OXFORD



TRIHEALTH recognizes nurses annually for their noteworthy accomplishments. This year, Katie Maddock, RNC, a staff nurse on the Perinatal Unit at McCullough-Hyde Memorial Hospital | TriHealth (MHMH) for over 20 years, received a 2023 Directors’ Award for Excellence in Nursing at the Recognition Celebration held May 8 at the Cintas Center. Maddock was one of 19 nurses nominated for the prestigious award, one of only six winners and the first from MHMH.
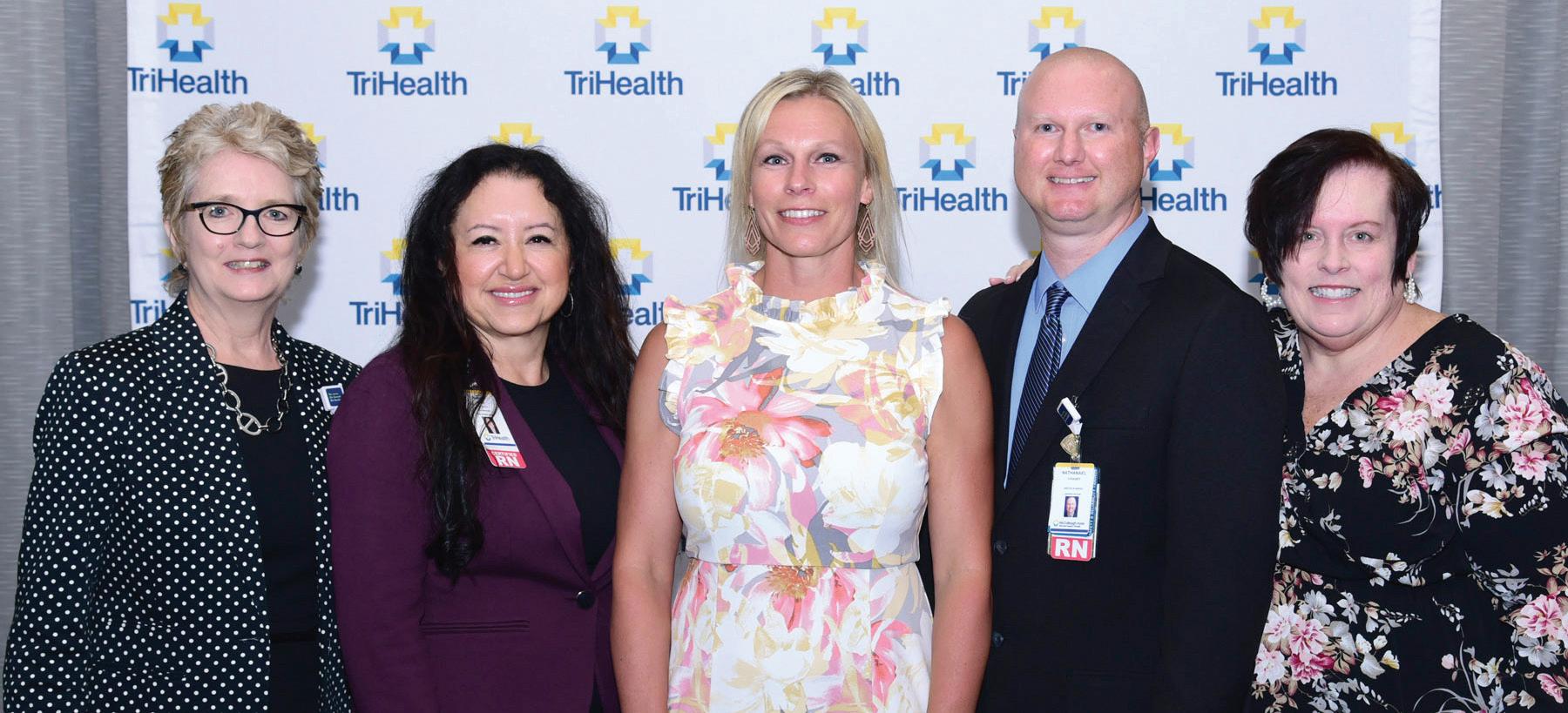
Maddock was nominated by her nurse manager Lyndsey Bengal, MSN, RN, C-EFM, and Director of Nursing Nate Chaney, MSOL, BSN, RN. “TriHealth has over 4,000 nurses among its five hospitals and many ambulatory sites,” says Chaney, who has nominated nurses since MHMH joined TriHealth in 2015. “It’s significant that Katie’s outstanding work at our community hospital is being recognized.” Nurses nominated for the award are leaders who demonstrate two or more components
of the Magnet Model, exemplifying clinical and professional excellence. (Created and managed by the American Nurses Credentialing Center, the Magnet program recognizes hospitals that offer patients the highest standard of nursing care. MHMH received Magnet designation in 2020—an achievement reached by only 8 percent of hospitals worldwide.)
“Katie has been a clinical bedside nurse on the McCullough-Hyde Perinatal Unit since 2002,” says Bengal. The unit includes antepartum, labor and delivery, postpartum and the newborn nursery. “Nurses on the unit look up to Katie,” Bengal says, noting that Maddock holds four specialty certifications, has achieved level III nursing status and is a neonatal resuscitation advanced provider.
An active member of the Association of Women’s Health, Obstetric and Neonatal Nurses, Maddock serves as a clinical coach, charge nurse and
mentor at MHMH. “She is responsible for quality audits, is an EPIC supervisor and a resource to nursing colleagues and obstetric and pediatric providers,” Bengal says.
When not working, Maddock volunteers at the Oxford Free Clinic, providing medical care to community residents. She is frequently praised in patient surveys for her skill, kindness and respectful manner.
“I worked with Katie for six years,” says Chaney. “She’s a rock— levelheaded and a great decision maker. She wears a lot of hats and consistently does a great job for us. When Katie’s working the night shift, you can sleep well knowing she’s on duty!”
If you’ve been discharged from McCullough-Hyde Memorial Hospital or one of its outpatient centers, chances are you received a survey about your experience by mail, email or text.
“We constantly review responses,” says Shane Quinn, manager of patient experience, whose team generates weekly survey reports for hospital managers. Constructive comments have generated physical improvements, such as better signage, and procedural changes, such as streamlined registration and patient communication.
Filling out a survey is also the best way to recognize staff members who go above and beyond in their work. “Positive comments come in every day, singling out employees across the board from nursing and imaging to environmental services,” says Amanda Reiboldt, manager of quality improvement.
All comments are taken seriously. “Our goal is to constantly improve and live up to TriHealth standards every day,” says Quinn.
APPLY FOR A NURSING JOB AT M c CULLOUGH-HYDE MEMORIAL HOSPITAL, SCAN THIS CODE.
THE 2023 MOCK FAMILY AWARD FOR OUTSTANDING PATIENT CARE.
an Excellence in Nursing Award, and the McCullough-Hyde Foundation was able to make that happen.”
Tyler Wash, executive director of the foundation, and Mary Bennett, former chief development officer, helped the Mock family launch the fund and disseminate award information. They enlisted a volunteer committee to select nominees who were assessed on patient-care experience, care delivery, clinical skills, acts of kindness and safety.
WHEN JILL MOCK , CPNP, moved to Oxford in 1986, she found a job as an obstetrical nurse at McCulloughHyde Memorial Hospital (MHMH). “I wanted to work in the community where I lived and raised my children,” she says. “It was clear to me that McCullough-Hyde was a special place.” Mock became a pediatric nurse practitioner in 1990 and joined Oxford Pediatrics and Adolescents. “I continued to see newborns in the hospital nursery,” she says, “and feel blessed that I was able to stay connected with McCullough-Hyde.”
As longtime donors to Miami University where Mock’s husband,
Ray, completed his degree and worked, the couple decided it was Mock’s turn to choose a contribution-worthy cause. “Something near and dear to my heart,” says Mock, who instantly thought of MHMH. “I wanted to give back—to celebrate nurses who demonstrate compassionate care and outstanding nursing. I wanted them to feel recognized and valued. It made sense to establish
Angela Downard, RN, a staff nurse in the emergency department, was selected and honored at the hospital’s Excellence in Nursing Reception in May alongside nominees Emily Baldwin, Kathy Briar, Maggie Dingledine, Krista Jones, Sharon Klein, Katie Maddock, Lindsay Shell and Mary Wagner. “Angie provides outstanding clinical care to patients, always ensuring they are comfortable and emotionally supported,” says Amanda Stang, medical laboratory scientist. “She is the epitome of a compassionate nurse who loves what she does.”
Mock says she’s pleased future nurses will benefit from the Mock Family Award thanks to her family’s endowment. “They are the heart and soul of McCullough-Hyde,” she says of her nursing colleagues.

closely with community health organizations and Miami University Health to keep our community safe,” she says.
Ongoing continuing education at MHMH allows emergency nurses to stay current with evidencebased practices. Clinical Nurse Specialist Jeannie Burnie, MS, APRN, AGCNS-BC, CEN, FAEN, FCNS, senior education manager of Emergency Services, championed training for TriHealth’s six emergency departments, allowing MHMH ED nurses to take advantage of a state-of-theart simulation lab and obtain trauma nursing and neonatal resuscitation certifications. “Our ED nurses played an important role in the Acute Stroke Ready Center accreditation awarded last year,” says Rolfe.
THE EMERGENCY DEPARTMENT (ED) at McCulloughHyde Memorial Hospital | TriHealth (MHMH) earned a 2023 Lantern Award from the Emergency Nurses Association (ENA) for exceptional performance. It is one of only 53 hospitals nationwide to receive this three-year award. The stringent application process required detailed data and specific examples of how MHMH provides excellent emergency care and continuously improves its services.
“The Lantern Award is recognition given to emergency departments that demonstrate exceptional practice and commitment to quality care for patients, particularly in emergency nursing,” says Samantha Anderson, RN. “It’s a way to acknowledge and celebrate the efforts of emergency nurses and ED departments in providing excellent patient care during critical situations.”
“McCullough-Hyde’s ED treated the very first COVID-19 patient in Ohio,” says Jennifer Rolfe, MSN, RN, CEN, clinical nurse educator II of the MHMH and Good Samaritan Western Ridge emergency departments. “ED nursing staff pivoted throughout the pandemic, adapting to challenges like personal protective equipment shortages, hospital overflow and COVID-19 testing surges. They worked
Receiving the Lantern Award aligns MHMH with TriHealth emergency departments and validates the quality of care it provides, as well as its uniqueness. “As a rural ED, we look closely at transfer times because critically ill patients are often transferred to a higher level of care, and refining that process is critical to patient safety,” says Burnie. “Our location on a college campus also impacts the number and type of patients we treat. The Lantern Award shows that our emergency nurses are adaptable and able to handle any situation.”
The ability to assess, triage and prioritize patients is vital to ensuring that those in need receive timely and appropriate care. “In addition,” says Anderson, “our McCullough-Hyde emergency nurses offer emotional support to patients and families during stressful moments, making their role not only medically important but also essential for overall patient well-being.”
Representatives from MHMH’s emergency nursing team will accept the Lantern Award at the ENA National Conference in San Diego. They’ll bring back a glass lantern and a banner to be displayed at the ED entrance. “We are so proud of our amazing ED nurses,” says Rolfe. “When you or your family, friends or neighbors experience an emergency, our team will be here to help.”

Nathan Simmons, PharmD, RPh (left), and emergency medicine physician Aaron Bender, MD, collaborated to diagnose and treat a patient with a rare, potentially life-threatening condition. After the event, staff created a poster to heighten awareness of
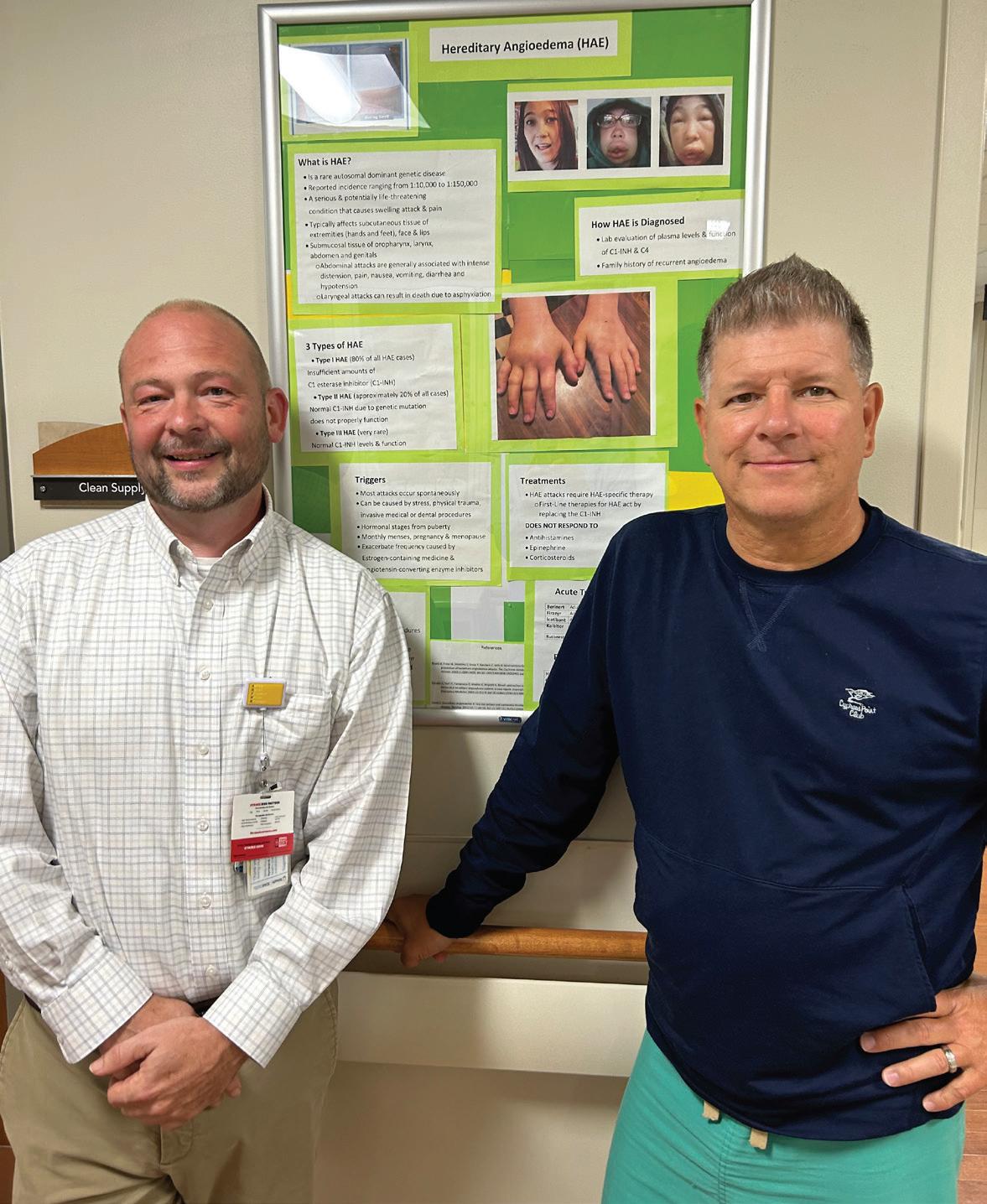
says Simmons, “because he wasn’t on medication that can cause swelling, such as an ACE inhibitor for hypertension.” The patient had no rash or hives, which might indicate an allergic reaction.
After reviewing the patient’s test results, the MHMH colleagues determined he likely has a rare type of angioedema known as hereditary angioedema (HAE), which affects one in 50,000 people in the United States. “Most people with HAE have a genetic defect that causes a deficiency in the blood protein called C1 inhibitor,” explains Dr. Bender.
Treatment for HAE attacks is a medication called Berinart, a plasma-derived C1 esterase inhibitor. “The drug wasn’t in stock at the McCulloughHyde pharmacy,” says Simmons of the rarely used medicine. After calculating the correct dosage for Dr. Bender’s patient, Simmons tracked the drug down at another TriHealth hospital pharmacy. “That’s the beauty of being part of a collegial system like TriHealth,” he says. “We have access to many resources and great communication and trust among colleagues.”
Realizing time was of the essence, Simmons picked up the medication at Bethesda-North Hospital and delivered it to Dr. Bender at the MHMH emergency department. “A courier service would’ve taken hours, and we didn’t have that kind of time,” says Simmons of his road trip. Dr. Bender administered the lifesaving drug, and the patient’s symptoms subsided. Additional tests to definitively establish an HAE diagnosis were ordered, and Dr. Bender referred the patient to a hematologist for follow-up.
NATHAN SIMMONS, PharmD, RPh, director of pharmacy at McCullough-Hyde Memorial Hospital | TriHealth (MHMH), was enjoying a Saturday morning cup of coffee at home when his cell phone rang. It was a call from emergency medicine physician Aaron Bender, MD.
“I called Nathan because we had a patient in the ED with typical signs of angioedema—swelling of the lips and tongue and upper airway,” says Dr. Bender. “If the tongue gets too big, it can restrict breathing and become lifethreatening fast.”
He and Simmons discussed the patient’s presentation and medical history. “We ruled out drug-induced angioedema,”
That hectic summer morning triggered positive changes at MHMH. Jennifer Rolfe, MSN, RN, CEN, clinical nurse educator, created a descriptive poster heightening awareness of HAE in the emergency department, and the pharmacy now routinely stocks Berinart. Dr. Bender says Simmons’s off-hours consult and round-trip drive are indicative of the MHMH culture. “The staff here is so dedicated,” he says, “that they will take any steps necessary to care for our patients.”
AFTER DIAGNOSING A PATIENT WITH A RARE, POTENTIALLY LIFETHREATENING CONDITION, MHMH STAFF PARTNERED WITH TRIHEALTH COLLEAGUES TO QUICKLY PROVIDE THE RIGHT TREATMENT.

YOU HEAR IT on the news: Young athletes get hurt—a high school quarterback collapses or a middle school shortstop suffers a concussion. It’s enough to make parents wonder how kids who participate in sports can stay safe. These six tips can help protect athletes and keep them on the field.
Until about third grade, an informal approach that stresses basic skills is more appropriate in kids’ team sports than an all-out emphasis on victory, because young children are still developing motor skills. Younger children should also be given a chance to explore a variety of sports rather than concentrating heavily on one, because they’re especially vulnerable to injuries caused by overuse of one joint or limb.
2 VISIT THE
FIRST.
Students should get a medical evaluation before participating in middle school, high school or college sports— or even younger athletes’ recreational or travel sports. Start by searching online for “preparticipation physical evaluation forms.” Numerous examples can help guide parents and doctors through relevant medical history and physical exam findings. For example, certain conditions require special considerations. These include respiratory ailments; preexisting head, bone and soft tissue injuries; or a family history of early cardiac illness. Ask your physician what best suits your child’s needs given the intended sport and any school or state requirements.
3 CONSIDER A BASELINE NEUROCOGNITIVE TEST.
This is especially important if your child is at least 13 and will play a rough sport where head injuries are a significant risk. Tests can measure brain functions

that may be affected by a concussion such as attention, memory, processing speed and reaction time. Having a baseline neurocognitive test provides comparison data that can later help physicians evaluate a head injury and assess when it’s safe for an athlete to play again. Age-related norms can help as well, but children can vary, so comparing with a child’s own baseline is ideal. Even without serious effects such as skull fracture or intracranial bleeding, concussions can warrant staying on the sidelines for extended periods to avoid risk of further brain injury.
4 CHECK OUT COACHES. Attend several practices to get a sense of a coach’s capabilities and training philosophy. Many coaches are well-intended parents who have undergone safety training. Others may use potentially dangerous strategies such as having kids run long distances in hot weather without enough water breaks.
5 INSIST ON PROPER EQUIPMENT.
Check that your young athlete will have all the necessary gear such as shoulder pads and leg and mouth guards. Make sure that protective equipment is in good condition and used properly.
6 ENFORCE A SOUND DIET.
It’s important for kids to follow a balanced diet that limits junk food. Before a big game, they should consume mostly carbohydrates and a moderate amount of protein. Go easy on fatty foods that can slow digestion. Avoid foods your child’s body is unfamiliar with and may not tolerate well: Even otherwise healthy foods such as high-fiber items and vegetables like cauliflower and broccoli can cause gas or cramping that could hinder performance in a competition.
TO SEE A PEDIATRICIAN, CALL OXFORD PEDIATRICS AT 513.523.2156 .
WHEN WAS THE LAST TIME you saw— or even had—a primary care physician? Research suggests the number of Americans who regularly see one is dropping. But going to a primary care doctor has important health benefits.
A primary care physician typically specializes in a discipline such as family
or internal medicine and provides a first point of entry into the healthcare system. It’s important to have a go-to health professional in your corner who can assess and treat a broad variety of conditions.
In fact, regularly seeing a primary care doctor can improve your health for reasons like these:
REGULAR VISITS TO A BIG-PICTURE DOCTOR CAN HELP KEEP YOU HEALTHIER.
1 YOU’LL
IF YOU GET ILL. After just one meeting, your primary care physician will know at least some of your medical history and possibly baseline results from a number of routine screening tests. When something goes wrong, your doctor will know what “normal” looks like for you, which will help in addressing both your acute and chronic medical problems more effectively.
People who use prescription drugs often take more than one, sometimes prescribed by different doctors. Many take vitamins and supplements as well. A primary care physician can monitor and track all your medications, helping to protect you from drug interactions. Your primary care doctor can also keep records of any changes in dosages that might cause unwanted side effects, and speak with your other doctors to help fine-tune your regimen.
Seeking out a primary care physician regularly even when
you’re feeling fine can help prevent you from becoming seriously ill down the road. From your health profile, your doctor will be able to recommend tests that can assess your chances of developing heart disease, diabetes, cancer and other serious-but-common problems. If your medical history and tests indicate that you’re prone to specific illnesses, your primary care physician can suggest healthy lifestyle changes and regular screenings to reduce your risks.
4 REMOTE CONSULTS MAY BE READILY AVAILABLE. Baseline health information that your primary care physician collects may allow your doctor to be comfortable treating certain problems over the phone, knowing you can always schedule a follow-up if your symptoms don’t improve. Without a primary care doctor, you’re likelier to need a trip to a medical office.
5 YOU’LL HAVE AN
TIME FINDING SPECIALISTS. When you need the care of an expert in a certain specialty, your primary care physician can help you find the right person—not only someone with the proper qualifications, but a provider who will mesh well with your personality and care preferences. If you prefer aggressive treatments, for instance, you can communicate this to
your primary care physician, who can recommend specialists who align with your approach.
Wondering if you should head to the emergency room? If you have a relationship with a primary care physician, you can touch base with the practice office and get guidance from your doctor, potentially sparing you a trip. If you do need to seek emergency care, your doctor may be able to call ahead and provide pertinent medical details that could shorten your wait time when appropriate.
People with primary care physicians tend to receive significantly more high-value healthcare such as flu shots and cancer screenings. They often have better patient experiences and overall access to healthcare as well.
8 YOU MIGHT LIVE LONGER. Research suggests that people who live in areas where primary care physicians are readily available on average have longer life spans. But benefiting from their services depends on actually going to your primary care doctor.
1. Colorectal cancer can often be prevented.
2. Colorectal cancer is only a problem for older people.
3. If I have no symptoms, I don’t need to get screened.









1. TRUE. Regular colorectal cancer screening can find abnormal colon growths called polyps, and they can be removed before they develop into cancer. You can also lower your risk with regular physical activity, by maintaining a healthy weight and by eating a nutritious diet with minimal sugar and processed foods.
2. FALSE. While the disease most commonly appears after age 50, recent research finds that the rate of colon and rectal cancers has been steadily increasing in younger people. If you are at high risk based on family history or other factors, you may need to start screening earlier. Talk with your doctor.
4. Colonoscopy is the only test used to screen for colorectal cancer in people who have no symptoms of it.

5. Early detection leads to a high survival rate. n T n F
















3. FALSE. Many people with early-stage colorectal cancer don’t have symptoms. If you do have symptoms, check with your doctor. The cause could be any number of things besides cancer, but you want to find out what it is so it can be treated. Warning signs include:
• A change in bowel habits that lasts for more than a few days
• A feeling that you need to have a bowel movement that’s not relieved by defecating



• Rectal bleeding, dark stools or blood in the stool









































• Cramping or belly pain
• Weakness and extreme tiredness that doesn’t get better with rest
• Unintended weight loss
4. FALSE. Tests can be divided into two groups: stool tests, which check the stool (feces) for signs of cancer, and visual (structural) exams, which look at the structure inside the colon and rectum. Besides colonoscopy, visual exams include CT colonography (virtual colonoscopy) and flexible sigmoidoscopy.
5. TRUE. American Cancer Society statistics show that the five-year survival rate for people with localized colon or rectal cancer is about 90 percent. In addition, treatments and therapies continue to improve over time.



























Colorectal cancer begins in the colon or rectum, both of which are part of the large intestine. In a colonoscopy procedure, doctors use a small, flexible tube with a light and a small video camera on the end to look inside the colon and rectum. The procedure can detect polyps—small clumps of cells on the lining of the colon—that may later turn into cancer. Any polyps that are found can be removed during the same procedure.

TO APPRECIATE a food, it’s helpful to imagine if it didn’t exist, so let’s conjure up for a moment a world without pears. Certain Cézanne still lifes would show only an empty plate. We’d all miss out on nutrients, a moistly crunchy texture and a mildly sweet taste. And that wellknown 12-day holiday song would have to end each verse with “and a partridge in an undisclosed location.”
But never fear—the good old pear isn’t going anywhere. (Nor is its homonymhappy name: Pluck two and you’ve got a pair, peel the skin and you’ve begun to pare.) Known for broad bottoms and narrow tops (though some are rounder), the fibrous-centered genus Pyrus grows on trees, but doesn’t ripen well there. (It gets gritty.) Its skin is usually greenish to gold, though some varieties are pinkish— indeed, there are roughly 3,000 known kinds, including Bartlett, Red Bartlett, Red Anjou, Green Anjou, Bosc, Comice, Concorde and Starkrimson.
The cultivation of pears is believed to date back to 5,000 B.C. in China. In those days, so the story goes, a diplomat named Feng Li got so busy tending his pears that he neglected his diplomacy. Millennia later, Homer in the “Odyssey” called pears “the gift of the gods.” You just can’t buy PR like that.
Pears’ benefits to human health are legion. Tipping the calorie scale at a svelte 86, one small fruit (148 grams) can furnish 18 percent of your daily required fiber, 10 percent of your vitamin C, 8 percent of your vitamin K and 6 percent of your copper. (Yes, you need some
copper.) These nutrients’ antioxidant properties can help protect cells from the effects of free radicals, which are molecules that have been associated with the development of cancer.
Like apples but even more so, pears provide the soluble fiber known as pectin, which helps to regulate the bacteria in your gut.
Pears might also help to ward off cardiovascular disease, for which high blood pressure is a known risk. In a 2019 study, people with metabolic syndrome (a cluster of conditions that together raise the risk of heart disease, stroke and diabetes) who ate a daily pair of pears for 12 weeks experienced small decreases in systolic blood pressure and pulse pressure.

Containing 84 percent water, pears have a natural laxative effect that can help keep you regular. But you never want to pig out on pears all afternoon, lest gas and bloating result. “Medical
News Today” warns that “people with IBS [irritable bowel syndrome] should speak with a dietitian before including pears in the diet.”
Purchase pears at a grocery or fruit stand, and store them at room temperature until they ripen. (They’re subject to pear-peer pressure—place one in a fruit bowl next to a banana, and that yellow influencer gives off ethylene, prompting the pear to ripen.) Keep ripe pears in the fridge, where they’ll be good for two to three days. You can freeze cooked pears, but not fresh ones, which tend to come apart.
How to tell if a pear is ripe? Apply your thumb gently to the upper portion near the stem; if you feel a slight give, chances are the fruit is ripe and ready.
Picking your pear must be paired with your purpose: Plan to cook with the fruit, perhaps to bake, poach or grill? Think “ABC,” for the Anjous, Bosc and Concorde, firm varieties that hold their shape well.
Prefer to chomp on the fruit fresh? Then a juicy Cornice, Starkrimson or Bartlett pear is your best bet.
Pears are often canned (usually Bartlett) or dried, and are sometimes used in jams and jellies. Interested in other possibilities for your culinary pear-adise? Look online for recipes, including cinnamon baked pears, pears with pork chops and onions, pear streusel cakes, pears bordelaise (with wine), poached pears, pear crumbles (with flour, sugar and oats), pear and blue cheese crostini, pear oatmeal muffins and pear upside-down cake!
