UIC Applied Health Sciences
MAGAZINE


YOCHAI EISENBERG IS MAKING CITIES MORE ACCESSIBLE FOR PEOPLE WITH DISABILITIES
WINTER 2024
New scholarship a vote of confidence for firstgeneration OT students
Intermittent fasting: is it safe and effective?
MESSAGE FROM THE DEAN

Optimizing
For the past several months, I have been talking about three major principles, using the acronym OMG:
O for Optimizing our academic programs
M for Modernizing our facilities
G for Greater diversity in everything we do.
Of course, three letters can’t convey the complexity of our college or fully address our short- and long-term challenges.
What does optimization mean and how do we know we have achieved it? Are we meeting the needs of the communities we serve? Are we innovating to make a positive impact on their health? We will identify objectives and measurable goals, going back to the basics—student enrollment, retention and graduation rates, grants submitted, papers published, research expenditures, patients served, scholarships given and gifts received.
Modernizing
Our facilities were built in the 1940s for far different purposes than today. We will work with our stakeholders to prioritize years of deferred maintenance and create a modern space for learning, teaching, research and high-quality clinical care.
Greater diversity
Our most important asset is the diversity of our students, faculty and staff. A diverse biomedical workforce produces better health outcomes; research findings from diverse scientists are more impactful.
We are starting an undergraduate research training program for underrepresented students. Called Enhancing Cross-disciplinary Innovation and Training for Opportunity (EXITO), it will help identify, recruit and train underrepresented students to become scientists while they complete their undergraduate training.
In this issue of AHS Magazine, we bring you examples of our excellence. DHD researchers developed tools to create more accessible cities. Kinesiology students assisted Chicago Marathon runners. BHIS faculty raised ethical questions to consider in studies of chronic pain. And OT professor emerita Gail Fisher established a scholarship for first-generation college students like herself.
Our future looks bright, our students are exceptional, and our faculty and staff are working together to take the college to the next level. OMG indeed!
 Carlos J. Crespo Dean and professor College of Applied Health Sciences
Carlos J. Crespo Dean and professor College of Applied Health Sciences
UIC Applied Health Sciences Magazine
Winter 2024
EDITOR
Erika Chávez
Director of marketing and communications
DESIGN
Heidi Schlehlein
Webmaster and graphic designer
CONTRIBUTING WRITERS
Sonya Booth, Rob Mitchum, Kelsey Schagemann, Emily Stone and UIC News contributors
CONTRIBUTING PHOTOGRAPHERS
UIC Creative and Digital Services, UIC Office of Strategic Marketing and Communications
©2024 University of Illinois Chicago.
All rights reserved. Published by the Office of the Dean, UIC College of Applied Health Sciences, 808 S. Wood St., 169 CMET, Chicago, IL 60612-7305.
Views expressed in this publication do not necessarily reflect the opinions of the editor, the college or university.
Telephone (312) 996-6695
Fax (312) 413-0086
E-mail eachavez@uic.edu
Website ahs.uic.edu
You might notice abbreviations throughout this issue. They correlate to academic units and programs in the College of Applied Health Sciences.
AT Athletic Training
BHI Biomedical and Health Informatics
BHIS Department of Biomedical and Health Information Sciences
BVIS Biomedical Visualization
DHD Department of Disability and Human Development
DIS
EP Disability Studies
Exercise Physiology
HI Health Informatics
HIM Health Information Management
KINES Kinesiology
KN Department of Kinesiology and Nutrition
MLS Medical Laboratory Sciences
NUT Nutrition
OT Department of Occupational Therapy
PT Department of Physical Therapy
RS Rehabilitation Sciences
UIC Applied Health Sciences
MAGAZINE
TABLE OF CONTENTS
Features
Vote of confidence
Gail Fisher’s new scholarship fund supports first-generation OT students
14
Notebook
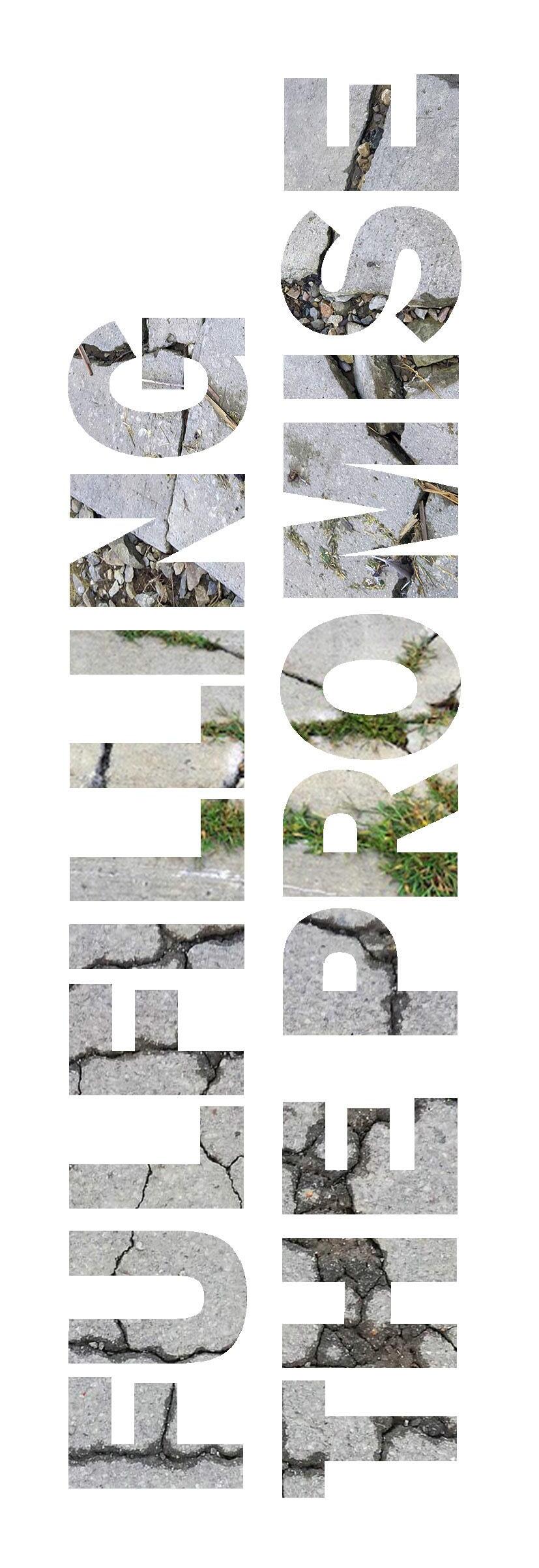
Fulfilling the promise
Yochai Eisenberg is making cities more accessible for people with disabilities
Ethics in studies of chronic pain and suicidal ideation


People
On
Helping injured athletes bounce back
Highlights from alumni and friends who established scholarships—and the students who received the awards
‛Everybody Moves!’ promotes fun physical activity


3
6 10
23
@UICAHS
the cover:
by Heidi Schlehlein ’10 MS BVIS
20 Illustration
NOTEBOOK AHS News and Notes
Students reach out to marathoners at the finish line
As 47,000 runners gasped their way past the finish line at the 2023 Chicago Marathon, UIC kinesiology students were there to help.
About 45 KN undergraduate and graduate students volunteered for the marathon’s Sweep and Psyching teams, supporting runners who were physically and emotionally spent after the grueling 26-mile race.
John Coumbe-Lilley, KN clinical professor, and Meredith Wekesser, KN clinical assistant professor, supervised the students over an eight-and-a-half hour shift before, during and after the race. The Oct. 8 marathon, an annual event, starts and ends in downtown Chicago’s Grant Park with a course through the streets of the Loop, Near West Side and South Side.
Students helped the runners move from the finish line through the finish chute, assessing whether they needed treatment by health care staff and providing emotional support after the often-overwhelming experience of completing a marathon.
For instance, fourth-year undergrads Michael Alvero and Alex Garber stayed with one runner for about 45 minutes until he could stand on his own, grateful for their help.
It was the second year KN students have worked at the marathon through a collaboration between Coumbe-Lilley and Michele Kerulis, a Northwestern University faculty member who is director of the Psyching Team and a member of the marathon medical committee. Last year, 30 KN students worked on the Sweep Team.
To prepare the students for their marathon duties, Coumbe-Lilley developed a training program of didactic, online interactive and hands-on simulation training, conducted by Tony Williams, Matt Dorey, Logan Gallaher and Dominique Martinez, all KN graduate students in the Resilient Athlete Program.
The undergrads also completed 10 hours of online training to receive certificates in psychological first aid from the National Child Trauma Service Network.

2
KN student volunteers and faculty pose for an early-morning photo before the 2023 Chicago Marathon Oct. 8. As members of the Sweep and Psyching teams, they provided support to runners at the finish line.
Ethics in studies of chronic pain and suicidal ideation
Researchers studying conditions that cause chronic pain often screen participants for signs of depression, since the two are connected.
Since depression can be linked to suicidal ideation, should researchers also ask participants if they have thoughts about harming themselves? And if the participant says yes, what is the researcher’s responsibility to act? Thinking about self-harm is not the same as having a plan to do so. If researchers alert doctors because a participant says they’ve thought about hurting themselves, it could violate the patient’s right to privacy and strain health resources.
These ethical questions were deliberated by a team led by Eric Swirsky, BHIS clinical associate professor, in a recent paper published in the journal Contemporary Clinical Trials Communications.
The discussion grew out of an ongoing National Institutes of Health-funded study, based at UIC, that is examining whether acupuncture or guided relaxation can help alleviate chronic pain from sickle cell disease. In the study, participants are screened remotely for a number of health indicators, including signs of depression and suicidality.
The ethics team agreed there’s an obligation to screen for suicidality when asking about depression. They proposed seven steps for researchers:
• understand the responsibility to act
• determine triggers for action
• examine responsibilities for action
• protect patient autonomy and privacy
• identify indirect and collateral participants
• mitigate risk of bias
• manage sociotechnical considerations of integrating research data into clinical practice.
The key takeaway for researchers is to think about these issues and their interconnectedness, said Swirsky, who studies medical ethics.
“Deliberate decision-making requires taking steps,” he said. “They don’t necessarily have to go in that order. They may not all be relevant to every trial. But they should each be considered.”
Other UIC authors involved in the study include BHIS associate professor Andrew Boyd, Carol Gu ’23 MS HI and BHI doctoral candidate Jonathan Leigh.
Read the complete paper


DHD researcher named to national transportation advisory board
Yochai Eisenberg, DHD assistant professor, is among 24 experts nationwide appointed to the U.S. Department of Transportation’s Advisory Committee on Transportation Equity.
The committee, established by transportation secretary Pete Buttigieg, will advise the Department of Transportation on issues of civil rights and transportation equity, including partnerships with underserved and underrepresented communities; concerns raised by local and regional transportation decisions; and equity in the department’s own policies, activities and decision-making.
Members, who will serve two-year terms, were selected from more than 240
applications. Eisenberg is one of three committee members from academia, who include committee chair Anthony Foxx, former secretary of transportation and professor at Harvard University’s Kennedy School of Government, and Gregory Winfree, agency director of Texas A&M University Transportation Institute.
Other committee members are from the private or nonprofit sector and city, state or regional transportation agencies.
The committee held its first meeting in the fall.

Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 3
Understanding mobile health technology

The use of wearable health technology has proliferated in recent years, with many people donning smartwatches, activity trackers and other devices to collect data and motivate positive behaviors. But what is needed to take the insights from these devices from the wrist to the clinic and laboratory?
Spyros Kitsiou, BHIS associate professor, joined the GovCIO program HealthCast to talk about the opportunities and challenges in this area. As director of the mHealth Innovation Lab at UIC, Kitsiou has overseen several trials of mobile health technologies and created new tools to integrate the data they collect into the laboratory and the clinic.
On the episode, Kitsiou spoke about the excitement around devices and algorithms that can detect irregular heart rhythms, monitor an individual’s blood glucose or use AI to create interactive virtual health coaches. But he also emphasized the need for more research to verify the efficacy and safety of these technologies.
“Sometimes it feels like we’re playing a catch-up game because by the time we establish some of this preliminary evidence,
that technology has evolved and requires sometimes additional testing,” said Kitsiou, who is also associate chief research information officer in the UIC Office of the Vice Chancellor for Research.
“This is a critical challenge in our field, which I think underlines the need for development of new, innovative study design methods to address this challenge.”
In one of his current trials, Kitsiou studies how consumer devices such as activity trackers, smart scales and blood pressure monitors can help patients avoid heart failure. To support this project and others like it, his group created a platform called iCardia to remotely collect data from patients in a secure and protected manner.
These privacy considerations are critical as the use of mobile devices becomes more tightly integrated with the health care system, Kitsiou cautioned. But with careful, user-centered design that promotes both patient engagement and cybersecurity, he sees a transformative role for these technologies.
“Mobile technologies have … transformed the social fabric of our life,” Kitsiou said. “And I think that they’re now poised to profoundly influence health care and disease management moving forward.”
Listen to the episode
Professional group honors DHD clinic physician

Kruti Acharya, DHD associate professor and physician in the Developmental Disabilities Family Clinic, is one of seven experts named 2024 fellows of the American Association on Intellectual and Developmental Disabilities.
A board-certified developmental and behavioral pediatrician, she is the director of LEND (the Illinois Leadership Education in Neurodevelopmental and other related Disabilities program). The interdisciplinary graduate-level training program develops leaders to care and advocate for individuals with disability, with a focus on autism. The program is funded by the Maternal Child Health Bureau in the U.S. Department of Health and Human Services.

Acharya uses a lifespan perspective to care for individuals with developmental disabilities from childhood to adulthood. She is particularly interested in supporting adolescents and young adults who have developmental disabilities as they transition to adult systems of care.
Her research focuses on the role of childhood, family and community adversity in health disparities experienced by individuals with disabilities, and the ethics of genetic testing for disability in various contexts.
Acharya earned an MD from Boston University and completed a residency at University of Chicago Hospitals.
AAIDD promotes universal human rights for people with intellectual and developmental disabilities through research, policy and practice. The new fellows will be honored at its annual meeting June 10-12 in Louisville, Kentucky.
4 NOTEBOOK
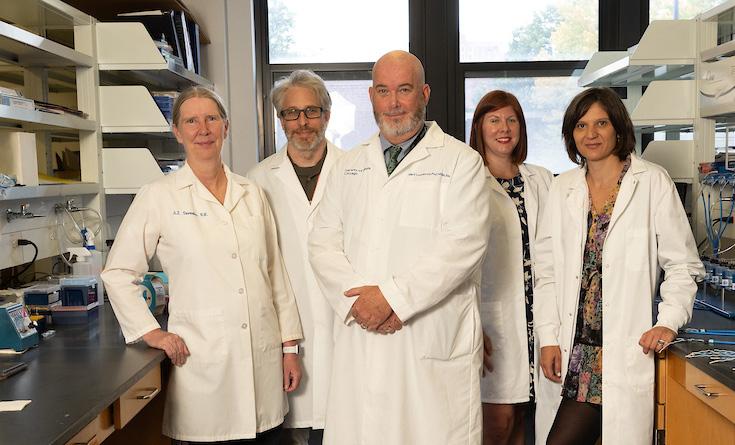
Post-transplant symptoms caused by gut microbiome
Lisa Tussing-Humphreys, KN associate professor, is among an interdisciplinary team of seven researchers who received a $3 million, five-year National Institutes of Health grant to study the relationship between the gut microbiome and symptoms that impact quality of life for nearly half of kidney transplant recipients.
The research builds off a pilot study that pointed to an association between changes in the gut microbiome and symptoms like pain, fatigue, trouble sleeping, depression and anxiety.
The researchers believe the gut microbiome could change after a kidney transplant due to dietary changes, immunosuppressive medications or stress related to the responsibility of taking care of a new kidney.
The study will enroll 120 living donor recipients, who will submit samples to assess their gut microbiome before surgery and monthly for six months after surgery. Participants will complete surveys to determine the severity of symptoms, level of stress and how their kidney disease impacts their quality of life. Researchers
will do a detailed dietary assessment before surgery and at three and six months after surgery.
Principal investigator is Mark Lockwood, associate professor of nursing.
IDHD awarded continued funding as center
The Institute on Disability and Human Development received a $3 million, five-year federal grant to continue its work as the state’s only University Center of Excellence in Developmental Disabilities Education, Research and Service.
The institute has been federally funded since 1987.
Tamar Heller, DHD professor and head, is head of the center and principal investigator for the award from the Administration for Community Living, part of the U.S. Department of Health and Human Services.
As one of 67 University Centers of Excellence in Developmental Disabilities nationwide, the UIC center promotes the self-determination, productivity, health and community inclusion of
of excellence
people with disabilities. There are four mandated activities: interdisciplinary pre-service training, community services (model services, community training and technical assistance), research and dissemination.

Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 5
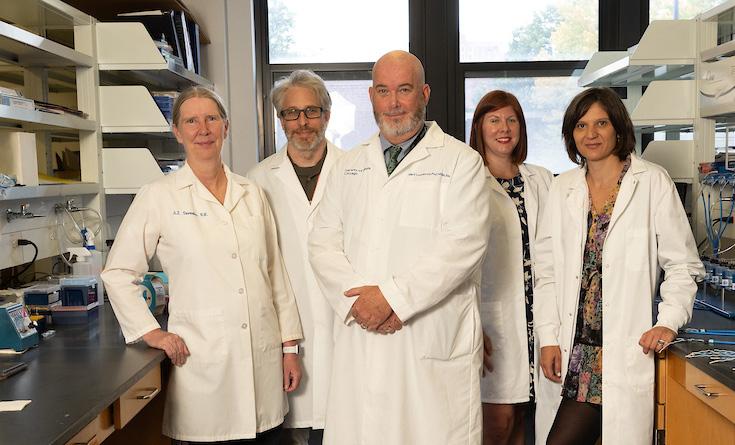
Photo: Jenny Fontaine
The interdisciplinary research team that received an NIH grant for gut microbiome research includes (L-R) Ardith Doorenbos, Stefan Green (Rush), Mark Lockwood, Lisa Tussing-Humphreys and Beatrix Peñalver Bernabé.
IDHD-affiliated students, faculty and staff participate in the 2023 Disability Pride Parade.
Photo: Jae Jin Pak
Helping injured athletes bounce back
The Resilient Athlete Program, possibly the only one of its kind in the nation, combines research-based treatment in sports psychology and sports injury to help injured athletes recover in mind and body.
“We partner with athletes to help them develop mental skills as they navigate their injury,” said KN clinical professor Karrie Hamstra-Wright, cofounder of the program with KN clinical professor John Coumbe-Lilley.
Hamstra-Wright’s research focuses on prevention and treatment of lower extremity injury, while Coumbe-Lilley’s work concerns emotional recovery after severe or catastrophic sports injuries. About three years ago they established the ASPIRE (Applied Sports Psychology and Injury Research and Education) Laboratory, which offers hands-on learning and research experience to undergrad and graduate students. In fall 2022, they launched the Resilient Athlete Program, which provides one-on-one support and consulting at no charge to athletes of all ages.
“We think of resilience as the ability to bounce back, regardless of what the return to sport looks like—a full return, return in a different way, not returning, return to a new sport,” Hamstra-Wright said.
In addition to Coumbe-Lilley and Hamstra-Wright, the staff includes graduate students in performance, sports and exercise psychology, a concentration in the kinesiology master’s program.
The athletes, who range in age from teens to 70s, include competitive runners, wrestlers, baseball and softball players, swimmers and power lifters. Some are UIC athletes; others come from all over the country, Canada and Mexico.
Besides the sport they love, injured athletes can lose their social community, their daily routine and their primary means of stress management.
In the Resilient Athlete Program, they meet with consultants three to six times in 30- to 60-minute sessions, either in person or online.
The interventions might include fear-based movement training, goal setting, biofeedback, imagery and visualization, self-talk strategies, simulation training, stress management and writing activities, Hamstra-Wright explained.
“We help them develop the mental skills that support wherever they are in their injury process.”

6 NOTEBOOK
Resilient Athlete Program services are free. Contact the staff at aspire@uic.edu or 312-996-0152.
Karrie Hamstra-Wright and John Coumbe-Lilley.
New Bridge to Faculty hire
Azadeh Safaeian, whose research concerns disability studies and trauma in literature and film in the context of the Middle East, joins DHD as the college’s second UIC Bridge to Faculty postdoctoral research associate.
Bridge2F, established in 2020, is a recruitment initiative to attract underrepresented postdoctoral scholars of color to faculty positions at UIC. The program is run by the Office of Diversity, Equity and Engagement with the support of the Office of the Chancellor. UIC departments chosen to participate must present a plan for successfully hiring, mentoring and supporting a postdoctoral scholar who will transition to a tenure-track faculty position after two years.

The first AHS Bridge scholar, Sabrin Rizk, selected in 2021, is now an OT assistant professor.
Safaeian is among 14 scholars in the fall 2023 cohort. She was a postdoctoral fellow in comparative literary studies at Northwestern University, where she earned a PhD and MA in comparative literary studies. She holds a bachelor’s in English literature from Ferdowsi University of Mashhad and a bachelor’s in biology from Azad University of Mashhad.
Her research and teaching interests include disability and trauma studies, care studies, postcolonial environmental humanities, animal studies and film theory.
Mediterranean diet may reduce depression during pregnancy
Pregnant women who ate a Mediterranean-style diet were less likely to show symptoms of depression, according to a recent study led by KN assistant professor Vanessa Oddo
The research used data from the National Health and Nutrition Examination Survey and focused on 540 pregnant women who gave information about their diets and filled out a survey about their mental health. The analysis showed that the pregnant women who largely adhered to a Mediterranean diet— which emphasizes whole grains, fruit, vegetables, extra virgin olive oil and moderate amounts of fatty fish—were less likely to report symptoms of depression. This was true even when controlling for sociodemographic factors such as race, education level and income.
The findings are important, the researchers explain, because about 12% of pregnant women in the U.S. are affected by prenatal depression, which increases the risk of adverse birth outcomes, maternal mortality and postpartum depression. Some pregnant women are hesitant to take antidepressant medications, making diet a particularly compelling tool in addressing depression.
“This relationship merits further examination, given the public health significance of promoting mental wellness among pregnant women,” the authors write.
The study was published in The Journal of Nutrition. UIC co-authors on the paper are Crussie Moise, Beatriz Peñalver Bernabé, Pauline Maki, Mary Dawn Koenig, Lacey Wisslead-Pezley, Yinglin Xia and Lisa Tussing-Humphreys.


Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 7
Read the complete study
Intermittent fasting effective, safe for weight loss

Intermittent fasting, an increasingly popular weight loss method, is an effective and safe way to lose weight, according to dozens of research studies by KN professor Krista Varady
Intermittent fasting includes alternate-day fasting (eating up to 500 calories one day and unrestricted eating the next) and time-restricted eating (eating only during a fixed period of time each day).
Her research has found that intermittent fasting is as good as calorie counting for weight loss, with people losing an average 3% to 8% of baseline weight, and provides health benefits such as decreased blood pressure and insulin resistance.
“People love intermittent fasting because it’s easy,” Varady said. “People need to find diets that they can stick to long term. It’s definitely effective for weight loss, and it’s gained popularity because there are no special foods or apps necessary.”
Highlights from her published studies include:
Weight loss in diabetes
Intermittent fasting can help people with Type 2 diabetes lose weight and control blood sugar levels.
Participants who ate only during an eight-hour window between noon and 8 p.m. each day lost more weight over six months than participants who reduced their calorie intake by 25%. Both groups had similar reductions in long-term blood sugar levels.
Just over half the participants were Black and another 40% were Latine. Diabetes is prevalent among both groups, so studies documenting the success of time-restricted eating are useful.
JAMA Network Open
Six-hour window of time-restricted eating
Researchers followed people who restricted their eating to four or six hours a day. After 10 weeks, participants in both groups
cut daily calorie intake by about 550 calories and lost about 3% of their body weight.
Compared with a control group that did not fast, both groups of fasters showed reduced insulin resistance and oxidative stress levels. There was no effect on blood pressure, cholesterol or triglycerides. There was no significant difference in weight loss or cardiometabolic risk factors between the four-hour and six-hour diet groups.
Cell Metabolism
Time-restricted eating works as well as calorie-counting
Participants were asked to either eat only between noon and 8 p.m. each day or reduce their calorie input by 25%. After 12 months, both groups lost, on average, about the same amount of weight.
Annals of Internal Medicine
Time-restricted eating for obese individuals
A 12-week study of 23 obese participants, who could eat whatever they wanted but only between 10 a.m. and 6 p.m., found that on average, they consumed about 350 fewer calories, lost about 3% of their body weight and their systolic blood pressure decreased.
Nutrition and Healthy Aging
Intermittent fasting and female reproductive hormones
Researchers followed a group of pre- and post-menopausal obese women on the “warrior diet,” a four-hour window of eating each day. Levels of several reproductive hormones were unchanged at the end of the eight-week study, but a hormone that improves ovarian function and egg quality was lower at the end of the eight weeks, though within normal range.
Obesity
Alternate-day fasting and fatty liver disease
A three-month study of 80 people with nonalcoholic fatty liver disease found that those who followed an alternate-day fasting diet and exercised improved their health.
Participants had increased insulin sensitivity and decreased liver fat, weight and enzymes markers for liver disease.
About 65% of obese adults have fatty liver disease, which is strongly related to the development of insulin resistance and Type 2 diabetes.
Cell Metabolism
8
NOTEBOOK
mHealth researcher named OT head

Susan Magasi ’02 MS OT, ’06 PhD DS, who develops mobile health (mHealth) technology to help people with disability overcome barriers to health care, was named professor and head of the Department of Occupational Therapy.
Magasi, also professor of disability and human development, works closely with the disability community and cancer survivors in a community-based, participatory approach to research.
“Dr. Magasi’s extensive research, teaching and community engagement experience is impressive,” said AHS dean Carlos Crespo.
Magasi led an mHealth project, funded by the Chicago Cancer Health Equity Collaborative, that developed an app to help cancer survivors manage longterm disabilities related to their illness and treatment.
She is principal investigator for a related project that is creating a peer navigator app to support people with newly acquired
disabilities who are transitioning to independent living. That research is supported by the National Institute on Disability, Independent Living, and Rehabilitation Research.
Magasi’s earlier mHealth research projects include an app to connect cancer patients with disabilities to disabled cancer survivors, and peer health navigation for Medicaid beneficiaries with physical disabilities.
Magasi has been honored as Researcher of the Year by both UIC and AHS. She is a fellow of the American Congress of Rehabilitation Medicine and chair of the Scientific Advisory Council for the American Occupational Therapy Foundation. She received the Meritorious Service Award from the American Occupational Therapy Foundation.
Magasi joined the UIC faculty in 2013. She succeeds Yolanda Suarez-Balcazar, who was OT department head from 2006 until 2022, when she stepped down to return to the faculty.

Nutrition professor honored by USDA
Vanessa Oddo, KN assistant professor, was named an E. Kika De La Garza education fellow by the U.S. Department of Agriculture.
She is among 30 faculty and staff members from Hispanic-Serving Institutions who were honored.
UIC was recognized for its success in graduating Latine students in USDA-focused majors such as nutrition.
Fellows spent a week in Washington, D.C., meeting with leaders from different USDA agencies to learn about national and regional issues, policy making and research.
Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 9
’Everybody Moves!’ promotes fun physical activity
Delphine Labbé, DHD assistant professor, was awarded a $600,000, three-year grant from the National Institute on Disability, Independent Living, and Rehabilitation Research for “Everybody Moves!”, a project to promote leisure-time physical activity for Latine and Black people with disability.
“We know that people from Black and Latino communities do less physical activity for different reasons—lack of programs, lack of access, other barriers like transportation and costs. There’s also a lack of information about what’s available,” Labbé said.
The researchers will survey individuals and the organizations that serve them to learn what activities are popular and currently available.
“We want to talk with individuals with disability about their needs, their current physical activity and the barriers they face,” Labbé said.
The researchers will survey park districts and community organizations to learn what activities are offered, how they are publicized and how issues of diversity and inclusion are addressed.
The project’s goal is to create recommendations that will result in programs for leisure-time physical activity that are enjoyable, accessible and culturally appropriate for Black and Latine people with disabilities.
“We want to make sure that organizations are reaching this population, because we know they’re poorly served right now,” Labbé said.
Co-PIs include Monika Stodolska, professor of recreation, sport and tourism in the University of Illinois Urbana-Champaign College of Applied Health Sciences, DHD assistant professor Yochai Eisenberg and DHD postdoctoral research fellow Casey Herman. Community liaison is T.J. Gordon Jr., Institute of Disability and Human Development.

10 NOTEBOOK
Outdoor enthusiasts during an adaptive bike camping trip sponsored by Out Our Front Door. The group biked to a campsite on the South Side, near South Shore Cultural Center.
Photo: Delphine Labbé
New center focuses on equity in dementia care
A new federally funded center co-led by faculty in AHS and the School of Public Health will focus on care for people with dementia, as well as their care providers, while supporting the research of underrepresented faculty.
The Center for Health Equity in Cognitive Aging, funded by a $3 million grant from the National Institute on Aging, is the newest of 18 Resource Centers for Minority Aging Research in the U.S. and the first in a Midwestern urban area.
Tanvi Bhatt, professor of PT and RS, is co-director with Naoko Muramatsu in the School of Public Health.
The center, based in the Institute for Health Research and Policy, will mentor underrepresented faculty and focus on the social, environmental and behavioral factors leading to inequities in Alzheimer's disease and other types of dementia.
The center's Scientist Program accepted three pilot projects in its first round for funding of up to $50,000.
Dalmina Arias, OT clinical assistant professor, will use her funding to expand a primary care-based program developed by OT associate professor Mansha Mirza. The program works to prevent hospitalization for older adults with chronic health conditions by connecting them to occupational therapists who assess their home environment. Arias will adapt the program for Spanish-speaking patients and families.
The center's other first-round grants were awarded to Kelechi Ibe-Lamberts and Jennifer Kwok in the School of Public Health.
Learn more at cognitivehealthequity.uic.edu

Clocking the disparities in youth sedentary time
Kinesiology researchers found differences between genders and across racial and ethnic groups in the amount of sedentary time they spend during the day.
Using a dataset where thousands of children ages 6 to 18 wore fitness trackers for a week, a team led by María Enid Santiago-Rodríguez ’21 PhD KINES analyzed the times of day when groups differed most in activity.
The study, published in PLoS ONE, found that more than half the sedentary time disparities between girls and boys were during


weekday school hours, with afterschool and weekday evenings contributing another 30% of the difference.
While surprising, given that students of both sexes have mostly the same routine at school, the result offered promise for intervention.
“School is a time where you can reach most of the students,” said Santiago-Rodríguez, now a postdoctoral researcher at University of Michigan. “It is a unique opportunity that we can take advantage of to reduce those sex disparities.”
Across racial and ethnic groups, weekend mornings emerged as the biggest difference. In some comparisons, such as between Mexican American and Black youth, two-thirds of the difference happened on weekends versus weekdays.
“It suggests that we need to work with families to think about what's happening at home to address those disparities,” said Eduardo Esteban Bustamante, KN assistant professor and the paper's senior author.
In his Healthy Kids Lab, Bustamante developed a family intervention called BUILT with activities for out-of-school hours. The new research will help make such programs more effective.
Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 11
Read the complete study
Resources for caregivers of older Asian Americans

Researchers in OT and DHD are developing a technical assistance and resource development center for caregivers, service organizations and community groups who work with older Asian American adults.
Called ASIAAN (Aging Services Inclusive of Asian American Networks), the project is led by principal investigator Mansha Mirza '04 MS OT, '09 PhD DS, OT associate professor, and co-PI Sumithra Murthy '22 PhD DS, DHD visiting clinical assistant professor.
The project is funded by a three-year, $620,000 grant from the Administration for Community Living in the Department of Health and Human Services.
“The idea is to strengthen aging services for Asian American elderly persons, so this could mean multiple things,” Mirza explained.

“For instance, educating community members about available aging services, enhancing cultural sensitivity within mainstream service providers for older adults, and supporting ethnic community-based organizations to serve as cultural liaisons with providers.
“And educating the next generation of health care providers to have a better cultural understanding of aging and caregiving from an Asian American perspective,” she added.
The project is working with a broad range of community and service organizations, including the Illinois Department on Aging, Chinese American Service League, Coalition for a Better Chinese American Community, South Asian American Policy and Research Institute, Metropolitan Asian Family Services and the South East Asia Center.
ASIAAN will develop culturally sensitive health literacy curricula for older Asian Americans and their caregivers, as well as an interactive map of age-related community resources, offered in several Asian languages.
Mirza said DHD undergraduate students will create intergenerational social media resources about aging and age-related needs for Asian Americans to generate more awareness among communities and families.
Other faculty included on the grant include Kelly Hsieh, DHD research associate professor; Yochai Eisenberg, DHD assistant professor; Rooshey Hasnain, DHD clinical associate professor; and Jenica Lee, OT clinical associate professor.
12 Read additional news and notes NOTEBOOK
A community education meeting, organized by AHS faculty, on the Medicaid redetermination process for older Medicaid beneficiaries, held at the Chinese American Service League.
Have your voice heard
participate in research
Help create a healthier future by changing the way people get involved in research.

AHS researchers pursue new knowledge that transforms health care practice and social systems. Behind every scientific breakthrough there is a dedicated team of scientists, clinicians, patients and volunteers who made it possible. Your participation as a volunteer is crucial in our ability to drive discovery and, as a result, make a positive difference in our diverse and ever-changing world.
Ready to make a difference?


Visit go.uic.edu/ParticipateInAHSResearch to view
list of AHS research studies
a
actively recruiting participants.
Vote of confidence
Gail Fisher’s new scholarship fund supports first-generation OT students
A quick glance at Gail Fisher’s resume reveals an impressive list of educational and career accom plishments. PhD? Check. Countless articles and book chapters? Check. Celebrated clinical professor in the Department of Occupational Therapy? Yes.
But there’s so much more to Fisher’s story. “I actually dropped out of college,” she says. “Things don’t always go according to plan.”
During her 34 years at UIC, Fisher ’80 BS OT, ’17 PhD met many OT students who faced challenges of their own. Financial struggles, health issues and unanticipated life changes sometimes derailed students’ goals. That’s one of the main reasons she established the UIC OT Gail Fisher Scholarship Fund.
While she hopes the scholar ships will provide a financial cushion to each recipient, Fisher also envisions her fund as a message of moral support.
“I want students to feel seen by this scholarship,” she says. “I know it’s hard, but stick with it. I did it, and you can, too. Most of all: I believe in you.”

14

Raised to achieve
The first people to believe in Fisher were her parents, Shirley and Leonard. The children of immigrants from Latvia and Germany, they took their family responsibili-

“My dad would have loved to go to college, but he had to support his family, so he became a watchmaker,” Fisher says. Her mother worked outside the home during an era when that was unusual; she had a part-time job in high school and continued to work after her children started school.
“Even though they never went to college, my parents were very smart and determined,” Fisher says. One thing they felt strongly about was that their three children would earn college degrees, ideally at the University of Illinois Urbana-Champaign. Its stellar reputation and in-state tuition made it the most appealing option.
Fisher discovered the OT program while flipping through her older sister’s course catalog. At the time, OT students spent three years in Champaign, then 18 months at UIC completing clinical OT courses and fieldwork. “Undergraduate courses included psychology, crafts, anatomy and physiology,” Fisher says. “I was interested in all of it.” Her parents told her to go for it, seeing their own drive reflected in their daughter.
The power of mentors
After Fisher’s junior year, she withdrew from school due to changes in her family situation.
“I had every intention of going back,” she says, but life threw some curveballs her way. She
was readmitted two more times in subsequent years—and had to turn those offers down.
Eventually, Fisher moved back to Champaign and applied one final time. She later learned that some faculty felt she’d been given enough chances. However, department head Barbara Loomis rallied other faculty to advocate for her readmission.
“I feel such a debt of gratitude for that,” Fisher says. “It easily could have gone the other way. I needed someone to believe in me. And they did.”

Thus began Fisher’s second journey toward an OT degree and a fulfilling career. In 1988, she joined the OT department faculty at UIC—and stayed until she retired as clinical professor emerita in 2022. In the late Gary Kielhofner, then department head, Fisher found an encouraging mentor and colleague.
“Gary saw more in me than I saw in myself,” Fisher says. “He got me started writing and presenting at the national conference. My roles kept changing over time as he gave me more opportunities to grow.”
Kielhofner applauded Fisher as she embarked on a PhD from the School of Public Health while working full time. That endeavor took 11 years and wouldn’t have been possible without the support of Fisher’s husband, Eric Davis Gyllenhaal, and their two sons.
Fisher also credits Kielhofner’s successor, Yolanda Suarez-Balcazar, and AHS associate dean Renée Taylor for facilitating her career success.
As an expert on Kielhofner’s Model of Human Occupation, Fisher has made a positive impact on students and therapists through courses, books, presentations, case studies, resources, assessments and more. In semi-retirement, she is collaborating with a former student, Jarrett Wolkse ’17 MS OT, ’21 OTD on the book “Re-envisioning Kielhofner’s Conceptual Foundations of Occupational Therapy: a Multi-Model Approach.”
 Fisher (right) with Barbara Loomis (left) during 2013 AHS Alumni Weekend.
Fisher (right) with Barbara Loomis (left) during 2013 AHS Alumni Weekend.
confidence
Fisher with Gary Kielhofner at a reception honoring his 20 years of service as OT department head.
Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 15
Fisher's first official photo as a UIC faculty member in 1989.
A lasting gift
Throughout her years in the OT department, Fisher oversaw admissions, a role that gave her an inside look at the needs and dreams of future practitioners. She witnessed changes that might surprise older alumni.
“Students take on a lot more debt today, knowing that they’re going to be in a field that doesn’t necessarily pay as well compared to some other fields,” Fisher says. She notes that many students work two or three jobs to stay afloat while pursuing their degrees.

At the same time, alumni of all ages can empathize with the motivation that drives students to obtain their OT degrees. “They want to problem-solve together with their clients and patients, they want to collaborate with them,” Fisher says. “They are committed to helping people.”
So is Fisher. Her scholarship fund is designated for first-generation college students and those with financial need. The scholarship announcement intentionally includes Fisher’s story.
“Applicants can read that my parents didn’t go to college; my grandparents didn’t graduate high school,” she says. “But I made it through with a lot of hard work and people supporting me. If I can do it, so can you.”
Fisher was inspired by the scholarship fund established by Loomis, who retired in 1981 as associate professor emerita.
“One of the things I appreciate about this opportunity is that it’s a lasting legacy,” she says.
“Your commitment to the students and the department is known in perpetuity; furthermore, it’s a legacy in honor of your mentors and your family.”
Targeting inflam-
For students, scholarships represent financial stability, educational opportunity, a connection to those who came before and a vote of confidence.

“When students see the list of donorfunded scholarships, it speaks to them because they know there are people investing in their generation,” Fisher says. “I hope my story encourages other alumni to support the future of our field.”
Hear Gail Fisher describe how she hopes her scholarship fund will help shape the careers of occupational therapy students, the practice and her legacy: go.uic.edu/GailFisherScholarship.
In December, Lejla Jakupovic ’22 BS RS received the inaugural scholarship from the Gail Fisher fund. A first-generation student born to Bosnian immigrants, Jakupovic navigated the undergraduate college application and financial aid process largely on her own. She majored in rehabilitation sciences, with minors in psychology and disability and human development.
Now a first-year student in the entry-level occupational therapy doctorate program, Jakupovic enjoys being a teaching assistant, learning theory and serving as an ally for fellow first-generation students.
Jakupovic was excited—and her parents were proud—when she received notice of the scholarship award.
“I am immensely grateful for this opportunity,” she says.
“Student loans are scary; scholarships really help. This scholarship makes me feel like I can do anything.”
Jakupovic hopes to follow in Fisher’s footsteps, both as an educator and as someone who leads with generosity.
“She’s made such a big impact in OT,” Jakupovic says. “It sounds cheesy, but I chose OT because I want to make a difference in people’s lives, too.”
 Fisher with former student Megan Win ’18 MS, ’19 OTD at spring 2019 commencement. Fisher, who was Win's adviser, continues to serve as a career mentor.
Fisher with former student Megan Win ’18 MS, ’19 OTD at spring 2019 commencement. Fisher, who was Win's adviser, continues to serve as a career mentor.
16
Fisher congratulates Brianna Bonner ’16 MS OT who gave the student response at 2016 AHS commencement. Bonner is now an OT faculty member who is working with Fisher on a publication.
The AHS Scholarship Fund
The AHS Scholarship Fund supports undergraduate students with financial need from academic programs across the college.
By donating, you cast your vote of confidence in the talent and promise of our students while easing their financial burden and inspiring them to be bold and go far.
Donate at ahs.uic.edu/support or contact Torine Pasek at torine@uic.edu or 312-996-1339.

‟I’m extremely grateful to receive this scholarship as it encourages me to continue to pursue my passion and hone my skills to better serve individuals and my community. Thanks to the generosity of donors who make this scholarship possible, I will be able to complete my education and apply what I’ve learned to make a positive impact and help a future student one day.”
- Isabel Perez-Correa ’24 BS NUT
Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 17

18

19
Illustration by UIC Biomedical Visualization students Khorizon Dunn, Susie Hammons and Keaton Mullins.
YOCHAI EISENBERG IS MAKING CITIES MORE ACCESSIBLE FOR PEOPLE WITH DISABILITIES
With his background in health policy, disability rights and urban planning—and an enthusiasm for collaboration with other researchers—Yochai Eisenberg works to create accessible cities for people with disabilities.
“I was interested in environmental design and how it affects people's behavior,” said Eisenberg, DHD assistant professor and researcher in the Great Lakes ADA Center, in explaining his career path.
“I saw how much difficulty people with disabilities have in public spaces, and the big gap in terms of training, research and application.”
He is co-investigator on five current federally funded research projects, based at UIC and two other universities, to provide resources for fulfilling the promise of the Americans with Disabilities Act.
“Our research, which focuses mostly on the pedestrian environment, has helped show that cities aren't making enough progress in becoming fully accessible for people with disabilities,” said Eisenberg, who was recently named to the U.S. Department of Transportation’s Advisory Committee on Transportation Equity.
Over 30 million people in the U.S.— including about 500,000 Chicago residents—have at least one physical disability that affects their ability to move around, and almost half of them rely on wheelchairs, canes, crutches and walkers. When they

travel about their neighborhood, they are often impeded by obstructions, broken concrete, lack of curb cuts, no audible crossing signals and other barriers.
Since 1999, courts have consistently ruled that sidewalk accessibility is guaranteed by the ADA. This leaves cities with two choices, Eisenberg said: be forced into it by lawsuits (Chicago lost a case last year for failure to provide audible pedestrian signals) or create their own ADA transition plan.
For the latter, Eisenberg and the Great Lakes ADA offer resources and technical assistance.
“It's
one thing to find a problem, but we want to offer ideas and best practices that local governments can use to implement solutions,”
he said.
Before a city can develop a plan to improve accessibility, problems must be defined and located. How can a city survey thousands of miles of sidewalks?
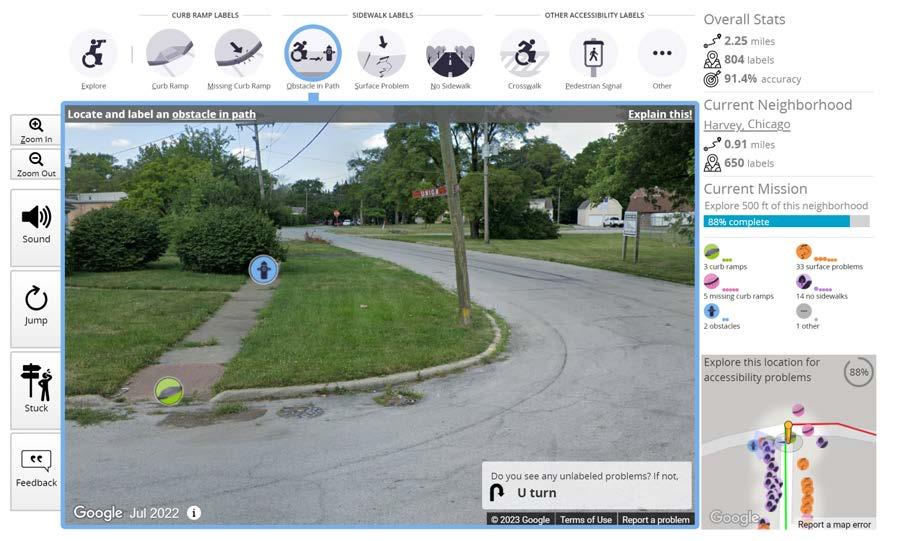
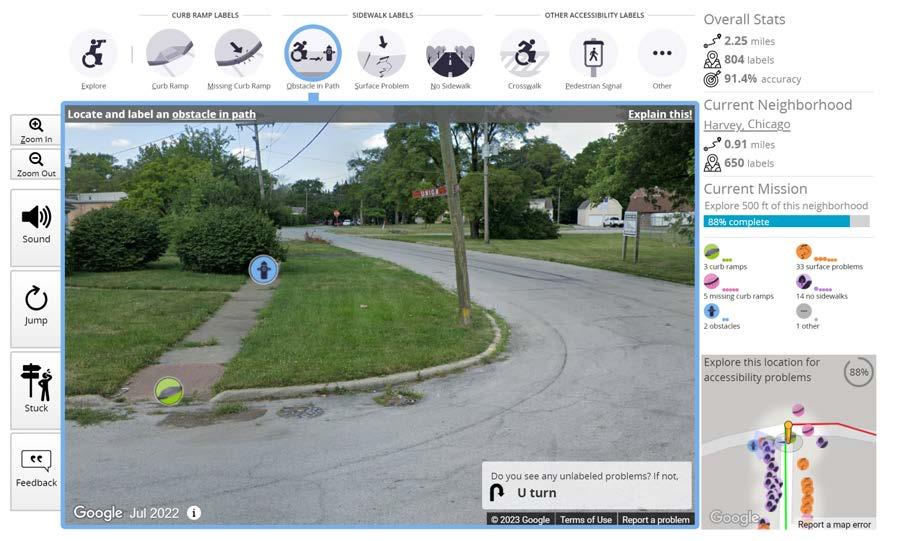
Answer: Project Sidewalk, a collaboration with computer scientists at the University of Washington Makeability Labs and Easterseals.
Funded by the National Science Foundation, Project Sidewalk uses community scientists and artificial intelligence to locate, catalog and create interactive maps of barriers to pedestrian accessibility.
20

“We’re working with city governments and different community organizations—including disability organizations and urban planning groups—to be involved in this crowdsourcing approach to data collection and mapping of the accessibility of sidewalks,” Eisenberg said.
“It's both applied research and technology development.”
The mapping is done online with an easy-to-use interface. Mappers include community members and college students; researchers are recruiting high school students for a service learning program that teaches them about accessibility and disability justice and trains them to use the crowdsourcing tool.
The project is partnering with Easterseals to create a workforce development curriculum for recent high school graduates with disabilities, who will learn to be community scientists with Project Sidewalk while developing skills for leadership and advocacy.
So far, Project Sidewalk includes data on pedestrian right-ofway accessibility for 11 cities: seven in the U.S. (including Chicago), three in Mexico and one in the Netherlands.

Part of the grant is working with cities to use the data, Eisenberg said.
“We explain that Project Sidewalk is a free resource to jumpstart your planning, because you’ll have all this data about accessibility.”
Newberg, Oregon, population 25,000, is one of Project Sidewalk’s success stories.
After all the streets were mapped, the town used the information to develop a pedestrian accessibility plan and fund improvements.
As a resource, the Great Lakes ADA Center created a casebook of cities that have suc-
cessfully implemented public accessibility projects, including suburban Naperville, Tempe, Arizona, and Bend, Oregon.
In Chicago, volunteers have mapped over 220 miles of streets and made nearly 42,000 ratings of pedestrian infrastructure.
Eisenberg’s team is working with aldermanic offices in Chicago’s 40th and 3rd wards to define the accessibility needs in those neighborhoods, which are interested in using a participatory budgeting process for accessibility improvements.
Working with the disability rights group Access Living, student volunteers from Eisenberg’s Disability, Urban Planning, and Geography course used Project Sidewalk to map barriers to accessibility around five Chicago transit stations.
Eisenberg is involved in a long list of other projects to develop tools and resources for improving accessibility.
With researchers at the University of Alabama Birmingham and the Centers for Disease Control and Prevention, he developed the Community Health Inclusion Index, which assesses barriers to physical activity and healthy eating. The tool is available online from the National Center on Health, Physical Activity and Disability.
“It's used by different communities to collect information about how inclusive their policies, systems and environments are,

Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 21
Eisenberg leads a Project Sidewalk training session.
Photo: Martin Hernandez Rosas
focused on aspects of health promotion within their communities,” said Eisenberg, who offers training to use the tool.
For example, in Worcester, Massachusetts, “they used the CHII assessment in every playground in the city, then used the results to prioritize grant funds for making certain playgrounds more inclusive,” he said.
Eisenberg is co-principal investigator on “We Walk 4 Health” with Kelly Hsieh, DHD research associate professor. Working with community-based organizations, the project uses mobile phones and fitness trackers to encourage physical activity and wellness for adults with intellectual and developmental disabilities.
He’s co-investigator for “Everybody Moves!”, a project led by Delphine Labbé, DHD assistant professor, to promote leisure-time physical activity for Latine and Black people with disability.
He’s also co-investigator for ADA PARC, a UIC-based national resource center led by Joy Hammel, OT, DHD and RS professor, that gathers and analyzes data about participation disparities for use in advocacy.
Other projects have included developing an algorithm to identify adults with mobility limitations, found through health care administrative
data, and an analysis of the use of ride-share by people with disabilities.
In “Mapping Disability Experiences During the Covid-19 Pandemic,” he and fellow researchers invited people with disabil ity to share submissions that illustrated how the pandemic affected their lives.
Besides his recent appoint ment to the Department of Transportation advisory committee, Eisenberg has been a member of advisory groups on accessibility for the Cook County Forest Preserve, the Centers for Dis ease Control and Prevention, the CTA and the American Public Health Association, among others.
He discusses accessibility is sues in presentations to ADA coordinators, mayors and metropolitan planning organizations, and to the public in news interviews, including NPR.
“I really do enjoy collaborations with different people across disciplines,” he said. “It’s so mutu ally beneficial when you find good collaborators.”


22
A screenshot of the Project Sidewalk virtual interface shows a Google Street View image of a sidewalk and corner in Harvey, Ilinois. The user placed labels to indicate a curb ramp and an obstacle on the sidewalk. The interface shows the user's stats in a panel on the right side and a graphic overview in the bottom right corner.
PEOPLE AHS Alumni Highlights
Editor’s note: in this issue of UIC Applied Health Sciences Magazine, we feature AHS alumni and friends who established scholarships—and the students who received the awards.
Rhoda P. Erhardt Scholarship
“From my perspective, the benefits of the ongoing funding are many. Not only do deserving students receive assistance, but the UIC Department of Occupational Therapy is strengthened, and other alumni may be motivated to contribute.”
Rhoda P. Erhardt ’54 BS OT


“I chose to attend UIC ’s E-OTD program as an out-of-state student to learn from renowned professionals and practitioners and become the best occupational therapist I could be. I am grateful to be awarded this scholarship in honor of Rhoda P. Erhardt, who embodies what it means to be a leader in occupational therapy. "
Frank Armitage Fellowship
“Even though my husband had a remarkable and impressive career at The Walt Disney Company, Walt Disney Imagineering and 20th Century Fox, to name a few, he was most proud of his contributions to medical illustration. He broke barriers! Frank was so grateful and proud to be associated with the UIC Program in Biomedical Visualization. From the very beginning, I have contributed to the Frank Armitage Fellowship to help younger students. It is what he would have wanted.”
Karen Connolly Armitage

“The scholarship award eased financial barriers, reduced my stress level and freed up time to focus on my educational needs. You are a key reason for my educational success.”
Elizabeth Perakes ’26 MS BVIS
Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 23
Arielle Buslovich ’25 E-OTD
Gottlieb Assistive Technology Certificate Program Scholarship
“I read that ‘you don’t have to be a millionaire to start a scholarship.’ That planted the seed to donate to AHS. During the pandemic I participated in a Zoom program where I learned more about the Certificate Program in Assistive Technology. I was impressed and inspired. I loved the idea that this scholarship could help stu dents achieve their goals, and they could help others achieve theirs.”


“I can enhance my knowledge and skills as a bicultural bilingual speech language pathologist, thanks to the generosity of donors. I have already begun to apply many of the strategies with my caseload in predominantly Spanish-speaking neighborhoods.”
Donna Roach Award
“My mother believed passion ately in the value of education. She worked her way through college without any help from her family but made sure her own children had the support they needed. I could think of no better way to honor her.”


“This scholarship has contributed to my educational success and inspired me to give back to others when I am able. I am very grateful and honored to be a recipient of this award!”
24 Summer 2023 UIC APPLIED HEALTH SCIENCES MAGAZINE 24
Carol Gottlieb
Melissa Tapia ’23 CERT ATECH
Kathryn Roach ’74 BS PT
Stay connected! Exciting life change? New milestone? Ready to get involved? Submit a class note to the UIC Alumni Association: go.uic.edu/UICAAClassNotes
Sophia Manokas ’24 DPT
PEOPLE
Kathryn Roach (right) and her mother, Donna Roach, at Kathryn’s graduation in 1974.

AHS department annual funds
When you donate to an AHS department annual fund, you directly support that department’s most urgent financial needs, giving its leadership the flexibility to use the funds when and where they are most effective.
Donations to department annual funds support:
• student scholarships and travel awards
• student-, faculty- and staff-led efforts
• improvements to academic and clinical facilities
• groundbreaking research and scholarship
Donate to the AHS department of your choice at ahs.uic.edu/support or contact Torine Pasek at torine@uic.edu or 312-996-1339.
Winter 2024 UIC APPLIED HEALTH SCIENCES MAGAZINE 25
College of Applied Health Sciences
University of Illinois Chicago
808 S. Wood St., 169 CMET
Chicago, Illinois 60612-7305
Address Service Requested

Nonprofit Org. U.S. Postage PAID Chicago, Illinois Permit No. 4860




 Carlos J. Crespo Dean and professor College of Applied Health Sciences
Carlos J. Crespo Dean and professor College of Applied Health Sciences
































 Fisher (right) with Barbara Loomis (left) during 2013 AHS Alumni Weekend.
Fisher (right) with Barbara Loomis (left) during 2013 AHS Alumni Weekend.


 Fisher with former student Megan Win ’18 MS, ’19 OTD at spring 2019 commencement. Fisher, who was Win's adviser, continues to serve as a career mentor.
Fisher with former student Megan Win ’18 MS, ’19 OTD at spring 2019 commencement. Fisher, who was Win's adviser, continues to serve as a career mentor.