
9 minute read
Chapter 8: Invasive Blood Gas Analysis and Monitoring Test Bank
Multiple Choice
1. A respiratory therapist has been ordered to obtain a blood gas sample from a nonintubated premature baby. After selecting the best site to obtain the sample, what should the RT suggest to ameliorate the pain associated with the procedure?
a. Administer a small dose of fentanyl b. Inject lidocaine at the injection site c. Give a pacifier dipped in 24% sucrose d. Administer a lidocaine drip
ANS: C
For infants more than 4 months of age and for children, anesthetic cream or a lidocaine injection may be used to control the pain felt during a blood gas procedure. For nonintubated infants and premature newborns, a pacifier dipped in 24% sucrose is effective in helping to ameliorate the effects of pain.
REF: p. 115 a. Radial artery b. Axillary artery c. Ulnar artery d. Popliteal artery
2. Which of the following arteries is considered the optimal puncture site for obtaining arterial blood samples from neonatal and pediatric patients?
ANS: A
The preferred site in both neonatal and pediatric populations is the radial artery. The radial artery provides good access as well as collateral circulation to the hand by the ulnar artery. No nerves or veins are directly adjacent to the radial artery, and the patient’s wrist is easier to manipulate than other body parts. The bone and firm ligaments of the wrist make it easy to palpate, stabilize, and compress the radial artery.
REF: pp. 115-116
3. If a blood gas sample is not obtained from an arterial stick in a premature baby without central access, which of the following sites should be considered because this blood vessel is larger than the radial artery at this age? a. Dorsalis pedis b. Temporal c. Posterior tibial d. Femoral
ANS: B
The dorsalis pedis or posterior tibial artery is considered if the radial artery shows signs of poor collateral circulation. In addition, the temporal artery provides an alternative site for the premature or newborn infant. Access is generally good because two branches are close to the scalp. In most premature and neonatal patients, the temporal artery branches are larger than the radial artery.
REF: p. 116
4. In addition to the dorsalis pedis, which of the following arteries is involved when the modified Allen’s test is performed using a foot as the potential arterial puncture site? a. Axillary artery b. Femoral artery c. Posterior tibial artery d. Dorsalis pedis
ANS: C
The modified Allen’s test can also be used to verify collateral circulation when using one of the arteries of the foot as a puncture site, by elevating the foot and compressing the dorsalis pedis and posterior tibial arteries. Collateral circulation is confirmed by releasing pressure from the artery that will not be punctured and assessing the nail beds and sole of the foot for return of blood flow.
REF: p. 116 b. Inform the therapist to turn the bevel downward. c. Tell the therapist to penetrate the infant’s skin at about a 60-degree angle. d. Advise the therapist to insert the needle in the same direction as the blood flows.
5. The neonatal intensive care unit (NICU) respiratory therapy supervisor is observing a therapist obtain an arterial blood sample from an infant’s radial artery and notices that the therapist has the bevel of the needle pointed upward, entering the patient’s skin at a 45-degree angle and in a direction against the arterial flow. What should the supervisor do at this time? a. Continue to observe the procedure.
ANS: A
Insert the needle of the syringe or butterfly catheter into the artery at a 35- to 45-degree angle with the bevel up and advance it gently. Enter the artery from the direction opposite, or against, the blood flow. A flash in the hub of the syringe or butterfly catheter verifies that the needle penetrated the artery and is located in the lumen. In the small pediatric patient it is quite easy to pass through the artery with the needle. If a good pulse is palpated and no blood return occurs after the needle is inserted, pull the needle back incrementally and continue to watch for a flash of blood. If resistance is met when inserting the needle, slowly withdraw it immediately and change direction because it has most likely touched the bone.
REF: p. 117 a. Have the patient maintain the arm in an elevated position for a couple of hours after the radial puncture. b. Have the patient shake the arm periodically throughout the day. c. Alternate arms used for arterial puncture and use other sites as well. d. Apply a bandage to the puncture site.
6. In addition to applying direct pressure to the puncture site immediately after the arterial puncture procedure, what can the therapist do to minimize the risk of hematoma formation in a patient who requires frequent radial arterial punctures?
ANS: C
Scarring, laceration of the artery, and hematoma formation are more likely to occur with repeated puncture of an artery. Alternating puncture sites decreases this risk.
REF: p. 118
7. Which of the following factors would adversely affect the correlation between arterial puncture measurements and those from a capillary sample? a. Hypotension b. Hyperventilation c. Hypoxemia d. Hyperthermia
ANS: A
The accuracy of capillary blood gas value measurements is severely compromised by the presence of hypotension, hypothermia, hypovolemia, and lack of perfusion.
REF: p. 118 a. Perform the heel stick as ordered. b. Instead of using the newborn’s heel, the therapist should use a finger as the site. c. Inform the physician that this procedure is inappropriate at this time. d. Explain to the doctor that an arterial puncture procedure is appropriate.
8. A 12-hour-old infant is experiencing respiratory distress, and the neonatologist orders a heel stick to assess the infant’s oxygenation status. What action should the therapist take at this time?
ANS: C
A capillary puncture is contraindicated in neonates less than 24 hours old. A newborn has a low systemic output, and vasoconstriction tends to be maximal during this stage secondary to a decrease in environmental temperature and an increase in circulating catecholamines. Capillary blood sampling is not recommended in a patient with decreased peripheral blood flow, especially in the case of hypotension.
REF: p. 120
9. With an umbilical artery catheter (UAC) in the “low position,” which of the following blood vessels should be avoided? a. Celiac artery b. Superior mesenteric artery c. Renal artery d. Descending aorta
ANS: C
The low position is usually at the third to fourth lumbar (L3 to L4) space, between the renal artery and aortic intersection and above the takeoff of the inferior mesenteric artery. The UAC is placed to avoid the large tributaries supplied by these vessels in an effort to minimize trauma and hemodynamic disturbances of vital organs.
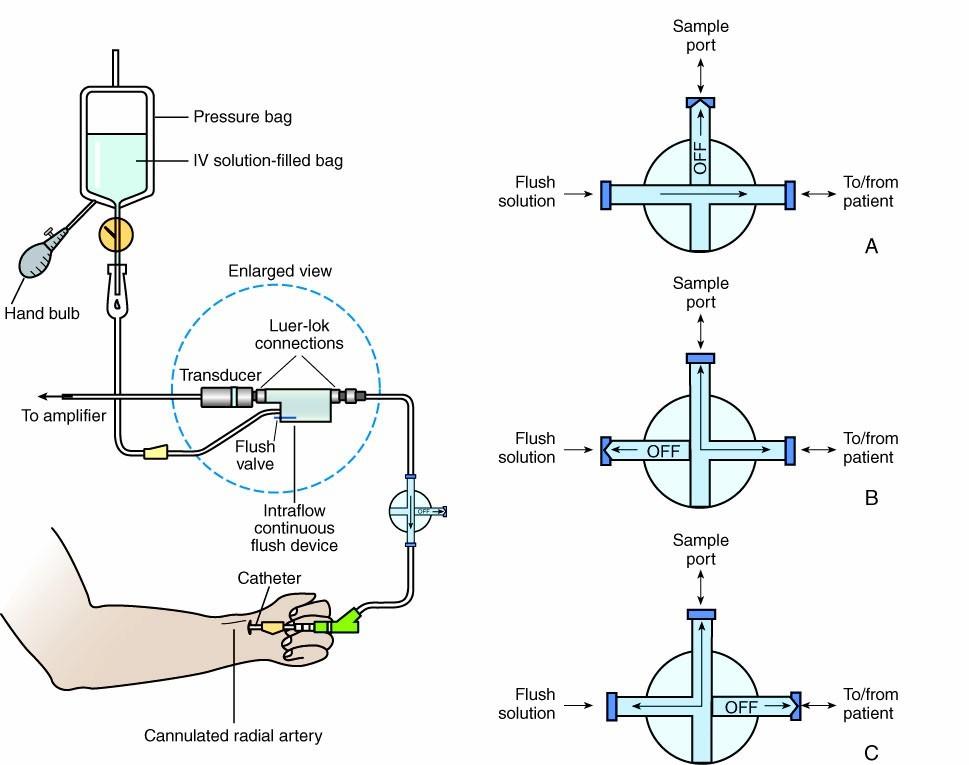
REF: p. 120 a. The therapist is aspirating blood diluted with infusion fluid. b. The therapist is withdrawing blood from the arterial line. c. The therapist is keeping the stopcock in its normal operational position. d. The therapist is infusing fluid back into the system after having removed a blood sample.
10. On the basis of the position of the three-way stopcock shown here, identify which of the following activities related to arterial line blood sampling is occurring.
ANS: C
REF: p. 122 a. 30 mL b. 60 mL c. 90 mL d. 120 mL ANS: C
11. A 3-kg neonate has lost 30% of his circulating blood volume. Approximately how much fluid should be infused to compensate for this loss?
The circulating blood volume in neonates and children is approximately 85 to 90 mL/kg and 70 to 75 ml/kg, respectively. Because the circulating blood volume in neonates and children is small, recording and limiting the volume of blood withdrawn from these patients and/or infused is important.
REF: p. 122 a. 25 mm Hg b. 58 mm Hg c. 83 mm Hg d. 175 mm Hg
12. A patient has a systolic blood pressure of 100 mm Hg and a diastolic pressure of 75 mm Hg. What is this patient’s mean arterial pressure?
ANS: C
Monitoring arterial pressure waveforms helps to determine the patency of an arterial line and the quality of the pulse pressure and to calculate the mean arterial pressure (MAP). The arterial line monitor calculates MAP internally. However, the formula to obtain an indirect measurement of MAP with a sphygmomanometer is as follows: MAP = [(2 X diastolic) = systolic]/3
REF: p. 123
13. Which of the following factors influence the central venous pressure (CVP) measurement?
I. Bicuspid valve function
II. Right ventricular pressure
III. Intravascular volumeIV. Systemic venous return a. I and III only b. II and III only c. II and IV only d. II, III, and IV only
ANS: D
The placement of a central venous catheter provides for the measurement of the right atrial pressure, which represents the filling pressure of the right atrium. Systemic venous return, intravascular volume, tricuspid valve performance, myocardial function, and right ventricular pressure all affect the right atrial pressure.
REF: p. 124 a. Elevate it above normal b. Cause it to fall below normal c. Produce fluctuations in the CVP value d. Have no effect in the CVP value
14. How would tricuspid stenosis be expected to influence a patient’s CVP value?
ANS: A
Increased CVP values may result from:
• Hypervolemia, as with sudden fluid shifts or volume overload
• Interference with the ability of the right ventricle to pump blood, such as in tricuspid valve regurgitation or tricuspid stenosis, right ventricular failure or infarction, increased pulmonary vascular resistance, or cardiac tamponade
• Increased systemic vasoconstriction
• Left ventricular failure
REF: p. 124 a. Right atrium b. Right ventricle c. Pulmonary artery d. Wedged position
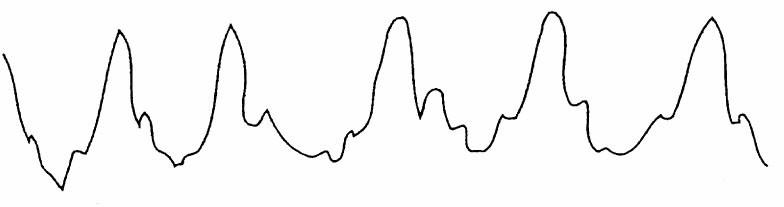
15. On the basis of the following waveform, in which of the following anatomic locations is the distal tip of the pulmonary artery catheter located?
ANS: D
The pressure waveform presented represents the characteristic tracing obtained when the balloon on the pulmonary artery catheter is inflated and the catheter is allowed to float into the wedged position.
REF: p. 125 a. Right atrium b. Right ventricle c. Pulmonary artery d. Wedged position
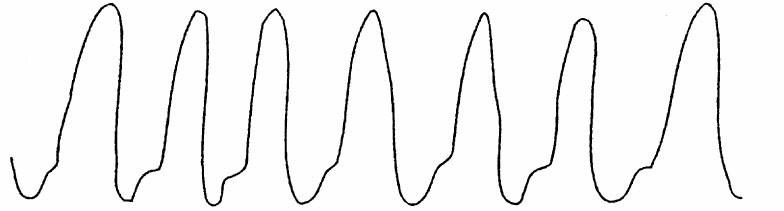
16. On the basis of the following waveform, in which of the following anatomic locations is the distal tip of the pulmonary artery catheter located?
ANS: C
The pressure waveform presented represents the characteristic tracing obtained when the distal tip of the pulmonary artery catheter is residing in the pulmonary artery.
REF: pp. 125-126 a. Right atrium b. Right ventricle c. Pulmonary artery d. Wedged position
17. On the basis of the following waveform, in which of the following anatomic locations is the distal tip of the pulmonary artery catheter located?
ANS: B
The pressure waveform presented illustrates the characteristic tracing obtained when the pulmonary artery catheter is located in the right ventricle. Notice the high right ventricular systolic pressure (30 mm Hg) and the low right ventricular diastolic pressure (below 5 mm Hg).
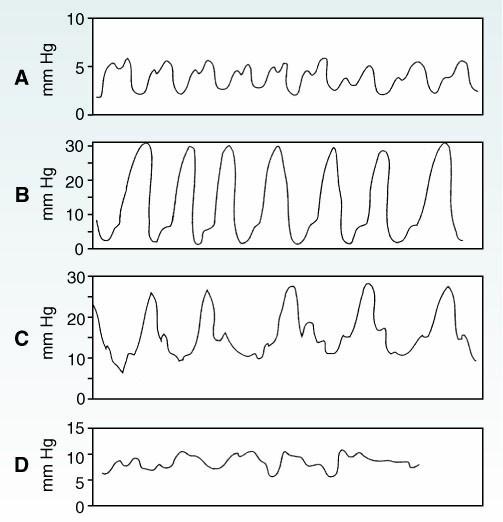
REF: p. 126 a. Right atrium b. Right ventricle c. Pulmonary artery d. Wedged position
18. Which of the following pulmonary artery catheter waveforms represents the catheter’s normal location?
ANS: C
This pressure waveform reflects the presence of the distal tip of the pulmonary artery catheter in the pulmonary artery, where this catheter should normally reside. After the pulmonary artery catheter has been placed in the proper position, the catheter’s monitor should show the catheter positioned to produce a pulmonary artery pressure waveform, except for times when pulmonary capillary wedge pressure readings are obtained.
REF: pp. 125-126
19. Which of the following is one of the most common arrhythmias observed as a complication from the insertion of a pulmonary artery catheter? a. Premature ventricular contraction b. S3 gallop c. Atrial fibrillation d. Paroxysmal atrial contraction
ANS: A
At insertion, complications include bleeding, pneumothorax, tricuspid or pulmonic valve damage, right atrium or right ventricle perforation, and arrhythmias resulting from the catheter traversing the right ventricle. The most frequently observed arrhythmias are premature ventricular contractions and ventricular tachycardia.
REF: p. 126
20. Calculate a patient’s total arterial oxygen content given the following data:
•Arterial oxygen tension (PaO2), 100 mm Hg
•Arterial carbon dioxide tension (PacO2), 45 mm Hg
•Arterial oxygen saturation (SaO2), 97.5%
•Hemoglobin concentration ([Hb]), 15 g/dL
•Cardiac output, 4.5 L/minute
•Stroke volume, 55 mL/beat a. 19.9 vol% b. 18.7 vol% c. 16.6 vol% d. 14.9 vol%
ANS: A
The formula for calculating the total arterial oxygen content (CaO2) is as follows: O2 delivery = O2 content = (Hb X 1.34 X SaO2) + (PaO2 X 0.003)
REF: pp. 129-130 a. Anemia b. Inhalation of nitric oxide (NO) c. Use of dobutamine d. High fraction of inspired oxygen
21. Which of the following conditions can cause methemoglobinemia?
ANS: B
Methemoglobin forms when hemoglobin is oxidized to the ferric state. It causes the oxyhemoglobin dissociation curve to shift to the left, resulting in a decrease in hemoglobin's ability to combine with oxygen. Nitrate-containing molecules in medications and therapeutic gases may cause methemoglobinemia.
REF: p. 131




