















The government has announced new rules for care providers recruiting international care workers, which will take effect from 9 April 2025.
Under the revised sponsorship requirements, care providers in England must first try to recruit an international worker who is already in the UK and in need of sponsorship before hiring from overseas.
This, the government says, ensures that those who came to the UK to pursue a career in adult social care can do so and will help end the reliance on overseas

recruitment as it seeks to “restore order” to the UK immigration system through its Plan for Change, which sets out a comprehensive plan to restore order to what is says is a “broken immigration system”, linking immigration, skills and visa systems to grow domestic skills, end reliance on overseas labour and boost economic growth.
(CONTINUED ON PAGE 3...)


Editor
Firstly, my apologies for the brevity of this week’s piece! I am currently writing from Birmingham’s NEC, where we are exhibiting at UK Care Week and the Alzheimer’s & Dementia Show.
It’s noon, the venue is buzzing, and the conversations taking place highlight the urgent concerns facing the sector.
Later today, I will be speaking with Nadia Ahmed, who, alongside her colleagues, has been at the forefront of advocating for the sector’s survival.
The primary issue dominating discussions is the looming financial pressure of next month’s National Insurance and National Minimum Wage increases.
With no clear indication from the government on how these will be funded, providers are deeply concerned about how they will cope with yet another financial strain.
Our lead story this week sheds light on another significant challenge: changes to the Skilled Worker visa system.
While the government’s intention to reduce reliance on overseas workers and prevent exploitation is understandable, the sector is already warning that these changes have not been fully thought through.
The care sector remains heavily dependent on skilled overseas workers,

and addressing this dependency will take years, not months.
The government’s proposed solution—to make social care a more attractive career domestically—can only succeed with serious investment and long-term support.
As providers repeatedly stress, improved funding, better working conditions, and recognition of the workforce’s vital role are essential to achieving this goal.
We will continue to raise these concerns and push for the support the sector so urgently needs. If you’re attending NEC today, do come by and say hello—I’d love to hear your thoughts!
I would encourage our readers to sign up for our bi-weekly digital newsletter at www.thecareruk.com and follow us on social media for all the latest news.
I can always be contacted at editor@thecareruk.com


(CONTINUED FROM FRONT COVER)
As well as continuing to tackle exploitation, the government is also continuing its clampdown on abuse in the immigration system with changes to the Short-Term Student route.
“FLOUT RULES”
Seema Malhotra, Minister for Migration and Citizenship, said:“Those who have come to the UK to support our adult care sector should have the opportunity to do so, free from abuse and exploitation.”
“We have already taken action to ensure employers are not able to flout the rules with little consequence or exploit international workers for costs they were always supposed to pay.”
“We are now going further, requiring employers in England to prioritise recruiting international care workers who are already here and seeking new sponsorship, before recruiting from overseas.”
‘The new requirements continue government action announced in November to crack down on employers who abuse the visa system; barring those who repeatedly break immigration or employment laws from hiring overseas workers and will help support those workers into new jobs.”
EXPLOITATION
The changes announced last year also ban companies from charging workers for the cost of their sponsorship, which has never been intended and led to exploitation, unfair treatment of staff and unsustainable levels of debt in the care sector.
Between July 2022 and December 2024, the government has revoked more than 470 sponsor licences in the care sector to clamp down on abuse and exploitation. More than 39,000 workers have been associated with these sponsors since October 2020.
The new changes will also see the minimum salary thresholds updated to reflect the latest data from the Office for National Statistics (ONS). This will ensure those working on the Skilled Worker visa, including care workers, are paid a minimum of £12.82 per hour.
Health and education occupations, including doctors, nurses, allied health professionals and teachers, will also see their minimum rates increased to reflect the latest national pay scales. “VITAL ROLE”
Stephen Kinnock, Minister of State for Care, said: “International care workers play a vital role in our social care workforce. We value their contribution and work supporting vulnerable people across the country every day.”
“As we crack down on shameful rogue operators exploiting overseas workers here in the UK, we must do all we can to get the victims back into rewarding careers in adult social care.”
“Prioritising care workers who are already in the UK will get people back to work reducing our reliance on international recruitment, and make sure our social care Responding to the announcement, the Royal College of Nursing head of independent health and social care, Claire Sutton, said: “It is encouraging that the government is taking steps to support those who have lost their sponsorship to stay working in the UK.
“However, without significant reform staff will still be left at the mercy of employers who unfairly withdraw visa sponsorship, leaving care workers just a matter of weeks to find a new sponsor.”
REQUIREMENT FOR SPONSORS
Oliver O’Sullivan, Director of Immigration, Migrate UK said: “Since the Skilled Worker Health and Care visa was introduced in August 2020, there was a very significant number of visas issued in the category. It has since transpired that a lot of people were being offered sponsorship, for which they were covering the entire costs and upon arriving to the UK were discovering that there was no position for them to fill. Other sponsors had been sponsorship multiple workers to fulfil a future contract, which then did not proceed. This means that there is an unknown number of Skilled Worker Health and Care visa holders who are in the UK without sufficient employment and held in limbo.”
“From 9 April 2025, the Home Office will introduce a requirement for future sponsors of workers in the Health and Care category to demonstrate that they have been unable to find a suitable worker from this pool of workers. Amendments are being made to the rules regarding approving a visa in this category, meaning that a visa can be refused if there is not sufficient evidence that they have attempted to recruit a worker under this provision."
Oliver O’Sullivan added: “The minimum salary requirement for Skilled Worker Health and Care visa holders will increase from 9 April to £25,000 per year (£12.82 per hour). Additionally, the going rate for several occupations for the Skilled Worker visa route are being amended, with minor increases in some cases and minor decreases in others. Employers will need to check the most recent salary before assigning a new Certificate of Sponsorship to a Skilled Worker applicant.”
“WITHOUT COORDINATION”
However, a recent report by the government’s spending watchdog, the National Audit office (NAO) said the department does not have a full understanding of how its skilled worker visa route is operating.
Nuffield Trust Researcher Cyril Lobont said: “This report makes clear that sudden immigration policy changes have happened without proper coordination across government, and with little regard for their impact on essential care services which are struggling to recruit enough staff domestically. Such changes can be implemented at speed, but the problems they create then take years to fix.”
“The social care sector remains hugely reliant on skilled overseas workers to deliver care and support to the people who need it, and we need to retain a route for them to come to the UK. At the same time, we know from our research that more must be done to make careers in social care more attractive domestically.“
“Findings of "widespread evidence" of exploitation and underpayment of wages in the care sector are sadly not surprising. This highlights how important it is that the government gets their new Fair Work Agency set up right to robustly stamp this out.”
“The NAO report is more evidence that there's a need for a clear workforce strategy for the social care sector as the current piecemeal approach just isn't coherent. We already have high vacancies, and projections suggest far more people will need to start working in the sector to meet growing care needs. Plans to build a stable workforce will have to include both a domestic and overseas pipeline, and the government should place evidence front-and-centre when making these critical decisions.”
“REBALANCE RELATIONSHIP”
The Royal College of Nursing head of independent health and social care, Claire Sutton, said: “It is encouraging that the government is taking steps to support those who have lost their sponsorship to stay working in the UK.
“However, without significant reform staff will still be left at the mercy of employers who unfairly withdraw visa sponsorship, leaving care workers just a matter of weeks to find a new sponsor.”
Ms Sutton urged ministers to “rebalance the relationship between migrant workers in health and care and their employers”.
It comes as the Royal College of Nursing (RCN) wrote to the home secretary to demand that she speeds up an investigation into migrant care worker exploitation, which was promised in the 2024 general election.
The union said it had seen an eightfold increase between 2020 and 2024 in enquiries from nursing staff who fear they are victims of exploitation within the social care sector.
Ms Sutton said: “Employers are using excessive repayment clauses to trap staff in their current [situation], providing poor quality accommodation and using threats of deportation to coerce staff into accepting poor pay, terms and conditions.
“A full government-led investigation, beginning urgently, is the only way to identify the scale and types of exploitation taking place and ensure there is a plan to end it.”


Ingrid McGhee, partner and employment lawyer at national law firm Weightmans (www.weightmans.com), shares her expert insight into the Domestic Abuse (Safe Leave) Bill, explaining what it means for care providers, why existing policies may fall short, and the essential steps organisations should take now to protect and support their workforce.
A proposed new law, the Domestic Abuse (Safe Leave) Bill, aims to provide victims with up to 10 days of paid “safe leave” to manage issues related to domestic abuse.
Recently, this Private Member’s Bill advanced to the next stage in Parliament, despite the government’s previous decisions not to introduce such a right.
Although its second reading is scheduled for June, the sponsoring MP, Alex McIntyre, has emphasised that the bill’s aim is to spark a nationwide conversation about making workplaces safer for victims of domestic violence.
Regardless of whether the bill becomes law, the growing focus on domestic violence has brought these issues to the forefront of workplace discussions, with many employers already introducing domestic abuse policies.
WHY THE CARE SECTOR SHOULD TAKE ACTION
Domestic abuse affects people from all walks of life, and the care sector – in which some 80% of workers are women - could be especially vulnerable. The sector also faces high turnover and retention challenges, making it even more crucial for employers to create a safe and supportive workplace.
Currently, many care employers do not offer employees a specific right to paid time off for domestic abuse. Victims are often forced to choose between taking time to seek help addressing their situation and retaining their income. In some cases, they may feel compelled to conceal the true reasons for their absence or declining performance, risking disciplinary action or performance management. Such processes not only intensify the pressure on an already vulnerable employee but also place additional strain on stretched management and HR resources.
Therefore, implementing a domestic abuse policy can offer vital support and reassurance.
A domestic abuse policy provides a formal framework that ensures employees can access the support they need without fear of stigma. This structured approach helps organisations handle sensitive disclosures and provide tangible assistance.
Such policies typically cover a range of practical considerations. For instance, training managers to recognise signs of domestic abuse - such as unexplained absences or behavioural changes - can help them respond appropriately.
Managers must be equipped to handle disclosures with empathy and discretion while ensuring that employees feel safe. Understanding the legal rights available to employees, such as flexible working and non-discrimination protections, is also crucial.
A supportive workplace culture begins with clear, confidential channels for employees to seek help. Care sector employers should offer guidance on how employees can access paid or unpaid leave, flexible working arrangements, or adjustments to work locations. In addition to internal support, employers should provide or signpost employees to external resources, such as Employee Assistance Programmes (EAPs) offering counselling, as well as local domestic abuse charities and legal services. Partnerships with specialist organisations can also help deliver training and additional support.
The benefits of a structured domestic abuse policy extend beyond immediate support. It fosters a culture of trust and compassion within the workplace. Employees who feel supported are more likely to stay in their roles, which helps improve staff retention and team stability — both crucial for a sector grappling with high turnover.
Care sector employers can take proactive steps to ensure they are equipped to support employees experiencing domestic abuse. Establishing a clear and comprehensive policy is a crucial first step, outlining how abuse – such as coercive control, stalking, harassment and malicious communications – will be addressed in the workplace. It should also set out the support available, including leave entitlements and flexible working arrangements.
Training for managers and HR teams is essential. Managers should be able to recognise the signs of domestic abuse and understand how to respond to disclosures appropriately, maintaining confidentiality and ensuring the dignity of the employee. HR teams need to be well-versed in the legal protections available, such as flexible working rights and protections against discrimination.
Furthermore, employers should provide or signpost employees to external support services, including counselling through EAPs, local helplines and legal support services. Access to these resources can help victims navigate difficult circumstances.
A STEP FORWARD FOR THE SECTOR
The Domestic Abuse (Safe Leave) Bill is an important step in raising awareness of domestic abuse in the workplace. While the government has historically resisted introducing paid leave, the bill’s progression perhaps signals a shift in how these issues are viewed.
Even if the bill does not become law, the conversation around domestic abuse in the workplace will continue to influence employer practices. Care sector employers who take proactive steps to support employees will not only protect staff but also foster a more compassionate, supportive workplace culture. By implementing robust policies, employers can improve retention and reduce turnover, helping to create more stable teams within the sector.

Goodwins Hall Care Home has once again demonstrated its unwavering commitment to charitable giving, donating an impressive £800 in the past couple of weeks for both local and national charities. With a long history of fundraising, there is always something happening at Goodwins Hall to support worthy causes.
One of the recent donations was a remarkable £400 contribution to Cancer Research UK. This incredible achievement was made possible by Christine, a dedicated resident at Goodwins Hall, who committed to walking around the home’s garden every day for a month—rain or shine. Christine’s hard work and determination paid off, and she successfully raised a significant amount for cancer research.
To celebrate Christine’s achievement, Goodwins Hall hosted a special high tea, prepared by the talented kitchen team, for Christine, Kerry—the shop manager from Cancer Research UK’s King’s Lynn branch—and fellow residents. The celebration was made even more special by stunning floral decorations provided by Nici’s Creations. Congratulations, Christine—you are an inspiration to us all!
Another £400 was raised for local charity Bridge for Heroes through a highly successful Goodwins Gatsby-themed murder mystery evening. The event was attended by the Mayor and Mayoress of King’s
Lynn, adding an extra touch of prestige to the occasion.
Funds raised from the night were formally presented to Greg from Bridge for Heroes at Goodwins Hall’s Veterans Brunch, a regular monthly event that brings together residents, families, and community members in support of veterans’ welfare. Home Manager Flavia shared her pride in the home’s commitment to charitable efforts: “For many of our residents, supporting charities and helping those less fortunate than themselves has always been a way of life, and it is important to the Goodwins family to carry on supporting local and national charities whenever we can.”
“Most of our open events and family functions have a fundraising element, and we are always delighted with the support we receive from the community, our families, and friends in the care sector for our endeavours. To have donated just a few pence short of £800 in the past week is a real achievement.”

Staff and residents at Elm Bank care home in Kettering are celebrating because their wonderful Regional Directors, Claire Brewer and Isabela Andriuca, from Barchester’s Central Division, are stepping completely out of their comfort zones to compete in the Barchester Charitable Foundation Cook Off 2025.
Swapping their business suits for chefs’ whites, Claire and Isabela are going head to head with two Regional Directors from each of Barchester’s four other divisions to cook up a storm and raise a vital funds for Barchester’s Charitable Foundation. The Foundation helps connect vulnerable people and those living with a disability to community groups in their local area by providing grants to improve mobility and quality of life. Each year the Foundation distributes thousands of pounds to individuals, small community groups and charities across England, Scotland and Wales. In 2024 the Foundation achieved a donation milestone of £335,000 which enabled the charity to provide

vital help to a staggering 239 small groups and charities, plus 104 individuals in one year alone.
Isabela and Claire are keeping their cards very close to their chests regarding what they will be cooking but they have been practising hard. Claire comments: “Isabela and I are passionate about the Foundation so we both jumped at the chance to be able to raise funds and give back. We both love cooking, I am self-taught because I think it is so important for my kids to eat well.” Isabela adds: “We’re both very competitive so really want to win, we will give it our very best shot! The pride of the division is at stake!”
General Manager of Elm Bank care home, Marvellous Bindura, said: “We are all so proud of Claire and Isabela for taking part in this challenge, they really are amazing – is there nothing they can’t do! Their dishes look absolutely fantastic and they will raise so much money for the Foundation, we think they are absolute super stars!

Actor Brian Cox, CBE, sat down with Jordan Adams, who is part of the ‘FTD Brothers’, for an emotional conversation that left a strong impression on Brian.
Jordan, 29, knows first-hand how devastating dementia can be, as his mum died from frontotemporal dementia at just 52. Jordan, and his brother Cian, both carry a rare inherited gene that means they will develop dementia symptoms in their 40s.
Both Brian and Jordan, Ambassadors of the charity, have come together for this moving film to support the Omaze Million Pound House Draw, Scotland. The partnership is raising funds to speed up the search for a cure.
Reflecting on his open conversation with Brian, Jordan said: “It was a once-in-a-lifetime experience sitting down with Brian and sharing my story with him, to support this fantastic campaign between Alzheimer’s Research UK and Omaze.
“Brian was very compassionate. As well as listening to my story, he also shared his own experience
with dementia within his family, which just goes to show that anyone can be impacted by this devastating condition.”
“Sharing my story to raise awareness and support dementia research has opened up some incredible opportunities for me, like this one with Omaze.

“The money raised from this partnership will do so much to help ensure other families won’t be devastated by dementia like my family has been.”
The Omaze draw will fund the Alzheimer’s Research UK Drug Discovery team. This is a team of dedicated researchers who are working tirelessly to speed up the development of desperately needed dementia treatments and bring us closer to a cure.
Actor Brian Cox said: “I am full of admiration for Jordan. Not many people of his age would have the courage to accept their diagnosis the way he has. This has taken huge courage on his part and that is something one has to admire and have respect for.”
Alzheimer’s Research Chief Executive, Hilary Evans-Newton, said: “We are grateful to Brian Cox and Jordan Adams for supporting Alzheimer’s Research UK and for sharing their personal experiences.”
“We hope it inspires more open conversations about dementia and the need for research.”
“Right now, there are no treatments available on the NHS to slow, stop or prevent dementia. But the support of Omaze and everyone who takes part will help to speed up the search for new treatments, bringing us closer to a cure.”






By Raje Ballagan-Evans, Policy and Impact Manager at Social Interest Group
As Social Care
Providers are already delivering solutions for fractional costs, Raje Ballagan-Evans asks, why are we being snubbed by the NHS?
In 2023/24, there were 450,000 delayed transfers of care (DToC), meaning huge numbers of people fit for medical discharge but blocking beds in hospitals as they await social care assessments and adjustments to be put in place.
As NHS Chief Executive Amanda Pritchard told the Health and Social Care committee earlier this year, these delays prevent new patients being admitted for medical help to the extent that A&E 4 hour performance is decreased by an estimated 6%.
Many of the people waiting are older people or those with multiple needs. Any new or increased care needs carry commitment and finance demands that family may be unwilling or unable to meet. Residential services may be unable to step in because of unviable fees being offered to them to deliver care. Whilst disputes are settled, a family member remains in a free bed with care provided by hospital staff.
Preferences of patients and their advocates must rightly be taken into consideration and it is hard to emphasis enough how important this is when it comes to care and support needs. This is enshrined into law for regulated activities (Health and Social Care Act 2014).
So what is the solution to managing the tension between the dignified and caring support we need to ensure for those leaving hospital to have appropriate provisions in place to be safe and independent, and freeing up beds for medical treatment, and preventing loss of life for those in an emergency?
Firstly, we need to understand the gravity of the impact of blocked beds; an NHS bed costs between £345 to £2,349 according to 2020/21 figures. In 2023, The King’s Fund estimated this to

equate to at least, £1.7 billion.
These are shocking statistics but the human cost is even higher. People who need treatment, even in an emergency, are unable to be admitted to A&E, whilst planned operations and surgeries are cancelled as there is no capacity on wards to receive patients once they come out of theatre.
Staff are left managing people in ambulances outside of hospitals, whilst wards take care of patients that should not be in hospital. And what about the patients stuck in the bed? They are left at increased risk of infection, and deterioration of health, mobility in particular.
In light of these stark facts, it is a cause of anger and dismay that despite ongoing inefficiencies as more and more money is pumped into the NHS, leaders continue to commission themselves to provide services.
Rather, they ought to be looking to social care organisations that can provide vital services and support, that are community based, efficient and great value for money. Sound too good to be true? SIG Penrose’s STEPS project is already delivering. The service facilitates direct support to people in Luton hospitals who have move on needs.
This is vital because in the midst of the current housing crisis, patients with complex needs are most likely to face homelessness and loss of tenancy. A myriad of housing and income challenges keeps them stuck in a hospital bed.
STEPS work on behalf of patients with social workers, housing officers and welfare agencies. Leaning into our community network of housing partners, we enable efficient and appropriate move on into safe accommodation. This service is evidenced to reduce the average length of hospital stay from 35 days to 19.
A return on investment analysis, conducted in partnership with a ward at Luton and Dunstable General Hospital, estimated that STEPS delivers the local NHS Trust an average saving of £12,208 per patient. This equates to over £2.1 million per year based on the 176 people supported by the programme last year. Or in ROI terms, £55 in savings for every £1 invested.
Person centred, efficient, value for money services are what we need nationally at a time when the NHS is in crisis. Obvious and well evidenced solutions from social care providers are abundant but statutory organisations must stop seeing us a less sophisticated sweep-up operation and fund us as equal partners in delivering fair care.
Chiltern Water & Environment was established in 1991 by Robert Hunt after gaining 25 years' experience as an operational and analytical scientist in the water supply industry. The company gained engineering and further management knowledge when David Hunt joined in 2012. Since then, other water industry professionals have added to the breadth of knowledge and experience within the company.

We have always provided high-quality consultancy, testing and remedial services in a professional but personable manner. Our steady growth has reflected our clients' trust in our services. Our current clients include large housing associations, pharmaceutical companies and facilities management companies, as well as individual landlords and small businesses. We ensure all our customers receive the same level of care and attention to detail.
Duty Holders of all commercial and public building premises are legally required to assess the risk from legionella to anyone using the water systems and put in place legionella control measures if required. The HSE has produced ACoP L8 and HSG274 as guidance for Duty Holders obligations. We have clients throughout the South East, London and the Midlands, and carry out water tests nationally and internationally. We currently provide regular water sampling and testing for over 500 sites.
Tel: 01844 347678
Email: info@chilternwater.co.uk www.chilternwater.co.uk
In a significant policy shift, Prime Minister Sir Keir Starmer has announced that NHS England will be abolished, with its responsibilities brought back under the Department of Health and Social Care.
The prime minister said the independent body which runs the NHS would go in a move to cut red tape and dramatically reduce costs by cutting duplication.
The reform, which marks a departure from the health service structure implemented over a decade ago, is expected to lead to a significant reduction in administrative roles, with approximately half of NHS England’s workforce set to be impacted.
Ministers argue that the restructuring will result in hundreds of millions of pounds in annual savings, which will be redirected towards reducing patient waiting times and improving direct care.
Speaking in Yorkshire, Sir Keir outlined his vision for a leaner, more efficient NHS, stating: “We are committed to cutting bureaucracy across government, ensuring that resources are focused where they are most needed – on patient care. By bringing NHS management back under democratic control, we can ensure that every pound is spent in the interests of the public.”
The Prime Minister highlighted the issue of duplication within NHS England, referencing parallel teams in both NHS England and the Department of Health and Social Care working on similar tasks. He described the change as a necessary step to eliminate inefficiencies, allowing for a clearer, more effective approach to healthcare management.
The move follows a wave of senior departures from NHS England, including its chief executive and medical director, and represents a fundamental shift in how the health service is administered.
Health Secretary Wes Streeting welcomed the decision, stating: “This marks the end of a structure that has not delivered the efficiency and effectiveness our NHS needs. Our priority is to ensure that the health service is focused on delivering timely, high-quality care to
patients.”
Nuffield Trust Chief Executive Thea Stein said: “Today’s news will be devastating for staff at all levels of NHS England, and we must remain mindful of the human cost of this decision. With the public finances under extraordinary pressure it does, however, make sense to remove the duplication and bureaucracy that exists currently – and patients and the public are probably not going to shed many tears over the shifting of power from an arm’s-length body into central government.”
“But profound problems facing the NHS remain: how to meet growing patient need in the face of spiralling waiting lists and how to invest in care closer to home with the NHS’s wider finances already underwater and social care reform in the long grass. It is not immediately clear that rearranging the locus of the power at the top will make a huge and immediate difference to these issues, which ultimately will be how patients and the public judge the Government.”
“Furthermore, the Government should be careful that this doesn’t lead to even more top-down micro-management of local services from Whitehall, which has been the bane of the health service. NHS England was set up to take the politics out of the NHS, but today politics has taken out NHS England.”
The planned restructuring has sparked discussions within the healthcare sector, with questions being raised about the potential impact on local NHS services, staffing, and long-term planning. The government has assured that while administrative changes will take place, patient care will remain the top priority, with a renewed focus on cutting waiting times and improving outcomes.
As details of the transition unfold, those working in the residential and nursing care sectors will be closely monitoring how these changes will influence care provision, staffing structures, and resource allocation in the coming months.
A ‘SEISMIC SHIFT’ FOR HEALTH AND SOCIAL CARE
Professor Martin Green OBE, Chief Executive of Care England, said:

“The decision to abolish NHS England is one of the most significant reforms to our health and social care system in a generation. While the full implications of this change are yet to be seen, this is a moment to ensure that social care is fully recognised as an equal partner in the health and care system. The success of the NHS depends on a sustainable and properly funded social care sector, and this announcement must mark the beginning of a new era of integration and collaboration.”
For too long, adult social care has been treated as a secondary consideration in health system reforms. With the government’s commitment to reducing bureaucracy and directing more resources to frontline staff, there is now a unique opportunity to develop innovative models of care that truly integrate social care and health services.
While we need to ensure that immediate changes do not disrupt Continuing Healthcare (CHC) funding processes for the current financial year, this is also a crucial opportunity to rethink how CHC is funded, and lay the foundation for a national framework that aligns CHC processes with Funded Nursing Care (FNC) practice, providing much needed fairness and predictability across the sector.
Care England is calling for:
• A clear strategy on how social care will be embedded in the new structures to drive better outcomes for people who rely on both services.
• A commitment to sustainable funding for social care to support hospital discharge, reduce pressure on the NHS, and enable people to live independently for longer.
• A national CHC framework that mirrors FNC practice, ensuring fair, consistent, and timely decisions across all local areas.
Professor Martin Green OBE added: “If this change is to succeed, it must not be a rebranding exercise. It must deliver real benefits for people who need care and support. Social care is not an adjunct to the NHS, it is a vital part of the system, and this reform must finally acknowledge that reality.”

•
and
• They can be bought as seen or refurbished and sign-written to your own requirements.
• Fully serviced, new mot & warranty
• Engineers inspection supplied if required.
•
•


By Derek Aaronson, Founder & CEO of Hart Home Group

Infection control and prevention are critical components in safeguarding the health and wellbeing of individuals in medical, commercial, and domestic environments. For the independent nursing and residential care home sector, maintaining stringent infection control measures is not just a matter of compliance, but a fundamental responsibility to ensure the safety of vulnerable residents. As the world continues to grapple with new and evolving health threats, the importance of infection prevention cannot be overstated.
THE IMPORTANCE OF INFECTION CONTROL IN CARE HOMES
For nursing and residential care homes, infection control is especially crucial. Residents often have weakened immune systems due to age or pre-existing conditions, making them more susceptible to infections. In such settings, even a minor lapse in hygiene protocols can lead to the rapid spread of pathogens, which can have devastating consequences. Healthcareassociated infections (HAIs) continue to be a significant risk in care homes, leading to longer hospital stays, higher medical costs, and, in severe cases, death.
Therefore, infection control in care homes requires a combination of effective policies, thorough cleaning routines, and specialised equipment. Staff must be well-trained in infection prevention, and robust systems need to be in place to manage outbreaks when they occur. However, achieving a high standard of hygiene in care homes comes with its own set of challenges.
THE CHALLENGES OF INFECTION CONTROL IN CARE HOMES
Maintaining high levels of hygiene in care homes can be difficult for several reasons. The close proximity of residents, especially in shared rooms, communal spaces, and bathrooms, increases the risk of crosscontamination. Frequent touching of high-contact surfaces such as handrails, doorknobs, and shared equipment can facilitate the spread
of germs. In addition, staff turnover and the demanding nature of care work mean that infection control protocols may not always be followed consistently.
The traditional reliance on manual cleaning methods can also be time-consuming and may not always be effective in eradicating harmful bacteria and viruses. With the rise of antimicrobial-resistant organisms (AROs), which are more difficult to treat, care homes must adopt more advanced solutions to combat the spread of infection.
SOLUTIONS TO ENHANCE INFECTION PREVENTION IN CARE HOMES
The solution to these challenges lies in a combination of better practices, staff training, and, crucially, the use of advanced infection control technologies and equipment. Specialised hospital-grade fixtures, such as antimicrobial door handles, bed rails, and mobility aids, are invaluable in preventing the spread of infection in care homes. These fixtures are designed with non-porous materials that are easy to clean and resistant to microbial growth, ensuring that harmful pathogens have fewer places to thrive.
In addition, the use of touchless technologies is gaining traction in care homes as a way to reduce human contact with frequently touched surfaces. For example, touchless faucets, soap dispensers, and hand sanitisers can significantly minimise the risk of cross-contamination. These innovations not only make it easier to maintain hygiene but also improve the overall user experience for both staff and residents, especially for those with limited mobility.
Innovative cleaning solutions, such as UV-C sterilisation devices, are also helping care homes maintain higher standards of hygiene. UV-C light has been shown to be effective at killing bacteria, viruses, and fungi on surfaces and in the air , providing an added layer of protection that manual cleaning alone cannot guarantee.
THE ROLE OF DESIGN AND PRODUCT INNOVATION
The role of design and product innovation in infection control is crucial. Products designed with infection prevention in mind—such as hospital-grade furniture, non-porous flooring, and antimicrobial textiles—play a crucial role in reducing the potential for cross-contamination in care homes. By choosing products made from materials that are resistant to bacterial growth and easier to sanitise, care homes can significantly reduce the risk of infections spreading.
Mobility aids, including walkers, wheelchairs, and lift chairs, are another area where innovation is making a difference. Many of these products now come with antimicrobial coatings that help reduce the risk of pathogens accumulating on surfaces frequently touched by
both residents and staff. These small changes in the design of everyday equipment can contribute to a cleaner, safer environment for both residents and caregivers.
Moreover, the growing use of digital solutions, such as automated temperature monitoring, air quality control systems, and remote monitoring devices, is transforming infection control in care homes. These technologies allow staff to track and manage infection risks more efficiently, making it easier to identify potential outbreaks before they escalate.
EMERGING TRENDS: TOUCHLESS TECHNOLOGY AND SUSTAINABLE MATERIALS
As the infection control industry evolves, there are two key trends that are gaining momentum: the integration of touchless technology and the use of sustainable materials. The increasing adoption of touchless systems, such as motion-activated doors and automated sanitation stations, is helping to prevent the transmission of pathogens, especially in high-traffic areas. These technologies not only improve infection control but also enhance the overall user experience by reducing the need for physical interaction, which is particularly beneficial in care settings where residents may have limited mobility or dexterity.
Sustainability is another important consideration in infection prevention. The use of environmentally friendly materials—such as biodegradable cleaning products, sustainable textiles, and recyclable medical supplies—ensures that infection control measures are both effective and responsible. The growing demand for eco-friendly solutions in care homes is part of a larger global movement towards sustainability, where reducing environmental impact goes hand-in-hand with enhancing hygiene standards.
Infection control and prevention are vital to ensuring the health and safety of residents in care homes. While the challenges of maintaining hygiene in these environments are significant, the solutions are becoming increasingly effective with advancements in technology and product innovation. From hospital-grade fixtures and antimicrobial mobility aids to touchless technology and sustainable materials, these innovations are helping to reduce cross-contamination and improve overall safety. As the sector continues to evolve, adopting these innovations will be key to enhancing infection prevention protocols and safeguarding the health of vulnerable individuals across nursing and residential care homes. Through a combination of best practices, innovation, and thoughtful design, care homes can create a safer, cleaner, and more resilient environment for residents and staff alike.
A resident at HC-One’s Hambleton Grange Care Home, in Thirsk, North Yorkshire, has revealed her secret to a long and happy life in celebration of her 104th birthday.
Jean Smith, resident at Hambleton Grange, is a quiet lady and did not want a fuss about her mega milestone birthday. Jean enjoyed her special day on Friday, March 7, along with her daughter Moira and the team at Hambleton Grange.
Jean chose a Dundee cake for her birthday and a poached salmon salad for lunch. She received lovely flowers and cards from friends and relatives, and she was very grateful for everyone's kind wishes.
Jean grew up in Aberdeen, where she married her husband and subsequently moved down to Thirsk during the 1950's. She worked as a shop
Social Care TV continue to fly the flag for highest quality online training for Health and Social Care, after unwavering commitment to excellence within the sector for over 25 years.
Their widely-used health and social care specific courses - produced and edited in-house - are expertly designed to make learning engaging, informative and, therefore, highly effective for learners.
Accredited by CPD and endorsed by Skills for Care, training with Social Care TV is quality assured, comprehensive and relevant. As one of the leading online training providers in the health and social care sector in the UK, they supply training for local authorities, recruitment agencies, care home groups and other health and social care organisations.
Their feature-rich Manager platform has further been enhanced this year with the introduction of several new Manager tools designed to aid with compliance, reporting and trainee management. Features now available include:
• Compliance Dashboard with Traffic Light System

• Downloadable Trainee Matrix
• Custom Bundles
• Trainee Groups
• Bulk Uploads
• Bulk Enrolment Onto Custom Bundles
• Course Enrolment Notifications
• Course Reminders
assistant before raising her daughter Moira.
Jean was the eldest of three siblings, as she had an older sister and brother, and Jean would help care for her mother when she was poorly. Jean’s life has revolved around her family, and she enjoys spending time with her grandchildren and great grandchildren when they visit.
When asked her secret to a long life, Jean said:
“I am very lucky everyone here is so kind to me, and I am lucky to live here. Show love, kindest and be grateful for every day.”
Elaine Snowden, Hambleton Grange Lifestyle Manager, stated:
“It is important to us to help our residents create memories that will last forever, and we feel privileged to have been able to celebrate Jean’s 104th birthday with her.”

SCTV regularly release new and updated high-quality courses. Previews for all courses can be viewed at: Courses - Social Care TV (www.social-care.tv/courses/course-details)
To enhance their learners' experience further they have created free, comprehensive subject-specific workbooks which were rolled out across all courses this year. This unique addition provides excellent value and a fully robust training package.
SCTV are delighted to have won several awards over the last 12 months including:
• Best Online Health and Social Care Learning Platform’ – Global
Health & Pharma Social Care Awards 2024
• ‘CPD Provider of the Year’ – The CPD Awards
• Social Care Training Provider of the Year’ - Corporate Livewire
Innovation & Excellence Awards
Gold standard customer service remains a core staple of the business, with expert support and guidance provided via telephone, email and live chat. They place great importance on the training and development of their customer services team to ensure that they continue
to provide a personal, friendly and knowledgeable service.
Their much-loved ‘Care Worker of the Month’ award recognises and rewards the selfless dedication shown by care workers across the UK and they proudly support the Care Workers Charity who aim to advance the financial, professional and mental wellbeing of social care workers.
SCTV believe that high quality training should be accessible to all and offer regular, free courses which include a digital certificate accessible via their website.
The company stands behind a clear mission and set of values which define their ethos and their dedication to both the Care Sector and those within it. These can be viewed at: Mission Statement and Core Values - Social Care TV
(www.social-care.tv/about/mission-statement-and-core-values) Social Care TV are a responsible business, committed to ensuring that their actions have a positive impact on their employees, customers, the wider health and social care community and the environment.
Above all, SCTV consistently strive to make a meaningful contribution to the wellbeing of those being cared for.
For more information please see: Homepage - Social Care TV (www.social-care.tv) and see advert on the facing page.
Social care experts at the University of Birmingham have launched a series of guides and a training video to improve support for older people, families and care staff when care homes close.
The three guides, released today (19th March), provide advice to help improve outcomes for care home managers, staff members and care home residents and their families when their care home is going through a closure process.
The guides and video were produced as part of a research project called ‘Achieving Closure’, funded by the National Institute for Health and Care Research (NIHR). The research explored the different experiences of older people, families, care staff, social workers and managers, and the impact that closures can have on the well-being of staff and outcomes for older people.
Jon Glasby, Professor of Health and Social Care at the University of Birmingham, who led the project said: “Care homes support their residents 24 hours a day and 365 days a year, so by definition, these are people’s homes. But many care homes close every year, whether through an emergency like a fire or flood, councils or care providers making strategic choices to develop new service models, the financial position of the home no longer being viable, a private provider might sell up or go bust, or a home is forced to close by authorities following the discovery of poor care.
“The closure of a home can negatively impact not only residents, but their families and of course the staff working there. Despite this there is almost no prior research and very little guidance to help Councils manage closures as best they can, to limit the potential harms that can be caused.”
Drawing on the experience of older people, families and staff directly involved in care home closures in different case study sites across the
country, the policy guide sets out ‘ten top tips’:
1. Closures are inherently distressing for everyone involved and should only be a last resort.
2. Councils, care home owners and managers should support care staff as best they can, emotionally and in terms of their future employment and financial well-being.
3. Time really matters – creating as much space as possible to work at the pace of the individual can make a real difference.
4. However much you communicate, it’s never enough – Communication is crucial and should be planned and frequent, keeping people informed is vital.
5. People may not be able to influence whether or not the home closes, but any choice and control they can have over what happens next is really valued.
6. It’s important to pay attention to the so-called ‘basics’, such as being compassionate and empathetic and sorting any practicalities.
7. Some people may need additional support – for example if they have dementia or a sensory impairment, or do not speak English as a first language.
8. Families provide really important support; however, we shouldn’t ‘exploit’ families’ during closure, and we need to make sure people don’t lose out if they don’t have family nearby.
9. The ‘little things’ matter for residents (how you like your tea, what sort of pudding you like, where you like to put your handbag etc) – paying detailed attention to these can make a big difference.
10. Things can get worse, but things can then get better as people settle into a new home.
The guide for older people and their families focuses on managing the stress that can be caused, practical advice from people who have
gone through closure and ways to focus on things within their control.
For staff, the guide focuses on the stress that staff can experience when they find out the care home is closing, how care workers can make a difference to residents during the closure, the importance of making time to spend with residents, identifying people who made need extra support, and advice from staff who have come out the other side of closures.
The training video is for anyone involved in closures – but will be particularly helpful for care staff who may not always have access to time or resources for training and development.
Caroline Abrahams, Charity Director at Age UK, chaired the study’s Advisory Board: “It’s been great to be involved with this project because sadly, care homes do sometimes have to close. When this happens, it is tremendously important that older people forced to move elsewhere, and their families, have the information and tools available to help them make a successful transition.
“Local authorities, care providers and their staff also need to understand what they can do to make the process as painless as possible. The project’s outputs provide all of these things, drawing on thorough research. I hope these materials will be widely used as they have the potential to make difficult situations less distressing for care home residents and staff, and commissioners alike.”
Professor Glasby concluded: “When people move into a care home, they assume it’s a home for life. But sadly, a number of care homes close each year, and Councils have not previously had detailed, research-based guidance to support them in undertaking such difficult and important work. We hope these resources help to improve support, make care home closures more manageable and protect people from the worst of what is often a scary and confusing situation.”
Residents and members of the community, were delighted to welcome PC Tricia and PCSO Len from the local police force to join the home at Mallard Court Care Home for their ‘Coffee with a Coppa’ event.
PC Tricia and PCSO Len spoke to the audience about their own career paths, why they wished to join the force, and shared updates about the latest goings-on within the town, before taking questions from the audience.
Ange Dooley-Widd, the General Manager of Mallard Court Care Home, has extended the invitation throughout the local area, stating

that “to say thank you for all of the great work our emergency services do for us, we here at Mallard Court are inviting all members of the police, ambulance, and fire services to pop in and take their duty break on us for free.
“We are pleased to offer all of our local service workers who stop in tea, coffee, juice, chilled water, delicious homemade cake and biscuits, and a healthy selection of fruit, available free of charge. Our comfortable facilities include free Wi-Fi and service with a smile; do stop in and say hi, we would be delighted to see you!”


Efforts to deliver one of the government’s major NHS priorities to shift more care into the community will need to be boosted by targeted capital investment in buildings, facilities and equipment for community providers, according to a new survey of senior health leaders.
Nearly nine in ten community provider leaders say they don’t have access to the capital funding they need. They say this is impeding their efforts to improve productivity and that it will make it harder to achieve the government’s ambitions to deliver more care out of hospitals and in the community.
Capital investment in the NHS has mainly prioritised hospitals, with little going towards community health providers which provide vital services including district nursing, health visiting, child health and other services. These community services are responsible for 13 per cent of all daily NHS activity and represent one in five NHS workers.
THE SURVEY BY THE COMMUNITY NETWORK –HOSTED BY THE NHS CONFEDERATION AND NHS PROVIDERS – FOUND:
• More than four in five respondents (86 per cent) said buildings and facilities were a barrier to greater productivity
• Two in three providers (66 per cent) said digital systems were a priority for investment to boost productivity
• Two in three (66% per cent) said that the state of community facilities isn’t improving patients’ experiences
• Nearly nine in ten (88 per cent) said they couldn’t secure adequate capital funding.
Siobhan Melia, Community Network chair and
chief executive of Sussex Community NHS Foundation Trust, said: “Community providers will play a central role in delivering the government’s commitment to shifting more care closer to home. For it to be a success, community providers need essential capital funding to scale up delivery and collaborate with system partners in line with the government’s aim.
“National leaders need to prioritise capital investment in technology and estates for community health services. Investing today will bring savings tomorrow and a better experience for patients and their families.”
Matthew Taylor, chief executive of NHS Confederation, said: “The government’s desire to provide more care closer to home is right, and community providers have a vital role to play in this. But the ambition will be jeopardised unless community services have access to targeted capital investment for building, equipment and technology which will enable them to deliver more care, provide a better patient experience and to improve productivity.”
Saffron Cordery, interim chief executive of NHS Providers, said: “Community services and patients are suffering the effects of years of national capital underinvestment. The sector’s buildings and systems are becoming increasingly inadequate for the task being asked of them.
“To fulfil government ambitions, to increase capacity, achieve greater productivity and improve experience for staff and patients, community providers need access to adequate capital funding.”



An issue which frequently arises for care home operators is when they need to make a financial claim against the estate of a deceased resident for unpaid or outstanding fees. This can be complicated if the former resident was married but most of their assets are tied up in the marital home which their spouse still lives in. Another common situation is where there are insufficient funds left in the estate and the former resident would have qualified for Local Authority funding had they survived.
To manage these situations effectively, it is best practice to maintain good records of the contractual terms agreed, of fees due and invoices raised and what is outstanding. This helps prevent parties disputing the quantity of the bills, or where executors were unaware of what had been agreed.
It is hoped the care home operator has a good rapport with the deceased’s family so they can sensitively approach them with the outstanding invoices and ask them to be included as debts of the Estate. This helps probate practitioners and will assist with debt recovery when the Grant of probate has been obtained. Thankfully in recent months it is now a faster process following the delays which built up following the Covid pandemic.
If the deceased owned a property (either under marriage or not), then there may be a right to pursue the debt against their asset. It would need to be considered if they died with a Will, whether a life interest trust was created under that Will (i.e. if people are still living in the house), and how the property was owned and
By Katarina Morgan, Associate Solicitor at Taylor Walton Solicitors
how much of it was owned by the deceased, whether there is any outstanding mortgage or equity release scheme in place. It is for this reason why good contractual terms need to be set out clearly and what happens in these circumstances.
If there are insufficient funds in the Estate, then the Estate will be insolvent. This means that the debts will be paid in a certain order:
o Secured creditors: mortgages or secured loans
o Funeral expenses: reasonable and proportionate to the size of the Estate
o Testamentary expenses: administrative costs
o Preferred and preferential debts: employee wages for example (not likely to apply)
o Unsecured creditors: care home fees, bank loans, other debts
o Interest on unsecured loans
o Deferred debts: informal loans between family members
If Local Authority funding may have been available, then the administrator of the deceased’s Estate (executor or administrator) may be able to make a retrospective claim. They will have to apply to the Integrated Care Board (ICB) which is the NHS body that assesses eligibility for NHS Continuing Healthcare funding where there is a need. That person will need to contact the ICB for guidance on how to deal with previously unassessed periods of care. It is likely that this may take a number of weeks if not months to be resolved and it would likely to be challenged given the universal squeeze on public budgets.
Prevention of debts building up is always the best option, but it is not always avoidable. Ultimately having good, clear contractual terms which explain what has been agreed in terms of fees and when they can expect to be recovered and how is essential for every care home operator. Each case will of course depend on its own facts, and you may want to take legal advice to help you recover larger amounts.
This winter, Recreo VR is offering care homes an exciting opportunity to enhance resident wellbeing through the power of Virtual Reality (VR). By signing up for one of our 24-month Recreo Theatres packages, you’ll receive a free VR headset and staff training.
Our platform provides person-centred, budget-friendly activities that are fun, engaging, and accessible, especially for residents who are bedbound or socially isolated. Co-created with Alzheimer’s Society and individuals with dementia, our service empowers staff to deliver personalised reminiscence and one-to-one sessions that promote memory recall and connection.
Our VR headsets have been recognised as good practice by the Care Quality
Commission (CQC), further validating their impact on care. Regular use of Recreo VR has a proven positive effect on wellbeing, with residents reporting increased activity, engagement, and social connection, often leading to a reduction in the need for PRN medication.
Whether combating loneliness, promoting relaxation, or enhancing cognitive health, VR offers a non-pharmacological solution to enrich care and elevate quality of life. Don’t miss out! Take advantage of this exclusive offer and see how VR can transform your care home experience.
For more information, visit recreovr.co.uk. Or contact us at info@recreovr.co.uk or 01482 526940.



Many people with mental health needs are not getting the care they need, the Care Quality Commission (CQC) highlighted in a report published this week.
As part of its monitoring activity in 2023/2024, CQC interviewed over 4,500 people who were detained under the Mental Health Act or ‘sectioned’, covering 870 wards, and speaking to relatives and people who were previously detained. This year’s Monitoring the Mental Health Act report once again raises that a lack of staff, beds, and training, are leading to harmful gaps in care and treatment.
With demand far outstripping capacity, there are not enough beds available, meaning people are placed far from home, their family, and their friends. One mother who was detained was placed 5 hours from home and because of this she didn’t receive any visitors during her time in hospital. Another woman had to wait hours in a police staff room, accompanied by two police officers, while a bed was sourced.

There are not enough staff to support all patients, which is affecting people’s access to care and leading to people being restricted from going outside as there is nobody to supervise them, or in the most extreme cases, people being inappropriately confined.
While many people describe healthcare workers as “caring” and “wonderful”, there are ongoing concerns with staff numbers and training. In particular, not all staff have undertaken the mandatory training to understand the needs of autistic people and people with a learning disability.
The combination of overwhelming demand and limited resources has led ward managers to feel pressure to discharge the “least unwell” patients. One woman reported being discharged before she was ready and without support to find her way home; she subsequently overdosed. Another person said, “I was only discharged because I was 18, not because I was better.”
Despite a legal entitlement to aftercare, overstretched general practice and community mental health services are not always able to provide a supportive transition back into the community, meaning people do not have the best chance at recovery. In nearly half of cases where a child or young person was detained, they had to be re-admitted within a year.
Young people, people from ethnic minority groups, and people from areas of deprivation face the biggest barriers to accessing care and are sectioned at higher rates than the general population. Black people in particular are detained at 3.5 times the rate of white people. Meanwhile people from the most deprived areas are attending A&E services for their mental health at 3.5 times the rate of people from the least deprived areas.
CQC remains concerned that a lack of suitable community resources continues to lead to inappropriate hospitalisation of people with a learning disability and autistic people, although our early work on Independent Care (Education) and Treatment Reviews has seen people move out of long-term segregation.
The regulator is calling for national action to tackle system-wide issues in community mental health. Better funding, improved community support, and a specialised and sustainable workforce is needed to ensure that people receive the care they need.
Interim director of mental health at the Care Quality Commission, Jenny Wilkes said: “These issues will be all too familiar to people in mental health crisis, and their loved ones. We urgently need more community support and a better understanding of people’s needs to reduce the number of people being detained. And we know the situation is even starker for people from deprived areas, people from ethnic minority groups, autistic people and people with a learning disability. While the Mental Health Bill aims to address inappropriate detentions and improve mental health care, this can’t be addressed by legislation alone as there simply aren’t the resources to fix these issues.
“Without timely access to necessary mental health support, people may find themselves being bounced from service to service without ever receiving the level of care that they need. This is a particular concern for children with mental health needs who risk missing out on school and their social life, and carrying their trauma and feelings of isolation into adulthood.
“It is essential that the government addresses these significant gaps now to protect people for the future. With the right funding, a sustainable and well-trained workforce and enough beds to meet demand, we can break this damaging cycle.”
Around Global Recycling Day (Tuesday 18th March), more than 40 Care UK homes have launched the pilot scheme for Generations of Change. This brings together primary school children and care home residents, encouraging them to share knowledge, learn from one another, and work together towards a more sustainable future.
By creating downloadable packs with resources for teachers, Care UK has created fun and interactive activities to help facilitate intergenerational lessons. Together, children and older people will explore topics like biodiversity and climate change and discover how everyone can contribute to making a positive difference in their community. Topics for the educational packs range from biodiversity to food sustainability, climate change to recycling and are available for free on Care UK’s website.

In honour of Global Recycling Day, homes from Edinburgh to Cambridgeshire’s St. Ives took part in a variety of activities to celebrate the beginning of Generations of Change. These included food markets with local schools, sowing seeds in care home gardens or allotments, upcycling old clothes and litter picking.
The pobroll® is the invention of Pat O’Brien, a physiotherapist, Moving and Handling trainer, and Conflict Management tutor with over two decades of experience in care homes and nursing homes
Care home managers often face challenges in delivering intimate care while balancing efficiency and managing costs, particularly when these essential tasks provoke behaviours that can be challenging to safely manage. Traditional methods—especially for bed-bound residents—often lead to lengthy processes and frequent linen changes, driving up costs and consuming valuable staff time. The pobroll® provides a transformative solution that supports dignified care, achieves significant cost savings, and reduces the need for additional staffing.
The pobroll® is an innovative bed-bathing wrap specifically designed to enhance comfort and dignity during personal washing for individuals who require in-bed care. Centred on the resident’s experience, it minimizes distress by providing sensory comfort. Crafted with two layers of high-quality cotton-terry toweling and a waterproof layer in between, it delivers a soothing, calming experience while keeping the bed completely dry. Sized for a standard single bed, the pobroll®’s dual-layer design offers warmth and a sense of security and privacy, allowing residents to maintain comfort and dignity during bed-based bathing routines.
BOOSTING COST SAVINGS AND OPERATIONAL EFFICIENCY
Generations of Change was originally the brainchild of Vicki Lambourne, the Senior Customer Relations Manager at Winchcombe Place in Newbury, who credits her home’s close relationship with the nearby Winchcombe School for the idea. The idea has now been adopted as a Care UK-wide initiative, complementing its ESG values and community commitment, as seen in their recent Harvest Festival campaign.
Tony Weedon, Care UK’s Strategic Programme Director, said: “At Care UK, we are continuing to create new ways to promote sustainability and encourage community-building. As a large provider, we take our responsibility as stewards of the environment seriously – whether this is in the village, town or borough that our individual homes are based in. “I am very excited to see how Generations of Change can bring together these two goals and support young children and older people in our communities to share knowledge and develop new skills. We know from experience that residents find spending time with children particularly valuable, and we believe the introduction of these free resources will encourage more schools to reach out to their local Care UK home and get involved.”

pobroll® provides an effective solution that supports both economic and environmental goals.
Managing resident agitation—particularly for those with dementia—often requires specialised training in restraint techniques. The pobroll® significantly reduces the need for physical intervention by providing a warm, secure covering that alleviates resident distress. This gentle approach minimizes aggressive or defensive reactions, reducing the number of staff needed for these interactions. As a result, facilities can potentially lower staffing levels without compromising care quality, yielding substantial cost savings. Additionally, reduced dependence on physical intervention decreases training costs associated with restraint techniques. By simplifying the process of intimate care, the pobroll® reduces the need for specialised training, making onboarding smoother and lowering turnover-related training expenses.
The pobroll® supports compliance with restraint reduction guidelines, helping facilities minimise documentation burdens and regulatory liabilities linked to physical interventions. This non-invasive solution improves safety for both residents and caregivers, fostering a culture of dignity and respect that boosts satisfaction among residents and their families.
CONCLUSION: A VALUABLE ASSET FOR QUALITY CARE AND COST MANAGEMENT
The pobroll®'s waterproof design enables caregivers to provide a complete wet wash without the risk of soaking the bed, minimising the need for frequent linen changes. This leads to fewer laundry loads, reducing labour and utility costs, as well as wear on linens. By reducing logistical tasks, caregivers have more time to focus on direct resident care, enhancing productivity overall. Additionally, reduced reliance on disposable wipes results in further cost savings and supports environmentally sustainable practices. With its durable, reusable design, the pobroll® maintains hygiene standards and allows for extended use across multiple residents. As care homes face increased pressure to adopt sustainable practices, the
For care homes, the pobroll® represents a strategic investment, offering measurable savings by reducing reliance on disposable products, lowering laundry and training costs, and enabling efficient staffing. Most importantly, it prioritises resident dignity and comfort, setting a high standard for compassionate, personcentred care. For facilities seeking to enhance financial performance and care quality, the pobroll® is an invaluable addition to their resources.
Fof further information, see the advert on the facing page.
Care England has announced the establishment of the Working Age Adult Policy Board, a significant step in strengthening advocacy and shaping policy for one of the most underserved areas of the sector.
The Working Age Adult Policy Board has been created to give a dedicated voice to providers supporting working-age adults and to tackle the distinct challenges this group faces within social care. By bringing together sector leaders, the board will play a pivotal role in influencing policy, ensuring that the needs of working-age adults remain a priority at the highest levels of decision-making.
The new board will provide a collaborative space for sharing expertise, identifying sector-wide challenges, and formulating impactful policy recommendations. It will also ensure that providers delivering services to working-age adults are properly represented in national and local advocacy efforts.
Key objectives include:
• Strengthening Care England’s current policy and advocacy work on behalf of working-age adults.
• Providing a strategic platform for sector leaders to influence government decisions.
• Enhancing the representation of working-age adults in broader social care policy discussions.
• Aligning with Care England’s wider policy agenda to drive lasting sector reform.
Professor Martin Green OBE, Chief Executive of Care England, commented:

working-age adults and the providers that support them. Through evidence-based advocacy and direct engagement with decision-makers, it will translate discussion into tangible action, ensuring that this vital area of social care remains a national priority.
Tim Davies, Group Chief Executive Officer of Ivolve Care & Support, and newly elected Chair of the Care England Working Age Adult Policy Board, commented:
“I am very pleased to have been elected as Chairman of the Working Age Adult Policy Board. I see this role as a tremendous opportunity to champion our sector’s unique challenges and to drive real, meaningful policy change for working-age adults. By harnessing the collective expertise and passion of our members, we will ensure that our voices are integrated into the broader Care England agenda.”
As the board begins its work, its members - leaders from across the sector - share their thoughts on joining and the impact they hope to achieve:
Peter Kinsey, Chair of Iris Care Group, commented:
“I fully support Care England’s establishment of the Working Age Adult Policy Board which will engage Chief Executives from across the sector in driving much needed policy development and improvement.”
Andrea Kinkade, Chief Executive of Lifeways, commented:
“The creation of the Working Age Adult Policy Board is a landmark moment in ensuring that the needs of working-age adults are fully recognised and addressed within social care policy. This dedicated board will provide a strong, united voice for providers and service users, helping to drive forward the reforms needed to improve care and support for this vital part of our society.”
This board will be outcomes-focused, driving measurable improvements in policy and practice to benefit
‘I am delighted to become a member of the new Working Age Adult Policy Board. Care England do so much to represent providers in the adult social care sector, recognition, that providers who support working age adults, face unique and often misunderstood challenges is a testament to the progressive vision of Care England. I hope, together, we can make great strides in championing the needs of adults who deserve to live fulfilling, hopeful and rewarding lives’.
Rebekah Cresswell, Chief Executive of Priory, commented:
“It is a privilege to represent this sector of social care during this critical time to collaborate with likeminded colleagues for solutions to sustain these vital services for people of the UK.”
Residents and staff at White Lodge in Braydon, Swindon celebrated all things Irish for St Patrick’s Day this week. The home was decorated with shamrocks and everyone dressed in green to mark the day.
Held on March 17th, Saint Patrick's Day actually observes the death of St Patrick, the patron saint of Ireland, but the day has come to be a huge celebration of Irish heritage and culture.
Staff and residents at the home marked the day by making shamrock decorations, learning some Irish words and phrases before enjoying a live performance from the amazing ‘Farrell School of Irish Dance’. Head

chef, Richard prepared a fantastic buffet all washed down with Guinness or an Irish whiskey.
General Manager, Ramona Gherendi said: “Our residents have all had a brilliant day today, everyone has enjoyed the festivities – I think we all agree St Patrick’s Day is the best of all the saints’ days! We had a fantastic time listening to Irish music and watching Irish dancing, we sampled some lovely Irish whiskeys too.”

Research led by Lancaster University has revealed that the exceptional circumstances early in the COVID-19 pandemic led to distressing experiences of death and dying in care homes.
Not only did care homes suffer significantly high death rates amongst residents , but this was compounded by the impact of social distancing restrictions on family visiting and external support from palliative care teams for some care home residents dying in the early months of the pandemic.
The study was led by Lancaster Professor Nancy Preston of the International Observatory on End-of-Life Care with colleagues from Newcastle University and the University of Sheffield.
The research explored the impact on care homes of the early waves of the pandemic between Autumn 2020 and Summer 2021. Interviews were conducted with 16 UK care home staff , three residents , five family members and health service staff working with ten care homes , exploring their experiences of death and dying.

Experiences of death and dying in care homes were particularly distressing for staff and families at this time for a number of reasons.
The findings suggest that care home staff found the prospect of preparing for, and managing a large number of deaths particularly difficult, with one care home manager telling researchers that “Just before lockdown we had a nurse came to the home and said to us, ‘Right you need to be prepared to hold bodies in the care home. Do you have any cold bedrooms where you can hold bodies?’ … and I think that kind of hit us.”
“I Never
I’d
Care home staff also found it very distressing enforcing strict social distancing restrictions on family visits when a care home resident was dying, which often brought them into conflict with their personal and professional instincts for supporting residents and families at these times.
One care home worker said: “It’s just an awful position to be in because who are we to say they can’t say their goodbyes and for how long. That’s the bit that I find difficult.”
Social distancing regulations were clearly also very distressing for families. As well as time restrictions on visits, they also had to choose a single family member to visit, which was difficult for all involved, and could cause family conflict. The findings suggest that the impact of these factors continued to affect families some months after their bereavement, with one telling researchers: “To end his life without having anyone there with him that he knows. That is just a terrible way to go and I don’t think we’ll ever forgive that really.”
Staff also found resident deaths extremely distressing, particularly witnessing the rapid decline of residents whom they had often known and worked with for months or years. They reported not being able to offer the type of end-of-life care that they would wish to, and some felt they had limited external support in managing end-of-life care.
Professor Nancy Preston said: “We don’t yet know the long-term impact of this distress for care home staff and families, but planning for future crises should have clear policies for end-of-life care, including prioritising family visiting and ensuring consistent access to external support services including specialist palliative care.”
A lifetime of memories, a dream she thought was lost, and a journey that brought it all back.
Droitwich Mews Care Home has made a resident’s deeply personal wish come true as part of its new Wishing Tree initiative.
Each month, the Avery Healthcare-owned care home in Droitwich grants a wish for one of its residents, helping them reconnect with cherished moments from their past or experience something they never thought possible.
The Wishing Tree is more than just an idea, it is a promise. Residents write their wishes on paper ‘leaves’, which are then hung on the tree, each one filled with hopes, dreams, and treasured memories.
Every month, a wish is chosen and brought to life by their care home’s dedicated team, creating magical moments that remind residents they are valued and celebrated.
For Christine Smith, 84, who has lived at Droitwich Mews Care Home since June 2024, that moment came last week.
She had always dreamed of returning to RAF Cosford, where she once worked, and visiting the village where she grew up in Shifnal and Albrighton. Time had passed, places had changed, and she never thought she would see them again, but as the minibus wove through winding country lanes, Christine’s face lit up with recognition.
She pointed out places she had not seen in decades, such as the airfield where she worked, the pub where she celebrated her wedding, and the church

where she stood hand-in-hand with Bryan, her husband, in 1960.
Arriving at RAF Cosford, Christine and her friends gazed in wonder at the towering aircraft. The same planes she had once known up close still stood strong.
Nostalgia filled the air as residents tried on RAF uniforms, with one resident joking, “It suits you!”
But the most emotional moment was yet to come. After lunch, the driver took a detour and the minibus pulled up outside the church where Christine had exchanged her vows many years before.
She clutched her hands to her chest, her eyes filling with tears. “I never thought I’d see this again,” she whispered.
An unexpected turn in the journey led the group to a small cottage with a familiar gate. Christine immediately recognised it as her childhood home. Overcome with emotion, she reminisced about her early years, running through fields, climbing old hangars with friends, and dancing to music on a transistor radio.
Christine returned to Droitwich Mews Care Home overcome with joy, still talking about her journey the next morning.
“I never thought I would ever see these places again, the Wishing Tree has definitely made my wishes come true. Thank you so much,” said Christine.
Deputy Manager at Droitwich Mews Care Home said, “An emotional day for everyone, it was just such an honour to be a part of making her wish come true.
A real pleasure to spend this quality time with Christine”.
Ida Mooney, a resident at The Oaks care home in Newtown, Powys, has celebrated her incredible 105th birthday, surrounded by her family, friends, and the care home staff who have grown so fond of her. Born in St Annes, Ida has lived a remarkable life filled with strength, resilience, and love.
During the Second World War, Ida contributed to the war effort by working on Wellington bombers at Blackpool Airport. She cycled to work across fields every day and even recalled being knocked off her bike by a nearby bomb explosion when returning planes dropped unused bombs in the fields.
After the war, Ida became a skilled carpet fitter, sewing 32-inch carpets for large hotels in Blackpool. She eventually set up her own business, working from a rented garage, and became well-known for her work. It was during this time that she met her best friend, Betty, who became a beloved figure in the family until her passing in 2008.

Ida’s independent spirit shone throughout her life. She passed her driving test at the age of 55 and took up swimming lessons in her 60s. She continued to attend keep-fit classes
well into her 80s. Ida also worked in her son’s shoe repair shop, glueing shoes and helping with the business well into her later years.
Family was always at the heart of Ida’s life. She has a son Raymond, known as Ray, and three grandchildren — Karen, Nina, and Nicola — who have fond memories of trips with their grandma and Betty to the Isle of Man, Chester Zoo, and Southport. Despite her advancing years, Ida remains close to Ray, who retired and moved to Wales to be closer to his daughters. In March 2024, just before her 104th birthday, the family successfully arranged for Ida to move to The Oaks so they could all be near each other once again.
On her special day, Ida was surrounded by love and laughter as she opened her birthday cards, including one from the King. When asked how old she was, Ida cheekily replied, "21!" to everyone's amusement. Jen Roberts, Home Manager at The Oaks, said: "It has been an absolute pleasure to care for Ida and celebrate such a milestone with her. She is an incredible lady, full of warmth and humour, and it’s clear how much she means to her family. We are honoured to have her as part of our community."

There is a growing mental health crisis in Scotland’s unpaid carer population – this is the message from Carers Scotland in ‘State of Caring in Scotland 2024: Health and social care support for unpaid carers’.
This new research, based on a survey of over 1,700 unpaid carers in Scotland, saw a 29% increase in the last 12 months of the number of unpaid carers who reported their mental health as “bad or very bad” – 36% of respondents in 2024, compared to 28% in 2023.
This statistic was even more severe when a carer reported struggling financially, with 59% of carers who are struggling to make ends meet saying they had “bad or very bad” mental health. 28% of respondents also rated their physical health as “bad or very bad”, with this number rising to 49% among carers struggling to make ends meet.

80% of unpaid carers from the research stated that the main challenge they will face over the next year is the impact of caring on their physical and/or mental health.
These new findings show that unpaid carers are not receiving the support they need to maintain their health and wellbeing whilst managing their caring responsibilities. More support with health and wellbeing was the number one need cited by unpaid carers in the research, with long waiting times for appointments, inflexible GP appointment systems, and insufficient replacement care all highlighted as barriers to support.
Another challenge is the inability of many unpaid carers to take a physical and mental break from their caring role.
Taking a break from caring is essential for carers to recharge, spend time with family and friends, and
engage with their own hobbies and interests to improve their wellbeing. However, 63% of carers who stated in the research that they felt overwhelmed in their caring role said that this was due to them not having a break from caring.
Richard Meade from Carers Scotland said: .“Unpaid carers in Scotland are in a mental and physical health crisis, which only threatens to get worse without immediate action. Unpaid carers continue to bear the weight of an overstretched health and social care system as they are increasingly expected to fill the growing gaps in service provision without increased support for themselves.”
“Whilst the Scottish Government has focused on reducing NHS waiting lists, improving hospital discharge delays and access to essential health services there still remains an urgent need for investment in social care and support for unpaid carers. Unpaid carers provide the equivalent of £15.9bn in health and social care support and without them the system would collapse, yet they receive a fraction of the support they need.”
“The stalled National Care Service provided hope for many unpaid carers that things could change. However, many feel their needs have been lost to a wider political debate and little has changed to improve their lives.”
“The Scottish Government, the NHS, and local councils must act now to ensure that carers can access the support they need to continue to care without such devastating consequences to their physical and mental health.”
A resident at a Sandbanks care home guided a Premier League footballer to victory in a series of football-themed games.
James Hill, a centre-back for AFC Bournemouth, visited Marjorie House on Crichel Mount Road near Sandbanks to view the facilities and play some seated football and beanbag throwing sessions with the residents.
He particularly struck up a friendship with Pam, a resident of Marjorie House and a keen football fan. Together they teamed up against the other care home residents and staff alongside AFC Bournemouth legend Steve ‘Fletch’ Fletcher. The afternoon was led by Steve Cuss and David Pudney from AFC Bournemouth Community Sports Trust, who host sessions across Care South’s Dorset-based care homes.
James said: “Pam and I had a good partnership going during the games. She was my team captain and she led me through to many victories, which I was very happy about.

“Marjorie House is the best care home I’ve ever seen in terms of how the staff accommodate the residents’ individual needs. It is amazing. It feels like a community with lots of nice communal areas to sit in and the views from the balcony are incredible. It feels like such a friendly environment and so homely. It doesn’t feel like it’s a care home.”
Reflecting on steering her team to success, Pam said: “James was wonderful. The games were such fun
and it was good exercise. The AFC Bournemouth team made it special for us. I have always enjoyed watching football on a Saturday night. I like living at Marjorie House very much.”
Marjorie House is owned and operated by not-for-profit care home and care at home provider, Care South. The visit was arranged as part of Care South’s ongoing partnership with AFC Bournemouth. This enables care home residents, care home clients, and staff to get involved in a range of activities including weekly seated football sessions, meeting players, coffee mornings, and tours of the stadium. Sebastian Wincelewski, Home Manager at Marjorie House, said: “We were thrilled to welcome James Hill to look around our care home and meet our residents. It was wonderful to see Pam and our other residents engaged in the activities with James’s help and guidance. The seated football will now become a regular activity in Marjorie House, as part of Care South’s partnership with AFC Bournemouth, which brings joy, laughter and fun to the home while enabling the residents to stay active.”
The Marjorie House team are celebrating after the home was listed as one of the Top 20 Care Homes in the South West by industry website carehome.co.uk based on reviews from residents, relatives and their loved ones.
People living in a Hereford care home put on their dancing shoes in an activity designed to help those with, or stave off, dementia.
The Brockington House Care Community was the venue for ‘Dance Away Dementia’, an initiative set up by international Latin dance performer and teacher John James.
This involved providing Salsa dance lessons for the ladies and gentlemen who live at the home in Hafod Road.
John, who is also a qualified Psychotherapist, has made a name for himself by delivering the lessons in care homes after setting up his business following the pandemic and on the back of research which shows how dancing can reduce the occurrence of dementia and Alzheimer’s.
John was joined at Brockington House by two members of his team, Stephanie and Mick. The latter is known affectionately as ‘Mick the Mambo’ and despite being in his 70s, he is still ‘busting’ the moves on the dancefloor.
They took residents (and staff) through various Salsa steps and ensured those who have mobility problems didn’t miss out by handing out instruments to play or Strictly Come Dancing-style scoring paddles so they could ‘judge’ the dancers.
John said: “Everyone did really well and it was fantastic to see so many taking people taking part, including staff.

“It’s a fun, unique way to keep fit but with real therapeutic value too.”
John decided to set up Dance Away Dementia after the pandemic forced him out of work, combining his dancing and psychotherapy skills.
He explains: “Dance is seen as viable therapy because it simultaneously combines physical and cognitive stimulation.
“It was only when I started delivering the sessions in the care homes that I started the seeing the results for myself.
“I asked one lady whether she had ever had dance classes and she said no but when we started dancing it was clear by the complex nature of her moves that she had, and this was later confirmed by her daughter. She had forgotten she had once been a dancer due to her now living with dementia but once she got on the floor, she did it naturally without thought.”
Tara Chatterly-Russell, Brockington House Activity Lead, said: “Our ladies and gentlemen don’t need any excuse to get up and dance, sit and tap their feet or clap their hands, so this was the perfect activity for them.
“It was a very stimulating experience for everyone.”
John’s Dance Away Dementia initiative was discovered on an activities website by Brockington House staff member Antonia Allert, who works as a Carer and supports the activities team.

By Ali Powell, CEO and Founder at Commercial

The latest UK Care Homes Trading Performance Review 2024 shows occupancy levels rising to 88.3%, a positive sign of market recovery. However, while this progress is encouraging, it reveals significant untapped potential in how care homes attract and convert prospective residents.
Presenting care homes effectively is not just about showcasing services—it's about creating emotional connection and trust. Families are making difficult decisions in emotionally charged situations, which requires a sophisticated approach to relationshipbuilding and conversion. Care homes are offering something no one truly wants to need, making the challenge even greater.
To truly drive sustainable occupancy growth, care homes must focus on transforming the customer journey—from raising awareness to handling enquiries and guiding families through to admissions. Many providers are still missing key opportunities. Too often, care homes fall short in delivering the basics well, leading to lost enquiries and missed revenue potential.
CRITICAL AREAS NEEDING IMPROVEMENT INCLUDE:
Generating Quality Leads: It's essential to attract the right audience from the outset through targeted campaigns, high-value content, and strategic outreach across multiple channels, including community outreach, digital marketing, partnerships, referral networks, local events, print ads, and door drops.
• Empathetic First Contact: Enquiries must be handled with care, expertise, and emotional sensitivity, recognising the difficult decisions families face.
Personalised Tours: Showrounds should go beyond listing services, highlighting quality of life benefits such as personalised care plans, engaging activities, and the warmth of community life.
Clear Value Communication: Families need transparent, outcome-driven explanations of the value of care— focusing on dignity, well-being, and peace of mind, not just amenities.
• Consistent Post-Visit Engagement: Many care homes neglect follow-up strategies after visits, losing potential residents who may need further reassurance or time to decide.
TRACKING THE RIGHT METRICS:
To ensure the customer journey is effective, care homes should track key performance metrics, including: Monthly Lead Generation: Number of leads that meet predefined criteria indicating genuine interest or fit.
Monthly Visits: The number of on-site or virtual tours conducted within the month.
• Monthly Admissions: The total number of new residents admitted each month.
Lead Source Performance: Breakdown of leads by marketing channel (e.g., online ads, social media, referrals, events) to identify the most effective sources.
Average Admission Cycle Length: The average time from initial lead generation to a confirmed admission.
Monthly Marketing Spend: Total amount spent on marketing each month.
Website Traffic: Total visitors to the website and engagement rates for the month.
Social Media: Total followers and engagement on platforms like Facebook, LinkedIn, and Instagram.
THE OPPORTUNITY:
Investing in marketing and relationship-building efforts is not a luxury—it's essential. The cost per acquisition is often minimal compared to the hundreds of thousands in lifetime revenue generated from new residents. By focusing on consistency and excellence throughout the entire customer journey, care homes can significantly impact both occupancy rates and short- and long-term growth. The data is clear: doing the fundamentals well is not just good practice—it’s essential for both immediate results and lasting success. It’s time for care homes to move beyond filling rooms and start focusing on creating an inspiring customer journey that builds confidence, trust, and emotional connection with families.
If you need an expert in this area, contact Ali at Commercial Acceleration—specialists in strategy and implementation for transformational and turnaround results.
ali@comaccel.co.uk | comaccel.co.uk


Rad Tingle, kitchen manager at Ribble Court Care Home in Much Hoole, Preston, part of Sandstone Care, is set to take on a daring abseil challenge down Peel Tower in Bolton to raise funds for the Renal Unit at Lancashire Teaching Hospitals NHS Foundation Trust.
A committed fundraiser, Rad has supported several charitable causes over the past few years and has previously raised money for the hospital, where he was once a patient.
His dedication to giving back stems from personal experience—he suffers from von Hippel-Lindau (VHL) syndrome, a rare inherited genetic disorder that causes tumours and cysts to grow in various parts of the body, including the brain, spinal cord, eyes, inner ear, pancreas, and kidneys.
In 2020, Rad, who is blind in his left eye and deaf in his left ear, underwent a life-changing kidney transplant in Manchester after spending two years as a dialysis patient at Lancashire Teaching Hospitals.
Having seen first-hand the positive impact of charity funding on patient care and wellbeing, he has since embarked on a series of adrenaline-fuelled fundraising events, including skydives and zipline challenges. His dedication was recognised when he was shortlisted for Charity Fundraiser of the Year at the

The staff and residents at Elm Bank care home in Kettering welcomed Jason from Falconry UK to their home for an afternoon learning all about the magnificent birds of prey.
Elm Bank care home residents and staff wanted to have something unique, Jason from falconry UK certainly provided a unique experience for all with his extensive range of Birds of Prey including… Vultures, Eagles, Falcons, Hawks and Owls. The residents were absolutely blown away with the afternoon, not only did Jason provide an interesting educational talk around all the birds, it was an extremely interactive session for all. The residents were captivated with all the facts and for many it was the first time being up close to a bird and having the chance to actually hold a bird was simply spectacular.
Best of Lancashire Awards 2023.
Rad said: “The Renal Unit played a vital role in my journey, and I want to give back in any way I can. Charity funding truly makes a difference to the lives of patients, and I hope my efforts will help support those going through similar experiences. I’ve tackled heights before, but this abseil will be a new challenge—one I’m ready to take on!
“Everyone at Ribble Court, and Sandstone Care has been very supportive and I hope to make them proud as well as raise lots of money for the hospital.”
Sandstone Care, which operates Ribble Court Care Home, is proud to support Rad in his fundraising efforts.
Steven Hamblett, operations director at Sandstone Care said: “Rad is an inspiration to everyone at Ribble Court and beyond. His resilience and passion for helping others are remarkable, and we are incredibly proud to support his latest fundraising challenge. We encourage everyone to get behind him and donate to this worthy cause.”

Rad’s abseil is set to take place at the end of March, with funds raised going directly to support the work of the Renal Unit at Lancashire Teaching Hospitals NHS Foundation Trust.
Tina, Activities Co-ordinator at Elm Bank care home, commented: “It is very important here at the home for all our residents to experience meaningful activities and to be able to offer these experiences to our residents is vital allowing us to enrich their lives. Jason certainly had everyone engaged, we all learnt so much about the amazing birds, and he provided a fantastic hands on experience for all the residents to actually get up close and handle the magnificent birds. The residents wish to have Jason back in the summer time, which we will do so for an outdoor event in the homes beautiful enclosed grounds.”
Our varied life enrichment programme keeps residents active, and provides a daily choice of engaging physical, mental and spiritual activities tailored to residents’ interests and abilities.


Adopt A Grandparent (AAG) is proud to announce new partnerships with both Care England and the National Activity Providers Association (NAPA) – two of the most influential organisations in the UK care sector. These collaborations mark a significant step forward in expanding intergenerational connections across care homes nationwide, ensuring more residents benefit from companionship, conversation, and meaningful social engagement.
With so many older adults in the UK experiencing chronic loneliness, AAG’s work is more vital than ever. By partnering with these leading organisations, the charity aims to increase access to its volunteer programme, offering care homes a fully supported way to enrich the lives of their residents.
A MOVEMENT BACKED BY INDUSTRY LEADERS

The National Activity Providers Association (NAPA) is the UK’s leading activity and engagement charity, working to improve quality of life through meaningful activities in care settings. Through this partnership, NAPA will support care homes in integrating AAG into their activity programmes, helping residents build relationships that enhance their mental and emotional wellbeing. Meanwhile, Care England – the representative body for care providers across England – advocates for innovative solutions that improve care services and resident experiences. By becoming a Supporter Member of Care England, AAG is now positioned as a key resource for care providers looking to tackle loneliness and prioritise social connection.
THE AAG DIFFERENCE: A SIMPLE, EFFECTIVE SOLUTION FOR CARE HOMES
AAG provides care homes with an easy-to-implement, fully safeguarded programme that manually matches residents with volunteers based on shared interests. These friendships are nurtured through a
secure AI-powered platform, ensuring calls are safe, engaging, and beneficial to residents’ wellbeing.
CARE HOMES THAT SIGN UP GAIN ACCESS TO:
· A structured, fully managed initiative that seamlessly integrates into existing activities.
· One-on-one video calls and ongoing engagement to create lasting social bonds.
· A proven approach to reducing loneliness, improving cognitive health, and increasing resident happiness.
· Endorsement from leading care sector organisations, demonstrating a commitment to innovation and resident wellbeing.
Shaleeza Hasham, Founder and CEO of Adopt A Grandparent, said:
“We are thrilled to be working with both Care England and NAPA – two organisations that share our commitment to improving quality of life for older adults. Loneliness should never be a normal part of ageing, and by joining forces with these sector leaders, we are making it easier than ever for care homes to introduce our programme and create meaningful connections for their residents. Together, we can ensure that no older person feels forgotten.”
AAG’s partnerships with NAPA and Care England mark a turning point in how care homes approach social engagement, bringing together industry expertise, volunteer support, and cutting-edge technology to tackle one of the most pressing public health challenges of our time.
HOW CARE HOMES CAN GET INVOLVED
Care homes across the UK are invited to sign up and join this movement to transform resident wellbeing. By partnering with AAG, care providers can offer their residents companionship, conversation, and a renewed sense of connection to the world around them.
Residents at Adelaide Care Home were on their toes with excitement as Baby Ballet Dartford pirouetted into the home for a memorable intergenerational dance session.
The young performers arrived at the Avery Healthcare-owned care home in Bexleyheath in their dazzling tutus, leaping straight into action with twirls, ribbon dancing, and musical fun.
The residents were enchanted, many stepping in time with the movements, guided by the wonderful Miss Jessie.
The atmosphere was nothing short of a showstopper as families, staff, and residents swayed along, proving that the joy of dance knows no age limit.
Baby Ballet is a much-loved group where babies and toddlers discover the magic of ballet through music, movement, and playful props.

When invited to bring their star-studded routine to Adelaide Care Home, they delivered a performance that had everyone tapping their toes and beaming with delight.
Karla, a parent of one of the Baby Ballet stars, described the event as a blessing, saying, “Seeing the residents’ happiness was truly heartwarming.”
Marjorie Carpenter, a resident, said, “It was so lovely to see them in their tutus and watch them dance.”
Doreen Armstrong, another resident, added, “They were brilliant. It was wonderful to be part of it.”
Miss Jessie, the ballet instructor, reflected on the event, saying, “It was a joy to bring Baby Ballet to Adelaide Care Home and see the residents light up as they danced and interacted with the children.”
The foundation of exceptional care home service lies in collaboration, efficiency, and reliability. For over a decade, Care Quality Pharmacy (CQP) has stood as a trusted partner for care homes across England, Scotland, and Wales. With a specialised approach to care home pharmacy services, CQP ensures residents receive timely and accurate medication, allowing carers to focus on what truly matters: quality time with their residents.
One of the most significant challenges for care homes is navigating missing or out-of-stock medications. CQP’s proactive system addresses this with precision. Their team checks prescriptions, liaises with GP services on behalf of the care home, and resolves discrepancies swiftly. Additionally, CQP’s access to national wholesale suppliers and long-standing relationships ensures a robust strategy for managing short supply issues, keeping residents’ needs a top priority.
Medication errors, often a stress point for staff, are almost eliminated thanks to CQP’s cutting-edge systems. Medications are picked using robotic technology, followed by a meticulous two-stage accuracy check by a pharmacist. This stringent robotic process has achieved an impressive error rate of less than two parts per million. Furthermore, integrations with market leading eMAR providers and coloured paper MAR entries are handled by CQP, reducing the administrative burden for care home teams.

Timely delivery is another hallmark of CQP’s service. Monthly deliveries are scheduled up to six days in advance, and their teams ensure precision and dependability making the booking-in process hassle free. For urgent needs, a 4pm interim cut-off guarantees next-day delivery, including Saturdays. CQP’s commitment to care extends beyond medication. Their open communication lines, available seven
days a week, foster seamless interactions. Moreover, their Quality Assurance Team conducts annual face-to-face compliance audits, enhancing regulatory compliance and resident satisfaction. Added services, such as guidance on covert medicine administration and homely remedies advice, showcase their dedication to meeting every need.
Leading national care home partners trust CQP completely to manage pharmacy services across their entire estates. This unwavering confidence is a testament to the expertise, efficiency, and reliability that CQP brings to the table. Care homes also benefit from no-cost residential returns collection and free online medication training sessions. CQP supports staff development, ensuring a high standard of care using the CQP systems and processes.
By embracing the ethos of collaborative working, Care Quality Pharmacy sets the benchmark for care home pharmacy services. Their efficiency, responsiveness, and focus on compliance empower care homes to achieve the best outcomes for their residents. In an ever-demanding sector, CQP remains a steadfast partner, proving that the right support makes all the difference.
NHS prescription item dispensing data from October 2024 shows CQP to be the
National care home only pharmacy operating since 2011, based in the Midlands – serving England, Scotland and Wales.
Missing medication? Our team checks all your prescriptions for you and informs you of missing medication - huge time and cost saving to the home, freeing up your quality time with your residents.
Out of stock medication? We manage the entire short supply and out-of-stock medication process. Medication errors? Our resident order is picked by robots, then a 2 – stage independent accuracy check by pharmacists ensures you have the right medicine, on time, every time.
eMAR Integrations - Our systems work alongside all major eMAR providers
Are your deliveries on time? Our monthly deliveries are up to 6 days in advance, giving you plenty of time to book in medication. Saturday deliveries included.
Open Communication - One direct communications team, answering calls & responding to emails giving you one SLA for all of your homes.
Compliance - Quality Assurance Team – guaranteed face-to-face annual compliance audits. Consistency of service and delivery with audit trail.
We are Specialists in care home only dispensingDouble labels, Covert administration and Homely remedies advice.
Free Residential Returns Residential home’s returns are collected – no cost implications to you.
Free Medication Training – Both online and face-toface options available.
Become part of the care home pharmacy delivering excellence in medication management across the country.
References available on request.
To organise an introductory meeting please contact National Partnerships Director, Patrick Bell: Email: patrick@cqpharmacy.co.uk
As 2025 gets into full swing, the social care sector finds itself grappling with the lingering challenges of a difficult 2024.
In response, Log my Care, the intuitive care management platform, has launched Shaping Social Care 2025, a new e-book full of expert perspectives and strategies to support the sector. This article by Mark Topps is an extract from the report, which features six additional chapters of predictions and advice from leading experts covering topics across legal, CQC, HR, complex care, and technology.
When discussing efficiency, we often focus on time savings, which shifts our attention from evaluating existing processes. Additionally, we must consider our teams and those we support, balancing efficiency with quality. Here are practical strategies to achieve both.
A large part of social care involves administration, making it an ideal area for streamlining. However, social care often lags in adopting digital tools and AI. While technology isn’t a cure-all, it’s an accessible way to improve workflows without hefty costs.
Many providers already use Digital Care Planning systems, but are these systems being fully utilised? Often, key features are disabled during setup, integrations face challenges, and tools go unused due to limited training. Revisiting these systems and addressing gaps can unlock untapped efficiencies. Proper training can save time, reduce manual work, and allow teams to focus on high-quality care. Here are some strategies and tools to enhance efficiency:
● Digital Care Planning and EHR Integration: Integrating Digital Care Planning systems with electronic health records (EHRs) ensures quick access to essential information, improves accuracy, and reduces time spent on communication with healthcare professionals.
● Digital Rostering: Tools like Log my Care’s Rostering add-on simplify rota creation, optimise staff deployment, and align carers with service users’ needs, improving both efficiency and care quality.
● Process Mapping: Visualise workflows to identify inefficiencies and bot-
tlenecks. Regular updates ensure relevance and provide clarity for teams.
● Simplify Workflows: Eliminate redundant tasks and combine actions where possible. Streamlined workflows save time and reduce errors. These strategies help create efficient systems, allowing more focus on delivering quality care.
Time management is crucial for productivity and quality care. Investing in training and development can significantly enhance efficiency. Consider the following:
● Time Management Training: Tools like the Eisenhower Matrix help staff prioritise tasks based on urgency and importance, ensuring critical items are addressed promptly.
● Goal-Setting and Task Management: Training staff to set realistic goals, break projects into manageable steps, and establish achievable deadlines fosters accomplishment and reduces burnout.
● Continuous Learning: Encourage staff to stay updated on best practices and emerging technologies. This keeps teams engaged, skilled, and ready for challenges.
● System Reviews and Innovations: Regularly evaluate current systems and explore new technologies to identify tools that enhance both efficiency and care quality.
Investing in these areas builds a proactive, capable team ready to meet the demands of modern social care.
While most claim to deliver person-centred care, it’s worth reflecting on whether unique needs are genuinely met. Consider the following:
● Reflect on Care Delivery: Imagine care without constraints like cost or staffing—what would you change? Use these insights to identify actionable steps, such as adopting new technology, reviewing care plans more frequently, or increasing staffing levels.
● Feedback Utilisation: Evaluate how feedback is gathered, analysed,
and acted upon. Effective systems not only highlight improvements but also show service users and staff their input is valued.
● Rethink Staffing Ratios and Rostering: Analyse staffing data to identify needs and explore different shift patterns or task-sharing opportunities. Involving staff in this process can lead to innovative solutions that enhance care and efficiency.
By reflecting, gathering feedback, and actively involving your team, you build a foundation for continuous improvement.
TEAM COLLABORATION AND COMMUNICATION
Streamlining communication is critical for operational efficiency:
● Consolidate Communication Tools: Using multiple systems can cause confusion and duplication. Centralising tools enhances coordination and reduces administrative burdens.
● Optimise Meetings: Regular, focused meetings with clear objectives are more effective than broad, infrequent gatherings. Purpose-specific meetings foster engagement and clarity.
● Collaborative Culture: Streamlined communication and purposeful meetings build trust and morale, empowering teams to work together effectively. This enhances processes and ensures exceptional personcentred care.
Efficiency in social care goes beyond saving time—it’s about maximising resources, eliminating unnecessary tasks, and streamlining processes.
The ultimate goal is improving outcomes for the people we support. By fostering collaboration, leveraging technology, and focusing on quality, we can create a system that balances efficiency and care excellence.
Scan the QR code to read the full ebook for free

Staff and residents at Melbourn Springs Care Home in Melbourn were treated to a fun-packed hour in the company of choir leader and vocal coach to the stars, Dan Cooper, who taught them to sing two feel-good songs to put a spring in their step: ‘Dancing Queen’ by Abba and ‘I wanna hold your hand’ by The Beatles.
In partnership with Biiah, Dan delivers regular singing events through their virtual platform which encourages people to sing for their wellbeing. A professional choir leader and vocal coach with over 10 years’ experience, Dan runs a successful choir; Love Soul Choir, and is codirector of a children’s group; Sound Pop Academy.
His choir has performed with Take That. He’s also worked on TV shows as a vocal coach including BBC’s ‘Little Mix The Search’ and is passionate about the positive impact that singing in a group has on wellbeing. Dan truly believes in the power of singing and wants more people to experience the joy it can bring.

Dan comments: “I have the best job in the world. I am never happier than when I am teaching people to sing and seeing how happy it makes them. It was an absolute privilege to spend the afternoon with the Barchester residents and teach them these fantastic songs.”
Bex Vernon, Resident Experience Coordinator for Barchester Healthcare, adds: “We are excited to work with super-talented people like Dan to bring a wide range of different experiences into our homes for all to enjoy, it was wonderful to see the joy on all of our residents’ faces as Dan taught them how to sing these feel-good songs.
General Manager, Magda Ulian, says: “Our residents absolutely loved their springtime singing session with Dan, it was so uplifting. We all love a good singalong and it was great to get Dan’s hints and tips on how we can improve our technique. We loved his energy and positivity!”

Residents, fondly referred to as family members, from Catherine House and Frome Nursing Home recently enjoyed a trip to Avon Valley Steam Railway, a day filled with conversation and connection. More than just an outing, the experience reflected the importance of staying engaged with the wider community, maintaining independence, and enjoying a day out as you would if living in your own home. With tea, pasties, and fruit cake shared among friends, the journey felt relaxed, and mirrored the routines and comforts of everyday life.
The trip began with tea in the buffet carriage, setting the scene for a comfortable and engaging experience. As the train set off, family members shared their thoughts on the journey. Michael summed up his experience, saying, “This is very
enjoyable – and so was the pasty!” Janet reflected, “I like being on an old train; I can’t remember the last time I was on one.” Ruby took pleasure in waving at passers-by from the window, while George described the outing as “very interesting.”
Before heading home, everyone had another hot drink and a slice of fruit cake, rounding off the trip with more conversation and shared moments. Michael was already looking ahead to future outings, asking, “When is the next one?”—a sign of how much these experiences mean to family members.
A big thank you goes to the Avon Valley Railway team for their warm welcome and support, and to Sharon the home’s activities coordinator for driving the minibus and making the journey possible.


17 – 23 March is Nutrition and Hydration Week, focusing on the value of food and drink in maintaining health and wellbeing in health and social care.
Being a patient or a resident in a health or social care setting can often limit a person’s ability and autonomy to drink and eat what they want as and when they want. Under-hydration and malnutrition contribute to delirium, falls, constipation, and urinary and respiratory tract infections, often leading to admissionto hospital. Proper nutrition and hydration are key for supporting independence and quality of life for older people in long term care settings.
The Richard Wells Research Centre at the University of West London (UWL) has led on two National Institute for Health and Care Research (NIHR) funded projects that focus on ensuring that older people in care homes are helped to eat and drink.

The I-Hydrate Project found that care home residents do not always receive or consume enough fluids to meet normal daily requirements. In collaboration with two care homes, researchers demonstrated that giving residents a larger choice of drinks and better equipment can increase fluid intake and that introducing protected drinks times and giving staff specific hydration tasks can help improve resident hydration. The team has produced a suite of resources that show that making just a few small changes can make all the difference to the amount of fluids residents consume. They are free to download and watch here The IHydrate Project.
Urinary tract infection (UTI) is common in older people living in care homes and is often difficult to recognise because signs and symptoms, such as changes in behaviour, may look like other conditions such as dementia. This can lead to antibiotics being prescribed unnecessarily, which lessens their effectiveness. It can also result in antibiotics not being given when needed.
The StOP UTI Project provides practical examples and recommendations relevant to care home staff, care home managers, researchers, educators, carers and relatives to improve the recognition and prevention of urinary tract infection in older people’s long-term care.
The project reviewed the evidence for strategies to prevent and recognise UTI. It used different types of evidence from research, improvement projects and information gathered from stakeholders to help understand how interventions to prevent and recognise UTI can be delivered effectively by staff working in care homes.
They found that for hydration to be recognised as a care priority for all residents, care routines need to include sufficient opportunities for drinking and enable care staff to devote the necessary time and resources to support residents to consume enough fluid every day.
The project identified the importance of knowing how much fluid a resident has consumed to ensure that poor fluid intake does not go unnoticed and can be addressed by care staff. A Policy Brief and Project Summary of the research findings are available to download.
Staff and residents at Hickathrift House Care Home in Marshland St James, Wisbech, welcomed James Bowman, creator of the Fens Flag for an educational talk on the history of the flag and its traction to becoming the official flag of the Fens.
Residents and staff all gathered for James to share his knowledge on the Fens and his passion for the Fen’s Flag. The flag was first designed in 2016, with the colours royal blue, to represent the waterways, custard yellow to represent agricultural prosperity and the Fen tiger. The campaign to make the flag official began in 2018 and is supported by many local businesses who display the flag proudly. Residents were fascinated to learn more about their local area as well as the flag, with many asking questions as to where the flags are

displayed and how to make it the official flag of the Fens.
General Manager of the home, Paula Melerski said: “This has been very educational for all of us. Both residents and staff have thoroughly enjoyed learning more about the Fens and the importance of the flag. At our monthly speaker events we welcome any opportunities to learn about the area and the passions of locals”.
Barrie, Resident Ambassador of Hickathrift said, “I have always been curious about the local area, not growing up around here I feel I missed out on my education of the Fens. I am so glad I have been able to learn more about the place I have been able to call my home for the last few years and feel very proud to support James and the flag”.

The care sector is no stranger to challenges. With an aging population, increasing demand for services, and financial pressures, care providers are constantly battling to stay ahead. Add to this the need for positive public perception in a media environment often fixated on crises, and it’s clear that strong communication isn’t just a nice-tohave—it’s essential. That’s where DAPS Agency Ltd comes in, a specialist communications agency helping care organizations navigate these turbulent waters and emerge stronger.
UNDERSTANDING THE CARE SECTOR’S UNIQUE CHALLENGES
DAPS Agency is no ordinary PR outfit. Founded by seasoned communications professionals Anneli Lort and Firgas Esack, the agency has carved out a niche for itself by understanding the unique hurdles faced by care providers, from technology innovators to care home operators.
“The care sector is about more than delivering services; it’s about creating meaningful experiences for residents, building trust with families, and supporting staff,” says Anneli Lort, co-founder of DAPS. “But these stories often get buried under the day-to-day pressures providers face.”
One of the biggest hurdles for care organizations, whether they’re home groups or care technology suppliers, is visibility. With so many competing voices in the sector, standing out is no easy feat. Providers need to balance the operational challenges of driving occupancy and adapting to new technologies while maintaining strong relationships with stakeholders. According to Firgas Esack, this is where targeted and tailored communications can make all the difference.
“Visibility is critical,” Esack explains. “We help care providers showcase their unique strengths, whether it’s innovative resident care programs or cutting-edge technology that’s changing how the sector operates. Our aim is to make sure their voices are heard where it matters most.”
PUTTING CARE PROVIDERS IN THE SPOTLIGHT
DAPS excels at elevating their clients’ profiles by crafting narratives that resonate. Whether it’s securing positive press coverage or positioning an organization as a thought leader through white papers and industry commentary, the agency’s strategies are rooted in authenticity.
“Care home groups face enormous pressures to attract and retain residents while maintaining financial sustainability,” says Esack. “We’ve worked with clients to highlight innovative approaches they’ve taken to deliver high-quality care on a budget, securing media coverage that positions them as forward-thinking leaders.”
The team’s expertise isn’t limited to traditional care providers. In an industry increasingly driven by technology, DAPS has also helped care tech companies gain recognition for their solutions. From illustrating how a software tool is transforming care home operations to showcasing new assistive technologies that improve residents’ quality of life, DAPS knows how to translate technical innovation into stories that matter. TACKLING THE TOUGHEST ISSUES
The care sector is not without its share of crises—media scrutiny, financial difficulties, and regulatory challenges can arise at any moment. This is where DAPS’ experience in crisis communications comes into play. Having run global press offices and handled high-stakes issues for clients, the agency offers a steady hand when it’s needed most.
“When a crisis hits, it’s easy to feel overwhelmed,” says Lort. “Our role is to step in, take control, and guide our clients through the storm while safeguarding their reputation.”
Their work doesn’t just stop at damage control. Proactive thought leadership—opinion pieces, keynote speeches, and lobbying efforts—ensures that their clients are shaping the narrative, rather than simply reacting to it. By working closely with stakeholders, DAPS ensures that their clients’ voices are heard at both local and national levels.
What sets DAPS apart is its unashamedly remote working model. Lort and Esack believe this approach allows them to deliver exceptional results without the traditional overheads of a bricks-and-mortar agency.
“Every penny our clients spend goes toward achieving results,” says Lort. “And because our team is made up of senior professionals, clients know they’re always working with experts who understand the complexities of their sector.”
This lean, results-driven ethos has helped DAPS build a reputation as a trusted partner for care organizations of all sizes. Whether working with a large care home group or a niche technology provider, the agency’s approach is the same: tailored, proactive, and relentlessly focused on outcomes.
One of the most rewarding aspects of DAPS’ work is celebrating the positive stories that come out of the care sector. In an industry that’s often under scrutiny, shining a light on success stories is vital.
“Whether it’s a care home running an innovative intergenerational program or a technology provider making a measurable difference in residents’ lives, we make sure these stories get the attention they deserve,” says Esack. “We want to celebrate the people and innovations driving the sector forward.”
This focus on positivity isn’t just good PR; it’s also good for morale. Recognizing and sharing achievements boosts confidence within organizations and strengthens their reputation with external stakeholders.
As the care sector continues to evolve, the need for strategic, impactful communications will only grow. For care providers looking to amplify their voice, tackle challenges head-on, and secure their place as leaders in the sector, DAPS Agency offers the expertise and passion to make it happen.
“We’re here to tell the stories that matter,” says Lort. “The care sector does incredible work, often under tough circumstances, and it’s our job to make sure that work is seen, understood, and celebrated.”
In a sector where the stakes couldn’t be higher, DAPS is proving that the right communications partner can be transformative. Whether navigating a crisis, celebrating a success, or shaping the future of care, this dynamic agency is helping its clients rise to the occasion.
To book a free, no-obligation one hour consultation with DAPS to discuss your communications challenges and needs, go to daps.life/DAPS60 www.dapsagency.com
Scottish Liberal Democrat leader Alex Cole-Hamilton MSP has called on the SNP Government to finally invest in care services and staff after a new report found that there are staff vacancies in almost three quarters of care homes and two thirds of care at homes services across Scotland.

The Staff Vacancies in Care Services 2023 report, published by the Care Inspectorate and the Scottish Social Services Council (SSSC), provides data on vacancies reported by care services as of 31 December 2023.
The previous joint report released revealed that vacancies had reached their highest level since the publication of figures began in 2017.
THE REPORT REVEALED THAT:
• 74% of care homes for older people were reporting vacancies.
• 68% of care homes for adults were reporting vacancies.
• 67% of care at home services were reporting vacancies.
Jackie Irvine, Chief Executive of the Care Inspectorate, said: “The report highlights the extent of the current recruitment and retention challenges being faced by the sector at a time when services are experiencing continued pressure.
“We know there are still many parts of the social service sector finding it challenging to fill vacancies, and this has been a persistent issue for several years. We remain grateful for the dedication and commitment of the skilled and qualified workforce
to those experiencing care during these challenging times.”
Maree Allison, Chief Executive of the Scottish Social Services Council, said: “It’s essential we continue to prioritise our work to attract people into careers in social services, providing accessible training, learning and qualifications for people before and after they join the workforce. We need to make sure workers feel valued, respected and supported to continue their social service careers.
“This report is just one aspect of the workforce planning activities undertaken by the Care Inspectorate and the SSSC. Both organisations will continue to work closely with Scottish Government and others to help employers to recruit, retain and develop their staff.”
Mr Cole-Hamilton, pictured left, said: “Care services are stretched to breaking point. Vacancies are rife, meaning more and more demand will simply not be met.”
“The SNP Government wasted four years and £30 million attempting a bureaucratic takeover of social care that was never going to fix core problems. Now they have finally ditched their plans, it’s time to finally invest in the staff and services who need help now.”
“Only Scottish Liberal Democrats have a plan to fix the crisis by introducing a new minimum wage for care workers that is £2 higher. That’s how we can people care at home or in the community, free up space in hospitals and help everyone get seen faster.”












In 2024 the Audley Foundation donated £77,000 for thirty charities, all of which were nominated by supporters. The total was the highest amount raised by the Foundation, which saw £48,000 raised in 2023.
The Foundation was established in 2022 with a clear purpose – to improve the lives of older people, particularly those facing loneliness and hardship. A key component of this year’s fundraising was through the Chatty Bench initiative.
These benches have become welcoming spots near several of Audley Group’s villages, and are designed to encourage conversations and connections between people in the local community. 2024 saw two new benches in Audley Redwood Village and Audley St.Elphin’s Park, with plans for four more to be added in 2025.
John Nettleton, Trustee and Chair of The Audley Foundation commented: “With a lot of effort from property owners in Audley Group villages, the Audley and Mayfield teams and our corporate partners, this year we have successfully grown the Foundation, which importantly has enabled us to both support more charities

and also give each charity more money. From the funds raised in 2024, we have donated over £67,000 to charities nominated by our supporters, and put £10,000 towards our own Chatty Benches initiative.
“I am consistently blown away by the sheer support and effort from everyone involved.
We genuinely couldn’t do this without the support of The Audley Group and I’m very much looking forward to another exciting year ahead. In these challenging times, charities need more help than ever and I’m so proud to be putting the money raised in 2024 and beyond towards the fantastic causes The Audley Foundation supports.”
Next year initiatives and fundraising days including the Foundation’s annual dinner, Foundation month, Partners Day and the very successful ‘Round the Pound’ will be returning, but with more to come and new initiatives across local communities and Audley and Mayfield Villages.
Older autistic people must be involved in decisions about their health and social care services, a new research project from Heriot-Watt Universityin Edinburgh and charity Scottish Autism suggests.
The project, titled “Autism, Ageing and Social Care”, used creative methods to begin a wider conversation about the support that autistic people will need when they get older.
The research team worked with autistic film-makers to create a documentary about the hopes, concerns and needs of autistic people as they get older. Workshops with autistic adults, whose ages range from 45 to 80, and care professionals, led to a series of artworks reflecting on what good support looks like for this population in older age. The project was funded by the Arts and Humanities Research Council (AHRC), which is part of UK Research and Innovation (UKRI) – the UK’s national funding agency for investing in science and research.

Professor Mary Stewart, Director of Social Interaction, Mental Health and Wellbeing at Heriot-Watt University, and member of the University’s Global Research Institute in Health and Care Technologies, is the academic lead for the project. She said: “Using filmmaking and art helped us to ask autistic people who communicate in diverse ways to express what’s important to them and how to plan for ageing and change.
“Everybody finds ageing difficult, but it can be particularly challenging for autistic people to access appropriate health and social care provision.”
Dr Joe Long, Director of Practice and Innovation at Scottish Autism, was a co-researcher on the project. He said: “The children Scottish Autism first supported in the 1960s are now reaching retirement age, so we know there’s a real need plan properly for the support that older autistic people will need. “It’s really important that those future services are shaped by the people who use them, so this project is about starting those conversations and amplifying the voices of older autistic people.”
In the documentary film, autistic adults are interviewed by Iceberg Productions, a group of autistic filmmakers who are supported by Scottish Autism, and The Untold Motion Picture Company, which specialises in filmmaking for the voluntary and community sectors. In the artworks, older autistic people’s visions of ageing and support are captured in hand-drawn scenes and diagrams by artist Clare Mills of Listen, Think, Draw.
Emma Stanley, a co-researcher on the initiative and a member of the Iceberg Productions team, sadly passed away during the project. Speaking in the films, in which she acted as interviewer, Emma said: “It’s an important project, because no matter what walk of life you’re in, you get old. My mum died a couple of years ago and there’s still not enough help out there for autistic people suffering bereavement. It will get more important when you get older.”
Th researchers say the project provides insights into how to start conversations around what a good life will look like in older age and the need to support understanding of change and loss. The project also shows the need for creating safer spaces for those dialogues, and for working together to develop a shared understanding of a person’s need – as well as the need for effective care pathways for older autistic people.
The NHS estimates that at least one in 100 people in Scotland is autistic, with some research showing more than double that number. Many older autistic people will not have a diagnosis. Scottish Autism says these figures underline the need to plan properly for inclusive and person-centred services in older age.
The findings of the research will be presented at an event in the Scottish Parliament at Holyrood in Edinburgh on Wednesday 19 March.
The event will be chaired by Daniel Johnson MSP and attended by Minister for Social Care, Mental Wellbeing and Sport, Maree Todd. The event will include a screening of the documentary and display of the artworks created from the project.
AS A RESULT OF THIS RESEARCH, PROJECT PARTNERS ARE CALLING FOR:
• Timely, multi-agency planning for transitions across the lifespan of autistic people, including the transition to older age
• Tools and resources to support autistic people to understand the changes they may face and to codesign their care as they age
• Holistic care pathways in older age, incorporating multi-disciplinary collaboration and bringing healthcare into familiar and safe environments for autistic people
• Data, transparency and accountability relating to the support provided for older autistic people and to the resulting outcomes. This will help maximise the lessons learned, in order to establish best practice.

WHAT’S ON THE AGENDA?
UK Care Week is an event exclusively for care professionals, designed to empower and equip you with the skills to enhance the lives of those in care. This event provides a vital platform to explore industry-leading content, innovative solutions, and hands-on product demonstrations.
With 100+ CPD-accredited sessions, innovative products from 150+ top suppliers, and tailored guidance at the CQC Inspector Hub, you’ll find resources to meet the highest standards. Dive into interactive features like the Virtual Dementia Tour and expert-led training to elevate care.
The event features an impressive lineup of sessions, workshops, and opportunities to engage with the latest developments in the care sector. Key highlights include: THE CARING VIEW THEATRE
Hosted by the passionate team behind the Caring View Podcast, this theatre promises engaging discussions and insights into the latest care practices and strategies.
Meet over 150 exhibitors showcasing solutions designed to stimulate business growth and help implement sustainable care models. Discover cutting-edge technologies and practical tools to elevate your care services.
Attend interactive seminars hosted by industry experts. These sessions tackle real-world challenges in
care settings and offer actionable solutions to overcome them. Gain up to 12 CPD points across 2 days.
CQC INSPECTOR HUB
Book a 1-2-1 meeting with a CQC Inspector to discuss any queries you may have; local inspectors will be able to answer any queries, as well as dealing with registration advice.
CO-LOCATED EVENTS
Gain access to additional CPD sessions and resources through co-located events, including The Alzheimer’s & Dementia Show, Neuro Convention, and Naidex. These events create a collaborative environment that unites aspects of health, social care, rehabilitation, inclusion, and diversity.
EXCLUSIVE TRAINING OPPORTUNITIES
In partnership with Training2Care, co-located event The Alzheimer’s & Dementia Show offers unique experiential training sessions tailored to dementia care:
• Virtual Dementia Tour: £60 + VAT per session
• Dementia Interpreters Workshop: £45 + VAT per session
• DIET, Dining Immersive Experiential Training: £60 + VAT per session
• Autism Reality Experience: £60 + VAT per session
Spaces for these sessions are limited, so early booking is highly recommended. Uk Care Week visitors can book onto these sessions via the Alzheimer’s & Dementia Show website - www.alzheimersshow.co.uk/training DON’T MISS OUT!
Join us at UK Care Week 2025 and take part in this essential gathering of care professionals. Connect with experts, explore innovative solutions, and access tools to drive care excellence. Register for your free ticket today
www.ukcareweek.com

TAKING PLACE THIS WEEK!

New survey insights reveal the far-reaching impact caregiving can have on physical and mental well-being, with over half (54%) of caregivers reporting weekly back, joint or muscle pain, and 1 in 5 (19%) experiencing daily stress or anxiety.[i] Dr Dawn Harper shares her tips to help cope.
There are approximately 4.7 million unpaid carers in the UK,[ii] defined as those who provide unpaid care for someone who is ill, disabled, older, has mental health issues or struggles with addiction. However, this figure excludes the many who regularly care for children, neighbours or friends and family needing support beyond the traditional definitions. Carers UK estimates that the number of unpaid carers could be as high as 10.6 million, highlighting a significant lack of personal and societal recognition of what it truly means to provide care.[iii]
A new survey, commissioned by GOPO® Joint Health – a leading supplement proven to reduce pain and stiffness and improve mobility – polled 1,001 self-defined caregivers. The findings reveal the true impact of caregiving on mental, emotional and physical health.
Over one-third (37%) have experienced significant strain, discomfort or injury to their joints as a result of assisting or lifting the person they care for, and almost half (47%) frequently endure persistent aches, stiffness or pain that lingers long after caregiving tasks.i As a result, one-third (32%) rely heavily on pain medication, putting their own long-term health at risk. The mental toll of caregiving is profound, with almost half (46%) of caregivers feeling emotionally drained by the relentless stress it brings. One in seven (13%) rely on support services for their well-being, while nearly half (44%) experience loneliness or isolation at least once a week, often facing the demands of caregiving alone.
Despite these challenges, almost half (49%) of respondents cannot remember the last time they practiced self-care, admitting that their own needs always come last.i While caregivers devote themselves to others, acknowledging the importance of self-care, and setting aside time for their own well-being is vital.
Dr Dawn Harper, formerly a caregiver to her mother, NHS doctor for over 30 years and author of ‘Live Well to 101’, comments: “Caregiving is a labour of love, but the selfless nature of the role puts many caregivers at serious risk of poor health. As a GP I see first-hand the impact that caring can have on both physical and mental ill health. To continue supporting others, it’s vital to care for yourself first. Just like the safety advice on an aeroplane – put on your own oxygen mask before helping others. Prioritising your own wellbeing ensures you have the strength, resilience and capacity to provide the care your loved ones need in the long-term.”
Dr Dawn Harper provides her top tips to support caregivers’ health and well-being: Seek support from peers: “It can be easy to lose your identity when providing care, so it’s important to connect with peers who are in a similar situation. If you are unable to leave the house often, online forums or virtual coffee sessions can provide an outlet to enable you to open up to someone who understands exactly
what you’re going through. Their acceptance and understanding can be a great way to support your emotional health and leave you feeling less alone.”
Schedule self-care: “Caregiving often leaves little time for personal well-being, but self-care isn’t a luxury, it’s a necessity. Schedule self-care just like any essential appointment and if you’re struggling to find the time, start with small manageable breaks of just 5-10 minutes and commit to doing one thing that makes you feel recharged. This could be as simple as having a cup of tea in silence or reading a few chapters of your favourite book.”
Build your mental resilience: “Mental resilience helps caregivers manage stress, maintain emotional balance and continue providing care without burning out. Incorporate techniques such as mindfulness, deep breathing, yoga or meditation, all of which can be practiced in as little as 15 minutes. If you are struggling with your mental health, make sure to reach out to mental health helplines or listening services, or discuss your feelings with your GP or pharmacist.”
Prioritise your physical health: “Caregiving is a physically demanding role, and these survey findings reveal the true toll caregiving can take on your physical health. Protect your joints and posture by using proper lifting techniques when assisting with mobility, and address any aches and pains early to help prevent chronic conditions from appearing later down the line. A joint health supplement such as the galactolipid, GOPO, a compound derived from rose-hip, may be of great benefit, with research indicating that it can effectively relieve joint pain.[iv] The natural anti-inflammatory properties of GOPO make it a viable replacement to pain killers,iv without the risk of harmful side effects, and a sustainable way to manage pain long-term.”
Extensive studies involving over 400 patients with chronic pain conditions, such as osteoarthritis, have shown that GOPO® produces significant and consistent pain relief and improved joint function. In one study, 8 out of 10 patients reported a significant reduction in pain after just 3 weeks of GOPO®.[v]
GOPO® Joint Health is available from Boots, Amazon, and independent chemists and retailers nationwide. Visit www.gopo.co.uk for further information.
[i] GOPO® Joint Health survey on 1,001 caregivers in the UK. January 2025.
[ii] The Kings Fund. 2024. What are unpaid carers, who are they and how often do they provide care? Available at: https://www.kingsfund.org.uk/insight-and-analysis/data-and-charts/unpaid-carersnutshell#:~:text=According%20to%20the%202021%20Census,females%20from%20the%202011%20Census. (Accessed: January 2024).
[iii] Carers UK. 2023. Annual Report 2022-2023. Available at: https://www.carersuk.org/media/ynfpnjwk/carers-uk-annual-report-22_23 (Accessed: January 2025).
[iv] Winther, K et al. “A powder made from seeds and shells of a rose-hip subspecies (Rosa canina) reduces symptoms of knee and hip osteoarthritis: a randomized, double-blind, placebo-controlled clinical trial.” Scandinavian journal of rheumatology vol. 34,4 (2005)
[v] Winther, K et al. “A powder made from seeds and shells of a rose-hip subspecies (Rosa canina) reduces symptoms of knee and hip osteoarthritis: a randomized, double-blind, placebo-controlled clinical trial.” Scandinavian journal of rheumatology vol. 34,4 (2005)
[vi] Rein E, Kharazmi A, Winther K. A herbal remedy, Hyben Vital (stand. Powder of a subspecies of Rosa canina fruits), reduces pain and improves general wellbeing in patients with OA – a double-blind, placebo-controlled, randomised trial. Phytomedicine 2004.
[vii] Christensen R et al. Does the hip powder of Rose canina (rosehip) reduce pain in osteoarthritis patients? – a meta-analysis of randomised controlled trials, Osteoarthritis Cartilage (2008)
[viii] Schwager J, Richard N, Wolfram S. Anti-inflammatory and chondro-protective effects of rosehip powder and its constituent galactolipids GOPO Poster presentation at the World Congress of Osteoarthritis (OARSI) 2008

GOPO® Joint Health contains specially-cultivated naturallysourced rose-hip with a uniquely high level of GOPO®
GOPO®, a key component of rose-hip, was discovered nearly 30 years ago in Denmark. Long-standing research projects have focused on rose-hip with a high level of GOPO® Rose-hips help maintain healthy and flexible joints.
www.gopo.co.uk
Food supplements should not be used as a substitute for a varied diet and healthy lifestyle.

Veterans living at a charity’s care homes and using its services have been sharing their views as part of a new project highlighting the value of veterans and older people.
Veterans’ Voice aims to give a platform to residents in Royal Star & Garter’s Homes, and the people who use its services, ensuring they are not hidden because of their disability or dementia. It also aims to recognise and celebrate the process of ageing by sharing their knowledge and supporting their beliefs and wishes for the country’s future.

Royal Star & Garter provides loving, compassionate care to veterans and their partners living with disability or dementia, from Homes in Solihull, Surbiton and High Wycombe and through services reaching into the community.
The charity has helped veterans find their voice, tackle loneliness, and support them to foster friendships and companionship through its Day Care and Lunch Clubs. Their free nationwide Telephone Friendship Service also addresses issues of isolation, with trained volunteers calling veterans and their partners who live in their own homes anywhere in the country.
As part of Veterans’ Voice, Royal Star & Garter residents have expressed their concerns and hopes for the future. RAF veteran Michael wants more understanding and equality: “I’d like to see a world where everyone is treated fairly. It’s wrong to pre-judge anyone.” And he added: “We must respect other people’s views. I think that is a problem, especially right now. I think politics today is too divisive.” Yvonne, whose husband served in the RAF, added: “I think there’s lots that needs to be changed because the world is in a mess.”


RAF veteran and resident John wants to see a future without armed conflict. He said: “People just seem to go into things without realising what they’re doing, and the consequences of what they’re doing. If I had the power to, I’d end all wars.”
Residents also feel more should be done to help and support Armed Forces personnel when they leave
the military. Michael called for better welfare, and for them to be treated with more respect. “I think that’s the least we can do, when you consider the sacrifices they have made for us,” he said.
Royal Star & Garter has also supported veterans to be heard and appreciated through its other services. Navy veteran John uses their Telephone Friendship Service fortnightly. He said the conversations allow him to speak to his volunteer about personal issues, which he doesn’t want to worry his family with. He said: “It’s nice to talk to someone who isn’t family, someone from the outside, to explain things to, and who relieves my concerns. I feel the burden and pressure that I carry relieved.” He added: “We all get lonely. There might be a time when I haven’t spoken to my children for a while, but I know that someone will call me and ask how I’m doing, which makes it a lot better.”
Royal Star & Garter is one of the charities supporting the Veteran Friendly Framework (VFF), which aims to improve the care and support given to veterans in all care homes in England. The Willows care home has been supported in achieving the Veteran Friendly Framework and sees huge benefits from this. Home Manager Julie Gregory said: “The recognition and celebrations shouldn’t stop just because veterans live in a care home. We can act as their voice and share with the community what they have achieved, ensuring they are not forgotten.”
Caley Eldred, the Director of Supporter Engagement at Royal Star & Garter, said: “We want to communicate the value of our older people, their views and their experiences. People living in adult social care are often overlooked and sidelined. Their views are relevant – they care about people having a safe place to live, they are passionate about the world being a peaceful one and they uphold the values of respect and equality. They are also positive about life in a care home and want to help us show that it can still be fun! We share the common desire to increase respect for each other in the local communities where we operate, and we hope Veterans’ Voice will contribute to this.”
Residents and staff joined together at Magnolia Court to celebrate the vibrant Jewish festival of Purim, in partnership with the local Chabad Jewish group.
The celebration brought the story of Purim to life, with the reading of the Megillah, the Book of Esther, in Hebrew. Residents and staff alike listened attentively as the ancient tale of courage and salvation unfolded, recounting the story of how Queen Esther and her cousin Mordechai saved the Jewish people from the evil Haman.
A highlight of the festivities was the enjoyment of traditional Purim pastries, Hamentashen, also known as Haman's ears. These triangular treats were savoured by all, adding a sweet touch to the joyous occasion.
In keeping with the festive spirit of Purim, which encourages fancy dress,
staff members embraced the tradition with enthusiasm, donning an array of creative and comical costumes.
"It was wonderful to see our residents so engaged and happy," said Cosmin Tiriteu, Home Manager at Magnolia Court. "Purim is a time of joy and celebration, and we were delighted to share this special occasion with our residents and the Chabad community. The costumes and the Megillah reading brought so much laughter and happiness to our home."
Chabad is a global movement dedicated to spreading Jewish awareness and providing support to Jewish communities worldwide. Their involvement in the Magnolia Court celebration helped to bring the rich traditions of Purim to the residents, enhancing their cultural and spiritual well-being.


If you’re involved in caring for others – whether you’re a care provider, a health and social care professional seeking the latest products and services, a family carer in need of support, or simply someone passionate about care – the Alzheimer’s & Dementia Show is the event for you.
As the UK’s leading dementia event, it offers a unique opportunity to explore a wide range of care exhibitors, hear from expert speakers, and experience innovative training sessions. This event is more than just an exhibition; it’s a platform for learning, discovering solutions, and connecting with people who share a commitment to improving dementia care.
Taking place at the NEC in Birmingham on 19-20 March 2025, the Alzheimer’s and Dementia Show provides a vital space for families, carers and healthcare professionals to access resources and knowledge that can transform the lives of those affected by dementia. WHAT’S ON THE AGENDA?
The show is packed with insightful sessions designed to address key aspects of dementia care. Discover the latest diagnostic tools and
treatment options that are revolutionising early intervention and improving patient outcomes!
CAREGIVER SUPPORT AND EDUCATION
Access practical strategies and resources that empower caregivers to provide compassionate and effective care, ensuring the well-being of those they look after.
DEMENTIA-FRIENDLY ENVIRONMENTS
Learn about innovative designs and technologies that create safer, more comfortable living spaces for individuals living with dementia. WHY ATTEND?
For those seeking specialised training, the show offers sessions delivered by Training2Care. These experiential programs provide actionable insights tailored to dementia care. Sessions include:
Virtual Dementia Tour: £60 + VAT per session
Dementia Interpreters Workshop: £45 + VAT per session
Dining Immersive Experiential Training (DIET): £60 + VAT per session
• Autism Reality Experience: £60 + VAT per session
Spaces are limited, so early booking is highly recommended. Book your space here - www.alzheimersshow.co.uk/training.
EXPERT-LED SESSIONS
Gain insights from top researchers, clinicians, and advocates. Key speakers include:
• Prof Fiona Ducotterd "Putting tools in the toolbox to treat dementia." Chief Scientific Officer, Alzheimer’s Research UK, UCL Drug Discovery Institute
• Hannah Gardner "Supporting children and young people living within
families affected by dementia." Consultant Admiral Nurse for Children and Young People, Dementia UK
• Prof Nathan Davies "Supporting people living with dementia through to end of life" Professor of Ageing, Applied Health and Care Research, Colead Centre for Psychiatry and Mental Health, Queen Mary University of London
1-TO-1 DEMENTIA CLINICS WITH ADMIRAL NURSES
For personalized advice and support, visit Dementia UK’s Admiral Nurses. These 1-to-1 clinics provide tailored guidance to address your specific questions and concerns.
NETWORKING OPPORTUNITIES
Connect with a diverse community of caregivers, healthcare professionals, and innovators. Share experiences, exchange ideas, and build valuable relationships within the dementia care sector.
EXHIBITOR HIGHLIGHTS
Explore an extensive range of exhibitors showcasing products and services designed to enhance the quality of life for individuals living with dementia. From cutting-edge technologies to practical caregiving tools, find innovative solutions to meet your needs.
DON’T MISS OUT!
Running alongside UK Care Week, Naidex, and the Neuro Convention, the Alzheimer’s and Dementia Show unites interconnected aspects of health, social care, rehabilitation, inclusion, and diversity. This collaborative environment provides a comprehensive look at the broader care community.
Find out more - www.alzheimersshow.co.uk






In an extraordinary twist of fate, two residents of Horse Fair Care Home in Rugeley have marked a truly remarkable milestone, both celebrating their 101st birthday on the same day.
Audrey Williams and Louie Wroe, both born on 3rd March 1924, have witnessed more than a century of history, from world wars to technological revolutions.
While reaching 101 is an achievement, the rare coincidence of two residents in the same care home sharing the same birthday makes this occasion even more special.
To honour their big day, the Avery Healthcare-owned care home hosted a joyful celebration with residents, staff, friends, and family.
The festivities featured a beautifully decorated cake, live music, and a special guest playing the organ to serenade the birthday ladies.
Audrey Williams, originally from Walsall, spent much of her life in Lichfield.
She met her husband, Arthur (Nat) Williams, during the Second World War and went on to raise eight children, who are now spread across the globe.
A devoted mother and community member, Audrey fondly recalls cycling everywhere in her younger years and spending summers in Guernsey with family.
Despite never learning to drive, she has travelled far and wide, visiting Australia, South Africa, and Canada.
"I never imagined I’d be celebrating my 101st birthday, let alone with someone who shares the same special day!" Audrey said with a smile. "It’s been a truly lovely surprise. I’ve been surrounded by so many wonderful people today, and I feel


incredibly lucky to have reached this age. Seeing everyone together to celebrate has made the day even more special."
Louie Wroe originally from London, lost her mother at a young age and was raised by her grandmother and aunt in Preston.
She later married her husband, Steve, during the war and built a happy life in Yorkshire, where they raised their son.
A former shoe shop assistant, Louie reminisces about the ‘old-fashioned days’ and has always enjoyed embroidery, walking, and colouring.
She holds fond memories of holidays in Scarborough and regular visits to family in Preston.
"It’s been a wonderful day. I feel so lucky to celebrate with friends, family, and of course, Audrey!" Louie said, beaming. "I never thought I’d see my 101st birthday, and to share it with someone else who has lived through so much of the same history makes it even more meaningful. The care home has made us feel like royalty today, and I couldn’t have asked for a better way to mark the occasion."
Julie Anderson, Manager of Horse Fair Care Home shared: "To have one resident reach 101 is an incredible moment, but for two to share the same birthday in the same home is something truly special. Audrey and Louie have led fascinating lives, and it has been a privilege to celebrate with them."
This rare double birthday celebration not only highlights the incredible lives both women have led but also showcases the strong sense of community within the care home.
Sundial Care Home, which sits in the heart of Tipton St John, Devon, recently held their very own bake off. Team members at the home, tied on their aprons and whipped up a selection of delicious bakes for residents to taste and judge, who the home fondly refer to as “family members”.
Those who chose to participate had their voting slips and pens at the ready as they sampled a piece of each cake. Mikyla Tribble, the homes Administrator, prepared a perfectly glazed banana cake, Sue Smith, Care Assistant, crafted a rich chocolate sponge, decorated with roses and fondant icing, Tina Sutton, a part of the Kitchen Team baked a classic coffee and walnut cake, and finally,
Baking is a skill that many family members have enjoyed throughout their lives, and the bake off provided a fun and familiar experience for them to test the teams baking skills, whilst igniting fond memories through the power of taste and aroma.
The Care Home near Sidmouth, Devon, continues to offer meaningful activities that reflect daily life, provide opportunities that reflect daily life, ensuring those living there remain engaged and connected in ways that feel natural and fulfilling.
Nothing could stop strong-willed 84-year-old Carol Stocks, who lives with dementia, from completing her mission to walk at least 30 minutes every day in February to raise funds for Dementia UK.
True to her word, Carol, a resident of Eckington Court Nursing Home in Derbyshire, walked for 28 straight days last month and surpassed her goal, raising over £150 for the charity.
Braving all weather conditions, Carol also inspired her friends and fellow residents at Eckington Court to join her on her daily walks.
Carol chose Dementia UK as the charity for her fundraising because, like many of her friends at Eckington Court, she is living with dementia. “The thought of the money raised going towards research into finding a cure for dementia kept me going,” she said.
Carol is a proud mother of two daughters and had a vibrant career as both a teacher and a window dresser.
Known for her outgoing personality, she’s always up for an adventure and loves to explore. Even now, she and her daughters regularly embark on exciting mini getaways, discovering new places and making lasting memories together.
At Eckington Court, Carol dives into every activity with enthusiasm - from crafting and knitting to bingo, music, and singing. Colleagues at the home describe her as ‘the life of the party, bringing energy and joy wherever she goes!’
Trudy Godley, Home Manager at Eckington Court Nursing Home, said: “We knew nothing was going to stop Carol once she put her mind to the task! Her enthusiasm was infectious, and quite soon many of us were taking part in Carol’s daily walks. We are incredibly proud of what she achieved.”


Residents from Bedhampton Court in Havant, Hampshire, part of the Healthcare Homes Group had a fantastic day out, taking a trip to Southsea to visit the Cumberland House Natural History Museum, followed by a relaxing stop at Canoe Lake. The outing, organised by Activities Coordinator Myle, was a wonderful opportunity for residents to enjoy a change of scenery, explore the wonders of nature, and reminisce about days gone by.
The visit began with a walk through the museum’s butterfly enclosure, where residents were surrounded by the delicate beauty of these fascinating creatures. They then explored the museum’s impressive A to Z collection of preserved species, featuring a wide variety of animals, birds, and marine life. A particular highlight for many was seeing ‘Emily’ the giant dinosaur, a well-loved exhibit that has been a fixture in the museum for years.
Following their time at the museum, the group took a short walk to Canoe Lake, where they enjoyed hot drinks and ice cream while taking in the peaceful surroundings. The resident swans were particularly welcoming, much to everyone’s

delight. To round off the trip, their friendly driver, John, took them on a scenic drive through Portsmouth, pointing out how the city has changed over the years. The journey brought back fond memories for many of the residents, who were able to reflect on the past while enjoying the sights of the present.
Care Assistant, Gertrude Abah, shared her thoughts on the day, saying, “I really enjoyed being with the residents and seeing them so happy. It was lovely to watch them have a change of scenery and enjoy some time out of the home. I think it was refreshing for them, and for me, too. It’s always special to see them enjoying themselves, and I feel lucky to be part of such moments.”
Resident Pat also expressed her appreciation, saying, “I had such a great time out today, it really lifted me.”
The trip was a great success, leaving residents with smiles on their faces and plenty of stories to share. The team at Bedhampton Court looks forward to planning more excursions that bring joy and meaningful experiences to the residents.
Health and social care charity Alternative Futures Group (AFG) has been recognised in the prestigious top 50 list of the UK Best Workplaces national award.
The not for profit organisation, which operates across the North West, has been recognised as the 45th best ‘super large’ employer by Great Place To Work (GPTW). AFG has been supporting people with learning disabilities or a mental health condition for the past 30 years.
GPTW carries out extensive staff surveys and assessments of employees’ daily experiences of innovation, the company’s values, and the effectiveness of their leaders. They ensure that the results reflect a consistent experience across departments and seniority levels.
Kirsty Murphy, Chief People Officer at AFG, said: “We are constantly seeking new ways to create meaningful, positive work environments. From investing in training to launching a new reward platform, we want to recruit and retain the best people to be able to deliver amazing personalised support that creates independence and value.
“Our people are our greatest asset. Their dedication, compassion and professionalism allow AFG to deliver personalised support and independence outcomes that goes above and beyond what other providers can do. That is why we are delighted

to be recognised as a top 50 great place to work, by those who matter – those who work for us.”
Andrew Dewhurst, AFG team leader from Blackburn, said: "I am incredibly proud of how far AFG has come since I began working here as a support worker in 2014. We truly are a great place to work and the recognition of this at the GPTW awards is completely deserved.”
As part of the application for Great Place to Work accreditation AFG carried out a colleague survey which had an 85 per cent response rate.
Some highlights include:
I understand how my job contributes to achieving organisational objectives – 85 per cent
I have good conversations with my manager – 84 per cent
My work has special meaning: this is not ‘just a job’ – 84 per cent
I am offered training and development to further myself professionally – 81 per cent
AFG employs 1,800 people working in Merseyside, Greater Manchester, Cheshire and Lancashire and works with around 900 people with learning disabilities and mental health issues.
Proof that you’re never too old for adventure, the oldest person in the North West, 110-year-old Marjorie Hodnett Aylward, has been getting out and about this year.
Also affectionately known as ‘Aunt Marj’, she’s a care home resident at New Care Homes’ Formby Manor and has so far taken part in two trips out this month, thanks to the never-wavering support of the Formby Manor care team and Myley, a bespoke tour services company. Oldest woman in the North West spends a day at the garden center
Most recently, the orchids were calling to Aunt Marj as she booked her first trip to the garden centre. No surprises here, she’s quickly booked for a second trip! Some may say there’s no stopping Aunt Marj once she’s been inspired to experience the world, and with the help of her care team and Myley, there’s nothing standing in her way.

Care Home and Myley work together to bring their residents a perfect day out Working with Myley gives Formby Manor’s care team the helping hand they need to make sure residents are getting the most from life outside of their care residence. They make sure no door is closed to their residents, no matter their age or abilities.
The care team at Formby Manor and the team at Myley work closely to craft the perfect outings for residents, taking into account their abilities, preferences and ideas. Myley takes on the logistics, assessing locations, arranging transportation and guiding the tours. So, Aunt Marj and Home Manager Nikki can focus
on their fun day out with the flowers!
What’s next for Aunt Marj?
Aunt Marj is officially the oldest person that Myley is currently working with, and she keeps the team on its toes. She’s known very affectionately by all of those she’s spent time with, both in Formby Manor and at Myley.
With a hefty milestone ahead of her, up next for Aunt Marj is her 111th birthday. She’s working with the Formby Manor team to organise a birthday blowout with music, great food, birthday cake and a well deserved toast.
Nikki Foster, Home Manager at Formby Manor says: “I want my residents to be happy, that’s always at the forefront of my mind.
“Myley trips are incredible for our residents. Exploring new places and experiences helps residents rediscover the joy and excitement of life’s adventures and promotes mental stimulation and curiosity. It also provides a refreshing change of scenery and a break from usual routines. Our residents simply need to sign up and Myley takes care of the rest.
“This is the second time that Myley has delivered a trip for Aunt Marj. The first one to Lady Green Garden Centre took place just over a week ago and Aunt Marj enjoyed it so much she immediately requested another one to check out the house plants and orchids at Dobbies. She has her heart set on a large dark green and silver house plant for her room.”
A colleague at HC-One Wales’s Abermill Care Home, in Abertridwr, Caerphilly, has revealed her aims to qualify for the 2025 World Para Athletics Championships in India.
Bree Cronin, 21, Carer at HC-One Wales’s Abermill, is a disability para-athlete in discus and shotput throwing after sustaining life-changing injuries that led to a lower leg impairment which affects her muscle power and range of movement.
Bree suffered an accident that led to broken bones. Bree did not want to go down the disability route and wanted to remain in the able-bodied sports category, but had to reconsider her options after her mobility was impaired due to her accident.
The young Welsh athlete was classified as an F44 for discus and shot put, which is lower limb competing without prosthesis affected by limb deficiency, leg length difference, impaired muscle power or impaired passive range of movement.
Last year, Bree was ranked number two in the F44 classification for discus throwing at 1kg. She was also ranked 23rd in the under-23 level for discus in 2024.

Bree is now focusing on qualifying for the 2025 World Para Athletics Championships in India. According to Bree, she needs to meet behavioural aspects for the team as well as the performance requirements – if she is ranked in the top eight positions for Team GB’s para-athletes, she believes she is likely to be selected to be on the team.
Bree Cronin, Carer at HC-One Wales’s Abermill Care Home, said:
“I am nearly at the stage of competing where I used to be before my accident. I’ve represented Cardiff Armchair Athletics Club since I started in 2018.
“I’m on a British Athletics program as a non-funded athlete, where there are stages to get there – the
higher you go, the more chance you have to get selected for the team.
“It would help to get to the World Championships in India by the end of this year. My goal is to qualify for the World Championships – that would be cool to compete on that stage, and I am optimistic that I will be selected to be on the team.”
Bree revealed that she is now throwing as far as she did when she was able-bodied, which gives her the belief and confidence that she will continue to progress. According to her Power of 10 results, Bree has a personal best of 41.79 metres for discus at 1kg.
Bree began training with Wales’ Paralympic team, and she has made friends, gained confidence, and learned to talk to people without feeling shy. Bree also has a long-term dream to compete at the next Paralympic Games in 2028.
Bree added:
“My mum is so proud of me! And I’m proud of her. As for my dad, I try not to discuss it too much with him — for my mental health. But I hope he’s proud too. My goal is to get to the 2028 Paralympic Games in Los Angeles.”
Bree faces daily physical and mental challenges due to her disability. She has overcome many obstacles with pain management and the support, encouragement, and patience of her tutor.
This includes rebuilding her confidence and learning not to be afraid to ask for support. Bree also took the opportunity to pursue a career in the care sector by making a positive difference to the lives of others through delivering individualised care.
Bree joined Abermill Care Home in August 2023, inspired by her mother's experience and the rewarding opportunities in the care sector. Helping others and providing compassionate care comes naturally to Bree, making her career path both sustainable and fulfilling.
Commercial Kitchen and Laundry Solutions (CKLS) are one of the UK's leading suppliers of commercial kitchen and laundry equipment.

Whether you are a small sized residential home or large scale nursing home group, CKLS has the expertise and equipment you need to keep your operations running smoothly.
At CKLS, we understand that the success of your business depends on the quality of the equipment you use. That's why we've made it our mission to provide businesses across the UK with the highest quality commercial laundry and kitchen equipment available. We work with only the best manufacturers in the industry to ensure that our customers get the most reliable and efficient equipment possible.
Our commitment to our customers doesn't end with the sale of our equipment. At CKLS, we know that maintenance and repairs are crucial to keeping your equipment functioning at its best. That's why we offer
a full range of maintenance and repair services to our customers, including emergency repair services available 24 hours a day, 7 days a week.
We believe that our success as a company is measured by the success of our customers. That's why we're constantly striving to provide better products and services to help our customers achieve their goals. We're proud to say that our commitment to excellence has earned us a reputation as the go-to provider of commercial laundry and kitchen equipment in the UK.
So, if you're looking for reliable, high-quality commercial laundry and kitchen equipment, look no further than CKLS. With our extensive range of products and services, we're confident that we can help you find the right equipment to meet your needs and keep your business running smoothly for years to come.
Visit our website www.ckls.co.uk contact by phone on 01200 411914 or email at sales@ckls.co.uk.
Mobile Kitchens Ltd specialises in the hire or sale of temporary catering facilities and foodservice equipment.
Ideal for events or to provide temporary catering facilities during your kitchen refurbishment, our versatile units and equipment offer an efficient and economic solution to the caterers’ needs.
Production Kitchens, Preparation Kitchens, Warewashing Units, Dry Store Units, Cold Rooms and Restaurant Units are available as individual units in their own right or they can be linked together on site to form a complete complex.

Alternatively, we can offer modular, open-plan facilities, usually for larger, longer-term hires.
We offer a free design service, and project management from concept through to delivery and installation on site, plus full technical support throughout the hire period.
The standard specification of our smallest Production Kitchen unit includes a six burner oven range, salamander grill, twin basket fryer, upright fridge, hot cupboard, single bowl sink unit with integral hand wash basin, plus ample power points to plug in Microwaves, Food Processors, Toasters etc. Internal equipment can be interchanged and clients can effectively specify their preferred layout.
We have many tried and tested design layouts and would be pleased to put forward our recommendations for your project. So if you’re planning a refurbishment or need to cater for an event then why not give us a call and we’ll be happy to provide advice and put forward a competitive proposal. For further information or to arrange a site visit, email: sales@mk-hire.co.uk or call us on 0345 812 0800, or visit our website: www.mk-hire.co.uk


Infection control is critical in care homes, where laundry processes play a vital role in hygiene management. Care homes face increased pressure and scrutiny with changes to the Care Quality Commission inspection framework, and it is absolutely fundamental that care homes know how to safely ensure efficient infection control across all areas. CQC inspections place heavy emphasis on evidence-based infection control practices, including rigorous checks on laundry processes. Compliance with these standards is essential to safeguard residents, maintain trust, and achieve strong CQC ratings.
There are various way to ensure the right levels of hygiene control; you should employ thermal and/ or chemical disinfection. Ozone is one of the disinfection options that can be successful, but it is essential to adhere to HSE recommendations, take appropriate safety precautions, and use control measures as outlined by COSHH as use of this powerful oxidant does carry potential health risks. Forbes Professional offers care homes alternatives to Ozone systems, that still meet the most exacting hygiene requirements. Their

Miele commercial laundry machines enable sluice, thermal and chemical disinfection, to meet all the industry requirements of WRAS and CQC. When paired with Forbes’ advanced chemical detergents, which kill pathogens even at low temperatures, these commercial machines deliver a complete laundry solution for optimal infection control.
Forbes understands that care homes require tailored solutions. Their industry specialists work closely with operators to recommend the right commercial machines to meet their specific needs. Beyond installation, they offer award-winning service support to ensure ongoing compliance and operational efficiency.
For any care home, laundry is a key part of infection control. It is imperative that appropriate commercial laundry equipment is used within a care setting, and that there is a reliable partnership in place for service and maintenance. By choosing Miele’s technology and Forbes Professional’s expert support, care homes can safely and effectively meet stringent hygiene standards.
See the advert on the facing page for further information on Forbes.
MAG Laundry Equipment is a multi-award-winning supplier of commercial washing machines & tumble dryers that supports over 10,000 care homes across the UK. Clean laundry and bedding is critical for care homes, hospices, nursing homes, hospitals and other healthcare organisations. With a nationwide fleet of accredited engineers MAG Laundry Equipment has successfully assisted over ten thousand care homes with their products, services, information and support.
MAG’s product range includes commercial washing machines, tumble dryers, ironers, presses and detergents. For 100 years, since 1922, MAG’s products have been developed and improved to become some of the most reliable, energy-efficient and

the machines, and giving them a check-over, to see which parts, if any, can be carried over the refurbishment. Lavamac will only carry over the highest-quality parts from the machine from pre to post refurbishment. The machine then undergoes an extensive refurbishment, with almost all the parts being replaced, with the refurbished machines being given specialist parts based on the model type.
not only contributing to a greener way of
but also saving our customers money!
We have recently set up a specialist facility in St. Neots, near Cambridge, in which we are going ahead with this specialist refurbishment programme. This programme involves purchasing existing machines, and replacing the parts on them, so that they are as good as new, whilst retaining the look and feel that existed before, but with a massively increased lifespan, and a warranty on the machines that’s as good as a warranty on a new machine to go with the refurbishment too. Our refurbishment programme in our specialist facility includes stripping down

We recently have been awarded a bronze award in sustainability by the groundworks trust, affirming our commitment to the sustainability industry – however, as much of a compliment as it is, it does not mean that the hard work stops there! The next step on our journey is to hopefully be awarded the prestigious silver sustainability award! For this, we need to ensure that our carbon emissions are being cut down from our vans, continue our sustainability and refurbishment programme and to keep making green decisions within the company! 0151 317 3127 info@laundrytec.com www.lavamac.eu


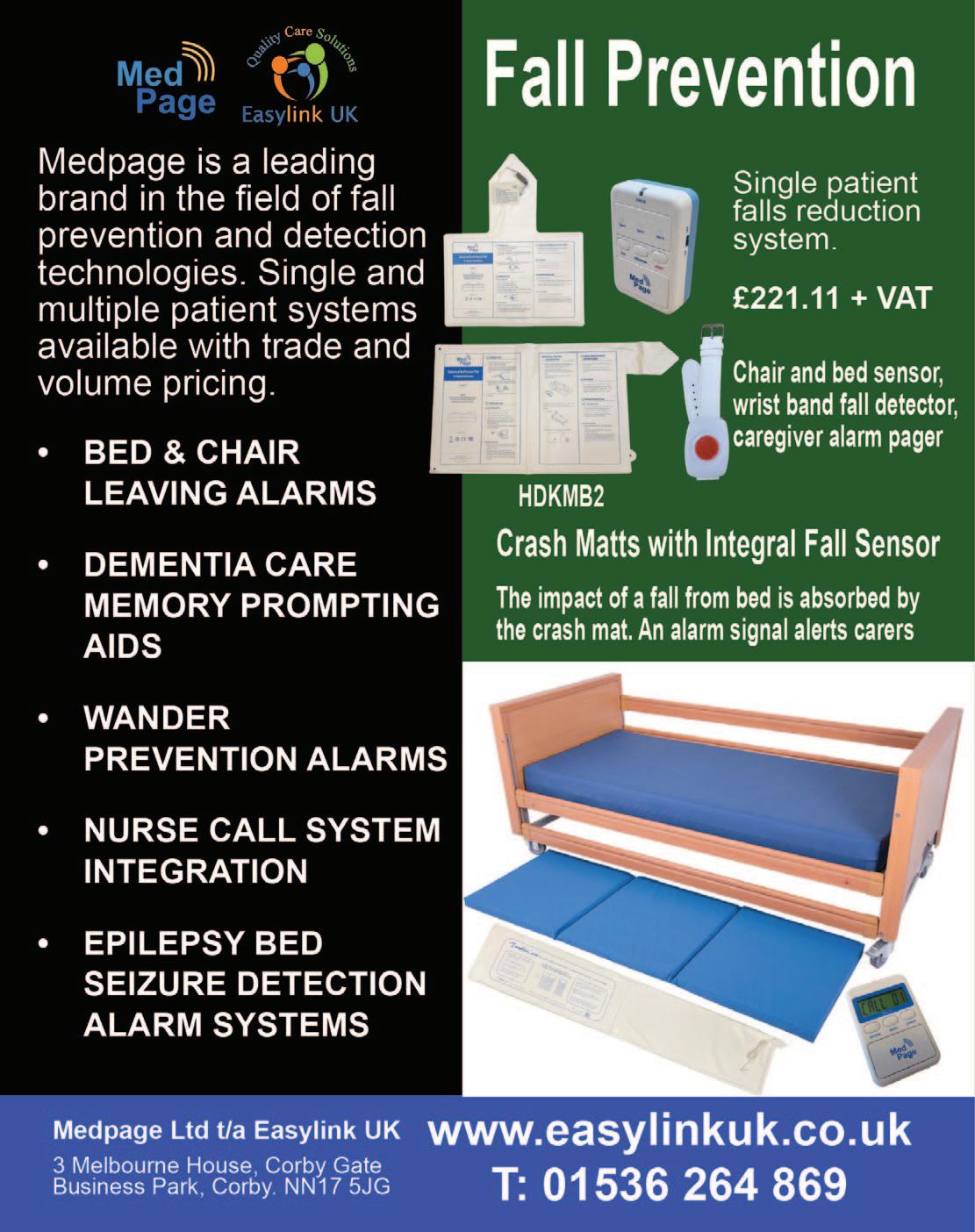
FALL SAVERS ® WIRELESS MONITOR

Eliminate all cables with our new generation falls management solutions!
Upgrade your falls programme with the latest technology from Fall Savers®.
eliminates the
between the monitor and sensor pad. This results in less work for nursing staff, improved safety for patients and reduced wear and tear on sensor pads. Wireless advantages include the ability to use one monitor with two sensor pads simultaneously and support for many new wireless devices.
BENEFITS INCLUDE:
Safer for patients; less work for staff Bed and chair pads available One monitor works with two sensor pads Integrates with most nurse call systems A variety of options, including: Call button Pager


In the post pandemic world, we have all seen the effects of supply chain problems with the invasion of Ukraine and other alarming global factors, ever increasing costs of living and other more local issues which have driven up the rate of inflation over the last few years. The impact of this meant that most manufacturers of electronic products had to increase their prices as costs spiralled. This, of course, has impacted the end user. The most dramatic impact has been on the Care Industry. An industry that has lacked the support it desperately needs in these trying times.
Courtney Thorne, at the same time, took a strategic decision to take a close look at our core products, right down to component level, the objective being to make us less vulnerable to future global supply chain issues, and to reduce the cost of each product with the amin of ensuring that we deliver the same high quality product at a cost protected price. We had to ensure that this would happen without jeopardising the superb lev-

els of support we provide to our valued customer base.
This ground up review involved all departments from Research and Development right through to the Field Service team (and everything in-between). This in-depth collaboration took time as we had to ensure that each and every element was refined, perfected and tested to our (and our customers) rigorous requirements.
Whilst many organisations have limited-time or end of product line offers, we are very pleased to announce a price reduction on our core Connect and Connect Health Nurse Call system ranges. With flexible terms, full integration with Care Apps, celebrated service delivery and the most reliable and robust solution now at a new lower price, there has never been a better time to talk to us about a new nurse call system.
For more information email us at: info@c-t.co.uk or see the advert on this page.
Blaucomm’s Nurse Call Messaging Service (NMS) is the market leading solution to remove the dependency on noisy nurse call panels and pagers, through its intelligent software, which delivers the alerts straight to the care staff who need them. Care homes are rapidly introducing smartphones for digital care planning and eMarnow, the same devices can be used to receive the nurse call alerts they need for the residents under their care.
Furthermore, Blaucomm NMS is deeply linked into Person Centred Software MCM, so call bell data is linked straight to care plans. This unlocks a huge benefit to care homes to enhance the staff performance with how they accept and respond to residents, which ultimately promotes better response times and visibility for management to audit their performance.

The best part is that Blaucomm NMS links into your existing nurse call system - we work with all major
brands such as Aidcall, ARM, Courtney Thorne, C-TEC, ENS, Intercall, Medicare, SAS and TeleAlarm.
Care operators are constantly recognising Blaucomm NMS for its reliability and dependability to their care operations, which is why we’ve been chosen time and time again over other solutions.
Head of IT Trudi Harrow at WCS Care had this to say about Blaucomm NMS:
“We find Blaucomm is a genuinely fantastic company with a reliable product.
"We would highly recommend this to anybody who wants to replace expensive pagers and silence those annoyingly loud nurse call screens!”
To find out more about Blaucomm NMS, visit
www.blaucomm.co.uk/healthcare
See the advert page 5 for more details.
Medpage Limited has collaborated with a leading UK manufacturer of crash mats to deliver a cost-effective tool for falls management strategies. The inclusion of the new TumbleCare full-length pressure mat sensor ensures that should a patient tumble out of bed, an alarm signal is generated to alert care staff to the incident, resulting in a recordable improvement to patient safety and service.
Crash mats act as a protective barrier, absorbing the impact of a fall and reducing the risk of serious injuries when a person tumbles out of bed. Beneficial for individuals who are at high risk of falling, such as older adults, patients recovering from surgery, or those with neurological conditions such as epilepsy.

Falls can pose significant risks, especially in healthcare settings and senior care facilities. Every year, thousands of people suffer injuries due to falls from beds and other furniture. To prevent these accidents and ensure the safety of patients and residents, it is essential to implement effective falls and safety management strategies.
Further details can be obtained by telephoning 01536 264 869 or emailing sales@easylinkuk.co.uk
See the advert on page 2 for details.

The care sector faces unprecedented challenges. A growing elderly population with increasingly complex needs, coupled with a shortage of qualified staff, puts immense pressure on care homes. But amidst these difficulties, technology offers a beacon of hope. We at 9Solutions, want to be at the forefront of tackling these issues, providing innovative solutions designed to empower caregivers and enhance the quality of life for residents.
Our location-based solution, with customizable safety zones and realtime alerts, allows for proactive intervention, ensuring resident safety while preserving their independence. Picture a fall occurring in a quiet corner. Instant notifications, pinpointing the exact location, enable staff to respond swiftly, minimizing potential harm.
Efficiency is key in today's demanding care environment. Care home staff are bombarded with alarms, leading to "alarm fatigue" and delayed responses. Our system personalizes alerts, directing them to the right caregiver, reducing workload and improving efficiency. One app manages calls, tracking, and tasks, allowing staff to focus on providing care.

Remote communication tools allow staff to check on residents virtually, reducing unnecessary physical rounds and minimizing disruptions. This frees up valuable time for personalized care and meaningful interactions – the heart of quality caregiving.
We understand that technology should be a support, not a burden. That's why our user-friendly system, developed with care professionals, combines diverse functionalities into a single intuitive platform. This min-
imizes the learning curve, allowing staff to focus on providing exceptional care. Crucially, it also integrates with Care Management softwares, ensuring smooth workflows and easy adoption.
BENEFITS OF 9SOLUTIONS TECHNOLOGY
Reduced workload: Automation and intelligent systems streamline tasks, easing the physical and emotional burden on caregivers.
Enhanced safety: Proactive alerts and location tracking ensure resident wellbeing and peace of mind for families.
Improved efficiency: Optimized workflows and personalized task management empower staff to deliver timely and effective care.
Increased resident satisfaction: Technology fosters independence while ensuring prompt assistance when needed.
The future of care is not about replacing human touch with technology, but about using technology to create space for more of it. It's about empowering caregivers, promoting resident well-being, and reimagining care in a way that prioritizes human connection.
Read more or contact us at www.9solutions.com or sales@9solutions.com

Technology has made people more connected with the world around them and the revolution in assistive care devices has made it possible for the elderly to spend their last years in a comfortable and familiar environment. These devices have also made it easier for home carers to provide quality care for their loved ones while managing their own lives. They allow you to care for your elderly whether they are travelling in the city for errands, staying alone at home, or staying in the same home as you. They are also helping nursing homes provide better care for them with discrete monitoring and quick responses to emergencies.

If you’re looking for these kinds of assistive care devices for your loved ones or nursing home, Frequency Precision produce some of the best systems available to help you with elderly care and mobility monitoring, ranging from bed, chair and floor sensor mats through fall monitoring and GPS tracking to fully integrated nurse call plug or wireless systems.
Phone: 01837 810590
Email: contact@frequencyprecision.com
Website: www.frequencyprecision.com


Since our founding in 2010, Activities to Share has been dedicated to enhancing the lives of those in care by providing thoughtfully designed activity products. Our mission is to support activity coordinators in delivering uplifting, engaging experiences that foster connection, joy, and well-being.
We achieve this by listening closely to your feedback and evolving with your needs. Whether over the phone, via email, WhatsApp, or Live Chat on our website, our team is always ready to offer advice and help you find just the right products to bring your ideas to life.
While we embrace the convenience of technology to expand our resources and share knowledge, we remain firm believers in the irreplaceable power of sensory

Angloplas are a UK manufacturer who specialise in producing dispensers for the health and hygiene industry. Although these are designed to keep the workplace tidy and uncluttered they are, more importantly, built knowing the control of healthcare-associated infections (HCAIs) are a priority for healthcare providers, and who are employing a combination of infection prevention and control strategies, including hand hygiene, cleaning, training and the adoption of new technologies, to tackle the problem. As a result, a wide range of infection control products and technologies are emerging on the market, including antimicrobial technology. Angloplas’ range of dispensers are produced in the world’s first proven Antimicrobial PVC with silver

ion technology and which is exclusive to Angloplas. This helps reduce the risk of cross infection by stopping the growth of bacteria and mould and works continuously for the lifetime of the product, reducing levels of bacteria such as MRSA, E Coli, Legionella, Salmonella and mould by up to 99.99%.
For non-clinical environments Angloplas has recently launched its new Budget Range of products which are made to the same exacting standards as the antimicrobial protected ones but with lower price tags.
You can order Angloplas products directly from its website at www.angloplas.co.uk See page 6 for details.
MOWOOT II – proven solution to chronic constipation without medication
Developed by a team of doctors and other healthcare professionals, MOWOOT II performs gentle abdominal massage to speed up intestinal passage in people experiencing chronic constipation.
Clinically proven, safe and effective, relaxing and sideeffects free, MOWOOT II Abdominal Massage Therapy System combats constipation and provides soothing relief to affected people.

Easy to use and comfortable, the MOWOOT II treats and manages constipation in people with spinal cord injuries, multiple sclerosis sufferers, Parkinson’s Disease patients and people with constipation related to prescription medication. MOWOOT II also helps to relieve idiopathic constipation experienced by menopausal and post-menopausal women
Consort Claudgen’s innovation in the electric heating industry takes another leap forward by introducing Wi-Fi-enabled heaters to their low surface temperature (LST) range. These cutting-edge heaters offer unparalleled convenience and efficiency. The heaters connect directly to Wi-Fi, enabling users to control heating through the digital control panel on the heater or via the Consort Connect app. With a comprehensive 7-day timer, which allows 24 individual heating periods per day, and features such as a lock function, open window detection, and custom automation, users can tailor their heating needs to their preferences. Adding to the ease of use, users can view the
and older and elderly people.
In clinical studies
MOWOOT II increased evacuation frequency, softened stools, improved regularity, reduced gasses, relieved bloating and eased off abdominal discomfort.
10 to 20 minutes daily of relaxing abdominal massage with MOWOOT II rapidly reduces symptoms of constipation. Evident results are experienced only a few days after the first treatment. Regular abdominal massage with MOOWOOT II ensures lasting health benefits and better quality of life.
MOWOOT II – effective solution to chronic constipation for better quality of life!
Supplied by Win Health Medical Ltd - 01835 864866 - www.win-health.com
See page 3 of this issue for other Win Health products.

energy consumption statistics of all connected heaters, providing insights into usage patterns and potential savings. The LST heaters with Wi-Fi and occupancy sensors have a self-learning control ability. They utilise inbuilt occupancy sensors to detect and learn a user’s weekly presence in a room, creating an intuitive heating schedule. When the space is unoccupied, the heater conserves energy by switching to a setback temperature or frost protection mode.
BIM (Building Information Modelling) objects for the heaters are available for download from Consort’s website. 01646 692172 | sales@consortepl.com | www.consortepl.com See the advert on page 6.
engagement. That’s why we continue to make our Reminiscence Kits and Sensory Bags with real, tactile items that stimulate the senses. Some experiences—like popping bubbles for the splash, breathing in a familiar scent, or piecing together a puzzle with others—simply can’t be replicated on a screen. These sensory moments are invaluable in encouraging storytelling, sparking memories, and fostering conversation.
Our values remain rooted in this commitment to meaningful connection. We’re here to partner with you—the professionals on the front lines of care—to create a sense of structure, well-being, and fun for those who need it most.
Are you longing for your activity diary to be full? Look no further www.activitiestoshare.co.uk are here for you! See the advert on page 7 or: customers@activitiestoshare.co.uk
0117 966 6761
07900 6751 50
C&S Seating Ltd have provided postural control equipment to residential homes, hospices, medical equipment services and NHS trust hospitals nationwide since 1991.
With 9 different sizes of TRolls and Log Rolls, in a removable and machine washable Waterproof Titex or Soft Knit material. These rolls are used to control posture and position of the body in either supine or side lying. Our Knee & Leg support wedges are

“Jolly
The new “Jolly Journey” from Little Islands is designed to simulate an old-fashioned travel carriage, featuring real wood panelled wall, brass luggage racks, ornate wall lights and table lamp, opposite-facing seating for four, including cushions, ‘First Class’ antimacassars and period memorabilia.
The Jolly Journey creates a familiar and stimulating environment for ‘passengers’ to return to their fondest memories, sparking conversations of time gone by. Reminisce about travel and holidays with loved ones

and furnish your opulent ‘First Class Carriage pod’ with all accessories and footage. All we require is 2.5M of clear wall space, a power socket and good access, to create your very own Jolly Journey. For more information please contact Little Islands: 01828 869802 or see the advert on page 5.


PASS supports over 1,000 care providers every day, giving them access to market leading care management tools hand in hand with unlimited 24/7/365 support from our dedicated and friendly PASS team.
Assured by NHS Transformation Directorate, PASS provides a secure platform that allows you to plan, record and evidence the care you deliver. The only assured solution built specifically for the home care sector, it provides comprehensive real-time functionality and allows you to share progress against outcomes with customisable, exportable reports.
CARE PLANNING AND ROSTERING FROM A SINGLE PLATFORM
To meet the wider needs of the PASS community All-in-one PASS has recently been launched , bringing advanced rostering functionality to our established digital care planning platform. As a result advanced staff scheduling, payroll and invoicing functionality is now seamlessly linked with care planning and reporting, reducing the technical complexity, risk and overhead associated with integrating two separate systems.
As a result, PASS now provides an all-in-one suite of digital care management tools, available from a single platform, designed to:
Save you time
Increase the efficiency of your teams
Improve the quality of care
Deliver better outcomes
INTEGRATED HEALTH AND SOCIAL CARE
Our commitment to the continual evolution of PASS is further illustrated by the addition of GP Connect. The first product of its type to offer this feature, PASS is still one of only a handful of digital care management solutions to have completed this NHS Digital integration, and is the only one offering it to the home care market. PASS GP Connect provides authorised social care staff with realtime access to their client’s GP records. It makes medical information available when and where it is needed, leading to improvements in both care safety and outcomes:
Visibility of allergies, vaccinations and medications, especially useful for clients unable to reliably share their personal information
Using medical information to inform care planning
Ensuring that the right medication is delivered to the right person in the timeliest manner. In one case, this allowed the administration of antibiotics on a Friday evening, aiding the service user’s swift recovery from infection
Available to all PASS users at no additional cost, PASS GP Connect is significantly more efficient than waiting for a GP response. It’s also a positive step forward on the path to the DHSC’s goal for widespread digitally enabled care and is in full alignment with their ambition for joined up care for everyone.
Get in touch: www.everylifetechnologies.com hello@everylifetechnologies.com
Envivo Group is at the forefront of care and support sector, driving innovation that enables people to live lives full of choices and opportunities. They have 202 locations that are now using Mainteno Facilities Management software.
“Our experience with Mainteno at TLC/Envivo Group has been really positive already. Since its rollout it has shown real and measurable benefits and has had a marked impact on the workload and assurance of our operations team.
"We can now raise issues whether large or minor, almost the instant they are spotted. We can denote the priority with which they need to be tackled and track the progress of works to rectify them. It has reduced almost completely the need to be directly contacting people to resolve issues. It has been obvious that the streamlined approach that it provides helps in prioritising works for maintenance teams and contractors, gives them plenty of detailed information
as to the exact issue and has given us an evidence base to show that issues are resolved in a consistent and effective timeframe.
"The details that are available once a job is logged are invaluable. We can evidence to regulators etc that there are plans to rectify any outstanding works that they may pick up. I've been very impressed with the details that are passed back to me through the platform as works are ongoing and also when they are completed. It's proved to be a valuable reference to ensure that we are not doubling up requests, working through tasks in a logical way and also to confirm the completion of works remotely.
"For a site of our size and complexity especially, a toolkit with this level of effectivity and scope has been an incredible help.”
Group Facilities Manager sales@redro.uk www.mainteno.com





The social care sector is evolving at an unprecedented pace, driven by increasing demand, tightened budgets, and the need to deliver exceptional care outcomes. At the heart of this shift lies digital transformation—a holistic approach to overhauling care operations, processes, and culture through the integration of modern technologies.
Far from simply replacing manual tasks, digital transformation reimagines how organisations operate. Tools like Digital Social Care Records (DSCRs) represent just the beginning. By adopting interoperable systems and cloud-based solutions, care providers can achieve seamless coordination across departments, optimise resource allocation, and ensure high-quality care. Processes such as care planning, rostering, compliance reporting, and data management become more efficient, freeing up teams to focus on providing person-centred care.
Digital solutions also offer significant benefits. Faster service delivery reduced administrative burdens, and more informed decision-making results in better care experiences for service users and care providers alike. For instance, interoperability enables real-time data sharing across platforms, reducing errors while providing a unified view of the organisation’s operations. This empowers leadership to make critical decisions backed by accurate, holistic insights. Additionally, tools like single sign-on (SSO) and multi-factor authentication bolster security, ensuring confidential data remains protected while reducing day-to-day inefficiencies for users.

For social care providers, the move toward digitalisation represents an investment in long-term sustainability. Enhanced efficiency helps reduce operational costs, allowing resources to be reinvested in vital areas such as workforce development or service user engagement. Standardised digital frameworks also simplify the complexities of acquiring new services or locations, ensuring continuity of care during periods of growth. Choosing a digital partner who understands the complexities of care is essential to navigating this transformation successfully and tailoring solutions to the unique needs of the sector.
However, the path to digital transformation requires a clear roadmap. Providers must assess their needs, define a vision, and secure stakeholder buy-in. Selecting the right software and delivering effective training is equally critical to ensuring a smooth transition. Continuous monitoring and adjustment allow providers to refine their approach, fostering a culture of improvement and resilience.
By adopting integrated intuitive software solutions, social care providers can not only stay ahead of industry challenges but also lead the way in delivering exceptional, sustainable services. Digital transformation may not solve every challenge, but its potential to enhance care quality, operational efficiency, and financial health is undeniable.
Visit OneAdvanced at stand H24 at UK Care Week to learn how we can support your journey or download our guide to digital transformation with the QR code.
SFIncS r/3 - A Fee Income System especially for Residential and Nursing Care Homes
Designed to deliver simplicity and ease of use coupled with speed, flexibility and accuracy, SFIncS r/3 (Simple Fee Income System release 3) has a proven track record of over 12 years in use.
Originally developed and prototyped as an MS Access database, since 2017 SFIncS r/3 has lived entirely on the cloud, so is available 24/7 from anywhere in the world.
As a completely bespoke package, born of necessity and collaboration between seasoned software consultants with ties to the care industry, SFIncS r/3 offers innovations and capabilities not found in any other system.
Separation of sponsor and service user responsibilities permits unlimited sponsor/service user relationships, and as any number of charge codes may be defined, this allows complete flexibility of service user/sponsor /charge code definition.
Its unique continuous billing function is the most efficient means possible of defining recurring charges (an entry is only required when a change occurs) and both an ad hoc charge function and a
cashbox module are available for incidental expenses (either or both can be used).
Use of the balance forward accounting principle (which makes unnecessary invoice matching a thing of the past - though invoicing is included) plus super quick receipts entry using just ‘six clicks’ makes SFIncS r/3 almost effortless to use.
Paula, who owns and operates Monkstone House Residential Home in Porthcawl testifies to it’s incredible prowess: “With 41 partly private and partly sponsored service users, some of whom are multiply funded, it takes me only 30 to 40 minutes per week to keep both my accounts and fee income up to date! More importantly, I never need to worry about underpaid or overpaid fees - everything is always spot on. And the invoices and statements produced let me present the polished and professional image I need.”

SFIncS r/3 integrates easily with any accounting package, can be used by any type of care home and by single or multiple home operators alike.
For more information email benjones@intracare.co
Better by Design: A Fee Income System especially for Residential and Nursing Care Homes
We've analysed every aspect of fee income processing to the nth degree and developed a bespoke solution that delivers simplicity and ease of use coupled with speed, flexibility and accuracy – all in one outstanding application package.
SFIncS r/3 is the ultimate fee income management and control system.
• Unlimited sponsor and charge code assignments allow complete flexibility of service user billing profiles.
• Perfect for all types of care homes - Nursing, Residential, Mixed, Specialist.
• Unique continuous billing functionality provides the most efficient charge definition possible. Only charge start points need to be maintained and all sponsor charges for each service user (including historic) are shown on just one screen.
• Completely flexible invoicing. Invoice any sponsor at any time for any charges for any service user for any period of time.
• Super fast receipt entry including ‘Six clicks’ copy functionality.
• Balance forward accounting means you can forget laborious invoice matching.
• Ad hoc charges functionality.
• Cashbox module included.
• Works for multiple or single home operators.
• Integrates with any accounting system.
• Plus all the reports, views and graphs you’ll ever need.
• In use for over 12 years.
• Free training and help with system set up.
• Historic data loading option available (charges may apply).
• 30 day free trial.
For a demo, free trial or for further information please email benjones@intracare.co or visit https://intracare.co/

By Dr Angela Brown, Founder and Chief Executive Officer of Training

several quick and easy changes which the government
could swiftly implement to significantly improve the sector in the shortterm.
A start would be to focus recruitment on the individual progression plan of the care worker. Afterall, surely a sector which traditionally has poor pay and responds to ever changing societal needs, deserves some control over what are perceived are important skills.
The sector still relies on recruitment via word of mouth and offers low pay and low recognition of the skills required in adult care as an incentive. While the workforce needs to respond to the needs of employers, we have a duty to understand the needs of the carer by providing progression of their own career pathway.
The early years sector faced a similar challenge with public perception. Since no one needs a qualification to have a child, it was perceived by many – and even some in government – that the skills required to work in the sector simply came natural.
Although the early years sector has not yet chased all of its demons, public perception of the skills required undertook a change andlargely helped by the excellent Sure Start system - parents began to understand the value of having a skilled workforce to look after our children. It seems an alien concept to us now, but it is very much where we’re at with care, and it doesn’t need to be that way.
In care today, we’re constantly seeing headlines of endemic staff shortages and staff burnout, but this could be significantly improved if the expectations of the sector are proactive rather than responsive.
This is what the Commission may conclude, but in the short-term, we need to invest in the current army of the workforce whose goodwill and compassion is relied upon to respond out of decency rather than an identified societal need.
Demands on the NHS can also only be supported by an adult care sector which is respected for the skills they possess.
For 2025 to herald in some immediate change, let’s utilise Government skills funding and Department of Social Care workforce development programmes to really drive the sector forward.
Let’s find out what the people receiving care really want from their care plan and let them have a say in what the devolved authorities are spending on.
Let’s be ambitious and listen to the sector, use its expertise and plan for a service which not only works well in conjunction with the NHS, but one which is respected and rewarded.
Let’s make 2025 the year we start seeing real change in the care sector.

In the ever-evolving landscape of adult social care, it is essential to ensure that training initiatives not only equip care professionals with the necessary knowledge and skills but also nurture an environment where they feel confident and supported to deliver their best.
As a Registered General Nurse with over two decades of experience in the care industry, I have seen first-hand how thoughtfully designed training programmes can bring about meaningful changes that resonate with both staff and residents. These programmes, when aligned with the real-world needs of care professionals, have the power to transform not only the quality of care but also the overall morale and satisfaction within the care setting.
One of the key features of impactful training is its accessibility, relevance, and applicability to the challenges faced by care staff on a daily basis. From comprehensive first aid instruction to specialised courses on dementia care, well-designed training modules can provide care professionals with the tools and techniques required to respond effectively to a variety of situations. By prioritising the development of our staff's clinical proficiency, we enable them to deliver high-quality, person-centred care that focuses on the well-being and dignity of residents.
However, building confidence and capability goes beyond technical skills alone. It is equally vital to focus on the interpersonal skills that underpin meaningful relationships with residents and contribute to their overall happiness and fulfilment. Training programmes that emphasise relational care, for instance, can help care staff appreciate the importance of creating an atmosphere of trust and understanding. By
encouraging staff to focus on these human aspects of care, we cultivate a setting that radiates warmth and kindness, ensuring that residents feel valued and respected.
Moreover, to ensure that staff can consistently provide the best possible care, our training must remain adaptable and responsive to emerging trends and best practices in the sector. By implementing regular refresher courses, we reinforce foundational knowledge, address any skill gaps, and ensure that care professionals are up to date with the latest advancements. Similarly, ongoing supervision and performance evaluations play a vital role in identifying opportunities for professional growth, creating a framework of accountability and continuous development. This commitment to lifelong learning not only enhances the quality of care but also reinforces a sense of purpose and pride among staff.
The ripple effect of robust training programmes extends far beyond individual care professionals. When staff feel confident, valued, and well-equipped, they are better positioned to deliver exceptional care that is tailored to the unique needs and preferences of each resident. This, in turn, results in improved well-being for residents, greater peace of mind for their families, and stronger outcomes for the care community as a whole.
At the core of our training philosophy lies the understanding that empowered staff lead to empowered residents. When care professionals are equipped with the knowledge, skills, and assurance to excel in their roles, they are better able to encourage residents to maintain their independence, involve them in decision-making, and take the time to truly listen to their stories and concerns.
In conclusion, aligning training with the practical needs of both staff and residents goes far beyond fulfilling regulatory requirements—it is the foundation for fostering confidence, compassion, and excellence in adult social care. As we look ahead to the challenges and opportunities of the future, let us remain steadfast in our commitment to investing in our staff, enabling them to make a lasting difference in the lives of those they care for.
By Elena Martin, Director
of
Operations
and Commissioning, Langdale Care Homes Group (www.langdalecarehomes.co.uk)
By Daniel O’Shaughnessy,

You wouldn’t run a care home without a health and safety lead, and the same should apply to data security and protection leads. Losing access to critical data, even briefly, can be devastating for residents’ welfare and your business’s viability. If care plans and medication records are unavailable due to a cyber incident or software issue, residents’ wellbeing is at risk.
Finance system failures can disrupt payroll, invoicing, and payments.
While data protection is everyone’s responsibility, having a named individual to lead on data security and protection is essential. This role provides senior leadership and ensures good practices are followed across the organisation. At Digital Care Hub, we use the term data security and protection lead to describe this role.
The lead should champion data security policies and set an example. While daily tasks can be delegated, the lead ensures standards are met. This role doesn’t have to fall to the Registered Manager but should be assigned to someone senior enough to oversee responsibilities effectively. In larger organisations, aspects of the role can be shared – for instance, one person might manage risks while another handles information governance.
It’s vital that leads have the right knowledge and skills. To address training gaps, Digital Care Hub’s Better Security, Better Care programme has launched a free, open-access elearning course tailored for data security and protection leads. This complements an existing course for all staff, which we recommend completing first.
The course, launched in January 2025, supports continuing professional development (CPD) and meets the training requirements of the Data Security and Protection Toolkit (DSPT). It is the only free resource designed specifically for this role in adult social care.
The training reflects real-world scenarios across care homes, supported living, home care, and community services, covering all client groups. The course includes four modules:
1. Data protection rights and responsibilities
Covers the lead’s responsibilities, other specialist roles, and key skills and
support needed for the role.
2. Keeping data secure
Explores managing data, understanding personal data rights, access to data, Information Asset Registers, and Data Protection Impact Assessments.
3. Threats to data security
Focuses on recognising, preparing for, and recovering from cyber incidents; reducing threats to digital systems, devices, and supply chains.
4. Data breaches
Explains how to differentiate between breaches, incidents, or near misses; record and learn from incidents; and respond to and report breaches appropriately.
By completing this course, data security and protection leads will enhance their knowledge of data protection and cyber security, ensuring they can safeguard their organisations, staff, and the people they support.
For more information about the course and other resources, visit www.digitalcarehub.co.uk/elearning.


Leanne Silverwood is the Founder and Managing Director of Local
Care Force

As Local Care Force celebrates 20 years of business, we look back on two decades of momentous changes in the health and social care sector. From technological advances to ongoing recruitment and retention issues, supply chain management companies driving down prices and quality, and changes to the agency landscape, the health, and social care sector, post-pandemic, has not only had to adapt but has also needed to rise to meet these challenges.
In 2020 the health & social care sector faced a devastating crisis in Covid19.
Care home staff were under unimaginable pressure, working long hours, managing PPE shortages, and the emotional toll of caring for residents who were isolated from their families. We had to adapt quickly, deploying staff where they were most needed, while maintaining their safety, and that of the residents they cared for. It demonstrated the resilience and dedication of our workforce - and we are so incredibly proud of the commitment they showed throughout this difficult time.
Post pandemic the issue of recruitment worsened. In 2023 the health & social care vacancy rates stood at 152,000 roles (9.9%) substantially higher than the overall UK rate of 3.4%. It was a challenging time, to say the least. Alongside issues around recruitment, were problems with retention which significantly impacted the health and social care landscape, with 390,000 (28.3%) leaving the sector in 2022/23. (The Kings Fund 2024).
As a health & social care agency, Local Care Force has been at the forefront of this ongoing crisis. The ever-growing demand for qualified healthcare professionals has proven to be a difficult obstacle to over-
come. Our role in providing experienced, skilled, and compassionate staff has never been more critical, or difficult, and it is the reason we offer specialist in-house training led by our clinical lead nurse, who also acts as a mentor to our team.
The agency sector has not been immune to challenges post-pandemic. In the past, agencies were regulated by the CQC, but for several years now, they have been unregulated. This lack of oversight has led to a surge in "back bedroom" agencies, which supply staff without conducting the necessary checks to ensure resident safety. Additionally, these agencies often disregard tax regulations when paying staff, leaving care homes liable for tax shortfalls. Consequently, we advise all clients to question any £14 hourly carer charges, as it has become easier for anyone to recruit and place nurses in care homes. This trend is particularly concerning, as we pride ourselves on our robust recruitment and safeguarding processes to ensure the wellbeing of the residents our staff support.
The Work Rights Centre report has highlighted another troubling issue within the industry: the flawed sponsorship visa system and the exploitation of foreign workers in the health and social care sector.
Migrants constitute 32% of care worker roles in England, many of whom face excessive hours or underemployment, struggling to change visa sponsorship, and fearing reprisals if they voice their concerns. As an agency, we cannot recruit staff requiring visas. However, we are disheartened to see hundreds of people on sponsorship visas applying for work with us due to unscrupulous agencies exploiting legal loopholes. We frequently hear from individuals who aren't receiving enough work from their sponsors to sustain themselves, yet they cannot legally work elsewhere without invalidating their visas. The well-being of our workforce has always been paramount at Local Care Force. We firmly believe that protecting our staff, which in turn, protects the residents they support, a principle on which Local Care Force prides itself.
As we reflect on our two-decade journey, acknowledging the significant challenges we have faced, it's equally important to celebrate the positive advances we have made during this time.
We know that with dedication, collaboration, and a focus on innovation, we can continue to weather the storm. As we celebrate this milestone, we are committed to providing the highest standard of care and supporting the health & social care sector in whatever challenges the next 20 years may bring.
The delivery of safe care is the paramount responsibility of social care providers. Central to achieving this is the governance framework adopted by service providers. And at the core of this framework are policies and procedures. These enable the provider to comply – and evidence compliance – with relevant legislation and regulations, as well as facilitating best practices, supporting business needs, and assisting in recognising and managing risks.
Providers have a legal duty of care to the people they employ. Policies and procedures should provide clear guidelines to staff on how the organisation operates, as well as informing them of best practices and processes to be followed.
Policies should be reviewed annually as a minimum to ensure they are still fit for purpose and align with legal and regulatory requirements. They should be reviewed not only by employees of the business, but also by experts in various subject matters (e.g.,

infection control or medicines management).
For many small- to medium-sized providers, there may not be the in-house skills, knowledge, and experience to complete such a robust annual review. Many choose instead to purchase their policies and procedures from a reputable provider like W&P Compliance & Training, who will also complete reviews and ensure their policies and procedures remain up to date. This way a provider not only ensures they remain compliant; they also benefit from best practice policies and procedures that provide a solid foundation for safe working practices and – ultimately – protect and support service users and staff.
Ben Erskine – Director at W&P Compliance & Training www.wandptraining.co.uk | Tel: 01305 767104 See the advert on page 2 for further information.
Training care home staff is vital for delivering high-quality care, especially when managing complex resident needs such as dementia, frailty, and mental health challenges. However, traditional methods often fall short in engaging staff, leaving critical gaps in understanding and preparedness. Innovative approaches, such as game-based learning and peer-to-peer collaboration, are revolutionising training, particularly in addressing the ethical and legal challenges of restrictive practices.
Restrictive practices—measures that limit an individual’s freedom—are sometimes necessary to ensure safety. However, they must be applied with great care, adhering to legal frameworks and ethical guidelines to protect residents’ dignity. A groundbreaking digital training resource, codesigned by Queen’s University Belfast and Focus Games, exemplifies this innovation. The resource uses interactive, expert-driven content to help staff navigate restrictive practices responsibly and effectively.

Game-based learning plays a central role, transforming topics like restrictive practices into engaging,
real-world scenarios. Simulations allow staff to explore ethical dilemmas, practice decision-making, and test alternative solutions in a safe, low-pressure environment. This approach enhances critical thinking, teamwork, and retention of essential knowledge.
Peer-to-peer learning further strengthens the training by encouraging staff to share experiences and insights, fostering collaboration and practical problem-solving. This creates a dynamic learning environment where staff feel supported and empowered to deliver compassionate care. By integrating these modern approaches, care homes can elevate training into a meaningful experience, equipping staff to balance safety with residents’ autonomy and dignity. At Focus Games, we are proud to offer tools designed to empower care home teams through innovative training. Visit www.FocusGames.com or email info@focusgames.com to learn more about our Restrictive Practice resource and how it can enhance care home outcomes for
At Meaningful Care Matters, we have the privilege of working with health and care teams across the UK, Ireland, Canada, Australia and more recently Singapore.
It is no surprise that those who can embrace the culture change of our ‘Butterfly’ and ‘Dragonfly’ Approaches - in terms of reducing the institutional and task-focused aspects of care in favour of creating a sense of fun, friendship and true belonging - have leaders who are very self-aware and emotionally intelligent. What does that look like in practice? It involves being genuine as a person, being able to acknowledge mistakes, and taking time to really get to know your team members as individuals and what makes them tick. Our team are Authorised Partners in delivering the methodology of the DiSC personality profiling assessments and the Five Behaviours of a Cohesive Team™ programme (Lencioni, P) to help support teams to work together more positively and ultimately productively. Having been through the process myself, it was striking how accurate the analysis was of what motivates and what stresses me. It also helped me to know those stressors and motivators for my peers and how to adapt my approach to better look out for each other.

our own relationship with trust, based on experiences in our lives? Do we find it easy, or does it take us time? Being in touch with your own vulnerability is not about spilling out all your deepest, darkest secrets to the people you support! But it is about being able to reflect on times in your life when you have felt lonely, scared or lost, and for these reflections to enhance our empathy for those who are struggling. Once we have established trust and a sense of belonging in our teams, we can more easily be open about the things we disagree about, and for those differences or conflicts to be regarded as healthy rather than threatening to the stability of a team - provided they are talked about openly and kindly. Many teams flounder because there is an artificial harmony i.e. conflicts are under the surface and gossip and cliques can create an unsafe and unhappy work culture.
A recent social media post caught my eye which said “Your company culture is not words on your website or posters on the wall. It’s how your people feel on a Sunday night.”
What is your response to that question, and do you think you and your team might need some time and attention in 2025 to get back on track and unlock your full potential?
People working in care homes often experience the deaths of residents but this doesn’t mean each death is easier to cope with.
Hospice UK’s Compassionate Employers Programme deliver workshops to help care professionals manage recurring and often overlooked experiences of grief through their work.

Our next virtual session will be on: Wednesday 5 March 2025, 10.00 - 12.30
The cost is just £120 +VAT per person.
At the foundation of a good team is what Patick Lencioni describes as vulnerability-based trust, and this is something we talk about a lot in training for leaders and their teams. People who we care for, and their families put a lot of trust in us. So, what is
Sally Knocker is a Consultant Trainer with Meaningful Care Matters www.meaningfulcarematters.com

Book your space or find out more at: www.hospiceuk.org/coping-professionalgrief-workshop-march

In a landmark ruling, the High Court delivered a significant judgment on 14 January 2025, in favour of Hartford Care Group Limited (HCG), challenging the Secretary of State for the Home Department's (SSHD) decision to reject HCG's application for 70 Defined Certificates of Sponsorship (DCoS). This case, The King (on the Application of Hartford Care Group Limited) v. The Secretary of State for the Home Department, sets a crucial precedent for how the Home Office assesses applications for Defined Certificate of Sponsorship (DCoS), particularly in the care sector.
THE CASE BACKGROUND
HCG, a prominent provider of care services in the UK, has held a sponsor license since April 2019. On 8 January 2024, Aston Brooke Solicitors applied for 70 DCoS on behalf of HCG. These certificates are vital for nonUK workers to obtain a visa to work in the UK. However, on 29 January 2024, the SSHD rejected HCG's application, citing insufficient evidence to demonstrate a genuine need for additional staff.
Aston Brooke Solicitors swiftly initiated a Judicial Review, challenging the legality of the decision, which could have significant consequences for the care sector, heavily reliant on overseas workers to meet staffing demands and stating HCG contracts with their service users and the Local Authority did not state the number of hours.
THE LEGAL CHALLENGE
Aston Brooke Solicitors argued that the SSHD’s decision was unlawful, irrational, and inconsistent with the Immigration Rules. Aston Brooke Solicitors contended that the Home Office had imposed requirements not set out in the rules, relied on unpublished policies, and failed to assess the evidence properly. In particular, the SSHD insisted on receiving contracts that guaranteed specific hours of work, which Aston Brooke Solicitors argued were not standard in the care sector.
The SSHD defended its position by stating that additional information could be requested to validate the applications THE ADMINISTRATIVE COURT'S RULING
"23 years, operating 4 Devon Nursing homes, has been pretty tough, as anyone in social care, knows, only too well. And if it was hard already, after 2024 budget, it's just got harder.
Anyway, at heart, I am just customer of Eden Alternative, and it was a stroke of luck to come across this whilst on holiday in New Zealand in 2009. It started in USA in 1994 and now runs in 22 countries.
The fact that I am now involved with this not-forprofit organisation (in the UK area) came about when one of the 2 main UK directors died suddenly just before Covid. But it's something I have run with for 11 years to help make 'vision' a reality, not a struggle. So,
On 14 January 2025, the High Court ruled in favour of HCG, stating that it was irrational for the SSHD to require contracts with guaranteed hours to prove the genuineness of care worker vacancies. The Judge highlighted that flexible contracts are standard in the care sector, where the demand for staff can vary depending on factors such as local authority funding and service user needs.
The Judge also criticised the SSHD’s assumption that local authorities impose staffing quotas, pointing out that care providers have discretion over how many workers they need to meet demand. Furthermore, the Judge found that HCG’s evidence adequately demonstrated the genuine need for additional staff, rendering the SSHD’s rejection of the application irrational.
The Judicial Review application was supported by Care England and Professor Martin Green OBE chief executive of Care England stated after the verdict was delivered: “In winning the Judicial Review, Aston Brooke Solicitors has done a great service to the care sector because this victory will cause The Secretary of State for the Home Department to rethink how they behave towards the independent care providers. No one should be in any doubt that when we see unacceptable behaviour, we will be prepared to challenge it and use the law to enforce our rights.”
Gemma Melhuish, People and Culture Director at HCG said: “We are thrilled the court ruled in our favour and agreed their decision was unlawful as it is important for other Care Providers to challenge decisions that are morally not correct. We are now looking forward to welcoming new starters to our Homes from our overseas recruitment campaign undertaken last year and continuing to provide high-quality care to our residents. “
THE OUTCOME AND ITS SIGNIFICANCE
The High Court granted a quashing order of the SSHD’s decision, declaring it unlawful. Aston Brooke Solicitors will now reapply for the DCoS for HCG without the commercial risks associated with the initial rejection.
being both a customer and helping the admin seems quite natural.
It is a modern philosophy of care, but moreover, it's a programme that is straight forward, tried and tested for 30 years and really works.
Its member care organisations generally become trainers for their own teams, and run it themselves.
The programme is run in person over 2-3 days or online 1 hr a wk for 7 weeks. You choose.
It addresses loneliness, helplessness and boredom and operates through 10 principles to underpin 7 critical domains of wellbeing.

Moreover, it's effective, transformational and really works. As residents, and team members wellbeing, matter so much , it's a must, in my opinion.
Geoffrey Cox Southernhealthcare.co.uk eden-alternative.co.uk"

Kashif Majeed, Head of Corporate Immigration at Aston Brooke Solicitors said, “For the care sector, the decision has significant implications. It emphasises that the Home Office must assess applications based on realistic criteria that reflect the sector's operational practices. While the SSHD can request additional information to verify the authenticity of job vacancies, it cannot impose unreasonable or unattainable requirements, particularly when those conditions do not align with the realities of the care sector.”
THE BIGGER PICTURE: IMPLICATIONS FOR THE CARE SECTOR
This case highlights the essential role that international workers play in the UK’s care sector, especially in light of the growing demand for care services due to an aging population. The judgment provides clarity for care providers seeking to hire overseas workers, reassuring them that their flexibility in staffing and contractual arrangements will be recognized.
The ruling also sets a precedent for future DCoS applications, ensuring that care providers are not burdened with unrealistic requirements. This decision affirms that decisions made by the SSHD must be grounded in the reality of the care industry, where staffing needs are often dynamic and flexible.
The King (on the Application of Hartford Care Group Limited) v. The Secretary of State for the Home Department is a major victory for the care sector, ensuring that the Home Office’s decision-making process is fair and aligned with the sector’s operational realities. The case reinforces the importance of reasonable and consistent policies in assessing DCoS applications and provides a vital precedent for care providers looking to hire international workers to meet the UK's growing care needs.
For further information on Ashton Brooke see the advert on the facing page.
Global assists clients throughout the U.K. who specialise in the healthcare sector to achieve their objectives of purchase, development and refinance.
We have organised over £1.8bn for clients in the past 30 years, providing clients with competitively priced funding to refinance existing debt, ease cashflow and develop businesses further.
From helping clients make their first purchase through to allowing groups to
grow significantly in size we assist at every stage of your business expansion. Every proposal is individual and deserves to be treated that way, so we hope you will allow us to be of assistance to you and call us to chat through your plans and requirements, I am sure we will be able to tailor a facility to your requirements.
Call us on 01242 227172 or e-mail us at enquiries@globalbusinessfinance.net


• Sponsor Licenses
• Skilled worker Visas ( Carers, Senior Carers, Nurses)
• Commercial Property, Leases, Developments, Sales & Acquisitions
• Commercial contracting & negotiating with Local Authorities regarding fees
• Refinancing
• Partnership agreements
• Dispute Resolution & Litigation
• Advice on Care Quality Commission (CQC) processes
• Assisting Care Providers to make License Applications, Registrations and Representation with CQC
• Wills, Probate & LPAs

