Nurses Driving Change and Creating New Avenues for Growth
GAINING TRACTION
texasnurses.org
NURSING MAGAZINE TNA: Empowering Texas Nurses to advance the profession | Issue 1, 2024
TEXAS
ISSUE 1, 2024
Volume 98, Number 1
EDITOR IN CHIEF: Serena Bumpus, DNP, RN, NEA-BC
MANAGING EDITOR: Julia Menegay
COPY EDITORS: Natalie Hill, Gabi Nintunze
4807 Spicewood Springs Rd., Bldg 3, Suite 100, Austin, TX 78759-8444
P: 800.TNA.2022 or 512.452.0645; F: 512.452.0648
tna@texasnurses.org | texasnurses.org
MISSION
Empowering Texas Nurses to advance the profession
VISION
Nurses transforming health
TEXAS NURSING (ISSN 0095-36X) is published quarterly— Winter, Spring, Summer, Fall—by the Texas Nurses Association, 4807 Spicewood Springs Rd., Bldg. 3, Suite 100, Austin, TX 78759-8444 Periodical postage is paid in Austin, Texas.
One-year subscriptions: $30 (nursing schools, libraries, hospitals, non-nurses, out-of-state nurses), foreign $35; single copy $3.00. Subscription is not available to non-member Texas nurses. Some back issues may be viewed online at texasnurses.org
PUBLISHING PARTNER
Monarch Media & Consulting, Inc.
P: 512.680.3989 or 512.293.9277; F: 866.328.7199
monarchmediainc.com | chellie@monarchmediainc.com
Advertising inquiries: call Chellie Thompson at 512.293.9277.
TEXAS NURSING is indexed in The Cumulative Index to Nursing and Allied Health Literature and in the International Nursing Index. 16mm, 35mm microfilm, 105mm microfiche, article copies available from University Microfilms International: 1.800.521.3044.
Statements of fact and opinion are made on the responsibility of the authors alone and do not imply an opinion on the part of the officers or the membership of TNA.
POSTMASTER
Send address changes to TEXAS NURSING , 4807 Spicewood Springs Rd., Bldg. 3, Suite 100, Austin, TX 78759-8444.
ARE YOU MOVING?
Need to change your address? If so, provide it quickly and easily in the Members Only section of the TNA website, texasnurses.org Or mail your new address—at least six weeks prior to your move— to Texas Nurses Association headquarters. We’ll make sure your TEXAS NURSING makes the move with you.
FEEDBACK EMAIL OR LETTER GUIDELINES
TEXAS NURSING will select emails/letters on the basis of readership interest and relevance to current nursing/health care events. TEXAS NURSING reserves the right to edit all letters. Guide: Limit to 200 words; focus on single issue; include writer’s name, mailing address, and daytime phone. Send to: editor@texasnurses.org
Copyright 2024 © Texas Nurses Association
BOARD OF DIRECTORS
OFFICERS:
Joyce Batcheller DNP, RN, NEA-BC, FAONL, FAAN, President jbatcheller7@yahoo.com
Amy McCarthy, DNP, RNC-MNN, NE-BC, President-elect amccarthyrn@gmail.com
Gloria Lorea, DNP, RN, NEA-BC, Treasurer glorialoeradnp@gmail.com
Missam Merchant, MBA, BSN, RN, CENP, CCRN-K, PCCN, CV-BC, GERO-BC, MEDSURG-BC, NE-BC, Secretary sam.merchant2017@gmail.com
DIRECTORS:
Jose Alejandro, PhD, RN, NEA-BC, MBA, CNE, FACHE, FAAN - Dallas josealexrn@gmail.com
Patricia “Pat” Francis-Johnson DNP, RN, CDP – Lubbock patricia.francis@ttuhsc.edu
Edtrina Moss, PhD, RN-BC edtrina@comcast.net
Brandon “Kit” Bredimus, DNP, RN, CEN, CPEN, CNML, NE-BC, CENP, NEA-BC kit.bredimus@midlandhealth.org
Mary Vitullo, MBA, MSN, RN-BC, PCCN, NE-BC, CLSBB vitullo.mary@yahoo.com
LVN REPRESENTATIVE
Adam Ramirez, LVN, WCN-C, IV-C adamramirez05@hotmail.com
CHIEF EXECUTIVE OFFICER:
Serena Bumpus, DNP, RN, NEA-BC sbumpus@texasnurses.org
TNA DISTRICT PRESIDENTS
Dist. 1: Sarah Yvonne Jimenez, PhD, RN syjimenez2@utep.edu
Dist. 3: Christopher Rougeux, MSN, RN, crougeux99@gmail.com; District office: Jamie R. Rivera, JamieRivera@texashealth.org
Dist. 4: Alaina Tellson, PhD, RN, CLNC, NPD-BC, NE-BC alaina@tellson.net; tnad4.nursingnetwork.com; District Secretary Lori Batchelor, batchelorb@prodigy.net
Dist. 5: Chelsea Vaughan, RN, chelseareneevaughan@gmail.com, tna5.org
Dist. 7: Connie Barker, APRN. PhD. FNP-C, crbarker1@yahoo.com, tnadistrict7@gmail.com
Dist. 8: Nelson Tuazon, DNP, DBA, RN, NEA-BC, FNAP, FACHE, FAAN, nelsonactuazon@gmail.com
Dist. 9: Marco Ollervides, MSN, RN, marco.ollervides@memorialhermann.org
District office: Melanie Truong, RN, Executive Secretary, tna9@tnadistrict9.com, tnadistrict9.com
Dist. 17: Mari Cuellar, NEA-BC, MSN, RN, mari.cuellar@christushealth.org
Dist. 18: Rebecca Clark, DNP, RN, CNE, MEDSURG-BC, rebecca.clark@ttuhsc.edu
Dist. 19: Dixie R. Rose, RN, dixiegtc@gmail.com
Dist. 35: Karen Koerber-Timmons, PhD, RN, CLNC, CNE, NEA-BC, CCRN, RN-BC mkkoerbertimmons@gmail.com
At-Large: Contact TNA, 800-862-2022, ext. 129, brichey@texasnurses.org
TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 2



PAGE 3 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE 5 PRESIDENT’S NOTES Increasing Momentum 6 TNA MEMBER NEWS Kudos Contents IN EVERY ISSUE ARTICLES AND FEATURES 8 WHAT'S NEW AND NEXT Update your Member Profile to Win TEXAS NURSING FIND US ONLINE View this issue and past issues of Texas Nursing in the Texas Nurses app for iPhone and Android. Sign in with your TNA login for free access. 16 ELECTION YEAR INFLUENCE ON TNA'S POLICY AGENDA Inviting Member Engagement Now By Jack Frazee, J.D. 20 NURSING IS SO UNIQUE IT NEEDS TWO UNIQUE IDENTIFIERS While Nursing Has Changed Billing Has Remained the Same By Katheren Koehn MA, RN, FAAN 14 CEO CORNER Full Speed Ahead Leveraging a Framework to Address the Nursing Shortage Thinking Outside of the Box New Year New Offerings By Serena Bumpus, DNP, RN, NEA-BC 8 REVAMP, REFRESH, RETAIN A Collaborative RN-LVN Care Model 18 12 By Adam Ramirez, LVN, WCN-C, IV-C and Mary Lee Potter, PhD, MBA, RN, CWOCN


A LOOK BACK
President’s Notes
Joyce Batcheller DNP, RN, NEA-BC, FAONL, FAAN
INCREASING MOMENTUM Innovation Across the Nursing Industry
In January, most of us do not get much snow or ice, but with the changing weather patterns, we might be concerned if we have enough traction to get to work safely. I have also been thinking of a different kind of traction—the kind that happens when an idea is repeated and becomes a substantive issue. As the TNA Board President, I have traveled the state with TNA’s CEO and other select staff members to meet nurses where they are through our roadshows. TNA represents the voice of nurses in Texas, and the roadshows have provided us an opportunity to understand some of the distinct challenges in various parts of the state and to hear from nurses in all areas of practice. That is creating traction! You may be asking, “What difference is this approach making? What are you hearing and most importantly, what is TNA doing to address the concerns that are being voiced?”
PLANS AND GOALS
The TNA Board worked to create a fiveyear strategic plan, launched in July 2023, that focuses on four unique pillars: sustainability, membership, policy, and the profession. The profession pillar is focused on supporting concerns brought forward at the roadshows. TNA is developing new partnerships with external stakeholders to ensure nurses are practicing in an environment that supports an inclusive and just culture, and promotes a healthy and safe work environment. In addition, new evidence-based programs will launch in 2024 that enhance nurses’ knowledge and ability to help us move the profession forward.
The next steps are critical, and so is understanding how you can help with this important work as we move forward. It is not surprising that the top concerns expressed during the roadshows were related to staffing and workforce needs and increased violence in the workplace. “Fixing” the staffing challenges in nursing requires multiple strategies and multiple key stakeholders.
TNA has seen an increase in membership and in the number of nurses wanting to engage in committees. We have greater diversity of members on both the TNA board and the committees, which is exciting. This diversity has allowed us to develop what I think of as better traction—we understand issues differently and see more solutions and possibilities. All of this enriches what TNA can do and mean to an individual or group and how it is seen in the bigger picture of creating health care policy and practices. However, this does not mean we do not have work to do. In January, TNA will embark on a journey toward becoming a more diverse, equitable and inclusive organization with the help of Dr. Rumay Alexander, who led ANA’s work on racial reckoning and the National Commission on Racism. TNA will begin its own work around DEIB and racial reckoning.
A LOOK AHEAD
For the 21st consecutive year, nurses ranked #1 on Gallup’s annual Most Honest and Ethical Professions poll. Nurses achieved this recognition despite the challenges presented by the lingering COVID-19 pandemic, high rates of flu and RSV infections, staffing issues, increased number of nurses out on strikes and increased threats of workplace vio -
For the 21st consecutive year, nurses ranked #1 on Gallup’s annual Most Honest and Ethical Professions poll.
lence. Despite these challenges, we are still caring for our patients and communities. We are hearing many examples of what nurses are doing right. We need to highlight these examples and share best practices rapidly.
The TNA board and CEO meet with the district presidents quarterly to be sure we continue alignment of goals, to learn from each other and to increase momentum on positive activities affecting members and communities. This continues to create traction across the state. What I really see is the need for more Texas nurses to engage with TNA and become part of the solution for the challenges we need to address—to help us create more traction, and to grow the momentum TNA has continued to build over the past year. Become curious about innovative technologies and share your innovative ideas with others. Participate in your local district meetings, submit the work happening in your organizations for publication in Texas Nursing , and attend TNA’s Annual Conference in San Antonio May 30 - June 1. It will be an incredible opportunity to learn from your peers, network with a broader group of colleagues and discover how you can help the nursing profession continue to gain traction. I hope to see you there. i
REFERENCES
www.nursingworld.org/news/news-releases/2022news-releases/americans-continue-to-rank-nursesmost-honest-and-ethical-professionals/
PAGE 5 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE
TNA MEMBER NEWS
SPOTLIGHT ON YOU
KUDOS
The following members were named among the South Plains Great 25:





Mary Bias , MSN, RN, Magnet Program Director at University Medical Center
Tonya Chapman , MSN, RN-BC, Assistant Director of Nursing at UMC Health System-Observation
Erla Diane Fernandez , MSN, RN, MedSerg-BC, Charge Nurse at University Medical Center
Whitney Haugland , DNP, RN, CEN, CPEN, NEA- BC, Nurse Director at University Medical Center
Julie Wright, MSN, RN, Managing Director, Telehealth and Digital Innovation at Texas Tech University Health Sciences Center





Tiffany Jackson , MSN, RN MedSurg/ICU Director Permian Regional Medical Center
Jordan Juarez , BSN, RN, CCRN, Critical Care Unit Midland Memorial Hospital
The following organizations have received ANCC’s Magnet redesignation:
Michael E. DeBakey VA Medical Center, Houston, Texas
Children’s Health Children’s Medical Center, Dallas, Texas
Congratulations to the Cizik School of Nursing at UTHealth Houston and Memorial Herman-Texas Medical Center for being presented with the 2023 New Era for Academic Nursing Award.
Kristen Nall , MSN, RN, CMSRN, Clinical Manager of the Endoscopy Department
Midland Memorial Hospital
Rene Rodriguez , DNP, RN, Divisional Director of Cardiovascular Services at Medical Center Hospital
The AARP Center for Health Equity Through Nursing and the Future of Nursing: Campaign for Action has awarded Kelly McGlothen-Bell , PhD, RN, FAWHONN the ‘EquityMinded Nurse Rising Star Award’.



The following organizations have received the prestigious Pathway to Excellence designation:
Memorial Hermann Rehabilitation Hospital-Katy, Katy, Texas
Medical City North Hills , North Richland Hills, Texas
Ambulatory Care Services, Harris Health System , Bellaire, Texas
Ascension Seton Northwest, Austin, Texas

The following members were named among the Permian Basin Great 25: Sharon Cannon , EdD, ANEF, RN, Retired Professor and Regional Dean Texas Tech University Health Sciences Center Permian Basin

Shonna Harris , MSN, FNP-C, Family Nurse Practitioner at Ward Memorial Hospital

Megan Gallegos , DNP, BS, RN, NEA-BC, has been named Chief Nursing Officer for Medical City Healthcare McKinney.

The following organization received ANCC’s Magnet designation:
HCA Houston Healthcare Northwest, Houston, Texas
Texas Health Hospital of Frisco, Frisco, Texas

Congratulations to Nelson Tuazon , DNP, DBA, RN, NEA-BC, CENP, CPHQ, CPPS, FNAP, FACHE, FAAN for being selected to receive the American Nurses Association Luther Christman Award. i
TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 6
WHAT'S NEW AND NEXT UPDATE YOUR MEMBER PROFILE
KEEP CURRENT AND WIN!
Keeping your information current with TNA is important to ensure that we can provide the best possible experience to you as a member, based on your needs.
Ensuring your name and credentials updated ensures that you are appropriately identified for name badges, committee listings, and any time we want to acknowledge your contributions to the association.
Demographic information is important because it helps TNA identify members’ expertise for appointments, discussions, presentations, and article submissions. Demographics also assist TNA in providing benefits and programing that appeal to our membership.
IS YOUR EMAIL CURRENT?
Updating your email address allows us to contact you quickly and helps ensure you don’t miss important information. TNA information that is sent electronically includes
Weekly e-Newsletter, TNA Checkup
Monthly Education Digest – coming March 2024
ALLMAN & ASSOCIATES, INC.
CERTIFIED PUBLIC ACCOUNTANTS
INDEPENDENT AUDITORS' REPORT
Call for comments on Policy Council Products
Call for volunteers and nominations for committees, task forces, and the Board of Directors
Monthly Nurse Talks Empowerment Series meetings
Texas Nursing Quarterly magazine–will soon be completely digital
Annual Ballot
And more!
DO IT TODAY AND WIN!
Update your profile during the month of March and YOU COULD WIN A $100 AMAZON GIFT CARD! TNA will give out 1 gift card each week in March to a member who is randomly selected from those who update their profile that week. Winners will receive their gift card electronically (so update that email!) and will be acknowledged in the TNA Checkup. Go to www.texasnurses.org, login and update your profile. Need help? Reach out to Kelsey Krohn, member services coordinator at tna@texasnurses.org or call her at 512/452-0645 x 133. i
In our opinion, the financial statements referred to above present fairly, in all material respects, the financial position of the Texas Nurses Association as of June 30, 2023, and the changes in its net assets and its cash flows for the year then ended in accordance with accounting principles generally accepted in the United States of America.
Current members can log in to view the audit at www.texasnurses.org/page/Financial.

HAVE YOU BEEN GETTING YOUR CHECK UP?
TNA's Check Up E-newsletter provides members with a weekly update on TNA activities, events, conferences, learning opportunities, grant, and scholarship opportunities, and much more.
If you don’t see the Check Up in your mailbox each Tuesday, look in your spam folder. If you still don’t see it, please contact tna@texasnurses.org and let us know!

PAGE 7 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE

Thinking Outside of the Box
Leveraging a Framework to Address the Nursing Shortage
By Serena Bumpus, DNP, RN, NEA-BC
TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 8
What are the factors causing nurses to leave the bedside at such a large rate?
WITH THE DEMAND FOR NURSES exceeding 3.6 million by 2030, we must address the exodus of those leaving the profession. While many have expressed concerns over the baby boomers hitting retirement age and exiting the workforce, the number of RNs aged 65 and older employed in nursing hit its highest level in 2021. Meanwhile, the number of nurses aged 25 to 34 declined 5.2% in 2021. The decline was 7.4% for those aged 35 to 44 years (Haines, 2022). These statistics raise concerns that the shortage may worsen due to who is leaving the profession. Factors that impacted a nurse’s decision to stay in their current position included safe work environments, work-life balance, a caring and trusting team, doing meaningful work, flexible work scheduling, and feeling valued by their organization and their manager (McKinsey & Company, 2023). Nurses with less than ten years of experience placed particular importance on presence of a safe work environment; feeling valued by the organization; compensation; ability to care for family; access to development opportunities, including opportunities for advancement; and education benefits as top factors influencing their decision to stay (McKinsey & Company, 2023).
A PRACTICAL FRAMEWORK
In January 2022, five professional organizations came together to form the Partners for Nurse Staffing, which aimed to create a framework to address the nurse staffing shortages across the country. Known as the Nurse Staffing Think Tank, the partnership included the American Association of Critical Care Nurses, American Nurses Association, American Organization for Nursing Leadership, Healthcare Financial Management Association, and the Institute for Healthcare Improvement. Representatives from these five organizations identified high-priority areas for organizations to maximize their investment in nursing. After three months, they produced actionable strategies that organizations could implement within 12 to 19 months with measurable outcomes.
OVERVIEW OF THE PRIORITY TOPICS AND RECOMMENDATIONS (2022).
PRIORITY TOPIC RECOMMENDATIONS
Healthy Work Environment
Diversity, Equity and Inclusion (DEI)
Work Schedule Flexibility
Stress Injury Continuum
Elevate clinician psychological and physical safety to equal importance with patient safety through federal regulation.
Specialty nursing organizations should investigate evidence related to scope of practice and minimum safe staffing levels for patients in their specialty.
Implement Inclusive Excellence, a change-focused iterative planning process whereby there is a deliberate integration of DEI ideals into leadership practices, daily operations, strategic planning, decision making, resource allocation and priorities.
Build a flexible workforce with flexible scheduling, flexible shifts and flexible roles.
Address burnout, moral distress, and compassion fatigue as barriers to nurse retention.
Incorporate well-being of nurses as an organizational value.
Innovative Care Delivery Models
Implement tribrid care delivery models that offer a holistic approach with three components, including onsite care delivery, IT integration of patient monitoring equipment, and ambulatory access and virtual/remote care delivery. This approach will improve access, patient and staff experience, and resource management, with continuous measurement for improvement and adjustment for sustainability and support. Total
Develop an organization-wide formalized and customizable total compensation program for nurses that is stratified based on market intelligence, generational needs and an innovative and transparent pay philosophy that is inclusive of benefits such as paid time off for self-care and wellness and wealth planning for all generations.


PAGE 9 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE
Compensation
Access the full Think Tank Recommendations Access the Think Tank Gap Analysis Toolkit
These priority topics and recommendations have the potential to be used by organizations to address common causes for nurses’ decisions to leave. Organizations can also utilize the Think Tank’s worksheet, a gap analysis tool they can use to evaluate and implement these recommendations, as well as monitor potential gaps that need to be addressed.
We invite you to share the work you are doing inside your organizations to address the unique needs of your workforce and communities and encourage you to submit your work for publishing in Texas Nursing.
We have made the decision to focus on these themes in 2024 for our annual conference, “Gaining Traction: Nurses Driving Change,” and as the sub-themes of the 2024 issues of our quarterly publication, Texas Nursing Magazine. We invite you to share the work you are doing inside your organizations to address the unique needs of your workforce and communities and encourage you to submit your work for publishing in Texas Nursing. Together we can share best practices and implement these priority topics and recommendations to improve the practice of nursing across the State of Texas. i
REFERENCES
Haines, J. (2022). The state of the nation’s nursing shortage. https://www.usnews.com/news/healthnews/articles/2022-11-01/the-state-of-the-nationsnursing-shortage.

Think tank Impact?
These priority topics and recommendations have the potential to be used by organizations to address common causes for nurses’ decisions to leave .
McKinsey and Company (2023). Nursing in 2023: How hospitals are confronting shortages. https://www. mckinsey.com/industries/healthcare/our-insights/ nursing-in-2023.
Partners for Nurse Staffing Think Tank. (2022). https:// www.nursingworld.org/practice-policy/nurse-staffing/ nurse-staffing-think-tank/.




TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 10





PAGE 11 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE Order yours today! All new for 2024! The Annotated Guide to the Texas Nursing Practice Act includes helpful explanations and background on laws that affect your practice. It’s a resource every nurse should have! Use the QR code to order or visit texasnurses.org/store JOBSEEKERS EMPLOYERS GET SUPPORT AND SAFEGUARD PATIENTS Nurses Helping Nurses If you, a coworker, or a family member need help with a substance use or mental health issue, call the Texas Peer Assistance Program for Nurses. TPAPN case managers provide guidance, support, and monitoring to help nurses recover and maintain their licenses. And TPAPN peer advocates provide an empathetic listening ear. You and those you care about are not alone! www.tpapn.org TEXAS PEER ASSISTANCE PROGRAM FO R NURSES
NEW YEAR NEW OFFERINGS



At the beginning of each year many of us take time to reflect on the previous year and set goals for the new one. The TNA team has been working on programs to increase membership and support our members, and as we move into 2024 we’re pleased to announce new programs available now and in the coming months.
NEW PROGRAMS
LVN Membership
LVNs can now join TNA! Realizing health care delivery is changing quickly, and that LVNs are being pulled in multiple directions to meet the needs of patients across all healthcare settings, the TNA Board of Directors included expanding membership to LVNs as part of our strategic plan. TNA collaborated with the Licensed Vocational Nurses Association of Texas (LVNAT) to create a statewide membership and benefits package for LVNs, and we are pleased to announce that we are now welcoming LVNs to our membership. We hope you will share this exciting news with your LVN colleagues and invite them to join and take advantage of everything TNA has to offer.
New CNE
Members get free unlimited access to CNE! Our professional development team is working hard to create new educational offerings that are timely and relevant to what you do every day, and we are excited to announce our new on-demand education offerings. We currently have over 30 hours of CNE available at no additional cost to our members, including recorded Nurse Talks events, the Texas Nurses Podcast, and new series covering Nursing Advocacy and Preceptor Competence. We continue to add new offerings with modules that are relevant to nursing practice and nursing issues. We hope you will take advantage of what we have to offer.
A. Louise Dietrich Scholarship
You could be eligible for $2,000 in scholarship money! We understand how important advanced degrees are to nurses and have created the new A. Louise Dietrich Scholarship Program. The first round of scholarships will be awarded in Spring of 2024. The scholarship program will fund up to three scholarships for
TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 12



registered nurses who have been a TNA member for at least one year and are advancing their education through an RN-BSN or graduate nursing program. Online applications are open January 15 through March 15. Recipients will be notified in early May. If you are currently in a nursing program, we hope you will take advantage of this benefit and submit an application.
Texas Nursing Magazine
Digital Edition
Texas Nursing Magazine is going green! You may have noticed the 2023 Issue 4 of Texas Nursing Magazine was sent in the digital version as well as print. That’s because this year, to be good stewards of our fiscal and environmental resources, we’re converting to an alldigital publication! The switch will begin with Issue 2, which is scheduled for May 2024. Moving to a digital publication will allow us to provide information in a

The Good, The Bad, The Unknown

timelier manner and will enable us to expand the magazine and include more content for our members. We’re excited about this change and hope you enjoy the new experience.
COMING SOON
We are continuously working on new programs and benefits. In Spring 2024, we will launch a financial wellness program and announce new community engagement partnerships. The financial wellness program will be available at no cost to TNA members. This new member benefit will provide resources and a personal dashboard to help set financial goals and stay on track. Our community engagement partnerships will provide members and districts an opportunity to get involved at the local level to increase awareness of TNA and nurses in the community.
CONTINUING PROGRAMS
We’re also continuing some of the initiatives from last year, including our Nurse Connect Mentor Program, TNA Roadshows and the Texas Nurses Podcast. Roadshows are continuing in 2024, with visits planned in East Texas, the Rio Grande Valley, and Corpus Christi. Dates will be announced soon, so watch your email and social media to register. The Texas Nurses Podcast team was busy in 2023 and released eight episodes in the fall. New and exciting episodes are in the works so watch for those to be released in the coming months!
We hope you’ll take advantage of what TNA has to offer and share the benefits of membership with your friends and colleagues. Most importantly, invite them to join! Texas nurses are stronger together, and we look forward to another great year with out members! i
PAGE 13 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE
texasnurses.org
NURSINGMAGAZINE
TNA: Empowering Texas Nurses to advance the profession |
Issue 4, 2023 TECHNOLOGY
 CEO
CEO
Corner
Serena Bumpus, DNP, RN, NEA-BC
FULL SPEED AHEAD
Reflecting on 2023, Driving into 2024
HAPPY NEW YEAR TEXAS NURSES!
In September 2023, I completed my first year as CEO of the Texas Nurses Association. As I reflect on my first year in this position, there is so much to be proud of, yet I remain humbled and grateful for the opportunity to serve the nursing profession in this capacity. TNA has been hard at work in the last year supporting Texas nurses.
REFLECTING BACK ON MY FIRST YEAR.
Three areas of success stand out for me in my first year as CEO – engagement, visibility, and legislation. In calendar year 2023, we welcomed 5000 new members to TNA. We experienced record attendance at our events with over 600 nurses attending Nurse Day at the Capitol and close to 300 in attendance at our Annual Conference. We met nurses in their hometowns across the state during our roadshows and had the opportunity to be visible and engage with over 1000 nurses in their communities. The 88th legislative session proved to be one of the most successful for Texas nurses in over a decade with the passing of the Workplace Violence Prevention Bill, the money appropriated to address the workforce shortage (both led by TNA) and supported other key legislative priorities such as the workplace violence felony bill, the Texas Advanced Directives Act, expansion of post-partum coverage, and legislation specific to school nurses and APRNs.
Also, TNA filled key staff vacancies which included our TPAPN Program Director, Director of Nursing Practice, and the Director of Nursing Professional Development. Brittney Majefski joined the TNA
family as the TPAPN Program Director in January 2023 while TNA’s Director of Practice, Dr. Laura Kincheloe, and TNA’s Director of Nursing Professional Development, Dr. Jamie Roney-Hernandez, joined us in May 2023. We now have a
high performing team leading important work to support Texas nurses.
LOOKING AHEAD
The Texas Nurses Association recently undertook a months-long strategic planning process with input from the Board of Directors, district presidents and staff. Below are the four pillars of the strategic plan, areas of focus in each, and goals for the future.

OBJECTIVE
TNA’s five-year strategic plan launched in July 2023 at the start of its fiscal year.
SUSTAINABILITY MEMBERSHIP
OBJECTIVE

Demonstrate organizational excellence through stewardship of human, fiscal, organizational, community, and environmental resources.
• Assess internal infrastructure and professional governance model to strengthen the organization’s ability to be nimble and responsive to emerging needs.
• Strengthen organizational finances through the diversification of revenue streams and deficit reduction by 30%.
Grow membership by acquiring, engaging, and retaining members.
• Develop a comprehensive plan to increase membership by 5% annually through collaborative initiatives, development of programs, and innovative recruitment and retention of members.
• Increase the visibility of TNA among members and external stakeholders.

POLICY
OBJECTIVE
Advance the quality and safety of patient care through policy initiatives that optimize professional nursing practice, advance positive nursing practice environments, and promote full use of the knowledge and skills of nurses.
• Develop new partnerships and lead opportunities to strengthen the voice of nursing in all healthcare policy related decisions.
• Increase engagement of the profession to influence and shape health policy in Texas.
• Develop programs and services to advance the knowledge of the nurse’s role in advocacy.
PROFESSION

OBJECTIVE
Optimize TNA’s ability to lead the advancement of the profession through engagement with nurses and others.
• Partner with external stakeholders to ensure nurses are practicing in an environment that supports an inclusive and just culture and promotes a healthy and safe work environment.
• Develop innovative and evidence-based programs and services that address all levels of experience within the profession.
• Engage the public through education and community outreach.
• Increase the recognition of nurses by leveraging partnerships with external stakeholders.
TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 14
Texas Nurses Association Strategic Plan 2023-2028
GOALS GOALS GOALS GOALS FOCUS AREAS Fiscal Responsibility | Governance | Non-dues Revenue | Human Resources | Operational Resources/Efficiencies FOCUS AREAS Value Proposition | Partnership Development | New Member Categories | Member Journey | Communication Efforts | Member Benefits FOCUS AREAS Legislative Initiatives | Coalitions | Member Engagement | Agency Relations FOCUS AREAS Education | Events | Publications | Recognition | Products and Programs STRATEGIC PLAN
The TNA board of directors developed this plan for the association with two key factors in mind – to ensure the sustainability of TNA and grow the organization. My work as TNA’s CEO centers around moving the plan forward through the engagement of volunteer members, the development of strategic partnerships, and ensuring TNA has the resources to carry the plan forward. We are now six months into the strategic plan, and I am excited about the progress made thus far.
Sustainability. TNA has gained traction in this pillar through proposed bylaws revisions on the development of competency-based board positions, reducing TNA’s deficit budget by 15% in FY24 and engaging in a partnership with the University of Houston School of Law to provide an externship for law students on health policy issues.
Membership. At the six-month mark, we successfully re-developed active district status criteria which was approved by the TNA board of directors in early November 2023 and presented to the District Presidents late November. This ensures we have a plan to keep our districts engaged and thriving in the years to come. District Presidents meet with the TNA Board of Directors quarterly. We hit the road and visited nurses in El Paso, Lubbock, Amarillo, Midland, and Odessa with plans to visit the Rio Grande Valley, Corpus Christi, Laredo, East Texas, Abilene, and San Angelo in 2024. Our most exciting work to date is the launch of our LVN membership program. Starting in January 2024, LVNs can now join TNA at the state level!

Policy. In November 2023, TNA held its first Nursing Student Policy Summit with over 300 student nurses in attendance. This event was designed to empower student nurses to engage in the policy process by educating them on how TNA determines its policy positions, TNA members sharing their personal stories and experiences engaging with TNA and advocating for the profession along with hearing from our State Legislators who are also nurses and why it’s so important for nurses to engage in the advocacy process. Another event is scheduled for April 2024.
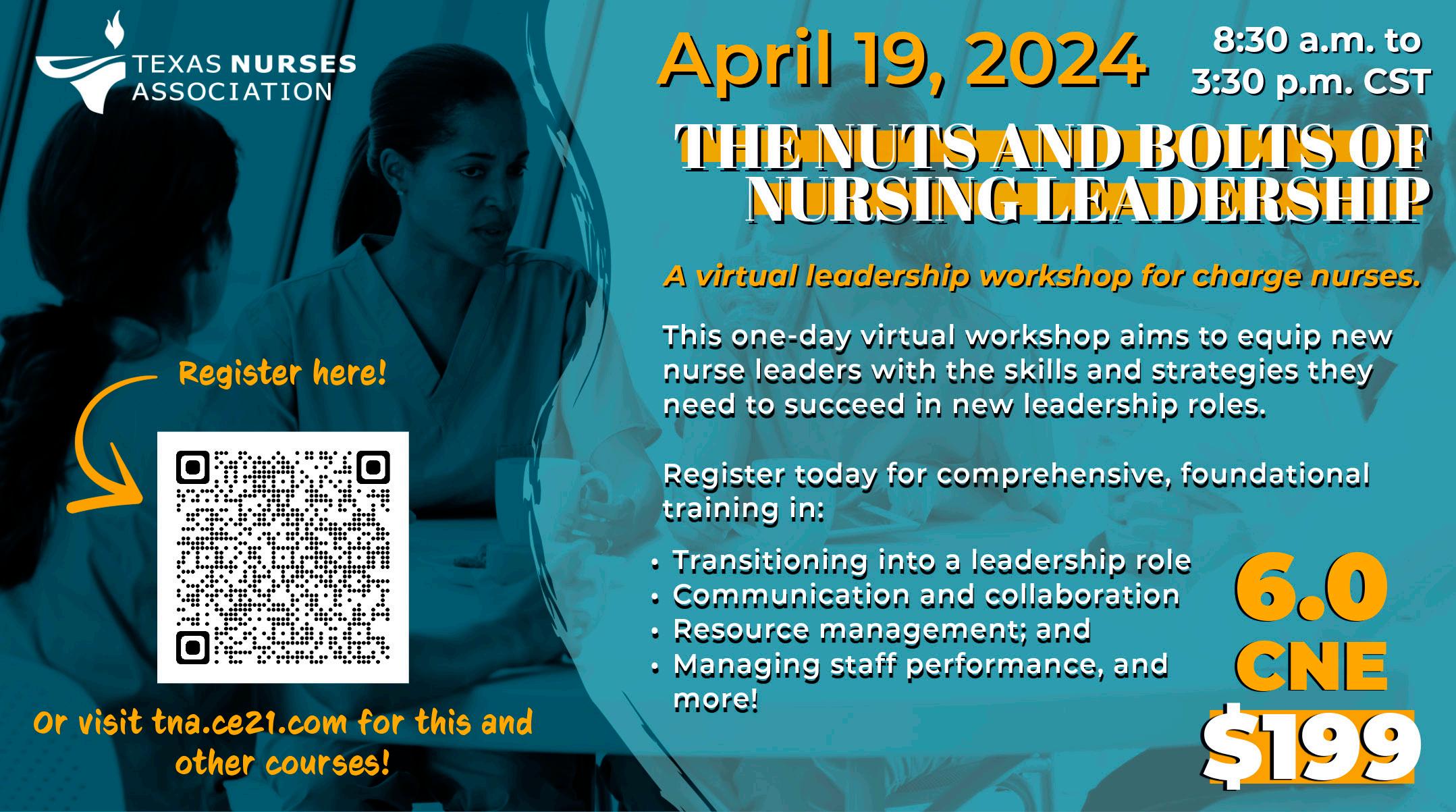
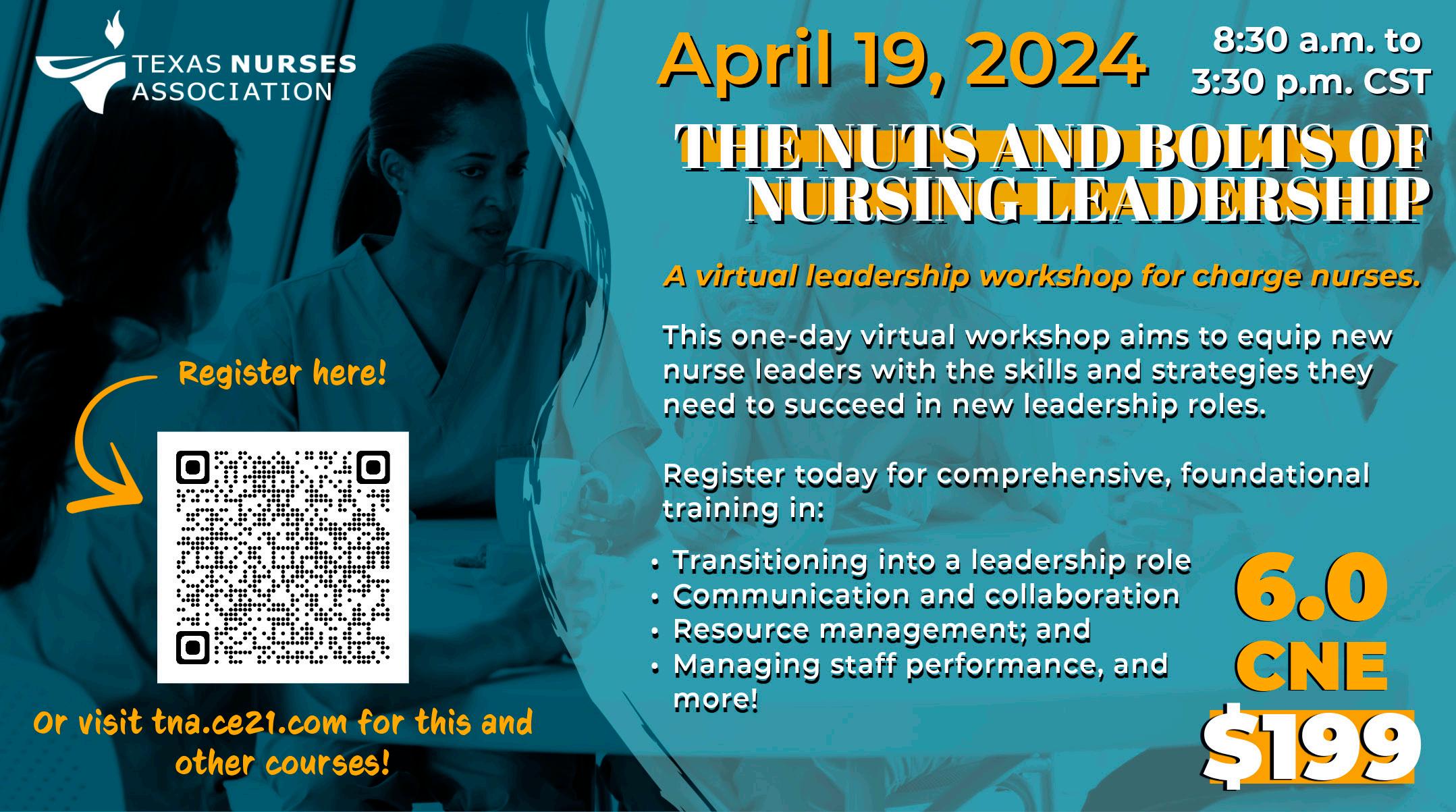
Profession. Exciting things happening here! TNA launched the NurseConnect mentor program in August. Our nursing peer review workshops are not only being offered virtually but also in person throughout the state during roadshows and at the request of hospitals around the state. We held the first workshop for Charge Nurses in October with over 30 attendees. Our next workshop is scheduled for April with a goal of 150 attendees. TNA partnered with the Texas Hospital Association to develop the



Workplace Violence Toolkit to provide healthcare organizations guidance in implementing the new workplace violence prevention laws and included reeducation on the staffing effectiveness law. TNA’s annual conference planning is well underway, and we have an exciting event planned!
HOW CAN YOU HELP?
While we have made great progress in the first half of our fiscal year, we have a lot more in store for our members. To move forward and gain traction with achieving our goals, we need the help of our membership: you are the fuel that keeps the car going! We look to you to help us grow membership and exceed our goal of 16,430 members at the end of FY24. We have so much more in store for you in 2024 and I cannot wait to share our progress with you. i
PAGE 15 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE
PEER REVIEW? LETTER OF INVESTIGATION? I CAN HELP! Joyce Stamp Lilly RN JD Registered Nurse and Attorney 713.759.6430 • jslilly@me.com www.Nurse-Lawyer.com www.NursingComplaintHelp.com YOUR BOARD COMPLAINT RESOURCE NursingComplaintHelp.com The most affordable and beneficial website to help you develop a plan and respond to Board complaints and Investigations against your license. SEE OUR NEW WORKPLACE VIOLENCE TOOLKIT.
Election Year influence
ALTHOUGH 2024 JUST STARTED, the 89th Regular Session doesn’t begin until 2025. This year will include an election for national, state, and local offices that will help crystallize TNA’s policy agenda for the 89th Regular Session. This is also the year that we expect to see large sums of state funds invested into nursing education based on decisions made in the 88th Regular Session, back in 2023.
This year will include an election for national, state, and local offices that will help crystallize TNA’s policy agenda for the 89th Regular Session.
TNA's policy agendA
The Policy Process: HOW TNA DEVELOPS POSITIONS
Hundreds of Texas nurses contribute
INVITING MEMBER ENGAGEMENT NOW
The TNA Board of Directors (BoD) appoints members to Policy Council (PC) and Government Affairs Committee (GAC) and approves final policy positions. BoD selects former PC and GAC members for wisdom councils to provide mentorship. PC: Vets and approves positions for consideration and final approval by the BoD, determines how committee and workgroup
By Jack Frazee, J.D., TNA Director of Governmental Affairs
should be enacted (legislative, regulatory, position or statement changes). Committees draft positions with input from issue advisors and Doctor of Nursing Practice student fellows. Small workgroups tackle focused topics and develop member materials. GAC: Takes positions from PC and enacts them into policies at the state level. District and at-large liaisons communicate local priorities to the GAC and GAC priorities back to local members. Members can take action in their communities to enact local policies and meet with their representatives during the interim.
In December of 2023, we launched, in collaboration with the Texas Hospital Association, a workplace violence toolkit for Texas nurses and healthcare organizations to use as the state works to implement The Workplace Violence Prevention Act of 2023. This toolkit provides an in-depth description of Texas law, a comparison of additionally applicable federal and state laws and regulations, and a model policy and signage for your organization to use. These are vital tools for complying with the new legal landscape as well as preventing violent events at work. We welcome your feedback as you use these tools.



TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 16
on
Policy Creation Policy Enaction Individual action, grassroots advocacy Local priorities and action State priorities and action Association action TNA Board of Directors Policy Council Standing committees Workgroups Workgroups Government Affairs Committee District and at-large liaisons Members NURSE PAC
© Texas Nurses Association 2021
efforts
TNA’s Policy Process
› TNA Board of Directors appoints members to the Government Affairs Committee (GAC) and Policy Council
› The Policy Council appoints members to its standing committees: Nursing Education and Workforce, Nursing Regulation and Practice Authority, Workplace Advocacy and Practice
› The Policy Council and its committees meet to explore and develop policy on pressing issues facing nursing
› The Policy Council and its committees develop policy documents
› Policy Documents are available to members for a 30-day comment period, then reviewed by the Board of Directors, who can approve or send back to the Policy Council for revision
› Approved policy documents guide the work of the Government Affairs Committee during the legislative session. The GAC's role is to track bills, strategize about furthering the nursing agenda and work with lawmakers, either directly or through GAC liaisons.

In spring of 2024, we expect to see rulemaking for TNA’s top priorities from the 88th Regular Session. These will include agency rules on how to prioritize and disperse funding for nurs -
ing education, criteria for grant applications, and gap-filling for substantive laws. TNA will submit comments when proposed rules are published to ensure the spirit of the law is carried into its regulatory framework.
Our Policy Council and its three subcommittees are hard at work to develop a policy agenda for 2025. We have gathered a significant amount of research and data on issues that are capturing nurses’ attention and are hard at work preparing policy recommendations for lawmakers. TNA publishes a call for comments on proposed policies, with a 30-day window for you to comment before the policies are considered by the TNA Board of Directors. Keep an eye out for publication of our policy positions, value statements, and issue briefs on our TNA Check Up newsletter so you can submit your feedback.
TNA publishes a call for comments on proposed policies, with a 30-day window for you to comment before the policies are considered by the TNA Board of Directors.
Our Government Affairs Committee is actively studying candidates as the primaries are taking shape. The committee will contact candidates and interview them to learn more about their nursing policy views. This work will inform our advocacy efforts and help us better understand the collective views of our elected officials once the election comes to an end. It also helps us make introductions, befriend our fellow Texans, and introduce them to the unique challenges and needs of nurses.
In 2023, we passed monumental nursing legislation, including the largest nursing education investment in state history and a comprehensive workplace violence prevention framework for the state. We accomplished those goals through bipartisan relationship building. No matter who wins or loses their elections this year, keep in mind that TNA will continue to work on your behalf. We encourage you to raise your voice with us in pursuit of better working conditions, better patient care, and a better society for Texans overall. i




PAGE 17 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE
We’re hiring for Registered Nurses, LVNs, Psychiatric Advanced Nurse Practitioners and more. Apply online at Even if you have no experience, we’re hiring Direct Care Staff and provide on-the-job training We offer competitive pay, paid health care, generous vacation, sick leave, 15 paid holidays, and free trainings to advance your career with the Health and Specialty Care System Health and Specialty Care System Join our team and make a difference! hhs.texas.gov/jobs You care. Make it a career. Scan to contact a recruiter or email a recruiter at healthcareers@hhsc.state.tx us If you’re dedicated to providing quality care and want to work in a positive and rewarding environment, APPLY NOW... because we want you to join our team!
JULY 2023 AUGUST –DECEMBER 2023 JANUARY –MAY 2024 JUNE –AUGUST 2024 JANUARY –MAY 2025

REVAMP, REFRESH, RETAIN A Collaborative RN-LVN Care Model
By Adam Ramirez, LVN, WCN-C, IV-C and Mary Lee Potter, PhD, MBA, RN, CWOCN
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
EVEN BEFORE THE COVID-19 PANDEMIC, nursing shortages were a topic of discussion among healthcare leaders. The pandemic hastened the exit of many Registered Nurses (RNs) and Licensed Vocational Nurses (LVNs) from the nursing profession, creating an epic shortage in an already stressed workforce.
According to the 2022 National Nursing Workforce Survey, during this time an estimated 200,000 experienced RNs and LVNs left the profession. (Smiley et al., 2023) As reported by the American Association of Colleges of Nursing, nursing schools cannot meet the growing demands and in 2021 turned away almost 92,000 qualified students partially due to the lack of faculty and available clinical sites (Rosseter, 2022). As a result, hospital leaders have been considering all their options in order to continue to provide safe quality patient care in this dynamic environment.
More than a decade ago, LVNs were phased out of many of
TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 18
the acute-care environments including a hospital in South Central Texas. Prior to transitioning to an RN-only model, LVNs were utilized widely throughout the organization including the intensive care units (ICUs). In light of the current staffing challenges, nursing leaders began exploring different staffing models, and LVNs were identified as an untapped resource. After considering the matter carefully, a previously used RN-LVN nursing model was revamped and transformed into an innovative Collaborative Care Model.
With the re-introduction of LVNs into the acute-care setting, nursing leadership created a platform to support the LVN to work to the full scope of their licensure guided by the Texas Board of Nursing (BON) rules. By re-vamping their role in the hospital, the LVNs work in collaboration with their RN partners to care for and manage a group of patients. The facility, which is a part of a larger for-profit health system, utilizes an RN-LVN partnership model, supporting the LVN to work at a higher level of responsibility and proficiency as allowed through the NPA. The RN-LVN partnership model reinforces a positive practice environment leading to higher nurse engagement.
To help support LVN’s transition back into the acute-care hospital setting, the hospital established an LVN Council which meets monthly. In addition, the facility developed a LVNfocused Clinical Support Resource Nurse (CSRN), which is a new role developed by the organization that is responsible for mentoring the new nurse transitioning into their first nursing position. The CSRN-LVN provides clinical support and professional guidance that extends past the orientation timeframe. Together, these resources have augmented the LVNs educational onboarding.
According to the Texas BON, in 2019 only 17% of LVNs worked in an acute-care setting. With this in mind, prior to the return of the LVNs into the hospital, policies, competencies, and onboarding tactics had to be refreshed to include the LVN scope of practice. While LVNs were educationally prepared to be competent in several nursing skills, the lack of hospital experience in many of the candidates created a steep learning curve for the LVN during the onboarding process , including both tenured LVNs and LVNs new to the profession.

Adding to the challenge, many (if not most) of the RNs and other healthcare providers had not worked in a RN-LVN model during their career, and in some cases, had misperceptions about LVNs that had to be addressed. Lessons learned with the initial onboarding cohorts included the identification of knowledge gaps with all levels of clinicians, confusion with interpretation of RN and LVN scope of practice, and LVN specific transitional needs from school to practice.
Using these lessons, LVN Onboarding Strategies were refined over a two-year period. Specifically, education provided to LVNs and RNs centered around scope of practice and best practices to support caring for patients collaboratively. A number of resources were also created such as a BON reference sheet, tips for success, and LVN Orientation Guide, made easily accessible to everyone. As the RNs and LVNs become more competent working within the new model, an atmosphere of mutual respect developed, creating strong team bonds.
Since the launch of the RN-LVN Collaborative Care Model in Fall 2021, improvements were seen in vacancy rates, nurse engagement scores, turnover rates, and the LVN and RN nurse engagement scores improved steadily over the past 18 months.
Across the country, retaining nurses of all types is a top priority for hospital leaders. Taking an active approach to recruiting LVNs had a significant impact on efforts to rebuild core staff following COVID. Since the launch of the RN-LVN Collaborative Care Model in Fall 2021, improvements were seen in vacancy rates, nurse engagement scores, turnover rates, and the LVN and RN nurse engagement scores improved steadily over the past 18 months. From 2022 to 2023, year-over-year annual externalized turnover improved almost 35% for RNs and 24% for LVNs. While the numbers tell part of the story, the connection among the staff is what really shines. As a hospital, a cornerstone of the culture is inclusivity, celebrating the strengths of the individual and the connected effort of many. Embracing the RN-LVN Collaborative Care Model has been a huge win for the campus, and ultimately for the communities served. Revamping previous staffing approaches and refreshing practices to include both the RN and LVN may help organizations with the challenges faced with nurse retention, while also promoting a culture that values the diverse contributions of a talented workforce. i
Acknowledgement for Editorial Support: Noah Zanville, PhD, RN
REFERENCES:
Rosseter, R. (2022, October 1). Fact Sheet: Nursing Shortage. Https://www.Aacnnursing. org/. Retrieved December 15, 2023, from https://www.aacnnursing.org/Portals/0/ PDFs/Fact-Sheets/Nursing-Shortage-Factsheet.pdf
Smiley, R., Allgeyer, R., Shobo, Y., Lyons, K., Letourneau, R., Zhong, E., . . . Alexander, M. (2023). The 2022 National Nursing Workforce Survey. Journal of Nursing Regulation, 14 (1), S1-S90.
https://www.bon.texas.gov/
https://www.aacnnursing.org/news-data/fact-sheets
PAGE 19 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE
IT NEEDS TWO UNIQUE NURSING IS SO UNIQUE IDENTIFIERS
By Katheren Koehn MA, RN, FAAN, Executive Director, MNORN

NURSE PROVIDER IDENTIFIER
NPIs are unique identifiers used by providers to bill Medicare and Medicaid for services they provide. They are currently the only identifiers allowed by the Centers for Medicaid and Medicare Services (CMS).
https://nppes.cms.hhs.gov/#/

UNIQUE NURSE IDENTIFIER
Uniquely identifies a U.S. nurse regardless of how many states in which the nurse is licensed. It is an eight-digit public identifier assigned to a nurse for life upon getting their first U.S. nurse license (LPN/ VN or RN) and will never expire or be recycled.
https://nppes.cms.hhs.gov/#/
This article previously appeared on ana-illinois.org and has been published by other state nursing associations.
Nursing has changed greatly in the past 100 years, but billing has remained the same.
THERE IS AN AGE-OLD PROBLEM when it comes to finding the cost of nursing services in a hospital bill, because nursing is buried in the room charge. We talked about this issue in the 1970’s when I became a nurse, and we are talking about it today.
This is not a subject that just a few of us are talking about. This is a subject nurses at every level are talking about. You can see some of the discussion by doing a quick google search. Enter “where is nursing in the hospital bill?” and out pops myriad articles. Among the articles I found were:
allnurses.com: Should nursing charges be separate from the room charges? (2003)
beckershospitalreview.com: Want to Fix the Nursing Shortage? Change this 100-year-old policy (2023)
thefreelibrary.com: Nursing is the room rate (2012)
HISTORY
“Want to Fix the Nursing Shortage?” explained how nursing got into the room charge in the first place. In the 192030’s, medical science expanded. More people were admitted to hospitals and the need for 24-hour nursing care also
TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 20
NPI
UNI
expanded. Rather than billing patients separately for nursing care, as they had done when patients paid for their own private-duty nurses, hospitals rolled the cost of nursing services into the hospital bill—where nursing has stayed for nearly 100 years. Nursing has changed greatly in the past 100 years, but billing has remained the same.
There are those who think that CMS is the best place, others who think NCSBN is the best place. It turns out that this isn’t an “either or”—this is an “and!”
History is important to know how we got where we are. Now it is time to change.
CURRENT DEBATE
Discussions about the need for a unique nurse identifier have turned into a debate about where the unique identifier should be located. The two options are within CMS as the Unique Provider Identifier (NPI) or within NCSBN within Nursys. Notice the word “debate.” There are those who think that CMS is the best place, others who think NCSBN is the best place. It turns out that this isn’t an “either or”—this is an “and!”
Currently most APRNs are registered in the CMS NPI Registry; they have to be in order to bill for Medicare and Medicaid services. Most registered nurses have not registered, but they can. There is no charge. All nurses who hold licenses are automatically assigned an unique identifier by the NCSBN for their Nursys database. One way to think about it is that the NPI via CMS is for billing; the NCSBN ID is for the use of aggregate data on nurses for research on nursing.
The ANA Position is that all nurses should enroll into the NPI Registry, so that registered-nurse payment could be extracted from the room charge.
The NCSBN Position is that all nurses
One way to think about it is that the NPI via CMS is for billing; the NCSBN ID is for the use of aggregate data on nurses for research on nursing.
ANA - NURSE PROVIDER IDENTIFIER
“Registered nurses (RNs) are integral parts of the health care team and spend significant time with patients providing clinical services. In the current health care financing system, this work is generally not accounted for, other than in the physician’s practice expense (PE) relative value unit (RVU). The lack of NPIs for nurses makes it extremely difficult to record, measure, and value the services they provide and their impact on patient outcomes…..Obtaining and recording NPIs in appropriate healthcare data systems would allow health systems, payers, and enterprise resource planning systems to extract nursing services from other providers. This then allows for a quantitative analysis and substantive demonstration of the nurse’s role and value as an integral member of a patient’s health care team.”
NCSBN - UNIQUE NURSE IDENTIFIER
UNI (nurse’s NCSBN ID) allows to uniquely identify a U.S. nurse regardless of how many states in which the nurse is licensed. It is an eight-digit public identifier assigned to a nurse for life upon getting their first U.S. nurse license (LPN/VN or RN) and will never expire or be recycled, just like SSN is to an individual.
Federal, State, Non-profit, For profit, Hospital systems, Educational institutions – ALL have nurse data sets for nurses in their systems and databases. With UNI embedded in their data sets, protected nurse personally identifiable information (PII) such as SSN, DOB, etc. will no longer be needed for nurse identification and will facilitate data sharing and exchange for research, operational and important public protection work. UNI is publicly available; however, it is the responsibility of each organization to securely protect their nurse data sets.
Information systems can relatively easily record nurse’s patient care contributions throughout the care continuum by simply using the UNI. Aggregate data analysis can help with meaningful evidence-based decisions. Searching for a nurse in databases can be made easy using ONLY the UNI.
have a NCSBN identifier that uniquely identifies all nurses, which could provide aggregate data to research nursings contributions through the care continuum.
NEXT STEPS
It is time to end the debate on either or. Understanding ANA’s position on NPI and NCSBN’s position on UNI begins the process of ensuring that all nurses have both. Since nurses are automatically enrolled in the NSCNB database, this means that we need to be encouraging all nurses to enroll in the NPI at https://nppes.cms.hhs.gov/#/, It is free and easy to do. It’s the first step in making sure our history does not become our future. It is time to bring nursing out of the room charge. i
REFERENCES
An Overview and Policy Implications of national nurse identifier systems: A Call for unity and integration https://www.nursingoutlook.org/article/ S0029-6554(22)00180-4/fulltext
A Unique Identifier: Frequently Asked Questions (FAQ) https://www.allianceni.org/sites/allianceni/files/ wysiwyg/inline-documents/Unique_Nurse_ID_FAQ_ Final.pdf
NPI: What You Need to Know https://www.cms.gov/ Outreach-and-Education/Medicare-LearningNetwork-MLN/MLNProducts/Downloads/NPI-WhatYou-Need-To-Know.pdf
Position Statement: National Patient Identifier (NPI) as the Unique Nurse Identifier https://www.nursingworld. org/~493c6b/globalassets/practiceandpolicy/ nursing-excellence/ana-position-statements/nursingpractice/npi-position-statement.pdf
Want to fix the nursing shortage? Change this 100-year-old policy https://www. beckershospitalreview.com/want-to-fix-the-nursingshortage-change-this-100-year-old-policy.html
PAGE 21 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE
ANA FREQUENTLY ASKED QUESTIONS ABOUT THE NPI
What is an NPI? NPIs are unique identifiers used by providers to bill Medicare and Medicaid for services they provide. They are currently the only identifiers allowed by the Centers for Medicaid and Medicare Services (CMS).
Why should I obtain an NPI? NPI numbers are the only numbering system currently approved for providers like APRNs to bill Medicare and Medicaid.
How do I obtain an NPI? Applications for NPIs can be found through CMS’ website: https://nppes.cms.hhs.gov/#/,
Why is it important to have an NPI to track the care that nurses provide? As nurses, we know that our care is a crucial component of healthcare quality and health outcomes. Yet an RN’s time and expertise are now completely invisible to the systems that pay for patient care. As a result, the value of RN care to the system is not quantified. Nursing care should be counted! Tracking that care with an NPI is an essential first step in changing how health systems and other practitioners view nurses and the work that they do. The ultimate goal is changing healthcare reimbursement to account for the role of RN care.
What is the cost for an NPI? There is no cost to obtain and maintain an NPI.
How long do I keep my NPI? The NPI lasts throughout your professional career and travels with you from position to position. Make sure to update the NPI system when you change employers.
How do I obtain more information from ANA on NPI? To obtain more information please contact ANA’s policy team at gova@ana.org.
Who administers the NPI process and why? The process is administered by CMS. Congress passed legislation requiring CMS to create a unique identifier for providers and the result of this was the NPI. CMS requires NPIs to process Medicare payments, and to support data analysis for the Medicare program.
Do private payers require NPI numbers? Most private payers require NPI numbers for billing, but it is not a legal requirement.
THE UNIVERSITY OF TEXAS MEDICAL BRANCH
A Reputation for Excellence!
Educating nurses since 1890, UTMB SON offers undergraduate, graduate and doctoral degree tracks, designed to meet the unique needs of each nursing professional. Our graduates are skilled in providing patient-centered care and are developed to become leaders in health care.
UTMB SON’s teaching innovations have resulted in consistently high national rankings and alumni who have distinguished themselves as leaders throughout Texas and the United States. Today, informed by tradition, our vision continues to be our mission—to be the best in nursing education, research and practice in order to improve health for people around the world.
To learn more about our programs, visit: https://nursing.utmb.edu

When nursing became part of the room charge. Look at this hospital bill from St Paul MN in 1938. The patient was in the hospital for 8 weeks. Note that the categories “special house nurse; graduate nurse board days; and graduate nurse board nights are blank. This bill suggests the hospital had at one time billed for nursing services, then stopped. It is time to remove nursing from the room charge!
Programs Offered
• Bachelor of Science in Nursing
• Traditional BSN (on campus)
• RN-BSN (online)
• Master of Science in Nursing (online)
• Certificate (online)
• Doctor of Nursing Practice (online)
• Doctor of Philosophy in Nursing (online)


TEXAS NURSING MAGAZINE | ISSUE 1, 2024 PAGE 22
Does the NPI cross state lines? Yes. NPIs are nationwide and cross state lines.
I am an APRN and bill under my practice/hospital NPI, why should I get an NPI?
Unless one has an NPI, it is impossible to track the work you do versus the work done by other clinicians in the practice. Additionally, if one chooses to start their own practice, they would need an NPI to bill Medicare and Medicaid for reimbursement.
I am an RN and I don’t bill separately, why should I get an NPI?
It is true that RNs do not currently bill, but we believe that
nurses are not paid appropriately for the work they perform. There is currently no way to track all the work that nurses do to show their full value, but by registering for an NPI we can start building the data to show the impact of nurses.
Other organizations are requesting that I use my NCSBN ID. Does this conflict with an NPI? This does not conflict with ANA’s recommendation of obtaining an NPI. Key organizations using NCSBN IDs are doing important research that can also help show the value of nursing. They are using this ID as all nurses are automatically given an NCSBN ID. The NPI was developed specifically for billing and reimbursement purposes, which is an area of priority focus for ANA advocacy. Both identifiers are important to changing how systems value and reimburse nurses. i



PAGE 23 ISSUE 1, 2024 | TEXAS NURSING MAGAZINE
I’m Attorney Rachael Levy, and I can help you keep your nursing license! Reach out today: (713) 581-4192 • RGLevyLaw.com Are you facing a Texas Nursing Board Complaint? 1. Review your malpractice insurance. 2. Seek legal counsel that specializes in defending nurses before the Board. 3. Obtain a copy of the Board’s file. 4. Prepare a thorough response to the Board’s allegations. 5. Comply with all Board deadlines. Rachael Levy Take these five steps:

4807 Spicewood Springs Rd. Bldg. 3, Suite 100 Austin, TX 78759 Find an Escape...Book your vacation today! Join Fellow Nursing Professionals ◆ Share Cruise Experiences Provide Tips and Recommendations ◆ Compare Cruise Lines NursesWantCruises.com
















































 CEO
CEO