguez, and the SOMOS team for a number of reasons.
First, they’re thinking holistically about Mexican and Latin American genetics. Rather than focus on higher-income consumers in big cities who are on the leading edge of genetic testing, they’re getting out in the community, making sure that a range of population groups are represented, so that future drugs and treatments work for everyone.
They’re also thinking equitably. Core to the SOMOS mission is the idea that indigenous communities should own their own genetic data, and that they should profit from it if and when it becomes marketable to the healthcare industry. They’re accomplishing this through blockchain technology that makes data ownership transparent and verifiable.
Finally, we’re excited to back SOMOS because they’re ushering in the next phase of personalized medicine. The health innovation industry has proven that we can use individualized health data to tailor treatments and improve outcomes. That was step one on the innovation curve. The next step is to scale this innovation by going deeper in the data we leverage. Startups like SOMOS are absolutely essential in this work and will open up amazing opportunities within the massive Latin American market.
contact:
somos@startuphealth.com

Robert Condon spent his career traveling the world to establish some of the first mobile phone networks. Now he’s leveraging that know-how to create a telecare infrastructure that can provide access to affordable primary healthcare to underserved global emerging markets.
AAs we’ve often said at StartUp Health, you can develop all the health tech in the world, but if people can’t access it, we’re not going to move the needle on health. Today, millions of people globally still lack access to high-quality primary healthcare for financial and geographic reasons. According to the World Health Organization (WHO), 40% of its 194 member states have fewer than 10 medical doctors per 10,000 people; some report only having three physicians. These medical professionals show up in rural areas so infrequently as to make it virtually impossible for many to plan for these visits, and in times of emergency, gaining access to care means traveling long distances only to then pay exorbitant costs. This makes in-person care not only an unaffordable luxury but a rarity, leaving wellness left to chance and ailments unchecked in vast pockets of the world’s population.
Through smartphones and digital mobile networks, we have the technology needed to bring high-quality, virtual healthcare services to remote communities. However, there are cultural barriers as well. In-person visits are the norm — al-
beit infrequent and often expensive — and getting entire populations to embrace receiving healthcare through a digital device can be a challenge.
How can a startup build the network infrastructures necessary for low-cost, high-quality virtual healthcare while simultaneously changing the culture of healthcare, educating the community, and helping populations acclimate to the tools and workflows of virtual care?
That’s just the question Robert Condon set out to address with Esprit Health.
Robert Condon is a pioneer of the international telecom industry. He spent decades traversing the globe establishing cellular networks and telecom platforms for some of the world’s largest telecommunications companies. Much of that time was spent building the first mobile networks in remote places – like China, which taught him two lasting lessons. The first was the power of bringing digital mobile access to the world. The second was the reality of the inequities that persist in remote and low-income regions.
His experience also taught him that while there could be initial cultural barriers to accepting mobile networks in a region unfamiliar with the technology, once accepted, these communities often experienced a leapfrog effect. Because they often lacked other supportive infrastructure, these under-resourced communities jumped at the opportunity to conduct every possible transaction via their new mobile device. Not only could they now communicate with loved ones all over the world, but with the digital wallet, they
could send money to family members, and access the Internet for e-commerce, news, and entertainment. Quite simply, the smartphone has become the de facto means of communication for most people in emerging markets.
As this concept of a “digital wallet” matured, Condon spotted an exciting opportunity for it to have a deeper impact on the world. What if he could use this new technology and his decades of experience in implementing mobile networks to leverage mobile infrastructure and deliver accessible, affordable, digital health in emerging markets via an m-health platform and “Health Wallet”?
The final tipping point was COVID-19. When it swept the globe, the need for accessible, affordable virtual healthcare moved from a benefit to a necessity. The spark for Esprit Health was lit. He formed a team and began building his platform, focusing first on East Africa.
Esprit Health’s new platform connects customers to medical, pharmaceutical, and insurance services. They have developed what they call an m-Health or Mobile Health platform to deploy in partnership with Mobile Network Operators (MNOs) taking advantage of their distribution channels. By creating the Digital Health Wallet, Esprit utilizes key elements of the traditional digital financial wallet as well as providing a repository for consumers to upload various health documents and manage medical payments. Consumers then make and conduct telemedicine ap -
pointments for their physical and mental health needs through their smartphones. Localization and cultural relevance are key to the business proposition and is a focal point to ensure relevant, appropriate care for Esprit’s customer base.
Just as with other telemedicine services, as soon as a patient downloads the app and accesses it, they are immediately connected to a host of products and services. Esprit Health plans to scale up by utilizing existing distribution channels. They’ll also pull the various healthcare service pro -
How they accomplish this role of virtual health intermediary comes down to experience. Robert and his team have faced similar challenges setting up mobile and telecommunication networks and will apply the same framework to digital health. That expertise allows the Esprit team to use repeatable and scalable methods as they expand to new countries.
viders in each country onto the network, then they’ll ramp up their digital marketing to attract customers and funnel them into those medical service providers, thus creating an effective Consumer healthcare marketplace.
How they accomplish this role of virtual health intermediary comes down to experience. Robert and his team have faced similar challenges setting up mobile and telecommunication networks and will apply the same framework to digital health. That expertise allows the Esprit team to use repeatable and scalable methods in each new country as they expand.
While the goal is to provide low-cost medical care and microinsurance support to underserved communities, the first target consumers for Esprit will be middle and pre-middle income earners. This will allow for early revenue and the opportunity to scale up quickly to then focus on low-income at-risk populations. Condon already has his eyes set on rolling out his platform throughout emerging markets in Africa and Southeast Asia.
Telehealth isn’t anything new, yet with all of our tech advances virtual care remains a distant reality in many lowincome and rural regions. We’re proud to back Robert Condon and his team at Esprit because they’re laser focused on providing access to care, with an eye towards bringing the best of virtual care to the people who have been left out in the past.
We’re also excited to support Esprit
because they’re porting knowledge and experience from the telecommunications industry over to health. A common complaint about healthcare is that it lags a decade behind other industries and hasn’t benefited from the same technological advances and consumer adoption that we’ve seen elsewhere. One way to fix that problem is to bring top minds from outside of health into the fold and rethink the system from the ground up. With his decades of experience building cellular networks around the world and navigating the infrastructure and cultural challenges of digital adoption, Condon is the right person for this job.
Finally, we’re proud to link arms with Condon and his team because they have a health moonshot mindset. After years of helping people communicate over mobile networks, Condon has made it his mission to do something ever greater: use digital mobile technology to save lives. He’s not just building a business; he’s building a legacy. It’s the culmination of his life’s work, and it’s the most important thing he’s ever done. That’s the kind of passion and dedication necessary to improve the health and wellbeing of everyone on the planet.
contact: esprit@startuphealth.com

Leah Houston, MD, turned a nightmare scenario of stolen identity and fraud into the catalyst for a world-changing idea. Now, she’s building a Web3 platform that could give physicians greater identity control, speeding up credentialing and giving them greater career mobility.
IImagine for a moment that you are a doctor (your parents are so proud). After years of countless hours in the library and long nights with little sleep, you’ve received your degree and made it through residency. It’s time for your first real job and your first real doctor paycheck. You need it to start paying off those loans. You apply for several promising positions and accept a position in a large hospital network.
Except before you can start work, they have to verify you are who you say you are. After all, they don’t want a ‘Catch Me if You Can’ situation. You have to present your proper certificates and wait while
they call your school and verify your degree. You wait, trying not to dwell on your lost income or think about the patients suffering at the hospital which is understaffed without you.
Finally the day comes when you get to start your new job. This is it. Time to embark on a career doing what you were trained to do: care for patients. You dive in and give it your all. After about a month, your supervisor sits you down for a review. It’s all positive–the staff loves you, the patients love you. But there’s one little thing: your hourly patient average is only 2.4 and we really want you to be above 2.6. See that doctor over there? He’s the highest paid in the group and averages three to four patients per hour. Nevermind that he sends his scribe to talk to take their history, orders tests, and only sees the patient if there are results to deliver.
You start looking for another job, one where the patients are the priority, but you know that it’ll take another few months to onboard again because of the credentialing process and you can’t lose your income — you just bought a house, or a parent or a child needs special care, or you doubt this new place will be any different. You feel stuck and you and the other doctors at the
hospital start calling it the “RVU factory,” because you all feel as if you are practicing assembly-line medicine. It’s not too long before you start experiencing burnout and no wellness program or meditation app seems to help.
Leah Houston, MD, experienced this exact scenario. After graduating and completing residency at Albany Medical College, she began her career as an emergency physician in Florida. Within a few months of practicing, she felt devastated. “I felt like I wasn’t given the tools to render proper care.”
She decided to become a locum tenens doctor, traveling to different hospitals as a 1099 contract employee. Since she was paid by the hour and not the number of patients she saw, it helped free her from the pressure of hospital metrics and she no longer felt the pressure to do the wrong thing to make more money. Dr. Houston felt like she reclaimed a bit of autonomy, of personhood, in a system that wanted to turn her into a number to be crunched.
Then her identity was stolen. In 2017 she received a letter from CMS that stated she was practicing without a license and her ability to work and bill under Medicare and Medicaid as a doctor was revoked. It turned out that a hospital system she once worked for was committing Medicaid and Medicare fraud using her name and licensing number to bill for tests and procedures that were never rendered by her. She hired a lawyer and eventually came to a settlement agreement with the hospital, but in
the meantime, she lost months of work and income.
How did this happen to her and how could she keep it from happening again? Following the settlement, Dr. Houston reflected on those questions as she took time off to care for her mother with cancer. She thought back to her time living and working in Silicon Valley in 2014 and some of the conversations she had then with early founders and investors working in Web3 and blockchain technology. She remembered learning about bitcoin from a doctor friend and how blockchain could be used to verify something as important as a currency. If it could work with currency, thought Dr. Houston, couldn’t it work with credentialing?
What doctors needed, she realized, was to own their own identities. They needed a secure way to prove they are who they said they are, something that would prevent fraud and allow doctors to move more quickly between positions without
Think of [Evercred] like ClearPass at the airport, but instead of getting someone through airport security, it helps doctors move more freely between jobs and health systems.
the months of income loss as they waited for hospitals to verify them. They needed autonomy to live and work as themselves.
So in 2018, Dr. Houston hopped a plane back to Silicon Valley and started talking to some of her contacts. She attended an internet ID workshop and told people her story to see if it was a viable use case for blockchain identity certification. The answer was a resounding yes. She started running her idea by doctors and although plenty were confused by the technical details, the people who understood what she was talking about expressed a great deal of enthusiasm.
Dr. Houston had the buy-in she needed and got to work. In the summer of 2019 she launched her company, HPEC (Humanitarian Physicians Empowerment Community). She raised an initial round of funding through friends and family and then a half a million more through crowd funding that enabled her to design, develop, and deploy the HPEC app to the app store. She brought on her first health system partner to pilot the app, Norman Regional, and began the process of bringing their physicians onto the app.
What had started as one woman’s quest to protect herself from identity theft expanded into a vision of a digital physicians’ guild that restores autonomy to doctors and allows them to rapidly authenticate who they are so they can more efficiently work, connect, and build a professional referral network outside of the typical constraints of their hospital network. In short, Dr. Houston was creating something that turned the status quo on its head.
At its core, HPEC is a digital wallet mobile application for doctors that issues permanently verifiable credentials using their own open standards-based credential system called “Evercred.” Think of it almost like ClearPass at the airport, but instead of getting someone through airport security, it helps doctors move more freely between jobs and health systems, and connect with each other as professionals without the constraints of third-party influences like insurance companies or professional networks.
Currently, it takes between four to six months to onboard and credential a physician for a hospital. This amounts to up to $1M in lost billing for the health system and an average of $100,000 in potential income lost for the physician. HPEC streamlines the onboarding process by letting the physicians prove their identity themselves, using self-sovereign and decentralized identity tools and technology.
“As soon as I talk to the CFO of a hospital and show them how much money we will save them on onboarding, it becomes an easy sell. We save money on the issuer’s side, the verifier’s side, and the doctor’s side.”
To understand HPEC’s current iteration, imagine for a moment you are the same doctor from the beginning of this piece, feeling trapped in that assembly-line medical system. A friend from med school gets in touch with an invite to HPEC. At first you’re confused — is this like Facebook for doctors? But you sign on and go through the system’s ID verifica-
tion system that uses your NPI (National Provider Identifier), a government ID, and facial recognition to confirm you are who you say you are.
As time goes on, you begin to understand how the platform provides you with autonomy as a physician. You can securely chat with a sub-specialist outside of your own network about a patient, you can pick up a few telemedicine consults through the platform, you get to contribute to a document on practice guidelines for your specialty. In short, you’re getting to be a doctor the way you imagined, providing care and furthering your field of medicine in the HPEC space.
Dr. Houston’s long-term vision for HPEC is for it to become a completely new paradigm for giving and receiving medical care; a marketplace where independent doctors can coordinate care for their patients and where patients can safely share their data with verified physicians. To that end, the company is currently fundraising to build out their platform to expand across these different potential healthcare applications, like health record management and digital health and telemedicine, as well as continuing to grow their network of health systems using their Evercred technology to onboard physicians.
“From cradle to grave, physicians authenticate patient information. Now that all that data is digital, we need methods to prove that the person authenticating is who they say they are. And we need to keep that information secure and private away from data miners who want to use
that data to exploit patient pain and suffering.”
StartUp Health is proud to back HPEC’s revolutionary approach to physician credentialing because of its founder’s hard-won knowledge in the healthcare field and the transformative effect this technology offers to doctors and hospitals.
Dr. Leah Houston knows firsthand what it feels like to be a physician trapped in a healthcare system that measures the worth of its providers by RVUs. With HPEC, she designed the tool she wished she had to practice independently as a physician and provide the best possible care for patients. HPEC is one of the only companies tackling the $5B credentialing market from the physician side, allowing them to own who they are through a selfsovereign identity system.
By empowering physicians this way, HPEC changes the terms in which they move through the world and creates new pathways for doctors to engage with each other and patients. If you picture the current healthcare industry as a game of foosball, the doctors are the players attached to the bars, and the bars are turned by the hospital administrators and insurance companies. HPEC comes along and takes the players off those bars so they can freely move across the table.
contact:
hpec@startuphealth.com
The team of Canadian and Dutch founders leveraged technology called photogrammetry in order to make scoliosis monitoring fast and safe for millions of patients.
OOften in business, the goal is to keep ahead of the curve. When it comes to the new telehealth company Momentum Health (formerly SeeSpine), that goal is literal. Adolescent Idiopathic Scoliosis (AIS), that curve of the spine your gym teacher might have checked for in elementary school, is the most preva-

lent spine deformity, affecting 1–3% of children (a million annually) in North America. And when it comes to treatment, every degree you can prevent the spine from curving helps.
The problem is that scoliosis can be hard to diagnose. Children aren’t regularly screened for the condition and their growth fluctuates wildly during childhood and early adolescence, meaning a curve that seems stable might dramatically change in a short amount of time. Catching a curve early is imperative: 75% of spinal curvature can be slowed or stopped through the use of a brace. While surgery is an option, it is incredibly invasive.
Even if a case of AIS is identified, monitoring its progression brings a whole other raft of challenges. The standard of care for tracking progression is four X-rays a year. Not only does this expose young patients to the harmful effects of radiation with some devastating results–for example, women with scoliosis are twice as likely to develop breast cancer later in life–but it also comes with a high rate of human error for reading these results. When a provider who isn’t skilled at treating scoliosis reads the X-ray there is an estimated 25% error rate.
This puts patients in a bit of a Catch-22 when it comes to their condition: their only option to effectively track and stabilize their curvature to prevent an invasive surgery involves risking their health through repeated X-rays — X-rays that might then be misread. The pervasive mood on chat boards devoted to scoliosis can be a sense of powerlessness; patients
wish they could know what was happening to their spines while they wait six months for their next X-ray or wish they could just DO something, anything, to have more ownership over what is happening to them.
Evan Dimentberg had some time on his hands. It was the first summer of the pandemic and there were limited work options for a medical masters student as hospitals limited non-essential staff and personnel. Dimentberg used this unexpectedly free summer to research, burying himself in scientific journals and studies. One particular article, detailing the problem of radiation and scoliosis monitoring for adolescents intrigued him. Back in high school, Dimentberg spent two weeks observing Jean Ouellet, MD, the President of the Canadian Pediatric Spine Society and a surgeon at Montreal Children’s Hospital, and he wondered what Dr. Ouellet might think of this problem. Dimentberg wrote it down and tucked the article away.
Fast forward a few months and Dimentberg needed to present his idea for a medical research project for his masters degree. He pitched his idea for coming up with a non-radiation monitoring system for scoliosis to Dr. Ouellet and got the green light to explore possible solutions as his research focus. But where to begin? What might possibly work?
After some false starts (and some nonstarters), Dimentberg heard about the idea of photogrammetry. It is used to make 3-D renderings and often used by engineers in
construction to identify and predict problems with buildings or bridges.
What if, Dimentberg wondered, you treated the human body like the structure of a building and used photogrammetry to identify structural issues, like the degree of a spinal curvature? It held promise, but
The standard of care for tracking scoliosis progression is four X-rays a year. This exposes young patients to the harmful effects of radiation – women with scoliosis are twice as likely to develop breast cancer later in life. It also comes with a high rate of human error. When a provider who isn’t skilled at treating scoliosis reads the X-ray there is an estimated 25% error rate.

he had a lot of questions. To answer them, he hopped on Upwork, the freelancerfor-hire site, searched “photogrammetry,” picked the first guy that came up, someone in South Africa, and paid him $50 for an hour of simply answering questions.
Not only did this conversation help corroborate Dimentberg’s hunch that he was on the right track with the methodology, this freelancer in South Africa also made a connection between Dimentberg and two photogrammetry specialists in the Netherlands, Frank de Wijk and Leander Goor. He sent them an email and now two years later, they are on board with Momentum Health as co-CTOs and cofounders.
“That hour through Upwork was the
best $50 I’ve ever spent,” says Dimentberg with a laugh.
Over the course of 2021, Dimentberg and Dr. Ouellet conducted research and development on their concept, running a clinical trial that proved out their hunch that photogammetry and AI algorithms could predict spinal curvature–the outside topography of a body revealing issues in the internal structure. Instead of expensive and potentially harmful X-rays, they were developing a feasible way for patients to monitor themselves from home using the camera on their phone. What they found answered the two main challenges of tracking scoliosis: radiation exposure and discontinuous follow-up riddled with human error.
Momentum Health is a mobile application that allows you to remotely recreate the 3-D surface topography of a body using a smartphone camera. This scan is used to assess and predict spinal curve progression and guide clinical decisions for the treatment of scoliosis. It takes 15 seconds, can be done as often as the patient wants, and tracks spinal curvature progression with greater precision.
“Our goal is to allow patients to take control of their care, manage and track their progression, and feel a little bit more in control of their disease,” explains Phillippe Miller, Momentum Health’s CEO and Co-founder. Miller’s been engaging with scoliosis support groups and patients to get a read on what they are looking for when it comes to their condition.
“Patients feel lost in their care. They see a doctor and are told to come back six months later and they have no idea what’s happening in the meantime. They want to feel like they’re doing something, like they have more ownership over their bodies.”
Momentum Health also aims to empower primary care physicians who don’t have the experience or tools to follow up with their scoliosis patients. Orthopedic surgeons should only see that 5% or so of patients who require bracing or surgery. Ideally, 95% of patients should be able to stay with their family doctor, but because measuring scoliosis is a complex process, patients end up in flux, with their family doctor passing them off to the ortho, only for the ortho to send them right back since surgery or bracing isn’t required.
Momentum Health addresses these issues of accuracy and consistency in treatment in a few ways. First, because the AI is automated it helps take out the issue of human error in reading a scan. There are controls built into the software that point out if an image wasn’t made correctly, for example, if the lighting is off or the wrong body part is captured. Second, because the measurements are made more frequently, it helps correct for mistakes: the repetition weeds out aberrations. And because the method is radiation free, there’s no harm redoing a scan as often as needed to get it right.
Currently, the team is building out their mobile app for patients with an existing scoliosis diagnosis to use at home or at their point of care. The scan uploads to a physician web portal to track progression
of their curvature. It’s a B2B2C approach where they market the product to physicians who then invite patients to use the app for at-home tracking. In the future, they plan to add a direct to consumer diagnosis platform that allows families to screen for scoliosis at home.
As they talk with consumers and physicians, they are gaining a lot of traction in remote communities who don’t have access to regular monitoring. As Dimentberg explains, “Even in Quebec where we are based, we hear about patients who have a five-to-six-hour drive just to get a consult with a pediatric spine surgeon. They drive all that way to get an X-ray that they don’t actually need.”
They are launching further trials to help build out a comprehensive data set and provide proof of concept. This data will be important to help Momentum Health overcome some of the skepticism in the scoliosis community. “People have been trying to tackle this issue of monitoring without radiation for so long and the attempts haven’t hit the mark. We are going to show that we are different,” says Miller.
Momentum Health’s mission to detect and track spine curve progression in a safer, more effective way, because of their founding team’s combination of deep technical background with medical knowhow. They’ve assembled a global team that combines the best of photogrammetry in their dual CTOs de Wijk and Goor, with acclaimed pediatric spine surgeon Dr. Jean
Ouellet’s expertise in the field directing their clinical steps.
It’s also a team that balances each other’s personalities and proclivities well. The two young co-founders, Dimentberg and Miller, bring a healthy amount of ambition and drive to the workflow, which helps in a field like medicine where advancements in methodology tend to move at a more glacial pace. Dr. Ouellet’s steadying hand makes sure they are checking the boxes when it comes to confirming and demonstrating the effectiveness of the app, and Wiljk and Goor stand in the middle, using their deep domain expertise to help the team move forward on important decisions.
We’re also proud to invest because of their innovative approach that brings the best of 3-D topography to the healthcare world. It’s an unusual approach with far-reaching implications. It also shows Momentum Health is willing to look at old problems in new ways and aren’t afraid to take calculated risks. Their initial findings indicate that this risk stands to return substantial rewards for scoliosis patients and their care providers and puts them ahead of the curve in revolutionizing spinal monitoring.
contact:
momentum@startuphealth.com

CEO & Co-founder Bechara Saab, PhD, spent years in the lab understanding how the brain works. With Mobio, he’s built a novel way to identify mental health challenges early and offer digital solutions that can scale globally.
SSome problems seem too difficult. Suppose you were tasked with the job of finding 800 million psychiatrists who could deliver top-notch care for everyone suffering from mental illness around the globe. You’d just as well try to clear all the seashells from a beach. “Daunting” doesn’t begin to describe it.
We have a mental health problem in the world and it’s rapidly becoming humanity’s greatest crisis. One in ten people need mental healthcare. Globally, that number sits at around 800 million. Therapists and psychiatrists have tools to deal with the individual challenges; there just aren’t enough of them.
Cost is also a huge barrier to mental healthcare. If you’re one of the few who
can access psychotherapy, you could drop $25,000 in a year of care. Mental illness is costly. $1.8 trillion is spent on direct care for mental health. Mental illness writ large is a $16 trillion per year crisis.
If you can access mental healthcare and pay for it, there is the added problem of measuring success. There is a lack of precision and accountability in our current mental health standards of care. It’s hard to tell what each patient will need and how people will respond to various treatments.
In recent years, mental healthcare has seen the rise of digital therapeutics (DTx), where solutions are designed for scalability and affordability. The DTx industry is growing annually at 31.4%. But while DTx is suited for scale, quality of care remains a challenge. Mental health apps that take a one-size-fits-all approach are going to have limited success. Without personalization and the ability to collect data on the mental health of the individual patient, these tools will remain limited in their impact.
Enter Mobio Interactive, a startup bringing real-time mental health data to the world of DTx solutions.
solving the mental health crisis is impossible. CEO and Chief Scientist at Mobio Interactive (MI), Bechara Saab, approaches the solution with a personal history in both technology and medicine. After completing a PhD in neuroscience at Mount Sinai in Toronto and postdoctoral research at the Swiss Federal Institute of Technology, Saab found himself in a lab with mice. He had opened a pre-clinical laboratory at a psychiatry hospital in Zurich. Saab’s research focused on circuitry that underlies one’s motivation to explore. In other words: how does the wiring of your brain make you curious? At the time, a media storm gathered around one of his discoveries which linked curiosity and intelligence at the molecular level.
Since Saab was based at a psychiatric hospital, his curiosity led to a new interest. He observed that one of the most common characteristics of mental illness was the dearth of exploratory behavior. After a mental illness is developed, the person’s desire to explore either ends or is overpowered by manifest fears. He wondered: If we could stimulate and kickstart the curiosity circuitry, could this help mental illness?
Saab began to experiment on mice, restoring these parts of the brain through injecting a virus into the brain, installing a fiber optic, and planting a cap which controls it.
While this wasn’t a scalable solution for humans, it was the beginning of a bigger conversation around mental health. Around this time, Saab was approached with the idea of starting Mobio Interactive.
In 2016, the company’s launch corresponded with their first clinical results.
Saab quit his job and began full-time as Chief Scientist for MI in 2017. In 2020, a paper was published with the world’s most-accurate stress modification using a selfie video. In 2021, MI signed their first health insurers, and they partnered with their first hospital in 2022.
Mobio combines digital therapy with technology, delivering both a scalable solution and a personalized approach. One side of the business will seem familiar to many. They currently offer more than 1,000 unique psychotherapy and psychoeducation sessions with more than 70 guides, psychiatrists, and clinical psychologists across seven languages. These sessions, which are accessed asynchronously and on-demand through a smartphone, introduce the user to The Journeys — most of which are clinically-validated tracks unlocked via a physician’s prescription.
The other side of the business — and the technology that powers the patient’s
After a mental illness is developed, the person’s desire to explore either ends or is overpowered by manifest fears. What if we could stimulate and kickstart the curiosity circuitry?
personalized therapy — is where Mobio Interactive clearly stands out. They are the first company to offer digital therapy with personalization driven by objective measures without relying on a wearable. Using nothing more than a camera phone, MI can quantify stress within 30 seconds.
“One can only fake how they feel for so long,” Saab explains. Their face tells the whole story. MI skillfully combines computer vision with artificial intelligence and self-assessment. With technology reading the patient’s heart rate, relative oxygen saturation, and breath rate, stress levels are determined. Through the selfie, however, MI can also pull out three different pigments from the face and read micro facial expressions, tracking 200 intersection points around the eyes. As a result, MI determines the user’s stress level with an 80% accuracy. By combining digital therapy with video technology, MI produces accurate mental health analysis and personalized therapy at scale.
Strategically based out of Singapore due to its global connections, MI has their sights set on the world. Currently, MI is delivering therapy at scale through partner hospitals, spanning seven languages and ten major markets. United with expert advisors and directors, and a supportive network of investors and programs, MI anticipates FDA approval for their first Class II SaMD (Software as a Medical Device) in 2023.
Mobio Interactive is an innovative company with a bold mission. With seven
years of research, testing, and implementation, MI has proven to be a sensible solution for a significant problem.
As MI has tested their product in a controlled setting, analyzing stress before and after meditation training, MI has clinically proven decreases in anxiety, stress, and other symptoms of mental illness for a variety of medical conditions. It is the first such platform to beat the placebo. And having tested their product thousands of times, on ethnicities in more than 100 countries, we believe they can make an impact on the global market. This highly differentiated product has withstood clinical rigor and proven itself.
MI is just beginning. Curiosity hasn’t declined as exploration continues. We’re excited about future developments with MI as they seek to monitor distribution of blood in the face through the camera. Perhaps blood expression patterns correspond with different emotional states that computers can interpret in clinically meaningful ways. Right now, virtually all technologies use six different basic emotions, however the brain doesn’t have just six. Tracking blood flow in the face may prove a better way to analyze the user’s brain. Additionally, MI is seeking to mimic the patterns of human eyes, gaining a better assessment and feeding that data to the network. Step by careful step, MI is showing the world that precision psychiatry is possible at scale.
contact:
mobio@startuphealth.com

Co-founders Christian Dansereau, PhD, and César Laurent, PhD, have put together a world-class team of experts in AI and deep learning in order to bring precision medicine to the masses and streamline clinical trials.
IImagine you are packing your bag for a trip without knowing your destination. Do you bring a winter coat and a bathing suit, just to cover your bases? If you don’t know where you’re going, it’s impossible to know what to bring on your journey. You are packing blind.
We’ve grown to expect that we can know the forecast before we pack for a trip, yet on the long road towards developing effective new drugs and treatments, researchers and physicians aren’t as fortunate. Disease progression varies wildly from patient to patient, making it incredibly difficult to forecast which patients might benefit from a treatment or clinical trial in the future.
Researchers end up doing the equivalent of packing a little bit of everything — a one-size-fits-most approach to medicine
that fails to address the heterogeneity of the patient population and disease progression. For example, a clinical trial for a new drug to prevent a second heart attack will go to enormous expense to recruit a large population size of people to test its efficacy. But only 10% of the recruited population will ultimately develop a second cardiovascular event. Not only were hundreds of millions of dollars spent on a trial that is irrelevant to 90% of its participants, but it also exposed patients who didn’t need the drug to unnecessary risks.
Or take a degenerative disease like Alzheimer’s. It’s incredibly hard for primary care physicians to predict which patients with mild cognitive symptoms are more likely to progress or remain stable. Given the uncertainty, doctors postpone their diagnosis and care until the condition clearly deteriorates to a point where diagnosis is obvious but unfortunately miss the optimal window for early treatment. Without an individualized forecast for a patient, there’s a lost opportunity for early intervention when patients are still functional.
When you calculate the amount of money these delayed diagnoses cost the healthcare system, the total is staggering. For Alzheimer’s disease alone, the lifetime cost of delayed diagnosis and interven-
tions is estimated to be $7T. And it costs more than $5.7B to bring a new therapy to market, part of this cost comes from the high failure rate of clinical trials for Alzheimer’s disease. There’s simply too much variability in the disease progression to create a targeted intervention.
In 2017, Christian Dansereau was finishing his PhD in Computer Science from the University of Montreal. His research focused on how to apply machine learning and AI in the field of neuroscience.
“I was working with a pharmaceutical company assisting on late-phase clinical trials for Alzheimer’s disease and I saw their challenges in recruiting individuals whose progression was unknown. The trial had a huge risk of failure and ineffectiveness because of this uncertainty.”
What if, Dansereau wondered, you could better predict which patients would benefit from a particular intervention? What if you could take the wealth of patient data that can be gathered and leverage it to optimize diagnosis and prognosis? What if clinical trials didn’t need to be such a shot in the dark?
These were just the sort of research questions an academic like Dansereau could spend years turning over, but he wanted to do more than contemplate the problem. Over the course of his studies, he saw firsthand the stories and the lives behind the technology, the impact on patients and their families.
“I knew if you don’t take matters into your hands, it won’t happen. I needed to
push to turn something from a research subject into a product that really impacted people’s health.”
In 2018, Dansereau launched Perceiv AI with his co-founder César Laurent, PhD. Laurent, a deep learning researcher from the prestigious Mila Institute, shared Dansereau’s passion for applying machine learning and AI to the healthcare field. Together they developed the initial software for the company, focusing on Alzheimer’s clinical trials as their first vertical, building off of Dansereau’s doctoral research.
A big turning point for the company came at the end of 2018 when they presented on the main stage at the Clinical Trials on Alzheimer’s Disease (CTAD) annual conference. After they walked off the stage, multiple pharmaceutical companies approached them to discuss the application of their AI for trial recruitment. These conversations lead to the company’s first contract in 2019.
Close to half a million in grant funding allowed Perceiv AI to build out its team in 2019 and 2020, bringing on Angela Tam, PhD, as Senior Scientist and Adrián Noriega de la Colina, MD, PhD, as the Clinical and Regulatory Lead. The team launched their first product offering, Foresight AD™, at the CTAD conference in 2021, a full-circle moment for Dansereau and Laurent. In three years, they took their idea from theory to a realworld tool.
Perceiv AI predicts disease progression
using a platform powered by machine learning and AI. It’s a forecasting tool that allows for precision medicine: treatments and interventions that take into account individual clinical risk factors, cognition, genetic biomarkers, environment, imaging, and other information across different modalities to more accurately address a condition. Instead of a one-size-fits-most approach to healthcare, Perceiv AI’s platform empowers targeted research and care to find out what specific strategies work best based on the many factors in play.
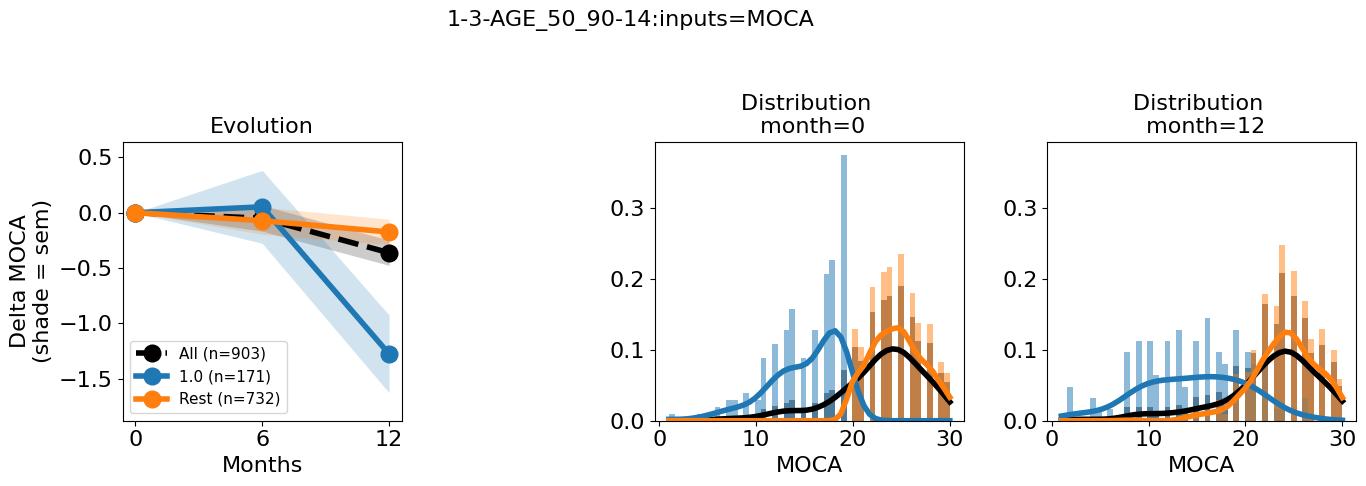
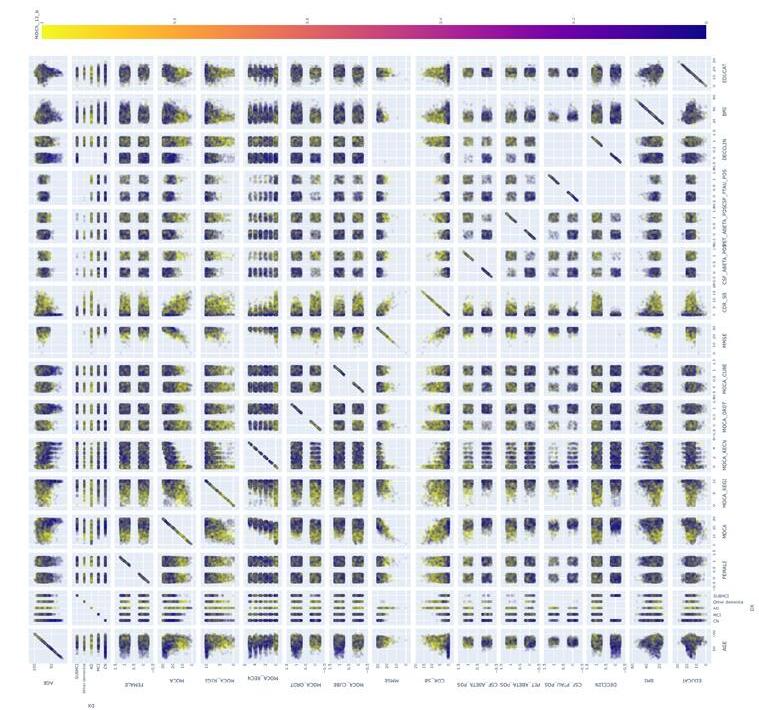
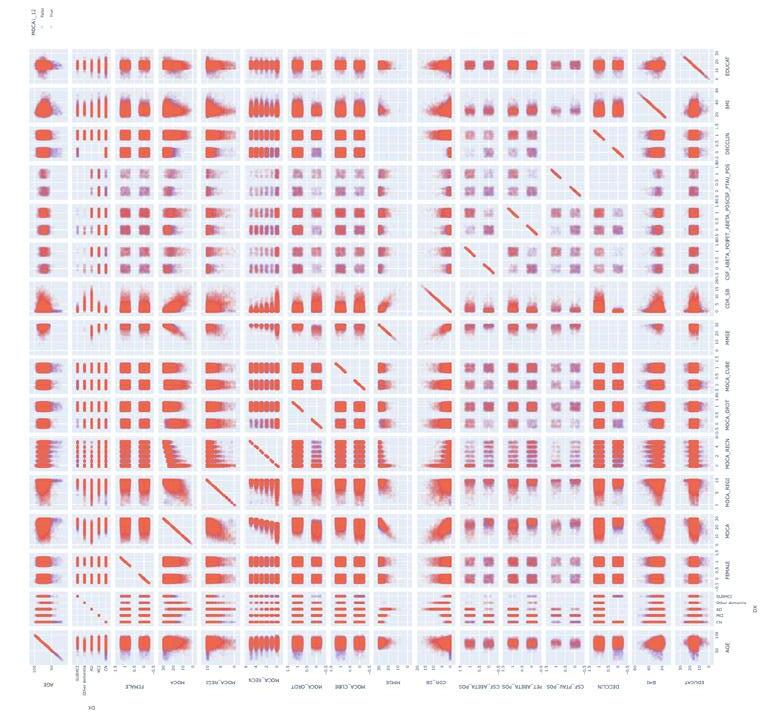
Their first product, Foresight AD™, specifically forecasts the progression of cognitive decline in Alzheimer’s disease. They spent several years building a comprehensive database of patient informa-
tion using imaging, genetic, phenotypic, molecular, and clinical variables to train their algorithms to make its predictions. It took deep expertise to integrate multiple data sets across multiple modalities together, but the proof has certainly been in the pudding. While other strategies can reduce the sample size of a trial by 15%, Foresight AD™ proved able to reduce a sample size by 51%. An optimally enrolled clinical trial significantly reduces costs while increasing the power of a study to prove efficacy of a treatment.

Because of their success with Foresight, Perceiv AI is also looking into applications in the clinic to assist physicians in a timelier diagnosis so that interventions start sooner; this is critical with the new disease
modifying drugs that will become available in a year or so.
Perceiv AI plans to expand from clinical trials to the exam rooms of primary care physicians as a clinical decision support tool. They have already applied for breakthrough designation from the FDA to start their path towards bringing that product to market. Their vision is to integrate directly with the physician’s interface and EMR platform, so that as the physician gathers information from a patient through different modalities, the Perceiv AI algorithm can predict likely progression and recommend followup tests and treatments.
In the long run they are also looking into expanding to other neurological disease areas, like MS and Parkinson’s, where they can leverage the same learnings and wealth of information they have aggregated for Alzheimer’s.
“There is a lot of space in the market,” explains Dansereau. “It’s very nascent. People are just starting to understand the use of AI in these studies and in the clinic.”
“We are in dire need of precision medicine and a more thoughtful approach to treatment. You see it happening in the oncology space currently and it’s about time to bring that thinking and success into other areas as well. We can reduce cost and show more value for patients.”
highly skilled people from the worlds of neuroscience and AI to offer a product that increases the efficacy of trials and treatments for patients. With the prognostic tools they produce, researchers and physicians no longer have to “pack blind.”
Thanks to their connections at various academic institutions, their advisory team includes such luminaries as Yoshua Bengio, PhD, known for his pioneering work in deep learning, Serge Gauthier, MD, FRCPC, the Director of the Alzheimer’s Disease Research Unit at McGill University, and Betsabeh Madani Hermann, MEng, MBA, an advocate for translational research and thought-tech innovations, among other respected innovators and thought leaders. These advisors represent the wealth of insight and knowledge backing Perceiv AI’s work and keep the company striving for novel applications and new verticals to tackle.
Finally, we’re proud to back Perceiv AI because of the way they ensure that their insights are actionable. It would be easy to get caught in the ether of the vast amounts of data and information they process and its implications. But Perceiv AI has a clear North Star: the patients. People drive their processes. Their digital biomarkers are highly specific and thoroughly validated so they are actually useful and usable in clinical settings.
WHY
TO INVEST StartUp Health is backing Perceiv AI because of the way they combine visionary thinking and processes with the academic know-how. Their team brings together
contact:
perceivai@startuphealth.com

Co-founders Sam Miller, PhD, and Olly Styles, PhD, are taking their combination of experience in AI, computer vision, and weight lifting to bring to market a new tool for athome fitness. With a simple plug-in, anyone working out online can get personalized feedback on form and progress.
IIt comes as no surprise that the most cited New Year’s resolution is to exercise more. It also comes as no surprise that after three months, 90% of people have abandoned this resolution. It is hard to stay motivated to exercise: hard to find the time, the energy, the right program. It’s hard to feel like you are making progress and hard to know if you are doing it right to reap the most benefits.
Despite the difficulties, we all know we
ought to be doing it. The research is clear: regular exercise reduces a person’s risk of heart disease, diabetes, and some cancers. It also improves mental health and mood, promotes healthy aging, improves sleep and sexual health. If you want to feel better, be healthier and live longer, you should incorporate a fitness routine into your life.
In some ways, it’s never been easier. Thanks to online streaming platforms like YouTube, Instagram, or even TikTok, any room in your home can become your gym. The pandemic accelerated the adoption of these programs, as gyms closed temporarily and sometimes permanently. Little wonder that the online fitness industry has grown 77% since 2019.
The problem with online workouts — particularly on YouTube — is that people are exercising in a vacuum without feedback or goals. When you complete a workout, you don’t know if your form was correct or how many reps you completed. When you do a video the next day, there’s no sense of progression. There’s also little to no community, which provides both comradery and sometimes a healthy dose of competition to take your performance to the next level.
All these factors — clear, achievable goals, progress tracking, community, competition — are proven to motivate people to continue working out and are difficult to find in the stream-on-demand workout space. There’s also a question of safety. Common injuries such as pulled or strained muscles and sprains are largely preventable with proper form, but working out independently at home means a
coach or instructor can’t see if you’re overrotating your shoulder during a dumbbell thruster or doing a squat correctly to protect your knees.
Sam Miller knows all about squats. While at Cambridge studying economics, he was also a member of the weightlifting team, competing as a powerlifter.
“People don’t associate a place like Cambridge with weightlifting, but we were the best university team in the UK. There’s actually quite a geeky element to weightlifting; you plan a training program carefully and calculate your way to your goals.”
Over time, Miller moved into physical coaching as a side gig, starting casually and then more formally coaching the college rugby team. He honed in on form, knowing that a nasty injury is likely if the moves aren’t executed correctly. But Miller quickly identified a problem: he couldn’t always be on hand to correct someone’s form.
He found a clever workaround using what was then a new technology: WhatsApp. He’d get his clients to record themselves doing their workouts, then critique the videos and reply telling them how to adjust. Even when he moved to London to start his career with the Bank of England, Miller was able to continue coaching some clients from a distance.
As he worked in London, Miller began to teach himself Python programming and developed an interest in artificial intelligence and machine learning. He wanted to go deeper in his understanding and de-
cided to pursue a PhD.
“It was a leap for someone with an economics background to move into AI. The connection I made in my mind was statistics; both fields work in likelihoods and anticipating chances.”
Early in the program, Miller came across the concept of computer vision; the same kind of technology that allows computers to recognize and diagnose cancers. A fellow researcher in his program was extracting components of the human body and their location using computer vision, and the proverbial lightbulb went off in Miller’s head.
“My thought was if a computer could recognize the points on the human body, then it could be used to identify these parts when engaged in exercise. In essence, you could use computer vision to judge a squat and know if the knees are where they should be or hips, etc. It could automate coaching.”
Miller knew just who could corroborate his theory; Olly Styles, a friend from his
Cambridge weightlifting days who just so happened to be getting his doctorate in computer vision. When Styles told him he thought it could be done, the two friends took on the idea as a side project during their PhD studies. Their initial programming and application of computer vision worked surprisingly well, due to several big advancements in computer vision at the time. Buoyed by this success, Miller and Styles decided to make a go of a startup and pulled in Vlad Ursu, their founding lead engineer.

In February 2020, they launched their first iteration of Atlas AI and immediately faced a true startup baptism by fire. Their initial business plan involved bolting a camera with their program directly to gym equipment, because setting up a phone to film a gym workout is time consuming and difficult. The individual consumers would pay for the program to give them feedback on how they used the equipment. But in March 2020, COVID-19 hit and the gyms closed. Their in-person business model was no longer viable.
This would have been enough to make any startup consider giving up. Thankfully, Miller describes himself as incredibly stubborn. He continued to pitch the ideas to gyms when they reopened in the fall of 2020 and, as often is the case,
knocking on door after door provided an unexpected opening.
When Miller pitched to a gym owner in London that October, the owner said he didn’t want the product in his gym. He was, however, setting up an online coaching platform for clients to do remote workouts with his trainers and was interested in licensing the AI for this platform.
That wasn’t the commercial model Atlas AI planned, and the team hesitated. Then the gyms closed again in November.
“That’s when I realized our commercial model was more flexible than I thought,” says Miller with a laugh.
By the middle of 2021, the company worked with three clients, creating a backend product that converted videos of people exercising into performance data. They picked up two more online platforms as clients and pivoted to a SaaS model, integrating their AI into different virtual trainer-led workouts.
Following this success, the Atlas team was accepted into the Techstars accelerator program. Through this mentorship they ultimately expanded their vision even further, to address an even bigger opportunity in the fitness market.
Atlas delivers AI personal training to users for workouts on any streaming platform, including huge untapped markets like YouTube where five billion workouts are logged each year. It works as a browser plug-in, similar to Grammarly, popping up unobtrusive suggestions during the workout itself and providing a detailed, post-
workout progress report.
Let’s say you and a few friends decide to do a squat challenge using a TikTok video. You’re already working out in front of your phone which means the camera is pointed right at you. As you squat, the Atlas plugin tracks your form and gives you some immediate audio feedback that doesn’t stop the flow of your workout: “Try going lower in your squat so your hips are parallel to your knees.” After the workout is done, you pull up the progress report and see personalized visual data on how to improve your squats, a technique score, and a way to share your results with your friends.
Atlas’s big differentiator is the fact that the user can pick whatever streaming workout they want, on any platform. The AI is flexible enough to follow different content, unlike their competitors in the MSK space whose AI requires the user to follow a set routine.
“Because our original plan involved partnering with gyms during live classes and training sessions, we built our AI to work without a plan. It recognizes what you’re doing as you do it.”
Thanks to Atlas, these online home workouts no longer take place in a vacuum. Someone with incorrect form can receive that input and start achieving better results. A person nervous about aggravating an old injury (or injuring themselves again) can make sure their body is in proper alignment. A group of friends can do the same YouTube workout and share their progress reports afterwards, spurring each other on to better achievement.
Currently, Atlas is beta-testing its direct-
to-consumer model using a freemium subscription model, similar to the Strava running app. They’ve used targeted partnerships with YouTube fitness content creators to create their first users, offering free performance tracking. Next, they’ll build out the premium features to be offered at a low monthly price — features like workout planning, deeper fitness analysis and personalized tips, and synced group workouts.
StartUp Health is proud to invest in the work of Atlas AI because of the scope of their vision, their strong founding team, and their ability to persevere through setbacks. Regular exercise is one of the best things a person can do for their longterm health, but less than a quarter of Americans get the recommended amount. By focusing on motivation and injury prevention for the at-home streaming workout market, Atlas AI tackles a huge sector of the population with tools to benefit their overall health and wellbeing.
Thanks to the two PhDs on their founding team, these tools are backed with the latest and best research in artificial intelligence and computer vision. There’s no one else coming to market with tech like this that can identify exercise moves on the fly and create immediate, actionable data for the user. Not only do Sam Miller and Olly Styles have PhDs, but they have lived experience as weightlifting coaches and know firsthand what kind of information helps push someone on to better outcomes and achievement.
Finally, what Miller calls his “stubbornness,” we call grit. It would have been easy to give up when you launched a product designed to be used in gyms right before a global pandemic shut them. It would have been easy to stop when the gyms turned you away because they didn’t want to upset their trainers on staff. It would have been easy to stop when you had to pivot and create a new SaaS model and then your mentors told you that model wouldn’t work in the long term. But Miller and the Atlas team didn’t stop. They persevered and leveled up, showing the kind of radical determination to succeed that every startup needs.
Although the first two years as a startup saw a variety of setbacks and challenges, Miller and the Atlas team proved themselves willing to pause and analyze their results along the way, and readjust as necessary. Like in weightlifting, the challenges stressed the muscles of the company and they grew to meet them. The hard work isn’t over, but Miller sees the gains starting to show.
“Atlas really can motivate people to get better at their workouts, to keep coming back, to experience the benefits of regular exercise on their mental and overall health. I know the impact on my life personally and it excites me to see the scale of the market and the impact we could have.”
contact:
atlasai@startuphealth.com

Founder Katharine Barnard, PhD, designed — and clinically validated — a new way for patients to communicate their needs to physicians. The result is an assessment tool that helps patients feel heard and doctors feel empowered to care.
EEarlier this year in the New England Journal of Medicine, Surgeon General Dr. Vivek Murthy said this about the rise in burnout among healthcare workers: “Burnout is not only about long hours. It’s about the fundamental disconnect between health workers and the mission to serve that motivates them.”
Between administrative burdens, escalating workloads, and staffing shortages, medical providers get less time with patients to really hear and understand what
they need to improve their health. At the same time, there’s a growing wealth of research to say that the psychological and social landscape of a patient’s life is the key to better health outcomes. A doctor needs to discern the unique health needs of each patient to create a map to the right kind of support. And so this fundamental disconnect — between what a healthcare provider requires to truly care for a patient and the kind of care they have the time and resources to deliver — grows.
Take, for example, a person living with Type 1 diabetes. Despite major advances in how we monitor and deliver insulin, health outcomes for diabetes patients have not shifted in the last 20 years. This is because when a patient comes in to talk to their provider about their diabetes, the only thing discussed is their glycemic numbers. There’s no time to figure out how to achieve behavioral changes or what support a patient needs to access and understand new diabetes technology or how family dynamics might hinder compliance to recommendations. There’s no time for a doctor to fulfill their mission to improve the health of their patients.
“Hear me: that’s what’s broken about the healthcare system,” says Katharine Barnard, PhD. “The patient is not heard.”
Barnard knows better than most how hard it is for patients and healthcare personnel to communicate within the constraints of the healthcare system. For her master’s thesis, she studied the conversations between patients and healthcare
personnel at a diabetes center. What she found was that half of the time, patients and physicians recalled different things being said at the appointments and that doctors tended to remember making more decisions than were actually made.
“The lack of accurate recall, of writing things in patient notes that weren’t actually said, about not coming to an agreement on a course of action for a patient, all contributed to negative outcomes,” she explains.
Barnard followed her master’s work with a PhD in health psychology, specializing in the psychosocial impact and management of illness and long-term conditions. Her goal was to find ways to help healthcare professionals do a better job without adding to their burden. To that end, she developed The Kaleidoscope Model of Care, a cohesive, holistic model, tailored to individual needs to support op -
Burnout is not only about long hours. It’s about the fundamental disconnect between health workers and the mission to serve that motivates them.
-Vivek Murthy, MD US Surgeon General
timum diabetes outcomes.
“I had three rules when making this model. It had to work for any healthcare professional, with any patient, in any length of consultation. It needed to fit into existing healthcare delivery modes.”
Barnard began building a platform to support this model of care, one that took into account the driving forces behind behavior to create real impact on their ability to manage their diabetes. She co-designed it with patients, creating a pre-appointment survey tool that zeroes in on what a patient’s current issues are with their diabetes management through a short and simple series of questions.
The effect was immediate. In a pilot study across three different diabetes care centers, they found that the questionnaire improved health outcomes for patients while also shortening the length of consultations by 11–21%. The providers used the survey results to get to the heart of what patients needed to improve their health, no longer having to “magic up the answers” with half the information they needed, as Barnard puts it. And the patients finally felt seen and understood.
“When the patients get presented with their survey results, they often cry. The focus is so often on their therapies that they don’t realize what their real challenges actually are in managing their care — the social and environmental factors that impact their health.”
Spotlight-AQ is a pre-clinical assessment platform that identifies what a pa-
tient and healthcare provider need to focus on for better management of chronic diseases such as diabetes. It helps doctors provide the right care to their patients through immediately available psychosocial resources mapped to the unique needs of each patient — precision medicine — and helps them provide it within the current constraints of medical practice, reducing the burden of care for providers while improving patient results.
“Our goal,” Barnard explains, “is to focus the consultation so that healthcare providers can deliver the care that needs to be delivered.”
Now that they’ve proven their methods for diabetes care, Spotlight-AQ is looking to expand into other chronic disease areas, using their systematic, evidence-based approach to identify the psycho-social
“When the patients get presented with their survey results, they often cry. The focus is so often on their therapies that they don’t realize what their real challenges actually are in managing their care — the social and environmental factors that impact their health.”
factors that impact patient behaviors. They are also wrapping up a randomized controlled trial focused on children and young people in the US, which will help them expand their reach to a younger demographic.
Spotlight-AQ is currently fundraising to build out their team and platform to improve the user experience and get themselves ready for some partnerships coming down the pipeline. “Now that we have the science right, it’s time to move ahead.” They plan to launch in the US in 2023 and are joining forces with large diabetes tech companies like Dexcom to help fund a direct-to-patient version of the platform.
With diabetes rates estimated to grow as much as 54% by 2030 in the US alone, the timing couldn’t be better or more urgent for patients to receive the kind of proven, precise care that Spotlight-AQ offers, especially considering the burden of care these numbers represent to healthcare workers. As much as the platform helps to reduce costs for patients and insurers by streamlining care and increasing adherence to treatment plans, the team always has its eye on that fundamental disconnect between healthcare workers and their mission described by SG Murthy.
“At the end of the day, we want healthcare providers to be happy in their role knowing they are delivering the healthcare they went to medical school to do,” emphasizes Barnard.
StartUp Health gladly backs the mission of Spotlight-AQ because of its sim-
ple, evidence-based solution that transforms patient care for chronic illnesses, particularly diabetes. It’s a rare healthtech company that lands on the scene with their premise proven out and the research to back their claims. Thanks to the academic work of Dr. Katherine Barnard at the core of what they offer, Spotlight-AQ is uniquely situated to quickly and effectively integrate into existing healthcare delivery models and change patient health outcomes for the better.
Not only is Barnard the only (yes, only) person to hold an FDA approval for a psychosocial measure in diabetes, she also has lived experience navigating diabetes care for her child. What started as an academic focus while pursuing her master’s degree, became a highly personalized mission during her PhD years. Her research tells her how to best scaffold questions to get to the heart of complex patient behaviors and motivation. Her family reminds her of why it matters.
Chronic diseases like diabetes, heart disease, Alzheimer’s disease, and cancers are the leading causes of death and disability in America and the leading drivers of healthcare costs. As people live longer, these numbers and associated costs only continue to rise. The Kaleidoscope Model of Care that Spotlight-AQ deploys is adaptable to suit any condition, setting the company up for rapid growth as they integrate themselves into other medical focus areas.
contact:
spotlightaq@startuphealth.com

Founder Sunny Liang used his struggle with insomnia as a catalyst to bring clinically-validated sleep therapy to the masses.
SSleep. It is as necessary as a good diet and exercise to our health, yet much less likely to end up on the cover of a fitness magazine. On the one hand, most of us know the bliss of a good night’s sleep and its power to improve mood and energy. On the other hand, it’s easy to treat getting enough sleep as a luxury — nice but not necessary, especially if a deadline at work is looming or there’s a Netflix show to catch up on.
Here’s the rub (and it’s not what dreams may come): too little sleep is linked to several chronic diseases and conditions, like Type 2 diabetes, heart disease, obesity, and depression and other mood disorders. Lack of sleep also contributes to car and work-related accidents. Overly tired employees are 70% more likely to be involved in workplace accidents and drivers who get less than six hours of sleep a night are 33% more likely to be involved in a car accident.
When you start taking these health and safety implications seriously, it becomes
clear that encouraging healthy sleep ought to be a priority for a workplace, a community, and a society. There’s more on the line than just dragging a little at work or feeling run down, especially when you take into account that up to one out of three adults suffer from chronic insomnia, a number that has grown since the onset of the pandemic.
But knowing you need help with sleep and getting that help are two different things. While 70 million Americans suffer from sleep disorders, there is a scarcity of sleep doctors and specialists to meet that need. Patients, desperate for help, end up going to their GP and getting prescribed sleeping pills that are hard to quit and have long-term negative health implications. Or, taking matters into their own hands, people try melatonin, alcohol, Benadryl, or whatever will help them turn off at night. Sleep, however, is like sand. The harder you try to grasp it, the more it slips through your fingers.
Sunny Liang knows what it’s like to grapple with sleep. A lifelong insomniac, he can remember walking into his parents’ room at three in the morning to tell them he couldn’t sleep as young as third grade. Over the years, his insomnia came and went, triggered by life changes, envi-
ronments, and different stressors. Then he started his career on Wall Street as a private equity investor.
“It might just be the worst profession for an insomniac. I was on call 24/7. When I tried to sleep, it became a psychological snowball — you’re so anxious about getting sleep you can’t get sleep.”
Eventually, Liang saw a sleep doctor (he now knows he’s one of the lucky few with access to one). It was at that 2018 appointment that he encountered CBT-I, cognitive behavioral therapy for insomnia. CBT-I examines what behaviors, thoughts, and feelings might be contributing to insomnia and helps people restructure their actions and attitudes for better sleep. It’s a combination of sleep hygiene tools — like cutting off caffeine by a certain time a day — and tools to reduce anxious thoughts about sleep itself.
For the first time, Liang understood what he could change in his life to help with his insomnia. Putting it into practice proved more difficult. He left the appointment with a 40-point checklist and resorted to Post-it notes around his desk and apartment to remind him to do things like stop looking at screens by a certain time or make sure he got some fresh air and sunshine. It took time, but his insomnia got better. Understanding how sleep worked and the fundamentals about what created better sleep did what no amount of melatonin could.
Perhaps all those good nights of sleep helped Liang dream up the idea to bring CBT-I tools and interventions to the millions of people struggling with sleep like
he did. His Post-it note experience certainly helped him understand the very human struggles in doing CBT-I, specifically keeping track of the behavioral interventions that promote good sleep. What people needed, he thought, was a sleep coach in their pocket, something that took into account their unique lives, schedules, and sleep challenges and provided customized support.
Zen Sleep is a comprehensive sleep coaching platform that leads users towards better sleep using personalized routines and interventions based on the principles of CBT-I. It helps its users build better sleepy hygiene habits — the behavioral side — while addressing the cognitive challenges to good sleep like stress and anxiety through guided meditations and access to a real-life sleep coach. Along the way, Zen Sleep incorporates data from a user’s wearable devices to track progress and changes, leveraging the data to guide next steps.
“We’re not here to compete with wearables, but to partner with them and provide wisdom and an actionable plan for the user based on their numbers from these devices,” explains Liang.
The process starts with a detailed questionnaire — developed with Zen Sleep co-founder and board-certified sleep physician Neil Klein, MD — that zeroes in on choices, practices, and attitudes that impact sleep. The app then integrates seamlessly with the user’s wearable device, if available, to do a deep dive into its metrics
to create a suggested daily routine. Backed by its proprietary AI, Zen Sleep creates an automated reminder and suggestion system, available 24/7 to support better sleep habits and hygiene. Additional coaching and help comes by connecting to a sleep coach, who can access a patient’s data from the app to provide next-level insight based on real numbers.
It’s a thoughtfully tiered solution that uses technology to help people disengage from technology for better sleep. For Liang, it’s been most gratifying to see customers who had given up hope for better sleep see improvements. He describes one user case, a middle-aged woman who was the third generation in her family to rely on sleeping pills. She worried about the long-term effects, but after ten years of use, the pills seemed like a permanent part of her life. She became a beta tester for Zen Sleep and has slowly decreased her Ambien use. For the first time in a long time, she has hope.
In the year ahead, Zen Sleep looks to partner with large employers and insurers who want to incentivize sleep for employees. Businesses are starting to wake up to the fact that rested employees are healthier, more productive, and less likely to call out of work. In fact, it’s estimated that employers in the United States lose $3,000 per employee in absenteeism due to sleep issues, contributing to the estimated $400B in GDP lost because of poor sleep.
“It used to be that insurers didn’t pay any attention to sleep but that’s starting to change. They ask if you smoke or drink but not about your sleep, and it’s connect-
ed to so many health outcomes.”
StartUp Health proudly backs Zen Sleep’s innovative CBT-I delivery system that offers drug-free relief to millions of people suffering from sleep disorders. Better sleep without the use of sedatives is not only a dream come true to those patients but offers long-term health benefits and savings costs. Despite the growing pile of evidence on the importance of sleep for health, it’s a relatively untapped market, positioning Zen Sleep well as a potential leader in the sleep tech market.
Not only are they poised to lead the way in sleep coaching technology, Liang and his team’s partnership mentality sets them apart from other sleep products. They aren’t competing with wearables or other tracking devices — they’re providing the wisdom around those metrics for their users. It’s one thing to know your sleep trends; it’s a very different thing to know how to change them for the better and be held accountable to do so.
Changing your behavior is hard. Zen Sleep knows this and created a user experience that goes deep to establish new routines, new patterns, and new ways of thinking about sleep. The individualized plans for each user take into account their real-life schedule and challenges, and the original content, CBT-I lessons, and community help change ingrained thoughts and anxieties around sleep.
contact:
zensleep@startuphealth.com
A doctor and an expert in hospital logistics have teamed up to create a new platform for automating and digitizing medication tracking in the hospital and during surgery. By eliminating handwritten labels on medications they’re reducing errors and improving life for nurses.

IIt’s well known that healthcare lags behind many other industries when it comes to basic technology upgrades. Medical bills are often sent by mail, in paper form. Requests for patient records often arrive by fax. And nurses have to painstakingly label syringes by hand in order to track what medications have been given.
This last example is an anomaly of today’s out-of-date healthcare system that
many patients are unaware of, but which would doubtless leave them very concerned. Today, when a nurse changes an IV, it has to be labeled, dated, and color coded according to its expiration date, all by hand. Nurses are required to calculate the hours required for each drug in the moment and code them according to the day they need to be changed.
When a nurse goes to the drug cabinet for insulin and pulls the insulin into a syringe, the syringe must then be labeled. While many drugs arrive pre-labeled, 30% are unlabeled and also require additional handwritten labeling. Administering a drug in the middle of surgery, an anesthesiologist must write on the syringe and immediately enter the data, all the while preserving a patient’s life.
Imagine attempting to write legibly on the curved side of a narrow syringe in the middle of surgery. Envision a nurse, moving from patient to patient in an overcrowded hospital, handwriting crucial information on each IV tube, every syringe. This often results in illegible, smudged, smeared information. Or worse, because it’s so difficult and time-consuming, the medication tracking doesn’t happen at all. When that happens, the results can be fatal.
This isn’t a theoretical concern. In one well-publicized case, a man was admitted for a standard procedure. He had two pumps running, neither had been labeled, and one was fentanyl. When the nurse confused the two, he died. In another case, a patient nearly died when an anesthesia provider failed to label a syringe, mixed
up the drug with another, and wrongly administered it.
Medication tracking in the hospital and surgical setting isn’t something that should be analog anymore. Handwriting on syringes and mental math about dosing need to go the way of the fax machine. It’s time for a digital upgrade to the process of medication tracking that makes patients safer and gives nurses the tools they need to succeed and thrive.
That’s the mission behind Vigilant, one of the newest members of the StartUp Health portfolio.
Vigilant was born out of a serendipitous partnership.
It began when Peter Baek, MD, almost made a big mistake. Dr. Baek was actively working as an anesthesiologist when he nearly administered the wrong drug to a patient due to an unlabeled syringe. It shook him up; then as he thought about it longer he realized this problem wasn’t his alone. For a solution to work, Dr. Baek believed it must be easy. If the medication labeling solution could not be completed within a matter of seconds, it wouldn’t be used by overworked nurses. He was well aware of the daily challenge doctors and nurses face as they seek to care well.
In 2016, Dr. Baek decided that he would create a solution himself. As a hobby-programmer, Dr. Baek went to work and founded Vigilant. A few others who had experience with printers, sales, and fundraising joined him in the effort. When the anesthesiologist who had made
a large hospital and, today, this hospital remains their largest customer with over 90 units installed and a compliance rate greater than 99%.
In 2020, Vigilant received its first two patents. During the dawning of the COVID-19 pandemic, CEO Fox Holt joined the team and raised $300,000 in capital. Fox came with years of experience selling printers to hospitals and a background in startup businesses and finance. This initial round of funding allowed the company to expand from anesthesiology to other parts of the hospital. Dr. Baek had developed a product that would make clinicians more productive and effective. Together, they believed that something as simple as a sales pitch for a new printer and labels could save lives.
Given Dr. Baek’s own background, Vigilant’s initial focus was in anesthesiology. Quickly, their product was expanded to serve other areas of the hospital. Vigilant then moved to the ICU, focusing on labels for IV tubes. Now, Vigilant’s products serve the operating room, emergency room, pharmacy, PACU, and beyond. They have developed labeling solutions for every area of the hospital.
The heart of Vigilant’s product is a
Instead of forcing nurses to write and calculate information by hand on the side of a syringe or IV, Vigilant installs a printer and scanner in the hospital that can print labels with all of the information necessary to track a given medication.

Vigilant software is installed directly onto a Honeywell printer. The system comes with a multi-colored series of labels. As a drug is pulled and a barcode is scanned, the software translates the drug name, date and time, and hospital-specific rules for that drug. The clinician’s badge may also be scanned and included on the label. Within two seconds, the label is then printed with this specific information, providing a place for the clinicians initials. The label is simply removed from its backing and placed directly on the syringe, vial, or tube.
An anesthesiologist entering into the operating room chooses the type of surgery, enters the bar code for the set of drugs to be used in that surgery, prints labels, and places each on a syringe. Once the drug is administered, they scan it and the system automatically records it in. A nurse changing an IV simply scans the barcode, prints all three labels, color coordinated according to the day of the week.
Getting started with Vigilant is easy. A new hospital purchases the software-
Envision a nurse moving from patient to patient in an overcrowded hospital, handwriting crucial information on each syringe. This often results in illegible, smudged, smeared information. Or worse, because it’s so difficult and time-consuming, the medication tracking doesn’t happen at all. When that happens, the results can be fatal.

fueled printer for an initial fee of $1,495. Since the solution doesn’t require a network, it can be installed and used right away, without going through the hospital’s IT department. A yearly maintenance fee of $300 covers new drugs and bi-annual software updates. Labels for the printer are purchased from Vigilant at the same price as the old labels. Training takes no more than two minutes.
Over a few short years, Vigilant has made a big splash. They are currently in eighteen of the top forty health systems. With a conversion rate of 92%, Vigilant has discovered that if they can get a pilot into a hospital, it doesn’t come out.
With more than 6,000 hospitals in the United States, the market opportunity is $1.2B, says Fox Holt. Arriving on the market with vast experience and knowledge in
both medications and printing, Vigilant is focused on the details. They know and feel what doctors and nurses need. They intentionally use thermal printers which they know are best for hospitals. The team has thought through every part of the problem and the solution. Their product is a smart design and a necessary fix.
In addition to solving a critical need in medication tracking, Vigilant brings newly-generated data to bear for the hospital system. This helps hospitals level-up their compliance reporting and mine medication analytics for new efficiencies. Bottom line: Vigilant digitizes a side of the healthcare business that has lagged behind for far too long. Formerly-analog medication labels will now be scannable, trackable, and predictable. It’s about time.
contact: vigilant@startuphealth.com
Learn HEALTH TRANSFORMER UNIVERSITY

rolled a decade of battletested lessons into Health Transformer University.
we’ve worked to organize a global army of Health Transformers and partners – the superhero founders and mission-aligned funders passionate about reinventing the future of health – in our quest to solve what many skeptics say is an impossible dream: to improve the health and wellbeing of all people everywhere.
While we are more optimistic than ever about the potential to achieve global health moonshots, and we are proud of our contributions in helping inspire a generation of Health Transformers to solve big health challenges, we have a lot more work to do to drive transformative outcomes.
On the plus side, we have built the world’s first and only ecosystem dedicated to achieving health moonshots and pioneered a collaborative learning model that multiplies the collective power of those building health innovation with the magic accelerant of network effects. We’re learning in real-time from our 1,000+ Health Transformers and the nearly 500 health moonshot companies across
29 countries that are in our portfolio community.
Despite these accomplishments and even with billions of dollars flooding into health technology startups, we are seeing a widening valley of death between the extraordinary health innovation at the early R&D stages and what actually makes it to the essential commercialization phase where great innovation should become accessible and improve health outcomes. Too much transformative health innovation is stunted by legacy business models, outdated regulatory frameworks and the opaque complexities of the healthcare industry.
These hard realities have given us the opportunity to reflect, assess and recalibrate our plans for the future. We have dissected and audited every aspect of our platform to figure out what’s working and where we can improve so that we can make exponential leaps forward. The result is the establishment of a new paradigm, unmatched in the market, in community-driven support and education for healthcare innovation and the people driving it: Health Transformer University.
Universities have always played a critical role in educating the next generation of leaders and advancing knowledge through research and scholarship. They are where we as hu-
mans go to transform and maximize our potential.
They serve as engines of economic growth and innovation, helping to create jobs and develop innovation that benefit society as a whole. Many of the world’s most significant innovations in science, biology and medicine start in universities because they are such powerful catalysts of innovation.
For the past year, we have been busy reimagining and building Health Transformer University, expanding on everything we have learned over the past decade with StartUp Health Academy.
Health Transformer University is for ambitious founders and funders who are working together to solve the biggest health challenges of our time. We are building a global institution and place to collaborate – both virtually and IRL – for people anywhere in the world dedicated to achieving health moonshots. Our university is designed for entrepreneurs and innovators to provide the tools, structures and networks they need to speed up innovation cycles, and build and scale transformative solutions through every stage of growth. Its focus is not only on building health moonshot companies, but on the founders whose mission it is to achieve their transformative endgame.
While there are so many extraordinary academic medical schools and institu-
tions around the world advancing science, technology and biology for the benefit of humanity; there has not been a global university that exists to help educate the world’s Health Transformers on how to achieve a health moonshot and navigate the process of building, commercializing and scaling a health moonshot company.
The first residency program for doctors in the United States was established at Johns Hopkins Hospital in Baltimore, Maryland in 1889. At the time, medical education was not standardized, and many newly graduated physicians lacked the necessary clinical experience to practice medicine effectively.
Just as the first residency program was created to provide clinicians with a structured, supervised training program to prepare them to improve their practice of medicine, we have created a Health Moonshot Fellowship program for Health Transformers to guide them, and a community of like-minded, equally ambitious founders as they build their health moonshot company. The program is designed to bridge the gap between R&D and the grueling journey of commercializing and scaling health innovation.
To make Health Transformer University accessible to as many entrepreneurs and innovators as possible, we are partnering with passionate families, foundations and industry organizations, we call Health Moonshot Champions, to help
We’re taking more than 10 years of battle-tested lessons learned and rolling out the next generation of our platform. It’s called Health Transformer University and it represents our best thinking of the past and a vision for an even more collaborative future.
fund Fellowships in Health Transformer University. This makes it possible for entrepreneurs driving innovation to get access to Health Transformer University’s community-driven coaching and curriculum and StartUp Health’s thought leadership engine and collaboration networks to help them scale.
We hope the success of Health
Transformer University will quickly spread, so that our frameworks and programming become a core curriculum that can be easily added to complement the best university training, medical schools and medical residency programs around the world. Most importantly, we intend to make it available to the world’s best Health Transformers, all the entrepreneurs and in-
novators already working to build health moonshot companies.
Health Transformer University isn’t a traditional university. There’s no ivycovered library or freshmen quad (not this year, at least). It is a purpose-built next-generation university where Health Transformers always have access to the best practical learning tools, peer support, and networks to succeed.
First and foremost, transforming health requires a community of people who gather around common principles and mindsets. This is true for great uni-
In a world full of limited-scope, short-form, quick-hit business advice, we’re building Health Transformer University with longterm transformation in mind. That means being stage agnostic, unbound by time and globally connected.
versities – which are more than the sum of their buildings – and it’s true for us. Health Transformer University isn’t defined by term sheets or cap tables, but by the generations of people who will gather to learn and innovate. That means building networks for faculty, alumni and partners so that we can advance our family of health moonshots. Universities empower communities of people to learn, which in turn enable essential shifts in broader society.
Transforming health also requires focus. Health Transformer University is organized around specific health moonshot themes – not unlike a college major. The goal is to both prepare and organize a global army of Health Transformers on how to tackle complex health challenges through interdisciplinary and innovative approaches. For instance, we’ve recently launched a Type 1 Diabetes Moonshot in order to speed up innovation in this important area. In university parlance, the first step was to choose a dean (our Chief Impact Officer), appoint faculty (our Impact Board) and then begin identifying and selecting students (our Health Transformers who are awarded T1D Moonshot Fellowships).
Transforming health requires long-
term commitment and a longitudinal focus. That’s why the Health Moonshot Fellowship is a three year program, operating on a quarterly rhythm. All universities recognize that gaining mastery in a subject takes time. Learning to grow and scale a health innovation company in today’s complex market is no exception.
Health Transformer University will leverage the passion of a network of like-minded funders. Like the families that have endowed the great universities of our time, “Health Moonshot Champions” invest their financial muscle – and their good name – behind global health initiatives that will change the world. The more partners who support a health moonshot, the more Health Transformers we can grant Health Moonshot Fellowships.
Every great university is driven by a solid curriculum. Ours emphasizes hands-on learning via business building and a collaborative innovation model that unites industry and community partners to ensure Health Transformers are equipped with the skills and knowledge necessary to drive impact.
To transform health we have to track our progress and adjust when necessary. Universities use exams and grades to ac-
complish this. At Health Transformer University we leverage StartUp Health’s system of Health Moonshot Scorecards to make sure that those going through our program are making progress, driving impact to benefit a health moonshot and continually leveling up, no matter what stage their companies are at when they start.
Health Transformer University is guided by core principles – a school charter rooted in a codified set of Health Transformer Mindsets. These mindsets like long-term commitment, collaboration and communication were inspired by the original moon landing in the 1960s, an apt metaphor for breaking down silos to achieve the impossible.
With a focus on developing leaders in the health sector, Health Transformer University is cultivating a global culture of innovation and entrepreneurship that will inspire generations of leaders, builders and innovators to think big and tackle the toughest health problems facing our world today.
In a world full of limited-scope, shortform, quick-hit business advice, we’re building Health Transformer University with long-term transformation in mind. On the business side, that means being stage agnostic, unbound by time and connected globally. It also means getting personal and treating Health Transformers as human beings. We firmly believe in the power of entrepreneurs and their ability to effect change. In fact, we are betting on their ability to do so. We know that
if we can give them a place to learn and grow, supported by a community unlike any other, they will transform health for everyone while thriving both personally and professionally. Health Transformer University is our framework for making this vision a reality.
This is no small feat which is why we have a multi-decade masterplan to expand and scale Health Transformer University, and why we are calling on all those who believe health moonshots are possible to join our mission. Our success depends on more like-minded champions to fund health moonshots, passionate Health Transformers to build health moonshot solutions, and like-minded network partners, faculty and team members to support the mission.
It’s time to get to work. Together, we will show that our dream of improving health for all is possible.

For the last decade co-founders Steven Krein and Unity Stoakes have been leading and shaping the digital health market. They’ve built a mission-aligned team with deep domain expertise and continue to grow their various health moonshots with the top minds in health.
One thing that is so powerful about StartUp Health is the sheer breadth and depth of its network. With more than 450 investments across 29 countries, they’ve truly created the largest, most active, and collaborative digital health ecosystem in the world. This is a rising tide, and the power in these networks shouldn’t be underestimated.
I’ve also been drawn to the unique way that StartUp Health works to inspire, educate, and invest in health tech founders. Through media and community we work to inspire the world to achieve health moonshots. Through masterclasses and office hours and events, we're educating the next generation of health entrepreneurs.
For twelve years StartUp Health has laid the groundwork for 15 health moonshots. Now, there’s a unique opportunity for passionate investors and families to champion a specific global health moonshot and bring it from initial development to exponential progress. Funds are used to educate ambitious founders in Health Transformer University and to invest directly in the most promising breakout companies. It’s a unique double bottom line strategy that is poised to do well while doing a lot of good.
Contact:
elizabeth@startuphealth.com (215) 620-4482
In our year-end StartUp Health Insights report, we explore the factors that could make 2023 a breakout year for early-stage health startups (in spite of gloomy macro-ecomonic trends) and explain why a health moonshot mindset should always involve a long view of the market.
For the latest in health innovation funding go to startuphealth.com/insights-reports
a dramatic decline in venture funding across the health innovation landscape compared to the year prior. While deal volume also dropped, the dip may signal an important opportunity to usher in a transformative phase of progress and create room for a new generation of health moonshot innovation — the kind that leaps us forward in previously unimaginable ways.
betes, and heart disease. The metrics on health outcomes are painful to examine for anyone investing in progress, transformation, and health moonshots as we are.
So why are we more optimistic than ever in the face of such sobering data?
Through history, so many of the great transformations have occurred during and following great recalibrations. And we are in a Great Recalibration.
Ask battle-tested entrepreneurs and innovators and they will tell you this truth: more capital does not ensure better solutions. In fact, some would argue that the noise and frothiness of recent years made it even harder for radically new ideas to get oxygen and traction.
Ask battle-tested entrepreneurs and innovators and they will tell you this truth: more capital does not ensure better solutions. In fact, some would argue that the noise and frothiness of recent years made it even harder for radically new ideas to get oxygen and traction. The momentum of groupthink moves fast with investors and industry alike, and unfortunately we’ve seen first hand how often true innovations get overshadowed and crowded out when the market is at a fever pitch.
Most alarmingly, it’s not only funding that has declined. Health outcomes have also gotten worse by most any measure: life expectancy has gone down, mental health is challenging the world, suicides have skyrocketed, addiction and related deaths are catastrophic as are obesity, dia-
In the post-COVID era of innovation, it’s not certain where the world is going and that can be a good thing. These are the moments when innovators and entrepreneurs lead the way forward and, in our view, when health moonshots not only become possible, but essential.
Here’s some brief insights from the past year and our topline takeaway for why there’s a fresh opportunity for those focusing on transformative solutions for the healthcare industry and people’s health and wellness.
StartUp Health tracked $23.3B in health innovation funding globally, marking a roughly 50% decline over 2021. We saw 857 total deals (down from 1,013), topped by mega-deals for Ultima Genomics in the United States ($600M) and Doctolib outside the US ($549M). The decline in funding, while appear-
ing dramatic within a two-year window, still puts 2022 health innovation funding ahead of 2020, if only by a nose, and continues the upward trend of digital health funding that we’ve been tracking since 2010. Put another way, there was still a tremendous amount of investment into hundreds of businesses; furthermore, with so
many new funds launching in recent years, many investors are sitting on capital they are anxious to deploy.
When we began the process of tracking digital health funding and publishing StartUp Health Insights we were the only company tracking early stage funding data globally. The term “digital health” wasn’t
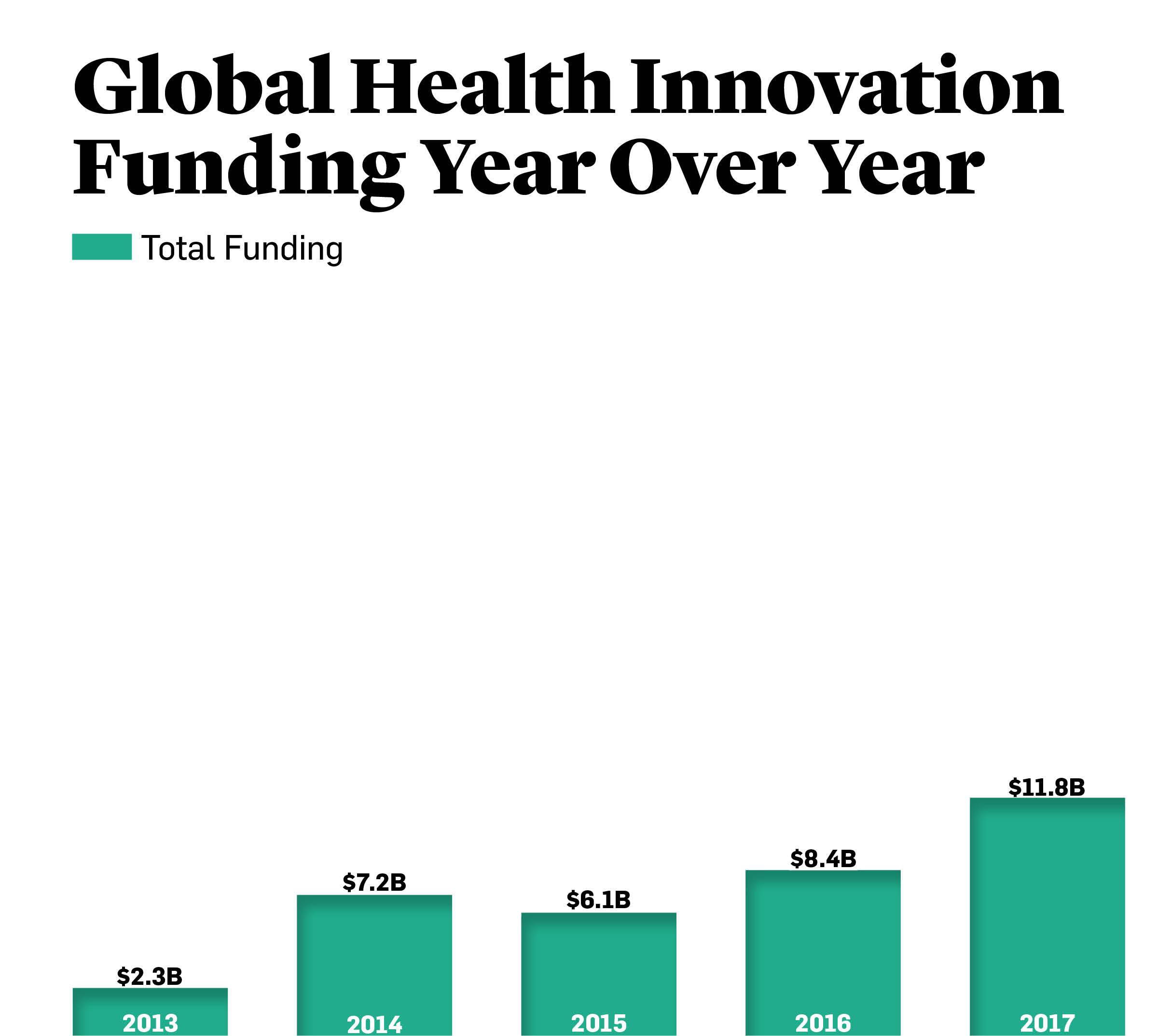
even a category yet.
Day by day, we tracked every deal we could get information on and scoured the internet for health innovation fundraising activity. We didn’t do it to sell data reports. We did it because we believed, passionately, that we were in the early days of a transformation phase we and others called
a moment for the “creative destruction of health” and our “Insights” funding data helped to track the growth of the industry. Most importantly, we used Insights to provide our community of Health Transformers important actionable intelligence they could use to grow their health moonshot companies.
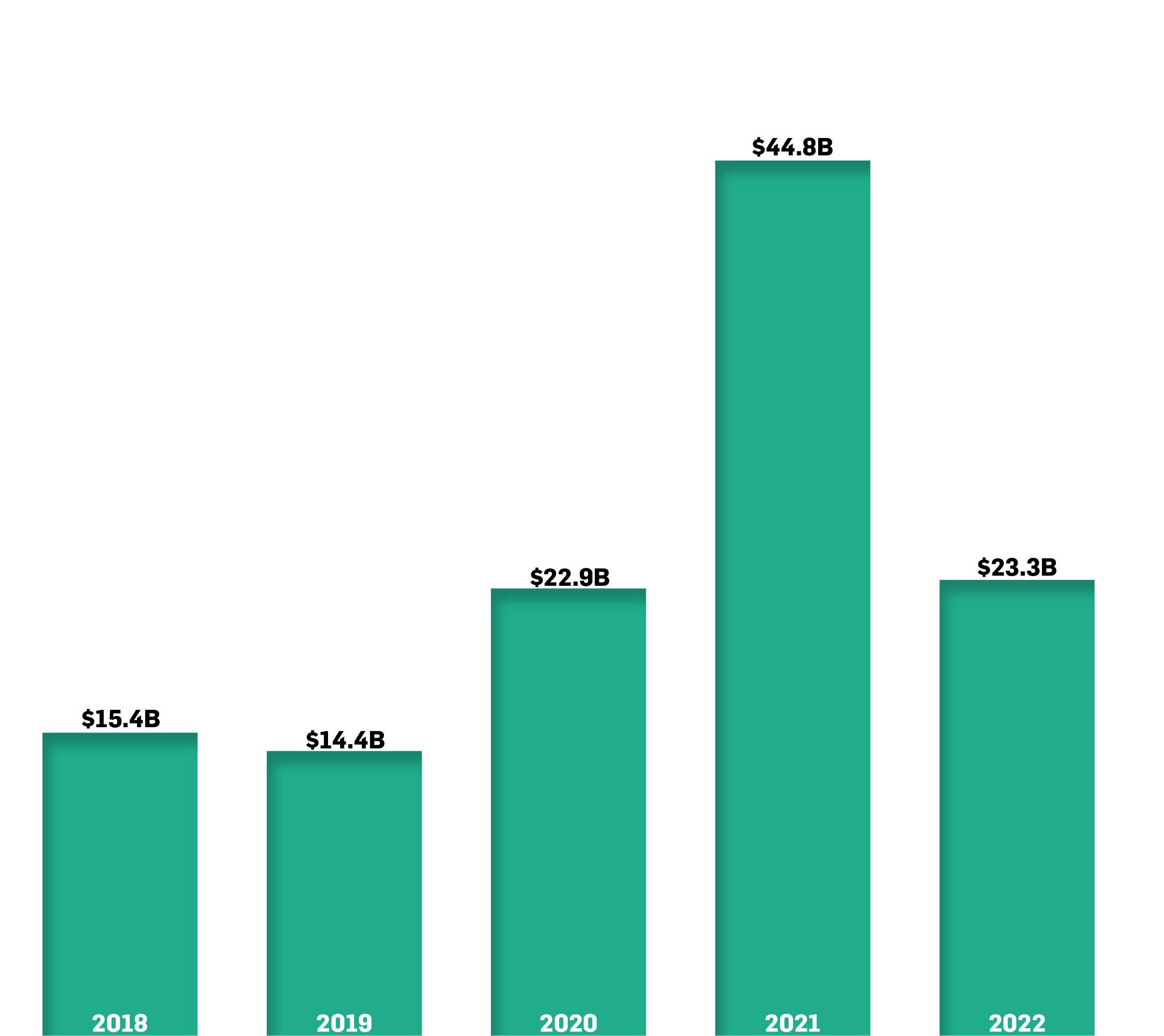
In 2010, we tracked about $1.2B in funding across 151 deals globally. It seems paltry now, but we celebrated these funding rounds, knowing that it was building towards something much, much bigger. At that time, there was no way of knowing that just 11 years later, Devoted Health, a StartUp Health portfolio company, would pull in $1.15B in a single raise.
In our 2014 report, we celebrated that global health innovation funding had grown from $1.2B in 2010 to $7.2B, a six-fold increase in four years. We called it “The Year Digital Health Broke Out.” And it was, though it proved the first of many such milestones.
“The healthcare industry continues to be one of the biggest opportunities for entrepreneurs and investors,” wrote Venrock partner Bob Kocher in 2014. “Today market forces are driving new incentives and paving the way for disruption.” His words remain prescient today.
2014 confirmed our vision that the time was right for a health moonshot mission to empower healthcare entrepreneurs — our Health Transformers — to improve health for everyone in the world. Yet we knew we were still in the early innings.
In 2017, funding jumped to $11.5B globally and we saw more than $2B raised in a single quarter for the first time. Unity Stoakes, StartUp Health’s president and co-founder, called this health innovation’s “second wave.”
Then, in early 2020, COVID-19 hit. The world went to ground and at first investors put deals on ice, waiting to see how
this new paradigm would shake out. But then, the tide turned. It became painfully evident to patients, doctors, and funders that the need for tech-enabled healthcare was upon us and, frankly, a generation overdue. Whether it was telemedicine, virtual clinics, remote monitoring, or health-tracking apps, investors sat up, paid attention, opened up their wallets, and set in motion an exuberant year of health innovation investing. When the dust settled on 2021, we’d tracked a whopping $44B in global health innovation, doubling the amount raised in 2020, which itself was a
strong year.
That brings us to today.
Why this walk down memory lane? Because when we look at the funding numbers from 2022, we can choose to take a short view or a long view. We search to examine the long view of health innovation trends and insights because health moonshots take years, not months. Systems change over time, and yes then all at once. But that “all at once” is a journey in our experience.
Is funding down by half year over year?
Yes. Has health innovation been on a historic, ceiling-breaking upward trend in funding over the last 12 years? Absolutely. Does health innovation recede in importance when investors tighten their belts? No, but it creates an opportunity for recalibration — and critically, for new solutions to rise.
development, and we’re still defining our terms. It’s also a reminder that trends in the United States and globally don’t always align. At StartUp Health, we’ve taken a global lens to health moonshots from day one, knowing that if we’re to meet the greatest health challenges of our time, it’s going to take a collaborative global army of entrepreneurs.
San Francisco, New York and Boston continue to top the charts as the most active hubs for health innovation funding.
Now for a look at some of the important data we’ve looked at in the market. CB Insights reported a 57% decline in digital health funding, year over year, while Galen Growth put the deficit at 41%. Rock Health (which tracks US-only data) and StartUp Health split the middle, showing approximately a 50% reduction in funding. The spread is a reminder that “digital health” is still a market in
According to our StartUp Health data, total deal count is down only 15% year over year, compared with the nearly 50% drop in funding. This suggests a move towards smaller, earlier-stage investments, a trend that was also picked up by Pitchbook in their “2023 US Venture Capital Outlook” report. The report projects that “seed-stage startup valuations and deal sizes will continue their ascent, reaching new annual highs,” because “seed-stage startups are more insulated from public market volatility than their early- and late-stage counterparts…Having just raised their first round of institutional capital, they are farther away from an IPO and can bide their time until paths to liquidity reopen.”
The same sentiment was on display at JP Morgan Healthcare Conference in January, says Unity Stoakes, who noted an increase in early stage M&A activity. “With so many new funds in the market, there is deep interest in making invest-
ments in companies that still have not yet set their valuations during the past cycle,” says Stoakes. “This could signal a positive year for strong companies and teams at the earliest stages of development.” One rationale? With less hype noise and more focus, early-stage healthcare companies with clearly defined solutions have a big opportunity not just to do deals and fundraise this year, but to lean-in aggressively to stand out and gain traction while the later stage companies restructure and recalibrate.
Rock Health concurred in their year-end report: “In the current VC climate, strong horses (earlier stage companies with established product market fit… and paths to profitability) will beat out unicorns, though investors run the risk of betting on the wrong equine.”
So
levels of 2019, more regulatory filings than 2021, and a 1.5x increase in partnering activity.”
The report projects that “seed-stage startup valuations and deal sizes will continue their ascent, reaching new annual highs,” because “Seed-stage startups are more insulated from public market volatility than their early- and late-stage counterparts."
Our conclusion is, maybe unsurprisingly, as optimistic as it was in 2010, but for rather different reasons. We believe that the 2022 decrease in funding for health innovation may usher in a Great Recalibration during which frothy market noise is de creased and great com panies get the attention — and capital — they deserve. It’s a time for macro market recalibration — a shift towards innovations that truly and finally move the needle on health metrics — as well as at the individual startup level. We believe that smart startups will have an opportunity in 2023 to reframe their offering in light of this new market reality and put lasting health moonshot progress back at the center of the conversation.
Rock Health writes that 2022 “signals the tail end of a macro funding cycle” and suggests that 2023 could see a year of rebalancing, with investors preferring “boring” strategies like managing cash and investing in tech infrastructure. Galen Growth took a slightly more positive spin, writing that digital health “showed resilience with funding levels far exceeding pre-pandemic
This report was written and designed by Logan Plaster based on data collected and managed by Tara Salamone, Jennifer Hankin, and Nicole Kinsey. Additional analysis by Unity Stoakes, Priya Reddy, Padma Rao, and Josh Cherry-Seto.
To the Health Transformers of the world: We created StartUp Health to help you, the entrepreneur, thrive, scale and ultimately achieve health moonshots.
StartUp Health is educating, inspiring, and investing in a global army of Health Transformers to achieve health moonshots. Since 2011, we have supported nearly 500 innovative health companies.

Entrepreneurs, learn how you can get the support of the world's largest health innovation ecosystem startuphealth.com/gettingstarted
Investors, learn how you can become a Health Moonshot Champion moonshots@startuphealth.com
The HLTH conference has taken the health innovation market by storm, becoming a must-attend event in the United States in just a few short years. In June 2024 they'll expand across the pond with HLTH Europe, first landing in Amsterdam. We caught up with Katy Fryatt, Managing Director of HLTH Europe, to learn about the opportunity they see for creating space for new global partnerships.
Can you tell us more about the vision behind HLTH Europe and how it differs from other healthcare events in the industry?
Katy Fryatt: Building on the incredible success of HLTH in the US, HLTH Europe is taking the winning HLTH Inc. formula and adding a local team to build what we believe will be Europe’s most important event on healthcare innovation.
HLTH Europe will stand out in a few key ways. Firstly, we’ll be bringing together the entire European ecosystem. That means providers, payers, government, lifesciences, medtech, startups, health tech, and investors together at the most senior level. In the US over a fifth of our audience are CEOs or founders. We’ll be bringing those groups together from across Europe, with a key focus on core markets including the UK, Germany, France, the Netherlands, and Scandinavia. It’s a big challenge!

Katy Fryatt: Europe, in many ways, has been market leading in building an infrastructure for health technology adoption in healthcare. From DIGA in Germany to UK’s NICE early evaluation framework for digital, there are lots of great examples of Europe opening up funding for health technology adoption and governments endorsing the role of technology for health.
The European health tech market also presents an exciting challenge for companies. With highly regulated, largely state-run health systems, a growing ageing population and varying funding and reimbursement models, health tech solutions cannot be one-size-fits-all. Companies who are winning in Europe have cracked one country or market and expanded to the next. HLTH Europe will help them do that faster and help others to expand into the region.
Katy Fryatt: There are huge opportunities for American companies in Europe. Many companies coming over choose one local market to start in (such as the UK) and then springboard from there. Anyone looking to do business with ministries of health and government-level procurement should be prepared to understand the different reimbursement and approval models in Europe. Europe isn’t homogenous, it’s a jigsaw of countries, cultures, policies, and people. There’s also an increasing amount of companies with a direct-to-consumer model, although the US is still ahead in terms of the ‘retailifcation’ of health.

At StartUp Health we work to inspire, educate, and invest in entrepreneurs who are working to address health moonshots –the greatest health challenges of our time. By organizing our portfolio around these global goals, we encourage collaboration and long-term thinking.
ACCESS TO CARE
COST TO ZERO
DISEASE PREVENTION & CURES
END CANCER
WOMEN'S HEALTH
CHILDREN'S HEALTH
NUTRITION & FITNESS
BRAIN HEALTH
MENTAL HEALTH & HAPPINESS
HEALTHY LONGEVITY & AGING
ADDICTION & OPIOID CRISIS
PANDEMIC RESPONSE
TYPE 1 DIABETES
HEALTH EQUITY
ALZHEIMER'S DISEASE


Together we can deliver quality care to everyone regardless of location or income
Founded in 2017, Cityblock Health is a value-based healthcare provider for Medicaid and lower income Medicare beneficiaries. Cityblock partners with community-based organizations and health plans to deliver medical care, behavioral health, and social services virtually, in-home, and in community-based clinics. They use custom-built tools to support care team operations and member interactions. Cityblock serves more than 100k members across six states and Washington DC. Partners include EmblemHealth, ConnectiCare and CareFirst. Cityblock Health is #29 on Fast Company’s list of the World’s 50 Most Innovative Companies of 2023.


















 (Acquired by Press Ganey)
(Acquired by AmWell)
(Acquired by Sharecare & Generali)
(Acquired by Press Ganey)
(Acquired by AmWell)
(Acquired by Sharecare & Generali)
Together













 Ed Park CEO & Co-founder
Ed Park CEO & Co-founder



Devoted Health, founded in 2017, is an all-in-one healthcare company on a mission to dramatically improve the health and well-being of older Americans by caring for every person like family. Members of the company’s best-in-class MA insurance plans are also able to receive care through Devoted Medical, the first virtual and in-home medical group built from the ground up to serve the specific needs of the Medicare population. Devoted now serves over nearly 125k members and operates in 13 states.


Together we can rid the world of disease















9amHealth offers a seamless, virtual solution to people living with Type 2 diabetes, prediabetes, high blood pressure, and high cholesterol. The personalized membership plans include same-day prescriptions with at-home delivery and at-home labs, unlimited virtual access to medical experts, lifestyle guidance, and more. 9amHealth was founded in 2021 by the team behind mySugr, and is backed by 7Wire Ventures, Human Capital, Founders Fund, and Define Ventures.
9am Health
SELECT PORTFOLIO COMPANIES




 Frank Westermann
Co-CEO & Co-founder
Frank Westermann
Co-CEO & Co-founder

Together








Gabbi is on a mission to decrease delayed diagnosis of preventable diseases for women, starting with breast cancer. The Gabbi Risk Assessment Model (GRAM) uses artificial intelligence to predict a woman’s two year risk of breast cancer. The Gabbi App provides a risk assessment, personalized action plan, and community support. The company completed a successful pilot with a national payor on the world’s largest claims dataset to train, test, and validate the GRAM, and will be starting a pilot this quarter with a self-funded employer with more than 60k members.


(Acquired by Clarapath)

Together we can improve the health of every woman


Mammha is on a mission to provide a complete and comprehensive maternal mental health solution. Mammha is a web platform that alleviates the burden of in-office or remote screening for maternal mental health, provides patients with real time results, and enables immediate contact with a care coordinator. Mammha has paid pilots with Children's National Hospital, March of Dimes and Inova Health System in Virginia, and Early Intervention in Maine. From 2021 to 2022, there was nearly a 700% increase in routine physician users. Mammha was a recent winner of HHS’ Racial Equity in Postpartum Care Challenge and HITLAB’s Breakthrough Technology Alliance.














Together we can ensure that every child has access to high-quality care







Alerje is a Detroit-based company developing digital tools for food allergy management. In 2021, Alerje was granted a utility patent for their flagship epinephrine auto-injector smartphone case combo and received a Phase I SBIR grant from the National Science Foundation to develop a platform that collects, analyses, and distributes clinically relevant data to build a bridge between patients and their care teams. Alerje was named one of the best allergy apps by My Allergy Kitchen and was award an investment from the Black Founders Fund by Google for Startups.



Together we can ensure access to food, water and a healthy lifestyle

Edamam organizes the world’s food knowledge and provides nutrition data solutions to health, wellness, and food businesses. Using a proprietary semantic technology platform, it delivers real-time nutrition analysis and diet recommendations via APIs. Edamam has built the most extensive recipe database in the industry with 5M+ recipes and 800k individual foods, each tagged for 40+ diets and 130+ nutrients to address over 200 chronic conditions. More than 90k companies have subscribed to Edamam’s APIs. Clients include Nestle, Microsoft, Amazon, New York Times, The Food Network, Hearst, Barilla, and Ocean Spray.












Together we can unlock the mysteries of the brain to improve health and wellbeing








 Renee Ryan CEO Cala Health
Renee Ryan CEO Cala Health

Cala Health, a bioelectronic medicine company transforming the standard of care for chronic disease, was founded in 2014 as a Stanford University spinout. Their lead product the Cala Trio, which received FDA de novo clearance in 2018 and 510(k) clearance in 2021, is a wrist-based wearable that uses electrical stimulation to temporarily relieve tremor symptoms. The 40 minute treatment sessions are individually calibrated to the patient's unique brain signal pattern. A recent post-market surveillance study of the Cala TAPS therapy found that the Cala Trio device reduced patients’ tremor power by 71% with no loss of effect over time.
SELECT PORTFOLIO COMPANIES
Together we can connect mind, body, and spirit in the pursuit of wellbeing
PORTFOLIO SPOTLIGHT










Arcade Therapeutics (fka Wise Therapeutics) uses breakthrough neuroscientific research to improve mental health through casual, accessible mobile games. To date they’ve completed seven NIH backed placebo controlled clinical trials on its “hyper casual” mobile gamebased cognitive training method. Research collaborators include NYU Langone Health, Weill Cornell Medicine, CUNY, and Soterix Medical. In 2022, Arcade was named a UCSF Health Hub Digital Health Rising Star in the Mental & Behavioral Health category.





SELECT PORTFOLIO COMPANIES

Together we can add 50 healthy years to every human life
Satish Movva CEO & Founder CarePredict
CarePredict's mission is to help caregivers of seniors take timely action in any care setting. Their unique multi-function platform caters to senior living operators, valuebased care systems, RPM/CCM services providers, and families. According to research that studied 500 seniors over a two year period, the data collected through CarePredict’s wearable devices was able to reduce hospitalizations by nearly 40% and reduce falls by nearly 70%. CarePredict's remote patient monitoring solution, CareGuide, was named a CES 2023 Innovation Award Honoree, marking the third time the company has received recognition from CES.

SELECT PORTFOLIO COMPANIES










Together we can end addiction and the opioid epidemic
Quit Genius is the world’s first digital clinic for treating nicotine, alcohol, and opioid addictions. Built on the evidencebased practice of Medication-Assisted Treatment (MAT), Quit Genius combines virtual behavioral therapy with approved medication and connected devices to help employers tackle the high cost of addiction in the workplace while improving the lives of their employees. To date, Quit Genius has helped more than 750k people quit their addictions and has published nine peerreviewed studies.

SELECT PORTFOLIO COMPANIES










 Yusuf Sherwani, MD CEO & Co-founder
Yusuf Sherwani, MD CEO & Co-founder
Together we can prevent, mitigate, and manage pandemics
 Cristian Pascual CEO & Co-founder Mediktor
Cristian Pascual CEO & Co-founder Mediktor

Mediktor is the most accurate AI medical assistant for triage and prediagnosis, directing patients to the right level of care. Their SAAS white labeled software is ready to be embedded into any interface and has been clinically validated with a success rate of up to 91.3% in trials with real patients. Initially created in Barcelona, Spain, Mediktor’s technology is available in 15 languages and the company is established in more than 25 countries, serving 10M+ users. Columbia Memorial Health in New York, serving more than 100k residents, recently launched the region's first digital "symptom checker" powered by Mediktor.
SELECT PORTFOLIO COMPANIES











Launched: 2022
T1D Moonshot Impact Board:
Currently accepting applications for T1D Fellowships. Email t1d@startuphealth.com for details.
david weingard, Founder & Chairman, Cecelia Health; T1D patient & advocate; Chief Impact Officer, T1D Moonshot
david panzirer, Trustee, Helmsley Charitable Trust
aaron kowalski, phd, CEO, JDRF International
jennifer sherr, md, phd, Professor, Yale School of Medicine
mike mason, SVP & President, Lilly Diabetes
sarah oltmans, Chief of Grant Strategy, Robin Hood
robert oringer, Chairman & Board Director, AMG Medical
albert tzeel, md, Regional Vice President, Humana
claudia graham, phd, Former SVP of Global Access, Dexcom; Board of Directors, JDRF
norma kenyon, phd, Deputy Director, Diabetes Research Institute; CIO, University of Miami School of Medicine
Contact:
T1D@startuphealth.com
Launched: 2022
Health Equity Moonshot
Impact Board:
kaakpema "kp" yelpaala, Founder, InOn Health; Chief Impact Officer, Health Equity
Moonshot
aletha maybank, md, mph, Chief Health Equity Officer & SVP, American Medical Association (AMA)
chris gibbons, md, mph, CEO & Founder, The Greystone Group
félix manuel chinea, md Health Equity & Inclusion
Strategy, Doximity
additional members to be announced
Contact: healthequity@startuphealth.com
Launch Schedule:
Launching 2023
Alzheimer's Moonshot
Impact Board:
mylea charvat, phd, Former CEO, Savonix; Fellow, Stanford Neuroscience
phyllis barkman ferrell, Global Head of External Engagement, Alzheimer’s & Neurodegeneration, Eli Lilly
meryl comer, Co-founder, UsAgainstAlzheimer's craig ritchie, md, phd, CEO & Founder, Scottish Brain Sciences
braden bishop, Founder of 4MOM Charity; Professional Baseball Player
peter kash, edd, Co-founder, Belum Therapeutics
Contact: alzheimers@startuphealth.com
DR. NATALIA KANEM has used her position as executive director at the UN Population Fund to fight genderbased violence and lower maternal mortality around the globe.

