
6 minute read
Interview with Dr Kirsty Biggs: Infant feeding education
Interview with Kirsty Biggs: Infant feeding education
Kirsty Biggs is an academic foundation year 2 doctor who works in Stoke. She went to medical school in Brighton and did an intercalated BSc in Reproductive science at Imperial. During her intercalation, she did a cross-sectional project on formula supplementation in the postnatal ward. It was after this (when she returned back to medical school) that she then started her breastfeeding education work, after she witnessed doctors giving inappropriate advice during a pediatric placement. Her main interest is in Infant feeding, but she is also involved in other obstetrics and gynecology topics.
Advertisement
MV: Did you enjoy your medical school, and was it hard to intercalate externally ?
KB: I had a great time at med school, like I hope most people do, and got myself involved in lots of fun extra-curricular stuff as well as some research and teaching projects. At Brighton, they made it really easy for us to intercalate externally. I knew I wanted to do something O+G related and fancied the chance of experiencing student life in a different city.
MV: Why do you think you are so interested in Infant Feeding?
KB: Prior to intercalation, I knew very little about infant feeding. I was aware that ‘breast is best’, however really didn’t understand the true extent of the benefits. I think it is just amazing that something completely natural, and free, can have such an impact on health, economy and wider society. Breastfeeding plays a key role in achieving sustainable development goals, encompassing health, poverty, education, gender equality and sustainable consumption.
MV: Do you think medical students get enough training on Infant feeding?
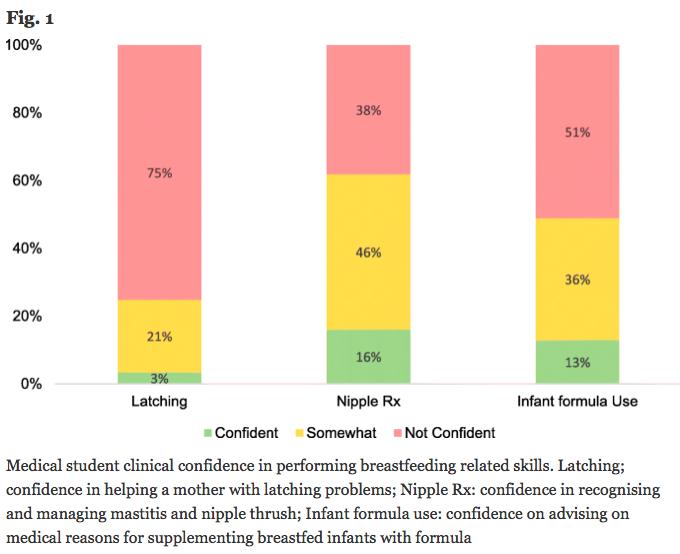
KB: This was my motivation for the breastfeeding education project! The only reason I really knew anything about infant feeding is because I happened to do my dissertation on it, so I suspected it was under-taught. As doctors we are important role models for women, and it is important we have the knowledge and skills to support mothers and help them to make informed feeding choices. I was delighted to find that 97% medical students* believed doctors to play a role in supporting breastfeeding, with 93% expressing a desire for further teaching on the subject. *based on 411 students (years 4/5 or 5/6).
MV: What made you pick an academic F1 compared to the mainstream programme?
KB: I realised during intercalation how much I enjoyed research and decided I’d like it to be part of my career. The academic foundation programme (AFP) gives you, paid, dedicated time to work on something you’re interested in, alongside the usual clinical work. It’s a great combination and adds some variability to my week. I have a flexible schedule which has allowed me to develop new skills, build my CV and undergo multiple projects.
MV: What is your proudest piece of research so far?
KB: My breastfeeding education project; a national survey on the inclusion of breastfeeding in the undergraduate medical school curriculum, and assessment of students’ related knowledge, skills and attitudes.
MV: Through my own research, I have found that infant feeding is vastly impacted by sociocultural factors. For example, the most deprived areas of Bristol have the lowest breast-feeding rates compared to more affluent areas. I asked a doctor who is currently doing a sustainability fellowship why he thought this was. He suggested that we should lie a lot of the blame with formula milk companies who advertised their products as more beneficial to a baby’s health. Do you think this is true? What other factors do you think are involved with this issue?
KB: I agree, a significant responsibility lies with the formula industry. Under the WHO International Code of Marketing of Breastmilk Substitutes, companies are not allowed to advertise artificial formula for babies under the age of 6 months. This has unfortunately left a loophole which essentially allows widespread advertising of their products. By using similar branding for all their products, businesses can in effect advertise all their products without breaking the law. Most of the components in infant formula are unnecessary and can actually be harmful. In short, the formula industry is unethically misleading parents and undermining the value of breastmilk.
MV: A recent survey in Bristol found that 63% of the mothers interviewed stopped breast feeding early due to embarrassment of feeding their child in a public place. Do you think the government and companies are doing enough to support these women? What other steps do you think could be taken to reduced stigma?
KB: A difficult question. Normalising breastfeeding is sadly not going to happen overnight, and as always there is a balance to strike. Although formula-milk companies are only allowed to advertise follow-on milk, there is no breastfeeding promotion in the media to ‘sell’ breastfeeding. Bottle-feeding is all around us from slogans on baby clothes and bottles
for dolls, to the mothers we see on television programmes. I think education (in schools) and increased early exposure to the benefits of human milk could play an important role in normalizing breastfeeding for our future generations.
MV: The benefits of breast feeding one’s child include mental health, physical health and saving the planet. How do we encourage new mothers to breast feed without alienating those who simply cannot?
KB: There are several targets set by the Baby Friendly Initiative including antenatal infant feeding discussions and early inpatient support. From the work I did in London, it was apparent that many mothers, including those breastfeeding, were not aware of many of the benefits of breast milk. I think really the focus needs to lie with helping women make informed choices and supporting them to continue breastfeeding. I often get asked why I am so pro-breastfeeding and I try to explain that it’s not about pressurising women who have chosen to use infant formula but providing women with the support to do what is best for them. National data suggests that 80% women stop breastfeeding before they want to. This gives a really important message that we need to improve our support.
MV: What are the three most important things you would like all medical students to know about Infant Feeding?
1. Breast milk is an incredible resource. As quoted in the Lancet ‘If breastfeeding did not already exist, someone who invented it today would deserve a dual Nobel Prize in medicine and economics. 2. Please remember, as a doctor you are a role model. Women will listen and respect what you say. Be careful not to give inappropriate advice. It is much better to refer them to someone who does know, than to undermine the correct advice a woman may have received from her midwife. 3. I also would advise everyone to watch ‘Embarrassed’ by Hollie McNish on YouTube.
MV: If you could give one piece of advice to your first-year medical self what would you say?
KB: Not advice really, but I’d tell her to keep having fun.
Thank you so much to Dr Kirsty Biggs for allowing us to interview her. If you want to get more involved with breast feeding education, then please do check out the Bristol breast project online. The Breast Project is the first UK-wide scheme created to enhance breast education in medical school and inspire the next generation of aspiring surgeons to consider breast surgery as a future career.
Follow them online @breastproject.bristol










