





































































Sometimes,the nurseswho aredeserving of recognition forNational Nurses Day arenolonger with us hereonEarth.Sadly,nurse Teri Ann Reed passed away tragicallylast year.Wesharethe wordsof her husband, Keith, to honor her memoryand contributions.


“Teri, my wifeand lifepartnerof40-plus years, wasalong-time nurse at StillwaterMedical Center.InJanuaryof2021, she wasrun over and killed as she wasattempting to cross thefour-lane highwaybetween the hospital and her car. Averylong dayofaverylong month of averylong year.”
From Teri’s obituary: Teri was many things to many people, but at the very core of her being, she wasanurse.Teri began her career as a16-year-old volunteer at Newman Memorial Hospital in Shattuck, Oklahoma. Teri attended nursing school at West TexasState University, whereshe graduated with honors. Teri’snursing career took severalturns over the decades,adjusting her work as needed so she could care forher family firstand foremost.
Had Teri’slifenot been tragicallycut short, thereislittle doubt she would have ended her career as it began; as avolunteer in the halls of StillwaterMedical Center, running circles around everyone elsewhile she caredfor her patients.
Formany, acareer in nursing is acalling. At Saint Francis Health System, we areprofoundly grateful forthe thousands of nurses who makeour health systemwhat it is—a true team, interconnected and united in serving one mission: To extend the presenceand healing ministry of Christ in all we do.Wecelebrateand thank all of our nurses forfulfilling their unique vocation, fortheir manysacrifices and fortheir extraordinary dedication in serving the people of eastern Oklahoma.

RyanMorales has been aregistered nurse with Saint Francis Health System forthe last three yearsand served in avarietyofrolesasanemer gencyroom and critical care registered nurse.

Morales is currentlyone of fewnursesfromSaint Francis whoisemployedasacritical care systemwide float. That means he is sent to anyofthe Saint Francis hospitals (Main, South, Muskogee, Vinita) to assist in the care of the highest acuitypatientsand help with any staffing shortages.

Morales has primarilybeen working in COVID-19 unitssinceSpring 2022.


He has received special training on advanced treatment procedurestoassist those battling COVID-19.His nominatorssaid that during the last twoyears,Morales has continuallyworkedadditional hoursevery week to help coverany staff shortages to make sureall patients continue to receivethe qualityofcaretheydeserve and provideassistanceand support to his co-workers. Due to hishardworkand knowledge, he continuallyreceives complimentsand accolades from his colleagues and those patientsheassists. Hisnominators said thatit’sapparent thatMorales has found his calling in nursing due to his calm, yetconfident demeanor,his compassion, his abilityto educateand comfort those in his care,and his willingnesstogoabove and beyond wheneverpossible.







FORMORE THAN











YEARS,


























The nominatorsfor nurse Kellye Mead of StillwaterMedical Center said:


Our 8-year-oldson wasdiagnosedwithbrain cancer the week beforethis past Christmas. Kellye wasarockfor us during our 10-dayhospital stay after his brain surgery.She wasveryencouraging and explained thingsevery step of the way. Kellye was alsothe perfect balanceoftender care and pushing forprogress. Our familylooked forwardtothe shifts she worked. Kellye made the scariest time in our life peaceful, manageable and even fun at times.She will always have aplaceinour hearts.

madethescariest time inourlifepeaceful, manageableandeven funat times. Shewillalwayshavea placeinour hearts.
“





CourtneyPacehas been on the front lines against COVID-19 sincethe beginning of 2020 in the ICUof Hillcrest Hospital South.
Hernominatorssaid thatshe has been influential in ensuring that patients have constant contactwith theirfamily membersvia FaceTime and video conferencing when families were not allowedto seetheir lovedones.


Throughout the peak of COVID-19 cases,Courtney enteredgraduateschool forher doctorateofnursing practice. She has been aconstant advocate for nursing and patient safety even in order to ensurethat patientshavethe best care.Rather than deciding to leaveto take acontract job, she stayed in Tulsa because she wasborninTulsaand wants to practiceasa nurse practitionerinher hometown.
Pace has workedtirelesslytoprotect those from her home state, and she has shown constant dedication to improving her skillsand providing patient care to the best of her abilities.



Breanna Grubbsisadedicated and caring nurse at Saint Francis Health System, her nominators said.

She is alsoa mom,friend andanactivecommunitypatronof the Adair School District.
Grubbsbalances her lifeasamother of four,and she still finds time in her busyschedule not onlyasa professional nurse,but alsotoserve as a school boardmember forher community.


Grubbsvolunteers her talentsasan artist forseasonal decorations in the school cafeteria.
Those whonominated her said that she is an active presenceinher children’sbusyschedules of extracurricular activities.
Grubbs’ children areinvolvedinband, softball, basketball, cheerleading and Johnson O’Malleyactivities.Her familyeven finds time to participateinlawn mowerracing events.

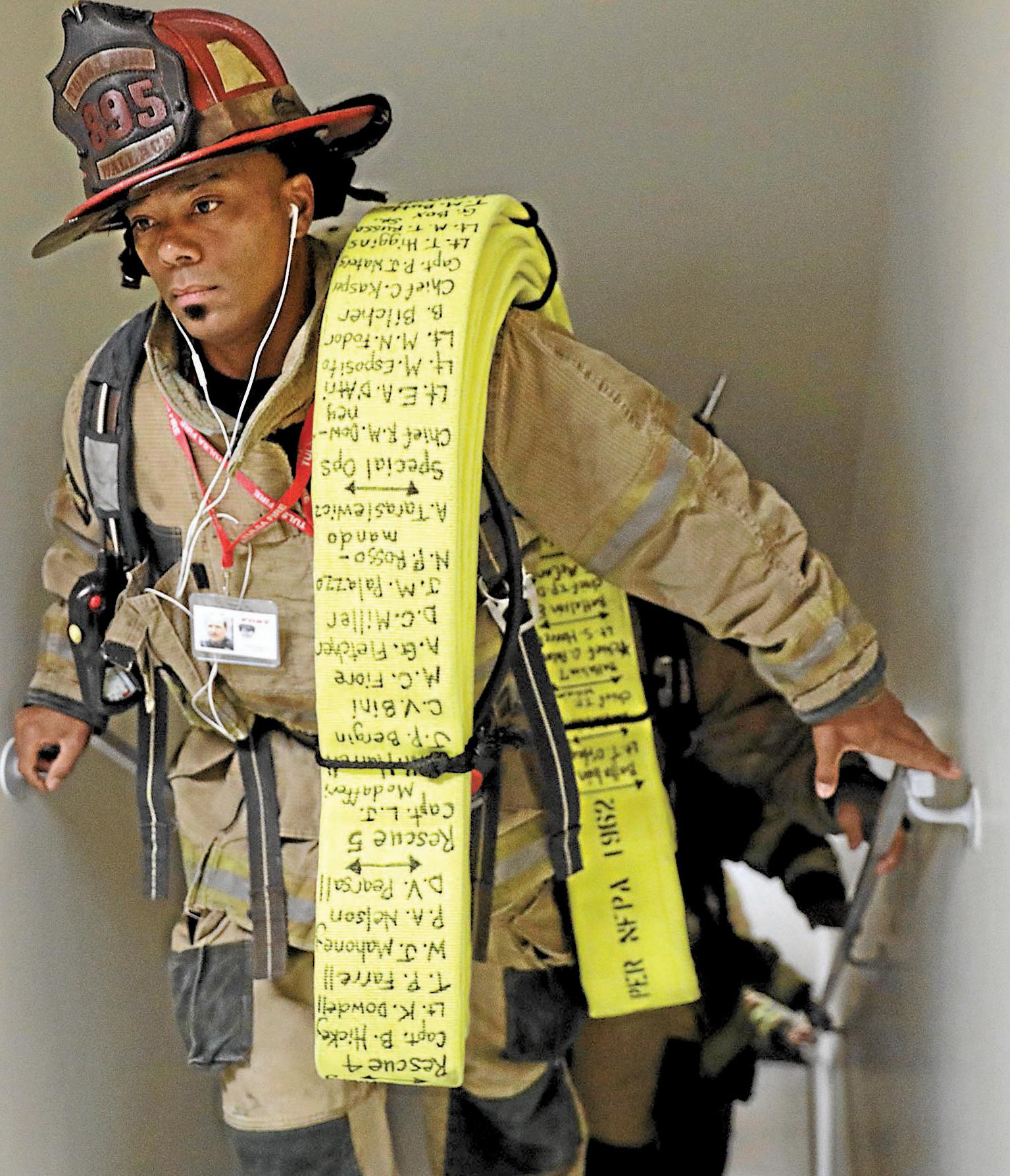


Kofi Wallaceisn’tastranger to saving lives. serves as director of EmergencyMedical Se vices at TulsaFireDepartment, wherehe’s been since1999.
Inaddition,he’saregisterednurseatTulsaER&Hos pital. As if that wasn’tenough, Wallaceis finishing up bachelorofscienceinnursing,andherecentlygotaccept to Maryville foranew challengeofnurse practitioner.





“Throughout my career on the fire department, I’ always been working on something,”hesaid.

Wallacewas an EMT when he movedfromCalifornia. Then he workedtoward becoming aparamedic while serving at the fire department.
At the start of the COVID-19 pandemic,Wallace brought his positive spirit to the St. John ICUand part time forEMSAbeforehetransitioned to TulsaER.
“One of the thingsIlikeabout the fire department is younever reallyknowwhat you’re going to get into. Everything is always different. It’s always something new.”
The same thing is true forthe ER, he said.
“I have apassion to help people, so I’ve done lotso in that realm. I’mliterallyonlytheretomakethe situation better and do everything Ican to help them,”Wallacea
“It reallyprovidesalot of meaning formylifetobea impactspeople so much.”do something that impacts people so
Everything is always different. It’salways something new. .
“ “
































































































































































Kameron Dugan gothis start in nursing six yearsago,following in his mother’sfootsteps. She’sbeen anurse fornearly twodecades.
As farasbeing nominated, Dugan said he wasexcited and shocked.
“It’s just my dailylife. Idon’tfeel likeit’sextra,”hesaid.
He’s worked in theIntensive CareUnitasthe critical care nurse at McAlester Regional Health Center forthe last five years. He is currentlythe ICUnurse manager.

“I love ICU.Ilovebeing ableto geta critical patientand keep them from start to finish, to actuallybeable to seethem through to get better,” he said.
In addition, Dugan said he alsolikes the faster pace of the emer gencyroom and the diversityofpatients, and he still worksinthe ER from time to time.
Dugan’s favorite thing about nursing in general is helping people getbetter and that there’salwayssomething newtolearn.

“I come to work and Ilearn something newevery day, whether it be from apatient or from one of our other nursesor physicians,” Dugan said.

He prides himself in communicating with patientsand family membersduring stressful situations.
“Peopleare complex,and it’s fun to figureout what’s going on with them and howyou canbest help them.”









Lorri Myersisaregistered nurse and worksatOklahoma State UniversityMedical Center as a health supervisor.She’sbeen a nurse formorethan 30 years.

“It is acalling. Either you’re destinedtobeanurse or you’re not. You have to be absolutelypositive that that’s what youwant to do,”she said.
Myersdecided in high school that she wanted to be anurse after visiting the hospital whereher mother worked.
“I just stuck with my decision, and Ihavenot regretted it at all,”she added.

Myers’ daughter alsocaught the “passion bug”for nursing and is a certified burn center nurse at Hillcrest. Myersdescribed what it was liketoworkduring peak COVID-19 hospitalization casesin2020:

“The most grateful and appreciative that I’ve seen of patientsand families wasduring COVID.That wastrulyanexhausting time and afrightening time for manypeople,”she said.
y people,” she

Myerssaid that families areabig part of healing and so nurses became thosepeople.
“Nursesatthis point,theywerethe familyand still arebecausefamilymembers couldn’tcome in.”
ForMyers and her work family,the COVID-19 pandemic is amemory that won’tbesoon forgotten.
“During the midst of it, it was hard. Being in administration, Isaw it all and hearditall. Isaw nurses with their ownphones doing Face time with family, patientsinICU whoweren’tdoing well,”Myers said.

She said that the trying time brought about adifferent perspective fornurses.
“There’smoreofa confidenceinwhy we actuallywent intodothis,” she said.


melia Garrett’s patientsloveher!”
Those whonominated Garrett with Tulsa Spine &SpecialtyHospital said that she is frequentlyrecognized forbeing so kind and helpful at her jobasa nurse.


But, her jobisactuallya passion that sparkedduring high school, inspired by her family.
She learned alot from her grandparents, wholived close to her.
Garrett’s grandmother had Alzheimer’s, and she was instrumental in her care.She learned so muchduring that time, which laid the foundation forher futurecareer.
She was able to watch her grandfather,who was a ra diologist, read X-rays and describe what he saw.
Although she knewthat she wanted to enter acareer thatwould helpothers, not everyone wasonboard at firstwith the thought of pursuing anursing career.
Garrett’s dadknewthat she wasgoing to become a nurse,but it wasn’tuntil high school that she felt led in that direction.
By her senior year,she shared her goal of becoming a nurse with her dad.She lovedlearningabout the human bodyinanatomyclassinhigh school, and her teacher told her that she would be agreat nurse.
Garrett is motivatedbyher faithand enjoystaking care of people to makesuretheyfeel special and caredfor.
She said that it is rewarding to love people in such a direct way.

Rhonda Hanan is asenior nursing leader with 40 years of nursing experienceaccompanied by an extensive and diversebackground as being a chief nursing officerand chief operating officerathospitals and medical facilities in Oklahoma.



Currentlyshe serves as the executive director of nursing at OSUMedical Center under the management of Saint Francis Health System. Herpassion forleadership and drive for achieving and sustaining positive clinicaloutcomeshas been at the forefront of her nursing career along with creating high quality, reliable systems of care and developing the next gener ation of nurses.
Hanan has received several honorsand awards throughout her nursing career such as the American Association of Nurse Assessment Coordination (AANAC)National DirectorofNursing Awardand the National Best PracticeAward
LisaMedina,RN,BSN,MHA, CPHQ,isthe Ascension St. John marketchief nursing of ficer. From 2017to2019, she wasASJ chiefqualityofficer. Beginning in 2011 she held the position of vicepresident of quality& safety.Previouslyshe wasdirector of quality&safety andhas served in other St.John cardiology clinical leadership positions

She originallyjoined St.John in 1987,and after an eight-year relocation to SanDiego,CA,returned in 1999.She is amember of Sigma ThetaTau, ANA, ONA, OONE and ACHE. She is amember of the Oklahoma Hospital Association Council on Quality&Patient Safety She previouslyservedon the Board of Directorsfor the American Heart Association. She is agraduateofthe Ascension Leadership Academy.
LindyBauer,MHA,BSN,RN, is the chief nursing officerfor Muscogee Nation Department of Health-Hospital Services, whereshe provides oversight fornursing practiceand clinicaloperations.Prior to joining the Muscogee Nation, Lindy wasthe director foremergency services at Hillcrest Medical Center.
She has workedinthe nursing fieldfor morethan 19 years. Lindyreceived her master of scienceinhealth care administration from Oklahoma State University, bachelor of science in nursing from Northeastern StateUniversityand associate’sdegree in nursing from Oklahoma StateUniversity InstituteofTechnology
Cynthia Leathersisvice president and chief nursing officeratSaintFrancis Health System and since2017inthe role of executive director,Patient CareServices.

She has been in this current rolesince2022.Sheisamulti-dimensionalpassionate seniorexecutivewith25yearsofextensive experienceofworkinghealthcare operations.Leathershasexperiencewithfinance,strategicplan ning,change management,program growth and development, servicelinequalityimprovement andregulatorycompliance.

Leathersreceivedher bachelor of scienceinnursing from Langston University, then her master’sinbusinessadministrationhealthcaremanagement from the Universityof Phoenix. She seekstomotivate, encour age, and empowerateamof zealous professionals in the quest of prevailing business success.She is amember of the AmericanCollegeofHealthcare Executives, American Organization of Nurse Executives,and American NursesAssociation.
BenStutzman has been chief nursing officeratHillcrest Hospital Pryorsince2017.Prior to this,his time wasspent as an emergencydepartment registerednurse in Tulsaand Joplin areassincegraduating from NEOA&M Nursing School in 2008,mostrecentlyasHillcrest Claremore’sEDmanager from 2014-2017.
He received his BSNfrom Oklahoma Wesleyanin2011 and MS in healthcareadministration in 2016. Hiswife, Danielle, is alsoanurse and theyhavethree beautiful, or nerychildren: Sophie 8, Jaxon 7, and Ezekiel 4.

Atthe beginning of the pandemic, PennyWeismuller, director of Cal StateFullerton’sSchool of Nursing,said everyone in her Southern Californianeigh borhoodwouldcomeoutside at 7p.m. to makenoise in celebrationof the health care workerson the front lines.

Herneighborhood still comes out to honor the resiliencyofhealth care work ers, especiallynurses.
Nurseshavealwayshad to be resilient, Weismuller said. The pandemic showcasedthat resiliencyand pushed itslimits in some cases.
She said forsome nurses, this is their firstdisease outbreak. Weismuller,who for30years workedin disease control and
Front-line workers, includinghealth careworkers, who areconcerned about their mental health can visit Mental HealthAmerica tobescreened and find resourcesand support.
epidemiology,has experienced multiple outbreaks.But this pandemic “has been very difficult forall of us.”
With multiple wavesofcases,hospi talizations anddeaths, some nursesand other health care professionals areburning out.
In aMental Health Americasurveyfrom June to September 2020,93% of the more than 1,100 health care workers surveyed were experiencing stress. The survey found that 86%reportedexperiencing anxiety, 77%reported frustration, 76% reported exhaustionand burnout,and 75% said theywereoverwhelmed.
Emotional exhaustion wasthe most common answerwhen health care workers were asked what had changed forthem recently—followedbytrou ble sleeping, physical exhaustion and
The American Nurses Association recommends nurses contacttheir orga nization’s employeeassistanceprogram if stress,anxiety, fear,rumination or depressed moods areinterferingwith their functioning. Be proactive and do not wait until you’re in crisis.
HealthyNurse,HealthyNation Grand Challengeisa program thataims to createahealthynurse population.
The American Psychiatric Nurses Associationprovides self-carestrategies.
Nurse associations collaboratedtocreate the Well-BeingInitiative, a nurses’guidetomental health supportservices.
The National AllianceonMental Illness created aguidefor health care professionals that covers when to reach out,confidential and professional support, peersupportresources, buildingresilienceand other resources.
work-related dread.
About 39%ofhealth care workers said that theydid not feel liketheyhad adequatesupport.
We spoketofour nurseson the front
lines of the pandemic in LosAngeles Countyand one in academia to ask what challengesthey’ve facedsinceMarch 2020 and howtheyare coping, personallyand professionally. Here’s what theysaid.
Anahiz Correa remembers astrong connection with apatient at South L.A.’s Mar tin Luther King Jr.Community Hospital, whereshe is the head of nursing forthe intensive care unit.

She and the patient shared alast name, and he happened to be from the same town in Mexicoasher grandfather.
Correa had to fill in on night shiftswhen thehospital wasshort-staffed, on topof her normalduties.That’show she met and connected with this man.
“Weknewthat the chances of his sur vivalweren’thigh,” Correa said.
He had been in the intensive care unit forabout twoweeks, and by theend of his second, the unit’s physician, with the patient’s consent, madethe decision to intubatehim.
Correa helped the patient call his wife, knowing it might be the last time he would be able to speak to her.Correa and the other nursesstood by thepatient to supporthim and each other in that moment.
“Witnessing that conversation, it really putmethrough howmanytimes my staff has witnessedthese conversations during this time,”Correa said.
Correa’s advice:After that phone call, Correa and herteamstepped out of the room and talked about what theywitnessedand howitmade them feel.
Correa said those kinds of conversations occurred often. Forsome membersofher team, that wasenough. Otherschose to seek professional help —including Correa. She began talking to atherapist about her work in the ICU.
Anahiz Cortez lifts weights last year at the UFC GyminLa Mirada, Calif.Workingout is one of the activities Anahiz does forher self-care.

She alsorelies on meditation and momentsof gratitude beforeand after work to getherself in the right mindset to perform her duties in caring forher community.
When it came to helping her staff,Cor reawas integral in establishingapost-ICU clinic at Martin Luther King Jr.hospital.
She said nursesworried about whether dischargedpatientswould getthe specialtycaretheyneeded to completelyrecoverfromabout with severe COVID-19.
“Our nurseswerefeeling like, ‘We’re saving thesepatients, but what wasgoing to happen to them after?’” she said.
Correa collaborated with aphysician to create the clinic whereICU nursescan participateinpatients’ follow-up care.
“It’s absolutely healing for a lot of them to knowthat our patientsare being taken care of,” she said.
JoyceLeido is asupport system at work and at home. Leido,chief nurse executive forKaiserPermanenteLos Angeles Medi calCenter,looked after her team of nurses during the pandemic as well as her hus band, whoisaregistered nurse in an ICU at another Kaiser hospital.
Herhusband would come home from work with stories about telling apatient’s out-of-townrelativesthat their lovedone wasgoing to die,orofcaringfor acritically ill patient.
She knewthat if her husband wascoming home with“this emotional and mental anguish and pain,”then everysingle nurse at her hospital wasdealing with the same thing.
“It wasamagnifying glass. Ijust don’t gettohearall of the stories from our 1,300 nurses(at Kaiser LosAngeles), but Iknow they’re feeling the same thing,”she said.
As aleader,Leido said, she wasintentional about providing resourcesfor them.
Leido’sadvice:Leido said she did alot of listening —not onlyabout day-to-day experiences,but alsofears.Manyofthe concerns she heardfromher staff (and her husband) were about not knowing when the increase in patientswould slow down or when the pandemic would end.
She provided aspace to talk or cryfor
anyone whoneeded it. From that, she learned that manynursescarried alot of guilt —especiallywhen apatient died.
“He’s an excellent nurse, but he would say, ‘I wish Icould have done something different,’” she said about her husband.
In thesescenarios, she could tell areassuring truth: Theydid the best theycould; the patient knewtheywerecared forwith 120% of you; this is aterrible disease;and there’snothing morethat youoranyone elsecould have done becauseweall are doing our best.
Another wayLeido has helped her team is by certifying her dogs Lani, asoftcoatedWheaten terrier,and Feta,a golden retriever, to be therapydogs. Lani wasa respitefor Leido after along dayat work, so she shared her furrysupport withher staff.Her dogs go to work onceaweek,and just about everyemployeeat the hospital finds amoment to destresswith them.

Typically, studentsattending Cal State Fullerton’snursing programneed to ful fill acertain amount of direct-carehours, earned by working in ahospital setting, to become anurse.In2020, studentsearned their hoursbyassisting OrangeCounty’s emergencypandemic operations.
PennyWeismuller,director of the program, said the countypublic health department had studentsplan the con version of avacation facilitytoa hospi talsetting, conduct contact tracing and administer COVID-19 testsand vaccines.
“The hospitals didn’thavethe capacity forthemtogointocriticalcarebecausethey
didn’tneed the stressofastudent at that moment,”Weismuller said.
Weismuller’sadvice: People needto recognizethat healthcareworkers areall humans and don’thaveunlimited capacitytoendurestress.
“Inorder to continue to provide care to other people, we have to take care of ourselves. ...Wecannotburnthrough our bank of theamount of stresswecan endureinour life,”she said.“It’s so important right nowthatthose of us that arehereneedtobeable to stay hereas we getthroughthe end of this pandemic hopefully.”
Whennursesare reaching theirlimits, Weismuller said, all publicand private medical entities need to helpthemdevelop resilience.
She serves on theboard of the Califor niaAssn. of Colleges of Nursing, which preaches “resilience, reflectionand reimagination.”
“In order to develop resilience, we need atime to reflectonwhatwe’ve learned, what we coulddodifferently,and reimagine howwecan enhance our care forourselves and others,for thefuture,” Weismuller said.
NancySumner just celebrated her 45th anniversaryatthe DignityHealth Glendale Memorial Hospital and Health Center. She’saregistered nurse in the emergency room and aretiredcolonel in the U.S. Air National Guard, whereshe specialized in aeromedical evacuation.

What has helped Sumner cope through the various phases of the pandemic?
“I always sayAir Forcecorevalues which (are) integrity, servicebeforeself, and excellence—havebeen my mantra,” she said.
It reminds her,she said, to focus on what she candofor apatient and not allowherself to feel overwhelmed beforeexhausting other options or asking forhelp.
“You have to cope, getitdone and move on,”Sumner said.
Lately, Sumner’steamhas had to cope with anew challenge: political divisions entering the hospital room.
Sumner said afamilyrecentlydenied that ayoung patient whodied had been infected with COVID-19.Itwas frustrating to deal with familymemberswho were not vaccinated, refused to wear masksin the emergencyroom and yelled at nurses. The familyhas everyright to be angryafterthe death of aloved one, Sumner said. Butother peoplein the packed emergency room alsoneeded to be kept safe.
“Pre-COVID-19,nurses, front-liners,
youwererespected alittle bit more. Now alot of nursesdon’tfeel as respected. ... We do feel respected by our hospital and staff,” she said.
The other challengefor Sumner is that she doesn’ttalk about her experiences at work with her family,citing patient confidentialityand not wanting to scare them.
It’s not easy forthem to understand that she’staking precautions at work andfeels safe,becausefamilymembersare thinking onlyabout her exposuretothe virus.
But her adult children cantell when she’sespeciallytired or when Sumner mentions she “dealt with alot of COVID” that day.
Sumner’sadvice: She finds solacein the fact that she canremoveher scrubsat the end of her shift and changeintoclean clothes beforeleaving the hospital.
“It reallymade adifferencefor our staff becausetheyfelt theycan leaveeverything (from the day) behind,”she said.
especiallyfromexpecting or newmothers.
During the pandemic,expecting moth ershaveworried about possible exposure to the coronavirus when going to the hospital forprenatal care.Gomezsaidshe participated in alot of communityoutreach through public forums to educate the communityabout the safety protocols the hospital implemented.
The other challengein the prenatal unit wasthat families couldn’talwaysbe physicallypresent.
ABOVE: Noemi Gomez, a perinatal nursingsupervisor forEast LosAngeles Doctors Hospital in LosAngeles.

LEFT: Emergency DepartmentRegistered Nurse and retired California Air National GuardCol. NancySumner at Dignity Health-Glendale Memorial Hospital and Health Center in Glendale,Calif.
When she has adifficult day, Sumner will take alonger routehome. It givesher time to debrief,think about what she can do differentlyanother day.She alsolistens to calming music or ameditation app.Or sometimes she just yells in the car, which she finds cathartic.
On her days off,decompressing means playing with her grandchildren, taking them horseback riding, going on awalk or swimming.
Noemi Gomezisaregisterednurse,a certified lactation consultant and aperinatal nursing supervisor forEast LosAngeles DoctorsHospital. Gomezsaidshe continues to find her work emotionally fulfilling, despitethe challenges brought on by the pandemic.
She said East LosAngeles DoctorsHos pital caresfor an underserved community so the gratitudefrompatients is visible,
“Weprovide averyfamily-centered approach here, and having to limitthe number of visitorsthat could be at the bedside during that time wasachallenge. We had to be able to accommodatethe patient with the father of the baby or a designated support person throughout their hospital stay,while simultaneously keeping the other patientsand ourselves safe,” Gomezsaid.
Forpregnant women whotested positive forCOVID-19,a designated support personwasn’t able to be in the delivery room, so Gomezand other nursesin the unit were their support system.
“The role of the nurse as being also emotional support, Ithink, wa sjust so much moreenhanced during this pandemic becauseour pregnant mommies reallyneeded us.It’slikewebecame their second moms becausetheir mom wasn’t able to be with them and give them guidanceatthis moment of becoming anew mommy,”she said.
Gomez’sadvice: She said she always tries to find the positive.
“Ashardasthat might be sometimes, Itry to surround myself with people that areoptimistic,” she said.
That positivity, forGomez, canoften be found in nature. So she regularly hikes and jogs.
She equates it to finding alittle nor malcyin the midst of all the chaos.
NursesThe Times spoketowereunani mous: Saying asimple “thank you” goes a long wayfor health care workers.
Theyalsotalked about working together as acommunitytoend the pandemic by practicing hand hygiene, wearingamask and following local safety guidelines.
And Kaiser’sLeido emphasized vaccination.
“The best waythat youcan help and provide support to all of our front-line health care workers,all of our essential workers,istoget vaccinated,”Leido said.
For nearly everyindicator,the AmericanNursingAssociation says,America’snursesare lesshealthythan the average American.




They’re morelikelytobeoverweight, stressedout and tired. Workplaceviolence, injuries on the job and the 24/7 demands of the health care environment push manynursestothe breaking point.
TheU.S.BureauofLabor Statistics says that registered nurseshavethe fourthhighest rate of injuries and illnessesthat result in days away from work when comparedtoall other occupations.Yes,even lumberjacks.
To improvethe health of America’s 4million registered nurses, the ANA launched the HealthyNurse,HealthyNation movement five yearsago.Its mission is to nnect and engag ur nd orga
nizations to help nursesget more exercise, rest, nutrition, abetter qualityoflifeand be moresafeonthe job.It’s afreeprogram, open to everyone in the industry.Thereare more than 230,000 participantsand more than 580 partner organizations.
It wasparticularly vital during the CO VID-19 pandemic,which tried nurses’ health likenever before.



“Weencourageemployers,professional associations and schools of nursing to shareand amplifythe vital HNHN resourcesthathelpnurses combat burnout, manage stress and overcome trauma,”ANA PresidentErnest J. Grant, RN,FAAN,


said.“Together,wecan ensureour nurs ingworkforce is at itspeakhealth and wellness.”
One of the thingsthe programdoesisto matchnurseswithmentalhealthresources, offeringthings likea free subscription to HeadspacePLUSand other apps to im provethe mental healthand resilience of nurses across thecountry.It also organizes challengesfor nurses to participate in for
healthyeating, exerciseand more.

“Nurses’ physical and mental well-being have never been more important to the profession and to everyone of us who countsonnursesfor health care and leadership,”said KateJudge,executive director of the American NursesFoundation.


MatthewS.Howardisanurse whopar ticipates in the HNHN challenge. He said he walksthe dogand connectswith familyand friends regularly,evenvirtually, to improvehis well-being.

“A healthymental lifestyleissoimpor tant to me right now,”hesaid.
SonyaL.Clayton, another participant, said she carves out quiet time to help her mental health.
connect engage nurses and ‘Nurses’physicaland mental well-being have neverbeen more important’







“Atnight, Itry to have at least 30 minutes of quiet time reading or doing something calming,”she said.“Ialso talk to my prayer partner everyday,and that connection is so reassuring.”








