27 minute read
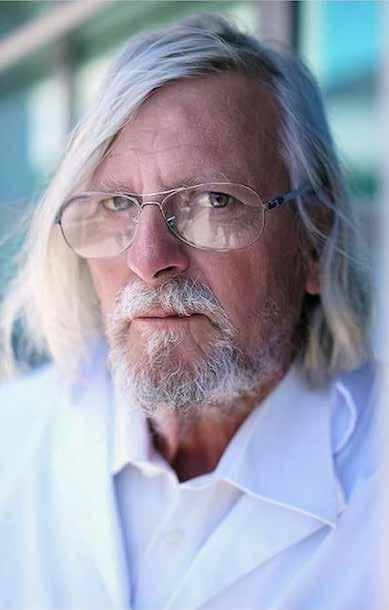
Noubar Afeyan
Co-founder and Chairman of Moderna Noubar Afeyan
Advertisement
By Olivier O’Mahony and Zeina Trad for "Hospitals" magazine
After having been able to get in touch with his company Flagship Pioneering that founded Moderna, its chairman Noubar Afeyan remembers his career as a biochemical engineer that has pushed him for thirty years to dedicate his life to innovating and transforming inventions into viable businesses. Thus, he created fifty companies and submitted a hundred patents! As early as February, Moderna announced that it had developed a new innovative type of vaccine against Covid-19 that had never been deployed in humans: the messenger RNA (mRNA) vaccine. This technology consists of administering a molecule capable of causing the patient's cells to generate their own medicine.
Is, mRNA-1273 developed by Moderna, the laboratory you co-founded, the miracle vaccine that the whole world is waiting for?
It is 94.5% effective and offers long-lasting protection for 120 days, according to a study we just published. It’s a great result. This vaccine is much easier to handle compared to other vaccines. Our vaccine can be kept for one day at room temperature, thirty days in a fridge, and six months in -20 degrees, while Pfizer's vaccine requires a storage temperature of -70 degrees. This vaccine is injected while Pfizer's needs to be diluted, which wastes time and leads to a risk of error.
However, a recent scientific study shows that the severity of side effects (fatigue, headaches, chills) increases with the second injection. Should we be worried?
No, this is a common reaction to all vaccines. And out of the 30,000 patients tested, we did not see any severe side effects.
You are one of the creators of this vaccine which was developed in record time. How did you accomplish that?
I am a biochemical engineer, and for thirty years I have dedicated my life to innovating and transforming inventions into viable businesses. Thus, I created fifty companies and submitted a hundred patents. This experience made me realize that contrary to popular belief, entrepreneurship is not improvisation. There are common points from one project to another and there are also rules to follow. Therefore, I created the investment company Flagship Pioneering, which founded Moderna.
Inventing new concepts, how do you accomplish that?
Instead of wondering what can be achieved with existing science, I ask the question: “what if?” (“And if it was possible?”). I rely on imagination. Invention is a process, in which one question leads to another.
What was the idea behind Moderna?
It was about coming up with a way to inject a molecule into the human body that causes the patient's cells to generate their own medicine instead of administering a drug or a vaccine that will help them heal. This is a revolutionary approach, which went against the ideas established in the scientific world in 2010, and against my training as a biochemist, whose main mission INSTEAD OF WONDERING WHAT CAN BE ACHIEVED WITH EXISTING SCIENCE, I ASK THE QUESTION: “WHAT IF?” (“AND IF IT WAS POSSIBLE?”). I RELY ON IMAGINATION. INVENTION IS A PROCESS, IN WHICH ONE QUESTION LEADS TO ANOTHER.
is to create proteins to heal people. In this case, there is no need to create proteins: it is the human body that makes them, stimulated by mRNA. And the simple fact of asking ourselves if this method was viable led us to ask ourselves several related questions. We thought: “OK, if we want to do this, then we have to inject molecules capable of carrying information.” DNA or messenger RNA fall into this category.
DNA, which was already used in gene therapy, with varying degrees of success, was of little interest to us. On the other hand, the messenger RNA has never been used to produce drugs or vaccines, to the best of our knowledge; simply because when injected into a living organism, it is rejected by cells, as if it were a virus. So in 2010-2011, we looked and found a way to overcome the obstacle. We thus established a protocol that allowed us to design the Covid-19 vaccine nine years later.
Has anyone raised this question before you did?
No one came to me to put this idea forward. I brought it up to Professor Bob Langer (a biotech expert, Editor's note), with whom I had a lot of discussions. I later learned that Genentech, a very reputable company, had previously tried the experiment and failed. But science has advanced: Derrick Rossi, a professor at Harvard, who worked on stem cells, managed to integrate the messenger RNA into a plate (dish: not sure about the French translation). So I thought to myself that the same could be done in a human body.

When did you discover your mission of becoming an inventor?
I have always been interested in science. When I was twelve, I used to dream about America and had heard of MIT, the Massachusetts Institute of Technology, where I ended up doing my PhD. But I come from an immigrant family, like many inventors.
I think immigration and innovation go hand in hand. In both cases, the process is the same: getting out of your comfort zone.
How did it become a reality?
There was an exile in my family for three generations. My grandparents who are Armenians, had to flee Turkey for Bulgaria, a neighboring country that they knew. My father was born there, but communism emerged, so he had to move to Greece and then to Lebanon, where he had never set foot. He was an architect but had to reinvent himself in the plastic import-export in Beirut where I was born. His business was going well, but he had to flee the civil war. I was thirteen years old and the youngest in a family of three sons. We settled in Montreal and today, I am an American citizen. My wife Anna is Swedish and is also a biochemist.
How did you become an entrepreneur?
Totally by chance. When I started my PhD at MIT, after graduating from McGill University in Montreal, I had no idea what I was going to do with my life. Then I thought about becoming a lab employee. But one day in 1985, I went to a conference in Washington about japanese competitiveness, which at the time was thought to be a great threat to America.
At lunchtime, a very nice guy sitting next to me told me that in the 1930s he had created one of the first oscilloscopes. Then he told me his name was David Packard. I had no idea he was actually the co-founder of tech giant Hewlett-Packard. We stayed together and talked for an hour after the conference. He told me that as a student, he was part of a new generation of engineers, the “electronics engineers”.
I was 23 years old and I was a student in a new engineering specialty, biochemistry, so I ended up asking him how he got started, how he knew which product to start with. “It doesn't matter which product you choose, most importantly is to get started and learn as you move forward,” he replied. As simple as that. I will never forget this piece of advice.
After that, I went to see a corporate sociologist, Professor Ed Roberts, at MIT, who warned me, “You don't become an entrepreneur, you either are or you aren't.” I think I was, because at the end of my PhD, I followed the example of Hewlett-Packard and created my first company specializing in the creation of tools for engineers in my specialty, biochemistry.
25 years later, you created Moderna, of which you are the Chairman. When you were certain that your approach works?
In 2011. We had just injected messenger RNA into a mouse, which by reaction, made exactly the protein we wanted. I was ecstatic when I received the results, my wife still talks to me about it. For me, that was the ultimate proof of the correctness of our approach. That's when I recruited Stéphane Bancel, who is French.
Why him?
It was a headhunter who gave me his name when I was looking for an administrator for one of my companies, BG Medicine, which specializes in medical diagnostics. Stéphane was then the head of BioMerieux laboratory, the French laboratory whose headquarters had just been relocated to Cambridge, Massachusetts (the biotech Mecca, Editor's note), right next to our premises. He's a great guy, curious about everything, highly motivated leader and very interested in starting a business. While maintaining his job, he became administrator and then chairman of BG. He's a biochemist like me and one of his teachers was a friend and a classmate. We had a lot in common. I offered him to join me, he was hesitant until I told him about my LS-18 project, Moderna’s code name. LS for Life Science. 18, because it was the eighteenth project of this type that I launched.
It was not easy to convince him to leave a well-known established French pharmaceutical company with more than 6,000 employees, for a completely new project with a limited budget of $ 2 million, without a website.
Indeed. I still remember it as if it was only yesterday: I called him as he was walking across the Longfellow Bridge, a famous bridge that connects Boston and Cambridge over the Charles River and told him, “I'm working on a crazy project, which can become Apple's equivalent in biotechnology.” Except that I didn't have any specific detail to give him. “It’s never going to work,” he replied, but I could tell he was interTHE MRNA TECHNOLOGY IS APPLICABLE TO ANY DISEASE: CANCER, ALZHEIMER'S, HIV...THE RNA MESSENGER IS A MOLECULE THAT CARRIES INFORMATION. IF IT MANAGES TO GET INTO THE HUMAN BODY, NOTHING CAN STOP IT. IF TECHNOLOGY WORKS, THERE REALLY WILL BE A BEFORE AND AFTER IN MEDICINE.
ested. His wife, Brenda, later told me that when he got home that night, he was very annoyed that I was right. I was firing on all cylinders to convince him. I told him an old saying: “If you don't throw the ball, you can't score”. The mRNA technology is applicable to any disease: cancer, Alzheimer's, HIV...The RNA messenger is a molecule that carries information. If it manages to get into the human body, nothing can stop it. If technology works, there really will be a before and after in medicine. Stéphane felt he would forever blame himself if he missed this opportunity, therefore, he joined me.
Were Moderna's beginnings challenging?
I would be lying to you if I told you we were short of money. We initially invested $2 million, which is not a lot, but we knew we could raise it very easily, which we managed to do quickly. Many experts doubted us but we didn’t.
Until today, Moderna has never made a profit or produced any medicine. How does the emergence of Covid-19 change the game for you?
When the first alarming news came from Wuhan, China, we were working on other plans. There was a debate within Moderna: some were against the idea of finding a vaccine against Covid-19. But one evening in January, I received an unusual phone call from Stéphane
He was then at the Davos forum, where he was harassed with questions on the subject. Stéphane’s calls were always preceded by text messages. When I saw his number displayed on my phone, as I was celebrating my daughter's birthday, it was 3 a.m. in Switzerland where he was and I got worried.
In fact, he was very keen on getting into the vaccine race, and wanted to talk to me about it. The mARN technology works in all areas, why not in relation to Covid-19? We agreed: we must get on with that, it will be an opportunity to demonstrate the efficiency and especially the speed of our approach. As of January 11, the day China released the genome of the virus, it only took us a few days to establish the protocol. 42 days later, we suggested a vaccine vial injectable into the human body, which is a world record according to Dr. Anthony Fauci. We have raised a lot of money from our shareholders, up to $ 1 billion.
The American authorities have given us a lot of money as well. Then the tests began. It was stressful and exhilarating at the same time. The teams started with 100 people and then, in the end, tested 30,000 people, which was an achievement. When phase 3 was successful, my wife told me that I was as excited as the day the mouse experiment was successful.
Moderna has been “burnt” by Pfizer’s vaccine where England began it Covid-19 vaccination program a week ago? Do you regret it?
Not at all, because the need for vaccines is going to be huge where there will be room for everyone. We opted for diversity, which delayed the testing phase, and we fully accept it. It seemed important to us that all population groups be represented. We have also included a large number of people of color. When we announced it last September, we knew that this choice would cause us to fall behind the competition.
Moderna's vaccine should be approved on December 17 in the United States and then on January 12 in Europe. Are you optimistic?
I am always worried: optimism and confidence are not part of my vocabulary. What I know is that we have done everything we can to get these necessary approvals. Now, I cannot prejudge the decision of the supervisory authorities.
If all goes well, you will be credited with saving millions of lives. Is it staggering?
No. I'm just doing my job. And there is still a lot to do: upon approval, it will take us two years to grasp and control the introduction of the vaccine to the market: we won’t have time to be staggered.
Have you been vaccinated? Would you vaccinate your children?
Not yet, but as soon as possible I will of course. I have three daughters and a son. Everyone is looking forward to it! Paris Match I HAVE ALWAYS BEEN INTERESTED IN SCIENCE. WHEN I WAS TWELVE, I USED TO DREAM ABOUT AMERICA AND HAD HEARD OF MIT, THE MASSACHUSETTS INSTITUTE OF TECHNOLOGY, WHERE I ENDED UP DOING MY PHD. BUT I COME FROM AN IMMIGRANT FAMILY, LIKE MANY INVENTORS. I THINK IMMIGRATION AND INNOVATION GO HAND IN HAND. IN BOTH CASES, THE PROCESS IS THE SAME: GETTING OUT OF YOUR COMFORT ZONE.
Next level IVF treatment: What is in store for the future?
Insights by an IVF expert who never says “impossible”
Professor Ercan Bastu
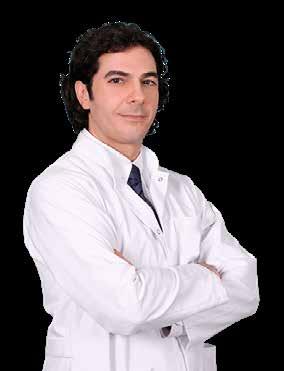
Imagine a future where human reproductive system can be restarted by stem cells and infertility treatment is aided by artificial intelligence to ensure successful pregnancy for couples failing to conceive naturally. These science-fiction plots are already on the way in some of the best reproductive centers worldwide, says Professor Ercan Bastu, M.D, an infertility specialist at Acibadem Healthcare Group in Istanbul, Turkey. In the modern world, where families tend to postpone parenthood until fulfilling their career or personal goals, medical solutions are being developed to meet their changing needs.
Half of IVF patients are aged 40+
Fertility issues affect an average of 10 to 15% of all couples. It is recommended to see a doctor when they have been regularly trying to conceive a baby for at least one year, in case that the woman is below 35 years of age. If the female partner is above 35, then 6-month attempts are enough before consulting a speA NEW TREATMENT OPTION IS AVAILABLE EVEN FOR MEN WHO HAVE NO MATURE SPERM CELLS – A CONDITION CALLED AZOOSPERMIA THAT WAS PREVIOUSLY ASSOCIATED WITH LITTLE OR NO CHANCE OF SUCCESS IN IVF TREATMENT. AN ADVANCED TECHNIQUE CALLED ROSI HELPS TO ACTIVATE SPERM CELLS WITH ELECTRICAL STIMULATION.
cialist for some tests and evaluation. Recently, patients over 40 years of age become the prevalent group of candidates for in vitro fertilization (IVF). Professor Ercan Baştu explains: “For example, last month half of my patients were over 40. Lots of women postpone their pregnancy and it’s definitely harder for them to succeed because finding the oocytes of good quality and number is not that easy compared to a younger age.”
IVF alone is not enough, new techniques come to light
In our changing environment, the best specialists in assisted reproduction are adjusting to the new reality, exploring new treatment options. Technology comes to help with modern devices, such as the embryoscope that allows tracking the development and quality of the embryos. Genetic tests (PGD) let to evaluate the embryos’ genetics and identify any abnormalities that would impede a successful pregnancy. A new treatment option is available even for men who have no mature sperm cells – a condition called azoospermia that was previously associated with little or no chance of success in IVF treatment. An advanced technique called ROSI helps to activate sperm cells with electri-

cal stimulation, explains Professor Baştu who is among the first to apply the new method at Acibadem. “For women who don’t have enough ovarian reserve, we can use some new treatment modalities to get oocytes of good quality, like platelet-rich plasma (PRP) or stem cells. We are currently working on getting approval from the Health Ministry for stem cells” the fertility expert adds. What about the future? Professor Baştu gives some precious insights: “Artificial intelligence is a very hot topic nowadays, and we have done some research on it, because AI will help us to decide which embryo has an implantation potential, which embryo is of good quality, and it will be very objective and very quick. We will also have some sort of new diagnostic testing for embryos’ chromosome status without touching or harming the embryo. We will take the embryo culture and analyze it. In the future we will learn the crosstalk between the endometrium and the embryo in detail, especially to understand their genetic situation on molecular interaction, and we can help them to establish a good relation between the embryo and endometrium. I think we’ll see it in the future.”
Comprehensive approach to infertility treatment
Successful assisted reproduction requires a good understanding of the health conditions impeding the pregnancy. That’s why a comprehensive approach is crucial, states Professor Ercan Baştu, whose career development includes a masterclass in clinical embryology at the University of Leeds, UK; advanced endoscopy masterclass at the University of Surrey in UK, as well as some scientific research at Harvard University in USA.
The reason for IVF failures cannot be named in all cases but additional tests and changing the type of treatment might help to improve the outcomes. Sometimes, surgery might be needed to allow conceiving, says the IVF expert who provides complex infertility treatment, including FERTILITY ISSUES AFFECT AN AVERAGE OF 10 TO 15% OF ALL COUPLES. IT IS RECOMMENDED TO SEE A DOCTOR WHEN THEY HAVE BEEN REGULARLY TRYING TO CONCEIVE A BABY FOR AT LEAST ONE YEAR, IN CASE THAT THE WOMAN IS BELOW 35 YEARS OF AGE.
endoscopic surgeries, to patients from all over the world. Endometriosis, blocked fallopian tubes, myomas and abnormalities of the uterus that need to be corrected with hysteroscopy are some examples of conditions that need a good surgery. With proper treatment, these patients might even be able to conceive naturally, without assisted reproduction. Nowadays, laparoscopic techniques and robot-assisted surgeries make operations safer than ever.

What makes a good IVF clinic?
Quality of service and patients’ comfort are the key prerequisites to successful IVF, says Professor Ercan Baştu. “We provide high-quality services, this is the main thing. We are an updated clinic and we have done a lot of research about infertility. We usually have the latest technology in our lab, and the latest developments in medicine; we can use it. Every new thing in Europe or the US,
we’ve got it and we can use it. Our success rate is similar and maybe higher when compared to other countries. That’s why patients are usually satisfied with their treatment in Acibadem.”
The infertility specialist explains that success rates depend on many factors, especially the age. For example, when there is one blastocyst or day 5 embryo with good genetics, there is 60 to 70% chance for pregnancy. However, it would be difficult to have a quality blastocyst above the age 40 and in this case pregnancy rate drops to 30-40% for this age group. And still, what makes the patients satisfied is to have their questions answered in details and feel comfortably even away from home during the treatment. At Acibadem, their jourPROFESSOR ERCAN BASTU HAS HUNDREDS OF HAPPY STORIES IN HIS CAREER BUT ONE OF THEM HE REMEMBERS MOST CLEARLY – HE SAYS IT CHANGED HIS APPROACH TO PATIENTS ONCE AND FOREVER.

ney starts with a detailed conversation – either in English or another native language for the couple, aided by an experienced translator. Then, an ultrasound is performed, test results are evaluated and a road map for treatment is presented and explained to the patients. During the treatment, couples may ask their questions directly to the doctor, who usually shares his phone number for patients’ comfort.
IVF as a happy ending story
Professor Ercan Baştu has hundreds of happy stories in his career but one of them he remembers most clearly – he says it changed his approach to patients once and forever. “They came to me so sad, nearly crying, and told me that they wanted a baby. The woman was 46 years old, so I told them: I cannot do an IVF procedure for you, it’s nearly impossible, don’t waste your time and money. Then the woman told me that they had a boy, 19 years old, and they had lost him 2 months ago. He had always wanted a brother or sister and they wanted to try it, even if they didn’t have a chance. I said: okay, if you understand your chances, let’s try it. The woman had just one oocyte and we took it. The same day the man had to give sperm but he couldn’t because after his boy’s death he had started drinking. We needed to freeze the oocyte. The woman came again 2 months later and told me that she wanted to try again. We got 2 oocytes but this time their quality was not good. Two months later she came again, she was 47. She insisted to try again and we tried. This time we had 2 oocytes, and I took the one we had frozen the first time. The man managed to give sperm this time. We had one embryo with an average quality; I did the transfer and she got pregnant. Two months ago she gave birth to a boy. And look at the pictures above my desk – there are no patients’ pictures, just one and that’s him. This is incredible! Now I never say “impossible”: if they say they want to try, I just accompany them. One is one, it can still help.”
10 important rules for living with a Covid-19 positive patient

Professor Ahmet Cagri Buke
There are more Coronavirus cases at homes nowadays! Stating that the Covid-19 infection, which has been increasingly spreading almost every day at global scale, evolves into a state of one infected person in almost every house, Professor of Infectious Diseases and Clinical Microbiology Çağrı Büke, M.D., from Acıbadem Healthcare Group says “Considering the fact that about 80% of the patients diagnosed with Covid-19 through PCR test can be cared at home setting, one should always remember that Covid-19 is mostly contracted in indoor environments. This fact pushes us to review considerations for living together with a Coronavirus-positive case in the same house.” So, what are the considerations that should not be neglected even for a moment while living together with a Coronavirus-positive patient? Professor of Infectious Diseases and Clinical Microbiology Çağrı Büke informs about 10 golden rules and make important advice and warnings.
It is necessary to live in separate rooms
A person with positive Covid-19 test must live in a separate room for a while. Door of the room should always be closed and the patient should eat in this room, reserved for him/her for a while, away from other family members.
A mask should necessarily be worn when getting into the room
Nobody should get into the patient’s room unless it's really necessary and the patient should not leave the room except for compelling reasons. If it is necessary to enter the patient’s room, a mask should be worn such that it completely covers the nose and mouth. The rule of wearing mask should not be neglected even for a moment and social distancing should not be ignored.
Bathroom should be cleaned after each use
If possible, a separate bathroom is reserved for the patient to have toilet and bath needs met. If it is not possible and other family members need to use the same bathroom, then toilet, sink, basin, taps, surfaces and floor should be cleaned with a disinfecting agent after each use.
Laundry and eating utensils should not be shared

Laundry, cutlery and other items, such as water glasses, used by the coronavirus patient should not be shared. His/her laundry should be washed separately in a washing machine, while eating utensils should be washed in dishwasher or under running water by hand using detergent.
Hands should be washed after contacting the common areas
Hands should be washed with soap and water for 20 seconds immediately after contacting any surface at common areas, before and after meal, after bathroom, before and after cooking and after contacting with objects in indoor areas. Hand sanitizers can be used as well for hand hygiene.
Coronavirus patient should wear a mask at home
Coronavirus patient should wear a mask, such that it completely covers the mouth and nose, when it is necessary to go to the bathroom or other rooms.
Surfaces should be cleaned frequently
Door handles, electric switches and other surfaces that may be touched should be cleaned with disinfecting agent and detergent after each contact.
A separate towel should be used
As towels pose high risk of transmission, a separate towel should be used by each family member under normal circumstances. Especially if there is a coronavirus patient at home, towels should never be shared. A separate towel should be allocated or paper towel can be used. Paper towel and toilet paper waste should be kept in a separate bag and disposed after the bag is tightly sealed.
Pillowcases should be changed every day
Pillowcases of a coronavirus patient should be changed every day and washed in washing HANDS SHOULD BE WASHED WITH SOAP AND WATER FOR 20 SECONDS IMMEDIATELY AFTER CONTACTING ANY SURFACE AT COMMON AREAS, BEFORE AND AFTER MEAL, AFTER BATHROOM, BEFORE AND AFTER COOKING AND AFTER CONTACTING WITH OBJECTS IN INDOOR AREAS. HAND SANITIZERS CAN BE USED AS WELL FOR HAND HYGIENE.
machine at minimum 60 degrees Celsius and bed clothes should be changed once every three days and washed at minimum 60 degrees Celsius.

Home should be ventilated regularly
Coronavirus patient’s room and all other areas of the home should be ventilated for several minutes on daily basis. Also, Covid-negative family members should never allow ‘get-well’ visits. Because visits pose high risk of spread in indoor areas!
Professor of Infectious Diseases and Clinical Microbiology Çağrı Büke adds “Such measures should be maintained for a while after Covid-19 test result become negative; if no test has been done, these measures should be maintained for 48 hours after symptoms disappear completely or approximately for 14 days following onset of the symptoms. However, it should be kept in mind that this virus may, sometimes, be excreted by the body after a longer interval.”
Why was Hôtel-Dieu de France chosen as the first Lebanese hospital to join the international “Breast Centres Network”?

The Breast Centres Network, that includes many specialized centers exclusively dedicated to breast cancer diagnosis and treatment, is a joint program between the European School of Oncology and the Senologic International Society. This network aspires to enable all women worldwide to have access to fully equipped, quality-assured, dedicated breast centers or units that provide competent and comprehensive care. It shares the goal of improving breast cancer care throughout the world. Therefore, according to state-of-the-art international standards, some mandatory criteria have been set for giving eligible and qualified centers providing multidisciplinary breast cancer care, full membership to this network. BREAST CANCER IS NO LONGER A DISEASE THAT KILLS WOMEN LIKE IT USED TO.
Accordingly, the Breast Unit at Hôtel-Dieu de France hospital has succeeded in joining this network as a Full Member, since it meets all the required BCN Full Membership criteria, given its comprehensive health services, its multidisciplinary approach and its advanced technologies used for breast cancer diagnosis and treatment at all stages in just one hospital.
The Breast Unit at Hôtel-Dieu de France has a Radiology Department, including two dedicated radiologists and breast radiographers. The department performs around 3500 mammograms per year and provides a variety of tests to detect breast cancer. This department is fully equipped, as it has all the necessary breast imaging equipment for diagnosing breast cancer, as well as breast tissue sampling equipment or procedures to perform all kinds of biopsies.
As for breast surgery, the Unit performs around 400 cases per year. The hospital has two breast surgeons and a team of dedicated breast nurses. Nearly ten beds are available for breast cancer patients, and ambulatory surgery can be carried out, allowing women to be discharged from the hospital on the same day. Many are the breast surgeries skillfully performed by Hôtel-Dieu's breast surgeons, ensuring high-quality healthcare for women, such as the intraoperative sentinel lymph node, which is a minimally invasive procedure to avoid removing all the lymph nodes in the armpits, immediate breast reconstruction and other reconstructive procedures performed by the plastic surgeon collaborating with the Unit.
The Breast Unit also collaborates with the Pathology Department that comprises all the equipment, technology and special techniques for breast cancer detection, the Oncology Department that includes several medical oncologists dedicated to breast cancer cases, and the Radiation Oncology Department that is considered as one of the best departments at the national level and that includes radiation oncologists specialized in providing the best breast cancer treatment depending on each case. The Breast Unit is also characterized by the nuclear medicine techniques it has, which are often not offered at other hospitals. Doctors have sometimes recourse to the Nuclear Medicine Department to perform scintigraphy, which means placing a nuclear marker in the breast that heads towards the first lymph node that is likely to develop cancer in order to carry out a minimally invasive intraoperative sentinel lymph node, a technique that does not harm a woman's arm and has no post-surgical complications. Women can also benefit from the Leatitia Hatem Rehabilitation Center services at Hôtel-Dieu, a center that ensures post-operation follow-up to help women regain their strength.
The hospital also provides genetic counseling to check the history of tumors in the family and advise individuals at risk to detect breast cancer at early stages.
For better coordination between the Breast Unit departments, a weekly multidisciplinary meeting for case management is held to discuss every breast cancer case and treatment plans.
After fulfilling all the listed requirements, the Breast Unit of Hôtel-Dieu de France was eligible to join the Breast Centres Network. It thus became the first Lebanese member within this international group. It has proved to be a comprehensive unit that provides all the necessary services for breast cancer treatment, starting from detection, diagnosis and therapy, all the way to post-treatment stages.
Breast cancer is no longer a disease that kills women like it used to. With recent improvements in treatment, many options and solutions are available to treat this type of cancer that is now being regarded as a chronic disease. The focus has nowadays shifted towards the need to control and prevent this disease through early detection to cure it, guarantee higher survival rates for patients and extend their lives. THE BREAST UNIT AT HÔTEL-DIEU DE FRANCE PERFORMS AROUND 3500 MAMMOGRAMS PER YEAR AND PROVIDES A VARIETY OF TESTS TO DETECT BREAST CANCER. THIS DEPARTMENT IS FULLY EQUIPPED, AS IT HAS ALL THE NECESSARY BREAST IMAGING EQUIPMENT FOR DIAGNOSING BREAST CANCER, AS WELL AS BREAST TISSUE SAMPLING EQUIPMENT OR PROCEDURES TO PERFORM ALL KINDS OF BIOPSIES.