MATTERS HEALTH 2023























2




Can you stop an overdose death?
Updated guidelines may help.
Breast cancer FAQ 3




























































































































A psychiatrist explains the neuroscience and physiology of fear 6
How anxiety works in the brain
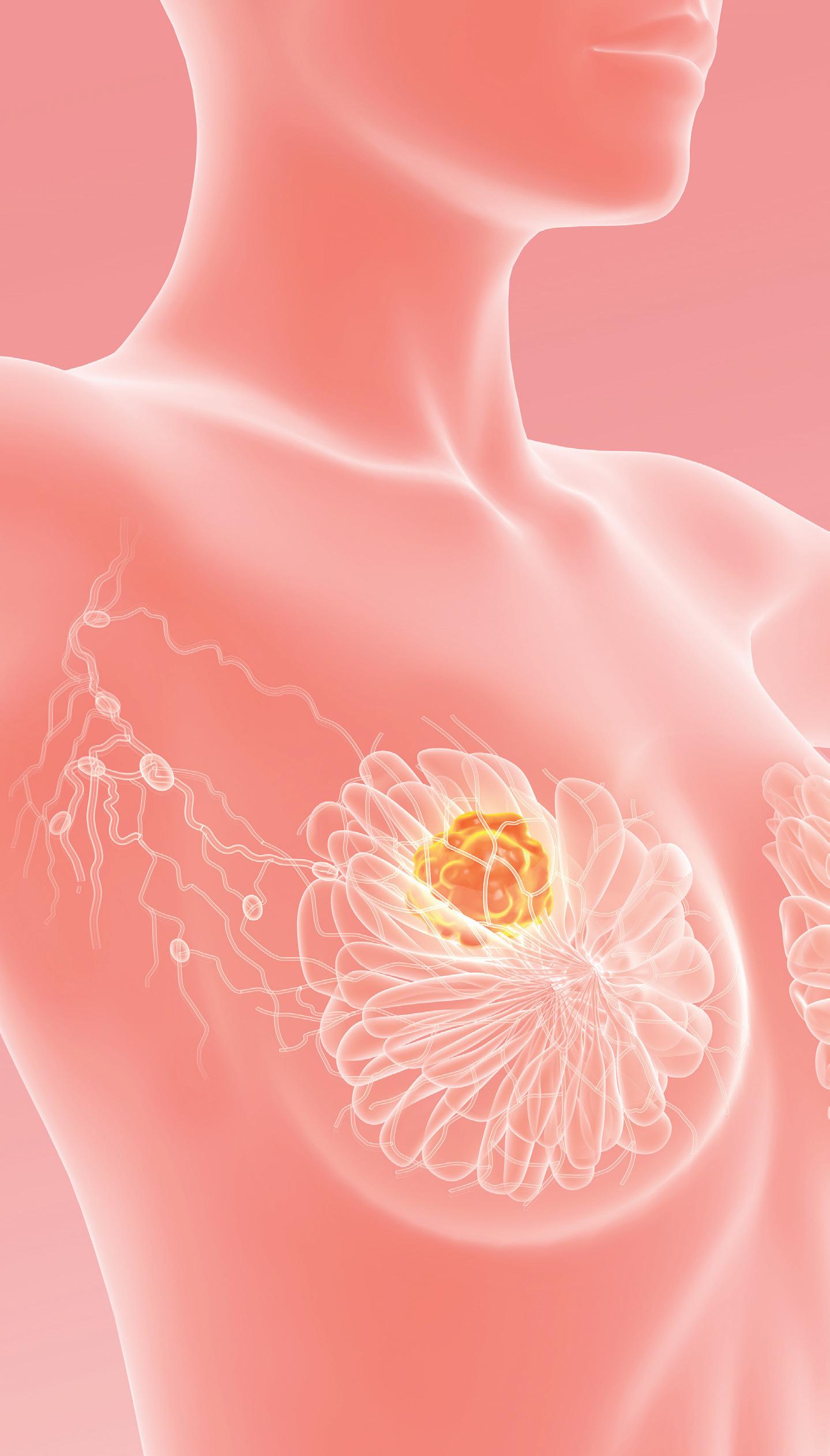
What distinguishes the different types of breast cancer? 8









Healthy habits that could help women reduce their breast cancer risk




Cancer is a formidable disease that the World Health Organization reports is the leading cause of death worldwide. Figures vary, but organizations such as the WHO and the American Cancer Society estimate that around 9.5 million people die from cancer every year.


No type of cancer causes more deaths in women across the globe than breast cancer. Though the five-year survival rate for breast cancer patients has increased by a significant margin in recent decades, a 2019 study published in The Asian Pacific Journal of Cancer Prevention reported a significant increase in breast cancer mortality rate in the 25-year period preceding the study. The researchers
behind the study theorized that the spike in mortality rate could be due to an increase in incidence and prevalence of breast cancer. Like all cancers, breast cancer cannot be prevented. However, various healthy habits could help women reduce their risk for the disease.
• AVOID ALCOHOL. The ACS reports that alcohol consumption is a clear risk factor for breast cancer. Risk increases with the amount of alcohol a woman consumes. For example, a woman who consumes one alcoholic drink per day has a 7 to 10% higher risk of getting breast cancer than a woman who abstains from alcohol. Drinking two to
three drinks per day could increase risk by around 20%.
• ESTABLISH AND MAINTAIN A HEALTHY WEIGHT. Being overweight or obese increases breast cancer risk, particularly among postmenopausal women. According to the ACS, after menopause women get most of their estrogen from fat tissue. Fat tissue increases estrogen levels in the body, which in turn increases a woman’s risk for breast cancer. Elevated levels of insulin in the body, which is common among individuals who are overweight, also has been linked to higher breast cancer risk. Establishing and maintaining a healthy weight cannot prevent breast cancer, but

it can help women reduce their risk for the disease.

• MAINTAIN A PHYSICALLY ACTIVE LIFESTYLE. A sedentary lifestyle increases a person’s risk for various conditions and diseases. Women who live such a lifestyle are at elevated risk for breast cancer. The ACS notes that sedentary behavior such as sitting, lying down, watching television or engaging with screen-based forms of entertainment that do not require physical activity can increase breast cancer risk, especially for women who spend most of their work day sitting down. A more physically active lifestyle that includes routine exercise can help women reduce their breast cancer
risk.
• ADOPT A NUTRITIOUS DIET. Eating right is another way for women to reduce their breast cancer risk. Vegetables, fiber-rich legumes such as beans and peas, fruits across the color spectrum and whole grains are some components of a healthy, nutrient-rich diet that can help lower breast cancer risk. Women also can avoid certain foods, such as red and processed meats and refined grains, to lower their breast cancer risk. Though there’s no guaranteed way to prevent breast cancer, women can embrace various healthy habits to lower their risk for the disease.
D1 | OCTOBER 7- OCTOBER 9, 2023 2023 HEALTH MATTERS THE SUMTER ITEM
Can you stop an overdose death?
 By Michael Merschel American Heart Association News
By Michael Merschel American Heart Association News













in this. You don’t have to manage patients with these guidelines in a vacuum.”


Lavonas said that in his emergency room, most of the overdose patients he treats have been rescued by someone who was trained in naloxone and had it on hand. “Unfortunately, some people who use opioids by themselves, or use opioids where someone’s not there to help, don’t survive to see me.”
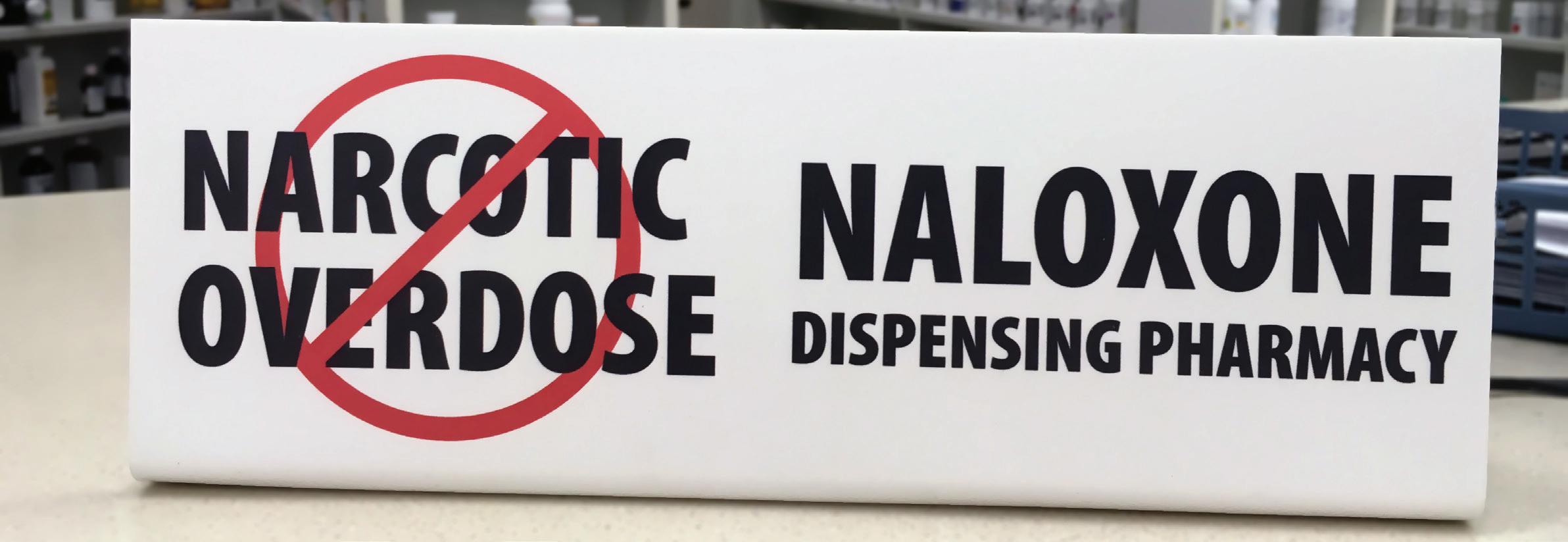
Saving lives after an opioid overdose isn’t just the job of emergency department workers, according to guidelines on how to treat heart-stopping poisonings.
Opioids are just one of the substances addressed in the updated American Heart Association guidelines. But the threat posed by overdoses from such drugs, particularly fentanyl, is immense, said Dr. Eric Lavonas, professor of emergency medicine at Denver Health and the Rocky Mountain Poison and Drug Center.
“Opioids kill more Americans than all other poisons together by a lot,” said Lavonas, who led the expert panel that wrote the updated guidelines, published in the journal Circulation.
“They kill more Americans than motor vehicles, and the death rate keeps climbing. It’s getting insane.”
The guidelines address substances that cause cardiac arrest, when the heart suddenly stops beating.
Although the update affirms much of the previous science on the topic, it’s the first comprehensive review since 2010, Lavonas said. It includes recommendations for the treatment of 12 common types of poisoning, including drug overdose, chemical exposure and drug interactions. It also offers guidance on when to use the latest life-sustaining technology to help patients “whose hearts are so badly affected by a poison that they otherwise could not sustain life,” he said.
That technology, called ECMO, is the most important new advance in the treatment of poisonings, Lavonas said. ECMO, which stands for extracorporeal membrane oxygenation, pumps blood when the heart is unable to do so, buying time for the poison to leave the body.
Although primarily available in large medical centers, he said, it’s saving lives. Earlier this summer, Lavonas helped take care of a young woman who had overdosed on an antide-
pressant. “Despite every antidote in our arsenal, she was in shock and dying. We were able to mobilize an ECMO team, who supported her blood pressure for several days while her liver metabolized the toxin. She is now home from the hospital, fully recovered.”
But a doctor might encounter a life-threatening overdose of that particular drug once every few years, Lavonas said. By contrast, he treats someone for opioid overdose almost every emergency room shift. “On many shifts, it’s multiple,” he said.
The new guidelines reflect the fact that opioid overdoses are becoming common enough to upend traditional thinking about cardiac arrest patients, said co-author Dr. Maryann Amirshahi, a professor of emergency medicine at Georgetown University School of Medicine in Washington, D.C.
“A lot of these patients have healthy hearts,” said Amirshahi, who also is an emergency medicine physician at MedStar Washington Hospital Center and a medical toxicologist for the National Capital Poison Center. “A clogged artery isn’t their primary pathology. They stopped breathing because of an opioid, and that caused their heart to stop.”
The guidelines note that in the 12-month period ending in April 2021, more than 75,000 people in the United States died from an opioid overdose, which makes it the leading cause of cardiac arrest due to poisoning in North America.
According to a study published in July in JAMA Network Open, as of 2021, accidental opioid overdoses caused 1 of every 22 U.S. deaths. Opioid overdoses were responsible for 1 in 10 deaths of people ages 15 to 19 and more than 1 in 5 deaths among those ages 20 to 39.
Patterns of drug abuse vary by city, said Amirshahi, whose medical system covers Baltimore and Washington. In her D.C. hospital,
she’s seen opioid overdoses grow in relation to other drugs over the past five years to the point that she sees an overdose every shift she works.
In Denver, the primary problem is fentanyl, Lavonas said. People with addiction seek it out instead of heroin, and fentanyl shows up in counterfeit pills that are sold as oxycodone or ecstasy.
Victims can turn up anywhere, he said. “You can go to the bathroom in a department store, and maybe that person in the stall next to you is passed out. I came upon someone when I was driving to the bank, and he had passed out in a car. These situations are so common that any person who moves about in our society may run into someone with an opioid overdose and have the opportunity to save a life.”
Which is why everybody needs to be prepared, Lavonas said.
“Every teenager and adult should know how to perform CPR, use a defibrillator and administer naloxone,” Lavonas said.
If you find someone passed out and unresponsive, he said:
– Call 911.

– If the person is not responding and not breathing normally, start CPR.
– Have someone get an automated external defibrillator, or AED, if one is available.

– If you have reason to think opioids might be involved, get and give naloxone.
– Continue CPR, including using the AED, until help arrives.
The primary reason somebody has a cardiac arrest from an opioid overdose is that they stopped breathing, Amirshahi said. Naloxone is now an overthe-counter medication that temporarily reverses the effects of opioids. It can restore breathing, and it may make the victim more awake and alert.
Naloxone is sold overthe-counter as an auto-


matic injector or as a nasal spray, and is easy to administer, Lavonas said. “Our Denver public librarians save lives with naloxone on a regular basis. Both my teenage kids carry naloxone in their school bags, just in case.”
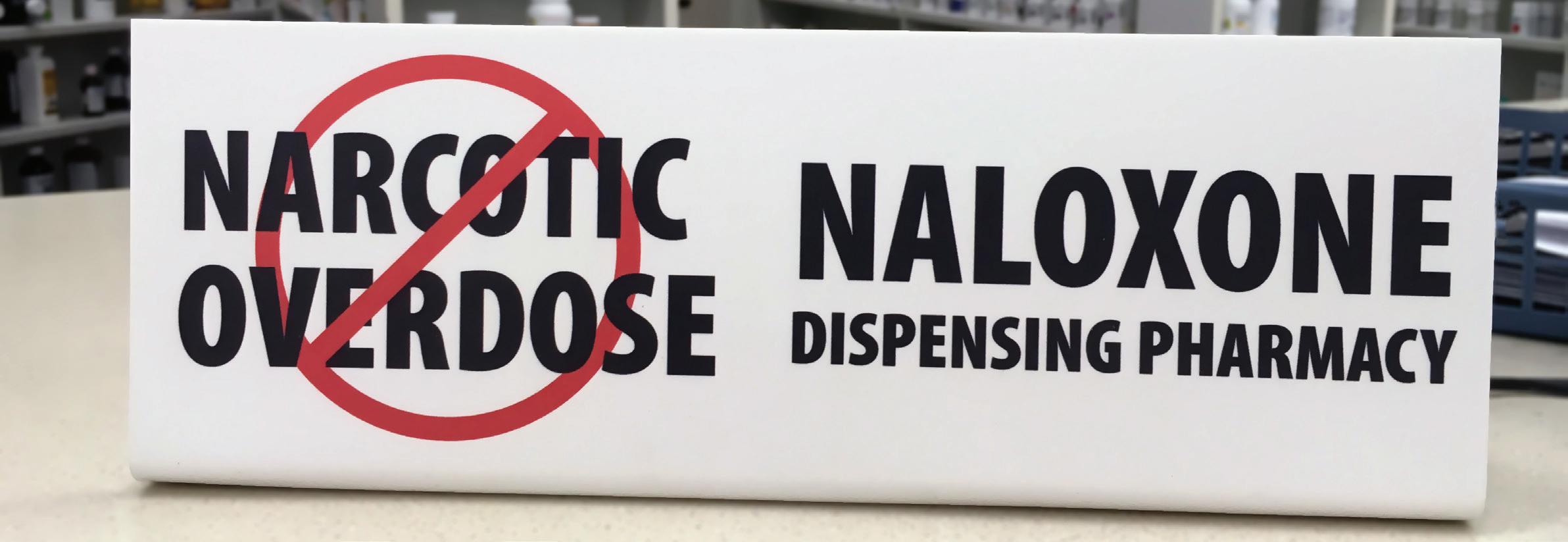
Amirshahi said that although it might not be practical for everyone to carry naloxone, she wants it to be widely accessible. “I think that we should really push to have it more in public places, because you never know where you’re going to need it.”
She emphasized the importance of starting CPR before seeking out naloxone if the patient is believed to be in cardiac arrest. “Once the heart stops, the naloxone doesn’t help.”
The guidelines note the importance of fast action and educating friends, families and close contacts of people at risk of opioid overdose. That would include people taking opioids legally to control pain. But, Amirshahi said, it’s important for people to be willing to dial 911 even if illegal drugs are involved.
Lavonas personally would like to see naloxone treatment worked into all CPR training. Meanwhile, he said, training on naloxone is offered by community groups across the country. Information can be found online through the Centers for Disease Control and Prevention, state health departments and elsewhere.
As a toxicologist, Amirshahi said doctors should be willing to ask for guidance, too – either from a regional center or from an expert colleague. “Please call us,” she said. “We have tremendous expertise
Which is why more people need training –urgently, he said. “Opioid poisoning is so common that everyone should be prepared.”
In a 12-month period ending in April 2021, more than 75,000 people in the United States died from an opioid overdose
By the numbers
Accidental opioid overdoses caused 1 of every 22 U.S. deaths
Opioid overdoses were responsible for 1 in 10 deaths of people ages 15 to 19
Opioid overdoses were responsible for more than 1 in 5 deaths among those ages 20 to 39.
D2 | OCTOBER 7- OCTOBER 9, 2023 2023 HEALTH MATTERS THE SUMTER ITEM
Updated guidelines may help.
117 S Brooks StreetManning, SC 29102 OPEN ENROLLMENT Medicare Oct. 15–Dec 7 Healthcare Marketplace 65 & under Nov. 1–Jan. 15 803-775-1168 CRWINS.COM 25 E. Calhoun Street Sumter, SC 29150 Devin Rice
BREAST CANCER FAQ































The World Health Organization reports that roughly 2.3 million women were diagnosed with breast cancer in 2020. By the end of that year, there were nearly eight million women alive who had been diagnosed with the disease in the previous half decade.





A breast cancer diagnosis inevitably leads to questions about the disease. The bulk of those questions undoubtedly are asked by the millions of women who are diagnosed with breast cancer. But millions more individuals, including friends and family members of recently diagnosed women, may have their own questions. Women can discuss the specifics of their diagnosis with their physicians. In the meantime, the following
are some frequently asked questions and answers that can help anyone better understand this potentially deadly disease.

What is breast cancer?

Cancer is a disease marked by the abnormal growth of cells that invade healthy cells in the body.

Breast cancer is a form of the disease that begins in the cells of the breast. The National Breast Cancer Foundation notes that the cancer can then invade surrounding tissues or spread to other areas of the body.


Can exercise help to reduce my breast cancer risk?
The NBCF notes that exercise strengthens the immune system and women who commit to as little

as three hours of physical activity per week can begin to reduce their risk for breast cancer. However, even routine exercise does not completely eliminate a woman’s risk of developing breast cancer.
Is there a link between diet and breast cancer?
The organization Susan G. Komen®, a nonprofit source of funding for the fight against breast cancer, reports that studies have shown eating fruits and vegetables may be linked to a lower risk for breast cancer, while consuming alcohol is linked to an increased risk for the disease.
In addition, the NBCF reports that a high-fat diet increases breast cancer risk because fat triggers estrogen production that can fuel tumor growth.
Is there a link between oral contraceptives and breast cancer?



The NBCF reports that women who have been using birth control pills for more than five years are at an increased risk of developing breast cancer. However, the organization notes that risk is very small because modern birth control pills contain low amounts of hormones.
Can breastfeeding reduce breast cancer risk?


Breastfeeding and breast cancer are linked, though the NBCF notes that the role breastfeeding plays in lowering cancer risk depends on how long a woman breastfeeds. The World Cancer Research Fund International notes that evidence indicates that the greater number of
months women continue breastfeeding, the greater the protection they have against breast cancer.
Is there a connection between stress and breast cancer?
The NBCF notes that researchers have found that traumatic events and losses can alter how the immune system functions, which can provide an opportunity for cancer cells to establish themselves within a person’s body. The NBCF urges women to identify ways to keep their stress levels in check. Breast cancer education can be a valuable asset as women seek to reduce their risk for the disease.
HERE FOR LIFE Did you know?
When facing a cancer diagnosis, it is important to put yourself in the right medical hands. Home to the region’s only nationally accredited comprehensive cancer program, our top cancer specialists, cutting edge and targeted treatment options, and compassionate support services provide everything you need to fight cancer McLeod Health is Here for Life. while remaining close to home.
McLeod Center for Cancer Treatment and Research
McLeodCancer.org








Family history is considered a risk factor for various diseases, and breast cancer is no exception. According to Cancer Research UK, having a fi rst degree relative, which includes a mother, sister or daughter, diagnosed with breast cancer approximately doubles a woman’s risk for breast cancer. However, the American Cancer Society notes that only about 5 to 10% of breast cancer cases are thought to be hereditary. Hereditary cases of breast cancer are those that result directly from gene mutations passed on from a parent. The relatively small percentage of hereditary cases is important to note, as it means that the vast majority of women who are diagnosed with the disease have no family history of breast

THE SUMTER ITEM 2023 HEALTH MATTERS OCTOBER 7 - OCTOBER 9, 2023 | D3





















































































































































































































































D4 | OCTOBER 7- OCTOBER 9, 2023 2023 HEALTH MATTERS THE SUMTER ITEM DALZELL APPLIANCE PARTS, SERVICE AND SALES Where Quality Counts! • ELECTROLUX • FRIGIDAIRE • TAPPAN • GE • KELVINATOR • • WHITE WESTINGHOUSE • GIBSON • MAGIC CHEF • HOTPOINT KENMORE WHIRLPOOL Parts & Service on most major brands: FRIGIDAIRE DEALER • OVER 40 YEARS EXPERIENCE PARTS IN STOCK • WE BUY AND SELL USED APPLIANCES 803-499-2200 We Service What We Sell 4195 Thomas Sumter Hwy. Hwy 521 N. Dalzell Mon-Thurs: 9-5 • Fri: 9-4 RELIABLE MEDICAL EQUIPMENT 2580 Lin - Do Ct.,Suite B. • Sumter, SC • 803-934-9212 PROSTHETICS, BRACING, & DURABLE MEDICAL EQUIPMENT WE HAVE A CERTIFIED PROSTHETIST / ORTHOTIST ON STAFF VOTED #1 YEAR AFTER YEAR! A cure worth fighting for #togetherwefight 803.774.4040 53 W. Wesmark Blvd., Sumter, SC Over 150 Years of Service sumterinsurancegroup.com 803-778-1937 Visit us atwww.boykinacs.com COOK’S PARTS CITY Auto Parts 3170 Frierson Rd. • Dalzell, SC 29040 • Phone: 803-499-9086 HOURS: MONDAY-FRIDAY 7AM-6PM • SATURDAY 8AM-5PM FAMILY OWNED & OPERATED FOR 35 YEARS! PROPANE GAS 24 HOUR TOWING SERVICE WE CARRY A COMPLETE LINE OF AUTO PARTS COME CHECK US OUT! DOES YOUR CAR NEED SOME TLC? Blakely’s Mobile Detailing Cars • Trucks • Semis • Boats • RV Campers 803.398.6785 I draccb@gmail.com No job too big or small! In memory of Betty Jean Blakely A Ring Around The Roses 95B MARKET STREET • SUMTER 934-8000 | www.aringaroundtheroses.com Supporting Early Detection The Ultimate Girls’ Night! Jamil Gill 803-847-5201 PROUD MEMBER OF THE CHAMBER OF COMMERCE HOME OF FIRST COME FIRST SERVED SATURDAYS 70 W. Wesmark Blvd. Sumter, SC 29150 www.biltonlincoln.com 803-773-7339 Bilton M&M Carpets, Inc. 1285 Peach Orchard Rd. • Sumter, SC 29154 (Behind Shaw AFB) SALES • INSTALLATION • REPAIRS & CLEANING Complete Floor Covering Services & 24 Hour Water Restoration Cell: 803-972-3758 Work: 803-494-2100 Fax: 803-494-2434 E-mail: mrazor@ftc-i.net Michael L. Razor President Notary Public TEAM ROBINSON 337 W. Liberty St., Sumter, SC • (803) 236-0803 50% Off Registration Fee Present ad for discount About ONE MONTH FREE! Partin’s Auto Sales Best Deals on Wheels Butch Carraway Owner 1265 Peach Orchard Rd. Sumter, SC 29154 803-494-8667 of ce 803-494-9307 fax Open: Mon-Fri 9:30am-7pm Sat 9:30am-5pm Closed Sunday 2891 Broad St., Sumter, SC 29150 803-469-8733 SHOP & ORDER TODAY! CELEBRATING33YEARS IN BUSINESS Voted #1 Place to Buy Furniture & Mattresses 11 Years Straight Supporting the Fight! Mary Kathryn Hulme Operations Manager/Interior Designer nndsmk@gmail.com nicolenorrisdesign.com Main O ce: 47 N. Main St. Sumter, SC 29150 Phone 803.773.8083 Charleston O ce: 1600 Long Grove Dr. Unit 1723 Mt. Pleasant, SC 29464 warriors and survivors Local businesses support
































































2023 HEALTH MATTERS OCTOBER 7 - OCTOBER 9, 2023 | D5
CANCER AFFECTS
DAUGHTERS AND FRIENDS FROM ALL WALKS OF LIFE. HELP IN THE ONGOING FIGHT AGAINST BREAST CANCER BY SCHEDULING A MAMMOGRAM FOR YOURSELF TODAY. ALSO, ENCOURAGE OTHERS YOU KNOW TO DO THE SAME. In honor of Our loved ones during National Breast Cancer Awareness Month Hallie Fleischman Last treatment 6/2023 Susan Heimbigner 13 years Mozell S. Thompson 16 years Mary T. Baker 15 years Mary Dinkins Allen 7 years Rosetta Dinkins Collins 12 years Elizabeth White 20 years Pauline D. Bogger 25 years Chylene Burdick 6 years Margaret M. Davey 21 years Patty Hackett Pecko 2.5 years Tawana B. Deschamps 10 years Betty Woods 7 years Laura Yates 19 years Leavy D. Yates 8 years Denise Christmas Robinson 18 years Patsy Morris 16 years Danessa Wierschem 4 years Lisa W. McCoy 2 years Merline Brown 36 years Cheryl R. Pierce 4 years Willodine James Debra Ragin Brailsford 10 years Elise Oxendine 14 years Deborah Carroll Norman 11 years Diane Werner 3 years Tamekia Hunter Ross 5 years Myra W. Dyson 4 years April McFadden 4 months Eartha M Moore 14 years Birtie Nathaniel 20 years Willie Mae McQuilla 6 months Mamie Wilder 3 years Annette Smothers 15 years Loretta Logan 48 years 361 Myrtle Beach Hwy. Sumter, SC 29153 773-6010 OFFICE 469-5533 PAGER 877-747-7642 TOLL FREE We Do Automotive Service With A Smile. www.newmansautomotivesumter.com Support Breast Cancer Awareness • Oil Changes • Tune-Ups • Computer Diagnostics Brake Service & Repair • Tires • AC Service • Wheel Balance • Starters • Radiators Shocks & Struts • Belts and Hoses • Air Conditioning Call Today! (803) 773-3379 WRIGHT WAY PLUMBING 3425 Thomas Sumter Highway, Dalzell, SC 29040 803-499-4108 • wrightwayplumbingllc.com At Your Service Home Care Proud Provider of Veterans Administration 19 S. Harvin St., 29150 • Sumter, SC 401 S. Mill St., • Manning, SC 29102 803-607-9677 Voted Best Year After Year Gary’s Florist, LLC Gary & Ann Duby, Owners 803-775-7768 / 803-775-7769 Mon-Fri 8:30-6:00 Sat 8:30-11:00 In honor and memory of friends and loved ones. Wesmark Plaza • 773-2262 • Mon-Sat 10-7 • www.MayosDiscountSuits.com Mayo’s Suit City With any purchase of $100 or more, get PINK tie and handkerchief set FREE! “Think Pink in October!”
BREAST
MOTHERS,
A psychiatrist explains the neuroscience and physiology of fear
By Arash Javanbakht Wayne State University The Conversation









Heart in your throat.
Butterflies in your stomach. Bad gut feeling. These are all phrases many people use to describe fear and anxiety. You have likely felt anxiety inside your chest or stomach, and your brain usually doesn’t hurt when you’re scared. Many cultures tie cowardice and bravery more to the heartor the guts than to the brain.
But science has traditionally seen the brain as the birthplace and processing site of fear and anxiety. Then why and how do you feel these emotions in other parts of your body?

I am a psychiatrist and neuroscientist who researches and treats fear and anxiety. In my book “Afraid,” I explain how fear works in the brain and the body and what too much anxiety does to the body. Research confirms that while emotions do originate in your brain, it’s your body that carries out the orders.


Fear and the brain
While your brain evolved to save you from a falling rock or speeding predator, the anxieties of modern life are often a lot more abstract. Fifty-thousand years ago, being rejected by your tribe could mean death, but not doing a great job on a public speech at school or at work doesn’t have the same consequences. Your brain, however, might not know the difference.
There are a few key areas of the brain that are heavily involved in processing fear.
When you perceive something as dangerous, whether it’s a gun pointed at you or a group of people looking unhappily at you, these sensory inputs are first relayed to the amygdala. This small, almond-shaped area of the brain located near your ears detects salience, or the emotional relevance of a situation and how to react to it. When you see something, it determines whether you should eat it, attack it, run away from it or have sex with it.
Threat detection is a vital part of this process, and it has to be fast. Early humans did not have much time to think when a lion

was lunging toward them. They had to act quickly. For this reason, the amygdala evolved to bypass brain areas involved in logical thinking and can directly engage physical responses. For example, seeing an angry face on a computer screen can immediately trigger a detectable response from the amygdala without the viewer even being aware of this reaction.

The hippocampus is near and tightly connected to the amygdala. It’s involved in memorizing what is safe and what is dangerous, especially in relation to the environment – it puts fear in context. For example, seeing an angry lion in the zoo and in the Sahara both trigger a fear response in the amygdala. But the hippocampus steps in and blocks this response when you’re at the zoo because you aren’t in danger.

The prefrontal cortex, located above your eyes, is mostly involved in the cognitive and social aspects of fear processing. For example, you might be scared of a snake until you read a sign that the snake is nonpoisonous or the owner tells you it’s their friendly pet.

Although the prefrontal cortex is usually seen as the part of the brain that regulates emotions, it can also teach you fear based on your social environment. For example, you might feel neutral about a meeting with your boss but immediately feel nervous when a colleague tells you about rumors of layoffs. Many prejudices like racism are rooted in learning fear through tribalism.


Fear and the rest of the body
If your brain decides that a fear response is justified in a particular situation, it activates a cascade of neuronal and hormonal pathways to prepare you for immediate action. Some of the fight-or-flight response – like heightened attention and threat detection – takes place in the brain. But the body is where most of the action happens.
Several pathways prepare different body systems for intense physical action.
The motor cortex of the brain sends rapid signals to your muscles to prepare them for quick and forceful movements. These include muscles in the chest and stomach that help protect vital organs in those areas. That might contribute to a feeling of tightness in your chest and stomach in stressful conditions.
The sympathetic nervous system is the gas pedal that speeds up the systems involved in fight or flight. Sympathetic neurons are spread throughout the body and are especially dense in places like the heart, lungs and intestines. These neurons trigger the adrenal gland to release hormones like adrenaline that travel through the blood to reach those organs and increase the rate at which they undergo the fear response.
To assure sufficient blood supply to your muscles when they’re in high demand, signals from the sympathetic nervous system increase the rate your heart beats and the force with which it contracts. You feel both increased heart rate and contraction force in your chest, which is why you may connect the feeling of intense emotions to your heart.
In your lungs, signals from the sympathetic nervous system dilate airways and often increase your breathing rate and depth. Sometimes this results in a feeling of shortness of breath.
As digestion is the last priority during a fight-or-flight situation, sympathetic activation slows down your gut and reduces blood flow to your stomach to save oxygen and nutrients for more vital organs like the heart and the brain. These changes to your gastrointestinal system can be perceived as the discomfort linked to fear and anxiety.
It all goes back to the brain
All bodily sensations, including those visceral feelings from your chest and stomach, are relayed






















back to the brain through the pathways via the spinal cord. Your already anxious and highly alert brain then processes these signals at both conscious and unconscious levels.
The insula is a part of the brain specifically involved in conscious awareness of your emotions, pain and bodily sensations. The prefrontal cortex also engages in self-awareness, especially by labeling and naming these physical sensations, like feeling tightness or pain in your stomach, and attributing cognitive value to them, like “this is fine and will go away” or “this is terrible and I am dying.”
These physical sensations can sometimes create a loop of increasing anxiety as they make the brain feel more scared of the situation because of the turmoil it






senses in the body.

Although the feelings of fear and anxiety start in your brain, you also feel them in your body because your brain alters your bodily functions. Emotions take place in both your body and your brain, but you become aware of their existence with your brain. As the rapper Eminem recounted in his song “Lose Yourself,” the reason his palms were sweaty, his knees weak and his arms heavy was because his brain was nervous.
(The Conversation is an independent and nonprofit source of news, analysis and commentary from academic experts.)









































D6 | OCTOBER 7- OCTOBER 9, 2023 2023 HEALTH MATTERS THE SUMTER ITEM
If anxiety is in my brain, why is my heart pounding?
WANT TO IMPROVE SALES? Call an Item sales representative to advertise in our many publications! markp@theitem.com (803) 464-8917 MARK PEKURI devin@theitem.com (803) 983-0786 DEVIN MCDONALD karen@theitem.com (803) 774-1242 KAREN CAVE NOTICES 803-774-12 Do I still have to wear a mask? What about kids? A room for teachers to get some R&R U.S. wants Israel to wind down offensive The Grind: Swampcats’ internet fame with life on the gridiron Where she needs to be back to the lake, a fishing rod and feeling close to God. Learn about your local leaders GET OUTSIDE RECREATION, DINING AND PUBLIC ART MORE Personalized Care Access Specialists PrismaHealth.org/ExploreTuomey 2023 March 23 - April 2, 2023 Iris Festival 2023 242,153 VOTES 342 WINNERS
RÁPIDO
RÁPIDO aims to get native Spanish speakers to recognize stroke signs fast
By Lourdes Medrano American Heart Association News


Norma Hernández was preparing for choir practice for a church service when someone came looking for help. Another church member, a friend of hers, had fallen ill.
Hernández rushed to her friend and found him slumped in a chair, his wife standing beside him. He looked tired and pale, recalled Hernández, a certified community health worker in Fort Worth, Texas. “I was talking to him at the same time I was assessing him,” she said. “But the more questions I asked, the more I thought something was not right.”
When Hernández asked him what day it was, his words came out slow and garbled. She recognized his slurred speech as a sign of a stroke. She told his wife to call 911, and soon after, her friend was on his way to the hospital.
Doctors discovered a blockage in her friend’s brain had caused a ministroke, Hernández said. A mini-stroke, or transient ischemic attack, occurs when the blood supply to the brain is temporarily interrupted by a blockage in an artery. TIAs might not cause permanent damage, but they can be a signal of a possible larger stroke to come.
Hernández’s friend recovered – and was able to avoid a full-blown stroke, she said.
Recognizing the signs of a stroke and acting quickly to seek treatment, as Hernández did, are key to stroke survival, medical experts say. It’s a message intended to resonate through FAST, an acronym long touted by the American Stroke Association to help people remember the signs of a stroke: Face drooping, Arm weakness, Speech difficulty, Time to call 911.
But for people who speak Spanish, FAST doesn’t translate well. So, in 2021, researchers at UTHealth Houston released data about a new
Spanish-language acronym. They soon teamed up with the ASA to further refine it. Called RÁPIDO, it stands for Rostro caído, Alteración del equilibrio, Pérdida de la fuerza en el brazo o una pierna, Impedimento visual repentino, Dificultad para hablar, Obtén ayuda y llama al 911.
Just 58% of Hispanic adults in the U.S. can recognize stroke signs, compared to 64% of Black adults and 71% of white adults, according to a Centers for Disease Control and Prevention report based on a 2017 survey. Dr. José Biller, a professor and chair of neurology at Loyola University Chicago’s Stritch School of Medicine, said RÁPIDO is a culturally tailored tool that can boost stroke awareness education in Hispanic populations with a high burden of stroke. “And because of the time-sensitive nature of stroke, every second counts,” he said.


Stroke is the fifth-leading cause of death in the U.S. It is the No. 3 cause of death for Hispanic women and No. 4 for Hispanic men. Moreover, Biller said, the average age for strokes among Hispanics is 67, but 80 for non-Hispanic white people.
Research also shows that Hispanic people are disproportionately more likely to develop high blood pressure, diabetes and obesity – all risk factors for stroke. Social determinants of health, such as access to quality health care, language barriers and education level, also can affect stroke risk. “We need to remain sensitive to these issues because they can affect health,” Biller said.
Dr. Fernando Testai, the director of vascular neurology and a professor at the University of Illinois at Chicago College of Medicine, said research has established the pivotal
role sociocultural factors play on the higher rates of stroke in the Hispanic and Latino population. Limited English proficiency stands out to Testai as a barrier to equitable care and has been consistently linked to poor stroke outcomes.
“Consequently, the development of efficient and culturally sensitive stroke screening tools that address this challenge represents a substantial stride toward our goal of bridging important quality gaps observed in stroke care,” said Testai, who uses RÁPIDO to educate his Spanish-speaking patients about stroke.
Roughly 9.4 million U.S. adults – 3.3% of the population as of 2020 – report having had a stroke, according to American Heart Association statistics. Between 2012 and 2030, stroke prevalence is expected to rise the most among Hispanic men.
Biller, who helped develop RÁPIDO, said he hopes the acronym will become a fixture among hospital systems, health clinics and community organizations in areas with Spanish-speaking populations to help improve stroke outcomes among Hispanic people. In the U.S., Spanish is spoken in 13% of households, census data show.
Hernández, the community health worker, said the experience with her friend’s mini-stroke has inspired her to showcase RÁPIDO posters and other materials at church health fairs and elsewhere. “More education is needed about stroke symptoms in the Spanish-speaking community,” she said. “It will be a good way of bringing more attention to stroke.”

THE SUMTER ITEM 2023 HEALTH MATTERS OCTOBER 7 - OCTOBER 9, 2023 | D7
SUMTER FAMILY YMCA 510 Miller Road 803.773.1404 ymcasumter.org STRONGHEART COMMIT TO BE YFIT LIVE WELL WITH DIABETES PERSONAL TRAINING LIVE LONG, STAY STRONG
What distinguishes the different types of breast cancer?















Individuals can experience a whirlwind of emotion upon being diagnosed with cancer. No one ever expects to receive such a diagnosis, so the moment a physician delivers such news can be emotional and compromise a person’s ability to focus. Once those emotions settle down and individuals resolve to overcome the disease, they typically have a lot of questions.


One of the questions doctors will attempt to answer is which subtype of cancer a person has. For example, when doctors initially deliver a breast cancer diagnosis, they may explain that further testing will be necessary to determine precisely which type of breast cancer an individual has. Identifying the subtype of breast cancer helps doctors choose the most effective course of treatment, but it’s understandable if patients and their families become confused during the process. The following rundown can help breast cancer patients understand this crucial next step after diagnosis.

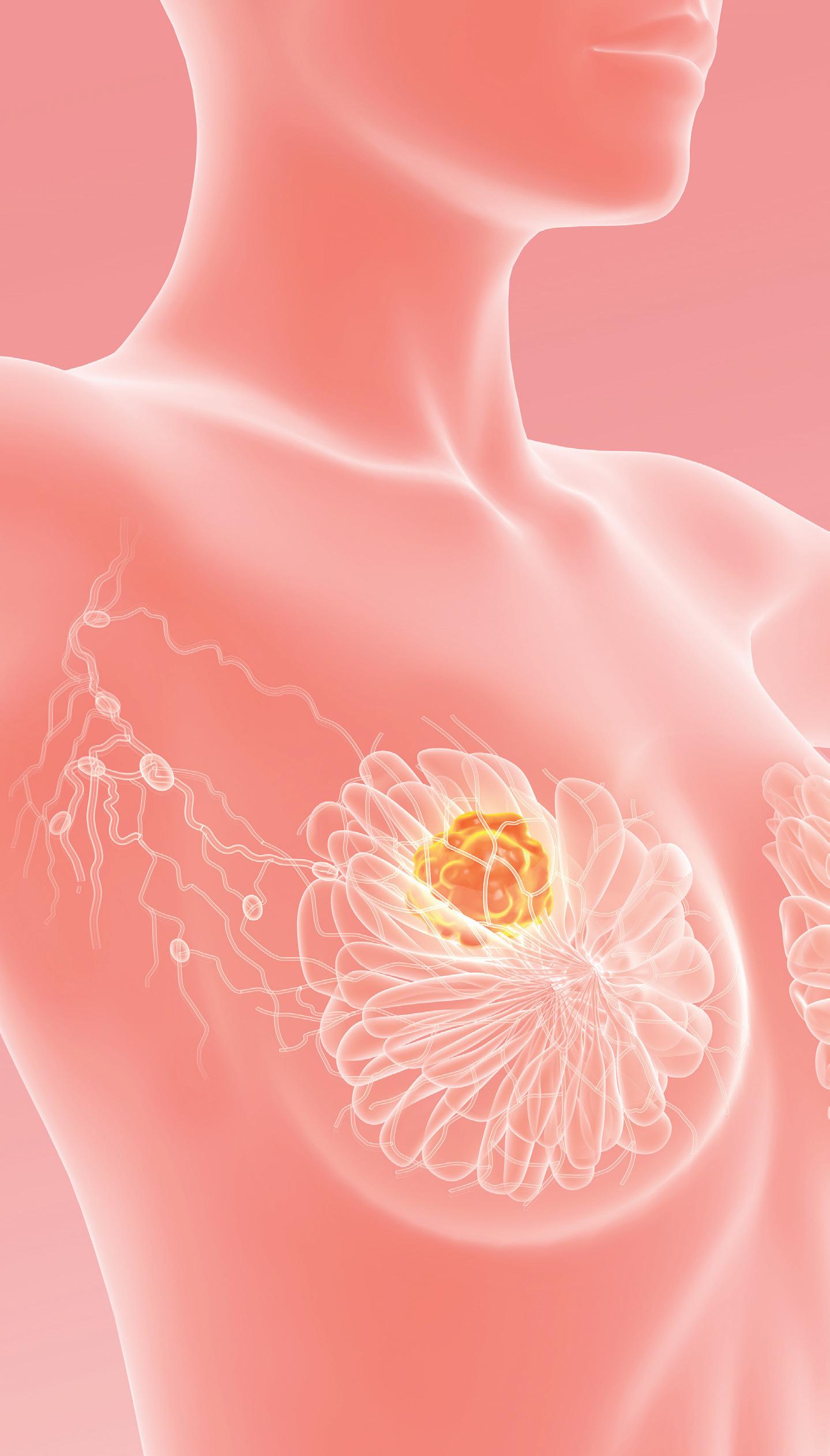
Did you know?
The length of time a women will receive treatment for breast cancer will ultimately depend on a host of variables unique to each individual. According to the nonprofit organization Living Beyond Breast Cancer, an individual diagnosed with early-stage breast cancer can be in active treatment for about one year. The administration of medicine, the performance or surgery and ongoing therapies are all considered part of active treatment. The Mayo Clinic reports that chemotherapy, a treatment option that utilizes various drugs to destroy cancer cells or slow their growth, can last between three to six months for patients diagnosed with early-stage breast cancer. Treatment with chemotherapy can extend beyond six months for individuals with advanced stage breast cancer. Hormonal therapy also can extend the time breast cancer patients are in treatment, as the American Cancer Society reports that this option typically requires patients to take a pill for five years. However, hormonal therapy can extend past five years in certain instances.
How is breast cancer type determined?





The American Cancer Society notes that breast cancer type is determined by the specific cells in the breast that become cancer. The Mayo Clinic reports that a medical team will use a tissue sample from a patient’s breast biopsy or, for patients who have already undergone surgery, the tumor to identify the cancer type.



What are the types of breast cancer I might be diagnosed with?














There are many types of breast cancer, but some are more common than others. Invasive and non-invasive (also referred to as “carcinoma in situ”) are the two main subtypes of breast cancer.
According to the University of Pittsburgh Medical Center, the most common types of invasive breast cancer are invasive ductal carcinoma, which affects the inner lining of the milk ducts, and invasive lobular carcinoma, which originates from the glands that produce milk.
The UPMC reports






















































































































































































that the most common in situ types are ductal carcinoma in situ, which is cancer that remains within the milk ducts, and lobular carcinoma in situ, which does not often develop into breast cancer though it is considered a risk factor for an invasive form of the disease.
The ACS notes that triple-negative breast cancer is an aggressive form of breast cancer that accounts for roughly 15 percent of all breast cancers. Triple-negative breast cancer can be difficult to treat.


































Less common types of breast cancer, each of which account for between 1 and 3 percent of diagnoses in a given year, include Paget disease of the breast, angiosarcoma and phyllodes tumor.
A breast cancer diagnosis marks the beginning of a sometimes lengthy but often successful journey that has ended in full recovery for millions of women across the globe. More information about the various types of breast cancer can be found at cancer. org.







D8 | OCTOBER 7- OCTOBER 9, 2023 2023 HEALTH MATTERS THE SUMTER ITEM
“When you need care NOW” 3440 Declaration Blvd • Sumter (803) 905-FAST (3278) www.FasterCareSumter.com Our Services Include: • Urgent Care • Ultrasound, CAT Scan & X-rays • Outpatient Labs • D.O.T. Physicals • Physicals • Workman’s Compensation Injuries









































































































































 By Michael Merschel American Heart Association News
By Michael Merschel American Heart Association News