
THE SCIENTIST CEO
How Mark Taubman’s Unique Approach Reshaped URMC
Global Research
Changing Lives from Argentina to Zambia
The Teenage Whisperer Alum Helps Thousands
Overcome Trauma
PLUS: A Gift Forever Appreciated
UNIVERSITY OF ROCHESTER MEDICAL CENTER | SCHOOL OF MEDICINE AND DENTISTRY | 2024 VOLUME 1

POINT OF VIEW
 Ania Stolarczyk hugs Antonio Bottos (with Irianna Torres in background) during Match Day 2024.
Photo by J. Adam Fenster
On the cover
Mark Taubman stands in the Craig Morrell lab at the Aab Cardiovascular Research Institute.
Ania Stolarczyk hugs Antonio Bottos (with Irianna Torres in background) during Match Day 2024.
Photo by J. Adam Fenster
On the cover
Mark Taubman stands in the Craig Morrell lab at the Aab Cardiovascular Research Institute.
ROCHESTER MEDICINE | 2024 – V1
Photo by Matt Wittmeyer
Ania Stolarczyk still remembers the slip of paper she found in the pocket of her coat at her White Coat Ceremony. It read:
"Be kind. Be kind to your patients. Be kind to the staff you work with. And be kind to yourself. Kindness can save a life and kindness can relieve suffering that nothing else can."
Every new School of Medicine and Dentistry doctor had a similar card containing “words of wisdom” from alums. The tradition builds a heartfelt connection between generations of students and doctors.
Four years later, Stolarczyk still holds onto that card—and its message.
“Now, at the end of medical school, I see how wise that truly is,” she said.
She thought of it often as a student, realizing the best role she could take on was spending time with patients and showing them kindness.
And now, after matching with Rochester for her residency, Stolarczyk will take that message of wisdom with her: “I always kept it close to heart.”
For more Match Day photos, turn to page 30..

Alumni: Share Your Words of Wisdom with a Student
To be a part of this annual tradition, visit uofr.us/whitecoatwisdom or scan the QR code. Your message will be placed in the pocket of a student's white coat at the ceremony in August.

1 ROCHESTER MEDICINE | 2024 – V1

David Linehan, MD
CEO, University of Rochester Medical Center
Dean, School of Medicine and Dentistry
Senior Vice President for Health Sciences
As I begin my tenure as CEO and dean, I’m looking forward to sharing exciting news about SMD and beyond. But my first message here must be one of thanks to my predecessor.
You’ll read much in the following pages about Mark Taubman, MD, whose record of accomplishment stands as an inspiration to me and to all those who will lead SMD and URMC in the years to come. He set a high standard and laid a solid foundation for us to build on. That might be the biggest gift a dean and CEO can leave.
Unlike at many medical schools, Mark set up a reliable and consistent financial structure that protects our academic mission. Ensuring support for research and education is one of our institution’s core values.
Mark saw us through challenge after challenge, including the pandemic. All the while, his commitment to our students never wavered. He had a keen appreciation for the biopsychosocial model, and he strove to adapt our educational offerings to the needs of today’s students.
I’ve seen the success of those efforts in recent months as I’ve met with learners, clinicians, and researchers across SMD and URMC. It’s a legacy that will long be remembered in Rochester and beyond, and one that I am proud to have an opportunity to build upon in the years to come.
In this issue, you’ll also see the inspiring work our researchers are doing around the world, and you’ll meet a fascinating alum who was ahead of her time.
Altogether, these stories show the many different ways our school and alums make the world a better place. I’m honored to step into my new role and be a part of it all.
RochesterMedicine.urmc.edu
RochesterMedicineMagazine@urmc.rochester.edu
Rochester
University
Box
Read more Rochester Medicine
Submit Class Notes
Write to Us
Medicine magazine
of Rochester Medical Center 601 Elmwood Avenue
643 Rochester, New York 14642 What do you think? Rochester Medicine welcomes letters from readers. The editor reserves the right to select letters for publication and to edit for style and space. Brief letters are encouraged. RochesterMedicineMagazine@urmc.rochester.edu
2 ROCHESTER MEDICINE | 2024 – V1

Ways to Support Street Outreach
Several readers reached out to us, asking for ways to contribute to the program featured in our last issue’s cover story (“What the Streets Teach: An Outreach Program Helps People in Need. It’s Also Changing the Lives of Its Volunteers”).
If you’re interested in supporting this student-run program, you can go online to uofr.us/givestreetoutreach or call 866-673-0181.

CONTENTS 5 Medical Center Rounds 10 The Scientist CEO How Mark Taubman Used His Research (and Musical) Mind to Reshape URMC 20 Think Locally, Research Globally Rochester Physician-Scientists Are Venturing Around the World for Their Studies. The Benefits Are Hitting Home as Well as Abroad. 26 The Third Way How Hildegard Messenbaugh’s New Approach Salvaged the Lives of Troubled Youth 30 Match Day 2024 in Photos 32 Faculty News 37 A Gift “Forever Appreciated” 38 Class Notes 40 In Memoriam Cover Story Find us on facebook at: www.facebook.com/urochestermed Rochester Medicine is published by: The University of Rochester Medical Center, Department of Communications, in conjunction with the Department of Alumni Relations and Advancement for the School of Medicine and Dentistry Editor Mark Liu Art Direction & Design Karen Ver Steeg Staff Writers Bethany Bushen Jim Miller Production Manager Bethany Bushen Feature Photography Matt Wittmeyer Contributors Sydney Burrows Karin Christensen Scott Hesel Mark Michaud Leslie Orr Susanne Pallo Sandra Parker
Smith-Hayduk Kristine Kappel Thompson Assistant Vice President B. Chip Partner of Communications, URMC For questions or comments, contact: Dept. of Alumni Relations and Advancement for the School of Medicine and Dentistry 300 East River Road, Rochester, NY 14627 Phone 800.333.4428 585.273.5954 Fax 585.461.2081 To comment on this issue, e-mail: RochesterMedicineMagazine@urmc.rochester.edu Feature
3 ROCHESTER MEDICINE | 2024 – V1
Kelsie
Story
Here’s How Academic Medicine Can Thrive Plus: Donors’ Gift Goes Way Beyond Dollars Bonding at Meliora Weekend WHAT THE STREETS TEACH Outreach Changes Lives and Minds
Dreams fulfilled A gift from one generation to another
”
If I can help students realize dreams that lead to a career as fulfilling as mine has been, this will remain my legacy.”
ALAN JAMES KOZAK ’65, ’69M (MD), ’72M (RES) Cooperstown, NY
Member, Wilson Society
Member, George Eastman Circle

When Alan Kozak arrived at the University of Rochester as a college student, he had never spent a day away from home. Quickly his universe expanded through friendship, the demands of his coursework, and a dream to continue his education at the School of Medicine and Dentistry and become a physician.
Thanks to scholarship support, Alan was able to graduate from college and then medical school without debt. A fulfilling career in medicine followed. Now, in gratitude, he supports the University of Rochester so that future students can have the same educational opportunities that he did.
Alan included the University in his estate plans, with provisions for both undergraduate and medical education scholarships. He hopes to ease the journey for students and believes there is great importance in paying his good fortune forward.
4 ROCHESTER MEDICINE | 2024 – V1 rochester.edu/together #TogetherForRochester IMAGINE YOUR LEGACY. To learn more about bequest intentions and other planned giving methods, contact the Office of Trusts, Estates & Gift Planning (800) 635-4672 • (585) 275-8894 • rochester.giftplans.org • giftplanning@rochester.edu
David Linehan Begins Tenure as CEO of the Medical Center and SMD Dean
David C. Linehan, MD, has succeeded Mark Taubman, MD, as CEO of the University of Rochester Medical Center and dean of the School of Medicine and Dentistry. He is also senior vice president for health sciences.
Linehan joined the University of Rochester in 2014 as chair of the Department of Surgery at URMC, recruited from Washington University School of Medicine in St. Louis. He is also associate director for clinical research at the Wilmot Cancer Institute and the Seymour I. Schwartz Professor in Surgery—a faculty position he will retain.
Linehan is a surgical oncologist internationally renowned for his clinical innovation and research into new treatments for pancreatic cancer. He guided URMC’s Department of Surgery through a period of tremendous growth. Under his leadership, the surgical faculty has flourished. He has:
• Recruited more than 50 surgeons, bringing new talent and specialty services to Rochester.
• Attracted scientists and promoted the growth of surgeon-scientists, securing millions in research funding.
• Attracted the best and brightest trainees, continuing the Department of Surgery’s legacy as a top-tier surgical training program.
• Achieved significant fiscal improvements through revenue growth and prudent fiscal management.
An accomplished surgeon-scientist, Linehan specializes in treating malignancies of the liver, pancreas, and biliary tract. He is recognized for studying and introducing novel and innovative therapies for patients with hard-to-treat cancers and has spent more than 20 years conducting immunotherapy research. One of his primary areas of focus is finding new ways to attack the biology of pancreatic tumors through activating anti-tumor immunity.
Linehan also treats benign surgical conditions of the liver, pancreas, gallbladder, and bile ducts.
“Moving to Rochester almost 10 years ago to be the Seymour Schwartz Professor of Surgery has proven to be the best professional decision I ever made,” says Linehan. “I am so grateful and honored for the opportunity to lead the Medical Center as CEO and the School of Medicine and Dentistry as dean. At the end of the day, it is the people that matter, and my wife, Janice, and I have felt so supported by both our URMC colleagues and so many members of the Rochester community.”
University of Rochester President Sarah Mangelsdorf said that Linehan “brings to the role of CEO and dean a vision for advancing the Medical Center, including the School of Medicine and Dentistry and School of Nursing, that draws on his outstanding track record of leadership and expertise as a physician, surgeon, researcher, and academic administrator. He is well-poised to lead our world-class clinical operations and our nationally recognized medical school into the next chapters of success.”
Linehan served as the Neidorff Family and Robert C. Packman Professor of Surgery at Washington University School of Medicine in St. Louis and was chief of hepatobiliary-pancreatic and gastrointestinal surgery before coming to Rochester. In 2018, he was named associate director of clinical research at the Wilmot Cancer Institute, where his contributions have bridged the clinic and the laboratory while building upon the Institute’s strengths in solid-tumor treatment and research.
His laboratory has been continuously funded by the National Cancer Institute for nearly two decades, and in addition to maintaining a busy surgical practice, he has established himself as a prolific bench-to-bedside researcher at Wilmot.
He and his team are conducting studies on new, targeted treatments with the goal of using newly discovered drugs in combination with immunotherapy, radiation therapy, and chemotherapy to improve outcomes for pancreatic cancer patients.
Linehan is also known for being a highly successful educator with a passion

for training the next generation of physician-scientists. He fosters a culture of collaboration that brings physicians, allied health professionals, and basic and health-services research scientists together to focus on projects that solve unmet clinical needs.
From 2017 to 2021, Linehan served as the University of Rochester Medical Faculty Group Finance Committee chair and he currently continues as a member of the Medical Faculty Group Executive Committee. Since 2014, he has served on the executive committee of the Wilmot Cancer Institute and as chair of the Wilmot Cancer Institute Clinical Research Leadership Committee.
A graduate of Dartmouth College and the University of Massachusetts Medical School, Linehan completed his internship and residency at DeaconessHarvard Surgical Service in Boston. He was chief resident in surgery at Beth Israel Deaconess Medical Center and completed a research fellowship at Brigham and Women’s Hospital in Boston. He was subsequently the Kristin Ann Carr Fellow in Surgical Oncology at Memorial Sloan-Kettering Cancer Center in New York City.
MEDICAL CENTER ROUNDS 5 ROCHESTER MEDICINE | 2024 – V1
Researchers Find Possible Neuromarker for Juvenile-Onset Batten Disease
by Kelsie Smith Hayduk

The progression of symptoms can be devastating: A child’s personality and behavior may change, and clumsiness or stumbling tends to develop between ages five and 10. Over time, cognitive impairment sets in, seizures emerge or worsen, vision loss begins, and motor skills decline.
This is the course of Batten disease, a progressive, inherited disorder that results from mutations to the CLN3 gene.
Now, a research team has measured changes in brain function in study participants and found that the functioning of the auditory sensory
Neuromedicine
memory system appears to decrease as the disease progresses. This suggests that this easy-to-measure brain process may be a target or biomarker in assessing treatment outcomes in clinical trials. John Foxe, PhD, director of the Del Monte Institute for Neuroscience and co-director of the University of Rochester Intellectual and Developmental Disabilities Research Center (UR-IDDRC), and a team of researchers from the University of Rochester Medical Center published their findings in the Journal of Neurodevelopmental Disorders.
The University’s Batten Center (URBC) is a leader in research and treatment of this condition and is designated a Center of Excellence by the Batten Disease Support and Research Association (BDSRA). With several potential gene therapies for Batten disease currently in advanced stages of development, this finding continues the mission at URMC to identify biomarkers to evaluate the effectiveness of these experimental treatments.
Researchers in the Frederick J. and Marion A. Schindler Cognitive
Neurophysiology Lab, where Foxe is co-principal investigator with Edward Freedman, PhD, are working to measure the impact that pharmaceuticals have on the auditory perceptual system. They are starting with treatments already on the market for other conditions.
“The auditory sensory memory marker provides a sensitive measure,” Foxe said. “We’ll be able to tell you pretty quickly if a treatment is having an impact and know if it is actually changing dynamics—i.e., whether the system in the brain is improving, what the speed of improvement is, etc. I think that is a big deal.”
Additional URMC authors include first author Tufikameni Brima, PhD; Kevin Prinsloo, PhD; Heather Adams, PhD; Kuan Hong Wang, PhD; Luke Shaw; and Emma Mantel. This research is supported by the Schmitt Program in Integrative Neuroscience (SPIN) through the Del Monte Institute pilot program, the National Institute of Neurological Disorders and Stroke, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Manipulating Fluid Flows in the Brain Could Save Lives, Improve Recovery Post-TBI
by Mark Michaud

Maiken
Nedergaard, MD, DMSc
Physicians have very few tools to effectively treat cerebral edema in traumatic brain injury (TBI), but a study by URMC researchers that appeared in the journal Nature could change that. It showed that a cocktail of drugs approved to treat high blood pressure quickly reduces brain swelling and improves outcomes in animal models of brain injury.
“Our research shows that cerebral edema is the consequence of impaired fluid flow through the glymphatic system and its associated lymphatic drainage,” said Maiken Nedergaard, MD, DMSc, co-director of URMC’s Center for Translational Neuromedicine and senior
author of the study. “This impairment is under adrenergic control and can therefore be rescued pharmacologically by broadly inhibiting adrenergic receptors. Because these drugs are already being used clinically and have observed neurological benefits, there is the potential to move quickly to clinical studies to confirm these findings.”
Nedergaard’s lab discovered the glymphatic system in 2012 as the brain’s unique waste-removal process. A growing understanding of its mechanics—aided by AI-driven models of fluid dynamics—has allowed researchers to better predict and manipulate the movement of cerebrospinal fluid (CSF) in the central nervous system.
This study points to the potential to repurpose the glymphatic system to act as an emergency “pressure release valve.”
One of the main triggers of cerebral edema is noradrenaline, a
neurotransmitter that floods the brain immediately after TBI. This restricts the movement of fluid through the glymphatic system’s “plumbing” section, where CSF drains from the brain and flows into the meningeal and cervical lymph nodes in the neck.
This observation led the team to test if reopening these gates to the lymph nodes could flush excess CSF from the brain, relieving pressure. They used a cocktail of drugs including prazosin, atipamezole, and propranolol, administered to mice soon after TBI. This resulted in an almost immediate elimination of cerebral edema and a sustained return to normal intracranial pressure. The treatment led to significant recovery of cognitive, behavioral, and motor function.
Assistant Professor Rashad Hussain, PhD, in the Center for Translational Neuromedicine was first author of the study.
6 ROCHESTER MEDICINE | 2024 – V1
MEDICAL CENTER ROUNDS
Neuroscience
Finding Obstacles and Opportunities in Rural Cancer Care
by Leslie Orr
“[The surgeon] told me he wanted to operate on the next Monday, and I told him I didn’t think I could get rid of the cows that fast because I’m a dairy farmer and I had 60 cows to milk every day.”
This was a cancer survivor from a rural area speaking in open-ended interviews with investigators from Wilmot Cancer Institute. It was part of a research study reported in the journal BMC Cancer, which showed that farmers and other rural-dwelling older adults who are underserved in cancer care are dealing with unique challenges.
The authors’ conclusion: Health-care providers should consider the particular needs of rural, older adults and educate them on survivorship care and how to overcome challenges to improve quality of life.
The objective of the study was to heighten awareness of survivorship needs from the perspective of the patients, said senior author Supriya Mohile, MD, a pioneer in geriatric oncology and co-leader of Wilmot’s Cancer Prevention and Control research program.
The study also called attention to the need for expanded services (including telehealth options) and deeper doctor-patient relationships.
Several themes emerged from study participants, including a general lack of communication about survivorship with their care team, physical and psychological challenges, and worry over paying medical bills. Many said they wanted professional advice about nutrition and exercise.
Transportation was a key issue for many patients, who did not like to drive to Rochester for care and had to rely on others to get to cancer-care appointments, whether in the city or in their rural hometowns.


Cancer Care
7 ROCHESTER MEDICINE | 2024 – V1
Supriya Mohile, MD
Pancreatic Cancer Discovery Opens the Door for New Clinical Trial at Wilmot
by Leslie Orr

URMC researchers made a breakthrough in learning about the genetic changes that occur during tumor migration in pancreatic cancer— and also found a drug that can obstruct the process.
The next step is a groundbreaking clinical trial at Wilmot Cancer Institute, planned for this year, to test that drug.
“We will be the first institution in the US to study the safety and effectiveness of the experimental anti-cancer drug NP137 on pancreatic cancer that has spread to the liver,” said senior investigator Darren Carpizo, MD, PhD, co-leader of Wilmot’s Genetics, Epigenetics and Metabolism research program, and chief of Surgical Oncology at the University of Rochester Medical Center.
Carpizo and several collaborators published the results of their bench-science investigation in the journal Cell Reports
In their latest work, the researchers built on what was already known about a key gene, Netrin-1, involved in pancreas, breast, and colon cancers. They discovered the complex mechanisms that allow Netrin-1 to drive the lethal genetic changes as pancreatic cancer cells migrate to the liver.
They also showed how Netrin-1 activates hepatic stellate cells, which are involved in the serious chronic disease
liver fibrosis, priming the liver as a host for cancer.
In mice and in tissue studies, when researchers suppressed Netrin-1 with NP137, cancer was less likely to spread, and cancer-cell death occurred.
NP137 is made by Netris Pharma, of Lyon, France, and is currently being tested in clinical trials in that country.
The Pancreatic Cancer Action Network (PanCAN) funded much of the work through a grant to Carpizo; Wilmot also provided pilot funding.
Carpizo will lead the Wilmot clinical trial with Aram Hezel, MD, chief of Hematology/Oncology at Wilmot, and Nabeel Badri, MBChB, a medical oncologist at Wilmot.
Carpizo’s study is part of a larger collaborative effort at Wilmot aimed at pancreatic cancer. Others, including URMC CEO David Linehan, MD; Wilmot investigator Scott Gerber, PhD; and members of the Cancer Microenvironment research program are also conducting studies on new, targeted treatments.
URMC First in Nation to Use Sound Wave Therapy for Liver Tumors by
Karin Christensen
Doctors at URMC are the first in the nation to use a cutting-edge therapy for patients with cancerous tumors in their livers. Using high-intensity sound waves, doctors are able to remove cancerous liver tissue without any incisions.
The procedure, called histotripsy, uses technology developed by HistoSonics. It can be a standalone procedure or serve as a

bridge to liver tumor resection or transplantation, especially for those with colorectal metastasis or primary liver tumors.
The first person in the US to undergo this procedure was treated December 18 by the URMC liver care team, working with the Wilmot Cancer Institute. URMC’s second and third patients were treated December 20.
MEDICAL CENTER ROUNDS Cancer Treatment
Cancer Treatment
8 ROCHESTER MEDICINE | 2024 – V1
Darren Carpizo, MD, PhD

Keeping a Human in the Loop: Managing the Ethics of AI in Medicine
by Susanne Pallo
Artificial intelligence is increasingly used to improve diagnosis and treatment and to avoid unnecessary screening for patients. But according to an international task force that included URMC’s bioethicist Jonathan Herington, PhD, AI medical devices could also harm patients and worsen inequities if they are not designed, tested, and used with care.
Currently, AI medical devices are being trained on datasets in which Latino and Black patients are underrepresented, meaning the devices are less likely to make accurate predictions for patients from these groups.
To avoid deepening health inequities, the task force said developers must ensure their AI models are calibrated for all racial and gender groups by training them with datasets that represent all of the populations the medical device or system will ultimately serve.
Herington was a member of the AI Task Force of the Society for Nuclear Medicine and Medical Imaging, which laid out recommendations on how to
ethically develop and use AI medical devices.
In two papers published in the Journal of Nuclear Medicine, the task force called for increased transparency about the accuracy and limits of AI and outlined ways to ensure all people have access to AI medical devices that work for them—regardless of their race, ethnicity, gender, or wealth.
While the burden of proper design and testing falls to AI developers, health care providers are ultimately responsible for properly using AI and shouldn’t rely too heavily on AI predictions in patient-care decisions.
“There should always be a human in the loop,” said Herington, assistant professor of Health Humanities and Bioethics. “Clinicians should use AI as an input into their own decisionmaking rather than replacing their decision-making.”
This requires that doctors truly understand how a given AI medical device is intended to be used, how well it
performs at that task, and any limitations. Doctors must also weigh the relative risks of false positives versus false negatives for a given situation, all while taking structural inequities into account.
“What that means for the developers of these systems is that they need to be very transparent,” said Herington.
According to the task force, it’s up to the AI developers to make accurate information readily available about their medical device’s intended use, clinical performance, and limitations. Developers must carefully define the data they use to train and test their AI models and should use clinically relevant criteria to evaluate the model’s performance.
It’s not enough to simply validate algorithms used by a device or system. AI medical devices should be tested in so-called “silent trials,” in which researchers evaluate the devices’ performance on real patients in real time without being used in actual clinical decision-making.
The Impact of AI
9 ROCHESTER MEDICINE | 2024 – V1
The Scientist CEO
How Mark Taubman used his research (and musical) mind to reshape URMC

As Taubman steps down as CEO and dean, we look at the legacy of his leadership and what it means for the future.
By Barbara Ficarra
Cover Story 10 ROCHESTER MEDICINE | 2024 – V1
Mark Taubman, MD, in the Craig Morrell lab at the Aab Cardiovascular Research Institute.

They were some of the biggest challenges that health care, and URMC, had ever seen.
Surging patient volumes. Rising costs of care outpacing reimbursements. Rural hospitals staring down bankruptcy, and urban populations wracked by economic downturns and disparities in care delivery. The seismic shift from fee-for-service to value-based payments. Precious dollars stretched thin between new technology and aging facilities. Fierce competition for research funding.
And all that culminating later in a global pandemic that shook the nation’s health care infrastructure to its roots.
Who would be the right person to lead Rochester through it?
How about someone who didn’t want the job in the first place? An accomplished pianist who might have chosen music over medicine. A research scientist who would have been happy never leaving the lab bench.
Twice, Mark Taubman, MD, was called to lead—as dean of the School of Medicine and Dentistry (SMD) in 2010 and then, in addition, as CEO of the University of Rochester Medical Center in 2015.
As it turned out, Taubman didn’t have to give up what he loved. Instead, in a sense, he brought the lab to the CEO office—with a musician’s ear for harmonizing competing needs and agendas.
What he helped change and establish during those years of health care crises and challenges—and what that means for the future of the School of Medicine as his successor, David Linehan, MD, takes the helm—is a lesson in using one’s strengths and understanding how to bring out the strengths of others.
First, though, they needed a plan.
Do the Job That’s in Front of You
Early in his career, Taubman didn’t seem focused on rising to the top. His longtime friend, Bradford Berk, MD, PhD, had recruited Taubman in 2003 to join URMC from Mt. Sinai to be chief of Cardiology. Taubman established his Cellular and Molecular Cardiology lab at the same time.
“In my first faculty jobs, I was a practicing cardiologist spending 75 percent of my time in the lab,” Taubman said. “I could have done that forever.”
But in 2009, SMD Dean David Guzick, MD, PhD, announced he was leaving for a position as president of UF Health at the University of Florida; Strong Memorial Hospital CEO Steve Goldstein and Chief Operating Officer Kathy Parrinello, PhD, encouraged Taubman to apply.
Accountable Health Partners Established
The clinically integrated network of physicians, hospitals, and other providers covers more than 400,000 patients in value-based contracts with insurers and has created $120 million in gain-sharing since its inception.

2013
11 ROCHESTER MEDICINE | 2024 – V1
“I told Steve and Kathy back then, ‘I don’t want to be dean—that’s not what I aspire to. The only job that could be worse would be CEO.’”
Clearly, his tendency to pour everything into what was in front of him caught people’s eye. “I’ve never looked ahead to the next job,” he explained.
But the next jobs had appeared. That same year, Berk—then CEO—suffered a debilitating spinal injury in a bicycling accident. Taubman stepped into both roles, as interim CEO for nine months as Berk recuperated, and then as dean following that. In 2014, Berk transitioned out of the position, and Taubman was tapped to be CEO.
The years working closely with Berk proved crucial. It was in 2014 that URMC would finalize a major strategic plan, begun under Berk’s leadership with input from Taubman.
In many organizations, a strategic plan arrives with fanfare and quickly fizzles out. But at URMC, it was a living document. It had to be, considering the challenges facing health care.
There was an urgent need to grow the system, expand the patient base, build a network across the region to bolster struggling rural hospitals, and fend off competitors from western New York and Pennsylvania.
“Mark played a big role in the strategic plan,” Berk said. “He did a lot of modeling around what were the key fiscal elements in the strategic plan that would enable us to provide money to the medical school for research while giving the hospital a voice in making those decisions. Bottom line: a holistic budget that looked at the two pieces not as separate but as inextricably linked.”
The plan’s centerpiece was to create a regional network by affiliating with struggling rural hospitals throughout the Finger Lakes region. Bolstering facilities would improve care for these communities, bringing more primary and secondary care close to home. This would also expand the number of patients to support the highly specialized care delivered in Rochester.
Creating a plan is one thing. Executing it is another. Over the next eight years, Taubman would need to bring home the very ambitious objectives of the plan with the patience and pragmatic approach he used in his research lab. He did it with the touch of another long-held skill of his: music.

Taubman became CEO after Bradford Berk, MD, PhD, (left) stepped down.
Leader as Conductor
In addition to performing as a pianist, Taubman always dreamed of being an orchestra conductor, and he sees the CEO role in that vein: “In music, the orchestra is doing the performance. The conductor is the interpretation: What voices to bring out, what instrumentation to bring in. What speed, what are you trying to convey.”
For Taubman, executing the vital elements of the strategic plan meant listening to how all the parts could work together to create a harmonious whole.
“I don’t remember him ever saying, ‘Adam, go do this,’ ” said Adam Anolik, senior vice president and chief financial officer for the Medical Center. “When discussing an idea, he seeks the input of everyone in the room. A lot of CEOs come in with a big personality, and you can’t talk until the CEO does. Mark is the opposite of that; he empowers not just people he works with on a regular basis but the entire Medical Center and University.”

2015
Noyes Memorial Hospital in Dansville and Jones Memorial Hospital in Wellsville Join UR Medicine
The affiliations expand UR Medicine’s network to five hospitals, including Strong Memorial, Highland Hospital, and Thompson Health.

2015
School of Nursing Receives National Recognition for Interprofessional Collaboration
The School’s Integrated Leadership Model was presented at the American Nurses Credentialing Center national leadership summit for academic nursing.
ROCHESTER MEDICINE | 2024 – V1
Cover Story: The Scientist CEO Cover Story: The Scientist CEO
Adam Anolik
12

2015-2022
Urgent Care Network Expands
The health system adds new sites to offer consumers convenient access and to reduce the burden on hospital EDs.
2016 Academic Reserve Fund Created
The fund functions essentially as a second endowment, strengthening the sustainability of SMD.
2016 URMC Tapped for National Residency Initiative
Accreditation Council for Graduate Medical Education names Rochester one of eight sites in the nation to lead a multi-year initiative to optimize residency training.
13 ROCHESTER MEDICINE | 2024 – V1
That approach helped turn ideas into action. “We all had a very clear vision,” Taubman said. “Whether research, clinical, education—it was very clear what we were trying to achieve strategically. When you have that you can do things quicker.”
And you can do more. “I like to think big,” he said. “That’s really how this started. When Brad was stepping down, at that point I saw a real opportunity to integrate the whole system.” He thought the idea of being both dean and CEO “would be critical to support the research mission and be more efficient.”
Since most academic medical centers have two people in those roles, those people tend to compete with each other. In a sense, integrating the roles at Rochester mirrored the goal of integrating the system as a whole.
When Taubman started his tenure as CEO, the Medical Center had two affiliate hospitals, Highland and FF Thompson. Affiliates now number seven, and URMC also has working agreements with other organizations in New York State.

“The importance of the regional network can’t be overemphasized,” said Jonathan W. Friedberg, MD, MMSc, director of the James P. Wilmot Cancer Institute and the Samuel Durand Professor of Medicine. “It has been critical to our success. During Mark’s term, URMC doubled the volume of cancer patients we see, and all the other clinical services grew as well.
“For an institution that provides tertiary and quaternary care, we have to serve a large enough population to justify having specialty services in cancer and other services. There aren’t enough patients in Monroe County alone. Now Wilmot is caring for a large portion of New York state; it provides the most quaternary procedures such as CAR-T cell treatments in the state outside of New York City.”
While a strategic plan can’t be as experimental as a science study, it can keep changing as needed—if someone has the eye for it.
“I like challenges,” Taubman said. “Science is a challenge. When you’re doing basic science, most of the time you know your experiment’s not going to work. You start with a hypothesis, you do an experiment, it doesn’t work, and you have to change your hypothesis. My whole upbringing in science is you’re always analyzing it.”
A strategic plan doesn’t have the same margin of error. But Taubman approached problems like a physician-scientist, gathering the most and best information possible in a given timeframe and proceeding with the best option. In that way, the strategic plan became “a plan that changes every year,” Taubman said. “It has to breathe.”
To balance the Medical Center’s many needs, Taubman would bring another skill to the table—one that surprised even the most experienced of leaders.
The Mathematics of Medicine
With such an ambitious plan, Taubman needed to make the numbers work.
“He had a very instinctive understanding of the finances of the Medical Center—that would be the thing you’d think he wouldn’t have,” said Tom Richards, former URMC Board chair and a UR trustee. “But he did and does. He seemed to easily adapt and understand it,” even in chaotic times.
“The ground is changing underneath him here—it’s not like you can memorize a formula.”

But Taubman brought an eclectic background to the job—one born out of a lifetime of interests and curiosity as he was growing up an only child in Brooklyn. His mother was famed piano instructor Dorothy Taubman, who devised the Taubman Approach to help pianists recover from musculoskeletal injury.
At age 12, he attended a science and music camp at Ithaca College. “I remember them taking us to the agricultural school and a room where they were doing a dissection of a horse. An entire horse.
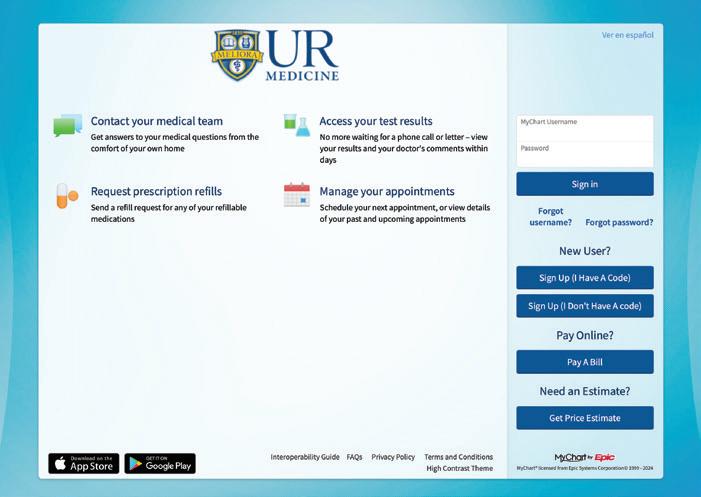
2017-2018 eRecord Expands
Upgrades to the system enable patient access to provider notes and bill pay through MyChart.
The hospital becomes the sixth to affiliate with UR Medicine.
Hospital Joins UR Medicine
2018 St. James
Cover Story: The Scientist CEO
Jonathan W. Friedberg, MD, MMSc
14 ROCHESTER MEDICINE | 2024 – V1
Tom Richards
Sixty percent of the boys ran out in horror, and the rest of us stayed. I was totally fixated. By the time I came back from that camp, I wanted to be a doctor. I also wanted to be a scientist.”
As a biochemistry major at Columbia, he learned to love mathematical modeling. In medical school at NYU, he met the man he would succeed as dean at Rochester: David Guzick.
“We started medical school on the same day,” Guzick said. “Mark and I were accepted into the MD-PhD program at NYU …. I was thrilled, as I’m sure Mark was as well, because it allowed us to be trained as investigators as well as physicians. The first-principles training we received in our respective disciplines turned out to be pivotal in the trajectory and scope of our careers in academic medicine.”
Guzick recalls that as a medical student, Taubman, true to form, was focused on the job in front of him: learning.
“Mark was always the first one there, last to leave,” Guzick said. “Because of his scientific background, he could bring information on the underlying pathophysiology of the patient’s
 Guzick, MD, PhD
Guzick, MD, PhD
20 19
Pathology Expands
UR Medicine consolidates and expands lab capacity in a new facility in Henrietta. Enabling all of our hospitals to share these services lowers costs and boosts quality.

2020
Golisano Pediatric Behavioral Health and Wellness Center Opens
New center addresses the growing pediatric behavioral health crisis by easing the burden of long waitlists in Monroe County.
 David
David
15 ROCHESTER MEDICINE | 2024 – V1
condition on rounds. Mark would always add a lot to the conversation.”
 Eliav, DMD, PhD
Eliav, DMD, PhD
His ability to continue connecting the dots helped him all along the way. Eli Eliav, DMD, PhD, director of the Eastman Institute for Oral Health and vice dean for Oral Health at the School of Medicine and Dentistry, noted what “an amazing researcher he was. As a cardiologist dealing with the system of the human body or as leader of the Medical Center, he is comfortable with complexity.”
This proved vital, especially considering the complexity of the Medical Center and of the strategic plan to transform it.
“I would watch him at meetings run through so many issues, from medical student credentialing to what’s going on with Excellus negotiations to a crisis in the Emergency Department,” said Friedberg. “He would go from one thing to the next without missing a beat. It’s very impressive how much he knows.”
Taubman, though, is quick to share the credit. And he returns to the conducting analogy to explain.
“If you’ve got the right people running your departments, hospitals, clinical services, then you’re directing them—helping push in a direction—but you’re not telling them what to do.”
At the same time, he used his fiscal and mathematical understanding to make sure SMD would thrive well into the future.
“The support for the academic medical mission has never been higher,” CFO Anolik said. “Under his leadership, he implemented an integrated financial model across the Medical Center that enabled us to invest some of Strong Memorial’s cash alongside

2020
Equity & Anti-Racism Action Plan Launches
URMC works with medical students, residents, trainees, faculty members, staff, and the community to create a blueprint for coordinating work to foster a more diverse and inclusive environment for all.

2022
Batavia Campus Opens
To better serve patients west of Rochester, URMC builds a campus that combines primary care and specialty services in a single location.
Cover Story: The Scientist CEO
16 ROCHESTER MEDICINE | 2024 – V1
Eli
the University endowment in an Academic Reserve Fund. Today, that fund generates over $16 million in annual earnings that directly benefit the Medical School.”
Yet nothing would challenge the fiscal and operational balance of the system more than what hit five years into his CEO tenure: COVID-19.
Walking the Walk in a Pandemic
“The leadership of the response to COVID is a good example of how Mark conducts business,” Richards said. He noted that Taubman had Strong Memorial’s COO Parrinello and Chief Medical Officer Michael Apostolakos, MD, chair the meetings, not himself, because they were responsible for leading hospital operations.

This is where his listening ear, and his belief in empowering individuals to lead, proved vital. It took the combined knowledge and leadership of thousands of people in the organization, both from hospital operations and the scientific side of the house, to guide the Medical Center through the pandemic. Taubman’s experience as a researcher gave him the confidence to trust others’ expertise and recommendations. Parrinello said, “Good researchers realize how complex problems can be, and they respect others’ expertise. The best researchers get a team together to meet the challenges of the times. Mark as a leader appreciated unique skill sets and supported people who had those skill sets to lead. He was inclusive of everyone’s perspective. He gathered voices and got the best solution.”
Taubman’s management-by-fact mindset was the right leadership approach for physicians and researchers. “Mark would say to me, ‘These people are scientists, and you need to lead them through the scientific process,’ ” said Richards. “ ‛They are not going to move unless you demonstrate with the processes they use every day that this approach is going to work.’ That matches with the institution we are—not just a hospital, but a large research organization.”
2022
Medical Ethics and Humanities Department Launches
One of the first medical school departments dedicated to using methodologies and inspiration from the humanities to reinforce the biopsychosocial model and instill humanistic values in faculty and student experiences.
Kathy Rideout, EdD, former dean of the School of Nursing, remembers seeing patients in the hospital during COVID and finding Taubman—a walker who tallies his daily steps—making laps around the building. She’d fall into step to discuss the issues of the day.
“He never lost his cool, never showed tension or anxiety,” Rideout said. “He just kept saying, ‘We will make it through.’ That calm demeanor from the top helped all of us. That kind of leadership is contagious.”

Even amid the crisis of COVID, he continued to think big. While other institutions were retrenching, URMC was not only sustaining itself but growing.
“In August 2020, we borrowed $225 million for the ED and patient-tower expansion and the orthopaedics campus,” Anolik said. “Mark had the foresight to recognize the short-term challenges but also say, ‘We have to build for the future.’”
Today the Medical Center is three times the size it was in 2010. “The growth has been tremendous—in buildings, faculty, staff. He’s never been afraid to invest in the future.”
It’s not just a matter of sheer size. “We’ve grown substantially, internally and externally,” Richards said. “We are a much more accomplished, established, and successful place than when he first came here, but always focused on medicine of the highest order.”
Research and Problem-Solving
“I’m grateful for having a CEO who is a researcher, who has had a lab and knows what it’s like to do research on a tight budget,” said University Vice President for Research and Chief Research Officer Stephen Dewhurst, PhD. “He values research very much—it’s part of the way he works to get to some form of ‘yes’ when it comes to research investments.”
Clinical revenues that support the research mission tripled under his leadership, from $40 million to $120 million, endowed research chairs from $45 million to $126 million. He has placed emphasis on
2022
Office of Health Equity Research Opens
The office supports innovative research exploring the causes and effects of health disparities to enable more equitable care.
2022-2023
Orthopaedics & Physical Performance Center Opens
The $227 million project greatly expands capacity and creates one of the largest ambulatory orthopaedics campuses in the United States.
17 ROCHESTER MEDICINE | 2024 – V1
Kathy Parrinello, PhD
Kathy Rideout, EdD
early-career faculty; the number of assistant professors in research rose from 84 in 2014 to 133 now.
The investment and foresight, said Dewhurst, will sustain the research mission over time: “URMC has a cadre of outstanding early-career faculty, as well as a highly collaborative and interactive research environment. Those assets will serve us very well long into the future and will enable us to achieve research goals and develop new research partnerships that would be extremely difficult to do in other places. The culture here that he has helped sustain at the highest level makes a profound difference. Over the next several years, Rochester will be increasingly attractive for many academics.”
Taubman places great emphasis on recruitment—for himself and for the people he recruits into leadership. All but four of the current chairs are his recruits, as was new Dean and CEO David Linehan, MD.
“The whole key of everything is picking great people and empowering them,” Taubman said. “Everything we’ve achieved has been achieved because we get great chairs, great associate vice deans, and senior associate deans who get it done, with support from the entire staff at URMC.”

For him, a good recruit is also a good recruiter. When Ophthalmology Chair and Flaum Eye Institute Director David DiLoreto, MD, PhD, interviewed for the position, Taubman asked about his strength in recruiting. DiLoreto took it as motivation to become a great recruiter himself.
“He supported recruitment of 29 Ophthalmology faculty in the last four years,” DiLoreto said. “We’ve had huge growth—basically doubled our department in size and grew from six to 11 satellite offices.”
“People want to come to a place where they think they can accomplish something, which means they are going to get the resources,” Taubman said. “We have done very well, compared
to our peers, through COVID. People don’t see an institution retrenching or downsizing here. They see an institution that’s vital.”
Leadership as a Partnership
Taubman said his approach to leading is straightforward. “Everyone knows it’s an open door. Anybody who wants to talk to me, they can. I also want to make it clear that they can say anything. Maybe I’ve yelled twice. Nobody is going to hear me yell or disparage them. Most everyone who comes in here with an idea, it’s a good idea. Let’s work on how we get this done.”
People discussing Taubman’s leadership style use many of the same words: Open door. Empowerment. Listener. Kind.
Taubman describes it this way: “I’m here to make you succeed; you’re not here to make me succeed. I will succeed if you succeed, but ultimately, you’re not here for me—I’m here for you.”
Again, it’s the calm patience of a researcher who knows he’s working on the problem. DiLoreto shared a saying Taubman would use: “The Medical Center could be losing money, losing patients, we have COVID, but everything would be better if the Yankees would just start hitting.” A stalwart Yankees fan since he was a child (ever since the Dodgers left Brooklyn), Taubman’s irrepressible sense of humor has helped the people around him.
“He has a very different vibe than a lot of leaders I’ve worked with,” DiLoreto added. “He gives people confidence, accessibility, hope, motivation. We always feel good about leaving a meeting with Mark,” regardless of the outcome. “He said no, but why do I feel better?”
And he has done it amid the complexity of all he oversees.
“Mark has exceptional leadership skills,” said Medical Center Board Chair Diana Kurty. “He was able to handle the complex issues that faced the Medical Center. This ability was crucial in collaborating with our varied constituencies at the Medical Center and University. That’s

2023
Finger Lakes Health Affiliation Established
The agreement adds Geneva General Hospital and Soldiers and Sailors Memorial Hospital, as well as long-term care facilities, primary care practices, specialty care practices, and subsidized housing for seniors.
2023
Highland Hospital South Tower Completed
The modernization project adds 58 private patient rooms and also adds space for clinical programs.

Cover Story: The Scientist CEO
David DiLoreto, MD, PhD
18 ROCHESTER MEDICINE | 2024 – V1
Diana Kurty

a very important aspect of his leadership style.”
He has done it by being a collaborator and partner instead of being hierarchical, said Michael Rotondo, MD, vice dean for Clinical Affairs and CEO of the UR Medical Faculty Group.
“He’s someone who really enjoys solving complex problems, and he’s particularly skilled at bringing people around the table to do that. There are always many different viewpoints; he doesn’t get locked into a decision until he has worked collaboratively with people. What kind of person does that? Someone who’s analytical, with enough emotional intelligence to look at complex problems with equipoise, and then he acts. That is uncommon.”

And he did it amid the ongoing challenges facing the Medical Center. “Every era presents financial and operational challenges, but no Medical Center CEO saw more challenges than Mark,” said Steven I. Goldstein, MHA, senior vice president of the Medical Center, who also serves as president and CEO of Strong Memorial and Highland hospitals.
Goldstein cites the enormous amount of time Taubman spent traveling the region to build the network of hospitals, reflecting his commitment to establishing trust between the institutions—a trust that proved invaluable when the pandemic hit.
What’s Next: More Exploration
Taubman isn’t really leaving. He’s working part time on select projects to keep moving URMC forward, splitting his time between Rochester and New York City, where he still has season tickets to the Met.
“We have a large health care system, but it needs much greater integration to reflect the fact that we’re a system,” Taubman said. “There’s a lot I’d love to do in care management. Ultimately, we will get into all value-based contracts, take more financial risks. There’s an enormous amount we can do to take out waste in health care delivery.”
As CEO, he launched the Diversity, Equity, and Inclusion program to address disparities in the region, but he knows that’s just a start. “We put things in place but there is much more that needs to be done. We clearly have a way to go in diversity in terms of the faculty.”
But he leaves behind an academic medical center that has changed immeasurably since the beginning of his tenure.
“He has charted a vision and a future that includes all our missions,” Apostolakos said. “Other health care organizations, in the face of challenges of the past few years, have cut back on the services they provide. We’ve never done that, and we’ve always kept research and education at the forefront. I think that’s really his legacy.”

Taubman can look back and know he helped lay the groundwork for whatever future problems need to be solved.
“It’s a real honor to have been CEO and dean for a great medical center, and I’m thrilled to help it move forward. With the regional network, we now have the size to be able to navigate under almost any reimbursement circumstance, and we can focus increasingly on delivering value. Integrating the budget has ‘de-risked’ the future of education and research. I’m very proud of the increase in endowed professorships. Eleven percent of everyone applying to a medical school apply here.
“What more can you ask for?”
Now if the Yankees would just start hitting. RM
2023-2027
ED and Patient Tower Construction Begins
The project will more than triple the size of Strong Memorial Hospital’s Emergency Department and add a nine-story patient tower to create 650,000 square feet of new patient-care space.
 Michael Apostolakos, MD
Michael Apostolakos, MD
19 ROCHESTER MEDICINE | 2024 – V1
Michael Rotondo, MD
Steven I. Goldstein, MHA

Think Locally, Research Globally
Rochester physician-scientists are venturing around the world for their studies.
The benefits are hitting home as well as abroad.
By Sandra J. Parker
20 ROCHESTER MEDICINE | 2024 – V1
In a Zambian hospital far from the country’s famous view of Victoria Falls plunging into the Zambezi River, URMC neurologist Gretchen L. Birbeck, MD, MPH, works on something equally lofty—global health.
Birbeck’s research on how to prevent post-malaria epilepsy may benefit Zambians and populations around the globe, including patients living 7,000 miles away in Rochester.
Continents away, in Argentina and Mexico, Francisco CartujanoBarrera, MD, conducts smoking-cessation research where community support and infrastructure can be stronger than in the United States. That means results can arrive more quickly and sometimes with lower costs—and what’s learned can help inform studies done here involving hard-to-reach populations.
“Global health equity is an obligation for rich countries,” says Paul R. Bohjanen, MD, chief of URMC’s Infectious Diseases Division and an HIV researcher in Uganda for the past 20 years. “Without international research, HIV would have decimated much of the world.”
Birbeck, Cartujano-Barrera, and Bohjanen are just three of the many Rochester doctors and researchers engaged in international research. It’s not only about investigation into treatment of disease but also about building sustainable health care “capacity” in the host country, preparing it to prevent, treat, and stem the spread of disease.
In a sense, given the depth of global connections in the 21st century, all medical research has international implications. A disease spreading in one country is a threat to every country. And there’s the humanitarian piece.
“It’s in our own best interest to participate in global health,” says Birbeck, who has conducted research in Zambia for 30 years.

“Many of the insights we gain from work conducted in places like rural Zambia inform research and care for patients in the US as well.”
And in some cases, the research can only be done internationally. Whatever the reason, these efforts come with challenges and rewards. In big ways and small, they are changing lives—those of participants and international populations and, in some cases, of the researchers themselves.
Helping There Helps Here
The ultimate cycle of international research occurs when a local program leads to global efforts that eventually come back home to enrich local research.
When James P. Wilmot Cancer Institute Director Jonathan W. Friedberg, MD, MMSc, used a data-mapping tool to assess the needs of residents in the Rochester region, he found high rates of cancer, particularly lung cancer: Incidences were 20 percent above the national average.
Smoking is the leading cause of lung cancer, so the Institute’s Office of Community Outreach and Engagement (COE) decided to focus on a cessation program. But that meant breaking down barriers in order to do it effectively, especially with the program’s emphasis on underrepresented and underserved populations.
Reaching an accurately diverse population requires coming up with solutions “with the community,” says social-behavioral scientist Ana Paula Cupertino, PhD, who was recruited four years ago to serve as the new COE associate director. “We must get out from our walls—we have to get out there to the community.”
 Francisco Cartujano-Barrera, MD
Francisco Cartujano-Barrera, MD
21 ROCHESTER MEDICINE | 2024 – V1
Gretchen L. Birbeck, MD, MPH, conducting research in Zambia.

Caption
Caption
“Global health equity is an obligation for rich countries.”
Moving beyond the walls of the Medical Center has meant hosting community discussions, conducting local studies to determine effectiveness—and drawing on the advantages of international research.
Cupertino and Cartujano-Barrera—a COE assistant director—have decades of experience between the two of them conducting research in Brazil, Guatemala, and Mexico.
This is proving important because in the US, Latinos have often been overlooked in research due to a lack of outreach programs. Generally, the only Latinos included in studies used to be the ones who participated on their own. That amounted to very few. Language barriers and disconnection from some mainstream institutions mean that important health messages, including research studies, don’t always reach this population.
Information about studies was often not translated, and some of it was culturally insensitive. For example, to some Latinos, the Spanish word cigarros can mean cigars or cigarettes, depending on their country of birth. Conversely, cigarettes can mean cigarettes or cigars. So it’s unhelpful to suggest that someone who smokes cigars enter a program designed to help them quit smoking cigarettes. Cartujano-Barrera also notes that many Latinos have an “I can do this by myself” attitude when trying to quit smoking. But research shows that culturally appropriate methods can draw Latinos into cessation programs.
Past mistakes such as linguistic and culturally inappropriate messaging have contributed to a sense of distrust that many US Latinos harbor toward medical institutions. As a result, it can be a lengthy process for researchers to make strong connections with community groups and build enough trust to draw participants to a study.
Those barriers, Cartujano-Barrera says, are lower or altogether absent in Mexico, where universal health care provides an infrastructure that allows researchers to
22 ROCHESTER MEDICINE | 2024 – V1
Argentina Mexico Rochester Uganda
Zambia
quickly identify individuals who would benefit from a smokingcessation program—regardless of their socioeconomic status. A strong community connection and more trust in medical institutions also boosts the ease of conducting a study.
Data gathered in studies conducted in Mexico continue to provide valuable information about how to effectively implement new smoking-cessation programs at home, says Cartujano-Barrera, who focuses on using mobile phones to deliver messaging. The research can be applied to the large Mexican population in the US as well, and it contributes to global health equity through shared research expertise.
Cartujano-Barrera is also heading up a five-year, NCI-funded smoking-cessation study in Argentina that is focused on the transgender community. Argentina, like Mexico, has strong community support and an established infrastructure to enable effective implementation of the study.
And solutions are needed there. More than 40 percent of transgender individuals smoke, placing an additional health burden on a vulnerable community already plagued by high rates of HIV and suicide. Often treated as social outcasts, members of this community generally suffer from high stress levels.
Most significant is that the researchers aren’t imposing their agenda on the population. It’s something that the transgender community wants because they see a need for solutions.
“The transgender community in Argentina set smoking cessation as a priority; this is their project. They are empowered,” says Cartujano-Barrera, who will serve as principal investigator along with Ines Aristegui, PhD, and Raul Meja, MD, PhD, researchers from Fundación Huésped, a nonprofit organization in Argentina. The team is enhanced by the leadership of Nadir Cardozo, a stakeholder in the transgender community.
Among transgender women in Argentina, cigarette smoking is associated with low educational levels, hazardous drinking, and drug use. The study seeks to answer how these and other factors—such as experiencing transphobia—affect a person’s ability to quit.
Argentina is the perfect setting to effectively implement this first-ever smoking-cessation trial with the transgender community, and the study has important implications for the US. Findings will expand the global understanding of tobacco use and cessation among transgender individuals. Moreover, methodologies are replicable and can inform subsequent smoking-cessation trials for US transgender individuals.
In a study published on December 5, 2023, in Frontiers in Public Health, Cartujano-Barrera and his team reported that transgender women in Argentina smoke at twice the rate as cisgender women. This supplies critical information in building a cessation plan both there and at home.
Key to making participants feel comfortable is the use of mobile messaging, which helps protect their privacy. It’s this sort of research expertise that can translate around the world.
“Good Intentions Are Not Enough”
Conducting international research adds complexity to researchers’ ethical responsibilities. The study in Argentina, addressing a community’s stated needs, is an ideal model. In past years, research was sometimes conducted in a paternalistic or predatory manner. The wealthy country used the population of a poorer country as study subjects, then went home—leaving participants no better off or only temporarily helped.
Without building the host country’s capacity, international research is unethical. “Good intentions are not enough, and every donation is not a gift,” Birbeck and others noted in a viewpoint article in the January 2, 2024, issue of JAMA Neurology
International research should fulfill the needs and priorities of the local population, make effective use of skilled local professionals, and create a sustainable mentoring program to ensure that the country receives long-term benefits.
For example, Birbeck explains it’s unethical for a researcher to test treatment on an international study participant with no intention of ensuring a reliable supply of medications.

Dr. Cartujano-Barrera's research in Argentina has strong community support.
23 ROCHESTER MEDICINE | 2024 – V1
Paul

“We are so interwoven into global health that it’s hard to imagine international research not being there.”
She has her own rules of engagement: “I actively avoid facilitating global engagement with individuals who think they are coming to save Africa, researchers who want to parachute in to collect data without any meaningful local collaboration, and bored people looking for a holiday thinly disguised as work.”
Sometimes international studies are the only way to understand a disease.
Bohjanen researches HIV in Uganda because patients there still develop complications as a result of HIV infection. The US population still experiences such complications but at a much lower rate, so it’s difficult to study the best treatments based only on research performed in the US.
International research can also serve as an agent for change in public policy. In Uganda, Bohjanen’s work has demonstrated to the country’s government what can be done to alleviate health problems. Solid evidence from research is an essential
24 ROCHESTER MEDICINE | 2024 – V1
Bohjanen, MD, PhD (fourth from left), with UR faculty and staff and local partners on a recent trip to Lira University in Uganda.
ingredient in refocusing local and global efforts to address health equity.
When Bohjanen made his first trip to Uganda in 2003, he visited a hospice and asked doctors how many had family members with HIV.
“Every one of these doctors raised their hands,” Bohjanen says. “Now I think less than 20 percent would raise their hands.”
The prevalence of HIV infections in Uganda’s capital of Kampala has dropped from 28 percent to just 3 percent in the past 20 years; deaths have also decreased.
“When I retire, I’m not going to stop working on global health in Uganda. I will keep doing this to make an impact,” Bohjanen says. “All diseases are still problems, but many are no longer devastating. We are so interwoven into global health that it’s hard to imagine international research not being there.”
In his many trips to Uganda, Bohjanen has lived in the country for up to a year at a time. The slower pace of life and the importance placed on relationships over possessions is “impressive” and a valuable part of the experience, he says.
Two of Birbeck’s NIH-funded studies examine the use of aggressive antipyretic therapy for fever control and the neuroprotective and/or side effects of the therapy. In addition to malaria deaths, more than a third of pediatric cerebralmalaria sufferers—about 200,000 children each year—end up with neurological disabilities. Her findings are key to reducing the effects of the disease and the accompanying disability for sufferers in malaria-endemic regions, but also has implications around the world.
In 2023, nine people living in the US were diagnosed with malaria even though they had not traveled to a country where the disease is endemic. These cases are not cause for panic, doctors say, but they show that even diseases once eradicated can return.
Global warming contributes to malaria incidence because the mosquito’s capacity to transmit malaria is temperature dependent. In other words, things change, and we aren’t finished learning about or dealing with problems like malaria here in the United States.
It Takes a Village to Get Supplies
There are challenges to conducting international research, particularly supply chain issues for medical necessities and for even basic necessities such as water. Nevertheless, Birbeck finds the community support “refreshing” and the doctor-patient relationship stronger.
“There are challenges everywhere, but the Zambian people are willing to try to make things work,” she says. “They don’t see anything as hopeless.”
 Paul R. Bohjanen, MD, PhD
Paul R. Bohjanen, MD, PhD
During the COVID pandemic, in a clinical trial being conducted in Zambia and neighboring Malawi, transporting supplies became difficult when Malawi shut down. But people found a way. Supplies were flown to the Zambian capital and transferred overland to the border. A minibus driver retrieved the supplies and passed them on to his gardener, who dropped them off with his brother, who then delivered the supplies to the hospital in Malawi. It took five days, but no supplies were lost.
“People are resilient and resourceful, so the study was able to continue uninterrupted,” she says.
When Birbeck first began international research, it was not considered a “real career or a legitimate academic endeavor,” she says, adding that now there is more of a recognition that science has no boundaries. The US field of research is crowded, but here in Zambia, research is “low-hanging fruit,” she says. “We’re stepping on fruit. There are so many questions you could ask.”
Thirty years ago, she was the only neurologist in all of Zambia. Now there are 10 local neurologists and a number of residents. During a recent visit by the NIH, the team made 47 presentations, almost all of them by Zambian professionals. Birbeck doesn’t take credit for the evolution but is happy to see it.
Birbeck plans to retire in Zambia. She owns property and pets in the capital city of Lukasa and in Rochester. When she’s in Zambia for six months of the year, she misses her URMC colleagues. She also misses beefsteak tomatoes, sweet corn, the Rochester foodie scene, and The Little Theatre. When she’s in Rochester, she misses her Zambian friends and “avocados the size of footballs.” RM
25 ROCHESTER MEDICINE | 2024 – V1

The Third Way
How Hildegard Messenbaugh’s new approach has salvaged the lives of troubled youth by Bethany Bushen
26 ROCHESTER MEDICINE | 2024 – V1
They call her “The Teenage Whisperer.” She’s an intent listener, caring and curious. Teens talk to her, unprompted, at street corners and in airports. Even now, at the age of 83, Hildegard Messenbaugh (MD ’66) is someone kids and teens are comfortable being around.
Messenbaugh turned her ability to connect with youth, along with her own exposure to childhood adversity, into a groundbreaking career. Five decades ago, she founded the Denver-based nonprofit Third Way Center and began challenging conventional thinking about mental health.
Her pioneering approach created a haven for thousands of youth— many deemed hopeless in the eyes of society. Teens grappling with drug-addicted parents, physical and psychological abuse, and life on the streets as runaways have worked through their problems at Third Way and turned their lives around.
Her vision was ahead of the curve in many ways. In 1970, the idea that trauma can be a root cause of troubled teen behavior wasn’t widely accepted. Decades ago, it was also assumed that damage done by trauma was permanent.
“When I was in medical school, I was taught the brain doesn’t change,” Messenbaugh said. “Nothing could have been further from the truth.”
Ignoring conventional wisdom, Messenbaugh developed an approach that addresses the trauma—not the behavior—in teens, using a series of structured steps.
Her approach has created lifelong believers, especially among those who have benefited from it. Their stories are living proof that The Third Way can be a life-changing way.
Prison or One Last Chance
Brendan Bartic, a successful real estate broker and entrepreneur in Colorado, is an Army veteran, national sales trainer, and president of the Third Way board of directors. You wouldn’t know it now, but by the age of 14 he was on the fast track to federal prison.
His father, a Vietnam War veteran, was an abusive alcoholic. His mother was a bipolar schizophrenic. Home was not a safe or stable place for their two children, so Bartic found himself avoiding it whenever possible, leading him to a harmful crowd and a path of crime that landed him behind bars.
He had been in and out of the foster system before ending up in juvenile detention. As a teen, he faced triple charges tied to drugs, theft, and drawing a firearm. His caseworker struck a deal with a judge who gave him one chance to turn things around—on the condition that he reside and receive treatment at Third Way.
With nowhere else to turn, Bartic took the deal. He arrived at Third Way in 1994 with nothing but a trash bag, jeans, and a t-shirt. He moved into Pontiac House, one of the residences on campus, where he met other teens with stories like his.

Third Way Center offers services for people ages 14 to 21 who lack the skills to live on their own. These include a five-house residential treatment program, two alternative high schools, and four specialized treatment programs.
The treatment process starts with an attempt to reconcile the family situation. In these meetings, Messenbaugh made an impression on Bartic right away.
She wasn’t afraid to smack you—not physically—but “emotionally, in a way that would help you move forward.”
Central to the work is her “Six Boxes” methodology, a structured approach to treating trauma in steps, from identifying destructive behaviors to processing trauma and taking steps toward restorative justice.
“We’ve understood since the inception of Third Way that behavior is related to trauma,” said Kristi Edmonds, PhD, LPC, clinical director at Third Way. “And if you only address the behavior, you’re not making real change unless you really deal with the trauma that is behind those behaviors.”
A key pillar of the Center’s approach is encephalopathy—the principle that trauma causes physical damage to the brain. The good news, however, is that the brain can heal with the right interventions.
“That gives us hope,” Messenbaugh said. “It makes us invent new ways of treating people and curing them.” The turn comes when counselors can “see the lights go on in an adolescent’s eyes, when they see what they have to do.”
After a few explosive meetings with his parents, Bartic says it was clear that reconciliation wasn’t going to happen.
“At that time, I didn’t know why I was so angry,” he said. “My whole life I was told our family was cursed. It was just kind of embedded in me that I was either going to just be a criminal or a security guard at Walmart because that’s all I knew.”
27 ROCHESTER MEDICINE | 2024 – V1
Hildegard Messenbaugh, MD

Over the course of months and years, he faced his trauma with help from counselors. It’s neither fun nor easy work. Bartic remembers a lot of screaming, crying, and storming out of sessions.
“What I respected was that her message to me wasn’t ‘Poor you.’ It was trying to find emotional justice,” he explained. “I was told that you don’t have to be OK with what happened to you, but she made me realize I had to take responsibility for my actions in order to process what I’d gone through and deal with it.”
Eventually he was able to move from Pontiac House to a more independent spot, Lincoln House, as he progressed through phases of treatment. Unlike foster homes, where he wasn’t permitted to leave the house, he had an apartment on campus where he learned skills like cooking and doing laundry for himself.
He got a job working for a company that made phone cards and learned how to open a checking account and balance a checkbook. He started to see what life could be like and that he wasn’t doomed to a lesser life. At the age of 17, he was emancipated from his parents and joined the Army.
Today his company hosts career-shadowing opportunities for Third Way teens. He is the president of the Center’s volunteer board, helping raise millions of dollars to keep the work going. He said he wouldn’t be doing it if he didn’t believe in the commitment of Messenbaugh and her team—even with the most difficult cases.
“If it wasn’t for Third Way and Dr. Messenbaugh, I would definitely be in prison,” he said.
He knows how much goes into turning a life around. “It’s an extremely difficult role to take people through their trauma,” he said. “She was tough. She was systematic. She’s seen everything and has probably been called every name under the sun by kids and parents from every walk of life.”
That’s how Third Way has helped thousands of people. But Messenbaugh almost didn’t survive her own childhood to do any of it.
A Story of Survival
At the age of four, Messenbaugh and her family were forced into concentration camps during World War II, not because they were Jewish but because they had fled her birthplace (present-day Serbia), where German-speaking natives were being targeted. They escaped to Austria but were considered fugitives by the Nazis and put into camps.
She remembers the sights and sounds of the year they spent in captivity, although she’s grateful to have been young enough for those flashes to remain dim in her memory. Messenbaugh later learned that she and her mother had been taken to the gas chamber but were spared. The reason? “They ran out of gas,” she recalls. “God saw fit to save my sorry behind for a reason.”
In 1945, she, her parents, and younger brother were liberated by the Allies. The family looked to the United States for a future, but her father died before he received immigration papers. Years passed before her mother finally received approval. By then, Messenbaugh was 16 and her younger brother was 11, and they were excited at the prospect of a new life in America.
But being an immigrant was “terrifying,” Messenbaugh admits. They settled in Rochester with almost no money, so her mother worked as a seamstress for the Hickey Freeman garment factory. A member of the employer’s family, Tom Hickey, kindly paid for Messenbaugh to attend Nazareth College, an all-female institution at the time.
She struggled to fit in. She distinctly remembers the words of a classmate who snapped at her for complaining one day, saying, “I’m sick of you. I didn’t come to your country—you came to mine. The least you can do is make an effort.”
That bit of tough love made her cry for a week. But it also struck a chord, and the two remain dear friends to this day.
Messenbaugh graduated from Nazareth in 1962 as president of her class, then attended the UR School of Medicine and Dentistry on a full scholarship. She quickly found the male-dominated setting different from the community in which she had thrived at Nazareth. Her goal was to become a neurosurgeon, but it would be a long road to get there.
Despite these difficulties, a bright spot came in the presence of George Engel, MD, Rochester’s legendary psychiatrist and teacher who pioneered the biopsychosocial model that thrives to this day. His idea that outside factors contribute to medical outcomes deeply influenced her holistic approach to care.
“He was probably the most fascinating human being I’d ever met. He was fabulous,” said Messenbaugh. “He was a brilliant teacher, and he taught me about a world that I’d never considered.”
Inspired by Engel and her own desire to help others, she found a clear path forward in psychiatry—one that offered the chance to help people process their pain and work to find a way out.
She completed her residency at University of Colorado Health Sciences Center. She and her husband, Bert, a surgeon, put down roots in Colorado, where they raised their children, Mark and Kristin, and still live today.
After completing her training, Messenbaugh volunteered for an after-school program for youth. She worked several years in the field and started a successful private practice in Denver. She then got the itch to found her own center. Of course, leaving a stable
28 ROCHESTER MEDICINE | 2024 – V1
Messenbaugh with two youths on a trip to Japan in 1976.
career behind came with risks, but she felt compelled to make a difference elsewhere.
In a stroke of good luck, she received a donation of $2,000 from a banker named Ken Caughey who had met Messenbaugh through her work at the University of Colorado, where she had been the medical director of the inpatient adolescent service. The gift was just enough to give her a jump start on the next chapter.
Studying psychiatry was partly accidental. But her first real clients happened to be teens, and she enjoyed working with them so much that she never looked back.

On the steps of the newly opened Lincoln House—a residence for older adolescents that first opened in 1992.
“When they get better, they really get better,” she said of adolescents. “For an adult to change a habit is really hard. But nature pushes towards equilibrium and growth at that age. So yes, there’s more Sturm and Drang, there’s more drama, there’s more carrying on. But there’s also that natural push.”
A Lasting Approach
How has Third Way stood the test of time? Bartic credits how the Center has evolved with medical and therapeutic treatments. In other facilities, he said, “they’re stuck in 1952, where when a kid yells, they’re tackled” and put in restraints. You see something altogether different, but no less demanding, at the Center.
“It was built on research and science, and I’ve been impressed with the continuance of innovation to never stop learning,” Bartic said. And that’s from Messenbaugh’s vision. “She researches constantly. It’s who she is.”
In the early days of Third Way, onlookers struggled to accept that negative behavior can be traced back to factors like physical and sexual abuse, violence, and poverty. It is a fact, however, that these can trap teens in a cycle of institutionalization, incarceration, or homelessness.
How can the cycle be broken? Restorative justice is an integral part of the Six Boxes methodology. It acknowledges that all abuse is unfair, but to keep it from controlling your life you must confront the

source of your abuse to move past it and thrive.
“I know one thing for sure. No one [messes] up their life on purpose,” said Messenbaugh. That’s been the cornerstone of the model she has built from the ground up—something she documented in her book, Getting Even: A Manual for Healing Childhood Trauma
David Eisner, MEd, executive director at Third Way, started working there in 1977 at the age of 23 and has watched it grow and evolve. He was struck by the way Messenbaugh has achieved a balance between showing empathy and being truthful about the road to resolution for patients. This helped shape his own outlook.
“She’s empathetic, but at the same time she’s truthful about what it takes for them to resolve it. She’s firm in terms of dealing with the abuse.”
Looking back, that firmness is what has inspired her team to stick with the most difficult cases and guide thousands of teens on their journey to recovery. Eisner is one of many who have chosen to stay at the nonprofit in large part due to her influence.
“It took me years to catch up to what she was doing,” said Eisner. “I wouldn’t be the person I am without her mentorship. She supported me in my growth and development when I really needed it.”
Today the center is staffed by 160 people and has an annual budget of more than $20 million. Messenbaugh continues to work full-time as medical director. The holistic, 24/7 approach requires grit and consistency from the care team and residents. But seeing results makes it all worth it, Messenbaugh says.
Their waitlist is long, with names from across the country. It’s a testament to Messenbaugh and her team, but she is grieved by the state of adolescent mental health care in the United States.
She points to outdated ideologies, improper allocation of resources to foster systems, and the closing of residential treatment centers. This ignores the science and sets up children and families for failure. Her convictions run as deep as her love for children and young adults. But love, she says, cannot cure a physical deficit. So, the work continues.
As far as the legacy she would like to leave behind, she laughs and says she’s just happy to get through the day. The numerous awards and accolades she has received are nice, but they’re not the point.
“The truth is,” she said, “I don’t deserve any of that because I’m having a great time.”
Visit www.ThirdWayCenter.org to learn more and to watch videos of patients sharing their stories.
29 ROCHESTER MEDICINE | 2024 – V1
One of the houses at Third Way's Lowry campus.
MATCH DAY 2024
Now in its 72nd edition: Match Day at SMD filled the Class of ’62 Auditorium with cheers and happy tears.
From Rochester's Class of 2024, 30 students will stay at the University of Rochester Medical Center for their residency training. The majority of the rest are staying in New York state (42), followed by Pennsylvania (7), and California (5). The rest matched in 26 other states and the District of Columbia.
The largest concentrations of specialties for SMD students are in Internal Medicine (15), Psychiatry (10), Family Medicine (8), and Pediatrics (7).
In all, 183 residents matched at URMC.





30 ROCHESTER MEDICINE | 2024 – V1





31 ROCHESTER MEDICINE | 2024 – V1
faculty news
URMC Taps Edith Williams to Lead the Center for Community Health & Prevention
by Susanne Pallo

A highly respected health researcher has been tapped to lead University of Rochester Medical Center’s Center for Community Health & Prevention (CCHP), which focuses on community outreach and public health. Edith M. Williams, MS, PhD, succeeds Nancy “Nana” Bennett, MD, MS, as director of the Center. Williams joined URMC in 2022 as the founding director of the Office of Health Equity Research.
Established in 2006, the CCHP works with communities in Rochester and the Finger Lakes to prevent disease and improve public health. The Center manages more than a dozen programs and initiatives to promote healthy living and prevent diseases such as cancer and diabetes and monitors infectious diseases such as flu, COVID, and RSV. It also promotes career pathway programs for underserved students and University employees.
Williams has more than 15 years of experience in community-based health equity research, and she has demonstrated the ability to build trust and relationships with patients and community members.
“Dr. Williams is a fast-rising star as a scientist who firmly believes that listening to the community is essential to improving public health,” said Martin Zand, MD, PhD, senior associate dean for Clinical Research and co-director of the Clinical and Translational Science Institute (CTSI), who co-led the search committee alongside Colleen Fogarty, MD, MSc, professor and William Rocktaschel Chair of Family Medicine. “With her dedication to improving health in our community and her demonstrated leadership skills, she is a perfect choice for this crucial role.”
Williams is also the Dean’s Associate Professor of Health Equity Research, as well as an associate professor in the Department of Public Health Sciences, the CCHP, the CTSI, and the Department of Medicine’s Allergy, Immunology, and Rheumatology Division.
As director, she wants to make sure the work of the Center is “solidly grounded in the needs and articulated priorities of the community.” That, she says, means supporting longstanding CCHP programs and expanding them to better reach special populations, such as Rochester’s Deaf community and socioeconomically disadvantaged rural and urban populations.
She also hopes to expand the Center’s strategic mission to address new community priorities, such as maternal and child mortality and the opioid crisis among underrepresented groups.
Williams will continue to oversee the Office of Health Equity Research.
“I am honored to be entrusted with the care and leadership of the CCHP,” said Williams. “Dr. Nana Bennett, who built the Center from the ground up, has set a high bar. I am both excited and grateful for the chance to carry on her legacy and advance the Center’s pivotal mission: to give everyone in our community the best chance at the best health possible.”
Bennett, who was the founding director of the CCHP, stepped down at the end of 2023 after 17 years in the position.
Before joining URMC, Williams served at the University of South Carolina as the deputy director for Research and Sustainability for the Institute for Partnerships to Eliminate Health Disparities and as assistant professor of Epidemiology and Biostatistics. Most recently, she was an associate professor of Public Health Sciences at the Medical University of South Carolina. She earned a master’s degree in Epidemiology and a doctorate in Epidemiology and Community Health from the State University of New York at Buffalo.
FACULTY NEWS
32 ROCHESTER MEDICINE | 2024 – V1
Edith M. Williams, MS, PhD
Jill Halterman Named Chair of Pediatrics, Physician-in-Chief of Golisano Children’s Hospital
by Scott Hesel

Jill Halterman (MD ’94, MPH ’94, Res ’98), Dr. Elizabeth R. McAnarney Professor in Pediatrics and executive vice-chair of the department of Pediatrics, has been named chair of the department of Pediatrics and physician-in-chief of Golisano Children’s Hospital (GCH). Halterman has served as interim chair since February 2023.
For the past 20 years, Halterman has supported GCH and the Rochester community by providing high-quality clinical care, conducting research to reduce barriers to care for children, and leading faculty and staff in Pediatrics.
She has in-depth knowledge of the children’s hospital and the people it serves, says Mark Taubman, MD, Emeritus Dean and CEO. “Dr. Halterman understands the unique needs of our community, having worked with children, parents, schools, and community groups for years. She is wholeheartedly dedicated to helping every child reach their full potential.”
Halterman has launched several successful regional programs that now serve as national models for improving care. For example, she
Lisa Lincoln Named Unsung Hero by
worked with a team to develop the Preventive Care Program for Children with Asthma, an initiative in partnership with the Rochester City School District and School Health Program.
“My goal as chair is to continue to support and grow programs that benefit children,” said Halterman. “From the perspective of a pediatric health-care provider, it is invaluable to be able to learn from the expertise of our patients, families, and partners in the community and work collaboratively to develop new approaches that lead to more equitable care and better health.”
Since 2015, Halterman has led the division of General Pediatrics, which includes research, education, and community programs, as well as the Golisano Children’s Hospital (GCH) Pediatric Practice.
She is also a distinguished researcher, having published more than 150 peer-reviewed articles and secured more than $28 million in extramural research funding.
Halterman served a one-year internship at the Children’s Hospital of Philadelphia before returning for her residency and fellowship at URMC. She has received multiple honors, including the Rochester Business Journal Health Care Heroes 2020 Physician Award, the 2019 Samuel Rosenthal Prize for Excellence in Academic Pediatrics, the 2019 Dr. David Satcher Community Health Improvement Award, and the 2013 Ruth A. Lawrence Academic Faculty Service Award for community-based research, mentoring, and leadership.
New York American College of Emergency Physicians

Lisa Lincoln (MD ’09, Res ’12), associate professor of Clinical Emergency Medicine, has been named a New York State Emergency Medicine Unsung Hero. This designation is awarded to physicians for their work ethic, compassion, and collegiality.
New York State Emergency Medicine Unsung Heroes are considered stalwarts of the Emergency Department.
“It is no secret that the current clinical practice environment in Emergency Medicine can be challenging,” said Timothy Lum, MD, FACEP, chief of Emergency Medicine for Highland Hospital. “It is these challenges that allow physicians like Dr. Lincoln to demonstrate just how exceptional they are. Dr. Lincoln is a role model within our department when it comes to patient care. She possesses integrity, truly cares about patients, and is unwaveringly kind, compassionate, and dedicated to the provision of excellent patient care. She does this all with an unparalleled humility.”
Lincoln, a Rochester native, was elected as a chief resident by her peers and Emergency Medicine faculty.
Jill Halterman,MD ’94, MPH ’94, Res ’98
33 ROCHESTER MEDICINE | 2024 – V1
Lisa Lincoln, MD ’09, Res ’12
Christa Whitney-Miller Named Chair of Pathology and Laboratory Medicine
 by Karin Christensen
by Karin Christensen
After a nationwide search, Christa L. Whitney-Miller, MD, professor of Pathology and Laboratory Medicine and vice chair of Anatomic Pathology at URMC, has been selected as chair of the department and named the Frieda Robscheit-Robbins Professor.
Whitney-Miller has served as interim chair since September 2022.
A surgical pathologist with a focus on gastrointestinal pathology, Whitney-Miller joined URMC in 2009 and has held numerous leadership positions, including director of the Gastrointestinal (GI) Pathology Service and director of Surgical Pathology. She is the founder and former director of the GI/Hepatobiliary Pathology Fellowship.
Whitney-Miller and the Pathology leadership team will continue to implement the department’s multi-phase expansion and consolidation project. Consolidating operations in a centralized facility will allow for sustained growth as volumes continue to increase.
Whitney-Miller will also continue to support efforts to expand the department’s homegrown training programs, developed to address the ongoing shortage of medical laboratory staff.
“It’s a privilege to have the opportunity to lead the Department of Pathology and Laboratory Medicine at the University of Rochester, including its 1,000-plus staff members, 70 faculty, and almost 100 trainees,” Whitney-Miller said. “Being from Rochester, I know the impact Strong Memorial and its affiliates have on our region.”
The department’s large clinical operation—more than 11.4 million tests are performed annually—supports all its missions: It keeps faculty engaged, provides great educational material for trainees, and is a rich resource for clinical and translational research studies.
Prior to joining URMC, Whitney-Miller served as a clinical assistant professor at the University of Pennsylvania School of Medicine and, subsequently, The Ohio State University College of Medicine.
Whitney-Miller is active in the Association of Directors of Anatomic and Surgical Pathology, where she serves on its executive committee. She has presented nationally at the United States and Canadian Academy of Pathologists, as well as at the College of American Pathologists.
She has received multiple honors, including the 2022 Margaret Billingham Award for Best Original Paper, published in Cardiovascular Pathology ; the resident award for best didactics in 2023; and the 2015 URMC Pathology Chair’s Recognition Award.
Elizabeth Santos Elected President of American Association for Geriatric Psychiatry

In March, Elizabeth Santos, MD (Flw ’06, MPH ’13), professor of Psychiatry, began her term as president of the American Association for Geriatric Psychiatry (AAGP). She is the latest of several AAGP presidents with URMC ties.
Established in 1978, AAGP works to improve the lives of its members, patients, and patients’ families; to train future geriatric mental health clinicians; and to advance research in the field. Its membership includes more than 1,000 geriatric psychiatrists and health-care professionals from the United States and Canada.
FACULTY NEWS
Elizabeth Santos, MD
34 ROCHESTER MEDICINE | 2024 – V1
Christa L. Whitney-Miller, MD
URMC Appoints Wellbeing Leadership Team and Inaugural Chief Wellbeing Officer
by Jim Miller

URMC’s first institution-wide Wellbeing Office is dedicated to improving the work and study environment of clinicians, staff, and learners.
S. Craig Rooney, PhD, who helped build a successful wellness program at the University of Missouri’s School of Medicine, will serve as URMC’s inaugural Chief Wellbeing Officer (CWO). Jessica Shand, MD (Res ’09), who has led URMC’s Medical Faculty and Clinician Wellness Program since 2022, will serve as associate CWO.
Together, they will spearhead efforts to advance professional fulfillment, health, and wellbeing across URMC’s clinical, education, and research missions. In a sign of the importance placed on the role, Rooney will serve as a URMC vice president and will report directly to URMC CEO David Linehan, MD
“We created these positions to ensure that wellbeing considerations are an integral part of everything we do and every decision we make,” said Mark Taubman, MD, emeritus dean and CEO. “Our employees devote their careers to caring for others; we have an institutional obligation to care for them.”
Rooney was hired following a national search and has moved to Rochester with his husband, Nathan. The partnership with Shand recognizes her passion for caring for her colleagues and the valuable work she has done.
“We want to help create a work environment in which every person feels valued and safe—one in which they know that they matter,” Rooney said. “And, of course, we want to assist in making sure that everyone at URMC has access to the meaningful wellness and wellbeing services they need to feel good in their work.”
Shand and Rooney said wellness is a larger issue than one leader can take on alone. “To me, one of the exciting things about our new partnership is that it represents institutional recognition of that fact,” Shand said.
For the past four years, Rooney has served as director of psychological services and wellbeing for the MU School of Medicine and MU Health Care, working in partnership with its CWO to establish a robust program.
Shand, a pediatrician, has been with URMC since 2013 and serves as associate professor of Pediatrics, Health Humanities, and Bioethics. She began working on wellness issues at the grassroots level in the Department of Pediatrics before joining the Medical Faculty and Clinician Wellness Program.
Alayna Loiselle Receives Orthopaedic Research Society Boskey Award
Alayna Loiselle (PhD ’09), associate professor of Orthopaedics, received the Orthopaedic Research Society’s Adele L. Boskey, PhD, Award for her contributions to musculoskeletal research and mentorship of next-generation scientists.
She leads the Loiselle Lab in the Center for Musculoskeletal Research, where her team’s work focuses on defining the fundamental cellular and molecular mediators of tendon homeostasis, tendinopathy development, and the tendon response to injury.
Loiselle’s research has been continuously funded by NIH since 2016, and she has been awarded more than $8.3 million in NIH funding as PI. Her lab has been at the cutting edge of the tendon-cell biology field, and she has been heavily involved in the adoption of emerging technologies.
Loiselle is also substantially involved in graduate education. She is MPI, along with Hani Awad, PhD, and Laura M. Calvi, MD, of CMSR’s T32 training program in Musculoskeletal Science and serves as Director of the center’s NIH P30-supported Histology, Biochemistry and Molecular Imaging (HBMI) Core.
In addition to receiving multiple F31, T32, and K99/R00 awards, her trainees also have been recognized with several major awards.
In 2016, Loiselle led the establishment of “MedClub,” a teen-empowerment initiative for Rochester City School District high school students. Loiselle’s lab also hosts students from the Summer Undergraduate Research Fellowship program—to attract and retain under-represented minority students to graduate or medical school. So far, three students from the program have completed medical school at SMD.

ORS gives the Boskey award annually to a mid-career member who has made significant contributions to the mentorship of rising scientists, engineers, and/or clinician/scientists in the fields of orthopaedics and musculoskeletal science and engineering. Awardees also have made significant research contributions and have demonstrated leadership.
Alayna Loiselle (PhD ’09)
35 ROCHESTER MEDICINE | 2024 – V1
S. Craig Rooney, PhD
In Memoriam
Microbiologist Barbara Iglewski, Champion of Female Scientists
by Emily Boynton
Scientist Barbara H. Iglewski, PhD, the first female department chair at SMD, passed away Dec. 10, 2023, at age 85.
Iglewski’s discovery that bacteria use a type of chemical language to coordinate attacks on human cells and initiate disease launched an entire field of study.
Recruited to Rochester from Oregon Health & Science University in 1986, Iglewski led the department of Microbiology and Immunology for 23 years. For many years, Iglewski was the sole woman among the school’s scientific department chairs. She went above and beyond to prove herself, working all day and frequently returning to work late at night.
“She had a drive that you would not believe, and her energy was just incredible,” said Dara W. Frank, PhD, a post-doctoral fellow in Iglewski’s lab at Oregon who moved with her to Rochester. “I will never understand how she was able to do what she did every day and also be able to fulfill all the demands of home and family.”
A role model for a generation of researchers, Iglewski was always on the lookout for talent. She took great pleasure in giving her faculty, students, and trainees opportunities for advancement.
Iglewski was especially interested in bolstering the careers of young women in Rochester and nationwide. She helped many women obtain editorial positions at scientific journals and tirelessly advocated for salary equity for female scientists.
“Barbara paved the way for many other female scientists and leaders, both here at the University of Rochester and across the country,” said SMD’s Vice Dean for Research Stephen Dewhurst, PhD, who succeeded her as chair of Microbiology and Immunology. “She left the department immeasurably stronger than she found it. As chair, she doubled the department’s tenure-track faculty members to 21 and grew its NIH funding from $1 million to $12.3 million, while also putting Rochester on the map with her groundbreaking research on bacterial quorum-sensing. At a personal level, she was an inspiring leader, a wonderful mentor to me and many others, and someone who earned the abiding loyalty of her staff.”
In 2015, Iglewski became the first woman from SMD to be inducted into the National Women’s Hall of Fame.
Her passion for science was no surprise. The daughter of a country physician, Iglewski grew up accompanying her father on house calls and playing with microscopes in his office.
All who worked with her recall her unfailing honesty; she spoke her mind and never minced words. Though she was tough and direct, former faculty members, trainees, students, and staff say you could tell her anything—and if you needed something, she got it for you.
Iglewski was also the University’s first female vice provost for research and graduate education. She received the University’s George Eastman Medal in 2019, SMD’s Lifetime Mentoring Award in 2009, the Susan B. Anthony Lifetime Achievement Award in 2001, and the Arthur Kornberg Research Award in 1999.

FACULTY NEWS
36 ROCHESTER MEDICINE | 2024 – V1
‘Gift Will Forever Be Appreciated’
Longtime Surgeon Helps Residents Attend Event that has Changed Lives
By Sydney Burrows
James L. Peacock, MD, FACS, spent his entire professional life at the University of Rochester Medical Center—and now he’s making sure others get some of the same crucial experiences he did.
Peacock established an endowed fund that allows every chief surgery resident at URMC to attend the American College of Surgeons Clinical Congress in their final year of study.
“The gratitude from the residents has been a special part of doing this,” Peacock says.
One recent graduate of the program, Kaci Schiavone, MD (Res ’23), says the Clinical Congress “was an excellent networking opportunity … to meet past faculty and graduates, surgeons from across town, and colleagues of current faculty members. I was able to experience firsthand just how vast the University of Rochester’s reach is. Dr. Peacock’s gift will forever be appreciated. It was an opportunity to see the true impact of academic medicine and see our co-residents present their hard work on a national stage.”
The experience was certainly important to Peacock. He arrived at the University in 1989—one of three new faculty members in the Department of Surgery—after connecting with Seymour I. Schwartz (Res ’57), the world-renowned surgeon and former chair of the department. The two met at the Clinical Congress, so Peacock appreciates the valuable connections and careerchanging opportunities that can come from these meetings.
“We were all from outside of Rochester, and we brought in different perspectives on surgery,” he says. “We were starting a new frontier in the department. The three of us—Dr. Harry Sax, Dr. David Krusch, and myself—worked together for nearly a decade.”
It was a rewarding time for him. “Dr. Schwartz opened the world of academic surgery to us, and his influence nationwide brought us opportunities. We became acquainted with various surgical dignitaries from around the country who would come to Rochester and visit. And when we would go elsewhere, people would recognize Rochester and Dr. Schwartz. It gave us instant credibility to be working at a place like this.”
Peacock, who has retired from his clinical practice but remains on the faculty, has praise for URMC’s academic environment: “The hospital and the Medical Center are strongly integrated with the University. You have the sense when you come on the premises that you’re part of an academic mission, just by proximity of the Medical Center to the University. But it’s more than that—it’s a sense of academic purpose that URMC has.”
As an educator and former residency director for the Department of Surgery, Peacock wanted to support training opportunities for residents. After a meeting of the American College of Surgeons in 2018, right after retiring from clinical practice, he attended a dinner for the Rochester residents who were attending the meeting, along with some of the graduates and faculty. It sparked an idea.
“I reflected on that event more than I had previously, maybe because I was in a retirement phase and thinking more globally about my purpose in life. I came away from that dinner thinking that this was something I would like to see happen in perpetuity.”
Peacock has gotten positive feedback from his colleagues as well, “because the fund allows a person to give within the scope of their financial means while creating a big impact for residents. It’s a win-win.”
James L. Peacock, MD, FACS (second from right), and chief surgery residents (from left) Katherine Rosen, MD (Res ’23), Kaci Schiavone (MD ’13, Res ’23), and Andreas Giannakou, MD (Res ’23).

37
PHILANTHROPY
Share your news
Your classmates want to hear about you! Did you move to a new city, begin a new project, or make a career shift?
Tell us about your recent travels, job developments, family updates, or anything else you want to share by submitting a class note.
Submit notes to your class agent or to uofr.us/smdclassnotes.
Or use this QR code:

Note: Alumni are listed by decade, then chronologically by class year under their respective degree categories, which include Resident & Fellows and PhD & Graduate Alumni.
CLASS NOTES
1960s
Louis Aledort (Res ’64) was featured in an article in ASH Clinical News, discussing his love of art and his extensive at-home collection of near-museum-worthy pieces, which he displays in his Upper West Side apartment in Manhattan. Aledort has been building his collection since completing his undergraduate studies at Queens College, fueled by a passion for art that matches his passion for medicine.
Joel Richmon (MD ’64) performed his final piano recital in March 2023 in front of an audience of several hundred people. This was the culmination of a decades-long career for Richmon in neurology at Kaiser Oakland while he simultaneously pursued his passion for piano.

1970s
John A. Vanek (MD ’74) is retired from medicine and is pursuing a second career writing mysteries. The fifth book in his Father Jake Austin mystery series, Epiphany, was recently released worldwide in paperback and eBook (Coffeetown Press). The series includes such titles as DEROS, Miracles, and Absolution. All three are also available in large-print hardbound editions.

Ross McKinney (MD ’79) retired from the Association of American Medical Colleges in November 2023 after seven years as its chief scientific officer. He and his wife, Holly, are looking forward to traveling and spending time with their four grandchildren, who live within a five-mile radius of their home in North Carolina. He previously retired from Duke Pediatric Infectious Diseases in 2016, where he did research on treatment of Pediatric HIV Disease and directed the Trent Center for Bioethics, Humanities, and History of Medicine. This time, he says, he’s fully retired.

1980s
Richard Schreiber (MD ’83) has been retired from clinical practice and administrative tasks for a year. He continues clinical informatics work and publishes collaborative research, including a chapter on governance and implementation of clinical decision support in Clinical Decision Support and Beyond (third edition). Now he has more time for vacationing and skiing with his family, which includes two grandchildren.

38 ROCHESTER MEDICINE | 2024 – V1
CLASS NOTES
1990s
Antonio Eppolito (MD ’94) retired as a Lt. Colonel in the United States Air Force after 28 years of active-duty service as a family physician and flight surgeon. His career spanned seven locations worldwide in inpatient, outpatient, and remote austere-environment deployments. His last assignment was as chief of Air Force Telehealth for the office of the Air Force Surgeon General at the Pentagon in Washington, DC. His current position as a civilian is as an outpatient family physician in the Primary Care Physicians Group at the Virginia Hospital Center in Arlington, Virginia.



A Class of 1978 mini-reunion: (from left) Doug Kamerow (MD ’78), Steve Birnbaum (MD ’78), Cyndi Jones, Helane Fronek, John Heller (MD ’78), and Jan Fronek (MD ’78).
A Trailblazer Remembered
Ernie Bates (MD ’62), pioneering neurosurgeon, died on March 19, 2024, at the age 87.
Dr. Bates was the only African American student in his class at SMD and one of only a few in the program, and at times he faced discrimination. He was also the first Black student to graduate from Johns Hopkins University's Krieger School of Arts and Sciences, in 1958.
He persisted and later became one of the first three African American board-certified neurosurgeons in the country—after serving in the United States Air Force in Japan for three years.
In 1977 he founded American Shared Hospital Services, which provides surgical operating equipment globally, and the Ernest Bates Foundation, providing grants to nonprofit healthcare organizations in African American and Latino communities.
He served as a University of Rochester trustee for two decades and was a cabinet member of The Meliora Challenge: The Campaign for the University of Rochester.
From philanthropy to medical trailblazing, Dr. Bates inspired throughout his lifetime.
39 ROCHESTER MEDICINE | 2024 – V1
In Memoriam
The School of Medicine and Dentistry expresses its sympathy to the loved ones of alumni and friends who have passed. (Updated January 2024)
John L. Goble (MD ’52), Oct. 20, 2023
Edwin Melvin Bradley (MD ’56), Dec. 15, 2023
William H. Marshall Jr. (BA ’53, MD ’56), Dec. 16, 2023
Richard Henry Pollen (MD ’56, Res ’60), Oct. 1, 2023
Mark H. Elias (MD ’57), Dec. 9, 2023
William K. Mangum (MD ’57), Nov. 27, 2023
Robert John Demuth (MD ’59, Res ’66), Jan. 16, 2024
Lewis B. Morrow (MD ’60), Nov. 28, 2023
Peter Jerome Leadley (MD ’64, Res ’66), Nov. 17, 2023
Donald Hardt Catlin (MD ’65), Jan. 16, 2024
Pierre E. Bertrand (Res ’65), Sept. 7, 2023
John Michael Dluhy (Res ’66), Jan. 10, 2023
Alan Jon Levine (BA ’64, MD ’68), Jan. 28, 2024
Adolph Matthew Hutter (Res ’68), Dec. 5, 2023
David August Mathison (Res ’68), Jan. 21, 2024
Paul N. Samuelson (MD ’68, Res ’72), Oct. 14, 2023
Ronald E. Feldman (MD ’69), Sept. 14, 2023
Frederick G. Guggenheim (Res ’69), Sept. 6, 2023
James A. Block (Res ’70), Oct. 9, 2023
Thomas W. Broughton (Res ’72), Nov. 12, 2023
David Nelson Smith (MD ’73, Res ’77), Oct. 3, 2023
Husayn A. Rashid (Res ’75), Oct. 2, 2023
David C. Thurber (MD ’77), Nov. 8, 2023
Leo Anthony Waickman (MD ’77), Nov. 2, 2023
Kathy L. Chrismer (MD ’82, Res ’84), Dec. 16, 2023
Jeffrey S. Clark (MD ’03), Oct. 18, 2023

In Memoriam 40 ROCHESTER MEDICINE | 2024 – V1

WILMOT BREAKAWAY leaving cancer in the dust Doug Phillips, Senior Vice President and Chief Investment Officer, University of Rochester #WilmotWarrior Register | Form a team | Sponsor warriorweekend.urmc.edu September 21-22, 2024 WARRIOR WEEKEND


NONPROFIT ORG U.S. POSTAGE PAID UNIVERSITY OF ROCHESTER PERMIT 780
SAVE THE DATE | SEPTEMBER 26-29, 2024 Don’t miss this exciting weekend filled with world-class entertainment, nostalgic reunion celebrations, presentations from faculty leaders, and more. #meliora | rochester.edu/melioraweekend
University of Rochester School of Medicine and Dentistry 601 Elmwood Avenue, Box 643 Rochester, NY 14642


 Ania Stolarczyk hugs Antonio Bottos (with Irianna Torres in background) during Match Day 2024.
Photo by J. Adam Fenster
On the cover
Mark Taubman stands in the Craig Morrell lab at the Aab Cardiovascular Research Institute.
Ania Stolarczyk hugs Antonio Bottos (with Irianna Torres in background) during Match Day 2024.
Photo by J. Adam Fenster
On the cover
Mark Taubman stands in the Craig Morrell lab at the Aab Cardiovascular Research Institute.
























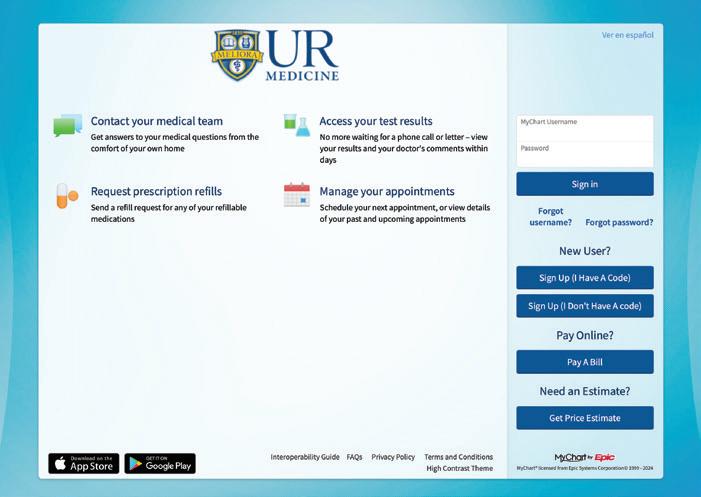
 Guzick, MD, PhD
Guzick, MD, PhD

 David
David
 Eliav, DMD, PhD
Eliav, DMD, PhD










 Michael Apostolakos, MD
Michael Apostolakos, MD


 Francisco Cartujano-Barrera, MD
Francisco Cartujano-Barrera, MD



 Paul R. Bohjanen, MD, PhD
Paul R. Bohjanen, MD, PhD


















 by Karin Christensen
by Karin Christensen
















