37 minute read
Digital transformation in the time of coronavirus
The health sector is the biggest winner
The health sector has undoubtedly benefited from the digital transformation that is gaining ground due to the precautionary measures that have taken over all countries of the world, prompting many hospitals and medical centers to adopt digital transformation strategies in line with the global change imposed by the coronavirus pandemic. Digital health technologies have significantly grown and we have been relying on them tremendously in the time being.
Advertisement
Specialized companies have rushed to develop programs and work mechanisms that ensure that the patient and the hospital alike have access to the necessary facilities for communication, case diagnosis and other benefits. Hence, telemedicine has become a tangible reality with the help of electronic health records, online consultations and other innovations.
Doctors and hospitals have adopted digital communications, health platforms and applications during complete lockdown, therefore, the concept of global digital health has expanded, which includes telemedicine, electronic pharmacies, wearable devices and many others, at a time when the demand for digital health services is still growing so that healthcare providers can benefit from the available technical options in addition to the advanced systems and programs. Patients can benefit from remote healthcare thanks to the digitization provided by health institutions that provide remote medical services, hence, the patient receives immediate medical consultations with the ability to closely monitor and follow up on the medical condition remotely, especially for those who suffer from chronic diseases and are unable to leave their house. THE CORONAVIRUS PANDEMIC HAS LED TO THE GROWTH OF DIGITAL HEALTH TECHNOLOGIES.


Digitization in Hospitals
Smart hospitals rely on digitization in their operations by adopting digital healthcare solutions, which has evolved even more with the coronavirus outbreak, especially in terms of patient data and records through the electronic personal health records that collect information about the patient’s health that includes test results, clinical notes, diagnoses and health problems that the patient suffers from in addition to the medications he takes, procedures he underwent, etc.
Smart hospital infrastructures rely on a wide range of devices necessary to automate and digitize work to enhance productivity and increase healthcare accuracy.
The modern methods available today for telemedicine give the patient a speedy response by the medical team following up on his condition by connecting the home device with the hospital, so the patient gets clinical monitoring at home, but remotely, which guarantees his access to medical services through coordination with the medical team with improved patient participation. Most importantly, the patient receives a medical consultation without the need to leave the house.
This type of services would reduce the burden on healthcare systems and doctors, so the patient does not always have to go to the doctor’s clinic, saving effort and time on the one hand, and increasing the productivity of healthcare providers on the other hand. In addition, telemedicine enables people who live in distant locations to receive the medical service they need without the hassle of commuting.
Telemedicine
Dependence on telemedicine and remote consultations has increased in light of the coronavirus pandemic, and it has proven to be a preferred method for many patients to practice MOST HEALTHCARE INSTITUTIONS AND HOSPITALS IN THE REGION REALIZED THE DANGER OF THE EMERGENCE OF THE CORONAVIRUS, SO THEY WORKED TO ACTIVATE WEBSITES AND TURN THEM INTO A PLATFORM THAT ALLOWS THE PATIENT TO COMMUNICATE WITH THE DOCTOR.
home quarantine and social distancing by saving the hassle of commuting to the hospital and waiting at a time when we urgently need it.
Most healthcare institutions and hospitals in the region realized the danger of the emergence of the coronavirus, so they worked to activate websites and turn them into a platform that allows the patient to communicate with the doctor, from anywhere and around the clock, in order to obtain remote medical consultations and answer their inquiries, which contributes to providing patients with healthcare services and avoiding being in a crowded place as one of the precautionary measures taken to prevent the spread of the virus.
Today, health institutions and hospitals have advanced programs run by health professionals and human resources working with a high level of professionalism, as they have demonstrated high competence and professionalism in terms of communicating with the patient or his family through video technology with the aim to provide medical consultations, lab test results and radiology results, and give the necessary prescription.
Remote medical consultations provide the opportunity to connect the patient with the specialist physician to carry out the necessary and accurate consultations about the disease, so that the doctor listens to the complaint and type pf pain with the help of the data and information provided.
The coronavirus pandemic and the accompanying home quarantine and the difficult patient access to hospitals and doctors' clinics was a strong driver behind the unprecedented increased demand for electronic medical platforms, after a large number of patients relied on those platforms in search of the right doctor. The advanced mobile technology has helped in the growth of telemedicine to provide healthcare services such as initial diagnostics, consultations, and comprehensive monitoring of the patient's health condition, among others.
Wearable Devices
The market of wearable devices and tools containing sensors to quickly monitor vital signs and various conditions of the human body has THE USE OF WEARABLE DEVICES HAS EXPANDED AT THE PRESENT TIME, WHICH LED TO ITS TECHNICAL DEVELOPMENT. WEARABLE TECHNOLOGY CAN BE WORN AS CLOTHES OR ACCESSORIES, SUCH AS WATCHES, GLASSES AND CLOTHES, AS THESE DEVICES CAN PROVIDE INSTANT INFORMATION THAT SUITS SPECIFIC CONTEXTS, THROUGH DATA RECORDING, ANALYSIS AND DELIVERY.
expanded, so that the information issued is transmitted directly to the personal doctor, enabling him to closely monitor the medical condition through data collection and analysis by artificial intelligence algorithms in order to identify diseases and health problems. The aim is to obtain an early diagnosis, successful treatment, while reducing complications that may result from the development of the condition.
This technology has been able to change many trends in healthcare industry, as it has become possible to monitor the patient's vital functions from home and there is no need for him to be permanently in the hospital, through small devices that the patient can wear anytime and anywhere, enabling the medical staff to follow up on his health condition while receiving detailed and real-time information about blood pressure or heart rate, for instance.
The use of wearable devices has expanded at the present time, which led to its technical development. Wearable technology can be worn as clothes or accessories, such as watches, glasses and clothes, as these devices can provide instant information that suits specific contexts, through data recording, analysis and delivery. These devices monitor and analyze the health of individuals according to several indicators such as heart rate, blood pressure and others.

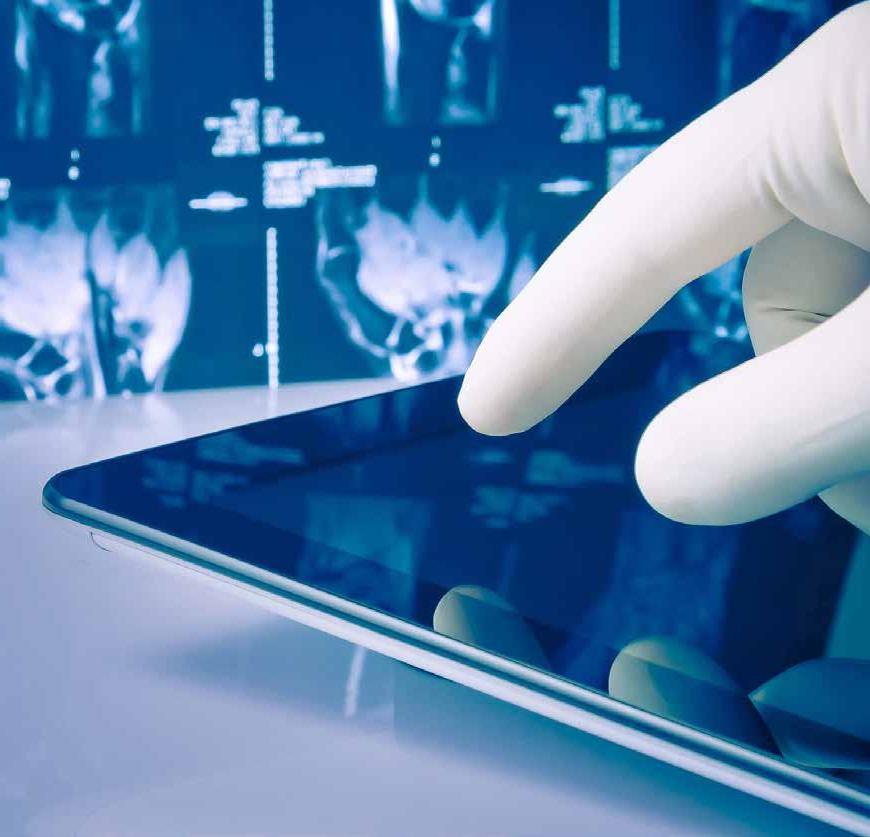
Mobile X-ray equipments
High in demand at hospitals in light of the coronavirus pandemic
The novel coronavirus has brought about drastic changes in the radiology departments in hospitals in general, so the companies involved in the production and manufacture of medical imaging devices have been ready to fight this pandemic by enhancing their production capacity and producing mobile X-ray devices that limit the movement of patients and communication with them. X-rays can be performed near the patient's bed while obtaining a high-quality clinical image.
Most hospitals, especially those specialized in receiving coronavirus patients, realized the key presence of mobile imaging devices and proceeded to acquire them since the beginning of the crisis, that is, during the first quarter of this year. It was obvious that they definitely needed this type of medical imaging devices for early diagnosis of Covid-19 patients and to follow-up on their condition.
In response to keeping pace with the coronavirus pandemic and the precautionary measures it imposed, medical imaging companies have doubled their production of mobile devices that allow the radiologist to photograph the patient and diagnose his condition while in bed without the need to transfer him to another room and expose others to the risks of spreading the infection, especially in advanced cases in intensive care and the difficulty of transporting the patient to the imaging department.
Mobile medical imaging is an urgent need today in light of the pandemic outbreak, which prompted manufacturers to increase their production capacities in order to manufacture portable imaging devices. The radiologist brings the imaging device to the side of the patient's bed whenever needed and obtains high-resolution digital images.
Mobile X-ray devices have been at the forefront of devices used to care for coronavirus patients and diagnose their condition, taking into account prevention factors, as this device can be used in several places within the hospital, such as the emergency room, intensive care units, isolation and quarantine departments, and even regular rooms. This type of imaging device has facilitated the possibility of transferring the device from one department to another within the hospital or even from one hospital to another, according to the diagnostic needs, provided that sterilization is one of the basic conditions for the transfer of the device in order to preserve the safety of the radiologist, the patient, and other healthcare providers within the hospital.
In light of the application of social and physical distancing, mobile devices have thus provided effective solutions to reduce the spread of MOBILE MEDICAL IMAGING IS AN URGENT NEED TODAY IN LIGHT OF THE PANDEMIC OUTBREAK, WHICH PROMPTED MANUFACTURERS TO INCREASE THEIR PRODUCTION CAPACITIES IN ORDER TO MANUFACTURE PORTABLE IMAGING DEVICES.
This device can be used in several places within the hospital, such as the emergency room, intensive care units, isolation and quarantine departments, and even regular rooms.
infection, as medical imaging has been available at the side of the patient's bed, which was of great importance for coronavirus patients on the one hand and facilitated the work of healthcare providers on the other hand at a time when they are in dire need of this type of support in light of the overcrowding in coronavirus departments and the extent of the risk of infection transmission.
Manufacturers have been able to introduce several features to such devices in order to help reduce contamination and to be smoothly sterilized after each use allowing the radiologist to use them again quickly, between one patient and another. Those companies were also keen to take into account the easy transportation of the device, as it was designed to be small and lightweight.
Portable digital X-ray devices are used extensively to monitor the condition of pneumonia patients that coronavirus patients suffer from, after the device is placed at the side of the bed, allowing it to be used in emergency rooms and in the intensive care unit.
This type of digital radiography has several benefits, such as providing faster and less expensive imaging services than other methods, with the same accuracy and quality, which makes it an effective alternative to a fixed radiography room, allowing the radiologist to bring the device to the patient instead of having to bring the patient to the device.
Bringing the device to the side of the patient greatly helps in saving effort, time and fear of transmitting infection in serious Covid-19 cases, which will positively affect the increase in efficiency in the workflow and the protection of everyone in the hospital. In addition, the easyto-use device in several hospital departments is very important in reducing the spread of infection. The use of this type of imaging device requires strict conditions. Firstly, the radiologist must wear personal protective equipment (PPE) and take the utmost precautionary measures of sterilization and others, and then apply the highest level of cleaning, sterilization and disinfection to all parts of the device and surfaces.
Pocramé, the start-up at the forefront of the fight against the coronavirus and all its variants
Zeina Trad, Marseille
THE FIRST, CALLED MEPHILAB, IS A MINI MEDICAL ANALYSIS LABORATORY ON ITS OWN. CAPABLE OF IDENTIFYING A MYRIAD OF PATHOGENS (VIRUSES, BACTERIA, FUNGI, PARASITES) FROM A SIMPLE SWAB, IT OBVIOUSLY RECOGNIZES SARSCOV-2 BY PCR, EXCEPT THAT IT GIVES RESULTS IN JUST 22 MINUTES, FOR AN ESTIMATED COST OF AROUND 10 EUROS PER TEST.
The MephiLab, a real mini medical analysis lab, gives a result in just 22 minutes and is developed by the Pocramé company at the IHU-Méditerranée Infection. Two analysis and infection prevention tools have witnessed unprecedented success in 2020 within hospitals in the South region, faced with the Covid-19 pandemic. A look back at a Provençal success story which has mainly benefited Provençal people for the time being! POCRAMÉ, is short for Point Of Care RAoult MÉditérannée.
The year 2020 will undoubtedly remain associated with the Covid-19 pandemic in the minds of most people around the world. For Pocramé, a start-up incubated since 2014 at the Institut Hospitalo-Universitaire (IHU) Méditerranée Infection, 2020 will also be remembered as the year when its business boomed, with sales exceeding 3 million euros for the first time. This success is obviously due to the sudden Sars-Cov-2 outbreak all over the world and the exponential needs for microbiological tests induced by this pandemic. Because the only two products marketed (for the moment) by Pocramé meet the current needs. Without the “IHU bashing” following the media coverage of its iconic boss, Didier Raoult, these innovations could have even made it possible to accelerate the deployment of tests throughout the country in the spring.
A mini mobile medical analysis laboratory
The first, called MephiLab, is a mini medical analysis laboratory on its own. Capable of identifying a myriad of pathogens (viruses, bacteria, fungi, parasites) from a simple swab, it obviously recognizes Sars-Cov-2 by PCR, except that it gives results in just 22 minutes, for an estimated cost of around 10 euros per test.
Used by the IHU's healthcare teams, there is a good reason that MephiLab was used in Marseille in terms of tests. For a long time, this hospital specializing in infectious diseases was even the only French enterprise capable of mass testing and delivering results in a few hours. But this was not enough to open up national prospects for MephiLab, their deployment during the crisis having been limited to a handful of medium-sized enterprises in Bouches-du-Rhône, Vaucluse and Hautes-Alpes (1). However, this machine could have rendered great service, when a large number of doctors

across the country wanted to subject their patients to a Covid-19 test and the ministry claimed that it was technically impossible, if not unnecessary. The CMA / CGM was not mistaken. The 3rd largest shipping company in the world has equipped around sixty of its container ships for two years, in order to be able to establish a reliable and precise diagnosis when a crew member or a passenger falls ill at sea.
Because the Marseille-based company obviously cares about the health of its employees and customers, and also because such a tool aboard a ship makes it possible to resort to a helicopter evacuation or a medical deviation only with full knowledge of the facts. When you know the cost of an additional day at sea for a container ship, CMA / CGM's decision also seems to be the result of economic thinking. Billed between 5,000 and 12,000 euros each depending on the options, a misery for stateof-the-art medical equipment, a MephiLab can indeed provide the shipowner with substantial savings. Not to mention the cost of a deviation or helicopter winching in the open sea.
How does this mobile lab work?
The secret of MephiLab? It has a PCR analyzer, a device capable of determining several hundred or even several thousand germs in a biological sample.
Thus, it embodies a diagnostic strategy developed over many years at the IHU, namely, the syndromic approach. It consists of listing a patient's symptoms, comparing them with the known symptoms of one or more diseases and looking in the patient's sample for pathogens that correspond to these diseases. A technique which makes it possible to know very quickly and almost certainly what exactly the patient is suffering from. In order to secure test results, each MephiLab, whether on land or aboard a ship, is connected to the IHU, where a biologist can continuously check the data sent by these mobile laboratories. THE SECRET OF MEPHILAB? IT HAS A PCR ANALYZER, A DEVICE CAPABLE OF DETERMINING SEVERAL HUNDRED OR EVEN SEVERAL THOUSAND GERMS IN A BIOLOGICAL SAMPLE. THUS, IT EMBODIES A DIAGNOSTIC STRATEGY DEVELOPED OVER MANY YEARS AT THE IHU, NAMELY, THE SYNDROMIC APPROACH. IT CONSISTS OF LISTING A PATIENT'S SYMPTOMS, COMPARING THEM WITH THE KNOWN SYMPTOMS OF ONE OR MORE DISEASES AND LOOKING IN THE PATIENT'S SAMPLE FOR PATHOGENS THAT CORRESPOND TO THESE DISEASES.
Fighting against hospital-acquired infections
The second tool developed by Pocramé, the MephiBox, also achieved considerable success in 2020, with several thousand units sold during the year and more than 450 units ordered to be delivered. Installed in the corridor of a hospital ward, at the door of a hospital room or a nursing home, the MephiBox allows healthcare workers to permanently have disposable protective equipment against infections (gloves, masks, glasses, gowns, etc.) and to manage them in the best safety conditions for them, for inpatients and for their visitors.
Developed with the aim of preventing hospital-acquired infections, which are diseases contracted in hospitals where pathogens are inevitably more present, the MephiBox is very useful in the control of Sars-Cov-2 and its dissemination in hospitals or in nursing homes for the elderly.
The MephiLab and the MephiBox are both manufactured in the South of France, not far from Marseille. Regarding the former, the PCR machine which is at its core, is manufactured at the IHU, before being mounted on a mobile chassis at ACA Plastiques in Signes (Var), in a body conceived and designed by Idéact in Géménos (Bouches-du-Rhône). As for the MephiBox, they involve the same subcontractors, generating new jobs.


HOSPITALS magazine had the privilege to meet with Dr. Stavros Malas, Professor of Mammalian Developmental Neuroscience and Genetics at the University of Nicosia Medical School to talk about Having finished my studies in London, I have worked for several years at the UK Medical Research where I developed several projects in how specific sets of genes control fetal brain development in mice. I have continued this work in Cyprus, where I founded the first and only unit for producing genetically modified animals.
In 2011, I have taken a short break from academic life and served as a Minister of Health of the Republic of Cyprus for a period of fourteen months. As a strong believer in quality Medical Education, I had pushed through the legal and regulatory framework, which led to the establishment of three Medical Schools, one public (national) and two private (international).
I am pleased to see all three Schools thriving, training between them more than 300 students annually making a very positive financial and reputational contribution to Cyprus. Two years ago, I have been recruited by the University of Nicosia to help in the development of a Veterinary School, to run alongside the Medical School. These are exciting times for the University, which aspires to become a leading regional his background and career, and tell us more about the University of Nicosia
Let's start with a little background info about your career, and how you ended up here at the University of Nicosia Medical School?
Medical School, their affiliations among others. Below is the full interview: educational establishment of international programs in such highly competitive fields of study, PARTNERSHIP WITH ST GEORGE’S, UNIVERSITY OF LONDON. THIS as Human and Animal Medicine.
How many people do you administer? Can you tell us about the staff and doctors who teach at your university?
The School has more than 600 contributing staff and faculty. As a multicultural University, our staff and faculty reflect this diverse background. We have clinical placements in four countries, so our clinical education department is similarly diverse which impacts students' holistic understanding of medicine being able to learn and work with global professionals.
What are the medical programs you offer at the institute? In which language you teach? And what admission test a student needs to get into your school?
We offer the six medical programs below, which are all taught in English:
Medical Programs
• Doctor of Medicine (MD), a 6-year undergraduate-entry degree quality assured by the World Federation for
Medical Education (WFME) via the
WE HAVE A LONG-STANDING Cyprus Agency of Quality Assurance
250+-YEAR-OLD UNIVERSITY IS THE ONLY SPECIALIST MEDICAL AND HEALTHCARE HIGHER EDUCATION INSTITUTION IN THE UNITED KINGDOM.
and Accreditation in Higher Education (CYQAA) and awarded by University of Nicosia Medical School. St George’s, University of London Bachelor of Medicine and Bachelor of Surgery (MBBS), a 4-year graduate-entry British medical degree quality assured by the UK General Medical Council and awarded by St George’s, University of London.
Postgraduate Degrees
• Master of Public Health (MPH), a fully online degree for working professionals and new graduates. • Master in Family Medicine (MSc FM), a degree for practicing doctors delivered entirely online. • Master of Science in Health Services
Administration (MHSA), a fully online degree for working professionals and new graduates. • Doctorate in Medical Sciences (Ph.D.), for research in all disciplines or specialties of Medicine. The admissions requirements vary depending on the program, so you can visit our website for specifics.

What are the conditions for students to apply and get accepted at the medical school? And what about the foreign students coming from abroad?
The University of Nicosia Medical School is truly multicultural, so foreign students come from around the world to attend. We host more than 1,000 students from 64 countries, coming from as far away as the United States, Canada, Australia and New Zealand.
Parents are comforted by the fact that Cyprus is ranked the safest country in the world for people aged 15 to 29 by the World Health Organization, and its people are famous for the warm and friendly welcome they extend to visitors. The Financial Times ranked Nicosia as the number one city under 500,000 in Europe for lifestyle and education. The majority of our programs begin in the autumn, so prospective students must complete their application and other requirements to be considered for entry prior to the start of the academic term. THE UNIVERSITY OF NICOSIA CONTINUES TO STRIVE FOR EXCELLENCE GLOBALLY. THE 2020 TIMES HIGHER EDUCATION (THE) UNIVERSITY IMPACT RANKINGS, RANKED THE UNIVERSITY OF NICOSIA (UNIC) AS THE NUMBER 42 UNIVERSITY IN THE WORLD IN THE CORE AREA OF QUALITY EDUCATION, AND AMONG THE TOP 301-400 UNIVERSITIES GLOBALLY IN TERMS OF ITS OVERALL SOCIAL AND ECONOMIC IMPACT.
Do you have any affiliations with medical schools outside Cyprus?
We have a long-standing partnership with St George’s, University of London. This 250+-yearold university is the only specialist medical and healthcare higher education institution in the United Kingdom. Partnering with the University of Nicosia (UNIC), the largest university in Cyprus, St George’s offers students the graduate-entry 4-year MBBS (Bachelor of Medicine and Bachelor of Surgery) program in Nicosia, Cyprus since 2011. This truly patient-centered program provides students with a global approach to medicine.
Below are some of our other international partnerships:
UK Royal College of General Practitioners (RCGP) Karolinska Institutet, Sweden Universidad de Oviedo, Spain Royal College of Surgeons of England

What are the advantages you offer to students compared to other med schools and where do you position yourself in the ranking worldwide?
The University of Nicosia continues to strive for excellence globally. The 2020 Times Higher Education (THE) University Impact Rankings, ranked the University of Nicosia (UNIC) as the number 42 university in the world in the core area of Quality Education, and among the top 301-400 universities globally in terms of its overIT WAS THE FIRST UNIVERSITY IN THE EU TO BE AWARDED 5 QS STARS IN DISTANCE EDUCATION AND THE FIRST UNIVERSITY GLOBALLY TO RECEIVE TRIPLE ACCREDITATION FOR ITS ONLINE LEARNING QUALITY.
all social and economic impact. It was the first University in the EU to be awarded 5 QS Stars in Distance Education and the first university globally to receive triple accreditation for its online learning quality. Our University has been a pioneer in online/distance learning education in Europe, supporting both its own degree programs, as well as those of its joint degree partners. This online expertise has proved exceptional to curricula delivery while transitioning to blended learning to meet public health regulations during the pandemic.
In comparing other med schools, there are several advantages:
With such a global population of students, we are proud of our graduates practicing as physicians across the world, including the USA, Canada, UK, Australia, EU countries, Israel, Lebanon and others. The Medical School Careers Office is devoted to student success evident by the 99% post-graduate placement rate at medical centres worldwide. More specifically, the Doctor of Medicine (MD) graduates have reached an absolute 100% employability record and for the Bachelor of Medicine and Bachelor of Surgery (MBBS) graduates this percentage was 99.35%.
Students are matched with a personal tutor from day one and have regular one-on-one meetings with our career advisers to track their studies, steps to practice in the country they wish to work. By outlining these pathways to practice, all students can plan with Career Advisers to put together timelines and application requirements based on the country and specialty they are seeking to practice in the future.
All incoming students at the University of Nicosia Medical School are guaranteed accommodation in our brand-new student residences which redefine modern student living. They consist of three separate complexes – SIX, U and TRIANGLE – which are among the most stunning student accommodations constructed in Europe.
The combination of a multicultural population, modern infrastructure, English language knowledge, reasonable cost of living, rich history and a beautiful natural environment makes it an ideal place to study for our global student body.

What kind of research opportunities do you offer to your students?
Students have many opportunities for research at our school: 1. Students in the MBBS, MD and Master’s programs can do research projects as part of their degrees. 2. We also run the Students in Research Programme in which students can engage with research projects outside their curriculum. Faculty offers a variety of research projects which include original research projects (e.g. lab-based projects, questionnaire surveys, systematic reviews and narrative reviews, etc.). 3. Students can also engage in ongoing research projects by contacting faculty directly or by contacting the Associate Dean for Research. THE UNIVERSITY OF NICOSIA MEDICAL SCHOOL IS TRULY MULTICULTURAL, SO FOREIGN STUDENTS COME FROM AROUND THE WORLD TO ATTEND. WE HOST MORE THAN 1,000 STUDENTS FROM 64 COUNTRIES, COMING FROM AS FAR AWAY AS THE UNITED STATES, CANADA, AUSTRALIA AND NEW ZEALAND.

Advanced Medicine. Premium Care.
Dr. Jessica Adam Chief Medical Officer

Dr. Jessica Adam in an exclusive interview with The Arab Hospital Magazine “Alfardan Medical with Northwestern Medicine is a new healthcare concept in Qatar and the region.” “We adopt an American patient-centric model where the patient always comes first.” Alfardan Medical with Northwestern Medicine (AMNM) has recently opened its doors to patients looking to access advanced medicine and world-class medical services. The new ambulatory care center is not just a continuation of the impressive growth momentum Qatar has seen in the past decades, but a new concept for healthcare in the region. AMNM’s focus on patient centricity and service excellence nurtures personalized healthcare experiences and ensures that patients are actively involved in their healthcare journey at every step of the way, said Dr. Jessica Adam, AMNM Chief Medical Officer, in an exclusive interview with The Arab Hospital Magazine. Praising the medical team at AMNM, Dr. Adam said: “AMNM’s world-class healthcare services are powered by a multinational collective of specialized medical staff and professionals from leading markets, including a large contingent from the U.S.A. We are responsible for the selection of medical staff and specialists, in compliance with Northwestern Medicine’s stringent talent recruitment and development standards.” Dr. Adam noted that the unique collaboration between Alfardan Group and Northwestern Medicine leverages both organizations’ complementary strengths: Alfardan Group’s legacy and scale in offering hospitality and luxury experiences, and Northwestern Medicine’s longstanding history and leadership in the medical field. Integrating the merits and experiences of both organizations truly differentiates AMNM as a premier healthcare provider in Qatar and the region, she added.
Details from the interview: The Arab Hospital Magazine: What services does AMNM provide? Dr. Jessica Adam: AMNM is an ambulatory care center that provides high-quality, multidisciplinary medical care, and patient service. At AMNM’s state-of-the-art treatment facility, advanced and patient-centric care, from a multinational multidisciplinary medical team, is combined with service excellence. AMNM is currently welcoming patients looking to access high quality evidence-based medical services in Dermatology, Internal Medicine, Gastroenterology, Reproductive Endocrinology, Infertility and Gynecology, Dentistry, Ear Nose and Throat, Orthopedics, Physical Medicine and Rehabilitation. Highly credentialed allied health professionals specialized in Exercise Physiology, Physiotherapy, Clinical Nutrition and Diagnostic Imaging and Lab are also available. This further reinforces AMNM’s patient-centric approach to healthcare that is buttressed by collaborative multidisciplinary teamwork. Other AMNM medical specialties that will be introduced in the near future include: Executive Health, Ophthalmology and Plastic and Cosmetic Surgery, among others. How is your American model different from other models? AMNM’s mission builds on the American patient-centric model of designing a seamless healthcare journey for the wellbeing of patients through infrastructure, architecture, and services. Designed around human connections, AMNM has created an end-to-end healthcare experience for patients. From welcoming and guiding patients around the facility, to overseeing patient conditions, AMNM services are attuned to the comfort and needs of the patients.

The expert medical team at AMNM is dedicated to realizing patients’ individuality, values, and preferences and aligning healthcare decisions with their needs and comfort.
What kind of medical experts are available at AMNM? AMNM’s world-class healthcare services are powered by a multinational collective of highly credentialed, specialized medical staff and professionals from leading markets, including a large contingent from the U.S.A. AMNM’s high-caliber physicians and experienced multidisciplinary medical team offer patients a holistic wellness experience that is stemmed from the interdisciplinary collaboration between the different departments at AMNM, and when needed, includes expertise input from Chicago-based Northwestern Medicine.
How are AMNM’s medical facilities different? At AMNM, patients receive world-class medical care from highly credentialed doctors and medical staff using state-of-the-art, U.S.A. Food and Drug Administration (FDA) approved equipment. The introduction and application of medical technological solutions at the ambulatory care center extends further than its specialties and can also be found across AMNM diagnostic services, laboratory medicine and radiology, and operating rooms. We have implemented advanced technological solutions to an array of our specialties, including innovations by industry pioneers such as Phillips, Olympus, ZEISS and many more. AMNM’s efficient 1.5T Magnetic Resonance Imaging (MRI) system, aims to make patients feel comfortable and secure, and provides higher-quality images in a shorter amount of time. Our 128 Slice Computerized Tomography (CT) scan machine maximizes CT capabilities with its intuitive advancements and reduces time to offer results with %19 adaptive intelligence at every step of the scan. Additionally, we have a flexible solution that helps us perform vertical, horizontal, and seated tests, as well as additional angulated views that contribute to accurate diagnoses. For our Ear, Nose, and Throat (ENT) specialty, the HD video rhino-laryngoscope allows HD image quality visualization of the nose, pharynx, and larynx. With its protective frame, disposable components, convenient instrument management, and hygienic maintenance of the unit, the Otopront hygiene solution unit for ENT diagnostic and treatment is practical for any and all hygiene issues. Technological solutions offered in our operating rooms include the C-arm, which is used for diagnostic imaging during surgical procedures. The C-arm delivers excellent image quality and increases the efficiency of surgical operations at AMNM, allowing our surgeons to obtain necessary imaging intra-operatively for better surgical outcomes. Additionally, the endoscopy systems set new standards for technologies by focusing on advancing control and workflow, lend convenience to the team with their high-resolution images and extended recording time of endoscopic procedures. AMNM’s highly anticipated Executive Health specialty, which encompasses preventive health screening, is inclusive of several lifestyle consultations with a Clinical Dietitian and an Exercise Physiologist. The unit is equipped with the Bod Pod test for body composition, which is highly accurate and accessible for all and supplements the measuring and monitoring of risk for obesity. In addition, the unit is fully equipped to provide health and fitness assessment using tools to investigate underlying mechanisms of physical activity to produce exercise programs tailored for each client. Our Dental specialty offers an optimized patient experience with its high-tech intraoral cameras, which are small yet powerful devices that capture photos of inside the mouth, leading our team to better diagnosis and results. The specialty is also furnished with state-of-the-art Dental Chairs, which are comfortable, versatile, and user friendly. The chairs ensure the safety of both patients and staff by reducing any risk of cross-contamination and comes with the Full Touch panel which give users full access over the sanitization process.
AMNM’s Reproductive Endocrinology, Infertility and Gynecology specialty utilizes an ultra-modern technology that enables a safe and stable environment for embryos and allows them to be analyzed with minimal disturbances. AMNM’s world-class healthcare services are offered in the heart of Lusail, Qatar’s city of the future and the embodiment of a national vision that strives towards a sustainable and healthy society. Strategically located at the iconic Burj Alfardan, AMNM spans over six dedicated floors. For appointments or more information, you can contact the center on 6000 4004 or visit its website amnm.com.
You can also follow AMNM’s social media channels on Facebook, Instagram, and Twitter: @amnm_qa.
AMNM’s Dermatology, and Plastic and Cosmetic Surgery specialties are powered with the Duetto MT Quanta Laser Machine for hair reduction, which performs hair removal processes and rejuvenation treatments. The Dermatology specialty also operates with the innovative and unparalleled Q-Switched ND YAG laser, which is useful in the treating of pigment-related issues such as the removal of moles, freckles, and even pigmented lesions and tattoos. Fractional CO2 lasers are also used in non-invasive procedures to remove the outer layers of damaged and aged skin. Realizing the need for efficiency and accuracy in achieving diagnoses, AMNM’s laboratories and are equipped with the latest technological solutions that help in time-sensitive situations. Our laboratory microscopes help the AMNM team document, prepare and tweak cells samples, and help them evaluate the characteristics of the samples. The way AMNM has incorporated technological solutions as part of its highly advanced specialties contributes to the overall comfort and assurance patients feel when they interact with our services, further leading to our one-of-a-kind patient-centric healthcare experience. How can people from the region benefit from AMNM? Regional and international patients can receive comprehensive healthcare advice within their planned stay in Qatar. Introducing specialized programs such as Executive Health to the region enhances Qatar’s position as a hub for premium medical services and medical tourism. AMNM’s Executive Health services offer a personalized medical assessment, which determines the presence or absence of risk factors associated with diseases of high complexity through a series of tests and procedures of early detection and diagnosis. Tailored for convenience and to support busy schedules of executives, business owners and entrepreneurs, AMNM’s Executive Health service provides an efficient yet complete medical evaluation to help maintain good health in years to come. Which insurance providers are accepted at AMNM? AMNM partnered with QLM Life and Medical Insurance Company (QLM), a subsidiary of Qatar Insurance Company (QIC) Group, and AlKoot Insurance & Reinsurance company (AlKoot), a leading insurance solutions provider in Qatar, to offer their cardholders access to AMNM’s innovative, tech-powered, and patient-centric healthcare. We have several other agreements with major insurance providers underway.

GE Healthcare Announces First X-ray AI to Help Assess Endotracheal Tube Placement for COVID-19 Patients

GE Healthcare announced a new artificial intelligence (AI) algorithm to help clinicians assess Endotracheal Tube (ETT) placements, a necessary and important step when ventilating critically ill COVID-19 patients. The AI solution is one of five included in GE
Healthcare’s Critical Care Suite 2.02 an industry-first collection of AI algorithms embedded on a mobile x-ray device for automated measurements, case prioritization and quality control.
Research shows that up to 25 percent3,4,5,6,7
of patients intubated outside of the operating room have misplaced ETTs on chest x-rays, which can lead to severe complications for patients, including hyperinflation, pneumothorax, cardiac arrest and death. Moreover, as COVID-19 cases climb, with more than 50 million confirmed worldwide8, anywhere from 5-15 percent require intensive care surveillance and intubation for ventilatory support9 .
“Today, clinicians are overwhelmed, experiencing mounting pressure as a result of an ever-increasing number of patients,” said Jan Makela, President and CEO, Imaging at GE Healthcare. “The pandemic has proven what we already knew – that data, AI and connectivity are central to helping those on the front lines deliver intelligently efficient care. GE Healthcare is not only providing new tools to help hospital staff keep up with demand without compromising diagnostic precision, but also leading the way on COVID-era advancements that will have a long-lasting impact on the industry, long after the pandemic ends.”
Up to 45% of ICU patients, including severe COVID-19 cases, receive ETT intubation for ventilation10,11,12. While proper ETT placement can be difficult, Critical Care Suite 2.0 uses AI to automatically detect ETTs in chest x-ray images and provides an accurate and automated measurement of ETT positioning to clinicians within seconds of image acquisition, right on the monitor of the x-ray system. In 94% of cases the ET Tube tip-to-Carina distance calculation is accurate to within 1.0 cm13. With these measurements, clinicians can determine if the ETT is placed correctly or if additional attention is required for proper placement. The AI generated measurements – along with an image overlay CRITICAL CARE SUITE 2.0 HELPS BEDSIDE STAFF AND RADIOLOGISTS ASSESS ENDOTRACHEAL TUBE (ETT) PLACEMENT FOR INTUBATED PATIENTS, INCLUDING CRITICAL COVID-19 PATIENTS A FEW MINUTES.

– are then made accessible in a picture archiving and communication systems (PACS).
Improper positioning of the ETT during intubation can lead to various complications, including a pneumothorax, a type of collapsed lung. While the chest x-ray images of a suspected pneumothorax patient are often marked “STAT,” they can sit waiting for up to eight hours for a radiologist’s review14 .
However, when a patient is scanned on a device with Critical Care Suite 2.015, the system automatically analyzes images and sends an alert for cases with a suspected pneumothorax – along with the original chest x-ray – to the radiologist for review via PACS. The technologist also receives a subsequent on-device notification16 to provide awareness of the prioritized cases.

“Seconds and minutes matter when dealing with a collapsed lung or assessing endotracheal tube positioning in a critically ill patient,” explains Dr. Amit Gupta, Modality Director of Diagnostic Radiography at University Hospital Cleveland Medical Center and Assistant Professor of Radiology at Case Western Reserve UP TO 45% OF ICU PATIENTS, INCLUDING SEVERE COVID-19 CASES, RECEIVE ETT INTUBATION FOR VENTILATION10,11,12 .
University, Cleveland. “In several COVID-19 patient cases, the pneumothorax AI algorithm has proved prophetic – accurately identifying pneumothoraces/barotrauma in intubated COVID-19 patients, flagging them to radiologist and radiology residents, and enabling expedited patient treatment. Altogether, this technology is a game changer, helping us operate more efficiently as a practice, without compromising diagnostic precision. We will soon evaluate the new ETT placement AI algorithm, which we hope will be equally valuable tool as we continue caring for critically ill COVID-19 patients.”
To make the AI suite more accessible, Critical Care Suite 2.0 is embedded on a mobile x-ray device – offering hospitals an opportunity to try AI without making investments into additional IT infrastructure, security assessments or cybersecurity precautions for routing images offsite.
Furthermore, the on-device AI offers several benefits to radiologists and technologists: ETT positioning and critical findings: GE Healthcare’s algorithms are a fast and reliable way to ensure AI results are generated within seconds of image acquisition, without any dependency on connectivity or transfer speeds to produce the AI results. Eliminating processing delays: Results are then sent to the radiologist while the device sends the original diagnostic image, ensuring no additional processing delay.
Ensuring quality: The AI suite also includes several quality-focused AI algorithms to analyze and flag protocol and field of view errors as well as auto rotate the images on-device. By automatically running these quality checks ondevice, it integrates them into the technologist’s standard workflow and enables technologist actions – such as rejections or reprocessing – to occur at the patient’s bedside and before the images are sent to PACS.
GE Healthcare and UC San Francisco co-developed Critical Care Suite 2.0 using GE Healthcare’s Edison platform, which helps deploy AI algorithms quickly and securely. Critical Care Suite 2.0 is available on the company’s AMX 240 mobile x-ray system.
For more information on GE Healthcare and Critical Care Suite 2.0 visit gehealthcare.com Clinicians can also test the Critical Care Suite 2.0 algorithms by uploading their own chest x-ray images to www.gexray.ai
NEW AI SUITE INCLUDES ALGORITHMS THAT HELP RADIOLOGISTS PRIORITIZE CRITICAL CASES AND AUTOMATE PROCESSES TO HELP CUT AVERAGE REVIEW TIME FROM UP TO EIGHT HOURS1 .
References
1. Rachh, Pratik et al. “Reducing STAT Portable Chest Radiograph Turnaround Times: A Pilot Study.” Current Problems in Diagnostic Radiology Vol. 47, No. 3 (n.d.): 156–60. https://www.sciencedirect.com/science/article/abs/pii/S0363018817300312?via=S0363018817300312?via=ihub. 2. Critical Care Suite 2.0 is only available in the United States. Not cleared or approved by the FDA. Distributed in accordance with FDA imaging guidance regarding COVID-19 public health emergency. 3. Jemmett ME, Kendal KM, Fourre MW, Burton JH. Unrecognized misplacement of endotracheal tubes in a mixed urban to rural emergency medical services setting. Acad Emerg Med 2003;10:961–5. 4. Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med 2001;37:32–7. 5. Lotano R, Gerber D, Aseron C, Santarelli R, Pratter M. Utility of postintubation chest radiographs in the intensive care unit. Crit Care 2000;4:50–3. 6. McGillicuddy DC, Babineau MR, Fisher J, Ban K, Sanchez LD. 7. Is a postintubation chest radiograph necessary in the emergency department? Int J Emerg Med 2009;2:247–9. 8. WHO Coronavirus Disease (COVID-19) Dashboard. Published June 17, 2020. Retrieved November 10, 2020, from https://covid19.who.int/. 9. Möhlenkamp S, Thiele H. “Ventilation of COVID-19 patients in intensive care units.” Nature Public Health Emergency Collection. 2020 Apr 20 :1–3 10. Hannah Wunsch, Jason Wagner, Maximilian Herlim, David Chong, Andrew Kramer, and Scott D. Halpern. ICU Occupancy and mechanical ventilator use in the United States. Crit Care Med. 2013 Dec; 41(12): 10.1097/CCM.0b013e318298a139. 11. Dawei Wang, Bo Hu, Chang Hu, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. doi:10.1001/jama.2020.1585 12. Lingzhong Meng, M.D.; Haibo Qiu, M.D.; Li Wan, M.D.; Yuhang Ai, M.D.; Zhanggang Xue, M.D.; et al. Intubation and Ventilation amid the COVID-19 Outbreak: Wuhan’s Experience. Anesthesiology 6 2020, Vol.132, 1317-1332. 13. GE Healthcare data on file. 14. Rachh, Pratik et al. “Reducing STAT Portable Chest Radiograph Turnaround Times: A Pilot Study.” Current Problems in Diagnostic Radiology Vol. 47, No. 3 (n.d.): 156–60. https://www.sciencedirect.com/science/article/abs/pii/S0363018817300312?via=ihub. 15. Algorithm also available with GE Healthcare’s Critical Care Suite 16. The technologist on-device notification is generated after a delay, post exam closure, and it does not provide any diagnostic information, nor is it intended to inform any clinical decision, prioritization, or action.