CONNECTING ALUMNI, FRIENDS AND COMMUNITY
JACOBS SCHOOL OF MEDICINE AND BIOMEDICAL SCIENCES UNIVERSITY AT BUFFALO













Dr. Timothy F. Murphy Scholar, leader, humanitarian, community connector

CONNECTING ALUMNI, FRIENDS AND COMMUNITY
JACOBS SCHOOL OF MEDICINE AND BIOMEDICAL SCIENCES UNIVERSITY AT BUFFALO













Dr. Timothy F. Murphy Scholar, leader, humanitarian, community connector
Dear friends,
Research has always been at the heart of the Jacobs School of Medicine and Biomedical Sciences, driving innovation in health care. In this edition of UB Medicine, we proudly highlight our researchers who are deeply committed to addressing health disparities.
Through groundbreaking research and collaborative partnerships, they are forging new connections between our school and the community, driving impactful change.
With a dynamic team of seasoned and emerging leaders, the Jacobs School is poised to redefine health care. Our vision is a future where everyone, regardless of background or location, has access to exceptional care.
I am incredibly proud of our Jacobs School faculty, whose extraordinary achievements have been recognized by esteemed institutions and the highest levels of academia.
Among these outstanding individuals is Timothy F. Murphy, MD, a SUNY Distinguished Professor and key leader in our Jacobs School. As senior associate dean for clinical and translational research and director of UB’s Clinical and Translational Science Institute, Dr. Murphy has significantly advanced our university’s mission. His visionary leadership has fostered a culture of innovation and collaboration, transforming the institute into a hub for cutting-edge research, attracting top-tier talent, and securing substantial funding. Dr. Murphy’s dedication and achievements have been recognized with the UB President’s Medal, honoring his exceptional scholarly achievement, humanitarian acts, generosity and exemplary leadership.

We are also thrilled to welcome several new chairs and key leaders to our team whose expertise and vision will further strengthen our mission.
While we celebrate these accomplishments, we also pause to honor the legacy of departing colleagues whose dedication has shaped our institution. Their mentorship and expertise will continue to inspire us.
As we look ahead, we remain steadfast in our commitment to fostering an inclusive environment where every perspective is valued. Together, we will advance medical research and education, making health equity a reality for all.
I hope you enjoy this edition of UB Medicine as we celebrate the remarkable work being done at the Jacobs School.
Warmest wishes,

Allison Brashear, MD, MBA Vice President for Health Sciences and Dean, Jacobs School of Medicine and Biomedical Sciences
UB Medicine is published by the Jacobs School of Medicine and Biomedical Sciences at UB to inform alumni, friends and community about the school’s pivotal role in medical education, research and advanced patient care in Buffalo, Western New York and beyond.
VISIT US: medicine.buffalo.edu/alumni
COVER IMAGE
Timothy F. Murphy, MD, champion for health equity, and 2024 recipient of the University at Buffalo President’s Medal.
Photo: Sandra Kicman
24 BUILDING MOMENTUM
UB, Jacobs School researchers fueling acceleration of community-focused movement addressing health disparities
26 MURPHY RECOGNIZED FOR CAREER ACHIEVEMENTS WITH PRESIDENT’S MEDAL
28 ART OF DIVERSITY
Larger-than-life mural reflects Jacobs School’s commitment to community, inclusivity
30 NIELSEN’S ROLE IN PASSAGE OF AFFORDABLE CARE ACT DOCUMENTED IN OBAMA PRESIDENCY ORAL HISTORY
One of the “extraordinary people” invited to tell the story of the 44th president

Decades of UB research have dramatic effect on the lives of patients with cystic fibrosis

ALLISON BRASHEAR, MD, MBA
Vice President for Health Sciences and Dean, Jacobs School of Medicine and Biomedical Sciences
Jeffry Comanici
Assistant Vice President for Principal Gifts, Executive Director of Advancement
Editor Patrick S. Broadwater
Contributing Writers
Dawn Cwierley
Ellen Goldbaum
Dirk Hoffman
Copyeditor Ann Whitcher Gentzke
Photography Sandra Kicman
Meredith Forrest Kulwicki Douglas Levere Nancy Parisi
Art Direction & Design Ellen Stay
Editorial Adviser
John J. Bodkin II, MD ’76
Affiliated Teaching Hospitals Erie County Medical Center
Roswell Park Comprehensive Cancer Center
Veterans Affairs Western New York Healthcare System
Kaleida Health Buffalo General Medical Center Gates Vascular Institute
John R. Oishei Children’s Hospital Millard Fillmore Suburban Hospital
Catholic Health Mercy Hospital of Buffalo Sisters of Charity Hospital
Correspondence, including requests to be added to or removed from the mailing list, should be sent to: Editor, UB Medicine, 955 Main Street, Buffalo, NY 14203; or email ubmedicine-news@buffalo.edu
A select collection of images from events happening at the Jacobs School over the past few months.

In recognition of Mental Health Awareness Month, SUNY Chancellor John B. King Jr. visited the Jacobs School on May 15 to join President Satish K. Tripathi, Dean Allison Brashear, MD, MBA, and others for a comprehensive discussion about mental health
All eyes were turned skyward— wearing the proper protective eyewear, of course—on April 8 for the once-in-a-lifetime solar eclipse. Buffalo was one of the locations in the path of totality. Hundreds of spectators gathered on South Campus to view the rare celestial event, which impressed despite cloudy skies. Photo: Douglas Levere.
resources for students. The discussion also addressed research to develop new therapies and outreach services for the community, made possible, in large part, through substantial New York State investment. Photo: Meredith Forrest Kulwicki.

A packed house was on hand in M&T Auditorium in November for a kickoff event celebrating the launch of the Future of Health report, a joint effort from the Jacobs School and the Jacobs Institute. The event featured nearly a dozen guest speakers discussing key takeaways from the groundbreaking report. A reception followed in the Jacobs School atrium. To learn more or get your free copy of the report, scan the QR code.

David A. Milling, MD, speaks as New York State Commissioner of Health James V. McDonald, MD, and Jacobs School Dean and Vice President for Health Sciences Allison Brashear, MD, MBA, look on during a press conference at the Jacobs School last December announcing $4.6 million in state funding to help increase diversity among the physician workforce in New York. Photo: Sandra Kicman.


A delegation from Uzbekistan’s Ministry of Health visited Buffalo in early February, stopping to visit several sites at the University at Buffalo as part of a tour of the U.S. to bolster the Asian country’s public health capabilities. After stops at UB’s Clinical and Translational Science Institute and the School of Public Health and Health Professions, the Uzbeki scientists learned about the Jacobs School’s medical curriculum and toured the Downtown Campus, including stopping at UBRISE2 Surgical Center, where they were photographed with Michael Rauh, MD, assistant professor of orthopaedics. Photo: Sandra Kicman.
The Jacobs School of Medicine and Biomedical Sciences recently added several new associate deans to its leadership team.
• Gustavo A. Arrizabalaga, PhD, joins the Jacobs School as senior associate dean for faculty affairs.
• Jennifer A. Surtees, PhD, professor of biochemistry, has been named associate dean for undergraduate education and STEM outreach.
• Kara M. Kelly, MD ’89, has been tabbed as associate dean for pediatric translational and population health research.
• Robert F. McCormack, MD, chair of the Department of Emergency Medicine, has been named associate dean for ambulatory strategy.
Arrizabalaga joins the Jacobs School from the Indiana University School of Medicine (IUSM), where he distinguished himself as a professor in the Departments of Pharmacology and Toxicology, and Microbiology and Immunology.
Arrizabalaga has served as the assistant dean for faculty affairs and professional development, assistant director of the independent investigator incubator and director of faculty mentoring at Indiana University.
research portfolio includes numerous peer-reviewed publications that have significantly advanced our understanding of parasitic diseases.
As senior associate dean for faculty affairs, Arrizabalaga oversees faculty recognition, career development and mentoring. He works closely with the dean and Jacobs School leadership to lead recruitment, appointments, promotions and tenure decisions. His strategic leadership will support faculty success and promote a diverse and inclusive academic environment.

Surtees has been a member of the Jacobs School faculty since 2007. She has served as co-director of the Genome, Environment and Microbiome (GEM) Community of Excellence at UB, which advances understanding of the genome and microbiome, and their interaction with the environment, through research, education, community programs and art.


He earned his PhD from the Massachusetts Institute of Technology, where he conducted pioneering research on the Drosophila protein nanos. He further honed his expertise during his postdoctoral fellowship at Stanford University School of Medicine, focusing on molecular and genetic studies of Toxoplasma gondii. His impressive
In her new role, Surtees provides oversight of and strategic vision for the Jacobs School’s undergraduate educational programs, provides strategic vision for K-12 STEM educational outreach and engagement in the Jacobs School, and initiates STEM-focused community outreach for adults.
An internationally recognized expert on genome stability and genetic diversity, Surtees has focused her research on the general problem of maintaining genome stability, which refers to an organism’s or cell’s ability to accurately transmit genetic material to a new generation.

As co-director of GEM, Surtees spearheaded genome and microbiome literacy programs in the community, particularly the city of Buffalo, through engaging events to promote conversation and hands-on inquiry-based activities, workshops and lessons for K-12 and adult populations.
For her work, she was honored with the Jacobs School’s Community Service Award for Excellence in Promoting Inclusion and Diversity.
In close collaboration with Roswell Park Comprehensive Cancer Center and UB’s research offices, Kelly focuses on overcoming barriers in research processes, fostering innovative research projects and strategically enhancing research expenditures at the Jacobs School. In addition to her vital role in expanding research training programs and developing initiatives to strengthen the clinical-translational workforce within the region, she facilitates faculty research by connecting them with local research cores, such as the UB Biorepository, and enhancing available services.
In her new role, Kelly’s leadership deepens UB’s research relationship with Roswell Park, where she occupies the Waldemar J. Kaminski Endowed Chair of Pediatrics and is a professor of oncology.
Kelly has extensive experience and recognized expertise as professor of pediatrics and chief of the department’s Division of Hematology/Oncology at the Jacobs School. She also serves as program director of pediatric hematology/oncology at Oishei Children’s Hospital.
In his new role, McCormack, a faculty member and leader at the Jacobs School for over 25 years, is spearheading a crucial transformation initiative: shaping the non-surgical ambulatory practice plans of UBMD Physicians’ Group into a cohesive, patient-centric unit designed to thrive in the evolving health care landscape.
This marks a significant step forward in the Jacobs School’s commitment to enhancing health care access and experience for Western New Yorkers. Working closely with UBMD leadership, clinical partners and university stakeholders, McCormack will create a shared vision and actionable strategies for non-surgical ambulatory care.
Beyond his current position as chair of the Department of Emergency Medicine and president of UBMD Emergency Medicine, McCormack boasts extensive clinical expertise in emergency medicine and a strong record of community leadership and partnership, recognized through numerous awards and honors.
McCormack’s research delves into crucial areas of emergency medicine, contributing to improved patient care and understanding of critical conditions.

HWI
Hauptman-Woodward Medical Research Institute (HWI) will join the University at Buffalo, a move designed to strengthen the two organizations’ joint mission to advance medical science research and education in Western New York and beyond.
With HWI joining UB, the long-standing partnership between the two institutions will be strengthened and will further the legacy of Nobel Prize winner Herbert A. Hauptman, who led HWI for decades while serving as a UB faculty member.
When the transaction is finalized, HWI will be known as the University at Buffalo Hauptman-Woodward Institute (UB-HWI).
UB will maintain HWI’s research center—700 Ellicott St., on the Buffalo Niagara Medical Campus—as a hub for medical science research, and will keep UB-HWI as the building’s anchor. The HWI building will be gifted to the university, subject to required approvals, so that the facility will continue to serve as a hub of scientific research and innovation.
The agreement will build upon HWI’s excellence in structural biology research while leveraging UB’s world-class strengths in drug discovery, artificial intelligence, computational chemistry and other fields.
“Honoring the initial philanthropy of Helen Woodward Rivas, continued by the Constantine family, as well as the many incredible scientific achievements of Dr. Herbert Hauptman and the many talented researchers that followed, past and present, is of paramount importance to our board of directors,” said HWI Board Chairman Sam Russo.
“As we explored possibilities with UB, we sensed clear alignment, and a unique opportunity emerged to meaningfully accelerate our collective research efforts by combining forces. With the entire combined UB-HWI team, we are excited by the potential to grow our impact on the Buffalo community and the world,” he added.
UB President Satish K. Tripathi said that “with UB’s and HWI’s shared mission of research, education and community engagement, the university is very excited to welcome the members of the HWI community into the UB community.”
HWI was founded in 1956 as the Medical Foundation of Buffalo by Woodward Rivas and George Koepf, a Buffalo physician who believed basic research was critical to improving human health. It is believed to be the oldest independent nonprofit

medical research institute in the nation that is dedicated to understanding and curing disease.
In 1985, Hauptman and Jerome Karle received the Nobel Prize in Chemistry for discovering new methods to visualize pharmaceuticals and proteins, and how they interact. These techniques have been adopted worldwide in the development of pharmaceuticals. In recognition of Hauptman’s achievement and to honor Woodward Rivas, the foundation was renamed the Hauptman-Woodward Medical Research Institute in 1994.
Today, HWI researchers continue to make critical advancements in structural biology, studying, among other things, the structures of the body’s proteins. This enables HWI scientists—many of whom have appointments at UB—to see what proteins look like when functioning properly, and what they look like in cancer, cardiovascular disease and other diseased states. The work has applications in medicine, biotechnology, agriculture and other fields.
“With the entire combined UB-HWI team, we are excited by the potential to grow our impact on the Buffalo community and the world.”
-Sam Russo, HWI Board Chairman
Pairing the two organizations will spur cutting-edge research and innovation, officials say. For example, UB is home to Empire AI, Gov. Kathy Hochul’s $400 million artificial intelligence consortium. UB will partner with colleagues in UBHWI to explore how AI can advance their understanding of diseases and potential treatments.
Additionally, UB envisions the new UB-HWI facility as a hub for community outreach and other programs designed to build interest in science, health and well-being.
Left: Hauptman-Woodward Medical Research Institute will join UB, the two groups announced at a press conference in May 2024 at the Center of Excellence in Bioinformatics and Life Sciences. From left: Christopher Greene, HWI interim CEO; Provost A. Scott Weber; Connie Constantine, emeritus HWI board chair; President Satish K. Tripathi; and Sam Russo, HWI board chair. Photo: Meredith Forrest Kulwicki.
JAMA Paper: Telemedicine Treatment Twice as Successful as Off-Site Referral for Vulnerable Populations
People with opioid use disorder who have hepatitis C virus (HCV) were twice as likely to be successfully treated and cured from HCV if they received facilitated telemedicine treatment at their opioid treatment program (OTP) than if they were referred off-site to another provider, according to findings published by a University at Buffalo team of researchers in the Journal of the American Medical Association (JAMA).
The study is one of only a few randomized controlled trials that have been conducted to determine the effectiveness of using telemedicine to improve health care access for vulnerable populations.
Led by Andrew H. Talal, MD, MPH, professor of medicine in the Jacobs School, this study explored the effectiveness of integrating telemedicine into OTPs for HCV management, thereby removing the need for off-site referrals.
The study was conducted from 2017 to 2022 at 12 OTPs in New York State that dispense methadone. Researchers enrolled 602 participants with opioid use disorder who had been diagnosed with HCV. Participants received treatment with direct acting antiviral medications for HCV and were followed for two years after being cured to evaluate for reinfection.
The researchers found that 90.3% of those in the telemedicine arm at an OTP were cured of HCV infection compared to 39.4% of participants referred to an off-site specialist. Two-thirds of those in the referral arm never initiated HCV treatment at all.
The researchers also found that being cured of HCV resulted in subsequent health and well-being improvements for participants, including significant reductions in substance use.
“Our study demonstrates how telemedicine successfully integrates medical and behavioral treatment,” Talal said.

The National Cancer Institute has awarded a five-year, $3 million grant to Remi M. Adelaiye-Ogala, PhD, assistant professor of medicine, to continue studying mechanistic determinants of therapeutic resistance in advanced prostate cancers.
Most prostate cancer deaths occur in men with advanced prostate cancer that has become resistant to current treatments, including androgen receptor (AR)-targeted therapies, according to Adelaiye-Ogala.
“The glucocorticoid receptor (GR) has emerged as a focus for developing inhibitors/modulators that block its activity by competitively binding to its hormone-binding site,” she said. “However, GR can also be activated through mechanisms independent of this site.”
Adelaiye-Ogala said her study aims to understand these alternative activation pathways, specifically focusing on how posttranslationalmodifications activate GR as an oncogene in advanced prostate cancer.
“Our research will help create precise and effective treatments for this subpopulation of patients that are safe and improve outcomes for men with high-risk, advanced prostate cancer.”
To address the increasingly urgent needs of the growing population of adults aged 65 years and older, UB is dedicating $4 million to aging-related research.
The investment will leverage the university’s wide-ranging expertise in age-related issues and research throughout its 12 academic units. It will allow UB to expand and enrich educational programming, enhance faculty recruitment, and strengthen multidisciplinary research collaborations with the goal of generating solutions that address the physiological and societal elements of aging.
The new initiative will dedicate resources toward bolstering these efforts, while also supporting the recruitment of new faculty who are focused on novel approaches to aging-related challenges.
“As a city that is home to minority and aging populations growing more rapidly than in other U.S. regions, Buffalo is uniquely positioned to be the place where innovations targeted to these communities should be developed and implemented,” said Allison Brashear, MD, MBA, dean of the Jacobs School and vice president for health sciences. “This new focus will allow UB to more powerfully leverage its scholarship and innovation to address the increasingly complex needs of our region’s aging population.”
New research published in Nature Neuroscience reveals how memory works on a cellular level, findings that are critical to the understanding and treatment of memory disorders, such as Alzheimer’s disease.
The research focuses on engrams, which are neuronal cells in the brain that store memory information. “Engrams are the neurons that are reactivated to support memory recall,” said Dheeraj S. Roy, PhD, one of the paper’s senior authors and an assistant professor in the Department of Physiology and Biophysics. “When engrams are disrupted, you get amnesia.”
In the minutes and hours that immediately follow an experience, he explains, the brain needs to consolidate the engram to store it.

Remi Adelaiye-Ogala was awarded a $3 million grant to study mechanistic determinants of therapeutic resistance in advanced prostate cancers.
The researchers developed a computational model for learning and memory formation that starts with sensory information, which is the stimulus. Once that information gets to the hippocampus, the part of the brain where memories form, different neurons are activated.
When neurons are activated in the hippocampus, not all are going to be firing at once. As memories form, neurons that happen to be activated closely in time become a part of the engram and strengthen their connectivity to support future recall.
“This research tells us that a very likely candidate for why memory dysfunction occurs is that there is something wrong with the early window after memory formation where engrams must be changing,” said Roy.
Physicians have hesitated to prescribe GLP-1RA medications, such as those with brand names of Ozempic and Victoza, to patients with a history of pancreatitis because it was believed that they could increase the risk of acute pancreatitis.
Now, researchers from the Jacobs School report that their research has found that these medications don’t put these patients at increased risk for pancreatitis, and the drugs may actually lower their risk.
The work was presented June 1 at ENDO 2024 in Boston.
“Our clinic often sees patients with a history of pancreatitis who could benefit from GLP-1RA treatments,” said Mahmoud Nassar, MD, PhD, a fellow in the Division of Endocrinology, Diabetes and Metabolism in the Department of Medicine at the Jacobs School.
“GLP-1RA drugs work through a mechanism that not only controls diabetes and aids in weight loss but also has antiinflammatory properties, which likely contributed to the reduced risk,” Nassar explained. “Our research offers good news for patients with a history of pancreatitis. They can now use GLP-1RA drugs to effectively manage Type 2 diabetes and obesity without an increased risk of pancreatitis, expanding their treatment options.”
Stem cell therapy to treat diseases such as multiple sclerosis often has disappointing results because the transplanted cells die off before they can take effect. In fact, more than 95% of neural progenitor cells (NPCs) transplanted into individuals with a spinal cord injury die following injection. This is partly because the
process of injecting the cells can damage them.
Two University at Buffalo researchers are working on a possible solution: injecting shear-thinning hydrogels (STH) into the brain, which protect the cells and result in more successful therapy.
Stelios Andreadis, PhD, SUNY Distinguished Professor of chemical and biological engineering, and biomedical engineering, and Fraser J. Sim, PhD, professor of pharmacology and toxicology and director of UB’s Neuroscience Program, were recently awarded a $2.9 million, five-year grant from the National Institute of Neurological Disorders and Stroke to further investigate this technology.
“STHs have emerged as promising candidates for the injection of Schwann cells and oligodendrocytes, the cells that form the myelin sheath in the brain and spinal cord,” said Andreadis, who also directs UB’s Cell, Gene and Tissue Engineering Center (CGTE), of which Sim is a member.
“The work we plan to undertake has significant implications for regenerative medicine, as it has the potential to develop novel strategies to enhance stem cell delivery for treatment of devastating neurological diseases that remain intractable to current treatments.”
Stem Cell Study Reveals How Infantile Cystinosis Causes Kidney Failure—and How to Potentially Cure It
University at Buffalo research has identified how a misstep in the genesis of a key component of the kidney causes infantile cystinosis, a rare disease that significantly shortens the lifespan of patients.
Published Nov. 30 in the International Journal of Molecular Sciences, the work reveals that the mechanisms that cause the disease could be addressed and potentially cured through the genome-editing technique CRISPR. That could make kidney transplants, the most effective treatment currently available for these patients, unnecessary.
Infantile cystinosis, the most common and most severe type of cystinosis, occurs as the result of an accumulation in the body’s cells of cystine, an amino acid. The buildup damages cells throughout the body, especially the kidneys and the eyes.
Human-induced pluripotent stem cells (hiPSCs) are stem cells that can differentiate into many different cell types. They hold tremendous potential for studying genetic diseases; the drawback has been that differentiation into certain cell types has been problematic. Such is the case with many cell types found in the kidney.
But a new protocol developed by this research team was successful.
“When our normal human-induced pluripotent stem cells were subjected to the differentiation protocol we developed, we were able to demonstrate extensive expression of physiologically important markers of the renal proximal tubule, the specific nephron segment that is altered in this disease,” said Mary L. Taub, PhD, senior author on the paper and professor of biochemistry.
The protocol involved extracting stem cells from a healthy individual and an individual with infantile cystinosis. The researchers developed a culture medium to grow stem cells that included a small number of defined components present in blood, including insulin, specific proteins, growth factors and others. That finding means that the CRISPR genome-editing technique could be used to repair the defective genome and potentially cure the disease.
Allison Brashear, MD, MBA, vice president for health sciences at the University at Buffalo and dean of the Jacobs School of Medicine and Biomedical Sciences at UB, has been appointed to the board of directors of the Association of American Medical Colleges (AAMC).
One of 19 board members, most of whom are deans of the nation’s leading medical schools, Brashear will serve from November 2024 to November 2025.
The AAMC represents the nation’s medical schools and teaching hospitals and is dedicated to transforming health care through innovative medical education, cutting-edge patient care and groundbreaking medical research.
“UB is proud that Dr. Brashear has been named to the board of directors of the AAMC. This appointment recognizes her national reputation as an academic health leader, as well as her excellence as a medical researcher and educator,” said A. Scott Weber, PhD, provost and executive vice president for academic affairs at UB.
Brashear was elected to the AAMC Council of Deans in 2022 and assumes the role of chair-elect in the fall of 2024. She was an AAMC Council of Deans Fellow for 2014-15.
A powerful advocate for promoting diverse leaders in medicine, Brashear was instrumental in creating one of the first national leadership programs in neurology for women. She is a frequent lecturer on the importance of diversity in medicine, and a lifelong champion of advancing women’s leadership in medicine.

Several Jacobs School faculty members received recognition from national, state and university organizations. Among them:
Liise K. Kayler, MD, clinical professor of surgery, and Michal K. Stachowiak, PhD, professor of pathology and anatomical sciences, were recipients of 2024 SUNY Chancellor’s Awards for Excellence.
The Chancellor’s Award for Excellence in Scholarship and Creative Activities recognizes the work of those who engage actively in scholarly and creative pursuits beyond their teaching responsibilities.
An advocate for diversity, equity and inclusion in health care and combating structural racism, Kayler co-founded and is president of the New York Center for Kidney Transplantation, a statewide collaborative to improve access to kidney transplantation, and serves on the board of directors of the Kidney Foundation of WNY.
Stachowiak is regarded as one of the world’s leading researchers on fibroblast growth factor signaling and, more broadly, as a firmly established leader in the neuroscience community. Stachowiak has made several seminal discoveries and developed innovative concepts to significantly influence our perception of the genome—its function, structure and regulation.
Amit Kandel, MD, MBA, associate professor of neurology, has been honored by the American Academy of Neurology (AAN) with its 2024 Clerkship Director Innovation Award.
The award recognizes individuals who have developed unique tools to teach medical students, assess knowledge and benchmark progress.
Kandel, who directed the clerkship in the Department of Neurology from 2019 to 2023, was honored in part for his use of facilities in the school’s Behling Human Simulation Center.
Four Jacobs School faculty
members have been named SUNY Distinguished Professors, the highest faculty rank in the SUNY system.
Appointed to the distinguished professor ranks by the SUNY Board of Trustees at its meeting on April 16 were:
• Ralph H.B. Benedict, PhD, professor of neurology
• Michael E. Duffey, PhD, professor of physiology and biophysics, and medicine
• Jeffrey M. Lackner, PsyD, professor of medicine and chief of the Division of Behavioral Medicine
• Sanjay Sethi, MD, professor of medicine and chief of the Division of Pulmonary, Critical Care and Sleep Medicine
The rank of distinguished professor is an order above full professorship and has three co-equal designations: distinguished professor, distinguished service professor and distinguished teaching professor. Duffey was named a Distinguished Teaching Professor; Benedict, Lackner and Sethi were named Distinguished Professors.
Benedict is a pioneer in the understanding of cognitive disorders, and the treatment of people with multiple sclerosis (MS). He is one of the top investigators worldwide in standardized neuropsychological testing and quantitative brain imaging used in assessing cognitive dysfunction in MS and other neurological diseases.
Duffey has demonstrated excellence in teaching, curricular development, student mentoring and academic scholarship. He co-founded the interdisciplinary graduate program in biomedical sciences, a revolutionary umbrella curriculum that unified six graduate basic science programs and has served as a model for other institutions.
Lackner is an international expert in the field of cognitive behavior therapy (CBT) for the treatment of gastrointestinal and chronic pain disorders such as irritable bowel syndrome (IBS). His work on nonpharmacological approaches to chronic
pain has dramatically changed clinical practice guidelines in the U.S., Europe and Asia.
Sethi, assistant vice president for health sciences, is an internationally regarded pulmonologist with a primary clinical and research interest in chronic obstructive pulmonary disease (COPD), the third leading cause of death worldwide.
Gabriela K. Popescu, PhD, and Thomas A. Russo, MD, have been elected Fellows of the American Association for the Advancement of Science (AAAS), which is the world’s largest general scientific society and publisher of the journal Science. Popescu is a professor of biochemistry in the Jacobs School. Her research centers around NMDA receptors, which produce electrical currents that are essential for cognition, learning and memory. Her current eight-year research grant from the National Institutes of Health focuses on the excess activation of these receptors, which can cause pathological cellular loss in stroke, brain and spinal cord diseases, including Alzheimer’s and Parkinson’s disease.
Russo, SUNY Distinguished Professor in the Department of Medicine and chief of its Division of Infectious Diseases, is an expert in infectious diseases. He conducts research on gram-negative bacterial infections, antibiotic-resistant infections and works on developing targeted vaccines and drugs.
Anne B. Curtis, MD, SUNY Distinguished Professor of medicine, is recipient of the 2024 Dr. Carolyn McCue Award for Woman Cardiologist of the Year. Curtis was presented with the award at the Heart Health in Women Symposium on Feb. 3.
A Jacobs School faculty member since 2010, Curtis is both a clinician, caring for patients at UBMD Internal Medicine, and a Jacobs School researcher, specializing in clinical cardiac electrophysiology, the field of cardiology that studies, diagnoses and treats disorders of the electrical activity of the heart. She was the Charles & Mary Bauer Chair of the Department of Medicine in the Jacobs School from 2010 to 2022.
Leslie J. Bisson, MD, the Buffalo Bills medical director and the June A. and Eugene R. Mindell, MD, Professor and Chair of the Department of Orthopaedics at the University at Buffalo, has received the top research award from the NFL Physicians Society (NFLPS).
Bisson was awarded the Arthur C. Rettig Award for Academic Excellence at the NFLPS Scientific Meeting in Indianapolis, where he presented “How to Leverage an Athletic Training Outreach Program to Deliver Hands-Only CPR Training in Underserved Communities.”
Last October, the Mother Cabrini Health Foundation awarded Bisson a $300,000 grant to address barriers to bystander
cardiopulmonary resuscitation/automated external defibrillator (CPR/AED) training in underserved communities in Buffalo. The aim was to train 60 providers as AHAcertified CPR instructors, and to train 8,000 Western New York student-athletes and their families in hands-only CPR/AED use. In the first 12 months of the program, Bisson and his partners have trained more than 12,000 athletes, their families and members of underserved communities.
Margarita L. Dubocovich, PhD, has been honored by the Association for Clinical and Translational Science (ACTS) as the 2024 recipient of its Award for Contributing to the Diversity and Inclusiveness of the Translational Workforce.
Dubocovich, a SUNY Distinguished Professor of pharmacology and toxicology, received the award April 3 at Translational Science 2024, the annual meeting of ACTS, in Las Vegas.
The ACTS Award for Contributing to the Diversity and Inclusiveness of the Translational Workforce recognizes individuals who, through their careers of mentoring, policymaking or team building, have contributed to a more inclusive and diverse workforce.
Because of her tireless focus on and success in increasing diversity and inclusion in STEM, Dubocovich was named the Jacobs School’s inaugural senior associate dean for diversity and inclusion in 2012, becoming the first diversity officer at UB.
Jeffry Comanici has joined the Jacobs School as the new assistant vice president for principal gifts and executive director of advancement.
Comanici brings a wealth of experience and a deep commitment to fostering academic excellence and community engagement to his role at the Jacobs School. He most recently served as the executive director of post-traditional advancement at Syracuse University. In that capacity, he developed and implemented strategies to engage post-traditional alumni, resulting in significant increases in alumni support and engagement.
He is an active Syracuse University alumnus, having graduated from the Martin J. Whitman School of Management
with a Bachelor of Science in marketing and finance. He also holds a Master of Public Administration from the Maxwell School of Citizenship and Public Affairs. His career at Syracuse University included roles as assistant dean for advancement at the College of Visual and Performing Arts and chief development officer and leadership positions within the School of Information Studies.
Beyond academia, Comanici has made a significant impact in Central New York. He served as president and executive director of the Syracuse Symphony Orchestra and played a pivotal role in designing and managing a comprehensive principal/ planned/major gift program at the Crouse Health Foundation.

On a dramatic day, surrounded by friends and family, 169 Jacobs School medical students found out where they’ll be heading next in their quest to be a doctor. Precisely at noon on March 15—in synch with thousands of their peers across the country— UB students opened their white envelopes to reveal where they will train in residency.

Jelyn Cruz Eustaquio matched with Brown University for a residency in anesthesiology with a first-year internship in Buffalo.
For Jelyn Cruz Eustaquio, Match Day was like a dream.
The Philippines native matched with Brown University for a residency in anesthesiology with a first-year internship in Buffalo.
That was the ideal scenario for Eustaquio, engaged to an endodontist, whose Western New York contract expires next year.
“Next year, we will go to Rhode Island together,” she said. “I matched in the advanced program, so my first year at UB and my last three years will be at Brown.
“It’s like a dream come true to go to an Ivy League school, but it was also a dream come true for me to go to a SUNY school for medical school. This is the best that I could

have hoped for.”
Eustaquio’s unique journey into medicine began well after she moved to the United States as an 18-year-old. After witnessing health scares affecting her mother and sister, she was inspired by the doctors who provided their care to change careers and pursue a degree in medicine.
She eventually ended up at the Jacobs School, where she felt she could receive personalized attention and mentorship. She credits that guidance with helping her land a competitive Tylenol Care Future Scholarship in 2021, one of only 10 health professions students nationwide to win the top $10,000 prize.
“When I interviewed at UB, I was amazed by the building—it was brand new at that time—but it was really the people I met on the interviews that guided me here. I have no regrets. I am so happy I ended up here because it has gotten me where I wanted to be.
“When I moved here, I had no idea I would end up on this journey. I’m going to be the first person in my family to be a doctor, and this is really huge for me. The barriers, the challenges, when I look back, those pushed me to where I am. But I think it’s the people along the way that really got me where I am—being inspired by the people around me and a lot of the exposures that I had.”
Eustaquio, who lived for a time in Connecticut, is excited to head back to New England for her residency at Brown. But she’s also thankful for the opportunity to
spend another year in Buffalo.
“I’m so grateful I’m going to end up working with people I already know at UB for the first year. I think it’s going to be an easier transition into residency, knowing that I’m familiar with the rotation and the people.”
The only hiccup in Eustaquio’s day was a brief moment when she wasn’t able to get her envelope open.
“I couldn’t rip the envelope, and I realized I don’t know how to use a letter opener,” she joked. “At that moment, I just closed my eyes, and I could feel my heart pumping. I was scared, but I couldn’t wait any longer to see where I was going.”
After tearing into the envelope, she got a good look into what was in store for her in the future while taking a moment to consider where she has been.
“Everyone in this room felt the same way—you work so hard for the past four years, this is a testament to all the work we’ve put in. I’m really proud of everyone here. It’s an amazing feeling. I know it will be hard—residency will be hard—but it’s a new chapter, and every story has a positive and a negative. This is a moment of the positive. You have to celebrate it.”
For a full list of matches and photo gallery from the 2024 Match Day event at the Powerhouse in South Buffalo, visit https://bit.ly/3LNRjGc

David A. Milling, executive director of the Office of Medical Education and senior associate dean for medical education, announced each of the students in attendance, then led a 10-second countdown to the moment students could find out their matches.
“Today, dreams are realized, futures are shaped, and the culmination of years of hard work and dedication is celebrated,” said Allison Brashear, MD, MBA, UB’s vice president for health sciences and dean of the Jacobs School of Medicine and Biomedical Sciences, in her welcome address to the crowd of students, family, faculty and friends.
“Your potential knows no bounds, and we cannot wait to see what the future holds for each of you.”
The Jacobs School continued its strong tradition of retaining graduates to stay in Buffalo for their advanced training
In all, 27 percent of the class—45 students—have chosen to stay at the Jacobs School for their residencies.
“We see this as a testament to their dedication to our community, the City of Good Neighbors, and their dedication to contributing to our robust health care systems,” Brashear said.
“By continuing their training in Western New York, these future physicians directly contribute to improving health care access and addressing gaps in care delivery, especially for underserved communities.”
Among the specialties that have the most matches from the UB class are: internal medicine (seven), psychiatry (five), family medicine (four), internal medicine - prelim (four), pediatrics (four) and med-peds (three).
This year’s class included two MD/PhD, one MD/MBA, one MD/MPH and two MD/ OMFS dual-degree students.
Alyssa Reese matched into a plastic surgery residency at Eastern Virginia Medical Center in Norfolk.
“I’m really excited, I’m really lucky to match into such a competitive specialty,” she said.
Asked about how she feels about heading to Virginia, the Rochester native who also earned her undergrad degree at UB said she’s looking forward to it. She did a rotation in Virginia and is happy to be headed back there.
“It’s been a wild ride, a rollercoaster, a lot of ups, a lot of downs, but it was all worth it in the end,” said Kelsey Gibson, who matched with her first choice, pediatrics at New York Presbyterian Hospital. “I’m here with my family and my best friends, so to come together and to have such an amazing outcome, it was worth the whole journey.”
Shelley Verma matched into a primary care track in medicine at Strong Memorial Hospital at the University of Rochester.
The Syracuse native said she was elated to be moving a bit closer to home. She is also proud to be pursuing primary care.
“I want to develop better skills to prevent disease in my patients,” Verma said.
Jake Zipp, a Williamsville native, attended UB as an undergrad, enrolled in the Jacobs School for medical school, and is one of three generalist scholars who will be doing their residency in family medicine at UB.
“Doing the General Scholars program, I kind of knew I was coming here, so I was not as nervous as everybody else, but still opening the letter is a cool experience,” he said. “I’m really glad to be staying here. I love the city. I don’t see any reason to leave.”

“It’s been a wild ride, a rollercoaster, a lot of ups, a lot of downs, but it was all worth it in the end.”
-Kelsey Gibson, 2024 Jacobs School medical school graduate

John Ciarletta and Kirsten Frauens met during the first year of medical school and planned to marry a week after graduating from UB.
Engaged couple Kirsten Frauens and John Ciarletta each matched at Strong Memorial Hospital at the University of Rochester.
Frauens, a Rochester native, matched in physical medicine, while Ciarletta, originally from Long Island, matched in neurology.
“We’re going together, so I am good with that,” said Ciarletta. “I’m just very grateful for all the people that help you get to this point. It’s definitely a big milestone, and it’s a mix of excitement and fear of the unknown, but at the end of the day you just have to be grateful for how you got here and all the people that helped you.”
The couple met as first-year medical students and have been inseparable ever since. They planned to get married a week after graduating from UB.
“Neither of us thought we were going to end up in Buffalo for med school, but we did,” Frauens said. “We met each other early on and ended up getting engaged, and now we’re getting married. Everything worked out.”
“Coming to UB was the best decision I ever made,” Ciarletta said. “It was lifechanging for the better.”
Medical School Commencement
Friday, April 26, 2024
3 p.m., Center for the Arts
The Jacobs School of Medicine and Biomedical Sciences graduated 169 medical students during its 178th commencement.
Six students earned dual degrees, including two MD/PhD graduates; one MD/MBA graduate; two MD/oral and maxillofacial surgery graduates; and one MD/MPH graduate.

The Class of 2024 entered medical school at the height of the COVID pandemic, which further strengthened the bonds between classmates, said class speaker Susan Maureen Eichhorn.
“Over these last four years, I have seen people go from strangers to peers to family. We not only worked and studied together, but we watched each other grow into the mature, confident people you see in front of you today.
“We have struggled together, we have persevered together, and more importantly, we have achieved together. This is a success that deserves to be magnified.”
Eichhorn then encouraged her classmates to look ahead to the next chapter.
“As you embark on this phase of your journey, I hope you continue to push the boundaries of what is possible and never lose sight of your capacity to change patients’ lives.”
James V. McDonald, MD, New York State commissioner of health, was the keynote speaker, and James S. Marks, MD ’73, PhD, was awarded a SUNY Honorary Doctoral Degree in Science.
McDonald’s diverse career includes serving as an officer in the U.S. Navy, as well as private practice in rural areas where health care shortages existed. Prior to becoming New York State commissioner in 2022, he served at the Rhode Island Department of Health for 10 years.
He told the graduates that the word “resilience” comes to mind when he thinks of them.
“You started medical school during a pandemic, when there was no vaccine and no treatment. It was a time of uncertainty like had never been seen in this country,” McDonald said. “Resilience has been important to me because medicine is a career full of challenges. It was never on

my bingo card for life to be the physician for 20 million people, but taking care of a large group of people is a privilege.”
Marks is the former executive vice president of the Robert Wood Johnson Foundation (RWJF) and an elected member of the National Academy of Medicine.
A pioneer in public health and health equity, and a global leader in child and maternal health, health promotion and chronic disease prevention, he has dedicated his career to reducing health disparities and improving access to quality health care.
Before joining the RWJF, Marks held important leadership roles in public health, including serving as assistant surgeon general and director of the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
In 2018, Marks and his wife, Judi, BA ’69, MEd ’72, created the James and Judith Marks Family Scholarship Fund, which provides financial support to students in the Jacobs School.
Marks said receiving the honorary degree is special because UB is where he earned his medical degree more than 50 years ago. He said his father and grandfather also earned their degrees at UB and his wife earned her Bachelor of Arts and master’s in education in school counseling degrees from UB.
Marks asked rhetorically what does one hope to gain from a college?
“A sense of connectedness and community with students and faculty,” he answered. “My wife and I got that here, and that is why this recognition is all the more meaningful.”

Biomedical Sciences Commencement
Sunday, May 19, 2024
9 a.m., Center for the Arts
Thirty-five doctoral, 76 master’s and 209 baccalaureate candidates received degrees in biomedical science fields during the May commencement ceremony. Fifteen of the doctoral degrees and eight of the master’s degrees were awarded to students in the Roswell Park Graduate Division.
Four Jacobs School graduates received a Chancellor’s Award, the highest State University of New York undergraduate honor:
• Sarah Bukhari, a biochemistry major, who was an undergraduate researcher in the lab of Jennifer A. Surtees, PhD, professor of biochemistry. Bukhari secured funding from the Experiential Learning Network and was deeply involved in community engagement, serving as both the volunteer coordinator and vice president of the largest student-run prehealth organization, the Association of Pre-Medical Students.
where she earned the 2023 Inspire Spotlight Award.
Among the outstanding graduate students recognized, doctoral graduate Haley Victoria Hobble was honored with the Biochemistry Graduate Student Research Achievement Award and the Dean’s Award for Outstanding Dissertation Research.
Commencement speaker Styliani-Anna “Stella” E. Tsirka, PhD, the Miriam and David Donoho Distinguished Professor of pharmacological sciences and vice dean for faculty affairs at the Renaissance School of Medicine at Stony Brook University, spoke about empathy and persistence.

“Beyond the technical skills and academic achievements that you have earned and will continue to earn, what will set you apart is your capacity for empathy, for compassion, your ethical responsibility,” she said. “In the pursuit of scientific advancement, try not to lose sight of the human element and the living organisms whose lives may be impacted by our work.”


• Lea Kyle, a biochemistry major with minors in physics and public health, was a University Honors College Scholar. She was the president of UB Rotaract, a volunteering club on campus, and was also a student researcher in the Department of Microbiology and Immunology, focusing on the effects of chronic inflammation on muscle function due to chronic infection.
• Bryan Renzoni was a biochemistry major, a University Honors College Presidential Scholar and Honors College Ambassador. As a BioXFEL Scholar, he has received multiple research internship positions and worked in two different laboratories, contributing to work on the development of novel organic and organometallic compounds with applications as cancer therapies.
• Rachel Esther Sanyu, an international student from Uganda, majored in pharmacology and toxicology. She was an Honors College Scholar who conducted oncology research within the lab of Wendy Huss, PhD, at Roswell Park Comprehensive Cancer Center and at Johnson & Johnson,
Above: Styliani-Anna”Stella” Tsirka, of Stony Brook University, gave the keynote address at the Biomedical Sciences commencement.


Associate professor of sociology at the University of Tennessee, Knoxville, Deadric T. Williams, PhD, was the keynote speaker for the fourth edition of the University at Buffalo’s “Beyond the Knife” endowed lecture series established by the Department of Surgery in the Jacobs School of Medicine and Biomedical Sciences.
The title of Williams’ talk was “Structural Anti-Blackness and the Persistent Racial Inequality.”
Williams noted there is a tendency for people to think that racism is an individual-level attribute whereby you have to be intentional to be racist. But intentionality is not a necessary condition for the maintenance of white supremacy and anti-Black racism, he said.
“It is sufficient, but not necessary, especially when we think about this thing called racial disparities in health,”
Last September, approximately 300 community members along with UB students, faculty and staff gathered for the sixth annual “Igniting Hope” conference. The gathering has matured into what organizers describe as a movement aimed at bringing lasting change to the region by ending race-based disparities and their devastating impacts on the health of Black people, Hispanic people and other underrepresented groups.

Williams said. African Americans are more likely to die at earlier ages, he said, noting that maternal mortality and infant mortality rates, in particular, vary across racial lines.
“The debate often emerges when we start talking about why they exist and why they persist,” Williams said.
Deadric Williams, associate professor of sociology at the University of Tennessee, Knoxville, delivered the Beyond the Knife lecture in M&T Auditorium on Feb. 22.
“Racism is an ongoing feature in the U.S. It is not episodic. Policies and laws are responsible for racial inequality.
“Instead of asking for what accounts for racial disparities in health, I argue we should be asking what are the mechanisms that maintain racial disparities in health,” he said. “When we answer that question we can understand its genesis, how it ends, and becomes recreated and then we can start highlighting the mechanisms, not to account for the gap in health, but what maintains it. And if we can answer the question of what maintains it, then we can find ways to end it.”
“The system was created before any of us were ever born,” he said. “Remember, racial inequality is America’s equilibrium. So anytime there is a social movement (Civil Rights Movement, Black Lives Matter) fighting against the system, it corrects itself because it does not know how to do anything else.”
Williams also talked about how stress gets under the skin to affect health disparities—noting how our brains interpret stressors in a particular way, based on past experiences.
“Our bodies are equipped to deal with acute stress, but are not equipped to deal with chronic stress,” he said.
Williams said the country’s racial disparities are so prevalent and so normative, that it has created a political and racial divide.
“As we move forward, we need to think about racial inequalities as a failure of human rights, period,” he said. “It is not just differences in some outcomes. It is a violation of human rights.”
A central part of the discussion at the conference delved into issues at the core of medical research, such as informed consent and medical mistrust. Moderated by Jamal B. Williams, PhD, assistant professor of psychiatry in the Jacobs School, the session featured David Lacks and Veronica Robinson, the grandson and great-granddaughter, respectively, of Henrietta Lacks.
Lacks was the young, African American mother whose cancerous cell tissue has become, since her untimely death in 1951, one of the most important medical research tools ever discovered. Without her knowledge or consent, tissue was removed during a biopsy she underwent at Johns Hopkins Medicine and shared with the hospital’s tissue lab.
Unlike all other cells, hers (now named HeLa cells after her) didn’t die in the lab. Instead, they rapidly divided over and over, a phenomenon that to this day remains a unique medical mystery. HeLa cells have played a key role in the development of major medical advances, from new cancer treatments to the invention of vaccines that protect against polio and COVID-19 to in vitro fertilization.
Today, Lacks family members are active in the National Institutes of Health’s HeLa Genome Committee, but for decades they had no idea of the extraordinary role Henrietta played in modern medicine. Neither she nor her family was ever given the opportunity to provide informed consent. Only after a tenacious science writer named Rebecca Skloot started researching the story, which eventually became “The Immortal Life of Henrietta Lacks,”

did the family learn about their ancestor’s incredible legacy.
“The Henrietta Lacks story is a story of science at its best and at its worst,” said Williams.
The Jacobs School of Medicine and Biomedical Sciences welcomed the 2024 Can-Am Clinical Anesthesia Conference to Buffalo in May, marking the first time the international event was held on the American side of the border.
Founded by McMaster University in Hamilton, Ontario, Canada, in 1983, the conference brings together leaders in anesthesia from Canada and the United States to share cutting-edge advancements, foster collaboration and inspire transformative change.
The University at Buffalo traditionally participated in the event

Stacey A. Watt led a move to bring the international Can-Am Clinical Anesthesia Conference to Buffalo, marking the first time the event had been held on American soil.
Gender equity, belonging and retention took center stage at the UB DoctHERS Annual Symposium, celebrating women in medicine while tackling persistent challenges.
DoctHERS is a leadership network of female physicians, scientists, faculty, health care professionals, residents and students whose goal is to address current issues in the medical and scientific fields to enhance advancement, mentorship and equal opportunities for future generations of women in medicine and science.
This year’s event, held Feb. 13 in the M&T Auditorium, featured Julie K. Silver, MD, a leading expert on gender equity, as the keynote speaker. Silver was an associate professor and associate chair in the Department of Physical Medicine and Rehabilitation at Harvard Medical School. She has published groundbreaking research on workforce diversity and inclusion topics.
Silver said accelerating gender equity is really about disparities.
“We have made a lot of progress, but this was probably the most discouraging study for women in medicine when it came out in 2020,” she said, noting a NEJM study titled “Women Physicians and Promotion in Academic Medicine” that included a sample of 559,098 graduates from 134 U.S. medical schools.
“It found that over a 35-year period, women physicians in academic medicine centers were less likely than men to be promoted to the rank of associate or full professor or to be appointed to department chairs, and there was no apparent narrowing in the gap over time,” Silver noted. “We know that critical mass theory does not work in gender equity.”
She said she decided to use her strategic experience to look for tipping points in the process to assist women in medicine in advancing in their careers.
that was hosted in Niagara Falls, Canada, but the last in-person CanAm conference was in 2019.
Stacey A. Watt, MD, MBA, clinical professor of anesthesiology at the Jacobs School, said after the COVID-19 pandemic interrupted inperson gatherings, the conference did not seem to be coming back.
She made a bold decision to act to resuscitate the conference and contacted McMaster University officials.
“I felt it was the perfect opportunity to showcase UB and allow for the American side of the Can-Am conference to have its turn,” she said.
“It has been and will always be a collaborative event, bringing the best of both sides of the border together to discuss differences, similarities and share opportunities,” Watt added. “Our plan is to continue the Can-Am conference here at UB for at least the next five years, if not longer.”
The 2024 conference featured moderators and panelists from partner institutions McMaster University, Albany Medical College, the University of Rochester Medical Center and Western University in Canada.
The keynote address, titled “Addiction in Medicine,” was given by Joshua J. Lynch, DO, clinical associate professor of emergency medicine at the Jacobs School, and the founder of MATTERS, an innovative opioid treatment program.

At this year’s DoctHERS event, Jacobs School Dean Allison Brashear welcomed Julie K. Silver as the keynote speaker. Silver is a leading expert on gender equality and has published groundbreaking research on workforce diversity and inclusion.
“The hardest thing to do is find the tipping points, but when you do, that’s gold because you can drive change really fast,” Silver said. “I decided I was going to start with medical societies and recognition awards.”
Another tipping point Silver said was a Lancet study that showed women in medicine were underrepresented in clinical practice guidelines.
That led her to author a paper in the journal Cell that presented a novel concept Silver called “interorganizational structural discrimination.”
“The idea behind it is if an organization that has known problems with structural sexism or racism or whatever, that if you work with those organizations and they have fixable problems, then you are complicit,” she said.
In response to the growing demand for genetic counseling services nationally and regionally, the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo has hired a program director to launch a master’s degree program in genetic counseling.
Lindsey M. Alico, a Western New York native who was co-director of the genetic counseling program at Sarah Lawrence College, has been hired to implement and direct the genetic counseling program at UB.
Alico, a clinical assistant professor, is a board-certified genetic counselor who earned her master’s degree in human genetics from Sarah Lawrence in 2011. She will guide the UB program through accreditation.

Approved by the New York State Education Department and SUNY, UB’s program is pursuing accreditation by the Accreditation Council for Genetic Counseling, which will allow graduates to sit for the American Board of Genetic Counseling certification exam. Genetic counselors who pass the exam are granted the Certified Genetic Counselor credential, which is required to practice in most areas.
Genetic counselors are experts in genetics and genomics; they provide
Jacobs School of Medicine and Biomedical Sciences medical students working with community anti-violence groups in Buffalo have developed an elective course on “trauma surgery and trauma-informed care.”
The purpose is to train medical students, particularly those interested in surgery, in trauma-informed care in Buffalo’s Level 1 Adult Trauma Center at the Erie County Medical Center (ECMC).
Critical partners are Buffalo’s two antiviolence organizations—Buffalo SNUG (Should Never Use Guns) and Buffalo Rising Against Violence (BRAVE) Trauma Recovery Center—housed within ECMC. BRAVE is Western New York’s only Trauma Recovery Center, having attained that distinction from the National Alliance of Trauma Recovery Centers late last year.
“Students spend half their time working on the trauma service at ECMC alongside attendings and residents, and the other half with BRAVE and SNUG,” said Michael Lamb, PhD, director of surgical education in the Jacobs School and instructor for the elective. “The students serve as navigators for trauma patients and their families, offering support and advocacy during their hospital stay, clinical follow-ups and home visits.”
“The whole goal is to bridge two worlds
patients with information and guidance about inherited diseases and conditions that may affect them and their families. Patients who have received a disease diagnosis may be referred to a genetic counselor to determine if there may be a genetic component to it; couples who are expecting a child or are trying to conceive may also see genetic counselors.
Unlike other members of the health care team, genetic counselors don’t directly diagnose or prescribe. Instead, they help interpret complex genetic and genomic information for patients and empower them to make decisions about their health that are best for them.
“We are trained to facilitate decisionmaking,” said Alico. “We aren’t going to say ‘you need this genetic test.’ Our job is to evaluate and communicate genetic risk information so you can decide if you want the test or not.”
that usually don’t collide,” said Gaby Cordero, MD, a recent Jacobs School graduate who was the first person to take the elective.
The idea to create a trauma-informed curriculum developed from conversations between Jacobs School students Pia Corujo Avila, Katherine Foote and Sydney Johnson, all of whom had been awarded the Department of Surgery’s summer diversity research fellowship for underrepresented students in 2022.
WATCH: Scan the QR code to learn more about the Jacobs School’s innovative approach.



“As the surgeon, the only time you may see the patient is in the OR,” Johnson said. “You need a bit more humanity. When you understand the world the patient comes from, the injury that brought them to the hospital, and what they are going home to, you can be more proactive in their care. When you, the provider, are able to take all of this into consideration, the patient will have better outcomes.”

After years of research and planning, the Jacobs School has launched its brand-new medical school curriculum. Class of 2028 students arrived on campus in July 2024 and were the first to participate in the Well Beyond Curriculum, a cuttingedge approach that will redefine medical education in Buffalo for years to come. Learn more at medicine. buffalo.edu/well-beyond
This spring, 100 farmers and villagers throughout Belize underwent training in lifesaving “Stop the Bleed” techniques provided by a team led by Jacobs School medical students.
Members of the Global Surgery Student Alliance at the University at Buffalo made the trip during their spring break to provide “Stop the Bleed” training, a program of the American College of Surgeons, which has been shared with more than 4 million people worldwide. As a result, many more Belizeans now know how to quickly control bleeding, a critical skill for residents who often live far from health care facilities.
In just a week, the team of Buffalo and Rochester-based students, nurses and physicians traveled to five different locations in rural Belize to do the training.
The idea for the Belize trip started with Rachel Yerden, a second-year student in the Jacobs School who had been working with InterVol, an organization that also repurposes unused extra medical supplies and sends to global areas of need.
Wanting to provide more hands-on assistance to those in need, Yerden began discussing with her peers ways to leave a lasting impact.
“We wondered, what’s the most sustainable way for us to be involved?”
Yerden said. “We knew teaching was highly sought after in these communities, but we didn’t know what we could teach because we are just students.”
But once they discussed the medical disparities experienced by people in rural Belize with Belizean health care workers, it became clear that one of the biggest causes of morbidity and mortality was the inability to get severely injured people treated because of their remote locations. It quickly became apparent that “Stop the Bleed” training would go a long way toward saving lives.
InterVol was on board with the idea and helped connect Yerden with emergency medical technicians (EMTs) in Belize. Yerden organized and led the trip with Seth Baker, another second-year student in the Jacobs School. Buffalo and Rochesterbased health professionals, including those from InterVol, went on the trip as well.
Upon arrival in Belize City, Yerden, who is fluent in Spanish, taught the first class for the volunteers on the trip, as well as

some local EMTs. That training certified 10 physicians and EMTs who traveled with the group throughout the week. These Belizeans are now certified as instructors
Second-year medical student Rachel Yerden said one thing she was most proud of was the eclectic group of people they offered “Stop the Bleed” training to on the trip to Belize. “I taught classes to cacao farmers, banana farmers, families, elementary school teachers, children and health care workers,” she said.
for “Stop the Bleed,” who will, in turn, train more people in their respective communities.
Gender-affirming health care is a bit easier to access in Western New York, thanks to a new webpage developed by Jacobs School medical students working with local clinicians.
The webpage, LGBTQIA2S+ Healthcare Resources in Erie County, went live this past summer and is hosted by the Erie County Department of Health. It provides information about local health care resources specifically for patients who identify as LGBTQIA2S+. (The acronym stands for lesbian, gay, bisexual, trans, queer or questioning, intersex, asexual and 2-spirit.)
“People who are seeking genderaffirming health care should know that our region has a solid foundation of clinical and medical resources,”said Gale R. Burstein, MD, Erie County commissioner of health and clinical professor of pediatrics in the Jacobs School. “LGTBQIA2S+ patients are more likely to be disproportionately affected by health disparities. This comprehensive list will save patients time as they research medical care options.”
The need for such a resource became obvious when a new faculty member at the Jacobs School who provides genderaffirming care had difficulty finding other local clinicians who do the same. Genderaffirming health care providers often refer
patients to each other so it’s important for them to be familiar with each other and the scope of their colleagues’ practices.
A quick search turned up only one name: Elana Tal, MD, clinical assistant professor of obstetrics and gynecology in the Jacobs School. She knew there were plenty of other clinicians in Buffalo and Erie County providing gender-affirming care, but the fact that they were hard to find was a concern.
Tal organized several students who she knew were interested in improving gender-affirming care in Western New York and gender-affirming education in the Jacobs School. The group included Virginia Alexandria Headd, MD, a 2024 graduate of the Jacobs School; Madison Clague of the Class of 2026; and Zoe Arditi and Berkley Sawester of the Class of 2027.
“We were dismayed at how hard it was to find providers, but also pleasantly surprised by the depth and breadth of services being provided by physicians once we identified them,” said Tal.
Gender-affirming care encompasses a range far broader than people may assume. It can range from medical and psychiatric treatments to many different types of plastic surgery, including oral and maxillofacial surgery and otolaryngology, to speech and language coaching, all of which are available in Erie County.
The Oct. 7 attack on Israel dramatically changed everything in that country. For the Haroush family, living in central Israel, life had begun to change prior to that date, but for very different reasons.
For months, Noa Haroush, 18, had been complaining of weakness on her left side. At first it didn’t seem severe, but as time went on it got worse. By late summer, Noa was experiencing shakiness in her hand and arm, her mother Sharon said.
“It was scary,” Noa recalled. “I didn’t know what it was. I thought maybe it could be from stress from school or maybe a medication.”
Clearly, something was very wrong and the family took her to the hospital. After more than a week of tests and imaging, they received a diagnosis: Noa had Moyamoya disease, a rare condition in which the arteries that go to the brain become blocked, putting the patient at high risk for stroke and bleeding in the brain.

Endowed Chair of Neurosurgery at UB, co-director of the Gates Stroke Center and Cerebrovascular Surgery at Kaleida Health, and president of UB Neurosurgery. “It was on both sides of her brain. She was already having symptoms throughout her whole left side.”
Noa needed surgery immediately. Levy teamed up with his longtime surgery partner, Adnan Siddiqui, MD, PhD, CEO and CMO of the Jacobs Institute, and vice chair and professor in the Department of Neurosurgery at the Jacobs School.
The surgery felt endless, Sharon recalled. It lasted eight long hours. “It was very hard to just be in the waiting room.”
The surgery was completely successful, but Levy told the family it had been one of the most complicated surgeries his team had ever done. The family’s relief was hard to put into words, especially after they learned that Noa’s condition was so severe she could have been very close to having a stroke.
“I really want to thank Dr. Levy, Dr. Siddiqui and their team and all the nurses,” Sharon said. “Everyone took such good care of us. They did such a wonderful job.”

The condition can be cured if brain surgery is done in time. Israel has sophisticated medical facilities. But surgery for such a complex, rare condition is best done at a high-volume facility where surgeons have experience operating on such patients—such as Gates Vascular Institute, where UB neurosurgeons have done this operation numerous times.
The family already had a connection with Buffalo. Elad I. Levy, MD, who chairs the Department of Neurosurgery in the Jacobs School, was born in Israel. His father and Noa’s grandfather have been best friends for decades.
The family made a quick decision to come to Buffalo once they learned of the Hamas attack. Noa arrived in Buffalo with her parents and three siblings on Oct. 8.
While imaging of her brain had been done in Israel, Levy decided to do another cerebral angiography. The procedure involves using a catheter to inject contrast dye into the bloodstream. X-ray imaging then reveals how blocked the arteries have become.
The new images told a terrifying story that hadn’t been evident in the original images, providing a much better roadmap for the surgery.
“She had one of the worst cases of Moyamoya we’ve ever seen,” said Levy, SUNY Distinguished Professor, L. Nelson Hopkins
In addition to state-of-the-art stroke care, complex neurosurgeries for rare conditions are increasingly being done at Gates Vascular Institute, a Kaleida Health facility, by Jacobs School neurosurgeons, making it a top site for complex neurosurgeries.
“We’re an international destination for neurovascular surgery,” said Levy. “When people need this kind of care, and they start to research who can deliver it, we are at the top of the list.”
“We’re an international destination for neurovascular surgery. When people need this kind of care, and they start to research who can deliver it, we are at the top of the list.”
Elad I. Levy, MD, SUNY Distinguished Professor and L. Nelson Hopkins Endowed Chair of Neurosurgery
NYS funding helps grow geographic footprint, introduces ‘no stigma’ vending machines
MATTERS, an innovative opioid treatment program that grew out of a University at Buffalo physician’s frustration with the limitations of care for patients who had overdosed, is expanding its services throughout New York State, thanks to funding from the state’s Department of Health.
end bias and discrimination surrounding opioid use disorder,” said James V. McDonald, MD, commissioner of the New York State Department of Health. “The department welcomes the collaboration with the University at Buffalo’s opioidtreatment program and the deployment of vending machines as an innovative tool to supplement existing harmreduction programs throughout the state.”
Starting last fall, MATTERS has installed 12 “no stigma” vending machines throughout New York State (see map below), including here in Western New York. They provide free naloxone, the overdose antidote, and free test strips for fentanyl and xylazine.

The first one in Erie County is located outside the Kenmore Volunteer Fire Department, which hosts the machine; it is owned and serviced by Save the Michaels of the World, which raises awareness about drug addiction and its risks. Additional machines in Western New York are on Virginia Street in Buffalo and Main Street in Lockport.

One of the 12 “no stigma” vending machines installed throughout New York State by MATTERS. They provide free naloxone, the overdose antidote, and free test strips for fentanyl and xylazine.
stigma, increase awareness and build a future free from addiction’s grip,” said Allison Brashear, MD, MBA, vice president for health sciences at UB, dean of the Jacobs School and president of UBMD Physicians’ Group.
Chinazo Cunningham, commissioner of the New York State Office of Addiction Services and Supports, said: “OASAS is proud to partner with MATTERS in our work dedicated to serving people with substance use disorders. The new MATTERS harm-reduction vending machine builds on OASAS efforts to expand the availability of such lifesaving materials. This is important work, and we look forward to working with MATTERS on future projects.”
With the $8 million grant—part of the opioid settlement funds distributed throughout the state last year—MATTERS is hiring additional regional outreach coordinators to expand its geographic reach, supporting “no stigma” vending machines and working with neighboring municipalities that want to model programs after MATTERS.
“The MATTERS program makes a difference and is a critical component of the department’s ongoing efforts to expand access to harm-reduction services and
“People with opioid use disorder can be reluctant to walk into a pharmacy to obtain test strips or naloxone,” said Joshua J. Lynch, DO, founder of MATTERS, a clinical associate professor of emergency medicine in the Jacobs School of Medicine and Biomedical Sciences at UB and a physician with UBMD Emergency Medicine. “So, we wanted the vending machines to be in different types of places, outside and always accessible.”
To use the machines, an individual types in the code found on the outside of the machine, their birth year and zip code, and selects the items they want, which are immediately dispensed for free.
“The Jacobs School is proud to be part of a larger movement working to overcome
Lynch explains that the MATTERS network is based on the premise that patients must be linked to treatment promptly and they must see that they have plenty of choices.
“We know that the window of opportunity when we can intervene with a patient may only be open for a very short time,” said Lynch. “Through the many partnerships we’ve established, we developed an electronic platform where we can link a patient to their first clinic appointment within 24-48 hours pretty much anywhere in New York State.”

WATCH: Learn more about MATTERS and its “no stigma” harm reduction services.
The University at Buffalo has been awarded a highly competitive $3.6 million grant from the National Institute on Minority Health and Health Disparities to train earlycareer faculty members to address health inequities in Western New York.

Both UB’s strong community partnerships and the university’s range and breadth of expertise were instrumental in getting the award, university leaders said.
The five-year grant from the institute, part of the National Institutes of Health, aims to inspire and mentor early-career faculty researchers from a wide range of academic disciplines to address the entire range of social determinants of health. This includes poverty, substandard housing, unequal access to health care, lack of educational opportunity, racism and more.
UB will use the award to establish the Center of Excellence in Investigator Development and Community Engagement, which will be embedded in the universitywide Community Health Equity Research Institute. The center will encourage and support research that benefits people who experience health inequities caused by adverse social determinants of health.
“Today’s $3.6 million grant will help ensure all Western New Yorkers have access to the quality health care they need and deserve, no matter their means or background,” U.S. Rep. Tim Kennedy said. “It will provide UB with the resources it needs to recruit and develop the next generation of researchers to better understand the social disparities that impact the health care and services people rely on in order to level the playing field. This is just another example of the ways Western New York is becoming a better and more equitable place to live, work, and raise a family—for everyone.”
Allison Brashear, MD, MBA, vice
president for health sciences and dean of the Jacobs School of Medicine and Biomedical Sciences, said: “This award underscores UB’s unwavering dedication to enhancing the health of the Buffalo community. Leveraging UB’s robust expertise in health sciences and our extensive research capabilities, we are fully committed to advancing health outcomes.”
She added: “Through our strong partnerships with numerous community organizations, we believe we can transform the health landscape of our region. Although this award is centered at UB, its true purpose is to empower and transform the health of Buffalo and Western New York.”
The grant, titled “Igniting Hope in Buffalo, New York Communities: Training the Next Generation of Health Equity Researchers,” provides UB with resources to attract early-career faculty researchers and postdoctoral fellows from health care disciplines, as well as non-health care fields, to work on problems that impact the social determinants of health. The center will utilize a “community-based participatory research” approach, where community members are a partner in the research, helping to design, plan and conduct the research so that they can gain the greatest benefit from it.
While advances in medical interventions have dramatically accelerated in recent years, such interventions cannot overcome the systemic inequities that are so deeply rooted in complex social systems. For that reason, the center will prioritize attracting investigators working in fields outside health care to address, for example, inequities in the criminal justice system, substandard housing, access to healthy food and many other issues.
“Adverse health outcomes are a result of these social determinants of health,” said Timothy F. Murphy, MD, principal investigator on the grant, SUNY Distinguished Professor and director of UB’s Community Health Equity Research Institute. “If we could solve all health care access problems, we’ll still only change health outcomes in our at-risk communities by about 15%. What we are trying to do with this grant is to attract researchers in non-health-care disciplines, who are working in urban planning or education or law or management, and to make them aware that their work is absolutely critical to solving health disparities in Western New York.”
“What we are trying to do with this grant is to attract researchers
in non-healthcare disciplines, who are working in urban planning or education or law or management, and to make them aware that their work is absolutely critical to solving health disparities in Western New York.”
- Timothy F. Murphy, MD
“Health inequity remains a serious and complicated issue in Buffalo and its surrounding communities,” said state Sen. Sean Ryan. “To solve this crisis, we must understand its root causes and develop innovative solutions. I am pleased to support the University at Buffalo and community leaders who are addressing this urgent problem, and look forward to building stronger and healthier communities in Western New York.”
From left, speakers Kelly Wofford, Rev. George F. Nicholas, NYS Assembly Majority Leader Crystal Peoples-Stokes, U.S. Rep. Timothy M. Kennedy, Dean Allison Brashear, and Timothy F. Murphy pose for a photo following an Aug. 6 press conference announcing the NIH grant.
In 2019, UB established the Community Health Equity Research Institute with strong community involvement. In 2021, Erie County established its Office of Health Equity. That same year, UB’s Center for Urban Studies partnered with the Community Health Equity Research Institute, linking the institute to urban planning and neighborhood development.
These connections have further cemented local, coordinated universitycommunity-government efforts to address health inequities, some of which may depend on legislative and policy changes.
In a reflection of those connections, Rev. George F. Nicholas, CEO of the Buffalo Center for Health Equity, is associate director of the UB Center of Excellence in Investigator Development and Community Engagement. He says that without research, many well-intentioned efforts don’t have the expected benefit.
“The work of health equity has got to be data-driven,” he said. “A lot of work that is done to address social problems often gets tied up in theoretical approaches or philosophical approaches and history has taught us while they may do some good, they don’t bring real change. Research gives us a clear picture on the depth of the problems and what is driving them. When we better understand the scope of the problems and what’s driving them, then we can develop approaches and remedies to solve them.”
With the grant, UB will provide faculty researchers and postdoctoral fellows with pilot funding for projects with community partners that have the potential to generate transformational change. These changes will not be quick fixes, Murphy cautions.
“A Black person in Buffalo dies 10 to 12 years younger than a white person in Buffalo,” said Murphy. “That’s a tragedy and unfortunately it’s not one that’s going to change anytime soon. But what if a researcher develops a green infrastructure project that actually reduces pollution in a neighborhood and that then causes a drop in the number of kids with asthma who end up in the emergency room? That’s going to have a bigger outcome down the road, kids won’t be missing school, their education improves. That’s the kind of change we’re going to see with this new research.”
The center could even change how research is viewed in the community, Nicholas adds, and it will encourage people in at-risk communities to get involved.
“You don’t hear a lot of young people say, ‘Hey, I want to be a researcher,’” he said. “But we want to make being a researcher not only a possibility but make it attainable and desirable, to say ‘This is something you could do that will have an impact on your community, on the neighborhood you live in.’”

The Jacobs School is among the nation’s most diverse medical schools, according to the 2024-2025 America’s Best Graduate School rankings released July 23 by U.S. News & World Report.
The Jacobs School tied for 18th among public institutions in the publication’s ranking of most diverse medical schools. Overall, the Jacobs School ranked 28th out of a total of 168 schools.
The diversity index measures how successful medical schools are at enrolling students historically underrepresented in medicine. It considers the percentage of underrepresented students enrolled at a school and the ratio of that population in comparison to state or national figures. Nearly 23 percent of medical students enrolled at the Jacobs School come from groups underrepresented in medicine.
The Jacobs School of Medicine and Biomedical Sciences will have several new faces chairing its departments in the 2024-25 academic year.
The school successfully recruited three visionary leaders to head up its departments of medicine, pediatrics and anesthesiology.
• Leonard E. Egede, MD, joined the Jacobs School on July 1 as Charles and Mary Bauer Endowed Chair of Medicine and president and CEO of UBMD Internal Medicine.
• Benny L. Joyner Jr., MD, was appointed the A. Conger Goodyear Professor and Chair of the Department of Pediatrics in the Jacobs School effective Jan. 6, 2025. He will also serve as president and CEO of UBMD Pediatrics.
• Brian M. Parker, MD, was named chair of the Department of Anesthesiology, effective Oct. 1. He will also serve as senior associate dean for clinical affairs in the Jacobs School and chief medical officer for UBMD Physicians’ Group.
Egede, who comes to UB from the Medical College of Wisconsin, served as the chief of the Division of Internal Medicine and director of the college’s Center for Advancing Population Science. He is a nationally recognized health disparities researcher whose work focuses on developing and testing innovative interventions aimed at addressing and ultimately eliminating health disparities in chronic medical and mental health conditions that result from race/ethnicity, socioeconomic status and geographic location.

a clinical practitioner and educator of trainees a deep understanding of the social determinants of health in his community.




development. His research endeavors include leading numerous National Institutes of Health grants, including five R01 grants and an R21, and securing nearly $20 million total in funding. He has published more than 450 manuscripts in peer-reviewed journals, reflecting his impactful research and commitment to advancing health equity.







The Department of Medicine is the Jacobs School’s largest, comprising 13 divisions spanning a wide range of specialties, from general internal medicine and infectious disease to diabetes and geriatrics. The department is home to nearly 200 faculty members who teach, conduct research and provide patient care in Western New York.



He directs a six-year, $2.8 million project funded by Advancing Healthier Wisconsin focused on addressing health disparities in Milwaukee’s African American community. As the inaugural Milwaukee Community Chair in Health Equity Research, Egede is committed to bringing to his work as a researcher,






With more than 24 years of academic leadership, Egede has spearheaded significant initiatives in research, mentorship and faculty







Egede grew up in the central part of Nigeria and earned his medical degree from the University of Benin, Benin City, Nigeria, and his master’s from the Medical University of South Carolina. His postgraduate training and fellowship appointments include an internship and residency in internal medicine at Greater Baltimore Medical Center, where he also served as chief resident. He completed a Health Services Research Fellowship at the Medical University of South Carolina. He is a fellow of the American College of Physicians, and board-certified by the American Board of Internal Medicine.
A professor of medicine, Egede replaces Brian Murray, MD, who had served as interim chair of the department since January 2023.
Joyner currently serves as professor and chief of the Division of Pediatric Critical Care Medicine and vice chair of clinical operations for the Department of Pediatrics at the University of North Carolina at Chapel Hill School of Medicine. He is a prominent pediatric intensivist, providing care to seriously ill children in intensive care environments. He is renowned for his pioneering work in simulation training and innovative medical education. He has focused his career on advancing pediatric critical care and medical simulation, with accomplishments that include expanding faculty and fellowship programs, leading
national and international collaborations, and enhancing educational practices.
A tenured professor at the UNC School of Medicine, Joyner was awarded the Charles Everette and Katherine M. Brewer Endowed Professorship in the Department of Pediatrics earlier this year; it was established to advance children’s research and health care programs.
In addition, Joyner is adjunct professor in the departments of anesthesia and social medicine and associate chief medical officer for pediatric professional services at UNC Health. He previously served as director of the UNC Clinical Skills and Patient Simulation Center.
Joyner has been honored with the Craver Medical Student Teaching Award, which recognizes outstanding teachers in internal medicine, pediatrics and surgery who inspire and significantly impact the lives of medical students through their teaching. He also received the H. Fleming Fuller Award from UNC, in recognition of his dedication to high standards of patient care, teaching, and community service.


His research focuses on the development of novel simulation strategies using high-fidelity technology to enhance medical training.

Medicine and a master’s of public health from the university’s School of Public Health.
He completed his residency at the Albert Einstein College of Medicine Pediatric Residency Program at Montefiore Medical Center, Bronx, New York, where he also served as chief resident in pediatrics. He completed his fellowship in pediatric critical care medicine at UNC School of Medicine.
He will also serve as pediatrician-inchief at John R. Oishei Children’s Hospital and chief of service for pediatrics for Kaleida Health.
Joyner replaces Anne Marie Reynolds, MD, who served as interim president and CEO of UBMD Pediatrics and interim chair of the Department of Pediatrics since




Through this work, Joyner aims to improve the training and confidence of health care providers who have limited exposure to critically ill pediatric patients. His efforts in simulation training address the challenges of rare, high-stakes events in patient care and the implementation of advanced technologies in resource-limited settings. Joyner employs these techniques in order to prepare trainees to provide excellent care in complex situations.





Allegheny Health Network.
He is a member of the American Society of Anesthesiologists; the Society for Ambulatory Anesthesia, where he served as a past president; the Pennsylvania Society of Anesthesiologists; and the International Liver Transplantation Society.
With significant leadership experience, Joyner is an innovator in medical education and interprofessional education. He has given invited talks across the country on simulation in health care, collaboration and teamwork. A passionate educator, he initially trained to be a high school teacher, then went on to earn his medical degree from the UNC School of

Parker, who earned both his undergraduate and medical degrees at UB and completed his anesthesiology residency and liver transplantation fellowship training at the University of Pittsburgh, returns to the Jacobs School after serving as chief quality and learning officer at Allegheny Health Network, part of Highmark Health.
In his role as chief quality and learning officer for Allegheny Health Network, he was responsible for ensuring that the highest standards of patient care quality, safety and service excellence are achieved across the system’s 14 hospitals and its hundreds of clinical locations, primary care offices and specialty practices.
He also served as chair of the Enterprise Quality, Safety and Value Operations Committee, and was instrumental in driving system-wide quality initiatives for both Highmark Health and Allegheny Health Network.
Parker twice served as an interim chair of anesthesiology at both the Cleveland Clinic and the Anesthesiology Institute at
As the Department of Anesthesiology’s academic and clinical head, Parker will focus on expanding research, building a strong clinical practice, and leading the department’s commitment to educating medical students and residents. In his dual role as senior associate dean for clinical affairs and CMO of UBMD, he will partner with UBMD leadership to expand access to high-quality care in the region and continue to build on UB’s goal of improving the health of patients in Western New York. He replaces Stacey A. Watt, MD, who served as interim chair of the Department of Anesthesiology since January 2023.
“The recent hiring of these three new department chairs at the Jacobs School reflects our commitment to excellence and innovation in medical education and patient care. Each of these leaders—Dr. Egede, Dr. Joyner and Dr. Parker —brings a wealth of experience and vision that will undoubtedly inspire our community and drive us forward in our mission to improve health outcomes.”
—Allison Brashear,
MD, MBA, Vice President for Health Sciences and Dean of the Jacobs School




By Ellen Goldbaum










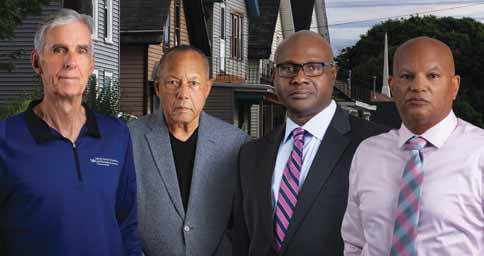
It was 2015. Local Buffalo pastors and community leaders who had formed the African American Health Equity Task Force had just released their report on the region’s shocking health disparities. Among the most alarming findings were these: that a Black person in Buffalo dies 10 to 12 years sooner than a white person and is 300% more likely to suffer from a chronic disease.
The grim story those numbers told launched unprecedented meetings between task force members, community, government and church leaders and UB researchers.
Timothy F. Murphy, MD, SUNY Distinguished Professor in the Jacobs School and senior associate dean for clinical and translational research, was one of them.
“For the first two, three years, I hardly said a word,” he recalled in a recent Buffalo News story. “I just listened and listened— and learned a lot.”

Collaborative partnerships are fueling the movement to address health disparities in Buffalo and Western New York. Among the key players, left to right, Timothy F. Murphy, HenryLouis Taylor Jr., Leonard E. Egede and Rev. George Nicholas.

That connection, between those who spoke their truths and those who listened to them, started a movement that has begun to address and reverse those deep disparities. And those meetings continue today.
“For the first two, three years, I hardly said a word. I just listened and listened— and learned a lot.”
Timothy F. Murphy, MD
The movement is changing how UB researchers work with the community. UB researchers now see community members as critical local experts who must be equal partners from the start.
In August, in what many see as an elevation and recognition of that focus, the National Institute on Minority Health and Health Disparities awarded UB a highly
competitive, $3.6 million grant to train early-career faculty members to address health inequities in Western New York. (See story, pages 20-21.)
Research is communitybased, participatory
The grant establishes a center that utilizes a “community-based participatory research” approach, where community members are partners in the research, helping to design, plan and conduct the research so that they can gain the greatest benefit from it.
Titled “Igniting Hope in Buffalo, New York Communities: Training the Next Generation of Health Equity Researchers,” the grant provides UB with resources to attract early-career faculty researchers and postdoctoral fellows from health care disciplines, as well as non-health care fields, to directly work on problems that impact the social determinants of health.
A key reason that UB was awarded the grant was the strong connection researchers have developed with the community. In a reflection of that connection, the center’s associate director is Rev. George F. Nicholas, CEO of the Buffalo Center for Health Equity, which has been a critical partner with UB since 2015. Those connections help demonstrate that UB is committed to addressing health disparities in the region and have helped draw the attention of national leaders in the field.
In July, Leonard E. Egede, MD, became the chair of the Department of Medicine. Previously at the Medical College of Wisconsin, Egede is a nationally recognized health disparities researcher. His work focuses on developing and testing innovative interventions aimed at addressing and ultimately eliminating health disparities in chronic medical and mental health conditions that result from race/ethnicity, socioeconomic status and geographic location.
With over 24 years of academic leadership, Egede has led numerous grants from the National Institutes of Health (NIH), securing nearly $20 million total in funding. He has published more than 450 manuscripts in peer-reviewed journals, reflecting his impactful research and commitment to advancing health equity.
Egede has brought a team of researchers with him to UB. The goal of the Health Equity Research Group he leads is to develop and test individual- and community-level interventions and programs that improve health equity by engaging community members in research, maintaining dynamic and adaptable processes and building trust.
“Dr. Egede’s appointment reflects the commitment of the Jacobs School to expanding and elevating UB’s work in health disparities,” said Murphy. “In meetings with local leaders, Dr. Egede had the chance to see just how engaged and energized this community is. He saw that UB’s community partners are people with ideas, plans and absolute commitments to this work.”
Community partnerships are also integral to the development of a novel neighborhood pilot project that is being launched on the city’s East Side. “How We Change the Black East Side: A Neighborhood Planning and Development Framework” is a demonstration project designed to radically improve and transform a selected East Side neighborhood.
see less infant mortality, fewer children born with birth weights that are too low, stresses will be reduced and so will a lot of illnesses that are catalyzed by high levels of stress.”
A packed public meeting held at the Jacobs School last winter to kick off the project attracted more than 400 enthusiastic attendees. Among them were community activists, church leaders, local legislators and UB faculty and trainees.
Such an eclectic audience, gathering in a Jacobs School auditorium to discuss how to address persistent local issues is not an anomaly. Back in 2015, the earliest conversations about Western New York health disparities resulted in the proposal

Led by Henry-Louis Taylor Jr., PhD, director of UB’s Center for Urban Studies, professor of urban and regional planning in the School of Architecture and Planning and an associate director of the Community Health Equity Research Institute, the project followed the center’s 2021 report, “The Harder We Run: The State of Black Buffalo in 1990 and the Present.” That report clearly demonstrated that Black Buffalo has not made progress during the past three-plus decades. It found that conditions in physical neighborhoods had deteriorated and that now there was a new, even more dangerous threat: gentrification.
Taylor explained: “The goal of this neighborhood transformation is that people will live longer and better. We will
to hold a university-community conference with extensive collaboration from all sectors of the community. A free, public conference was envisioned as a way for community members, students, faculty and university and local leaders to come together to begin to address Buffalo’s social determinants of health.
The Jacobs School made the decision that it would support the annual conference at no cost to the organizers. That’s been the case since the conference was first held in 2018.
Rev. Nicholas explained the goal of the Igniting Hope conferences. “Along with our partner, the University at Buffalo, we have brought national experts to engage in robust dialogue with local community leaders as we work to address the root causes which drive health disparities,” he
said. “We are promoting a public dialogue on health equity while advocating for real systems change, which will eliminate racebased health disparities.”
In a paper published in 2022, community leaders and faculty from four UB units describe how even the planning process for the conference became a space where important community interactions that had never happened before were taking place.
“The planning of the conference kept us meeting every month and coming together every month,” said Murphy. “The most important thing that the conference did was, it created awareness in the community about these problems, which was the first step toward addressing them.”
Around the same time UB was awarded a $15 million Clinical and Translational Science Award (CTSA) from the NIH. It was followed in 2020 with the awarding of a second CTSA, for $21.7 million. The NIH sees the ultimate goal of these awards as improving the health of communities nationwide.
Those awards led to UB’s establishment of a pilot funding program through the Clinical and Translational Science Institute (CTSI). The program provides seed funding to launch novel translational research studies that can then be used to attract major external funding.
One of the early projects funded was Project ASTHMA (Aligning Schools to Help Manage Asthma), led by Lucy C. Holmes, MD, clinical associate professor of pediatrics. Project ASTHMA is a research program supporting school-based asthma care for students aged 4-13 years living below the poverty line. Earlier this year, the project was awarded $3.2 million in funding by the National Institute on Minority Health and Health Disparities.
“Our hypothesis is that we can improve the health of these kids who have uncontrolled asthma by giving them high quality health care in the schools through school-based health centers,” said Holmes, also a physician with UBMD Pediatrics and at John R. Oishei Children’s Hospital, who is working with a multidisciplinary team of investigators from UB and external partners. “Novel ways of providing top-quality medical care for asthma to children in economically disadvantaged
communities are needed to help decrease health inequities,” she said.
Other research projects both at the medical school and beyond are focusing on food insecurity and improving diet in underserved areas; culturally tailored breastfeeding interventions for Black women; improving communication to increase live donor kidney transplantation; prenatal and childhood mechanisms of health disparities; and
“Through
our strong partnerships with numerous community organizations, we believe we can transform the health landscape of our region. Although this award is centered at UB, its true purpose is to empower and transform the health of Buffalo and Western New York.”
Allison Brashear, MD, MBA, vice president for health sciences and dean of the Jacobs School
air pollution and coronary events in susceptible populations, among many others.
Health equity work continues to inform education and service throughout the Jacobs School and UB. Students worked with physicians and community antiviolence groups to create an elective for their peers in trauma-informed care; students also have established an annual conference designed to attract Indigenous students into health care fields and the Jacobs School was ranked one of the nation’s most diverse medical schools by U.S. News & World Report.
At the August press briefing announcing the NIH Igniting Hope grant, Allison Brashear, vice president for health sciences and dean of the Jacobs School, said: “Through our strong partnerships with numerous community organizations, we believe we can transform the health landscape of our region. Although this award is centered at UB, its true purpose is to empower and transform the health of Buffalo and Western New York.”
By Ellen Goldbaum
On Aug. 21, UB President Satish K. Tripathi presented Timothy F. Murphy, MD, with the President’s Medal. It recognizes “outstanding scholarly or artistic achievements, humanitarian acts, contributions of time or treasure, exemplary leadership or any other major contribution to the development of the University at Buffalo and the quality of life in the UB community.”
In his multiple roles, Murphy checks every one of those boxes. He is a SUNY Distinguished Professor, senior associate dean for clinical and translational research, founding director of UB’s Clinical and Translational Science Institute and director of UB’s Community Health Equity Research Institute.
An internationally recognized expert in respiratory infections, Murphy has transformed understanding of bacterial infections in chronic obstructive pulmonary disease (COPD) and vaccine development for otitis media (ear infections) and COPD. With continuous National Institutes of Health funding for 40 years, he has published hundreds of major papers and authored chapters in major textbooks; he also holds 13 patents.
Tripathi described Murphy’s talents as a pioneering researcher, a community advocate and a beloved mentor. “Tim always works on others’ behalf,” Tripathi said, while being “one of the most humble, down-to-Earth, genuine people you will ever be fortunate to meet.”
“All of us have people in our lives who changed the culture of an institution, made all of us better, and set an institution on a new trajectory,” said Allison Brashear, MD, MBA, vice president for health sciences and dean of the Jacobs School. “Tim is one of those people.”
That evening, Murphy learned that U.S. Rep. Tim Kennedy has recognized his service to UB and to Western New York with a tribute published in the Congressional Record of the 118th Congress.
In a recent interview, Murphy traced how his current roles advocating for health equity grew out of his lifelong passions for science and medicine.
From a young age, Murphy wanted to go into medicine. As a kid he enjoyed playing with science kits. His mother encouraged it, often casually adding that perhaps he could find a cure for an illness that someone in the family had developed.
Murphy said, “My parents often told me, ‘you can do anything you want if you put your mind to it.’ We didn’t have a lot of money but it was an incredibly supportive environment to grow up in.”
Paying for college would have been a challenge. But Murphy, who played basketball in high school, caught a lucky break. Weeks before his freshman year began, New York University, then Division 1, offered him a full basketball scholarship.
At the time, NYU didn’t have its own sports facilities. So Murphy got to play with a team whose “home” court was none other than the then-newly constructed Madison Square Garden.

Timothy F. Murphy,
In 1976, Murphy earned his MD from Tufts University.
“My biggest problem was, I loved everything,” Murphy recalled. “I’d be doing GI and I’d be like, ‘wow, GI is great!’ and then I’d start doing cardio and I’d be like ‘wow, cardio is great!’”
He decided to focus on infectious disease. “I liked the idea that infectious disease spans so many different areas,” he said. “You don’t just focus on the kidneys or the heart or lungs. Infections can impact many
organ systems at once.”
Originally, his focus was patient care. But research appealed to him, too.
“One of the things I’ve spent a lot of time on is vaccine development for kids with ear infections,” Murphy said. “I started to think, well if I were a pediatrician, maybe I’d take care of 10-15 kids a day with these infections. But if I could develop a vaccine to prevent infections, I could impact more than a million kids each year in the U.S. alone! Research has huge societal benefit. I started to see the big picture.”

Murphy shared the celebration of his President’s Medal honor with his family, including his wife, Vicki, their children and their spouses and two of their four grandchildren.
From 1981 to 2009, Murphy worked in what he calls his ID bubble at UB. “I loved doing research, caring for patients, having grad students,” he said. “I worked with Tom Russo and Alan Lesse and we helped each other. It was an amazing group to be part of.”
In 2009, Michael E. Cain, MD, then the dean and vice president for health sciences, asked Murphy to lead UB’s application for a Clinical and Translational Science Award from the NIH.
The award, granted in 2015, was followed in 2020 with the awarding of a second CTSA, for $21.7 million. Murphy is principal investigator on both.
“Not only did he bring the CTSA to UB, one of 68 in the country, but he is such a smart, nice, and even-tempered leader that everyone trusts and respects him,” said Nancy H. Nielsen, MD, PhD, senior associate dean for health policy in the Jacobs School. “His leadership since the inception of the African American Health Equity Task Force has been masterful: He listens and seeks to understand, then helps guide efforts to move forward and solve problems.”
“I knew about disparities and I knew the numbers, but I didn’t feel it in my heart,” said Murphy. “I didn’t understand the impact they have on the people who live it every day. Those experiences changed my life and my view of the world, quite frankly.”
Rev. George F. Nicholas, CEO of the Buffalo Center for Health Equity, saw that change happen.
“Tim is a guy who has real compassion for those who are suffering,” he said. “Once he knew the historical roots of health disparities, and had a deeper understanding, it was just like a switch that turned on. He was sincerely interested in doing whatever he could to be an asset. He has been a real help to us on the issues of dealing with health equity.”
And while working with the community means that Murphy sees the problems right up close, it also makes him more optimistic.
“Tim
is a guy who has real compassion for those who are suffering. Once he knew the historical roots of health disparities ... it was just like a switch that turned on. He was sincerely interested in doing whatever he could to be an asset.”
Rev. George F. Nicholas, CEO of the Buffalo Center for Health Equity
“Before, I sort of thought OK, I’ll take the best care of patients that I can but I won’t be able to solve these problems,” he said. “But these community folks are brilliant. They have all kinds of ideas. They bring a new perspective. I started to have hope. I was attracted to join the battle.”

By Ellen Goldbaum
On most evenings and weekends throughout the cold winter months, artist Julia Bottoms could be found on a scissor lift in the atrium of the Jacobs School applying a vivid explosion of color to the previously plain white walls.
Brushstroke by brushstroke over a three-month period, Bottoms converted a blank space on the east side of the building into a vibrant celebration of diversity within the medical school and its close partnership with the surrounding community.
When she was through, the “Celebration of Diversity” mural was unveiled at a Feb. 22 ribbon-cutting ceremony.
“The completion of this beautiful mural, featuring actual members of our Jacobs School community, holds deep significance for us,” said Allison Brashear, MD, MBA, vice president for health sciences at UB and dean of the Jacobs School. “It embodies our diversity and our commitment to Buffalo, reflecting our shared dedication to an
inclusive environment where all can flourish.”
Stretching from floor to ceiling along a wall of the Jacobs School’s second-floor atrium, the mural measures 50-feet-wide-by-16-feet-tall.
Ten UB students and alumni, selected from an open casting call, served as models for the mural. Their likenesses are scattered throughout the tableau, some in scrubs and white coats, others walking and jogging along a streetscape or sitting on a bench in a park, capturing the harmonious blend of the school and city.

With the help of a scissor lift, Julia Bottoms was able to create a celebration of diversity, inclusivity and community that stretches more than 50 feet wide and 16 feet tall.
The mural has been in the works since 2019. Discussions among Raul Vazquez, MD, a 1989 Jacobs School graduate; his wife, Toni Gaiter-Vazquez, EdD, a 1991 UB graduate; and the late Jonathan D. Daniels, MD, a 1998 Jacobs School graduate and formerly associate director of admissions, began about how the medical school needed more color after the new building opened.
The Jacobs School itself was changing as
well. In 2018, the school held its first Second Look Weekend, an opportunity dedicated to hosting underrepresented students who had been accepted to the medical education program, but who hadn’t yet decided to enroll.
The event was inspired by Karole Collier, MD, then a first-year student at the Jacobs School and a member of the UB chapter of the Student National Medical Association (SNMA), the national organization committed to supporting current and future underrepresented medical students.
Collier saw that more could be done to attract students to the school who were underrepresented in medicine (URM). Working with Daniels and Dori R. Marshall, MD, who was director of admissions, Collier took her idea to Vazquez and other physicians and businesses on Buffalo’s East Side who embraced the idea. Vazquez is a leading sponsor of Second Look Weekend. In the first year, the Jacobs School nearly doubled its number of students underrepresented in medicine over the previous year. These efforts have been changing the face of the Jacobs School ever since.
The question was how to communicate those changes to faculty, students, staff and visitors in a more compelling way. The idea for a mural was born. But figuring out who or what to include in such a mural was another question that sparked numerous conversations among the Office of Medical Advancement, students, alumni and the community.
The decision was made to show current students, residents, alumni and community members as they are today.
Bottoms embraced the concept. “We started out talking about history and then decided, well we want to capture this moment because one day this will be history, as well,” she said.
The first major art installation requisitioned by the Jacobs School, the mural was made possible by funds provided by the Vazquez family. Vazquez, a clinical assistant professor of family medicine at the Jacobs School, is president of CINQCARE New York; he and his wife are the founders of Urban Family Practice and the Greater Buffalo United Accountable Healthcare Network (GBUAHN) in Buffalo. Their daughter, Nina, graduated from the Jacobs School with an MD in 2023, while another daughter, Nadia, recently completed her second year in the program.
Before Bottoms could begin applying paint to wall, the Office of Inclusion and Cultural Enhancement held a casting call, seeking people in every year of medical school, in the doctoral and master’s programs in biomedical sciences, as well as residents and alumni to serve as models.
Daniel Olutalabi, MD, a Jacobs School graduate now doing his radiology residency at the Jacobs School, is shown
wearing a suit in the mural. He says the mural serves multiple purposes.
“If the mural helps continue to show the Jacobs School’s dedication toward diversity and training culturally competent doctors, then people will recognize that this is the kind of place where you get that kind of training,” he said.

Olutalabi adds that the mural is more than a statement; it can also serve to stimulate dialogue. “The mural sparks a conversation, like ‘hey, what’s this mural about?’ It gets us talking, especially for individuals who may not know the struggles that URMs are going through.”
For Narayan Dhimal, the mural powerfully reflects his deep connection to Buffalo and UB. Dhimal was born in a refugee camp in Nepal; his parents had fled their home in Bhutan. He lived in the camp until he was 15, when the family was given an opportunity to relocate to the United States. They came to Buffalo and have been here ever since.
Dhimal did his undergraduate work at UB, and recently finished his doctorate in neuroscience. In July, he became a firstyear medical student in the Jacobs School.
“I am a minority,” he said, “and diverse people are the face of UB. The mural promotes the idea of inclusion and the dedication of people to work in the health care system and in research.
“Having my presence on the mural reinforces the idea that our differences, whether in upbringing, experiences or perspectives, collectively contribute to the richness of our shared environment,” he said. “I’m thankful for the opportunity to be a part of such a meaningful and impactful project.”
In addition to Bottoms, the Vazquez family and the late Dr. Daniels, the mural was made possible by the Medical Alumni
A joyful ribbon-cutting took place at the Jacobs School on Feb. 22, 2024, when the “Celebration of Diversity” mural was unveiled. From left, Allison Brashear, vice president for health sciences and Jacobs School dean; Raul Vazquez, and Toni Gaiter-Vazquez, whose donation made the mural possible; and artist Julia Bottoms.
Association; the Jacobs School’s Office of Inclusion and Cultural Enhancement; the Office of Medical Admissions; the Office of the Dean at the Jacobs School; the Office of Medical Advancement in University Advancement; the art committees of UB; the Jacobs School’s facilities team; and Jacobs School medical alumni, students and faculty/staff models.
Featured on the mural are Olutalabi, MD, and Yamini Mulla, MD, UB medical residents; Fabrizio Passalacqua, MD Class of 2026; Ifeoma Ezeilo and Seoyoung Han, both in the MD Class of 2025; Jazmin Corral and Jitendra Singh, doctoral candidates; Narayan Dhimal, PhD, alumnus; Jessica A. Donhauser, MD, alumna and clinical assistant professor of pediatrics; and Parveen Attai, MD Class of 2027.


WATCH: Time-lapse footage brings the mural to life in less than a minute.
By Ellen Goldbaum
Growing up in Elkins, West Virginia (current population 6,800), Nancy H. Nielsen, MD ’76, PhD, could not have fathomed that she would one day not only meet the president of the United States but would work with his administration to completely transform health care in America.
Now her work on the Affordable Care Act, from advocacy to implementation, has been documented for posterity in the Obama Presidency Oral History.
Nielsen, senior associate dean for health policy in the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, is one of the “extraordinary people from all walks of life” invited to participate in the Obama Presidency Oral History project.
Compiled by Columbia University, the history is based on more than 1,000 hours of interviews with hundreds of people. Just being invited to do the interview was an incredible honor, Nielsen said. It also gave her a chance to review how she came to take part in one of the most significant health care reforms in the U.S.

In 1973, with a PhD in microbiology and a faculty position at the Jacobs School, Nielsen was accepted to the UB medical school. She was a “nontraditional” student, since she already had a faculty position and was also raising five small children. She was one of just 30 women in her class of 135.
After graduating and serving as the first woman chief resident in internal medicine at Buffalo General, Nielsen was board-certified as an internist. In addition to running a busy private practice, she was drawn to the policy side of medicine. She served as president of the Erie County Medical Society, became involved with the state medical society and started working at the national level.
She served four consecutive terms as speaker of the American Medical Association House of Delegates, and in 2008 was elected AMA president, a term that coincided with the intensifying national health care debate.
While Nielsen was president-elect, the AMA launched its Voice for the Uninsured campaign, advocating for health care reforms that would extend health insurance coverage to Americans who didn’t have it.
In preparing for the campaign, the AMA media relations staff asked if Nielsen had any patients who were uninsured.
That’s when Nielsen revealed that she had once been uninsured.


WATCH: Nancy Nielsen discusses her background, her role in the passage of the Affordable Care Act, and what it was like being part of the Obama Presidency Oral History Project.
“During graduate school, I delivered two babies when I was uninsured,” she said, “and that became the cause of my life: to make sure all Americans got health insurance.”
She recalled that at the time the Affordable Care Act was passed, 19% of the U.S. population had no health insurance.

“It really was a national scandal, to tell you the truth, and there were places where it was even worse than that,” she said. “There is nothing good about being uninsured. That was the whole point of the Voice for the Uninsured. They didn’t have a voice. So we became that voice.”
Once implemented, the Affordable Care Act (ACA) cut the uninsured rate in the U.S. from 19% to 9%. It would have cut it even more, Nielsen explained, but the U.S. Supreme Court intervened and said the expansion of Medicaid, which was supposed to insure millions, was a states’ rights issue.
Since then, more states have come on board. Nielsen said it’s now down to about 10 states that haven’t expanded Medicaid, about half of which are considering it, or are about to expand.
A few months after Nielsen finished her term as immediate past president of the AMA, she got a call from the White House. She was asked to come work at the newly established Innovation Center in the Center for Medicare and Medicaid Services in the Department of Health and Human Services.
“It was a brand-new part of HHS, and they said they needed me to come to bring the physician voice, as they were implementing this new part of the government,” said Nielsen.
As senior adviser for stakeholder engagement, she would be “on loan” from UB to the federal government, a stint that would last two years. Her role was to interact with, and share the concerns of, clinicians throughout the health care system.
“UB gave me a chance. I was lucky that the admissions committee let me in, and I will never forget it. My whole career has been here and I’ve just been very fortunate. I owe it all to UB.”
Nancy H. Nielsen, MD ’76, PhD
“The Innovation Center is unique in government,” explained Nielsen. “It was enshrined in the ACA law so that instead of making a big policy change and then having unintended consequences, the Innovation Center would do pilots and actually evaluate whether the care was improved and whether there were savings. That was the purpose. There was no place else in government where there was the flexibility to try something to see if it worked.”
She assumed additional responsibilities working with then-HHS Secretary Kathleen Sebelius, advising on policy and sometimes attending events when the
secretary could not.
“It was just an extraordinarily exciting time and I loved it,” recalled Nielsen. She admitted that working in Washington was “seductive,” but she always intended to return to UB.
“I owe my career to UB,” she said simply. “I always wanted to be a physician. I didn’t have money. After my fifth child was born, I finally applied. I was 29 when I started medical school, and my fifth child was 2 months old.
“UB gave me a chance. I was lucky that the admissions committee let me in, and I will never forget it. My whole career has been here and I’ve just been very fortunate. I owe it all to UB.”
Now she’s passing her passion for policy to the next generation of physicians. Nielsen was recently asked to be faculty advisor to a group of Jacobs School students who want to develop a policy elective.
“Why is policy important?” she asked. “Policy is the road map that we use to get to the society we want. For me, it meant getting affordable health insurance for every American. I tell the students, ‘your cause will be different.’ My role here is to help the students change the world, whatever that means to them.”
Nielsen with her extended family after receiving the Jacobs School’s Distinguished Alumni Award in the fall of 2023.













Stories by Dirk Hoffman

It’s not a stretch to say that the treatment of cystic fibrosis is one of the most dramatic success stories in modern medicine.

During the 1950s, a child with cystic fibrosis (CF) rarely lived long enough to attend elementary school. Today, many people with CF are achieving their dreams of pursuing careers, getting married, having children and living into retirement.
Over the past three decades, critical aspects of that dramatic success story have unfolded in the laboratories and clinics of faculty members in the Jacobs School of Medicine and Biomedical Sciences.
On the following pages, we share a handful of stories that examine the changes transforming CF care and what UB’s role has been in these developments, starting with development of the cystic fibrosis transmembrane conductance regulator (CFTR) modulator therapies. These therapies precisely correct the malfunctioning protein that is made by the CFTR gene.
real, tangible improvements in patients’ lives. Patients describe how they had grown up thinking their lives would be prematurely cut short and now find themselves able to live fully into adulthood.

The first patient in the U.S. in a multisite clinical trial of CFTR modulators was enrolled in Buffalo in 2009. The first of these drugs was approved for adults with CF in 2012, and this past February it was approved for use in infants as young as 1 month old. If diagnosis is made that early, UB researchers say, this drug can prevent most CF symptoms from occurring, an almost unimaginable improvement in the patient’s quality of life compared to those born just 10 or 20 years earlier.
Through all the stories, a single theme emerges: how dramatically the research breakthroughs have led to
“Honestly, we owe everything to Dr. [Carla] Frederick and that team in Buffalo, including Dr. [Drucy] Borowitz, who was my doctor my whole childhood,” said Carley Gelder, 27, who tested positive for CF prior to birth but now works full time as a pediatric nurse and got married last year. “They are family to us … there are not enough words to describe how grateful I am.”


“Honestly, we owe everything to Dr. [Carla] Frederick and that team in Buffalo, including Dr. [Drucy] Borowitz, who was my doctor my whole childhood.” Carley Gelder, 27






Four Jacobs School faculty members involved with cystic fibrosis recently sat for a roundtable discussion on the state of the disease, new therapeutics and clinical guidelines, and some of the new challenges facing the population.



The faculty members are:
Carla A. Frederick, MD, associate professor of medicine. She is an adult pulmonologist who takes care of individuals with CF at the Cystic Fibrosis Center of Western New York. She co-directs the CF research program at the center through the Cystic Fibrosis Foundation’s Therapeutics Development Network (TDN).
Danielle M. Goetz, MD, clinical associate professor of pediatrics. She is a pediatric pulmonologist at Oishei Children’s Hospital and UBMD Pediatrics and director of the Cystic Fibrosis Center of Western New York. She co-directs the CF research program at the center through the Cystic Fibrosis Foundation’s TDN.


Ryan C. Hunter, PhD, associate professor of microbiology and immunology. His lab is a group of microbiologists who focus on the bacterial infections that impact the lungs of individuals with cystic fibrosis.
Beth A. Smith, MD, clinical professor of psychiatry and pediatrics and interim chair of psychiatry and division chief for child and adolescent psychiatry. On the national level, she serves as chair of the Cystic Fibrosis Foundation’s Mental Health Advisory Committee, whose goal is the integration of mental health care into routine CF care. Smith also serves on the CF Foundation’s North American Planning Committee as its pyschosocial chair, and on its Clinical Research Advisory Board.
An excerpt of their conversation is as follows. To read the entire discussion, visit: https://bit.ly/4c8vts7.


What is the current state of cystic fibrosis and the research and clinical care surrounding it?
Goetz: It is an exciting time because for those of us who have been involved with CF for many years, we have seen a lot of changes such as a lot of treatments that we did not have previously. These therapies are helping people live longer lives; they help their pulmonary function and their weight gain. Their overall quality of life improves.
Frederick: When I first started in medicine, I saw so many young patients that did not have a very long life expectancy. Now, it is almost like a midcareer change for me. Earlier in my career, I was caring for adults who were inevitably getting sicker and who were going for lung transplants, on oxygen, and would need to apply for disability.
Now, in addition to routine daily care, the most common issues adults with CF face are things like thinking about careers, figuring out what they are going do with their life that they never thought they would have to do before—having kids, having grandchildren.


In Buffalo, we have a high percentage of people who have access to CFTR modulator therapy. We currently have 116 adult patients and 68 pediatric patients. It has completely flipped from when we started. There used to be more pediatric patients than adult patients.
Hunter: From a research perspective, it is an exciting time as well. We are most interested in the bacterial infections of the lungs and the nature of those are changing. With these modulator therapies, lung function is improving.
The pathogens are still hanging around, but lung function is getting better. It’s interesting to think about what airway infections are going to look like, moving forward. We are shaping our research in that direction, just trying to think about what lung infection might become, but also some of the comorbidities as well.
For instance, there is an increased risk in colorectal cancer in the aging CF population, so my lab is also now thinking about gut microbes and what kind of role they might play in gastrointestinal manifestations of the disease.



Can you speak to the importance of multidisciplinary teams at the CF centers?
Goetz: I think they are a key to the outcomes we have had, even prior to the modulators. The concept of a multidisciplinary care network idea started in the 1960s. In 1997, it became more standardized as there was a guidebook made by the CF Foundation and others.
Key team members are respiratory therapists, dietitians, social workers/mental health providers, physicians and nurses, along with other subspecialists.
Having that team has helped us in our assessment and treatment of the patients. We are assessing the whole person and making sure we are addressing all aspects of care. Each person focuses on and becomes experts in the area of the daily treatments that patients with CF have to undergo.

It is a collaborative effort. We do a lot of pre-visit planning, prior to the clinic visits and try to include the patients in that.

Goetz: In children, we are doing observational studies on preschoolers who are on Trikafta, and seeing what happens to their growth parameters and pulmonary function.
We are also doing surveys on personal experience with Trikafta in adolescents. We received a grant from the CF Foundation for all the newborn screening programs at the CF centers in New York state to assure all people with CF and their families have genetic counseling from a genetic counselor trained in CF. This is important due to the increasing complexity of CF genetics and to address unique CF mutations in diverse populations.
Frederick: We are involved in a rollover study from a head-to-head trial between current modulator therapy (elexacaftor/tezacaftor/ ivacaftor) versus a once-a day alternative. It is in the rollover phase where everyone is getting the once-a-day alternative therapy. Taking a pill twice a day versus once-a-day may seem simple, but it isn’t. There is not a one-size-fits-all. Some people may feel that the current therapy is not good enough because side effects happen— weight gain, mental health side effects such as anxiety, etc. Some simply do not have as strong of an improvement as desired. These therapies are life-changing, so more personalized medicine is in the works elsewhere to help make that therapy really great for everybody.

We also have the longest longitudinal database for depression and anxiety screening and are looking at the longitudinal trajectories of depression and anxiety in patients with CF 12 years and older and associations with important health outcomes.
Is there something about Buffalo or UB’s collaborative spirit that helps your efforts?
Smith: When I first got involved with Drucy (Drucy S. Borowitz, MD, who served as the Cystic Fibrosis Center director at the former Women & Children’s Hospital of Buffalo for more than 25 years) and some of the other pulmonologists, they were excited to have a child and adolescent psychiatrist who was interested in chronic illness and recognized the need for that.
They were doing collaborative care before it was called collaborative care. I was brought in as another specialist and wound up spending my career in CF because of the multidisciplinary nature and the spirit of collaboration.

Goetz: I became the CF center director in 2014, so we did a year where Dr. Borowitz and I were co-directors before that. She mentored me and we transitioned, but then she was still here until she went to the CF Foundation. Even while working at the CF Foundation, Dr. Borowitz was always there as our mentor. She was always in our corner, always available.
We are trying to carry on the tradition she started.
Smith: Buffalo is a small center and yet we are involved in so many of these groundbreaking CF research projects. We have such a cohort.
I think it is due to Dr. Borowitz and her culture that patients and their families are very giving of themselves to our studies. Our rates of participation in studies are higher than most centers. Although we are small, we are mighty.
And the individuals are a part of this team of researchers. We have patient advisors on every one of our grants. And all of the educational materials are co-written with individuals with CF. It has been just a great experience because many of them have said, “I never thought I was going to be a researcher” or “I never thought I was going to be an author.”
Smith: In addition to the medication trials, we’ve had a few mental health trials. We worked hard on a randomized, controlled trial of a cystic fibrosis-specific cognitive behavioral intervention for depression and anxiety. We are now in the adolescent pilot phase of the study.
Buffalo is also involved in a national randomized, controlled implementation trial. We are implementing different models of how to disseminate this cognitive behavioral therapy that is specific to CF, and we are studying it in a randomized way. Buffalo is also the lead site in a multisite project to develop a CF-specific general mental health screener to pick up on other important and impactful mental health conditions in addition to depression and general anxiety for adults with CF.


Goetz: We are working on a CF Foundation position paper that I am helping to write in a group that includes patients and parents. It is asking the question if we need to change the care model now that we have modulators.
Patients and families should be a part of those discussions because they are the ones living it.
Smith: Their lived experience puts everything that we do into context. They are able to look at what we are producing and give us that feedback.
There is so much resilience in this population. Their survival stories are now thriving stories.



Drucy S. Borowitz, MD, clinical professor emeritus of pediatrics at the Jacobs School of Medicine and Biomedical Sciences, has been a leading figure in cystic fibrosis care and research in Western New York for decades.


She directed the Cystic Fibrosis Center at the former Women & Children’s Hospital of Buffalo (WCHOB) for more than 25 years, where she also served as chief of pediatric pulmonology.
Borowitz is an internationally recognized expert in nutrition and the involvement of the intestine and lung in cystic fibrosis and was a leading researcher of enzyme replacement therapy to correct digestive abnormalities in cystic fibrosis patients.
She led the CF Therapeutics Development Center at WCHOB, which helped in the development of the breakthrough drug ivacaftor—a cystic fibrosis transmembrane conductance regulator (CFTR) modulator. The first patient in a multisite clinical trial study was enrolled in Buffalo in 2009.
“Ivacaftor was a ‘proof of concept’ medicine. Although it did not treat the most common CF

mutation, it was the first time we used a CFTR modulator,” Borowitz said. “If it hadn’t worked, it would have meant that we were going down a blind alley and would have to start all over. Ivacaftor has been used in combination with other modulator drugs to ‘fix’ the CFTR protein produced by other CFTR mutations, some of which are common and some of which are quite rare. Ivacaftor is a basic building block of modulator therapy.”
When drugs are developed, they are usually tried in adults first, with a steady expansion of age eligibility once safety studies are complete.
In February 2024, ivacaftor was approved for use in infants as young as 1 month of age.

“Using this powerful drug shortly after the diagnosis is made can prevent most symptoms of CF from occurring,” Borowitz said.
Borowitz says the newest medication has dramatically changed the course of the disease for many people with CF. (It’s actually a combination of three drugs: elexacaftor-tezacaftor-ivacaftor; brand name Trikafta, often called ETI).
“People with CF did not live beyond childhood when Dr. Erika Bruck, the first ‘CF physician’ in Western New York started to provide care,” she said. “By the time I started in 1989, some people with CF were living to mid-adulthood, but not most. There were still many deaths of people in their teens and 20s.

“The CF Foundation now estimates the median survival for all people with CF in the U.S. to be 56 years of age or older,” Borowitz added. “Our expectation for children and young infants who are able to start modulator drugs such as ETI early in life is that they will have a full lifespan.”


“Our Therapeutics Development Center in Western New York helped to study almost every drug of the modern CF era,” she said. “Progress has been incremental and many of the drugs we studied and helped bring to market are not as transformative as ETI but are still important.”
Borowitz noted one of the great things about ETI is that it improves function in many parts of the body. For example, women with CF often had problems becoming pregnant or chose not to because of poor lung function.
“We have seen a ‘baby boom’ since ETI became available. CF is an autosomal recessive disease. Those babies are CF carriers but will only have a chance to have CF if the father is a carrier,” she said.
ETI is not a complete panacea and research continues into treating ongoing problems, Borowitz noted.
and caring about each other have enabled successful collaboration.”
Borowitz said she also “truly admires the resilience of people with CF and their families.”
“They have had to commit to following a treatment plan every day. In an odd way, as we developed more drugs to keep people stable and their life expectancy increased, the complexity of the treatment was at odds with people feeling better and wanting to lead a full life.”

“Some people still have challenges with difficult-to-treat infections or gastrointestinal issues. Some people cannot tolerate ETI and other modulator drugs are being studied, with a new combination drug being reviewed by the FDA this year,” she said. “And some people have mutations that make them unable to ever be treated with any modulators.
“Gene editing, gene therapy or mRNA treatment could help them and all people with CF, but the science is very complex.”
Borowitz said she is forever indebted to all of the people with CF and their families who participated in more than 60 clinical trials in Western New York.

After retiring from UB in 2016, Borowitz joined the CF Foundation as its senior vice president of community partnerships, where she led numerous initiatives to improve patient care and advance new treatments before retiring in 2020.
Even in retirement, Borowitz continues to improve the lives of people with CF. About 85 percent of people with CF have a pancreas that doesn’t work, and they need to swallow many capsules with digestive enzymes before every meal and snack to prevent malnutrition.

“There have been very few improvements in these enzyme supplements since the 1970s,” she said. “Although modulators can improve pancreatic function in some children, most
people with CF still have to take enzyme supplements.”
Borowitz is working with a small biotechnology company as a scientific advisor and board member to use what has been learned over the years to create a better enzyme. Using machine learning, they have engineered a more potent enzyme that could be a single small pill or even a liquid. Phase 1 trials are currently underway.

Borowitz is an internationally recognized expert in nutrition and the involvement of the intestine and lung in cystic fibrosis and was
a
leading researcher of enzyme replacement therapy to correct digestive abnormalities in cystic fibrosis patients.
“In addition, our research coordinators, especially Nadine Caci and Chris Roach, have played key roles in explaining the various studies, answering questions, and going out of their way to make participating in a clinical trial as smooth as possible,” she said.
“Despite many challenges, we have had a stable team over many years. Truly caring about the lives of people we serve

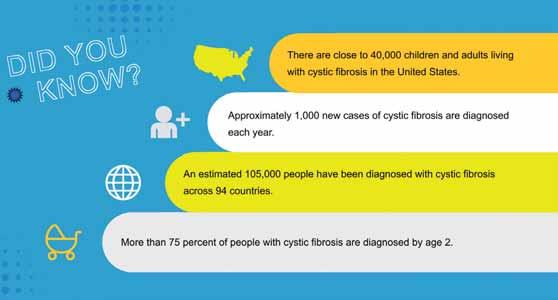

The Argentieri family of Hornell, New York, is living proof of the wondrous scientific and medical advances that have been made in the treatment of cystic fibrosis.
Colleen and Fran Argentieri have three adult daughters, two of whom have CF, yet both are thriving: working full time, getting married and starting families.
But their road to bright futures was a winding one, sometimes paved with uncertainty.
The couple’s oldest daughter, Alexandra Fitzpatrick, 33, was diagnosed with CF at 15 months old.
“We had been taking Alexandra to a gastroenterologist pediatric specialist for 10 months and she was getting progressively worse, so we decided we needed to take her to the former Women & Children’s Hospital in Buffalo, and they shared with us they were going to do a sweat test for CF,” Colleen said.
The Argentieris went to their local library to read about CF and learned that people afflicted with the disease suffered terribly and many of them died before entering kindergarten.
They were devastated.
Shortly after they arrived home, they received a telephone call informing them that Alexandra’s test results were positive. The family returned to the lung center the next day to meet with Drucy S. Borowitz, MD, and an entire team of specialists—a pulmonologist, social worker, respiratory therapist and nutritionist. Alexandra was immediately placed on enzymes to help with her pancreatic insufficiency.
That same week, Colleen, found out she was pregnant with her second daughter, Ashtin McKercher, 31. The couple had an amniocentesis performed and found out Ashtin did not carry the CF gene.
A few years later, their youngest daughter, Carley Gelder, 27, tested positive for CF prior to birth and immediately began undergoing treatments as a newborn.

“One of the things Dr. Borowitz told us in that first meeting was not to let this disease define our children and not to put limitations on them. She said we could look at it as a curse or a challenge,” Colleen said.
“Those words really resonated with us, so they were involved in all kinds of sports. We allowed them to define their own limitations,” she said.
“My mom and dad never let us believe there was not anything we couldn’t do. My sister and I both played all the sports, we were starters on our soccer team,” Alexandra said. “We played basketball and Carley was a cheerleader who won at States.”
When Alexandra reached age 12, she started needing to be hospitalized from time to time. Carley had severe sinus issues and at the age of 6, she had her first sinus surgery. At 9, her pulmonary functions were dropping, and she had severe reflux, necessitating fundoplication surgery, where the stomach is sewed around the esophagus.
“Both of them had the Bard Button
gastrostomy feeding tubes that go directly into the stomach. They would have nightly feeds to increase their weight gain,” Colleen recalled.
“Their daily routine was to remove the feeding tube in the morning, hook themselves up to their chest vest and do chest physical therapy exercises for 30 minutes, take two medications to help open up their airways so the mucus could come out when they did their chest PT, take more medications, including an inhaled antibiotic that they had to do through a nebulizer.
“Then they would go about their day, come home and do chest PT again. In the meantime, they would also be taking enzymes every time they ate anything. And then at night we would hook them back up to the feeding tubes.”
Alexandra says despite the grueling daily routines, she and Carley led otherwise normal lives and rarely thought about the difficulty of living with a disease that may not be outwardly apparent.
At one time, Alexandra was on 11 different forms of medication throughout the day.
“Despite doing all the right things, the disease just takes control of the lungs,” Colleen said. “She went off to college and after she got a four-year degree, her health began to drastically and quickly decline.”
Alexandra had advanced lung disease. She was eventually placed in a medically induced coma, intubated and placed on a respirator, and flown by medical transport to New York-Presbyterian Hospital/ Columbia University Irving Medical Center where her condition could be stabilized, and she could be considered for a double lung transplant.
Because the respirator was not sufficient to keep Alexandra alive, she was also placed on a second form of life support, an ECMO (extracorporeal membrane oxygenation) machine. An evaluation period was still needed to qualify for the transplant list.
Awakened from the coma after four days, Alexandra was required to get up and walk each day as part of the evaluation process in order to prove she was a viable candidate for a double lung transplant.
“Since she was in such critical condition, she was number one on the transplant list. For an agonizing three weeks, they kept her alive until a set of lungs became available,” Colleen said.
Alexandra remembers being very scared at the time.
“I always took care of myself so when I ended up needing a transplant, that was kind of a shock to me. It came very quickly. I crashed and burned within six months.”
Alexandra was doing her chest physical therapy four times a day and was on IV antibiotics constantly.
Borowitz was her primary doctor when she was young, and Carla A. Frederick, MD, and physician assistant Lynne Fries took over her care when she was 20.
“Dr. Frederick has kind of become one of my best friends. I remember when I was sick, she told me that no matter what happened she promised she would keep me alive, and she did,” Alexandra said.
‘IT’S ALMOST LIKE A DIFFERENT LIFE’

After the double lung transplant, Alexandra’s life changed dramatically.
“It is a whole different world for me now because I do not have to do any treatments. It all just suddenly stopped—no more chest physical therapy, no more breathing treatments, no more IVs,” she says.
Alexandra works full time for Fairleigh Dickinson University as the prospect manager of research and database. She is married to her high school sweetheart and last November, the couple welcomed a son, Brooks, their biological baby through gestational surrogacy.
“The advancements in science afforded her a second chance to live. Weighing
only 48 pounds at the age of 25, in prior years, she would never have been selected to receive a lifesaving transplant,” said Colleen.
Both Alexandra and Carley also credit Fries, part of the adult CF care team, as being an influential component in their health care.
does chest PT every couple of days.
“I still take my enzymes and my medications, but my overall day-to-day life

“The night that I was rushed to Buffalo General prior to my transplant, Lynne was the one behind the scenes calling in my team from Women & Children’s to make sure I was cared for properly to be kept alive,” Alexandra said.
“We truly could not have asked for a better care team,” Carley said. “My sister and I are both so fortunate to have had both Lynne and Dr. Frederick continuously care for us. Neither one of us would have the life and health that we do without either one!”
Trikafta, a fixed-dose combination medicine consisting of a chloride channel opener and two cystic fibrosis transmembrane conductance regulator modulators, was approved for use in the United States in October 2019.
Around that time, Carley Gelder’s life was taking a turn for the worse.
“I struggled just going to work. I was drastically going down the same path as Alexandra. I did not have the energy to do anything.”
Carley had been a bit healthier than Alexandra throughout her life due to being treated from birth and due to the advancements in treatments, her mother said.
But after going to college and getting a nursing degree, her health started to decline.
After being hospitalized in late 2019, Carley began taking Trikafta and her life took a 180-degree turn for the better.
“Taking Trikafta truly changed my life. Before, I was in and out of the hospital every three or four months.” Carley said. “Since I started taking Trikafta, I have not been back to the hospital.” When she was sick, Carley was doing her treatments three times a day. Since taking Trifakta, she only
is so different now,” Carley added. “I don’t have to sit on my couch for 30 to 45 minutes and do my treatments to feel good, to feel like I can take a deep breath or prevent myself from coughing all day. It is very, very different than what I was living like before.”
Carley got married last December and works full time as a pediatric nurse.
“I always knew that I wanted to be in health care and wanted to make a difference for people,” she said. “Going into nursing felt like a calling to me.”
Carley sees Frederick, Fries and the rest of the CF team in Buffalo every three or four months for checkups.
“Honestly, we owe everything to Dr. Frederick, Lynne, and that team in Buffalo, including Dr. Borowitz who was my doctor my whole childhood. They are family to us,” she said. “With everything Alexandra went through and Dr. Frederick and Lynne fighting for her, there are not enough words to describe how grateful I am.”
“Who could have dreamt that our two children with cystic fibrosis would be at this point in their lives?—breathing easy, having careers, getting married and starting to have families. That truly is a dream come true,” Colleen said.
“It marks the first time in our lives, for my husband and me, that our children have all been well and healthy. We have a lot to be thankful for. We are so blessed.”
Interprofessional collaboration was the theme during the 2024 Harrington Lecture as part of the University at Buffalo’s Alumni Weekend.
“The bottom line is that team science matters. Team science has the most impact,” said Lawrence A. Tabak, DDS, PhD ’81, principal deputy director at the National Institutes of Health (NIH), who gave the keynote address titled “Collaborative Frontiers: Exploring Interdisciplinary Science and Leadership.”
In her introduction of Tabak, Allison Brashear, MD, MBA, UB’s vice president for health sciences and dean of the Jacobs School of Medicine and Biomedical Sciences, made note of his doctoral degree in oral biology and his advanced certificate in endodontics, both from UB’s School of Dental Medicine.
Prior to joining the NIH, Tabak was the senior associate dean for research and professor of dentistry, biochemistry and biophysics in the School of Medicine and Dentistry at the University of Rochester. He served as acting NIH director from December 2021 to November 2023.
Brashear noted the Jacobs School has over 80 faculty members who have funding from the NIH supporting 122 research projects, the combined amount of which is $51 million, making up more than 50 percent of NIH awards across the entire university.
“Thanks to the NIH, our faculty are undertaking groundbreaking research that addresses some of the most critical health care challenges. Their work is shaping the future of medicine,” she said. “Our goal is to have UB be a leader in research that impacts health. Our goal is to improve health and increase the lifespan here in Western New York and across the country.”
Brashear said Tabak, as an alumnus of UB, “embodies the spirit of collaboration that defines our institution.
“His tireless efforts have fostered interdisciplinary partnerships, bridging the gap between dentistry, medicine and biomedical research,” she said. “His remarkable journey has left an indelible mark on the field of dentistry and the broader health sciences community.”

“Dr. Tabak is a true champion of interprofessional collaboration and a beacon of inspiration for all of us at UB,” Brashear added.
In his opening remarks, Tabak said that “UB was very important to my career development, so it is wonderful to be back here.”
He noted that following dental school, he wanted to get a doctoral degree and at that time there were only two programs in the country available to dentists who wanted to get a PhD, one of which was at UB.
Tabak said he was fortunate to be able to work with Michael J. Levine, DDS, PhD, who was a relatively new faculty member at UB at the time, and who was the first DDS/ PhD student at UB.
“He taught me how to be a rigorous scientist; lessons I use to this very day,” he said.
Tabak gave a brief view of the NIH and its priorities.
“We support basic research to fuel progress, translational research to move the basic discoveries forward, and clinical research to turn the discoveries into prevention, treatments and cures.”
Panelists discuss innovative ways to encourage interprofessional collaboration.

Tabak then displayed a graphic of the NIH, noting “only the Congress of the United States could create something like this—27 different institutes and centers.”
“The first one and largest is the National Cancer Institute and the last one was the National Center for Advancing Translational Sciences and there is everything in between.
“We are legally decentralized because each institute gets its own individual appropriation directly from Congress, but notice how siloed this structure is,” Tabak said.
The NIH’s budget for this fiscal year is $47.4 billion.
“Eighty percent of that is spent supporting institutions like this one,” Tabak noted.
Tabak concluded his talk by pointing out the NIH continues to fund more and more multi-authored team science.
“His tireless efforts have fostered interdisciplinary partnerships, bridging the gap between dentistry, medicine and biomedical research. His remarkable journey has left an indelible mark on the field of dentistry and the broader health sciences community.”
Allison Brashear, vice president for health sciences and dean of the Jacobs School
“The more authors you have, the more impact the publication has, as measured by something we call the relative citation ratio,” he said. “We have done some experiments on our own intramural program and we find that if we look at that impact factor, when more institutes are collaborating on the research, the impact factor goes up.”
The June 1 event was made possible by the D.W. Harrington Lecture Endowment. The Harrington is UB’s longest-running lecture series, established in 1896. The event is a collaboration between partners in the Jacobs School, the Medical Alumni Association, Office of Medical Advancement and the Office of Graduate Medical Education.
Following Tabak’s lecture, he was invited to sit on a panel to further discuss interprofessional collaboration, which was moderated by Nicholas M. Fusco, PharmD, interim executive director of interprofessional education at UB.
Other panelists were:
• Marcelo W.B. Araujo, DDS, PhD, dean of UB’s School of Dental Medicine
• Remi Adelaiye-Ogala, PhD, assistant professor of medicine
• Liise Kayler, MD, professor of surgery, chief of the Division of Transplant Surgery and program director of kidney and pancreas transplantation
• Ranjit Singh, MB BChir, MBA, associate professor of family medicine and vice chair for research in the Department of Family Medicine
As part of Reunion Weekend 2024, the Jacobs School presented Distinguished Alumni Awards to:
Lawrence A. Tabak, DDS, PhD ’81, who is the first to receive the new “Distinguished Health Sciences Alumnus” award. Tabak is the principal deputy director of the National Institutes of Health.
Tabak continues to lead an active research laboratory within the NIH intramural program studying glycoprotein biosynthesis and function in addition to his administrative duties.
Lillian Vitanza Ney, MD ’64, who received the “Distinguished Medical Alumna” award.
Vitanza Ney is a retired cardiologist and former medical director and vice president of WCA Hospital. She also was the coordinator of Jamestown Area Medical Association and was an interim acting medical director of Heritage Park Health Care Center.
She also stepped in to serve a short term as acting county health commissioner for the Chautauqua County Health Department in 1975.
Andrew I. Soiefer, PhD ’84, who received the “Distinguished Biomedical Alumnus” award.
As an expert in chemical risk, Soiefer is one of a small group of occupational toxicologists setting safe exposure levels for chemicals in the workplace.
He was board certified in toxicology in 1990 and maintained certification for 30 years. He is a full member of the Society of Toxicology and the American Chemical Society.
In 1999, he started North Jersey Toxicology Associates, LLC, a consulting firm providing environmental, health and safety services to the pharmaceutical and chemical industries.
For the next 18 years until his retirement, Soiefer was chief scientist at NJTA.
Daniel Alexander, MD ’99, who received the “Distinguished Volunteer of the Year” award.
Alexander, along with his spouse, Gail Alexander, served as UB’s Boldly Buffalo campaign co-chairs, leading the way to helping the university surpass its billion dollar campaign goal—the largest in SUNY history.
The Alexanders are the founders of Finger Lakes Bone and Joint Center. Dan worked as an orthopedic surgeon and Gail served as practice administrator until they sold the business to Rochester Regional Health in 2016.

Over 250 alumni and guests returned to Buffalo on May 31 and June 1 for a memorable reunion weekend. Representing 26 different states, attendees enjoyed visits to Buffalo’s cultural and historic landmarks, including the AKG Art Museum, the Terrace at Delaware Park, the Buffalo Club, and the Mansion on Delaware Avenue. The weekend provided a wonderful opportunity for alumni to reconnect with classmates, faculty and the medical school.
We are grateful and thank our alumni who made a reunion gift and generously contributed almost $1 million collectively in support of scholarships and unrestricted funding for the school. As always, the reunion tradition continues to celebrate alumni bonds and provide vital support for our school’s priorities.
For more information about the Medical Alumni Association and upcoming events, see the inside back cover.












Orthopaedics resident receives ultimate tribute from national organization, which renamed its courage award in her honor
By Dirk Hoffman

Jessica “Jessi” Block, MD, a trainee in the orthopaedic surgery residency program at the Jacobs School of Medicine and Biomedical Sciences who was the epitome of courageousness during her lengthy battle with an aggressive form of oral cancer, died on Nov. 30, 2023. She was 37.
Block first noticed a sore on the right side of her tongue in August 2021, but initially attributed it to the stress of applying to fellowships. By early 2022, she was having a problem dictating in clinic at Oishei Children’s Hospital and realized for the first time her tongue was deviating to the side. A subsequent biopsy showed that a 4 cm mass on her tongue was squamous cell carcinoma.
Over the next year-and-a-half, Block underwent multiple treatments of chemotherapy and radiation, all while continuing her residency training when she was feeling well enough to do so.
Last year, she was awarded the Ruth Jackson Orthopaedic Society’s (RJOS) annual Courage Award and was presented with the award via teleconference on Nov. 26, just four days before she died.
A contingent of members of the Department of Orthopaedics attended the RJOS annual meeting in February in San Francisco, where Jessi’s mother, Sherri Block, accepted the award on her daughter’s behalf.
The society, whose mission is to promote the professional development of women in orthopaedics throughout all stages of their careers, also announced it has renamed the award as the “Dr. Jessica Block Courage Award” beginning with the 2025 recipient.
Leslie J. Bisson, MD, June A. and Eugene R. Mindell, MD, Professor and Chair of the Department of Orthopaedics, says he was impressed with how much Block continued to focus on developing into an orthopaedic surgeon after receiving her cancer diagnosis.
“She wanted to keep learning and did not want to interrupt her residency training,” he said. “I told her multiple times that she was inspirational in the way that she was handling her illness. She was just an amazingly selfless person.”
Due to Block’s illness, her classmates and colleagues had to go about their daily routines without the full participation of one of their chief residents.
“We depend on our residents. They are an integral part of the educational product that we deliver,” Bisson said. “It was just amazing that everyone just rose to the occasion. A lot of it speaks to the type of person she was. People wanted to step up and do everything they possibly could to help her.”
Block was focused on the subspecialty of arthroplasty and was “incredibly driven and tireless in her work ethic,” said Matthew J. Phillips, MD, clinical assistant professor of orthopaedics, who is the director of the Jacobs School’s adult reconstructive surgery fellowship program.
“She was a self-starter in terms of her own education. Sometimes that is a difficult transition for people to make from being a lifetime student to actually directing your own education, which is what you do when you are a resident,” he said. “She was aggressive about learning. She was always prepared for cases.”
Phillips says Block took the same approach to everything in her life.
“She was very talented, technically. Some people don’t have as much talent, and they work at it, and they wind up being pretty good. With other people, it seems like it is effortless for them. She was a combination of both. She was very good to begin with, but she worked hard to be the best.”
Block matched to a very competitive and prestigious adult reconstruction arthroplasty fellowship at Washington University in St. Louis, Missouri. It was her first choice, and its director, Robert Barrick, MD, is “one of the most recognizable names in arthroplasty in North America,” Phillips said.
“I talked to Dr. Barrick multiple times to let him know where Jessi was at in her treatments and he told me he would keep a spot open for her in the fellowship in perpetuity so that if and when she was well enough to come, she would have a spot. That speaks volumes about what they thought about Jessi.”
Role Model and a Passionate Mentor
Block was also an active mentor and was passionate about helping her fellow residents.
“Jessi was a phenomenal mentor. Even after she became too sick to operate, she still was available to us for mentorship advice, to teach and to offer her insight,” said Ellen E. Lutnick, MD, a PGY-2 trainee in the orthopaedic surgery residency program.
“The word that comes to mind is grace ... she somehow managed a litany of setbacks, pain, disappointment and life-altering circumstances with complete grace.”
Alexander J. Macfarlane, MD, a PGY-5 orthopaedics resident, said, “Jessi was a born leader. She was in a class of her own. I am thankful that she will be remembered and honored by a society that champions excellence in orthopaedics and elevates women in orthopaedics, because Jessi would have no doubt been leading the RJOS or another major society if things would have worked out differently.”
“When I joined the residency program, Jessi was the only other female in the program,” said Lauren M. Harte, MD, a PGY-3 orthopaedics resident. “She quickly became a role model, mentor and good friend of mine.
“Throughout her battle with cancer, we called Jessi our warrior. She was strong and resilient,” Harte said. “She always had a positive mindset, and you would never hear her complain. We all miss her very much. She will always be our warrior.”
Lived Her Life With Perseverance and Grace
Sherri Block says Jessi was always serving others, so she feels becoming a doctor was a natural progression for her daughter.
She mentored female students as an undergraduate at the University of Michigan and also participated in “alternative spring breaks.”
“Instead of going to Florida or somewhere warm and having a party, she went to underserved areas. She went twice to New Orleans right after Hurricane Katrina. She went to inner-city Detroit,” her mother said.
After graduating, Block joined AmeriCorps and accepted an assignment called Operation Safety Net in Pittsburgh.
“That was a group that would go out at night and provide medical care to the homeless. They worked in the alleys and under the bridges,” Sherri Block said.
Block then went to work at an orthopaedics clinical practice in Arlington, Virginia, where her interest for the specialty really blossomed. She later enrolled in a postbaccalaureate program at Drexel University in Philadelphia, and after a year was offered a spot in its medical school class.
“She was very talented, technically. Some people don’t have as much talent, and they work at it, and they wind up being
pretty
good.
With other people, it seems like it is effortless for them. She was a combination of both. She was very good to begin with, but she worked hard to be the best.”
Matthew J. Phillips, MD
Sherri Block says her daughter was surprised when she matched into the orthopaedics surgery residency at UB because she had not done any of her away rotations there and did not have contacts in Buffalo.
“It turned out to be the best thing that ever happened to her.”
Sherri Block says she hopes when people think of her daughter they will remember “that she walked the walk.”
“She approached the cancer with perseverance and grace. That is how she lived,” her mother said. “Jessi loved to teach. She loved to share knowledge with others and encourage others in their life paths. She got excited when others succeeded. It wasn’t a competition with her. She was in competition with herself, but she liked to see everyone win.”
Internationally acclaimed researcher was a SUNY Distinguished Professor and director of Institute for Myelin and Glia Exploration
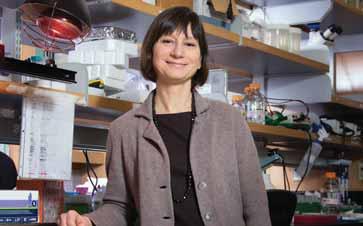
M. Laura Feltri, MD, an internationally renowned pioneer in the study and treatment of myelin diseases in the nervous system, died Dec. 25, 2023, in her native Italy after a long and courageous battle with cancer. She was 60.
A widely respected scholar and a member of the Jacobs School of Medicine and Biomedical Sciences faculty, she was a SUNY Distinguished Professor of biochemistry and neurology in the Jacobs School and director of UB’s Institute for Myelin and Glia Exploration.
She was elected a fellow of the American Association for the Advancement of Science (AAAS) earlier in 2023 for her lifetime achievements.
“Dr. Feltri was an internationally recognized neuroscientist, a mentor to many and a friend to all,” said Allison Brashear, MD, MBA, vice president for health sciences at UB and dean of the Jacobs School.
Her research focused on multiple sclerosis; Charcot-MarieTooth disease, which affects the peripheral nerves; and Krabbe leukodystrophy, a rare, fatal neurological disease that afflicts newborns.
With major funding from the National Institutes of Health, Feltri made numerous seminal discoveries in her field, including developing the first mutagenesis tool for studying the development of Schwann cells, which generate myelin, and the signals that regulate myelination. In collaboration with her husband, Lawrence Wrabetz, MD, she pioneered the use of transgenic animals to
model neurological diseases and develop new therapies.
In her career, Feltri authored more than 140 peer-reviewed research articles.
Numerous national and international organizations sought Feltri’s expertise. She served on the review panel of the Muscular Dystrophy Association and the National Multiple Sclerosis Society. She was first a member and then chair of the Cellular & Molecular Biology of Glia Study section of the National Institute of Neurological Disorders and Stroke of the NIH. She also served as scientific advisor to the Charcot-Marie-Tooth Association, the CMT4B3 Research Foundation and KrabbeConnect.
“Laura was a joy to work with. Despite receiving many accolades, she was self-critical and sought constantly to improve her scholarship, teaching and mentoring,” said Mark R. O’Brian, PhD, professor and chair of the Jacobs School’s Department of Biochemistry. “She made us all better.”
Early in her career, Feltri was awarded the International Society
“Dr. Feltri was an internationally recognized neuroscientist, a mentor to many and a friend to all.”
Allison Brashear, MD, MBA
for Neurochemistry’s Young Investigators’ Colloquia Award. In 2020, she was an invited speaker at the Nobel Mini-Symposium at the Karolinska Institute in Stockholm.
Feltri was an excellent advisor and mentor to numerous undergraduate, master’s and doctoral students, and in 2013 UB’s Office of Postdoctoral Scholars awarded her a Distinguished Postdoc Mentor Award.
She was president-elect of the Peripheral Nerve Society and served on the editorial boards of various journals and the boards of several scientific organizations.
Feltri earned her MD and did her residency in neurology at the University of Milan, Italy. She was a postdoctoral fellow at Thomas Jefferson University. She was a faculty member and head of the NeuroGlia Unit at the San Raffaele Scientific Institute in Milan before joining the UB faculty in 2011.
Survivors include her husband and five children.
Accomplished physician-scientist, educator, clinician was one of the world’s foremost experts on endometriosis

Robert N. Taylor, MD, PhD, assistant dean and program director of the MD-PhD program and professor of obstetrics and gynecology in the Jacobs School of Medicine and Biomedical Sciences, died on Jan. 22, 2024. He was 71.
Taylor was an accomplished physician-scientist, educator and clinician, who had a distinguished 40-year career in medicine and reproductive health. He was among the world’s top researchers studying endometriosis, a chronic, painful and poorly understood condition that affects 5% to 10% of women worldwide.
The author of hundreds of scientific papers, five books and many book chapters, he was a prolific researcher who focused on endometriosis, human endometrial function, uterine biology and embryonic implantation. His laboratory was continuously funded by the National Institutes of Health since 1987 and was focused on investigations of the molecular and cell biology of the human uterus and placenta.
Taylor’s most recent work was focused on the relationship between endometriosis lesions and pain, investigations that may lead to new therapeutic targets for the condition.
Those who knew Taylor, whether in his role as a researcher, clinician or educator, speak of him as a kind, generous and empathetic mentor and colleague.
A recipient of the American Society for Reproductive Medicine Distinguished Researcher Award, Taylor was a frequent lecturer both nationally and internationally.
Taylor joined the Jacobs School faculty in 2020 as an assistant dean and program director of the MD-PhD program, for which he was a strong advocate.
A board-certified obstetrician-gynecologist and reproductive endocrinologist, he served on executive committees of the American Board of Obstetrics and Gynecology, the NIH Reproductive Scientist Development Program and the California Institute for Regenerative Medicine. He was a past honorary secretary of the World Endometriosis Society and past president of the Society for Reproductive Investigation.
He had previously led the MD-PhD program at the University of Utah School of Medicine, where he also held the positions of professor of obstetrics and gynecology, and research director of the Division of Reproductive Endocrinology and Infertility.
Prior to that he was professor and vice chair for research in the Department of Obstetrics and Gynecology at Wake Forest University School of Medicine and was also co-director of its Molecular Medicine and Translational Sciences Program.
He served as the Willaford Leach/Armand Hendee Chair and Professor in the Department of Gynecology and Obstetrics at Emory University School of Medicine, and as assistant, associate and professor and vice chair for research in the Department of Obstetrics, Gynecology and Reproductive Sciences at the University of California, San Francisco.
Taylor completed his residency in the Department of Obstetrics, Gynecology and Reproductive Sciences and a fellowship in reproductive endocrinology, both at the University of California, San Francisco. He also completed a research fellowship in molecular cardiovascular biology at the Howard Hughes Medical Institute, University of California, San Francisco.
He received his undergraduate degree in biological sciences from Stanford University. He received his MD-PhD (Department of Cell Biology) from Baylor College of Medicine in Houston.
He is survived by his wife, Sarah L. Berga, MD, professor and chair of the Department of Obstetrics and Gynecology in the Jacobs School; his brother, Scott Taylor; sons Christopher (Sam Riley) and Patrick (Sarah Wintner); former spouse and mother of his children, Martha Miller Welch, MD; stepchildren, Alexis Sherman-Roe, MD (Allyson), and Nathaniel Sherman (Ellie), and their three children, Ella Scott, Isla and Walker; as well as many cousins in California and New York.
Memorial gifts honoring Taylor may be made to the Robert N. Taylor, MD, PhD, Memorial Fund for Reproductive Medicine at http://giving.buffalo.edu/giveto/01-3-0-09522.
Passionate educator, researcher and mentor made her mark in emergency medicine

E. Brooke Lerner, PhD ’01, MS ’98, BS ’93, passed away on Oct. 4, 2023, after a courageous battle with cancer. She was 52 years old.
Over the past two decades, Lerner dedicated her career to the advancement of pre-hospital care, from spending time as a paramedic to joining her alma mater as a tenured professor and vice chair for research in the Department of Emergency Medicine and serving on the Board of Directors of the National Association of EMS Physicians (NAEMSP).
She continued to work during her illness and had been awarded four more years of funding as the principal investigator to lead research on improving pre-hospital care for children through the federally funded Pediatric Emergency Care Applied Research Network (PECARN), for which she was a past chair of the steering committee.
“I realized I was putting myself in a box before I was really in a box,” she said about returning to work. “I love what I do and I love using my brain, so I worked with my chair to come back … with an eye on succession planning and all those hard conversations.”
Following her diagnosis, she also worked with the NAEMSP and the GMR Foundation for Research and Education to establish the E. Brooke Lerner Research Fund with the goal of supporting early career EMS researchers.
See Brooke Lerner discuss her decision to create a legacy for others:
“I’ve spent my career on improving pre-hospital care, and I wanted to leave something behind to keep that legacy moving forward,” she said shortly after creating the fund in 2022.
In lieu of flowers, the family requests that donations be made to that fund.
Survivors include her husband and two children.
Illustrious researcher whose seminal discovery identified and characterized the first mechanosensitive ion channels

Frederick Sachs, PhD, a world-renowned biophysicist and a SUNY Distinguished Professor of physiology and biophysics at the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, died Dec. 27, 2023, at the age of 82.
He began his career at UB in 1975 as an assistant professor.
His greatest lifetime achievement—and one that will undoubtedly stand the test of time—is his profound contributions to the field of biomedical research called mechanical transduction.
In 1983, Sachs made his seminal discovery, identifying and characterizing the first mechanosensitive ion channels. Found in every cell of the body, these sensors form the basis of our senses of hearing, touch, balance and tissue volume.
His laboratory rapidly became a center for work on mechanosensitive ion channels, and researchers from around the world visited to learn techniques used to study these channels in different cells.
Sachs was awarded the 2013 Kenneth S. Cole Award from the Biophysical Society. He received the award—given to only one investigator annually—for his significant contributions to the understanding of cell membrane biophysics.
He was nominated for the Nobel Prize in Physics in 2011 by Alexander Petrov.
He earned his doctoral degree in physiology from the SUNY Upstate Medical Center after earning a Bachelor of Arts degree in physics from the University of Rochester.
He is survived by his wife, Jane Jacobson, and his four children: Shana Pergande, Janna Willoughby-Lohr, Benjamin Sachs, Bobbie Sachs, four grandchildren, and two brothers, Jon and Dan Sachs.

“I am so grateful and excited to serve as the president of the Medical Alumni Association this year. I look forward to activities with our alumni, faculty, residents, students, and connecting with you!” – Melissa L. Rayhill, MD ’10
Save the Date!
May 2-3, 2025
Alumni Reunion Weekend and Harrington Lecture
Welcome Cocktail Reception
Distinguished Alumnus Awards
Exclusive class dinners for reunion classes ending in 5s and 0s.
Nominate a Deserving Alumnus Today!
Honor an individual who has outstanding achievements as a physician or a biomedical scientist, has shown personal leadership and provides exemplary services to their community!
Nominate a Distinguished Alumnus/Alumna today!

Thursday, Oct. 10, 2024
Jacobs School of Medicine and Biomedical Sciences
5:30 p.m.
We Want to Hear from You!
Have news? Stay connected and share your updates with fellow alumni.

To learn more about the above and to get more involved, contact Jennifer Britton, Senior Director of Alumni and Constituent Engagement, at (716) 8292586, or ubmed@buffalo.edu.
Donnica Moore is a SUNY honorary degree holder and a highly regarded national women’s health advocate. As president of Sapphire Women’s Health Group, she is also a prominent physician educator, media commentator, and host of both the podcast “In The Ladies’ Room with Dr. Donnica” and the popular health website DrDonnica.com. This program will focus on health care advocacy and the role of media in health education, featuring discussions and shared experiences.


One historic campaign, nearly 84,000 donors and more than $1 billion raised
Because of the overwhelming generosity of alumni, donors and friends, more UB students will achieve their dreams, and UB will continue changing the world for the better. Learn more at buffalo.edu/campaign.
