


























Staying hydrated is important all year, but especially in warmer weather. Fluid plays vital functions in the body such as regulating temperature, dissolving and transporting nutrients, delivering oxygen, lubricating joints, flushing waste and sustaining organ health. Keep your body working well with these simple tips.





















Beyond water: ways to increase fluid intake



















11.5 8-OZ. CUPS OF FLUID PER DAY (WOMEN)
15.5 8-OZ. CUPS OF FLUID PER DAY (MEN)
Signs of dehydration







Decaf coffee or tea SoupSeltzer (flavor it yourself with fruit)
HIGH-WATER-CONTENT FRUITS AND VEGETABLES:
Watermelon
Strawberries
• Thirst
• Dry lips and mouth
• Irritability
• Headache
• Dizziness

• Flushed skin
• Muscle cramps






• Constipation
Peaches
Oranges
A quick hydration check
Check the color of your urine. Pale yellow = adequate hydration

Dark yellow or amber = increase fluids

Serves 4
INGREDIENTS:
• 1 cup frozen strawberries
• 1 cup frozen blueberries



• 1 cup strawberry-flavored seltzer


• 1 tablespoon honey




DIRECTIONS:
Combine all ingredients in a blender until smooth.




Zucchini
Cucumbers
Lettuce
Celery Tomatoes
Note: Caffeinated beverages and alcohol have a diuretic (creating more urine) effect, which may contribute to hydration loss.
NEED A PRIMARY CARE PROVIDER? TO MAKE AN APPOINTMENT, CALL OXFORD INTERNAL MEDICINE AT 513.523.4195









SHANNAN BOWMAN at first noticed tingling in her hand. Then the sensation gradually became more disruptive. “At night, I had pain and numbness that woke me up at times,” says Shannan, who works in Central Supply at McCulloughHyde Memorial Hospital | TriHealth (MHMH).
The problem: She had developed carpal tunnel syndrome. The condition occurs when the median nerve—which governs hand sensation and movement in most fingers—becomes pinched as it passes through a space between bones in the wrist called the carpal tunnel. More common in women than men, the syndrome typically gets worse over time.






Fortunately, a solution was close at hand: An outpatient procedure at MHMH called carpal tunnel release could relieve her pain and numbness.
Yet the prospect initially seemed daunting. “I did not really want surgery,” says Shannan. She first tried wearing a

wrist brace in hopes of taking pressure off the nerve. “But that became impractical,” she says. “I decided surgery just needed to be done.”
Carpal tunnel release is one of numerous surgeries performed at MHMH on an outpatient basis, meaning patients can go home shortly after their procedures. “Patients are discharged the same day in about 80 percent of our surgeries,” says Jessica Goeke, BSN, CNOR, Perioperative Nurse Manager at the hospital.
Many outpatient surgeries are orthopedic, including (along with carpal tunnel release) arthroscopic knee and shoulder procedures to remove scar
tissue or make repairs, or even relatively complex operations such as repairing torn anterior cruciate ligaments (ACLs). More general surgeries such as gynecologic procedures, hernia repairs and gallbladder operations can also often be done on an outpatient basis.
“Being at home with family and able to sleep in your own bed helps calm the natural anxiety people feel about surgery,” Goeke says. “That can improve the healing and recovery process.”
“It’s much better to recover at home,” agrees Shannan, who had her surgery at MHMH in December 2022. In a minimally invasive endoscopic procedure, Craig Lindsey Bierer, DO, an orthopedic surgeon who had also performed shoulder surgery on Shannan’s husband, made a small incision and snipped a tendon to relieve pressure and create more space in the cramped carpal tunnel.
“My hand is much better now,” Shannan says. “Every person involved in my care made me feel relaxed, comfortable and safe.”
Patient comfort and safety are priorities for the dedicated and experienced team in the Same Day Surgery Department, Goeke says. Another priority is easy scheduling, with surgery booked soon after a patient decides to undergo a procedure—often before the patient leaves the doctor’s office.


“I found the people in Same Day Surgery and the operating room at MHMH to be smart, kind, professional, warm and caring,” Shannan says. “The whole team worked together and didn’t miss a beat. It was a very smooth process.”
TO SCHEDULE AN OUTPATIENT PROCEDURE (REFERRALS REQUIRED) AT McCULLOUGH-HYDE MEMORIAL HOSPITAL, CALL THE CENTRAL SCHEDULING DEPARTMENT AT 513.524.5555 .
The carpal tunnel release surgery that Shannan Bowman (far left, with surgeon Craig Lindsey Bierer, DO) underwent is just one of many outpatient procedures available at MHMH, says Jessica Goeke, BSN, CNOR (left).AMY KHERA, DO, and Ricardo Maddela, DO, were such good friends before they became a couple that they’re not entirely agreed on what counts as their first date. They usually went out with a group of friends and had known each other for years. But one night in 2001, they went to dinner first, just the two of them. “Our friends were like, ‘You went on a date,’” Dr. Khera laughs, “and Rico said, ‘That wasn’t a date.’” But shortly afterward, the two attended a concert together. “At that point, he was saying, ‘OK, now we’re dating,’” she says.
Enrolled in premed studies at Xavier University in Cincinnati at the time, they’ve since become physicians and have been married for 15 years. Now they’ve both joined the medical staff at McCullough-Hyde Memorial Hospital | TriHealth (MHMH).
Dr. Maddela is a general surgeon trained in robotic techniques who handles a range of procedures such as hernia repairs; bowel surgeries; gallbladder and appendix removal; breast cancer surgery; treatment for cysts and abscesses; and wound care. Dr. Khera is a family medicine physician with Oxford Internal Medicine who works with patients and loved ones on an ongoing basis to treat problems, improve health and reduce risks.
“We both like the size and family-oriented nature of community hospitals,” says Dr. Maddela. “Oxford seems like the perfect place for us.”
Community medicine seems to be in their blood. Dr. Maddela grew up in Henderson, Kentucky, the son of two physicians—his father a general surgeon and his mother in internal medicine. One of his sisters is a nurse practitioner, and another is an obstetrician-gynecologist. Dr. Khera has cousins and aunts in medicine. “He and I have a bond in growing up around the medical field,” Dr. Khera says.
The two met early in their undergraduate studies. “We were in several of the same classes and have similar interests,” Dr. Maddela says. Their broader circle of friends saw—before the couple did—that the two had a special spark. “We were kind of oblivious,” Dr. Khera says. “Our friends would say, ‘Can you guys just go on a date?’”
After college, Dr. Khera spent a year in the corporate world before joining Dr. Maddela at the University of Pikeville’s Kentucky College of Osteopathic Medicine. “I chose family medicine because I love the continuity of care and
SHARING A LOVE FOR HEALTHCARE HELPS A PHYSICIAN COUPLE SUPPORT EACH OTHER AND THEIR PATIENTS.
developing long-term relationships with patients and families,” Dr. Khera says. “He enjoys the way general surgery involves solving problems and helping people immediately.”
Both did their residency programs at Grandview Medical Center (now Kettering Health Dayton) in Dayton, Ohio. And both initially practiced at a community hospital in Henderson, where Dr. Maddela and his father sometimes did surgeries together.
Sharing their profession helps the couple support each other—and patients. “She helps me understand the primary care side of medicine,” Dr. Maddela says. “She also knows the stress of our jobs. She’s always been very supportive and there for me.”
“It’s comforting that the other person understands what you’re talking about and may have insights you’re not considering,” Dr. Khera says. That’s especially true if they share a patient, which was common in Henderson. Care receivers—given an open field of doctors to choose from— often seemed more comfortable having specialists who were close to each other.
Just as electronic medical records improve care by allowing physicians to view notes from other healthcare providers, Dr. Maddela and Dr. Khera sometimes help each other track the progress of patients they have in common. “I can ask him, ‘How did So-and-So’s surgery go today?’ and he can tell me immediately that they’re doing well,” Dr. Khera says. “Or I can tell him I saw the patient and he can say, ‘How did their sutures look?’ It’s like an extra layer of patient support.”
After 12 years in Kentucky, Dr. Khera wanted to be closer to her father in West Chester, Ohio, where she grew up, and the couple was pleased to find opportunities awaiting both of them in Oxford. “I enjoy the small-town vibe and family atmosphere,” Dr. Maddela says. “Oxford is a very nice town, and Miami University’s campus is beautiful.”
Off-duty, the couple prioritizes time with their 12-year-old son. He and they enjoy collecting sports-related trading cards and sports overall, including going to Cincinnati Bengals and Xavier games. They also enjoy traveling when possible, such as a major excursion to Asia in 2018 that included seeing members of Dr. Maddela’s family in the Philippines and Dr. Khera’s family in India.


They’ve found Oxford-area colleagues and patients to be open, friendly and welcoming, often offering recommendations for restaurants or places for outdoor activities such as hiking at Hueston Woods State Park— appealing to osteopathic physicians whose approach to medicine embraces a holistic interest in body, mind, spirit, lifestyle, diet and exercise.
“Our hope is not only to care for patients and help them manage their health in a positive way, but to make the community a healthier place overall,” Dr. Khera says. “We’ve found people to be really nice and grateful to have us, and we are just happy to be here.”
TO SCHEDULE AN APPOINTMENT WITH DR. AMY KHERA AT OXFORD INTERNAL MEDICINE, CALL 513.523.4195
FOR A GENERAL SURGERY APPOINTMENT WITH DR. RICARDO MADDELA AT TRIHEALTH SURGICAL INSTITUTE—OXFORD, CALL 513.853.9000
OWEN KING came to appreciate athletic trainers from McCullough-Hyde Memorial Hospital | TriHealth (MHMH) almost immediately upon joining the Talawanda High School football team. “It happened in the first scrimmage of my freshman year,” says the now-16-yearold junior of his first high school sports injury.

In a game at Roger Bacon High School, Owen tackled an opponent as a teammate rushed in to assist. Owen’s forearm became pinned between the players as he rolled one way and the opponent rolled the other. “My elbow bent in the completely wrong direction,” Owen recalls.
MHMH athletic trainer Greg Daniels, MS, LAT, ATC, was on-site under the Friday night lights for just such a moment. “Owen dislocated his elbow,” says Daniels, who had reduced, or realigned, another Talawanda player’s dislocated elbow just two weeks before. “Owen also had an associated fracture of his medial epicondyle”—a bony protuberance at the end of the humerus. “Due to the complication of the fracture, I asked the orthopedic doctor on-site from the other team to reduce Owen’s injury,” Daniels says.
That was just the start of Daniels’ care for Owen. With the elbow back in place, Daniels used ice to decrease swelling
and placed a sling to immobilize the joint. Then he contacted team physician Bryan McCullough, DO, an orthopedic surgeon and sports medicine specialist with Beacon Orthopaedics & Sports Medicine, for further evaluation, tests such as X-rays and eventually surgery.
“When an athlete has a major injury, it’s important to start healing as soon as possible,” Daniels says. He later spent weeks helping Owen rehabilitate.
“By the morning after the game, Greg already had an appointment for Owen to see Dr. McCullough first thing Monday,” marvels Owen’s mother, Dawn King.
“Surgery happened Wednesday. Our athletic trainers do an incredible job.”
Daniels and colleague Kendall Cramer, LAT, ATC, exemplify what athletic trainers do for local student athletes, their families, coaches and the community. As multiskilled healthcare professionals, trainers not only provide on-demand, on-site care during games, practices and more, but also forestall injuries by identifying high-risk behaviors and building preventive care programs.
When injuries do occur, athletic trainers provide comprehensive evaluations, create care plans, refer athletes to specialists and promote healing through therapeutic exercise, taping, protective gear and other methods.
“We’re there from the time an athlete is injured until their return to their sport, guiding them every step of the way,” says Cramer. “We often witness athletic injuries, which is a huge benefit because we can see the mechanism of what happened and understand what could be wrong even before we evaluate. We then tailor treatment and rehabilitation to their specific needs.”
MHMH athletic trainers are present full-time throughout the year and help students in sports including basketball, soccer, baseball, softball, lacrosse and track and field. MHMH provides athletic trainers not only to Talawanda but also to Ross High School and, in Indiana, Franklin County High School and Union County High School. Trainers prepare athletes for action, ensure that medical and safety equipment is available at competitions and practices, and maintain school training rooms in addition to observing, evaluating, treating and rehabilitating injuries.
“We take a team approach to enhancing recovery,” Daniels says. That entails communicating with everyone supporting an athlete. “It’s important that athletes, parents/guardians, doctors, physical therapists and coaches are all on the same page so that the athlete continues doing the right things to get back on track,” Daniels says.
Athletic trainers also watch students for internal challenges. “Well-being extends beyond physical health,” Cramer says. “If an athlete struggles with mental
health issues such as depression or anxiety surrounding an injury, they may heal more slowly. We spend time with athletes, get to know them and advocate for them in every setting to get them the care they need.”
After elbow surgery, Owen worked with an MHMH physical therapist through December of his freshman year to heal and regain range of motion. Coordinating with the therapist, Daniels added supplemental exercises and stretches. “We also did cold treatments and taped or braced Owen’s elbow once he returned to football,” Daniels says.
When Owen sustained an off-season high ankle sprain heading into junior year, range-of-motion and strengthening exercises along with taping and bracing helped heal the sprain in time for football season.


Then came another first-game injury. “Someone’s helmet went straight into my shin,” says Owen. He struggled to walk
off the field. Daniels texted Owen’s father to come from the stands to the sidelines as Daniels and Dr. McCullough evaluated the injury. “They told my husband there was a good chance of a fracture,” Dawn says.
Owen was afraid he’d miss another season. But prompt X-rays showed a manageable stress fracture. “Getting an answer so quickly eliminated a lot of distress for Owen,” Dawn says.
After a period of rest, in consultation with Dr. McCullough, Daniels and Cramer had Owen do lower extremity exercises to target critical muscles and tendons, fashioned a shin guard to protect the injury site and applied ice bags after games to suppress pain and swelling. “Greg and I made sure Owen was as safe as possible while continuing to play the sport he loves,” Cramer says. In time, the injury completely healed.
“They’re really nice, understanding and helpful,” Owen says of his athletic trainers. “If you have any issue, they’re always there for you.”
TO LEARN MORE ABOUT ATHLETIC TRAINING SERVICES PROVIDED BY McCULLOUGH-HYDE MEMORIAL HOSPITAL, EMAIL PROGRAM MANAGER KYLENE SPALDING AT KYLENE_SPALDING@TRIHEALTH.COM OR CALL 513-893-8363
careand oversight.
ABOUT ONE IN 50 PEOPLE in the United States has a brain aneurysm—a “balloon” of blood protruding from an artery. The majority of these will never burst or even require treatment.
But for the approximately 30,000 people each year whose aneurysms do burst, the consequences can be devastating, leading to brain damage, stroke or death.
Awareness about aneurysms is important because studies have indicated that some people who have a ruptured aneurysm die due to a misdiagnosis. What’s more, many
doctors have seen an increase in ruptured aneurysms since the start of the COVID-19 pandemic. This may be because people have been less active, perhaps gaining weight or not controlling high blood pressure. In addition, people who may have warning signs of an aneurysm often neglect them, assuming symptoms will simply go away.
The classic indication of an aneurysm is a severe headache—one that feels like the worst headache of your life. Not every headache is an aneurysm, of course; most of the time,
headaches are not anything serious. But if you have a terrible headache along with neck stiffness and/or a sense that bright light is bothersome, you should head to the Emergency Department to have these potentially serious symptoms investigated.
Aneurysms can be diagnosed by a CT (computed tomography) scan, which uses X-rays to determine whether blood has leaked into the brain. Doctors may also order an MRI (magnetic resonance imaging), which uses a combination of
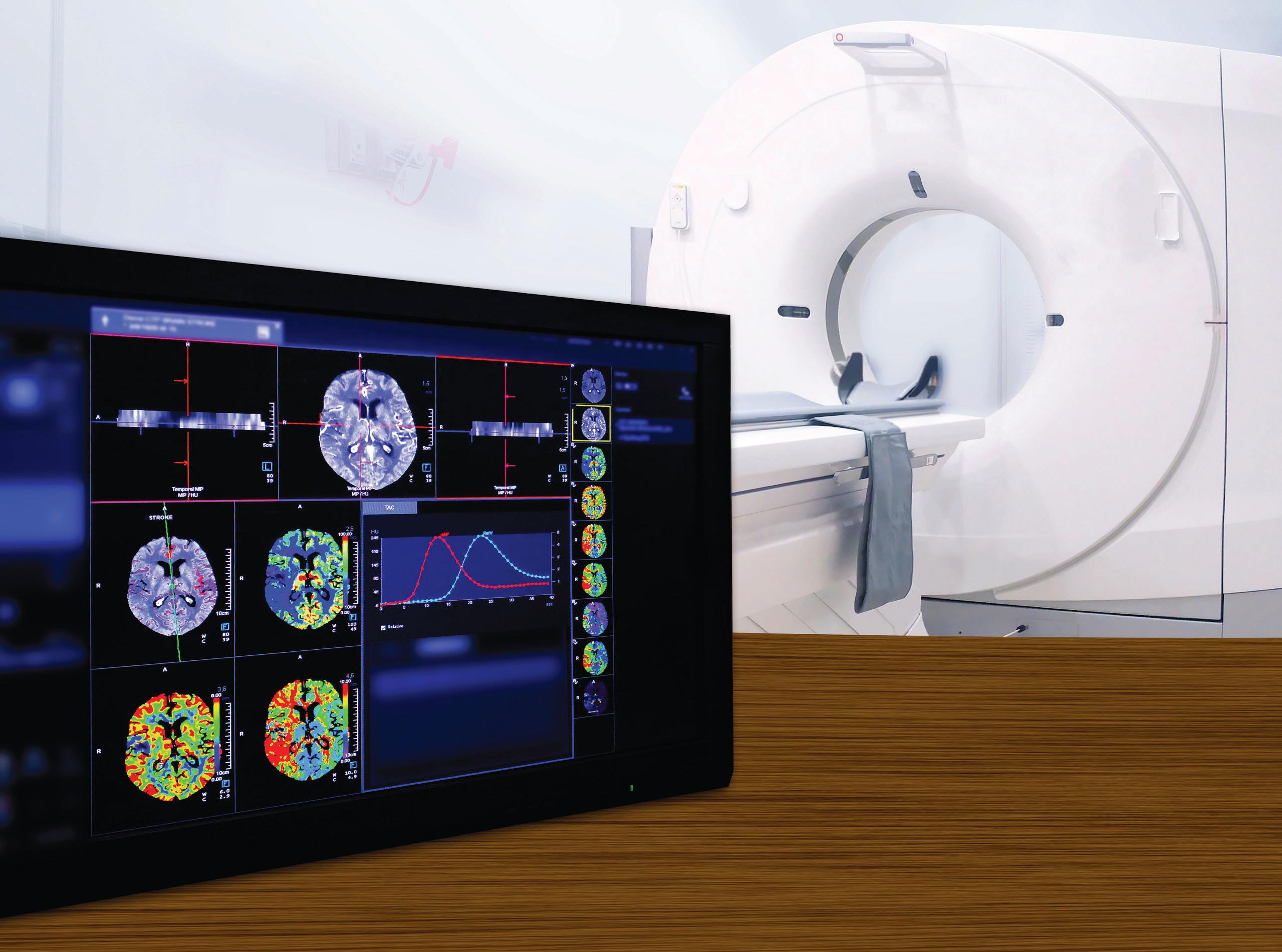
radio waves, a powerful magnet and a computer to create detailed images of the brain.
Other diagnostic tests include a cerebral angiography, which is performed by passing a catheter (a long, flexible tube) from the groin artery to inject a small amount of contrast dye into neck and brain arteries, and a cerebrospinal fluid analysis, which measures chemicals that indicate bleeding in the brain.
If medical experts such as those at McCullough-Hyde Memorial Hospital | TriHealth (MHMH) determine an aneurysm is present, whether it’s ruptured or in danger of bursting, they look at the risk factors and determine an appropriate course of action. If surgery is indicated, a team will gather to perform the procedure, usually within 12 to 24 hours.
For years, a procedure called clipping was the only way to fix an aneurysm. In this procedure, surgeons perform a craniotomy, which creates an opening in the skull, and place a small metal clip on the aneurysm to stop
harmful blood flow.
Clipping is still the best solution for some cases. Today, however, a mainstay of treatment is coiling, in which doctors can thread a catheter through a groin artery to place a coil on the aneurysm, so there is no need to open the skull.
Decisions about treatment are made on a case-by-case basis. The multidisciplinary team at MHMH includes a range of experts including
A cerebral (brain) aneurysm is a weak spot on a brain artery that balloons or bulges out and fills with blood. If it bursts, it spills blood into the surrounding tissue, an event that’s called a hemorrhage. Brain cells, deprived of oxygen, begin to die, and the patient may have a stroke.

neurologists, neurosurgeons, a neuropsychologist, a neuroradiology team and endovascular specialists. All provide input about what will be the most effective approach for a given patient. Nurse practitioners, neurology nurses and neurophysiology technologists round out the care team.
With expert care, many people recover from aneurysms. But preventing aneurysms and taking prompt action if one takes place can help forestall problems and improve outcomes.
• Uncontrolled blood pressure
• Smoking
• Family history of aneurysms
• Older age
• Head injury
• Substance abuse, particularly cocaine
• Heavy alcohol consumption
• Conditions present at birth, including polycystic kidney disease and cerebral arteriovenous malformation (an abnormal connection between arteries and vessels in the brain)
If you experience any of these symptoms, call 911:
• Sudden, severe headache
• Double vision
• Nausea and vomiting
• Stiff neck
• Sensitivity to light

• Seizures
• Loss of consciousness, even if brief
• Cardiac arrest
If you experience any of the following, consult your doctor right away:
• Drooping eyelid

• Dilated pupil in one eye




• Pain above and behind the eye
• Changes in vision or double vision
• Confusion
• Weakness and/or numbness on one side of the body









































































HOW TO BE SAFETY-SMART WHILE PLAYING OR WORKING OUTSIDE






















































IF YOU’RE like most people, you enjoy the time of year that allows you to get outside and be active. Unfortunately, spending time in or on the water, playing sports or even doing repairs around the house can put you at an increased risk of joint injury.
Specialized orthopedic care at McCullough-Hyde Memorial Hospital | TriHealth (MHMH) can help treat mishaps when they occur, but you can avoid some injuries altogether. Here are places and activities that often lead to orthopedic injuries—and tips for what you can do about them.
Diving— whether from the side of a swimming pool or a high spot at a local watering hole—is a major cause of spinal cord injuries, especially among men. In addition, high-speed water sports like jet skiing and waterskiing can put people at risk of bone fractures and joint injuries. It’s easy to get a false sense of security on water, which at first glance seems a forgiving surface, but falling in water at high speed can feel like hitting concrete.
• Prevention: Wear a life jacket and helmet during high-speed water sports and never jump or dive into unknown waters. If water is murky and you don’t know how deep it is, don’t dive.
• Treatment: Anyone with a water sports injury should be stabilized by a health professional, then taken to the Emergency Department to be checked for cervical spine and traumatic brain injuries. Healthcare providers
may also treat for shock, neck trauma and concussion.
The most common injuries from activities like tennis, golf and outdoor team sports are muscle sprains. Many “weekend warriors” experience issues such as tennis elbow or back problems related to their golf swings.
• Prevention: The best protections against strains, sprains and joint pain are starting slowly, stretching and warming up before playing, and then gradually building up your level of play to build muscle strength.
• Treatment: Most strains and sprains simply require rest, hot and cold compresses and possibly a few weeks of physical therapy. More severe injuries such as a ruptured hamstring or joint damage may require surgery.

Running is an excellent way to exercise, but it can sometimes lead to injury. Running in and of itself is not harmful to healthy joints, but it’s not recommended for damaged joints.
• Prevention: If you’re new to running, start slowly and use common sense. (For example, don’t run five miles on your first outing.) Proper footwear is important, so
good running shoes are a worthy investment.
• Treatment: Acute pain from sore muscles and joints will go away on its own with rest and over-the-counter pain medications. Long-term joint damage and arthritis may eventually require joint replacement surgery.
You may be most susceptible to injuries in your own home, especially if your chore list has you climbing ladders or firing up a power tool. For example, about half a million Americans are treated for ladderrelated injuries every year, according to the American Academy of Orthopaedic Surgeons. Summer and fall are prime time for ladder-related accidents, which often occur while fixing roofs or cleaning gutters. Also use caution with power tools such as lawn mowers and hedge trimmers.
• Prevention: If a task calls for climbing a ladder, make sure it rests on a firm, level surface. Check that the soles of your shoes are dry and not slippery. Have equipment such as leaf blowers serviced before you use them. Consider hiring a professional or asking a skilled friend to do more complicated home repairs if you’re not sure how to do them safely yourself. And take care that young people always have proper adult supervision around power tools.
• Treatment: People who fall off ladders most commonly break bones. Treatment usually requires surgery or a cast for up to three months, followed by physical therapy. Power tool injuries often require surgery to repair or reattach affected body parts.





































































