
9 minute read
Sustainable biomaterial face shield
Sustainable biomaterial face shield system developed for the NHS
A West Midlands manufacturer is leading the field in the development of sustainable high-quality, British-made PPE with Optec – a new biomaterial reusable face shield system designed to help the NHS reach its carbon emission reduction targets.
At the start of COVID-19, the urgent need for safe and comfortable PPE to protect frontline healthcare workers enabled British manufacturing to demonstrate incredible agility. But it simultaneously raised concerns about the environmental impact of more disposable commodities. In fact, in a recent survey carried out by Tecman, 90 per cent of the 156 healthcare workers surveyed communicated growing concerns about the environmental impact of PPE.
Tecman’s product lines help to address these concerns, due to their compact packaging and innovative processes saving tonnes of waste compared to other products on the market. All of their products are underpinned by their Four Pillars of Comfort, which ensure comfort to the wearer across four key areas – feel, performance, sustainability and cost.
However, Tecman’s latest development goes one step further and tackles sustainability concerns head on. The Optec reusable face shield system from the Leamington-based company uses biomaterials made from sustainably forested trees, manufactured with low carbon footprint processes. This biomaterial reusable design with cleanable screens vastly reduces plastic waste.
With this new, more sustainable protective face shield system, Tecman has responded to the government’s recommendations for reusable PPE and has been developing the eco-friendly face shield alongside the NHS.
Benefits of Tecman’s new biomaterial reusable face shields include:

l Supports NHS targets for carbon reduction l Reusable biomaterials reduce plastic use and environmental impact of PPE l Sustainably managed solution reduces pressure on waste management l Easy to clean whilst minimising bacteria build-up l New ergonomic design for improved wearer comfort and protection l Cost-effective with a low price per wear l Cleanable screens for a more sustainable product
Leading the way in Britishmade PPE
Since spring 2020, the Tecman team has been on a mission to make Britishengineered protective visors the number one choice for NHS workers and has been working closely with the NHS ever since.
As part of this drive, the company invested over £500,000 in state-of-the-art machinery which enabled them to boost production of their protective face shields to over 1 million units per week. Their efforts were rewarded when, in June 2020, their original face shield became one of the first to receive the sought-after category III complex design PPE level. In recognition of the product’s quality and comfort, the company’s face shield is specified by the NHS in its product framework and catalogue, and has already been used by hundreds of thousands of frontline healthcare workers.
Tecman have been running hospital trials for Optec and incorporating wearer feedback on comfort, safety and durability into its final round of improvements, ensuring it is optimised for the best possible wearer experience.
A boost for the UK economy
The West Midlands-based company currently exports its protective face shields throughout Europe, and has been working with global organisations such as UNICEF and the World Health Organization (WHO) to ensure production remains at peak levels.
“We’ve worked hard alongside the NHS to develop a more sustainable reusable faceshield system which is competitive on price and quality whilst providing ecological benefits, and we’re delighted with the results. Optec has been well received by the healthcare sector and we’re working closely with the DHSC to ensure it’s fairly considered in their next procurement process. Optec addresses rising concerns about the environmental impact of PPE, provides value to the NHS, and prioritises wearer comfort and the safety of our vital healthcare workers.”
Kevin Porter, Tecman’s Technical Director
Precision medicine biomarkers for early detection of ‘immunofrailty’
Nina Skorytchenko and Dr Daryl Fernandes, CEO and CSO of medtech startup Avenna, discuss a novel approach to prediction of serious inflammatory episodes in inflammatory bowel disease (IBD) and COVID-19 using prodromal glycomics signals from blood immune system glycoproteins.
COVID-19 and IBD are inflammatory diseases (IDs) that cause considerable sickness and death across the globe. COVID-19 deaths now exceed 2.4 million while diagnosed IBD patients total around 11 million, with both numbers increasing. Neither disease has a cure, nor are there any dependable tests for either condition that allow medics to predict which patients will suffer the worst health outcomes. Consequently, medical intervention for these IDs is largely reactive, kicking in only after tissue and organ damage has occurred. The illnesses do run with very different timeframes. COVID-19 is an acute ID that kills within weeks, while IBD is a chronic ID that exerts progressive damage to the gut over many years.
As part of our work on personalised precision medicine for IDs, we have been studying changes in the glycomics patterns of blood immune components in IBD and COVID-19 patients. The results indicate that those affected by either disease share some common underlying aetiological pathways correlating with immune dysfunctions. We call these ‘immunofrailty pathways’ and the resulting degradation of immune fitness ‘immunofrailty’. We are now exploiting use of blood glycomics patterns as metrics of immunofrailty, with the aim of developing reliable early prognostic and predictive biomarkers for COVID-19 and IBD.
The project builds on our Immunofraility Model (IFM). This uses a systems science approach to model the complex and diverse mechanisms of degradation in immune system structure and function in different IDs. IFM considers alterations to: (a) the integrity of skin, mucous membranes of the gut and respiratory systems and vascular endothelium, (b) the occurrence of chronic and acute inflammatory processes, (c) tissue and organ damage, and (d) the glycomics patterns of immune system glycoproteins. From this we propose that: (a) immunofraility is highly complex with multiple causal pathways, (b) immunofraility correlates closely with chronic inflammation, (c) chronic inflammation has both systemic and diseasespecific components, (d) both immunofraility and chronic inflammation typically rise in phases throughout progression of IBD and other chronic IDs throughout the life of each individual, and (e) the most vulnerable COVID-19 patients are immunofrail individuals who mount disordered immune responses after SARS-Cov-2 infection due to dysfunctions in their innate and humoral immune systems.
If these are true, then tracking changes in system and disease-specific chronic inflammation processes, particularly at early stages of inflammatory episodes, is key to prognosis and prediction in IBD and COVID-19. However, current biomarkers of inflammation such as hs-CRP and interleukin-6 cannot measure chronic inflammation because of interference from acute inflammation. This is like trying to measure climate change but failing because the weather gets in the way.
GlyHealth, our family of medical glycomics biomarkers, changes this picture for ID medicine.
The glycomics patterns are prodromal signals which presage the inflammatory storms that lead to morbidity and death in IDs. This means that GlyHealth tests give early warnings of vulnerability to poor health outcomes from inflammatory diseases.
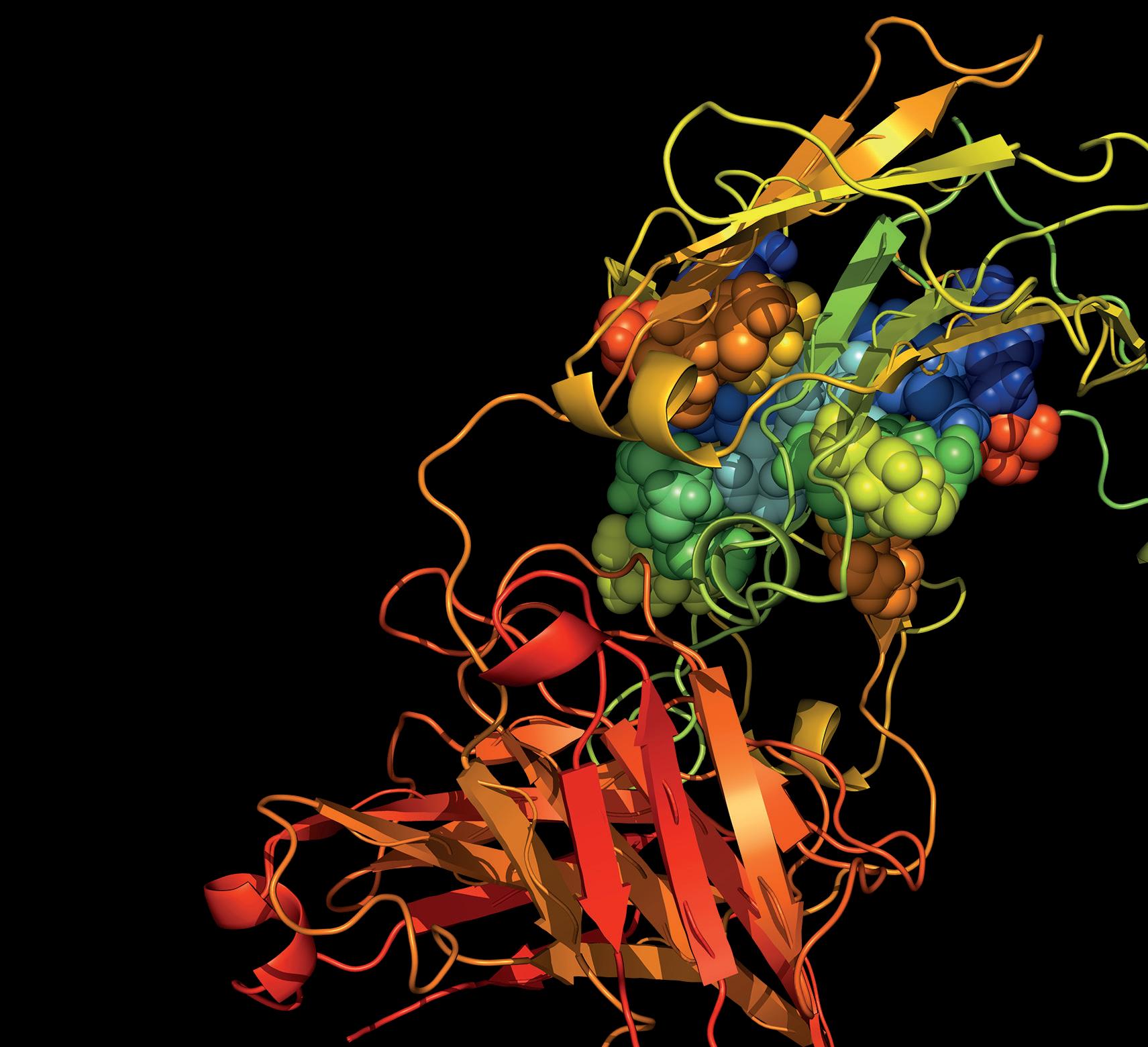
The technnology is an In-vitro Diagnostic platform designed to reliably measure IF and chronic inflammation in individuals from changes in the glycomics patterns of immune components in their blood. Unlike current inflammation markers, this is done without interference from acute inflammation and seems to work reliably even at very early subclinical stages of IDs. The glycomics patterns we measure are complex, information-rich prodromal signals which presage inflammatory episodes that lead to morbidity and death. This early warning can buy critical time for patients and the medics who care for them. This is seen in GlyHealth-IBD, the most advanced of the GlyHealth variants in our development pipeline.
Avenna has been working in collaboration with its sister company, Ludger, and Translational Gastroenterology Unit (TGU) at the University of Oxford to further develop and commercialise GlyHealth technology. GlyHealth-IBD is a prognostic and predictive biomarker to support clinical decision-making in IBD. This followed our discovery that IBD patients have aberrant blood plasma glycomics patterns that correlate with IBD-specific inflammatory processes. Preliminary studies on over 400 patients showed that GlyHealth-IBD reliably estimated IBD severity, future disease course and future need for treatment escalation in newly diagnosed IBD patients up to 18 months from testing. The tests were able to predict IBD disease severity with ROC sensitivity and specificity scores in the range 0.88 - 0.92 (a perfect score is 1.0) compared to hsCRP and albumin with a combined score of 0.57 (0.5 is the lowest possible score). The studies and method are described in our paper ‘Serum N-Glycomic Biomarkers Predict Treatment Escalation in Inflammatory Bowel Disease’ submitted to Nature Comms.
GlyHealth-COVID is based on GlyHealth-IBD technology and is being developed to identify immunofrail individuals likely to suffer serious inflammatory episodes if they were to be infected with SARS-Cov-2 virus. The first phase of this is being funded as part of the UKRI initiative for research addressing COVID-19 with blood samples from individuals from the UK, Europe and the US. These include patients who have suffered COVID-19 as well as various types of control groups. The preliminary results look interesting. However, the data is very complex and we must do much more work before we can make sense of the relationships between all the variables which include age, sex, ethnicity, blood glycomics patterns before, during and SARSCov-2 infection, health outcomes from COVID-19, known pre-existing chronic diseases and preexisting sub-clinical chronic conditions.
Our next steps involve expansion of existing work, as well as conducting detailed N-of-1 lifecourse studies on immunofrailty and health outcomes in individuals. Our study would ideally include IBD patients as well as those without IBD who either have or will contract COVID-19. The study would require access to detailed information on the development of each person’s inflammatory state to date as well as prospective longitudinal measurements of their blood GlyHealth profiles now and several years into the future. The idea is to map changes in their blood glycomics patterns that could be potential prodromal markers of future alterations to their state of immunofraility. The results of this study should allow us to update IFM and further refine our models for prognosis and predictive of inflammatory events in IBD patients. Further studies on GlyHealth-COVID and, if it is possible, developing it into a practical tool to aid clinical management of COVID-19 patients are high priorities for us. To advance these projects ,we are applying to tap into UK medical research resources such as Gut Reaction, the NIHR Health Data Research Hub for IBD, as well as expanding our network of collaboration partners including clinicians and patient groups. Financing the R&D is a critical issue too and we are exploring ways we can access funding for specific parts of these precision medicine programmes.
Avenna specialises in early detection, prevention and treatment of both chronic IDs and acute IDs. In partnership with sister company Ludger, they are developing glycomic blood biomarkers to enable personalised preventative approach for inflammatory bowel disease and COVID-19. Avenna is looking to collaborate with forward-thinking clinicians and biopharma companies who are working in this field.











