COURSE DESCRIPTION
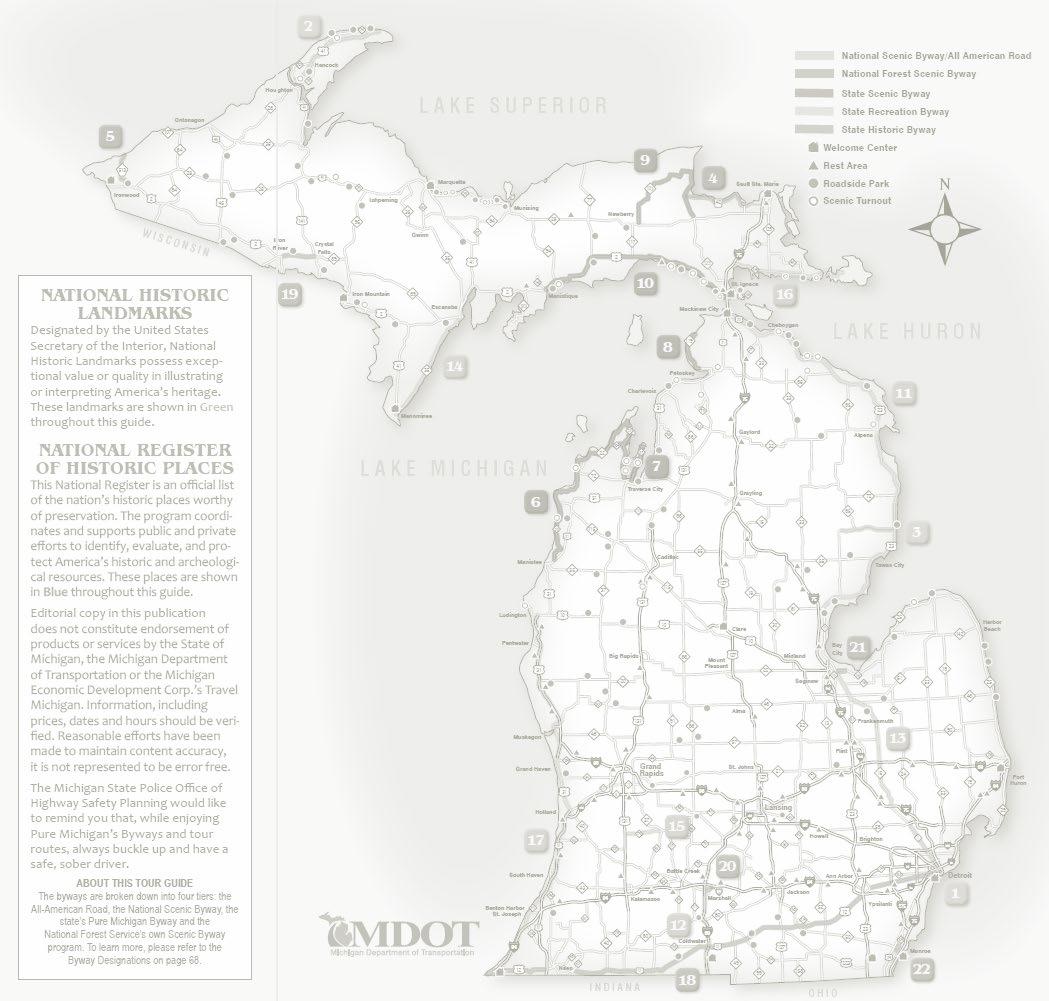
Join Us on Sept 14th and 15th, 2023 in Ann Arbor for Championship Updates in Sleep Medicine. Diverse & Multidisciplinary Speakers will provide evidence based and practical strategies to improve care of patients with sleep disorders and provide updates on innovations in sleep medicine. This 1.5-day conference will provide continuing education credits as applicable to attendees (Physicians, Advance Practice Providers and Sleep Technologists, etc.) commensurate with the extent of their participation in the activity. After this activity, sleep providers will be able to apply new knowledge regarding best practices and guidelines to the everyday care of the sleep medicine patient.
LEARNING OBJECTIVES
At the end of this activity, participant should be able to:
1. apply new knowledge regarding best practices and current society guidelines to the evaluation and management of patients with sleep disorders.
2. educate patients regarding treatment options for sleep disorders.
ACCREDITATIONS & CREDIT DESIGNATION
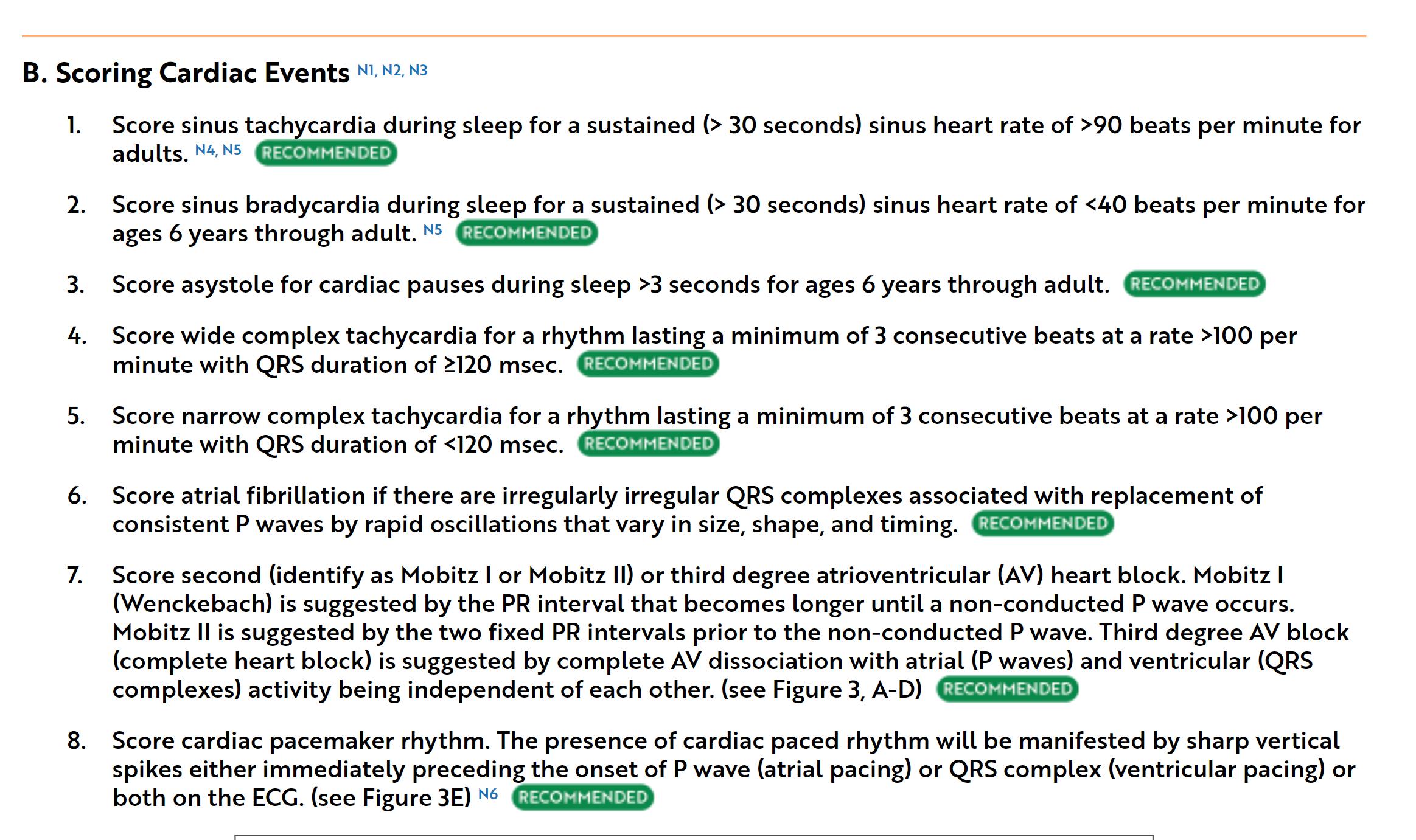
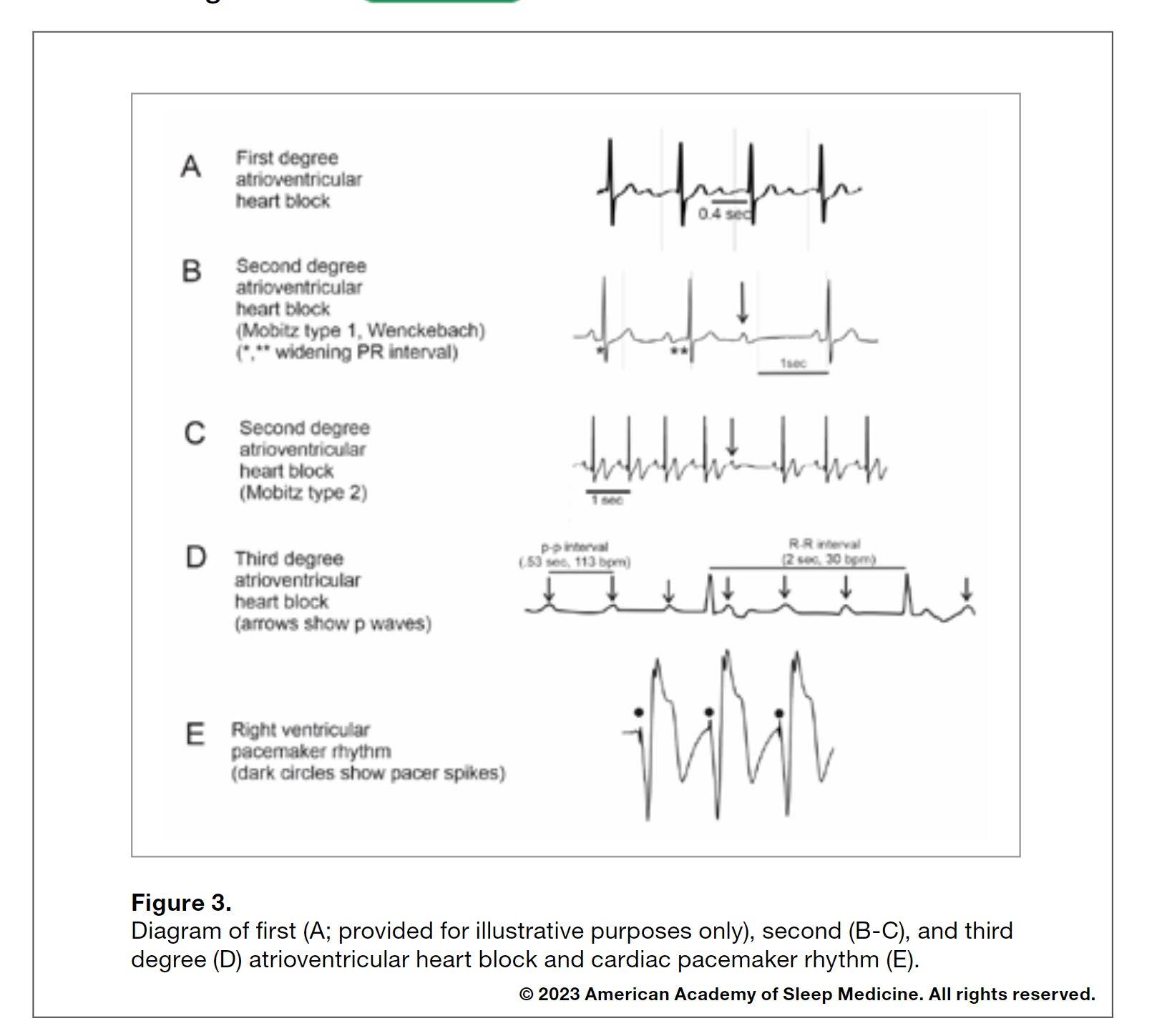
The University of Michigan Medical School is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The University of Michigan Medical School designates this live activity for a maximum of 12.75 AMA PRA Category 1 Credit(s) ™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
PLANNING COMMITTEE
Educational Planners
Neeraj Kaplish, M.B., B.S.
Associate Professor, Neurology
University of Michigan Health
Cathy A Goldstein, MD
Clinical Professor, Neurology
University of Michigan Health
Activity Coordinator
Erika Laszlo
Outreach Manager
University of Michigan Health

TABLE OF CONTENTS Decoding Fatigue: Lessons from Neurological Conditions....................................................................................4–64 Tiffany J. Braley, MD, MS Pharmacological Management of Sleep in Older Adults.......................................................................................65–130 Chandra Cherukuri MD, MS Best Practices for the Management of Chronic Insomnia Disorder.......................................................................131–162 J. Todd Arnedt, Ph.D. Artificial Intelligence in Sleep Medicine:Where are we Now and Where are we Going?........................................163–234 Cathy Goldstein, MD High Acuity Patients in Sleep Labs: Ensuring Patient Safety.................................................................................235–310 Douglas Kirsch, MD, FAAN, FAASM
Decoding Fatigue: Lessons from Neurological Conditions

Tiffany J. Braley, MD, MS
Associate Professor of Neurology
Holtom-Garrett Family Professor of Neurology
Divisions of MS/Neuroimmunology and Sleep
Department of Neurology, University of Michigan
1
Disclosures
• Current/recent research support:
• NIH/NCCIH(1R01AT011341-01)
• NIH/NIA (1R01AG074342-01)
• Patient Centered Outcomes Research Institute (MS-1610-36980)
• National Multiple Sclerosis Society (RG 5280-A-2)
• American Academy of Sleep Medicine Foundation (115-SR-15)
• Intellectual property: patent application for sleep apnea treatment
• Consulting/Advising: Jazz Pharmaceuticals
2
Objectives
• Review the prevalence and impact of pathological symptomatic fatigue
• Discuss causes and contributors to fatigue, with an emphasis on sleep disorders
• Describe lessons from the multiple sclerosis (MS) population as an ideal basis for the study of fatigue measurements and interventions
• Discuss limitations of current measures used in fatigue research/clinical care, and potential solutions
• Review current pharmacological and non-pharmacological therapies MS fatigue, and discuss new approaches to treatment optimization
3
Fatigue as a symptom
• Subjective symptom
• Perceived lack of physical or mental energy, that occurs following lower than expected levels of exertion
• May be:
• Acute (triggered by illness, bout of unusual stress or over-exertion), temporary
• Chronic (>=6 months), present with lower-than-expected levels of exertion, interferes with usual or desired activities
• Distinct construct from sleepiness, not a tendency to doze
4
Consequences of Chronic Fatigue

• Absenteeism
• Loss of employment
• Reduced productivity
• Accidents
• Reduced social participation

• Worse quality of life
• Early recognition is crucial
5
Who is at risk?
• Common, cuts across multiple medical conditions and stages of life
• Older adults (age 65 and above)
• Perimenopausal women
• Mood disorders (depression)
• Endocrine disorders
• Chronic heart and lung conditions
• Cancer
• Obesity
• Connective tissue disease (RA)
• Osteoarthritis
• Fibromyalgia
• Chronic Fatigue Syndrome (Myalgic Encephalomyelitis)
• Chronic infection (post-COVID)
• Chronic neurological conditions
• Stroke
• Parkinson’s
• Multiple Sclerosis
• One of the top 10 reasons for primary care consultation
• Direct relevance for all providers
6
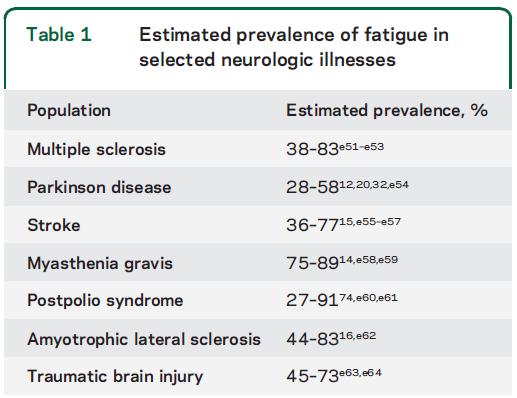
Kluger et al, Neurology 2013 7
Multiple Sclerosis
• Chronic, inflammatory disorder of the central nervous system which results in myelin damage and axonal degeneration (causes multifocal but also widespread inflammation and damage)
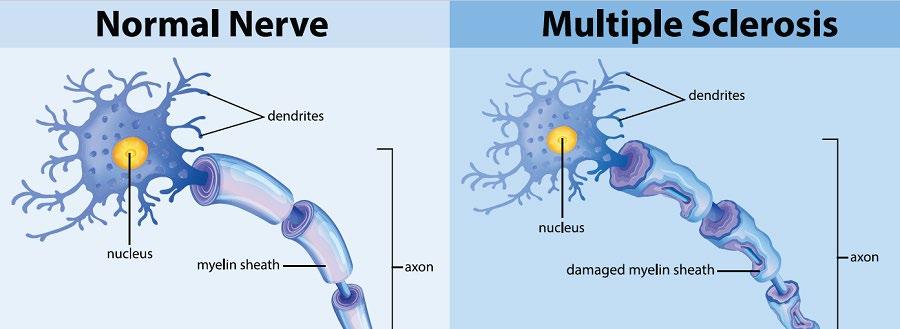
• Most common cause of non-traumatic disability among young adults
• Nearly 1 Million people in the US affected
*Wallin et al, ECTRIMS 2017 8
“Invisible” Symptoms of MS
• FATIGUE (90%!)

• Sleep disturbances
• Chronic pain
• Cognitive impairment
• Depression
• Anxiety
9
One of the most challenging symptoms to treat
10
Main challenges/barriers
1) No unified definition of fatigue
2) Limitations of current measures used in research/clinical care
3) Multifactorial nature of fatigue (importance of sleep)
4) Limitations in clinical trials of interventions
11
Challenge #1: No unified definition
• “A subjective lack of physical and/or mental energy that is perceived by the individual or caregiver to interfere with usual or desired activity”* (PVA consensus statement for MS fatigue)
• Subjective, complex symptom without a unified definition
• Terms may be interpreted differently depending on cultural or educational backgrounds
*Multiple Sclerosis Council for Clinical Practice Guidelines. Washington, DC: Paralyzed Veterans of America; 1998.
12
Overlapping descriptors
• Exhaustion
• Tiredness
• Lack of energy
• Sleepiness
• Separate construct, propensity to doze (sedentary situations exacerbate)
• Term used interchangeably with fatigue with moderate correlation (rho=0.3-0.5)
• May be present concomitantly
• MS patients with sleepiness may share a propensity for terms other than sleepiness to describe their symptoms
Braley et al, Mult Scler Int’l 2012 Braley et al, JCSM 2013 Brass et al, JCSM 2013 Kaminska et al, Mult Scler 2012 Popp et al, Sleep Med Rev 2017 13
Challenge #2: Limitations of measures
• No gold standard exists by which to measure fatigue
• Self-report measures assess fatigue within a set, retrospective time frame
• Fatigue Severity Scale (7 days)
• Fatigue Impact Scale/Modified Fatigue Impact Scale (4 weeks)
• Chalder Fatigue Scale (last month)
• PROMIS Fatigue Short form (7 days)
• Limited by recall bias and memory decay
• Do not define fatigue from the outset (what if the patient is sleepy?)
• No accounting for temporal variability or activity level
• Better assessment methods are needed for clinical practice and interventional research
14
Fatigue Severity Scale (“over the past 7 days…”)

Krupp 1988 15
A tale of two fatigue treatments
16
Participant A Participant B
A tale of two fatigue treatments
Participant A
• 49 year old male
Participant B
• 47 year old male
17
A tale of two fatigue treatments
Participant A
• 49 year old male
• RRMS, EDSS: 3.5
Participant B
• 47 year old male
• RRMS, EDSS:4.0
18
A tale of two fatigue treatments
Participant A
• 49 year old male
• RRMS, EDSS: 3.5
• Baseline FSS: 42
Participant B
• 47 year old male
• RRMS, EDSS:4.0
• Baseline FSS: 42
19
A tale of two fatigue treatments
Participant A
• 49 year old male
• RRMS, EDSS: 3.5
• Baseline FSS: 42
• Followup FSS at 6 months: 40
Participant B
• 47 year old male
• RRMS, EDSS:4.0
• Baseline FSS: 42
• Followup FSS at 6 months: 30
20
Is treatment B more effective?
21
A tale of two fatigue treatments
Participant A
• 49 year old male
• RRMS, EDSS: 3.5
• Baseline FSS (past week): 42
• Followup FSS at 6 months: 40
22
A tale of two fatigue treatments
Participant A
• 49 year old male
• RRMS, EDSS: 3.5
• Baseline FSS (past week): 42
• Followup FSS at 6 months: 40
• Over the past 6 months, adopted a regular exercise program and just ran his first 5K
23
A tale of two fatigue treatments

Participant B
• 47 year old male
• RRMS, EDSS: 4.0
• Baseline FSS: 42
• Followup FSS at 6 months: 30
24
A tale of two fatigue treatments
Participant B
• 47 year old male
• RRMS, EDSS: 4.0
• Baseline FSS: 42
• Followup FSS at 6 months: 30
• Over the past 6 months, received social security disability, has scaled back on activities
Overall, this patient’s fatigue may have improved at the expense of daily activities

25
Perceived (Subjective) Fatigability
Subjective fatigability = self-rated fatigue/objective activity
*B.A. Eldadah, 2010

“A whole-person construct in which fatigue, a self-reported parameter, is normalized to a level of activity.”*
26
Within-person variability
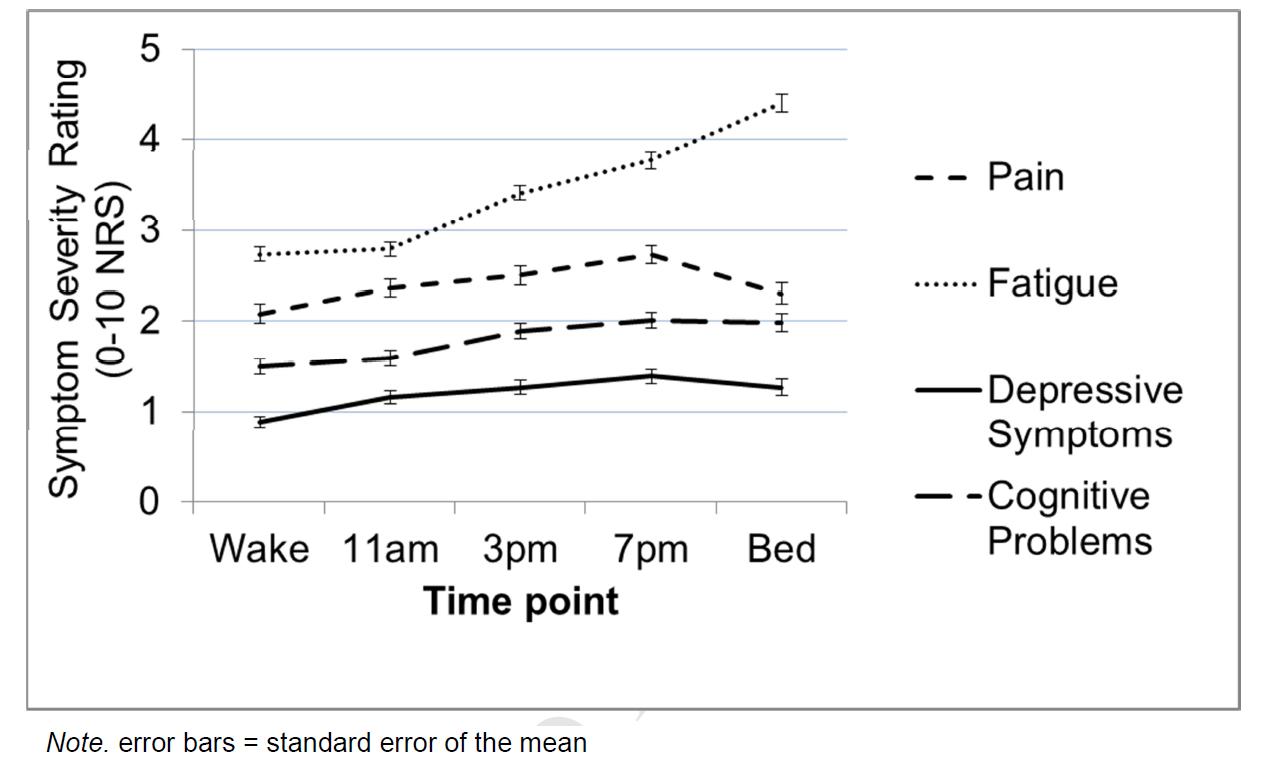
• Repeated-measures observational study n=107 MS patients
• Objective: Characterize within- and between- day experience of fatigue and other symptoms in PwMS
• PRO-Diary® Ecological Momentary Assessment:

• Allows for self-rating repeated measures of fatigue and other common symptoms on a 0-10 numerical rating scale (“What is your level of fatigue right now?”)
• Assessed fatigue, pain, perceived cognitive function, and depressive symptoms
• 5 times per day for 7 days
• Findings
• Fatigue levels are dynamic throughout the day
• Diurnal fluctuations in fatigue levels also correlate with other symptoms
• Within-day Higher pain was associated with higher subsequent fatigue
• Within-day Higher fatigue related to higher subsequent pain
• Across days - A day of higher than average fatigue was associated with lower fatigue the next day
2017 27
Kratz, Murphy, and Braley, Arch Phys Med Rehab
28

29
Challenge #3: Fatigue is multifactorial
Proposed neuroanatomical and immunological (primary) causes in MS
- Inflammatory causes
1. Braley TJ et al,.J Clin Sleep Med 2014;10:155–162.
2. Brass et al. J Clin Sleep Med 2014;10:1025–1031.
3. Bøe Lunde HM et al. PLoS One 2012;7:e49996.
4. Neau J-P et al. Eur Neurol 2012; 68:8–15.
5. Merlino G et al. Sleep Med 2009;10:26–34.
6. Tachibana N et al. Eur Neurol 1994;34:320–3.
7. Amtmann D et al. Rehabil Psychol 2015;60:81–90.
8. Novo AM et al. Neurol Clin Pract 2018;8:492–500.
9. Heesen C et al. J Neurol Neurosurg Psychiatry 2006;77:34–39.
10. Ehde DM et al. Arch Phys Med Rehabil 2015;96:1945–1958.
11. Patrick E et al. Mult Scler 2009;15:258–261.
12. Fiest KM et al. Int J MS Care 2016:18:96–104.
CNS, central nervous system
Comorbid
physiological causes
or contributors in MS
- Sleep disorders
- Pain
- Medical Comorbidities
- Polypharmacy
- Endocrine influences
- Micro/macrostructural and functional changes in the brain
Fatigue
Psychological or behavioral contributors
- Mood disorders
- Maladaptive behaviors
- Lifestyle factors
30
Cognitive and behavioral model for fatigue in MS

31
Van Kessel et al 2006
Where does sleep fit in?

32
Obstructive sleep apnea (OSA)
• Underdiagnosed in MS*
• Higher prevalence/greater severity in MS?*
• Brainstem involvement

• C-spine lesions?
• Progressive MS subtypes
• Symptomatic therapies
• DMTs protective?
• OSA and other sleep disturbances linked to fatigue in MS†
*Braley et al, JCSM 2014, Braley et al, Neurology 2012
Brass et al, JCSM 2014
Braley et al, SLEEP 2018
†Braley et al SLEEP 2016
Brass et al, JCSM 2014
Brass et al, JCSM 2014
Kaminska et al,
Veauthier et al,
Braley et al, SLEEP 2018
Whibley et al, MSARD 2021
33
Fatigue (in addition to sleepiness) is a common consequence of OSA

• Chervin RD, CHEST 2000
• Observational study: 117 men and 73 women referred for PSG with AHI>=5
34
Chervin, CHEST 2000 Con’t
• Results
• Subjects more frequently reported problems with fatigue, tiredness, and lack of energy than sleepiness (57%, 61%, and 62%... vs 47%)
• Lack of energy was most frequently reported as the most problematic
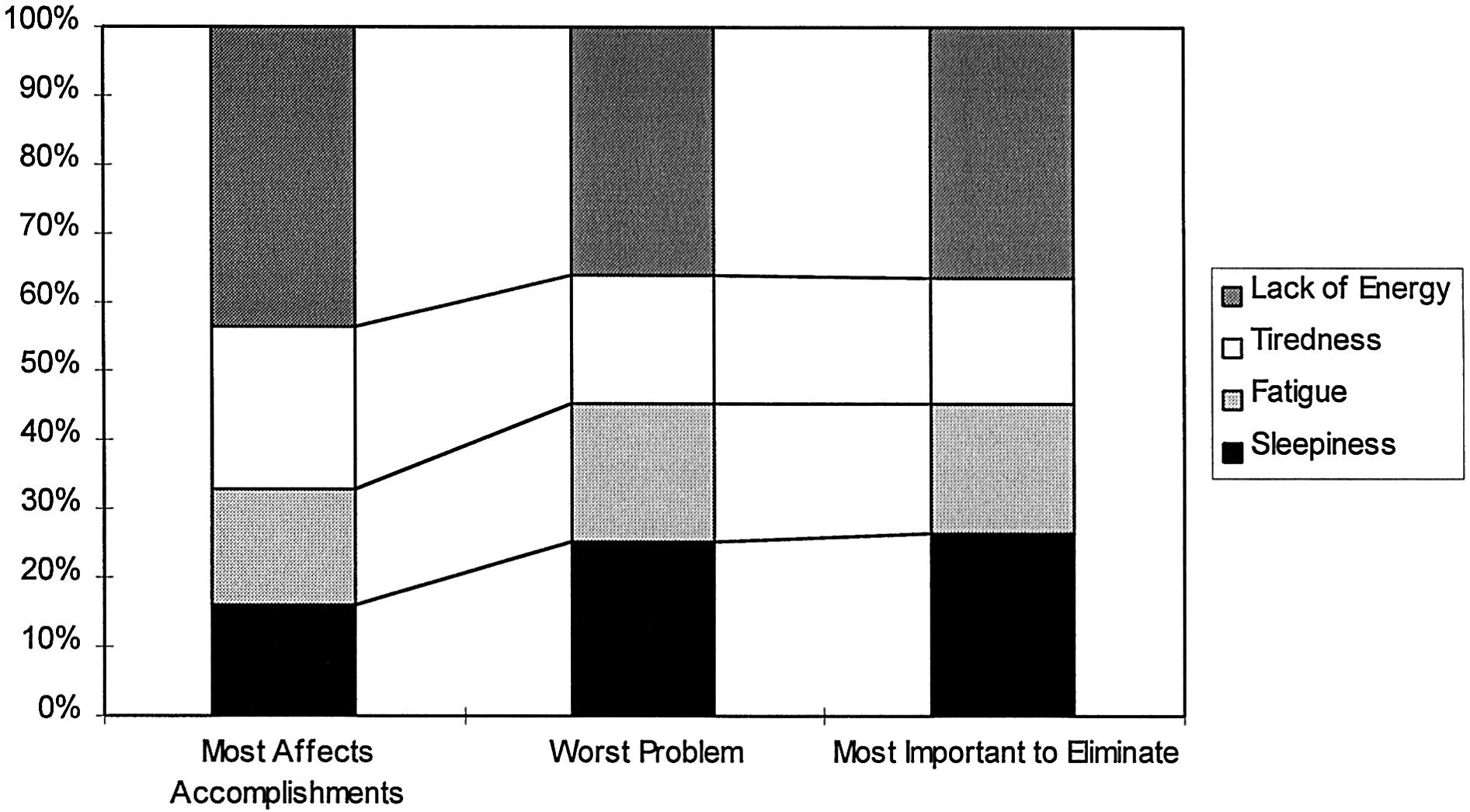
• Conclusions:
• People with OSA may experience more issues with fatigue, tiredness, or lack of energy, than sleepiness
• The diagnosis of OSA should not be excluded based only on a person’s tendency to emphasize fatigue, tiredness, or lack of energy more than sleepiness
35
Treatment of OSA alleviates fatigue
• Chotinaiwattarakul et al, JCSM 2009
• Surveys querying same questions regarding fatigue, tiredness, lack of energy, and sleepiness mailed to patients diagnosed with OSA, 6 months to 3 years after they were prescribed PAP
• Adequate PAP adherence was defined as greater than 5.0 hours of selfreported PAP use per night on average • 279 OSA patients (183 adherent to PAP and 96 inadequately treated or untreated) were analyzed
36
• At follow-up, each symptom was significantly less common among PAP-adherent subjects than among inadequately treated subjects
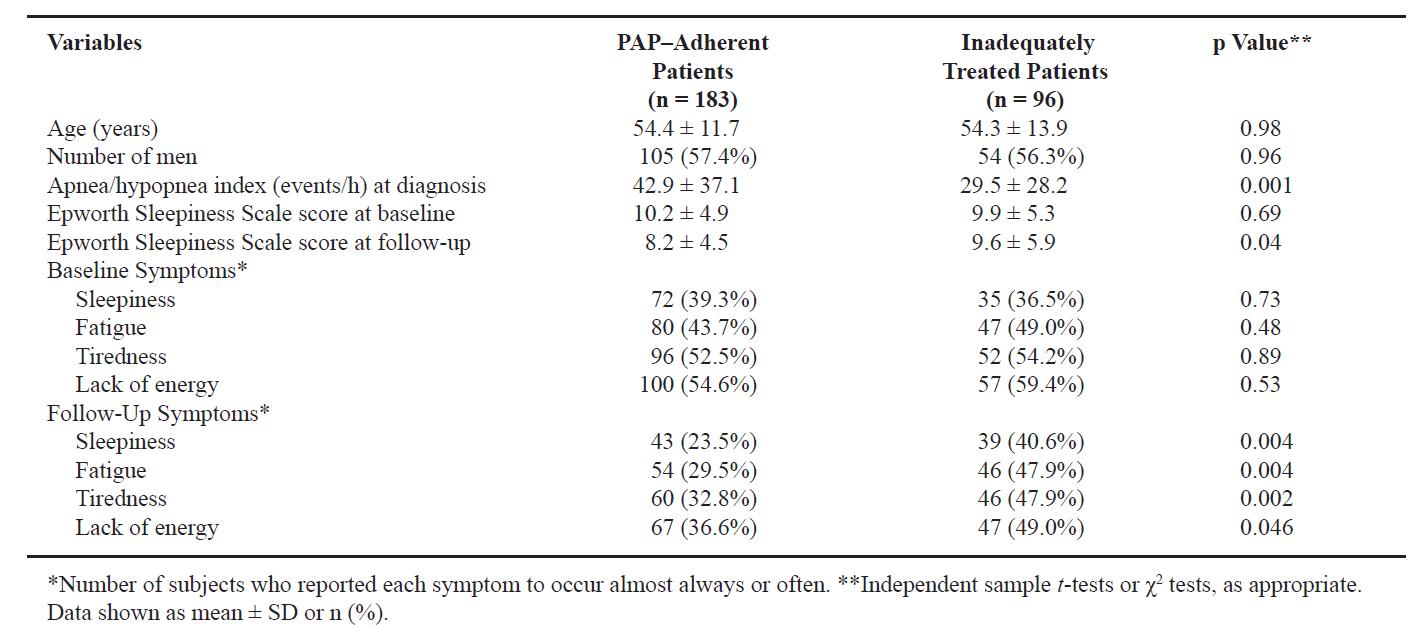
Chotinaiwattarakul et al, JCSM 2009
37
Restless Legs Syndrome
• Literature regarding links between RLS and fatigue in the general population is scarce, but consensus statements support an association
• Several studies more clearing linking RLS to fatigue in chronic conditions, including MS:
• Cederberg et al, J Sleep Res 2020 (MS)
• Pascazio et al, Mult Scler Relat Disord 2023 (MS)
• Giannaki et al, World J Nephrol 2017 (hemodialysis)
• Cavalcante et al, Sleep Med 2012 (COPD)
• More research needed to understand the scope and mechanisms of fatigue in RLS, and how RLS and its treatment could influence fatigue approaches
38
Insomnia
• Fatigue is a core symptom of chronic insomnia, more so than sleepiness*
• Several core insomnia symptoms overlap with common “invisible” symptoms in chronic diseases like MS (cognitive, mood, occupational issues) – consider insomnia screen if such symptoms are present
• Mechanisms underlying the association between insomnia and fatigue are likely complex, and may vary across populations
• CBT-I is beneficial for fatigue associated with insomnia, in both MS and non-MS samples† and is generally favored in MS over pharmacological approaches
*Schutte-Rodin et al, JCSM 2017
†Redeker et al, SLEEP 2022
Smyth et al, Australas J Ageing 2023 39
Approach to fatigue assessment/treatment
• Ask patient to provide a thorough description of the symptom
• Assess aggravating/alleviating factors
• Is sedentary behavior vs. sustained activity a trigger?
• Is napping vs non-sleep rest periods restorative?
• Rule out/address secondary causes first
• Thorough history and physical examination, and/or referral to PCP or appropriate specialists for evaluation (SLEEP)
• Consider symptomatic fatigue treatment if residual symptoms are present
40
Complex problems, interdisciplinary solutions
Mood disturbances
Medical Comorbidities
Fatigue
Sleep problems
Medications, polypharmacy
Chronic Pain
Spasticity
Cognitive dysfunction
41
Multidisciplinary MS Fatigue and Sleep Clinic
• Launched in 2015 at Michigan Medicine

• Mission: to provide a comprehensive, multidisciplinary approach to MS fatigue that incorporates dedicated sleep assessment
• Thorough evaluation of potential underlying causes, with an emphasis on sleep disorders and nocturnal symptoms)
• Management tailored to the patient’s clinical picture
42
Challenge #4: Major Interventional
Research Gaps
(1) Limitations of clinical trial designs/lack of”real-world” approaches, including trials of combination therapies
(2) Lack of accounting for common treatment effect modifiers associated with MS that contribute to fatigue (depression, sleep, and progressive MS/disability severity)
(3) Lack of patient-centered fatigue outcome measures
43
Fatigue Interventions
44
Rehabilitative and pharmacological approaches used in MS and neurological disorders
Rehabilitation (non-pharmacological) Interventions
Physical
Exercise therapies
Aquatic therapy
Tai-Chi
Cooling therapy
Behavioral/Psychological Pharmacological Interventions
Modafinil
Amantadine
Cognitive behavioral therapy
Energy conservational strategies
Mindfulness-based strategies
Methylphenidate
Dextroamphetamine-Amphetamine
Dalfampridine
Aspirin?
Acetyl-L-carnitine?
45
Cognitive Behavioral Therapy (CBT)
• Promotes effective self-management skills
• Teaches goal-setting and behavioral activation strategies to target maladaptive thoughts and beliefs that can perpetuate symptoms
• Effective for multiple symptoms, across conditions
• Depression/PTSD
• Insomnia
• Pain
• Considered 1st line treatment for MS fatigue*
• Access for MS-related fatigue remains limited
*Edhe et al Arch PMR 2015 Van den Akker Mult Scler 2017 Finlayson et al Mult Scler 2011 Van Kessel et al Psychosom Med 2008 46
Cognitive and behavioral model for fatigue in MS

Van Kessel et al 2006
47
Pharmacological Treatments
• Most commonly prescribed/studied for generalized fatigue:
• Amantadine
• Modafinil/Armodafinil
• Stimulants
• Methylphenidate
• Amphetamine/Dextroamphetamine
• Under investigation for generalized fatigue
• Aspirin
• Acetyl-L-carnitine
• Walking speed/endurance
• Dalfampridine – observational study in support of generalized fatigue(?)
48
Amantadine (Symmetrel®, GOCOVRI®)
• FDA approved for prophylaxis/treatment of influenza A
• Also FDA-indicated for parkinsonism and drug-induced extrapyramidial reactions, PD-induced dyskinesia
• Mechanism of action for MS-related fatigue remains unclear
• Affects dopaminergic transmission
• Also anticholinergic properties (nicotinic antagonist)
• Weak NMDA receptor antagonist
• Although generally accepted as modestly effective and “first line” pharmacological therapy for MS fatigue, prior Cochrane review does not support its use (Pucci 2007)
Pucci E, et al. Cochrane Database Syst Rev 2007 49
Modafinil (Provigil®)
• Commonly used for MS-fatigue
• FDA-approved to treat sleepiness/fatigue secondary to sleep disorders
• Obstructive sleep apnea
• Narcolepsy
• Shift work disorder
• “Wake-promoting agent” (possible motivational/cognitive enhancement*)
• Stimulates histamine, norepinephrine, serotonin, dopamine (DA transporter blockade)*, and orexin systems
• Prior trials have yielded mixed outcomes precluding formal recommendations regarding use of this drug for MS fatigue
*Volkow et al, JAMA 2009 Young et al, Biol Psych 2010 Minzenberg et al, Neuropsychopharmacology 200850
Methylphenidate (Ritalin®)
• CNS stimulant
• FDA approved for ADHD and narcolepsy
• Prior dedicated trials for MS fatigue are scarce
• 1 small study that focused on people with balance/walking difficulties showed no benefit over placebo for MS fatigue*
• Mixed data for fatigue in other medical conditions *Cameron et al Mult Scler
2017 51
Incorporates personalized fatigue measures
Additional research is needed that….
Considers personal traits that may influence response to treatment (effect modifiers)
• Sleep
• Disability
• Depression
• Comorbidities
Employ multimodal (pharmacological + nonpharmacological) treatment approaches

52
Multimodal approaches
Fatigue is multifactorial
In some cases, CBT is most effective when it's combined with other treatments (depression)

53
Multimodal approaches that combine behavioral and pharmacological strategies are insufficiently studied in MS fatigue
A randomized controlled trial of telephone-delivered COgnitive behavioral-therapy, Modafinil, and combination therapy of BOth interventions for fatigue in MS (“COMBO-MS”)
• Pragmatic 2-center RCT (U Michigan and U Washington)
• Sponsor: Patient-Centered Outcomes Research Institute (PCORI)
• Measure benefits and harms to determine which clinically available therapies work best for different types of patients
• Employ “real world” approach - trials reflect the complexities of real world patient populations and clinical practices
• Informed by stakeholder input
• Inventions:
• Modafinil (50 mg daily – 200 mg BID) X 12 weeks
• Telephone-based CBT (8 weekly sessions + 2 biweekly booster sessions)
• Combination therapy
PIs: Braley and Kratz
UM Co-I’s: Ron Chervin
Ben Segal
Rod Little Deirdre Conroy
UW Co-Is: Kevin Alschuler (site PI)

Dawn Ehde
Gloria Von Geldern
Stakeholders: Patients (UM and UW)

Providers (UM + community)
NMSS
Blue Care Network
IHPI 54
COMBO-MS Trial
• Measures
• Modified Fatigue Impact Scale
• EMA measures of fatigue severity and impact (4 times per day)

• Accelerometry (activity level)

• Fatigue severity/activity level = subjective fatigability
• Effect Modification
• MS subtype (relapsing vs. progressive)
• Sleep (sleep disorders, sleep hygiene, excessive daytime sleepiness)
• Depression
55
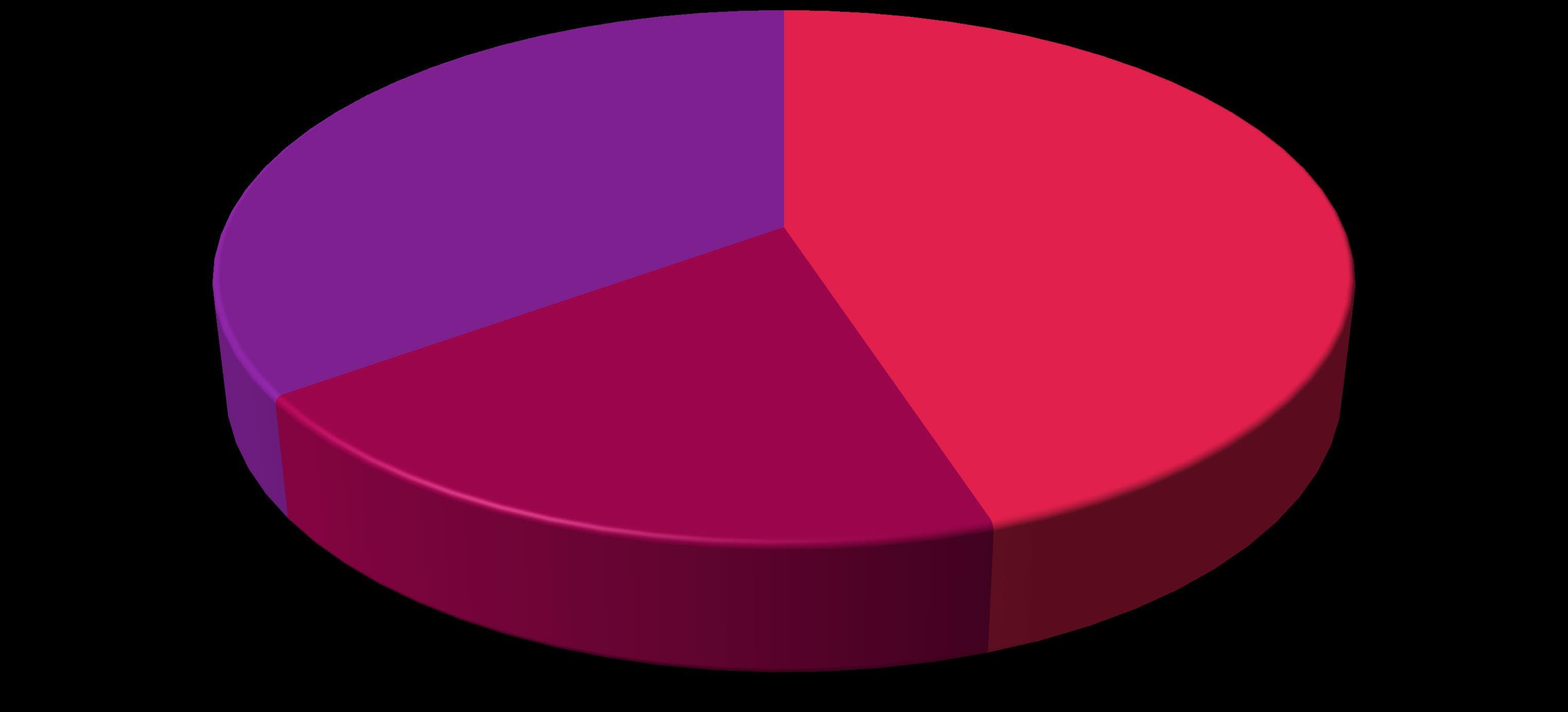
Results
• 336 participants completed the study
• At 12 weeks, all 3 interventions were associated with statistically significant and clinically meaningful reductions in MFIS score
• CBT: 15.2 (SD=11.9)
• Modafinil: 16.9 (SD=15.9)
• COMBO: 17.3 (SD=16.2)
• Patient Global Impression of Change scores were highest for COMBO therapy
Data under review
56

Data under review 57
Responder analyses
Improvement in Modified Fatigue Impact Scale (MFIS) Score from baseline to week 12

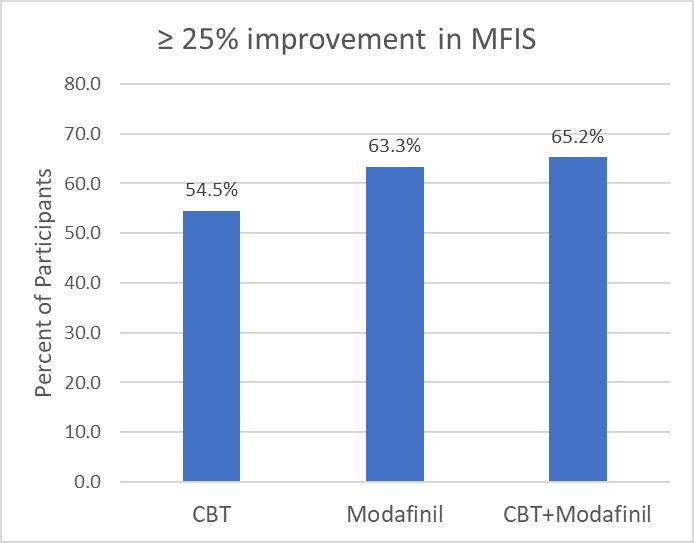

Data under review 58
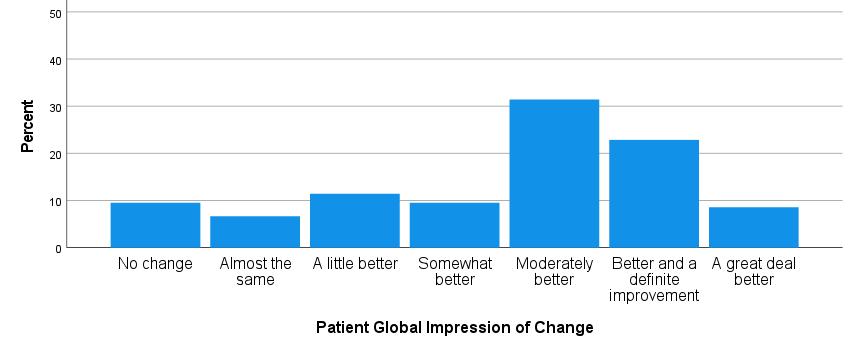

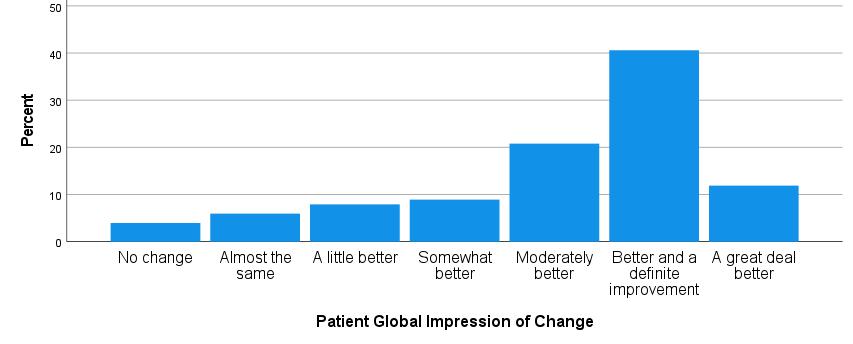
Modafinil CBT Combo Mean ± SD Median (IQR) 4.5 ± 1.7 5.0 (3,5,6) Mean ± SD Median (IQR) 4.74 ± 1.6 5.0 (4,5,6) Mean ± SD Median (IQR) 5.06 ± 1.6 6.0 (4,6,6) *p<0.01 Data under review 59
Direct effects of sleepiness (ESS) on MFIS and EMA Fatigue scores
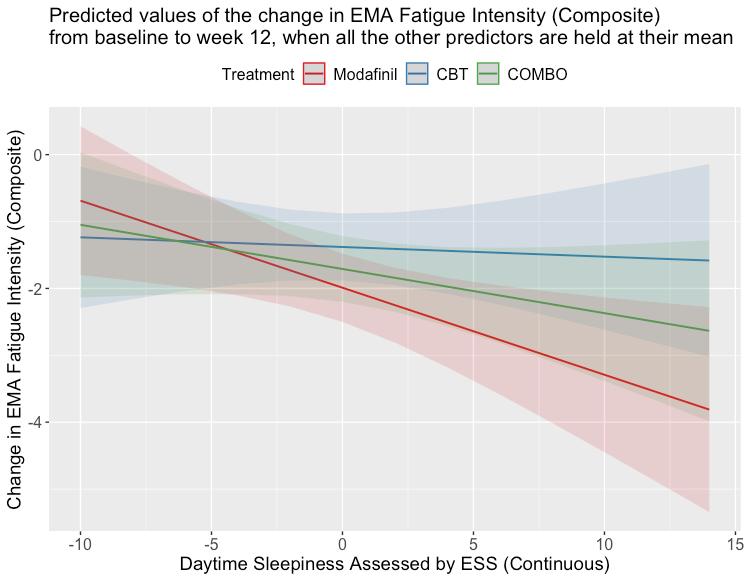

Data under review 60
Sleep Hygiene as an effect modifier on MFIS
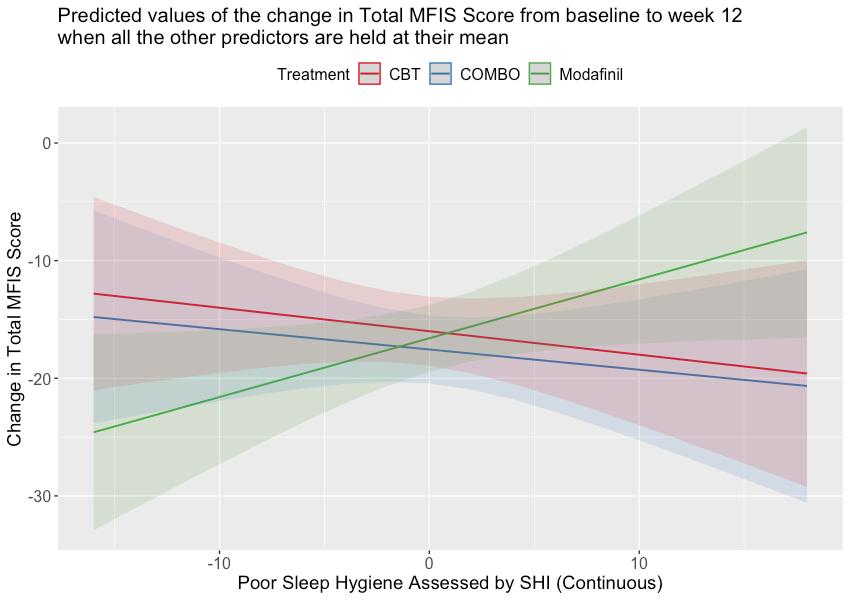
Data under review 61
Future Directions
Longitudinal sleep and circadian tracking MS outcomes and interventions

62
Conclusion
• Fatigue is common
• Impactful with potentially far-reaching consequences
• Dynamic, highly personalized symptom with many potential causes/contributors
• Treatable, but requires a detailed evaluation
• Useful treatments available, but additional research on more personalized treatment approaches is necessary
63
Special thanks
UM Sleep Division
• Ronald Chervin, MD, MS
• Galit Dunietz, PhD
• Cathy Goldstein, MD, MS
• Neeraj Kaplish, MD
• Shelley Hershner, MD
• Sonja Schuetz, MD

UM Physical Medicine and Rehabilitation

• Anna Kratz, PhD
• Daniel Whibley, PhD
• Tom Valentine, PhD
• David Johnson, RRT, CCRP
• Kristin Pickup, MSW
• Shay Robison
Michigan Technological University
• Joseph Burns, PhD
UM Chronic Pain and Fatigue Research center/Anesthesiology


• Daniel Clauw, MD
• Kevin Boehnke, PHD
UM Mathematics/Arcascope, LLC
• Olivia Walch, PhD
UW Physical Medicine and Rehabilitation
• Kevin Alschuler, PhD
• Dawn Ehde, PhD
• Gloria von Geldern, MD
64
Pharmacological Management of Sleep in
Older Adults
- Chandra Cherukuri MD, MS
65
Disclosures
66
• I have no actual or potential conflict of interest in relation to this program/presentation

aa 67
Life Expectancy by AGE

• The longer you have already lived, the longer you can expect to live! 78.8 77 83.5 91.1 National Center for Health Statistics, National Vital Statistics System, Mortality 68

National Center for Health Statistics, National Vital Statistics System, Mortality 69
70

71
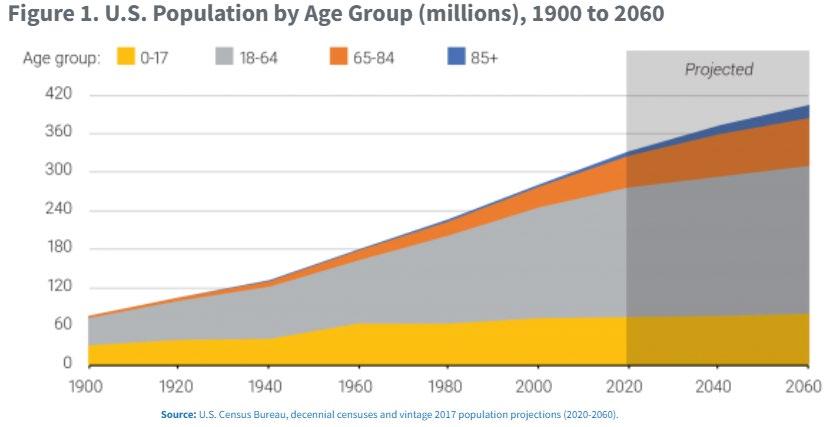
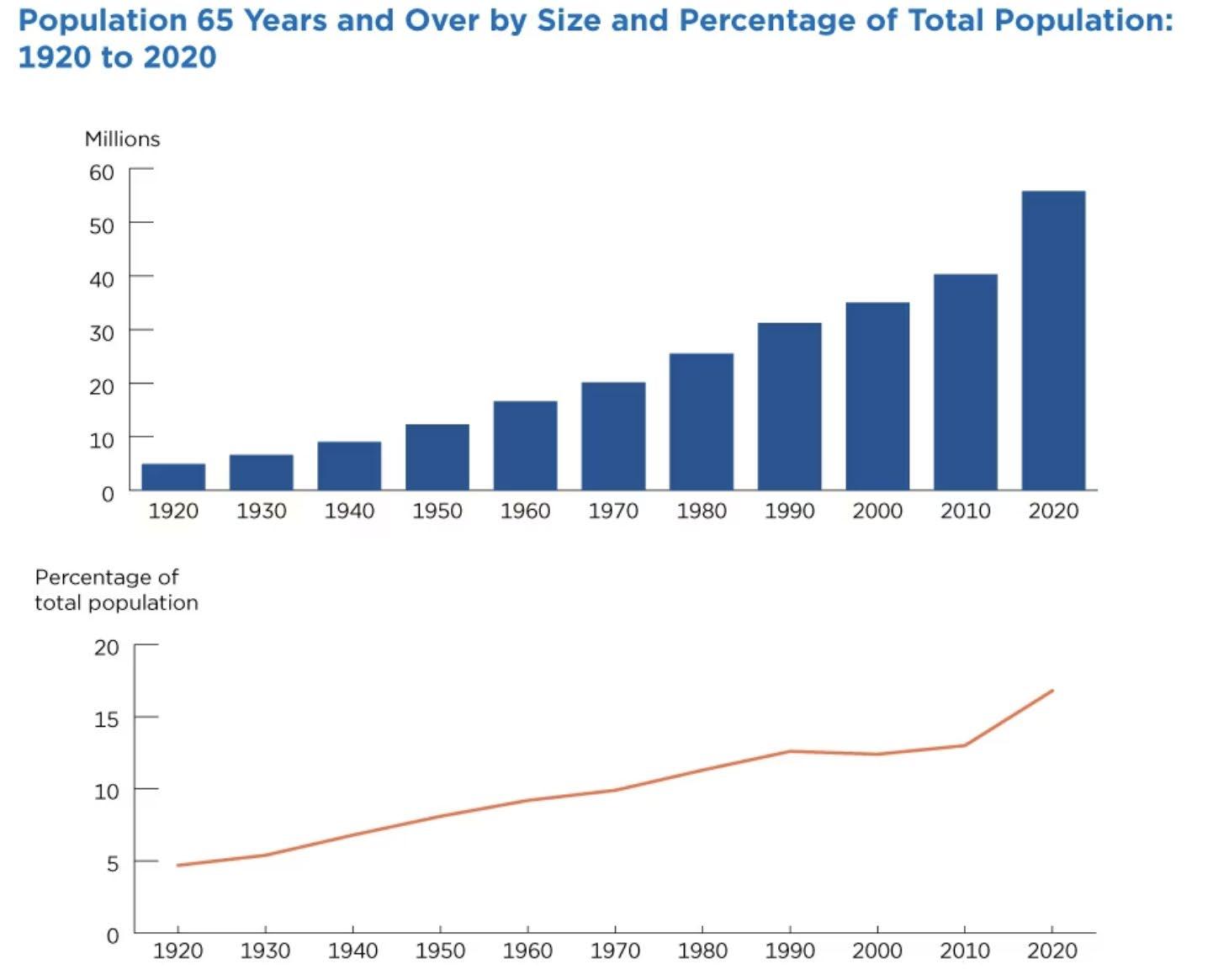
Aging population
Older adults (>65 yrs)
• By 2030, • ~72 million older adults (1 in 5 people)
72
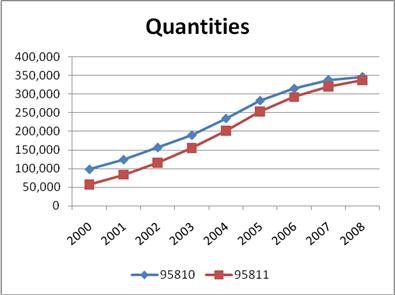
Over the past decade,
• significant rise in clinic visits and
• med use for insomnia (>5.5 mil clinic visits annually)
•
73

Sleep Health. 2015;1(1):40–43 74
75
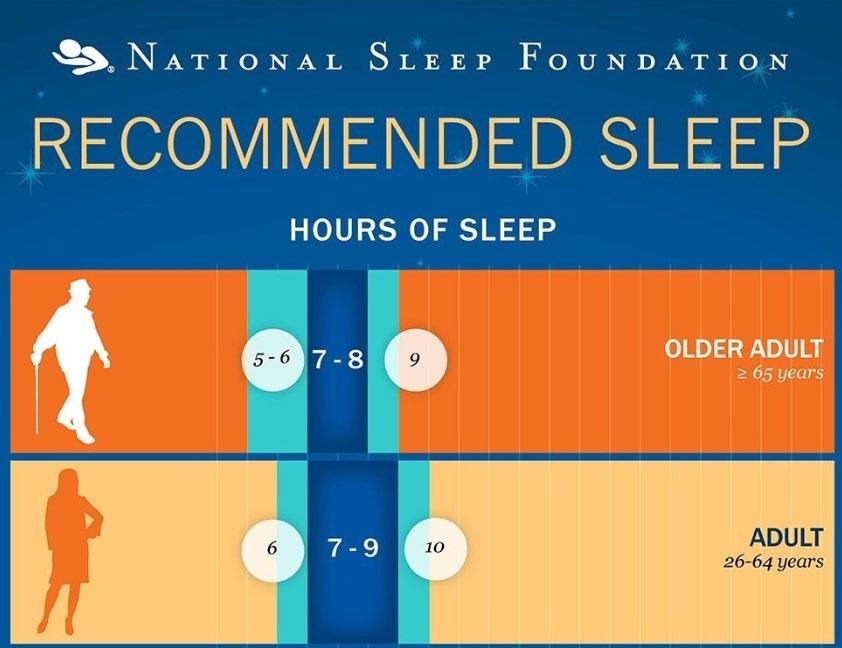
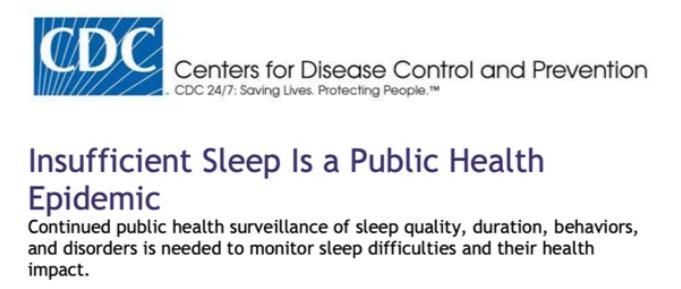
Prevalence of Short Sleep duration by US state

76
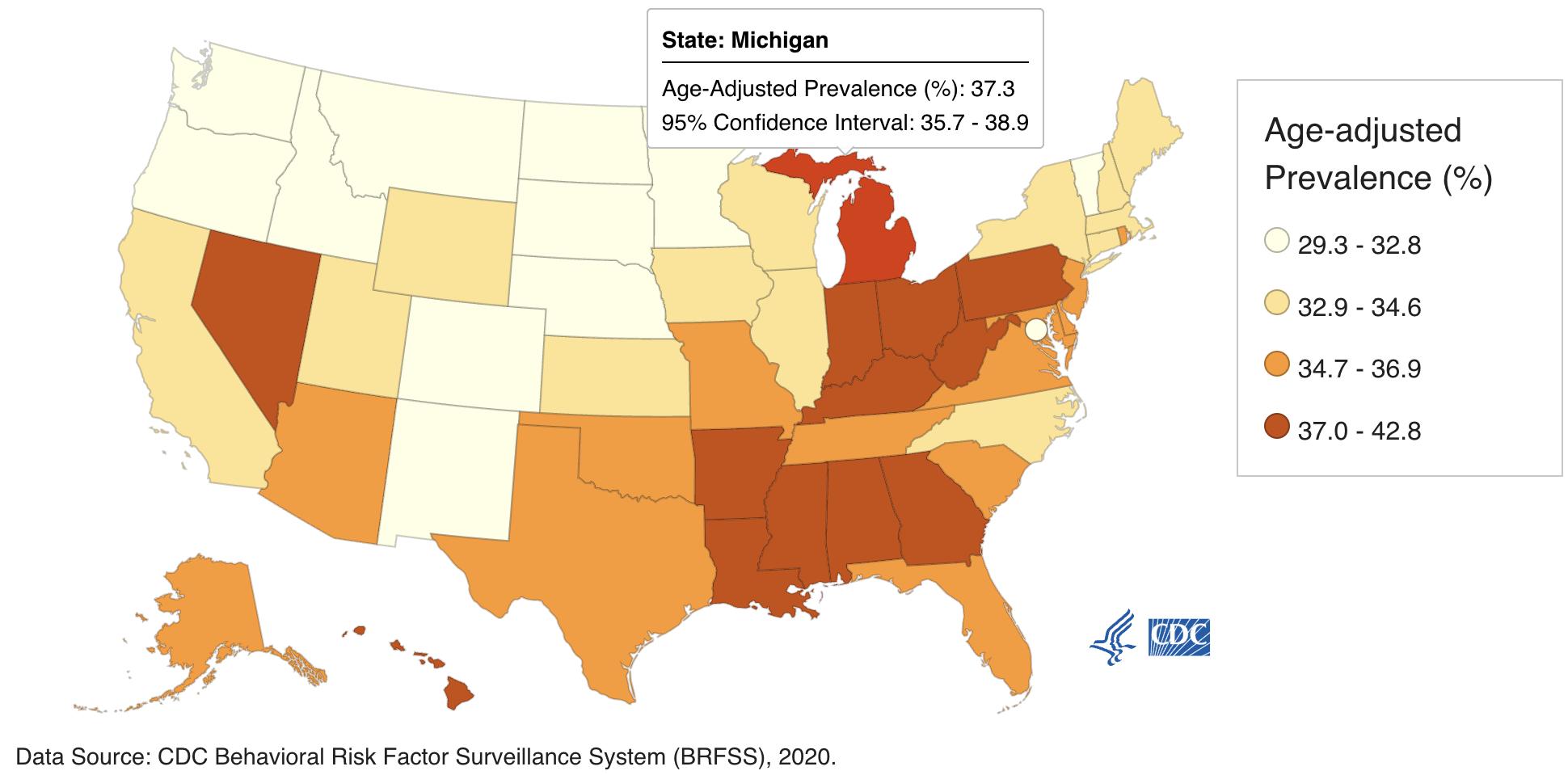
Prevalence Of Short Sleep By Age
Source: CDC Behavioral Risk Factor Surveillance System (BRFSS), 2020.
Older Adults- 26.1%
77
Physiological changes with normal human aging
• Advanced sleep timing
• More fragile sleep
• higher likelihood of waking by external stimuli
78
Sleep Architecture Across Life Span
Shorter and fewer NREM-REM sleep cycles
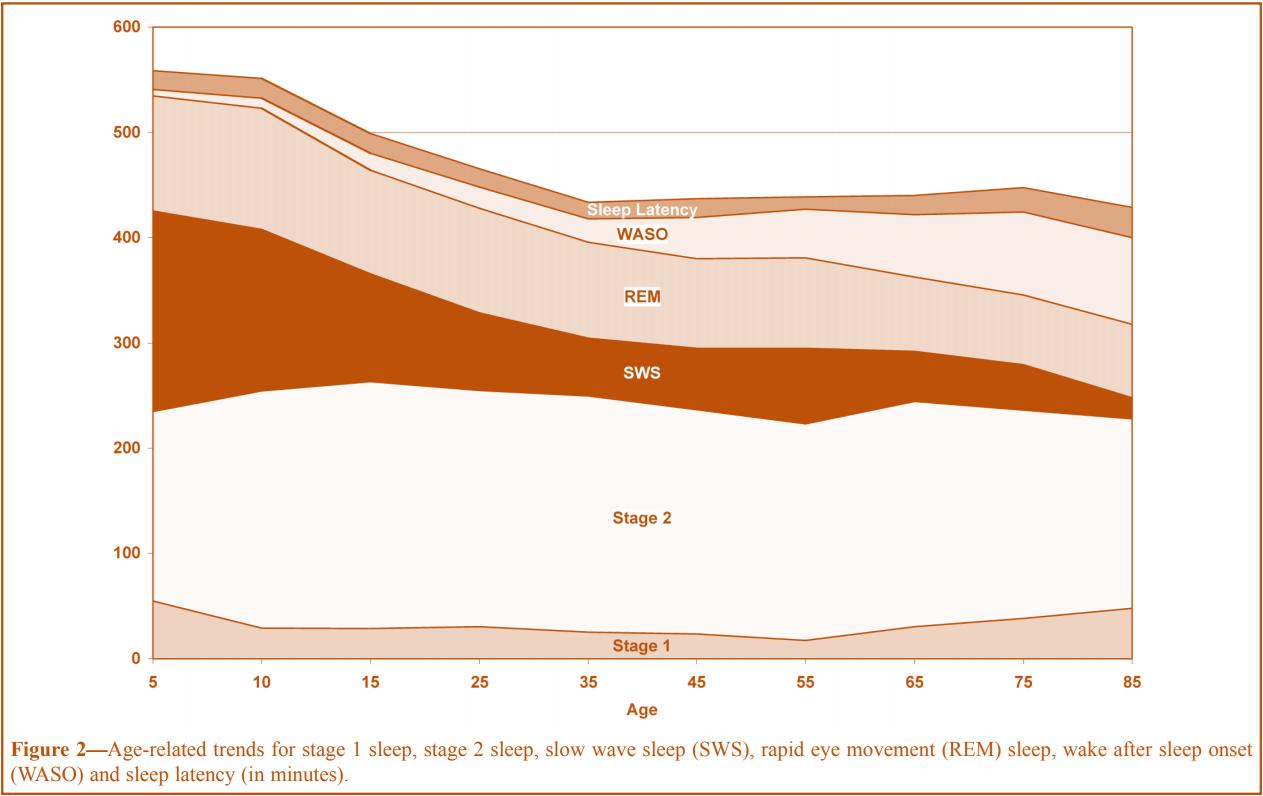
Increased NREM 1 & 2
Reduced NREM 3/ SWS
Shorter Latency to REM
Reduced Total REM sleep
Ohayon et al, Sleep 1994; 27(7): 1255-73 79
Macro sleep changes in older adults

Decrease Sleep Efficiency
Longer SOL
Increased FNA
Increased WASO
Decreased TST
80
Prevalence of Insomnia by age and sex
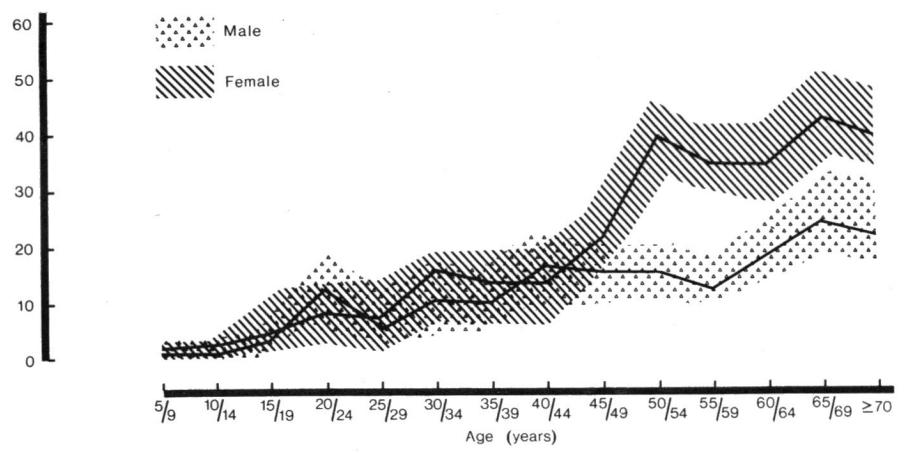
Cirignotta, et al. Clin Neuropharm, vol. 8, 1985 81
Insomnia as a predictor of Depression
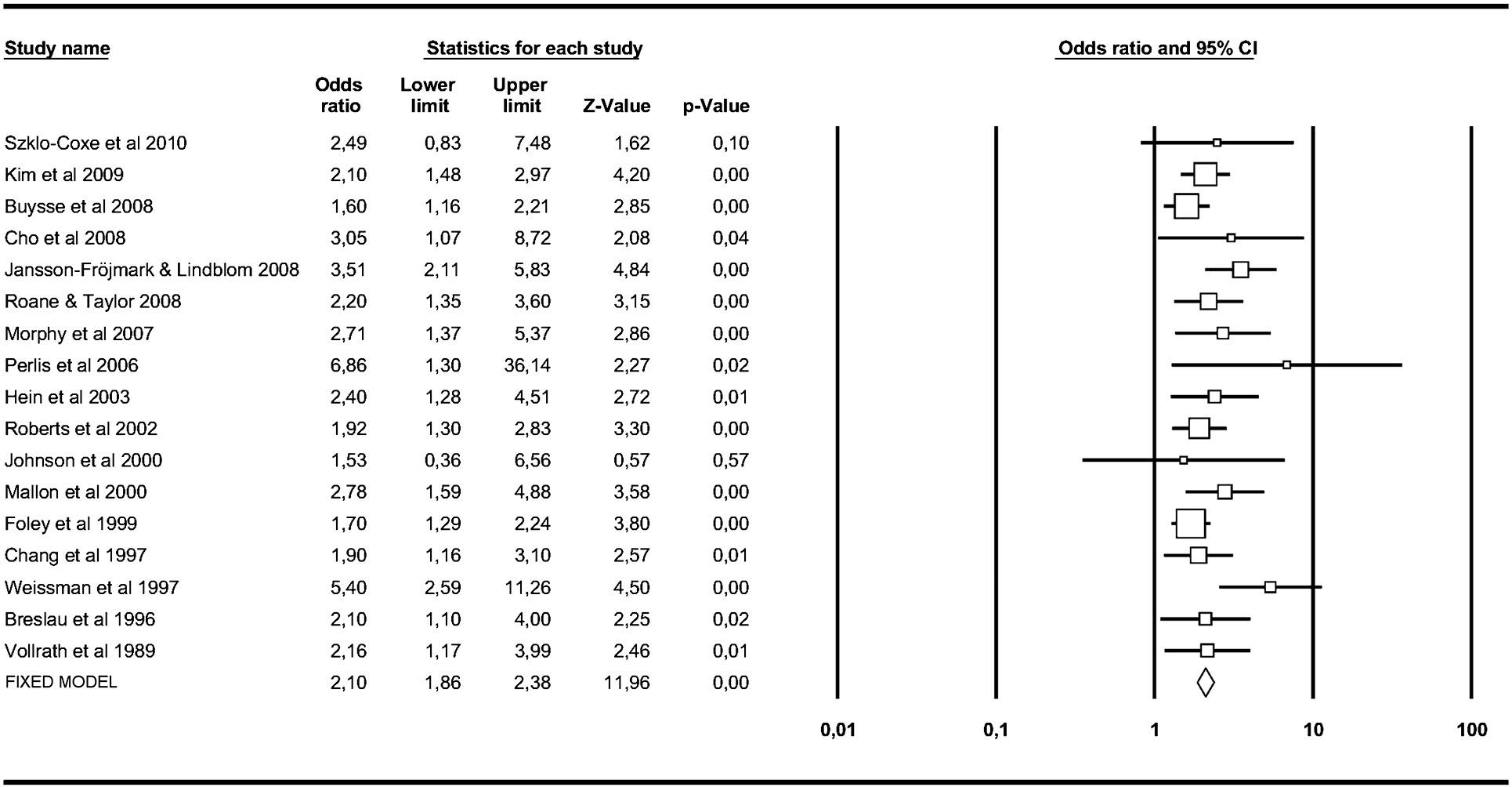
Baglioni et al. Journal of affective disorders vol. 135,1-3 (2011): 10-9. 82
Comorbidity of Sleep problems with DSM-IV disorders (NCS-R)
0 1 2 3 4 5 6 7 8 Sleep onset Sleep Maintainence Early morning Awake Non-restorative Sleep Any symptom ODDS RATIO Insomnia Symptoms Anxiety Disorder Mood Disorder Impulse Control Substance use disorder Any 3 or more Roth et al. Biological psychiatry vol. 60,12 (2006): 1364-71. 83
Risk Factors Associated with Poor Sleep
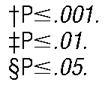
D A, and C A McHorney. Arch of intern med 1998; 158: 1099-107 84
Katz,
Impact of Insomnia symptoms on Health Care
Utilization in Older Adults (NHAT study)
0 0.2 0.4 0.6 0.8 1 1.2 1.4 1.6 1.8 2 ED visit Hospitalization 30-day Readmit Odds Ratio 2 symptoms 1 symptom *** * *** P < 0.001 * P < 0.05 * Tzuang M et al, Sleep 2021 May 14:44 (5) 85
CAUSES OF DISTURBED SLEEP IN OLDER ADULTS
Physiologic – Phase advance
Decreased Exposure to Zeitgebers (Light, social contacts)
Behv/ Social/ Environmental
New home/ Downsizing/ Retirement community/ Institutionalization
Bereavement
Retirement- no need for reg sleep and wake times
Sleep disorders- OSA, RLS, Insomnia
Medical Illness- Pain, GERD, Nocturia, Heart failure
Medications- Diuretics, Beta-blockers, OTC meds, etc
Mood disorders
86
Nocturia and Disturbed Sleep in Older Adults
CareGiving
Family problems
Money Problems
Health Concerns
Headache
Heart Burn
Uncomfortable bed
Prevalence (%) of Self-Reported Causes of Disturbed Sleep
0 10 20 30 40 50 60
Physical Pain Nocturia Few nights/ month Few weeks/ night Every night
Bliwise et al. Sleep med vol. 10,5 (2009): 540-8. 87
Drug Induced effects on Sleep/ Wakefulness
• Prescription Drugs
Recreational Drugs • Alcohol
Caffeine
•
•
88
Pathophysiology
• Disruption of Neurotransmitters/ receptors
• Pre-existing sleep disorder
• Ability of meds to cross BBB
• Degree of Lipophilicity
• Any med crossing BBB can potentially alter sleep architecture
89
Neurotransmitters for Wakefulness/ Sleep







Sleep Ach Histamine NE HT Dopamine Glutamate GABA Wake Adenosine 90
Neurotransmitters for sleep/ wakefulness
GABA-a
• Major inhibitor. Target of many meds (BZD, non-BZD Agonists)
• Potentiation or inhibition can promote sleep or alertness
Acetylcholine (Ach)
• Wakefulness and REM sleep
• “Anticholinergics" – block/ inhibit activity of Ach (Atropine, Oxybutynin, Scopolamine, TCA’s)
91
Neurotransmitters for Sleep/ Wakefulness
Adenosine
• Breakdown product of ATP
• Adenosine A-1 and A-2a receptors
• antagonized by caffeine/ theophylline
Opioids
• Disrupt REM sleep by ↑ Ach and Adenosine
92
Neurotransmitters for sleep/ wakefulness
Serotonin
• 5HT-1 a, 5HT-1b, 5HT-2a/2c, 5HT 3 agonist- Wake (Think SSRI/SNRI)
• Trazadone - 5HT-2a Antagonist
• Mirtazapine - 5HT-3 Antagonist
NE
• Locus Coeruleus- Wake, inhibits REM sleep
• Clonidine and Precedex - A2 Agonists and ↓ NE
• Mirtazapine- A2 blocker- ↑NE
93
Neurotransmitters for sleep/ wakefulness
• Histamine
• H1, H2 and H3 – wake
• Diphenhydramine, Doxepin- Histamine blockers
• Dopamine
• D1-D5 promotes wake
• Parkinson's meds- Dopamine agonists; Wellbutrin –Dopamine reuptake inhibitor
• Glutamate
• Activates AMPA, NMDA receptors
• Ketamine antagonizes Glutamate
94
Altered Pharmaco-kinetics in the Elderly
• Absorption
• ↓ gastric emptying
• ↓ gastric CYP450
• Distribution
• ↓ albumin
• ↓ lean body mass and ↑ fat wt
• Metabolism
• ↓ hep blood flow and biotransformation
• Elimination
• ↓ renal and hepatic clearance
95
Drug Induced Sleep disorders
96
Drug Induced Drowsiness
• Benzodiazepines
• Opioids
• Psych meds
• Antidepressants (TCA’s) and antipsychotics
• Antihistamines
• OTC
• Antiepileptics
• Phenytoin, Valproic acid (Depakote)
97
Drug induced Insomnia
• Bronchodilators
• Antiarrhythmics
• Amiodarone
• Steroids
• Antidepressants
• SSR/SNRI
• Parkinson’s meds
• Anti-epileptics
• Lamotrigine
• CNS stimulants
• Nicotine
• Drug w/d
• Alcohol, BZD, Opioids
• Theophylline
98
Drug-induced/ Worsening Sleep apnea
• Alcohol , BZD, Opioids
• Baclofen
• Meds that can increase weight gain
• Neuroleptics
• Insulin, SU
• SSRI, Mirtazapine, TCA’s
• Steroids
• Hormonal Contraceptives
99
Drug induced/ Worsening RLS
• Alcohol, Caffeine, Nicotine
• Donepezil
• B2 receptor Agonists
• Salmeterol
• Salbutamol
• Terbutaline
• Levalbuterol
• SSRI’s
• Sertraline, Fluoxetine
100
Drug induced Vivid Dreams or Nightmares
• CV meds-
• Digoxin
• Beta blockers- propranolol- BBB
• Dementia meds
• Donepezil, memantine
• Parkinson’s meds
• Levodopa, Amantadine
• Steroids
• Infections meds
• Voriconazole, FluoroQ , Efavirenez (Anti-HIV)
• Antipsychotics
• Antidepressants
• SSRI’s and SNRI’s
• Opioids
• Ketamine
101
Drug induced Enuresis
• Diuretics
Valproic acid • Antipsychotics
• 2nd gen Antipsychotics- Risperidone and Clozapine
•
102
Substance use
Alcohol-
• ↓ SOL
• ↑ arousal, causing poor quality sleep and ↓ duration.
• Worsen SDB by ↓ pharyngeal muscle tone.
Caffeine-
• Stimulating effects ↑ SOL and arousals
• short sleep
Tobacco-
• Nicotine promote wakefulness via Ach transmission in CNS
103
Polypharmacy In Dementia in Older Adults
% Days of use
0 10 20 30 40 50 60 70 80 90 100
drugs Benzodiazapine Anti- Psychotic Anti-Depressant Anti-Epileptics Opioid
Z-
Maust et al. JAMA. 2021;325(10):952–961104
Polypharmacy In Dementia in Older Adults
Tramadol
Hydrocodone
Oxycodone
Gabapentin
Olanzapine
Risperidone
Quetiapine
Trazodone
Mirtazapine
Escitalopram
Sertraline
Venlafaxine
Duloxetine
Alprazolam
Clonazepam
Lorazepam
Z- drugs
% Days of use
0 5 10 15 20 25 30 35
Maust et al. JAMA. 2021;325(10):952–961
105
Pharmacotherapy for Insomnia
• Check medical history and their medications (prone to polypharmacy)
• Check for Wake-promoting agents
• Check for co-morbidities causing Insomnia
- GAD, MDD, PTSD, Heart disease, Dementia, or underlying SDB
• Check adverse effects and possible drug interactions with hypnotics
106
Pharmacotherapy for Insomnia
• CBTi- is still the first line Rx of insomnia
• Initially Combination Rx with a hypnotics + CBTi
• Hypnotics should be tapered within 8 weeks, ideally.
107
108
Drug Dose in elderly Onset of action Duration of action t ½ in elderly (hrs.) Benzodiazepines (BZD) Triazolam (Halcion) 0.125 mg 15-30 min short 1.5-5.5 Temazepam (Restoril) 7.5 mg 45-60 min intermediate 3.5-18.4 Flurazepam (Dalmane) 7.5 mg 30-60 min long 120-160 Quazepam (Doral) 7.5 mg 20-45 min long 39-73 109
Drug Dose in elderly Onset of action Duration of action t ½ in elderly (hrs.) Non-BZD Receptor Agonists Zolpidem SL (Intermezzo) 1.75 mg 20 min very-short 1.4-3.6 Zaleplon (Sonata) 5 mg 15-30 min very-short 1.0 Zolpidem (Ambien) 5 mg < 30 min short 2.9-3.7 Zolpidem CR (Ambien CR) 6.25 mg <30 min intermediate 1.9-7.3 Eszopiclone (Lunesta) 1-2 mg 15- 30 min intermediate 9 110
Drug Dose in elderly Onset of action Duration of action t ½ in elderly (hrs.) Melatonin receptor agonists Ramelteon (Rozerem) 8 mg 15-30 min short 1.0-2.6 H1 antagonists (antihistamines) Doxepin (Silenor) 3 mg 30 min long 15.3-31 Orexin receptor antagonist Suvorexant (Belsomra) 10-20 mg 30 min intermediate 12 111
Benzodiazepines (BZD)
• Have active binding sites within the GABAA receptor
• α and γ subunits (ie, “benzodiazepine site”)
• promote sleep, mitigate anxiety, and act as an anticonvulsant
• AASM recommends the usage of short-acting agents
• Temazepam and
• Triazolam
• Adverse effects - dizziness, lethargy, dry mouth, HA, ↑risk of falls w/ fractures, MVA, and memory impairment.
• Higher adverse effects of BZD’s due to altered PK and PD with aging.
• Risk of dependence, abuse and developing tolerance.
112
Benzodiazepines (BZD)
Temazepam
• is less lipophilic and has a slower onset of action (1 hour)
• T ½ of 9 - 12 hrs
Triazolam
• Rapid onset 15-30 min and short T ½ 1.5-5 hrs,
• Rebound insomnia, anterograde amnesia
Flurazepam and Quazepam
• Very long t ½ due to active metabolites,
• Avoid in older adults.
113
Nonbenzodiazepine BZD Receptor Agonists (Z-drugs)
• Most prescribed class
• Target Selective subunits of GABAA receptors
• Mtb by CYP3A4 in Liver- caution in liver failure
• Adverse effects –
• HA, dizziness, nausea, and myalgias.
• Increase risk for fractures, falls, and injuries,
• Parasomnias-
• Sleep-related eating disorder, sleep driving, and Somnambulism
• Next day Psychomotor and Cognitive impairment
114
Nonbenzodiazepine BZD Receptor Agonists (Z-drugs)
Zolpidem
• α1 and α5 subunits on GABAA receptors
• Onset of action- ~ 30 minutes
Oral (Ambien)
• T ½ of 2.9-3.7 hrs (IR)
• T ½ of 1.9-7.3 hrs (ER)
Sublingual (Edular, Sublinox, and Intermezzo)
• T ½ of 1.4-3.6 hrs
Nasal (Zolpimist)
• T ½ of 0.9 hrs
115
Nonbenzodiazepine BZD Receptor Agonists (Z-drugs)
Eszopiclone (Lunesta)
• α1-3, and 5 subunits on GABAA receptors
• T½ of 9 hrs; Peak levels in 1 hour
Zaleplon (Sonata)
• α1-3, β2, and γ2 subunits on GABAA receptors
• T ½ of 1 hr with a rapid onset of action
• Short T1/2 - Typically no Next-day effects
116
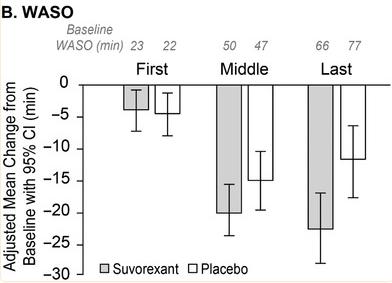
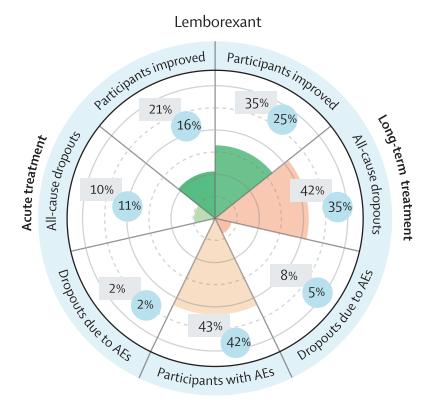
Dual Orexin receptor Antagonist (DORA)
Indication- Sleep onset and/or Maintenance
Contraindications- Narcolepsy
MC Adverse Effect- Somnolence, HA, Fatigue
Schedule IV medication
• Suvorexant (2014)
• Lemborexant (2019)
• Daridorexant (2022)
• Seltorexant (Investigational)-
Single Orexin Receptor Antagonist (2-SORA)
117
Dual Orexin receptor Antagonist (DORA)
Geriatric considerations: Equal efficacy in older and younger patients.
Somnolence may increase fall risk
- Suvorexant- No dose change
- Lemborexant- Caution at doses >5 mg
-
Daridorexant- No dose change
118
Suvorexant in Alz Dementia- PSG-Based RCT


Herring et al. Alz Ass vol. 16,3 (2020): 541-551.
119
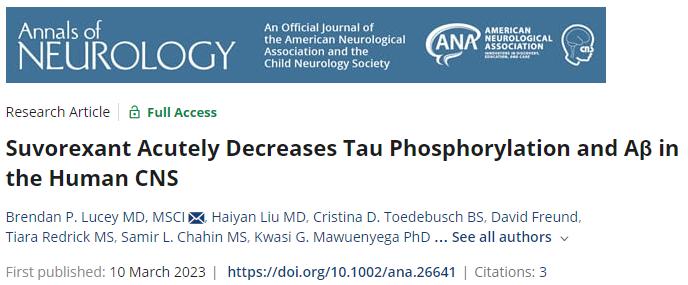
120
Anti-Histamines
Doxepin
• TCA with sedative effects
• High dose- Anti-depressive effects via 5HT and NE
• Low dose- Drowsiness/ Sleep via selective H1
• T ½ is 6 - 8 hrs ; Metb in liver
• Start @ 3 mg and max of 6 mg for Insomnia
• Low doses doxepin
• Is tolerable
• Lacks serious AE
121
Melatonin and Melatonin receptor agonists
• Melatonin binds to two melatonin receptors.
• MT1 receptors -> initiate and maintain sleep, and
• MT2 receptors -> regulate the circadian rhythm
• Melatonin can be given directly or as an MT1 and MT2 receptor agonist.
122
Melatonin
• Not FDA regulated
• Regarded as a dietary supplement, OTC,
• Stated dosages on products may not reflect actual dosages
• Melatonin
• ↓SOL, but
• REM latency, TST, and WASO do not improve.
• T1/2 ~1 hour, and the peak conc ~ 60 min
• In Europe, it has been regulated
• IR tablets - 0.3 to 0.5 mg and
• ER tabs- 2 mg
123
Ramelteon
• MT1 and MT2 receptor agonist
• T1/2 - 1- 2.5 hrs; Rapid onset of action.
• ↓ subjective SOL and ↑ TST
• Insomnia dose- 8 mg qhs
• Not studied in elderly patients
• Has little effect on respiratory function, safe in COPD
124
Do not RECOMMEND
• Trazodone (B<H)
• Diphenhydramine (B=H)
• Melatonin (B=H)
• L-tryptophan (B<H)
• Valerian (B=H)
B- Benefit, H-Harm
125
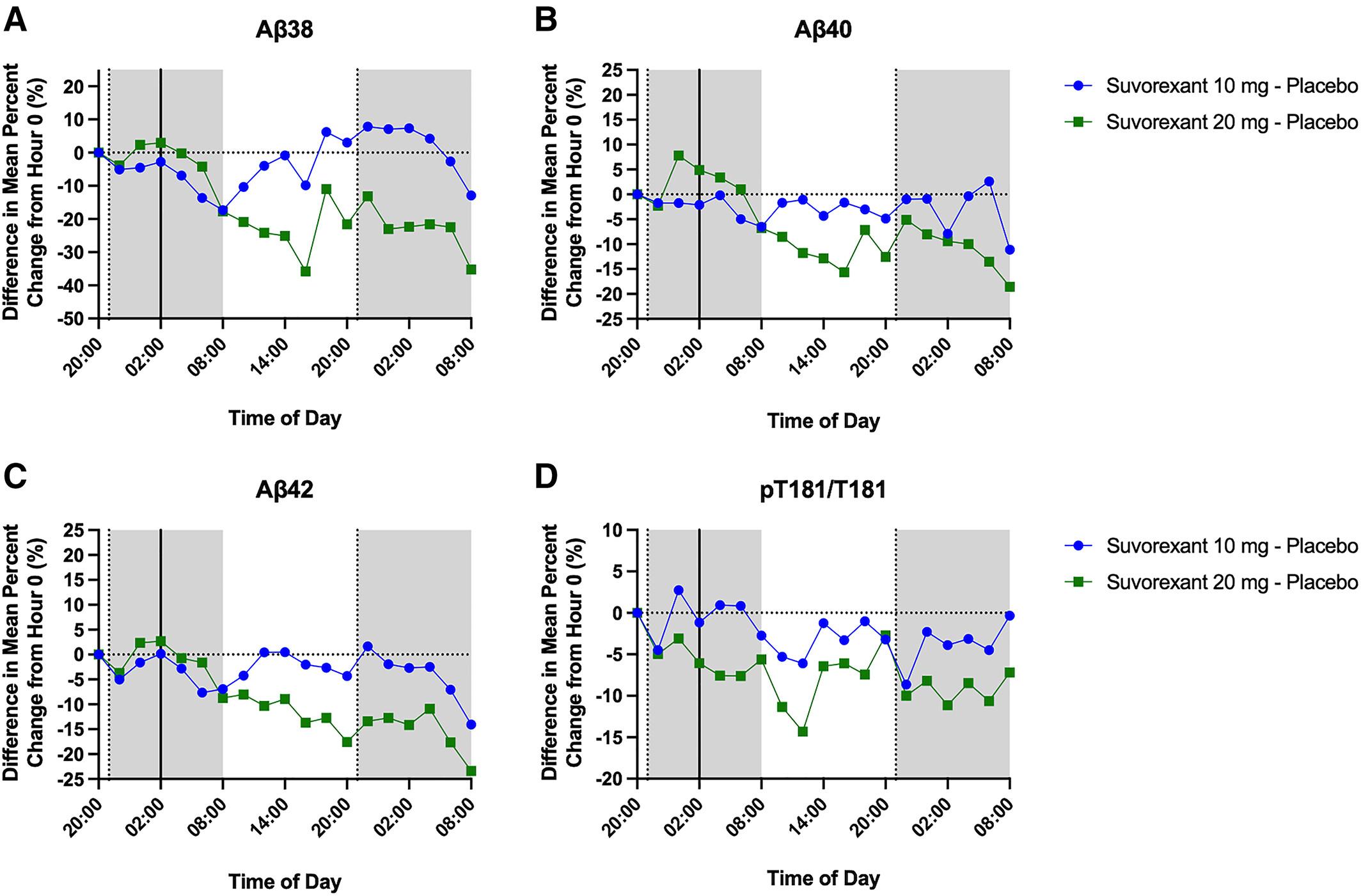
Sleep onset Sleep maintenance
Drugs Zolpidem
Zaleplon
Ramelteon
Triazolam
Sleep onset and sleep maintenance
Doxepin 1
Zolpidem SL 2
Zaleplon 2
Suvorexant
Lemborexant
Daridorexant
Eszopiclone
Temazepam
Zolpidem CR
Suvorexant
Lemborexant
Daridorexant
1 For difficulties in the last 2 hours of the night, Doxepin 3 to 6 mg.
2 Dosed in middle-of-the-night, if >4 hours of sleep time remaining before wakening.
126
CBT-insomnia is still best option
• Cognitive therapy may be limited
• Enhance circadian cues (light/dark and physical activity)
• Quiet, comfortable place to sleep
• Avoid medications that could be contributing to insomnia
• Trials using CBI-i in the elderly and with MCI have shown that this is an effective and safe treatment
(Cassidy-Eagle, et al. Clin Gerontol, 2018)
127
128
129
Thank You!
130
Best Practices for the Management of Chronic Insomnia Disorder

 J. Todd Arnedt, Ph.D. Professor of Psychiatry and Neurology Director, Behavioral Sleep Medicine Program
J. Todd Arnedt, Ph.D. Professor of Psychiatry and Neurology Director, Behavioral Sleep Medicine Program
Co-Director, Sleep and Circadian Research Laboratory Michigan Medicine, University of Michigan, Ann Arbor, MI
131
X
Conflict of Interest Disclosures for
Speakers
1. I do not have any relationships with any entities producing, marketing, re-selling, or distributing health care goods or services consumed by, or used on, patients, OR
2. I have the following relationships with entities producing, marketing, re-selling, or distributing health care goods or services consumed by, or used on, patients.
Type of Potential Conflict
Details of Potential Conflict
Grant/Research Support
Apple, Inc
Consultant Eisai Inc., Idorsia Pharmaceuticals Ltd, Purdue Pharma L.P.
Speakers’ Bureaus
Financial support
Other
3. The material presented in this lecture has no relationship with any of these potential conflicts, OR
X 4. This talk presents material that is related to one or more of these potential conflicts, and the following objective references are provided as support for this lecture:
1.
Mignot E. Lancet Neurol 2022;21:125-39.
2.
Kunz D. CNS Drugs. 2023;37(1):93-106.
3.
132
Discuss the scope and significance of chronic insomnia disorder 1 Integrate best practices for insomnia assessment in adults 2 Appraise benefits and risks of primary treatment options for insomnia in adults 3 133
Learning Objectives

134
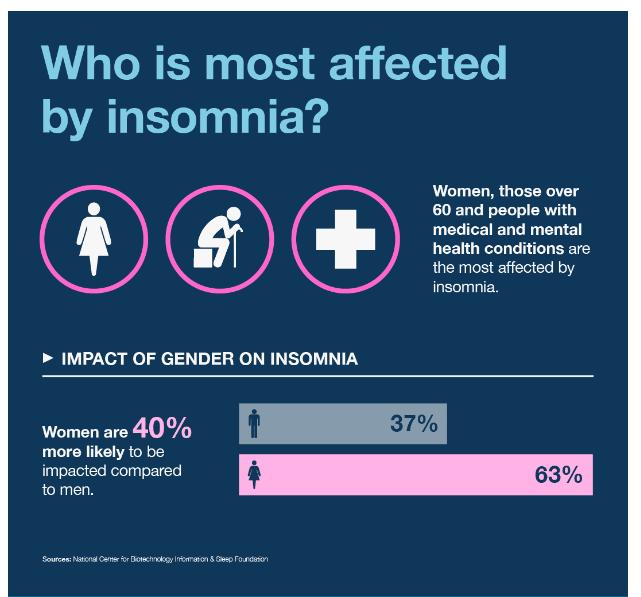
https://www.healthline.com/health/insomnia/infographic-facts-stats-on-insomnia

- Prevalence
135
https://www.thegoodbody.com/insomnia-statistics/
Untreated insomnia adversely impacts health and well-being
• Adversely affects QOL and work performance1,2
• Increases risk for mental health disorders (e.g., depression)3 and medical conditions (e.g., HTN)4
• Increases fall risk among older adults5
• Is associated with elevated healthcare costs6
• Becomes chronic problem if left untreated7
1Katz and McHorney. J Fam Practice 2002; 51(3): 229-235; 2Léger D. Sleep 2006;29(2):171-8; 3Breslau N. Biol Psychiatry. 1996;39:411-8; 4Vgontzas AN. Sleep 2009;32(4):491-7; 5Avidan AY. J Am Geriatr Soc 2005;53:955-6; 6Stoller MK. Clin Therapeutics 1994;16:873-97; 7Katz DA. Arch Int Med 1998;158(10):1099-107 136
Keys to optimizing insomnia management
Assess nature of the complaint
Initiate evidence-based treatment
Consider need for additional assessments (PSG, blood work)
Regular and consistent patient follow-up
Characterize insomnia complaint further
137
Assessment Tools: Insomnia Severity Index

• 7-item instrument assessing nature, severity, and impact of insomnia
• 0-7 (None); 8-14 (Mild); 15-21 (Moderate); 22-28 (Severe)

• Scores ≥11 suggestive of insomnia disorder diagnosis
• Validated criteria for treatment response (>7 point reduction) and remission (final score ≤7)
Morin CM. 138
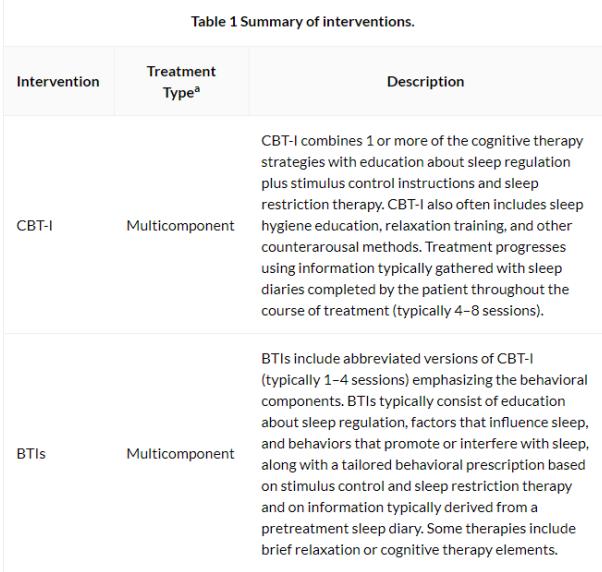
Assessment Tools: Daily Sleep Diary/Sleep
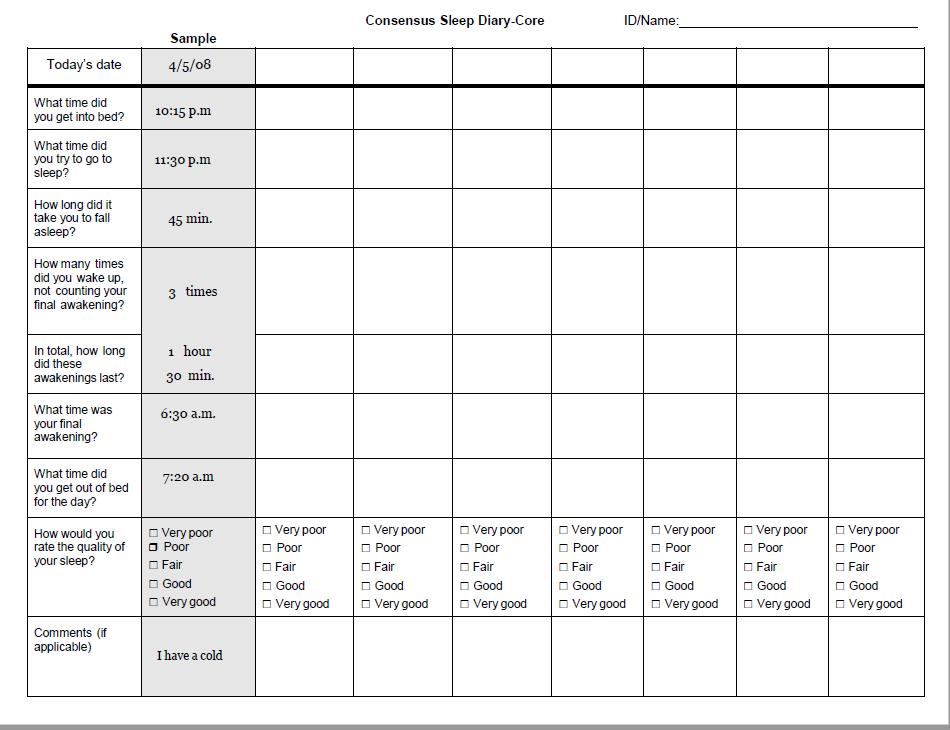
Log 139
Use of PSG in the Assessment of Chronic Insomnia
PSG and daytime MSLT are not indicated in the routine evaluation of insomnia, including insomnia due to psychiatric or neuropsychiatric disorders [Standard]
PSG is indicated when there is reasonable clinical suspicion of breathing (OSA) or movement disorders, when initial diagnosis is uncertain, treatment fails (behavioral or pharmacologic), or precipitous arousals occur with violent or injurious behavior [Guideline]
•
•
Schutte-Rodin et al. J Clin Sleep Med 2008;4(5): 487-504 140
Insomnia: Treatments


141
Insomnia Treatment Options
• Prescription Medications
• BZDs: temazepam (Restoril)*, triazolam (Halcion)*, clonazepam
• BZRAs: zolpidem (Ambien/Edluar/Intermezzo/Zolpimist)*, zolpidem-ER (Ambien-CR)*, zaleplon (Sonata)*, eszopiclone (Lunesta)*
• Melatonin receptor agonists (MelRAs): ramelteon (Rozerem)*, tasimelteon (Hetlioz)*
• Orexin antagonists: suvorexant (Belsomra)*, lemborexant (Dayvigo)*, daridorexant (Quviviq)*
• Antidepressants: trazodone, doxepin (Silenor)*, amitriptyline, mirtazepine
• Others: e.g., antipsychotics, anticonvulsants
• Non-prescription OTC agents
• Antihistamines (diphenhydramine/doxylamine), herbal remedies (valerian/chamomile/melatonin), alcohol, cannabis
• Non-pharmacological treatments
• Cognitive-behavioral therapy (CBT), CAM Treatments (e.g., Mind-body practices/Acupuncture) *FDA-Approved
142
Weighing Insomnia Treatment Options
Medications
Advantages
Work quickly
Disadvantages
Side effects
Well tolerated Tolerance
CBT for Insomnia
Advantages
Efficacious
Disadvantages
Delayed gains
Maintenance of benefits
Greater patient burden
Efficacious
Drug interactions
Fewer side effects Close follow-up needed
Minimal patient burden
Safety concerns in certain populations
Increased patient selfefficacy Less availability
143

144
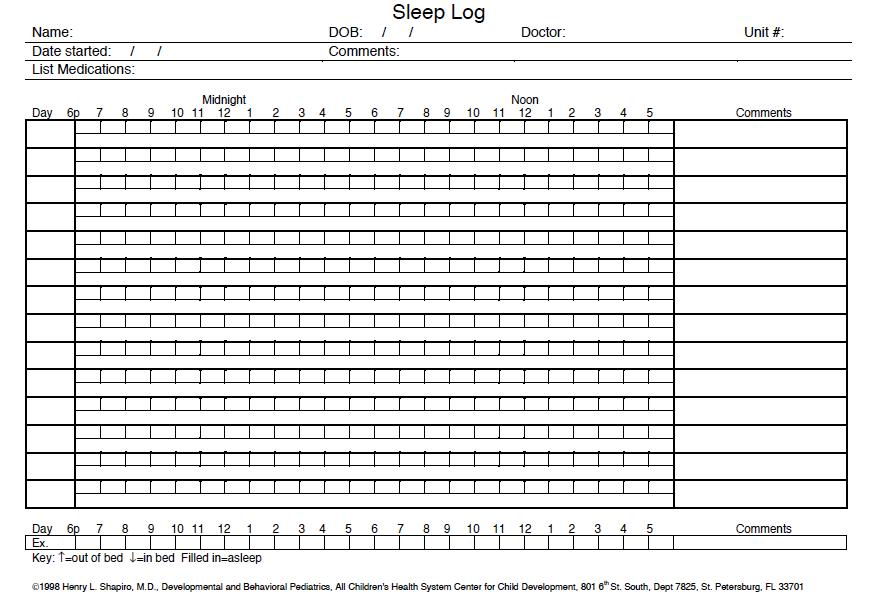
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a brief, multicomponent non-medication treatment
BEHAVIORAL Sleep Restriction
Stimulus Control
Counter-Arousal Strategies
COGNITIVE Beliefs/Attitudes
EDUCATIONAL Sleep Hygiene
TREATMENT TARGETS
Excessive time in bed
Irregular sleep schedules
Sleep incompatible activities
Hyperarousal
TREATMENT TARGETS
Unrealistic sleep expectations
Misconceptions about sleep
Sleep anticipatory anxiety
Poor cognitive coping skills
TREATMENT TARGETS
Inadequate sleep hygiene
Adapted from Morin CM. 145
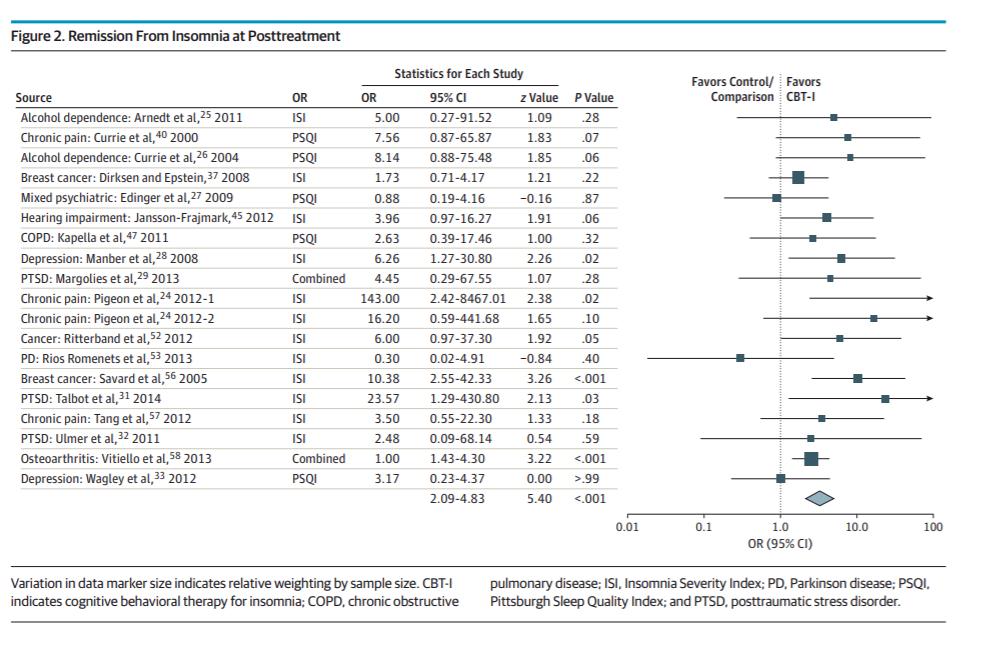
CBT-I is beneficial and safe for chronic insomnia with and without comorbid health conditions No other health conditions1 With other health conditions2 1Trauer JM. Ann Intern Med 2015;163:191-204 2Wu JQ. JAMA Intern Med 2015; 175(9):1461-72 Pooled OR = 3.28 (95% CI 2.30 – 4.68, p<.001) 146
In head-to head comparisons, CBT-I does better than
46 older adults (mean age 60.8 years) with chronic insomnia randomized to 6 weeks of CBT-I, zopiclone, or placebo
0 50 100 150 200 Placebo CBT-I Zopiclone 7.5 mg Pre-tx Post-tx (6 wks) 6 mos f/u * * Total Wake Time (min) *p<.001
medication
Sivertsen B. JAMA 2006;295:2851-8.
at post-treatment and follow-up.
* 147
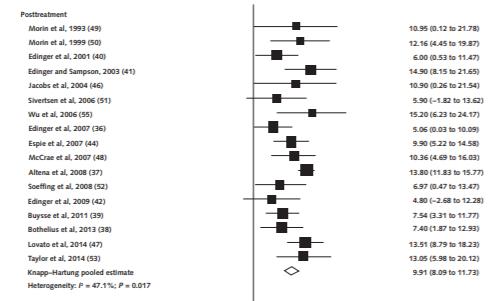
Benefits of CBT-I are sustained up to 2 years post-treatment
Morin CM. JAMA 1999;281:991-9.
-40 -30 -20 -10 0 10 20 30 % Change from Pretreatment CBT-I Medication Wake during the night Sleep efficiency Total sleep time 24 Month Follow-Up 148
Self-help CBT is Effective Multiple self-help formats for CBT-I have been developed to extend its reach



149
Effect sizes for different CBT-I formats range from moderate to
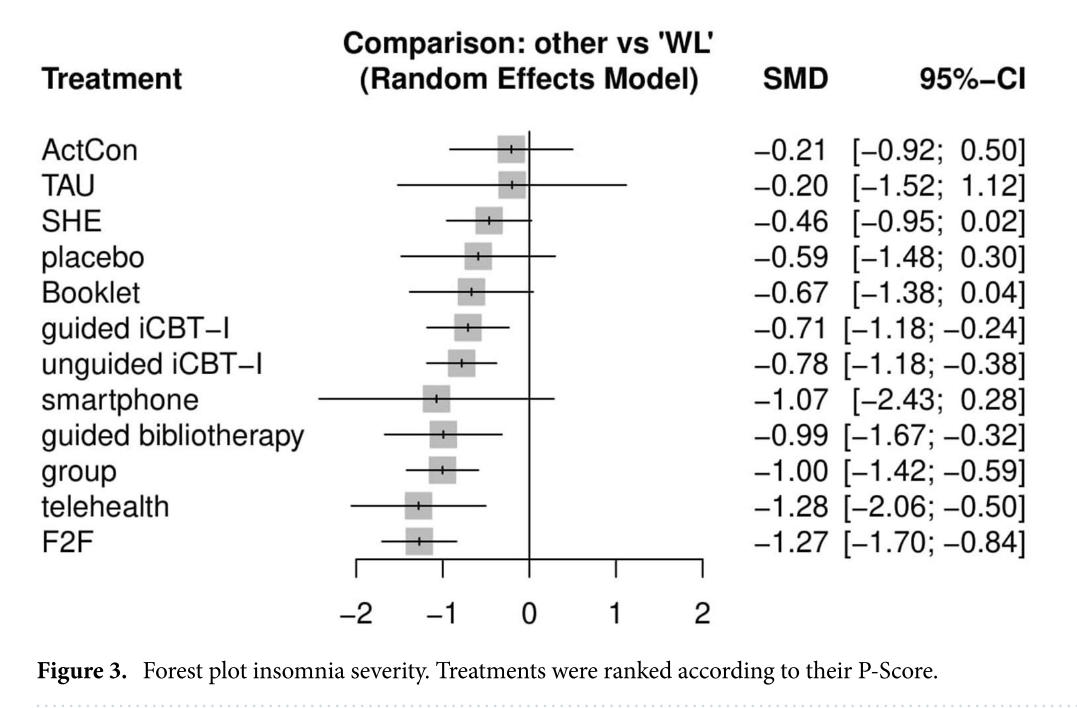
n=52 studies, representing 12,544 participants with insomnia disorder

Simon L. Sci Rep. 2023;13(1):1929.
large, consistent with gold-standard face-to-face
150
Brief Behavioral Treatment for Insomnia (BBT-I) improves remission/response rates and is less time intensive than CBT-I
Buysse DJ. Arch Intern Med 2011;171(10):887-895.
X2=16.9, p<.001 0 10 20 30 40 50 60 70 Remission Response Partial Response No Response BBTI IC % Participants X2=16.9, p<.001
older adults with chronic insomnia 151
n=79


Mindfulness-based interventions de Entrambasaguas M. Clin Psychol Psychother. 2023. 0 4 8 12 16 20 24 28 CBT-I (n=17) ACT (n=18) Pre-tx Post-tx 6-mo F/U ISI Score Acceptance and Commitment Therapy (ACT) El Rafihi-Ferreira R. Behav Sleep Med. 2023;21(2):193-207. Emerging nonpharmacological therapies for chronic insomnia target hyperarousal and acceptance 152
Zolpidem
Eszopiclone
Zaleplon
Triazolam
Temazepam
Ramelteon
Doxepin
Suvorexant
Recommended Medications
Sleep Onset Sleep Maintenance
Medications Not Recommended
Trazodone
Tiagabine
Diphenhydramine

Melatonin
Tryptophan
Valerian
MJ. J Clin Sleep Med 2017;13(2):307-349.
Sateia
153
1N=22 studies, tx length=35 days; 2N=7 studies, tx length=14 days
*small: 0.2 to 0.5, medium: 0.5 to 0.8, large: >0.8
Sleep Parameter Nowell et al. (1997)1 Smith et al. (2002)2 Sleep Latency 0.56* 0.45 Wake after Sleep Onset - 0.89 Number of Awakenings 0.65 0.97 Total Sleep Time 0.71 0.84 Sleep Quality 0.62 1.20 1Nowell PD et al. JAMA
2Smith MT et al., Am J Psychiatry 2002;159:5-11.
BZD/BzRA hypnotics are efficacious in the short-term
1997;278:2170-7.
154
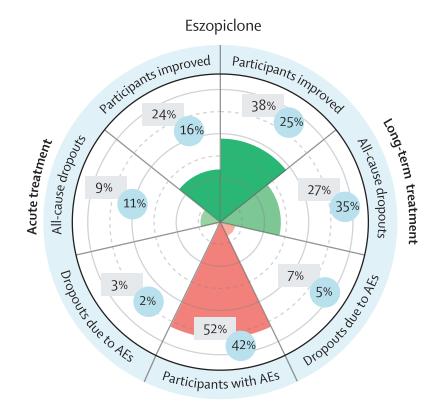
Lunesta® (eszopiclone) shows sustained efficacy relative to placebo over 6 months of nightly use





n=788 adults with chronic insomnia

0 20 40 60 80 100 Baseline Month 1 Month 2 Month 3 Month 4 Month 5 Month 6 Pbo SL Esz 3 mg SL Pbo WASO Esz 3 mg WASO Minutes awake
Pbo
SL
WASO at all
*p<.001 Esz vs.
for
and
assessments
Krystal AD. Sleep. 2003;26:793-9.
155
Eszopiclone
accelerates remission to depression among people with comorbid depression and insomnia
n=545 adults with depression and insomnia
18.6 32.8 22.3 42 0 15 30 45 60 Week 4
FLX + PBO FLX + ESZ % patients achieving remission P=0.3 P=0.03 Fava M. Biol Psychiatry 2006;59:1052-60.
Week 8
156
BzRAs have moderately high abuse liability for people with substance use disorders

• Abuse liability assessed as:
• Likelihood of abuse
• Consequences of abuse (toxicity)
• All BzRAs = class IV controlled substances
• MelRAs = non-scheduled

Griffiths RR & Johnson MW. J Clin Psychiatry 2005;66(Suppl 9):31-41. 157
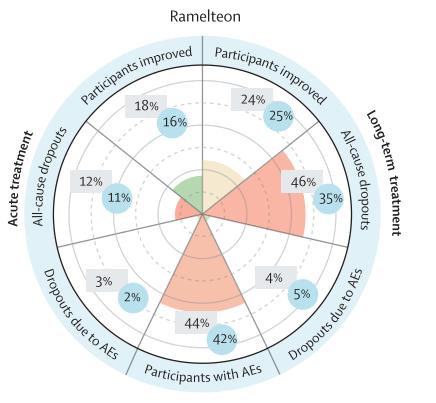
Rozerem® (ramelteon), a selective MT1/MT2 receptor agonist, improves sleep initiation but not sleep maintenance
No differences pbo vs. ramelteon at week 5 for total sleep time, sleep efficiency, or time awake during the night
*p<.01, **p<.001 vs. placebo for latency to persistent sleep
Baseline Week 1 Week 5
n=400 adults with chronic insomnia
0 10 20 30 40 50 60 70
Minutes Placebo Ramelteon 8 mg Ramelteon 16 mg ** * Zammit G. J Clin Sleep Med
2007;3:495-504.
158
Silenor® (doxepin) improves sleep maintenance putatively through histaminergic (H1) antagonism
50 70 90 110 130 150 Baseline Night 1 Night 29 Night 85 PSG Minutes WASO Placebo Doxepin 1 mg Doxepin 3 mg Krystal A. Sleep 2010;33(11):1553-61. *p<.05 vs. pbo **p<.01 vs. pbo **p<.0001 vs. pbo * ** *** * *** *** 43.7 47.2 47.6 203.1 220.2 223.2 39.6 28.9 35.7 57.3 64.2 67.2 0 50 100 150 200 250 300 350 400 Placebo DXP 1 mg DXP 3 mg Minutes (mean) Sleep Stage Effects at Night 85 Stage 1 Stage 2 Stage 3/4 Stage REM n=240 older adults *** * * * 159
Quviviq™ (daridorexant), an OR-1 and OR-2 antagonist, improved sleep onset and maintenance across 3 months; effects on self-reported total sleep time sustained across 40 additional weeks

n=930 adults with moderate to severe chronic insomnia disorder
Mignot E. Lancet Neurol 2022;21:125-39. Kunz D. CNS Drugs. 2023;37(1):93-106.

40 50 60 70 80 90 100 110 Baseline Month 1 Month 3 PSG Minutes WASO Placebo Daridorexant 25 mg Daridorexant 50 mg * * * *
pbo
*p<.001 vs.
160


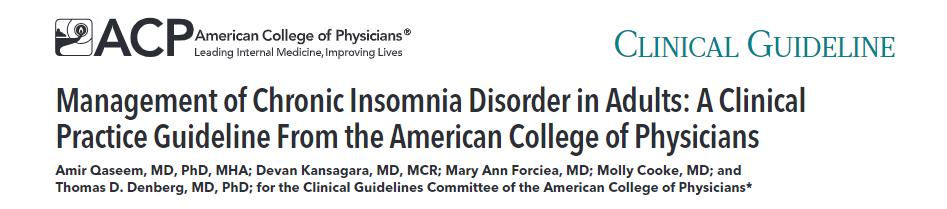
De Crescenzo F. Lancet (London, England).2022;400(10347):170-84. 161
Take Home Points
Chronic insomnia is common, persistent, and associated with significant morbidity
A comprehensive evaluation of the insomnia patient is critical for generating differential diagnoses and developing an appropriate treatment plan.
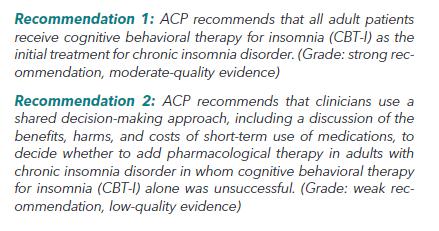
Nonpharmacological approaches to chronic insomnia are first-line. Choice of treatment should be shared between provider and patient based on evidence and other patient considerations
Insomnia research is active in insomnia mechanisms, novel pharmacological treatments, and optimization of nonpharmacological treatments.
Future research is needed on treatment effects on other health benefits, cost-benefit analyses, who responds to which treatments, and what treatment combinations optimize outcomes
162

Artificial Intelligence in Sleep Medicine: Where are we Now and Where are we Going? Cathy Goldstein, MD Professor of Neurology University of Michigan Sleep Disorders Center Cassie Blue, UM bipedal robot https://www.wired.com/story/the-punishing-polar-vortex-is-ideal-for-cassie-the-robot/ 163
Conflict of Interest Disclosures for Speakers
Medical Advisory Board, Huxley Medical
5% inventor of mobile app licensed to Arcascope, LLC

169 164
Academy of Sleep Medicine 2022
Conflict of Interest Disclosures for Speakers

DISCLOSURE
OUR LAB HAS NOT YET BEGUN USE OF AI POLYSOMNOGRAM SLEEP SCORING!
Medical Advisory Board, Huxley Medical 5% inventor of mobile app licensed to Arcascope, LLC Academy of Sleep Medicine 2022 169
165
Conflict of Interest Disclosures for Speakers





Medical Advisory Board, Huxley Medical 5% inventor of mobile app licensed to Arcascope, LLC Academy of Sleep Medicine 2022 169 DISCLOSURE
not going to talk about ChatGPT (generative AI) 166
I’m
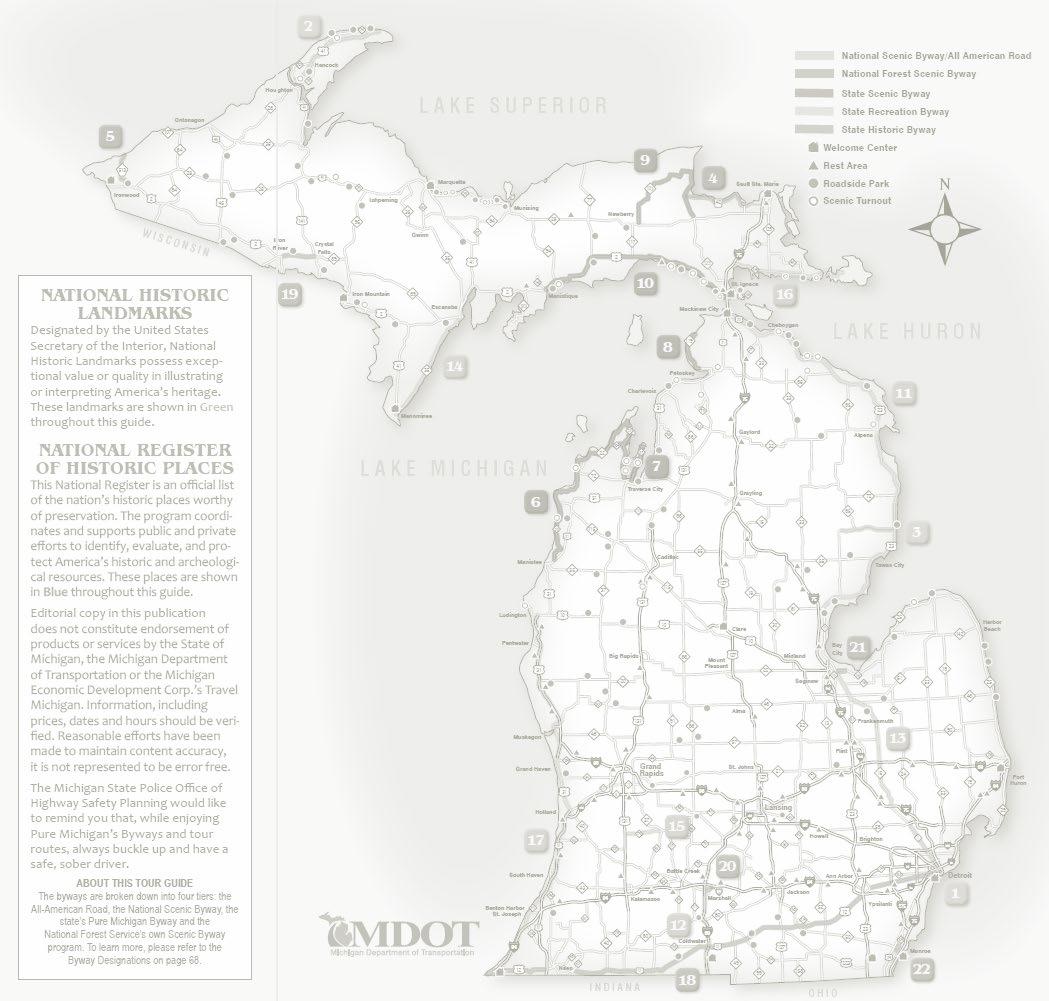
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)
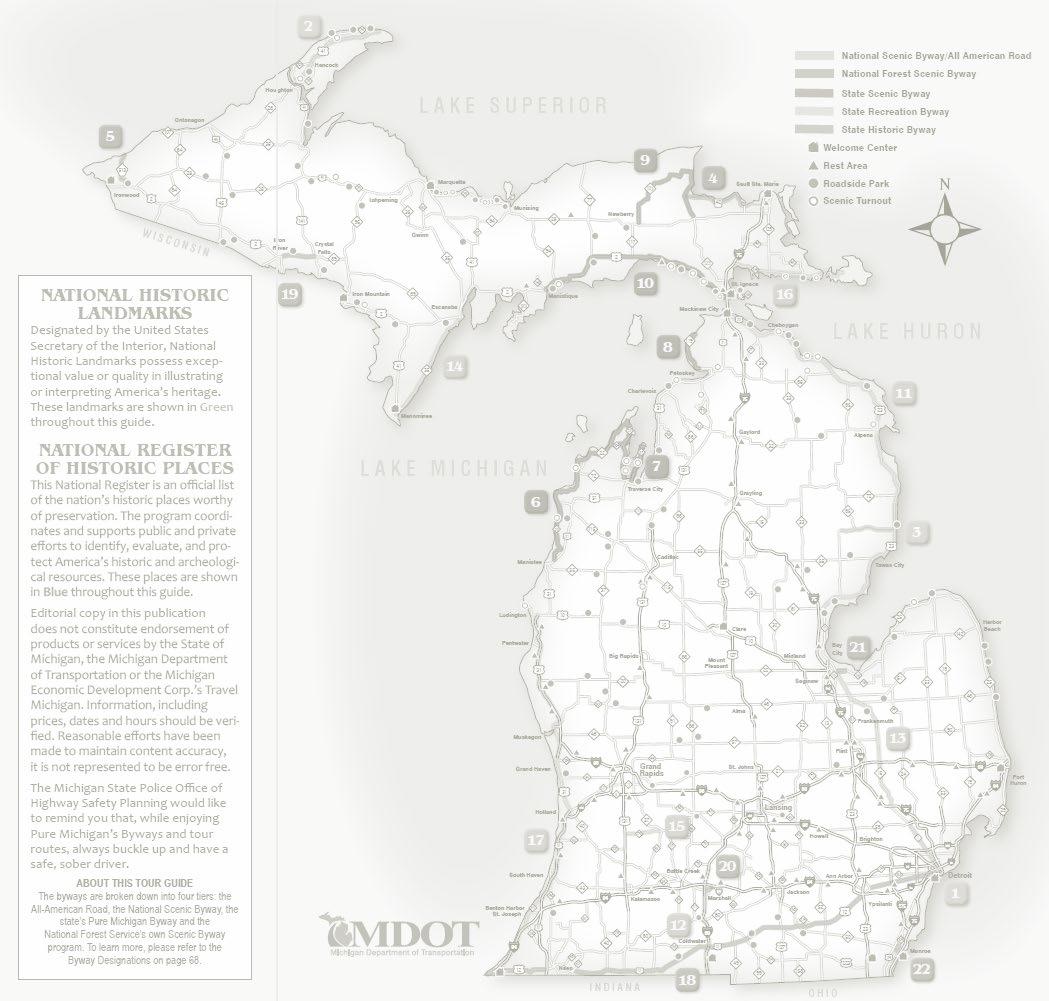

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 167
What is AI?
Machine learning (ML) and AI often used interchangeably ML subset of AI where algorithms learn from data (examples)

WITHOUT EXPLICIT PROGRAMMING
COMMANDS or RULES (however, humans can define features)
Different from statistical modeling (requires assumptions about data structure)
https://www.ibm.com/blogs/systems/ai-machine-learning-and-deep-learning-whats-the-difference/
DEEP LEARNING goes a step furtheralgorithm defined features

168
Some lingo…
TRAINING…data used to practice getting the right answer/complete a task. Iterative, automated.
TESTING and TUNING…how does the model perform when presented with new data?
Hold out data unseen during training
VALIDATION…assess model performance on new data from a NOVEL dataset to ensure generalizability

large
DATASETS
diverse (all OSA is not created equal)
appropriately annotated
Independent dataset (i.e. from another lab, institution; different acquisition methods)

SUPERVISED LEARNING-algorithm learns from labeled (ground truth) data (e.g. radiologist read chest xray)
how best to predict an output (e.g. pneumonia) from an input (chest xray image)
UNSUPERVISED LEARNING-algorithm reveals novel patterns in the data; no target (e.g. clustering-optimizes homogeneity within clusters and heterogeneity between clusters)
Bandyopadhyay A, Bae C, Cheng H, Chiang A, Deak M, Seixas A, Singh J. Smart sleep: what to consider when adopting AIenabled solutions in clinical practice of sleep medicine. Journal of Clinical Sleep Medicine. 2023 Jul 3:jcsm-10702. 169
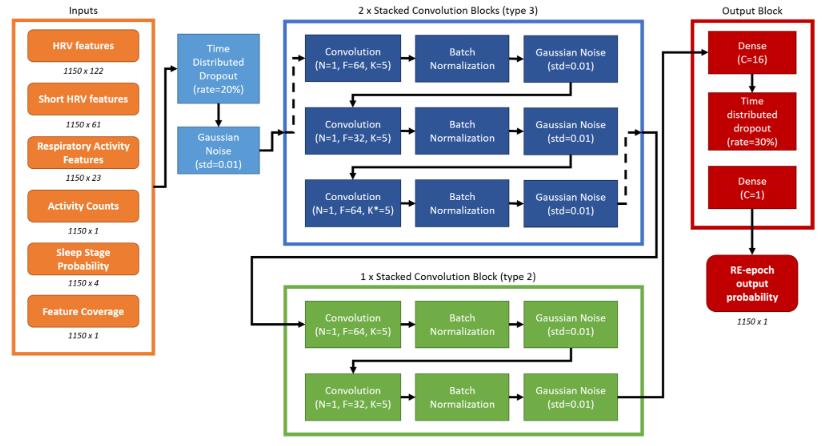
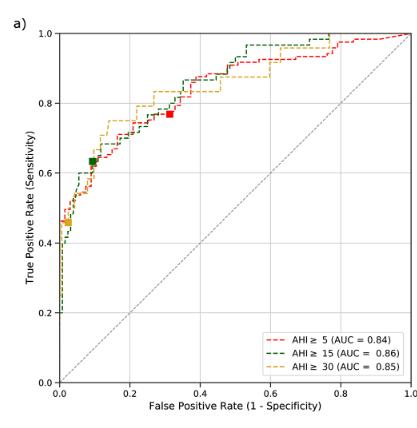
Performance assessment

accuracy, sensitivity, specificity, positive predictive value, negative predictive value, Cohen’s kappa, Bland-Altman plots and confusion matrices (NOT correlation)
RECEIVER OPERATING CHARACTERISTIC (ROC) curve
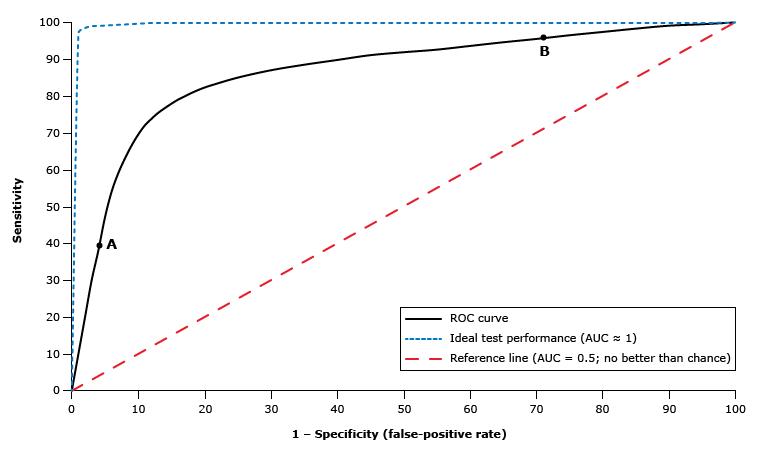
algorithm vs. gold standard y axis-true positive rate (Se) x axis-false positive rate (1-Sp)
AUC closer to 1 good, 0.5 chance
Bandyopadhyay A, Bae C, Cheng H, Chiang A, Deak M, Seixas A, Singh J. Smart sleep: what to consider when adopting AIenabled solutions in clinical practice of sleep medicine. Journal of Clinical Sleep Medicine. 2023 Jul 3:jcsm-10702.
ROC: receiver operating characteristic curve; AUC: area under the curve. From 2023 UpToDate, Inc.

170
Neural networks
Multiple connected processors (neurons) that mathematically transform input signal →output
Strength/weight of each neuron and connection iteratively adjusted (training) to ↑prediction accuracy
DEEP neural networks many layers, output of one layer provides → input to the next layer (nonlinear and hierarchical relationships)
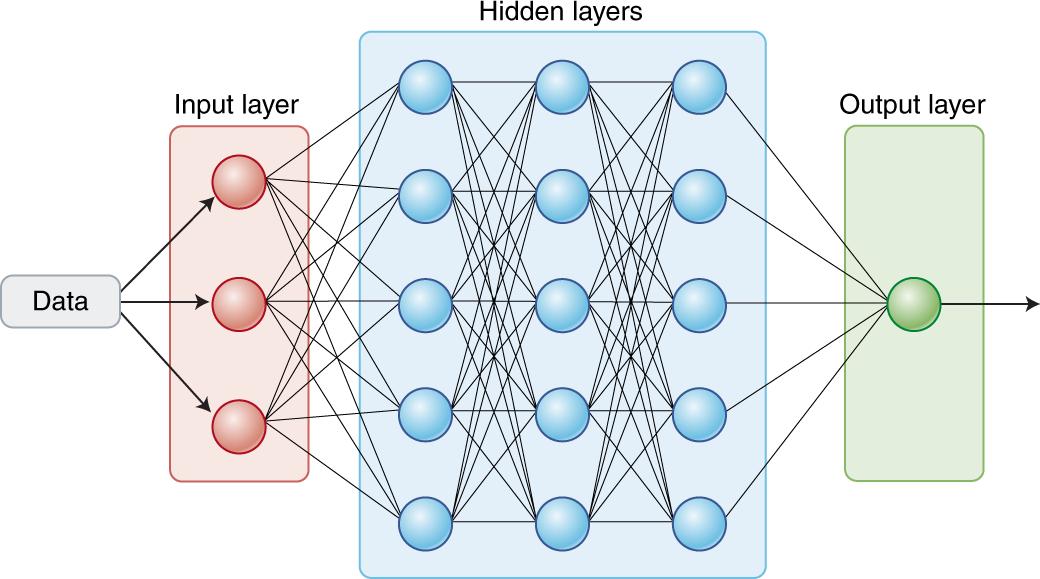
LAYER # determined by data not human

Convolutional neural networks emphasize patterns in close spatial proximity (image classification)
Recurrent neural networks information in sequence (language, next word ← immediately preceding data)
Topol EJ. Nature medicine. 2019 Jan;25(1):44-56. Zhang L, Fabbri D, Upender R, Kent D. Sleep. 2019 Nov;42(11):zsz159. 171
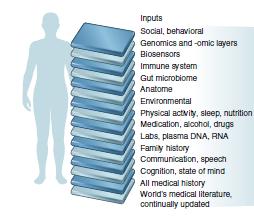
Healthcare AI, why now?
MEDICINE has complex problems
https://www.ibm.com/blogs/systems/ai-machine-learning-and-deep-learning-whats-the-difference/


Deep neural networks
↑processing power, ↑data to train
Last decade (ish)
↑↑↑computing power, storage
MASSIVE amounts of digital health data
172
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 173
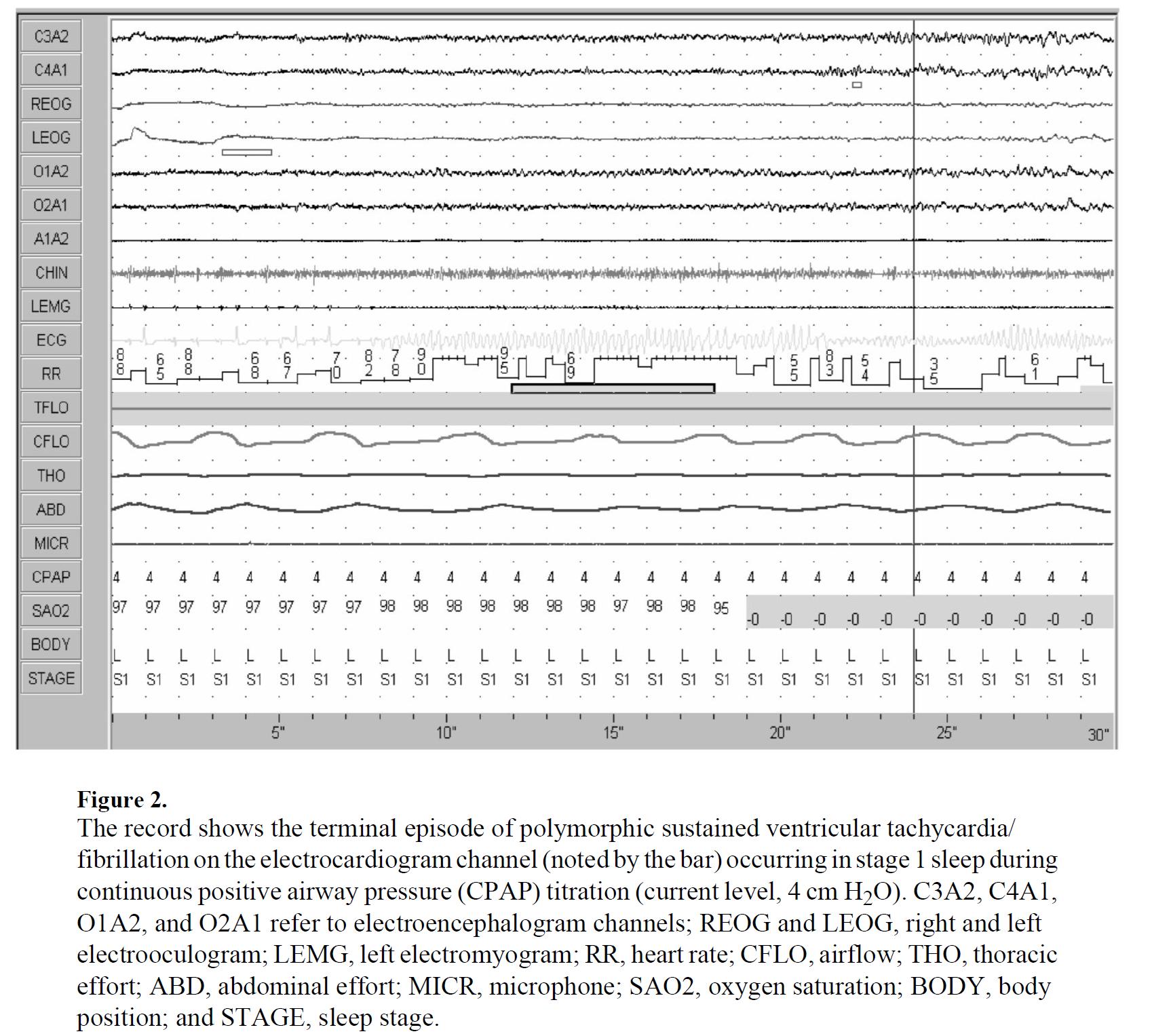
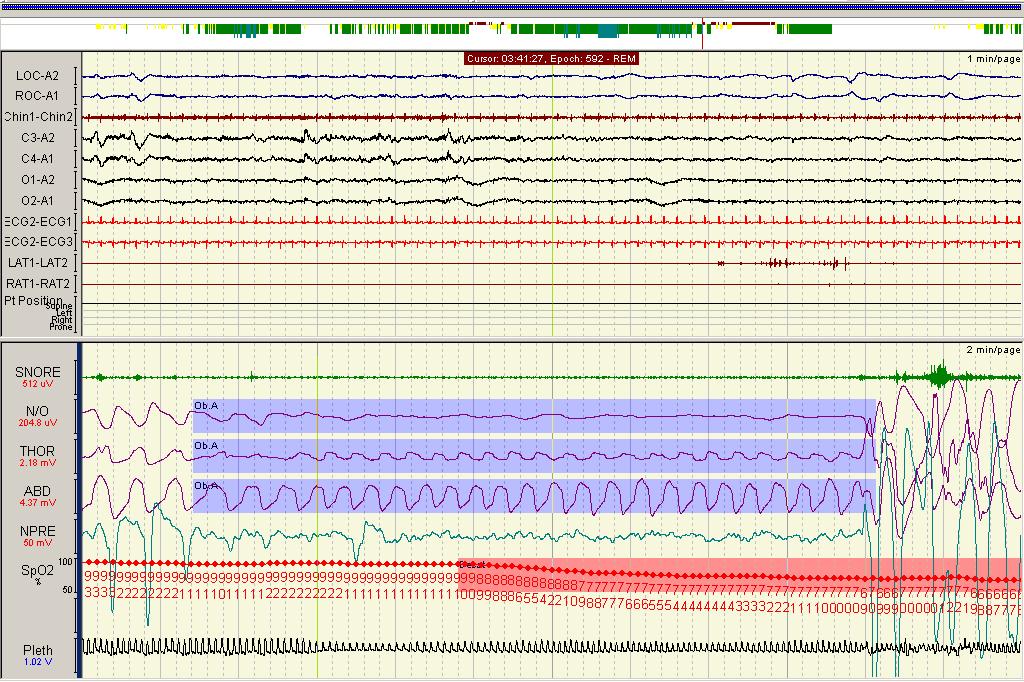
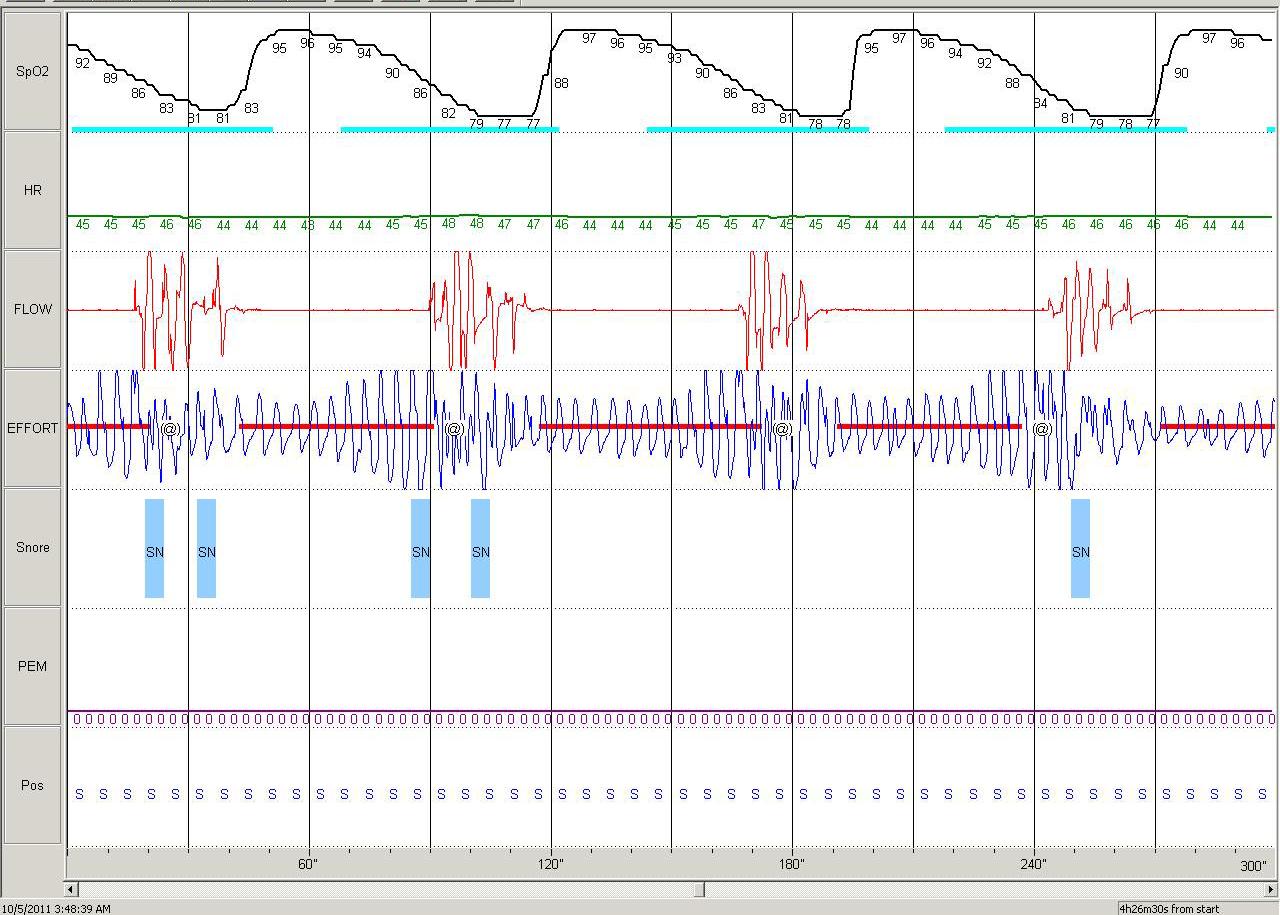
Polysomnogram (PSG) is our diagnostic cornerstone
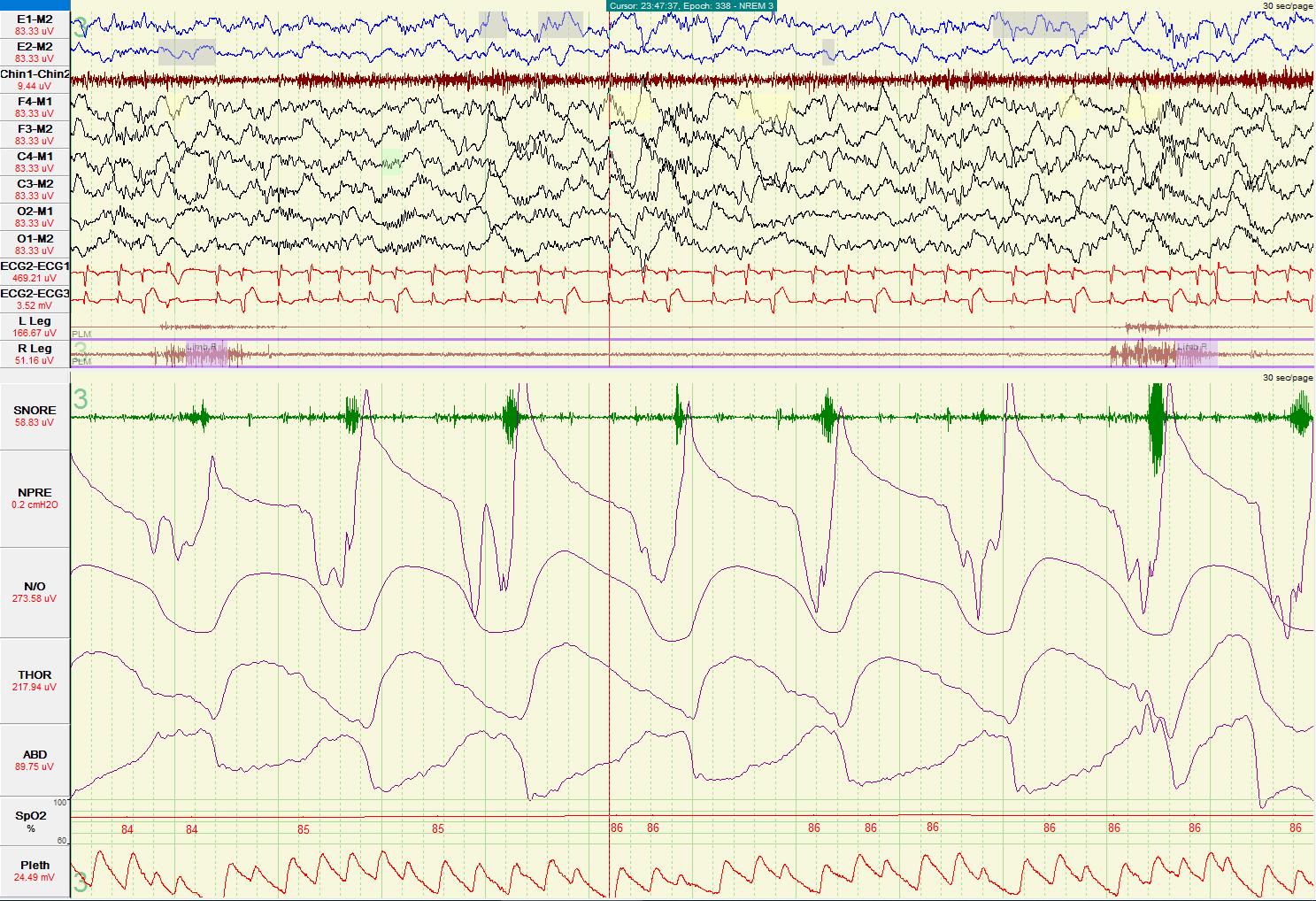

Multidimensional, complex, temporal
Annotation to label and quantify data
• Sleep stages (N1, N2, N3, stage R)
• Respiratory events (apneas, hypopneas; obstructive or central)
• Movements (PLMS)
174
Labor intensive work by technicians
30s manual visualization
Imperfect interrater reliability
interscorer agreement ≈83%
κ = 0.76
Large annotated/labeled ‘gold-standard’ datasets →
Ideal training of ML algorithms (lots of examples)
Previously, ML analyses of PSG →
hand extracted features
small N studies
complex signals, physiological heterogeneity
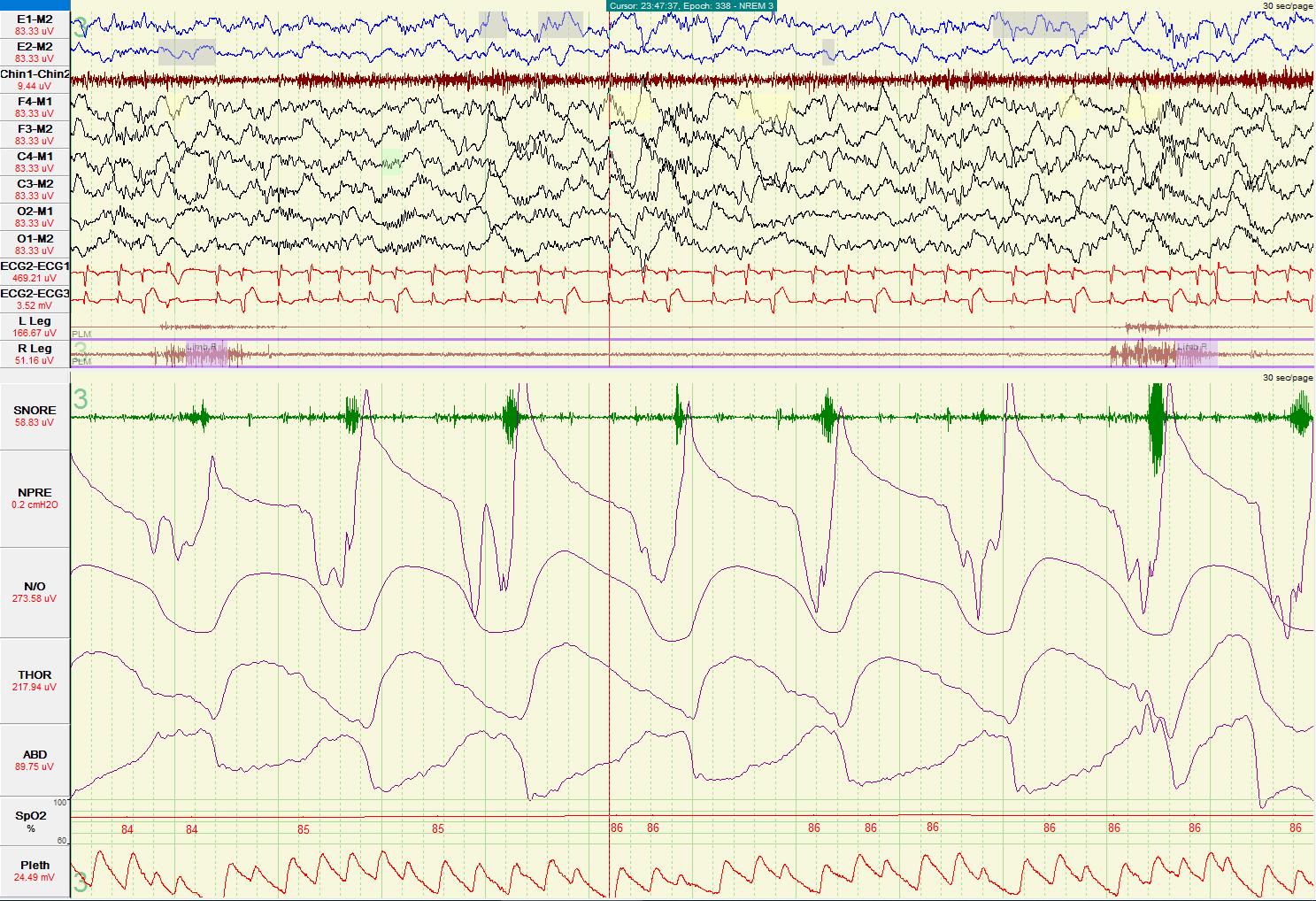
Improved with deep neural networks
✔PSG signal - spatial and temporal relationships
large N studies to capture heterogeneity

Lee YJ, Lee JY, Cho JH, Choi JH. Journal of Clinical Sleep Medicine. 2022 Jan 1;18(1):193-202. 175
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 176
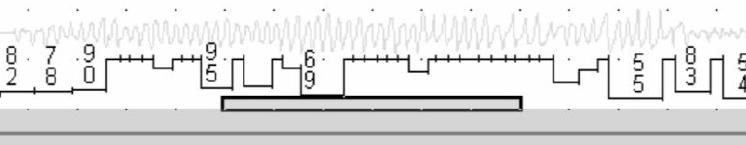
r squared= 0.85
B, D simple correlation of AHI and LMI (algorithm predicted versus ‘true’ expert scored)

r squared= 0.79
A, C confusion matrices probability that model predicts sleep stage/AHI class a, when truth [human scoring] is b; allows identification of misclassification tendencies

MGH
Test on held
MGH
Performance: Train on
dataset,
out
dataset
Biswal S, Sun H, Goparaju B, Westover MB, Sun J, Bianchi MT. Journal of the American Medical Informatics Association. 2018 Dec;25(12):1643-50. 177
Meta-analysis of 14 studies → overall (machine-human scorer) sleep staging agreement 85%, κ = 0.73-0.86 (0.76 against panel)

Same as human-human agreement!

178
Hold out testing data unseen by algorithm, but from same dataset used for training
Same hardware acquisition system
Single patient population
Same RPSGTs score
Mean κ of 14 studies with testing on same dataset 0.80 ± 0.03 VS
How do you ensure algorithm is generalizable to PSG from other sources?


A completely novel dataset
Mean κ of 13 studies with testing on different dataset 0.70 ± 0.06

179
Size and heterogeneity of data matter for performance
deep neural net sleep staging developed using 15,684 PSGs from 5 cohorts different size and diversity scenarios evaluated (single vs combined cohorts, varied % of dataset(s) used for training)
(how much of dataset used to train model)
SHAPES: accuracy, κ → single cohort used for training


LINES: accuracy, κ → ALL cohorts used for training
PERFORMANCE
↑training data set size
(plateaus when 75% data is used) AND
↑training set diversity
(use of all cohorts exceeded any single cohort)
Olesen AN, Jørgen Jennum P, Mignot E, Sorensen HBD. Sleep. 2021;44(1):zsaa161.
180
A tale of 2 uncertainties:
EPISTEMIC uncertainty arises from a lack of knowledge about the data or the optimal model. May be reduced through additional training and/or further data collection.

ALEATORIC uncertainty arises from the random nature of data and their measurements. Inherent to a specific measurement setup and cannot be reduced→ cap on both machine learning sleep-staging accuracy and interrater agreement (imperfect ground truth)


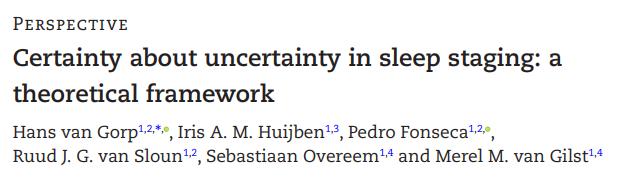
How good can we get?
No uncertainty Aleatoric uncertainty Epistemic uncertainty
current task 181
Data point outside of
Contributors to aleatoric and epistemic uncertainty in sleep staging


70%–80% of epochs will demonstrate some degree of sleep staging ambiguity across human scorers

van Gorp H, Huijben IAM, Fonseca P et al. Sleep. 2022;45(8):zsac134. doi:10.1093/sleep/zsac134
Bakker JP, Ross M, Cerny A, et al.Sleep. 2022; zsac154. doi:10.1093/sleep/zsac154 182
Score PSGs with 12 technicians and use consensus for true stage for each epoch (improve uncertainty?)

single technician scoring vs majority vote of 12
(
κ= colored shapes)
auto-scoring vs majority vote of 12
(
κ = black square)

auto-scoring almost always outperforms single human
in 98% of epochs, auto-scoring and at least one human scorer agree
Somnolyzer - bi-directional long short-term memory recurrent neural network
Bakker JP, Ross M, Cerny A, et al.Sleep. 2022; zsac154. doi:10.1093/sleep/zsac154
183
HYPNODENSITY GRAPH
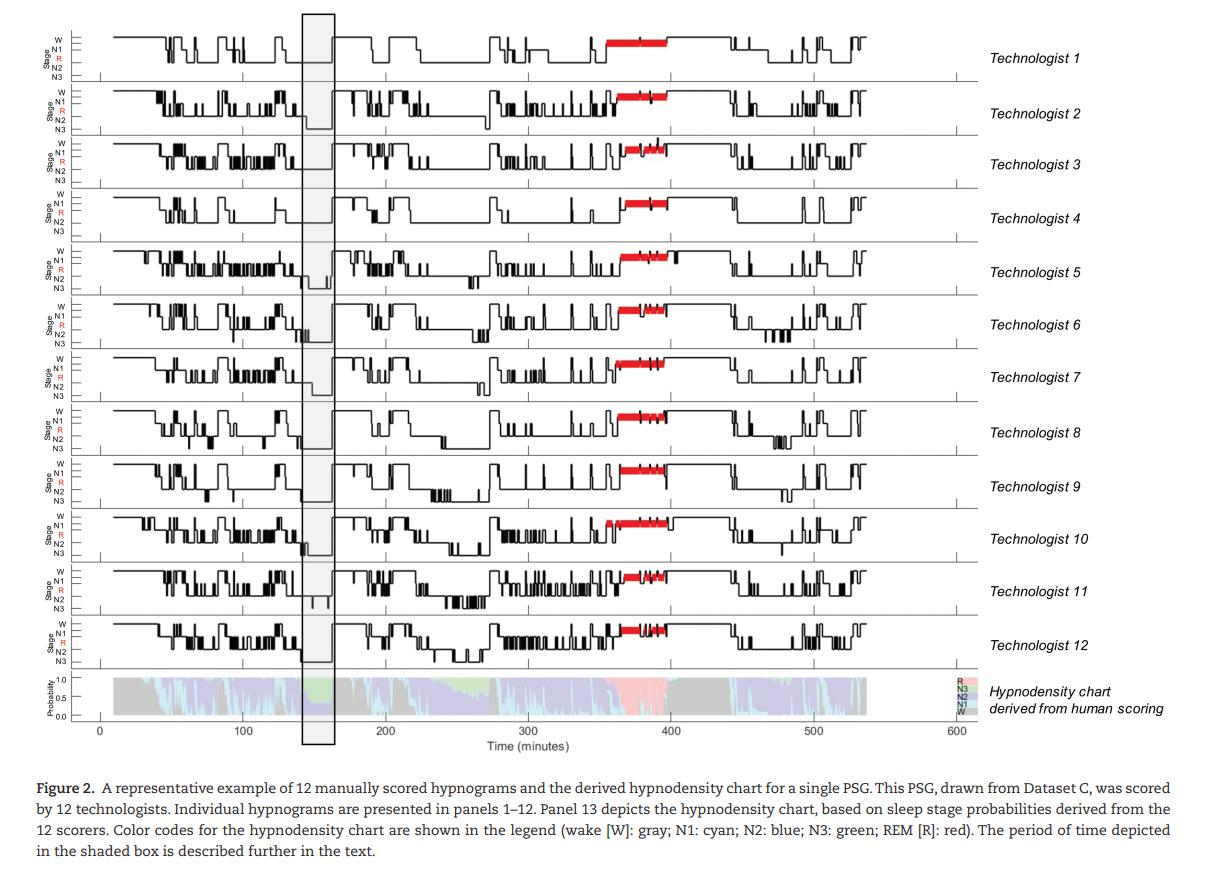

Sleep stage ambiguity is unavoidable →retain probabilities of sleep stages
184
Bakker JP, Ross M, Cerny A, et al.Sleep. 2022; zsac154. doi:10.1093/sleep/zsac154
Probabilities based on scoring of 12 humans
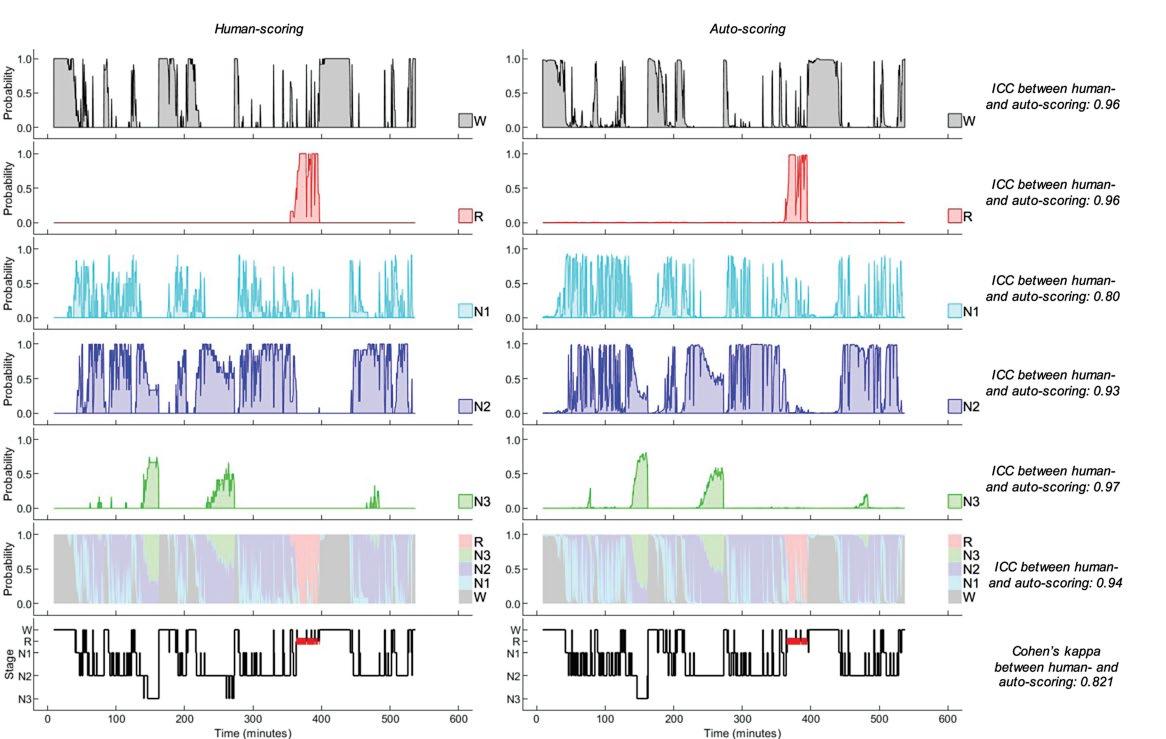
Auto scored (Somnolyzer) probabilities

1 PSG: Majority vote of scorers (consensus)
auto probability (consensus) 185
Highest
Alternative data sources for sleep staging
Previous studies:
AI applied to EEG signal →sleep stages
ECG and respiratory effort channels from 8682 PSGs: κ 0.585
Human scored Algorithm scored
Photoplethysmography (PPG) from finger pulse oximeter: κ 0.65

Respiratory effort signal (60s) derived stage probabilities
Respiratory effort spectrogram (whole night)
Relevant for … home testing (EEG monitoring difficult, impractical) to improve REI accuracy
Sun H, et al. Sleep staging from electrocardiography and respiration with deep learning. Sleep. 2020;43(7). Korkalainen H, et al. Deep learning enables sleep staging from photoplethysmogram for patients with suspected sleep apnea. Sleep. 2020;43(11).
from
186
Example
study subject
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 187
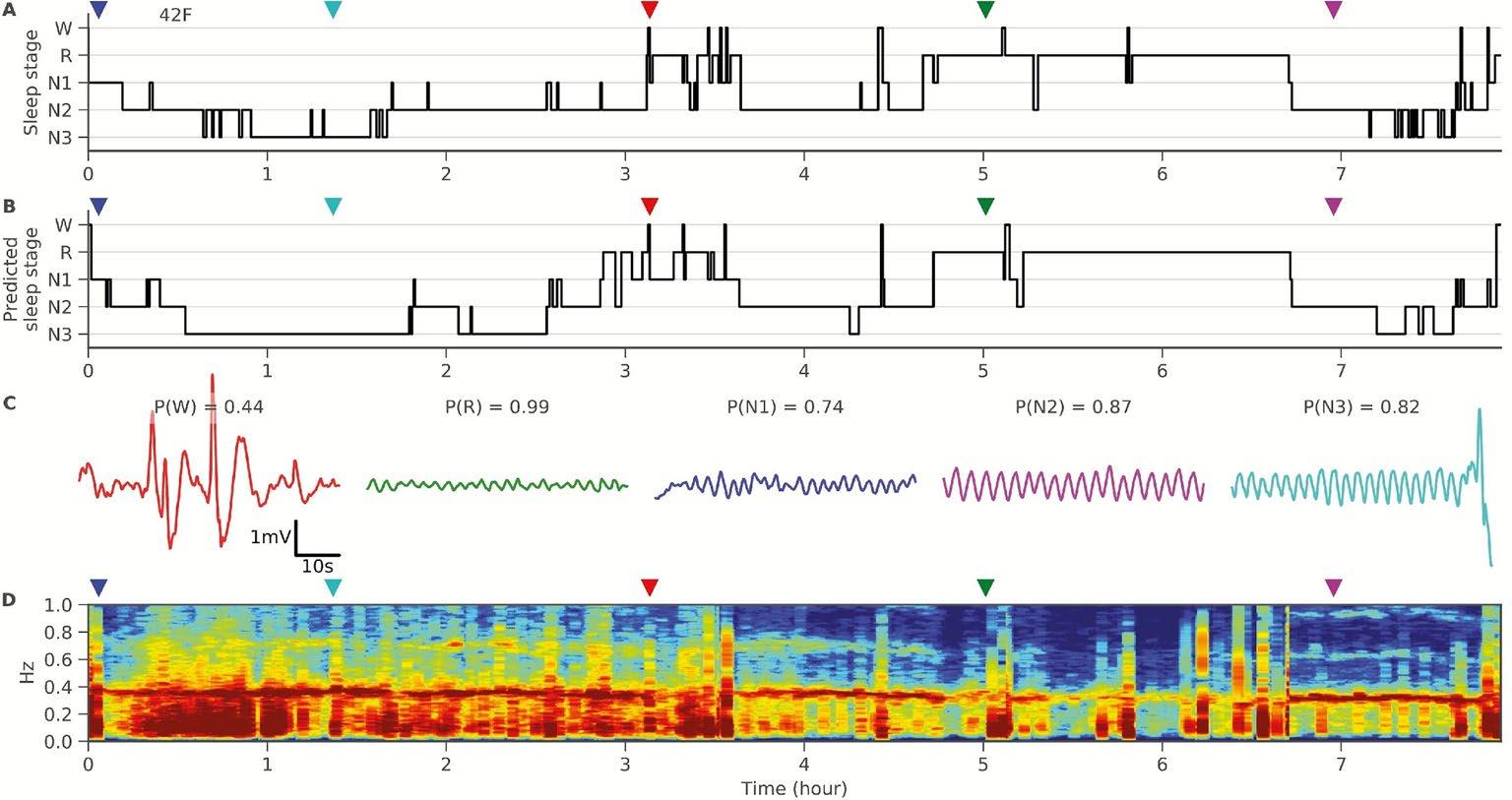
Diagnostic methodology: Narcolepsy
Current diagnostic method: PSG, next day multiple sleep latency test (MSLT)
mean sleep latency ≤8 minutes (MSLT)
≥2 SOREMPs (between PSG and MSLT)

Narcolepsy →short sleep latency, rapid transitions into REM sleep
Narcolepsy
Confirmation
ALSO poor nocturnal sleep consolidation, sleep state ambiguity, intrusion of REM (portions of REM) into other states
Can you use AI to diagnose Narcolepsy based on an overnight PSG ALONE?
Stephansen JB, Olesen AN, Olsen M, et al. Nature communications. 2018 Dec 6;9(1):1-5. 188
Neural network sleep staging in ≈3,000 controls and subjects with type I Narcolepsy (T1N, Narcolepsy with cataplexy)
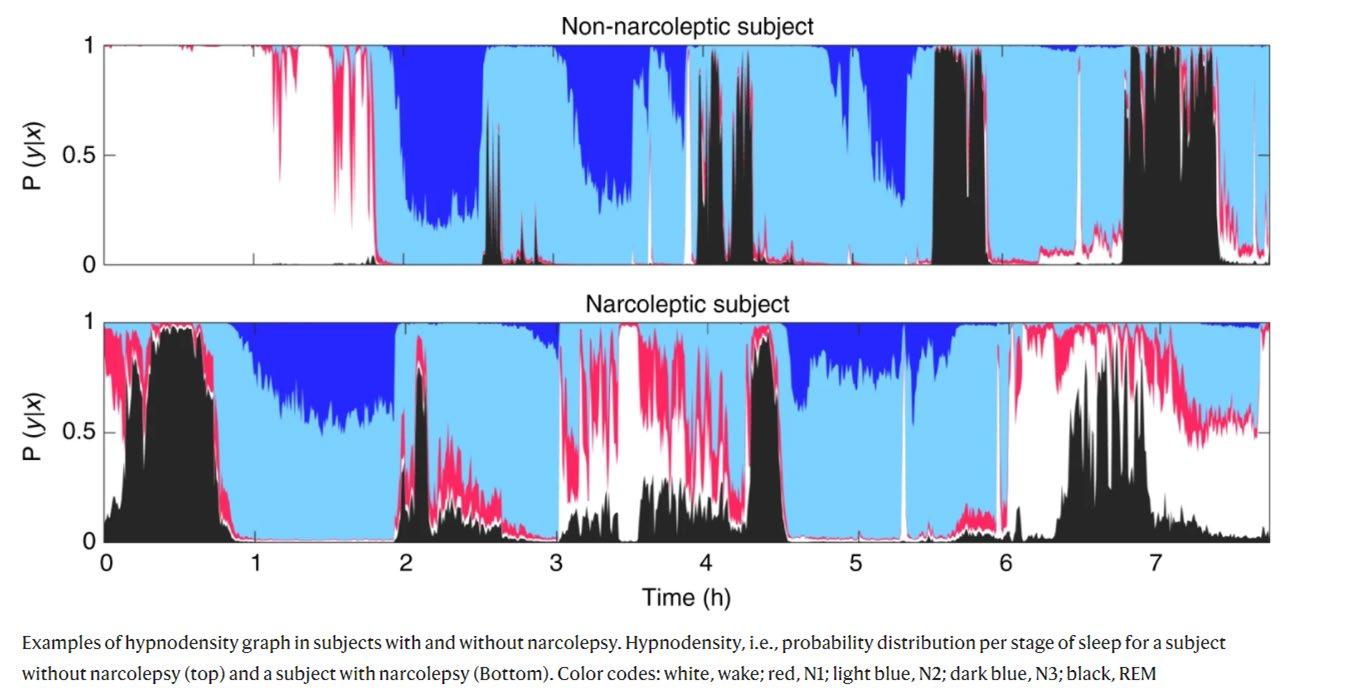

HYPNODENSITY GRAPH →visualization of probability of each sleep stage (rather than assigning definite categorical classification)
Controls
Expected progression of sleep stages
Minimal ambiguity
T1N
Sleep onset stage R, lack of expected progression
Increased sleep-stage uncertainty

Nature communications. 2018 Dec 6;9(1):1
189
Stephansen JB, Olesen AN, Olsen M, et al.
-5.
Electrophysiological T1N biomarker
Quantified features of sleep instability and dissociation



Gaussian predictor narcolepsy classifier
190
Stephansen JB, Olesen AN, Olsen M, et al. Nature communications. 2018 Dec 6;9(1):1-5.
Diagnostic methodology: REM sleep behavior disorder

RBD →incident synucleinopathies
RSWA on PSG electrophysiological hallmark
Confusing (inconsistently followed) scoring criteria
GAP in the field: systematic quantification and characterization of abnormal tone in stage R
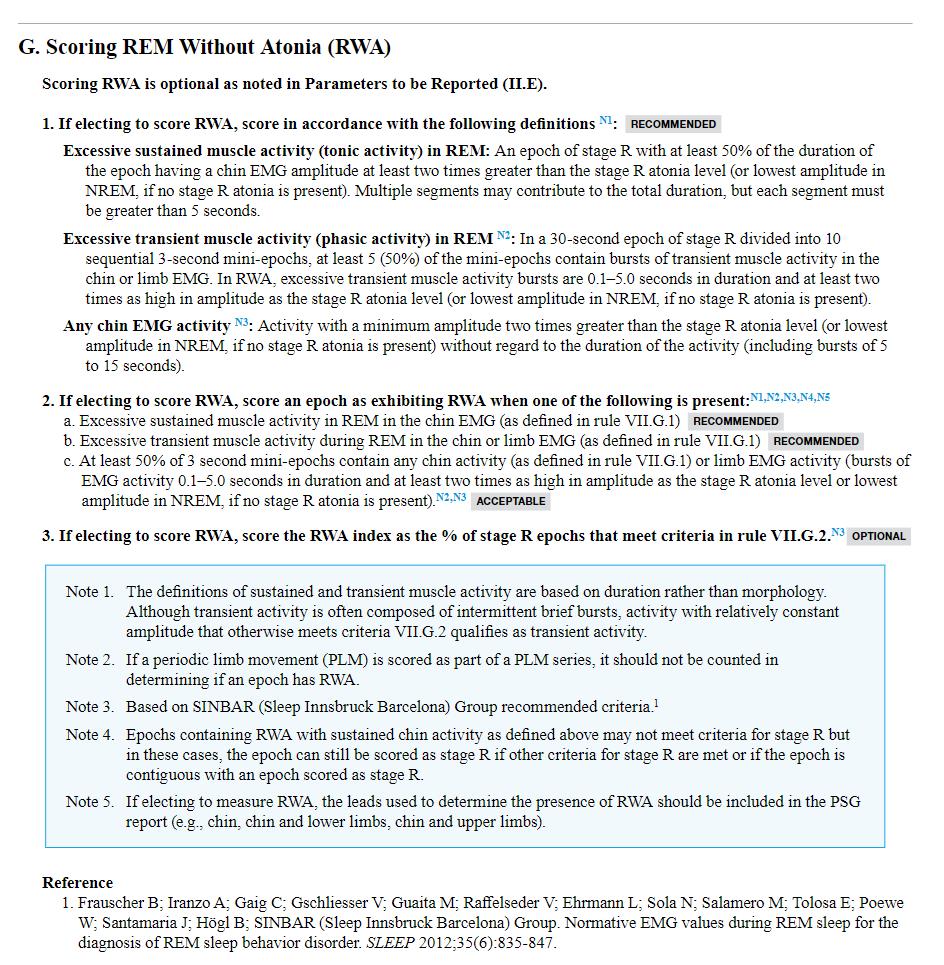
191
Diagnostic methodology: REM sleep behavior disorder
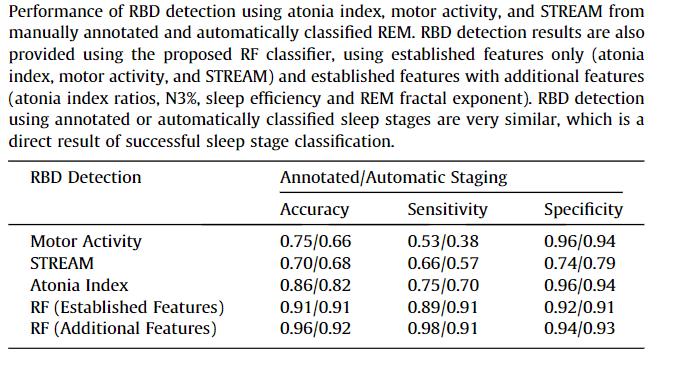
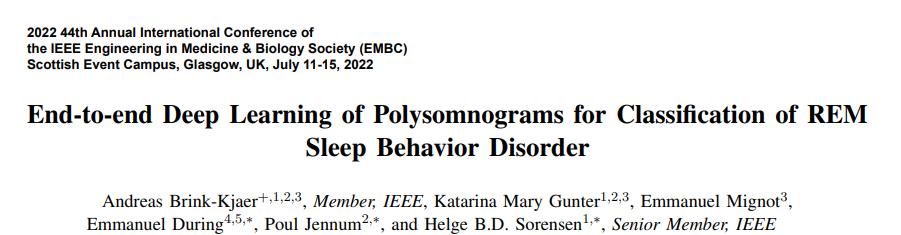

Random forest classifier
53 controls, 53 idiopathic RBD
Clinical Neurophysiology. 2019 Apr 1;130(4):505-14. 192
Cooray N, Andreotti F, Lo C, Symmonds M, Hu MT, De Vos M.
Diagnostic methodology: Non-PSG diagnosis of obstructive sleep apnea

Processed image input →convolutional neural networks

Supervised learning (output=PSG AHI)
Mean absolute error of 11 events/H
Accuracy (OSA dx) = 67% improved with addition of demographics, questionnaire data
Hanif U, Leary E, Schneider L, et al. IEEE J Biomed Health Inform. 2021;25(11):4185-4194 193
The most immediate applications of AI in sleep may be scoring automation and diagnostics …BUT what else?

194


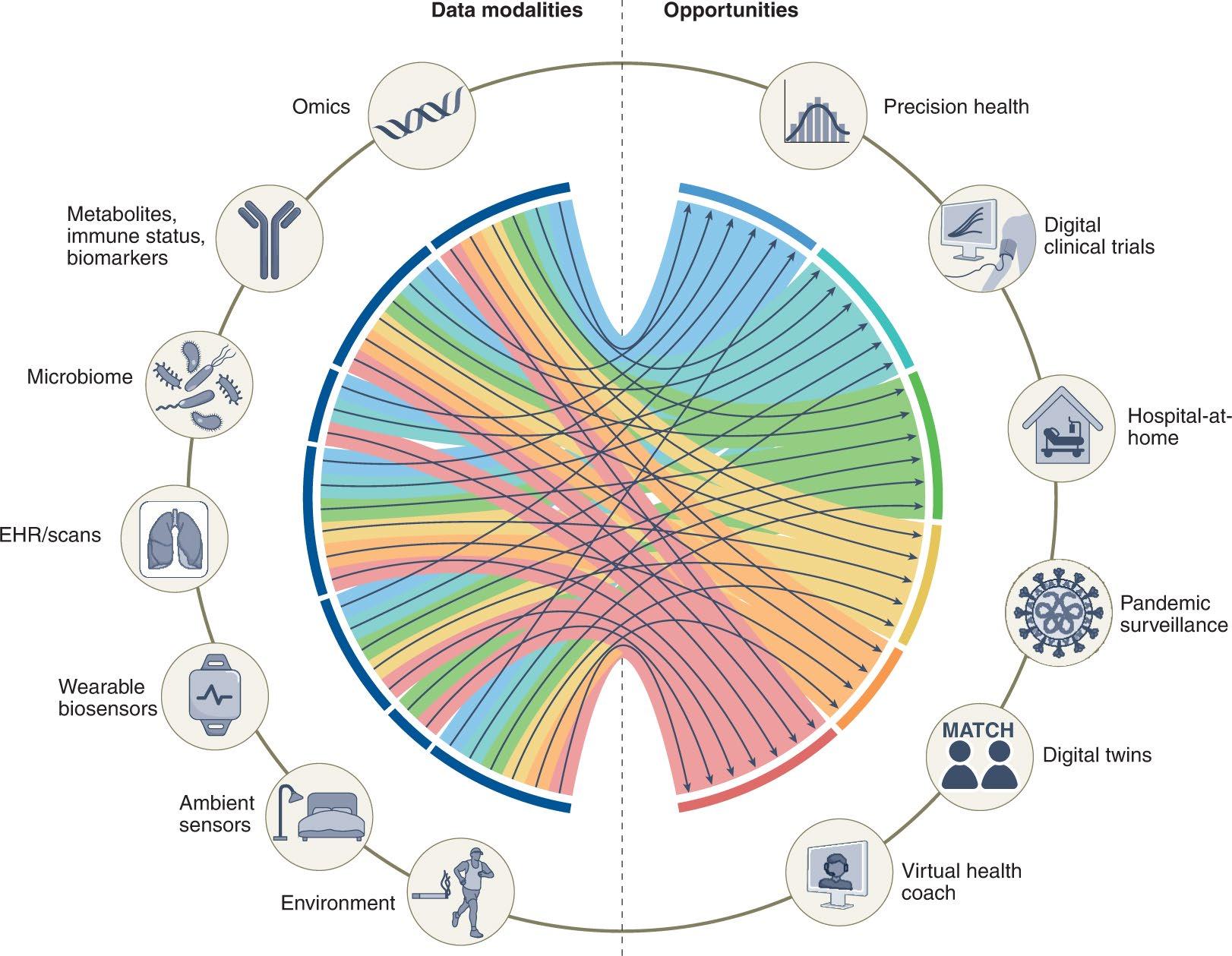
195
what do you think I ascertained after looking at 8 HOURS of beautiful, physiologically complex signal from multiple channels during the sleep state?


196


197
THAT’S IT??????

198
TABLES OF (somewhat) USEFUL SUMMARY METRICS


associate with patient symptoms
identify response to specific treatment predict sequela

199
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 200
Can we use AI to get more from what we already record?



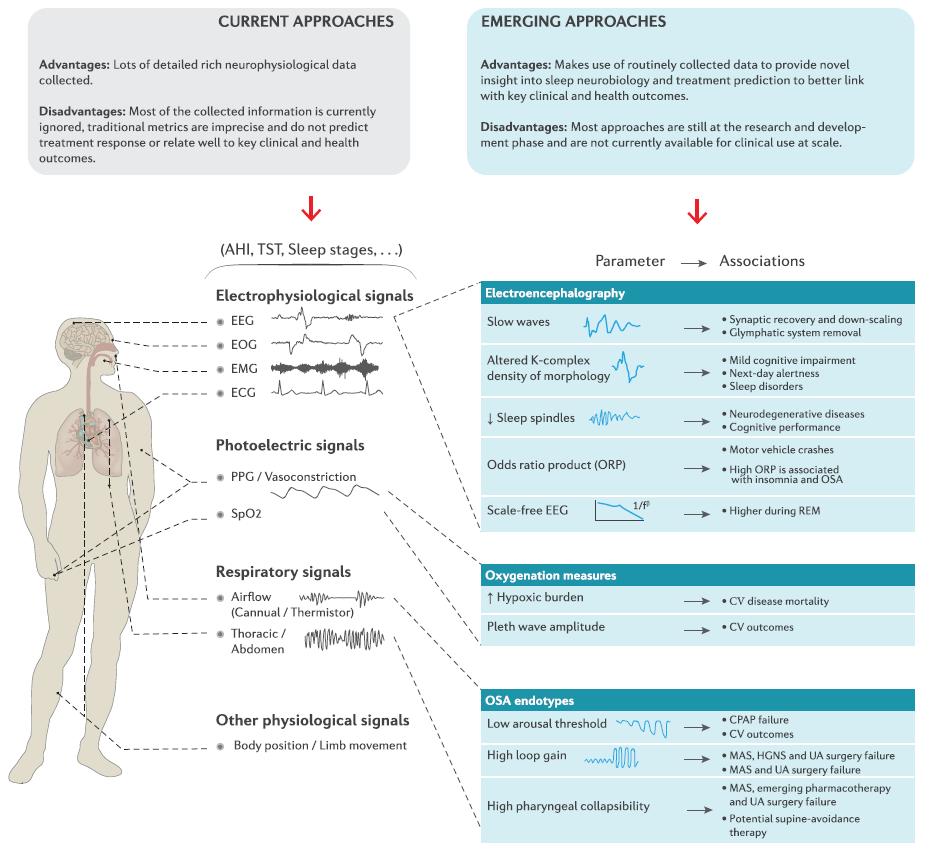

201
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 202
Current method depletes data from EEG



203
Current method depletes data from EEG
Don’t capture…
Deplete data from EEG

Morphological characteristics of slow waves, K complexes, and spindles related to cerebral blood flow, CSF flow, sleep homeostasis, synaptic downscaling, other memory/learning processes, vigilance, and alertness
Frequency characteristics (quantitative EEG) relevant for vigilance and cognition


Lechat B, Scott H, Naik G, et al. Front Neurosci. 2021;15:751730. Published 2021 Oct 7. doi:10.3389/fnins.2021.751730 204
MESA and MrOS cohorts
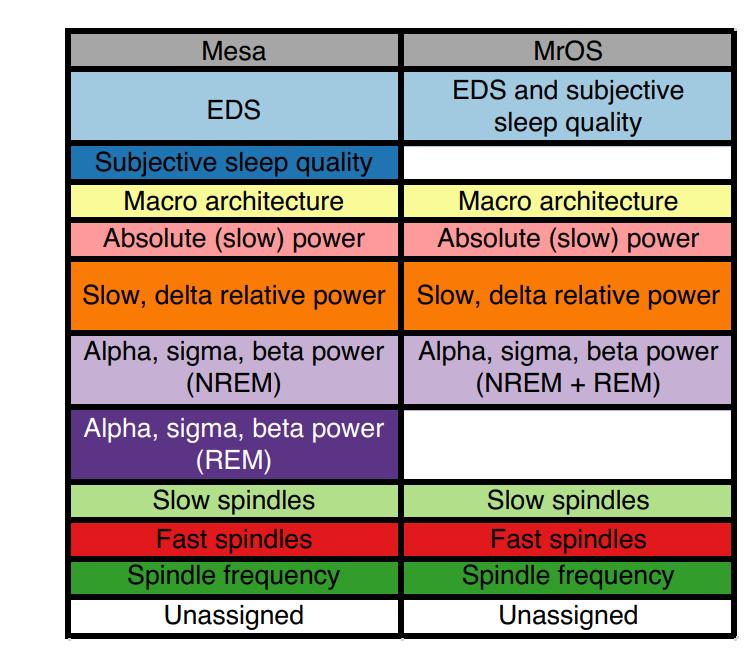
≈170 sleep metrics quantified in 3800 older adults (neuropsychological measures available)


dimension reduction/cluster analysis and principal spectral component analysis revealed → higher order structure of sleep
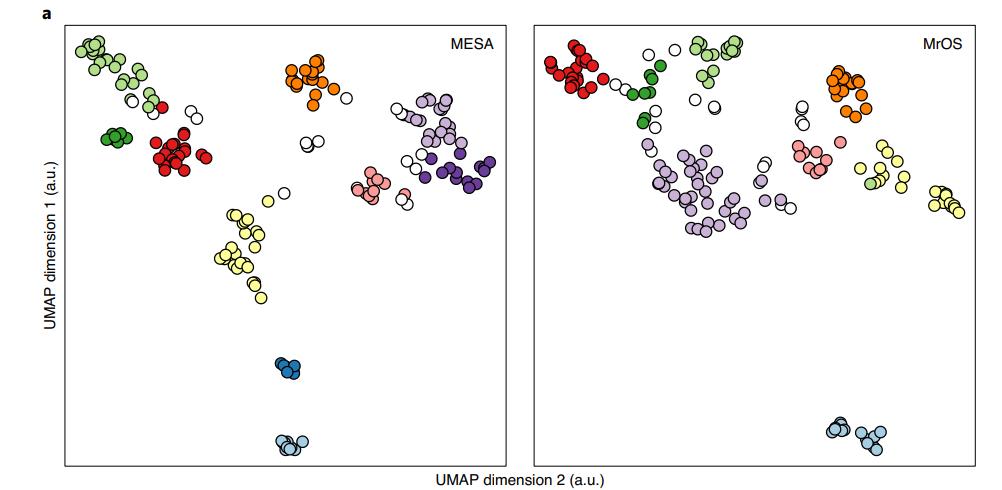
subjective sleep parameters
macroarchitecture microarchitecture
Djonlagic I, Mariani S, Fitzpatrick AL, et al. Nature human behaviour. 2021 Jan;5(1):123-45. 205
Macro structure
REM duration
sleep efficiency
Micro structure
sigma/beta ratio
fast spindle activity
slow spindle activity
slow oscillation (SO) duration (and slow/delta ratio)
strength of spindle–SO coupling

COGNITIVE PERFOMANCE
micro-architecture prediction of cognitive performance INDEPENDENT of macrostructure
subjective measures with only WEAK associations sleep EEG characteristics seen in younger individuals → better cognitive performance (even after adjustment for chronological age)

UNDERSTAND COGNITIVE HEALTH THROUGH NOVEL EEG metrics
(e.g. brain age index: ↑ from normal cognition to dementia; microstructure features distinguish normal cognition, MCI, dementia)

Djonlagic I, Mariani S, Fitzpatrick AL, et al. Nature human behaviour. 2021 Jan;5(1):123-45. Ye EM, Sun H, Krishnamurthy PV, et al. Sleep. 2022 Nov 30. 206
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 207
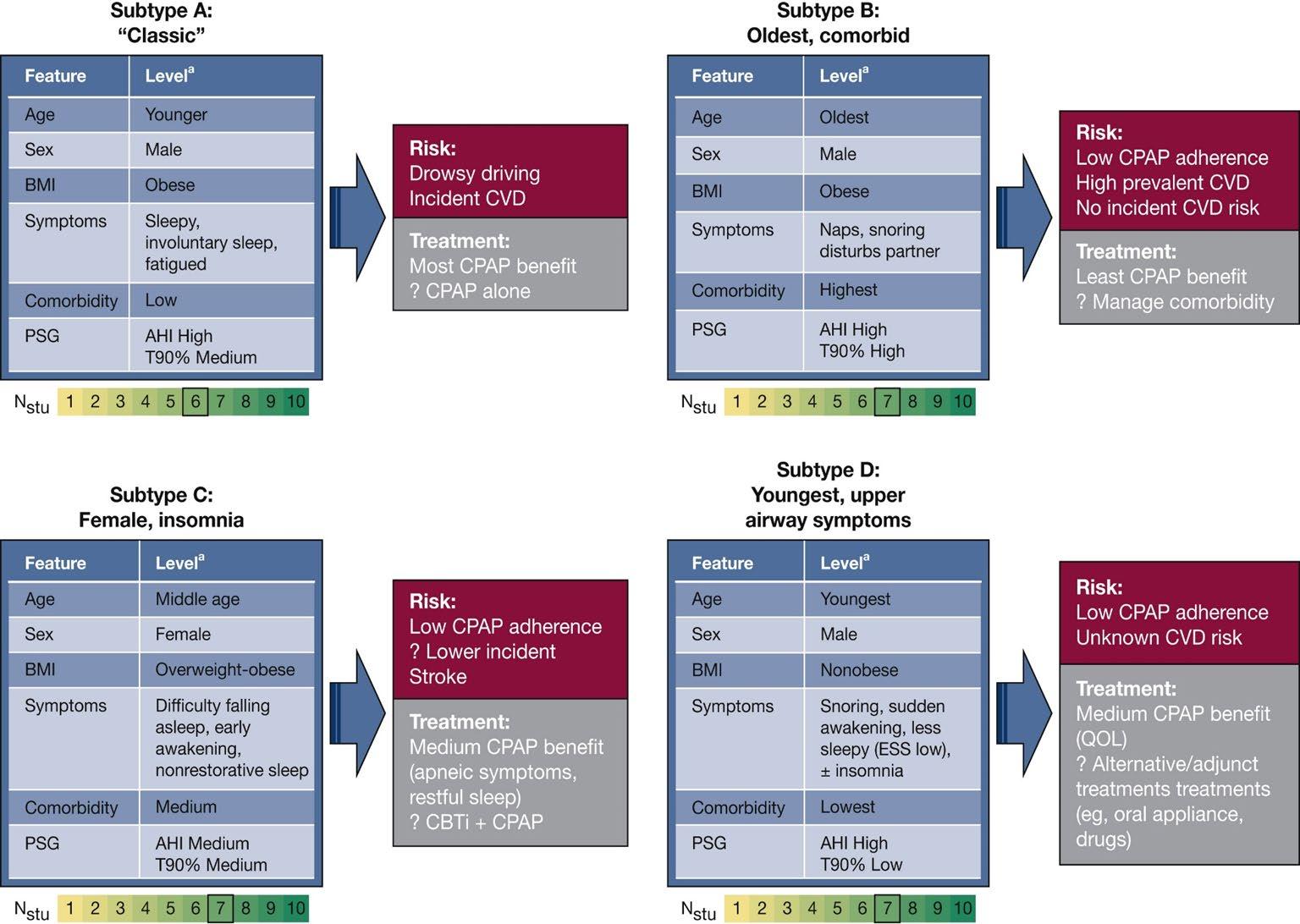
endotype subtype of a disease condition that is defined by a distinct pathophysiological mechanism phenotype observable characteristics of a disease without any implication of a mechanism
HETEROGENEOUS
physiological endotypes

symptoms
comorbidities
treatment responses

prognoses
genetic risk factors
SAME DIAGNOSIS

208
Phenotyping and Endotyping: DM vs OSA
clinical phenotype
hyperglycemia
airway obstruction during sleep
crowded pharyngeal anatomy/collapsible airway
(most)
endotype
(underlying mechanism)
loss of insulin production
diagnosis (treatment goal)
Type I DM (insulin)
resistance to insulin
+ non-anatomical (70%)
poor pharyngeal dilator muscle function
ventilatory instability
(high loop gain)
increased arousability from sleep
Type 2 DM (↑ insulin sensitivity)
NOT MEASURED!
OSA (fix CPAP deficiency?)

Edwards BA, Redline S, Sands SA, Owens RL. American journal of respiratory and critical care medicine. 2019 Sep 15;200(6):691-703.
209
OSA → CPAP intolerance → non-PAP treatments (oral appliance, surgical relief of airway obstruction, hypoglossal nerve stimulation)
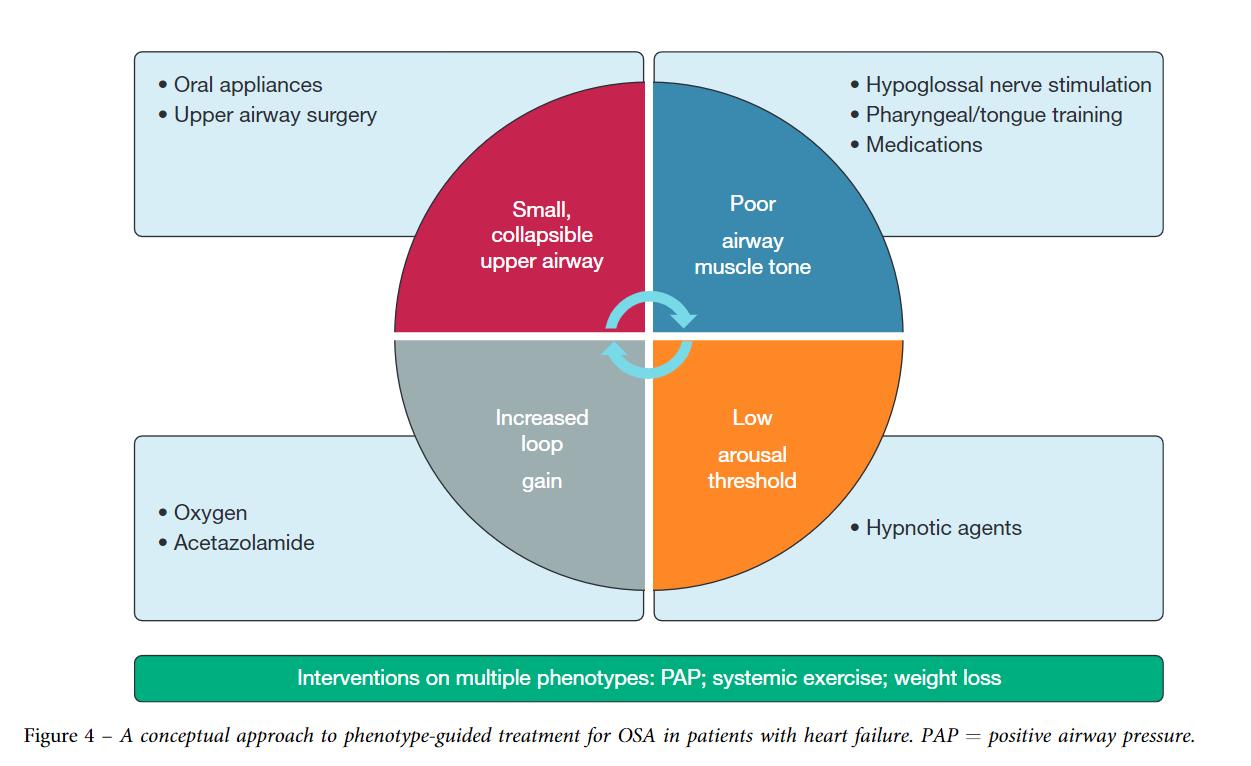
The FUTURE?
OSA → AI based PSG analysis to identify primary endotype

15;200(6):691-703.
2020;157(2):394-402.
OSA endotypes to personalize treatment
NOW
Edwards BA, Redline S, Sands SA, Owens RL. 2019 Sep
→ 210
Javaheri S, Brown LK, Abraham WT, Khayat R. AChest.



211
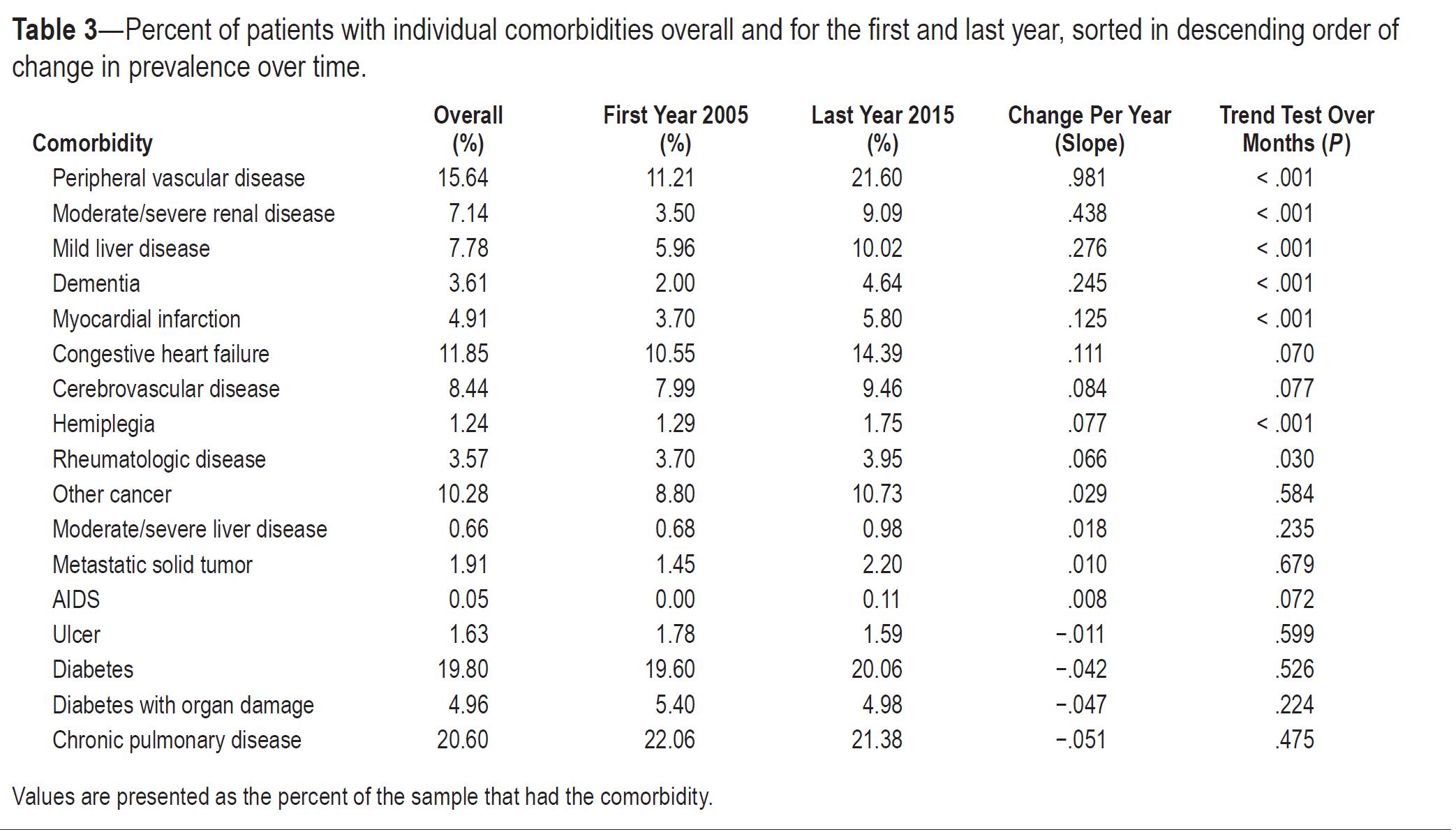
n=1247; K-means cluster analysis identified 7 OSA subgroups
MILD few respiratory events, ↑SE, normal REM sleep, near normal nocturnal SpO2


PLMS ↓ AHI, ↑PLMI
NREM and poor sleep NREM ↑AHI, ↑arousals, ↓SE

REM and hypoxia REM ↑AHI, lowest SpO2 nadir, greatest T<90%
Hypopnea and hypoxia ↑hypopneas with desaturations, ↑T<90%, preserved sleep architecture

Arousal and poor sleep apneas with arousals, minimal SpO2 desaturation, ↓T<90%, poor sleep architecture
Combined severe apneas with arousals and SpO2 desaturations, severe hypoxic burden, poor sleep architecture
212
4.9±1.9 years, ACS, TIA, stroke or death (n=271)
Risk of combined CV outcome by cluster (adjusted for Framingham and CPAP use)


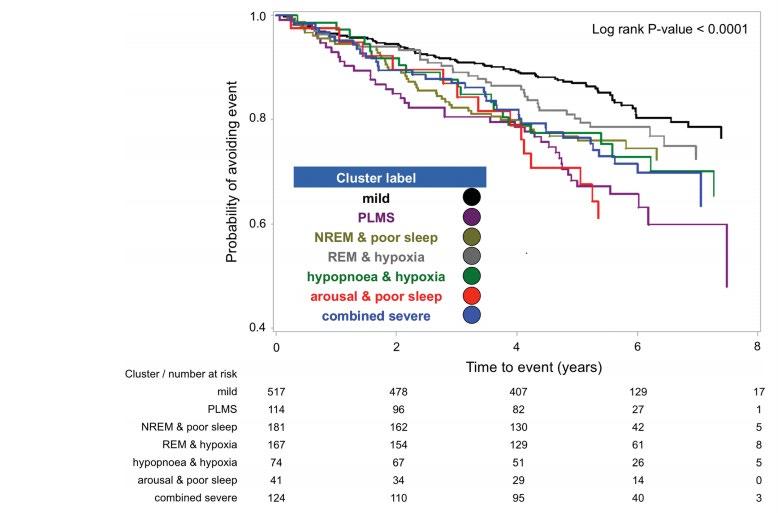
PLMS 2.02 (1.32 to 3.08)
hypopnea and hypoxia 1.74 (1.02 to 2.99)
combined severe 1.69 (1.09 to 2.62)

213
Traditional AHI severity categories association
cluster analysis to identify OSA phenotype subgroups → sequela, outcomes and PAP response

Zinchuk A, Yaggi HK. 2020 Feb 1;157(2):403-20. 214
Cluster 1 higher NIHSS scores.
Cluster 2 younger and had relatively low NIHSS scores.
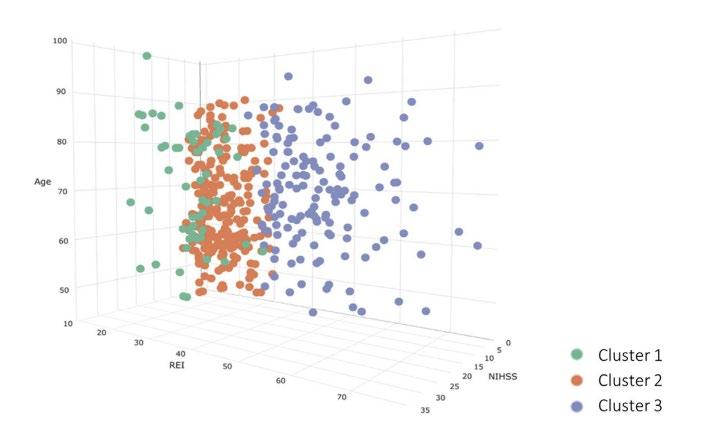

Cluster 3 participants with severe OSA and higher prevalence of medical comorbidities


215
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 216
Longitudinal sleep data from consumer sleep trackers



tri-axial accelerometer

optical photoplethysmography
(PPG)
Troiano et al. E Br J Sports Med. 2014;48(13):1019-23.
Spierer DK, Rosen Z, Litman LL, Fujii K. J Med Eng Technol. 2015;39(5):264-71.
MOTION PULSE 217
Some off-the shelf wearables let you access raw data (prior to sleep stage processing) for algorithm development and testing!



Staging accuracy=72%

https://github.com/ojwalch/sleep_ classifiers


Amazfit Arc (Huami, Inc.)
Apple Watch
Olsen M, Zeitzer JM, Richardson RN, et al. IEEE Trans Biomed Eng. 2022;PP:10.1109/TBME.2022.3187945. doi:10.1109/TBME.2022.3187945 Walch O, Huang Y, Forger D, Goldstein C. Sleep. 2019;42(12):zsz180. doi:10.1093/sleep/zsz180 218
https://github.com/StanfordSTAGES/SleepStagePrediction Staging accuracy=71-76%



Papini et al . Sci Rep. 2020 Aug 11;10(1):13512. 219



220
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 221
What can’t AI do?
Replace human providers and researchers entirely


222
What can’t AI do?
Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nature medicine. 2019 Jan;25(1):44-56.
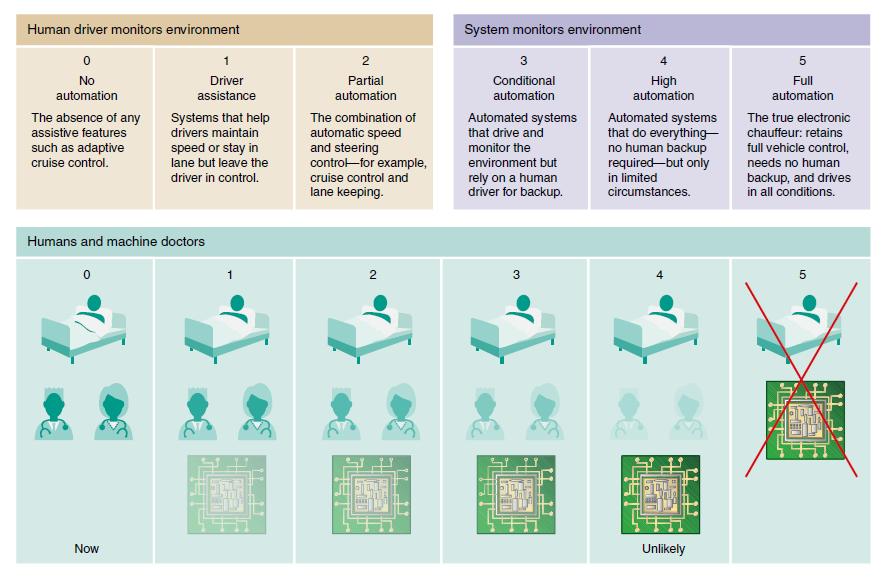


223
What can’t AI do? Replace human providers and researchers entirely
ALGORITHM DEVELOPMENT REQUIRES US TO WORK TOGETHER!
Federated learning → train models at different institutions


✔ reduce single-source bias
✔ data security
Development and execution of human subject studies for data collection
✔ optimization of algorithms requires ↑ size and heterogeneity of data
✔ enhanced disease recognition + understanding → opportunity to develop better therapies and different clinical models
✔ recognition of the need to adapt with changing populations + treatments
> OR Rajpurkar P, Chen E, Banerjee O, Topol EJ. AI in health and medicine. Nature Medicine. 2022 Jan 20:1-8. 224
What can’t AI do? Resolve bias and inequity
ETHICS, BIAS, EQUITY, LIABILITY – issues general to ALL AI applications
Machine learning models…LEARN: PERPETUATE and SCALE biases and inequity already present in data
✔ Incorrect annotations in datasets based on biased human labeling


✔ Underrepresented groups are underrepresented in datasets → algorithms don’t perform well in such populations
✔ Reduced access to opportunities/devices that allow their data to be included (e.g. reduced healthcare access in general)

✔ Big data collection methods may perform differently in different groups (e.g. green light PPG in wearables)

225
What can’t AI do? Obviate the need for sleep


226
Today’s ROADMAP for our AI journey
What is artificial intelligence?
Why sleep medicine?
AI staging of sleep and scoring of respiratory events
Improved diagnostic methodology (PSG and beyond)

OTHER USE CASES
EEG insights
Sleep disorder phenotyping and endotyping
Putting sleep back where it belongs
What AI can’t do
Regulation and Implementation 227
Current state of regulation- Software as a medical device (SaMD)


problem…machine learning algorithms…learn


LOCKED algorithm doesn’t change unless software version updated, can become outdated
ADAPTIVE algorithm adapts based on data, can learn from bias or have reduced performance in underrepresented groups
Current regulatory mechanisms not made for adaptive algorithms
228
FDA clearance often based on retrospective, single-institution data

(unpublished, proprietary)
AI pilot certification program

membership submits deidentified PSG EDFs

PSGs scored by expert panel


gold-standard annotated PSG database

Personal communication Steve Van Hout, Executive Director AASM; Azizi Seixas, PhD, Associate Professor at University of Miami Miller School of Medicine; Anuja Bandyopadhyay, MD Assistant Professor of Clinical Pediatrics in the Department of Pediatrics at Indiana University School of Medicine
manufacturers apply to program and test software on unscored PSGs compared to gold-standard scoring and ‘certified’ if benchmarks passed
Rajpurkar P, Chen E, Banerjee O, Topol EJ. AI in health and medicine. Nature Medicine. 2022 Jan 20:1-8. 229
Implementation: technology infrastructure
Integrated with current acquisition platform (easy)
Standalone software (may need middleware)
Institutional support (HL7 with EHR, IA, security)

Study file moved after acquisition?
Cloud vs central server?
System Requirements:
Operating System
Memory
Web Browser
High Speed Internet connection
230
Implementation: Workflow
technologist used to review AI scored PSGs first OR direct to physician for interpretation/report with return to technologist only for issues?
scoring technologist

interpreting physician interpreting physician
↓time from acquisition to available scored data
removal of rate limiting step for interpretation
∆staffing needs?
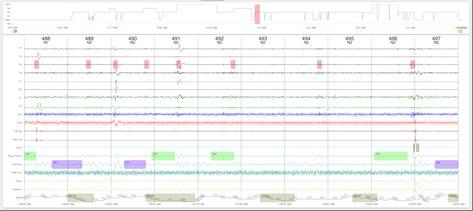
231
Reporting
New metrics quantified from clinical PSG
Education staff/patients
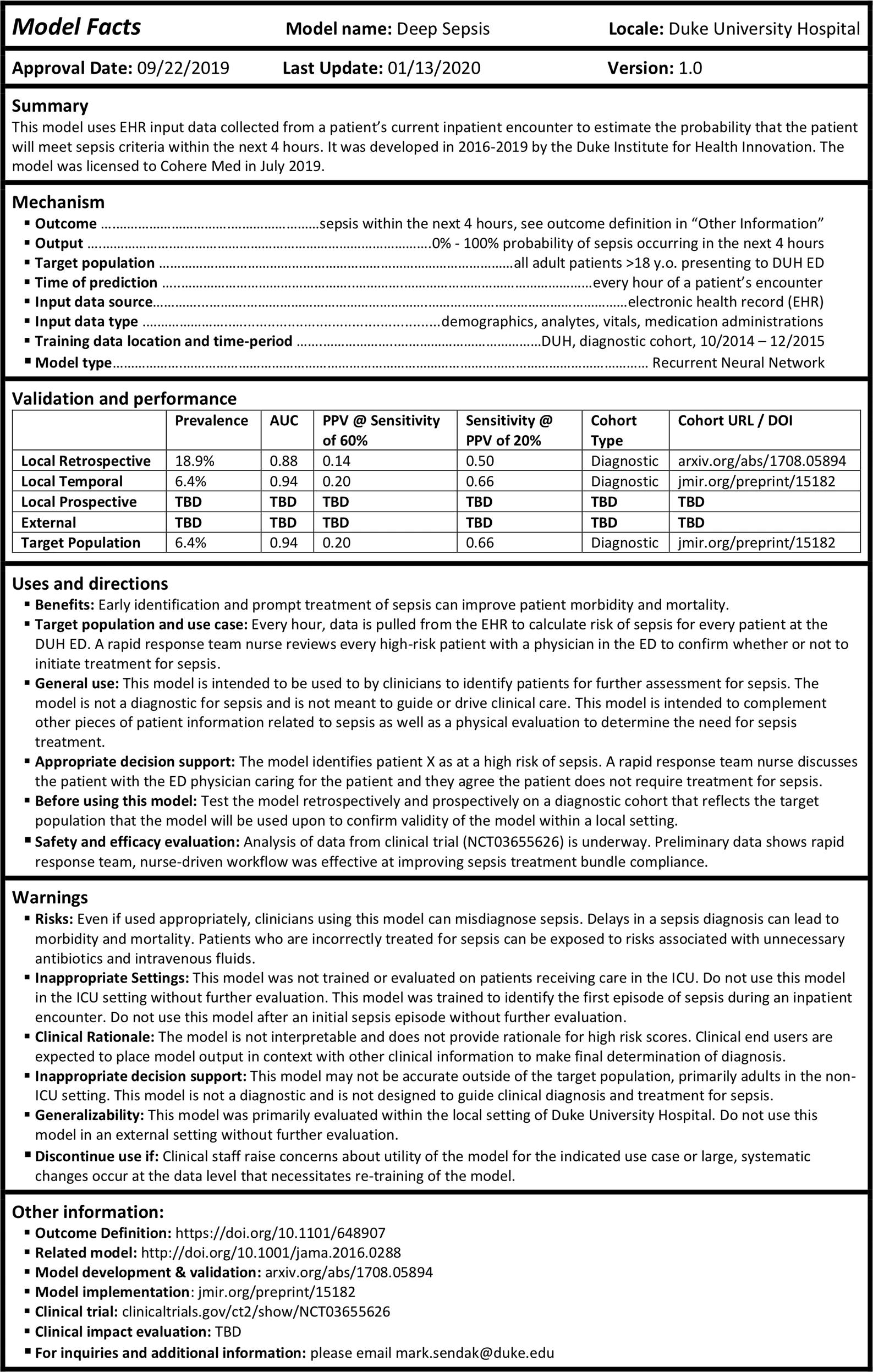

Labeling
The “Model Facts” label specifically serves the audience of clinical end users at the implementation stage and is distributed via channels that are closely integrated with the clinical decision support
Sendak MP, Gao M, Brajer N, Balu S. Presenting machine learning model information to clinical end users with model facts labels. NPJ digital medicine. 2020 Mar 23;3(1):1-4.
•
Implementation
•
•
•
232
SUMMARY
improved disease endotyping and phenotyping
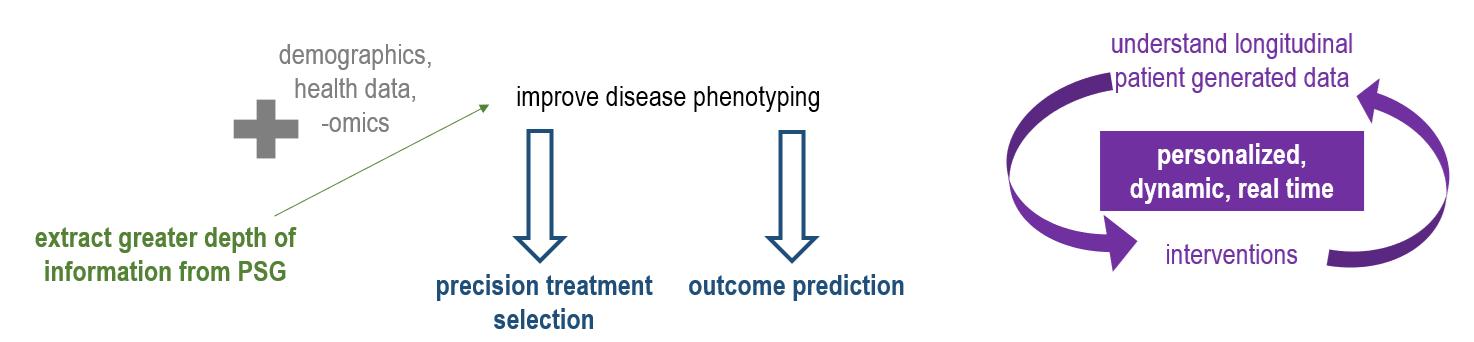
✔ Automated scoring of PSG
✔ Alternative diagnostic methods
✔ Reveal novel health assessments from PSG (brain age from EEG)

✔ Unsupervised learning to reveal previously undescribed disease subphenotypes (outcomes)
✔ Identify likely disease endotypes (personalized treatment) ✔ Longitudinal sleep assessments non-traditional sensors (consumer sleep technologies)
✔ Multimodal longitudinal patient generated data to guide precision, dynamic interventions; prediction
MORE (we barely scratched surface)… circadian assessments insomnia pediatrics screening with big data (EHR, questionnaires)
CPAP pressure setting estimation image recognition for cephalometrics, mask fitting video analysis clinical operations (AI scribe)
AI will augment, not automate human processes
Careful attention to scaling of bias and disparities
Regulation remains unclear
Implementation requires careful security, technical, and logistical considerations
GENERATIVE AI
233

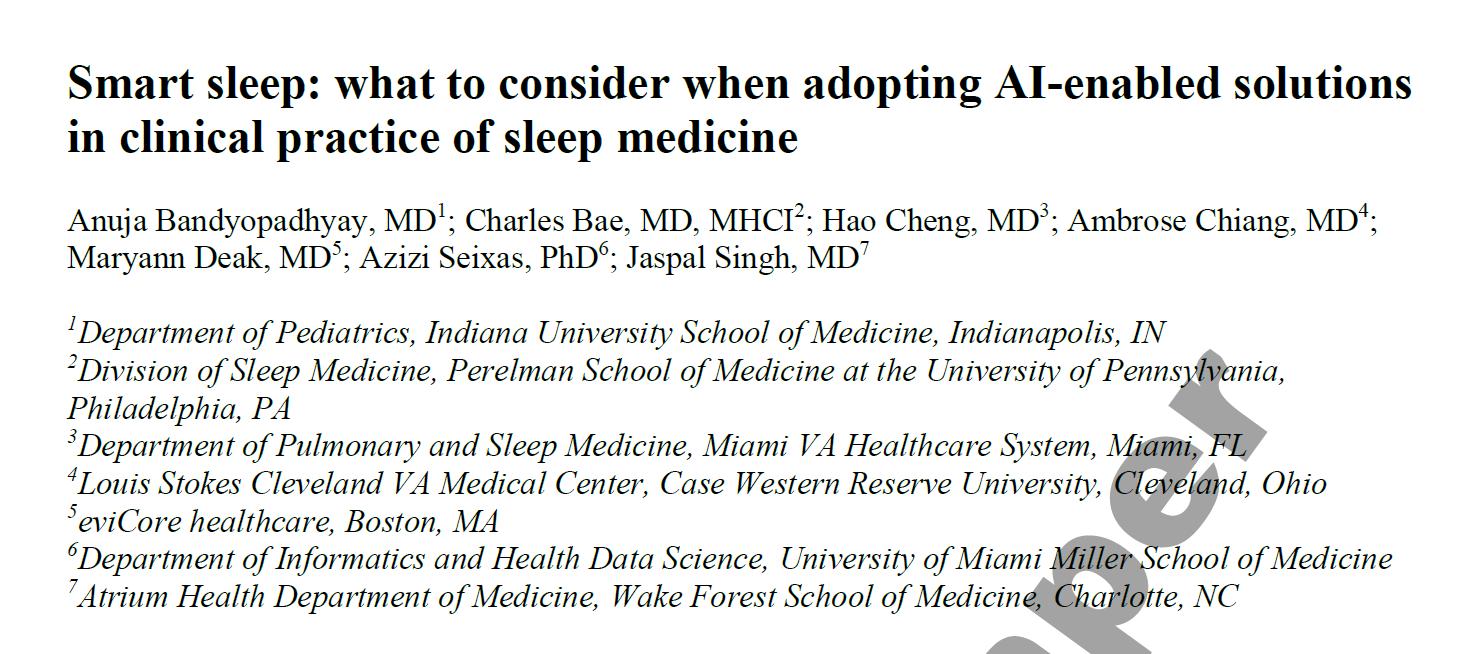

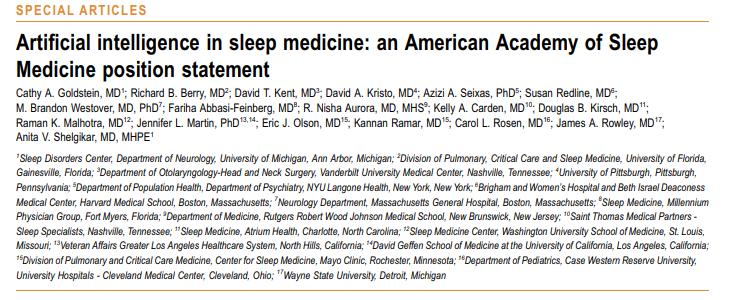






@cathygo_sleep 234
Want to learn more? cathygo@med.umich.edu
HIGH ACUITY PATIENTS IN SLEEP LABS: ENSURING PATIENT SAFETY
 Medical Director, Sleep Medicine, Atrium Health
Clinical Professor, Dept of Neurology, Wake Forest School of Medicine
Douglas Kirsch, MD, FAAN, FAASM
Medical Director, Sleep Medicine, Atrium Health
Clinical Professor, Dept of Neurology, Wake Forest School of Medicine
Douglas Kirsch, MD, FAAN, FAASM
235
DISCLOSURES
• Sleep Advisory Boards: AIM, Apnimed, Huxley Medical, SleepImage
• Committee Member, Alliance for Sleep (sponsored by Idorisa)
236
1) What risk occurs in a Sleep Laboratory?
2) Are there reasons risks in Sleep Laboratories may be climbing?
3) How do we ensure patient safety?
•
TO COVER:
•
•
237
Patient had a history of anorexia and prior cardiac arrests.
She was one of 20 volunteers being used to test the combination of lithium carbonate, an antidepressant, and AMPT (alpha-methyl-para-tryosine), an experimental drug. The study was to monitor the effects of the two drugs on sleep and mood patterns.
https://www.washingtonpost.com/archive/local/1980/06/04/nih-program-cleared-in-death-of-student-23-in-sleep-study/1a360f9a-50ae-4cc8-a8d6-bfadf1e26645/
JUNE 1980
238
SEPTEMBER 2015 https://www.ajc.com/news/crime law/verdict-for-family-after-man-dies-during-emory-sleep-test/IwVvH5egmT8QMqNKc0uGxK/ 239

240
SEPTEMBER 2015
https://www.boston.com/news/the-boston-globe/2023/05/01/boston-childrens-hospital-child-dies-sleep-study/

MAY 2023
241
https://www.boston.com/news/the-boston-globe/2023/05/01/boston-childrens-hospital-child-dies-sleep-study/
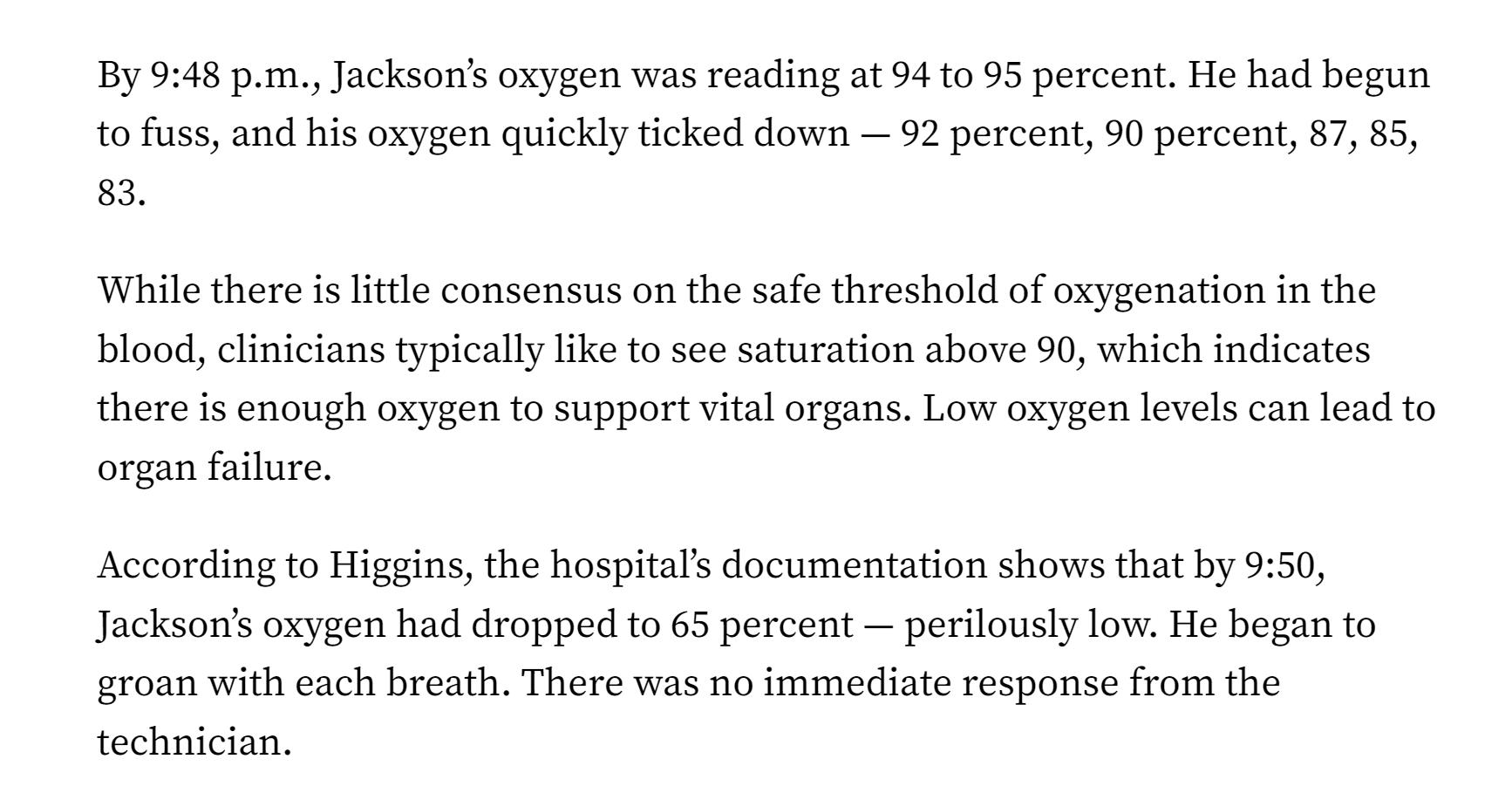
MAY 2023
242
https://www.boston.com/news/the-boston-globe/2023/05/01/boston-childrens-hospital-child-dies-sleep-study/
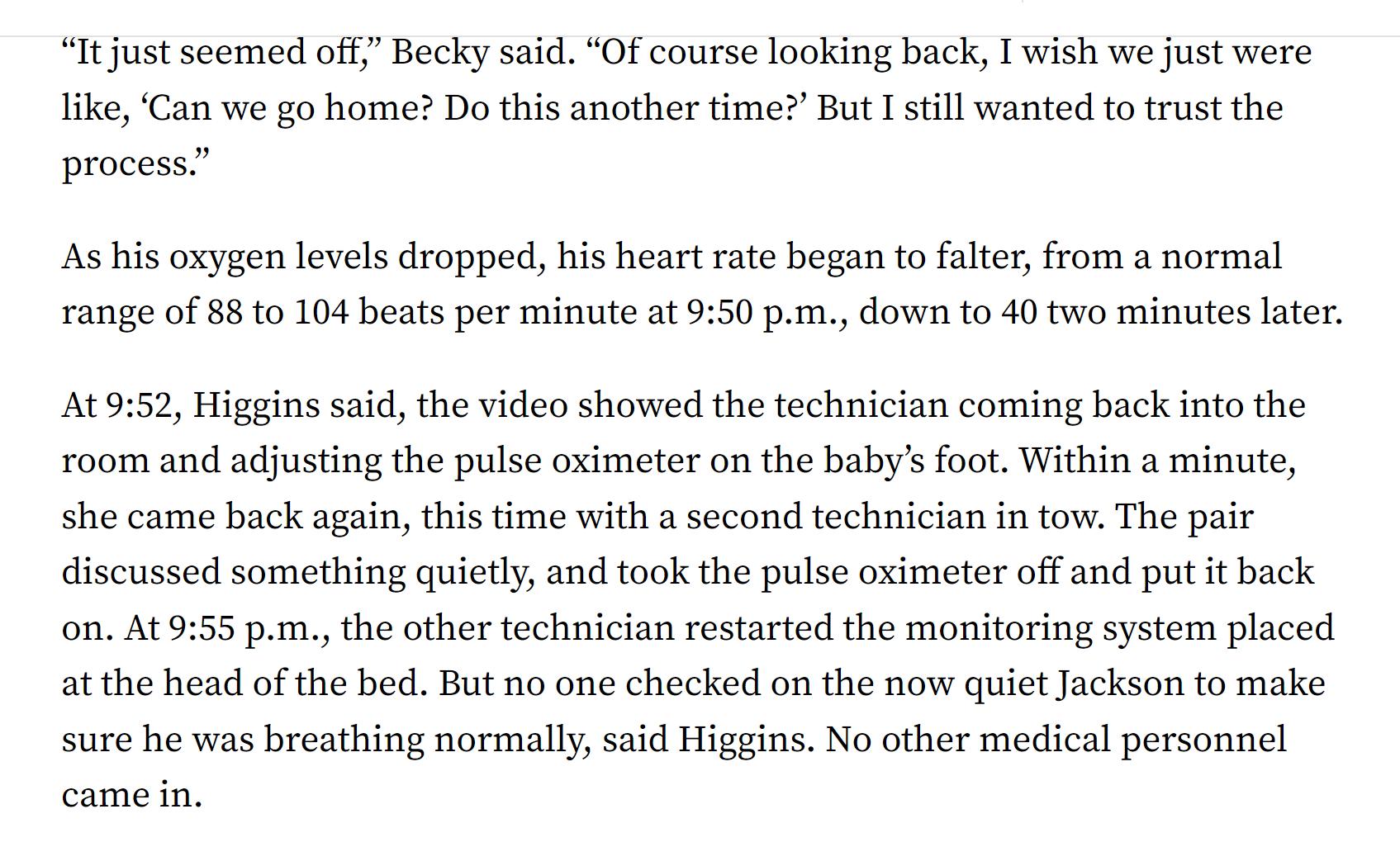
MAY 2023
243
BLACK SWAN EVENTS
https://thebulletin.org/2014/11/nuclear-war-the-black-swan-we-can-never-see/

244
BLACK SWANS
• Taleb's "black swan theory" refers only to unexpected events of large magnitude and consequence and their dominant role in history. Such events, considered extreme outliers, collectively play vastly larger roles than regular occurrences

245
MEHRA AND STROHL, 2004
• Problems encountered during polysomnography procedures fall primarily within 2 categories:
• (1) those resulting from the testing equipment and methods (ie, electrode placement, latex allergy, colloid use, or electrical safety)
• (2) adverse events noted by the technician or occurring to the patient during the study. These issues are listed in the literature in the form of anecdotal reports in textbooks or available by website.
SleepMed Incorporated (Columbia, SC) sleep centers in 4 states (Ohio, North Carolina, South Carolina, and Tennessee). Of the 17 sites, 1 was a free-standing (American Academy of Sleep Medicine-accredited) center; 1 was at a major hospital (> 500 beds) academic center; 1 was at another urban hospital (< 500 beds) center; and 14 were at nonurban hospitals (< 500 beds).
246
•
MEHRA AND STROHL
Out of 16,084 polysomnography studies, there was 1 fatality, occurring in the fifth month of the survey.
This death occurred in an approximately 60-year-old man with known history of coronary artery disease, dilated cardiomyopathy (ejection fraction 20%), and chronic hypertension who had undergone an elective split-night polysomnography for the indications of suspected sleep apnea (snoring and occasional pauses during sleep, but without reported sleepiness).
•
•
247
MEHRA AND STROHL
In 322 minutes of sleep prior to continuous positive airway pressure application, the respiratory-disturbance index was 37 events per hour associated with a nadir oxygen saturation of 80%.
The cardiac arrest occurred during sleep in the early morning, 101 minutes after application of continuous positive airway pressure with a respiratory disturbance index < 5 and a lowest oxygen saturation value of 91%.
•
•
248
PSG FRAGMENT
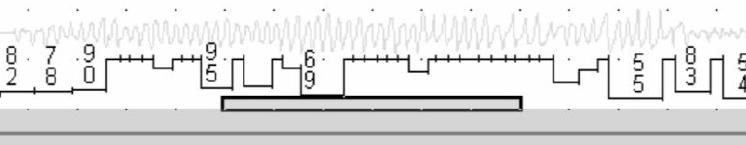
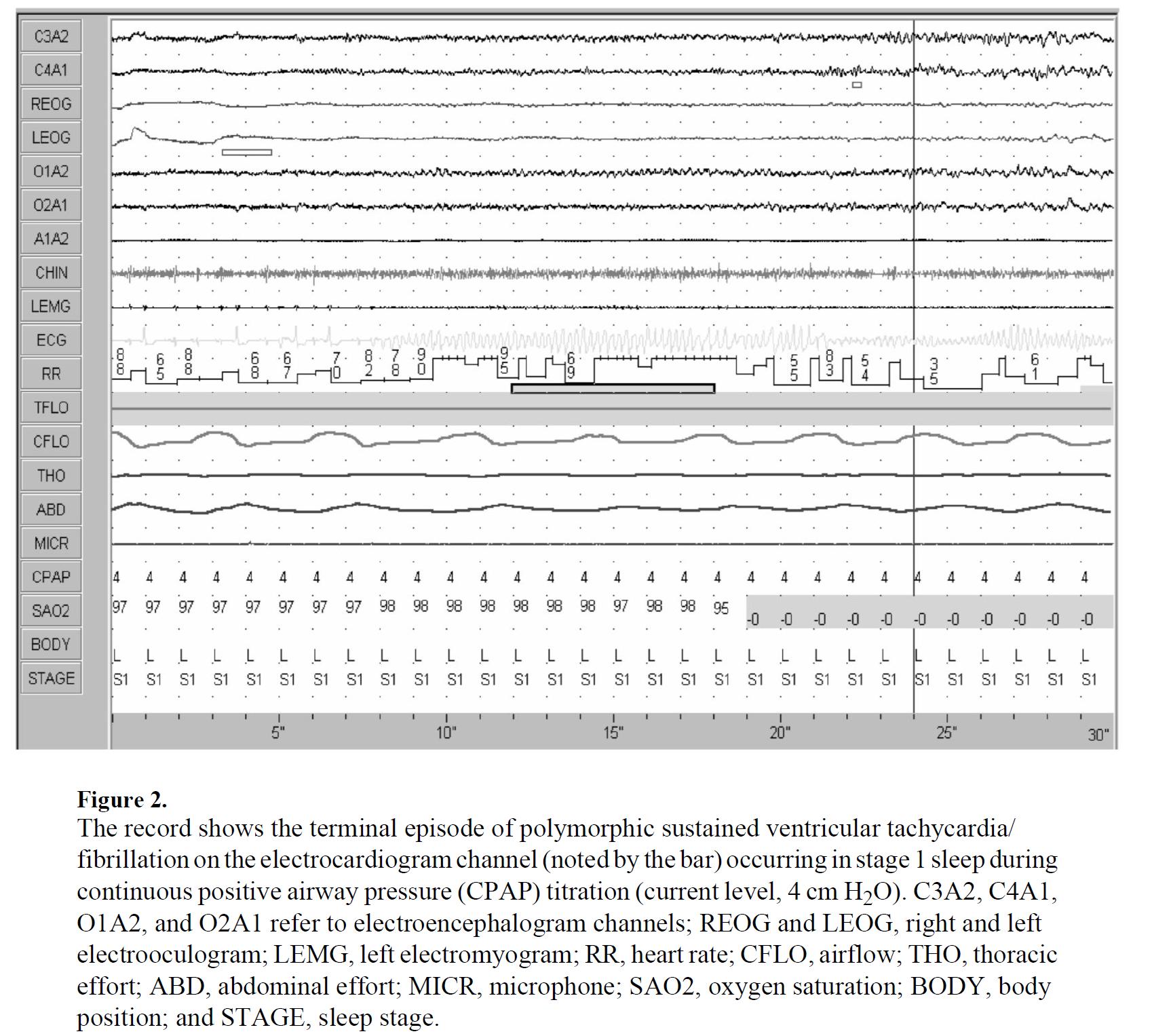
249
MEHRA AND STROHL

250
MEHRA AND STROHL

251
KOLLA ET AL, 2013
• We identified all reported safety incidents occurring at the Center for Sleep Medicine, Mayo Clinic, Rochester, MN, between Jan 1, 2005, and Dec 31, 2010. Safety incidents were defined as any patient safety concern that was reported to the medical director, the institutional safety “event line,” or events that resulted in summoning emergency medical personnel or that resulted in the patient being transferred to the emergency department. • During the study period, a total of 36,141 PSGs were performed at the Center for Sleep Medicine, Mayo Clinic, Rochester, MN. During this time period, a total of 111 calls were made to the emergency medical services. Thirty-nine adverse events were reported to the safety event line, and 27 events were reported to the medical director of the sleep lab
252
KOLLA ET AL., 2013

253

254
KOLLA ET AL, 2013
• “Our retrospective review of 36,141 PSGs revealed that adverse events during a PSG were relatively uncommon, and a minority of these requires hospitalization.
• Previous emphasis on cardiac arrhythmias may be overstated, as chest pain and patient falls were commonest and resulted in ED evaluation/ hospitalization more often.
• A small number of adverse events could have been anticipated and likely prevented if patients at risk were identified and medical personnel evaluated these patients prior to the PSG.
255
EVOLUTION OF THE SLEEP LABORATORY

256
https://www.witsendstore.com/details/p3224001_15537190.aspx
ANALOG SLEEP SYSTEM 1988
257
AASM Accredited Centers 1977-2010
0 500 1000 1500 2000 2500
2010 2000 1990 1980 1977 258
NUMBER OF SLEEP STUDIES (MEDICARE)
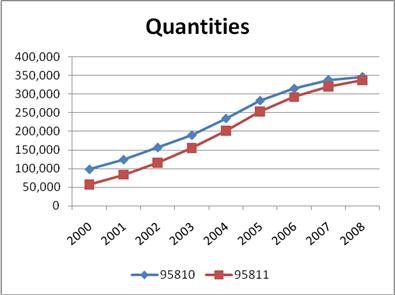
Medicare payments for polysomnography increased from $62 million in 2001 to $235 million in 2009 259
RELEVANT LAB SAFETY CONSIDERATIONS
• Safety in the sleep lab environment (Falls, injuries)
• Technologist monitoring!
• Emergencies
• 1) EEG – sei zures
• 2) EKG – arrhythmias
• 3) Respiratory – apnea/desaturations
• 4) Video – behaviors, including sleep and wake-related
260
IN-LAB POLYSOMNOGRAPHY (2M RESP)
37 y/o man (weight = 270 lbs) in stage REM sleep (2 minutes).
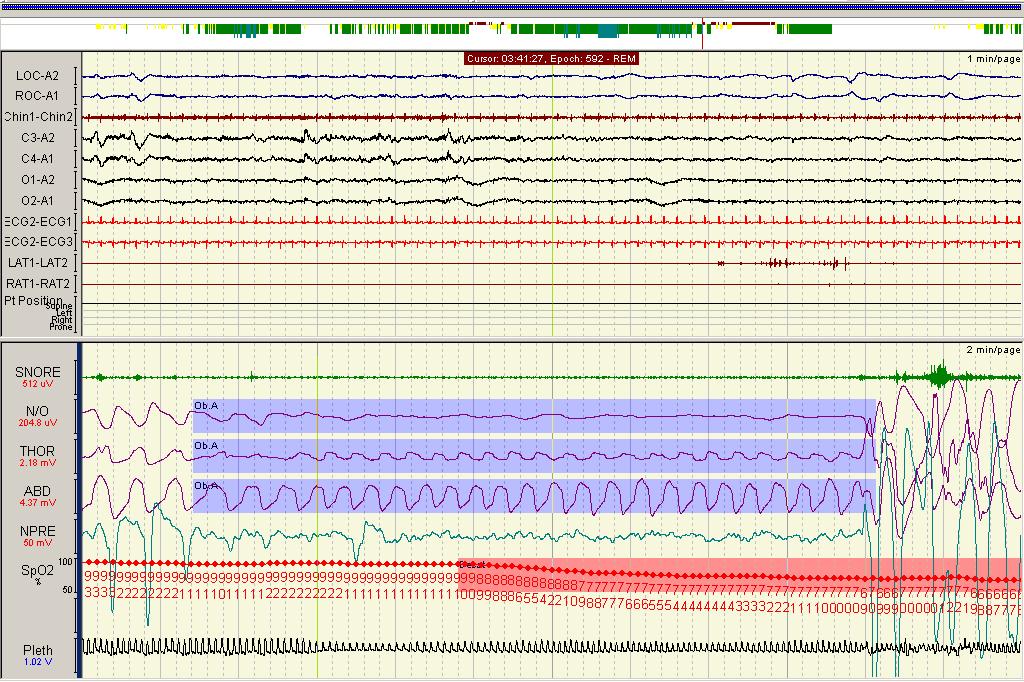
261
MEDICARE
0 50,000 100,000 150,000 200,000 250,000 300,000 350,000 400,000 2011 2012 2013 2014 2015 2016 2017 Medicare Claims Year HSAT PSG PSG w PAP American Medical Association RVS Update Committee (2018). RUC Database 2018 version 2. 262
CLAIMS 2011-17
THE RISE OF HOME TESTING
• Home Sleep Apnea Testing is:
• Cheaper
Convenient for patients
• Comparably effective in assessing OSA
• Downsides:
• Error rate (pos/neg)
• Fail rate
• Limited assessment (OSA only)
•
263
Patient presents to BCSS for eval. of suspected OSA
Does the patient have a high pretest probability of moderate to severe OSA?
Evaluate for other sleep disorders; consider in lab PSG
Does the patient have symptoms or signs of co-morbid medical disorders?
Does patient have symptoms or signs for co-morbid sleep disorders?
Sleep Study (PM or in-lab PSG) PM In-lab PSG OSA Diagnosed? Treatment No No No No Yes Yes Yes Yes No
264
2007 PM Flow Chart
Patient presents to Sleep
Clinician for eval. of suspected OSA
2023 HSAT Flow Chart
Does the patient have a high pretest probability of moderate to severe OSA?
Does the patient have symptoms or signs of co-morbid medical disorders?
Does patient have symptoms or signs for co-morbid sleep disorders?
HSAT OSA Diagnosed? Treatment No No Yes Yes Yes Yes No
No
(vs. Clinical Follow up) 265
PSG
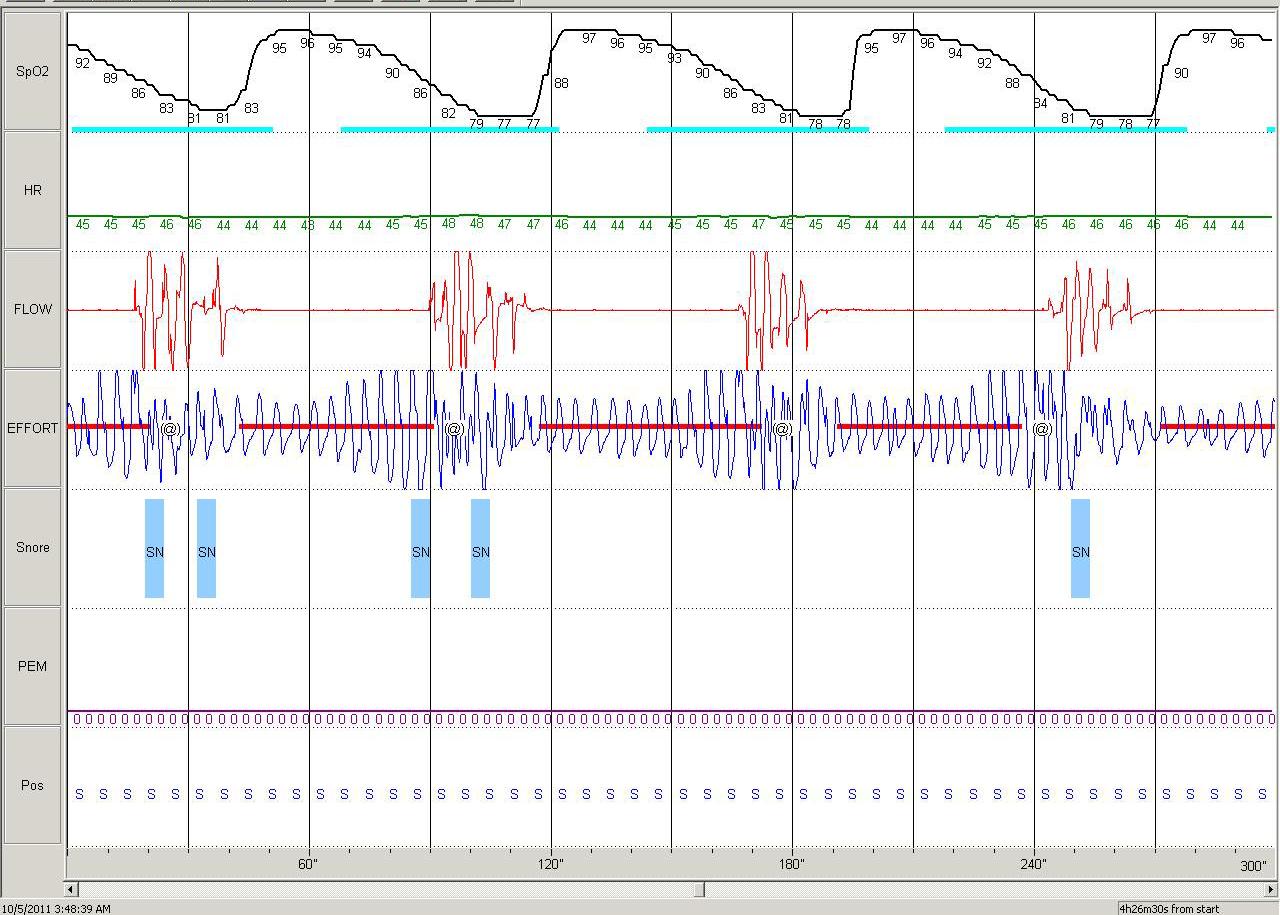
266
STARDUST II: OSA – 5 MIN
Growing volume over time
SO…
Geared for patients with straight-forward symptoms
Gated by Authorization companies, with increasing complexity of patients getting HSAT
•
•
Home Sleep Apnea Testing
•
•
267
HSAT performed on fairly healthy straightforward patients
HSAT PEELS OFF THE STRAIGHTFORWARD PATIENTS
Higher percentage of Complex/Sick patients In Sleep Laboratories
268
Mayo Clinic Center for Sleep Medicine from 2005 to June 2015 to calculate the Charlson and the Elixhauser comorbidity indices.
•
(1) in a subset of patients from the past 2 months of 2015, we evaluated correlation of these morbidity indices with an internally developed Polysomnogram Clinical Index (PSGCI) rating anticipated patient care needs from 0 to 3
•
(2) we measured the sleep study complexity based on polysomnography protocol design.
•
COLACO ET AL, JCSM 2018
269
COLACO ET AL, JCSM 2018


270
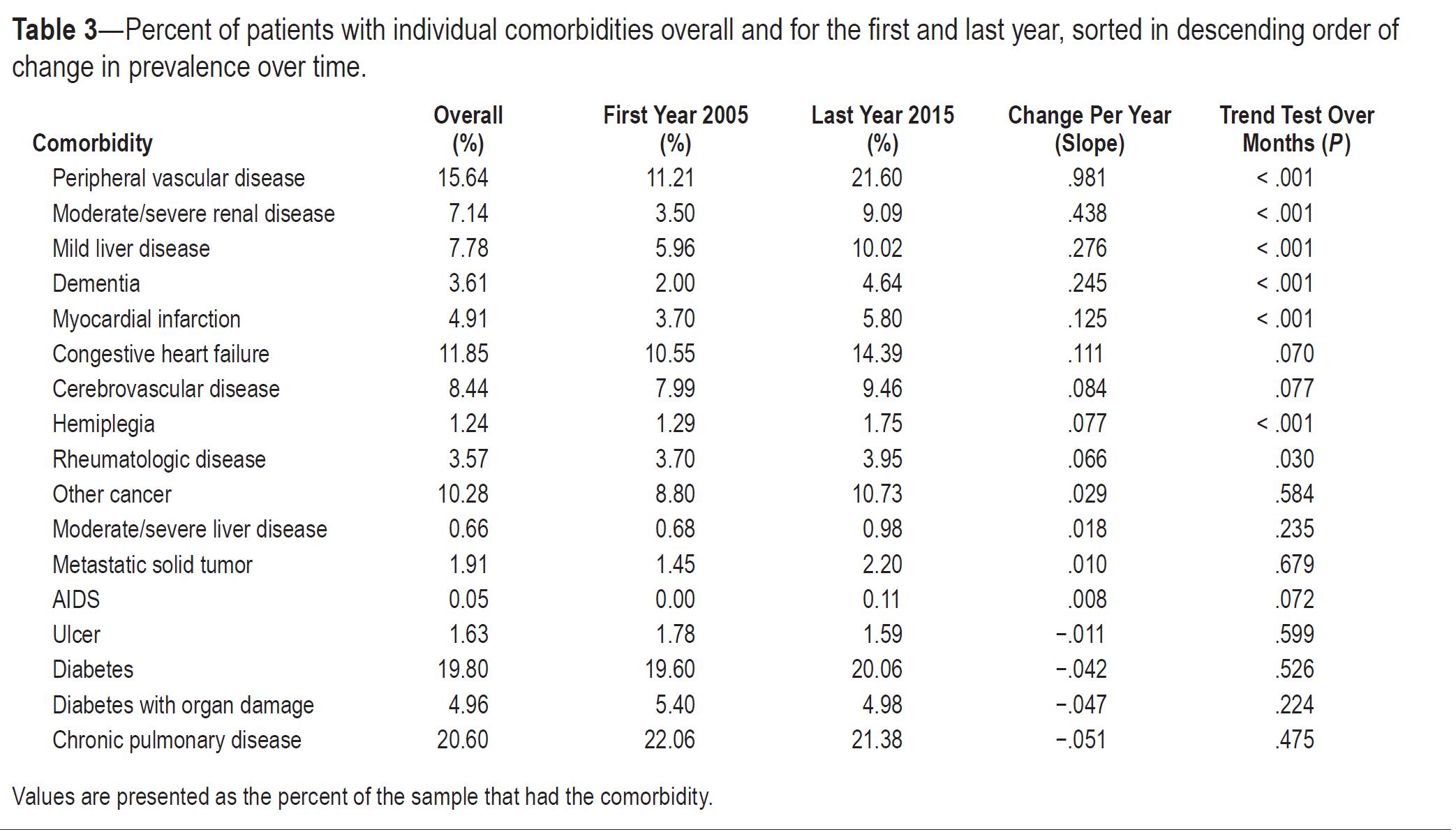
2018 271
COLACO ET AL, JCSM
COLACO ET AL, JCSM 2018
• Results: In 43,780 patients studied from 2005 to June 2015, the Charlson index increased from a mean of 1.38 to 1.88 (3.1% per year, P < .001) and the mean Elixhauser index increased from 2.61 to 3.35 (2.5% per year, P < .001). Both comorbidity indices were significantly higher at the highest (Level 3) level of the PSGCI (P < .001), and sleep study complexity increased over time.

272
Medicare patients without prior authorization -> higher percentage of PSG
HSAT USE IS TYPICALLY LESS IN PATIENTS WITH MEDICARE
Complex/Sick patients In Sleep Laboratories
273
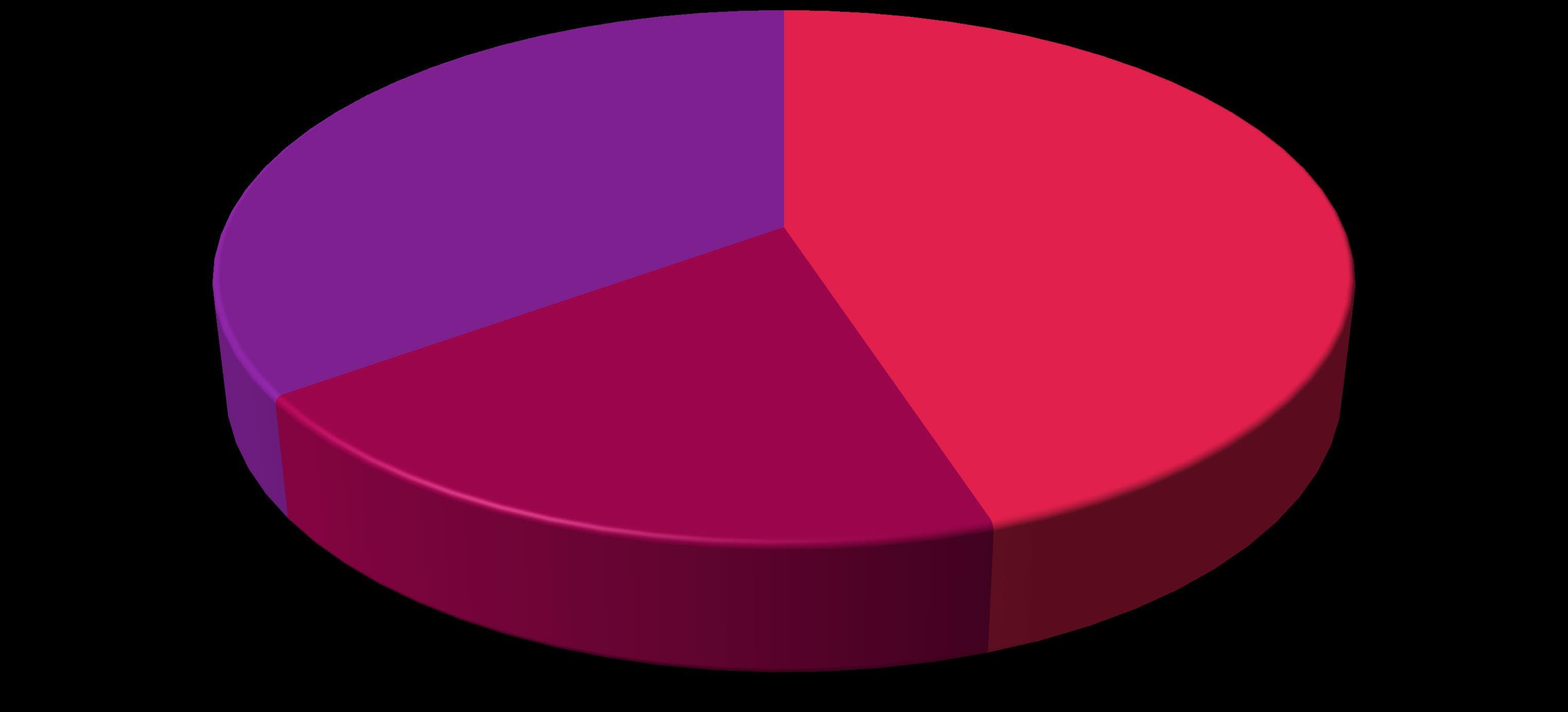
% OF PSG – 2022 ATRIUM HEALTH 274
Medicare Medicaid Commercial
Increasing awareness of comorbid disease linked with sleep disorders: For instance, Cardiology
CO-MORBID CONDITIONS
Sick/Complex patients In Sleep Laboratories
275
HSAT reveals Central Sleep Apnea Or Hypoventilation
COMPLEX HSAT RESULTS
Complex/Sick patients In Sleep Laboratories
276
HSAT Failure
HSAT FAILURE
Complex(?) patients In Sleep Laboratories
277
SICK PATIENTS FROM HOSPITAL
Post-hospital transfer patients needing positive airway devices
Sick/Complex patients In Sleep Laboratories
278
• New HSAT and PSG Rules (3% hypopneas as primary scoring mechanism)->
Fewer “Failures” of HSAT
• But higher number of false positives https://31.media.tumblr.com/687b7352a99961cb35cd92da9f39015a/tumblr_inline_nboumj5ZO61qersu1.png

THIS COMPLEXITY?
WILL RECENT SCORING RULES CHANGE AFFECT
279
STEPS TO MITIGATE RISK / IMPROVE SAFETY
280
FLYING IS SAFE
• Aviation is the safest form of long distance transport. •
In 2018, the all accident rate (measured in accidents per 1 million flights) was 1.35, which was the equivalent of one accident for every 740,000 flights. This was an improvement over the all accident rate of 1.79 for the previous 5-year period (2013-2017).
• Concretely, the 2018 fatality risk of 0.17 means that on average, a person would have to travel by air every day for 16,581 years to experience a 100% fatal accident.
https://www.iata.org/en/youandiata/travelers/aviation-safety/
281
WHY IS FLYING SAFE?
• Regulations • Training • Certification • Checklists • Data Tracking / Evaluation • Accidents/Errors with in-depth evaluation 282
• the American Academy of Sleep Medicine (AASM), or
• the Accreditation Commission for Health Care (ACHC), or
• the Ambulatory Care Accreditation Program of the Joint Commission https://www.cms.gov/medicare-coveragedatabase/view/article.aspx?articleId=55958&ver=4#:~:text=The%20sleep%20center%20or%20laboratory,Program%20of%20the%20Joint%20Com
•
ACCREDITATION -> SAFETY IN THE SLEEP LABORATORY
1) Accreditation (Regulations)
mission 283
RELEVANT STANDARDS FROM AASM
• Facility Directorship – board certified, responsibilities, continuing education requirements
• Staff – Interpreting MD, Technologist – training and continuing education requirements
• Background checks: the facility shall conduct criminal background checks of all new employees
284
RELEVANT STANDARDS FROM AASM
• Review of Direct Referrals: facility director or appropriately licensed medical staff member must review the information provided for each patient -This should include a history and physical received from the referring clinician
• D-7 Testing Bedrooms & Emergency Care: Patient testing bedrooms must not have any impediments to the delivery of emergency care. The patient testing rooms:
• 1. Must be of sufficient size to accommodate emergency personnel access with a minimum of 24 inches of available clear space on three sides of the bed; and
• 2. Must include a testing bed with a mattress not smaller than a standard hospital bed.
285
RELEVANT STANDARDS FROM AASM
• D-12 Video Recording: The facility must have continuous visual monitoring and video recording of patients during testing. Time-delayed photographs will not be considered compliant with this standard.
• E-5 Equipment Maintenance & Procedures:
• Written plan for monitoring of all in-lab and HSAT patient-related equipment for electrical and mechanical safety
• Written procedure for infection control including cleaning and inspecting all patient-related equipment; this includes sterilization, high-level disinfection, or the application of germicidal agent
286
RELEVANT STANDARDS FROM AASM
• I-1 Emergency Plan
• An emergency plan must be accessible in paper or electronic format delineating the following:
• 1. Mechanisms and specific details for contacting emergency personnel;
• 2. The facility personnel to be contacted in an emergency; and • 3. Specific responsibilities of the medical and technical staff.
• Emergency policies must include policies and procedures for the following:
• 1. Cardio-pulmonary emergencies with equipment required in Standard I-4
• 2. Neurologic emergencies, particularly seizures and strokes
• 3. Psychiatric emergencies, particularly suicidal ideation
• 4. Environmental emergencies including fire, weather, belligerent patients, and bomb threats
287
RELEVANT STANDARDS FROM AASM
I-2 HSAT Emergency Procedure: The facility must instruct the patient to call emergency services (911) in the event of an emergency during a HSAT.
I-3 Emergency Drills: Facilities must conduct and document drills of their emergency procedures on an annual basis. At a minimum, the facility conducts and documents annual drills of their response to cardio-pulmonary emergencies.
I-4 Emergency Equipment: Facilities must have appropriate equipment to address possible emergencies. At a minimum, all facilities must have either an automated external defibrillator (AED) or access to an on-site medical emergency response team. The facility maintains and documents the maintenance of all emergency equipment according to manufacturers’ recommendations. The facility maintains and documents training of personnel on emergency equipment.
•
•
•
288
RELEVANT STANDARDS FROM AASM
• Facilities using hospital code teams may use hospital-based policies for medical emergencies.
• STANDARD I-2 HSAT Emergency Procedure” The facility must instruct the patient to call emergency services (911) in the event of an emergency during a HSAT.
• STANDARD I-3 Emergency Drills: Facilities must conduct and document drills of their emergency procedures on an annual basis. At a minimum, the facility conducts and documents annual drills of their response to cardio-pulmonary emergencies.
• STANDARD I-4 Emergency Equipment: Facilities must have appropriate equipment to address possible emergencies. At a minimum, all facilities must have either an automated external defibrillator (AED) or access to an on-site medical emergency response team. The facility maintains and documents the maintenance of all emergency equipment according to manufacturers’ recommendations. The facility maintains and documents training of personnel on emergency equipment.
289

290
SLEEP LABORATORY REFERRAL PROCESS
• The presence of 1 of these factors or conditions on the electronic order prompted triage to the hospital-based Beth Israel Deaconess Hospital Needham sleep laboratory, which was identified as having increased medical support.
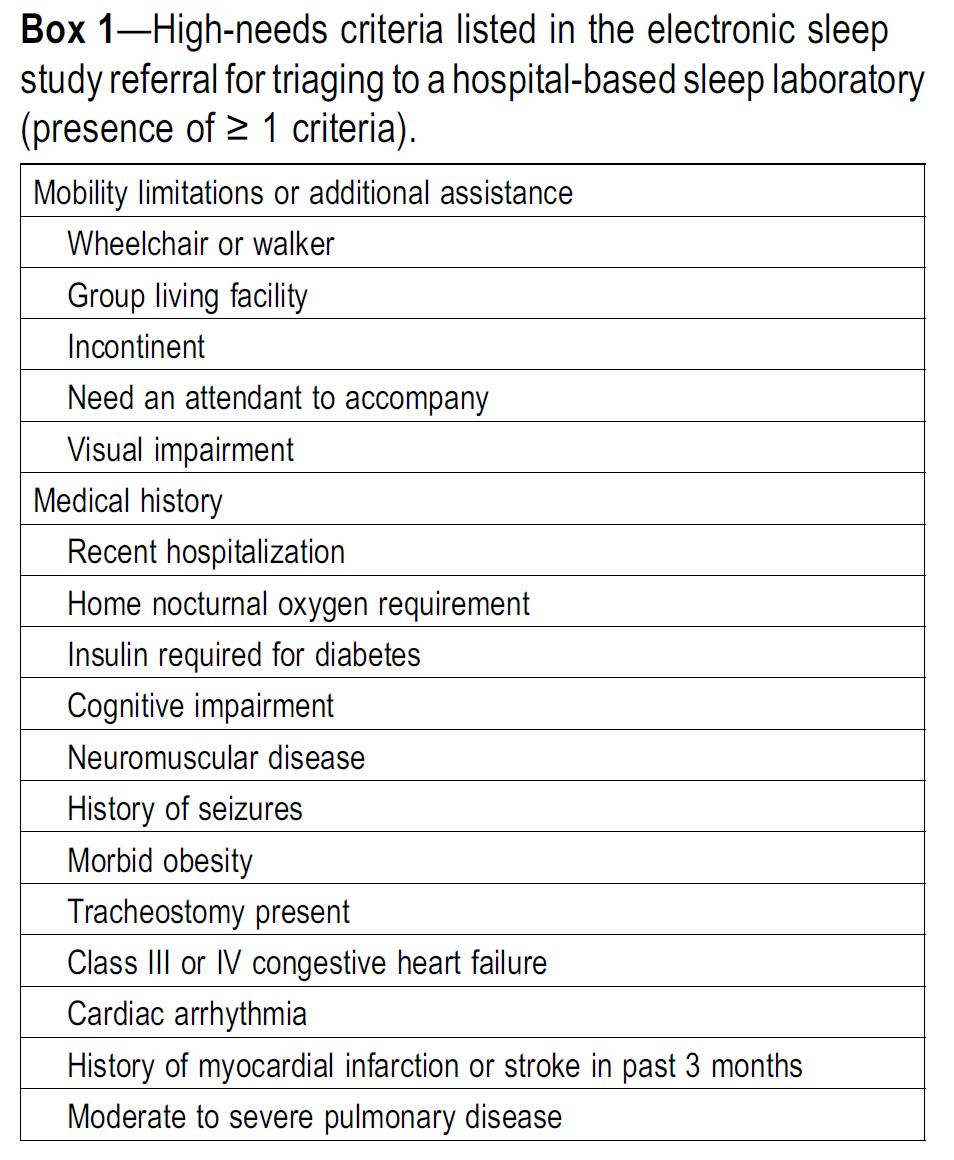
291
BI POLICIES
• Sedative use policy: This policy explicitly instructed patients to take their sedative medication by 10:30 PM and stated that if a sedative was to be used for the first time during the sleep study, then the patient was encouraged to arrange a ride home the morning following the study.
• Engaging the hospitalists and the RR and code teams: Implementation of protocols was coordinated with the hospital’s RR and code teams to delineate responsibilities of the RR or code teams and the sleep technicians. This included designating a location and maintaining a code cart within the sleep laboratory.
• Clinical symptom screening and triage upon arrival to the sleep laboratory
292
BI POLICIES
• Technician performed prestudy vital signs assessment using an automated blood pressure cuff and oximeter and administered a prestudy clinical symptom questionnaire.
• Acceptable baseline blood pressure and oximetry ranges as well as actions for vital signs that are out of range were explicitly defined in a “Take Quick Action” triage sign
• The prestudy questionnaire identified high-risk conditions as well as acute symptoms within the past 24 hours
• Sleep technicians were instructed to call the RR team for chest pain, shortness of breath, fall, seizure, stroke symptoms, voiced intent for self-harm,marked concern by patient or family member, or vital sign abnormalities (heart rate > 120 beats per minute for 2 minutes, wake SpO2 < 90%, systolic blood pressure < 90 mm Hg or > 200 mm Hg).
• Sleep technicians were instructed to call the code team for cardiac arrest or difficulty arousing the patient.
• Other concerns were directed to the sleep physician on call. All incidents were reported to the sleep physician in the morning and communicated to the referring clinician.
293
BI INCIDENTS
• Over the study period of January 2016– January 2020, there were 9,558 total inlaboratory polysomnograms completed. With 65 events reported over this time, the incidence of safety incidents was 1:147 for all in-laboratory sleep studies performed.
• The most common events were symptoms of chest pain (20/65, 31%) and shortness of breath (13/65, 20%).


294
CONCEPTS WORTH CONSIDERING
• Emergency training was implemented for all sleep technicians and included:
• An annual review of emergency procedures
• An annual review of electrocardiographic tracings and causes of respiratory distress
• Creation of an advanced electrocardiographic skills training program
• Creation of a script for how technicians should respond in an emergency with a review of scenarios
• Creation of a specific tracheostomy prestudy form.
295
https://pestleanalysis.com/examples-of-pestle-analysis/

EXAMPLES/RESPONSES
296

10 SEC 297
SCREENSHOT 1 –
SEIZURE PROTOCOL – THE
3 S MODEL
• STAY -Stay with the person during the seizure and until they are awake and alert
• Time the seizure
• Remain calm and reassuring
• SAFE – Keep the person safe away from objects (bedside stand, etc )
• SIDE – Turn the person onto their side if they are not awake or aware
• Do NOT:
• Put anything in the patient’s mouth
• Restrain the patient
298
WHAT TO DO WITH THIS 30S SEGMENT?
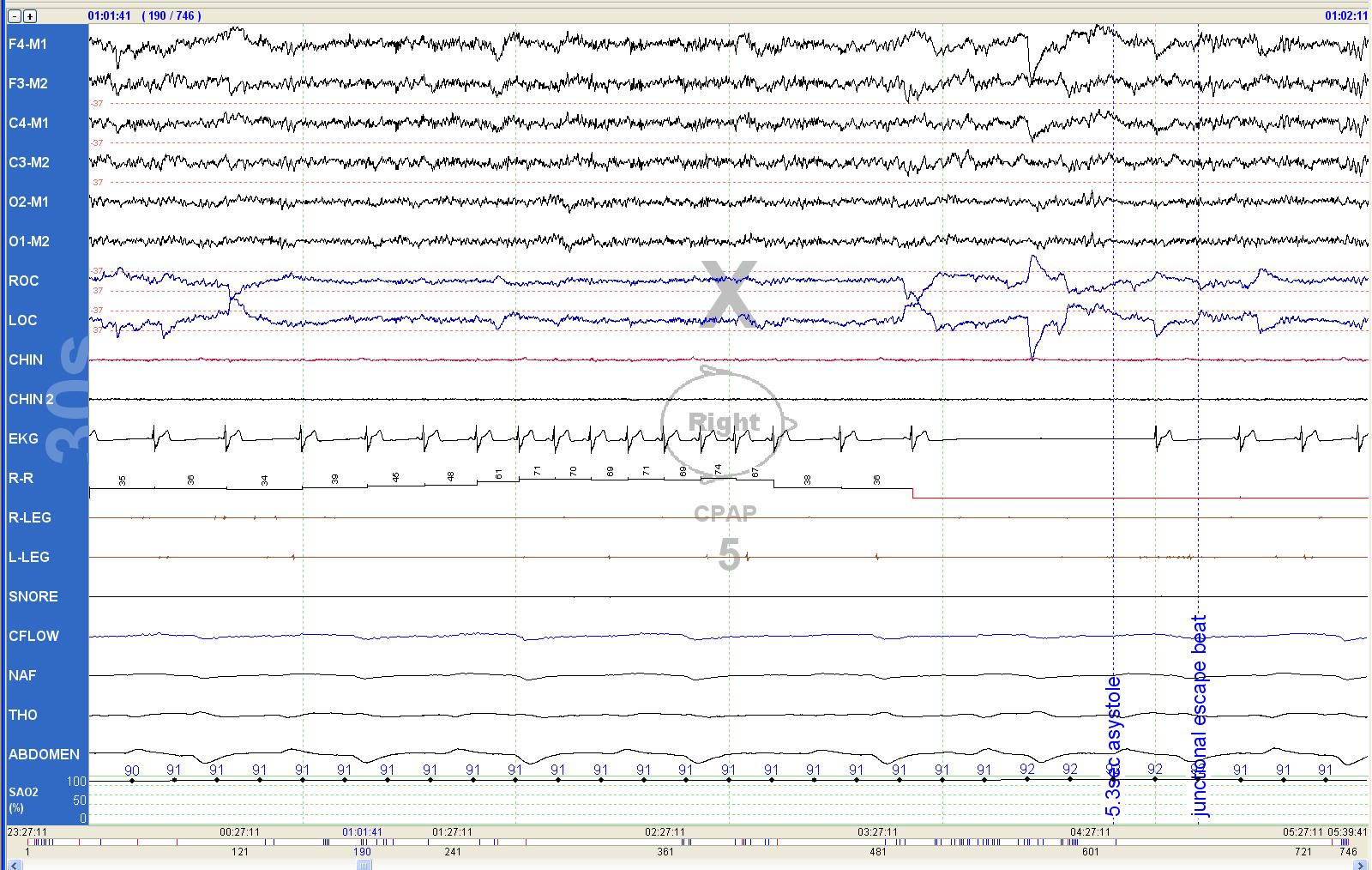
299
WHAT TO DO WITH THIS 30S SEGMENT?

300
Call EMS/Alert:
EKG PROTOCOLS - EMERGENT
Ventricular Tachycardia (sustained > 30 seconds)
Ventricular Fibrillation/Flutter (sustained > 30 seconds)
Asystole (sustained > 10 seconds)
301
EKG PROTOCOLS - URGENT
Call Physician at Nighttime:
Ventricular Tachycardia non-sustained (< 30 seconds) (greater than 4 beats)
Ventricular Fibrillation/Flutter non-sustained (<30 seconds)
Third Degree AV Block
Atrial Fibrillation / Flutter (if no prior history)
Sustained Sinus Tachycardia (rate > 120 bpm)
Asystole or pause >3 sec.
302
EKG PROTOCOLS - ATTENTION
Note to Physician in the AM:
High density PVC’s
Sustained Bradycardia (rate < 40)
Frequent Couplets or Triplets
Bigeminy
Trigeminy
Quadrageminy
Second Degree AV Block (Type I and II)
303
FROM THE SCORING MANUAL 3.0
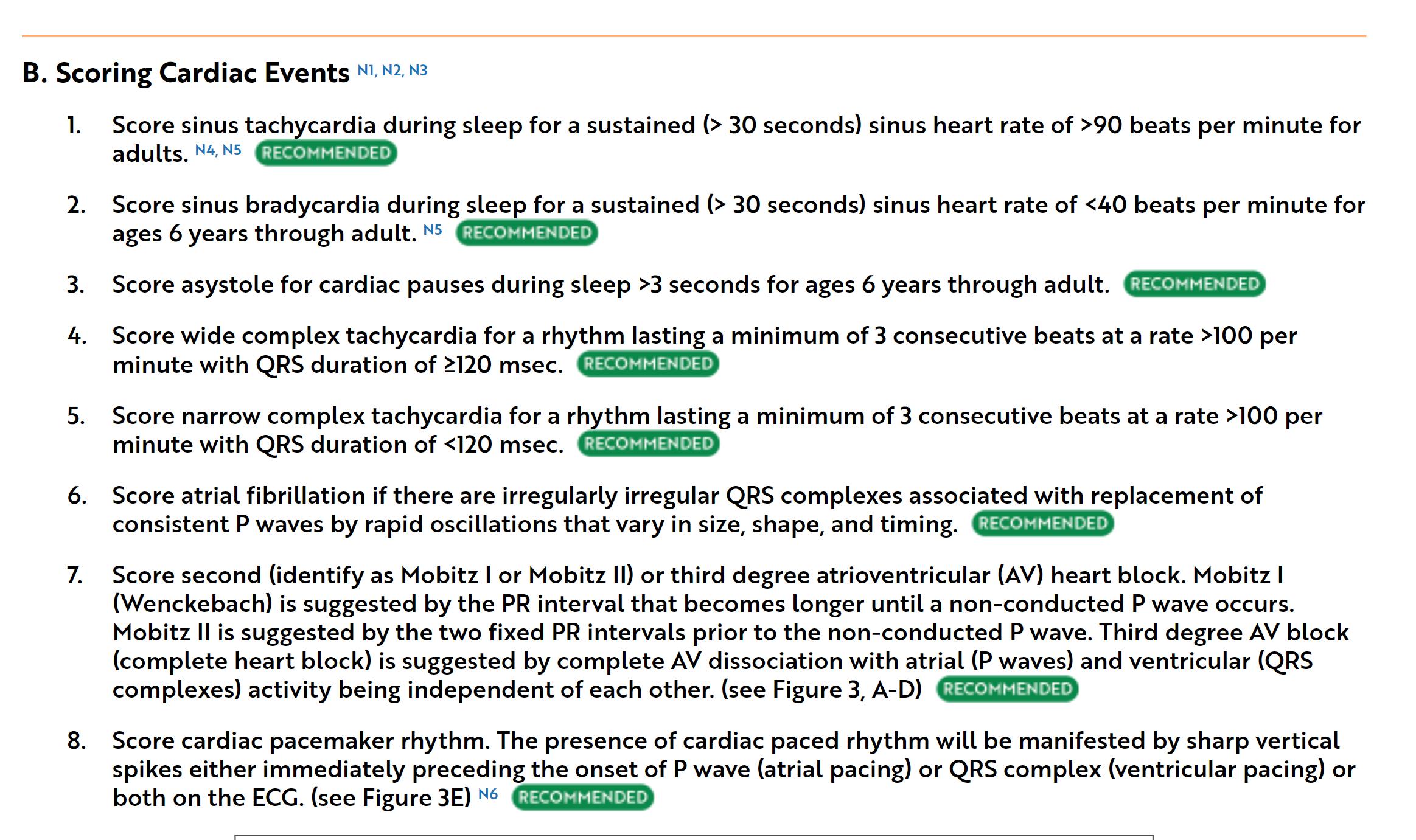
304
FROM THE SCORING MANUAL 3.0
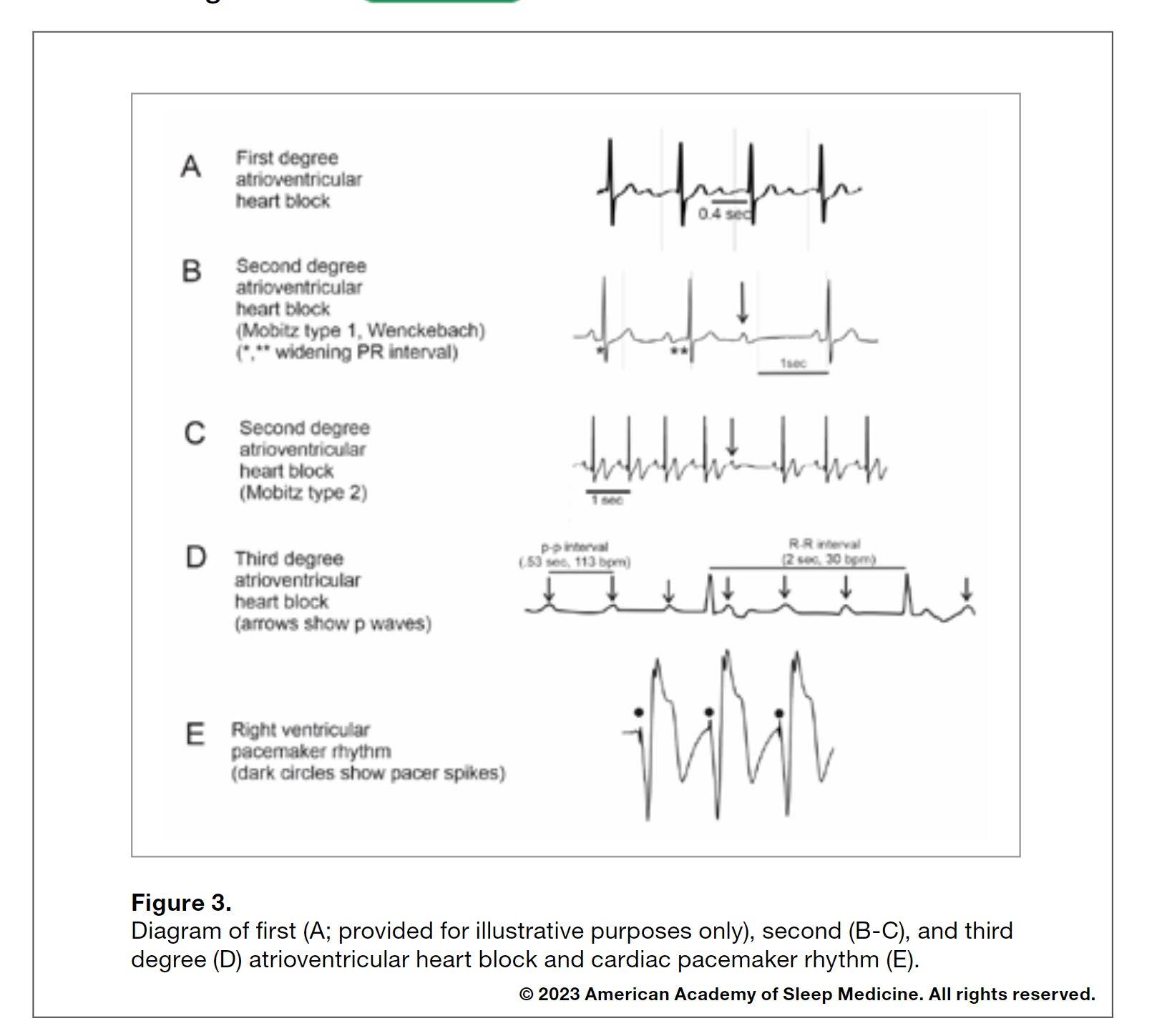
305
FOR THE ON-CALL CLINICIAN
• Patient has a prior history of arrhythmia
• If VS are stable and patient has no complaints, proceed with study
• Call referring MD next AM and describe event
• If symptoms or unstable or recurs
• – transfer to ED
• If patient has no history of arrhythmia
• Must use clinical judgement; if VS are stable and patient has no complaints, can usually proceed with study
• If symptoms or unstable – t ransfer to ED
• Call referring MD next AM and describe event
306
o A Fall Risk assessment is completed for each sleep center procedure.
o Patients scoring 4 or higher on the fall risk assessment are considered at high risk for falls.
o The “Fall Reduction Strategies” must be completed on all patients scoring 4 or higher on the Fall Risk Assessment.
Fall Reduction Strategies
o Review all appropriate items on the Fall Reduction Patient Education document with all patients identified as being at high risk for falls as indicated by a score of 4 or greater on the fall risk assessment. Check off each item as you review the item with the patient.
o Post a Fall Risk sign on the bedroom door, this will aide your co-workers in identifying your patient as a fall risk if they need to assist your patient during the night.
FALLS
•
307
SUMMARY
• Major health issues in the Sleep Laboratory are thankfully uncommon
• However, they may become more common with increasing patient complexity
• Continuously reviewing protocols with ongoing i mprovement of risk assessment/training is necessary to have optimal outcomes
308
DOUGLAS.KIRSCH@ ATRIUMHEALTH.ORG
309
AND….


310







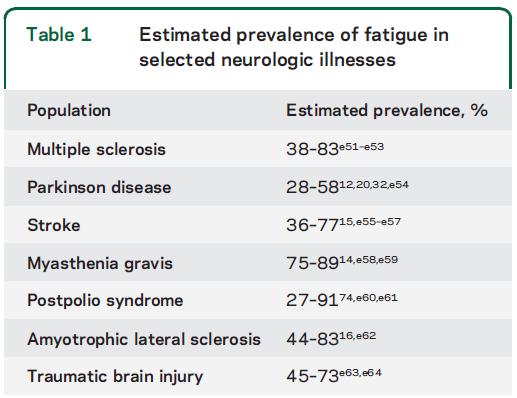
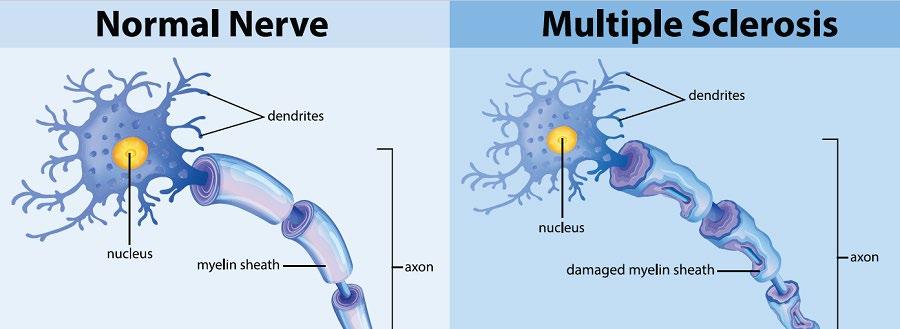





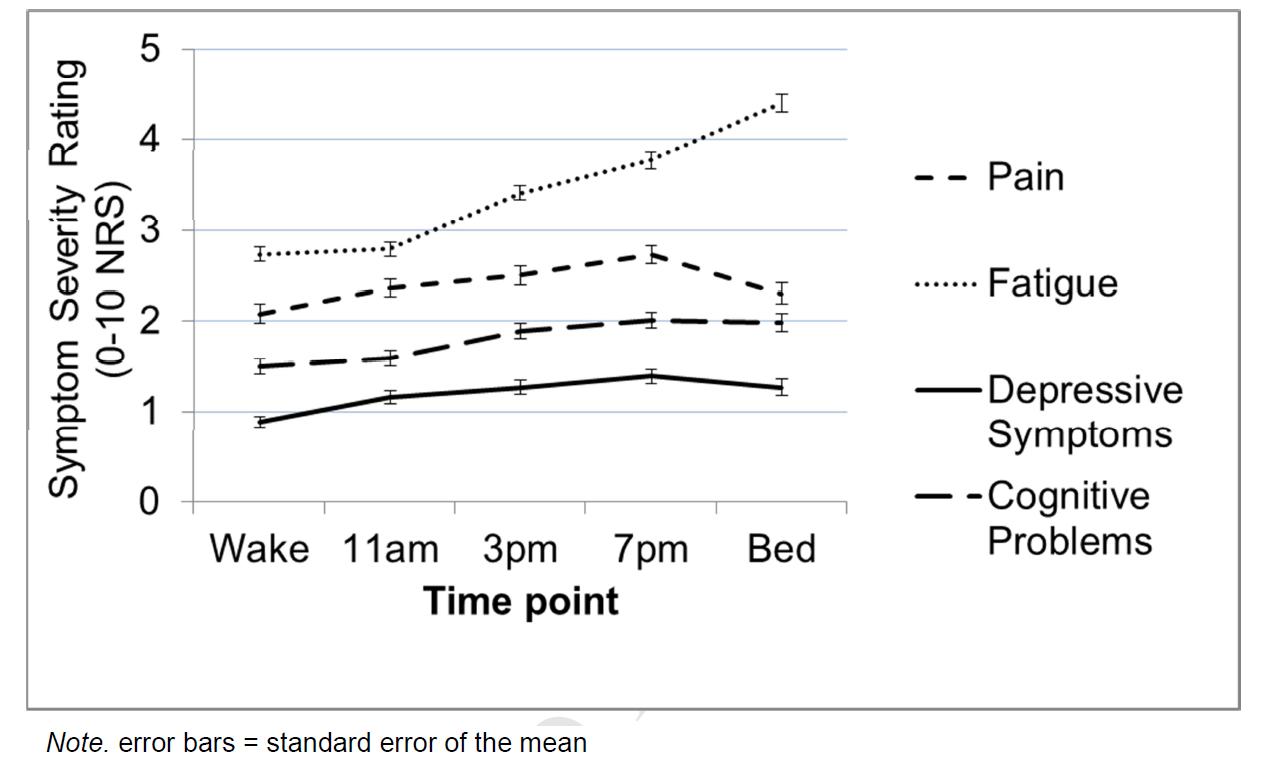





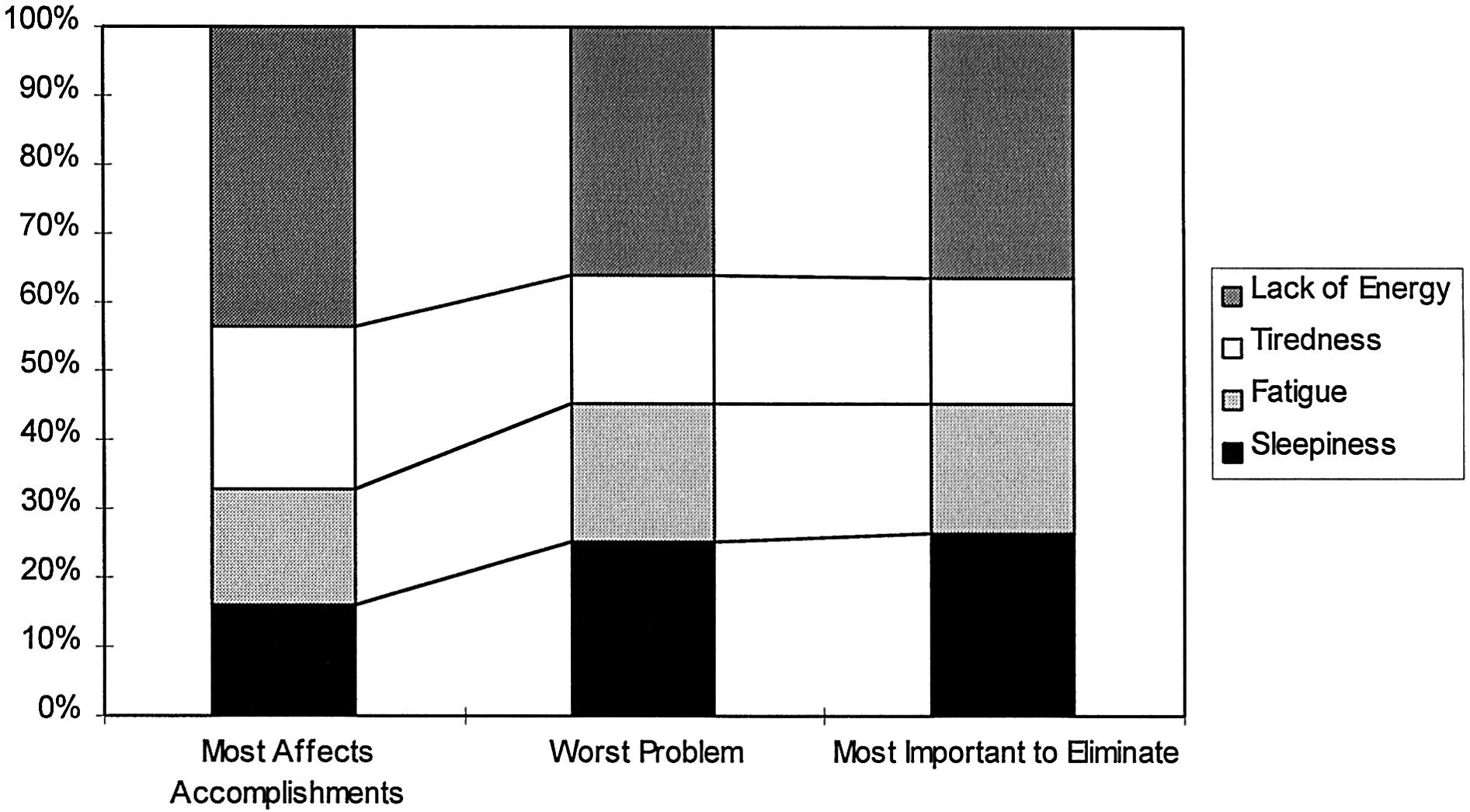
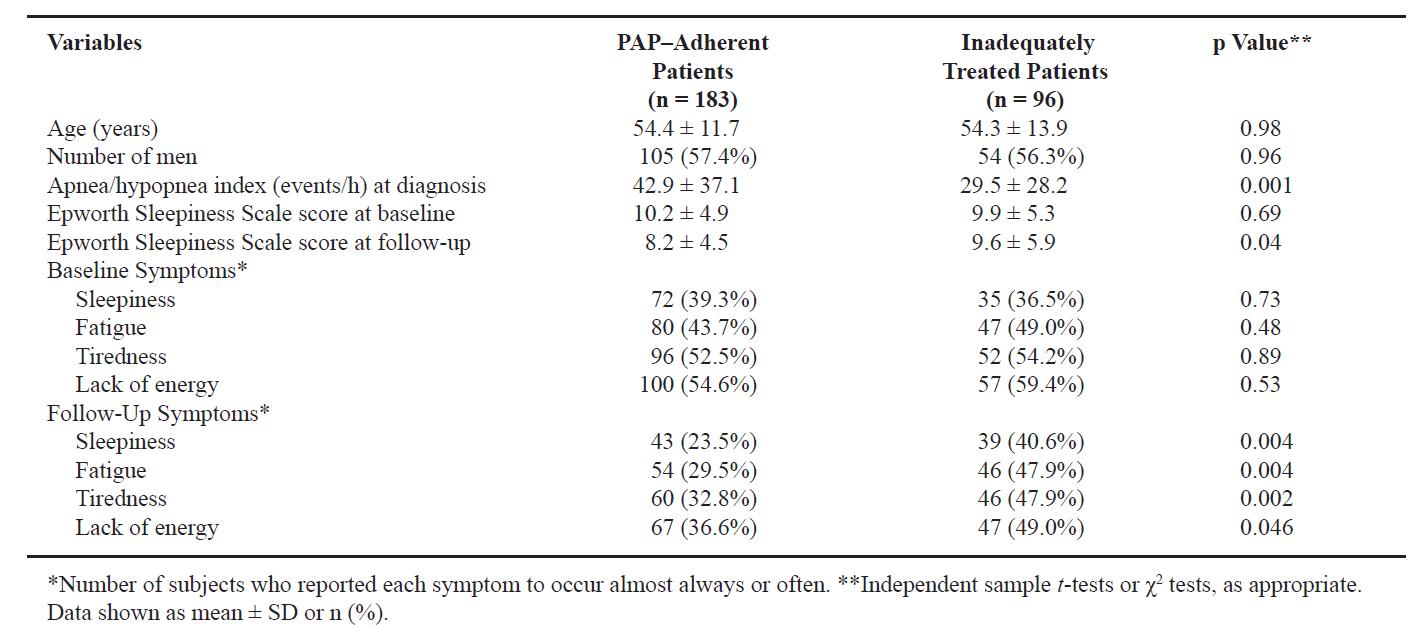







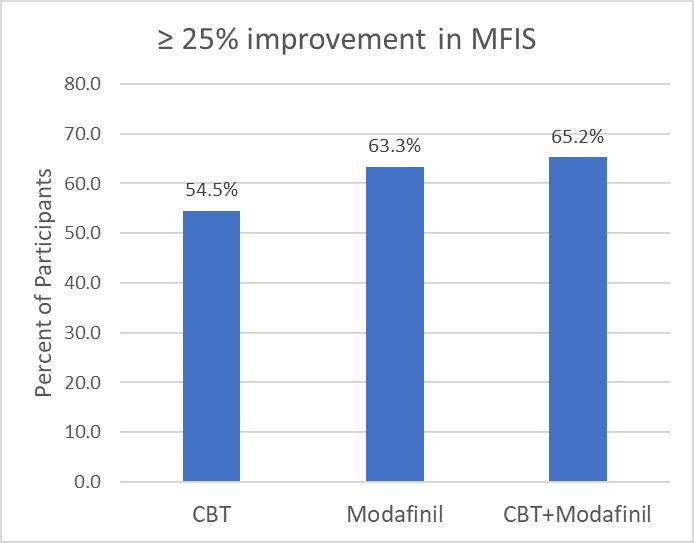

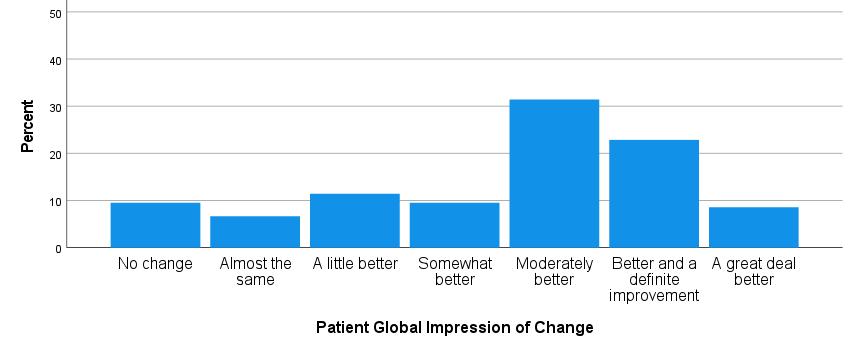

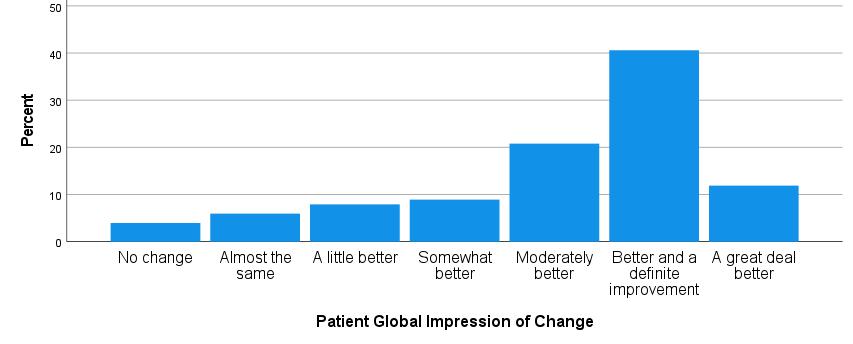
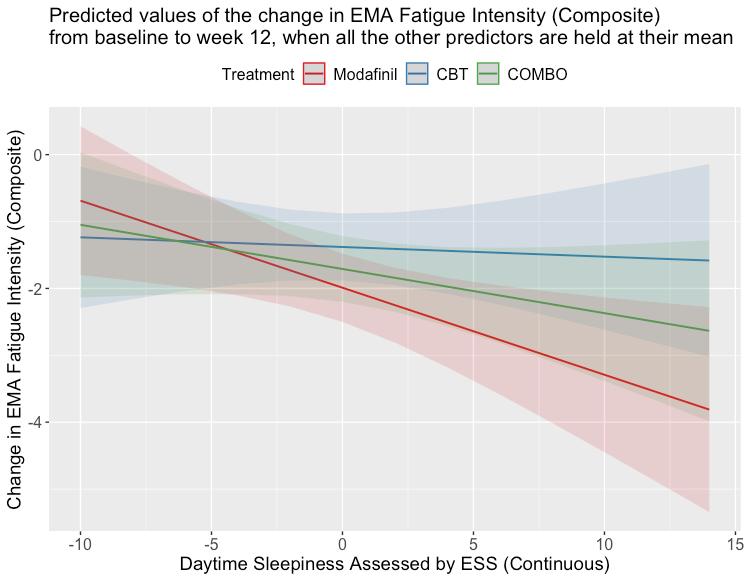

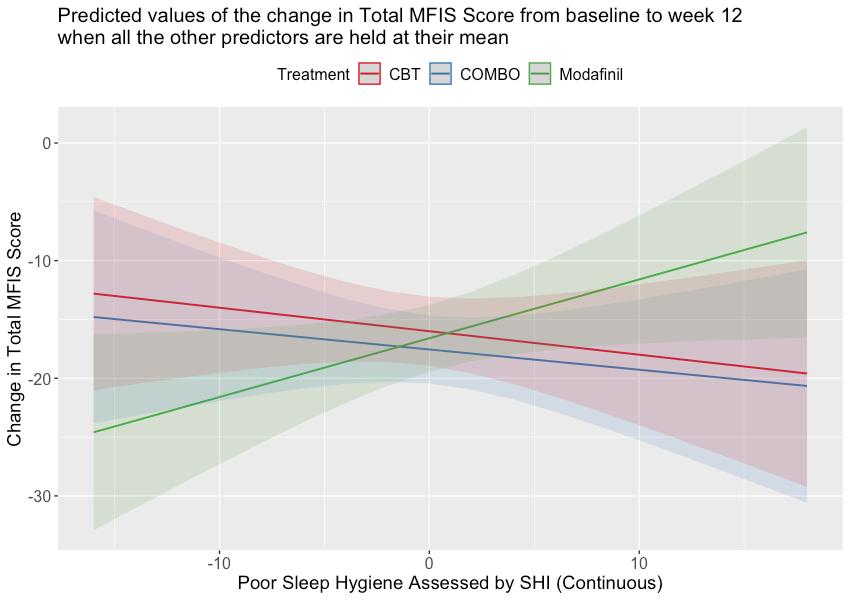





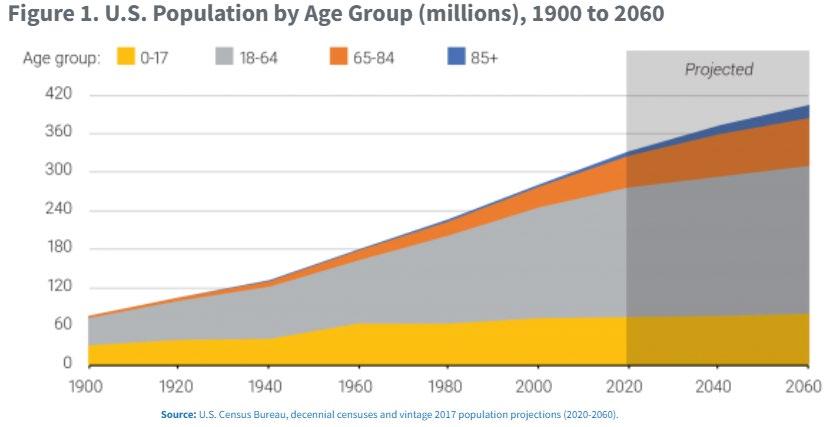



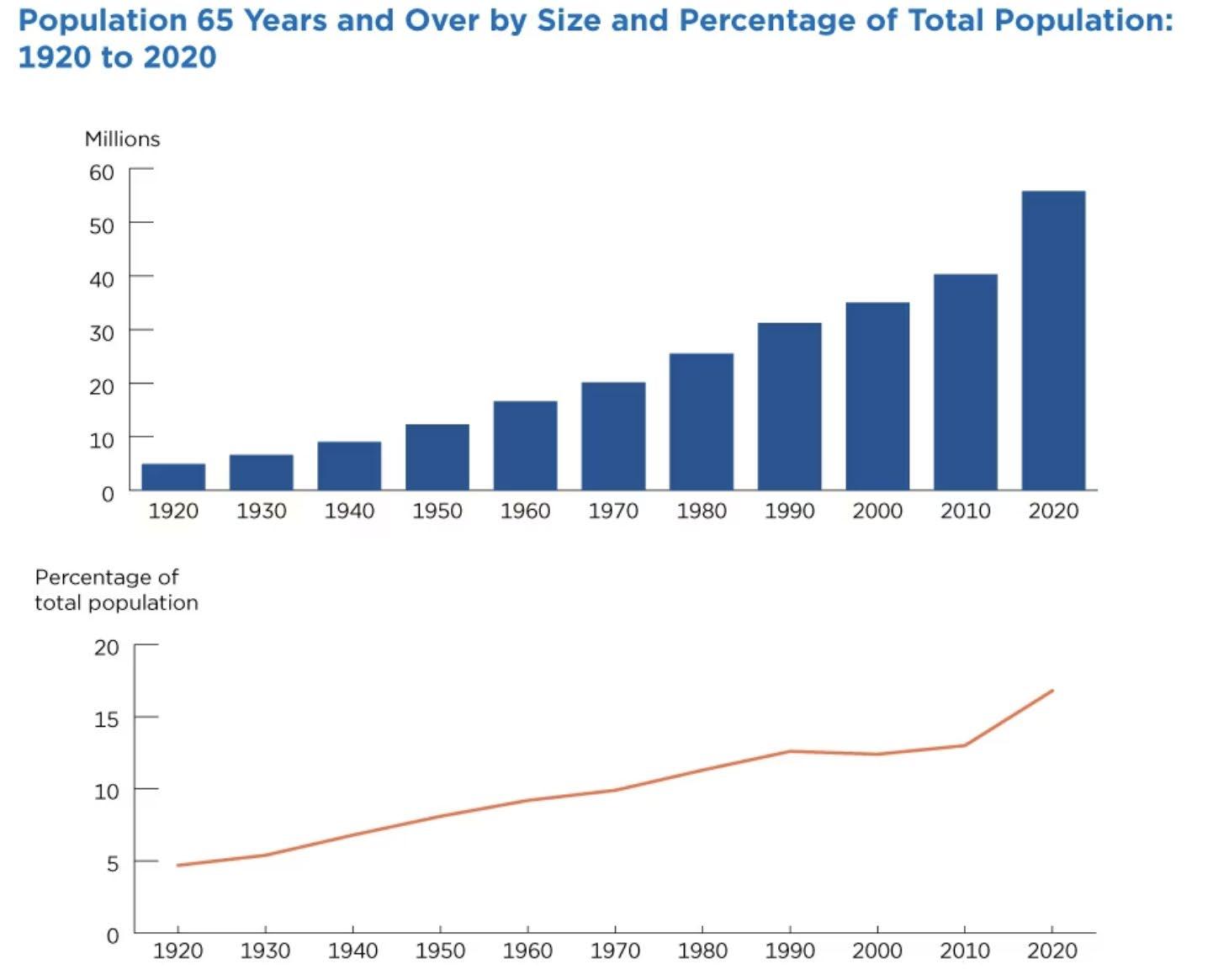

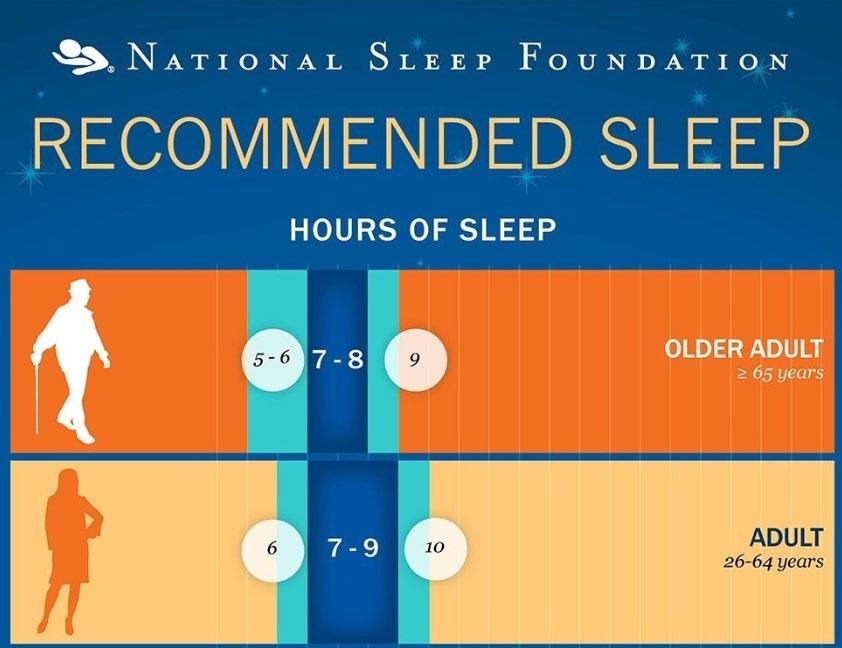

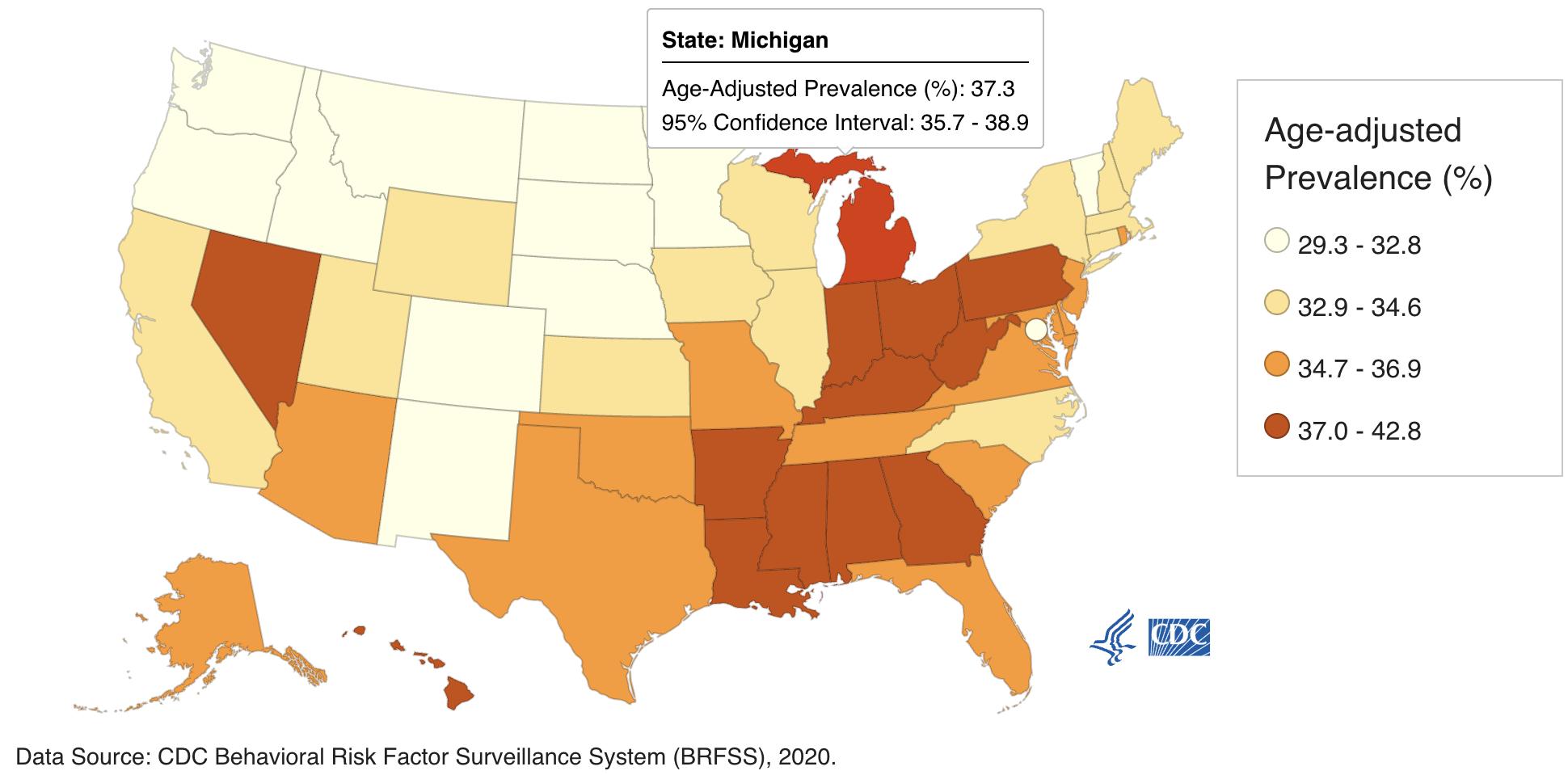

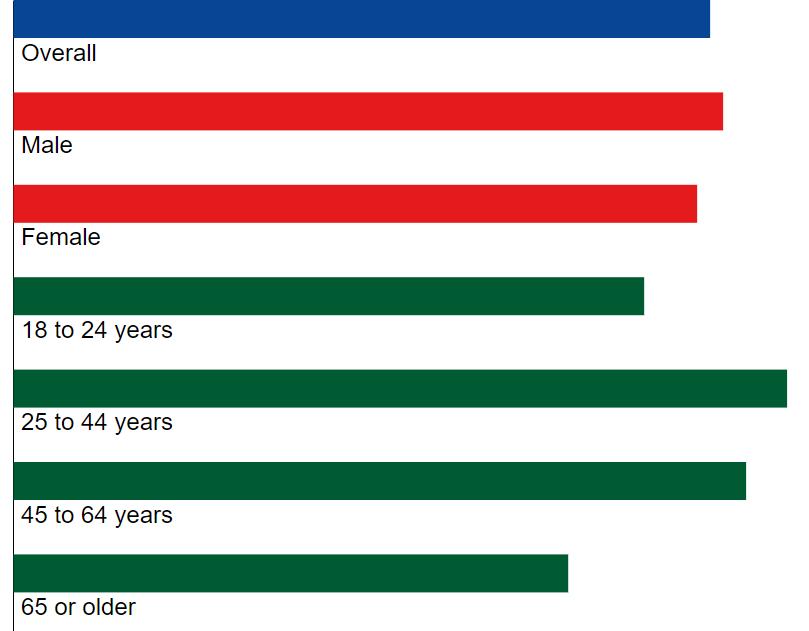
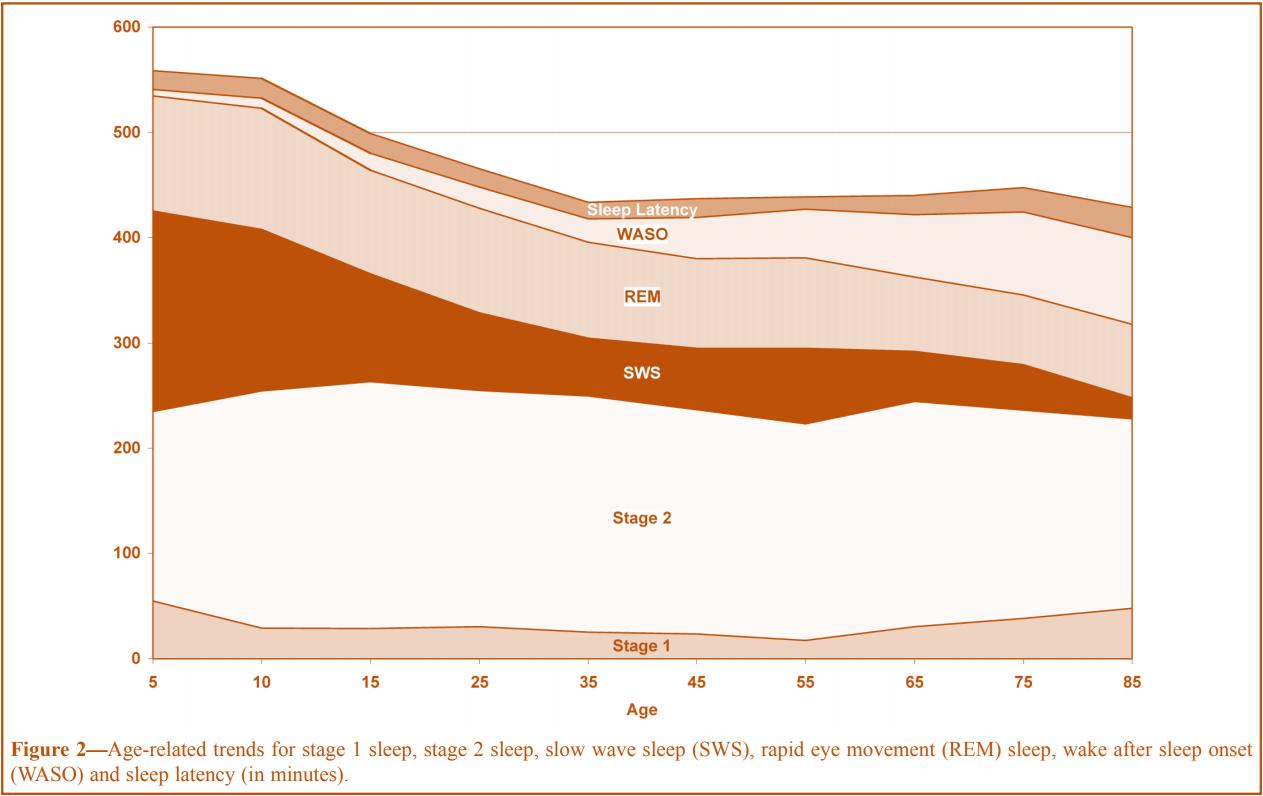

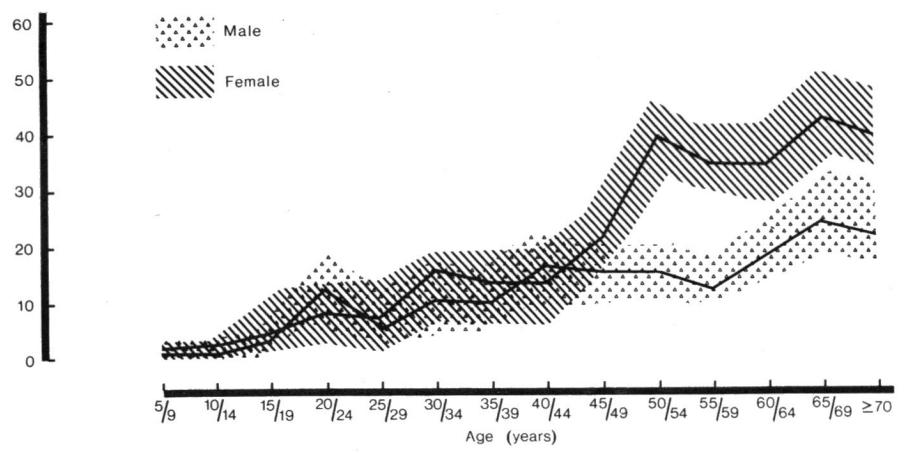
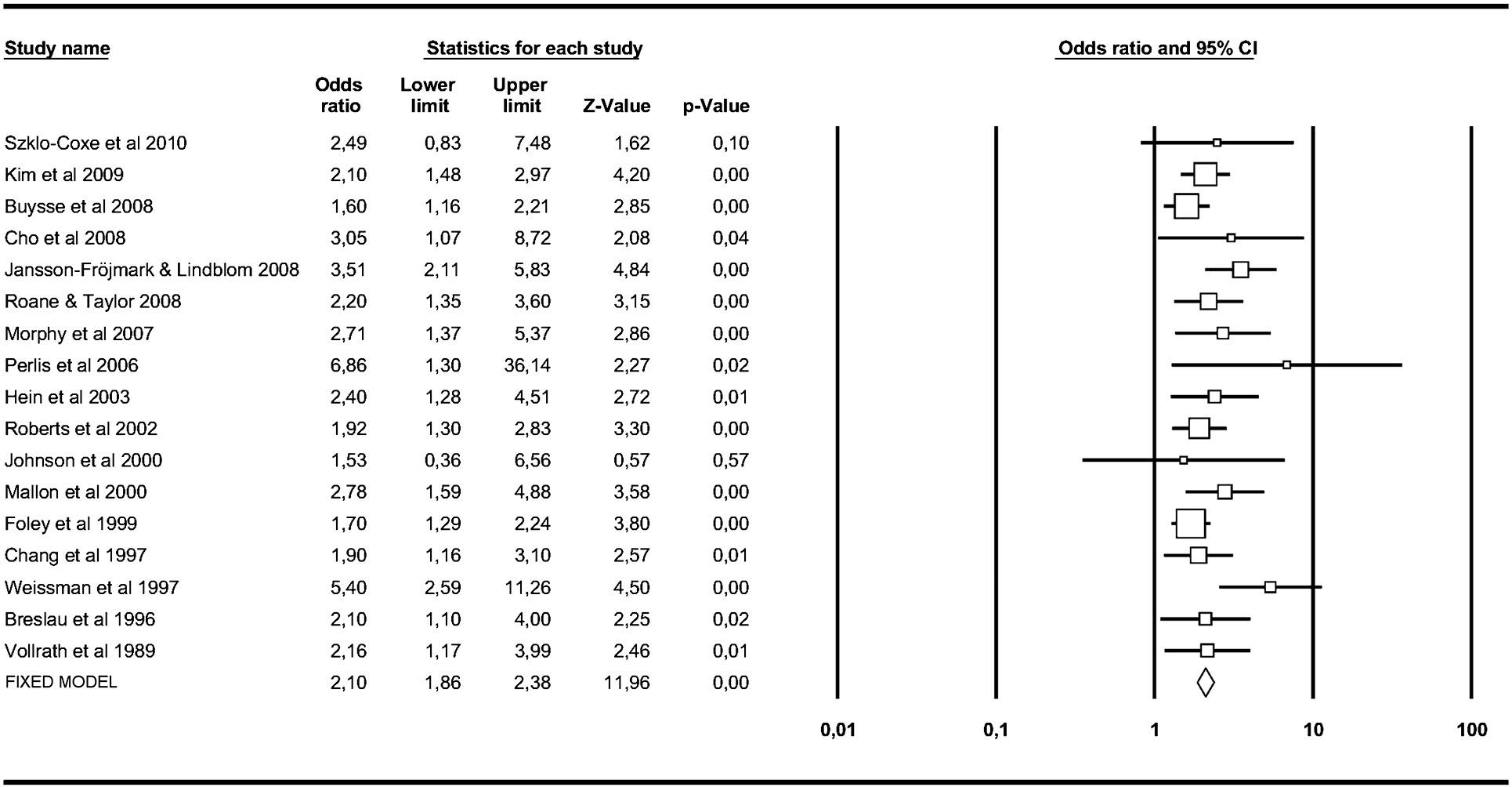
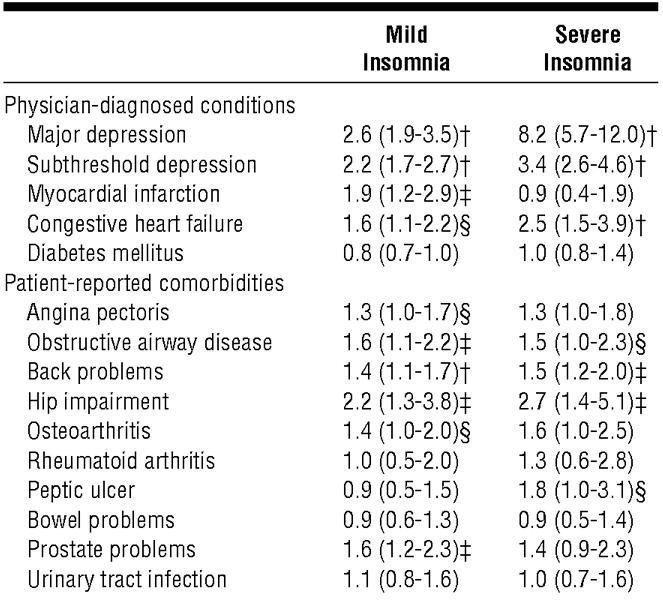







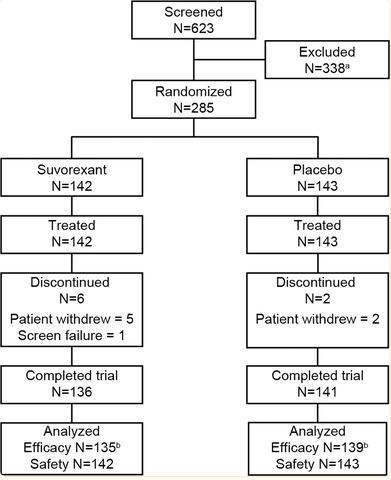

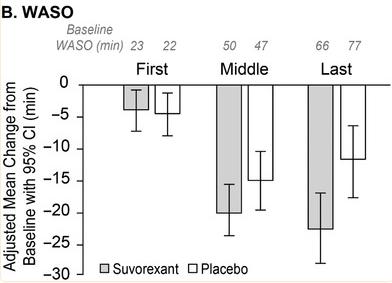
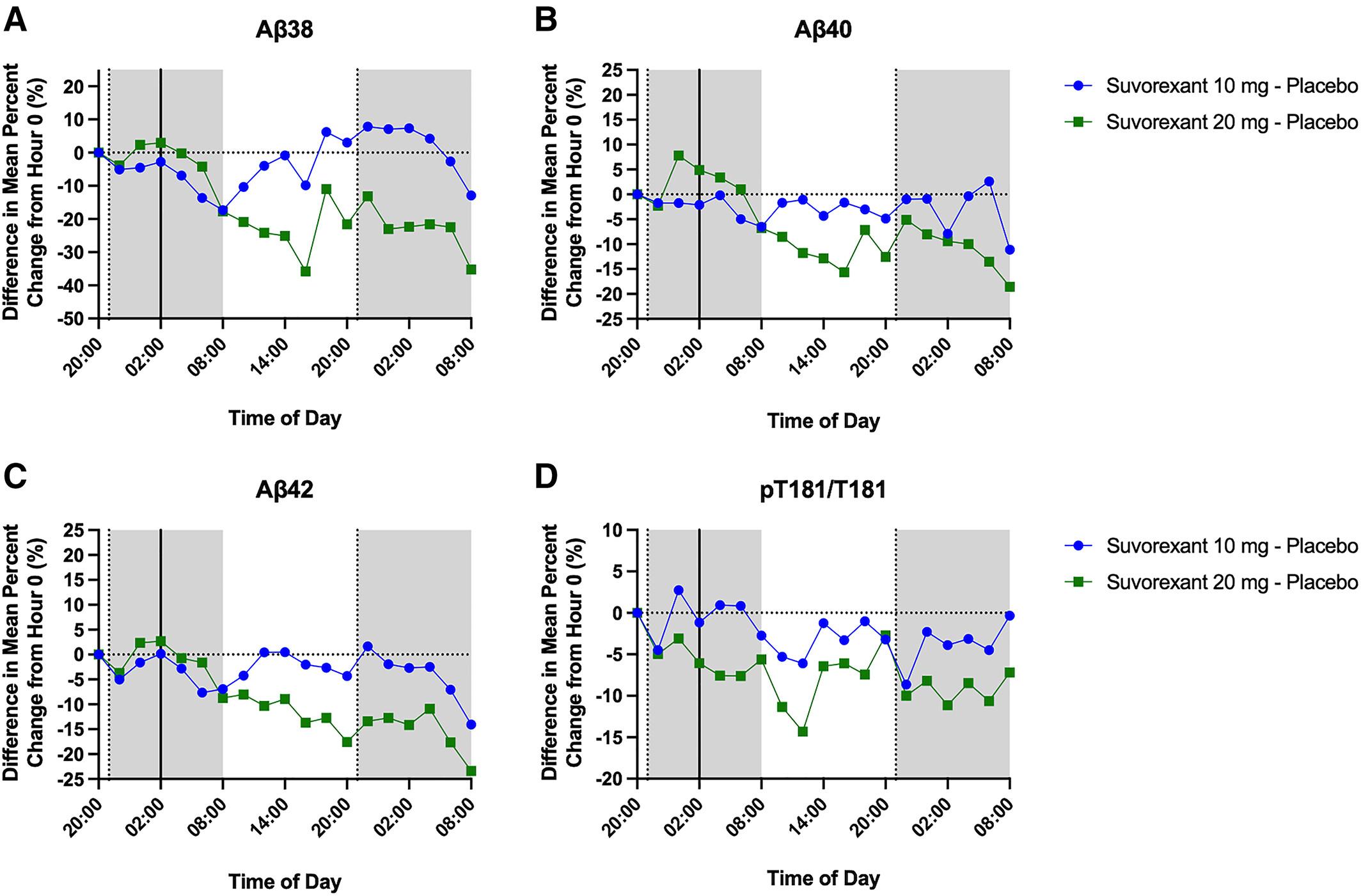
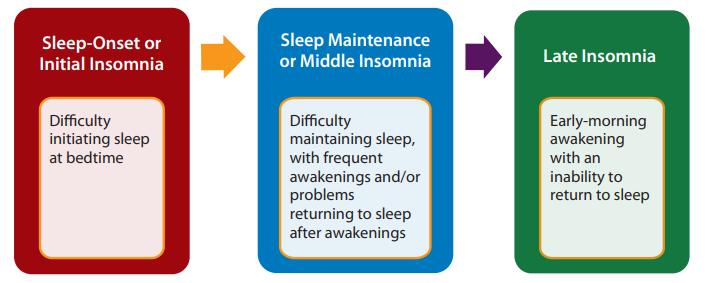
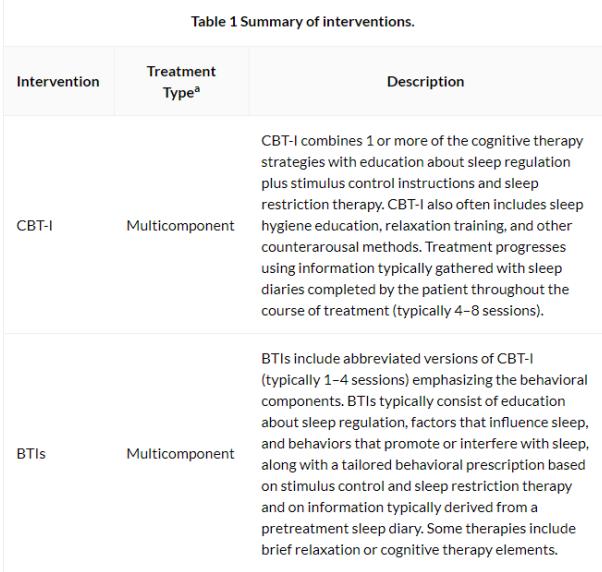

 J. Todd Arnedt, Ph.D. Professor of Psychiatry and Neurology Director, Behavioral Sleep Medicine Program
J. Todd Arnedt, Ph.D. Professor of Psychiatry and Neurology Director, Behavioral Sleep Medicine Program

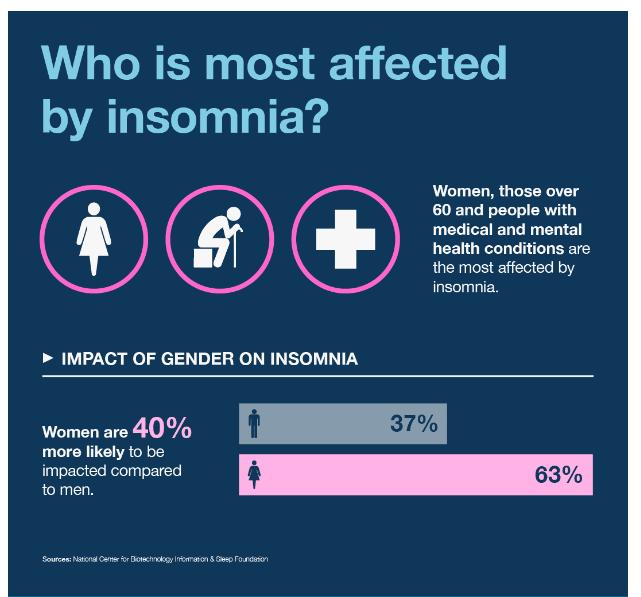



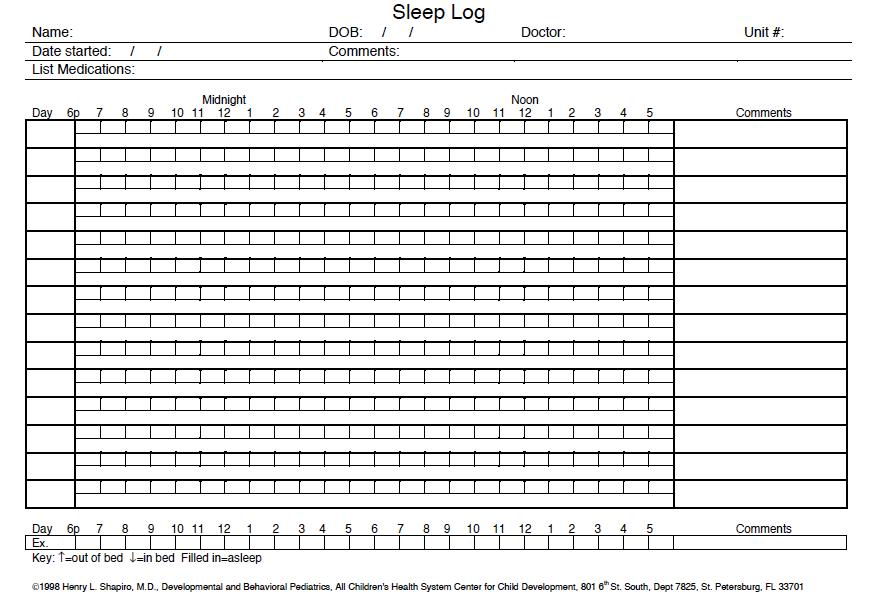
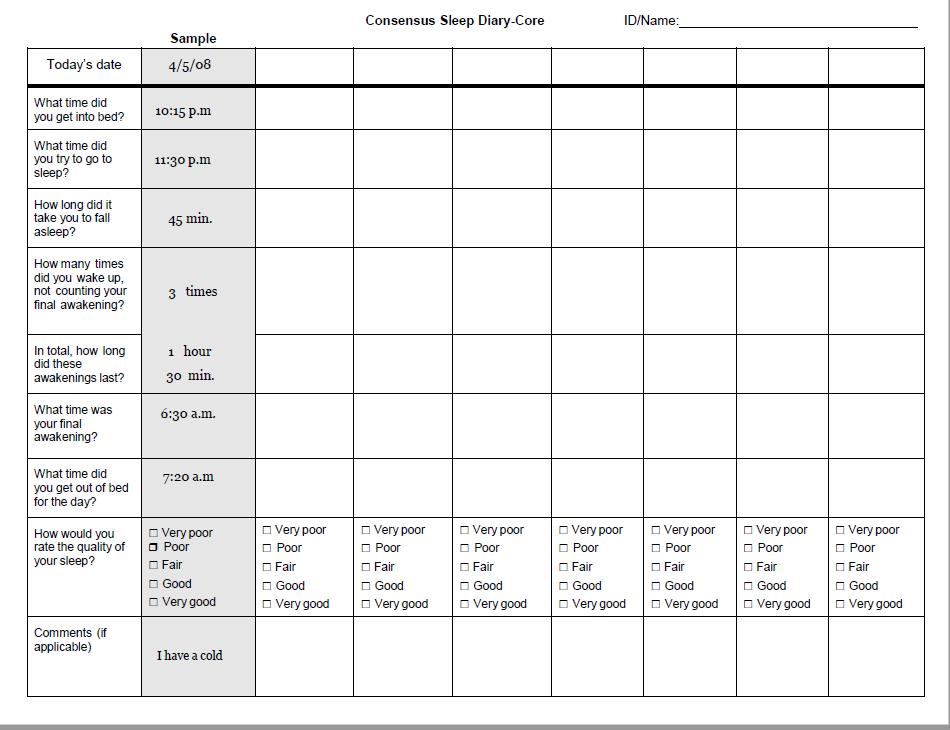



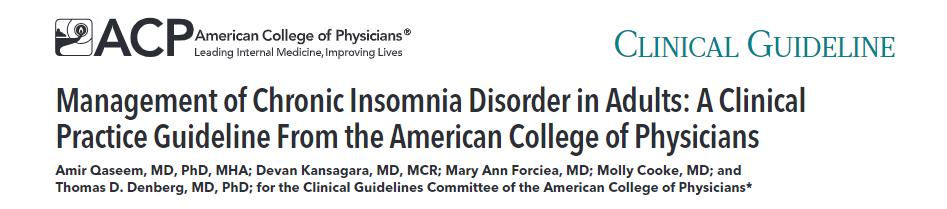
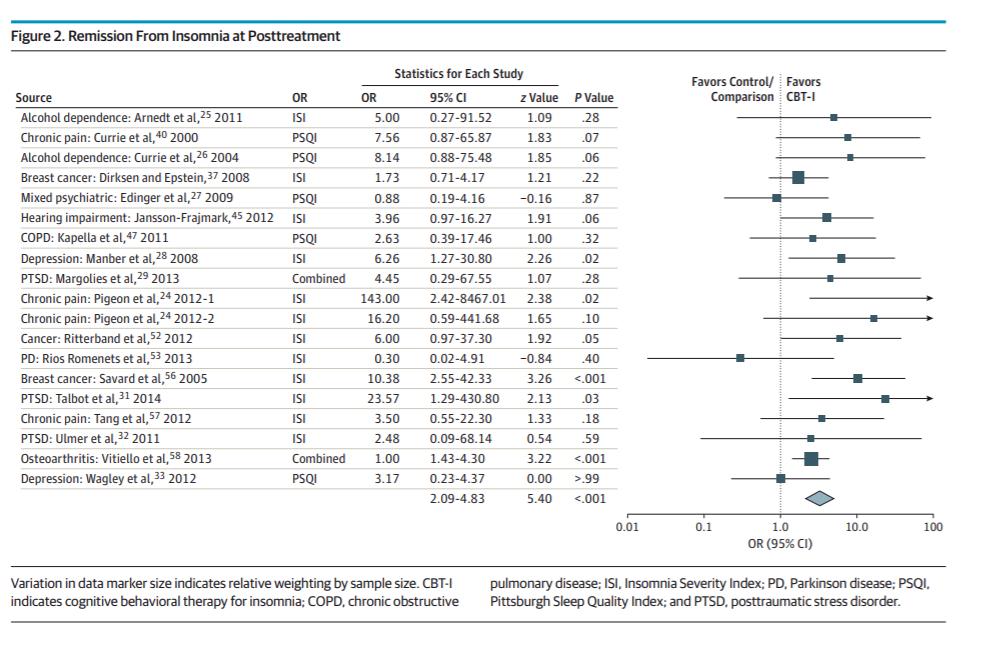
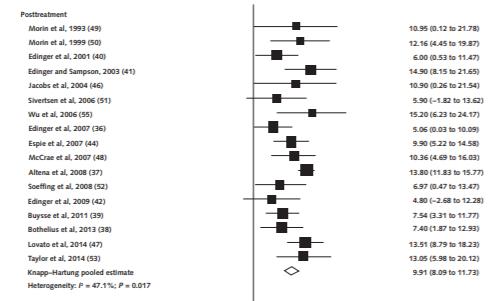



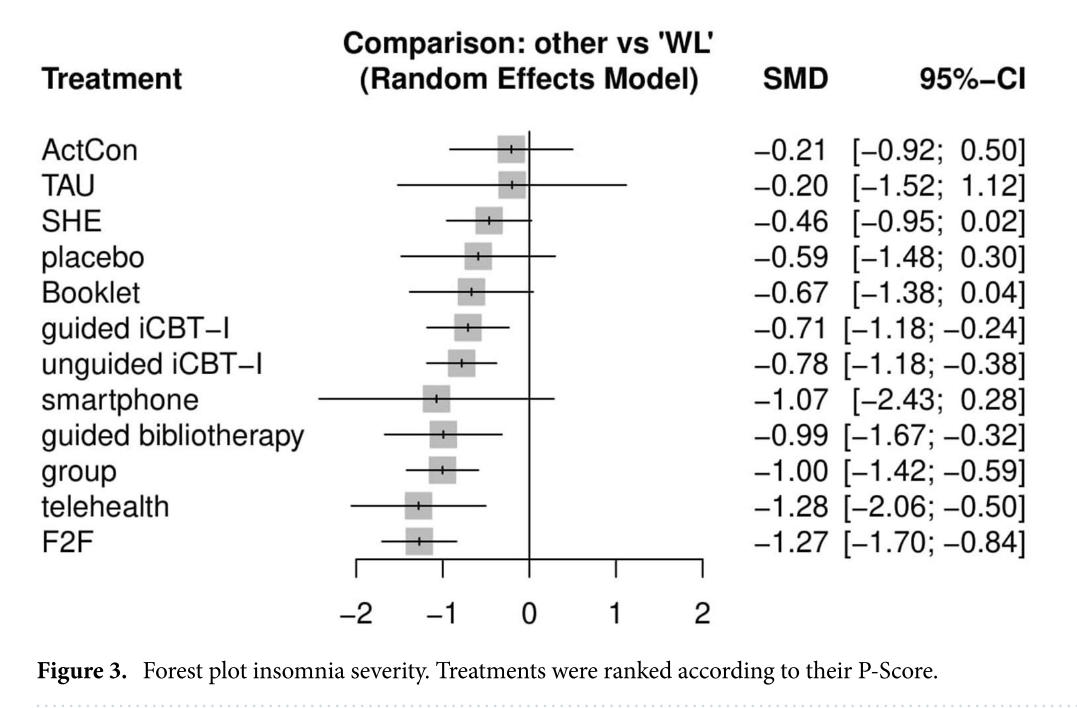







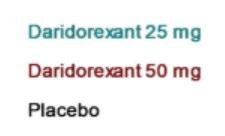



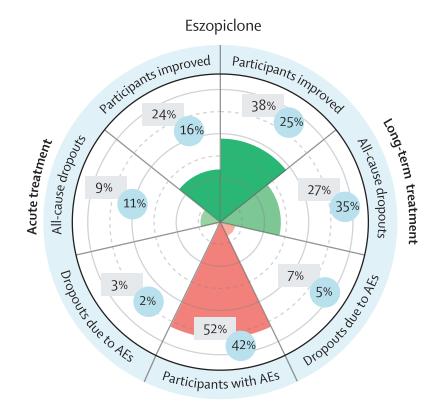
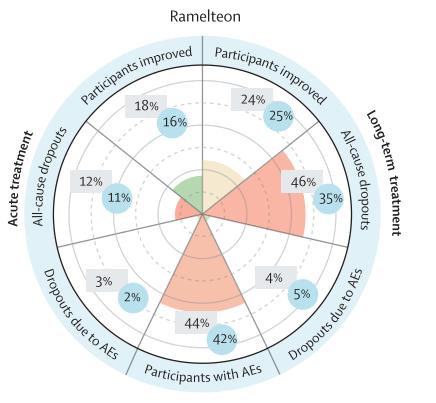

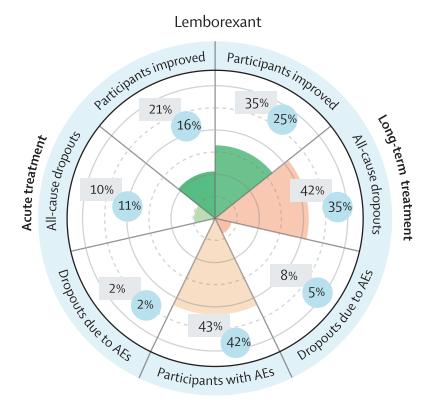
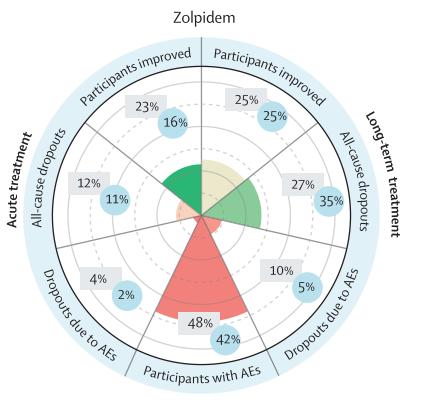










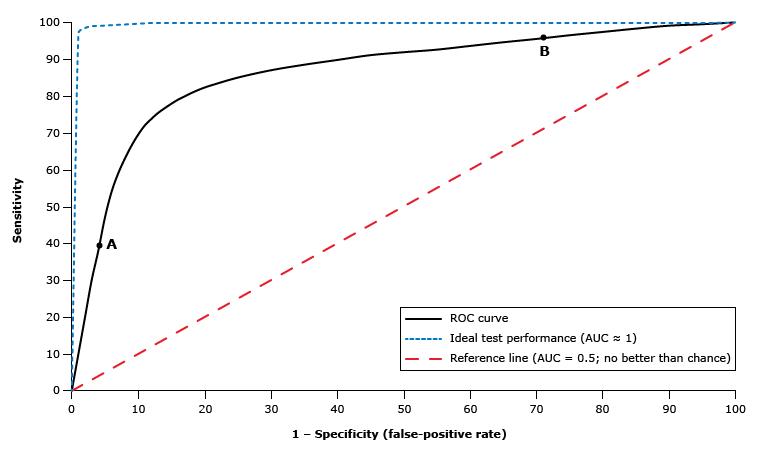
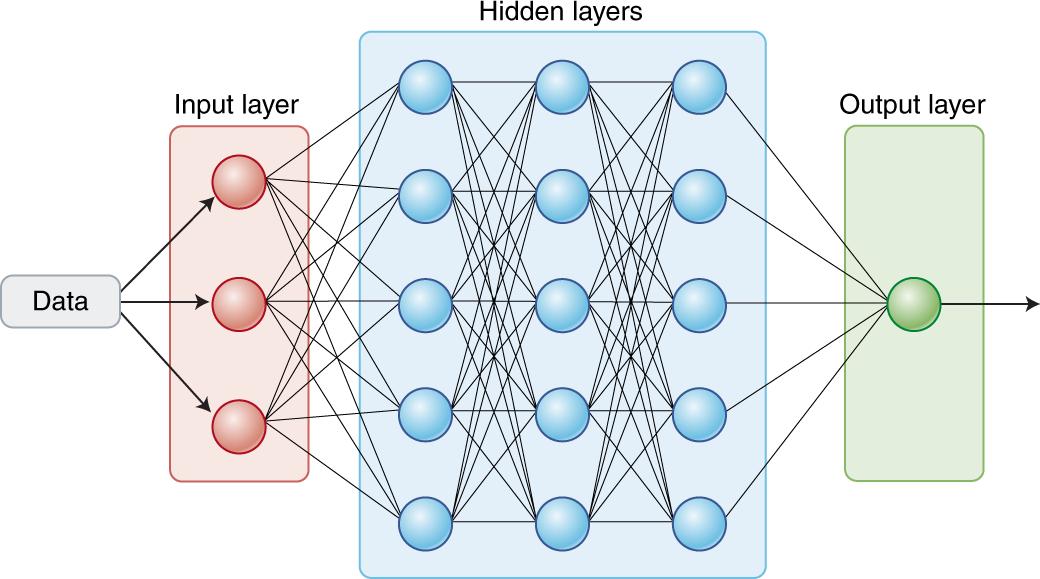

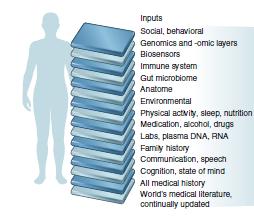
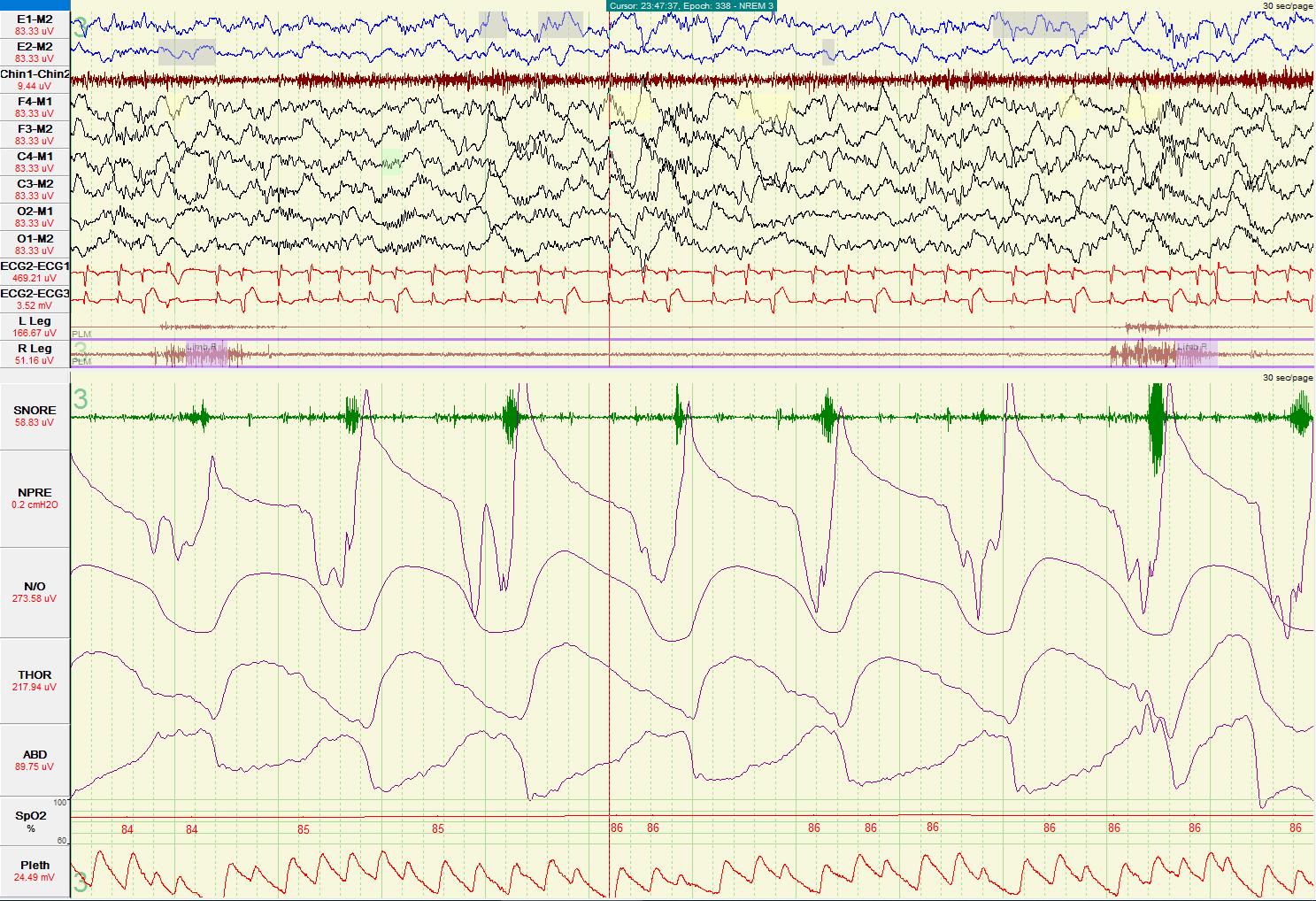







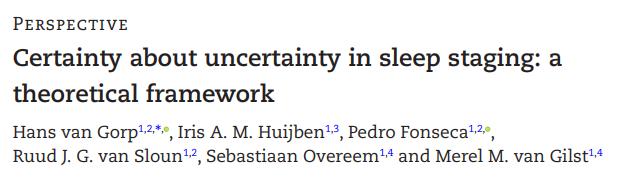



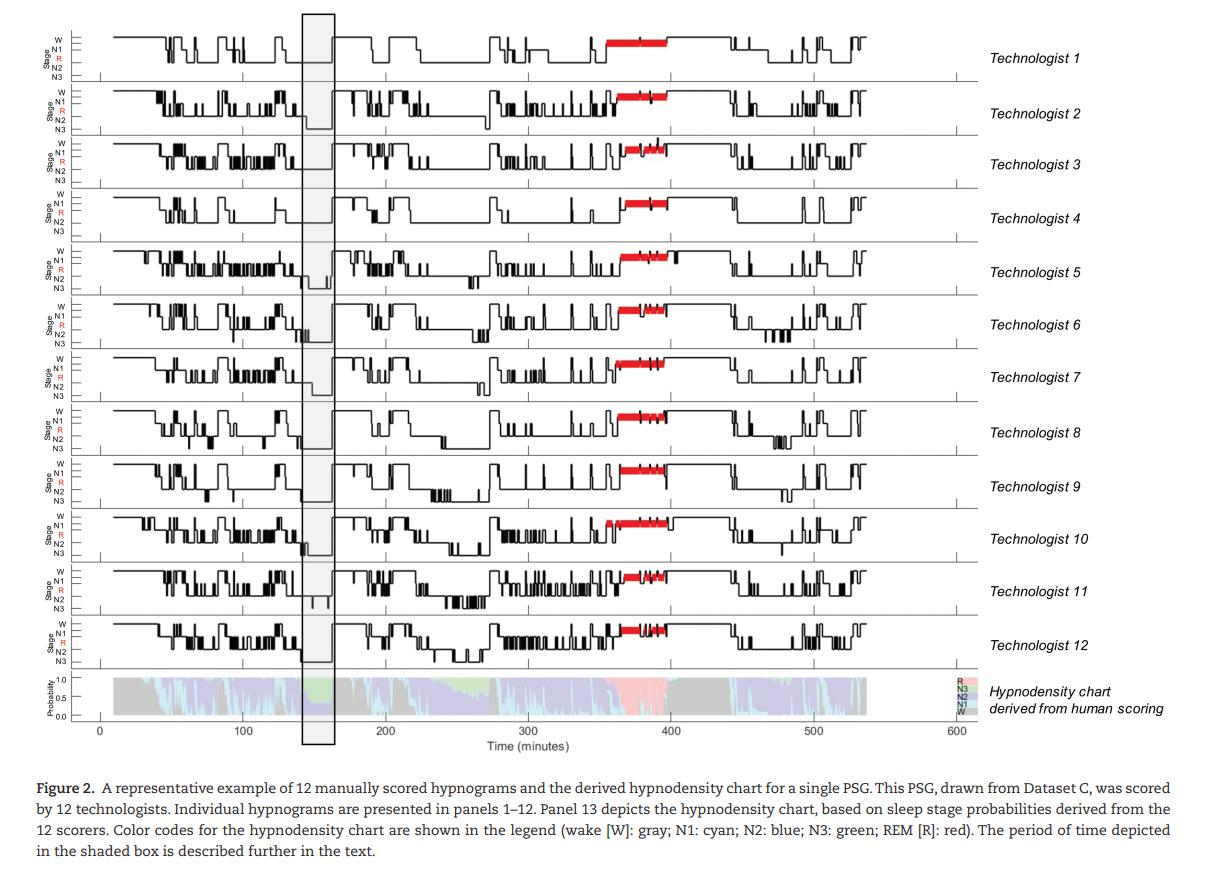
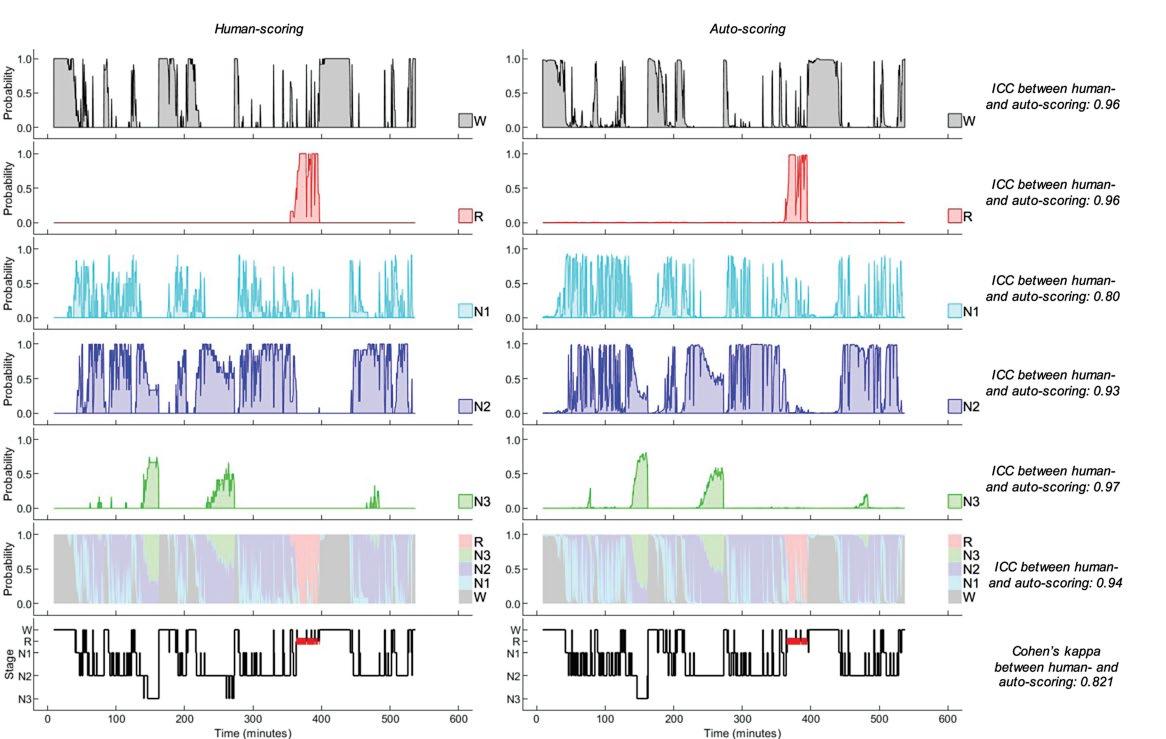
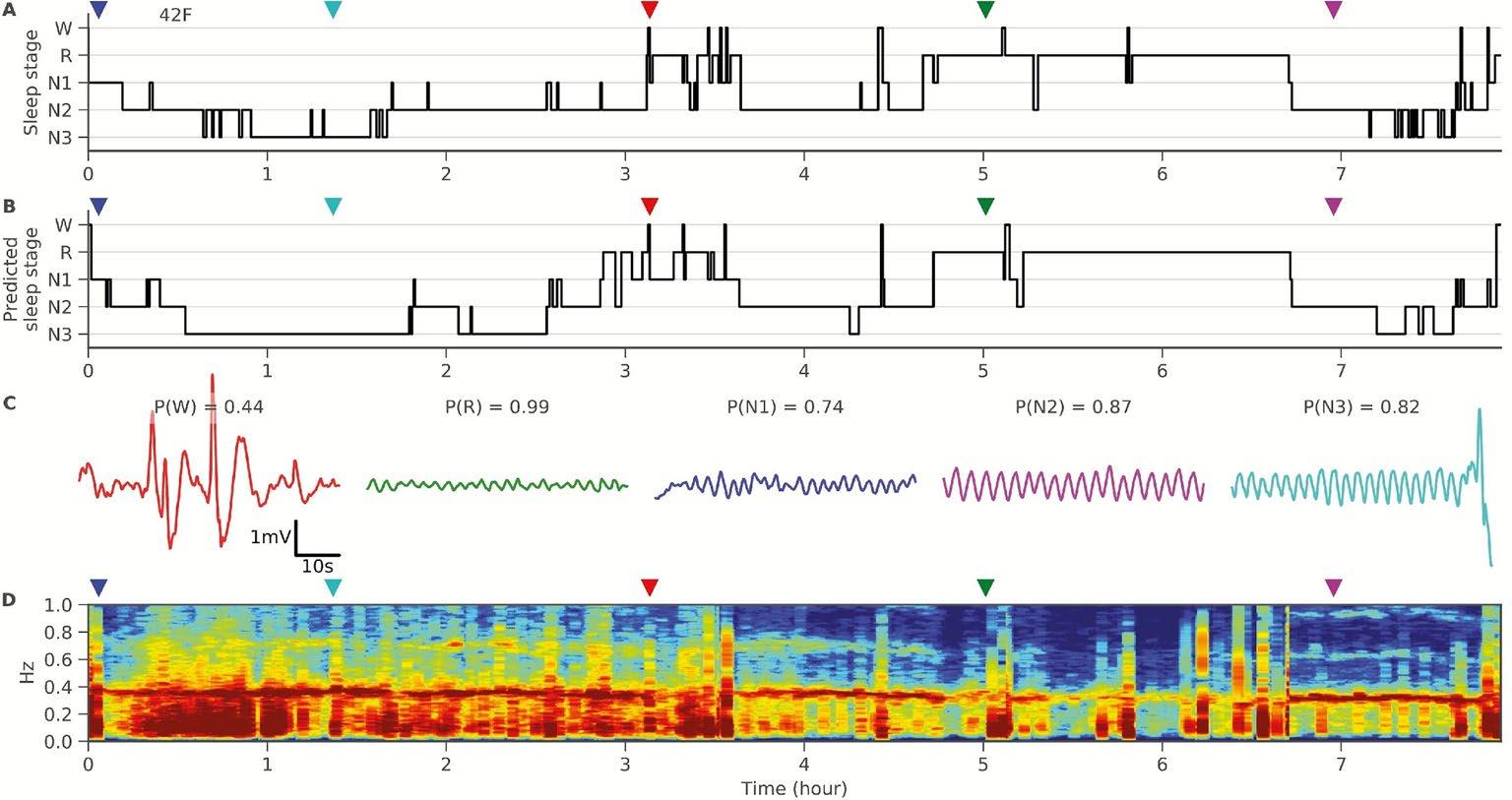
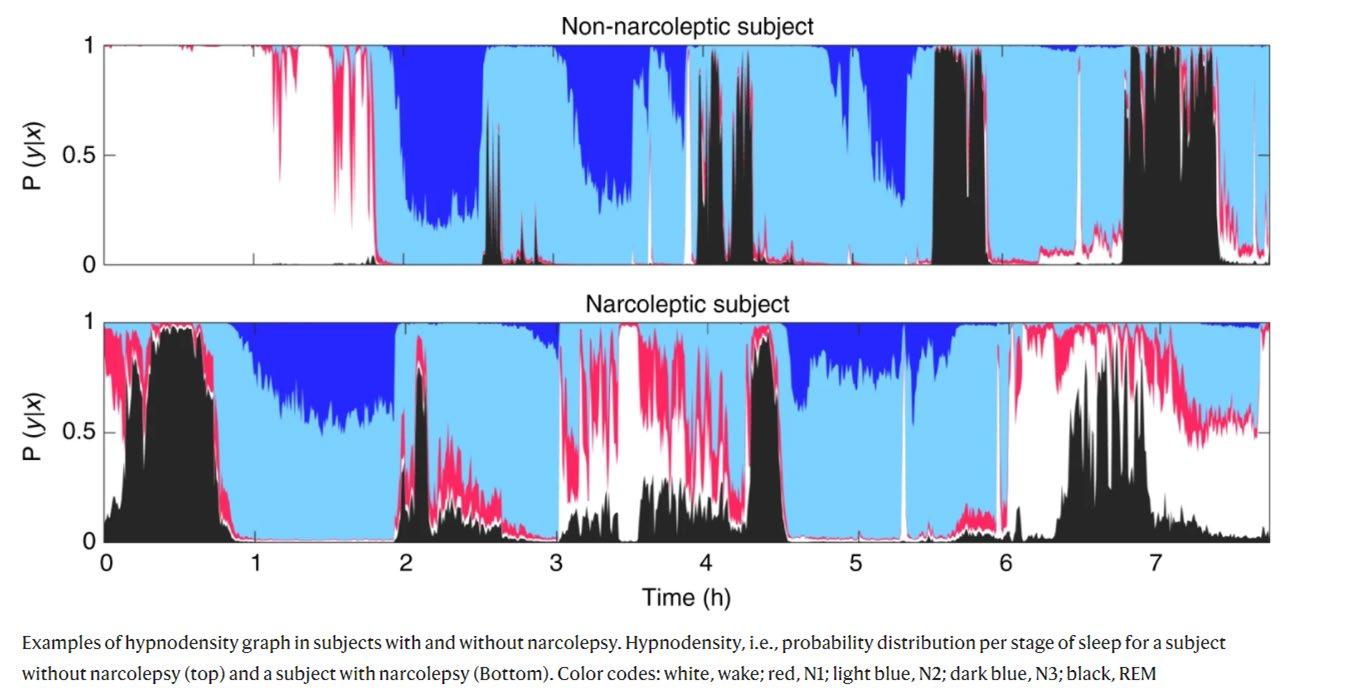



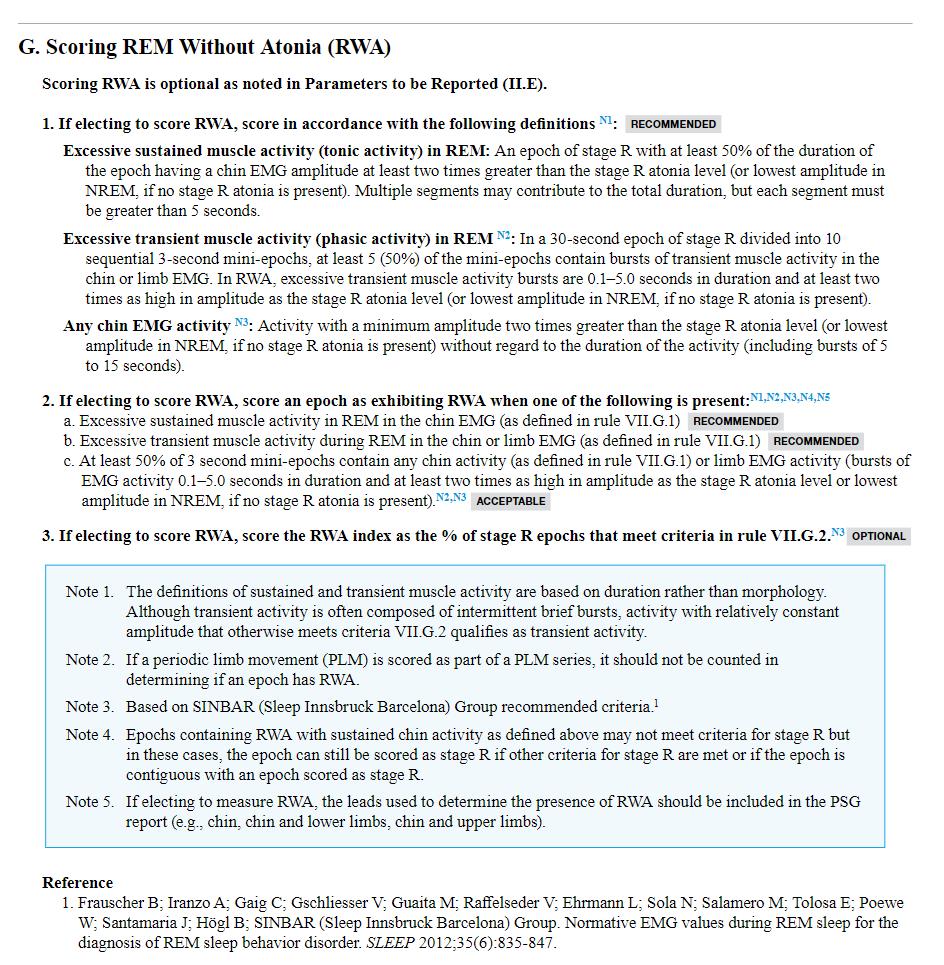
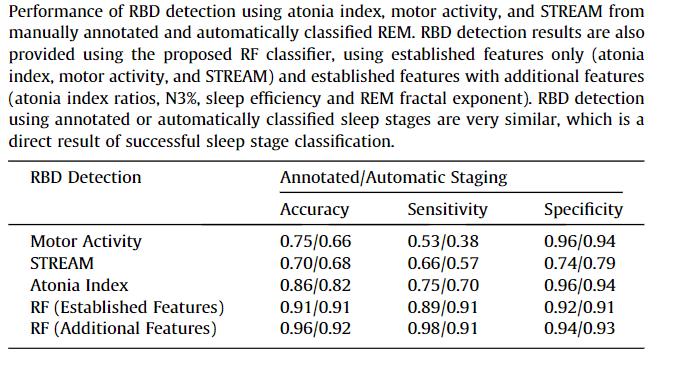








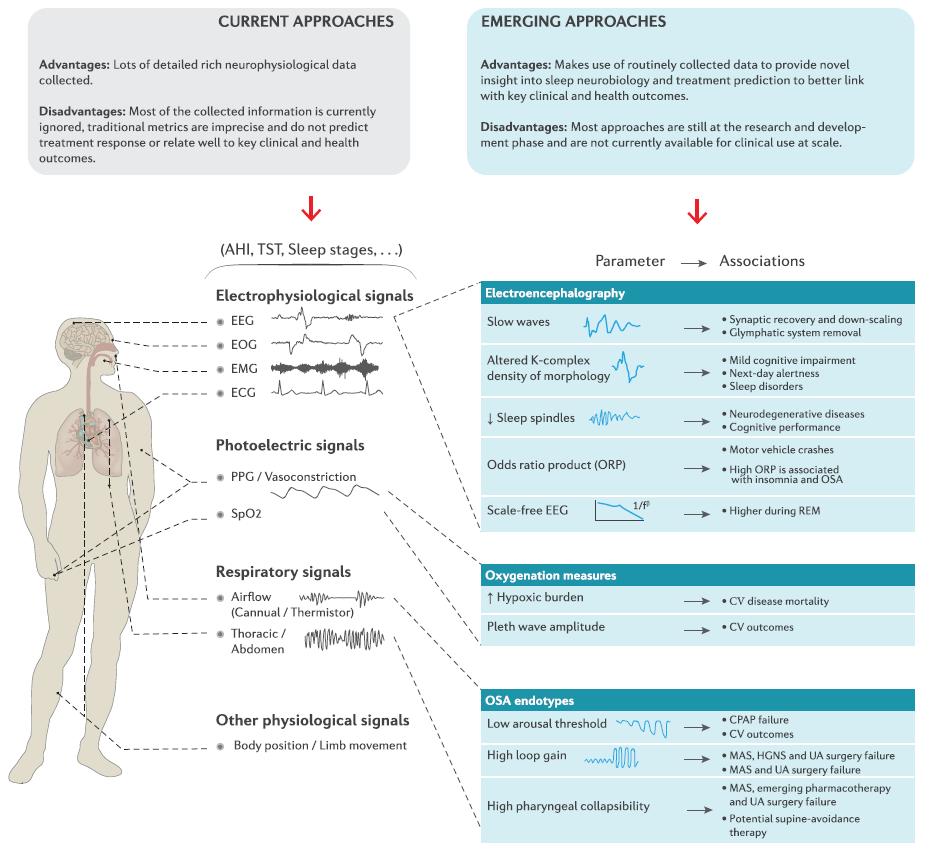


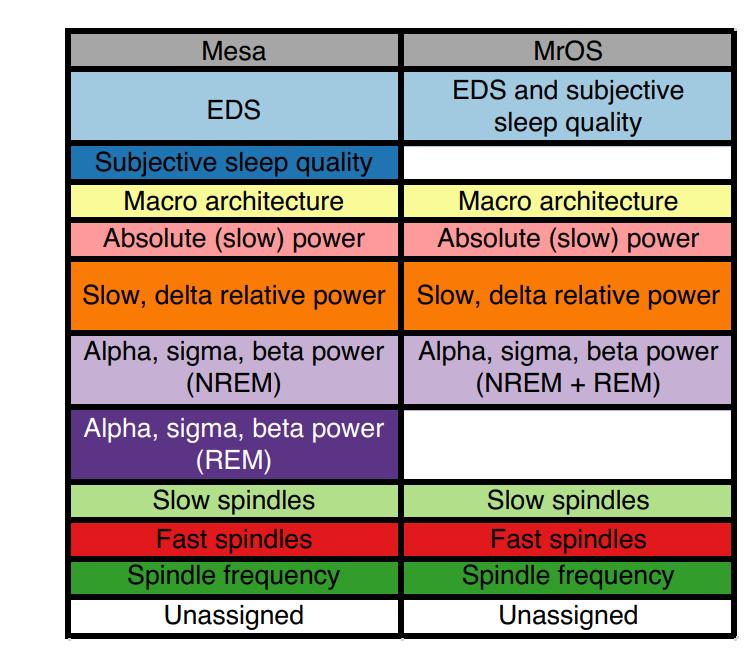

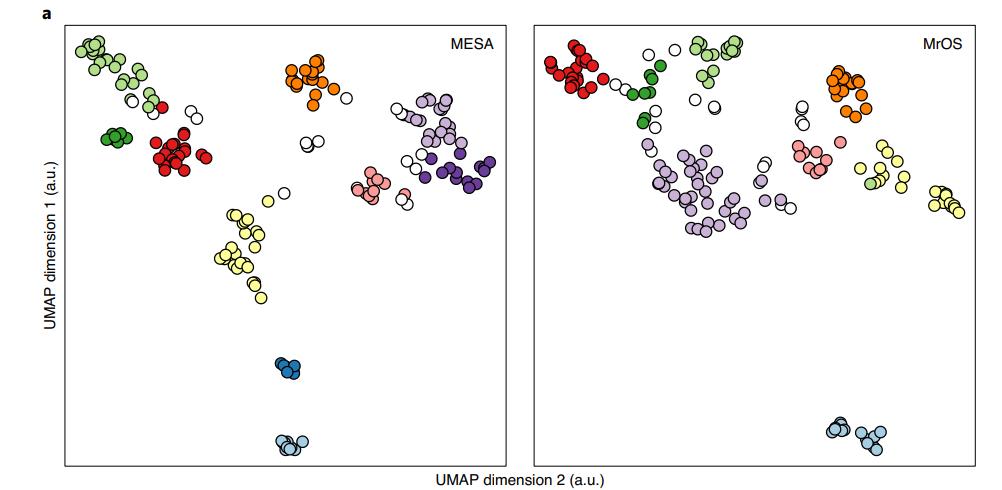

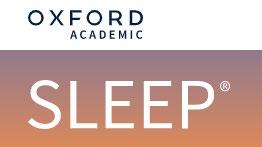







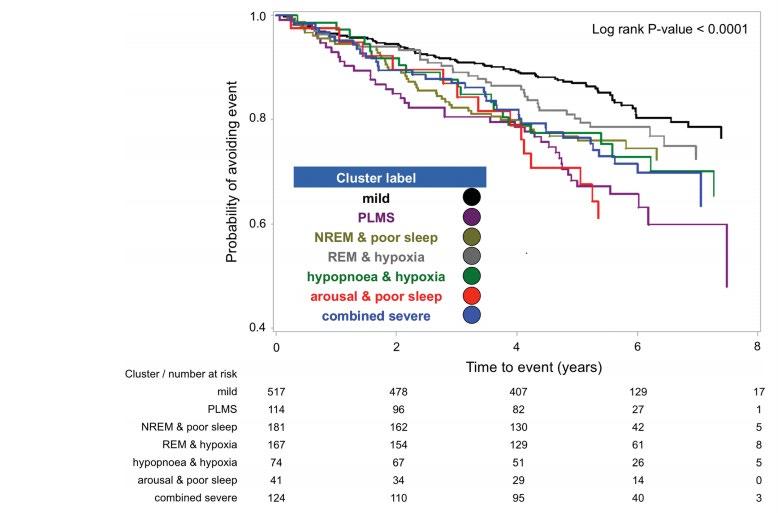
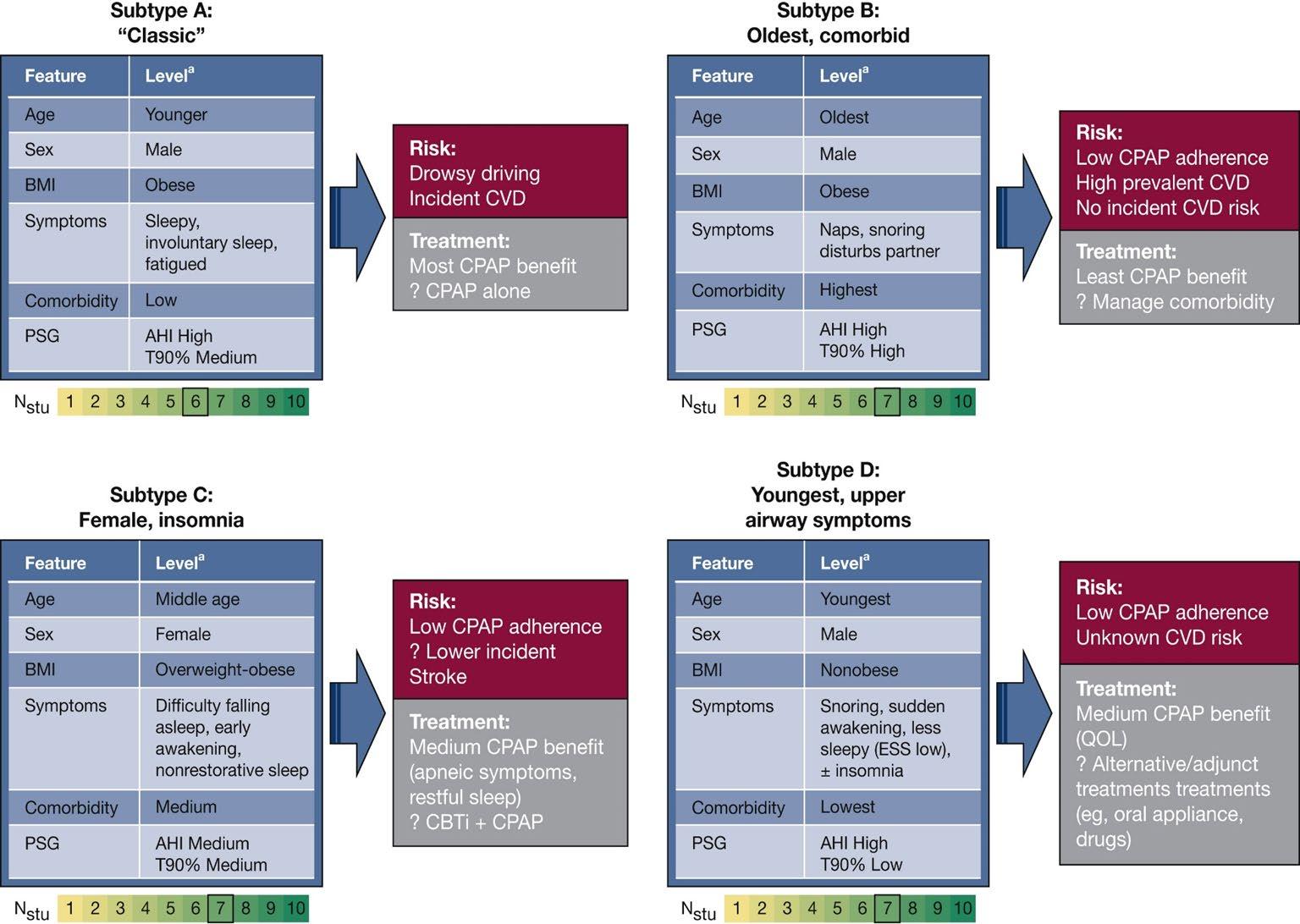
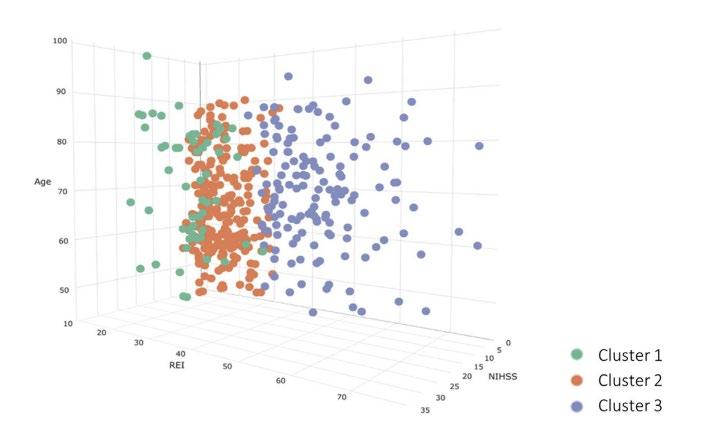









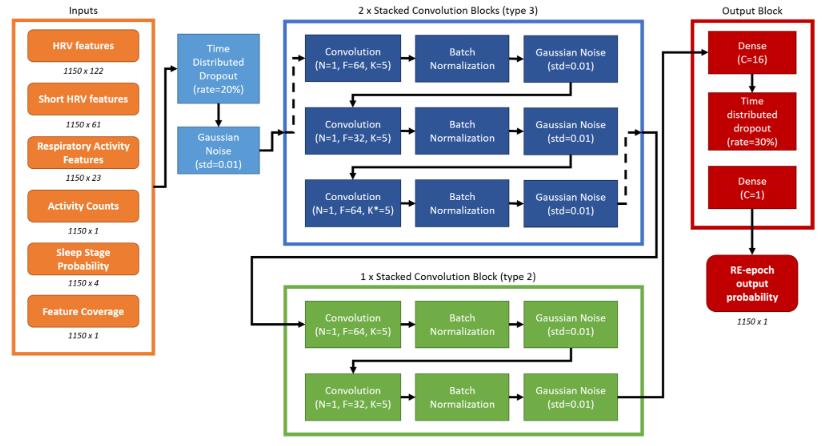
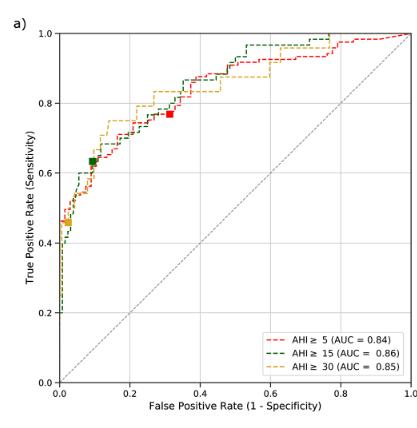



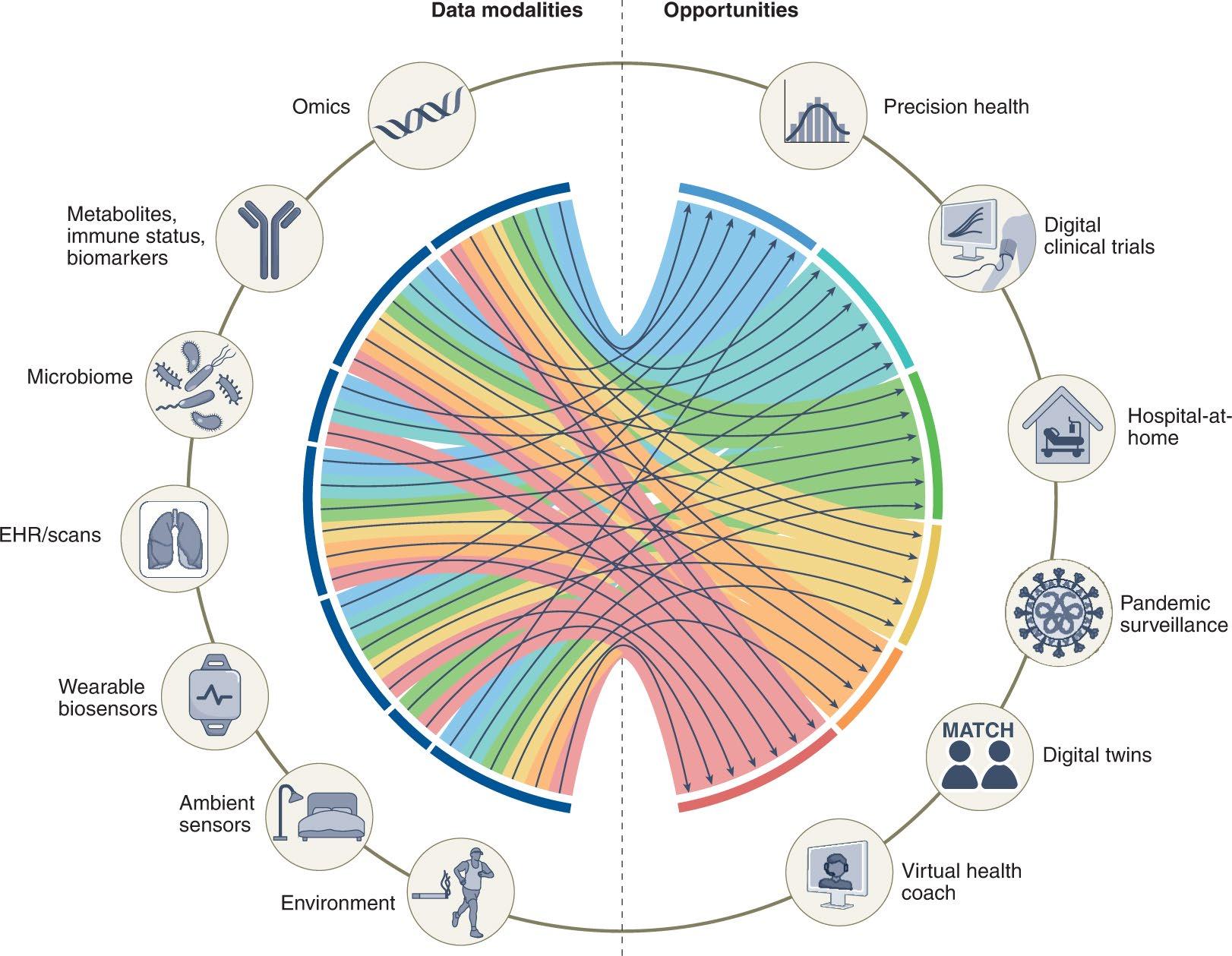


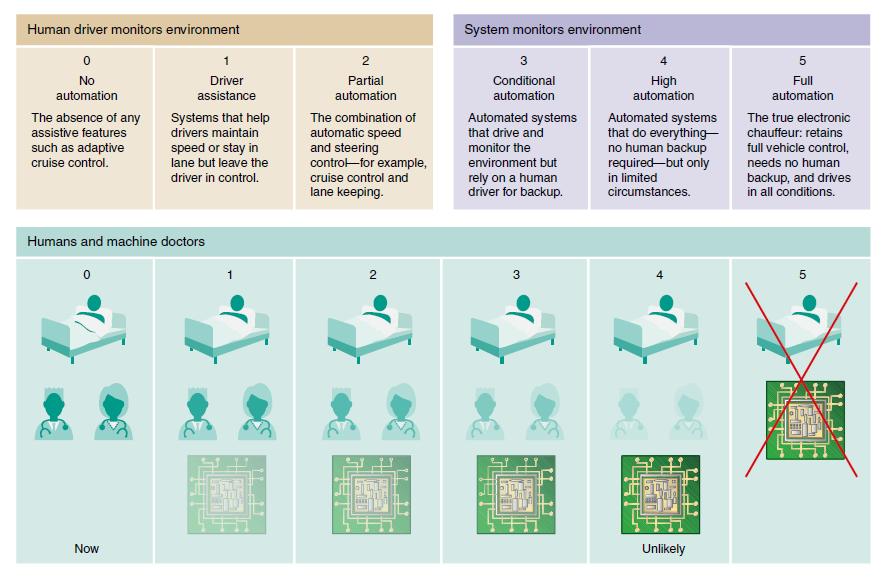













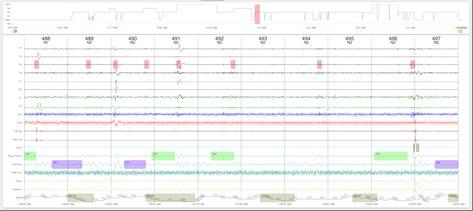
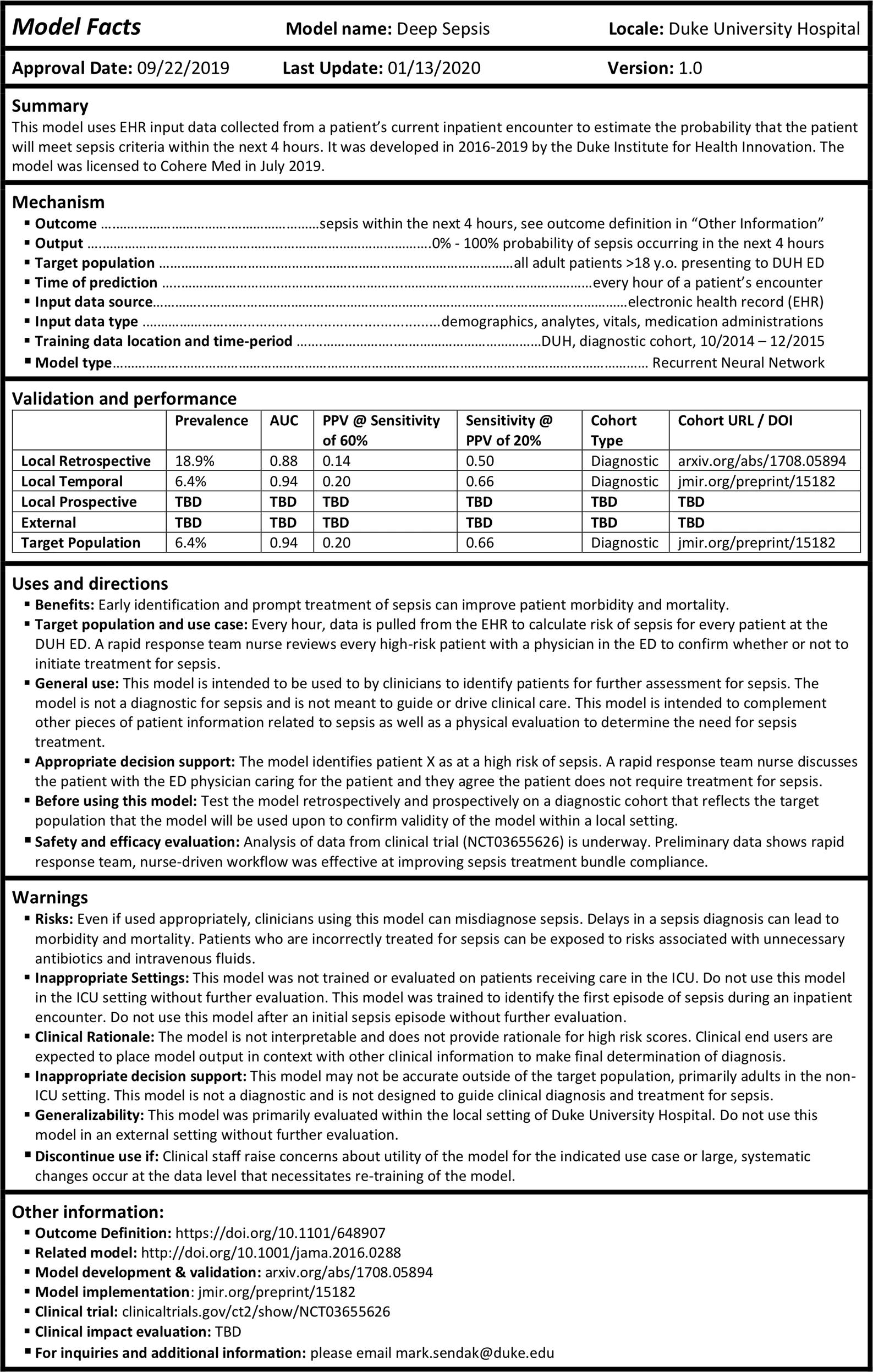
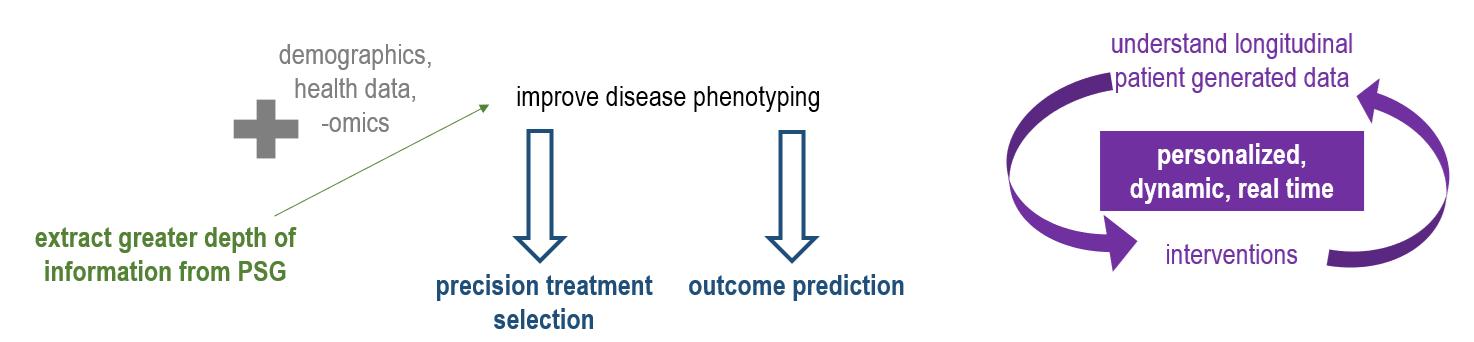






 Medical Director, Sleep Medicine, Atrium Health
Clinical Professor, Dept of Neurology, Wake Forest School of Medicine
Douglas Kirsch, MD, FAAN, FAASM
Medical Director, Sleep Medicine, Atrium Health
Clinical Professor, Dept of Neurology, Wake Forest School of Medicine
Douglas Kirsch, MD, FAAN, FAASM