DISRUPTING MEDICINE

DEPARTMENT OF MEDICINE



DEPARTMENT OF MEDICINE

Two thousand twenty-four has been an extraordinary year, with technological and medical discoveries disrupting medical practice and reshaping our thinking in unprecedented ways.
The Department of Medicine has embraced these challenges, and our faculty and learners are actively exploring these “fault lines” while fundamentally transforming the field of medicine.
Inside this report, you’ll learn about how our doctors are rising to the occasion by leveraging machine learning to precisely diagnose atrial fibrillation, studying the effects of GLP-1 agonists on epicardial adipose tissue, and utilizing artificial intelligence (AI) algorithms to improve patients’ access to care. These innovations are not only revolutionizing how we deliver healthcare, they’re helping to solidify the University of Miami Miller School of Medicine as a leading academic institution.

As we continue to push the boundaries of care in the 21st century, we remain dedicated to training the next generation of doctors to be leaders in this everevolving field. Together, we’re shaping the future of medicine, one disruptive breakthrough at a time.
All my best,

Roy E. Weiss, M.D., Ph.D.
Professor of Medicine
Chair, Department of Medicine
Kathleen & Stanley Glaser Distinguished Chair in Medicine
Rabbi Morris I. Esformes Endowed Chair in Medicine and Endocrinology
University of Miami Miller School of Medicine

The earliest known record of atrial fibrillation is found in a firstcentury BCE text titled The Yellow Emperor’s Classic of Internal Medicine. In this treatise, the author describes a mysterious condition where the heart beats irregularly. Centuries later, the medical community discovered that faulty electrical signals within the heart were to blame. Then, a simple device called an electrocardiogram (ECG) was developed to record the heart’s electrical activity, allowing physicians to see the heart beats as peaks and valleys inked on paper printouts.
As useful as the ECG has been over the last 30 years for indicating an irregular heartbeat, the diagnostic test, as currently used, has provided only limited information. Recent advances in medical technology, however, are changing that. Artificial intelligence (AI), specifically, has shown tremendous promise for not only detecting atrial fibrillation (AFib) but for delving into the ECG readings to provide enhanced information with unprecedented precision.
Dr. Goldberger
Jeffrey Goldberger, M.D., M.B.A., Professor of Medicine and Biomedical Engineering, Cardiac Electrophysiologist, and Director of the Center for Atrial Fibrillation at the University of Miami’s Miller School of Medicine, says AI has the potential to revolutionize cardiac care by enabling more precise, personalized treatment.

“We’ve completed a preliminary study of a small number of patients that shows that artificial intelligence can be used to classify which patients are responders to ablation (i.e., those patients who have no recurrent AFib after ablation) versus those individuals who are non-responders (i.e. those with recurrent AFib after ablation),” explains Dr. Goldberger. “We’re now expanding this research to include a much larger cohort to extract as much information as we can from one of the most basic tools that we have in cardiology.”
AFib occurs when the heart’s upper chambers are activated rapidly and chaotically, rather than in coordination with the lower chambers, which are the main pumping chambers. While it’s possible to have little to no symptoms with AFib, individuals with the condition often experience heart flutters or pounding, dizziness or lightheadedness, fatigue, weakness, or chest pain.
AFib is the most common form of arrhythmia diagnosed today. The Centers for Disease Control estimates between 3 and 6 million people in the United States suffer from the condition, which can increase the risk of blood clots, heart failure, and stroke.
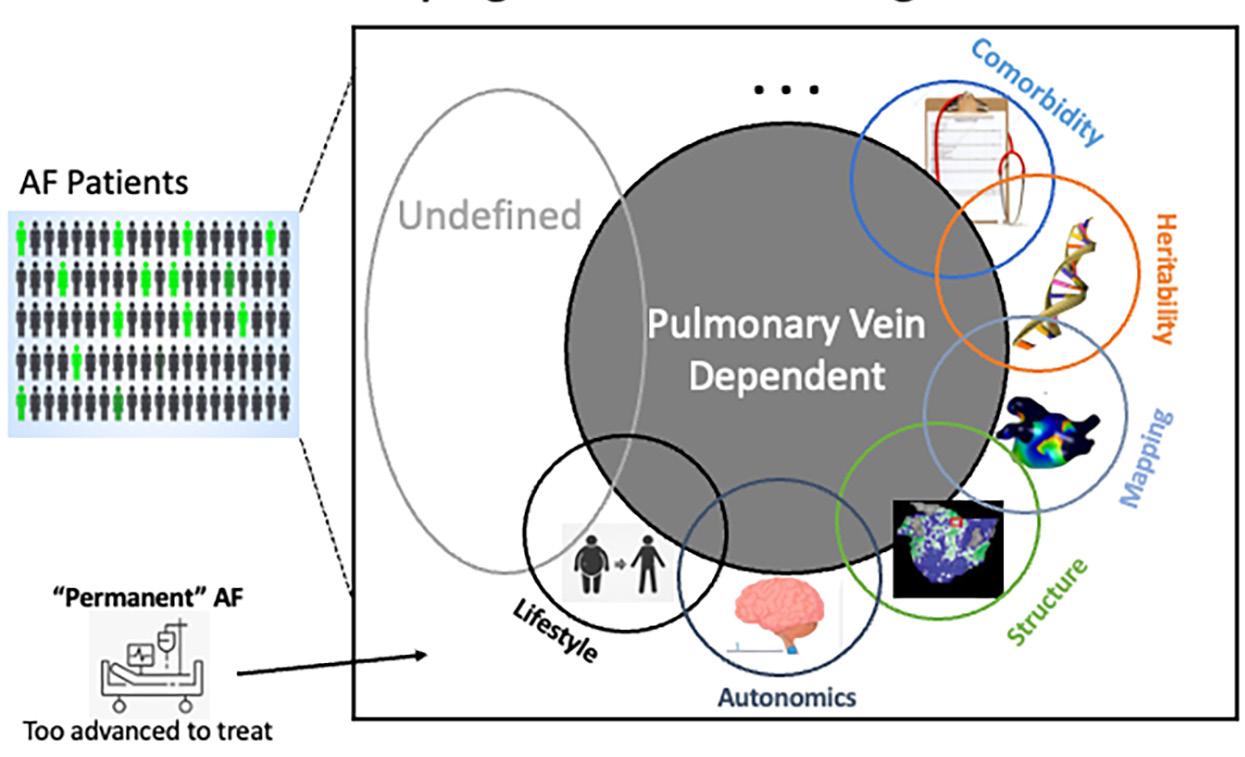
A number of physiological conditions may lead to AFib, including congenital heart defects, sleep apnea, thyroid disease, high blood pressure, heart valve disease, heart attack, lung disease, and infection. Lifestyle habits and other factors including obesity, smoking, excessive alcohol consumption, and abusing stimulants like caffeine and cold-allergy medication, can trigger AFib, even in the absence of heart disease.
There are several kinds of AFib: paroxysmal, persistent, longstanding persistent, chronic, valvular, nonvalvular, acute, and postoperative. For decades, cardiologists have relied on the same diagnostic tools to evaluate all types of AFib, which include blood tests, exercise stress tests, chest X-rays, echocardiograms, and the ubiquitous ECG. If the condition is detected, medications such as beta blockers and
AI

blood thinners are often used (but not always) as the first line of treatment. If these don’t work, the next step may be cardioversion therapy, which resets the heart’s rhythm.
Another treatment option is catheter ablation, which uses radiofrequency energy or other techniques to destroy or isolate the small areas of the heart that are responsible for causing the irregular heartbeat. The goal of the procedure is to disrupt the irregular signal and restore a normal heart rhythm.
Yet according to a 2023 preliminary study conducted by Dr. Goldberger, other Miller School of Medicine physician-scientists, and colleagues at the College of Engineering, “success rates for catheter ablation of atrial fibrillation (AFib), particularly persistent AFib, remain suboptimal.”
The issue at hand is the limited information provided by current diagnostic tools, particularly the ECG. An ECG can confirm if a patient has AFib but does not specify the type or severity of the condition. This lack
of detailed information often leads to treatments that are based on educated guesses rather than precise data. While this approach works for most patients, it is not effective for a significant minority.
“When you look at 100 ECGs from patients with atrial fibrillation, they all look different. Until now, we’ve been using qualitative descriptors for that. There’s coarse AFib or there’s fine AFib, but there really hasn’t been a standard way to characterize those fibrillatory waves. When you examine the ECG, you can see those fibrillatory waves, but you can’t extract much information from these waves on your own,” says Dr. Goldberger, who has been studying novel approaches to AFib for the past 15 years.
To clarify his point, Dr. Goldberger compares reading ECG waveforms to analyzing speech patterns. Acoustic analysis can detect sound and measure attributes such as pitch, loudness, and clarity, but it can’t distinguish between someone reciting “Mary Had a Little Lamb” versus “The
Gettysburg Address.” To understand the actual message, additional methods are needed. Recent technological advances now provide the tools to make these distinctions.
In the abovementioned study, researchers set out to test whether Machine Learning (ML) analysis of an ECG could predict the longterm outcomes of catheter ablation for patients with persistent atrial fibrillation. ML is a form of AI that uses algorithms to “cognate” or learn from data sets, extract otherwise indiscernible information, and subsequently predict outcomes.
Imagine an ECG recording as a vast ocean of cardiac waves, where larger swells obscure smaller ripples. In the study, Dr. Goldberger and his team first had to separate the smaller AFib waves from the much larger waves generated by the ventricles (the QRS-T complex). Advanced signal processing techniques, including QRS-T subtraction and independent component analysis, rigorously separated these waves. Once the ventricular components were removed, only the atrial signals were present, allowing for a clearer analysis of just the fibrillation waves. By isolating this crucial aspect of AFib, they were able to predict, with 90.4 percent accuracy, which patients would respond well to catheter ablation in the long term.
While larger studies and additional research are on the horizon, current findings suggest that cardiac care is entering a period of significant advancement—without the need to completely overhaul existing methods.
“In my view, there is a tremendous opportunity for AI here,” adds Dr. Goldberger. “It will allow us to significantly enhance how we personalize the assessment and subsequent treatment of atrial fibrillation.”

Recent advances in healthcare have generated an overwhelming amount of data that humans can’t manage alone. Artificial Intelligence (AI) plays a crucial role in quickly and accurately analyzing and synthesizing this information. One of the benefits of AI is its ability to develop solutions for various challenges by pushing the boundaries of existing technology. As a result, the potential for transforming medical practice is vast, leading to better patient outcomes, more efficient healthcare delivery, and improved access to care.
Maritza Suarez, M.D., Associate Professor of Clinical Medicine in the Division of General Internal Medicine and Chief Medical Informatics Officer at the University of Miami Miller School of Medicine, has successfully integrated AI into the medical school’s existing information technology (IT) systems. By combining creative thinking with data analytics, Dr. Suarez and her team of IT experts have been enhancing the overall productivity of the University’s healthcare system, making improvements one code at a time.

Suarez
“I’ve been involved in several initiatives aimed at improving care delivery and reducing some of the points of friction we encounter, whether it’s unlocking the potential to serve a greater number of patients or helping providers respond to patients more efficiently,” says Dr. Suarez.

“WHAT I DO NOW IMPACTS MANY PEOPLE BEYOND JUST PRIMARY CARE AND INTERNAL MEDICINE. THE KEY BENEFIT OF THE TECHNOLOGY IS WHEN YOU CAN IMPLEMENT IT AT THE RIGHT TIME AND WITH THE RIGHT SUPPORT TO MAKE IT ALL COME TOGETHER.”
– DR. SUAREZ

One example of IT’s impact is in the operating room, where the employee vacation time system (Workday ERP) is now connected to the OR scheduling system (UChart). A surgeon’s planned time off is recorded in Workday ERP, while procedures are scheduled in UChart. Previously, these two systems couldn’t communicate, requiring a person to manually check and adjust time slots. This often led to scheduling conflicts due to human error.
Dr. Suarez’s IT team resolved the issue by implementing an AI model that connects the separate scheduling systems. The algorithm compares surgeons’ planned time off with surgery schedules and sends notifications about available OR blocks. This allows human schedulers to match an available surgeon to those time slots without any errors. In the first four months, the new system resulted in 204 reallocated OR hours and a 16 percent increase in block usage.
“I believe the beauty of IT lies in its integration with the process,” says Dr. Suarez.
Other successful initiatives highlight the effectiveness of technology in enhancing communication. For example, UM’s bone marrow transplant process previously depended on lengthy email chains to manage all of its components. Dr. Suarez’s team introduced a process to streamline communication, ensuring that dates and times were coordinated for both patients and specialists to simplify scheduling the procedure.
The ability for AI technology to extract relevant data is crucial for matching patients with clinical trials. Patient charts often can become overwhelming with notes and scanned lab reports, making it easy for important details indicating eligibility for a study to get lost. To address this, Dr.
Suarez’s team developed a one-of-akind referral order process for clinical studies for Sylvester Comprehensive Cancer Center. This allows the physician, who is well-versed in the details of a patient, to refer them for a clinical trial. That referral is then sent to a disease-specific research group to review key data and determine the participant’s eligibility for a clinical trial. Within two months of launching this personalized referral for clinical trials, 472 orders were placed, resulting in 172 patients being matched to clinical trials.
“It really has made a difference, especially for patients receiving the actual drug in the trial,” says Dr. Suarez. “These patients gain access to innovative treatments they might not have accessed otherwise, due to important information being buried in the chart.”
A graduate of the Miller School of Medicine, Dr. Suarez is highly enthusiastic about the potential applications of AI. She is particularly impressed by its forecasting abilities. Her team, for instance, has begun developing predictive models for the electronic medical record (EMR)
system that assesses patients’ deterioration status, helping staff members identify which patients are likely to need the most assistance.
“Predictive analytics let you know what your census is going to look like, your throughput, how many beds you’re going to have open, how many you’re not going to have open, and your readmission risk score. We’re focusing attention on those patients who have a high-risk readmission score to be able to assist in their care and avoid having them go back to the hospital,” she says.
UHealth patients are also benefiting from the advancements of AI. At Sylvester Comprehensive Cancer Center, orders for patient-initiated preventive screenings for breast and lung cancers are now generated automatically. This has eliminated the need for phone calls, wait times, and sign-offs.
While AI saves patients time and energy, it also brings improvements not seen in decades. The widespread use of electronic recordkeeping requires physicians and nurses to type while talking to patients during office visits. As a result, healthcare
CLINICAL TRIAL MATCHING ORDERS AT SYLVESTER
472 REFFERALS PLACED
172 PATIENTS MATCHED
“THESE PATIENTS GAIN ACCESS TO INNOVATIVE TREATMENTS THEY MIGHT NOT HAVE ACCESSED OTHERWISE, DUE TO IMPORTANT INFORMATION BEING BURIED IN THE CHART.”
professionals have had to split their attention between the patient in the paper medical gown and their keyboard, rather than focusing fully on the individual in front of them.
In September, the IT team launched a pilot project involving 40 physicians aimed at recording information gathered in clinical settings while maintaining human interaction. With the patient’s consent, the program transcribes the conversation between the doctor and the patient, converting that discussion into structured medical notes without any unnecessary chatter.
AI-generated notes still require human verification, but they undoubtedly save valuable time. “It’s not just about the tools—there are plenty of flashy tools out there. If we don’t implement them in the right environment and with the proper buy-in, they won’t work effectively,” explains Dr. Suarez.
The University of Miami continues to explore and demonstrate the transformative applications of AI in areas that traditionally rely on human interaction. These two forces can coexist rather than exclude each other. Dr. Suarez, who balances practicing medicine with her work in IT, understands this paradox firsthand.
“My job is so fascinating,” adds Dr. Suarez, who was part of the team that implemented the electronic medical record (EMR) system back in 2010 and became the physician leader for that project. “Over the years, I transitioned from being a full-time primary care doctor to practicing just a couple of days a week. What I do now impacts many people beyond just primary care and internal medicine. The key benefit of the technology is when you can implement it at the right time and with the right support to make it all come together,” she says.
Gianluca Iacobellis, M.D., Ph.D., Professor of Clinical Medicine in the Division of Endocrinology, Diabetes, and Metabolism at the University of Miami Miller School of Medicine’s Department of Medicine, has been studying the role of epicardial adipose tissue (EAT) in cardiometabolic diseases for more than two decades. He has spearheaded groundbreaking research on the cardiovascular risks related to diabetes and obesity and pioneered a technique to measure the previously unquantifiable health risk associated with EAT. More recently, he’s been studying the effects of popular weight loss drugs (glucagon-like peptide-1 agonists (GLP-1As) – a class of medications that help lower blood sugar levels and promote weight loss) on the tissue itself. These drugs are one of the major disruptors of medicine in the treatment of obesity and its associated complications.

Dr. Iacobellis
“I am leading several clinical research projects on emerging diabetes/obesity pharmacotherapy that targets epicardial fat,” he says.
Dr. Iacobellis’ research on EAT established a new field of study, which reveals that this fat deposit, located on the surface of the heart muscle (myocardium) and beneath the pericardium, is a separate, active organ that directly affects the heart. The discovery has huge implications for predicting and preventing many related diseases and conditions.
Essentially, the medications make the heart’s adipose tissue function more efficiently. This is a major breakthrough because it explains how these drugs not only aid in weight loss and diabetes management but also provide significant cardiovascular benefits…
In the past, observable obesity was an unquestionable predictor of a myriad of diseases, including diabetes, atherosclerosis (the buildup of fats and cholesterol inside the arteries), kidney failure, and compromised liver function. Weight loss (fat reduction) was the obvious solution and was typically addressed with lifestyle interventions, including diet and exercise, bariatric surgery, and medications to lower cholesterol and blood sugar levels, as well as to suppress the patient’s appetite.
As the visible pounds dropped off, so too, did visceral tissue (internal fat deposited around organs like the heart, liver, and kidneys), but not in the order originally thought. Studies would show that these interventions impacted epicardial fat, a true visceral fat

deposit, sooner and more noticeably than any changes that could be read on a scale.
“If you calculate metabolic risk based on body mass index, or BMI, which is the officially accepted marker of obesity, you don’t have a detailed specification of the cardiovascular risk, because that marker doesn’t tell you where the fat is located,” says the Italian-born physician-scientist. Dr. Iacobellis attended Sapienza University of Rome, where he completed his residency and Ph.D. and went on to complete fellowships at the Karolinska Institute in Stockholm, Sweden; UT Southwestern Medical Center in Dallas, Texas; and the Cardiovascular Obesity Research and Management Department of Medicine at McMaster University in Ontario, Canada.
Until recently, it was not possible to see, much less measure, the covert culprit contributing to cardiometabolic disease. This was especially dangerous for patients who were asymptomatic and/or at a healthy weight, since no one would suspect these individuals could have excess internal fat.
“We know now, based on many studies, including mine and others, that you don’t have to be obese to be at a higher risk for cardiometabolic disease. You may have a completely normal weight, but if you have an increased visceral fat deposit inside your body, you’re actually at higher risk than a person who is grossly obese,” explains Dr. Iacobellis, who also serves as the director of the diabetes service at UHealth Tower, the University of Miami Health System’s academicbased hospital and is vice chair of the IRB, or institutional review board committee.

The implication of EAT being a specific marker of visceral fat is that it is also a measurable, trackable, and changeable indicator of cardiovascular risk, regardless of BMI. Until recently, though, that life-saving data had been impossible to collect.
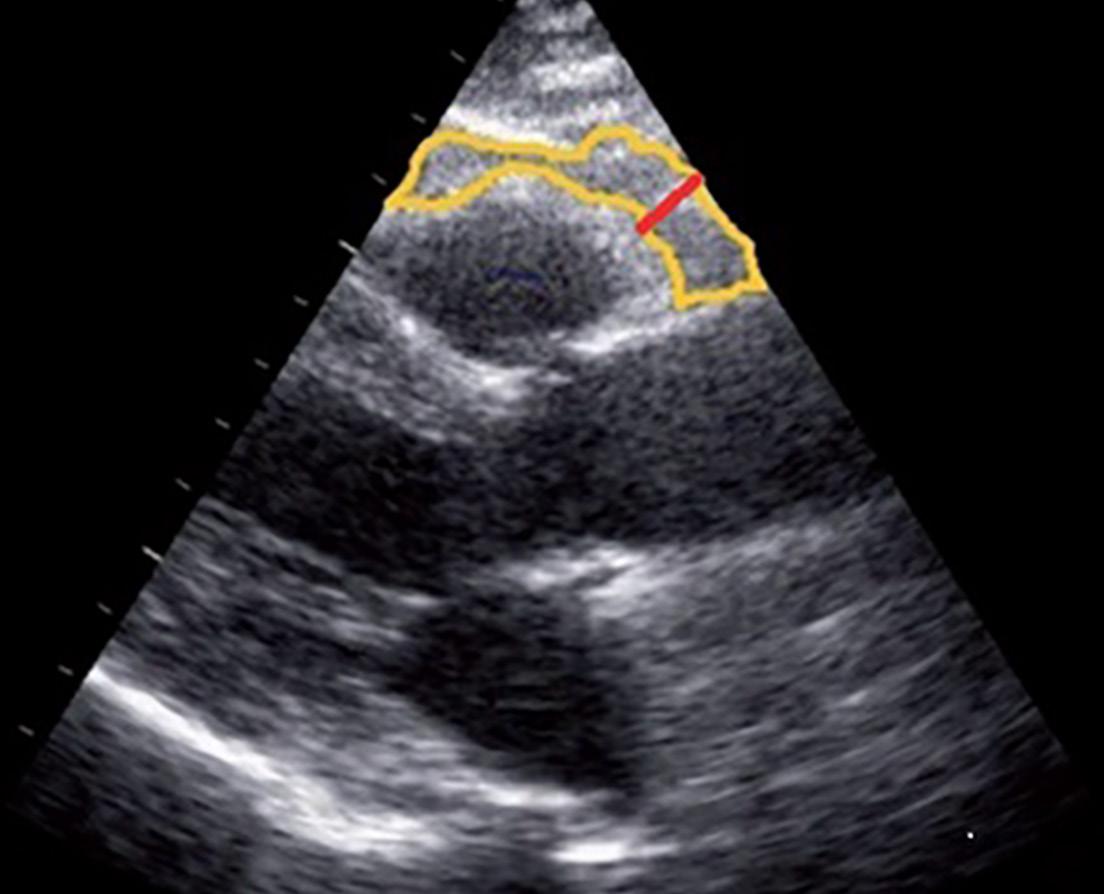
But in 2003, Dr. Iacobellis discovered that a standard ultrasound machine could do the job in the convenience of an outpatient clinical setting. Thanks to this inexpensive, noninvasive procedure he developed, healthcare professionals can not only detect and measure epicardial adipose tissue (EAT) but also predict and prevent diseases often associated with it.
After establishing a method to quantify EAT, Dr. Iacobellis set out to learn how the tissue responds to current drugs that have shown so much promise in treating diabetes and reducing overall fat: GLP-1As. GLP-1As, and more recent dual GLP-1-glucose-dependent insulinotropic polypeptide (GIP) agonists, work by mimicking the hormones that modulate the complex interaction between the gastrointestinal system and the brain that processes hunger and satiety. Marketed under names like Ozempic, Wegovy, Trulicity, Rybelsus, Mounjaro, and Zepbound, these drugs initially were manufactured to lower blood sugar levels in people with type 2
diabetes. Some of these medications now have been approved exclusively for weight loss or cardiovascular protection in people with type 2 diabetes.
With previous weight loss drugs, patients could expect a 5 to 10 percent weight loss but then regain much of the weight after discontinuing the medication. Newer GLP-1As and dual agonists increased those numbers to 20 and close to 25 percent. (For purposes of comparison, bariatric surgery can result in approximately 30 percent weight reduction.) However, more longitudinal studies are needed to evaluate the long-term effects of these drugs.
Hunger and satiety control is only one of the mechanisms behind the effects of these drugs. Dr. Iacobellis began researching how and which GLP-1As directly affect epicardial fat. Through his work, he found that not only can GLP-1As target this specific tissue, these drugs can help improve the condition of multiple organs,
including the heart, kidneys, and liver. (Recent studies have even suggested GLP-1As’ value in treating cancer.)
However, Dr. Iacobellis says that targeting adipose tissue is really the priority, since some of the beneficial effects come from the mediation and modulation of the fat. This is good news for patients who are not at obvious risk.
“When the medication targets and modulates GLP-1 receptors (a discovery made by Dr. Iacobellis’ group) there are profound changes within the adipose tissue of the heart. Not only does the adipose tissue of the heart shrink, but there are also important changes that help the heart better utilize some of the metabolites, including the lipids – the fat by itself,” explains Dr. Iacobellis, who is the author of 160 articles and 11 books on the topic. “Essentially, the medications make the heart’s adipose tissue function more efficiently. This is a major breakthrough because it explains how these drugs not only
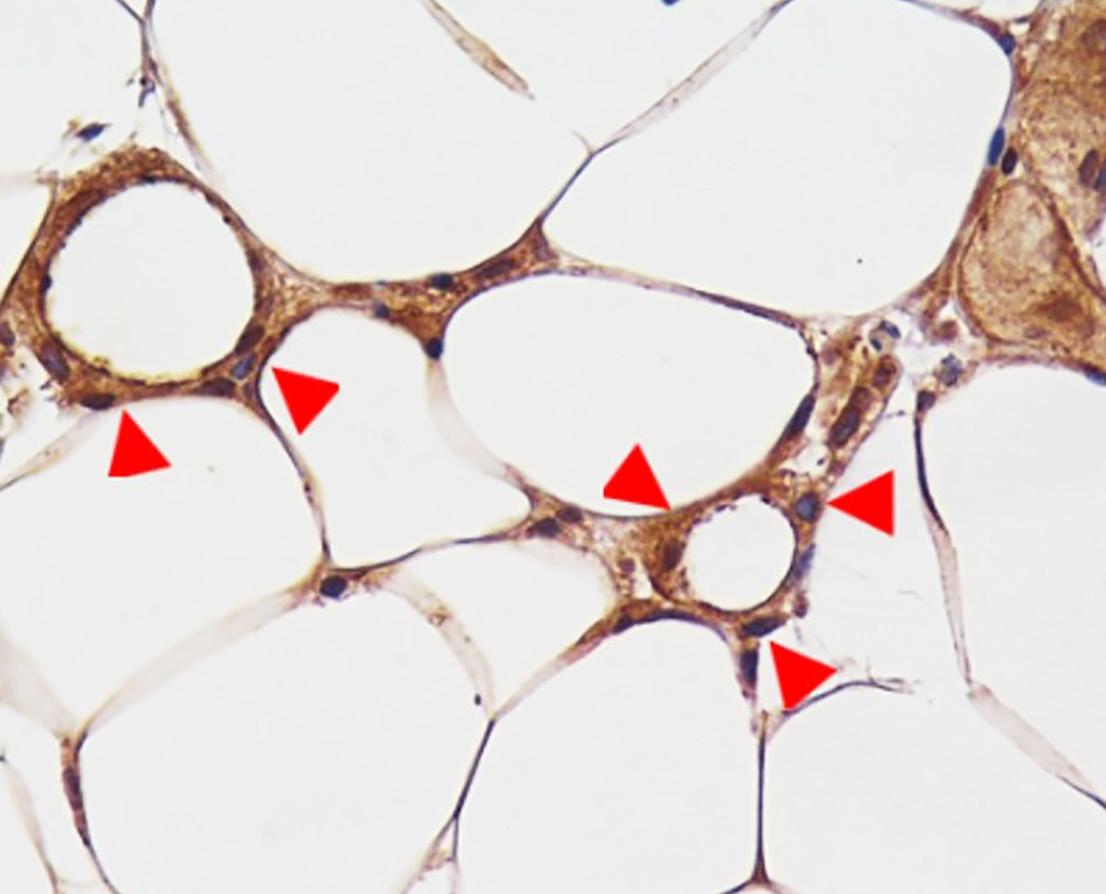
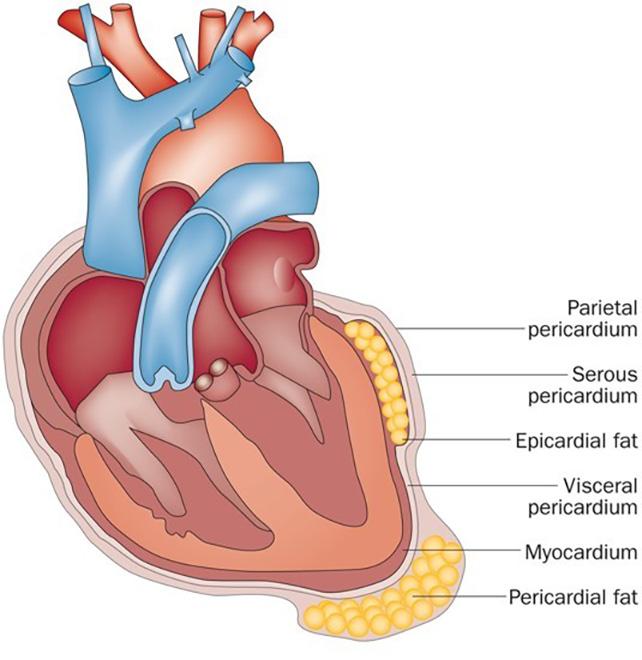
(Top left) Dr. Iacobellis’ group first discovered the presence of the receptors of the GLP-1 analogs (shown by the red arrows) within the epicardial adipocytes, highly suggesting that the beneficial cardiovascular effects of the GLP-1 analogs are mediated by epicardial fat. (Top right) Dr. Iacobellis invented a technique to measure the epicardial fat thickness (within the yellow line) using standard and not invasive ultrasound.
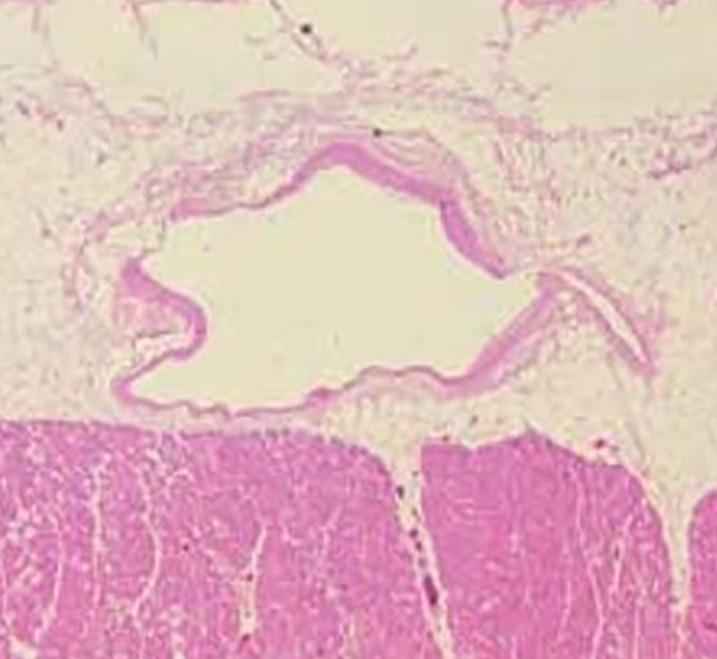
(Bottom left) This illustration depicts the macro-anatomy of the epicardial adipose tissue infiltrating and surrounding the heart. (Bottom right) This microscopic image shows the unobstructed proximity of the epicardial adipose tissue to the underlying myocardium. This feature, unique to the epicardial fat, was first discovered by Dr. Iacobellis’ group, and allows the cross-talk between the fat and the heart.
aid in weight loss and diabetes management but also provide significant cardiovascular benefits to patients.”
In the future, newer GLP-1As will facilitate precision medicine with customized treatment options for patients. Different drugs will target different fat-inducing mechanisms, and it will be possible to predict how a patient metabolizes and responds to one specific GLP-1A over another.
The combination of Dr. Iacobellis’ work and recent pharmaceutical advancements are clearly transforming healthcare and ushering patients into a new, improved era.
“It’s definitely revolutionary,” he adds.
In-Person Encounters for UHealth 30% from Department of Medicine 70% from All Other Departments
Tele-Medicine Encounters for UHealth 14% from Department of Medicine 86% from All Other Departments
Total Revenue for UHealth
17% from Department of Medicine
83% from All Other Departments






























PROGRAM DIRECTORS
RESIDENCIES
Stefanie Brown, M.D., M.B.A. Internal Medicine





















































































Jonathan Tolentino, M.D. Internal Medicine-Pediatrics









































































FELLOWSHIPS
Carlos Alfonso, M.D.
Cardiovascular
E. Joseph Bauerlein, M.D.
Cardiovascular – Advanced Heart Failure/Transplant
Raul Mitrani, M.D. Cardiovascular – Electrophysiology
Michael Dyal, M.D. Cardiovascular – Interventional Cardiology
Eduardo de Marchena, M.D. Cardiovascular – Interventional Structural HD Fellow Non-ACGME
Violet Lagari-Libhaber, D.O. Endocrinology
Morgan Sendzischew-Shane, M.D. Gastroenterology
Iriana Hammel, M.D. Geriatrics
Janaki Sharma, M.D. Hematology/Oncology
Eric Martin, M.D. Hepatology
Mariana Khawand-Azoulai, M.D. Hospice and Palliative Care
Jose Gonzales-Zamora, M.D. Infectious Diseases
Shweta Anjan, M.D. Transplant Infectious Disease Non-ACGME
Zain Mithani, M.D. Nephrology
Rachel Damico, M.D. Pulmonary/Critical Care
Carlos Lozada, M.D. Rheumatology
The Division of Cardiovascular Medicine witnessed many clinical advancements over the past year. In FY2024, outpatient clinic volume increased by 17 percent, with providers seeing 35,000 patients, including more than 9,000 new patient visits.
Patient schedule fill rates rose from 88 percent to 98 percent, thanks to improvements in the division’s centralized scheduling system. The new structure and workflow within the clinic, utilizing clinic navigators, reduced wait times from 60 to 30 days and decreased the number of no-show rates significantly. Additionally, the division’s new atrial fibrillation (AFib) center increased ablation procedures by 3 percent, bringing the total number of AFib ablations to 160.
The division expanded weekend operations for outpatient echocardiograms at UHealth Tower, which is being overseen by Mehrdad Ghahramani, M.D., F.A.C.C., Director of Echocardiography.
Efforts to reduce wait times have improved patient flow and overall patient satisfaction. Centralizing the echo reading panel has standardized quality and sped up test reviews. Additionally, CME-accredited monthly echo lectures now enhance the professional development of sonographers, trainees, and cardiologists. To improve the patient
experience, the division has also created the Echocardiography Laboratory Patient Guide and is developing similar informational booklets for preventive cardiology and catheterization lab procedures.

Dr. Lambrakos performed UHealth’s first procedure with Medtronic’s Aurora Ev-ICD system, enhancing patient outcomes and safety.
The Cardiovascular Division raised significant federal research funding. Jeffrey Goldberger, M.D., M.B.A., received a $7.9 million, five-year award for the CINEMAS project, assessing predictive markers for recurrent stroke in patients with embolic stroke of undetermined source. Yiannis Chatzizisis, M.D., Ph.D., leads the Center for Digital Cardiovascular Innovations, developing computational tools to guide cardiovascular interventions. Joshua Hare, M.D. is expanding studies on using stem cell therapies for heart repair.
In 2024, the Heart Month Campaign was the second largest in Heart Aware history, with 2,247 patients completing the online health risk assessment at a 93 percent completion rate. An impressive 86 percent of these patients underwent coronary artery calcium screenings, exceeding the national average. Nearly 1,500 CT calcium scans were conducted across four locations, supported by our multi-disciplinary teams and streamlined workflow.
The 2024 Miami Valves Conference, organized by Eduardo De Marchena, M.D., attracted close to 400 specialists from the U.S., Latin America, and Europe. Several division cardiologists attended the Caribbean Society of Cardiology Conference, forging relationships with neighboring cardiologists.
Recently, UHealth Cardiology, Heart, and Vascular Surgery was recognized as a high-performing center for treating heart attack, aortic valve disease, and heart failure, achieving the highest score in South Florida, according to U.S. News and World Report.
Raul Mitrani, M.D., performed three pulsed field ablations (PFA), establishing the University of Miami Miller School of Medicine as the first academic medical center and one of the few programs in Florida to offer this technology.


YIANNIS S. CHATZIZISIS, M.D., PH.D.
Chief
PROFESSORS
Simon C. Chakko, M.D. (Emeritus)
Yiannis S. Chatzizisis, M.D, Ph.D.
Eduardo J. De Marchena, M.D.
Chunming Dong, M.D.
Jeffrey Goldberger, M.D., M.B.A.
Joshua M. Hare, M.D.
Robert J. Myerburg, M.D. (Emeritus)
Rafael Sequeira, M.D. (Emeritus)
PROFESSORS OF CLINICAL MEDICINE
Carlos E. Alfonso, M.D.
Maureen H. Lowery, M.D. (Emeritus)
Claudia Martinez, M.D.
Raul Mitrani, M.D.
RESEARCH PROFESSOR
Lina Shehadeh, Ph.D.
ASSOCIATE PROFESSOR
Martin S. Bilsker, M.D. (Emeritus)
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Eugene J. Bauerlein, M.D.
Pedro Cox, M.D. (Pending Rank)
Litsa K. Lambrakos, M.D.
George Marzouka, M.D.
Alan H. Schob, M.D.
RESEARCH ASSOCIATE PROFESSOR
Wayne Balkan, Ph.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Sharon N. Andrade-Bucknor, M.D.
Pedro Covas, M.D.
Michael Dyal, M.D.
Joseph Esterson, M.D.
Mrudula Munagala, M.D.
Nikolaos Spilias, M.D., performed same-day patient discharge in the division’s Transcatheter Aortic Valve Replacement (TAVR) Program.
Maria Delgado-Lelievre, M.D., is pioneering a new blood pressure patch by Biobeat.
Litsa Lambrakos, M.D., performed UHealth’s first procedure using the Medtronic’s Aurora Ev-ICD system, a type of implantable cardioverterdefibrillator designed to manage and treat certain heart rhythm disorders.
Dr. Chatzizisis and Dr. Spilias performed the first renal denervation procedure in Florida and are among the first in the nation to treat arterial hypertension using this procedure. Renal denervation treats
Nikolaos Spilias, M.D.
Robert B. Stang, M.D.
Alex Velasquez, M.D.
RESEARCH ASSISTANT PROFESSORS
Jose Manuel Condor, Ph.D.
Martin Liu, M.D., Ph.D.
Wei Wu, Ph.D.
Shijia Zhao, Ph.D.
STAFF PHYSICIANS
Beteal Ashinne, M.D., M.P.H.
Antonio Barquet-Leon, M.D.
Andrew Bromley, M.D.
Hoda Butrous, M.D.
George Degheim, M.D.
Murry Drescher, M.D.
Thanh Duong-Wagner, M.D.
Mehrdad Ghahramani, M.D.
David Weininger, M.D.
Zachariah Zachariah, M.D.
FELLOWS
CARDIOVASCULAR DISEASE
First Year
Saahil Jumkhawala, M.D.
Fabricio Malaguez Webber, M.D.
Alan Mendez Ruiz, M.D.
Nicole Parellada, M.D.
Anastasios Roumeliotis, M.D.
Julio Cesar Santana, M.D.
Andrew Sephien, M.D.
arterial hypertension by targeting the sympathetic nerves that are located around the renal arteries. The procedure recently received FDA clearance to be used as an adjunct to medical therapy for the treatment of hypertension.
Second Year
Mohammed Ali, M.D.
Marina Byer, M.D.
Trevor I. Eisenberg, M.D.
Rafael J. Hernandez, M.D.
Beatriz P. R. Rodriguez, M.D.
Francisco J. Romeo, M.D.
Nayrana Tillman, M.D.
Third Year
Urvashi Hooda, M.D.
Fatima Lakhani, M.D.
Victor Y. Razuk, M.D.
Phillip Rubin, M.D.
Rahul B. Sheth, M.D.
Avinash A. Vernekar, M.D.
Louis T. Vincent, M.D.
INTERVENTIONAL CARDIOLOGY
Matthew M. Borkovich, M.D.
Bertrand F. Ebner, M.D.
Alam Zenith, M.D.
INTERVENTIONAL STRUCTURAL HEART DISEASE
Som Aftabi Bailey, M.D.
CLINICAL CARDIAC ELECTROPHYSIOLOGY
Yaniv Gura, M.D.
George Leonor-Lopez, M.D.

Dr. Chatzizisis and Dr. Spilias (center) performed Florida’s first renal denervation procedure. Renal denervation recently received FDA clearance to be used as an adjunct to medical therapy for the treatment of hypertension.
Under Dr. Chatzizisis’ leadership, the division was the first academic center in Florida and among the first centers in the country to use a drug-coated balloon (DCB) for the treatment of in-stent restenosis. In cases of in-stent
restenosis, a drug-coated balloon can be used to treat the narrowed area through catheter insertion, balloon inflation, and drug release.
Researchers from the Division of Clinical Pharmacology continue their work on several pivotal research studies. One such study examines the protection of bone marrow function in patients with lung cancer using a medication called trilaciclib. Trilaciclib is a first-in-class drug approved for reducing the incidence of chemotherapy-induced myelosuppression in adult patients with extensive-stage small cell lung cancer.
Trilaciclib has been shown to protect bone marrow cells from the detrimental effects of chemotherapy and reduce the occurrence of myelosuppression, a serious complication commonly associated with cancer treatment.
Myelosuppression is characterized by a decline in the production of red blood cells, white blood cells, and platelets, which can lead to anemia, infections, and bleeding.
Notably, trilaciclib is the first drug of its kind to receive approval from the U.S. Food and Drug Administration (FDA) for this indication, specifically
for patients with extensive-stage small cell lung cancer who are undergoing chemotherapy with a platinum/ etoposide-containing or topotecancontaining regimen.
Another open-label, parallelgroup study examined the impact of moderate and severe hepatic impairment on the pharmacokinetics of trilaciclib.
Approximately 4.5 million people in the United States have been diagnosed with liver disease but estimates indicate that many more have underlying subclinical liver disease. Approximately 827,000 patients have the diagnosis of cirrhosis and 51,642 patients died from liver disease in 2020.
The liver is central to the elimination of many drugs via phase I Cytochrome P450 metabolism, phase II conjugative reactions, or direct elimination of intact drug or metabolites via biliary excretion. Accordingly, the FDA has mandated that new compounds undergo PK/ safety studies in patients with hepatic impairment to demonstrate the effect

of liver disease on the elimination and safety profiles of these new drugs. It is known that mild hepatic impairment has no effect on the exposure of trilaciclib. However, patients with moderate and severe hepatic impairment were excluded from the clinical trials and there is a need to investigate the effect of moderate and severe hepatic dysfunction on trilaciclib PK. This study was conducted to characterize the impact of moderate and severe hepatic impairment on the PK of trilaciclib to inform dosing recommendations in participants with chronic liver disease.
Results from the study will allow the safe and rational administration of trilaciclib in patients with lung cancer and concomitant liver disease.
Early education efforts within the division focus on preventing adverse drug reactions. One ongoing initiative in this area is a clinical pharmacology course designed to integrate clinical pharmacology into the research and

training of residents, fellows, and faculty.
An adverse drug reaction (ADR) is a noxious response to a drug at the usual therapeutic dose. These adverse drug reactions happen much more often than anticipated. There are an estimated 2.2 million serious ADRs and more than 100,000 deaths caused by ADRs each year. In fact, ADRs contribute to 2 million hospital stays and 3.5 million office visits per year.
The economic burden of ADRs is estimated to be approximately $30.1 billion per year in the United States. Extensive national efforts to prevent ADRs and adverse drug events have been instituted, including the National Action Plan for ADE Prevention (Health. gov), pharmacy safety measures and automatic warnings, and software to predict ADR/drug interactions.
The Division of Clinical Pharmacology has adopted a physician-centric approach to the problem of ADRs: teaching the fundamentals of clinical pharmacology to medical residents, fellows, and faculty.
In the first segment of the course, participants will thoroughly learn the

basics of clinical pharmacokinetics.
The next segment is a series on clinical pharmacokinetics, liver metabolism of drugs, drug interactions, effects of organ dysfunction, and pharmacogenetics.
Learners will also discover how the kidney eliminates medicines from the body and the effects of kidney disease on proper dosing of medications.
The first class to access this updated curriculum completed the course in February 2024. Additional material and clinical exercises will be added prior to the upcoming academic year.
The division has moved its Phase I Research Center to the fifth floor of Dominion Tower. This expanded space will enable researchers to conduct larger studies, provide better educational facilities, and facilitate potential collaborations with investigators from other divisions.

RICHARD A. PRESTON, M.D., M.S.P.H., M.B.A. Division Chief
PROFESSOR OF CLINICAL MEDICINE
Richard A. Preston, M.D., M.S.P.H., M.B.A.

The Division of Digestive Health and Liver Diseases is expanding its clinical services across Miami-Dade County, which includes a current practice site in Doral and a future site planned for North Miami. Similar to the Lennar Foundation Medical Center in Coral Gables, the division will offer office-based gastroenterology and endoscopy services at these locations. Additionally, the division continues to offer a range of advanced

endoscopic procedures, including those for biliary tract disease, as well as exploring such novel areas as weight management.
The advanced endoscopy team has been successful in recruiting internationally renowned endoscopist Fabian Emura, M.D. to the division. Dr. Emura recently received the Master Endoscopist Award from the World Endoscopy Organization at its annual ENDO 2024 Conference last June.
The division continues to offer diagnostic and therapeutic interventions. In functional bowel disease and motility, Daniel Sussman, M.D., has continued to expand his clinic devoted to genetic gastrointestinal syndromes.
The Crohn’s and Colitis Center continues to act as a hub of innovation. A number of important papers have been published by this group over this past year, including insights into the effect of diet on the emergence of Crohn’s disease in immigrants to the United States. Maria Abreu, M.D.’s NIH-

funded lab continues to investigate basic mechanisms in the pathogenesis of inflammatory bowel disease (IBD).
The Crohn’s and Colitis Center has introduced gastrointestinal ultrasound to provide non-invasive monitoring for patients with Crohn’s disease and ulcerative colitis. The center is one of just a few programs in the United States offering this service.
In hepatology, several areas are being actively researched. These include the management of cholestatic liver disease, alcohol-related disorders, fatty liver disease, and viral hepatitis.
David Goldberg, M.D., M.S.C.E., continues his NIH-funded research on donor organ allocation and liver transplantation. In FY2024, his research was highlighted by two impactful publications that led to rule changes by the Centers for Medicine and Medicaid Services (CMS) and citation by the Senate Finance Committee.
The division continues to offer sophisticated medical and therapeutic interventions through its Pancreas Center, the only National Pancreas Foundation-certified Academic Center

PAUL MARTIN, M.D. Division Chief
PROFESSORS
Maria T. Abreu, M.D.
Jaime S. Barkin, M.D. (Emeritus)
Paul Martin, M.D.
Jeffrey B. Raskin, M.D. (Emeritus)
PROFESSORS OF CLINICAL MEDICINE
Amar Deshpande, M.D.
Cynthia Levy, M.D.
Daniel Sussman, M.D., M.S.P.H
ASSOCIATE PROFESSOR
David Goldberg, M.D., M.S.C.E.
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Sunil Amin, M.D., M.P.H.
Jodie Barkin, M.D.
Oriana Damas, M.D., M.S.C.T.I.
Jose Garrido, M.D.
Binu John, M.D. (Pending Rank)
Patricia Jones, M.D., M.S.C.R.
David Kerman, M.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Sean Bhalla, M.D.
Shria Kumar, M.D., M.S.C.E.
Emory Manten, M.D.
of Excellence in Pancreatitis and Pancreatic Cancer in the southern half of Florida.
In collaboration with our surgical and endocrinology colleagues, the division has initiated total pancreatectomy with islet cell autotransplantation (TPIAT) procedures for recurrent acute and chronic pancreatitis. Another project is a prospective multi-site national registry for exocrine pancreatic insufficiency.
As part of its educational mission, the division continues to train fellows in general gastroenterology, advanced hepatology, and advanced endoscopy. The robust educational program invites participation from both within the University and from colleagues across the community.
Shria Kumar, M.D., M.S.C.E., was awarded a traveling fellowship for
Eric Martin, M.D.
Il Joon Paik, M.D.
Siobhan Proksell, M.D.
Andrew Scheinberg, M.D.
Morgan Sendzischew Shane, M.D., M.S.C.T.I.
Ami Panara Shukla, M.D.
Joshua Turkeltaub, M.D.
STAFF PHYSICIANS
Paul Bermanski, M.D. (Per Diem)
Fabian Emura, M.D.
Mahmoud Mahfouz, M.D.
Michelle Pearlman, M.D. (Per Diem)
FELLOWS
GASTROENTEROLOGY DISEASE FELLOWS First Year
Helen Bermudez, M.D.
Keri Ann Buchanan-Peart, M.D.
Jonathan Gross, M.D.
Gala Martinez Godoy Brewer, M.D.
Myra Quiroga, M.D. Second Year
Chaitra Banala, M.D.
Nisa Desai, M.D.
Lauren L. Johnson, M.D.
Rahil H. Shah, M.D.
Shyam Vedantam, M.D. Third Year
Camilo J. Acosta, M.D.
Joseph H. Cioffi, M.D.
Stephanie Ioannou, M.D.
Smriti Kumar, M.D.
Elaheh Niroomand, M.D.
Sunny Sandhu, M.D.
TRANSPLANT HEPATOLOGY FELLOW
Jaimy Villavicencio Kim, M.D. ADVANCED ENDOSCOPY FELLOW
Abid Javed, M.D. (Clinical Instructor)
INFLAMMATORY BOWEL DISEASE FELLOW
Gabriella Alexandra Raffa, M.D. (Clinical Instructor)

The division’s 2024 GI fellows and faculty members.
her work in gastrointestinal cancer. The division’s fellowship program now includes an advanced endoscopy fellow each year.
The Division of Digestive Health and Liver Diseases continues to gain a growing national and international
reputation. Dr. Abreu, Director of the Crohn’s and Colitis Center, assumed the role of President of the American Gastroenterological Association (AGA). She is the first Latina president of AGA, the 16,000-member professional association dedicated to eradicating digestive diseases.
The Division of Endocrinology, Diabetes, and Metabolism has significantly expanded its clinical practice with the addition of three new physicians: Ashley Engel, M.D., Ayse Canturk, M.D., and Ron Varghese, M.D. This recruitment has been enhanced by adding a highly qualified team of advanced practice providers (APPs) to support the division’s clinical efforts. In addition, the division has extended its clinical services to various clinics in Broward County, improving patient care and access to services.
A new pituitary clinic, which offers advanced care for patients both before and after surgery, was also launched. Led by Carmen Villabona, M.D., the team includes Dr. Engel, physician assistant Ariana Chirinos, an endocrinology fellow, and various nurse navigators for triage and immediate

postoperative care. This collaboration has resulted in notable low readmission rates for pituitary cases.
Under the leadership of Violet Lagari-Libhaber, D.O., and Dr. Canturk, the division’s bone clinic has expanded its reach by extending specialized bone care to the Women’s Health Alliance.
In collaboration with Naresh Punjabi, M.D., Ph.D., from the Division of Pulmonary, Critical Care, and Sleep Medicine, Dr. Varghese has co-developed a clinical and research program focusing on obesity and obstructive sleep apnea.
Under the leadership of Mark Jara, M.D., the division has advanced the treatment of thyroid cancer and established a thyroid cancer survivorship clinic with the support of physician assistant Simran Shikh.
These new initiatives complement the division’s established strengths in diabetes care. The expertly trained diabetes team, which is comprised of Bresta Miranda, M.D., David Baidal, M.D., Gianluca Iacobellis, M.D., Ph.D., Francesco Vendrame, M.D., Ph.D., Rodolfo Galindo, M.D., and Ernesto Bernal-Mizrachi, M.D., remains at the forefront of advancements in diabetes technology and podiatry services, led by Jason Levine, D.P.M. The division’s outstanding reputation in diabetes care has earned it national recognition by U.S. News & World Report.

The division maintains a strong research presence within the Department of Medicine, securing the second-highest level of research funding.
Additionally, Matthias von Herrath, M.D., a world-renowned immunologist, has been named the new director of the Diabetes Research Institute.
The division’s basic research efforts in diabetes and islet biology continue to receive national acclaim. Manuel Blandino-Rosano, Ph.D., received R01 funding for research on dynorphin in paracrine regulation of insulin secretion. Such work highlights the division’s extensive basic research grant portfolio, which includes key contributions from Alejandro CaicedoVierkant, Ph.D., Joana Almaca, Ph.D., Rene Barro-Soria, Ph.D., Ernesto Bernal-Mizrachi, M.D., and Rayner Rodriguez-Diaz, Ph.D.
Dr. Caicedo-Vierkant’s work on rescuing glucagon secretion in type 1 diabetes and the nervous system’s role in insulin secretion has significant clinical implications. Complementing this, Dr. Rodriguez-Diaz and Dr. Almaca’s studies on islet vasculature and hormone secretion have received national and international recognition.
Ruy Andrade Louzada, Ph.D. and Dr. Bernal-Mizrachi’s research, in collaboration with Andrew Schally, Ph.D., M.D. (hc), has uncovered the potential of growth hormone-releasing hormone agonists as a treatment for type 1 diabetes.
Rodolfo Galindo, M.D., has been involved in major national committees and his NIH-funded research on diabetes management in chronic kidney failure complements the research of Dr. Iacobellis on epicardial fat, in collaboration with Jeffrey Goldberger, M.D., M.B.A., from the Division of Cardiovascular Medicine.
Dr. Vendrame was named the national co-chair for the Type 1 Diabetes Exchange Program, which focuses on technology use in underrepresented minorities, while David Baidal, M.D., is currently an investigator for TrialNet.
Supported by the Georgia Center for Diabetes Translation Research Pilot and Feasibility Program, Diana Soliman, M.D., is exploring the utility and acceptance of continuous glucose monitor (CGM) use among Hispanic patients with diabetes. In addition, Ronald Goldberg, M.D., as site PI for the Diabetes Prevention Program, has partnered with Dr. Soliman to expand this study and apply artificial intelligence in diabetes, in collaboration with Yelena Yesha, Ph.D., Knight Foundation Endowed Chair of Data Science and AI, at the Frost Institute for Data Science.
Education is fundamental to our mission. The division’s fellowship program, under the leadership of Dr. LagariLibhaber and Zeina Hannoush, M.D., continues to provide high-quality training to fellows, reflecting a commitment to educating and preparing the next generation of endocrinology specialists. Dr. Hannoush also significantly contributes to developing medical school curriculums and Dr. Soliman serves as associate program director for the Internal Medicine Residency Program.
Dr. Galindo serves as Chair of the American Association of Clinical Endocrinology’s (AACE) Obesity and Nutrition, Disease State Networks (DSN) Committee as well as Chair of the Endocrine Society’s Tenth Type 1 Diabetes Endocrine Fellows Forum. He is also a member of the Diabetes

Division Chief
PROFESSORS
Rodolfo Alejandro, M.D.
Ernesto Bernal-Mizrachi, M.D.
Alejandro CaicedoVierkant, Ph.D.
Ronald Goldberg, M.D.
Alberto Pugliese, M.D. (Emeritus)
Jay Skyler, M.D.
Jay Sosenko, M.D.
Roy E. Weiss, M.D., Ph.D.
PROFESSOR OF CLINICAL MEDICINE
Gianluca Iacobellis, M.D., Ph.D.
RESEARCH PROFESSOR
Ricardo Pastori, Ph.D. ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Rodolfo Galindo, M.D.
Zeina Hannoush, M.D.
Violet Lagari-Libhaber, D.O.
Francesco Vendrame, M.D., Ph.D.
RESEARCH ASSOCIATE PROFESSOR
Armando Mendez, Ph.D.
ASSISTANT PROFESSORS
Joana Almaça, Ph.D.
Rene Barro-Soria, Ph.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
David Baidal, M.D.
Ayse Canturk, M.D.
Mark Jara, M.D.
Jason Levine, D.P.M.
Diana Soliman, M.D.
Ron Varghese, M.D.
Technology Society Consensus Meeting, Use of CGM in Chronic Kidney Disease, 2024.
Dr. Caicedo was elected as a member of the planning committee for the scientific session of the American Diabetes Association.
Dr. Bernal-Mizrachi is a member of the planning committee for the ENDO society meeting and was invited to become a National Advisory Committee (NAC) member of DiabDocs.
Dr. Soliman is a co-investigator (along with Dr. Goldberg) of the Diabetes Prevention Program Outcome Study Phase 4 (DPPOS-4). She is also a member of the Diabetes Prevention Program Diversity, Outcomes, Inclusion Team and a member of the Type 1 Diabetes
RESEARCH ASSISTANT PROFESSORS
Ruy Andrade Louzada Neto, Ph.D.
Manuel Blandino, Ph.D.
Joana Lemos Oliviera, Ph.D.
Rahul Mittal, Ph.D.
Rayner Rodriguez-Diaz, Ph.D.
Joao Saar Werneck De Castro, Ph.D.
STAFF PHYSICIANS
Ashley Engel, M.D.
Silvia Gra Menendez, M.D.
Bresta Miranda, M.D. Anu Thekkumkattil, M.D.
Carmen Villabona, M.D. FELLOWS
First Year
Crystal M. Acosta, MD
Marie L. Aoun, M.D.
Karla A. Baez Rodriguez, M.D.
Ayoola Omobolande Olayiwola, M.D.
Second Year
Hery A. Mejia, M.D.
Alejandra Razzeto, M.D.
Susana B. Sacco, M.D.
Renato R. Savian, M.D.
Exchange Health Care Transition Workgroup.
Dr. Barro-Soria is a permanent member of the Drug Discovery and Molecular Pharmacology B (DMPB) Study Section, NIH Center for Scientific Review (CSR), as well as a permanent member of the Curator Committee of Biophysics-Colab peer review system.
Dr. Iacobellis was an invited speaker on epicardial fat research at the University Hospital Albert Einstein College in New York City, NY in March 2024 and presented the Dinon Lecture at Thomas Jefferson University in Philadelphia, PA in September 2023. He also published two papers in the Journal of the American College of Cardiology (JACC) (IF 24) and JAMA Cardiology (IF 24) in press.
The Division of General Internal Medicine explored the impact of disruptors, including artificial intelligence (AI), changes in technology, and novel medical education paradigms. It has been a productive year, with faculty producing work poised to transform medical education, and ultimately, the practice of medicine.
Aiming to transform the face of medicine here and abroad, Sonjia Kenya Harris, Ph.D., and Olveen Carrasquillo, M.D., M.P.H., along with
Deborah Jones Weiss, Ph.D., of the Miller School of Medicine’s Department of Psychiatry and Behavioral Sciences, initiated the Cardiovascular Research Empowerment Workforce Program, an R25 grant designed to cultivate interest and inform selected U.S. Virgin Islands undergraduate students in cardiovascular research and healthcare.
Ultimately, the program aims to expand the number of researchoriented healthcare providers in the U.S. Virgin Islands. Additionally, Dr. Kenya Harris and Dr. Carrasquillo

serve on the advisory board of the inaugural University of the Virgin Islands School of Medicine.
Faculty within the division made leading contributions to the Miller School of Medicine’s educational mission. As longitudinal clinical educators, program directors, and curriculum deans, faculty members continue to play pivotal roles across the educational continuum. In fact, division faculty received 14 of the 30 recognition of educational contribution merit awards that were granted to the Department of Medicine.
Paul Mendez, M.D., was recognized with the Excellence in Medical Education Award by the Department of Medicine while the dean recognized Sabrina Taldone, M.D., M.B.A., with the Faculty Citizenship Award and presented Hiram Rodriguez, M.D., and Sudha Lolayekar, M.D., with the Faculty Award for Service Excellence.
Dr. Taldone, far right with award, and Dr. Lolayekar, far left with award, two of the 2023 Dean Faculty Award recipients.

Interim Division Chief
PROFESSORS
Olveen Carrasquillo, M.D., M.P.H.
Laurence Gardner, M.D.
Kenneth Goodman, Ph.D.
S. Barry Issenberg, M.D.
PROFESSORS OF CLINICAL MEDICINE
Panagiota Caralis, M.D., J.D.
Daniel Lichtstein, M.D. (Emeritus)
Erin Marcus, M.D., M.P.H.
Joan St. Onge, M.D.
Ross Scalese, M.D.
PROFESSOR, EDUCATOR
Sonjia Kenya Harris, Ph.D.
ASSOCIATE PROFESSOR
Mark Gelbard, M.D. (Emeritus)
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Yvonne Diaz, M.D.
Hilit Mechaber, M.D.
Paul Mendez, M.D.
Maritza Suarez, M.D.
Frederick Williams, M.D.
Barry Issenberg, M.D., Director of the Gordon Center for Simulation and Innovation in Medical Education and Senior Associate Dean for Research in Medical Education, was elected President of the Society for Simulation in Healthcare. In this role, Dr. Issenberg provides strategic leadership and vision to this international organization, which seeks to improve healthcare quality, clinical performance, and patient safety through the use of simulation and other educational technologies.
AI will undoubtedly exert profound impact on the future of medicine.
Gauri Agarwal, M.D., F.A.C.P., has been integrating AI and the humanities into the curriculum to help students leverage AI to improve healthcare outcomes. Dr. Agarwal was also honored as a Gold Humanism Scholar for her novel curriculum that incorporates the humanities with AI applications in clinical practice.
As the co-director of the Global Institute at the University of
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Gauri Agarwal, M.D.
Howard Anapol, MD
Sarah Bland, M.D.
Stephanie Clauss, D.O.
Gregory Coleman M.D. Janelle Cuervo, D.O. Nemer Dabage-Forzoli, M.D. Elizabeth Greig, M.D. Janelis Gonzalez, M.D. Lilliam Guzman M.D. Brian Hagenlocker, M.D. Melanie Helfman, M.D.
Margarita Llinas M.D. Cristina Pravia, M.D. Anita Sikha, M.D. Katelin Snow, M.D. Sabrina Taldone, M.D. Jacobo Wajner, M.D.

Miami Miller School of Medicine, Elizabeth Greig, M.D., is changing the face of disaster responsiveness by focusing on primary care, strengthening resilience, and in
STAFF PHYSICIANS
Alexandra Calandriello, M.D.
Manuela Calvo, M.D.
Adria Cruz Labrada, M.D.
Ana de Diego, M.D.
Grettel Garcia, M.D. Janella Leon, D.O. Sudha Lolayekar, M.D. Marie Normil, M.D. Hiram Rodriguez, M.D. Nisha Verma, M.D.

Dr. Greig directs a simulation exercise with the Jamaican Defense Force and the United States Navy in Kingston, Jamaica after Hurricane Beryl.
selected sectors, preparing responders for thermal-related health threats. Her initiatives will inform a transformative evolution in disaster-related crisis management.
The Division of Geriatrics and Palliative Medicine, led by Division Chief Marcio Rotta Soares, M.D., continues to deliver on its mission of providing exceptional patient care to the elderly population of South Florida as well as patients suffering from serious illnesses.
The division continues to act as a regional leader in clinical care and education in the areas of geriatric
medicine as well as hospice and palliative medicine. The division was also ranked as a high-performing specialty in U.S. News and World Report’s 2024 ranking.
The division’s outpatient geriatric medicine service line continues to conduct comprehensive geriatric assessments on older patients at the Miami downtown and Coral Gables outpatient locations.
To meet the needs of patients suffering with serious illness, the palliative medicine team continues to expand its outpatient network. By expanding its presence in more geographic locations, the division is enhancing the delivery of high-quality symptom management and patientcentered palliative care to more patients in the community. Outpatient locations include Downtown Miami,

South Miami, Coral Gables, Deerfield, and Plantation. The division also offers telemedicine consults.
The division’s inpatient palliative medicine consult service provides care to patients admitted to UHealth Tower. This inpatient practice focuses on symptom management as well as transitions of care for those patients with serious, complex, and/or terminal illnesses.

Mariana Khawand-Azoulai, M.D., received an anonymous $250,000 donation to support clinical growth and promote educational mission in palliative medicine.
Michael Huber, M.D., was recognized as an emerging leader and received the Leadership Scholar Award in Palliative Medicine from the American Academy of Hospice and Palliative Medicine. He was also appointed to their Quality Committee. Dr. Huber has also published his work exploring hospital variation in withdrawal of life support policies in the journal Chest.
Our fellowship programs support six geriatric fellowship positions and five palliative medicine fellowship positions on a yearly basis. Through our partnership with Vitas Healthcare, the division secured additional funding to help support the division’s Geriatric Fellowship Program.


MARCIO ROTTA SOARES, M.D.
Division Chief
PROFESSORS OF CLINICAL MEDICINE
Stuti Dang, M.D., M.P.H.
Silvina Levis, M.D. (Emeritus)
RESEARCH PROFESSOR
Guy Howard, Ph.D.
RESEARCH ASSOCIATE PROFESSOR
Carlos Perez-Stable, Ph.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Enrique Aguilar, M.D.
Iriana Hammel, M.D.
Michael Huber, M.D.
Mariana Khawand-Azoulai, M.D.
Luis Samos-Gutierrez, M.D.
Julia Sanchez, M.D.
Marcio Soares, M.D.
Khin Zaw, M.D.
FELLOWS
COMBINED GERIATRIC & HOSPITALPALLIATIVE CARE
First Year
Jerry Bradley, M.D.
Second Year
Armando Sarasua, M.D.
GERIATRIC MEDICINE
Anabel Alonso, M.D.
Zeina Najib Georges, M.D.
Mohamad Hosni, M.D.
Raiyan Islam, M.D.
Nabeel Khan, M.D.
Laura Llabre, M.D.
HOSPICE AND PALLIATIVE CARE
MEDICINE
Michael Basir, M.D.
Jalisa Carvalho, M.D.
Oxana Harlamova, M.D.
Heba Waseem, M.D.
Caring for patients with hematologic disorders, research into these conditions, and hematology education have undergone dramatic, disruptive transformations. The use of nextgeneration sequencing to identify the genetic causes of hematologic conditions has become de rigueur, paving the way for improved prognostication, targeted therapies and immunotherapies, identification of drugs, and international collaborations. Team science and the development of large databases are requisite; they allow for more accurate and timely interventions, propelling treatments into a new era of precision medicine.
Faculty members within the Division of Hematology continue to
provide sophisticated hematological care at nine clinical sites throughout Miami-Dade and Broward counties. At all of our sites, faculty use cutting-edge diagnostics, collaborate with worldclass pathologists, and provide 56 interventional therapeutic trials, including investigator-initiated studies, with an emphasis on early-phase trials. More than 250 hematology patients were enrolled in therapeutic trials this year, a 105 percent increase over last year, with approximately 10 percent more patients seen year-over-year during the past five years.
The division also established one of the few clinics in the nation that is focused on clonal hematopoiesis and built databases of 300+ patients that have led to multiple collaborative international conference abstracts and published manuscripts.
Additionally, Jonathan Cohen, M.D., received the Dean’s Faculty Award for Clinical Excellence.
The development of individualized treatment plans based on the genetic profiles of a person’s cancer has led to more effective and tailored therapies. During FY2024, hematology faculty had publications in 82 scientific

journals, almost half with impact factors greater than 10.
Justin M. Watts, M.D., and Mikkael A. Sekeres, M.D., M.S., led and served on steering committees for clinical trials of three drugs: olutasidenib, quizartinib, and imetelstat that gained FDA approval this year. Results were published in Lancet Haematology and Lancet.
Izidore Lossos, M.D., published phase 1 and 2 studies on a new lymphoma therapy combination for patients diagnosed with diffuse large B-cell lymphoma and who are resistant to current standards of care or whose cancer returns in the journal Nature Medicine.
Juan Alderuccio, M.D., published “PET/CT Biomarkers Enable Risk Stratification of Patients with Relapsed/ Refractory Diffuse Large B-cell Lymphoma Enrolled in the LOTIS-2 Clinical Trial” in Clinical Cancer Research.
Justin Taylor, M.D., published “Kinase-impaired BTK mutations are susceptible to clinical-stage BTK and IKZF1/3 degrader NX-2127,” in Science. He continues to lead studies on CLL patients with BTK tumor-resistance drugs and was the recipient of a $1.92 million grant from National Institute of General Medical Sciences (NIGMS). He also is the recipient of the Department of Medicine’s Schally Research Award.
Jonathan Schatz, M.D., published “Bispecific antibodies and CAR-T cells: dueling immunotherapies for large B-cell lymphomas” in Blood Cancer Journal. He continues his Department of Defense-funded work on antiCD19 chimeric antigen receptor T-cell therapies.
Juan Ramos, M.D., received the Clinical Excellence Award from the HTLV International Retrovirology Association in recognition of his HTLV-1/Adult T-cell leukemialymphoma research.

MIKKAEL A. SEKERES, M.D., M.S.
Division Chief
PROFESSORS
John Byrnes, M.D.
Izidore Lossos, M.D.
Craig Moskowitz, M.D.
Stephen Nimer, M.D.
Joseph Rosenblatt, M.D.
Mikkael A. Sekeres, M.D., M.S.
Yeon Soong Ahn, M.D. (Emeritus)
PROFESSORS OF CLINICAL MEDICINE
Juan Carlos Ramos, M.D.
Jonathan Schatz, M.D.
Gerald Soff, M.D.
RESEARCH PROFESSOR
Ramiro Verdun, Ph.D.
ASSOCIATE PROFESSOR
Jack Temple, M.D. (Emeritus)
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Juan Alderuccio, M.D.
Alvaro Alencar, M.D.
Justin Taylor, M.D.
Justin Watts, M.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Ney Alves, M.D.
Felipe Novoa, A.P.R.N., was awarded the Staff Clinical Award for his outstanding service to leukemia patients at the Department of Medicine’s State of the Department Address (SODA).
Division faculty members help shape future hematology professionals by contributing to the NextGen’s curriculum, by acting as mentors and lecturing at national and global conferences.
Hematology faculty serve on seven American Society of Hematology (ASH) Committees, including the Executive Committee.
Alvaro Alencar, M.D., continues to chair SINTOMA, the annual malignant hematology conference in Brazil, which attended by more than 1,300 individuals.
Dr. Sekeres chaired the European School of Hematology’s conference on MDS in Budapest, Hungary, with 500 attendees, and chaired an FDA Symposium session on
Terrence Bradley, M.D.
Diana Byrnes, M.D.
Roberto Cano, M.D.
Namrata Chandhok, M.D.
Jonathan Cohen, M.D.
Thomas Harrington, M.D.
Georgios Pongas, M.D.
Michele Stanchina, D.O.
Sangeetha Venugopal, M.D., M.S.
Steven Weiss, M.D.
RESEARCH ASSISTANT PROFESSORS
Xiaoyu Jiang, Ph.D.
Jun Sun, Ph.D.
Yu Zhang, M.D.
STAFF PHYSICIANS
Diogenes Alayon, M.D.
Mayda Arias, M.D.
Erika Correa, M.D.
Douglas Faig, M.D.
David Lessen, M.D.
Overall Survival, attended by 4,000 participants.
Gerald Soff, M.D., leads the most popular online hematology course to an audience of trainees from more than 90 countries. He also published a review article on cancer-associated thromboses in the Journal of Clinical Oncology.
Dr. Lossos served on the organizing committee of the 17th ICML, the largest lymphoma meeting in the world. His work on mantle cell lymphoma earned him a contribution to the 5th edition of the “World Health Organization Classification of Haematolymphoid Tumours.”
Top right: Juan Ramos, M.D., right, speaking at the International HTLV conference in London, England, June 2024.
Bottom right, left to right: Samantha Sanchez, N.P.; Patricia Pupo, A.P.R.N.; Felipe Novoa, A.P.R.N.; Ellen Madarang, Clinical Pharmacologist; Terrence Bradley, M.D.; Sangeetha Venugopal, M.D., M.S.; Justin Taylor, M.D.; Namrata Chandhok, M.D.; Mikkael A. Sekeres, M.D., M.S., Anastasia Santiago, A.P.R.N.
Ashley Rose, M.D.
Daniel Tannenbaum, M.D.
FELLOWS
FIRST YEAR
Ali Al Sbihi, M.D.
Palash Asawa, M.D.
Chinmay Jani, M.D.
Traci King, M.D.
Amrit Paudel, M.D.
SECOND YEAR
Maryam Alasfour, M.D.
Raleigh Fatoki, M.D.
Gil Hevroni, M.D.
Deborah Soong, M.D.
Toufic Tannous, M.D.
THIRD YEAR
Priscila B. Coelho, M.D.
Samuel Kareff, M.D.
Jose M. O. Novaes, M.D.
Thomas Platé IV, M.D.
Asaad Trabolsi, M.D.

The Division of Hospital Medicine is undergoing significant growth to better serve the patient population across South Florida and beyond. Eighteen new providers are joining the division in FY2025 to support this growth.
In addition, the division has made several clinical strides this past year, including geographic allocation within the hospital and the cohorting of inpatient teams on specific floors. These strategies have improved
clinical efficiency while also optimizing patient safety.
The division is also working diligently to standardize its clinical note templates to enhance the quality and consistency of our documentation.
The division also has taken steps to reintroduce its monthly journal club, an academic tradition that was previously observed by faculty members before the pandemic.
Additionally, the onboarding
process for new faculty has been refined to ensure a smoother transition for those new members joining the division. These improvements are the result of the dedicated efforts of division hospitalists and leadership.
As we continue to grow and expand, we remain committed to enhancing teamwork and delivering exceptional patient care at the University of Miami Miller School of Medicine.




MARCIO ROTTA SOARES, M.D.
Division Chief
ASSOCIATE PROFESSOR OF CLINICAL MEDICINE
Efren Manjarrez, M.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Candido Anaya, M.D.
Armen Henderson, M.D.
Rafael Enrique Hernandez Oquet, M.D.
Joshua Laban, M.D.
Ahmed Luqman, M.D.
Vijay Mehta, M.D.
Maria Antonietta Mosetti, M.D.
Ayoola Olayiwola, M.D.
Ankita Saxena, M.D.
Sebastian Suarez Zarate, M.D.
Rachel Werne, M.D.
Pulkit Taunk, M.D.
Jessica Zuleta, M.D.
STAFF PHYSICIANS
Alberto R. Arancibia, M.D.
Scott Berger, M.D.
Erica Corredera, M.D.
Jorge Diaz Valdes, M.D.
Daniel Franco, M.D.
Rafael Garces, M.D.
Taaha Mendha, M.D.
Mina Meseha, M.D.
Bipte Modi, M.D.
Deepak Mummidavarapu, M.D.
Aldo Pavon Canseco, M.D.
Reubender Randhawa, M.D.
Zakia Rauf, M.D.
Allan Rubinfeld, M.D.
Jonathan Salter, M.D.

Juan Serralles Allongo, M.D.
Pamela Trotter, M.D.
Gilberto Velazco, M.D.
William Winter, M.D.
Liana Woodley-Pearson, M.D.
STAFF PHYSICIANS PER DIEM
Roberto Andino, M.D.
Kunal Gawri, M.D.
Oxana Harlamova, M.D.
Muhammad Khan, M.D.
Andrew Scheinberg, M.D.
Olga Tarasova, M.D.
Bruno Urrea, M.D.

Ricardo Fonseca Franco, M.D., an expert in implementation and dissemination of equitable care for HIV and hepatitis C, joined the division’s faculty as an infectious diseases specialist.
Yoichiro Natori, M.D., Medical Director of Solid Organ Transplant Infectious Diseases at the Miami Transplant Institute, was invited to participate in the American Society of Transplantation Infectious Diseases Community of Practice guidelines for screening, diagnosis, prevention, and treatment of Cytomegalovirus (CMV) in solid organ transplant recipients.
David Serota, M.D., M.Sc., received the Dean’s Faculty Award for Excellence in Clinical Medicine. Dr. Serota’s clinical and academic specialization has focused on improving care for people who use drugs and develop serious injectionrelated infections (SIRI).
Hansel Tookes, M.D., M.P.H., received the Dean’s Faculty Award for Community Engagement for his advocacy in legalizing syringe
exchange services statewide in Florida, and his leadership in creating and expanding the IDEA Exchange Program, which provides comprehensive risk reduction care for people who use drugs through innovative strategies.
Laura Beauchamps, M.D., received the Department of Medicine Distinguished Clinician Award. As an emerging leader who is innovatively approaching HIV inequities in prevention, through her work, Dr. Beauchamps has demonstrated the ability to shift approaches to delivery of PrEP for transgender women of color in a holistic, culturally appropriate manner.
Dr. Tookes and Tyler Bartholomew, Ph.D., received a $3.3 million R01 grant from the National Institute on Drug Abuse to support syringe services programs under the ACCESS initiative.
Mario Stevenson, Ph.D., and Dr. Tookes received a $3.1 million grant from the National Institute on Drug

Abuse for the ARES study, which will examine how methamphetamine use affects HIV progression in men who have sex with men.
Maria Alcaide, M.D., is a co-PI for the CROWN study, which will explore the links between oral and mental health in women with HIV. This work is supported by a $2 million grant from the National Institutes of Health (NIH).
Isabella Rosa-Cunha, M.D., is an investigator on a National Cancer Institute-funded, multisite study to investigate potential screening markers for anal dysplasia and cancer among diverse populations in Miami and Atlanta.
Jose Gonzales Zamora, M.D., became the Program Director of the University of Miami/Jackson Memorial Hospital ACGME-Accredited Infectious Disease Fellowship.
Paola Lichtenberger, M.D., will continue to support the program as the Associate Program Director, and Shweta Anjan, M.D., is now the


SUSANNE DOBLECKILEWIS, M.D., M.P.H.S.
Division Chief
PROFESSORS
Maria Alcaide, M.D.
Gordon Dickinson, M.D. (Emeritus)
Margaret Fischl, M.D.
Michael Kolber, M.D.
Mario Stevenson, Ph.D.
Hansel Tookes, M.D.
PROFESSORS OF CLINICAL MEDICINE
Lilian Abbo, M.D.
Gio Baracco, M.D.
Jose Castro, M.D.
Susanne Doblecki-Lewis, M.D., M.P.H.S.
Dushyantha Jayaweera, M.D.
Paola Lichtenberger, M.D.
Michele Morris, M.D.
Allan Rodriguez, M.D.
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Shweta Anjan, M.D.
Laura Beauchamps, M.D.
Catherine Boulanger, M.D.
Jose Camargo Galvis, M.D.
Ricardo Fonseca Franco, M.D. (Pending Rank)
Program Director for the Transplant Infectious Diseases Fellowship. The division has a total of 12 fellows including ten general infectious diseases (ID) fellows and two transplant ID fellows.
University of Miami Miller School of Medicine students, supported by Dr. Beauchamps and Susanne Doblecki-Lewis, M.D., M.P.H.S., opened a new free Department of Community Service (DOCS) clinic supporting sexual and gender minority health services in the Converge Building Rapid Access Wellness Clinic, providing infectious diseases prevention in an affirming environment.
Dr. Tookes has been selected to serve on the Presidential Advisory Council on HIV/AIDS and as an Emerging Leaders in Health and Medicine Scholar by the National Academy of Medicine. His IDEA Needle Exchange program was featured in the New York Times article “Why Miami’s Approach to Addiction is Working.”
Jose Gonzales Zamora, M.D.
Yoichiro Natori, M.D.
Isabella Rosa-Cunha, M.D.
David Serota, M.D.
Bhavarth Shukla, M.D.
Jacques Simkins-Cohen, M.D.
Stephen Symes, M.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Folusakin Ayoade, M.D.
Julia Bini Viotti, M.D.
Teresa Chueng, M.D.
Michael Gelman, M.D.
Alexis Powell, M.D.
Mohammed Raja, M.D.
Antoine Salloum, M.D.
Candice Sternberg, M.D.
RESEARCH ASSISTANT PROFESSOR
Mark Sharkey, Ph.D.
Dr. Alcaide was appointed Interim Vice Provost for Research and Scholarship.
Lilian Abbo, M.D., was a finalist in the Health Care Professional category for the 2023 Health Care Heroes Awards. She also has been invited to become a Defense Health board member.
Dr. Doblecki-Lewis’ Rapid Access Wellness PrEP Mobile Clinic was featured in a spotlight on the NIH website titled “NIH Ending the HIV Epidemic Projects Bridge Gaps Between HIV Research and Public Health Practice.”
CONNECT, a mobile unit she spearheaded, aims to extend the scope of clinical research focused on HIVrelated issues within the South Florida community. CONNECT was featured in a recent Miami Herald article on HIV.
CONNECT Mobile Research Unit service team in the Liberty City neighborhood of Miami, Florida.
FELLOWS
First Year
Madiha Ahmed, M.D.
Jason Victor Chavez, M.D.
Tara Herrera, M.D.
Deborah Jimenez, M.D.
Sudiksha Sethia, M.B.B.S
Second Year
Joseph Berger, M.D.
Maria Del Pilar Morel Almonte, M.D.
Divya Pandya, D.O.
Carlos Eduardo Plazola, M.D.
Ruth Graciela Ramon Tapia, M.D.
INFECTIOUS DISEASES TRANSPLANT FELLOWS
Christopher M. Lopez, D.O.
Lubna M.M. Osman, M.B.B.S


The Division of Internal MedicinePediatrics at the University of Miami Miller School of Medicine has recently expanded its clinical services in both inpatient and outpatient settings. New division faculty members, including Christina DeBenedictis, M.D., and Tiffani Houston, M.D., Ph.D., are now providing hospitalist care at UHealth Tower and Holtz Children’s Hospital. Additionally, Madeline Mlynczak, M.D., has joined the primary care team at UHealth Primary Care in Palmetto Bay.
The division’s greatest strength lies in the various partnerships it has forged. The division has collaborated with the UHealth Women’s Health
Alliance and Sylvester Comprehensive Cancer Center’s Long-Term Survivor program to provide excellent primary care to the community’s female population and long-term cancer survivors.
In addition, the division has forged two partnerships. One such partnership is with the Department of Pediatrics and its divisions of Psychology, Psychiatry, Adolescent Medicine, and Gastroenterology to create an Eating Disorders Collaborative that offers comprehensive care for individuals with eating disorders. The second partnership is with the divisions of Pediatric Urology, Neurology, Neurosurgery, Gastroenterology, Nephrology,
and Orthopedics that together support a comprehensive multidisciplinary practice for patients with spina bifida.
Victor Cueto, Jr., M.D., a recipient of the University of Miami’s Clinical and Translational Science Institute (CTSI) Pilot Program Award and one of a few physicians certified in obesity medicine, conducts pioneering research on the care of patients with limited English proficiency, a crucial but often overlooked area in Miami. His work, published in the Journal of General Internal Medicine, addresses the continuity of care and highlights the impact of language proficiency

on healthcare barriers during the COVID-19 pandemic.
Jonathan Tolentino, M.D., director of our PATH Clinic, continues his research on transition populations. He has contributed chapters on the care of patients with cerebral palsy and spina bifida in the textbook Care of the Adult with Chronic Childhood Conditions
Anjali Saxena, M.D., co-physician to the PATH Clinic, continues her grant-funded work with the National Leadership in Education and Neurodevelopmental Disabilities (LEND) Program, securing a supplemental grant for her related projects.
The division’s Med-Peds Residency Program remains in high demand, with residents actively participating in national activities, events, and programs. Their election to board positions in the National Med-Peds Residents Association (NMPRA) since 2020 highlights the division’s strong national reputation. Lawrence Rolle, M.D., M.B.A., will serve as the NMPRA president during the upcoming year, replacing Stephanie Lee, M.D., who is the outgoing president. Division interns Sarah Dempsey-Prioleaux, M.D., and Azaria Lewis, D.O., were elected as Public Relations Secretary and DEI Co-Chair, respectively.
Dr. Saxena, Dr. Gonzalez, and Dr. Van Kirk continue to provide education, clinical programming, and outreach to international communities through
Dr. Tolentino, Dr. Leyva, and Dr. Houston with Dr. Oboh and Dr. Rolle (PGY-4 residents in Med-Peds) representing the division’s student outreach efforts at the Student National Medical Association (SNMA) 2024 annual conference.
their work with the Global Institute at the University of Miami Miller School of Medicine. This year, Dr. Gonzalez spearheaded Global Institute outreach efforts in Puerto Rico, collaborating with Direct Relief, Universidad Central de Caribe, the Department of Health, and other community partners in a multidisciplinary effort providing direct patient care to the vulnerable communities of Culebra and Vieques, Puerto Rico.
Division Chief Stefanie Brown, M.D., M.B.A., and Dr. Tolentino continue to represent the division nationally. Dr. Brown serves as a member of the American Board of Internal Medicine’s General Internal Medicine Board, while Dr. Tolentino serves on the American Board of Pediatrics’ Item Writing Committee and the newly appointed Entrustable Professional Activities Writing Task Force. Starting in July 2024, Dr. Brown will begin her official appointment on the Internal Medicine Residency Review Committee for the Accreditation Council for Graduate Medical Education (ACGME).

STEFANIE BROWN, M.D., M.B.A. Division Chief
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Stefanie Brown, M.D., M.B.A.
Jonathan Tolentino, M.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Victor Cueto, M.D.
Christina DeBenedictus, M.D.
Chadwick Flowers, M.D.
Samantha Gonzalez, M.D.
Tiffani Houston, M.D.
Matthew Imm, M.D.
Bryan Leyva, M.D.
Anjali Saxena, M.D.
Kendra Van Kirk, M.D.
STAFF PHYSICIANS
Madeline Mlynczak, M.D.
Tobenna Ubu, M.D.

The Division of Medical Oncology is proud to report numerous accomplishments, changes, and initiatives in clinical care, research, and education during fiscal year 2024. Many of these accomplishments are made possible by our dedicated

providers, who work tirelessly to support our communities and make a positive impact both nationally and globally.
Carmen Calfa, M.D., received the 2024 South Florida Business and Wealth (SFBW) Prestigious Women Award. Coral Olazagasti, M.D., was named primary investigator and received the SCCC-ECAA-2024 Early Career Advancement Award.
Peter Hosein, M.D., has been appointed to the Scientific and Medical Advisory Board of the Pancreatic Cancer Action Network for 2023-2026. He also has been appointed to the Annual Meeting Scientific Committee of the American Society of Clinical Oncology (ASCO) for 2023-2026.
Alejandra Perez, M.D., was named the ASCO’s Advocacy Champion.
Estelamari Rodriguez, M.D., M.P.H., one of our Breast Medical Oncology/Thoracic Medical Oncology co-leads was awarded the GRACE Patient Educator of the Year Award in May 2024 for her exceptional

work in creating Spanish-language educational content on lung cancer.
Dr. Calfa, a breast cancer specialist and program director for the upcoming conference sponsored by the Miller School of Medicine, discussed the evolution of precision medicine. She highlighted the importance of applying precision medicine throughout a patient’s cancer journey, from assessing personal risk factors and genetics to developing personalized treatment, survivorship plans, and lifestyle and emotional interventions. Furthermore, Dr. Calfa designed, funded, and opened the Genetic Predisposition Syndrome (GPS) Clinic, a specialized facility dedicated to supporting patients with a genetic predisposition to cancer.
Clinical care remains the division’s top priority. Dr. D’Amato, a sarcoma medical oncologist and assistant director of clinical research, along with Jonathan Trent, M.D., Ph.D., the associate director for clinical research and director of the Bone and SoftTissue Sarcoma Group, take great pride in caring for their patients. They were recently recognized with a significant philanthropic gift for their work. One of their patients has a solitary fibrous tumor (SFT), which is one of the rarest tumors, affecting only about one in a million people each year.
Tracy Crane, Ph.D., R.D.N., had a notable year. She was awarded the FastER R01 grant and successfully launched the project in 2024. She also was appointed by the National Cancer Institute (NCI) to serve as the Vice Chair for Cancer Prevention and Control for the NCI Community Oncology Research Program (NCORP).
Dr. Calfa enjoyed various research achievements in 2024. Her abstract, for instance, has been accepted as an oral presentation at the ASCO 2024 Annual Meeting. Dr. Calfa will present on the topic “Outcomes of Advanced/ Metastatic Breast Cancer (aMBC) Treated with BRIA-IMT, an Allogeneic Whole Cell Immunotherapy.”
Dr. Perez, in collaboration with Maria Rueda-Lara, M.D., Joycelyn Lee, Ph.D., M.B.A., and Brittany Wright, Ph.D., submitted a proposal titled “Addressing Psychosocial Needs of Minoritized Patients at High Risk of Developing Breast Cancer” to the National Breast Cancer Foundation (NBCF). The proposal was awarded $175,000 for this year, with the potential for annual renewal.
Faculty members also have accomplished many notable professional achievements. Dr. Hosein and Gina D’Amato, M.D., were both promoted to Professor of Clinical Medicine.
Natasha Schaefer Solle, Ph.D., R.N., was promoted to Research Associate Professor.
Dr. Calfa directed the second biennial international Miami Precision Medicine Conference in May 2024, which had a prestigious speaker lineup, including keynote speakers featuring ASCO CMO and outstanding UM and internationally renowned presenters.
In March 2024, Lynn Feun, M.D., served as a panel speaker at the Pap Corps’ Men Conference, where he shared his expertise on cancer care and awareness.

GILBERTO LOPES, M.D., M.B.A.,
F.A.S.C.O.
Division Chief
PROFESSORS
Bach Ardalan, M.D.
Pasquale Benedetto, M.D.
Lynn Feun, M.D.
Erin Kobetz, Ph.D., M.P.H.
Marc Lippman, M.D. (Emeritus)
Jaime Merchan, M.D.
Stephen Richman, M.D. (Emeritus)
Jonathan Trent, M.D., Ph.D.
PROFESSORS OF CLINICAL MEDICINE
Marijo Bilusic, M.D., Ph.D.
Gina D’Amato, M.D.
Peter Hosein, M.D.
Judith Hurley, M.D.
Gilberto Lopes, M.D., M.B.A.
Jose Lutzky, M.D.
RESEARCH PROFESSOR
Niramol Savaraj, M.D.
ASSOCIATE PROFESSOR
Tracy Crane, Ph.D., R.D.N.
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Carmen Calfa, M.D.
Aman Chauhan, M.D. Chukwuemeka Ikpeazu, M.D.
Alejandra Perez, M.D.
Catherine Welsh, M.D.
RESEARCH ASSOCIATE PROFESSOR
Natasha Solle, Ph.D.
ASSISTANT PROFESSOR
Dionysios Watson, M.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Leonel Hernandez-Aya, M.D.
Emily Jonczak, M.D.
Lawrence Negret, M.D.
Coral Olazagasti, M.D.
Agustin Pimentel, M.D.
Pearl Seo, M.D.
Janaki Sharma, M.D.
Gretel Terrero, M.D.
Frances Valdes-Albini, M.D.
Luis Villa, M.D.
RESEARCH ASSISTANT PROFESSORS
Akina Natori, M.D.
STAFF PHYSICIANS
Steven Bialick, M.D.
Richa Dawar, M.D.
Milena Elimelakh, M.D.
Nkiruka Ezenwajiaku, M.D.
Gustavo Fernandez, M.D.
Elisa Krill Jackson, M.D.
Vinay Minocha, M.D.
Raja Mudad, M.D.
Joseph Pizzolato, M.D.
Estelamari Rodriguez, M.D.
Rakesh Singal, M.D.
Jose Carlos Suarez, M.D.
FELLOWS
First Year
Akshee Batra, M.D.
Robert Briski, M.D.
Michael Durante, M.D., Ph.D.
Samantha El Warrak, M.D.
Ernest Philon, D.O.
Daniel Tuerff, M.D.
Second Year
Ali Al Sbihi, M.D.
Palash Asawa, M.D.
Chinmay Jani, M.D.
Traci King, M.D.
Amrit Paudel, M.D.
Third Year
Maryam Alasfour, M.D.
Raleigh Fatoki, M.D.
Gil Hevroni, M.D.
Deborah Soong, M.D.
Toufic Tannous, M.D.
Dr. Chauhan, left, with the division’s inpatient APP team.

The American Cancer Society (ACS) estimates that there will be approximately 35,780 new cases of multiple myeloma in the United States in 2024. According to the ACS, 3,630 of those patients will be diagnosed with the disease in Florida. In fact, Florida has the highest number of newly diagnosed multiple myeloma patients in the nation. Thanks to the development of novel therapies for multiple myeloma, diagnosed patients are living longer.
During FY2024, the Division of Myeloma and Sylvester Myeloma Institute experienced significant growth. The division recorded nearly 6,500 outpatient multiple myeloma patient visits. Based on current data, this number is expected to increase by more than 20 percent annually in the coming years.
Reflective of the population in South Florida, our patient population is diverse. Fifty-one percent of the multiple myeloma patients seen by the division identify as Hispanic while 25 percent identify as Black.
FY2024 solidified the division’s commitment to education and research with the third-year renewal of Sylvester’s K12 Calabresi Clinical Oncology Research Career Development Program Award for Benjamin Diamond, M.D., and Marcella Kaddoura, M.D., as the new K12 recipient awardee. In addition, Dickran Kazandjian, M.D., Assistant Director, Clinical Research and Assistant Director of Protocol Development Unit Interventional Treatment Trials, has assumed various leadership roles.
Approximately 20 clinical trials are currently active, with the majority classified as Phase 1 or Phase 2 trials. An additional 10 clinical trials are in the current pipeline.
Thirty percent of the open clinical trials are investigator-initiated studies, which have been developed and launched by the division’s physicianscientists to meet the clinical needs in the catchment area. The goal of the program is to lead in drug
development and to advance the search for curative treatments for multiple myeloma.
The division and the Sylvester Myeloma Institute have a robust foundation in scientific discovery, which focuses on genomic and microenvironmental studies as well as translational research. Key strengths of the program include advanced minimal residual disease (MRD) tracking, novel drug development, molecular profiling, and the creation of new biomarkers for more personalized treatment strategies.
In April 2024, the Oncology Drug Advisory Committee (ODAC) voted unanimously, 12-0, to support using minimal residual disease (MRD) as an early endpoint for accelerated drug approval in multiple myeloma by the FDA. This approach, pioneered 15 years ago by Division Chief Carl Ola Landgren, M.D., Ph.D., will enable patients to access new therapies more quickly and efficiently.



C. OLA LANDGREN, M.D., Ph.D. Division Chief
PROFESSOR
C. Ola Landgren, M.D., Ph.D.
PROFESSOR OF CLINICAL MEDICINE
Dickran Kazandijan, M.D.
ASSOCIATE PROFESSOR OF CLINICAL MEDICINE
James Hoffman, M.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
David Coffey, M.D.
Benjamin Diamond, M.D. Marcella Ali Kaddoura, M.D. Francesco Maura, M.D.

Clinicians within the Katz Family Division of Nephrology and Hypertension serve across four hospital settings: UHealth Tower, Bruce W. Carter - Miami VA Medical Center, Jackson Memorial Hospital, and the Miami Transplant Institute. The division offers a broad range of nephrology services, including specialized care for glomerular diseases, hypertension, nephrolithiasis, polycystic kidney disease (PKD), and kidney transplantation. The PKD clinic is recognized as a Center of Excellence by the Polycystic Kidney Disease Foundation, making it one of just 37 centers nationwide and two in Florida to carry this distinction.


The division is part of a multidisciplinary team of specialists within the University of Miami Health System Comprehensive Hypertension Center, the only AHA-certified comprehensive center in Florida.
The division has made significant strides in patient access and appointment availability from FY2023 to FY2024, reducing the average lag time for new patients by 21 percent— from 103 days to 81 days. Outpatient visits increased by 12 percent, while new patient visits rose by 22 percent.
The DaVita Dialysis Home Program has positioned the nephrology unit as a leader in home dialysis in South Florida, currently serving 66 patients and surpassing the national average with a penetration rate of 19.5 percent. Notably, 29 percent of new patients are opting for peritoneal dialysis while 26.7 percent are beginning treatment urgently. This demonstrates the team’s adaptability and commitment to effectively addressing diverse patient needs.
Through its ongoing partnership with the Centers for Medicare and Medicaid Services (CMS) under the Comprehensive Kidney Care Contracting (CKCC) model, the division successfully processed patient health questionnaires (PHQ-9) for 60 percent of patients by the end of FY2024. This is a significant quality measure that assesses the mental health of CKCC patients.
Faculty members also are involved in significant research efforts, supported by the Peggy and Harold Katz Family Drug Discovery Center. Studies are focused on advancing treatments for kidney diseases and improving patient outcomes.
The division received notable recognition at the 10th annual Eugene J. Sayfie, M.D. Research Day, hosted
by the Department of Medicine. Demonstrating an unwavering commitment to advancing medical science, the division’s team of faculty members, residents, fellows, and students secured the second-highest number of abstract submissions.
Serving as the co-director of the Medical Scientist Training Program (MSTP), Alessia Fornoni, M.D., Ph.D., secured the renewal of the NIH MSTP Award for Physician Scientist Development. She also became PI in one of five U.S. institutions able to secure a NIH UE5 grant for the development of unrepresentative faculty minorities with NIDDK-relevant research interest.
Gabriel Contreras, M.D., M.P.H., secured federal funding from the Immune Tolerance Network to act as a co-investigator in a clinical trial evaluating an innovative therapy for patients with lupus nephritis. He also has collaborated on five publications in leading peer-reviewed journals in nephrology, rheumatology, and cardiology.
The division’s faculty is dedicated to educating the next generation of nephrologists through comprehensive training programs for medical students, residents, and fellows.
Under the leadership of Zain Mithani, M.D., Yelena Rekhtman Drexler, M.D., Marco Ladino Avellaneda, M.D., and Tali Elfassy, Ph.D., the team has diligently led efforts to solidify an innovative approach to curriculum development while staying up to date on the latest educational methodologies. As part of this effort, they have implemented several new features for the fellowship curriculum, including revamping the March didactics to incorporate “NephMadness,” a
month-long interactive nephrology educational initiative taking place at academic nephrology programs across the country. It leverages social media tools to teach about the latest breakthroughs in nephrology.
Led by Dr. Ladino Avellaneda, the new dialysis rotation at the Miami Veterans Affairs Medical Center (VAMC) exemplifies a change in nephrology medicine by highlighting the impact of technological advancements on nephrology training and practice. The unit features state-of-the-art dialysis technology, enhancing clinical training and allowing fellows to master current practices.
Maria Anne Sosa, M.D., M.B.A., was appointed as the Interim Division Chief of the Katz Family Division of Nephrology and Hypertension. Dr. Sosa brings a wealth of experience and expertise to the role, having previously served as a key faculty member within the division.
Dr. Fornoni was awarded the 2024-2025 Provost Luis Glaser Mentorship Award for her exceptional commitment to mentoring students. As Scientific Chair of the World Congress of Nephrology held in Buenos Aires in April 2024, she successfully assembled a pool of diverse speakers from more than 40 different countries.
Dr. Avellaneda Ladino continues to serve in the U.S. Army Reserve as the Internal Medicine Consultant for the Surgeon General. He also offers afterhours telemedicine services to provide UHealth patients with greater access to care.
Jair Munoz Mendoza, M.D., was invited to speak at the World Congress of Nephrology in Buenos Aires, Argentina, where he presented his research on “Non-neoplastic Lesions

MARIE ANNE SOSA, M.D., M.B.A.
Interim Division Chief
PROFESSORS
Alessia Fornoni, M.D., Ph.D.
David Roth, M.D.
PROFESSORS OF CLINICAL MEDICINE
Gabriel Contreras, M.D., M.P.H.
Warren Kupin, M.D.
Oliver Lenz, M.D., M.B.A.
RESEARCH PROFESSOR
Sandra Merscher, Ph.D.
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Marco Ladino Avellaneda, M.D.
Franco Cabeza, M.D.
Juan Duque, M.D.
Adela Mattiazzi, M.D.
Zain Mithani, M.D.
Jair Munoz Mendoza, M.D.
Mariella OrtigosaGoggins, M.D.
Marie Anne Sosa, M.D. ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Adriana Dejman, M.D.
Yelena Drexler, M.D.
Vinodh Mechery, M.D.
Christopher Naranjo, D.O. Javier Pagan, M.D. Shobana Sivan, M.D.
in Nephrectomy Samples: Implications for Kidney Function.”
Efren Chavez Morales, M.D., led a quality improvement project at UHealth Tower to evaluate thrombosis rates related to midline use in patients with advanced kidney disease.
Daniel Del Castillo Rix, M.D., a PGY-2 resident and mentee of Juan Duque Ballesteros, M.D., won the Annual Robert Geronemus Memorial Renal Research Competition 2024 at
RESEARCH ASSISTANT PROFESSOR
Tali Elfassy, Ph.D. Alla Mitrofanova, Ph.D.
RESEARCH INSTRUCTOR
Jin-Ju Kim, Ph.D.
STAFF PHYSICIANS
Fernando Pedraza
Taborda, M.D.
Yanetsy Olivera Arencibia, M.D. FELLOWS
First year
Fabian Altamirano, M.D. Elias Kima, M.D. Saramarina Sanchez, M.D.
Satesh Saroop, D.O. Eduardo A. Villa, M.D.
Second year
Shawn Alonso, D.O. Derek Casey, D.O. Gretchen Marrero
Lozada, M.D.
Glenda Sosa, M.D.
Gina Suarez Corujo, M.D.
the 57th Annual Florida Society of Nephrology Meeting.
David Roth, M.D., presented at the Department of Medicine’s Grand Rounds with a memorable presentation titled “The History of Kidney Transplantation: The People and Events Behind the Story.”
Franco Cabeza, M.D., won a firstplace award at the Ross University School of Medicine’s 66th Research Day Symposium.
During the past fiscal year, the Division of Pulmonary, Critical Care, and Sleep Medicine has reached several significant milestones that are transforming respiratory medicine.
Faculty within the division have crafted novel approaches to evaluate lung disease and sleep disorders, while several faculty members were awarded extramural grants to support these efforts.
On the clinical side, advances in nursing-driven rounding and specialty

care have the potential to disrupt barriers in care and provide precision approaches that will change the way medicine is practiced for generations to come.
Saramaria Afanador, M.D., and Kori Ascher, D.O., successfully secured external grant funding for their pilot research projects from the American Thoracic Society and the National Institutes of Health (NIH), respectively, for their pilot projects further contributing to the growing momentum of research within the division.
Dr. Afanador will be assessing the utility of high-flow nasal cannula in COPD and phenotyping patients utilizing novel imaging modalities to predict response to therapy.
Dr. Ascher will be exploring novel sleep interventions to promote smoking cessation that target addiction and sleep disorders. These efforts highlight the need for multimodal approaches to improve health outcomes.
The division remains a national leader in functional lung imaging, employing AI techniques to segment the lungs and discover new
biomarkers that offer deeper insights into respiratory diseases.
In the ICU, Christopher Mallow, M.D., along with the division’s critical care physicians, are working with nursing leadership to implement nursing-driven ICU rounds, allowing for greater participation in teambased critical care.
In the outpatient setting, specialty clinics — including the non-tuberculous mycobacterium clinic and noncystic fibrosis bronchiectasis clinics managed by Lisa Domaradzki, M.D., Maria Gabriela Tupayachi, M.D., Rene Rico, M.D., and Michael Campos, M.D. — highlight how multidisciplinary approaches bridging infectious disease, immunology, and pulmonary medicine will drive comprehensive care in the future.
Precision-based approaches, including a dedicated clinic for biologic therapy for asthma and COPD, led by Trishul Siddharthan, M.D., F.C.C.P., and an endobronchial valve program led by Sixto Arias, M.D., offers a preview of the kind of targeted treatments that will be available to patients in South Florida in the future.


NARESH PUNJABI, M.D., PH.D.
Division Chief
PROFESSORS
Horst J. Baier, M.D. (Emeritus)
Rachel Damico, M.D., Ph.D. (Pending Rank)
Franco D’Alessio, M.D. (Pending Rank)
Robert M. Jackson, M.D.
Naresh Punjabi, M.D., Ph.D.
Matthias A. Salathe, M.D. (Emeritus)
Roland M. Schein, M.D.
Adam Wanner, M.D.
Philip Whitney, Ph.D. (Emeritus)
The division is eager to continue supporting the three core goals of the Department of Medicine in the upcoming fiscal year.
The strategic recruitment of Rachel Damico, M.D., and Franco D’Alessio, M.D., has ushered in
PROFESSORS OF CLINICAL MEDICINE
Michael A. Campos, M.D.
Alejandro Chediak, M.D.
Hayley B. Gershengorn, M.D.
Daniel H. Kett, M.D.
Andrew Quartin, M.D.
Shirin Shafazand, M.D., M.S.
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Alexandre Abreu, M.D.
Sixto Arias, M.D.
David De La Zerda, M.D.
Elio Donna, M.D.
Tanira Ferreira, M.D.
Gregory Holt, M.D., Ph.D.
Diane Lim, M.D.
Andres Pelaez, M.D. (Pending Rank)
Juan Salgado, M.D. (Pending Rank)
Trishul Siddharthan, M.D.
Neeraj Sinha, M.D.
ASSISTANT PROFESSORS OF CLINICAL MEDICINE
Brian Adkinson, M.D.
Saramaria AfanadorCastiblanco, M.D.
Kori Ascher, D.O.
Jonathan Auerbach, M.D.
Yaroslav Buryk, M.D.
Jorge Cabrera, D.O.
Morgan Carbajal, M.D.
Oveimar De La Cruz, M.D.
Lisa Domaradzki, M.D.
Lesley Farquharson, M.D.
Hannah Ferenchick, M.D.
Brian Garnet, M.D.
Sergey Gerasim, M.D.
Daniel Gorman, M.D.
Adhiraj Gosine, M.D.
Abigail Koch, M.D.
Eric Lang, M.D.
Christopher Mallow, M.D.
Suresh Manickavel, M.D.
Erick Palma, M.D.
Yoslay Perez, M.D.
Andrea Shioleno, M.D.
Waleed Sneij, M.D.
Rene Rico Tresgallo, M.D.
Maria Tupayachi Ortiz, M.D.
Susan Vehar, M.D.
Martin Zak, M.D.
STAFF PHYSICIANS
Andrew Calzadilla, M.D.
Hyasil Gonsalves-Barriero, M.D.
Sajid Kadir, M.D.
Laiqua Khalid, M.D.
Hemal Parekh, M.D.
Bianca Sarmento, M.D.
Jeffrey Scott, D.O.
Andres Sosa, M.D.
Moe Zaw, M.D.
FELLOWS
First Year
Nulma Carguill, M.D.
Kareem Eid, M.D.
a transformative phase for the division. Their combined expertise will significantly advance our understanding and treatment of a range of critical areas, including the basic biology of acute lung injury, lung immunology, lung transplantation, cancer, and pulmonary hypertension.

Fredy Huertero, M.D.
Claudia Marcano, M.D.
Deborah Mi, M.D.
Yaisa Moreno Hernandez, M.D.
Katarina Pitka, M.D.
Lilien Socorro, M.D.
Juan Valdes Infante, M.D.
Second Year
Felipe De Andrade Arnaud, M.D.
Bianca Maria Dominguez, M.D.
Farhad Ghamsari, M.D.
Matthew Edward Hodge, M.D.
Eduardo A. Lopez Gonzalez, M.D.
Kelly O’Boyle, M.D.
Lauren Michele Pascual, M.D.
Guil Rozenbaum Lerner, M.D.
Lee Seifer, M.D.
Third Year
Ankur Aneja, M.D.
Irina Yuseth Gutierrez Puentes, M.D.
Alda Daisy Huang, M.D.
Dipan Nishikant Karmali, M.D.
Michaela Lynne Murphy, M.D.
Mauricio Tellez, M.D.
Jeany Paola Villamizar Rivero, M.D.
With work spanning both basic and translational research, the division is now positioned at the forefront of these crucial fields. The appointment of Dr. Damico as the director of the post-doctoral fellowship program marks the beginning of a new era in the division, which is focused on continuous improvement and ensuring the program remains at the forefront of excellence in both clinical and research endeavors.
2024 American Thoracic Society Research Program grant awardees, including Dr. Afanador, fourth from right.
The division welcomed a new clinician-educator, Kelly Corbitt, D.O. Dr. Corbitt brings her passion for clinical medicine and teaching, with a specific focus on students, residents, and fellows. She cares for patients with complex multisystem diseases and has spearheaded the development of a multi-disciplinary interstitial lung disease (ILD) clinic. In collaboration with Susan Vehar, M.D., from the Division of Pulmonary, Critical Care, and Sleep Medicine, Dr. Corbitt ensures that patients diagnosed with ILD and autoimmune rheumatic conditions receive multidisciplinary care during a combined clinic visit.
The division welcomed physician-scientist Estefania Quesada-Masachs, M.D., Ph.D. An immunologist trained in clinical rheumatology, Dr. Quesada-Masachs will initially engage in basic research.
Dr. Quesada-Masachs’ work
is funded by an NIH R01 award and focuses on autoimmune diseases, where she investigates the pathogenesis and disease mechanisms. Her ultimate objective is to contribute to the prevention and cure of these conditions.
The division also leads National Institutes of Health and VA-funded programs. These programs delve into the comparative safety of nonopioid medications and aim to define the role of pharmacogenomics in the effectiveness and safety of immunosuppressant drugs.
Additionally, the division has many ongoing clinical trials to test new therapeutic options for patients with autoimmune rheumatic conditions.
To demonstrate its commitment to training future leaders in academic rheumatology, the division has launched the Tozman Scholars Program. This program is named in honor of the esteemed clinician-
educator, Elaine Tozman, M.D., and is specifically designed for internal medicine residents who are interested in pursuing a career in academic rheumatology. Participants benefit from personalized mentorship and monthly meetings with faculty members and the division chief. Since its inception, the program has welcomed eight scholars. The scholars have presented their work at the annual Department of Medicine Eugene J. Sayfie, M.D. Research Day and have successfully competed at local and national levels.
In November, three scholars received awards from the Rheumatology Research Foundation to attend the American College of Rheumatology (ACR) Convergence 2023 meeting, and in May, four scholars attended the 2024 ACR Research Workshop. Additionally, one resident received the Resident Research Preceptorship Award.



CECILIA P. CHUNG, M.D., M.P.H.
Division Chief
PROFESSOR
Cecilia P. Chung, M.D., M.P.H.
PROFESSOR OF CLINICAL MEDICINE
Carlos J. Lozada, M.D.
ASSOCIATE PROFESSOR
Eric Greidinger, M.D.
ASSOCIATE PROFESSOR OF CLINICAL MEDICINE
Elaine C. Tozman, M.D.
ASSISTANT PROFESSORS OF MEDICINE
Maria F. Carpintero, M.D.
Kelly Corbitt, D.O.
Ozlem Pala, M.D., M.P.H.
STAFF PHYSICIANS
Schartess Culpepper-Pace, M.D. FELLOWS
First Year
Aakriti Alisha Arora, M.D.
Maria Intriago Williams, M.D.
Second Year
Jose A. Cano, M.D.
Miriam Maria Marti, M.D.
Dr. Chung (center) with Tozman Scholars (from left to right): Katelyn Kaufman, M.D., Sachalee Campbell, M.B.B.S., M.P.H., Sergio Maldonado, M.D., Dr. Chung, Danielle Henry, M.D., and Don Woody, M.D.
The Division of Transplantation and Cellular Therapy continues to receive increasing recognition both nationally and internationally for providing outstanding clinical care to patients undergoing hematopoietic stem cell transplantation or those receiving cellular immunotherapy.
The division has made significant strides in transplantation and cellular therapy over the past fiscal year. These efforts include establishing a clinic specifically for chronic graftversus-host disease and developing

an infrastructure to meet the needs of geriatric patients.
The combined expertise of the division’s faculty, nurses, coordinators, and study teams facilitates the delivery of unparalleled care to residents across South Florida, while our capacity to conduct breakthrough translational science benefits patients around the globe.
Division faculty are establishing especially strong research collaborations within the University of Miami’s academic community, including serving as both principal investigators or co-investigators on federal grants that focus on cancer survivorship and supportive care, multiple myeloma, and hematology.
Additionally, the division is widening its focus beyond hematologic malignancies. Currently, several faculty members are actively collaborating with colleagues to conduct clinical trials in breast cancer, lung cancer, rheumatology, neurology, pediatrics, and dermatology.
Antonio Jimenez Jimenez, M.D., is conducting disruptive research that

aims to improve access and outcomes for patients in the absence of an ideally matched stem cell donor. Faculty have delivered oral presentations at American Society of Hematology (ASH), International Workshop on CAR-T Cell Therapy (iwCAR), Society of Hematologic Oncology (SOHO), and the American Society for Transplantation and Cellular Therapy (ASTCT), and have delivered presentations at locations around the globe.
The division’s commitment to changing the face of medicine is reflected by its continual support of the research efforts conducted by junior faculty, including Noa Holtzman, M.D., who successfully applied for the Sylvester K12 award (Dr. A. Jimenez Jimenez - Mentor). This work focuses on strategies to leverage NK cell reconstitution after stem cell transplant to enhance graft function.
Additionally, Jay Spiegel, M.D., successful applied for V Foundation Grant support to study multi-modality multi-targeted immunotherapy for the treatment of aggressive large B-cell lymphomas, in collaboration with Lazaros Lekakis, M.D. (Damian Green, M.D. - Mentor).
Division faculty have a sustained commitment to teaching undergraduates, medical students, and post-doctoral fellows through formal didactics in the classroom, in clinical settings, as well as participation in research projects. These efforts are highlighted by the contributions of Amer Beitinjaneh, M.D., which led to University of Miami being designated as a new site for official training for the Broward Health Hematology Oncology ACGME Fellowship Program and a similar relationship he is establishing with the Cleveland Clinic.
Our faculty serve as Foundation for the Accreditation of Cellular Therapy (FACT) inspectors, and on a broad spectrum of educational and policymaking committees for the Center for International Blood and Marrow Transplant Research (CIMTR), the American Society of Hematology (ASH), the American Society of Transplantation-Clinical Trial Network (AST-CTN), the American Society for Transplantation and Cellular Therapy (ASTCT), the International Myeloma Working Group (IMWG) and others.
Two faculty members achieved well-deserved academic promotions (Dr. Lekakis to Full Professor and Trent Wang, D.O. to Associate Professor).
The division underwent FACT review/inspections of both our clinical and Cellular Therapy Laboratory programs. Denise Pereira, M.D., completed her tenure as Interim Division Chief and was universally lauded for doing an outstanding job before handing the reigns over to Dr. Green on March 1.
The division recently welcomed two new research faculty who started in September 2024 and is continuing to build its preclinical and translational research footprint.
The division’s 11 faculty members were authors on 66 peer-reviewed publications over the past 12 months, including in high-impact journals such as Nature, Lancet Oncology, Blood, JCO, Lancet, Science Immunology, and Nature Communications.
Successful collaborations between division members are frequent, as highlighted by a publication in the journal Leukemia, authored by Dr. Wang and Dr. Jimenez Jimenez (first and senior author respectively), addressing the use of CAR-T cell therapy in large B cell lymphoma.

DAMIAN J. GREEN, M.D.
Division Chief
PROFESSORS
Damian J. Green, M.D. (Pending Rank)
Krishna Komanduri, M.D. (Emeritus)
Lazaros J. Lekakis, M.D.
ASSOCIATE PROFESSORS OF CLINICAL MEDICINE
Amer Beitinjaneh, M.D.
Mark S. Goodman, M.D
Antonio M. Jimenez Jimenez, M.D.
Denise L. Pereira, M.D.
Trent Wang, D.O.
RESEARCH ASSOCIATE PROFESSOR
Eric Wieder, Ph.D.
ASSISTANT PROFESSOR OF CLINICAL MEDICINE
Cara Benjamin, Ph.D.
RESEARCH ASSISTANT PROFESSORS
Pinar Ataca Atilla, M.D.
Erden Atilla, M.D.

LOCATIONS IN MIAMI-DADE, BROWARD, AND PALM BEACH COUNTIES
1. UHealth Palm Beach Gardens 3401 PGA Boulevard, Suite 400 Palm Beach Gardens, FL 33410
2. UHealth Downtown West Palm Beach 185 Banyan Boulevard West West Palm Beach, FL 33401
3. UHealth Concierge Medicine Palm Beach 218 Royal Palm Way Palm Beach, FL 33480
4. UHealth Boca Raton 3848 FAU Boulevard, Suite 305 Boca Raton, FL 33431
5. UHealth Fort Lauderdale 4800 N.E. 20 Terrace, Suite 201, Building C Fort Lauderdale, FL 33308
6. UHealth Plantation 8100 S.W. 10 Street Plantation, FL 33324
7. UHealth SoLé Mia (coming soon) 2111 SoLé Mia Way North Miami, FL 33181
8. UHealth Miami Beach 1045 5th Street, Suites 303 and 305 Miami Beach, FL 33139
9. UHealth Fisher Island 41214 Fisher Island Drive Miami, FL 33109
10. UHealth Jackson 1400 N.W. 12 Avenue Miami, FL 33136
11. UHealth Doral 8375 N.W. 53 Terrace Doral, FL 33166
12. UHealth LeJeune 351 N.W. 42 Avenue Miami, FL 33126
13. Lennar Foundation Medical Center 5555 Ponce de Leon Boulevard Coral Gables, FL 33146
14. UHealth Kendall 8932 S.W. 97 Avenue Miami, FL 33176
15. UHealth Palmetto Bay 15155 S.W. 97 Avenue, Suite 100 Palmetto Bay, FL 33176
1. Sylvester Coral Springs 8170 Royal Palm Boulevard, 1st Floor Coral Springs, FL 33065
2. Sylvester Deerfield Beach 1192 E. Newport Center Drive Deerfield Beach, FL 33442
3. Sylvester Fort Lauderdale 5700 N. Federal Highway, Suite 5 Fort Lauderdale, FL 33308
4. Sylvester Plantation 8100 S.W. 10 Street, 1st Floor Plantation, FL 33324
5. Sylvester Hollywood 3850 Hollywood Boulevard, Suite 1B Hollywood, FL 33021
6. Sylvester Aventura 2801 N.E. 213 Street, Suite 1101 Aventura, FL 33180
7. Sylvester Miami 1475 N.W. 12 Avenue, 1st Floor Miami, FL 33136
8. Sylvester Doral 8333 N.W. 53 Street, 1st Floor Doral, FL 33166
9. Sylvester Kendall 8932 S.W. 97 Avenue Miami, FL 33176
10. Sylvester Naples 2390 9th Street North Naples, FL 34103
5. Bascom Naples 3880 Tamiami Trail North Naples, FL 334103 BASCOM PALMER EYE
1. Bascom Palm Beach Gardens 7101 Fairway Drive Palm Beach Gardens, FL 33418
2. Bascom Plantation 8100 S.W. 10 Street, 3rd Floor Plantation, FL 33324
3. Bascom Palmer Eye Institute 900 N.W. 17 Street Miami, FL 33136
4. Bascom/Lennar Foundation Medical Center 5555 Ponce de Leon Boulevard Coral Gables, FL 33146
$1 million+
$100,000-$999,999 15 $2,837,516
$10,000-$99,999 38 $963,483
$1,000-$9,999 49 $95,749
$999 and below 134 $25,591

UNIVERSITY OF MIAMI LEADERSHIP
Joseph J. Echevarria
President, University of Miami
C.E.O., UHealth
Dipen J. Parekh, M.D. C.O.O., UHealth
Henri R. Ford, M.D., M.H.A.
Dean and Chief Academic Officer
DEPARTMENT LEADERSHIP
Roy E. Weiss, M.D., Ph.D. Chair
Anna Carol Herman-Giddens, R.N., B.S.N.
Senior Administrative Officer
Maureen Lowery, M.D.
Vice Chair of Faculty Development and Diversity
Michael Kolber, M.D., Ph.D.
Vice Chair for Clinical Affairs
Amar Deshpande, M.D. Vice Chair for Education
Ernesto Bernal-Mizrachi, M.D.
Vice Chair for Research
Khemraj Hirani, M.D.
Associate Vice Chair for Research Regulatory Compliance
David H. Kerman, M.D.
Chief Medical Officer
Carlos Prieto
Executive Director, Clinical Operations
Ivelisse Rodriguez
Executive Director, Finance
Laura J. Pinzón, M.B.A.
Director, Administrative Operations
Lily Ferrer, M.B.A., C.R.A. (Interim)
Senior Director, Sponsored Research
Iliana Vera, M.B.A.
Director, Department Planning and Operations
Jannet Yern, B.S.A.
Executive Director, Employee and Student Health Services
Jennifer Lasso, M.S.
Department Administrator, Faculty and Staff Planning and Operations
Daniela Cespedes, B.S.N., R.N., A.M.B.-B.C. Director, Nursing
DIVISION CHIEFS
Yiannis S. Chatzizisis, M.D., M.P.H. Cardiovascular Medicine
Richard A. Preston, M.D., M.S.P.H., M.B.A.
Clinical Pharmacology
Ernesto Bernal-Mizrachi, M.D. Endocrinology, Diabetes and Metabolism
Paul Martin, M.D. Digestive Health and Liver Diseases
Alejandro D. Chediak, M.D. (Interim) General Internal Medicine
Marcio Soares, M.D. Geriatrics and Palliative Medicine
Mikkael A. Sekeres, M.D., M.S. Hematology
Marcio Soares, M.D. Hospital Medicine
Stefanie Brown, M.D., M.B.A., Internal Medicine-Pediatrics
Susanne Doblecki-Lewis, M.D., M.S.P.H. Infectious Diseases
Gilberto de Lima Lopes Junior, M.D., M.B.A.
Medical Oncology
C. Ola Landgren, M.D., Ph.D. Myeloma
Marie Anne Sosa, M.D. (Interim)
Katz Family Division of Nephrology and Hypertension
Naresh M. Punjabi, M.D., Ph.D.
Pulmonary, Critical Care and Sleep Medicine
Cecilia Chung, M.D., M.P.H. Rheumatology and Immunology
Damian Green, M.D.
Transplantation and Cellular Therapy
DIVISION ADMINISTRATION
Francisco M. Rodriguez, M.S. Cardiovascular Medicine
Cristina Calderon-Parra
Endocrinology, Diabetes and Metabolism
Carol Cottrell
Digestive Health and Liver Diseases
Joanne Alonso, M.B.A. General Internal Medicine
Joanne Alonso, M.B.A. Geriatrics and Palliative Medicine
Ali R. Ismail Hematology
Austin Ambrose Hospital Medicine
Lily Ferrer, M.B.A., C.R.A. Infectious Diseases
Frances Castellvi Senti, M.B.A. Internal Medicine-Pediatrics
Ingrid V. Rodriguez, M.B.A. Medical Oncology
Christina Villanueva
Katz Family Division of Nephrology and Hypertension
Austin Pitts, M.H.A.
Pulmonary, Critical Care, and Sleep Medicine
Carol Cottrell
Rheumatology and Immunology
Debra Chinquee, M.S.N., A.P.R.N.-B.C., O.C.N.
Transplantation and Cellular Therapy

1120 N.W. 14 Street, Suite 310 Miami, FL 33136
305-243-9120
med.miami.edu/departments/medicine