Vol 12 Issue 5 2023 www.modernequinevet.com Battling Endometrial Biofilms Can Horses Follow Directions? Technician Update: Facial Wounds Improving QoL for PPID Equine Vet The Modern
SALES: ModernEquineVet@gmail.com


EDITOR: Marie Rosenthal
ART DIRECTOR: Jennifer Barlow
CONTRIBUTING WRITERS: Paul Basilio • Rob Warren

COPY EDITOR: Patty Wall
LEGAL DISCLAIMER: The content in this digital issue is for general informational purposes only. PercyBo Publishing Media LLC makes no representations or warranties of any kind about the completeness, accuracy, timeliness, reliability or suitability of any of the information, including content or advertisements, contained in any of its digital content and expressly disclaims liability of any errors or omissions that may be presented within its content. PercyBo Publishing Media LLC reserves the right to alter or correct any content without any obligations. Furthermore, PercyBo disclaims any and all liability for any direct, indirect, or other damages arising from the use or misuse of the information presented in its digital content. The views expressed in its digital content are those of sources and authors and do not necessarily reflect the opinion or policy of PercyBo. The content is for veterinary professionals. ALL RIGHTS RESERVED. Reproduction in whole or in part without permission is prohibited.
2 Issue 5/2032 | ModernEquineVet.com TABLE OF CONTENTS
Published by PERCY BO media publishing PO Box 935 • Morrisville, PA 19067 Marie Rosenthal and Jennifer Barlow, Publishers Equine Vet The Modern INFECTIOUS DISEASES Strength in Numbers: Combination Therapy Busts Up Endometrial Biofilms 8 BEHAVIOR Which Horses Are Better at Following Directions? .................................... 11 TECHNICIAN UPDATE Traumatic Facial Wound in a Miniature Donkey 13 NEWS NOTES Early Removal of Osteochondral Fragments Could Be Helpful 12 Minimally Invasive Technique Helped Sheep, Could Someday Help Foals 17 PPID Treatment Improves Quality of Life COVER STORY 4 Cover: Shutterstock/mariait ADVERTISERS Arenus Animal Health/AssureGuard Gold 3 Arenus Animal Health/Aleira-Releira 7 American Regent/Adequan 9
THE



Arenus Animal Health | 866-791-3344 | www.arenus.com SO INNOVATIVE...
Replace your mineral oil, electrolytes, adsorbents, or other treatment options with Assure Guard Gold-NG the only effective and easy to administer slow gelling quick relief formulation including 2 cups of ultra pure psyllium, 72 billion CFU of probiotics, prebiotics, antacids, L-glutamine, electrolytes and energy. For continued support, consider a 10 day supply of Assure Guard Gold after treatment. IT’S LIKE MAGIC Ask your Arenus Veterinary Solution Specialist how Assure Guard Gold-NG and Assure Guard Gold can help your equine patients quickly and effectively recover from the digestive upsets you treat daily.
® Assure Guard
Together, Assure Guard Gold-NG And Assure Guard Gold Create A Powerhouse Against Your Most Challenging Digestive Cases. Use Assure Guard Gold-NG For Fast Relief And Maintain Excellent Digestive Health With Assure Guard Gold.
REAL MAGIC IS IN THE RESULTS
The Ultimate Digestive Aid
Gold
PPID Treatment
Improves Quality of Life
Client satisfaction was also high
Equids with pituitary pars intermedia dysfunction (PPID) treated with pergolide (Prascend, Boehringer Ingelheim Animal Health) may not need progressively increased doses for long-term treatment, according to Harold C. Schott II, DVM, PhD, DACVIM, who with his colleagues at Michigan State University performed a multi-year study looking at long-term PPID treatment.
They found that although the treatment improved the quality of life of the equids, as well as saw high client satisfaction, it did not necessarily prolong life, according to Dr. Schott, who spoke at the AAEP Annual Convention 2022.

“We all know that PPID is increasingly being recognized and treated,” said Dr. Schott, a professor in equine internal medicine at Michigan State University. However, without long-term data it is difficult for clients to weigh the benefits of what could end up be-
ing life-long treatment for some diseases, especially when considering the possible financial implications of such treatment.
Dr. Schott and his colleagues had the opportunity to answer some of these questions after the pivotal FDA trial for Prascend, when Boehringer Ingelheim agreed to fund a truly long-term study—>10 years looking at some of the horses that were enrolled in the original study done for FDA approval.
The questions he was interested in were:
• Will we have to progressively increase the dose of pergolide to control the clinical signs and possibly endocrine test results in equids affected with PPID?
• Does pergolide treatment really improve quality of life?
• Does it potentially prolong the life of the horses?

• Are our clients satisfied with treatment outcomes?
By Marie Rosenthal MS
4 Issue 5/2022 | ModernEquineVet.com
ENDOCRINOLOGY
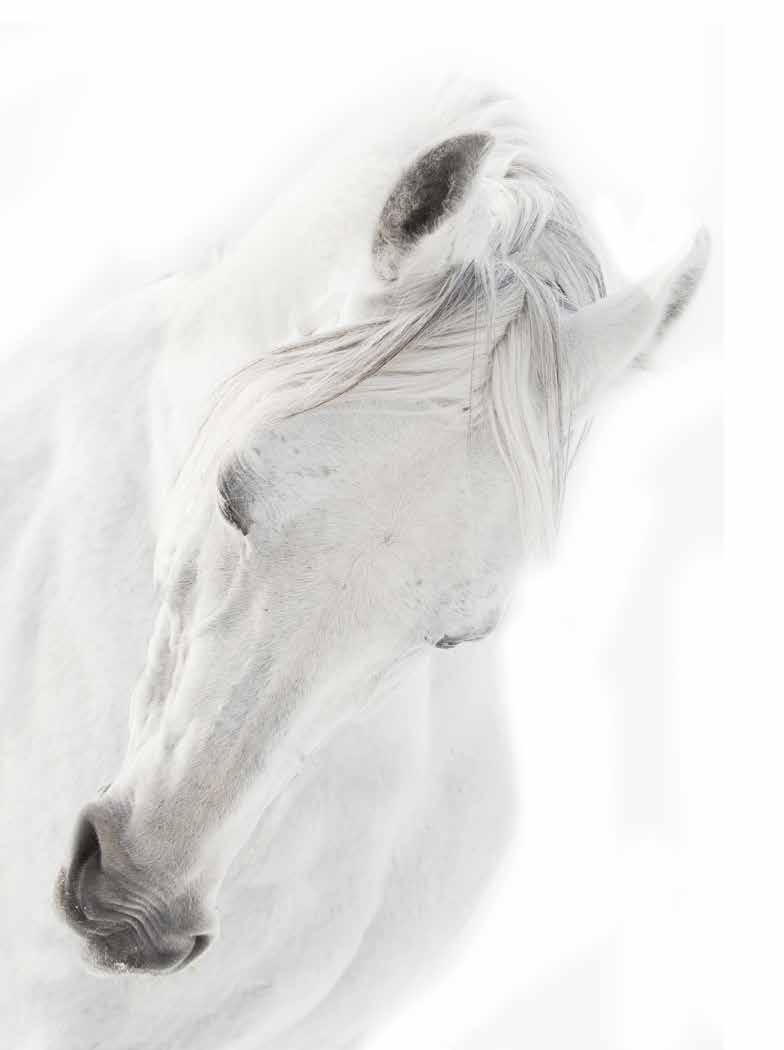
Horses with the typical hair coat of PPID.
Image courtesy of Dr. Harold C. Schott II
During the original trial, they managed 40 horses and asked their owners if they would be willing to participate in the longer trial. They enrolled 30 equids (28 horses and 2 ponies) from that original 6-month trial, and the second trial began in 2009. BI had a different endpoint. BI wanted to know about the longterm safety of the medication, which was also measured.

The researchers conducted follow up interviews by telephone every 3 months asking about any medical problems the equids were seeing, and the equids were examined every couple of years throughout the study, which lasted 12.5 years. One of the participants was Dr. Schott’s daughter’s pony, Rusty, who is still alive.
When the original study was performed, they did not have the adrenocorticotropic hormone (ACTH) assays that are used today, so the ACTH values were often lower in the older assays, he explained. They based on the original results on the classic overnight dexamethasone suppression test, so that was the endocrine test they continue to use as they monitored the animals over time.
“In the FDA open field trial, there were 113 equids and 86 of those or 76% were considered treatment successes. Our cohort was again, a subgroup of that, and 18 of 30 were considered treatment successes. So,
they were easily representative of the overall 113 horse cohort with possibly maybe a little bit more advanced PPID,” Dr. Schott explained.
In the original study, the average 500-kg horse received 2 µg/ kg/d and were reevaluated with clinical scores and endocrine tests after 3 and 6 months. If they passed their endocrine tests after 3 months (plasma cortisol <1 µg /dL 18 hours to 19 hours after dexamethasone administration) they stayed at the 2 µg/kg/d dose.
If they failed, the dose was increased to 4 µg/kg/d.
In the follow-up study, 7 of 15 equids saw an increase in dose to 4 µg/kg/d within 5 years of the study.
“Overall, what we can see here is for the next 4 to 5 years, most of these horses did well and continued to have a normal endocrine test results despite remaining on just 1 mg of pergolide per day,” he said.
By now, all but Rusty, Dr. Schott’s pony, has died or was euthanized.
“The median survival of these equids was 3.3 years over this period of time,” Dr. Schott said. “Now, to date, we've lost 29 of the 30 horses. Rusty's the only one that is still alive. Five of these were euthanized because of laminitis, so that we could say was associated with their PPID; 24 had other age-related disorders, arthritis, strangulating lipomas, a couple of fractures, and just things that we did not think were associated with PPID.”
At the 5.5-year follow-up, owners of 13 equids that were still alive said they continued to see clinical improvement in the horses, and 75% had normal endocrine test results.
However, normal endocrine tests were only seen in 2 of 6 surviving equids at 9.5 years.
“After about 10 years, we did a client satisfaction survey. We sent the survey out, and we had an 86% completion rate,” Dr. Schott said.
Most clients said they were satisfied with the animal’s treatment:
• 44% strongly agreed they would provide lifelong treatment if they had another equid with PPID; and
• 44% agreed they would provide treatment if they had another equid with PPID.
• 71% strongly agreed the treatment improved their equids quality of life; and
ModernEquineVet.com | Issue 5/2022 5
“Our equids with PPID [pituitary pars intermedia dysfunction] might not need a progressive increase in drug dose over time.”
—Dr. Harold C. Schott II
• 25% agreed the treatment improved their equids quality of life.




Specifically:
• 77% said the horse had more energy;
• 71% saw improvements in haircoat and shedding; and
• 41% saw a reduction in abnormal sweating. They were also asked what they were willing to pay for medication:
• 26% said $500;
• 56% said $1,000;
• 10% said $1,500;
• 4% said $2,000; and
• 4% said $2,500.
“The sweet spot was right about 1,000 dollars, and once the price got over that we started to see a decline—they would think about it a little bit more.
So that's important information to know what your clients may be willing to do in the future,” he said.
“Our equids with PPID might not need a progressive increase in drug dose over time. The endocrine test results can improve over a prolonged period even if they were abnormal for the first year.
“So, you might want to do a case-by-case base assessment. Treatment appears to improve quality of life, but it doesn't appear to prolong life,” he said.
Rusty, he said was still doing well. “He's a happy little boy,” MeV
Boehringer Ingelheim has been very generous in supporting this study over the years, as well as providing funding for the large animal clinical sciences department of MSU. Dr. Schott is a consultant for Boehringer Ingelheim on projects.
6 Issue 5/2032 | ModernEquineVet.com ENDOCRINOLOGY
Dr. Harold C. Schott's daughter's pony, Rusty, which had PPID and was part of the study, with his daughter through the years.

STRENGTH IN NUMBERS:
Combination therapy busts up endometrial biofilms
By Paul Basilio
To resolve most cases of bacterial endometritis, all that’s usually needed is a proper course of antimicrobials and the mare’s own immune system. In a small number of cases, however, the bacteria dig in and set up residence in a biofilm, making eradication much more difficult.

20%
“What we’re taught in veterinary school is what usually happens with single-celled organisms,” said Ryan Ferris, DVM, MS, DACT, during a presentation at the 68th Annual AAEP Convention. “Singlecell bacteria come in, they populate the uterus, they start replicating, and they cause inflammation. That’s what we’re taught, and that’s what our antibiotic sensitivity tests will report.”
With biofilms, however, the bacteria move from an “every cell for itself” model to a community of bacteria that have ways of surviving antimicrobial treatments and withstanding attacks from the host’s immune system.
The creation of biofilms has much to do with how the host responds to the bacteria in their single-cell stage. Mares may be more susceptible to biofilm if they have immune suppression, have metabolic syndrome, poor fluid clearance, or if they are cushingoid.
What is a biofilm?
One of the misconceptions about biofilms is that they are large masses containing billions of bacteria that take up a lot of real estate on an affected area. When Dr. Ferris and his team took a Pseudomonas
Shutterstock/Alberto Duran Photography
8 Issue 5/2032 | ModernEquineVet.com INFECTIOUS DISEASES
For more than 30 years, Adequan® i.m. (polysulfated glycosaminoglycan) has been administered millions of times1 to treat degenerative joint disease, and with good reason. From day one, it’s been the only FDA-Approved equine PSGAG joint treatment available, and the only one proven to.2, 3
Reduce inflammation
Restore synovial joint lubrication
Repair joint cartilage
Reverse the disease cycle
When you start with it early and stay with it as needed, horses may enjoy greater mobility over a lifetime.2, 4, 5 Discover if Adequan is the right choice. Visit adequan.com/Ordering-Information to find a distributor and place an order today.

BRIEF SUMMARY: Prior to use please consult the product insert, a summary of which follows: CAUTION: Federal law restricts this drug to use by or on the order of a licensed veterinarian. INDICATIONS: Adequan® i.m. is recommended for the intramuscular treatment of non-infectious degenerative and/or traumatic joint dysfunction and associated lameness of the carpal and hock joints in horses. CONTRAINDICATIONS: There are no known contraindications to the use of intramuscular Polysulfated Glycosaminoglycan. WARNINGS: Do not use in horses intended for human consumption. Not for use in humans. Keep this and all medications out of the reach of children. PRECAUTIONS: The safe use of Adequan® i.m. in horses used for breeding purposes, during pregnancy, or in lactating mares has not been evaluated. For customer care, or to obtain product information, visit www.adequan.com. To report an adverse event please contact American Regent, Inc. at 1-888-354-4857 or email pv@americanregent.com.
Please see Full Prescribing Information at www.adequan.com
1 Data on file.
2 Adequan® i.m. Package Insert, Rev 1/19.
3 Burba DJ, Collier MA, DeBault LE, Hanson-Painton O, Thompson HC, Holder CL: In vivo kinetic study on uptake and distribution of intramuscular tritium-labeled polysulfated glycosaminoglycan in equine body fluid compartments and articular cartilage in an osteochondral defect model. J Equine Vet Sci 1993; 13: 696-703.

4 Kim DY, Taylor HW, Moore RM, Paulsen DB, Cho DY. Articular chondrocyte apoptosis in equine osteoarthritis. The Veterinary Journal 2003; 166: 52-57.
5 McIlwraith CW, Frisbie DD, Kawcak CE, van Weeren PR. Joint Disease in the Horse.St. Louis, MO: Elsevier, 2016; 33-48.
All trademarks are the property of American Regent, Inc.
© 2021, American Regent, Inc.
PP-AI-US-0629 05/2021
There’s
nothing else like it. www.adequan.com
INFECTIOUS DISEASES
TAKE-HOME MESSAGE
Dr. Ryan Ferris wanted to make 1 thing clear above all else: Stay away from formalin if you’re suspicious of a biofilm.
“One of the issues [our team] had was that we didn’t know what to fix these samples in,” he said. “With Bouin’s solution, we were able to maintain the architecture of the adherent material, and we could evaluate it histologically. If we took similar samples and placed them in 10% formalin, the adherent material washed away.”
biofilm isolated from a mare’s uterus and genetically modified it to glow in the dark, the real image of a biofilm surprised him.
“This was probably one of the neatest studies I’ve had the opportunity to perform,” said Dr. Ferris, coowner of Summit Equine in Newberg, Ore. “The biofilm formed mostly at the base of the [uterine] horns up toward the tip, and very little was present over the uterine body.”
Histologic examination showed diffuse, severe lymphocytic infiltrate in areas with and without adherent material. It appeared as if the entire uterus was responding to the bacteria, regardless of whether the biofilm was present over a particular surface.
“This adherent material was made up of mostly host cells, such as uterine epithelial cells, white blood cells, proteins and mucus,” he explained. “That's similar to what we see in other species. The adherent material isn't all bacterial in nature—most of it is actually host in nature.”
Another surprising finding was just how few bacteria were present on the adherent material.
“When you hear the word ‘biofilm,’ you expect this coating throughout the entire uterus with billions of bacteria,” he added. “What was interesting was that these were small, focal communities of dozens to 100 bacteria. So, we're talking about small, tiny infections.”
How to treat
Bacteria in biofilms can be up to 1,000 times more resistant to treatment than bacteria that are free-living, or planktonic.
To identify worthwhile treatments, Dr. Ferris and his colleagues relied on good old-fashioned trial and error.
The team established a pre-formed biofilm in the lab and challenged the isolates with antibiotics, nonantibiotics, and then a combination for 3 days in a row to try to mimic a typical treatment period that might be used in clinical practice.

“I could show you a whole series of our failures,” he joked. “We screened a lot of products and tried to figure out how to disrupt the biofilm.”
The team tried loading the uterus with antibiotics, which didn’t work. Neither did a whole range of non-antibiotics.
“After all of that, we came up with a combination therapy that seemed to be the most effective,” he said.
On their own, ceftiofur monotherapy and TrisEDTA, a buffer solution, monotherapy performed well, but not great. Each treatment resulted in a 2-log decrease in colony-forming units (CFUs).
“Interestingly, when we mixed Tris-EDTA and ceftiofur, it resulted in a complete killing of all the bacteria,” Dr. Ferris said, adding that the combination also decreased the biofilm biomass to around the same level as the uncontaminated control isolate.
“That was pretty exciting,” he said, “but what was more eye-opening was that we identified a whole series of ineffective compounds.”
For example, acetylcysteine alone caused an approximate 2-log decrease in bacteria and performed admirably at breaking up the biofilm, but when combined with ceftiofur, it may as well have been a saline bolus, as the duo proved to be inert.
Other combinations also saw success, he said.
With a solid result in the lab, Dr. Ferris and his team took the treatment directly to the mares.
The team inoculated mares and allowed a biofilm infection to form, and then created 4 groups of horses: Those that were administered Tris-EDTA alone, ceftiofur alone, a combination of ceftiofur and TrisEDTA, and an untreated control group.
In the groups that received either monotherapy, some mares were able to eliminate the infection, but about half of them became chronically infected.
However, none of the 5 horses in the combination group were positive at the end of the study, suggesting that ceftiofur plus Tris-EDTA can offer a clinical benefit in affected mares. MeV
10 Issue 5/2022 | ModernEquineVet.com
Which Horses Are Better at Following Directions?
A new study shows that horses living in big enclosures and in groups of at least 3 horses are better at following directional indications from humans than horses kept in individual paddocks.
The results also indicate that familiarity to the person providing the indications does not matter for the horses.
Wild horses live in complex social groups and can move an average distance of 5 to 10 miles in a day. In contrast, domestic horses are kept in enclosures and groups varying in size and even in individual stalls or small paddocks.
Horses living in bigger fields or pastures are more active—they are free to move according to their needs—and, for example, to seek shade or shelter against wind and rain. When living in a group, horses can fulfil their social needs, interact in complex ways with many individuals, and have enough space to avoid unwanted interactions.
“It has been observed in earlier studies that horses with access to a pasture with other horses showed better learning performance and were less aggressive toward humans than horses kept in individual stables. Therefore, we wanted to explore whether horses' social and physical environment affect their responsiveness to human indications,” explained lead author, Océane Liehrmann, a PhD candidate, from the Department of Biology at the University of Turku, Finland.
The international research team from the University of Turku and the University of Helsinki in Finland, and the National Research Institute for Agriculture, Food and Environment (INRAE) in France, observed and analyzed horses’ responses to human indications according to the horses’ living environment. In addition, the researchers studied whether the horse reacted differently when the indications were given by the familiar owner or a stranger.
The researchers recruited 57 privately owned leisure horses from the Turku region in Finland to perform the behavioral tests.

In the research situation, the human informant— either the owner or the researcher—stood between 2 buckets, with a piece of carrot hidden in each of them. The horses were led by an assistant to stand in front of the human informant. The person would then move toward 1 of the buckets and gaze and point toward it to indicate that the horse should go to that bucket. The horse was then released and had the choice of going to the pointed bucket or the opposite one. If the horse followed the human's indi-
cation and approached the pointed bucket, the informant opened the lid and let the horse have the carrot. If the horse chose the opposite bucket, the informant caught the horse, and it did not get a carrot. The experiment was repeated 10 times per horse, and the researchers analyzed how many times the horses chose to follow the human indication over the 10 trials.
“Interestingly, horses living in groups of at least 3 individuals chose the pointed bucket more often than the horses living alone or in dyads. Similarly, horses living in pastures or big fields for at least 8 months per year followed the human indication more often than the horses living in stalls or small paddocks,” Ms. Liehrmann described.
In the study, the horses living in big pastures also lived in larger groups, whereas most of the horses living in small paddocks were alone or with just 1 other horse. Therefore, it was difficult to conclude
ModernEquineVet.com | Issue 5/2023 11 BEHAVIOR
Horses living in groups are better at following human indications that horses living in individual paddocks.
Image courtesy of Océane Liehrmann
whether social deprivation or the lack of space and enrichment has the greater impact on the results.
“However, domestic horses living in larger groups may benefit from stronger cognitive stimulation. Indeed, having the choice of interacting with various individuals promotes complex social situations from which the horses can learn and improve their sociocognitive skills. This may also explain why horses living in groups had better success in the task that involved communication with humans,” Ms. Liehrmann noted.
Context can impact the significance of familiarity to the humans.
The researchers also found that the horses’ success in the task did not depend on the familiarity of the person giving the indication. The success rate was similar whether the informant was the owner or a stranger. This is inconsistent with the findings from previous experiments based on the same population of horses. In the previous study, Ms. Liehrmann and her research group found that familiarity with the handler can affect the horse's behavior in novel situations.

“Our hypothesis is that the context may play a role when investigating the effect of human familiarity in human-animal interactions. In a more stressful environment, animals may rely more on a familiar
For more information:
https://link.springer.com/article/10.1007/s10071-023-01775-0
human than on a stranger, while in a positive context, where animals already feel safe and benefit from a food reward, the identity of the interacting human may matter less,” Ms. Liehrmann said:
“Overall, our study shows that the living conditions of the horses had an impact on their ability to follow human indications. The living and social environments of horses are a challenge and open to debate in the equestrian world. These results support the idea that offering an appropriate environment to horses by providing access to pasture and the ability to freely interact with their own kind could contribute to the development of their social behavior and extend to interaction with humans.” MeV
Early Removal of Osteochondral Fragments Could Be Helpful
Early removal of osteochondral fragments in the metacarpo−/metatarsophalangeal (MCP/MTP) joint could help prevent cartilage injuries in equine athletes (Equine Vet J. 2023 March 15. https://doi. org/10.1111/evj.13937 https://beva.onlinelibrary.wiley.com/doi/10.1111/evj.13937).
In this retrospective observational study, the researchers assessed the prevalence of cartilage injury in the joint and its association to fragment size, location, age and lameness in the MCP/MTP joint compared with fragments in the palmar/plantar compartment.
They also wanted to know if older horses with MCP/MTP joint fragments presented with more cartilage injury than younger ones.
They reviewed the clinical records of 823 MCP/
MTP joints in 640 horses that underwent arthroscopic fragment removal, noting the fragment size, intra-articular fragment location and cartilage injury score. They retrospectively evaluated synovitis in 157 joints.
They found cartilage injury in 28.8% of joints, but cartilage injury and lameness were not associated with fragment size. Age and lameness were associated with cartilage injury, as well as fragment location, with dorsal fragments being more likely to be associated with cartilage lesions than palmar/plantar fragments. They found no association between radiographic fragment size, presence of synovitis and cartilage injury, but the likelihood of a cartilage lesions increases with dorsal fragmentation, lameness and older age. MeV
12 Issue 5/2032 | ModernEquineVet.com
BEHAVIOR
Watch the video here
Liehrmann O, Cosnard C, Riihonen V, et al. What drives horse success at following human-given cues? An investigation of handler familiarity and living conditions. Anim Cog. 2023;1-12.DOI: 10.1007/s10071-023-01775-0
Traumatic Facial Wound in a Miniature Donkey
 By Megan Born, BT, AAS, LVT; Katherine MacGillivray, VMD, DACVIM; and Russell Freeland Jr, DVM, DACVS
By Megan Born, BT, AAS, LVT; Katherine MacGillivray, VMD, DACVIM; and Russell Freeland Jr, DVM, DACVS
A 32-kg male intact miniature 4-month-old donkey presented with extensive traumatic bite wounds over the left lateral mandible and maxilla after being attacked by a dog.

A large area of skin and muscles were no longer present after both the injury and necessary debridement. A portion of the masseter muscle, zygomaticus muscle, buccinator muscle and others were no longer intact. The nerves in this area that may have been affected by the trauma included the trigeminal nerve and the facial nerve.
The traumatized area was cleaned, lavaged, debrided and the patient was hospitalized for continued management of the wound and supportive care. Chest radiographs and ultrasound examinations of both the chest and abdomen were performed, and there was no evidence of trauma to other organ systems.
Bloodwork abnormalities showed:
• a lactate of 4.1 mmol/L, (ref. range 0.9 mmol/L);
• hematocrit of 33.60% (ref range 34-47%);
• WBC 17.9 K/uL (ref range 5.0-12 k/uL), (Neutrophils and platelets were high, hemoglobin, RBCs, and lymphocytes were low in the CBC);
• glucose 132 mg/dL (ref range 76-119 mg/dL);
• creatinine 0.7 mg/dL (ref range 0.8-2.0 mg/dL);
• total protein 5.0 g/dL(ref range 5.7-7.4 g/dL);
• albumin 2.8 g/dL (ref range 2.9-4.1g/dL);
• GGT 50 U/L (ref range 3-38U/L);
• AST 362 U/L (ref range 196-360 U/L);
• LDH 584 U/L (ref range 112-408 U/L); and
• CK 3235 U/L (ref range 120-320 U/L). The low hematocrit and platelet, hemoglobin and RBC values were likely in response to blood loss from the traumatic injury. The initial increased white blood cell count, with increased neutrophils and decreased lymphocytes was suspected to be due to a “stress leukogram” after the traumatic attack. Hemoconcentration was likely the cause of the increased liver values. Creatine kinase was increased due to the muscle trauma.
A bacterial culture was obtained from the wound, which yielded heavy growth of both gram-positive and -negative bacteria of mixed antimicrobial sensitivity that aided in selection of antibiotic therapy.
ModernEquineVet.com | Issue 5/2023 13
TECHNICIAN UPDATE Initial
hanging tissue Images courtesy of Megan Born
wound showing
Wound after debridement
Given the extensive damage and type of injury, wound management was focused on supporting healing by second intention.
Upon admission to the medicine facility, the colt’s heart rate was 86 beats per minute, temperature was 101.1° F, and the respiratory rate was 20 breaths per minute. The heart rate stayed in the range of 80-100 bpm over the course of the first day, and the respiratory rate decreased to 12 breaths per minute shortly after admission.
Silver sulfadiazine (SSD) was placed over the lesion.
A tetanus vaccine and 125 mg of SoluMedrol were administered at presentation. Amikacin and potassium penicillin were initiated for broad-spectrum antimicrobial activity and scheduled for serial IV administration. Flunixin Meglumine was also added to the treatment regimen.
A 16-gauge antimicrobial over the wire IV catheter was placed.
Crystalloid fluids of Normosol R with calcium, amino acids and dextrose were infused with a total of 4 L of fluids being given over the first 24 hours. The fluids provided circulatory support and replaced fluid losses from the large open wound. Dextrose and amino acids provided caloric and protein replacement as the donkey was not able to ingest feed material at this time.



A tracheostomy tube was placed several hours after admission due to the presence of increased respiratory effort, nasal edema and reduced airflow through the nasal passages. Prior to the tracheostomy air appeared to be passing predominantly through a hole in the dorsal aspect of the right nasal passage. Small amounts of water were offered.

14 Issue 5/2032 | ModernEquineVet.com TECHNICIAN UPDATE
Wound after granulation tissue started growing. SSD over large portion of exposed mandible
Out on a walk with stockinette and packing in place over wound
Showing edema over muzzle
Company in the stall!
The second day, the wound was lavaged with betadine and saline. Manuka honey and SSD were placed over the wound edges and the exposed portion of the mandible. The open area was packed with moist gauze, and a stockinette was placed over the cranium to hold the packing in place.
In addition to the fluids, partial parenteral nutrition was initiated with lipids for continued caloric support.
Butorphanol was added to the analgesic plan and scheduled for IV administration every 6 hours.
Small amounts of grass and hay were offered. A large plush stuffed horse was placed in the stall with the donkey for environmental enrichment, and the donkey stayed close to the plush horse over the next couple days.
Triglycerides were monitored throughout the donkey’s hospital stay to assess for hyperlipidemia and hyperlipemia, which are common in stressed or ill donkeys. Unaddressed hyperlipemia in donkeys can further complicate recovery from the initial clinical condition. This is due in part to fat deposition in the liver and secondary liver dysfunction, which can lead to other more serious clinical conditions that affect patient prognosis.
On day 2 of hospitalization, the triglycerides were 105 mg/dL (ref range 13-55mg/dL). To deter additional fat mobilization, heparin sodium and corn syrup were initiated to increase fat uptake by peripheral tissues and decrease risk of hyperlipidemia and hyperlipemia.
Over the next few days, the wound was managed by periodic lavages, debridement and bandage changes. Debridement required sedation. Osteostixis was performed with a 2.5 drill bit in the lateral exposed mandible to help provide a blood flow to the area and promote granulation tissue formation.


The exposed bone was kept moist with Manuka honey and SSD.
The donkey was able to eat some grass and hay and a senior feed slurry, although some of the feed material would become lodged in the bandage due to the large cheek area deficit.

Scheduled walks during which the colt was allowed to walk on his own within a large confined indoor area were performed to help the patient’s activity and wellbeing.
PPN and fluids were weaned slowly as the donkey was able to ingest more of his nutrient requirement. At discharge, the donkey weighed 28 kg compared with 32 kg on arrival.
The tracheostomy tube was left in place at discharge, and recheck appointments were scheduled for further wound care and assessment.
The donkey went home and watched the Olym-
ModernEquineVet.com | Issue 5/2023 15
Healthy granulation tissue filling in defect
Wound epithelialization
Final photo showing wound resolution and facial paralysis
Teaching Points
The successful practice of veterinary medicine involves treating the animal as a whole considering their behavioral and instinctual characteristics that contribute to their well-being. In addition to treating the primary wounds and secondary disease processes, this overall well-being of the animal is cared for with enrichment strategies. Environmental enrichment is defined as an improvement in the biological functioning of captive animals resulting from modifications to their environment.
Environmental enrichment for equine species in the hospital setting includes social companionship, the ability to find and eat forage, turnout or walking, and sensory stimulation, which can be provided by items such as jolly balls.
Caring for the animals well-being through environmental enrichment is particularly important for donkeys as they can become easily stressed in a hospital setting, which can lead to a negative energy balance and delay healing.
Donkeys prefer to be in a herd or with a bonded partner and providing this in a hospital can improve the overall wellbeing of the individual. This young donkey did not have a pasture mate, however; so the plush horse provided some initial company and hospital staff spent extra time with the donkey over the course of hospitalization. Scientific studies have also shown that environmental enrichment accelerates wound healing. The wound on this donkey was extensive necessitating there be no impedance to growth by concurrent illness brought on by inadequate environmental enrichment. A quick return to the donkey's home environment with at home care and periodic veterinary support further increased this young donkey’s morale improving the wound’s biological support system.
weeks after the injury. The age of the animal likely helped with the quick and efficient healing as well as the presence of a large blood supply to the cranium.
This wound would probably not have been a candidate for grafts due to the motion of the jaw and the extensive area involved. MeV
About the Authors
Megan Born, MS, LVT, has worked in the Internal Medicine and Critical Care Unit at Hagyard Equine Medical Institute since 2012. She is also a part time instructor for veterinary technicians at the University of Missouri Online. She enjoys showing reining horses and attends Clays Mill Baptist Church.


Kathy C. MacGillivray,VMD, DACVIM, attended the University of Pennsylvania and obtained her veterinary degree in 1998. Following her internship at Peterson and Smith in Ocala Florida from June of 1998 through June of 1999, Dr. MacGillivray returned to New Bolton Center for her internal medicine residency. After her residency, Dr. MacGillivray worked as an emergency clinician at New Bolton Center and for some local private ambulatory practices. Dr. MacGillivray joined the Hagyard Equine Medical Institute McGee Medicine Center in Lexington, Kentucky as an Internal Medicine Associate in 2003.
pics with his family during recovery after day 5 of hospitalization.
The wound granulated very well with second intention healing. A releasing incision was necessary mid-way through the healing process to preserve mobility, because the face was healing with a tight band of scar tissue that was restricting movement.
The extensive damage of the initial wound caused nerve damage with a sequela of facial paralysis requiring a permanent tracheostomy.
The final picture shows a completely epithelialized site with hair growth filled in. This picture is from 12
Dr. Freeland grew up in agriculture in southwest Louisiana. He attended Louisiana State University earning a bachelor’s degree in wildlife ecology and a Doctor of Veterinary Medicine. Trained as a surgeon, Dr. Freeland has a special interest in orthopedics and lameness in the performance horse. He is a board-certified large animal surgeon by the American College of Veterinary Surgeons. He is a member of the American Association of Equine Practitioners, American Association of Bovine Practitioners, and the American Veterinary Medical Association. Outside of practice, Dr. Freeland enjoys the outdoors, spending most of his free time hunting, fishing, flying and diving.

16 Issue 5/2032 | ModernEquineVet.com Shutterstock/nelelena
TECHNICIAN UPDATE
Minimally Invasive Technique Helped Lamb, Could Someday Help Foals
By Sheri Hall
A team of Cornell veterinarians successfully repaired a rare congenital defect affecting the vessels around the esophagus of a lamb using a minimally-invasive technique. Not only did this procedure save the sheep’s life, but it opens the door to treating other large animals, particularly foals, with this congenital defect.

Petey, a babydoll wether lamb, was born with a vascular ring anomaly, an embryonic vessel that turned into a ligament which wrapped around his esophagus, preventing him from swallowing. As a result, he was malnourished, and his growth was stunted. The team used a scope and minimally invasive surgical tools to dissect the ligament from the esophagus and then cut it.
“I’m proud of the procedure because it brought together so many specialists from the small and large animal medicine sides,” said Nicole Buote, DVM, associate professor of small animal surgery and the lead surgeon on the case. Dr. Buote, an expert in minimally invasive surgery, typically performs this procedure on dogs.
Four other Cornell veterinarians worked on the case. Katharyn Mitchell, DVM, PhD, BVSc, DACVIM (LAIM), chief of large animal internal medicine, initially learned about Petey’s case on an academic veterinary listserv. She coordinated the team and looked after Petey before and after surgery, while assisting in surgery by shining an endoscopic light down Petey’s esophagus that allowed the team to see the constriction clearly.
Eileen Hackett, DVM, professor of large animal surgery, provided her expertise in minimally invasive surgical techniques on sheep. Peter V. Scrivani, DVM, associate professor of diagnostic imaging, reviewed the imaging studies that allowed the Cornell team to identify the defect and plan the surgery. And Stephanie Hon, DVN, assistant professor of anesthesiology, managed the anesthesia for the surgery, which involved purposely collapsing part of Petey’s lungs to improve the field of vision for the surgeons.
Before the procedure, the team was not completely confident about Petey’s chances for recovery because veterinary literature reported that previous surgeries for this defect in alpacas resulted in many complications. But the minimally invasive techniques made a big difference for Petey, Dr. Mitchell said.
“Because of our minimally invasive approach, his recovery was extraordinarily smooth,” she said. “It was remarkable how quickly he recovered from anesthesia, and his lung recovered from the collapse. The biggest
problem we had was stopping him from overeating!”
After the surgery, the Cornell team built a special raised box to elevate Petey’s head while he ate. They had to use a muzzle to prevent him from eating his straw bedding.
The Cornell veterinary team hopes they will be able to help other large animals—particularly foals—with this defect in the future.
Petey is from the Avalon Nature Preserve, a 216acre preserve in Stony Brook, NY, that includes a restored farm. Preserve Director Kathy Griffiths noticed Petey’s struggles to swallow and gain weight after he was weaned. She reached out to a professor at the Tufts School of Veterinary Medicine, who examined Petey and posted his case on the listserv.
“We brought him home with a modified diet, but the prognosis wasn’t great,” Ms. Griffiths said. “When Cornell reached out to say they may be able to help, we figured was the best way to give him a fighting chance. We also really liked the idea of possibly helping other animals down the line.”
Typically, foals with this defect are euthanized.
“This really was a perfect storm of a wonderful owner who had the financial means to do this, and a dream team here,” Dr. Buote said. She hopes more people will recognize the technique can havae a good outcome.
In the meantime, Petey has fully recovered and rejoined his flock at the nature preserve. “By all visual signs, he is thriving,” Ms. Griffiths said.
That’s exactly the outcome the Cornell team wanted. “Petey is extremely lucky that his owners were motivated to get a diagnosis and provide a solution,” Dr. Mitchell said. “This was an opportunity to help a young animal have a normal life. It’s an exciting for us to be able to intervene early and make a difference.” MeV
The article originally appeared on the Cornell webiste and was edited for space and style. https://bit.ly/439o3RD-MeV
ModernEquineVet.com | Issue 5/2023 17
NEWS NOTES

Reach your veterinarians wherever they are, whenever they want. FOR ADVERTISING RATES AND INFORMATION, EMAIL ModernEquineVet@gmail.com Equine Vet The Modern CHECK OUT OUR NEW WEBSITE AT www.modernequinevet.com





















 By Megan Born, BT, AAS, LVT; Katherine MacGillivray, VMD, DACVIM; and Russell Freeland Jr, DVM, DACVS
By Megan Born, BT, AAS, LVT; Katherine MacGillivray, VMD, DACVIM; and Russell Freeland Jr, DVM, DACVS

















