Vincent Buscemi Partner and Head of Independent Health
Vincent Buscemi Partner and Head of Independent Health

vincent.buscemi@bevanbrittan.com
Letitia Winterflood-Blood Senior Associateletitia.winterflood-blood@bevanbrittan.com
 Jodie Sinclair Senior Partner Employment, Immigration and Pensions
Jodie Sinclair Senior Partner Employment, Immigration and Pensions





jodie.sinclair@bevanbrittan.com


Bevan Brittan is the market-leader in the provision of legal, governance and regulatory advisory services to businesses delivering and providing healthcare services within the UK and internationally. Our award-winning healthcare teams provide organisations with outstanding corporate, commercial, clinical negligence, litigation, regulatory, property and employment legal advice.

With years of experience and global exposure, Bevan Brittan’s healthcare teams have the expertise to support client’s endeavours anywhere in the world. Our reputation as a leading healthcare firm has taken us across the globe, working with a wide range of clients (from NHS bodies to independent health and social care providers, operators and developers as well as funders and investors) on a multitude of commercial health projects. Our in-depth practical and commercial knowledge of the challenges and opportunities of expanding overseas are second-to-none and a true benefit to our clients in the increasingly global healthcare market.

Welcome to the Arab Health 2023 edition of Healthcare World. It seems only five minutes ago since we were all in Dubai last year, but the wheels of healthcare turn far more quickly these days than ever before. There’s a fascinating mix of innovation, integration and automation at the event this year, and we’re proud to bring you some of the best.
Much of the focus will be on the Kingdom of Saudi Arabia and Vision 2030. The future organisation of global healthcare systems lies firmly in the Kingdom as they look for the perfect partners to achieve their ideal ecosystem. Dr Ahmed Al-Musaed from the Eastern Health Cluster explains how the Eastern Cluster fits into the KSA healthcare transformation, while companies such as Huma, Linea, Accumed and Methods Analytics outline their expertise on o er there.
It’s become increasingly clear that data analytics and integration holds the key to more rapid universal health care. Organisations such as Beamtree, Radar Healthcare, AdviseInc, Lyniate, Vamstar and Patients Know Best o er solutions to enable health ministries and providers identify focus areas and deliver optimum solutions.
But in any healthcare system, primary care has to be the centre of attention. Dr Patrick Wynn of Health Care First stresses that the correct use of data is the way forward to streamline the gatekeeper and argues that the Middle East is perfectly poised to deliver the ideal primary care system. Isabel Arango, Mott MacDonald’s Principal Healthcare Lead in the region, agrees with him, saying that spend on primary and preventive care is more e ective in improving healthcare outcomes. And Christina Sochacki, Senior Counsel at Al Tamimi & Co, outlines the key changes as the region moves towards a primary care model.
Among the innovations featured in this year’s Arab Health are solutions in FemTech. Since 2016 this has been a growth area - companies now recognise that
 Sarah Cartledge Group Editor
Sarah Cartledge Group Editor
women hold the healthcare knowledge and also the purse strings when it comes to family health. Lawyers Bevan Brittan examine the rise of FemTech and suggest it shouldn’t be dismissed as a niche area because the benefits for public health are substantial.

We also examine the focus on Net Zero and Net Zero Carbon in other parts of the world, looking at the importance of reducing carbon emissions which can be high in hospitals and clinics. While it may not be a key consideration in the Middle East at the moment, it’s a fascinating area which both Mott MacDonald and Currie & Brown shine a light on.
Last but not least is the Metaverse, a shi in how healthcare can interact with technology. It has the means to impact healthcare by taking advantage of artificial intelligence (AI), augmented reality (AR), and virtual reality (VR) to improve patient outcomes. The Future Health Summit at the Museum of the Future is an exclusive, fully immersive event for senior government o icials and CEOs in healthcare, examining the future of health and delving deep into the amazing possibilities of healthcare in the Metaverse.
There has been a huge leap in the development of technology to enable clinicians to deliver care remotely via AR. A keynote speaker is Dr Timothy F. Witham, Johns Hopkins Professor of Neurosurgery and Orthopaedic Surgery, one of the surgeons who performed the. world’s first augmented reality spinal surgery. This exciting event is just the beginning of new possibilities, revealing how healthcare can evolve once we have a grasp on the right digital solutions.
So it’s incumbent on all us involved in the sector, from government ministers to health o icials, from so ware developers to clinical entrepreneurs, and most importantly, the providers themselves to identify the optimum solutions to deliver futuristic healthcareand incorporate them sooner rather than later.









26 Healthcare World Editor Sarah Cartledge speaks to Rebecca Stubbs, Principal Net Zero Carbon Consultant Mott MacDonald, about the NHS road to Net Zero
30 Sarah Cartledge speaks to Dr Ali Haydar, Chief Medical Officer, Aman Hospital in Qatar, and Alistair Russell at Imperial Private Healthcare about the International Affiliate Network
36 Healthcare World’s Sarah Cartledge speaks to Helen Featherstone, General Manager of GMC Services International about the importance of a comprehensive regulatory framework
38 The global FemTech market is valued at $25bn and projected to rise by 15 per cent in the next few years, so it deserves greater attention, say Vincent Buscemi and Letitia Winterflood-Blood of Bevan Brittan LLP
42 Health systems strengthening and the UK

44 As the UK’s National Health Service approaches its 75th birthday, International Director Ged Byrne discusses new ways for global health systems to access its experience and knowledge via the NHS Consortium
46 Inclusive use of technology can improve patient outcomes and service quality, says Alex Kafetz, Director of International Projects Beamtree
50 The supply chain revolution - Mat Oram of AdviseInc discusses whether improved procurement procedures lead to better patient outcomes
52 Primary and preventive care are the fundamental building block of healthcare systems, says Isabel Arango, Mott MacDonald Principal Advisor and Regional Healthcare Consulting Lead
54 Automation can create a better healthcare ecosystem, Praful Mehta CEO of Vamstar tells Healthcare World
56 Actively choosing to make decisions informed by data is the way forward for healthcare, say Simon Swift and Richard Oakley of Methods Analytics
60 Virtual Reality is a valuable tool for better hospital design, say Nick Ainscough, Regional Design Technology Lead, and Nick Clarke, 3D Visualiser, at Arcadis IBI Group

62 The challenge of providing infrastructure that responds to and mitigates the impact of our changing climate is a key focus for future healthcare delivery, say Currie & Brown’s Helen Pickering, Global Head of Healthcare, and Adam Mactavish, Global Sustainability Lead

64 Feedback Medical enables clinical data to travel with the patient, says CEO Dr Tom Oakley
67 Group Editor Sarah Cartledge explores Lyniate’s new Partner Program initiative, speaking to regional partners Mozon, Virtus Informatics, Aamal Medical and YMH-IT Solutions about their place in the ecosystem
70 Patients can now receive the same standard of care in a nursing home or their own home, says Ian Chambers, CEO of Linea
74 Paul Johnson, Founder and CEO of Radar Healthcare, discusses how organisations can improve patient safety through technology
78 Healthcare World CEO and Director of Consultancy Emma Sheldon MBE examines the ways in which healthcare businesses can grow post pandemic
80 Advanced Clinical Solutions director Josie Winter explains to Healthcare World how international organisations can enhance patient safety
83 The importance of sharing healthcare data - Dr Patrick Wynn
84 The Midlands region is home to one of the most important life sciences ecosystems in the UK says Shaz Chaudhary, Director Midlands Region, Department for International Trade
86 Improving revenue cycle management in the Middle East - Managing Director Mohammed Aldar outlines the role of Accumed in cementing its role in the future of healthcare
88 Clinical trials are an effective method to know if a new treatment is safe and functional in people, says Mike Failly, Founder and Managing Director of Zanteris

90 Resilient and Responsive Healthcare Systems - Leveraging the Power of CDVC (Concurrent Digitalised Value Chain) is key, say Dr Hesham Dinana VP EFESO MEA and Dr Mohamed Fayek Director– Head of Healthcare and Life Science EFESO MEA
94 Opinionated – Preparing for the next pandemic, Steve Gardner, MD Healthcare World

CO-CREATING HEALTHCARE FUTURE

40+ Years of Experience


37 Offices
75 Countries
90% Client Retention


Aligning medical education with the needs of public health will help the Kingdom of Saudi Arabia plug the workforce gap, says Mansoor Ahmed, Colliers Executive Director (MEA) and Head of Development Solutions
The economic transformation and diversification plans under Vision 2030 are expected to spur demand for higher education. However, the current enrolment distribution in public universities lacks alignment with the requirements of the employment market, with significant
enrolment in humanities, Islamic studies and behavioural sciences.
Colliers expects the demand to shi from traditional o erings to Technology, Artificial Intelligence (AI), Robotic Sciences, Nuclear Energy, Sustainable Energy, Renewable Energy, Solar Energy etc. Additionally, the demand is
expected to shi toward evidence-based Research & Development (R&D) studies taking into consideration the economic transformation agenda in Vision 2030 and the changing market demand, rather than traditional fields of study, to reduce the “mis-match” of degrees attained and the requirements of the employment market.
Colliers also expects a significant increase in o ering in the health, hospitality and SME sectors. Furthermore, the Saudisation drive in various sectors will drive demand for higher education. Again, Colliers expects the demand in each to be focused on sub-specialties rather than traditional degree courses.

One of the key, yet o en ignored, requisites to provide quality healthcare service is the availability of human capital. Without the availability of qualified and specialised human resources, even the best medical facilities with the most advanced medical equipment are not enough.
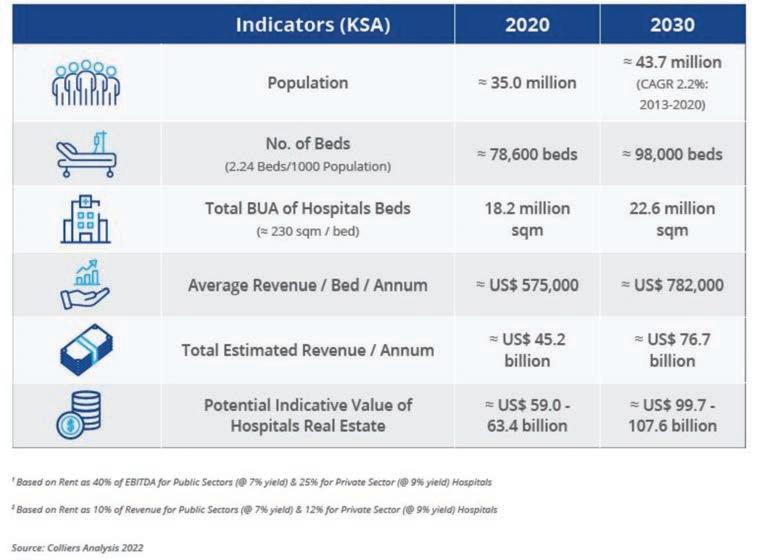
By 2030, due to an increase in population, which is expected to reach 45m, and the requirement of new healthcare facilities, an additional 19,000 to 20,000 beds will be required based on the KSA’s current average of 2.4 beds/1,000 population respectively.
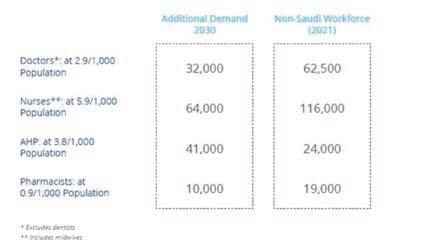
There will be additional demand for doctors, nurses, pharmacists and allied health professionals (AHP).
The demand will be even higher as a part of the Saudisation drive in the healthcare sector as the majority of these jobs must be filled by Saudi nationals. Presently, 63 per cent of doctors, 47 per cent of dentists, 57 per cent of nurses, 18 per cent of AHPs and 61 per cent of pharmacists, a total of around 223,000 medical professionals, are expatriates.
Furthermore, as the Kingdom embarks on the adoption of new medical technologies resulting in demand moving from traditional courses to advanced medical education, additional facilities will be required. Artificial Intelligence (AI), data analytics, robotic medical sciences,

“One of the key, yet often ignored, requisites to provide quality healthcare service is the availability of human capital”
Mansoor Ahmed, Executive Director (MEA) and Head of Development Solutions MENA Region at Colliers
Between 2015 and 2050, about 21m children will be born in KSA, creating demand for healthcare facilities and services relating to mother and childcare, such as obstetrics, gynaecology, and paediatrics.
There is not only a huge demand and supply (capacity) gap but also a definite capability gap. The short-tomedium term areas are mother and child health, geriatrics, oncology and long-term care. Life expectancy in KSA has also increased. These changes will lead to increasing requirement for a larger number of long-term care facilities.
Saudis have traditionally gone oversees for healthcare, and it is Colliers’ opinion that they can be targeted if the same hospital brands where they have this treatment can establish branches in KSA.

genome sequences and short courses will enhance the skillset of doctors, registered nurses (RN) and AHPs, enabling them to opt for specialised positions.
Saudi Arabia will need an additional 32,000 doctors by 2030 and, if we add replacement of expatriate doctors with the Saudi national doctors, it will need 62,500 additional doctors in additional to 32,000. A total of 95,000 doctors is required to tackle critical bed shortages and meet the needs of its growing population, experts have warned.
Significant increases in nurses, technicians and medical sta are essential to plug the Kingdom’s chronic bed shortfall with more incentives, such as easing visa regulations, being suggested as ways of attracting and retaining overseas expertise.
There is a direct correlation between number of beds and medical sta . Based on a Colliers estimate, by 2030 KSA will require an additional 200,000 medical sta as follows:
There are two ways of filling this gap — producing more doctors and nursing sta locally, and attracting medical sta from other Arab and Asian countries. However, to do this, KSA needs to look easing its visa rules and regulations. One of the main challenges faced by private operators in the region, including KSA, is attracting and retaining quality sta , prompting health-care providers to ‘poach’ doctors from the local market rather than hiring from abroad. With a limited pool of established physicians, their salaries have witnessed exceptional growth, to an extent that it is negatively a ecting the profitability of hospitals/ clinics in KSA.
A large number of doctors, nurses and paramedical sta in KSA migrate to Western countries a er a few years due to better opportunities and training facilities. In addition, the current Saudi regulations for recruitment further increase the sta cost due to limited available resources.
The growing and changing composition of the population will dictate the types of bed required.
The focus should be not simply on increasing the number of beds, but in creating more centres of excellence dedicated to day-care surgery, which will reduce demand for bed space.
The government’s role is extremely important in establishing careerfocused educational institutions, such as medical and nursing colleges, to increase the supply of local medical professionals and to drive qualified Saudi talent into jobs. Moreover, to overcome the supply gap, the government needs to provide funding to the private sector and improved employment regulations to be able to attract qualified resources from abroad.
With more targeted medical education within KSA itself, there should be a plentiful supply of homegrown talent to take up the slack and drive the Saudisation of the healthcare system.





fits into the KSA healthcare transformation
Vision 2030 is a comprehensive plan for reform of the entire economic structure of Saudi Arabia. While aiming to reducing the Kingdom’s reliance on oil as the main income stream, it has also been put in place to decrease public spending by inviting partnerships with the private sector.
For healthcare in particular, Vision 2030 has created the possibility of an entirely new healthcare system. By reorganising its structure and separating the regulator from the provider, more than 21 Clusters will be formed that will essentially be Accountable Care Organisations or ACOs. Healthcare leaders across Saudi Arabia have been examining ways to transform their existing structure into a modern, digitally enabled system that will change the way healthcare is provided while allowing its population to manage its own health via new and innovative methods.
The o ering of Vision 2030 is to deliver a comprehensive transformation for the whole country, focusing on the existing governmental processes, including all services such as education, hotels, municipalities, and housing. There is a massive focus on optimising and transforming the services delivered for these activities.
Prior to Vision 2030, the governmentbased health care system formed the main part of the sector, with 60 per cent. The second was the military and the nongovernmental part, and the third was the private sector at around 20 per cent. The goal of Vision 2030 is to transform the government practices and increase the private sector participation in the health sector to more than 55 per cent.
The government sector is led by the Ministry of Health which used to be the regulator as well as the provider under one entity. With Vision 2030 the plan is to separate the regulator from the provider, so the Ministry of Health will focus more on the regulatory side and will transform into the National Centre for National Health Insurance, separate from the Ministry of Health. The providers, which have more than 250 hospital and 2,200 primary care centres, will migrate under the umbrella of the health holding company and divided into some 20 regional clusters, along the geographic distribution of the country.
The Eastern Cluster was the first to launch in 2017 with 22 secondary and tertiary hospitals and 133 primary healthcare centres which are public facilities. The university medical school teaching hospitals and the health care systems of the three administrative arms, the National Guard, the armed forces, and the Minister of Interior have their own health care systems. And then there is the private sector.
The Eastern Cluster developed its two year business plan in 2018 and developed a five year long term strategic plan which was approved by His Excellency the Minister in 2020.
The vision for the cluster is to transform into a world class health care provider, creating an integrated practice with one medical city, 21 secondary hospitals and a specialised hospital, and 133 primary care centres. This arrangement will begin to transform into a comprehensive, accountable care organisation for roughly around 4m population in the Eastern Province.
The ultimate goal of the cluster is to develop and transform to become an accountable care organisation based on total transformation, population health management, partnership with the private sector and NGOs locally and internationally in cooperation and delivery of hospital and primary care services, and optimising our capital planning and investment for the long term. It will become responsible for the overall population health, including prevention. This requires us to think di erently about the delivery of care from facility-based delivery to population health-based delivery, running facilities and running accountable care for the beneficiaries that we are responsible for.

Digital transformation has been an essential component of driving this change. There are a number of dimensions we need to consider in putting all these providers under one umbrella, creating the sense of accountability not only for the people coming to their doorsteps, but also for the overall community. Integrated practices are key, including community and primary care centres especially following in-hospital care.
Digital transformation has been used as an important enabler in the past to provide health information for health systems.
It’s essential that digital also transforms the way we conduct business, not only through virtual care and telemedicine, but also relying on digital health for mobility, personal devices and more that can enforce the self-care goal that we are trying to achieve with our population.
The focus on prevention has been growing, especially around the screening programme for most chronic diseases. We are increasing accessibility to the system for people, aiming for a unified health record and a single form for appointments and follow up. In addition, we are moving to our service line practices, such as bringing specialist care outside the referral system
into a closed system to involve community practices by connecting through a single platform and a single team.
The Eastern Cluster is taking the lead with regard to transplant services, especially for pancreas, liver and kidney. We would like to have more room for cancer diagnostics and widen our ground for preventative screening. We would also like to maximise our capacity for paediatric and adult care, as well as learn more about outpatient diagnostics and therapeutics because that is the modality for today’s cancer care. Equally, the associated home care will help us manage our hospital beds. There is also
a transformation required to move from interventional cardiology to more imaging cardiology, and we plan to rely more on primary care for patients with hypertension as well.
Ultimately, the Eastern Cluster will be a leading provider of healthcare services through KSA, striving for innovation, accountability and delivery in its provision to the community.

Walid Hallassou, Vice President, Healthcare MENA, Huma Therapeutics, tells HW Editor Sarah Cartledge why there has never been a better time to embrace digital health

Digital technology played a significant role in the hugely successful football World Cup hosted by Qatar a few weeks ago. Not only in the emotive VAR decisions but also in providing rapid player analytics, crowd metrics, underpinning security, media streaming and visible sponsorship. The tournament reflected the extent to which the region has embraced digital technology for sport and entertainment and the same is happening in the healthcare sector too.
According to a McKinsey & Co report from January 2023, the degree of digital penetration among Middle East consumers
over the previous six months is equal to that of leading European and North American countries. Within digital devices, Middle East users overwhelmingly favour mobile apps as their preferred channel. An earlier McKinsey & Co report also states that smartphone penetration rates in the UAE and Saudi Arabia (KSA), where more than 65 per cent of the population is under 30 years of age, are among the world’s highest at around 93 per cent. This smartphone landscape provides the optimal setting for Huma’s digital platform.
Huma has worked in the Middle East since 2021. The company signed its first agreement with Mediclinic Middle East in the United Arab Emirates (UAE) and together they provided the Abu Dhabi Department of Health with the digital tools
to care for high-risk patients during the COVID-19 pandemic in an approach known as Remote Patient Monitoring (RPM).
“Most people in the region have mobile phones,” says Walid Hallassou, Huma’s Commercial Vice President for Healthcare in the Middle East and Northern Africa. “Our platforms use the patient’s mobile phone, wearable devices and other sensors to provide doctors with a stream of data on their health. The data enables healthcare teams to monitor patients’ evolving symptoms, advise on what care is required and alert them to when a visit from a clinician or hospital admission is needed.”
Being able to monitor a patient’s health and disease indicators from the comfort of their own home is particularly attractive for chronic non-communicable diseases (NCD) such as heart disease and diabetes, which are on the rise in some Middle East countries. For example, NCDs are now responsible for 73 per cent of all deaths in KSA. Taking measurements via RPM not only means that patients are spared unnecessary visits to a clinic, but that clinician time is better managed by seeing only those patients whose measurements require in-person assessment.
“Instead of building more clinics or hospitals, we can match patients with a platform to help them while they are at home, at work, or even travelling, because collecting information can happen from anywhere,” explains Walid. “A diabetic patient, for example, is prompted by our app to take their blood glucose every morning, to record weight every week and to answer questionnaires. Maybe every month they have a reminder to go and see a doctor but, instead of doing the majority of assessments physically, we’re taking everything we can onto the digital space. This limits burdensome clinic visits and evidence shows that it helps patients stay compliant with a treatment plan.”
Developing new solutions to tackle NCD is one of the priorities of KSA’s Vision 2030. A new Health and Wellness RDI (research, development, and innovation) will be announced later this year with countrywide aspirations stretching over the next two decades. The RDI will include a focus on disruptive
digital healthcare, health equity, and cutting edge biotech/pharmaceutical technologies.

“There are huge challenges that come with any major transformation,” says Walid. “Vision 2030 divides the Ministry of Health into three di erent organisations that are completely independent. At Huma, we see it as a great opportunity to be part of these reforms and we are currently talking to the Ministry to understand how our experience might help them in the design of an optimal digital roadmap to serve healthcare requirements.”
Established in 2011, Huma has longstanding experience in the field. Its award-winning digital-first platforms support a global network of patients, reaching more than 27m people via more than 3,000 hospitals and clinics. With 90-95 per cent patient adherence rates, Huma has demonstrated that its digital platform can double clinical capacity and reduce hospital readmission rates.
Huma is well-equipped to operate in an environment where insurers must be persuaded of the value of an intervention because its digital platform is underpinned by robust clinical and scientific research publications and its scientists have contributed to more than 50 peer-reviewed studies to-date. Its most recent scientific study, in collaboration with a department from the University of Cambridge, UK, provides evidence for the high engagement and long-term retention of participants with Huma’s app-based monitoring system. This is because Huma understands people. Its platform has been built on a deep clinical knowledge of complex patient needs and how people engage with technology.
Importantly, Huma’s platform is modular and therefore highly flexible,

enabling partners to rapidly configure some of the most complex digital health solutions. “We pride ourselves on being agnostic,” says Walid. “Our platform is agnostic to diseases, agnostic to devices, agnostic to clouds and agnostic to hospital or clinical information systems. For example, there are many good organisations that have a great app to monitor diabetes, hypertension or multiple sclerosis, but Huma has created a digital tool whereby the clinician can configure any disease. The advantage is that one tool can manage a population that has comorbidities or a range of diseases. Our solution is also cloud agnostic too, which means that patient data can stay hosted within the user’s system.”

Healthcare systems with active clinical research programmes have better patient care outcomes. In January, Huma announced that it has acquired Alcedis GmbH, a market-leader for data driven clinical research and technology. Through the acquisition, Huma is forming an advanced clinical trials division o ering digital solutions across the entire clinical development pipeline, from early stage trials through to Phase IV hybrid and fully decentralised, or virtual, trials.
“Healthcare advances through clinical research and this evolution in Huma’s business model will redefine clinical trials,” says Walid. The company will now o er a one-stop shop for remote access, data, logistics and the execution of clinical trials with advanced digital technology.
World Cup Qatar 2022 was voted the ‘best World Cup this century’ in a survey by the BBC, amasssing 78 per cent votes. Just as it has set a new standard for possibility in World Cup football, there is an opportunity for the Middle East region to show what is achievable in the innovative application of digital technology to healthcare. For Walid, “Huma’s platform can be used in a variety of di erent ways, and we are excited to see how such a forward-looking region leverages it.”
“The advantage is that one tool can manage a population that has comorbidities or a range of diseases”
Walid Hallassou Vice President, Healthcare MENA Huma
Patient engagement with their own data is vital to help them manage their own health, says Dr
Mohammad Al-Ubaydli, CEO and Founder of Patients Know BestOne of the current buzz phrases in healthcare is ‘putting the patient at the centre’ of any solution, including provision of care. But this is increasingly di icult when patient data is o en in many di erent locations and not aggregated in any way. If treatment take place in one facility discrepancies shouldn’t arise, but when it’s anywhere between a primary care facility, a private or a public hospital or clinic, and even individual therapists across several continents, it can lead to knowledge gaps and treatment delays.
In other circumstances, it can be down to di erent reasons. For Mohammad, he
found that having a rare disease meant he o en knew more about the condition than the specialist he was seeing. He realised that if there was one repository for all the requisite information, it would make for a better interaction with the consultant, helping both to manage his condition in an optimum manner.
It led him to design Patients Know Best (PKB), a social enterprise and technology platform, to help health and social care providers bring together patient data, along with the patient’s own data, to create one secure Personal Health Record (PHR) for the patient. It is the first PHR to integrate with

the NHS App, making it more accessible to more people across the UK.
As a trained doctor and so ware designer, Mohammad has been able to leverage his medical knowledge to design a system that incorporates all patient requirements, from appointment letters and test results to multi-disciplinary care plans. It shares medical information (such the outcome of GP appointments or recent test results), so that any clinician can better understand the required care and support.
In the same way, patients can share all or parts of their record with family, carers and other healthcare professionals, anywhere in the world. It enables patients to own a copy of all their health information, to understand it and use the information to make shared decisions with healthcare professionals. In addition, it allows patients to play an active role in their health and wellbeing through specially designed tools to monitor and track their health condition.
“This way care is centred around patients by default,” says Mohammad, who started his training as a GP in the NHS.

Surprisingly, many older doctors are in favour of an integrated service such as PKB. According to Mohammad, this is because they are confident in their knowledge base and understand others have useful knowledge, like the patient. “We found it was the junior doctors who were threatened by it, but the consultants were very supportive.”
In the UK, Patients Know Best (PKB) integrates local digital transformations with the national infrastructure of the NHS App and login. Since 2013, more than 13m patient records have been shared across every county in the United Kingdom, with over a million patients using the platform. PKB is also present in the Netherlands and the Republic of Ireland and has data centres
in the UK and the EU. They also have a pro-bono deployment in South Africa’s top cancer hospital which went live last year.
Currently the company is aiming to set up data centres in each of the Gulf states, working directly with the government to implement the system throughout the healthcare structure. “For a government trying to change attitudes in healthcare, using a system like PKB that encourages patients to manage their own healthcare and giving them the tools to do so is the easiest way forward. Universal health coverage or UHC will only be achieved if those who can engage with technology do so, leaving more traditional methods to those less able.”
Until now, he considers that most governments have looked at data as a compliance exercise, but now they realise that data is the key to unlocking their healthcare issues.

A hospital in the Netherlands built the country’s blood cancer app on top of PKB, and in the UK the NHS uses PKB in their back end. “Any innovation from anywhere can be deployed and that’s the model we want to give governments across the Middle East,” he says. “I see a lot of my job as liberating the data to the person who has the solution.”
UHC is one of the targets set by the nations of the world when they adopted the 2030 Sustainable Development Goals (SDGs) in 2015. For governments, achieving the ideal of all citizens with access to public health without financial hardship is looking more challenging as we near 2030. However, digital health is driving change across the world and the global population is far more accustomed to managing their lives via digital services than ever before.
“Families drive a patient behaviour change,” Mohammad adds. “There is usually a ‘Chief Medical O icer’ in each family, and they are the repositories of that information. So it’s important to engage with everyone so they can keep an eye on their health and give valuable information to clinicians when it’s required, rather than for example a GP appointment being a ‘data dump’”.
In his opinion, the smart phone is a great driver of change – he thinks FemTech is a good example of women leading the way to manage their own health via apps on their phones. “That’s what structurally changes the cost of care delivery and also the quality,” he says. “80 per cent of healthcare spending is determined by what the patient does. If they have appendicitis, what the surgeon does is what matters. If the patient has diabetes, what the patient does is what matters. We have to move from compliance to engagement to activation. That’s what’s going to structurally change care delivery in the 21st century.”
From this experience, Mohammad understood that patients not only have the power to change their own health destinies but they also hold the key to a more sustainable and responsive healthcare system which better meets the needs and expectations of citizens. However, to make this a reality, they need access to and accountability of their health records.
Greater access to the most appropriate care and support services should be the norm, patients can therefore feel empowered to manage their own health. In a world where healthcare professionals not only have more time, but access to reliable patient information from all providers at the point of care; everything from lab results, care plans, discharge summaries, diagnosis information and monitoring data, with the ability to engage with patients online, early warning signs can be spotted and addressed before problems escalate. However, that world isn’t confined to the future. It’s the reality now and it’s happening across the world with Patients Know Best.
“We have to move from compliance to engagement to activation. That’s what’s going to structurally change care delivery in the 21st century”
Dr Mohammad Al-Ubaydli CEO & Founder Patients Know Best
Transformation in the healthcare sector represents more than just technical advancement – it represents an opportunity to deliver progress for patients. This drives us forward.
We’re focused on opportunities to use data and technology to:
• help services recover from the effects of the COVID-19 pandemic
• reduce pressure and deliver benefits for the workforce
• improve population health, so people enjoy longer, healthier lives
To get started email analytics@methods.co.uk

Government owned Skåne Care is the international gateway to the skills, services, and expertise o ered by the Swedish public healthcare and dental care system. Sweden is in the top rankings internationally for having the consistently highest level of quality in healthcare as well as the longest life expectancy globally. We are also the number one EU innovation leader.

We o er comprehensive worldclass healthcare for international patients, training programs for medical professionals, and healthcare consulting services for clinics, hospitals, and administrators.
Our healthcare managers have over time developed the Swedish model – and are ready to take your healthcare to the


next level. We o er you a government partnership where we bring the learning points from the Swedish model. Skåne Care pride ourselves in understanding your needs and adapting advice to your situation.
Whether you seek to ambitiously upgrade your entire healthcare system or focus on a single task e.g., establishing a stroke pathway, we can help. Our healthcare consulting services can firstly help you
enhance quality, secondly increase e iciency, and thirdly cut costs within existing services.
As part of the day-to-day services as a healthcare provider in Sweden we understand the challenges you face and provide hands-on advice to ensure cost e ective transformation. We give you PowerPoint-free consulting, focusing on ensuring strategy gets implemented for real.
Whether you just need a second opinion on your plans, a study visit to get inspired by another country, leadership training for your management team or some clinical upskilling for your sta … or you need comprehensive on-site support on a larger project.
Sweden can help! bjorn.almer@skanecare.com
Christina Sochacki, Senior Counsel, Head of Healthcare & Life Sciences, KSA at Al Tamimi, looks at key changes in UAE and KSA
According to the World Health Organisation, primary healthcare is a core basis of a successful healthcare system.
The intention in the UAE and Saudi Arabia is that primary healthcare facilities will be able to better guide the care of patients, while reducing the burden on specialist and emergency medical services, arguably reducing the costs of the healthcare industry on the economy.
Across the region, healthcare systems are faced with a rising demand on services, due to a rapidly expanding population
caused by natural growth and a positive net migration. One of the challenges of the current model of care is the lack of su icient prevention programmes integrated into care plans and patients’ direct access to services and specialty care, leading to an increase in the inappropriate use and oversupply of services. At present, patients opt to approach specialists directly as the first point of care for general medicine needs and, in some cases, approaching more than one facility and specialist (‘doctor shopping’), placing an unnecessary burden and expense on the healthcare system.
Set out below, policy changes in Abu Dhabi in the UAE that were aimed at driving primary care in the Emirate are as follows:
1. Abu Dhabi
With e ect from 1 January 2018, the Department of Health – Abu Dhabi (‘DOH’) stopped issuing licences for general clinics, with limited exceptions. All licensed general clinics had until 20 December 2018 to change their facility type to meet the requirements of a primary healthcare centre, or another type of specialist healthcare facility.
This change put into full e ect the DOH Standard for Primary Health Care in the Emirate of Abu Dhabi (‘Standard’), which is applicable to all healthcare providers, both public and private, wishing to provide primary healthcare in the Emirate of Abu Dhabi. The Standard, which was issued in August 2016 and

updated in September 2022, defines the requirements for ‘Primary Healthcare Services’ in the Emirate of Abu Dhabi, aims to improve patient access to quality and safe primary healthcare services, and sets the minimum requirements and specifications that healthcare providers are required to comply with in providing healthcare in a primary care setting. These changes reflect the authority’s initiative to create a more patient-centric care model, ensure continuity of care, and reduce fragmentation in the healthcare system.
Excluding certain exceptions (clinics located in construction sites, hotels, schools, sports and social clubs, and companies), DOH no longer issues new licences for ‘general’ healthcare clinics in Abu Dhabi. Moreover, all licensed specialised clinics and medical centres wishing to practise family medicine must meet the Standard and submit a ‘change in type’ application in order to change
the healthcare facility type to a ‘Primary Health Care Centre’. Likewise, hospitals in Abu Dhabi wishing to provide primary healthcare services must request to include such services under their clinical support services list approved by the DOH.
Clinics that provide only general healthcare from general practitioners will have to employ a specialist or consultant to lead the care. Such supervising physician must be a consultant or specialist in family medicine, internal medicine or paediatrics, depending on the local population demographics served and in accordance with DOH health professional licensing requirements. It is expected that primary healthcare facilities will provide advanced levels of treatment led by a specialist or consultant, guiding the patients towards receiving the best care.
The DOH has determined that primary healthcare services in Abu Dhabi comprise a range of services provided in support of preventive, curative, and palliative healthcare. Services that must be provided in a primary care setting include:
• family medicine, including planned and unplanned primary care services
• chronic disease management
• healthcare screening and prevention services
• vaccinations and immunisations
• non-communicable diseases management
• communicable diseases management
• unplanned and urgent primary care services, including, initial management, stabilisation and transfer of any presenting emergencies to an emergency department, as appropriate
• a pharmacy on site (this is discretionary if one already exists within 10 minute walk of the facility)
• access to basic on-site diagnostic services.
There is also a list of additional services that may be provided, if required by the local population.
DOH’s ultimate aim is to have a licensed family medicine care provider within each precinct in Abu Dhabi. As a result, the DOH anticipates that there will be improved patient access to quality and safe primary healthcare services.
In 2016, Saudi Arabia announced Vision 2030, an ambition plan for reform across the Kingdom and seeks to create a more diverse and sustainable economy. The Vision 2030 strategic objectives include a number that are dedicated to healthcare, including targeting the privatisation of 290 hospitals and 2,300 primary health centres by 2030. Through the various Vision 2030 programmes, the Kingdom seeks to introduce new strategies to fulfil public health needs through insurance-based financing and increasing private sector participation.
Included in the goals of the health sector reform is: improving integration and continuity in service provision by developing the primary care, reforming and restructuring of primary health care, and updating and expanding primary care across Saudi Arabia.
We can expect to see a number of licensing, regulation, and reimbursement changes.

On 12 July 2021, Law No. 13 of 2021 establishing the Dubai Academic Health Corporation (‘DAHC Establishing Law’) and Law No. 14 of 2021 amending some clauses of Law No. 6 of 2018 pertaining to the Dubai Health Authority (‘DHA Amendment’) was issued in Dubai. The goal of these two pieces of legislation was to shi the operation of DHA governmental facilities to the Dubai Academic Health Corporation (‘DAHC’), strengthen Dubai’s leadership in medical education and scientific research through the DAHC, and position the Dubai Healthcare Authority (“DHA”) as the unified regulator for the emirate of Dubai, including its free zones.
The DAHC will not take over the functions of the DHA; the two entities retain separate authorities. It is

“The intention in the UAE and Saudi Arabia is that primary healthcare facilities will be able to better guide the care of patients”
Christina Sochacki Senior Counsel, Head of Healthcare & Life Sciences, KSA Al Tamimi & Co
intended that the DAHC will operate and manage public sector services, with the DHA retaining its existing regulatory functions. In accordance with the DHA Amendment, the DHA will coordinate with the DAHC when preparing and supervising the implementation of strategies necessary for improving healthcare services in line with the Strategic Plan of the Emirate. The DHA will also coordinate with the DAHC when preparing a database for the health sector, healthcare services, and patients, as well as updating and developing the same on a regular basis.
Under the DHA Amendment, the regulatory purview of the Dubai Healthcare City (“DHCC”) towards healthcare facilities and professionals registered in the DHCC was transferred to the DHA, as of 24 October 2021. The DHA now replaces the DHCC Authority as regards health regulation responsibilities and competencies including, but not limited to, licensing of healthcare professionals and healthcare facilities in the DHCC, supervising and inspecting healthcare professionals and facilities in the DHCC, and managing patient complaints in relation to DHCC healthcare professionals and facilities. The transfer of the public health system including all assets to the DAHC was completed by 31 December 2022. The DAHC took control of the public health budget from the Department of Finance of Dubai on 1 January 2023.

The DAHC Establishing Law recognises the DAHC as an academic health system, with financial and administrative independency. The DAHC seeks to strengthen Dubai as a global leader in medical education, research, and scientific innovation as part of the broader strategy to strengthen the knowledge economy in Dubai. Furthermore, the DAHC seeks to enhance the capabilities of Dubai’s healthcare sector to prevent and treat diseases and epidemics. The new corporation also aims to develop educational and professional programmes for healthcare personnel and promote strategic public-private sector partnerships to meet its objectives. The DAHC will also strive to attract strategic investments in life sciences and promote research and innovation in health and biomedical sciences.
The DAHC is tasked with managing and operating the following healthcare facilities:

• all DHA hospitals, primary healthcare centres, specialised care centres, medical fitness centres, and public health and occupational health centres
• the Mohammed Bin Rashid University of Medicine and Health Sciences
• Dubai Dental Hospital
• Al Jalila Foundation
• Al Jalila Children’s Specialty Hospital
• any other entities mandated to be part of the DAHC as per the legislation issued by the Ruler of Dubai.
(‘DAHC Entities’)
2. Abu Dhabi
Abu Dhabi’s government-owned ADQ is tasked with responsibility for centralising and consolidating the public health system of the Emirate of Abu Dhabi. It has consolidated several companies within one of its subsidiaries, Pure Health, creating the largest healthcare provider in the UAE.
The Abu Dhabi Health Services Company (SEHA) and The National Health Insurance Company PJSC (Daman) will merge into
Pure Health as part of the restructuring. Other healthcare groups were also acquired in parallel to further strengthen the range of activities of the provider platform. These included, Tamouh Healthcare, Yas Clinic Group, and Abu Dhabi Stem Cell Centre, which further diversified the portfolio of hospital management, laboratory services, medical supplies and healthcare informatics.
“DOH’s ultimate aim is to have a licensed family medicine care provider within each precinct in Abu Dhabi”
Christina Sochacki Senior Counsel, Head of Healthcare & Life Sciences, KSA Al Tamimi & Co
In the summer of 2022, a new Cabinet Resolution was issued, establishing the Health Holding Company (“HHC”). It is a significant legal step in formally implementing the transformation plan for the Kingdom’s healthcare system.

The plan is for the Ministry of Health’s (“MOH”) current role, as regulator and provider of public healthcare services, to be bifurcated. Under the plan, the MOH will become the regulator and supervisor of public and private health institutions. All public health services will be transferred to the HHC, in due course. Public health services will be provided by HHC through its subsidiaries (or other legal bodies to be determined), including the Health Clusters (see below for further details), who are tasked with providing integrated healthcare services to beneficiaries in all regions of the Kingdom in accordance with the Kingdom’s “modern healthcare model”, which will be defined and requirements set by the MOH.
In due course, it is planned that all sta who are currently involved in providing healthcare services, at all levels, under the MOH will be transferred to the HHC, or to the company’s subsidiaries (such as the Health Clusters that are being formed).
It is expected that, the HHC will establish health clusters in the form of independent companies to provide public healthcare services. As part of Vision 2030 and the Healthcare Transformation Strategy, all existing MOH/HHC providers will be migrated into Healthcare Clusters, which will amount to approximately 20-30 geographically defined, vertically integrated, “Accountable Care Organisations”, serving around 1-2m people each. These clusters will be established as “corporatised” public bodies, with substantial and defined decision rights. This strategy was drawn widely from the NHS experience in corporatising public healthcare providers. Healthcare Clusters have already begun
issuing tenders and contracts for private companies to provide consulting services to assist the formation, management, and operation of these clusters and their facilities.
The goals of decentralisation and clustering public health service delivery is to increase competition, transparency, and e iciency as Health Clusters compete with each other as well as the private sector for clients and health care professionals.
Under these new models of care, it is anticipated that privatisation initiatives will be accelerated as the clusters will be encouraged to transfer the ownership, management and operations of their facilities to private companies, in due course.
The Resolution also established the National Health Insurance Center (“NHIC”), which will purchase health services provided by the HHC or its subsidiaries. The NHIC is expected to submit for approval the comprehensive health insurance vision for Saudi citizens in due course. Essentially, we can expect to see a form of universal health coverage emerge in the Kingdom.
The budgetary allocations for the MoH for the provision of healthcare services are expected to be transferred to the NHIC, in accordance with the plan, phases and mechanisms decided by the supervisory committee for the privatisation of the health sector. The NHIC will purchase health services provided by the HHC or its subsidiaries. The beneficiaries of the NHIC insurance include Saudis working in the public and private sectors, their family members as well as children of a Saudi mother from a non-Saudi husband residing in the Kingdom or non-Saudi wife married to a Saudi, and a non-Saudi married to a Saudi woman residing in the Kingdom, in the event their healthcare is not covered by a cooperative health insurance policy (being the private health insurance). The beneficiaries of NHIC healthcare service also include non-Saudi workers in government sectors, if they are not covered by special healthcare systems, programmes or services.
The largest healthcare event in the Middle East is back
With 70 countries in attendance, represented by nearly 3,000 exhibitors, and visitors from 185 countries, Arab Health 2023 presents a truly global health experience, alongside more than 45 country pavilions, welcoming pioneers and giants alike from across the healthcare industry to discuss the latest products and technologies in the market.
This year exhibitors have been split into nine product sectors, making it easier than ever to navigate all that Arab Health 2023 has to o er. More than 200 companies can be found under healthcare transformation, with another 150 supplying IT systems and solutions.
Healthcare and general services provides connections and updates on the sector from more than 300 dedicated companies, while market insights and comprehensive comparisons are on o er in the healthcare infrastructure and assets sector.

For practical tools, sourcing and distribution, Arab Health 2023 is host to almost 3,000 brands showcasing their expertise in the following sectors: medical equipment and devices, disposables and consumer goods, orthopaedics and physiotherapy, and imaging and diagnostics.
Finally, a wealth of opportunities are being presented in the wellness and prevention space by more than 1,500 brands.
Arab Health Pavilions
The Village has been designed to complement the show, providing a space for networking. The relaxing atmosphere o ers a range of seating options and refreshments throughout the course of the show.
To experience the next generation of healthcare, the Intelligent Health Pavilion provides state of the art digital health enabled hospital environments. Real-life situations are accessible for observation in a variety of formats. An Intensive Care Unit enables guests to experience the latest transformative tech, covering topics in
infection control, patient safety and CSSD. Remote patient monitoring, wearables, sensors and voice tech are on display in the Emergency Room and an intelligent Operating Room with integrated tech systems showcases the latest in enhanced surgical advancements.
A key focus of the Intelligent Health Pavilion is collaboration and interoperability. Through the exhibition of use cases, entrepreneurs are able to demonstrate their capacity and skills within a unique environment. These presentations of seamless co-existence aim to highlight how multiple technologies can operate alongside medical equipment to facilitate the delivery of improved patient care.
As a main feature of the exhibition, the Intelligent Health Pavilion showcases the capabilities of equipment manufacturers, e-health solution providers and digital health disruptors to key decision makers from the MENA region, and the world.
In addition, companies are able to share their innovations and the latest solutions through talks and product showcases at the Transformation Zone. Here, entrepreneurs can find immersive Innov8 Talks which provide comprehensive updates on the current evolution of the healthcare landscape. Innov8 Talks provides a space for collaborative discussions around sustainability, FemTech, UN SDGs and wellbeing.
On Thursday, Arab Health and Medlab Middle East is presenting the Future Health Summit at the visionary Museum of the Future. Professor of Neurosurgery and Orthopaedic Surgery, Dr. Timothy F. Witham joins a panel of guests to discuss ‘Healthcare in the Metaverse’. As well as sharing his insights from conducting the world’s first augmented reality spinal surgery, Dr Witham will be detailing his thoughts on the future direction of healthcare and its relationship with the metaverse. Keynote speakers, tech showcases and hologram presentations gives guests a
fully immersive experience, taking them on a comprehensive journey through the metaverse.
Starting with an explorative discussion to introduce the metaverse, as a new concept presenting possibilities it is essential for decision makers and innovators. Understanding the intricacies of the impact the metaverse has on healthcare will enable the harnessing of the advantages it presents.
The dedicated forum will explore artificial intelligence, augmented reality and virtual reality in a clinical setting to improve patient outcomes globally.

The summit will provide key insights to invited senior government o icials
and executives from the global healthcare sector, taking guests on a tour of the future of health, deep diving into the amazing possibilities of healthcare in the metaverse. Following this delve into the metaverse, industry leading innovators have the opportunity to showcase how their harnessing the power of the metaverse and how implementation can lead to better patient care.


In October 2020, the NHS became the first healthcare service in the world to commit to becoming net zero carbon (NZC). This pledge will see Europe’s largest employer reduce their carbon emissions by 2040, proactively improving public health for the future.
Rebecca Stubbs has been involved in the biggest UK hospital restructuring project in this area. She has advised the UK government on its approach to tackling hospital emissions and has worked very closely with NHS England and the Green NHS team over the past two years, leading the development of the NHS net zero building standard.
HW: How do you describe NZC?
NZC is a science-based target driven approach to tackling climate change. This means that we are trying to reduce our emissions to levels that are aligned with trajectories of 1.5 degrees. Practically speaking, this will require incremental steps, year on year, to reduce about 90 per cent, if not 95 per cent, of emissions before the specific NZC year. This end dates varies depending on scope of emissions. Emissions reductions are not linear. The NHS has 80 per cent reduction targets for 2030, which is approaching very quickly. To achieve NZC, we must o set any residual emissions - that is the key di erence between NZC and true zero carbon. In true zero carbon, there are no residual
emissions! The other key di erence is that carbon neutral is di erent from carbon neutral within net zero. The o set is sequestering carbon - actually removing emissions from the atmosphere and not just paying for them to be mitigated or reduced somewhere else.
As an analogy, if you imagine a balance scales, on one side are the positive emissions into the atmosphere and on the other side the negative emissions that are removing them via carbon sequestering o sets which we need to balance to zero.
The climate emergency is a health emergency. By lowering emissions, the NHS is able to minimise the negative health impacts of climate change. The NHS is responsible for 4 per cent of UK emissions and so it has taken ambitious steps to reduce this including incorporating it into legislation within the Social Care Act 2022. Estates and facilities are typically about 15 per cent of the NHS footprint and are within direct control of the NHS, whereas much of the NHS footprint is supply chain emissions e.g. through produced goods and services, medicines and equipment, and other induced emissions e.g. patient and sta travel. These are less easy to assess and influence. Facilities are largely ‘in-house’, hence the Net Zero Building Standard for NHS facilities, that Mott MacDonald supported.
NHS ‘facilities’ is a very broad term. It might include GP centres, any kind of operating theatres, containment labs or inpatient facilities. The degree of variability within the estate is huge, therefore, there are both quantitative and qualitative expectations in the NHS Net Zero Building Standard. We must also be respectful of the variability of specialisms in di erent spaces and create a bespoke approach to accommodate this diversity.
Healthcare facilities and services are also very highly constrained; infection control is pertinent to ensure the highest levels of patient safety are maintained. When
trying to decarbonise, it’s very much safety first, which has produced several barriers for basic changes in improving energy e iciency. As a result, a tension is created between optimising patient care in the short term that is likely to adversely impact the health of future generations.
HW: Why are healthcare facilities so challenging to decarbonise?
We need to capture all the emissions from the construction and from the materiality of these buildings, which is typically about 50 per cent of the total emissions of a building over its whole life. If a building is in place for 60 to 100 years and it is demolished, it will create more emissions to reduce the operational carbon from the construction of a new one. Materials are energy intensive and carbon intensive at the moment, and will be for the next decade. Construction in the short to medium term is really carbon intensive because we haven’t decarbonised raw materials such as concrete and steel, or machinery used on site or in transportation of goods, thus we haven’t decarbonised construction.
It is important that we refurbish existing buildings where we can, but there are challenges in terms of clinical standards. There are many old buildings where immediate changes can be implemented, such as facade upgrades and general amendments, to increase energy e iciency. But sometimes there is little to no benefit in refurbishing a building to establish high energy e iciency because it’s not fit for clinical need. There are some very old, highly constrained buildings belonging to healthcare providers today which are going to be incredibly expensive and disruptive to refurbish, so it’s about a balanced approach across our estates.
HW: Are the answers to the NZC challenge as simple as reducing their emissions?
No, we also need climate resilient buildings. We have a real challenge in the UK as everyone is focused on heating in terms of the e iciency of hospitals. The equally important question is, how are we going to cool these buildings down? With temperatures rising above 40 degrees during the summer of 2022, cooling is vital across much longer periods of the year, and there are real problems with patient safety trying to keep hospital facilities at the
“The transformation of systemwide clinical pathways is often complex and requires engagement across multiple healthcare professionals”
Rebecca Stubbs Principal Net Zero Carbon Consultant Mott MacDonald
right temperature, especially for vulnerable patients and sta .
The answer is a bespoke, strategic approach to each building. It can take a huge amount of coordination; it is very dependent on those operational constraints of the spaces within the building and how much decant space there might be to allow for refurbishments. Ensuring resilience of energy systems is also crucial within this design and strategy process.
HW: In addition to buildings, does there need to be a focus on any other areas to achieve NZC within a healthcare system?
Yes, the achievement of NZC within healthcare will be the result of hundreds of projects spanning multiple areas, including procurement, food and nutrition, sta and patient behavioural change, and sustainable models of care, to name a few.
Sustainable models of care is an area of particular interest and focus for us at Mott MacDonald. Historically, healthcare services have been redesigned or transformed to deliver improved patient outcomes, or financial e iciencies, or both. However, through an approach underpinned with NZC and sustainable principles, future models of care can be reconfigured to achieve both these areas as well as reducing their carbon footprints. Examples of this include the adoption of digital solutions to enable the delivery of virtual wards and telemedicine, or undertaking more surgical procedures within appropriate community settings to release hospital theatre space.
Mott MacDonald has been supporting various NHS Trusts with their decarbonisation journeys. The transformation of systemwide clinical pathways is o en complex and requires engagement across multiple healthcare professionals, including

commissioners, clinicians, finance, clinical governance, estates and facilities, medicines management and most importantly, patients themselves. However, this a worthwhile undertaking with benefits that could be profound for patients, healthcare professionals and for our planet.
In summary, I strongly suggest that all healthcare operators follow the leadership shown by NHS England and formulate a strategy and roadmap of priorities to give clear direction of travel to suppliers for their required contribution, to align collective e orts and step up to this challenge of a generation.
Healthcare systems across the world need to ensure they work as an effective, integrated ecosystem that sets the health of every member of society at the forefront. We believe this can only be achieved when you put the patient first in all decisions made. Whether that be planning infrastructure, integrating systems and processes, or securing finance for new facilities, using multidisciplinary expertise and understanding of what patients need will enable a world-class healthcare system to become a reality.
At Currie & Brown we have the knowledge, experience and data to not only identify the plan, but help it become a sustainable reality for everyone - the community, the doctors, nurses and wider workforce, but most importantly the patient.
Currie & Brown is one of the world’s leading physical assets management and construction consultancies, dedicated to advising clients in respect of the management and utilisation of their physical assets, and is differentiated by innovation, expertise and experience.
We bring knowledge and experience spanning the entire life cycle of healthcare, from the development of effective system-wide integrated models of care and determining viable infrastructure and digital plans, through to developing optimised PPP models and the cost and project management of infrastructure delivery itself.

With principal offices in London, Dubai, Hong Kong, Mumbai, New York and Shanghai, we operate throughout the Americas, Asia Pacific, Europe, India and the Middle East.
Currie & Brown has been a Dar Group company since 2012.
www.curriebrown.com

“A focus on the patient will enable the delivery of world-class integrated and sustainable healthcare systems and infrastructure.”
Helen Pickering
Global Head of Healthcare helen.pickering@curriebrown.com
You wouldn’tspend10 times more than you hadto on somethingsimple…

Wouldyou?
Because this is happening in our hospitals, every day. AdviseInc bring transparency and clarity to spend in the healthcare system.
Using the latest tools we give every hospital the abilit y to understand pricing and control once hidden costs. AdviseInc, make sense.
Sarah Cartledge speaks to Dr Ali Haydar, Chief Medical Officer, Aman Hospital in Qatar, and Alistair Russell at Imperial Private Healthcare about the International Affiliate Network

Co-operation is absolutely key to the development of best practice in healthcare at large. Development, innovation, and ingenuity can only come about when we challenge our ways of approaching problems - and the best way to do this is through the sharing of our learnings, especially so at the forefront of healthcare.
Earlier this year Imperial Private Healthcare launched their new project, the International A iliate Network, established to develop relationships between ambitious hospitals across the world, enabling them to share knowledge and expertise, and advance patient care. The network strives to ensure that member hospitals can not only widen their services
and care through collaboration, but that they can share their learning with other organisations. As such, this network is not simply a one-way improvement service, but a truly collective project.
Aman Hospital in Qatar is the first partner in the International A iliate Network and is already benefitting from being part of the programme. A leading hospital in the region, Aman Hospital prides itself on providing cuttingedge standards of care, delivered by experienced clinicians. With practitioners who have graduated from Johns Hopkins, Harvard, Chelsea and Westminster Hospital in London, the Mayo Clinic, and many more, the sta at Aman have obtained their certifications from the best medical institutions in the world.
This new 100+ bed hospital aims to define the future of healthcare delivery in Qatar and the region by combining unparalleled professional expertise, cutting-edge technology, state-of-theart equipment, service excellence, a relentless pursuit of medical innovation, and deluxe hospitality, all with a focus on patient-centred care. The main goal is to integrate the quality of care with the highest quality services which include 5 Centres of Excellence, 16 speciality clinics, VIP and Royal suites and hospitalitytrained sta .
Building a true partnership

These days it’s common for hospitals to partner with other organisations,

especially ones far away from them. Yet all too o en, these partnerships are in name only. They still sit as separate organisations, and the benefit of the ‘partnership’ is merely for recognition. “As a hospital we wanted a stronger a iliation than just a standard partnership. This isn’t an a iliation just by name, but one whereby you actually serve the community better together; you improve the quality of care together, and the quality of teaching and education together,” says Dr Ali Haydar, Chief Medical O icer at Aman Hospital.
Imperial Private Healthcare is part of Imperial College Healthcare NHS Trust, one of the largest teaching hospital groups in the UK, and consists of 5 London hospitals – Queen Mary’s, The Lindo Wing,
Charing Cross, Hammersmith, Queen Charlotte’s and Chelsea, and The Western Eye Hospital. With more than 500 medical consultants it covers all clinical areas and specialities, and has a long-standing tradition as one of the most important medical institutions in the UK.
“The network’s aim is principally around developing healthcare capability around the world. The NHS values that surround the knowledge transfer are really important to embrace improving healthcare in the regions where we have worked for years and from where we continue to receive patients,” says Alistair Russell, Business Development Manager at Imperial Private Healthcare.
Another benefit of the network is that in addition to the deep-rooted nature of the partnership, it also allows member organisations to tailor-make their partnership, based on their vision, strategy, and needs and requirements. “The benefit of this a iliation has been developed together between Imperial and Aman when we were forming the partnership, and it turned out to be a very interesting concept and idea,” says Dr Haydar.
“The concept of the transfer of knowledge with Imperial was really developed to go both ways - we are two di erent worlds, with two di erent pathologies and two di erent sets of requirements, so it’s really reciprocal,” he continues.
Aman Hospital is a fully digital and paperless organisation – the only paper to be printed is the consent form which cannot be digitally signed in Qatar. “We have seven operating theatres that are all connected to an advanced digital system that allows us to transfer data either internally to our conference rooms or externally. So if we’re doing an operation and there’s a question, I can easily log in someone outside the theatre, even at Imperial, and ask for an opinion
“This isn’t an affiliation just by name, but one whereby you actually serve the community better together”
Dr Ali Haydar Chief Medical Officer Aman Hospital in Qatar
on the spot. The same thing would apply to endoscopy, even radiology or interventional radiology procedures.”
As Aman is a private hospital, they do not normally recruit all specialities or deal with all pathologies. They can treat 80 per cent of the pathologies but 20 per cent will need di erent expertise, perhaps in a specialist centre. With the a iliation

in place, the consultants can reach out to Imperial and transfer a patient if the MDT team across both hospitals considers it necessary, ensuring continuous care across continents. “It’s absolutely a win-win as we specialise in di erent things and without the network, neither of us can o er a full pathway to certain patients,” says Alistair.
“Imperial can’t o er clinical services in Qatar, but we really want to be able to tap into that market,” he continues. “Aman Hospital wants to specialise in certain centres of excellence that we provide, but they can’t necessarily access or provide everything they need due to justifying the investment for the volume of patients. But together, using each other’s services, and sharing our expertise,
we can o er the full pathway. So, from the patient perspective, they’re getting the full pathway under one roof.”
The almost universal use of digital meetings on platforms such as Teams has made second opinions and knowledge transfer much easier. For patients travelling to London for surgery, they will have already met the doctor virtually and
the notes can be transferred instantly, reducing anxiety and long on-boarding procedures.

“When a patient presents in Qatar and is diagnosed, they can be treated up to a certain point and they may choose to have an opinion from an Imperial consultant on a peer-to-peer basis. If they decide to transfer to London, it becomes a managed
service by our teams, says Alistair. “Before this, patients would have had to do it themselves. Now we are confident that we are all updated when the patient arrives, and that we are discharging them back to a team we know. It’s all been enabled through telemedicine and advisory work, and the benefit to Aman Hospital is the complete end-to-end pathway.”
For Clinical Lead Dr Bassem Safadi, this knowledge transfer is extremely beneficial. “Through the network we can connect with a big institution and actually get people from there to train our sta , or send some of our sta to London to get special expertise, and that’s something we think is very important,” he says.
Alistair Russell Director of Business Development Imperial Private Healthcare
Again, this is not a one-way street. “For example, Aman called us up and asked for our thoughts on Lasik equipment and if we use it,” says Alistair. “We checked with our consultants and they confirmed what the sta at Aman wanted to know, giving them the guidelines that we follow. Equally, Aman Hospital operates brand new equipment not available yet at Imperial.”
The peer-to-peer learning is highly regarded by both institutions. “We will hopefully sign up all their doctors as observers and participate in life with us and vice versa, blended with face-to-face contact,” he adds. For Dr Safadi, it’s also a personal benefit; “There is also much to be gained for the clinical team, as well as for the institution and the patients,” he says.
“It’s absolutely a win-win as we specialise in different things and without the network, neither of us can offer a full pathway to certain patients”
From Imperial’s point of view, Aman Hospital has an innovative approach to holistic care. Hassan Elbouatmani, Chief Hospitality and Operation O icer, comes from a hotel background, and his aim is to enhance the whole patient experience. “Treatment is also about what the patient hears and smells,” he says. “A calming and stress-free environment in a hospital can help the patient recover faster. We’re o ering a service that relies on hospitality and we are confident it can translate into the healing process.”
Aside from the gourmet restaurant and executive chefs, Hassan is keen to serve the patients the food they would like to eat at the time they would like. “It’s not about serving them breakfast when they need to sleep, or giving them dinner when they aren’t hungry,” he says. “They are more likely to eat appetising food when they are ready and reap the benefit. From that point of view, yes, it’s more like a hotel with room service, but it feeds into the patient recovery.”
Equally, Chief Nursing O icer, Trudy Rowsell, is promoting a multi-speciality concept that interests Imperial. With global workforce shortages an issue for all
providers, a new approach is vital. “I’m looking at an agile workforce, trying to move nurses around in di erent areas and giving them those skills so they gain a greater portfolio which delivers job retention for the hospital,” she says. “Again, this will deliver a better patient experience as the nurses will have a greater skillset to o er.”
Lastly, with the long period of tradition and history that Imperial enjoys, new institutions can benefit from the experience in areas around governance, policies and procedures, and patient safety. “We’re very interested in global healthcare and internationalising care,” says Dr Haydar. “Up to 90 pieces of our equipment are state of the art and some

of them are not available in the whole Gulf region, such as the transcranial magnetic stimulation, which is an FDA approved treatment for depression and chronic pain, and robotic interventional radiology, so we are able to o er a reverse pathway for those who would like to come to Qatar for treatment with our technology.”
All in all, the International A iliate Network provides an unprecedented opportunity for hospitals, clinicians, and patients to access higher standards of care around the world, and for organisations to build and grow together.
If you would be interested in joining Imperial’s International Affiliate network, please contact Alistair Russell, Imperial Private Healthcare.

www.imperialprivatehealthcare.co.uk/ affiliate-network/ www.amanhospital.org/
“We’re very interested in global healthcare and internationalising care”
Dr Ali Haydar Chief Medical Officer Aman Hospital in Qatar
The NHS Consortium for Global Health provides a single point of access to expertise from the UK’s national health organisations, including the major National Health Service executive agencies and public bodies.
Technical capabilities:
•Pandemic Response, Health Security, & Climate Change
•Workforce Planning & Development
•Health Financing & Strategic Purchasing
•Digital Health & Transformation
•Public Health & Reduction of Health Inequalities
•Health Technology Assessment, Clinical Guidelines & Quality Improvement
•Genomics in Healthcare
•Government Relations
•Monitoring, Evaluation & Learning
To find out more about working with the NHS Consortium for Global Health, contact:
Kevin Miles, Senior Lead Global Health Partnerships, Health Education England Stewart House, 32 Bloomsbury Square, London WC1B 5DN
E: kevin.miles@hee.nhs.uk
M: +44 (0)7467 004 560
Healthcare World’s Editor-in-Chief Sarah Cartledge speaks to Helen Featherstone, General Manager of GMC Services International about the importance of a comprehensive regulatory framework

Over the past 160 years, the UK’s General Medical Council (GMC) has become one of the leading professional healthcare regulators in the world. From medical school accreditation through to specialist licensing and revalidation, the GMC works through every phase of a doctor’s professional life. GMC Services International (GMCSI) has been established to support the core services provided by the GMC globally, delivering advisory services to ministries and regulators, through a nonUK-centric model.
At the centre of every healthcare system is a secure regulatory framework, surrounded by implementation processes and structures. GMCSI o ers a peoplecentre consulting approach across all elements of the regulatory framework, with patient safety at its core. The knowledge base in place at the GMC on which GMCSI relies, allows for flexibility through experience, o ering tailored services to improve the landscape for all healthcare professionals.
Helen Featherstone, General Manager of GMCSI, works closely with International Ministries of Health and Regulators to identify opportunities for more e ective regulatory systems. “Ethical guidance is the core of regulation,” she says. “We focus on prevention rather than punishment, and on culture, values, teamwork and leadership as well as process and standards.”
This approach allows the cultivation of a patient-focused culture within a healthcare system to improve safety, access, quality and consistency across highly diverse workforces in order to ‘professionalise the professionals.’ In delivering programmes GMCSI is able to access the GMC’s pool of 1,300 sta and a further 1,000 associates.
By creating supportive environments and nurturing healthcare workers through their professional journey, GMCSI is able to
provide structures to maintain and improve standards. These structures encourage and empower healthcare professionals to seek out opportunities and embark on a journey of life-long learning to develop their careers and provide patients with the best quality services.
“Medical doctor registrations ensure all practising professionals in the region are certified, and regulators can check that doctors keep their knowledge and competences up to date through revalidation processes every 5 years,” she says. These registers prove to be the key to successful regulation, providing a means for maintaining contact, collecting fees and supporting revalidation and fitness to practise or FTP decisions. Moreover, these systems give authorities the ability to proactively plan their workforce, ensuring compliance with key activities, as outlined by each region. These registers are made visible to the public through the General Medical Council website to foster public confidence in medical doctors working within the United Kingdom.

GMCSI has o ered advice and guidance on setting up robust registration and licensing processes to a number of countries which promoted revalidation as standard to encourage continuous career development for their workforce.
One example looked specifically at reforming an overly bureaucratic process in a country in the Middle East, that was unable to deliver the number of licensed doctors needed. The process delayed
newly qualified medics from registering and applicants were moving on to other regions before their registration had gone through. The system review undertaken by GMCSI led to the implementation of a fast-track system for applicants with certification from other reputable healthcare systems regulators, under the guidance of the GMC. The system enabled the establishment of an e ective process with a balance between competitiveness and risk. In order to ensure e iciency, a programme to reduce the wait time for primary source documentation verification for the regulation of new healthcare professionals was also produced.
Medical education standards and
“Ethical guidance is the core of regulation”
Helen Featherstone General Manager GMC Services International
outcomes also play an important role within the overall regulatory framework. “It is important to understand how to work with medical schools to make sure they are delivering against all the required standards,” states Helen, highlighting the importance of a fully comprehensive regulatory system from the schools through to the hospitals.
In order to deliver a completely comprehensive system, the regulatory framework must go even further.
“Fitness to practise is key, but actually we find the complaints process is of huge importance. GMCSI recently supported a new regulator of healthcare professionals in an African country, specifically focused
on the processes behind complaints handling. The regulator focused on setting up fitness to practise rules and was given guidance on legislative requirements, as well as dra ing decision outcomes, information handling, detailed triage decision making policy, sanctions and fitness to practice publications policy.
GMCSI is able to draw on a wealth of experience from the GMC to provide knowledge and guidance for every regulatory system, with access to consultants in registration, revalidation, fitness to practise, medical education and guidance on medical ethics. Regulatory system reviews are crucial, and up to date practices provide the foundations
for a stable healthcare landscape. A well-designed system allows for doctor satisfaction by encouraging career progression through continuous support systems surrounding revalidation. Taking care of this environment provides the best service possible to patients and enables positive outcomes through a reliable and trusted complaints procedure.
A well-designed system limits the risk of harm to the public, placing patient safety at the heart of the regulatory framework.


The global FemTech market is valued at $25bn and projected to rise by 15 per cent in the next few years, so it deserves greater attention, say Vincent Buscemi and Letitia Winterflood-Blood of Bevan Brittan LLP
There is no o icial definition of “FemTech”. But if you search online for this term, the consensus seems to be it refers to technology, services and products that improve women, females, and girls’ health and wellness. As women comprise 51 per cent of the global population, it seems strange that it needs its own classification as a subset of health tech. There is no doubt that femaletargeted apps provide invaluable medical advice to women, girls and others, so this
area of innovation rightly deserves to be in the spotlight and given greater attention. In terms of the benefits it can bring, this can particularly be the case in emerging economies where cultural traditions may have a disproportionately detrimental impact on females.
So is FemTech a misnomer? And if it is, how has it entered the mainstream and is now worth $25bn globally?
Vincent Buscemi (Partner) and Letitia Winterflood-Blood (Senior Associate)
from Bevan Brittan LLP, are particularly interested in the rise of FemTech, especially as a number of their digital, MedTech, life science and traditional healthcare clients are increasingly active in this space and, as a firm where the majority of the lawyers are women, equality is a priority.
FemTech was coined as a term as late as 2016. For Vincent Buscemi, the reality is that it has been a positive disruptor in healthcare because there are now many more people taking it into consideration. “At Bevan Brittan we are always very interested in following FemTech companies and looking at how they’re structured,” he says. “There are many more products and services specifically focused on women’s health and women’s health needs, particularly as GEN-Z and the younger generations now use technology for almost everything.”
FemTech encompasses everything from menstrual health, reproductive health, sexual health, maternal health and menopause. Until now FemTech founders have tended to be female, reinforcing the FemTech description. Indeed, in some contexts the term FemTech is used to describe women in tech more generally. It has additional relevance in that certain conditions not specific to females, such as osteoporosis, a ect more women than men or a ect women di erently.
For Letitia, there is the prevention agenda as well. “People are talking about women’s health more openly now, giving women the confidence to manage their own health and issues they would have shied away from previously,” she says. “We need to
take advantage of this shi and make it easy for women to manage those issues, particularly as health systems around the world are being reshaped following the COVID pandemic.”
As a general rule, women have always been more open about discussing health issues with their doctor, whereas men can o en be diagnosed too late for a positive outcome. Through wearables and FemTech apps, medical and healthcare information can be now disseminated widely and also privately, enabling women to understand when to approach their GP or indeed other support, relieving pressure on primary care services.
As with any healthcare product, FemTech has to take into consideration how people consume healthcare on the ground. To combat local cultural issues, “FemTech can be adapted at a cost at a local level to tailor products and services to di erent groups in di erent societies or parts of the world” Letitia says. This approach of tailoring the tech to local needs has potential to help those groups that have historically been marginalised – o en women. “There has been increased prevalence of telemedicine and remote monitoring/wearables to facilitate healthcare at home since COVID. This has been particularly helpful for rural communities and women’s health issues that have traditionally been stigmatised.”
For Vincent, “ultimately this is important because, across the world, one of the main thrusts of whole population healthcare and population health management is about identifying health needs and reducing health inequalities”. Apart from it being a good thing to do, this should be a key objective solely from a socioeconomic perspective – a healthier, happier population is likely to be a more productive one with fewer demands on other public services such as social care.
Vincent observes that some critics suggest that categorising FemTech reinforces certain gender stereotypes. “There’s no such thing as mentech or mantech, so FemTech could be seen as being somewhat exclusionary to certain groups. But that ought not to detract from the positive things that the whole FemTech market and industry is seeking to achieve.”
But surely FemTech is of relevance to the 49 per cent of the population that is male? Letitia agrees, saying the agenda
of FemTech is also about reducing health inequalities between men and women. “It provides an interface to connect communities and introduces a social aspect as a way to seek reassurance, for example through online forums. However, it’s also about being able to get care where you actually need it and identifying when an issue needs medical assistance,” she says. An app is unlikely to be the end of the road where medical intervention and treatment is needed but it will make a major contribution to ensuring the right treatment is sought at the right time. Given that women are – generally – more likely to seek medical assistance than men and at an earlier stage of an issue arising, perhaps the approach to health management which the FemTech industry is developing can lay the foundations for a male-centric equivalent.
However, by categorising femaletargeted products in this way, Letitia is concerned that it could result in further marginalisation. Adding the FemTech label does not necessarily mean it will meet female-specific needs. “It’s not a box ticking exercise around women’s health or simply an area in which women work,” she says. “It’s more about adjusting the default approach to everything, while acknowledging that there are some issues and conditions which will be more relevant or relevant in a di erent way to women.”

Where the focus is shi ing on to ‘women’s health’ issues, the danger emerges that everything else (e.g. orthopaedics, respiratory medicine) remains male-centric in terms of innovation, focus, design and funding. In Vincent’s opinion; “We need men working on FemTech because, apart from anything else, it will promote greater understanding in all areas of life.”
And this feeds into the rise of equality, diversity and ESG initiatives. From a legal point of view, it’s a di erent o ering as well. As one of the UK’s top law firms,

“FemTech can be adapted at a local level to tailor products and services to different groups”
Letitia Winterflood-Blood Senior Associate Bevan Brittan
Bevan Brittan has a high proportion of female lawyers (and partners) with several wellbeing and equality initiatives, such as a menopause group. “There may be certain clients who are more comfortable talking to a female lawyer about these issues, particularly in the Middle East, and we are happy to o er this,” says Vincent.
In Vincent’s opinion, many employers will have a reasonable number of females in the workforce, and a healthy, happy, welladjusted workforce o en leads to greater productivity and a positive contribution to the economy.
If nothing else – it’s good for business. On the consumer side there is a big market for more female-focussed products. On the organisational/ employee side, making changes in this area potentially unlocks a huge chunk of hidden talent that will lead to better productivity, more innovation, and potentially better profitability. Outside the FemTech arena, 51 per cent of any potential target market is female, so ensuring that women play a substantive role in product design, development and implementation is vital.
“If you’re carrying a female input for your products and the services, it is more likely to result in better adjusted and better designed products,” Vincent says. “It’s a slightly cold business angle, but it’s in the company’s interest to include this perspective from a purely economic and business point of view. It may be an area that some people or companies might like to ignore, but ignore it at your peril because ultimately it’s big and getting bigger.”
In practice, funding is also key. On the whole investors have bought into the idea that there is a major gap in the healthcare market and one that can reap rewards. “A range of private equity and other investors

are looking at healthcare because, over the last few years with the pandemic, they haven’t invested as much as they would have, so there is liquidity within those investor markets to invest in this area,” says Vincent.
There may be some who are deterred by the categorisation, but according to a report by Beauhurst, the industry globally is expected to reach $60bn by 2027. A February 2022 report by McKinsey noted that women account for 80 per cent of consumer purchasing decisions in the healthcare industry yet, remarkably, women’s health has been considered a niche market and a mere subset of healthcare. “Ultimately, with the rise of ESG and the prevalence that investors are putting on impact investment, and the fact that female health issues are all historically under-funded and under-researched, FemTech is an area where investors could make a real impact in a relatively short space of time,” Vincent concludes.

Contact
www.bevanbrittan.com vincent.buscemi@bevanbrittan.com letitia.Winterflood-blood@bevanbrittan.com
“We need men working on FemTech because it will promote greater understanding in all areas of life”
Vincent Buscemi Partner + Head Independent Health & Social Care Bevan Brittan
Supporting international health care providers to deliver best in class primary and step down care
Providing partnership opportunities for investors looking at building international and UK based portfolios


World-class healthcare needs integrated systems where every part works to improve patient outcomes
Health systems have adapted in response to new diseases, innovations, societal expectations and technological interventions for centuries. As the world emerges from the COVID-19 pandemic, there is renewed e ort by developed and developing countries to adapt their health systems again.
The pandemic has not only threatened the sustainability of established health systems, but crucially the health-related Sustainable Development Goals (SDGs) including the target to achieve Universal Health Coverage (UHC) by 2030 (SDG 3.8). Monitoring progress towards achieving UHC focuses on the proportion of a population that can access essential
quality health services, and how the burden of personal health costs can be reduced to protect households against financial hardship.
Achieving this requires all countries to continue to strengthen their health systems. The WHO defines health system strengthening as “any array of initiatives that improves one or more of the functions of the health systems and that leads to better health through improvements in access, coverage, quality or e iciency.”
The NHS is leading in new approaches to emerging challenges – sustainability and carbon neutral policy, cutting edge infrastructure and pandemic response.
The pandemic has shown research, innovation and its translation through to products, services and clinical practice are key to achieving continuous health improvements. The rapid pace in biomedical and technological innovations has transformed the lives of many people. The ability to research and deploy COVID-19 vaccinations is a good example from the UK. Yet, as one risk is reduced, others have emerged.
Health services across the globe have worked to transform their systems to respond to the changes in disease burden from infection to non-communicable disease (NCD) as causes for premature death or disability. In 2020, WHO reported the top three causes of death globally are ischaemic heart disease, stroke and chronic obstructive pulmonary disease. These causes of death remain the same, despite the COVID-19 pandemic, and have even been exacerbated.
In early 2020, health systems rapidly pivoted and managed patients with COVID-19, through information and the
reorganisation of services to treat patients su ering with the e ects of the virus, and with governments issuing urgent public health messages to underline the importance of transmission control. For many countries, this manifested in lockdowns that disrupted regular health treatment impacting, in particular the diagnosis, treatment and management of NCDs.
The figures are stark. In June 2020 – just weeks into the pandemic – WHO published a survey showing that prevention and treatment services for tackling NCDs had been severely disrupted since the start of the pandemic. WHO said that this situation was of significant concern because people living with NCDs were at higher risk of severe COVID-19-related illness and death.
The pandemic has highlighted the weakness of current health systems –especially those in middle and low-income countries progressing towards the UN’s 2030 goal of UHC, while in stronger health systems, alternative approaches have had to be found to deliver patient services di erently, including through digital health.
The UK system has multiple building blocks of a health system which the Department for International Trade has identified as:

Achieving system excellence need not take other countries systems decades; the UK can share its successes and learnings. A diverse range of innovative UK organisations are delivering on the NHS Long Term Plan and driving UHC to build resilience and sustainability into the systems.
DIT has brought a delegation of some of the amazing NHS Trusts on the UK Healthcare and Life Sciences Trade Mission to Arab Health, and the UK pavilion o ers hundreds of UK companies with interesting healthcare and MedTech innovations that are all open to international collaborations.
•The UK has an integrated model of care focused on the patient, built and developed over these 70 years. It draws together expertise in healthcare financing, policy & strategy, regulation and clinical guidelines to create comprehensive healthcare systems. Organisations such as NHS England/ Improvement set a strategic direction; NHS Trusts such as Imperial College Healthcare NHS Trust or Guy’s and St Thomas’ NHS Foundation Trust work to deliver and improve services to its local population; private consultancies such as Lexica, Mott MacDonald or Agencia support the UK system with strategic redesign and planning consultancy; and national bodies such as NICE or General Medical Council (GMC) provide guidelines to the wider system.
•It has a nationally coordinated workforce planning – monitoring of healthcare workforce, accreditation of training programmes, delivery of speciality education and continuous professional development. UK organisations such as Health Education England (HEE) build the foundations of capability, while organisations such as Kings Commercial, Linea, Royal College of Practitioners (RCGP) or NHS Leadership Academy provide education & training packages.
• An organised system with sophisticated data collection for direct care, service planning and research is the keystone of organised healthcare in the UK for 100 years. Rich data sources enable digital technology ecosystems, including teleconsultations, self-care and care management, and a highly diverse private sector. Organisations that strengthen the health system include digital health consultancies such BJSS, Difrent, Methods Analytics and AdviseInc, who o er various solutions bespoke to the needs of the system.
•Primary care and public healthfoundations of the NHS from education and professional development through to organisation and commissioning services –enable patients to access all NHS services. Organisations that provide innovative local primary care delivery in the UK include AT Medics and Modality to wider national resilience on public health including UK Health Security Agency (UKHSA).
•Quick systematic delivery of innovation is achieved through organisations like Accelerated Access Collaborative (AAC), NIHR, NICE and Academic Health Science Networks (AHSNs). New approaches to emerging challenges such as sustainability, cutting edge infrastructure and pandemic response can be found through organisations such as the Cell & Gene Therapy Catapult or Congenica in precision medicine, Currie & Brown in smarter infrastructure, Newcastle NHS Foundation Trust in decarbonisation and NHS South, Central and West or Diamond Light Source in pandemic resilience.
•The UK’s leadership in genomics is recognised globally, from the completion of the 100,000 Genome Project and UK Biobank, Genomics England through to the NHS Genomics Medicine Service. The Genome UK Strategy sets out an ambition for the UK to be the world’s most advanced genomic healthcare ecosystem. This presents opportunities to accelerate research, develop innovations in new technologies and data science, and to apply genomics in the clinical setting to diagnose disease at an earlier stage and also predict and prevent diseases before they might appear. At the cutting-edge of genomic healthcare are informatics tools and precision medicine evidenced by the genomic surveillance of the SARS-CoV-2 virus by the world-leading Wellcome Sanger Institute.
For more information and to share experiences, we would be delighted to put you in touch with the relevant teams. Please do get in touch with us.

“The NHS is leading in new approaches to emerging challenges – sustainability and carbon neutral policy, cutting edge infrastructure and pandemic response”
Rahul Agarwal
Deputy Head: Healthcare Department for International Trade UK
As the UK’s National Health Service approaches its 75th birthday, International Director Ged Byrne discusses new ways for global health systems to access its experience and knowledge via the NHS Consortium
The NHS has seen a huge amount of innovation in the past 75 years - from public private partnerships (PPPs) to pandemics, the rise of the internet and the birth of digital health to the beginnings of genomics and personalised medicine.
It saw the first IVF baby born and the earliest hand transplant take place.
It conducted the world’s first mass vaccination programme, for diphtheria and polio, in 1958 and it was the first health system to initiate the latest, for COVID-19 in 2020.
In nearly 75 years it has seen its share of mistakes, mis-steps, learning and lessons. It has amassed a huge amount of data, IP and experience, both right and wrong, in the delivery of universal healthcare. But there is always a long way to go on the journey to outstanding.
With a huge amount to learn and share, the NHS o ers an opportunity for health systems around the world to benefit from its experience. Through the NHS Consortium we have created an easier way for our international partners and friends to access the knowledge, expertise and

experience of our 75 years, while also giving us the facility to access their examples and opportunities for our own health system.
For the last 10-15 years the NHS has started to forge partnerships around the world. My own team at Health Education England (HEE) has worked extensively creating earn, learn and return programmes in Africa, the Middle East and South Asia. Individual NHS providers such as Imperial College Healthcare NHS Trust and Great Ormond Street Hospital have provided consultancy work and knowledge to their colleagues across the globe. Our ambition is to build on these strong foundations to create a single, broad and welcoming front door to the NHS for the international healthcare community.
The new NHS Consortium initiative, launching at Arab Health, will help
international healthcare leaders to reach into the NHS and be provided with expertise, partnership, collaboration and friendship. The aim is to help build and develop existing health systems, enhance the NHS and create long lasting alliances to help face down the global health challenges of the future.
In 2023 the re-organisation of the NHS will mean that some of our nationwide functions will merge.
My own department at Health Education England along with NHS Digital, our national public health function formerly known as Public Health England, our regulators at the Medicines and Healthcare Products Regulatory Agency and the National Institute of Clinical Excellence, along with our regional bodies for Scotland, Wales and Northern Ireland, will become a new ‘NHS England’.
As part of this merger, this body will sit within the centralised NHS and provide

international engagement and partnership for international opportunity, both commercial and philanthropic.
With ‘bottom up’ engagement from individual NHS trusts and organisations paving the way, and continuing to create opportunities for partnership, the NHS Consortium will create a ‘top down’ approach to engaging with the NHS for global partners.
Our hope is that we will have global conversations at every level, from Governments and health systems to operators and payors, to discover where our common problems and challenges lie. We will also explore how we can assist each other to deliver high quality universal health coverage worldwide.
By identifying the right individuals, experience, IP and, most importantly, the right peer to peer conversations we will shed light on mutual ways to help each other. Enabling other healthcare systems to learn from our successes and failures in the UK will ensure that our own knowledge and understanding of di erent global approaches are up to date.
It is only through direct consultation and collaboration from peer to peer, clinician to clinician, educator to educator and administrator to administrator that we will learn where we can have an impact through vital transfer of learnings.
The key to this engagement and activity is to understand what the NHS is and what it o ers.
• The NHS is the national healthcare system of the United Kingdom
• It is free at the point of delivery and provides universal health coverage to the entire population of the United Kingdom
• It is not an international clinical operator

While the NHS is made up of a multitude of provider organisations (or Trusts) that span everything from primary care to mental health and acute & specialist hospitals, it is not (by and large) an international clinical operator. In rare cases individual NHS trusts may get involved in operational partnerships outside the UK with overseas providers, but this is very much not the norm.
The NHS is an organisation with a wealth of knowledge, IP and experience that can be shared for the benefit of patients everywhere. By discovering the ways in which other global systems have dealt with their issues, the NHS will acquire valuable tools to move forward. Such is the nature of true partnership.
•It is philanthropic
Our partnerships extend to working with aid agencies, the WHO and across the world to support e orts to ensure universal health coverage for all, even the poorest in our global society.
•It is also commercial
The NHS also o ers paid-for consultancy. It has the ability to use knowledge, experience and IP to provide commercial and paid-for solutions to providers, Governments and payors across the world. Our knowledge and advice is not theoretical; it is real and practical, based on 75 years of valuable lived experience.
•Most important of all, we are listening and we are open for business
It’s about conversation, discussion and opportunity. Contact me, my team or our partners at Healthcare World and let’s have a conversation about where the NHS fits into your health systems, your plans, your aspirations and ideas.
kevin.miles@hee.nhs.uk
TCC@hee.nhs.uk https://global.hee.nhs.uk
“The aim is to help build and develop existing health systems”
Ged Byrne International Director HEE
Inclusive use of technology can improve patient outcomes and service quality, says Alex
Kafetz,Director of International Projects Beamtree
Healthcare organisations are overwhelmed by the amount of data they produce, and the number of market solutions o ering to solve this problem. It’s easier if senior executives have an idea of the value of their data and how it can be used to improve their services and thus their patient outcomes.

In today’s digital world, it should be simple enough to research a surgeon or the department he works in. But in practice, it’s been di icult to quantify rates of success and failure without the numbers to back them up.
Similarly, how can unused data in hospital systems be repurposed to create exciting new areas that will engage clinicians to adopt it?
For Alex Kafetz, Beamtree’s Director of International Projects, it has to be done in such a way that doesn’t complicate further the lives of busy frontline professionals. He says it’s about making their lives easier, giving them more time to spend with patients to discuss treatment options, and preventing risk.
Beamtree is an Australian company that understands how to collect and integrate data, interpreting information and gathering
insights. It focuses on allowing providers to reinvest their resources, so they can deliver better quality care, reducing avoidable deaths, readmissions rates and length of stay. In practice this means improving the accuracy and timeliness of data to enable tracking and enhance the quality of care, by providing clinical support for better decision-making, and delivering cost e iciency through activities such as price benchmarking.
“With respect to the big American EMR vendors, clinicians haven’t always been able to realise the full value of these systems,” Alex says. “However, they are a fantastic data repository, so much of our activity involves taking the data from the electronic medical record and turning it into meaningful applications, primarily for doctors. But we also spend a great deal of time with health information managers and clinical coders,
and we spend a large amount of investment in data quality as well.”
Beamtree’s solutions include PICQ®, the industry standard for or assessing and reporting on the accuracy and specificity of clinical coding data. A quality assessment tool, it uses more than 900 indicators to assess
and measure coding accuracy against the ICD-10 classification enabling benchmarking across hospitals, and provides insights to improve reported activity. There is also RippleDown Expert™, which automatically applies clinical expertise to generate patientcentric reports, replicating the expert’s unique decision-making process at scale. Developed by pathologists for pathologists, it improves the quality and speed of information delivered to clinicians. RippleDown Expert™ provides treatment recommendations, real-time alerts, and advanced reflex and appropriate testing recommendations. Added to the mix is RippleDown Auditor ™, which automates real time data reviews, ensuring accuracy in data entry and providing visibility. Beamtree’s clients operate across 25 countries and over 1,100 locations.
Beamtree is currently working with Saudi Arabia to improve the consistency of coding and data reporting. “In Saudi Arabia we audited a large number of hospitals on the ground actually during COVID restrictions, which was another challenge,” Alex says. “The aim was to help them with Vision 2030 by understanding the baseline for the quality of data in the Kingdom. Now we’re moving forward to help them consider how it can be improved, and the first step is top quality data.”
The complexity stems from local coding customs. The International Classification of Diseases (ICD10) system turns the patients journey into a set of codes which are used for planning and analysis, but the issue lies in the recording by humans - this is where the errors creep in. They can result in apparently poor performance by a provider, but on inspection there could be a simple reason. Alex tells the story of a UK hospital that had a high instance of foreign objects le in patients following surgery. On inspecting the data, it turned out to be synthetic lenses a er cataract operations, but the coder had thought they were errors.
Other examples can lead to price benchmarking – the classic story is hip replacements where one code can make a procedure more expensive than another. “Worldwide, we don’t have enough clinical coders,” Alex says. “It’s a very specialised profession and people with that mindset and that kind of skills are being diverted into data science roles. If we can automate the easy end of the scale, which frees up the coders to code manually the more complex material,
which is intellectually stimulating, we can protect that part of the workforce and also code quicker.”
A fascinating part of Beamtree’s Ainso Deterioration Index product is around patient deterioration, tracking their progress and seeing which interventions have benefit. This is based largely on the work of Beamtree’s lead clinician, cardiothoracic surgeon Dr Levi Bassin who is based in Sydney. Having spent many years unable to perform scheduled operations on patients because they had deteriorated unexpectedly, he decided to develop algorithms that could determine the risk of deterioration.
The system alerts clinicians if there is a high risk of deterioration in seemingly healthy patients and enables clinical conversations to manage the scenario. “We have fewer false positives than other systems, but our sensitivity remains,” says Alex, referring to a published paper. “Clearly this improves mortality rates, reduces admissions to intensive care and impacts the bottom line.” In addition, clinicians are able to determine whether patients could be discharged on an expedited pathway.

As much as anything, the company’s aim is to enable doctors to be part of the digital health revolution, involving clinicians and getting their buy in for technology that will make their job easier and patient outcomes better.

“Everything we do is underpinned by this amazing platform called RippleDown, which was invented in Sydney University 20 years ago and has been mainly used in pathology,” he says. “Now we’re widening it out, such as the deterioration example. It’s a rule builder, but it’s really simple. A clinician can build rules, write it in plain English, and it understands and matches it. With other systems, the clinicians have to send the rule to be hard coded in. In addition, it allows infinite rows and will immediately test that rule against any other rule you’ve written previously, even if it were three years ago, and it can have an infinite number of rules.”
So clinicians like the system – and that’s always a good start!
“Much of our activity involves taking the data from the electronic medical record and turning it into meaningful applications”
Alex Kafetz Director of International Projects Beamtree





Using real-world data, predictive algorithms, digital biomarkers to advance proactive, predictive medicine. Huma’s technology powers digital ‘hospitals at home’ and decentralized clinical trials.





We are a unique, forward thinking and specialist global healthcare consultancy focused on healthy populations. Together with our clients we are influencing the factors which a ect health outcomes – both in terms of preventative measures and healthcare interventions.

Our experts connect thinking between health and infrastructure – o ering a broad range of skills and expertise to support clients design, plan, implement and evaluate their healthcare services. In all our work, we take a digital first approach.
We have permanent o ces across the GCC, including Saudi Arabia, United Arab Emirates, Qatar, Bahrain and Oman.

Our services and expertise include:
• Strategic and capacity planning
• Healthcare planning
• Service design and reconfiguration
• Digital healthcare and digital hospitals

• Business case development
• Project management
• Built environment and estate strategies
• Facilities management advice
Opening opportunities with connected thinking.
Mat Oram of AdviseInc discusses whether improved procurement procedures lead to better patient outcomes
Discrepancies between hospitals and inbred ine iciencies have long led to increased cost and ine iciencies. Price benchmarking from a procurement perspective is o en solely around a product, not services or maintenance. However, the information in a purchase order line cannot provide enough detail to provide a side-by-side comparison for procurement managers to understand where the true savings lie.

For the past 8 years AdviseInc has been developing a revolutionary system to change the procurement landscape across hospital networks via a nationwide product price benchmarking system in the clinical theatre space. We deliver price benchmarking to 80 NHS Trusts in England, all NHS Wales, all Northern Ireland and 25 per cent of all Scottish NHS spend. We have provided transparency across billions of pounds of NHS spend for the first time.
By cross-referencing and cross-checking the product code, AdviseInc’s so ware allows visibility across the individual NHS trust networks, not only reducing variation, but saving money and reducing clinical risk. However, to address the need for direct price comparisons across the whole NHS, we have created a Procurement Dashboard or PD, an intuitive dashboard providing full spend analytics. Through PD, we see every non-pay related spend that goes through the hospital, whether it’s drugs, estates, or computers across most of the UK. We have data on about £150 billion of the NHS spend at our fingertips - we can tell you what was bought, who it was bought from and how much they spent, down to the
person who brought it to approval. We give each hospital full visibility.
Building on PD, we developed a further service - PD Plus, and that plus is us. We recognised that our customers struggled to optimise the features of PD due to a lack of time and capability, so we do it for them. We create very detailed reports, giving our
Mat CEO AdviseIncclients everything about clinical variation, from Trust to Trust.
Nobody has been able to classify this kind of data before. Not only do we present it back to the hospitals, but we are adding a layer of classification that nobody else has ever seen in the UK, and perhaps the world. It is the first time I have ever seen data like this, which is why we are so excited about it.

Crucially we are focusing on reporting levels of clinical variation and increasing levels of standardisation across the board. Too o en we see procurement o ices ordering 12 versions of the same product where others will limit their stock to one - all we do is ask the clinicians why.
It’s this sort of conversation that takes place through our PD Plus service that conducts more in-depth analysis and works with clinical teams to reduce this variation. In doing so, we are reducing clinical risk. Where there are di erent versions of products, there are di erent systems and sets of tools that go behind those products in the operating theatre. When a nurse or other practitioner comes in, they all have to be aware of these variations. If there is only one set of tools, the risk is reduced because there cannot be any overlap. To drive outcomes, one must reduce variation. That’s what we do and, by helping financially, we are also helping with better patient outcomes.
So how do we do this? We have developed analytics that sit on top of inventory management systems that help track all the products in a theatre storeroom, monitoring low stock, out of date equipment and pricing changes. Every time an order is raised we can track manufacturer changes, such as price increases, and eliminate administrative ine iciencies.
Going live in March, our NEW AdviseInc platform will launch, allowing a faster turnaround of data and analysis. We are going to be able to o er mobile optimisation, with a new, uncluttered visualisation package.
Further to this, we have developed Control Tower, that sits on top of lots of data in our new platform allowing Integrated Care Systems (ICSs) across the UK see which hospital is out of tolerance across key areas. It is designed to help a customer navigate massive volumes of data to get to an action point. We are allowing ICSs the best possible view of their landscape, enabling them to bolster their e ectiveness and again improving patient outcomes.
Our tools provide a self-serve analysis of colossal datasets to support quicker and smarter decisions across the procurement framework. Detailed product information, product pictures and information about the suppliers all contribute to a comprehensive support system for each hospital. We’ve become a one stop shop for everything to do with procurement analytics.

“We have data on about £150 billion of the NHS spend at our fingertips”
Oram
Primary and preventive care are the fundamental building block of healthcare systems, says
Isabel Arango, Mott Macdonald Principal Advisor and Regional Healthcare Consulting LeadAcross many healthcare systems, strategy is the intent or ongoing process to take population health management and primary care to the next level, as access to the primary care and preventive services are crucial for all populations throughout all stages of life. The adoption of valuebased models has further emphasised this need.
Why should there be an increased focus on primary and preventive care services?
Studies have demonstrated the e ects of a robust and accessible primary care and preventive delivery system. These e ects include improvements to population health, life expectancy and greater health equity at lower costs.

In the UK, for example, spending focused on prevention has been found to be three or four times more cost-e ective at improving health outcomes than money spent on curing illnesses.
Furthermore, regardless of the initiatives and improvements, lower life expectancies are still a challenge for many sections of the population due to several factors. Among these factors are location (rural areas), and cultural and socioeconomic challenges. These inequities became evident during the COVID-19 pandemic.
How can health systems ensure the entire population is served and improve health equity and e iciency throughout the system?
The answer involves a comprehensive and coordinated approach that engages all facets of social, mental, and physical health. The entire ecosystem and stakeholders (providers, policy makers, payers, and employers) and most importantly patients, must be engaged in order to produce the desired outcomes, addressing present and future needs. As the healthcare landscape continues to evolve, so should the way population health is integrated
and managed. There is a need for increased focus on initiatives that include disease prevention and management, care coordination, patient education and engagement, as well as other activities aimed at improving population health.
It is no surprise, then, that health systems throughout the world are reevaluating their current models of care and infrastructure, opting for designs that tackle the seen and unseen drivers of health with integrated primary care at its core. Technology, data, workforce capacity building, evidence-based medicine and patient empowerment tools are all components required to engineer and execute a design that will service the intended population and yield the desired outcomes while optimising care.
Given the complexities with the physical and operational design of said infrastructure, even the largest and most sophisticated health systems will find an undertaking of this magnitude a challenge. Particularly if this involves the continuation of operations during the implementation of initiatives. Post pandemic, many health systems are turning to technical experts with interdisciplinary expertise that can provide consulting and advisory services in order to assist them.
How can Mott MacDonald assist health systems in achieving their population management and primary care goals?
At Mott MacDonald our purpose is to improve society by considering social outcomes in everything we do. Our healthcare clients benefit from over 30 years’ in-house technical expertise in cross-cutting sectors essential to the development and improvement of health systems. With a focus on digital innovation, our dedicated healthcare team includes strategists, demand and capacity modelling specialists, operators, healthcare planners, clinicians, cost consultants, project managers, facility management, digital health (digital twin) and estate planning specialists. We are experts in Integrated
Impact Assessments (IIAs) – a key resource document to inform decision-makers, key stakeholders and the public of the potential impacts arising from the reconfiguration of healthcare services. This considers and evaluates the potential health outcomes and inequalities, carbon and environmental impacts from the reconfiguration plans.
More specifically, what is your primary care experience?
We have an in-depth understanding of primary care services and estates. Our experience encompasses an end-to-end process of estates requirements built upon
patient need and models of care. Our team members have clinical and operational primary care experience, including the development of clinical and estates strategies of primary care networks (groups of GP Practices in the NHS in England). This work involves the creation of primary care network profiles detailing clinical services, population need, growth and disease prevalence and profiling, future models of care and priorities, functional estates requirements and full costing and appraisal of current assets.
In the Kingdom of Saudi Arabia, we supported a similar exercise as part of the Vision 2030 programme to improve the
e iciency and delivery of public health sector services. This was completed across 75 primary healthcare centres (PHCs) in Riyadh and Jeddah.
And finally, for many years, we have also supported NHS England as their national evaluation partner. Initially evaluating primary care initiatives being piloted through a programme called The Prime Minister’s Challenge Fund and subsequently an evaluation of the General Practice Access Fund and latterly evaluation of the Time for Care team. Currently, we are the national evaluation partner for the NHS England Primary Care Transformation Team’s main programme of work.

Mott MacDonald employs 18,000 sta in 135 countries worldwide, of which over 1000 operate out of the Middle East. Across all our work, we are privileged to be part of clients’ solution in order to obtain their desired outcomes with primary and preventive care, while also satisfying our company’s goal of creating healthier people and healthier societies.
Automation can create a better healthcare ecosystem,
Praful Mehta CEO of Vamstar tells Healthcare WorldThere is a general recognition that the healthcare sector provides huge amounts of data. It’s also agreed that there is a huge amount of waste and duplication of processes, given the complexity of healthcare organisations and the clinical requirements. And again, that many clinicians and data scientists have devoted time and energy to resolving the issues that a ect them most closely.
For Praful Mehta, this has been supply and demand. A geneticist by training, he moved into the industry 20 odd years ago and has played roles in commercialising various products in Asia. He then moved to GlaxoSmithKline globally within the
senior leadership, and for the last decade has focused on pricing access and value in various countries, advising governments and suppliers and buyers in the market on how to create a better healthcare ecosystem.
HW: How is Vamstar di erent from other platforms?
VamStar is the first fully AI based supply chain platform that looks at the demand and supply patterns in the market, and matches to the needs of the local ecosystem. We work in 100 countries and we collect data on the buyers side, looking at the demand from public systems along
with its scope and structure. We then have suppliers in the system matched to that demand. We have a number of tools and technologies built to support that supply and demand and to improve the e iciency of the transaction and trading processes that exist within markets. Much of our platform is super localised from that point of view.
We started the company in 2019 from three co-founders to 150 people today in five countries. We work locally in the UAE and Saudi and we are also expanding significantly in other GCC markets. Similarly in Europe, we work locally in the UK, in many of the countries in in Europe and in the Far East as well.
HW: What was it that you were able to o er during the pandemic that enabled you to grow so exponentially?
Within healthcare, there was a big realisation that digital is the way forward and engaging with the buyers must move digitally, so we leveraged that on the backdrop of COVID. Our clear value is that
costly and manually run processes can be automated with the help of our tools and platform. In addition, both the buyers and suppliers have much better visibility of the market, including pharmaceutical drugs, vaccines, all hospital and care setting medical supplies, and also surgical products and equipment.
Our platform is a two-sided approach on both the supply and buyer side. We set specific companies and organisations on the platform so they can keep their processes completely aligned and scan the wider market. We o er the entire platform as so ware as a service, or SAAS, which means that the buyer or the supplier can access the data at a fraction of the cost.
We work with all major companies, so we are well-versed in large enterprise systems or ERP systems. This inclues procurement systems on the buyer side and with CRM systems on the supply side. It’s very expensive for most buyers and suppliers to gain access to harmonised data, so we do this at scale for them.
We work with local laws and regulations
when it comes to data hosting, data privacy and regulation standards. We follow all local protocols so it’s hyper-fast and superconnected in one single platform.

Large organisations in these regions approached us during COVID for technologies to make them more e icient in their supplier engagement. We expanded quite significantly in the UAE, especially in the private sector - we began with one or two hospital groups and now have up to 70 per cent of all private hospitals on the platform. We are slowly making our way into other GCC markets by working again with large buying groups, bringing the use of analytics and AI in terms of understanding what buyers buy and where they buy.
Many customers focus on common and generic products such as medical supplies and everyday items. They utilise us for specialised products with only one or two select suppliers, and we provide them with the ability to manage their supply chain on the platform.

The real value add is being able to scan the market for comparable products. And in terms of hyper-specialised product, we can provide visibility of products that can improve the level of care, for example in diabetes or in oncology. It’s about an in depth understanding of the products, along with the data, that helps buyers make the right product decisions for the care environment.
We are making investments going forward in Saudi and will be expanding our teams both in Saudi Arabia and in the UAE. From our supply chain platform point of view, we are selectively focussed on key markets within GCC, Europe and Latin America, targeting the countries where we see maximum ine iciencies which we can resolve.
HW: What is your vision for Vamstar?
There’s a sizeable amount of waste in healthcare because the same processes are repeated by suppliers and buyers many times over. Our goal would be to aggregate and standardise those processes in a common system to improve e iciencies. This could also mean a common exchange for medical supplies and pharmaceuticals, developing into a clearinghouse for the industry and standardising repeated processes where there is a lack of data. Automation allows this to become leaner and cleaner, meaning better profits for both suppliers and buyers.
As we mature our data and connect systems, this will enable both buyers and suppliers to plan for the future. Not only in regard to products and services, but also when it comes to new innovations and new solutions. It would be around collaborating and even merging some of these products together into one common unified system.
The lack of standardisation is one of the major pain points in healthcare, especially around data, and we are trying to solve this problem. But when it comes to actual utilisation of that data, whether it’s in clinical processes or in supply chain, it’s very limited. We are looking at developing systems and scaling technologies which can utilise that data and improve the quality of care.
HW: Do you see healthcare from global viewpoint?
Yes, there is a lot of willingness to look at health care systems holistically. One big realisation has been that healthcare supply chains are completely intertwined and very complex, and the costs are out of control in pretty much most major markets. We actually see a lot of harmonisation coming up as buyers or healthcare actors are learning from each other.
The UAE and Saudi Arabia in particular are already taking some fast moving forward steps for the future around the digitalisation of healthcare. And we have much to share and learn from the stakeholders as well.
“One big realisation has been that healthcare supply chains are completely intertwined and very complex, and the costs are out of control in pretty much most major markets”
Praful Mehta CEO Vamstar
Actively choosing to make decisions informed by data is the way forward for healthcare, say Simon Swift and Richard Oakley of Methods Analytics

We generate so much data in healthcare, but we haven’t reached the stage yet where we appreciate its richness and derive value fully. The benefits of data-orientated decision making are clearly obvious in healthcare settings, yet data is too o en relegated to examination by interested experts in a corner rather than using it to inform strategy and operations. So how as an organisation do you
become data-oriented - actively choosing to make decisions using data at all levels? Our approach is to ensure three questions are answered before looking to use data to inform a decision:
1.Why are we going to do this? Why do we need a data driven approach for this project or purpose and what is the benefit? Understanding the why and really scoping it down is key, otherwise
the business can’t drive forward accurately and cleanly.
2.The second thing is how? And that’s the technical question. You don’t do the how until you really know your why. What data do we have? How do we bring it together? How do we make sure it’s valid and accurate, and how are we going to analyse it and present it? It’s also making sure there’s a shared understanding of what numbers mean and having a very strict definition.
3.Once we have our data analysed and presented, so what? Do we know how to apply this to our problem or our purpose? So we have to define our goal and how we know we have got there. Then, are the management levers available so that these decisions actually impact the organisation. Otherwise, it’s a waste of time.
Healthcare organisations actually make a lot of data-orientated decisions. A high blood pressure reading will lead to action. When you work at this level, people can understand the concept, but it needs to be ingrained in the organisation’s culture and has to start from the top to really see the impact. Yet it’s really easy to transition into those data-led activities if you use examples like this to help people understand what being data-orientated means.
You can engage with data-oriented decision making at all levels in a business, the strategic level, the operational level and the tactical level. To inspire the move towards data-orientated decision-making, the way the boardroom uses data has to fundamentally change. They have to value the expertise of their data analysts – people whose expertise is data – and bring them

into meetings to present that data, not deal with data from a management perspective, presented by those whose expertise is management. In healthcare, in particular, we undervalue that expertise. We wouldn’t have the same attitude towards an expert whose field is clinical.
In a hospital, for example, if there are 56 stranded patients, (those who have been in for longer than two weeks), the
director of nursing, the site manager and the medical director will all have a slightly di erent sense of what 56 stranded patients means to their organisation. They need to have a shared understanding to be able to agree on a common solution and a set of actions, so there needs to be someone who deeply understands the data who can frame this for all of them and facilitate that shared understanding of what it means.
Decision makers must be clear about why they are looking at data; ideally it is for insight into a problem where clear actions can be taken; too o en it is in the hope of finding a magic easy fix or to look to validate a decision that is already made. For example, measuring the number and timing of patients attending the Emergency Room could be useful for forecasting, but if you can’t adjust sta ing or increase discharges to accommodate that demand there is little point operationally. Knowing you will be overwhelmed is something the people on the ground will have identified anyway, so it’s probably only useful for building a business case at a strategic level.
Equally, at a tactical level, using data to evaluate whether everything is in place for a patient to receive a particular care bundle on a given day could make the di erence between, for example, 10 or 15 patients receiving treatment or slots being reallocated just because the data was consulted and anomalies corrected in advance. So that is an exercise where dataorientated decisions have a direct impact.
Within data-orientated organisations there should be a team for exploratory analysis, another that concentrates on operational reporting and a platform that allows them to do both. The areas of expertise should be separated to ensure their e ectiveness, so the organisation of the data teams is important. This is true at the top level as well. The data team under the Director of Finance, for example, will be very di erent from the data team under the organisational vertical that reports into the medical director. The first will think about money and e iciency, while the other will consider quality, outcomes and safety.
In healthcare, your technical “how” is unlikely to be impacted by this choice, but your organisational feeling of

“You can engage with dataoriented decision making at all levels in a business”
Simon Swift Managing Director Methods Analytics
what is important shapes this. Thus it’s really important to have a centralised data function in large organisations. Otherwise there are competing aims. It should be designed in a way that serves the needs of the entire organisation, not just one specific niche, because otherwise data will be repurposed for something inappropriate. This is a pitfall that every organisation finds at some point, so it is key to centralise data function under one body and ideally professionalise it as much as possible. A data-orientated organisation should have a Chief Data O icer whose remit includes data use as well as just storage and governance.
A clear data strategy enables an organisation to understand and so deliver what the board intends; it should enable an organisation to deliver its business strategy better i.e. faster and cheaper. To execute a data strategy however, requires people in the organisation to be literate in the use of data, particularly C-suite and managers - anybody who is expected to use data to inform the decision or to be able to interpret data needs to have the requisite skills. Therefore, there is a training requirement and skills analysis to be undertaken. Data literacy is like any form of literacy - knowing when to use your own expertise and when to defer to others.

As an example of this literacy, if you set a target, you have to think about the unintended consequences of driving to performance against target. It’s helpful to know about examples such as the Cobra e ect of perverse incentive, where a government concerned about the number of cobras in the area started o ering a bounty. Initially, the numbers went down; then people started breeding snakes for money. In the same way, if you clamp down too hard on targets to discharge patients from hospital, you will start seeing suboptimal care.
However, data alone cannot be used to eliminate unintended consequences. It’s vital to get people psychologically in the right place so that they don’t start using inappropriate action in order to deliver. It’s also important to ensure you design companion metrics to look broadly at impacts and not be too narrow in your surveillance, ideally thinking in terms of driving overall behaviours primarily rather than numerical objectives. This is particularly important in human-
centric processes like healthcare where the complexity and individuality of the problems to be examined far exceeds the data collected or used.

Most data projects fail because the strategic goals are not tightly defined and the problem is not easily measurable. Data is turned to in hope rather than reasonable expectation, which is fine if the ambition is to explore what is possible. O en though the Why, the How or the What are missing, be that scope, timelines or other determinants. There need to be really hard
and measurable definitions, so it’s clear what will be delivered and how it can be done and when by. Once this is in place, of all things, data projects should be best able to prove benefit and return on investment. Methods Analytics’ particular expertise is with an open problem. We start at the strategy point, helping people understand how to use data to deliver business benefit. We analyse the data and present our findings anywhere along the data lifecycle. In healthcare no two patients are the same, so you need big numbers with meaningful data before you start to draw conclusions. But if you start to use data to directly influence decisions there is a virtuous circle in reach, one where the data-informed decision then has its impact evidenced by that same data in future and results in that most elusive thing in healthcare transformation - the change that sticks.
“A clear data strategy enables an organisation to understand and so deliver what the board intends”
Richard Oakley Director of Data Science and AI Methods Analytics
Oncology
Immuno-oncology
Immunology
Musculoskeletal
Cardiovascular
Gastrointestinal
Rare Diseases
Clinical Project Management Resources


Clinical Operations Consulting
Human Efficiency Consulting
Strategic
Virtual Reality is a valuable tool for better hospital design, say Nick Ainscough, Regional Design Technology Lead, and Nick Clarke, 3D Visualiser, at Arcadis IBI Group

Virtual reality (VR) has been around in some form since the 1950s, later revolutionising gaming and entertainment. Now having matured considerably, VR and Augmented Reality (AR) innovation has ushered in tremendous opportunities across many sectors. When applied to architecture, VR has the potential to transform the way we design, plan and deliver new buildings. Crucially, it can be applied to deliver futureproof healthcare facilities that better meet the evolving needs of the sector.
In 2021, the healthcare and medical devices sector was highlighted by 34% of experts surveyed as being the most disrupted by immersive technologies. That’s more than advertising, education or retail. Looking ahead, estimates suggest that VR in the healthcare market will reach around USD $2.8 billion by 2028, at a compound annual growth rate of 36.50% compared with 2022.
Adoption of VR headsets accelerated during the COVID-19 pandemic as
practitioners raced to find ways around social distancing requirements to ensure the continuity of critical services. Apart from the growth of virtual communications platforms and telemedicine, VR emerged as capable of solving serious challenges. For instance, training doctors and nurses in additional medical skills in a hyper-realistic virtual hospital environment is one way to address widespread sta shortages and overcrowded hospitals. Beyond that, we have seen first-hand how VR headsets can be used to optimise the design stage of hospital projects.
Hospital buildings are highly complex and subject to tight regulation (i.e. to prevent infections) and therefore physical models are o en used when building new facilities, to enable vital testing of emergency or operating rooms. However, the process of testing these mock-ups also takes place later in the design stages, meaning that any changes can be di icult and costly to make. VR technology, on the other hand, can support a more e icient approach to
testing, with greater flexibility to explore various layout options, identify issues and make corrections easily before construction even begins. It also opens the door for closer engagement with stakeholders and end users who can feed in their inputs while visualising spaces in a simulated environment.
Many people are involved in hospital design, from architects and planners to engineers and contractors, and it is also important to involve those who will be using the space every day – nurses, doctors, clinicians and other hospital sta – as early in the process as possible. This is something we focused on when delivering a new hospital Accident and Emergency (A&E) building in the UK. The project began pre-COVID-19, and the intention was to develop 3D VR models of the external building and interior spaces to demonstrate to the client what the finished building would look and feel like. The client was able to give immediate feedback and help us to better understand their needs. The interactive VR environment made it possible to check every detail, including the layout of furniture in a specific clinical room, the view from a nurse base to ensure patients are in sight, and much more. Clinical sta from every department were
also able to experience their own unique departments and guide the Arcadis IBI Group team to develop these individual spaces in the most e ective way. While we used Revit models for the departmental layout, connections and adjacencies, a more detailed and considered 3D model was generated to progress the materiality of the building
façade and internal spaces such as waiting rooms, reception and patient wards. The furniture, fittings and equipment (FF&E) library, for example, has been customproduced by Arcadis IBI with myriad options for a coordinated 1:50 loading process and enhanced visualisations.
It’s important to note that project teams can sometimes number hundreds of people spread across multiple locations. With a model with such a high degree of detail in plan and elevation, the interiors team could work simultaneously and collaboratively with the architects, landscape architects, 3D visualisers and all the other project teams. When the onset of the pandemic meant that visiting the hospital was impossible, we created a series of 360-degree panoramic renders that were linked together in a virtual walkthrough and hosted online for ease of access.
Virtual walkthroughs of buildings can be developed using the Building Information Model (BIM) and other so ware, which centres around the management of data-rich models to generate a digital representation of designs prior to them being realised in the real world. It can be challenging to read two-dimensional plans and imagine the end result, but an immersive virtual experience can help clients and clinicians visualise and understand proposed plans.
Another UK healthcare project involves delivery of landscape architecture and


interior design for a major hospital modernisation programme. Commencing in 2022 and due to be completed in 2027, it is being undertaken in three phases, with upgrades including everything from a critical care unit, sta facilities, a threestorey extension, a new main entrance, paediatrics ward and outpatient facilities, to a neonatal intensive care unit, new operating theatres, as well as private ward and outpatient facilities. Before construction started, and in the midst of pandemic lockdowns, clinicians were able to fully visualise all of these intricate plans with the help of a 360 walkthrough virtual tour. This enabled them to experience how the various new facilities would function in practice and provide valuable feedback to inform the entire process.
Overall, the promise of VR is a compelling one when it comes to hospital design. It can drive much quicker project timeframes, better consistency and accuracy, cost e iciencies and productivity. Moreover, it can cut down on the number of design meetings, site visits and waste, which renders it a sustainable option compared to more traditional methods.
Arcadis IBI’s integrated and technologyled approach to design enables us to provide quality advice, tailored solutions and significant process e iciencies while successfully involving key stakeholders and users from the earliest stages of design to ensure the highest standards and alignment with the hospital’s requirements. For us, it is a key component in the future design of hospitals and healthcare facilities worldwide.

“An immersive virtual experience can help clients and clinicians visualise and understand proposed plans”
Nick Ainscough Regional Design Technology Lead Arcadis IBI Group
The challenge of providing infrastructure that responds to and mitigates the impact of our changing climate is a key focus for future healthcare delivery, say Currie & Brown’s Helen Pickering, Global Head of Healthcare, and Adam Mactavish, Global Sustainability Lead

Climate change is the most important issue of our age. It is, according to the World Health Organisation (WHO), the biggest single threat facing humanity.
The health consequences of the growing climate emergency are both broad and profound. Heat, cold, flooding and other implications of climate change have both direct and indirect e ects, including impacts on disease and availability of essential resources such as food and water. Linkages between climate and health are particularly noticeable in the Middle East and Africa. A recent study led by Saudi Arabia into the impacts of climate on health in the Gulf Cooperation Council (GCC) area identified some of the e ects. This report makes for stark reading. Between 1979 and
2019, the region experienced an increase in temperature of more than 0.5 degrees centigrade each decade - over twice the global average.
Human health implications in the GCC region are widespread and significant. They include an increase in the number of dangerously hot days and subsequent heat related stress, through to impacts on air quality and on communicable disease as well as on maternal, reproductive and mental health.
The impact of the healthcare sector on climate change is substantial, it is responsible for almost 5 per cent of global greenhouse gas emissions and has a carbon footprint equivalent to 514 coal-fired power plants. If the sector were a country, it would be the fi h largest polluter on Earth.
The sector therefore has to deal with two issues. Firstly, it needs to minimise its own e ect on the climate by aiming for, and working proactively towards, net zero emissions; and secondly, it must prepare to meet the changing needs of populations that are experiencing a wide range of climate-induced stresses.
The carbon generated by healthcare can be attributed to a number of sources. Probably the most visible is the physical infrastructure - acute hospitals are some of the most energy intensive buildings in the world.
However, there are other less obvious activities that result in high carbon emissions. Travel, by patients, visitors, sta and the healthcare providers themselves; medicines, chemicals and inhalers; and, perhaps surprisingly, diagnostic equipment such as MRI’s, anaesthetic gases and metered dose inhalers. Figure X shows the full breakdown of the circa 25m tonnes of carbon emitted by the NHS and its supply chain in the UK.
“Decarbonisation of the healthcare sector and its infrastructure is a complex business, requiring input from di erent teams working in disciplines such as clinical, strategy, planning, as well as in the built environment,” says Helen Pickering, global head of healthcare, Currie & Brown.
There is, however, a strong determination to succeed. In the UK, Currie & Brown are working with leading healthcare institutions, such as the internationally renowned Great Ormond Street Children’s Hospital, who have declared Climate and Health Emergencies with ambitious targets for decarbonising their activities.

They have begun actively assessing options for radically improving energy e iciency reducing, and ultimately removing fossil fuel combustion across their facilities, together with a wide range of other measures aimed at reducing resource consumption, improving local environmental quality and the wellbeing of patients and sta .
In another visionary project where Currie & Brown are Lead Advisor, plans are being put in place as part of the Monklands Hospital Replacement Project in Scotland to eliminate fossil fuel use by creating an all-electric new hospital.
Currie & Brown is a leader in sustainable healthcare, working with providers who are dealing with the technical, commercial and operational challenges of bringing net zero carbon status to a number of new acute hospital projects, as well as helping existing hospitals and systems to develop their decarbonisation strategies. In existing hospitals, the focus is on managing the transition from legacy services to more e icient, modern and sustainable systems while factoring in both existing operating environments and budgets.
“The building of new healthcare infrastructure creates its own challenges. The construction process releases embodied carbon - along with use of materials, it can emit more than a tonne of carbon per square metre - and decreasing the overall footprint is a key consideration,” says Adam Mactavish, global sustainability lead, Currie & Brown
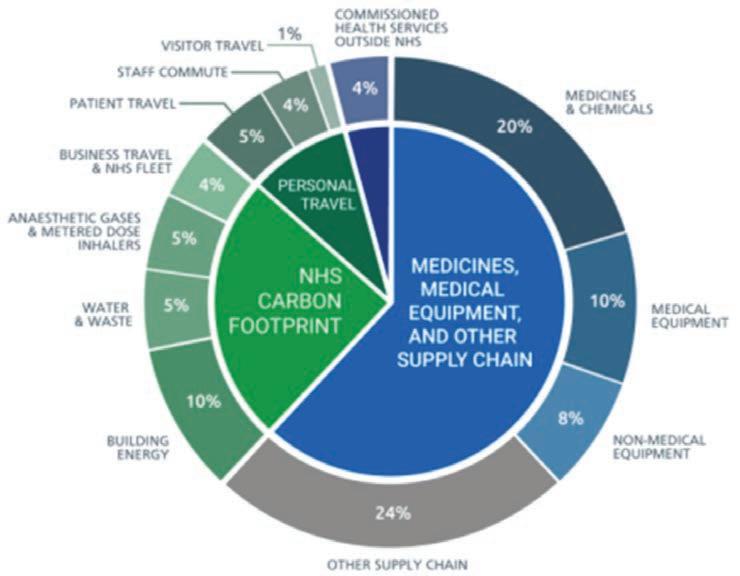
The use of digital healthcare, delivering care closer to home and smart buildings are all innovations that will help to minimise carbon emissions by reducing the amount of space and travel needed, leading to more e icient delivery of care and improved patient experience.
Using lower carbon materials in construction can also play an important role in increasing sustainability. For instance, part of the cement content of concrete mixes can be replaced or recycled steel used.
Although some lower carbon options are more expensive than using traditional materials and methods, there are also occasions when they may be less costly. It may be, for example, that energy e icient products such as brick or rendered cladding work out cheaper than higher carbon alternatives such as metal panelling.
For existing buildings, savings can be made by better understanding how the existing infrastructure operates and by introducing energy saving controls. High e iciency and performance lighting, ventilation and cooling systems and careful procurement of new imaging and diagnostic equipment can also play a big part in reducing power demand.
Removing fossil fuel use from heating and power systems plays a critical role in decarbonisation. In recent decades, combined heat and power systems have been installed, though in the long term they can be a block to decarbonisation if the grid itself is rapidly becoming a source of low carbon power.
All healthcare providers should be thinking about how their local climate will continue to change in the coming decades and take steps to ensure resilience under a range of future climate scenarios. Healthcare is at the forefront of helping mitigate emissions. These initiatives will have a material impact on national emission reduction goals, but importantly will also help to deliver operational e iciencies and improved patient wellbeing.
“Decarbonisation in healthcare requires input from many disciplinesclinical, strategy, planning and the built environment”
Helen Pickering Global Head of Healthcare Currie & Brown
Feedback Medical enables clinical data to travel with the patient, says CEO Dr Tom Oakley
Many healthcare systems are in a state of transformation, so patients and the clinical workforce need easy-to-use, flexible digital solutions available from anywhere. Feedback Medical enables clinicians to make better decisions faster from any location as our solutions are designed to be applicable to any care setting internationally.
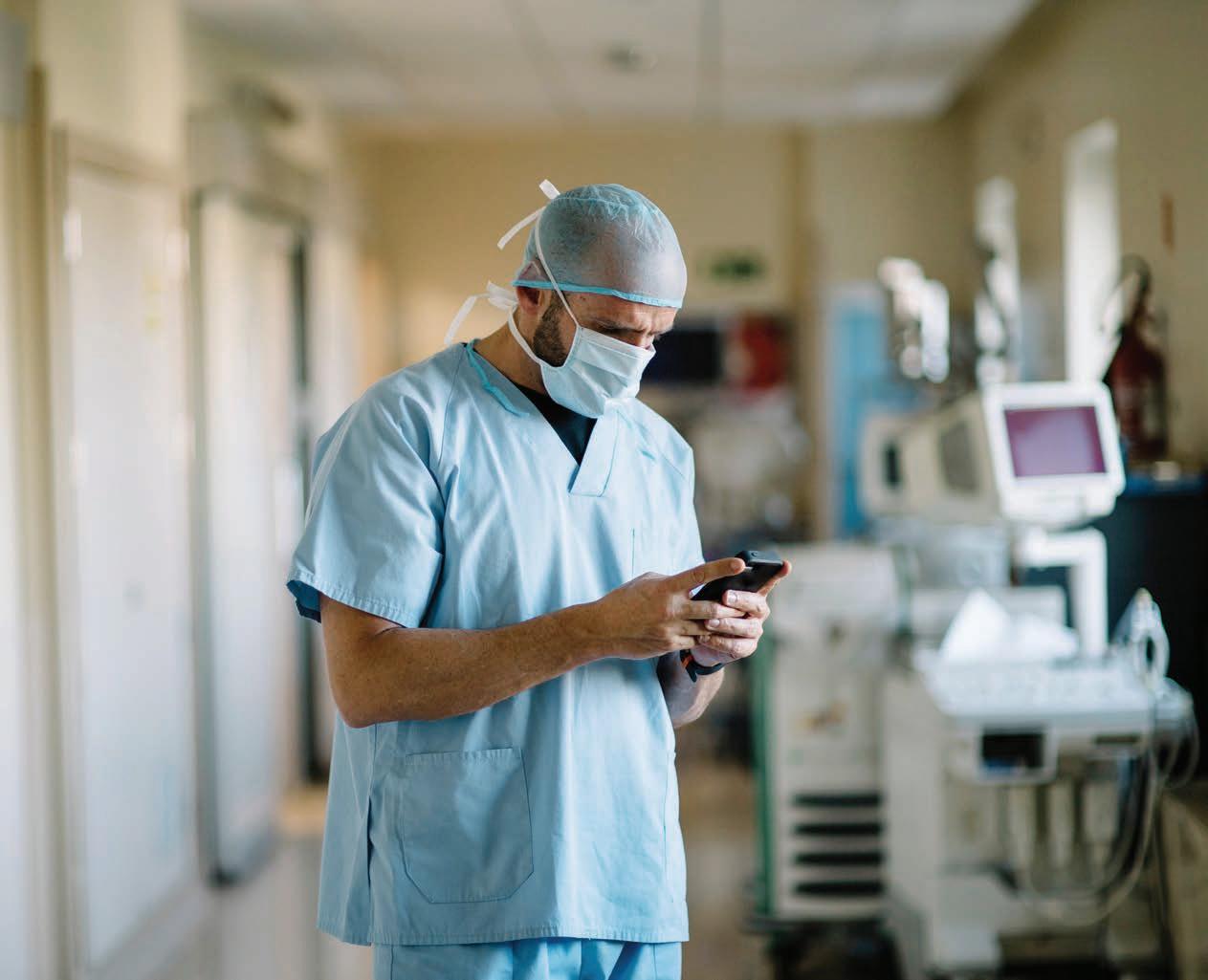
We provide a digital infrastructure that ensures clinical data travels with the patient
– making it available to all care settings and enabling clinicians to contribute to their care from anywhere. It also removes the geographic constraints of care, giving patients choice, clinicians flexibility and care providers workforce resilience.
Our solutions are currently in use in the UK National Health Service trusts (providers of state-funded acute, community and mental health services), regional NHS crossprovider care pathways and community diagnostic centres and private healthcare
facilities. In India they are found in remote care facilities and regional acute hospitals in Odisha State and clinical imaging centres in Indore.
Bleepa allows clinicians to review medical imaging and other clinical results and discuss cases collaboratively on the go. The Bleepa app on each clinician’s mobile device enables them to:
• Communicate with members of their clinical team who are based at other locations
• Work collaboratively with colleagues at times and at locations that work for them both
• Refer patients across their network with all relevant documentation
• Quickly take photographs for patient care (e.g. wounds, dermatological conditions and scar tissue)
• Easily capture the patient’s consent for their medical use. Securely upload photos and documents to the patient’s e-health record, to be viewed by a specialist at the most appropriate time

“The referral form in Bleepa allowed us to capture really important clinical information about the patient which importantly not only allowed us to plan treatment but also gave the clinicians more information, in one place, at one time, in order to aid them to triage patients’ requirements,” Janine Beattie, EPR Clinical Configuration Lead, told us.
Having centralised data around a patient in Bleepa, CareLocker provides a patientcentric way of storing that data in the cloud, ensuring its availability to any care setting that the patient attends. Patients can view their medical data on their own device, share it with others, and upload other documents allowing for a comprehensive care record.
In December 2019, when the respiratory team at the Royal Oldham Hospital in the UK wanted to improve the referral
process and response time for inpatient referrals, Feedback Medical deployed Bleepa to manage inpatient referrals to the respiratory team. By moving away from a process that was manual and paper based, the respiratory referral workflow was streamlined by ensuring a single point of access for inpatient specialist referrals. In addition, the use of Bleepa has standardised the referral process to include greater clinical detail, informing clinical decision making and collaboration.
The introduction of Bleepa and removal of manual administrative steps reduced the length of time for respiratory inpatient referrals to be actioned to just 0.4 days, an average saving of 1.7 days per referral. In addition, response time to referrals was reduced to less than one minute from an average 7.5 minutes, saving around 6.5 minutes per referral, or around 5.6 weeks of a full-time clinician’s time per year.
Similarly, over the past year Feedback Medical has been working with a UK regional cross-provider care system, connecting primary and secondary care via its community diagnostic centre (CDC), to deliver end-to-end symptom-based pathways. Our digital infrastructure enables patients to move seamlessly between primary and secondary care for definitive investigation and management based on their symptoms.
At Queen Victoria Hospital we have demonstrated that CDCs can be used
to successfully deliver cross-provider symptom-based diagnostic pathways that transform the patient journey within the NHS and we expect to be able to show a meaningful impact on patient waiting lists as a result. ICSs need to adopt a symptombased pathway approach to CDCs if they are going to deliver the expected impact on cancer and elective care waiting times. This pilot is the first example in the country of how this can be delivered, and our digital infrastructure is an essential component of delivering it.
Many healthcare systems globally face the challenge of a high proportion of people managing lifestyle-based non communicable diseases (NCDs). Bleepa can enable more proactive preventive care to reduce complications around chronic conditions like diabetes, chronic obstructive pulmonary disorder (COPD) and coronary heart disease by providing enhanced communication among primary care doctors to help keep patients out of a secondary care setting, as well as swi and flexible sharing of results and imaging for clinical review.
Feedback Medical provides both the digital and physical infrastructure for remote TB screening in Odisha state to enable frontline clinicians in remote areas to carry out X-ray studies and transmit them securely to specialists. Once the x-rays are transmitted by Bleepa to our CareLocker cloud store, the scans are then processed by our AI partner Qure.ai, which generates a patient report that is made available to the scanning clinician via Bleepa. The clinician is then able to quickly identify tuberculosis patients or those most at risk and act accordingly. Our initial pilot, which went live in March 2022, identified signs of TB in around 21 per cent of patients scanned in its first five months.
For patients, having their clinical data readily available is the best option, enabling better patient outcomes through streamlined care.
Advanced Clinical Solutions (ACS) are proud advocates of international health care initiatives





World Health Organisation (WHO) & Joint Commission International (JCI ) standards provide frameworks for a global benchmark of process and implementation. Helping global healthcare organisations measure against guidelines to assess and improve a global quality of care.
ACS adhere and support this by ensuring patient safety as the number one priority internationally.
Our key service is to support in maintaining and implementing evidenced based clinical practices.
Bespoke specialist services include:





Infection prevention and control
Quality and Governance initiatives


Specialist tailored education & training based on needs, through analysis and educational programmes
We are proud to say our carefully designed programs ensure that confident/competent practitioners are delivering safe and e ective care.
We have worked with Advanced Clinical Solutions on a recent project, engaging their services to provide input and support with development of our due diligence and quality assurance processes for the Imperial Private Healthcare international a liate network.



We found them to be professional, responsive and knowledgeable, engaging well with all Stakeholders involved.

Group Editor Sarah Cartledge explores The Lyniate Partner Program, speaking to regional partners Mozon, Virtus Informatics, Aamal Medical and YMH-IT Solutions about their place in the ecosystem
Lyniate collaborates with healthcare organisations around the globe delivering flexible interoperability solutions that connect people through increased access to data. The Lyniate Interoperability Suite includes Rhapsody integration tools for data exchange, master person index solutions, and semantic data quality services for mapping and normalising data, including clinical code sets. These solutions empower healthcare stakeholders to assemble and manage more complete and accurate patient information, resulting in reduced clinician burden, optimised patient
experiences and a solid data foundation for reporting and analytics.
Lyniate have also established a partner program that serves as a comprehensive black book of fellow industry leaders. Together, these pioneers deliver interoperability solutions across the healthcare landscape.
“Creating a truly interconnected healthcare ecosystem is our goal, and we knew we couldn’t do that entirely on our own”, says Erkan Akyuz, Lyniate CEO. “Around the world, we partner with local market leaders to bring all the best and brightest minds in healthcare technology together in
order to solve interoperability challenges for healthcare delivery organisations, national health systems, health insurance providers, healthcare technology solutions, diagnostic imaging, and reference labs”.
Digital transformation provider Mozon, systems integrator Virtus Informatics, medical equipment distributor and supplier Aamal Medical, and turnkey company YMH-IT Solutions are all part of Lyniate’s Partner Program to enhance their o ering to clients.
Founded with the mission of becoming the partner of choice for healthcare customers in driving digital transformation, Mozon is a leading partner delivering services needed to implement Lyniate Rhapsody.
“We believe in strategic and long-term partnerships that are based on win-win. Lyniate’s o erings and innovation are based on healthcare industry standards and a drive for digital transformation - its portfolio is rich.”
Through the Lyniate Partner Program, local healthcare organisations benefit from access to expertise across the world. Mozon provides the benchmark for digital transformation in the Kingdom of Saudi Arabia. Through innovative solution systems and a commitment to delivering excellence with state of the art solutions, Mozon is able to bring value to customers’ vision.
“In our work with Lyniate, we partner to personalise their global experience for local markets. Knowledge is the key word, we understand country initiatives and drivers, allowing us to engage in articulating business needs, and successfully deliver countrywide initiatives.”
Partnering with Lyniate presents mutual benefit. Lyniate provides partner organisations with a trusted product and an international reputation. “We find value in partnering with a global brand, a solution provider that is wellknown for its secure, reliable and flexible
interoperability solutions. Lyniate o erings are unique and go beyond simply delivering on one-time initiatives to supporting long-term growth”, say Mozon. “The Lyniate ecosystem is the bedrock of our digital health portfolio, it allows us to o er integrated solutions that can cover specific customer needs.”

Enabling workflow e iciency through digital transformation and making data seamlessly available to stakeholders through integration, Virtus Informatics provides solutions as a systems integration partner delivering Lyniate Rhapsody.
“Rhapsody’s multi-platform integration engine gave us access to the most modern and robust system, supporting multiple integration standards.
Partnering with Lyniate gives us the great flexibility of connecting many
applications in a fast, reliable, secure and cost-e ective manner.”
Through Virtus Informatics’ partnership with Lyniate, customers in Kuwait navigate the intensely complex landscape of healthcare information technology. Through an integrated

“Everyone is trying to ‘do’ interoperability. For that they need a certain toolbox, which we deliver through the Lyniate Interoperability Suite and an extensive network of trusted partners”
Erkan Akyuz CEO Lyniate
vision, the partnership is able to o er comprehensive, reliable and longlasting digital transformation.
As regional experts, Virtus Informatics can o er in-country knowledge and boots on the ground for prosperous stakeholder relationships, supporting cultural and organisational adoption for the Lyniate clientbase. Virtus o ers market experience to enable overseas operators to bridge complex, multichannel systems and deliver analytics across the expansive healthcare environment in the Middle East.
“Through our partnership with Lyniate we solve the communication barriers, irrespective of any HL7 version – V2 and V3 – and customers become ready for the future. Together, we support protocols such as SOAP, REST, SFTP, FTP and TCP, enabling connectivity to almost any type of system or device.”
“With many years of experience, and having introduced many cutting-edge
technologies, we have gained a reputation as the preferred digital transformation partner for hospitals across Kuwait. We provide the right combination of technology solutions, seasoned healthcare professionals, clinical experience and advanced analytics capabilities. We undertake the responsibility of foreseeing the apparent risks that healthcare organisations struggle with. We can develop flexible strategies to eliminate those risks.”
This impressive set of skills promoted through the Lyniate Partner Program further expands the reach of both Virtus Informatics and Lyniate. Lyniate clients benefit from Virtus Informatics’ position in Kuwait to aid transactions and negotiations. The complicated buying process, as an example, can be sped up by Virtus Informatics ability to see a gap in the market and anticipate the need for specialist solutions, enabling the initiation of purchases.
Leading strategic healthcare partner in Qatar, Aamal Medical provides end to end support to its clients throughout the supply chain and lifecycle from sourcing, delivery, implementation and maintenance. “The Aamal Medical and Lyniate partnershipis based on a shared vision, it is a natural partnership. We believe the integration of applications will help healthcare delivery be more innovative and a ordable.”
With ease and robustness, Rhapsody integration engine provides a stable foundation upon which Lyniate Partners can build the required architecture with confidence. Aamal Medical supports their clients by adding innovative layers on top of these foundations, including process experience, required applications and human capital.
“Being able to integrate without boundaries is the freedom we need as our customers have the freedom to choose from among the best, as well as maintaining a very competitive environment for solution providers. This helps reduce the costs which eventually pays back the investment into a robust integration engine.”
Through the Lyniate Partner Program, Aamal Medical is able to o er more than 20 years of market experience, allowing for the highest level of information to be accumulated and distilled.

“Most importantly, partnering with Lyniate brings us the cultural element of interoperability thinking. Sophistication of the ecosystem defines the innovation potential in any system. Lyniate gives both us and our customers the flexibility to target the best solution available - it reduces the vendor lock-outs, creating a healthy and functioning ecosystem.”
Focusing on turnkey Solutions, YMT-IT Solutions provides automation system integration solutions across Bahrain. With ten years’ experience, YMH-IT Solutions is able to deliver excellent local knowledge and cultural insights to their clients across the healthcare landscape.
As YMT-IT says, “We were looking for the best partners to help us integrate multiple solutions. Since medical equipment and data plays a very important role in this field, we had to ensure we chose the right partner, with the right solution and the right team to implement the requirements. With Rhapsody we were sure we could achieve big results and we have not been disappointed. In Bahrain, all the hospitals with automation run with Rhapsody as the middleware integration engine.”
Bahrain has developed inhouse HIS systems, with YMT-IT Solutions providing 33 types of equipment to the HIS, with the support of Lyniate Rhapsody. “Lyniate proves to be the bridge between these systems.”
For both Lyniate and YMT-IT Solutions, interoperability is in their company DNA. Through connecting multiple vendors via one platform, YMT-IT Solutions is able to create a complete interoperability ecosystem with Lyniate.
“Everyone is trying to ‘do’ interoperability”, Akyuz says. “For that they need a certain toolbox, which we deliver through the Lyniate Interoperability Suite and an extensive network of trusted partners”.
Patients can now receive the same standard of care in a nursing home or their own home, says Ian Chambers, CEO of Linea

Population ageing is increasing at a rapid pace. Between 2015 and 2050, the proportion of the world’s population over 60 years of age will double from 12 per cent to 22 per cent reaching 2.1bn, while those aged 80 plus will triple to 426m. Older age is characterised by the emergence of several complex health conditions, which are o en a consequence of multiple underlying factors including frailty, incontinence, falls, delirium and pressure ulcers.
There is strong evidence that extended periods of hospitalisation for frail older people leads to a decline in their physical & mental health, in addition to an increased prevalence of falls and the risks associated with hospital acquired infections.
The pressure of an ageing population on healthcare systems cannot be underestimated and will continue to exacerbate existing health and social care pressures, requiring a very di erent approach to healthcare provision - one which recognises the constraints on acute care beds, limited social / community care provision and the need for patient centric homecare.
What are virtual wards?
Fortunately, advancements in innovation and technology are enabling a new era of a ordable and dynamic patient-centric care, through which patients are encouraged to self-manage & monitor their personal
healthcare provision, especially in relation to the treatment of chronic health conditions. The term ‘Virtual Ward’ was coined to describe this approach to home-based healthcare provision. In essence, it describes a mix of remote services, technology and community care provision, which align to manage patients’ healthcare at home. The technology (including remote monitoring apps, technology platforms, wearables

“Advancements in innovation and technology are enabling a new era of affordable and dynamic patient-centric care”
Ian Chambers CEO Linea
and medical devices) enables healthcare professionals to examine and monitor patients remotely, providing interventions when necessary. However, this method does require a collaborative approach combining multidisciplinary teams facilitating a combination of remote monitoring, face-toface community care and the availability of specialist inputs, where required.
Many healthcare institutions are embracing virtual ward applications to improve care quality and increase the overall e iciency of their hospitals. The NHS in England currently has ambitious plans for 40 – 50 virtual ward beds per 100,000 population, as part of a coordinated approach to overcoming constraints in community bed capacity and to support the reduction in COVID-related waiting list pressures. There are numerous benefits from the adoption of virtual wards, including:
• The provision of care to patients unable to leave their homes for treatment, alleviating the associated burden placed on relatives caring for family members.
• Greater clinical e iciency and resource e iciency through minimising travel, improved productivity and enhanced patient outcomes, which helps in managing COVID-impacted waiting lists.
• Reduced costs through the provision of standardised and cost-e ective healthcare to numerous patients at the same time.
• An e ective and proactive discharge planning tool for hospitals to free up beds to reduce Delayed Transfers of Care (DTOCs) enabling continuation of elective care, while minimising unnecessary patient transfers and providing postsurgery recovery in a community setting.
• Enhanced community care provision, especially in rural and sparsely populated regions.
• Improved patient satisfaction through the provision of care in an environment
which is more comfortable and convenient for them.
• Streamlined and e ective patient communication with the ability for patients to connect directly with healthcare providers via a virtual application, without having to physically visit a clinic or hospital, thus increasing speed of communication and reducing errors.
There are a few potential drawbacks associated with virtual wards, although these can largely be managed and / or mitigated, namely:
•The use of telemedicine technology which can increase misdiagnosis prevalence.
•Potential privacy issues stemming from patient information being transmitted over unsecured networks.

• Patient resentment resulting from virtual monitoring and clinical oversight at the expense of regular face-to-face doctor appointments, particularly with the elderly who aren’t as technologically capable.
• The initial set-up costs associated with systems and technology, although in the long run these are o set by the reduced costs of care provision.
So, the virtues of integrated virtual wards are apparent, enabling patients to receive the same standard of care in a nursing home or their own home, which would otherwise require them to be admitted to a hospital bed. Patients can be admitted to a virtual ward to shorten length of stay, enable early transfer home before they are medically fit for discharges or alternatively, patients can be admitted directly from home as an alternative pathway, mitigating the need for hospital admission.
There are however some further key considerations for healthcare systems adopting virtual wards, particularly in MENA where considerable population growth is forecast and the requirement for additional

healthcare capacity is planned to increase exponentially:
The global healthcare workforce shortage is well documented. One way of minimising the impact is through the adoption of innovative care provision, which reduces the required acuity of care management and the number of clinicians required to provide it. Virtual wards require fewer doctors and nurses as much of the day-to-day care is provided through social care practitioners or via remote monitoring, thereby providing enhanced care quality, across a wider number of patients at a substantially reduced cost.
The pandemic resulted in many organisations increasing their clinical headcounts in order to provide COVID testing and vaccination provision. As the demand for these services has reduced,
healthcare organisations are facing a dilemma in retaining and redeploying these members of sta . The adoption of virtual wards provides a fantastic opportunity to retain experienced resources and utilise them to provide much needed community care provision across a diverse range of specialisms, enabling healthcare organisations to develop lucrative new markets.
Meeting increased demand through additional infrastructure capacity usually incurs a lead-time of 3 – 7 years and considerable expenditure (c.US$70m for a 100-bed facility). Planning today for healthcare requirements in 7 years’ time is fraught with challenges. Virtual wards provide an opportunity to ‘turn-on’ additional capacity immediately, whilst also providing a hedge against future increased infrastructure requirements, reducing associated costs or providing essential contingency. The move towards home based care provision also reduces the requirement for city centre land, which is due to be constrained over the next decade with prices increasing exponentially in key conurbations.
Virtual wards provide a great opportunity to adopt PPP relationships, principally across three aspects: specialist community care provision and expertise, technology provision and infrastructure capacity. Furthermore, the comparatively low capital outlay and ability to adopt a fragmented approach by specialism opens opportunity for SME involvement.
Linea are experts in healthcare improvement. Contact us to see how virtual wards could work for your organisation as part of an integrated community healthcare system. You may well be surprised by the speed of implementation, benefits realisation and return on investment.








Paul Johnson, Founder and CEO of Radar Healthcare, discusses how organisations can improve patient safety through technology

The World Health Organization (WHO) defines patient safety as the ‘reduction of risk of unnecessary harm associated with healthcare to an acceptable minimum’. Striving to embed patient safety within the culture of organisations has now become a significant concept for healthcare services across the globe in order to make a positive impact on the service and the care that they provide.
Patient safety failures are known to be extremely costly, dwarfing the costs of prevention. In the UK, of the entire healthcare budget for the NHS (National Health Service), clinical negligence claims have historically consumed about 2 per cent (BMJ). Therefore, if these were to be reduced, significant cost savings could be achieved.
Radar Healthcare works with several UK hospital trusts, aligning systems to create a single working interface that delivers both cost and time savings. User-friendly, compliant and transparent, it is a solution chosen most recently by Guy’s and St Thomas’ NHS Foundation Trust, starting in April this year, to integrate their risk management so ware systems across the whole Trust.
Health and care organisations across the world are facing the pressure of delivering high-quality, safe and e ective care to growing populations, with resources becoming increasingly stretched in an everchanging regulatory environment.
Radar Healthcare’s award-winning so ware takes a risk-based approach to managing quality and compliance. It supports the patient safety agenda and enhances health and care through comprehensive, innovative and personalised services that promote inclusivity and tolerance.
The Patient Safety Friendly Hospital Initiative (PSFHI) was created by the WHO to help and support healthcare organisations to launch a cohesive patient safety programme. It looks at five main domains:
• leadership and management
• patient and public involvement
• safe evidence-based clinical practices
• safe environment
• and lifelong learning
Health organisations such as the WHO, National Patient Safety Foundation (NPSF), the Joint Commission International (JCI), and the Institute for Health Care Improvement (IHI) are actively asking healthcare organisations to develop a culture of safety as an e ective strategy for improving patient safety.
The UAE’s Ministry of Health and Prevention (MOHAP) has commissioned Radar Healthcare to deliver its quality and compliance so ware to 17 hospitals and 72 primary care centres across the region. The system, delivered by local partner Memits Solutions, supports them in delivering clinical incident reporting and patient safety outcomes.
Such advanced regulatory compliance so ware helps health and social care organisations to have full visibility of all compliance processes to stay on top of patient safety, learn from previous incidents and events, handle complaints and compliments, monitor workforce compliance, improve services to reduce the risk of reoccurrence, and more.
A report by the OECD in 2017 entitled‘The Economics of Patient Safety’ strengthens a value-based approach to reducing patient harm at a national level. It highlighted that the 14th leading cause of the global disease burden (the impact of a health problem as measured by financial cost, mortality, morbidity, or other indicators) is estimated to be patient harm, comparable to diseases like tuberculosis. In some countries, patient harm is an even larger burden, comparable to diseases such as multiple sclerosis and some types of cancer.
It is thought that in OECD countries, 15 per cent of hospital expenditure and activity are caused by treating safety
failures. It is important to remember that there are knock-on e ects from adverse events, like the loss of trust in health systems. These issues are healthcareassociated infections (HAI), venous thromboembolism (VTE), pressure ulcers, medication error, and wrong or delayed diagnosis.
The reports identified that better policies and practices need to be in place to prevent harm and drive the quality improvement of care. Prevention programmes for issues such as HAI and VTE are much cheaper to run than paying for the financial burden they cause.
Fundamental system-level items should be invested in as a start, such as education, training, and safety standards,
forming the foundation of a national value-based approach where harm is reduced using limited resources.
An integrated patient safety strategy involves adopting a positive safety culture for all involved. Clinical governance frameworks are critical, as well as listening to the patients. A patient safety technology partner should provide the potential for continual improvements and sharing best practice.
Technology-powered healthcare can support the quest for excellence through incident management, risk

management and audit management so ware, as well as quality improvement plans and workforce compliance. In this way healthcare providers can improve patient safety, reduce risks, know they are compliant, increase productivity and delivery of care through quality assurance and operational e iciency.
There is a real need for joined-up, automated, integrated data to be the driving force for this continuous improvement, influencing whether or not an organisation becomes a well-oiled machine. Intelligent analytics plays a huge role by enabling actions to be triggered directly from data, in real time, by monitoring data patterns and using this data to create events, automate
notifications around concerns that need addressing, and improve operational intelligence across one or multiple organisations. It aligns with existing processes; it is interoperable and easy to use. Radar Healthcare is uniquely flexible to support quality, compliance and risk management in all areas of health and social care.
mena.radarhealthcare.com






















Healthcare World CEO and Director of Consultancy Emma Sheldon MBE examines the ways in which healthcare businesses can grow post pandemic

The pandemic has changed the way we live and work, from the newly remote nature of our interactions to the focus of our customers in dealing with new problems and systems.
Our businesses have been subjected to unprecedented levels of uncertainty over the last year or so, with a lack of clarity and understanding about everything
from the state of the global economy to questions as simple as whether we’ll even be able to go into our o ices.
That uncertainty leads to fear and doubt and there has rarely been such a shared volatile business environment in which to operate. Yet even a volatile business environment o ers the potential for significant opportunity when your o er matches the new needs.
We have all experienced the same global pandemic, but from di erent perspectives and through varying filters. Our usual routines have been disrupted to the extent that many of our usual ways of engaging with others have been removed and are only just starting to re-emerge.
What remains constant is that with change comes opportunity, with problems comes collaboration, and with a shared global focus comes innovation at an unprecedented pace and unusual scale.
Smart businesses have seen opportunities to match their innovations with need, to speed up adoption of their technologies, to improve patient care, and to share their successes as widely as they can to help others. To support our entrepreneurs and businesses they need the right advice, the right people, and the right money.
This requires a massive investment of time and e ort. Sometimes we’re running so hard at our goal that we fail to take the time to reflect on the changes that have impacted us, or to understand where our o erings can best fit. We aren’t able to shape and hone our strategy in the right way, or we don’t have the time to refine our messaging to make an impact with the right people.
This is where an experienced and independent pair of eyes is invaluable, equipped to support you in assessing where you are against where you want to be. They help you to plot your path to success, providing a diagnostic to help you identify and address any gaps in your business planning in a way that allows for the best chance of success.
In order to understand where you are and where you want to get to, there a number of critical areas to consider:
• Proposition development
o Cra ing and shaping your proposition for the best chance of success.
• Marketing
o Making an impact in the right places, generating leads and strengthening your message with strong targeting and significant amplification.
• International planning
o Ensure you have the right strategy for specific international markets, with good external intelligence, recommendations, insight and support.
• Strategy Development
o Tailor your strategy, including a review of your business, the current situation and your ambitions, the competitive landscape and the strategic imperatives for success.
• Preparing for investment
o Identify the key criteria to support the right investment, and ensure you tell your story succinctly and correctly.

• Recruiting for growth
o Design the resource strategy for your business, develop role descriptions, and support in finding the right people for your team. Remember that poor, costly recruitment decisions can be the most expensive mistakes you can make and ensure you engage the right people for the design of your organisational culture as you grow.
• Market and customer analysis
o Focus is critical when growing a business but narrowing down which markets or sectors can sometimes stop progress for business owners who are conflicted by numerous choices. Prioritise markets, sectors and customers, and design in metrics that will help you see how your choices are making a di erence and ensure you are able to quickly assess when to change direction.
• Business Development
o Once your strategy and messaging are where you want them to be, reaching
the right potential customers quickly and e iciently is vital. Use contacts, strong networks (like those of Healthcare World) to ensure you’re getting to the right customers.
Throughout the life cycle of any business, all these elements will be required, and never more so than now, as we live through a situation which is delivering a complex and fast changing landscape for our businesses, people and ideas.
I’ve spent my whole career working in and around the international healthcare space. With Healthcare UK I helped UK NHS Trusts to make their first steps to sell their services overseas. At Vernacare we exported a UK product to more than 50 countries around the world and I was lucky enough to be awarded an MBE for services to export.
In all cases, the kind of strategic insight and work I’ve outlined above was absolutely critical to the success of our endeavours. It provided the confidence and context to get beyond the fear, uncertainty and doubt that plagues any business in uncertain times and particularly in the current climate. Here at Healthcare World, the team and I are able to o er all the above, to give you the support you need and more through our experience, knowledge, contacts and expertise. And let’s not forget to mention the fantastic network that Healthcare World Magazine and the Healthcare World Festival brings to the table.
Emma Sheldon
“Even a volatile business environment offers the potential for significant opportunity when your offer matches the new needs”
Emma Sheldon CEO & Director of Consultancy Healthcare World

Advanced Clinical Solutions director Josie Winter explains to Healthcare World how international organisations can enhance patient safety
As healthcare becomes more global thanks to technological advances, the opportunity for knowledge sharing has increased. UK health standards have long been recognised for their excellence but thus far there are no global standards. For this reason, UK expertise is highly sought a er, as Josie Winter from Advanced Clinical Solutions has found.
The company helps healthcare organisations deliver high quality clinical care and service through a unique holistic partnership approach involving evaluation, audit, research, inspection, training and education.
“Standards are a very di icult issue to tackle in the hospital sector. In the UK we are very lucky – we have one set of rules, and one set of regulations to follow,”
says Josie, a former nurse. “Ensuring that you are up to standard can be a long and di icult process, but identifying the issues is a much simpler part of the process, thanks to institutions such as the JCI and the CQC (Care Quality Commission).”
So which standards?
In international markets, especially in emerging healthcare sectors, there can be multiple versions of standards and regulations, or none at all, or frequent changes – making it a minefield for providers to get their care settings and hospitals truly up to scratch. All too o en, governors can be unsure if they need to follow the JCI standards, or the UK or US standards, or their own local standards –and trying to do all of these is a sure recipe for failure without a plan.
Sometimes, it’s easier to adhere to local and national standards – lining these up with your patient needs and care, and ensuring that the clinical setting (whether it be a hospital, a clinic or a practice), truly meets the local and regional patient need. Sometimes it’s best to tackle the issue by striving for a JCI or a UK-standard hospital – avoiding the issues of regional and national di erences, and having a pretty concrete goal in mind. Neither of these decisions holds more merit than the other – it all depends on what your needs are.
Josie and her team of highly trained healthcare professionals are experts in patient safety, regulatory compliance and quality improvements. Having experience in both the NHS and private healthcare organisations including a large corporate med-tech organisation, they have developed and delivered hundreds of clinical audits and quality improvement plans that will fit any standard.
Currently the ACS team are working in Mozambique, Nigeria and Egypt on a World Bank project aimed at newly qualified professionals. Delivering the first module in the training programme
in person, Josie has already spent time in Mozambique. Each module takes 2-3 days and part of the programme is to implement a quality or safety programme in their hospital.


Among those who took part in the three day course were the Healthcare Quality Minister for Mozambique, the Head of the Mozambique Nursing Council (who has already looked at the UK Nursing and Midwifery Council approach), several hospital CEOs and complete beginners who have just graduated. “We had 25-30 hospital CEOs in the room and the peer-to-peer networking was a very high level. They are now connected in messaging groups and can drive these improvements together in the future,” she says.
The IFC or International Finance Corporation has provided the support for the projects, recognising the importance of quality and safety in healthcare. The Nigeria programme begins in the first quarter this year while the first module in the Egypt programme took place in November last year. “We met with nearly 40 dedicated healthcare quality professionals from across Egypt and had some fantastic engagement in the Healthcare Quality Leader programme. Their healthcare system is much more advanced with highly qualified quality managers, so their main focus in terms of case study was the NHS. We chose an advanced case study for them to gain an understanding of the UK situation,” she says.
The course covered the role of senior leaders in ensuring high standards of care and building capacity for health quality leaders. It included topics such as patient safety culture, incident management and reporting, and methodologies for incident investigation. The second module, entitled Building Capacity for Healthcare Leaders, includes navigating
quality and safety change with strategies for successful implementation, and setting clear goals and measurable KPIs for achieving outstanding safety and quality. It covers team dynamics, e ective communication, and the importance of data among many other subjects.

With a mixed use of teaching and case studies, the final QI project allows participants to implement their learnings in an improvised situation in their own healthcare facility. For Josie, this is her favourite part of the course. “I’m looking forward to the next modules this year, especially the third module as this is where it comes tangible,” she says. “It is so rewarding to see how the participants plan to put their knowledge into practice and make a di erence to patient safety and patient outcomes in their daily working lives.”

“It is so rewarding to see how the participants plan to put their knowledge into practice”
Josie Winter Clinical Operations Director Advanced Clinical Solutions
a healthier world.















Lyniate offers interoperability and enterprise health data management solutions that power meaningful interactions, connecting more than 1 million data endpoints across more than 1,700 healthcare organizations and over 3,000 applications.































We put the right data into the right hands at the right time, in the way people need.


The UK has healthcare data on 65m people. That’s a phenomenal amount of information and, as a nation, we are only just beginning to work out what we can achieve with it. But big data is one thing; ordinary data is another. We all have data; we are learning how valuable it is, and now we have to begin to share it.
In the UK, we’re historically inclined to resist information sharing. We must be one of the few European countries not to have identity cards. This doesn’t make sense when we share so much on social media. In fact, having identity cards would make more sense because then we could limit what information we share. And we’re also pathologically resistant to sharing our health data, despite the fact that it could deliver countless benefits if we did.
This isn’t just an individual bias; it’s also an institutional issue. Although most people think the NHS is one big national health service, it’s actually a group of di erent health trusts, ALBs, quangos and more that make up our medical provision. Each one has autonomy over its spending and decision on technology, with little national oversight.
So, as a GP in the north of England, we store our health records on two systems. There are a multitude of so ware add-ons and they come and go. Some are designed to optimise prescribing; some are designed to identify patients at risk; some add-ons are designed for accounting. Our principle system is SystmOne. There are a few others, but the problem is that they don’t communicate with each other.

This means that if a patient from one practice arrives at another practice, the doctors cannot see the patient history. That’s just madness. And the really big failure of communication is between di erent health care providers in terms of primary care, secondary care and the independent sector, none of whom have a common system.
In a hospital, there might be a laboratory that does cardiac scans with a scan machine that comes with its own so ware. The so ware will produce a report, but it has no mandatory requirement to directly communicate with the GP system or the hospital systems. As the patient’s GP, I cannot see it. But the patient assumes that I can, so I have to request it and this all takes time. And as we know, time is of the essence when it comes to medical symptoms.
Again, as a gynaecologist, when I sit as a specialist in a hospital, if I decide that a patient needs a tablet, I specify a tablet and dose, dra a letter which is sent, albeit electronically these days, to the GP. Someone reads the letter and manually enters the data onto the patient’s notes in the computer system. This is pure duplication - I could have entered that data on a single system and not needed to waste anybody else’s time. And I could have typed up my own records and there would be no letters
Dr Patrick Wynnto be sent, no opportunity for losing information or sending it to the wrong place. It would be so much more productive.
From birth, every person in the UK is allocated a GP. This dates from the founding of the NHS back in 1948. It’s a di erent world today and everyone should be able to hold their own patient record on their phone, allowing them to opt in and out of sharing, access appointments, results and see their own health data.
If someone comes into the surgery or hospital unconscious, as a doctor I should be able to access their medical records to see if they have any allergies or other issues. But I can’t. So Middle East countries should take a look at the issues the UK has, as they have huge potential to be overcome. There’s an inordinate amount of productivity gains that they would have over the current NHS operating systems.
I don’t advocate one system holding all records, just a common language that means all data can be accessed whatever system it is stored on. Rather like the internet allows us to book a hotel on the other side of the world, no matter what operating system we use. The patient gives permission for their data to be used and they can be treated quickly and e ectively with less risk. The clinicians or provider can treat the patient immediately, confident they have all the requisite knowledge to do so. It’s as simple as that – and there are companies out there that have the solutions to do this.
I understand that in the Gulf patients can selfsource specialists. But if they see a consultant for one issue, and a di erent one for another issue, is there a mechanism for the records to be combined? How much easier it would be if there was one central place to find such vital information.
I speak from the heart as an overworked and underresourced UK GP. Yet I do have experience and I hope my thoughts and insight are valuable. I hear that the Middle East health authorities are looking at primary care seriously as a gatekeeper for secondary care. Our role as GPs is to deliver preventative care, ensuring that appropriate cases are referred. With carefully curated systems, the Middle East could deliver the ideal primary care system that would be the envy of more established systems in other parts of the world.

The Midlands region is home to one of the most important life sciences ecosystems in the UK says Shaz Chaudhary, Director Midlands Region, Department for International Trade
The UK has a proud healthcare and life sciences heritage dating back to the late eighteenth century when British doctor Edward Jenner developed the first vaccine against the contagious disease, smallpox. We continue to innovate and deliver benefits to the world as demonstrated by the UK’s leading role in developing and administering the COVID-19 vaccine.
Businesses from across the healthcare and life sciences sector in the UK are delivering world-leading products and services globally. The Midlands region is home to one of the most important life sciences ecosystems in the UK with more than 1,200 life science companies, 33,000 highly skilled jobs and the second largest concentration of MedTech companies in the UK based in the region.
With a diverse population of more than 10m citizens, the Midlands region in the UK makes the ideal test bed for global health and multimorbidity interventions. It is also a major centre for clinical research which stems from the high number of world class universities, research centres and incubators in the area.
At Arab Health, we’re delighted to introduce you to innovative companies from the Midlands region in the UK, who
are well placed to work to provide the right sustainable and innovative solutions for your needs.
“I’m excited the UK will be able to demonstrate the best it has to o er within the Healthcare and Life Sciences industry at Arab Health 2023,” says Shaz Chaudhary, Director Midlands Region, Department for International Trade. “The UK government is supporting businesses from across the UK to exhibit at the show and 32 companies from the Midlands region will be showcasing.
“I encourage everyone to visit us in Hall 2, Stand H11 as we look to build partnerships between the UK and international businesses and stakeholders.”
The following Midlands-based companies will be part of the UK government-led trade mission to Arab Health and will be exhibiting at the show:
Adapttech is a biomedical innovation company that brings new smart technologies to the O&P market with the goal of empowering clinicians with better socket fitting and monitoring methods to improve the quality of life for people with lower-limb loss.
ADHD 360 is the largest provider in the UK market delivering assessments and
treatment for neurodiverse conditions including ADHD and ASD. The distinctive ADHD 360 care pathway is NICE compliant, and UK Care Quality Commission audited. The pathway is a combination of e icient process, telemedicine, video consultation, and a flexible workforce, all built upon the foundation of their bespoke enterprise IT system.
AG Instrument is a world leader in the design and manufacture of piped medical gas analysers. The company is known for its award-winning MGPS1000 and MGV100 All-in-One gas analysers that can measure all the gases required by the HTM02-01, ISO7396 and NFPA99 standards simultaneously.
Allgood manufacture and supply architectural ironmongery of the finest quality in design and cra smanship with the confidence of a lifetime’s performance.
Ariane Medical Systems Ltd o ers an X-ray Brachytherapy System for the management of lower rectal tumours, known as the Papillon Technique, a turnkey solution providing everything needed for successful rectal, superficial and intraoperative X-ray Brachytherapy treatments through its treatment modalities.
BioCare help people around the world be the healthiest version of themselves, by creating advanced, e ective food supplements without the use of unnecessary additives, made in the UK.
Biospear have developed a range of cleaning products that provide residual protection against bacteria, mould, so shell viruses and fungus.
Defib Store is the UK’s leading Automated External Defibrillator (AED) cabinet manufacturer with 30 years’ experience designing and manufacturing bespoke and specialist enclosures for hazardous environments.
Emedica is a leading UK provider of private medical education o ering courses and resources to help doctors pass professional exams and progress their careers.
Garland Surgical is a concept for a total hip prosthesis that could be “A Hip for Life” which would support healthcare systems to reach sustainability goals, and most importantly improve the quality of life of patients.
Gordon Ellis & Co design, manufacture and distribute Aids to Daily Living, assisting elderly and disabled people maintain their independence, dignity and safety in daily living tasks. Their products make a di erence to quality of life.
Hydro Physio is the market-leading manufacturer of aquatic therapy treadmills, designed to meet the needs of a wide range of mobility requirements. Hydro Physio has sold more than 1,000 HYDRO PHYSIO systems worldwide, improving health and wellbeing for both humans and animals.
IVC Brunel Healthcare is the UK’s number one vitamin manufacturer, specialising in the production of vitamin, mineral and nutritional supplements. IVC Brunel have a wealth of knowledge covering both private label and contract manufacture, and their customers include some of the globe’s bestknown retailers and many of the world’s best-known pharmaceutical brands.
Modality Partnership is an award-winning GP super-partnership that operates primary health care and community services serving more than 6m citizens across the UK. Modality can supply both provision and advisory services including but not limited to primary care, 20 speciality services, integrated care delivery, lifestyles / population health, leadership and workforce development, large scale organisation transformation, digital innovations, and service redesign and implementation.
NeoKare Nutrition Ltd manufactures quality human milk products o ering safe and screened breast milk products
when a mother’s own milk is not available. NeoKare has established the first and only pharmaceutical grade manufacturing facility for the testing and processing of human milk in Europe.
Paraid is a division of Evac+Chair International, with 40 years of UK design and manufacturing experience. Paraid is the leader in innovative medical transfer equipment, designed to assist in saving lives in medical emergencies.

Remcare is an end-to-end digital solution for the entire clinical pathway. Remcare has an algorithmic, speciality-specific risk stratification using up-to-date patientreported health status and disease-specific information to identify the risk of the patient before they come to the hospital, so that the right patient gets to the hospital at the right time.
RBT is a developer, formulator and manufacturer of advanced hygiene and infection control products. We have developed our products to be kinder to the environment and users than more traditional harsh disinfectants. In addition to supplying the global medical and healthcare sectors with our CE marked medical device disinfectants.
Serchem Ltd provides a premium quality solution for healthcare and facilities management. The products are scientifically designed and manufactured at UK premises for distribution both nationally and internationally.
Spirit Digital is a forward-looking digital healthcare organisation. Spirit Digital has saved the NHS millions of pounds and improved the lives of thousands of patients across the UK. Their proven remote patient monitoring so ware, Clinitouch, makes hospital at home a reality.
Spirit Healthcare is one of the UK’s fastest growing healthcare companies. For almost 14 years, Spirit have worked with the NHS by helping to improve patient care and e iciencies through launching and distributing medical devices and services into the UK health economy.
Starfish Labs develop mobile and web apps for healthcare providers, supporting learning disabilities, healthy ageing, remote support and education. Associate
company Hunter Bevan o ers bespoke marketing support services for healthcare organisations.
Sterimedix was founded in 1989 by a group of private individuals who believe in the concept of single use surgical products for eye surgery. Sterimedix has developed on its core competence and now manufactures millions of devices in modern cleanrooms for eye surgery and aesthetic procedures each year.
Sterling Pharmaceuticals Ltd is an innovative British pharmaceutical Contract Research, Development and Manufacturing Organisation (CRDMO) which has been operating since 2008, specialising in the research, development and commercial manufacturing of a wide range of pharmaceutical products.
Surgins is an award-winning UK manufacturer of titanium surgical instruments of all surgical disciplines. Surgins takes a ‘surgeon-centric approach’, building customised, signature, innovative and highest-functional quality range of surgical instruments to become the ‘instruments of choice’ for discerning surgeons and clinical end-users worldwide.
The Oxygenstore (Bar O2 Ltd) are a UKbased supplier of worldwide oxygen-related products specialising in cylinder storage products, including an extensive number and variety of oxygen cylinder trolleys, wall brackets and oxygen cylinder storage solutions.
TherapyAudit Ltd provide innovative solutions to the challenge of safely and e iciently monitoring patients who are prescribed potentially toxic drugs and/or living with cancer.
Uvamed Ltd is an R&D manufacturer of medical devices and the creator and owner of Rainbow Trays including tamperevident Rainbow Trays and Rainbow Labels. Uvamed is an innovator of new products and processes to address unmet needs within anaesthesia, field surgery and medical plastics recycling.
Managing Director Dr Mohammed Aldar outlines the role of Accumed in cementing its role in the future of healthcare
As healthcare grows as a global sector, revitalising itself through digital solutions and AI uptake, it’s vital that its revenues keep pace. Regulations and reimbursement models have been changing, so providers need to upgrade their own systems to ensure that they correctly bill patients and insurers for the care rendered.

For Dr Mohammed Aldar, the main goal of a company such as Accumed is to make sure that every claim is payable. To achieve this, accurate medical coding and invoicing is paramount, and Accumed handles everything related to the operations of health insurance and bill issuing, medical coding and ensuring that the medical documentation
is justifying the medical necessity. This includes scheduling, patient registration & eligibility check, charge capture, preauthorisation, medical coding, collection and reconciliation in addition to the denial management.
There are many stakeholders involved in the process, from patients to payers, medical to administration stakeholders. “The main pillars are people, process and technology,” Mohammed says. “We need medical data, operational data and financial data to make it a success. It’s a very complex, comprehensive handling process, but if done correctly can reduce costs across whole healthcare systems.”
For the individual client, Accumed is not just any revenue cycle management company. By outsourcing billing functions, operational burdens related to human
resources (i.e. sta salaries and benefits), o ice space, so ware licenses and upgrades – plus the headache of regulatory and payer compliance – are removed from the equation,” he says. “In this way clients can focus on o ering qualitative patient care and accelerating cash flow, rather than engaging in daily billing and collection concerns.”
Having a cohesive structure in place improves time management, communication, regulatory compliance, and the ability to spot possible coding and billing oversight, allowing providers to maximise revenue cycle opportunities at point of care. “Our target is to increase client revenue as well as increase collection. So instead of having like high rejection rate from the insurance companies, we will try to optimise the RCM processes in order to get the maximum possible.”
In the Middle East, revenue cycle management or RCM remains at a nascent stage. However, its prospects are bright as the region’s healthcare market holds untapped potential. According to industry estimates, healthcare spending in the wider Middle East and North Africa (MENA) is expected to reach USD144 billion by 2020.
The Middle East healthcare market is also evolving with new regulations, laws, systems, processes and financial dynamics, making RCM a cornerstone in the healthcare industry. Accumed was one of the first companies to operate in the Middle East and now works in eight di erent countries including the UAE and Saudi Arabia. They also have alignments in in Australia as well as the United States. “We are actually perceived as the first, if not the best, revenue site in the Middle East,” Mohammed says.
The company began working in Saudi Arabia in 2020, one of the first companies licensed there. They have strategic partnerships with Johns Hopkins Aramco, an elite high end provider hospital, and King Faisal Specialist Hospital and Research Centre, along with several partnerships with the Ministry of Health.

With a population of around 36.8m, the Kingdom is a huge market. According to Mohammed, 11.8m people are insured and there are more than 5500 approved providers. There are 24 approved insurance companies and also third party administrators. The size of the insurance market is $16bn with a growth of 26 per cent between 2021 and 2022.
The health estimates formation deliverables for Vision 2030 align to a certain extent with Accumed’s pillars. The first is providing people-centred integrated healthcare; the second is achieving e ective and sustainable financial resources management and the third is investing
in private sector integration to create strategic partnership. Last but not least is employing digital and virtual health tools, so investment is important to allow optimum revenue collection to allow for a sustainable healthcare infrastructure system.

E ective revenue collection management has greater relevance than a purely financial one. Providing the best service increases sta satisfaction, which then provides better service. This can be achieved at an administrative level by e ective RCM systems, providing clarity to sta , reducing turnaround times and admin burdens.
Value-based health care consists of delivering the best outcomes of the health care solution or system at an e ective cost. It reduces readmissions, delivering better patient outcomes and satisfied clients. But, according to Mohammed, you cannot build up your health care system without having the right tools for analytics. “If you don’t have the big data, you cannot set your strategy ahead,” he says. Clinical, financial and operational data are all required in order to come up with decisions. Data is also necessary to work out the standardisation of processes. Without it, price comparisons and benchmarking are impossible and value is di icult to establish.
The Saudi government has just approved convenience share models, which are basically RCM companies or any private sector companies in partnership with the government, based on a revenue share. For Mohammed, this is the future. “We are expediting digitalisation, optimising revenue and, like upselling and crossselling, opening up capacity through hybrid and blended solutions. Such activities build up the capacity within the governmental sector so that they don’t only outsource or request to outsource the RCN to us, but also enable us to take over the current manpower where we transmit the knowledge, so in 3 to 5 years’ time, they will be able to continue the journey on their own.”
“If you don’t have the big data, you cannot set your strategy ahead”
Dr Mohammed Aldar Managing Director Accumed
Clinical trials are an effective method to know if a new treatment is safe and functional in people, says Mike Failly, Founder and Managing Director of Zanteris

One of the benefits of the COVID-19 pandemic was the rapid appearance of drugs to overcome the disease. Scientists, researchers, ministers, and others came together to utilize the expertise already in existence and repurpose some of the research that was being undertaken into similar viruses. It
emphasized the importance of clinical trials and showed that new medicines could be accelerated into production when everyone was of the same mind.
“Clinical trials are an e ective method to know if a new treatment is safe and functional in people,” says Mike Failly, founder, and CEO of Zanteris. “Emerging healthcare systems can utilise the results
of clinical trials to treat patients and avoid harmful side e ects, especially whenever there is an unmet need. Clinical trials can also help healthcare systems to maintain intellectual curiosity and search for optimal health services for patients.”
A former scientist with a PhD in Neurobiology, Mike spent the early part of his career working on the proteins and genes of specific rare diseases. “I enjoyed cell signaling, making a sequence and sequencing analyses, but I felt I needed to contribute even more from a medical standpoint and health” he says. This led him to a Geneva University hospital where he worked in Oncology mainly in breast and ovarian cancer. He went on to biotech and clinical research organisation (CRO) where he worked in immunology,
cardiology, oncology as well as immunooncology.
From there he set up Zanteris to provide client-specific Clinical Operations services to provide the best customer experience and improve study deliverables, as well as team performance. Zanteris is a functional CRO in Clinical Operations, focusing on both the pharmaceutical and biotech industries. O ering Project Management resources, Clinical Operations, and Human E iciency Consulting, Zanteris plays an integral role in connecting the clinical team with any other internal part of the business.
“Our services can help health systems around the world by providing expert guidance and advice, with the skills


and knowledge necessary to improve CRO and/or vendor relationships with an overall focus in performance on their clinical development activities,” he says. This encompasses providing well-qualified human expert resources to support teams and overcome challenges that may delay clinical trials, o ering a cost-e ective approach to achieving the key performance indicators (KPIs) aligned with health organisation targets and helping pharmaceutical and biotech industries maximise their potential.
For pharmaceutical and biotech industries, Zanteris specialises in oncology trials. However, their background and expertise allows them to provide support or oversee complex clinical trials and global clinical trials. Examples include EMEA, NA, APAC, and LATAM. Zanteris o ers from Phase I to Phase IIIb studies expertise.
“We provide operational support getting new and innovative medicines to patients,” says Mike. “The overall population can benefit from more options for healthcare through clinical trials, including access to potentially life-saving medication and innovative treatment such as CAR-T trials. Healthy volunteers among the overall population can also claim to take part in these trials to contribute to improving science.”
Several considerations go into managing clinical trials, including patient diversity and patient disease prevalence but also standard of care treatment, healthcare expenditure, and technology infrastructure. Other essential data involves project planning details, budget, and regulatory requirements.
Depending on the status of the trial, it can require many resources. Zanteris takes on trials from the initial stages right through to rescue situations. Where some trials may take place in one hospital in a single country, others can consist of 200 sites across 30 countries, requiring as many as 150 people to run it.
“Running a trial requires a lot of experience,” Mike says. “You need top leadership skills to drive your customer and also your team. You need a project manager as a leader and CEO of your project, but also one who shines the light on the team. Your team is the most important element, so you need to protect them to find the perfect balance between making your customer happy and driving the clinical trial. Our core value is integrity, and we are here to provide expertise to our partners.”
Zanteris brings a smart approach to new markets by e ectively providing Clinical Operations consulting and clinical project research management. The advisory services of Zanteris are specifically designed to support small and medium biopharma market with their outsourcing and clinical operations challenges.
“We decided a few months ago to take a good look at the Middle East where there is a more stable population mix,” he says. “There are also unmet needs and medication because pharmaceutical companies are running clinical trials which are less innovative than the ones we run. I have been working in a very complex rare disease trial and have had exposure to several of these issues, challenges and di erent opportunities that drive a successful clinical trial, or at least how to mitigate or prevent any issues as part of a risk management strategy.”
For Mike, his job is his passion. “I love to contribute and I’m proud of doing so,” he reveals. “There is nothing better than to contribute to the care of a child. When you are part of history, you can be proud of years of dedication.” Contact
“The overall population can benefit from more options for healthcare through clinical trials, including access to potentially lifesaving medication”
Mike Failly Founder & Managing Director Zanteris
Leveraging the Power of CDVC (Concurrent
DigitalizedValue Chain) is key, say
 Dr Hesham Dinana VP EFESO MEA and Dr Mohamed Fayek Director – Head of Healthcare and Life Science EFESO MEA
Dr Hesham Dinana VP EFESO MEA and Dr Mohamed Fayek Director – Head of Healthcare and Life Science EFESO MEA
The world is in a continuous state of flux and the healthcare industry is no exception. With the unprecedented changes brought about by the COVID-19 pandemic, the healthcare sector has had to change the way it operates and deliver medical care. This has created a challenging environment for healthcare providers, as they must balance their need to be resilient and responsive to changes while also providing value to their customers. In such a VUCA (Volatility, Uncertainty, Complexity, Ambiguity) world, leveraging a digital value chain can help healthcare providers meet the demands of their customers while also delivering quality care.
The healthcare industry is undergoing a rapid transformation as digital technologies become more commonplace. With the help of a digital value chain, healthcare providers can deliver more e icient and e ective care. A digital value chain is to build a real time network between all ecosystem players with interconnected digital platforms and tools. This helps healthcare providers and other stakeholders coordinate, manage, and deliver care.
Concurrent Digitalized Value Chain (CDVC) by EFESO is a system that allows for improved collaboration between providers, patients, and other stakeholders, allowing for more streamlined care delivery. In addition, it improves the accuracy and security of patient data, helping to reduce medical errors and reducing the risk of data breaches. It develops the capability of healthcare
providers to better track patient progress and outcomes, allowing them to make more informed decisions.
The healthcare industry is facing numerous challenges in today’s VUCA world. First, the pandemic has created an unprecedented demand for healthcare services, forcing healthcare providers to take on more patients with limited resources. This has caused a strain on existing systems, leading to long wait times, overworked sta , and a lack of resources.
Second, the rapid changes in the healthcare landscape have caused the industry to become increasingly complex. With the emergence of new technologies, the need for highly specialised care has become more acute, increasing the complexity of care delivery. This has put a strain on healthcare providers, as they must be able to quickly respond to changes in order to remain competitive.
Third, the high cost of healthcare is placing a strain on budgets, making it di icult for healthcare providers to maintain their operations. Rising costs have forced healthcare providers to look for ways to reduce costs while still delivering quality care. This has led to a need for innovative solutions that can help healthcare providers optimise costs while still providing highquality care.
Finally, the healthcare industry is facing increasing pressure from regulators and the public to become more transparent and accountable. This has led to increased scrutiny of healthcare providers and the need for better data-driven solutions to improve patient outcomes.
The emergence of digital customers is creating new opportunities for healthcare providers to meet the demands of their

customers. Digital customers are more informed and empowered than ever before, and they are increasingly turning to technology to find and access healthcare services. As such, healthcare providers must leverage digital solutions to meet the needs of their digital customers.
This can be done in a variety of ways. For example, healthcare providers can use digital channels such as websites and mobile applications to provide information about their services and allow customers to book appointments. Additionally, they can use digital solutions to provide personalised care plans and engage customers through telemedicine. By doing so, healthcare providers can meet the demands of their digital customers while also providing quality care.
The digital transformation of the healthcare industry has revolutionised the way healthcare is delivered. By utilising a digital value chain, healthcare providers can e ectively manage their entire operation from one central location. This saves time, money and resources, as well as simplifies the delivery of quality care. From streamlining the booking process to providing faster patient access to medical information, digital value chains are making
“Healthcare providers must leverage digital solutions to meet the needs of their digital customers”
Dr Hesham Dinana Vice President EFESO MEA
healthcare delivery more e icient and reliable. Moreover, these value chains can also help to improve the accuracy of patient data and reduce the risk of medical errors. With the increasing demand for fast and easy access to medical information, digital value chains are becoming an invaluable tool in the healthcare industry.

The healthcare industry is highly complex and requires a variety of activities to be performed in order to deliver quality care. This is where the value chain comes in. EFESO state of art model Concurrent Digitalized value chain is a set of activities that healthcare providers must undertake to produce a product or service. It involves everything from sourcing and production to distribution and marketing.
In the healthcare industry, the value chain involves activities such as medical research, clinical trials, drug development, manufacturing, distribution, and marketing. It also involves activities such as billing, coding, and patient engagement. By understanding the value chain, healthcare providers can identify areas for improvement and optimise their processes in order to deliver better care.
The digital value chain is revolutionising the healthcare industry by enabling e icient and e ective delivery of services. By leveraging the latest digital

technologies such as cloud computing, big data, analytics, and AI, healthcare organisations can now automate processes and streamline communication between providers and patients. With digital value chain, healthcare data is securely stored, accessed, and shared in real-time, which allows for greater transparency and accuracy of patient care. It also enables healthcare organisations to provide more personalised patient care, as well as access a wealth of medical data. Furthermore, a digital value chain helps to reduce costs, reduce errors, and improve patient outcomes.

Digital value chains allow healthcare providers to quickly and accurately identify patient needs and then provide the right treatment in a timely manner. With digital value chains, healthcare providers can also track patient outcomes and make sure they are getting the best care possible. In addition, digital value chains can help healthcare providers reduce costs and improve the quality of care. The challenge for healthcare industry is the pace of change, pricing pressures, e ects of patents,
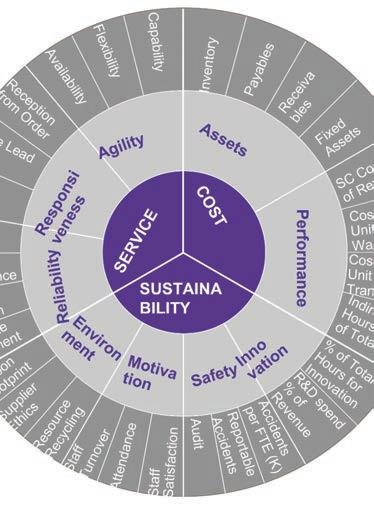
product development to commercialisation, competition, sourcing risks, changing patient needs, and more. The focus of CDVC is to help businesses gain alignment between external pressures and internal actions and to ‘think’ and ‘behave’ end-to-end across the entire value chain as a means of creating competitive advantage.
In fact, there is no ‘one size fits all’ approach to the healthcare sector and/ or sub-sectors and our approach is to help clients tackle current and future challenges by co-creating a tailored approach. In addition, the CDVC model provides a framework for identifying gaps and establishing ‘concurrent progression’ in the areas that have the greatest impact on the ‘value’ generated or ‘risk’ mitigation. Healthcare organisations can do this through the development of people’s understanding and leadership capabilities, support and enablement of the right digital environment and the management of process change across the business (Process-Human-Digital).
The EFESO Concurrent Digitalized Value Chain (CDVC) progression model works

holistically across all the E2E Value Chain domains to ensure they are improved upon in a on current manner against business and market aligned goals. By synchronising capabilities and performance improvement across these domains, key interdependencies are identified and work in parallel. This allows quicker progression and sustained gains. The CDVC Model first translates business goals by domain performance requirements, then assesses current state capabilities versus those requirements. An improvement plan is then plotted to span the CDVC Domains.
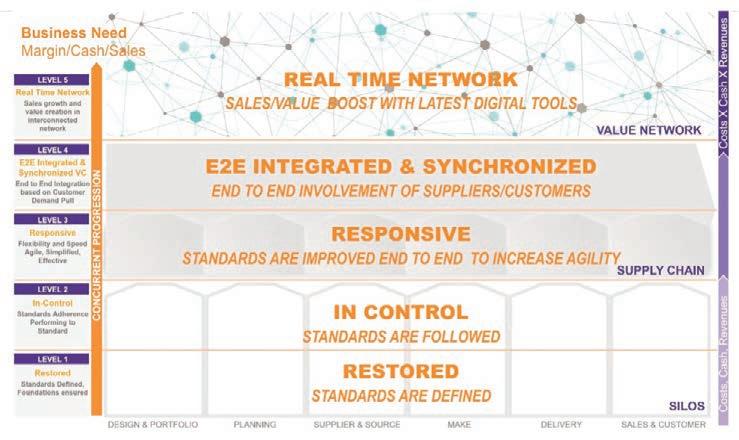
A digital value chain involves the use of digital tools to facilitate collaboration and partnerships between healthcare providers and their customers. Partnership with platforms can enhance sta productivity by lowering customer acquisition costs. For example, healthcare providers can use digital solutions such as cloud computing and blockchain to securely share data with their partners.

Building a Real Time Network digital value chain can help healthcare providers collaborate with other organisations, such as research institutes and pharmaceutical companies. This can help healthcare providers access the latest research and treatments in order to provide better care for their patients. By leveraging digital value chains, healthcare providers can improve their ability to collaborate and partner with
Concurrent Digitalised Value Chain - The CDVC Model

other organisations, leading to better care for their patients.
The EFESO Value Chain Service Lines are built into a CDVC Progression Plan. While some of these Service Lines are domain specific, others span multiple domains. The key to our approach is that the Progression Plan integrates this work in the most e ective manner possible by delivering the client tailored capabilities and result improvements. This focus on operationalising the plan is another strength of EFESO as we ensure capabilities are built across the Human Dynamics, Work Process and Digital Dynamics in order to achieve sustainable results. Thanks to our Data Engineers, Data Scientists and Human Dynamic experts, we are able to support our clients on all three legs of Process, People and Advanced Analytics. We typically see that our clients are well developed in Make and Distribution Operational Excellence but have large opportunities on the external interface with Suppliers and Customers. However, the largest gap is with Sales (Commercial/ Marketing) and this is where the value proposition of your value chain needs to be connected to drive growth and sales.
In today’s VUCA world, healthcare providers must be resilient and responsive to changes while also providing value to their customers. Leveraging a digital value chain can help healthcare providers meet the demands of their customers while also delivering quality care. By implementing a digital value chain, healthcare providers can optimise their processes, improve care delivery, and enhance collaboration and partnerships. In doing so, healthcare providers can create a resilient and responsive healthcare system that can meet the needs of their customers.
“Value chains can also help to improve the accuracy of patient data and reduce the risk of medical errors”
Dr Mohamed Fayek Director - Head of Healthcare and Life Science EFESO MEAFigure 2: CDVC Model
• Training programmes designed to meet your specific educational requirements
• Tailored consulting services to improve your operations and patient care
• Rapid access to second opinions from over 500 leading doctors

• Extended complex care pathway, with managed overseas referral service to our London hospitals and discharge to your hospital for onward care.
• The opportunity to promote your affiliation to Imperial Private Healthcare.
Join
Imperial College Healthcare Private Care International Affiliate Network is a global network of aspirational healthcare organisations, working collaboratively with Imperial Private Healthcare to improve patient care.

Expert multidisciplinary teams work with member hospitals to complement and develop patient care, by advancing clinical services and providing a managed complex overseas referral service to Imperial Private Healthcare.



Imperial Private Healthcare forms part of Imperial College Healthcare NHS Trust, one of the largest teaching hospital groups in the UK.
imperialprivatehealthcare.co.uk/affiliate-network/
Imperial Private Healthcare is proudly part of:
January is always the busiest time of the year for the Healthcare World team as Arab Health takes place.
I’m struck by how di erent the situation is from last year when we were returning to Dubai for the first time post COVID. So how much has really changed in our sector? How many lessons did we learn from two years of coronavirus and will we be better equipped for the next global healthcare crisis?
Of course, the first thing to point out is that COVID is by no means over. Recent events in China prove that we could expect a flare up at any moment. Equally we are still coming to terms with the long term e ects of the pandemic and trying to work out what exactly Long Covid is and how to deal with it.
The world, by and large, is certainly acting as if COVID is no longer with us and this is my point. There are clearly some huge positive developments that came out of the COVID crisis. We now know that we can develop an e ective vaccine in an amazingly short space of time.
The rise of data and digitally-led healthcare provision also received a huge shot in the arm as a result of COVID-19. We are now in an age where every element of healthcare delivery is digitally driven and the benefits of population health and data modelling for healthcare are known, desired and acted upon in every health system, driving more e icient delivery of care.
But this revolution in healthcare was going to happen anyway. The arrival of a global pandemic has not been the cause of a digital healthcare revolution, but it has hastened its arrival. That’s just as well, because one of the huge negatives of COVID has been its e ect on the global healthcare workforce.
An already impending crisis has been worsened massively by the pandemic causing a stressed, demotivated, underpaid and under-appreciated healthcare workforce. People have le the healthcare profession in droves and we cannot educate replacements quickly enough.
The wealthy economies of the globe must learn the lesson quickly that the time is rapidly approaching where health systems cannot rely on cheaper labour from less wealthy economies. Growing your own workforce will have to become a cornerstone of the development of any health economy. And that workforce will inevitably become far more expensive.
It’s notable to see that Dubai, traditionally a health sector with an almost 100 per cent rate of immigrant healthcare workers, is developing a strategy to create an indigenous workforce with the establishment of the Dubai Health Science Corporation. Their remit is not just as the Emirate’s dominant public healthcare provider, but also Sheik Rashid University and the promotion and training
 Steve Gardner Managing Director
Steve Gardner Managing Director

of healthcare workers for Dubai, in Dubai. Other systems should take note.
Crisis mitigation could come in many forms. Digital healthcare and the use of data will help us to focus stretched resources in their greatest areas of need. The rise of virtual reality and the Metaverse may provide opportunities for surgeons in one country to use technology to perform operations in another using a combination of robotics and VR.
And what about public health messaging? If our health systems need to learn one lesson for the next pandemic, it’s that we need clear, simple and decisive guidelines on what is and isn’t acceptable in the face of a threat from a deadly disease. This doesn’t mean choices about whether or not to be vaccinated. It means making sure that choice is properly informed and that the way in which a society behaves during the darkest days of a pandemic is better policed, clearer and easily understood.
The worst days of COVID-19 are behind us but, in our rush to return to normality, the concern is that those of us involved in policy making, decision making, funding and delivering healthcare have all too quickly forgotten the lessons of the pandemic.
There will be another pandemic down the track so will we deal with this one any better? And will we learn our lessons next time?