LEWIS KATZ SCHOOL OF MEDICINE AT TEMPLE UNIVERSITY | TEMPLE UNIVERSITY HEALTH SYSTEM
SUMMER 2019
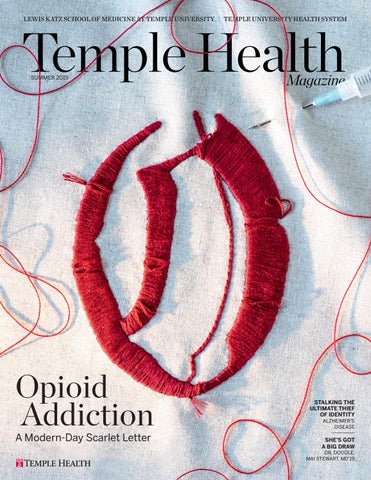
Opioid Addiction A Modern-Day Scarlet Letter
STALKING THE ULTIMATE THIEF OF IDENTITY ALZHEIMER’S DISEASE
SHE’S GOT A BIG DRAW DR. DOODLE, MAI STEWART, MD’19