
15 minute read
What is Huntington’s Disease?
by Melissa Bixby, MS, CCRC, Project Manager, Movement Disorders, Inland Northwest Research
Huntington’s Disease (HD) is a genetic disorder that causes a mutation or expansion in the Huntington’s gene, located on chromosome 4. This abnormal mutation in the Huntington’s gene causes the nerve cells in the brain to breakdown over time. HD affects a person’s movement (ability to walk, speak, control movement), cognitive ability (reason, memory, concentration) and emotions (aggression, mood, reaction). HD is an inherited disease, which means the gene for this disease is passed from parent to child. Every child of a parent with HD has a 50/50 (fifty percent) chance of inheriting the HD gene. Every person who inherits the expanded HD gene will eventually develop the disease. Symptoms usually appear between the ages of 30 to 50 and worsen over a 10 to 25year period. Today, there are approximately 30,000 symptomatic Americans and more than 200,000 at-risk of inheriting the disease. It is estimated that 3 to 7 out of every 100,000 people have HD.
Advertisement
Why is it important for research?
The HD gene was identified in 1993, and currently, there is no therapy which can halt, slow, or reverse the progression of HD. However, much of the current HD research is focused on understanding HD and how to modify or stop the progression of disease. Doctors and scientist are using gene-editing drugs to stop the formation of the harmful HD proteins in the brain. Unfortunately, because this disease is rare, there is not as much funding for research. Although there were recently several setbacks in latephase HD clinical trials, all trials (even failed ones) provide important knowledge, that scientists can learn from and build upon. Currently there are several new Phase I trials including, Branaplam, a repurposed spinal muscular atrophy drug, from
Parkinson’s Support Groups
In-person support groups have been suspended during the pandemic. Contact the individuals below to learn if they are meeting virtually, and what their plans are for resuming in-person groups.
COEUR D’ALENE
Lake City Center, 1916 N Lakewood Drive 1st Friday of the month at 1 - 2:30 pm Contact: Beth Hatcher 208-635-5243 Email: cdapsg@hotmail.com
Women with Parkinson’s
Affinity Apartments, 3594 N. Cederblom Street 3rd Friday at 1 pm. A casual get-together. Free to people with Parkinson’s and their caregivers.
KALISPELL
Gateway Community Center
1203 Hwy 2 West, United Way Conference Room Parkinson’s Disease Support Group of Flathead Valley 3rd Wednesday of the month at 3 - 4:30 pm Contact: Marjory McClaren 406-250-5577 Email: marjmccl@yahoo.com Contact: Lynnell Gravelle 406-756-7250 Email: lynnell@arspt.com
SANDPOINT
East Bonner County Library meeting room, 1407 Cedar St., 2nd Mondays at 2 - 3:30 pm. Contact: A.C. Woolnough 208-304-5756 Email: acwooly@gmail.com
SPOKANE
Women Affected by PD Support Group
Riverview Retirement, Dining Room 1801 E Upriver Drive, 1st Thursdays at 1 - 2:30 pm A group of remarkable women living well with Parkinson’s. Contact: Sally Sullivan 509-499-5113 Email: 22sullys@gmail.com
Parkinson’s Support Group
Touchmark on South Hill, 2929 S Waterford Drive 3rd Wednesdays at 2:30 - 4 pm Contact: Lori McCormick 509-321-8130 Email: lori.mccormick@touchmark.com
4th Wednesday of the month at 3 - 4:30 pm Contact: Lynn Woods 406-420-2321 Email: lynwoods@gmail.com This is a new group forming now to address the needs of Parkinson’s Care Partners. Please join us!
Check www.NWPF.org for details Follow us on Facebook! @NW Parkinson’s Foundation
Novartis, that has shown to reduce the levels of mutant huntingtin protein in preclinical models. Companies like Triplet Therapeutics, who specialize in triplicate repeat disorders, are conducting a data collection trial, to help develop their upcoming antisense oligonucleotide (ASO), and small interfering RNA drug trials. These research trials are designed to prevent or delay disease onset and stop or slow disease progression. This is great news for families affected by this devastating disease. Access to resources, education, and research are the cornerstones to successful identification, treatment, and prevention of neurodegenerative diseases. To learn more about these trials please go to the Huntington’s Disease Society of America (HDSA) website at, https://hdsa.org/ hd-research/hd-trial-finder/.
What options are there?
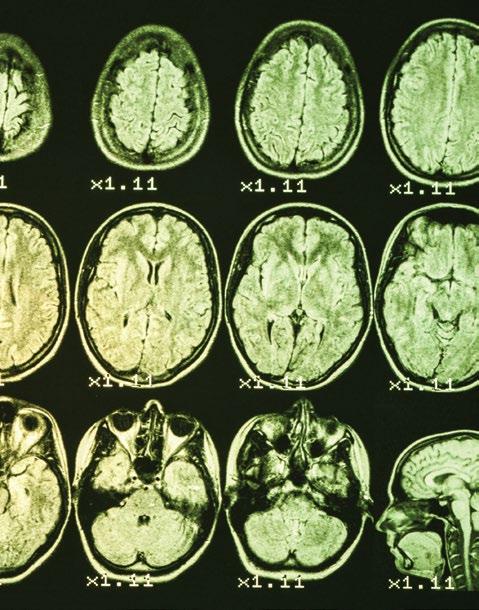
If you have a family history of Huntington’s Disease or know someone who does, it is important to identify what resources are available to support you or your loved ones. Genetic testing for HD can be a difficult and personal choice. Many people do not see benefit in knowing their genetic status, and others find value in understanding their genetic information and risk of disease. Knowing and understanding your genetic risk can you help navigate future medical and personal decisions but can also carry emotional concerns. Talk with your doctor or genetic counselor about moving forward with genetic testing. Typically, genetic testing is not recommended for children under the age of 18, as they may not fully understand what a positive genetic result would entail for their future. The exception would be to confirm a diagnosis of a juvenile onset of HD, should a child display early symptoms of HD. There is a large social support network for HD families through programs like the Huntington’s Disease Society of America who can provide access to social workers, genetic counselors, family planning, advocacy events and volunteer opportunities. The journey of how to navigate Huntington’s Disease is an intensely personal one and there is no right answer in how to complete it. Raising awareness and advocacy on a political and community level is what will help move us all forward in finding a cure. Inland Northwest Research are leaders in national and global research, focused on neurological disorders. We offer high impact clinical trial opportunities in Parkinson’s Disease, Huntington’s Disease, Multiple Sclerosis, Essential Tremor and dementia. We take great pride in helping those with neurological disorders navigate through clinical trial participation, and explore options that are the best fit for their needs. We are proud to partner with Invitae, to offer our community affordable genetic testing services. Genetic testing can be performed as part of a clinical trial registry or electively. Call us at 509-960-2818 and visit inwresearch.com for more information.
Melissa Bixby is the Project Manager for Movement Disorders at Inland Northwest Research. She is a Certified Clinical Research Coordinator (CCRC) and clinical lab scientist with over 15 years of experience in the medical field. She holds a degree in biochemistry from Towson University and a graduate degree in biomedical science from Johns Hopkins University. She runs many of the large Phase 1 and Phase 2 interventional trials and is a credentialed coordinator with both the Parkinson and Huntington Study Groups where she is involved with other collaborative academic trials with sites around the world.

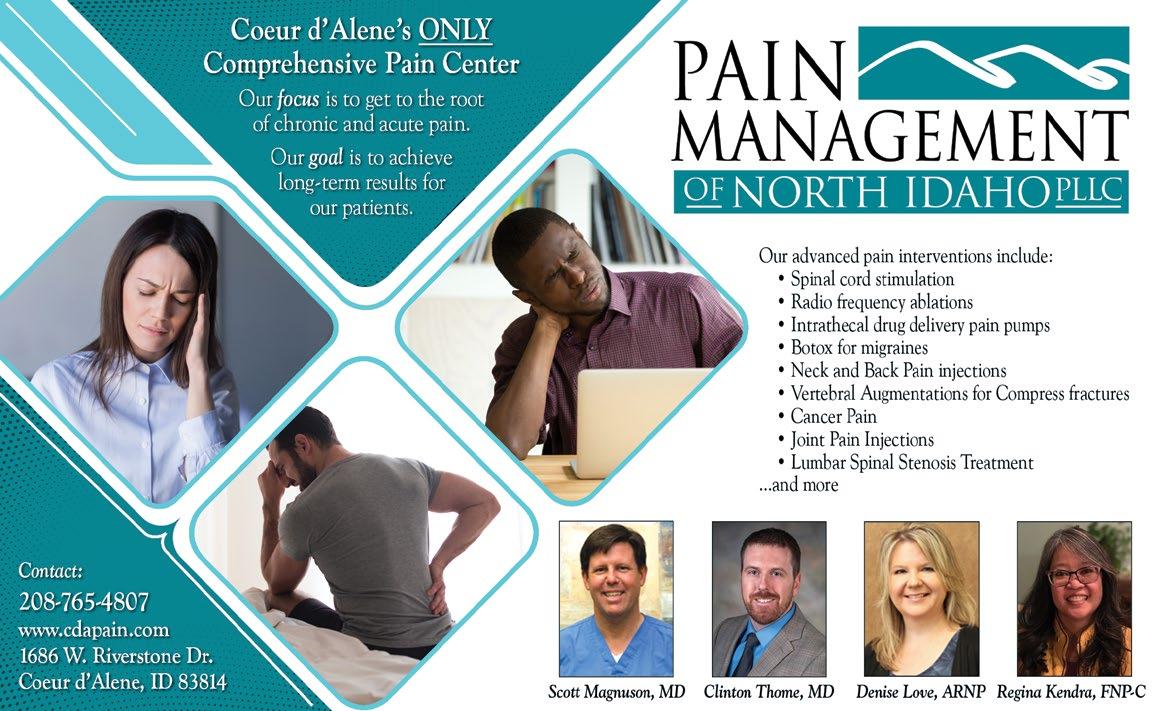
Interventional Pain Management
by Dr. Clinton M. Thome, Pain Management of North Idaho
Acute and chronic pain continue to be common medical problems despite advancements in pain management therapies. Chronic pain is typically more difficult to treat than acute pain requiring more frequent and diverse treatment. If chronic pain can be prevented before it’s occurrence or effectively treated once it has occurred there is dramatically reduced patient suffering, improved quality of life and reduced healthcare costs.
The most effective treatment of pain (both acute and chronic) requires applying the most precise and comprehensive therapies at our disposal while minimizing risks and side effects. The decision making for which therapies to apply for a specific pain presentation are not algorithmic and vary greatly depending on the source, severity, duration and secondary suffering.
Interventional pain management continues to be one of the mainstays of therapy for the treatment of both acute and chronic pain. Interventional pain management is best described as using a specific procedure, or intervention, to diagnose and/or treat a specific type of pain. We have a number of different interventions at our disposal. A combination of the patient’s history, physical examination and imaging helps us identify the source of the pain which will determine which type of treatment and intervention we will employ.
Some of the benefits of interventional pain management include reduced office visits, reduced patient suffering and reduced opioid requirements. Using a specific intervention targets the pain at the source compared to medication treatment which can affect the entire body. Most of the medications we use to treat pain are limited to a few different classes of medications; anti-inflammatories, muscle relaxants, and neuropathic medications. Side effects are common with pain management medications. Combining interventional therapy with medication treatment can reduce the dosage and frequency of medications minimizing unwanted side effects. For example, patients who suffer from arthritic joint pain commonly have to take anti-inflammatories such as ibuprofen or naproxen regularly for pain relief. Frequent use or high dose exposure to anti-inflammatories can result in damage to the stomach and kidneys. Patients with heart disease or on anticoagulants typically have to restrict or minimize anti-inflammatory usage. Employing interventional options such as a nerve block or injection to the painful arthritic joint can reduce or eliminate the need for medications. Newer treatments for arthritic joint pain include nerve blocks, radiofrequency ablation, and peripheral nerve stimulation. We continue to use steroid injections when effective as well as viscosupplementation.
Interventional pain management can commonly produce more rapid pain relief than other types of therapy. One of the most effective ways of treating chronic pain is stopping the formation of chronic pain before it starts. Interventional therapy can sometimes provide potent pain relief in hours to days. The sooner acute pain can effectively be treated, the less likely it is going to turn into a chronic problem. For example, one of the most common pain sources we see in our practice is acute low back pain that radiates down the leg(s). This is commonly secondary to a disc herniation compressing the spinal nerves as they exit the spine. This type of pain is quite common and it routinely goes away on its own. But when the pain is severe
and quality of life is impacted, the more important it is to treat that pain effectively and quickly. Using interventional therapy we can apply medication directly to the location of the disc herniation to reduce pain and inflammation. This therapy can produce significant pain relief within days. The pain relief results in improved quality of life, improved patient function and reduced disability which can ultimately prevent the formation of chronic pain or a surgical procedure.
There are interventional treatments for both acute and chronic pain. Specific interventional therapies are used to target different sources of pain including common sources like joint and spine pain. However, more complex pain like headaches, pelvic pain and neuropathy can sometimes be effectively managed with interventional therapy. Not all interventional therapy contains steroids or medications. New treatments such as peripheral nerve stimulation and spinal cord stimulation are non-medication, minimally invasive, interventional options that can provide long term pain relief. Radiofrequency ablation can be applied to certain locations to treat head pain, neck pain, back pain and certain joint pain.
Most of the interventional pain management therapies are minimally invasive and are performed in the office or as a same day outpatient procedure. Image guidance utilizing x-ray (fluoroscopy) and ultrasound are commonly employed improving safety and effectiveness. The side effects and complication rates are typically very low and the specific risks, benefits and alternatives would be discussed for the specific intervention being considered.
Interventional pain management is also commonly performed by a board certified pain medicine physician. These providers have completed medical school and residency training and then complete a separate fellowship specific for pain management. Common board certified pain specialists are anesthesiologists and physical medicine and rehabilitation doctors. One of the primary benefits of seeing a board certified specialist for pain management is the comprehensiveness of care. We can help diagnose and treat the pain problem from the onset and are not limited to only providing a single aspect of pain care. Because every patient’s pain is unique, the decision making for what diagnostic tools and treatments to utilize should depend on an individualized workup including patient history, examination, and review of appropriate diagnostic studies such as MRI. Effectively tailoring an individualized treatment plan from all of the available pain therapies including conservative therapy, medication management, interventional therapy will improve the efficiency and effectiveness of the patients pain management care. If you suffer from acute or chronic pain consider discussing your pain with the pain management specialists at Pain Management of North Idaho.
Dr. Thome, a fellowship trained pain management physician, completed his anesthesiology residency and fellowship at the University of Texas Health Science Center, San Antonio and was chief resident during his final year of residency training. He had the opportunity to train under some of the most highly regarded individuals in the field of pain medicine. Dr. Thome takes great pride in his medical understanding, exceptional clinical skills and ability to compassionately connect with patients to provide extraordinary care.
Finding Hope in Alzheimer’s Research
by Carrie McBride, Director of Marketing & Communications Alzheimer’s Association, Washington State Chapter
Currently, more than 6 million people in the U.S. are living with Alzheimer’s disease — a number that’s expected to nearly triple by 2050. Prior to the pandemic, Alzheimer’s was the sixth leading cause of death in the country, and the only disease in the top 10 with no way to prevent, cure or even slow its progression. While the impact of Alzheimer’s continues to grow, researchers across the globe are advancing basic knowledge about the disease, exploring ways to reduce risk and developing potential treatments.
The National Alzheimer’s Plan, first released in 2012, established an ambitious goal of developing preventions and effective treatments for the disease by 2025. The Alzheimer’s Association is leading the way as the world’s largest nonprofit funder of Alzheimer’s and dementia research. Currently, the Association is investing over $208 million in 590 research projects across the globe.
Federal funding for Alzheimer’s and dementia research is also critical in addressing the Alzheimer’s crisis. Again, the Alzheimer’s Association is playing a vital role as the largest Alzheimer’s advocacy organization in the world. With the help of grassroots advocates across the country, funding for Alzheimer’s and dementia research at the National Institutes of Health (NIH) has increased sevenfold since 2011. Today, funding for Alzheimer’s and dementia research at the NIH is at $3.1 billion annually — and we are calling on Congress to increase funding by an additional $289 million in 2022.
As a result of this unprecedented funding, scientists have been able to work at a more rapid pace and have made many strides in recent years. The latest advancements in Alzheimer’s research give us many reasons to be hopeful.

A blood test for Alzheimer’s is closer than ever.
It wasn’t that long ago that the only way to diagnose Alzheimer’s was through an autopsy. We’ve made some progress — Alzheimer’s can now be diagnosed through a PET scan, but it’s very costly and isn’t covered by Medicare, Medicaid or any kind of health insurance.
There is a global effort in the Alzheimer’s field to identify and develop accurate, less expensive diagnostic tools for Alzheimer’s and other dementias. Blood tests have emerged in the last few years as a potential solution. In fact, new research released at the Alzheimer’s Association International Conference last year identified a blood marker that shows both Amyloid plaques and Tau tangles — the two hallmark features of Alzheimer’s disease.
Why is finding a blood test so important? Blood tests would be a game changer for Alzheimer’s research. Scientists would be able to identify clinical participants more quickly and they would have an easy way to measure the efficacy of the drugs they’re testing. This would ultimately speed up the development of a drug to slow or stop the progression of the disease.
The drug pipeline for Alzheimer’s is heating up.
In late 2019, Biogen released promising data about its drug, aducanumab. In Phase 3 clinical trials, the company found a significant reduction of cognitive and functional decline in people with mild dementia and mild cognitive impairment (MCI) due to Alzheimer’s. The drug is currently being reviewed by the FDA, and if approved, it would be the first available treatment to potentially change the progression of Alzheimer’s disease.
Advanced Care Northwest LLC
In-Home Care at its Finest - Available 24/7
All clients & caregivers supervised by a Registered Nurse (RN)
Special focus on matching personnel with each client to bring compassion, comfort and enjoyment to your in-home care experience. Familiar with use of assistive devices. Serving all ages in Bonner, Boundary & Kootenai counties Call for a Free In-home Consultation 208-263-3225

In March, Eli Lilly & Co. reported detailed results of their Phase 2 clinical trial for their drug, donanemab. People taking the experimental drug did not maintain or improve their cognitive abilities; they continued to decline, but at a measurably slower rate. While these results are encouraging, longer and larger trials are needed to determine the safety and efficacy of the drug.

We’re learning more about prevention and risk reduction.
There is growing evidence that suggests choices we make throughout our lifespan may impact our risk of developing dementia. A 2020 report by the Lancet Commission identified 12 modifiable risk factors for dementia: less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, low social contact, alcohol consumption, traumatic brain injury and air pollution. They estimate that 40% of dementia cases worldwide could theoretically be prevented or delayed through these modifiable risk factors.
The US POINTER study, a two-year clinical trial led in part by the Alzheimer’s Association, is evaluating whether lifestyle changes can protect cognitive function in people at risk of developing dementia. The trial involves 2,000 volunteers, age 60-79, who will follow either a self-guided or structured program encouraging increased physical exercise, a healthier diet, cognitive and social stimulation, and self-management of heart and vascular health. Final results of the trial are expected in 2023. If the interventions prove effective, an evidence-based program for prevention could be developed and implemented in communities across the country.
Today, we have more momentum in Alzheimer’s and dementia research than ever before. With the advances being made in prevention, early diagnosis and drug therapies, we know that hope is on the horizon. Every day, we’re moving one step closer to our vision of a world without Alzheimer’s and all other dementia.
Carrie McBride is the Director of Marketing and Communications for the Alzheimer’s Association in North Idaho. She has a degree in Communications from University of Washington and 15+ years of experience working for health-related causes. She is also a member of the Dementia Action Collaborative, helping to implement the Alzheimer’s State Plan in Washington State.










