
30 minute read
Chapter 24: Congenital Cardiac Defects Test Bank
Multiple Choice
1. Which of the following vessels return blood to the right ventricle?
I. Pulmonary vein
II. Inferior vena cava
III. Superior vena cavaIV. Coronary sinus b. II and III only c. I, II, and III only d. II, III, and IV only
ANS: D a. I and IV only
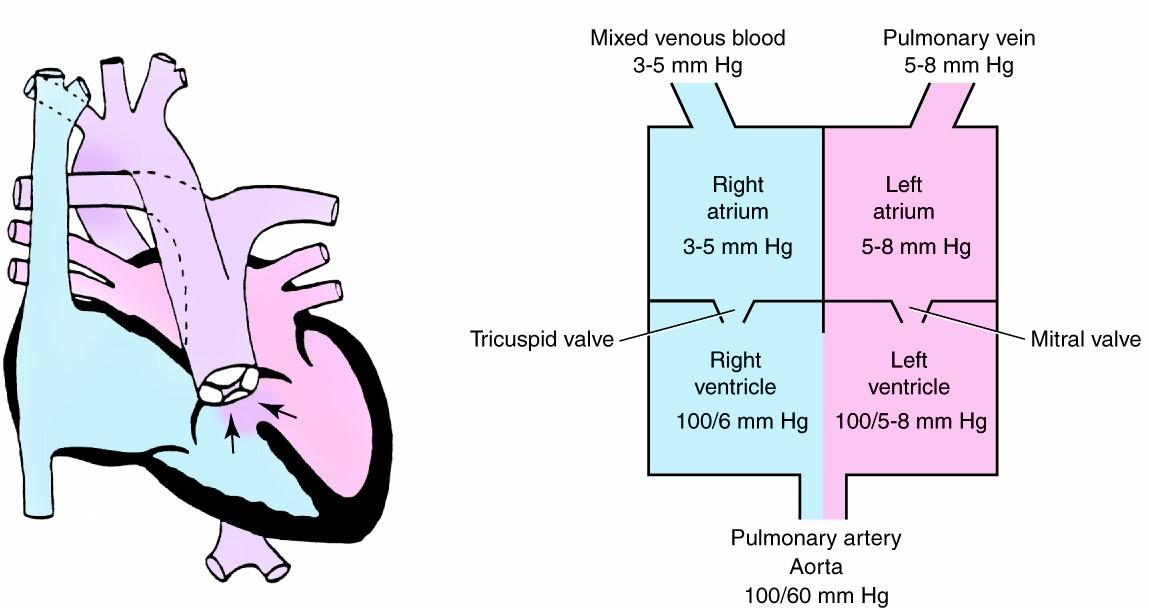
To understand the normal anatomy of the heart, one can trace the path of blood as it travels through the heart. This begins with deoxygenated venous blood that enters the right atrium (RA) from one of three sources. Venous blood from organs superior to the heart drains to the RA by way of the superior vena cava (SVC). Venous blood from organs inferior to the heart enters the RA via the inferior vena cava (IVC). Finally, venous blood from the heart itself drains into the RA by way of the coronary sinus.
REF: p. 471 a. Increased arterial partial pressure of oxygen (PaO2) b. Decreased arterial partial pressure of carbon dioxide (PaCO2) c. Lung inflation d. Circulating indomethacin
2. At birth, what factor causes dilation of the pulmonary vascular bed and a decrease in the pulmonary vascular resistance?
ANS: A
With inflation of the lungs and the beginning of their participation in gas exchange, PaO2 increases and PaCO2 decreases, both of which contribute to dilation of the pulmonary vasculature and a resultant reduction in pulmonary vascular resistance (PVR). This leads to reduced right ventricular pressures and increased pulmonary blood flow.
REF: p. 472 a. Increased PaO2 b. Increased pressure on the left side of the heart c. Blood flowing through the lungs d. High pulmonary vascular resistance
3. What factor is responsible for closure of the foramen ovale?
ANS: B
The increased fetal blood flow that results from the drop in PVR increases pulmonary venous blood return and, therefore, increases the left atrial pressure. At the same time, the RA pressure decreases when the umbilical cord is ligated and no longer provides placental blood flow to the IVC. The result of the higher LA pressures and the lower RA pressures is the closure of the foramen ovale.
REF: p. 472
4. For which of the following congenital cardiac defects may spontaneous closure of the ductus arteriosus be catastrophic?
I. Tetralogy of Fallot with pulmonary atresia
II. Atrial septal defect
III. Severe coarctation of the aortaIV. Hypoplastic left heart syndrome a. I and III only b. III and IV only c. I, II, and IV only d. I, III, and IV only
ANS: D
Shunting is potentially harmful, either due to prolonged cyanosis and decreased end organ oxygen delivery, or to increased PVR over time. However, shunting also has an important compensatory effect in patients with obstructed pulmonary or systemic blood flow. In these lesions, referred to as ductal-dependent lesions, the presence of a PDA provides lifesaving blood flow. Lesions with systemic outflow tract obstruction, such as critical coarctation of the aorta or hypoplastic left heart syndrome, rely on the PDA to provide systemic blood flow via a right-to-left shunt; these lesions have ductal-dependent systemic blood flow. With both rightto-left shunt (cyanotic cardiac defect) and left-to-right shunt (acyanotic cardiac defect), several lesions depend on a patent ductus arteriosus for adequate pulmonary and systemic blood flow. These anomalies are also called ductal-dependent lesions because spontaneous closure of the ductus arteriosus can prove catastrophic. Anomalies included in this group are severe coarctation of the aorta, hypoplastic left heart syndrome, and tetralogy of Fallot with pulmonary atresia.
REF: p. 472 a. Unreliable data b. Absence of ductal shunting c. Presence of ductal shunting d. Inconclusive data
5. How should the therapist interpret a preductal-to-postductal PaO2 difference of 8 mm Hg in a neonate?
ANS: B
Clinical signs of a PDA depend on the degree of left-to-right shunting but may include tachypnea and a continuous murmur. In addition to signs on exam, one can detect the presence of shunting by looking for a difference in oxygenation of preductal and postductal blood. A preductal blood gas should be obtained from the right radial or temporal artery, while a postductal gas may be obtained from the umbilical artery or from a peripheral artery in the lower extremity. A difference in PaO2 > 15 mm Hg indicates significant shunting across the PDA.
REF: p. 473 a. Increasing the circulating volume b. Maintaining/optimizing the hematocrit at the low end of normal hemoglobin level c. Administering indomethacin d. Administering digoxin
6. Which of the following methods is involved in the management of a PDA?
ANS: C
Medical management includes maintaining euvolemia and by optimizing the hemoglobin to ensure adequate oxygen delivery. In mechanically ventilated patients, increasing PEEP may serve to decrease the pulmonary blood flow by increasing PVR. In addition nonsteroidal antiinflammatory agents such as indomethacin and ibuprofen are often used in the medical management of PDA. Indomethacin may be used prophylactically to prevent PDA and therapeutically to treat a symptomatic PDA. A dose of indomethacin (0.2 mg/kg/dose IV) given in the first 24 hours of life can be effective in preventing a PDA. Therapy later in life is usually given over a 48-hour period. Doses of 0.1 to 0.2 mg/kg/dose IV every 12 to 24 hours are effective. Side effects are uncommon but include oliguria, renal insufficiency, and dilutional hyponatremia. Ibuprofen may also be used, though a recent meta-analysis found that the use of ibuprofen was associated with increased incidence of chronic lung disease when compared to indomethacin.
REF: p. 473 a. An ASD often causes congestive heart failure (because of decreased pulmonary blood flow). b. The right ventricle may become hypertrophic (right ventricular hypertrophy). c. Most patients with an ASD are symptomatic in the neonatal intensive care unit, presenting with right atrial enlargement. d. Chest radiographs are usually abnormal.
7. Which of the following clinical manifestations is consistent with an atrial septal defect (ASD)?
ANS: B
The pathophysiology of an ASD involves left-to-right shunting, leading to right atrial enlargement, right ventricular volume overload, and increased pulmonary blood flow. Over time this may result in right ventricular hypertrophy, congestive heart failure, and pulmonary vascular disease. Infants with ASDs rarely are symptomatic and may remain so well into adulthood. Only 8% of children with ASDs develop symptoms before 2 years of age. Chest radiographs are typically normal, unless the child has congestive heart failure, which may result in cardiomegaly and prominent pulmonary vascular markings.
REF: p. 473 a. II and III only b. I and IV only c. I, II, and III only d. II, III, and IV only
8. Which of the following clinical pathophysiologic manifestations are consistent with a large ventricular septal defect (VSD)?
I. The majority of the blood flow is shunted from left right to right left.
II. Shunting typically occurs during ventricular diastole, which causes left atrial enlargement.III. Chest radiography reveals an enlarged cardiac silhouette and increased pulmonary vascular markings, increasing pulmonary blood flow.
IV. Thickening and fibrosing of the pulmonary veins develop, decreasing pulmonary artery pressure.
ANS: A
The pathophysiology of VSDs involves left-to-right shunting, left ventricular volume overload, left atrial enlargement, and increased pulmonary blood flow. The size of the defect and the pulmonary vascular resistance determines the amount of shunting, which usually occurs during systole. Large defects may lead to large shunts, sometimes termed nonrestrictive VSDs, and may result in congestive heart failure and pulmonary hypertension.
REF: p. 474 a. To prevent the development of retinopathy of prematurity b. To avoid oxygen-induced hypoventilation c. To minimize pulmonary vascular dilation d. To reduce oxidative stress
9. Why must supplemental oxygen be judiciously administered to patients with an atrioventricular canal defect?
ANS: C
Oxygen saturations in these children may be low (75% to 90%) due to venous admixing but are tolerated well by most patients. Supplemental oxygen may be given judiciously, given the potential for oxygen to induce pulmonary vascular dilation and increased pulmonary blood flow.
REF: p. 476 a. Chest radiography reveals pleural effusion and pulmonary engorgement. b. The neonate often has metabolic alkalosis. c. The neonate presents in cardiogenic shock with hypotension. d. These infants are rarely symptomatic during the first month of life.
10. Which of the following clinical features characterize a critical aortic stenosis in a neonate?
ANS: C
The clinical presentation and natural history of aortic stenosis is determined by the time of presentation and the degree of stenosis. Neonates who present with critical aortic stenosis frequently present in cardiogenic shock with hypotension, poor perfusion, and metabolic acidosis. The chest radiograph frequently includes cardiomegaly and pulmonary edema.
REF: p. 476
11. Identify the congenital cardiac defect depicted in the following illustration: a. Atrial septal defect b. Hypoplastic left ventricular syndrome c. Hypoplastic right ventricular syndrome d. Atrioventricular canal defect
ANS: B
The cardiac anomaly depicted in this question is hypoplastic left ventricular syndrome, which can be viewed in the textbook in Figure 24-8.
REF: p. 478
12. Identify the following congenital cardiac anomaly: a. Truncus arteriosus b. Hypoplastic left ventricle c. Transposition of the great vessels d. Ventricular septal defect
ANS: A
The cardiac anomaly depicted in this question is truncus arteriosus, which can be viewed in the textbook in Figure 24-16.
REF: p. 483
13. Which of the following medications is the most common preoperative treatment to minimize preductal constriction until surgical correction of coarctation of the aorta can be achieved? a.
Indomethacin b. Prostaglandin E1 c. Negative inotropes d. Diuretics
ANS: B
Treatment of neonates with severe coarctation includes prostaglandin E1 to restore patency of the ductus arteriosus. These patients may also have significant ventricular dysfunction, congestive heart failure, and acidosis, requiring inotropes, diuresis, and ventilatory support.
REF: p. 477
14. Which of the following physiologic mechanisms need to be in place to ensure adequate systemic perfusion in infants with HLHS? a. Presence of an ASD b. Presence of a mitral regurgitation c. Adequate left atrial function d. Presence of a PDA
ANS: D
Adequate systemic perfusion in these infants depends on the presence of a nonrestrictive atrial septal connection, adequate right ventricular function, a patent ductus arteriosus, and a balance between the pulmonary and systemic circulations.
REF: p. 478
15. Which of the following strategies can be used to increase PVR in infants with HLHS? a. FiO2 < 0.21 b. Induce hypocapnia c. Administer indomethacin d. Close the PDA
ANS: A
A number of interventions may be employed to balance the systemic and pulmonary circulations. As the PVR decreases, minimizing the amount of administered oxygen can decrease pulmonary vasodilation and pulmonary blood flow. Occasionally, subambient oxygen concentrations (FiO2 < 0.21) are used to increase PVR. Target FIO2s are usually in the 0.17 to 0.21 range in order to keep systemic oxygen saturations 70% to 80%. Hypercarbia can also be utilized to elevate PVR.
REF: p. 480
16. What should the therapist select as target gas exchange parameters after surgical intervention for infants with hypoplastic left ventricular syndrome HLHS? a. pH < 7.35 b. PaO2 of 60 mm Hg and PaCO2 of 60 mm Hg c. pH > 7.45 d. PaO2 of 40 mm Hg and PaCO2 of 40 mm Hg
ANS: D
Goal gas exchange in these infants should follow the “rule of forties,” which targets PaO2 approximately 40 mm Hg and PaCO2 40 mm Hg. Any manipulation of the endotracheal tube in these patients should be conducted with caution.
REF: p. 480
17. The therapist is treating a child with TOF who appears to be having a “tet” spell. What should the therapist suggest to treat this event?
I. Beta blockers
II. Knee-chest position to increase SVR
III. Morphine sulfateIV. Oxygen a. IV only b. I and III only c. I and IV only d. I, II, III, and IV
ANS: D
See Box 24-1 in the text (Treatment of “tet” spells). Knee-chest position increases systemic vascular resistance and promotes blood flow from the right ventricle to the pulmonary artery rather than the aorta. Morphine sulfate decreases irritability and may lead to pulmonary artery dilation, which will increase pulmonary blood flow. Oxygen improves oxygenation and decreases pulmonary vascular resistance. Beta blockers (propranolol) may relax RVOT spasms. Systemic vasoconstrictors (phenylephrine) increase systemic vascular resistance to promote pulmonary blood flow. Sodium bicarbonate, administered to treat acidosis, decreases PVR.
REF: p. 483
18. Which of the following congenital cardiac anomalies is classified as conotruncal, associated with a “boot-shaped” appearance of the heart? a. Tetralogy of Fallot b. Transposition of the great vessels c. Coarctation of the aorta d. Atrioventricular canal defect
ANS: A
Chest radiography of patients with TOF classically reveals a “boot-shaped” appearance of the heart, which is a result of the narrow mediastinum and the effects of right ventricular outflow tract obstruction that leads to right ventricular hypertrophy.
REF: p. 482
19. Which of the following statements describe truncus arteriosus?
I. The pulmonary artery arises from the left ventricle, and the aorta stems from the right ventricle.
II. If PVR increases relative to systemic vascular resistance (SVR), more blood flows to the lungs through the truncus, decreasing systemic cardiac output.
III. If SVR decreases relative to PVR, blood flow will be shunted from right to left, bypassing the lungs.
IV. A large VSD allows total mixing of blood from the two ventricles.a. I and III only b. II and IV only c. I, II, and IV only d. I, III, and IV only
ANS: D
Truncus arteriosus refers to a rare defect where a single great artery arises from the ventricles of the heart, supplying the systemic, pulmonary, and coronary arteries (see Figure 24-18 in the textbook). A large VSD allows complete mixing of blood in the ventricles. The blood passes through a truncal valve before passing into the common truncus. The cardiac output and systemic oxygen saturations are determined by the balance between PVR and SVR. As PVR drops in the first several days of life, more blood flows to the lungs relative to the body, resulting in decreased systemic perfusion. If SVR decreases, blood will flow more to the body, leading to decreased pulmonary blood flow and hypoxemia.
REF: p. 483 a. The systemic venous blood passes through the right heart chambers. b. The pulmonary venous blood traverses the left side of the heart and then returns to the systemic circulation. c. When PVR increases relative to SVR, blood flow increases through the ductus arteriosus. d. Systemic venous blood flows to the lungs after leaving the right ventricle.
20. Which of the following blood flow patterns occurs in complete transposition of the great arteries?
ANS: A
In TGA the positions of the aorta and the pulmonary artery are reversed, with the aorta arising from the RV and the pulmonary artery arising from the LV (see Figure 24-17 in the textbook). The physiologic result is that the two circulations are in parallel rather than in series with each other. Deoxygenated systemic venous blood passes through the right heart and to the body without flowing through the lungs. Oxygenated pulmonary venous blood passes through the left heart and back to the lungs without flowing to the body. Survival depends on mixing at one or more points in the circulation. The potential sites for mixing of blood are ASDs, VSDs, or the PDA.
REF: p. 484
21. The therapist is treating a child with a congenital heart defect who is unresponsive to oxygen therapy. Although the chest X-ray is relatively normal, the heart is described as “egg-shaped.” Which of the following heart defects is more consistent with this description? a. Complete transposition of the great arteries b. Coarctation of the aorta c. Truncus arteriosus d. Tetralogy of Fallot
ANS: A
The main clinical sign of TGA is cyanosis that is not responsive to oxygen therapy. Chest radiography of TGA is frequently normal, though the cardiac silhouette may have the classic “egg on a string” appearance.
REF: p. 484
22. The therapist is setting pulse oximetry to determine the presence of right-to-left shunt in an infant suspected of having a heart defect. Where should the therapist place the pulse ox probe to obtain the most accurate measure of preductal oxygen saturation? a. Any finger of the right hand b. Any finger of the left hand c. Left earlobe d. Lower extremities
ANS: A
Pulse oximetry is a fundamental monitoring device in children with congenital heart disease. In addition to measuring systemic oxygenation, it can also be used to measure the degree of right-to-left shunting in lesions where this is a possibility. This is done by measuring preductal and postductal saturations. Preductal saturations are measured by placing the pulse oximeter on the right upper extremity. Postductal saturations are reflected by placing the pulse oximeter on any other extremity, though the lower extremities are preferred as preductal and postductal blood may be incompletely mixed at the left upper extremity. If postductal saturations are 5% to 10% lower than preductal saturations, then right-to-left shunting should be suspected.
REF: p. 487 a. The infant has dramatically improved ventilation by breathing deeply. b. The ETCO2 monitor is not accurate. c. Loss of pulmonary blood flow through the shunt d. Tricuspid regurgitation
23. A therapist monitoring an infant after a Blalock-Tausig shunt placement notices a significant drop in the end-tidal carbon dioxide (ETCO2) despite no changes in the infant’s respiratory rate. How should the therapist interpret this change?
ANS: C
The magnitude of the ETCO2 tracing may be used as a surrogate of efficacy of cardiopulmonary resuscitation (CPR). Finally, in children with a Blalock-Taussig shunt, a precipitous drop in the ETCO2 may indicate a loss of pulmonary blood flow due to shunt thrombosis.
REF: p. 488 a. >95% to 95% b. 85% to 90% c. 75% to 85% d. 70% to 80%
24. When using subambient oxygen therapy, what range of oxygen saturations should the therapist target?
ANS: C
When using this setup, special care must be taken in order to avoid inadvertent delivery of low oxygen. A continuous oxygen analyzer must be placed in the line with alarms for high and low levels of oxygen. Another safeguard that may be employed is requiring two clinicians to check the setup before applying it to the patient. Typically clinicians target oxygen saturations of 75% to 85%, utilizing an FiO2 as low as 0.16 to 0.17.
REF: p. 490
Chapter 25: Sudden Infant Death Syndrome & Sleep Disorders Test Bank
Multiple Choice
1. The mother of an 11-month-old infant suspected of suffering from sleep-disordered breathing reports that her child sleeps 15 hours per day. What should the therapist tell her regarding the sleep duration of her infant?
a. The sleep duration is consistent with the infant’s age.
b. The sleep duration is consistent with an infant in the first 24 hours of life.
c. The sleep duration is consistent with a that of a 10-year-old child.
d. The sleep duration is consistent with a midadolescent child.
ANS: A
Refer to Box 25-1 in the textbook (Sleep Duration by Age). Full-term Infant:16 to 18 hours; 1 year: 15 hours; 2 years: 13 to 14 hours; 4 years: 12 hours; 10 years: 8 to10 hours; midadolescence: 8.5 hours; later adolescence: 7 to 8 hours.
REF: p. 494 a. Newborns b. Infants c. Children d. Adults
2. Which age group is more often affected by periodic breathing?
ANS: D
Periodic breathing, a breathing pattern also common in infants, may be defined as a pattern of cycles of rapid breathing followed by pauses greater than 3 seconds in duration.
REF: p. 494
3. A 28-week-gestation newborn is demonstrating periods of apnea. In addition to ventilatory support, what other treatment can the therapist suggest? a. Placement of an oropharyngeal airway b. Caffeine c. Theophylline d. Beta blockers
ANS: B
Apnea of prematurity (AOP) is often treated with caffeine, which is thought to stimulate the respiratory centers.
REF: p. 495 a. Absence of respiratory effort and airflow b. Only abdominal movements occur with no airflow. c. Only thoracic movements occur. d. Paradoxical breathing movements occur.
4. Which of the following statements best describes central sleep apnea?
ANS: A
In central sleep apnea (CSA) there is an absence of respiratory effort and airflow.
REF: p. 495 a. Congenital malformations (e.g., heart defects) b. CSA c. SIDS d. ALTE
5. What is the leading cause of death in infants?
ANS: C
Sudden infant death syndrome (SIDS) is a devastating event that accounted for 2226 infant deaths in 2009. It is the leading cause of death in infants in the first 12 months of life and is the third leading cause of death in infants overall in the United States.
REF: p. 495
6. According to the American Academy of Pediatrics, in addition to cessation of breathing, which of the following clinical signs is associated with central sleep apnea? a.
Tachycardia b. Cyanosis c. Hypertension d. Hypertonia
ANS: B
The American Academy of Pediatrics defined CSA as "an unexplained episode of cessation of breathing for 20 seconds or longer, or a shorter respiratory pause associated with bradycardia, cyanosis, pallor, and/or marked hypotonia.”
REF: p. 495 a. More than 70% of victims are found in the late evening hours after the afternoon naps. b. Infants are most likely to experience SIDS in the first 12 to 24 months of life. c. SIDS is uncommon after infants are 6 months old. d. SIDS occurs exclusively when the infant is presumed to have been asleep during the night.
7. Which of the following statements best describes the condition sudden infant death syndrome (SIDS)?
ANS: C
SIDS almost always takes place when the infant is presumed to have been asleep, either during the day or night. However, more than 70% of its victims are found in the early morning hours after the nighttime sleep. The incidence peaks in infants from 2 to 4 months of life (see Figure 25-2 in the textbook). This period of time coincides with significant changes known to occur in sleep organization and in the modulation of brainstem centers involved in respiratory and arousal state control. SIDS is uncommon after 6 months of age, with 90% of SIDS victims affected in the first 6 months of life. It is rare after the first birthday.
REF: p. 495
8. Which of the following risk factors are associated with SIDS?
I. Maternal cigarette smoking
II. Breastfeeding
III. Loose bedding
IV. Bed sharing a. I and III only b. I, II, and III only c. I, II, and IV only d. I, III, and IV only
ANS: D
There are other risk factors that may be modified to reduce the incidence of SIDS. Maternal cigarette smoking during pregnancy has been found to be a major risk factor for SIDS and appears to be dose dependent. Postnatal exposure to cigarette smoke further increases the risk. Some studies have found breastfeeding to be partly protective against SIDS, but this finding has been inconsistent. Overheating and loose bedding have both been associated with SIDS. Bed sharing has been shown to be a hazardous practice. Overlying remains an important cause of unexplained death in infants and should be considered along with other forms of inadvertent suffocation during a death scene investigation. The most effective means of providing a safe sleeping environment is through meticulous risk mitigation. Box 25-3 in the textbook lists additional risk factors.
REF: p. 495
9. While working with a preterm neonate, the therapist notices the infant become apneic, cyanotic, and hypotonic. Consequently, the therapist nudges and stimulates the infant. On the basis of this scenario, what type of episode has occurred? a. Sudden infant death syndrome b. An apparent life-threatening event c. A resuscitative event d. An epileptiform activity
ANS: B
An Acute Life-Threatening Event (ALTE) is defined as “an episode that is frightening to the observer and is characterized by some combination of apnea (central and occasionally obstructive), color change (usually cyanotic or pallid but occasionally erythematous or plethoric), marked change in muscle tone (usually marked limpness), choking, or gagging.”
REF: p. 495
10. Which of the following body systems is the most important to evaluate when considering differential diagnoses for ALTE? a. Gastrointestinal b. Neurologic c. Respiratory d. Cardiac
ANS: A
Box 25-4 in the textbook (Differential Diagnosis of ALTE). Gastrointestinal (50%), neurologic (30%), , respiratory (20%), cardiac (5%), metabolic disease (under 5%).
REF: p. 498
11. Which of the following conditions is the major cause of OSA in children without any predisposing factor? a. Choanal atresia b. Macroglossia c. Adenotonsillar hypertrophy d. Pierre Robin Syndrome
ANS: C
The major cause of OSA in children without another predisposing condition (see Box 25-6 in the textbook) is adenotonsillar hypertrophy.
REF: p. 498 a. First 6 months b. 6 months to 1 year c. 1 to 2 years d. 2 years to 8 years
12. What is the age group with the highest prevalence of OSA?
ANS: D
It may occur in children of all ages but the prevalence peaks between 2 and 8 years of age, which coincides with the time at which the size of the tonsils is at its peak relative to the upper airway size.
REF: p. 499
13. Which of the following are typical features of the obstructive hypoventilation syndrome?
I. Disruption of sleep architecture
II. Degradation of sleep quality
III. Abnormal gas exchangeIV. Significant daytime symptoms a. I and III only b. II and IV only c. I, II, and IV only d. I, II, III, and IV
ANS: D
Obstructive hypoventilation (obstructive hypopnea) may occur in the absence of complete obstruction of the airway and cessation of airflow. These sleep-related events lead to disruption of sleep architecture, degradation of sleep quality, and gas exchange abnormalities that may cause significant daytime symptoms.
REF: p. 500
14. The childhood syndrome of OSA is distinct from adult OSA. Which of the following features are common in adult OSA but infrequent or less common in pediatric OSA? a.
Large neck circumference b. Snoring c. Excessive daytime sleepiness d. REM abnormality
ANS: C
While obesity and excessive daytime sleepiness are common in adult patients with OSA, they are infrequent or less common in pediatric patients with OSA. Refer to Box 25-5 in the textbook for more details.
REF: p. 499
15. Which of the following are typical daytime symptoms associated with SDB in children?
I. Poor school performance
II. Hypoactivity
III. InattentionIV. Passive behavior a. I and III only b. II and IV only c. I, II, and IV only d. I, II, III, and IV
ANS: A
Daytime symptoms include poor school performance, hyperactivity, and inattention or aggressive behavior.
REF: p. 500 b. Administer antireflux medications. c. Perform allergy tests to confirm that airway obstruction is due to other clinical condition. d. Provide continuous positive airway pressure.
16. A 7-year-old child was diagnosed with OSA due to tonsillar hypertrophy. Although adenotonsillectomy was performed, the child continues having daytime sleepiness and poor school performance. What should the therapist suggest at this time? a. Consider uvulectomy.
ANS: D
Continuous positive airway pressure (CPAP) is the treatment of choice in patients who either are not a suitable candidate for surgery or have persistent SDB.
REF: p. 500
Chapter 26: Pediatric Airway Disorders and Pulmonary Infections Test Bank
Multiple Choice
1. Relative to an adult’s larynx, where is an infant’s larynx situated?
a. C1-2 b. C2-3 c. C3-4 d. C4-5
ANS: C
The epiglottis is long, floppy, and angled away from the tracheal axis. It shrouds the laryngeal opening because of poor support by the surrounding tissues. Structurally, the infant’s larynx is positioned higher in the neck (near C3-4) compared with an adult’s larynx (at C4-5). Because of this superior location, the tongue base tends to “hide” the larynx from view during direct laryngoscopy.
REF: p. 506 a. The older child has a better developed immune system. b. The younger child has a less effective cough mechanism. c. The older child has a better developed mucociliary escalator. d. The younger child has fewer respiratory bronchioles.
2. Why does a respiratory syncytial viral infection have little adverse effect on an older child but is often life threatening to a younger child?
ANS: D
Because of the developmentally small airway cross-sectional area, small amounts of inflammation at the level of the respiratory bronchioles can result in severe respiratory embarrassment. In young children the respiratory bronchioles are commonly attacked by viruses, such as respiratory syncytial virus (RSV), resulting in respiratory failure. The same infection will have little or no respiratory effect on an adult or older child with a larger number of terminal airways.
REF: p. 507 a. Mild obstruction b. Moderate obstruction c. Severe obstruction d. Complete obstruction
3. As the therapist auscultates over an infant’s larynx, he hears a very low-pitched sound. On the basis of this finding, what impression is he likely to have regarding the nature of the upper airway obstruction?
ANS: A
Auscultation of air movement during inspiration and expiration aids in determining the severity and location of the obstruction. The pitch of the stridor can be used to assess improvement or worsening of the obstruction. Low-pitched sounds signify mild obstruction, whereas a higher pitch indicates that the child is in more distress and is attempting to generate a higher air flow rate.
REF: p. 508 a. Because the anterior nares widen more b. Because the infant breathes more through the mouth c. Because the infant is able to generate a stronger inspiratory effort d. Because accessory muscles of ventilation help stabilize the chest wall
4. Why does an infant’s respiratory distress from choanal atresia seem to lessen when the infant cries?
ANS: B
Choanal atresia, the stenosis or absence of the nasal passages (choanae), typically presents in the immediate postnatal period. The infant presents with severe respiratory distress that appears to lessen with crying, when the infant manages to exchange air through the mouth, and is exacerbated again once the crying stops.
REF: p. 508
5. A 30-month-old child is brought to the emergency room (ER) by the parents. The child appears to have a sore throat along with dysphagia, fever, and voice changes. The child exhibits “hot potato voice.” Visualization of the posterior pharynx reveals a displaced retropharynx. What condition does this child likely have? a. Peritonsillar abscess b. Retropharyngeal abscess c. Tonsillar enlargement d. Pierre Robin syndrome
ANS: B
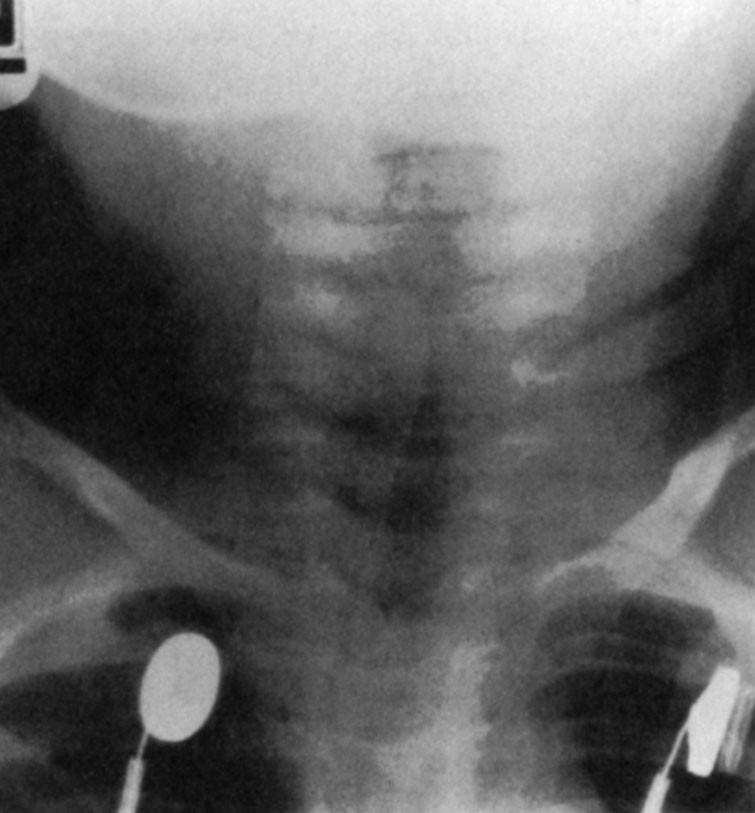
Retropharyngeal abscess commonly occurs in children younger than 3 years of age and can cause obstruction from forward displacement of the posterior pharyngeal wall. Infectious agents involved are Group A Streptococcus, Staphylococcus aureus, and, occasionally, anaerobic bacteria. The child often presents with a sore throat, fever, dysphagia, and voice changes. The voice sounds as if the child is attempting to speak without moving the tongue while maximally expanding the oropharyngeal airway. This is described as “hot potato voice.” A lateral neck radiograph is obtained to determine the tissue thickness surrounding the abscess. Visualization of the posterior pharynx may reveal a displaced retropharynx. Surgical drainage is the preferred treatment, along with administration of appropriate antibiotics based on culture results of the aspirated material.
REF: p. 509
6. A 4-year-old child is brought into the emergency room (ER) by her parents, who state that an abrupt high fever developed along with a severe sore throat, dysphagia with drooling, and cough. In the ER the girl exhibits stridor, muffled voice without hoarseness, air hunger, and cyanosis. She also has suprasternal, substernal, and intercostal retractions, with nasal flaring, bradypnea, and dyspnea. The child is sitting upright with her chin thrust forward and her neck hyperextended in a tripod position. What condition is she likely exhibiting? a.
Laryngotracheobronchitis b. Tracheomalacia c. Bacterial tracheitis d. Epiglottitis
ANS: D
Onset of bacterial epiglottitis is usually abrupt and associated with high fever; severe sore throat; dysphagia with drooling; cough, progressing rapidly over a few hours to stridor; muffled ("hot potato") voice without hoarseness; air hunger; and cyanosis. Suprasternal, substernal, and intercostal retractions, along with nasal flaring, bradypnea, and dyspnea, are frequently displayed. The child assumes a characteristic position of sitting upright with the chin thrust forward and with the neck hyperextended (sniffing position) in a tripod position. The streptococcal variant of epiglottitis may be associated with a longer prodrome lasting more than 24 hours.
REF: p. 510 a. Epiglottitis b. Laryngotracheobronchitis (LTB) c. Bronchitis d. Bronchiolitis
7. A 10-month-old child has been brought into the emergency room (ER) by her parents, who state that after few days with low-grade fever, malaise, and rhinorrhea, their child presented with a “barking” cough and increased work of breathing. What condition is this child likely exhibiting?
ANS: B
The child with LTB presents with a gradual prodrome of low-grade fever, malaise, rhinorrhea, and hoarse voice. Over several days the illness progresses to inspiratory stridor and a “barky” cough, often described as sounding like the bark of a seal. Physical examination reveals nasal flaring, nasal congestion, use of accessory muscles, and suprasternal, subcostal, and intercostal retractions that, along with the stridor, become worse when the child is agitated.
REF: p. 511 a. Posterior pharyngeal shadow b. Thumb sign c. Steeple sign d. Penumbra effect
8. Which of the following lateral neck radiographic presentations is characteristic of laryngotracheobronchitis?
ANS: C
A lateral neck radiograph, sometimes obtained to help differentiate laryngotracheobronchitis from epiglottitis, demonstrates a large retropharyngeal air shadow without epiglottic swelling. The anteroposterior (A-P) chest radiograph reveals the classic “steeple sign,” a sharply sloped, wedge-shaped, linear narrowing of the trachea. This demonstrates the subglottic tracheal edema that extends from the larynx to the thoracic trachea.
REF: p. 511
9. Which of the following medications should be administered to a 4-year-old child who develops postextubation stridor? a. Phenylephrine b. Racemic epinephrine c. Prednisolone d. Antibiotics
ANS: C
Today, patients are treated with dexamethasone and racemic epinephrine and discharged from the emergency department to home if they are free of intercostal retractions and stridor after a 2-hour waiting period.
REF: p. 512
10. A 3-year-old child has been diagnosed with epiglottitis and was intubated due to severe respiratory distress. After 24 hours of antibiotics the therapist is considering extubation. What will be an acceptable leak before considering extubation? a. 20 cm H2O b. 21-30 cm H2O c. 31-35 cm H2O d. An audible leak at any pressure level is enough to consider extubation.
ANS: A
Extubation is usually considered within 24 hours when signs of toxicity (e.g., fever) diminish and when an air leak at 20 cm H2O pressure develops around the ETT.
REF: p. 511 a. Trachea b. Terminal bronchioles c. Segmental bronchi d. Alveoli
11. While performing auscultation on a 2-month-old child, the therapist hears wheezes equal in pitch across all regions of the chest; however, they seem loudest in the vicinity of the sternum. From which of the following anatomic structures is the wheezing likely originating?
ANS: A
Discerning where the wheezes originate in a small child is often difficult. Wheezes that remain equal in pitch across all regions of the chest but are heard loudest around the sternum most likely have originated in the trachea. Larger bronchial lesions produce similar manifestations but are more localized to the side of the lesion.
REF: p. 513
12. Tracheomalacia is a condition of dynamic tracheal collapse. Which of the following injurious events can be associated with this condition? a. Neonatal ventilation with high pressures b. Excessive use of racemic epinephrine c. Tracheal trauma due to CPT d. Neonatal ventilation with high oxygen concentrations
ANS: A
Common injurious events include neonatal ventilation with high pressures, chronic trauma to the trachea from a malpositioned ETT or aggressive endotracheal suctioning, and external compressive structures, such as a vascular ring.
REF: p. 513
13. An 11-month-old child has been treated with bronchodilators for persistent wheezing without a positive clinical response. Which of the following conditions should the therapist suspect? a.
Bronchitis b. Aspergillosis c. Bronchiolitis d. Endobronchial compression
ANS: D
The diffuse, chronic wheeze associated with these disorders is often confused with asthma. Endobronchial compression is suspected in an infant or child with persistent wheezing that does not respond to bronchodilator therapy.
REF: p. 514
14. A therapist has been asked to evaluate a child suspected of having foreign body aspiration. Which of the following clinical conditions would guide the therapist to the diagnosis? a. Recurrent bronchitis b. Wheezing partially responsive to bronchodilators c. Unilateral wheezing d. Stridor
ANS: C
Signs and symptoms of foreign body aspiration vary with the location of impaction and the degree of airway obstruction. They can range from unilateral wheezing or recurrent pneumonia, as when peanuts or popcorn obstruct the smaller airways, to immediate occlusion of the upper airway with complete absence of air movement and rapid death from suffocation, as seen in hot dog or balloon aspiration fatalities. It is not necessary for the foreign body to be in the trachea: a big enough object stuck in the esophagus can elicit very similar symptoms of respiratory distress.
REF: p. 514 a. A standard portable A-P chest X-ray b. A lateral neck radiograph c. Either a right or left lateral decubitus film d. Inspiratory and expiratory A-P chest X-rays
15. Which of the following radiographic techniques is best for determining the presence of a ballvalve type obstruction?
ANS: D
Asymmetric lung hyperinflation can result from a ball-valve effect of foreign material localized in a major bronchus. This defect is most often apparent on an expiratory film. Comparison between expiratory and inspiratory films can also yield the diagnosis but depends greatly on the cooperation of the child.
REF: p. 515
16. The therapist is evaluating a child in the emergency department who displays the following signs: inability to cry, ineffective cough, high-pitched inspiratory sound, and cyanosis. What should the therapist suspect? a. Tracheomalacia b. Severe or complete airway obstruction c. Vascular ring d. Status asthmaticus
ANS: B
Pediatric Advanced Life Support (PALS) guidelines state that signs of severe or complete airway obstructions that require intervention are: inability to speak or cry audibly; weak, ineffective cough; high-pitched sound or no sound during inhalation; increased difficulty breathing with distress; cyanosis; and universal choking sign (thumb and index finger clutching neck).
REF: p. 515 a. RUL b. RML c. Lingula d. LUL
17. The therapist has been asked to evaluate the chest radiograph of a 3-month-old boy with atelectasis. Which pulmonary lobe has the greatest tendency to collapse in young infants?
ANS: B
The right middle lobe, which has the poorest collateral air circulation and smallest bronchial opening of the major lung segments, is particularly prone to mucus plugging and collapse. Intubated patients, particularly young infants, have a propensity toward right upper lobe collapse. This is most likely related to their supine positioning and tendency toward obstruction of the right upper lobe bronchus (the most proximal of all the lobar bronchi) by a migrating ETT.
REF: p. 516
18. In the ER, a chest radiograph reveals dilation of the segmental and subsegmental bronchi. The patient complains of expectorating copious amounts of thick mucus and frequent lung infections over the last year. Which of the following conditions does this child likely have? a. Atelectasis b. Bronchiectasis c. Foreign body aspiration d. Postoperative laryngotracheobronchitis
ANS: B
Bronchiectasis is defined as irreversible dilation of the bronchial tree. Typically, the segmental and subsegmental bronchi become irregularly shaped and dilated, leading to a loss of the typical funnel configuration that allows smooth central flow of secretions. Additionally, ciliary activity in the area of the dilation is inadequate and further contributes to the difficulty in mobilizing secretions. The secretions become infected as they pool. The lower lobes, particularly the left lower lobe, are most frequently involved.
REF: p. 517
19. A 3-year-old child has the following clinical presentations in the ER:
Profound nasal congestion and productive cough
Chest auscultation revealing diffuse coarse, “sticky” crackles (sounding like Velcro)
Chest radiograph revealing lung hyperinflation with flattened hemidiaphragms a. Bronchiectasis b. Primary ciliary dyskinesia c. Supralaryngeal obstruction d. Bronchiolitis
What pulmonary condition does this infant likely have?
ANS: D
Physical findings vary considerably with the patient’s age. Infants (younger than 1 year) develop coryza, cough, respiratory distress, wheezing, and tachypnea. The symptoms of infection usually peak at about 48 to 72 hours, and a previously healthy infant can progress from what was thought to be a simple cold to severe respiratory distress during that time. In contrast, the principal symptoms in children older than 2 years of age include profound nasal congestion and productive cough. Chest auscultation reveals diffuse coarse, “sticky” crackles (sounding like Velcro) that may be accompanied by wheezes. A chest radiograph typically reveals intense lung hyperinflation with flattened hemidiaphragms (obstructive), with occasional films showing evidence of collapse or consolidation.
REF: p. 518
20. An 18-month-old child has been admitted with a diagnosis of bronchiolitis due to RSV. The therapist has administered a single dose of albuterol and racemic epinephrine, but the child shows no signs of improvement. What should the therapist suggest at this time? a. Alternate albuterol and racemic epinephrine every 4 hours b. Use albuterol every 1 hour for 4 hours and then space treatments to every 4 hours c. Discontinue therapy d. Add an inhaled corticosteroid to the albuterol every 12 hours
ANS: C
A single inhalation trial using epinephrine or albuterol can be considered for respiratory distress on an individual basis, such as when there is history of asthma, allergy, or atopy. It is recommended to discontinue inhalation therapy if there is no clinical response such as improved respiratory distress or improved bronchiolitis scores. Nebulized racemic epinephrine demonstrates better short-term improvement in pulmonary physiology and clinical scores but only in the outpatient setting. However, continuation of inhalation therapy despite documented nonresponse exposes the patient to unnecessary therapy and cost.
REF: p. 519
21. Which of the following agents has been shown to significantly reduce bronchiolitis scores? a. Prednisone b. Nebulized 3% hypertonic saline c. Dexamethasone d. Theophylline
ANS: B
Nebulized hypertonic saline (3%) is considered an effective and safe treatment for infants with mild-moderate respiratory distress and has been shown to reduce LOS. The optimal treatment regime for nebulized hypertonic saline in the inpatient setting in acute bronchiolitis remains unclear. A recent RCT using Q2 hour hypertonic saline for 3 doses, every 4 hours for 5 doses, and every 6 hours until discharge has shown promising results and is an alternative; however, more evidence is needed on efficacy and dosing regimen. Hypertonic saline therapy significantly reduces bronchiolitis scores (pre/post) in patients with mild-moderate bronchiolitis.
REF: p. 520 a. Bronchitis b. Bronchiectasis c. Bronchiolitis d. Pneumonia
22. A child presents to the emergency department with fever, tachypnea, nasal flaring, and shallow breathing. The physical exam of the chest reveals the presence of crackles, increased tactile fremitus, and dullness to percussion. What should the therapist suspect the diagnosis is?
ANS: D
Prodromal symptoms are often nonpulmonary and include headache, fever, malaise, and abdominal pain. Productive cough, with sputum often swallowed, and chest pain during inspiration (pleuritic pain) are common complaints. Physical examination usually reveals nasal flaring, accessory muscle use, intercostal and subcostal retractions, tachypnea, and shallow breathing. Crackles, decreased breath sounds, increased fremitus, and dullness to percussion are often found during auscultation and examination of the chest.
REF: p. 523 a. Three consecutive days of gastric washings b. A positive skin test c. A positive chest X-ray d. One positive respiratory washing
23. Diagnosis of TB in children requires which of the following special considerations?
ANS: A
Diagnosis in the adult is based on identification of stains of gastric or respiratory washings that have bacteria uniquely resistant to acid decoloration (“acid fast”). In children, owing to the low number of bacilli, 3 consecutive days of gastric washings may increase the sensitivity of this test.
REF: p. 526
24. Which of the following clinical interventions are used to treat complications of sickle cell anemia?
I. Supplemental oxygen
II. Bronchodilators
III. Diuretics
IV. Red blood cell transfusionsa. I and IV only b. II and III only c. I, II, and IV only d. II, III, and IV only
ANS: C
Adequate hydration is an essential therapeutic modality and is used cautiously to avoid pulmonary edema. Red blood cell transfusions are provided to improve the ability of hemoglobin to transport oxygen and to reduce the incidence of acute chest syndrome, myocardial ischemia, and sickle cell chronic lung disease. Aerosolized bronchodilators for bronchiole constriction, incentive spirometry, and adequate pain control can be important adjuvants. Supplemental oxygen is used when indicated but, depending on the case, can foster additional sickling. In cases of impending respiratory failure, mechanical ventilation is instituted. Successful treatment of acute chest syndrome with venovenous extracorporeal membrane oxygenation (ECMO) has been reported in patients experiencing life-threatening acute chest syndrome despite maximal conventional ventilation support.
REF: p. 528




