
9 minute read
Diagnostic Discussion
DRS. LAUREN A. RUDDOCKS*, NEEL BHATTACHARYYA, DONALD M. COHEN AND NADIM M. ISLAM Read, Learn and Earn! A 40-year-old male presented to oral and maxillofacial surgeon Dr. Stephanie Reeder Henley in Jacksonville. His chief complaint was a two-week history of swelling affectVisit floridadental.org/online-ce for this FREE, MEMBERS-ONLY BENEFIT. You will be given the ing his lower jaw, with minimal associated pain. Tooth opportunity to review the “Diagnostic Discussion” and its accompanying photos. Answer five No. 30 had been extracted six months previously. Clinimultiple choice questions to earn one hour of CE. cal examination revealed a firm expansion of the right mandible with mobility of teeth Nos. 29 and 31 (Fig. 1). No contents were retrieved upon aspiration of the swelling. A panoramic radiograph revealed an ill-defined mixed radiolucent-radiopaque lesion with extension superiorly into the soft tissues and causing inferior displacement Contact FDC Marketing Coordinator Brooke Martin of the inferior alveolar canal (Fig. 2). Buccal and lingual at bmartin@floridadental.org or 800.877.9922. cortical destruction as well as irregular deposition of bone on the buccal and superior surfaces of the mandibular body is seen on CT imaging (Fig. 3). Dr. Reeder Henley performed an incisional biopsy that was submitted to the Oral Pathology Biopsy Service at University of Florida College of Dentistry in Gainesville. The microscopic features included atypical cartilaginous material, bone and cells resembling osteoblasts (Fig. 4). Question: Based on the above history, clinical photograph and imaging findings, what is the most likely diagnosis? A. Fibrous dysplasia B. Osteoblastoma C. Ossifying fibroma D. Osteomyelitis E. Osteosarcoma
Fig. 1: Swelling of the right mandible. Fig. 2: Ill-defined mixed density lesion in the area of missing tooth No. 30, causing inferior displacement of the inferior alveolar canal.


Fig. 3A: Cross-sectional CT images at 3 mm intervals showing an ill-defined, mixed lytic-sclerotic lesion, perforation of the buccal cortex and sunburst periosteal reaction.

Fig. 3C: (3D volume rendering) Buccal view showing a “moth-eaten” lesion with irregular bone deposition superior to the alveolar crest. Fig. 3B: (CT) Axial view showing a “moth-eaten,” mixed lytic-sclerotic lesion, perforation of the buccal and lingual cortices, and sunburst periosteal reaction on the buccal surface of the mandible.


Fig. 3D: (3D volume rendering) Lingual view showing an ill-defined “moth-eaten” lesion with perforation of the lingual cortical plate.
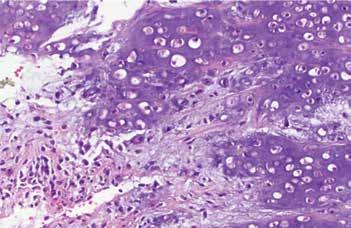
Fig. 4: Atypical cartilaginous matrix and osteoblastic cells.
FROM PAGE 89
A. Fibrous dysplasia Incorrect, but good thought. Fibrous dysplasia (FD) is a benign fibro-osseous lesion associated with mutations in the GNAS gene. It typically presents in patients younger than ours, with most cases presenting within the first three decades of life; however, it can be seen in patients of any age. Craniofacial involvement is common, with the maxilla affected more frequently than the mandible. The condition can affect one bone (monostotic) or multiple bones (polyostotic). The monostotic form accounts for 80-85% of cases, typically presenting unilaterally. As in our case, bony expansion is the presenting feature, with or without pain. Other symptoms resulting from nerve compression can be seen in FD, including vision and hearing loss. Radiographically, the lesions of FD have indistinct borders and may be radiolucent, radiopaque or a combination of both. However, they often exhibit a characteristic “groundglass” appearance. In contrast to osteosarcoma, the cortical bone is thinned but intact, and a periosteal reaction is not seen. Tooth displacement may occur, but root resorption is not a feature of FD. CT imaging is the gold standard for evaluation of craniofacial FD. Microscopically, the condition is characterized by curvilinear trabeculae of woven bone set within fibrous tissue. Antiresorptive drugs and monoclonal antibodies have shown success in slowing progression of the condition. Deformity is corrected by complete removal of affected bone and bone grafting. B. Osteoblastoma Incorrect, but a reasonable consideration. Osteoblastoma (OB) is a benign bone neoplasm with some clinical similarities to osteosarcoma. The spine is the most commonly involved location within the body, but in the craniofacial region, OB has a propensity to involve the posterior mandible. The average age of affected patients is younger than that of those with osteosarcoma, at around 25 years. However, cases have been reported in patients across a wide age range from 3 to 61 years (Cale Jones, 2006). As with osteosarcoma, the lesion typically presents with bony expansion accompanied by pain. Differentiation between OB and low-grade osteosarcoma can pose difficulty, as OB presents as a radiolucent, mixed radiolucent-radiopaque, or radiopaque lesion that can be well- or ill-defined, with cortical thinning and/or destruction. This is a particular problem in cases of “aggressive osteoblastoma,” reported to occur in older patients and to exhibit locally aggressive behavior. Microscopic examination of OB reveals deposition of trabecular bone by osteoblasts in a background of fibrous tissue. Although significant cellular atypia is not expected in benign lesions such as these, bizarre-looking osteoblasts have been reported in cases of aggressive OB, further blurring the distinction with osteosarcoma. However, even cases of aggressive OB should demonstrate a distinct microscopic boundary with normal bone, unlike osteosarcoma. Submission of representative sections of the entire lesion and providing the pathologist with a comprehensive clinical history are both critical to facilitate accurate diagnosis. Recurrence rates of OB are low (10-15%) but they are thought to be higher for aggressive OB. Treatment for both types of OBs consist of surgical resection. C. Ossifying fibroma Incorrect, but certainly among the differential diagnoses. Ossifying fibroma (OF), also known as cemento-ossifying fibroma, is another benign fibro-osseous lesion characterized by bony expansion. Conventional OF usually presents in the mandible in patients around the age of ours, but it is much more common in females than males. In contrast to osteosarcoma, OF presents as a well-demarcated, mixed radiolucentradiopaque, typically symmetrically expansile lesion. Cortical perforation and periosteal reaction are absent in conventional OF. Microscopic examination reveals irregular trabeculae and droplets of cementum-like material, typically surrounded by osteoblasts, in a background of fibrous tissue. Treatment is by enucleation, with lesions frequently reported to “shell-out” easily. Conventional OF does not tend to recur if completely excised.
D. Osteomyelitis Incorrect, but good thought. Osteomyelitis (OM) is the inflammation of bone, usually caused by infection. OM and osteosarcoma share several clinical features, including pain, swelling and sometimes paresthesia. OM of the jaws presents most commonly in males between the ages of 50 and 70 years. Radiographic features of OM also overlap with those of osteosarcoma: Acute OM shows irregular, “moth-eaten” radiolucencies, while sclerotic change, a periosteal reaction and Codman triangle can be present once the disease becomes chronic. Cortical destruction is another feature seen in both OM and osteosarcoma. Although widening of the PDL space can be seen in OM, it does not tend to affect the entire PDL space of
the teeth in the affected area, as is the case in osteosarcoma. In addition, the periosteal reaction of OM typically has a laminated or “onion-skin” appearance in contrast to the sunburst appearance of osteosarcoma. Root resorption is not a feature of osteomyelitis. Microscopically, the presence of an inflammatory infiltrate and fibrous replacement of bone marrow are suggestive of OM. Clinical correlation is required for definitive diagnosis. Successful treatment typically requires aggressive debridement of necrotic bone and administration of intravenous antibiotics.
E. Osteosarcoma Correct — well done! Osteosarcoma is the most common primary malignancy of bone. It arises most often in the long bones and is relatively rare in the craniofacial skeleton. When it does occur in this region, it most frequently affects those between the ages of 20 and 50 years. The tumor is seen in the maxilla and mandible with roughly equal frequency, while males are affected slightly more often than females. Osteosarcoma of the jaws usually presents with swelling, with or without features such as pain, paresthesia, tooth mobility and nasal obstruction (when tumors involve the maxilla). Enlargement of the swelling in the weeks following tooth extraction has been reported, as seen in our case. There is no single typical radiographic presentation of osteosarcoma, but rather a spectrum from completely radiopaque through mixed radiolucent-radiopaque to completely radiolucent. Lesional borders are ill-defined or “moth-eaten” in appearance. The presence of a periosteal reaction with a characteristic “sunburst” appearance may raise suspicion for osteosarcoma; however, this is seen in only around 25% of cases within the jaws. It’s evident on CT imaging in our case but is absent from the panoramic radiograph. Additional features include symmetrical widening of the periodontal ligament (PDL) space, expansion and destruction of cortical bone, and the Codman triangle: the elevation of periosteum from the cortex due to new bone formation over the rapidly growing tumor. Tooth roots may exhibit sharp, “spiking” resorption and symmetrical widening of the PDL space. Imaging modalities, including CT and MRI, are essential in the evaluation of suspected osteosarcoma. Our case is an example of the chondroblastic type of osteosarcoma, characterized histologically by the deposition of cartilaginous matrix as well as abnormal osteoid (the unmineralized precursor to bone) by malignant osteoblasts. Treatment of osteosarcoma of the head and neck consists of wide resection. Adjuvant radiation and/or chemotherapy can be beneficial in cases where there is difficulty achieving clear margins. Reported five-year survival rates range from 25% to 50%, with lower rates of metastasis and better outcomes seen in head and neck cases compared to those of the long bones. However, the recurrence rate of osteosarcoma of the jaws is higher than that of extragnathic tumors. References:
Availabe upon request
DR. BHATTACHARYYA Diagnostic Discussion is contributed by UFCD professors, Drs. Indraneel Bhattacharyya, Don Cohen and Nadim Islam who provide insight and feedback on common, important, new and challenging oral diseases.
The dental professors operate a large, multi-state biopsy service. The column’s case studies originate from the more than 12,000 specimens the service receives every year from all over the United States.
Clinicians are invited to submit cases from their own practices. Cases may be used in the “Diagnostic Discussion,” with credit given to the submitter.
DR. COHEN Drs. Bhattacharyya, Cohen and Islam, can be reached at oralpath@dental.ufl.edu.
Conflict of Interest Disclosure: None reported for Drs. Bhattacharyya, Cohen and Islam.
The Florida Dental Association is an ADA CERP Recognized Provider. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be directed to the provider or to ADA CERP at ada.org/goto/cerp.
*Third-year resident in Oral and Maxillofacial Pathology University of Florida College of Dentistry.
DR. ISLAM





