
36 minute read
Chapter 12: Airway Clearance Techniques and Lung Volume Expansion Test Bank
Multiple Choice
1. What are the main components of the traditional airway clearance techniques?
I. Palpation of the chest wall
II. Postural drainage
III. PercussionIV. Coughing a. II only b. I and III only c. II, III, and IV only d. I, II, III, and IV
ANS: C
Traditional airway clearance techniques (ACT) are designed to remove secretions from the lungs and include postural drainage, percussion, chest wall vibration, and coughing.

REF: p. 198 a. Posterior segment of the right upper lobe b. Apical segment of the right upper lobe c. Posterior basal segments of both lower lobes d. Anterior segments of both upper lobes
2. On the basis of the following diagram, which of the following lung segments is being drained?
ANS: C
What is shown here (and in Figure 12-3E in the textbook) is the postural drainage position for draining the posterior basal segments of the right and left lower lobes.
REF: p. 200 a. Right middle lobe b. Left lingular segment of the lower lobe c. Lateral basal segment of the right lower lobe d. Apical-posterior segment of the left upper lobe
3. On the basis of the following diagram, which of the following lung segments is being drained?
ANS: A
What is shown here (and in Figure 12-4H in the textbook) is the postural drainage position for draining the right middle lobe.
REF: p. 200
4. The following postural drainage positions are shown for an infant patient: a. Image A b. Image B c. Image C d. Image D

Which of the diagrams demonstrates the postural drainage position for draining the lingular segments of the left upper lobe in an infant?
ANS: C
What is shown here (and in Figure 12-3I in the textbook) are the lingular segments of the left upper lobe; choice A (see Figure 12-3F in the textbook) shows the lateral basal segment of the right lower lobe; choice B (see Figure 12-3G in the textbook) shows the anterior basal segment of the right lower lobe; and choice D (see Figure 12-3D in the textbook) shows the superior segments of both lower lobes.
REF: p. 200
5. The following postural drainage positions are shown for a pediatric patient: a. Image B b. Image C c. Image A d. Image D
Which of the diagrams demonstrates the postural drainage position for draining the posterior subsegment of the apical-posterior segment of the left upper lobe?

ANS: C
What is shown here (and in Figure 12-4A in the textbook) is the apical segment of the right upper lobe and the apical subsegment of the apical-posterior segment of the left upper lobe; choice B (see Figure 12-4B in the textbook) shows the posterior segment of the right upper lobe and the posterior subsegment of the apical-posterior segments of the left upper lobe; choice C (see Figure 12-4C in the textbook) shows the anterior segments of the right and left upper lobes; choice D (see Figure 12-4D in the textbook) shows the superior segments of both lower lobes.
REF: p. 200 a. To reduce the risk of inadvertent extubation with the suction catheter b. To prevent the development of bronchial stenosis and granulomas c. To decrease the chance of removing too much lung volume d. To minimize the risk of oxygen desaturation
6. When performing endotracheal suctioning on a neonate, why should the therapist routinely avoid advancing the catheter tip beyond the distal end of the endotracheal tube?
ANS: B
The trachea and bronchi of the newborn appear especially vulnerable to damaging effects from endotracheal tubes and suction catheters. Consequences of deep endotracheal suctioning include the development of bronchial stenosis and granulomas. Avoiding deep endotracheal suctioning minimizes these risks. Therefore when suctioning intubated infants after chest physical therapy (CPT), the therapist should not routinely advance the suction catheter beyond the distal end of the endotracheal tube. If evidence of persistent secretion retention exists despite adequate suctioning of the endotracheal tube, the suction catheter can be carefully and slowly advanced 1 or 2 cm beyond the tip of the endotracheal tube.
REF: p. 203
7. Which of the following maneuvers is characterized by having a patient forcibly exhale, from a middle to low lung volume, through an open glottis? a. Autogenic drainage b. Directed cough c. Positive expiratory pressure d. Active cycle of breathing
ANS: D
FET is also known as "huff" coughing. This maneuver requires the patient to forcibly exhale, from middle to low lung volumes, with an open glottis, but requires extreme cooperation and cannot be performed on infants or young children.
REF: p. 204 a. Total lung capacity b. Inspiratory reserve volume c. Expiratory reserve volume d. Tidal volume
8. During autogenic drainage, at which of the following levels does the patient begin breathing?
ANS: C
AD is a series of breathing exercises designed to mobilize secretions in patients with bronchiectasis or CF. To loosen secretions from the smallest airways, the patient begins breathing in a slow, controlled manner, first at the expiratory reserve volume level. The volume of ventilation is then increased, with the patient breathing in the normal tidal volume range but exhaling approximately halfway into the expiratory reserve volume.
REF: p. 205 a. By dislodging mucus directly from bronchial walls b. By advancing the mucociliary escalator at a faster than normal rate c. By mechanically lysing long molecules of mucus into smaller, more mobile segments d. By generating high expiratory air velocities
9. By which of the following mechanisms are high-frequency chest compressions purported to mobilize tracheobronchial secretions?
ANS: D
Commercially available devices have been developed that compress the entire chest wall at high frequencies by means of a snug-fitting inflatable vest connected to a high-performance air compressor (see Figure 12-6 in the textbook). Intermittent chest wall compression produces brief periods of high expiratory airflow, which loosens and mobilizes mucus from bronchial walls. This type of device is widely used in patients with CF.
REF: p. 205 b. They attempt to prevent dynamic airway collapse. c. They work toward increasing the functional residual capacity of patients. d. They are intended to promote the ability of patients to generate effective coughs.
10. What do postural drainage, positive expiratory pressure therapy, autogenic drainage, forced expiration techniques, and high-frequency chest compressions have in common? a. They dislodge mucus from the bronchial walls of patients.
ANS: B
Postural drainage, positive expiratory pressure (PEP), AD, FET, and HFCC attempt to prevent or compensate for dynamic airway collapse.
REF: p. 206
11. A patient with an excessive amount of secretions and atelectasis has been receiving ACT. What is the most commonly cited complication of ACT? a. Hypoxemia b. Hypercapnia c. Alterations of blood pressure d. Tachycardia
ANS: A
The most commonly cited adverse effect of ACT is hypoxemia.
REF: p. 207 a. Asthma b. Pneumonia c. Bronchiolitis d. Atelectasis
12. A respiratory therapist has been assigned to administer ACT to a number of patients on the ward. In which of the following conditions may ACT be beneficial?
ANS: D
The majority of patients with acute atelectasis secondary to mucous plugs respond with one ACT treatment.
REF: p. 209
13. A respiratory therapist has been assigned to administer ACT to a number of patients on the ward. In which of the following conditions may ACT be contraindicated?
I. Foreign body aspiration
II. Frank hemoptysis
III. Empyema
IV. Untreated pneumothoraxa. I, II, III, and IV b. II and IV only c. III and IV only d. I and IV only
ANS: A
Frank hemoptysis, empyema, foreign body aspiration, and untreated pneumothorax are often considered contraindications to all components of ACT.
REF: p. 211
14. A respiratory therapist has been assigned to administer CPT to a patient with cystic fibrosis. What areas of the body should the RT avoid when percussing the patient? a. Intercostal spaces b. Fractured ribs c. Precordium d. Areas between the scapulas
ANS: B
Chest percussion should not be performed directly over fractured ribs, areas of subcutaneous emphysema, or recently burned or grafted skin.
REF: p. 211
15. A respiratory therapist has been assigned to administer ACT to a patient with acute lobar atelectasis. What should the RT consider to determine the length and frequency of the treatment?
I. Most pediatric patients require ACTs for at least 45 minutes.
II. ACT is rarely needed more than every 4 hours.
III. ACT orders should be evaluated at least every 48 hours for patients in the ICU.IV. ACT for patients with atelectasis due to CF requires at least 30 to 45 minutes. a. I, II, and III only b. II and III only c. III and IV only d. II, III and IV only
ANS: D
Treatments for patients with CF or bronchiectasis should be performed for at least 30 minutes, with many patients benefiting from therapy lasting 45 minutes or longer. Patients with severe dyspnea may require rest periods, which will further prolong therapy. Most pediatric respiratory care departments limit routine ACT treatments to 15 to 20 minutes. ACT is rarely needed more than every 4 hours, although selected patients may benefit from more frequent suctioning or coughing. ACT orders should be evaluated at least every 48 hours for patients in intensive care units, at least every 72 hours for acute care patients, or whenever there is a change in a patient's status.
REF: p. 211 a. Request to cancel the order and change therapy. b. Try to instruct the child on how to perform FET. c. Apply gentle chest wall compression during the expiratory phase. d. Ask the child to forcefully cough after a deep breath.
16. A respiratory therapist has been assigned to administer FET to a 5-year-old patient. Since small children are typically unable to perform such a maneuver, what should the RT do at this time?
ANS: C
Infants and small children are unable to perform maneuvers such as FET or AD. Some clinicians have attempted to mimic these techniques with gentle chest wall compression during the expiratory phase, allowing the child to exhale to less than functional residual capacity. Like AD or FET performed in cooperative older patients, this technique results in increased expiratory air velocity at low lung volumes, improving mucous mobilization.
REF: p. 212 a. Quality of the chest radiograph b. Degree and persistence of coughing c. Changes in the color and consistency of mucus d. Amount of mucus obtained during and after treatment
17. What is the most important variable used to assess the efficacy of CPT?
ANS: D
Because the goal of CPT is to promote the removal of excessive bronchial secretions, the most important variable for evaluating the effectiveness of CPT is the amount of secretions expectorated with therapy.
REF: p. 212
18. Which of the following clinical parameters are important to determine a positive response to ACT?
I. Changes in sputum color
II. Breath sounds
III. Vital signs
IV. Lung mechanics a. I, II, and III only b. II and III only c. III and IV only d. II, III and IV only
ANS: D
Changes in sputum production, breath sounds, vital signs, chest radiographic findings, blood gas values, and lung mechanics may indicate a positive response to the therapy.
REF: p. 212
19. For which of the following patients is incentive spirometry contraindicated?
I. Uncooperative
II. Physically disabled
III. Grossly obeseIV. Very young a. IV only b. I and II only c. I, II, and IV only d. I, II, III, and IV
ANS: C
Incentive spirometry is contraindicated in patients who cannot cooperate or follow instructions concerning the proper use of the device. The child may be uncooperative, physically disabled, or simply too young to effectively perform the maneuvers. Alternative methods such as walking, getting up in a chair, frequent changes in position, or singing to improve lung volumes should then be considered.
REF: p. 213
20. The respiratory therapist has been asked to evaluate the effectiveness of incentive spirometry in some patients during their postoperative stage. What will the RT find to be most influential on the outcome associated with IS? a. Frequency of therapy b. Level of inspiratory capacity achieved by the patient c. Level of supervision and instruction of therapy d. Patient’s age
ANS: C
The majority of problems that patients experience with incentive spirometry are the result of inadequate supervision or instruction, or both. These two factors account for a large number of ineffective treatments.
REF: p. 213
Chapter 13: Airway Management Test Bank
Multiple Choice
1. Which of the following criteria are used to define ventilatory and hypoxemic dysfunction in patients who may need intubation?
I. PaO2 < 80 mm Hg with FiO2 > 0.60
II. PaCO2 > 50-60 mm Hg
III. pH < 7.3
IV. PaO2/FiO2 > 250 a. I and III only b. II and III only c. I, II, and III only d. I, III, and IV only
ANS: B
The need for intubation, due to a lack of pulmonary function, results from deficits in oxygenation, ventilation, or both taken in concert with the patient's clinical condition. Acute ventilatory dysfunction can be defined as an arterial partial pressure of carbon dioxide (PaCO2) greater than 50 to 60 mm Hg with a pH less than 7.3. Pulmonary dysfunction due to hypoxemia is defined as an arterial partial pressure of oxygen (PaO2) less than 60 mm Hg with a fraction of inspired oxygen (FiO2) greater than or equal to 0.60. These definitions assume that there is no intracardiac right-to-left shunt resulting from a congenital cardiac defect.
REF: p. 223
2. Which of the following conditions associated with upper airway obstruction may cause respiratory failure and require an artificial airway?
I. Laryngotracheobronchitis
II. Pneumonia
III. EpiglottitisIV. Subglottic stenosis a. I and III only b. II and IV only c. I, II, and III only d. I, III, and IV only
ANS: D
Upper airway obstruction may also cause respiratory failure. Examples that are included in this category are diseases such as laryngotracheobronchitis (i.e., croup), epiglottitis, laryngeal papillomatosis, and severe subglottic stenosis.
REF: p. 223 b. 4.0 mm I.D. c. 4.5 mm I.D. d. 5.0 mm I.D.
3. The therapist is about to perform endotracheal intubation on a 2-year-old infant. What size endotracheal tube needs to be used? a. 3.5 mm I.D.
ANS: C
Using the following formula, the therapist can calculate the approximate size endotracheal tube to use to intubate a 2-year-old infant: Internal diameter (mm) = (age [yr] ÷ 4) + 4 = (2 yr ÷ 4) + 4 = 0.5 + 4 = 4.5 mm I.D.
REF: p. 224 a. Because some lung volumes are so small cuffs are unnecessary b. Because in some infants the ETT creates a seal against the cricoid cartilage c. Because less airway resistance develops without a cuff, promoting lower ventilation pressures d. Because ETTs without cuffs enable pressure venting when an infant cries
4. Prior to 2005, why were endotracheal tubes (ETTs) without cuffs routinely recommended for children less than 8 years of age?
ANS: B
Because the cricoid cartilage is the narrowest portion of the pediatric airway until about 8 years of age, use of an uncuffed ETT was traditionally recommended until that time. In 2005, the American Heart Association's Pediatric Advance Life Support program (PALS) stopped recommending uncuffed tubes because there was no evidence to support one over the other. Today it is left up to the clinician to determine whether a cuff is needed for patients less than 8 years of age.
REF: p. 224 a. The epiglottis is directly lifted with the tip of the laryngoscope blade. b. The tip of the laryngoscope blade is placed in the vallecula. c. The tip of the laryngoscope blade is placed in the uvula. d. The laryngoscope blade is used to sweep the tongue to the left.
5. Where in the upper airway of an infant should the laryngoscope straight blade be placed to expose the glottis during endotracheal intubation?
ANS: A
When a straight blade is used, the epiglottis is lifted with the tip of the blade and pressed against the base of the tongue.
REF: p. 224 a. The LMA should be used only with conscious patients. b. The potential for aspiration is lower than with translaryngeal intubation. c. The LMA is a good alternative as an emergency airway when positive-pressure ventilation is needed. d. The LMA is placed into the larynx immediately above the epiglottis.
6. Which of the following statements describe the laryngeal mask airway (LMA)?
ANS: C
If endotracheal tube placement is unsuccessful, placement of an LMA can be used as a temporizing measure. It is essential to realize that the LMA does not provide a secure airway and that it may permit aspiration of gastric or oral secretions. The lubricated LMA is placed by itself into the pharynx above the epiglottis and can be used for gentle (<20 cm H2O) positive-pressure ventilation. The deflated mask is manually inserted into the patient's mouth and guided blindly along the hard palate. It is advanced until resistance is encountered (the distal tip of the LMA rests against the upper esophageal sphincter at this point).
REF: pp. 224-225 a. To prevent unnecessary pressure from being exerted on the occiput b. To enable the clinician to more easily move the patient’s tongue to the left c. To obtain a better alignment and visualization of the airway d. To assist in maintaining the patency of the upper airway
7. What is the purpose of placing a small towel under the occiput of a 4-year-old patient who is undergoing oral intubation?
ANS: C
The occiput of babies and infants is larger than that of older children. A small roll placed under the shoulders of these younger patients facilitates view of the vocal cord during laryngoscopy. Direct laryngoscopy may be facilitated by placing a roll under the shoulders of any patient lying on a soft mattress.
REF: p. 226 a. A b. B c. C d. D
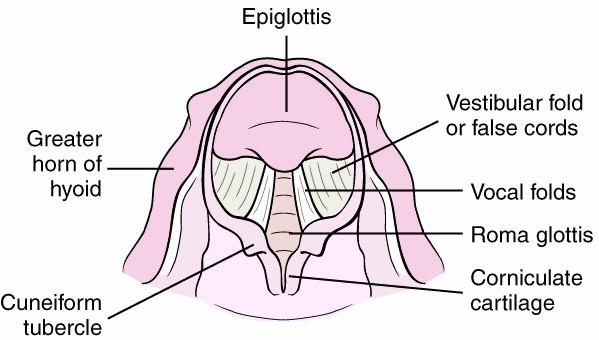
8. Which of the following labeled structures identifies the vocal cords?
ANS: C
In the illustration depicting the glottis and surrounding structures, A indicates the aryepiglottic folds; B indicates the epiglottis; C refers to the vocal cords; and D represents the corniculate cartilage. The dark center of the illustration depicts the glottis, or rima glottidis.
REF: p. 226 a. Just when the Murphy eye clears the vocal cords and enters the trachea b. At the location where the second double-ring mark just passes the glottis c. At the point where the first heavy black line just moves beyond the glottis d. Just after the distal third of the tube passes into the trachea past the glottis
9. How should the therapist determine the depth of insertion of an endotracheal tube marked with three rings in an infant during the intubation procedure?
ANS: B
The tip of the ETT is advanced through the glottic opening so that the single black ring is just distal to the opening of the glottis. If the ETT is marked with three rings, the ETT should be inserted until the double black ring is distal to the glottic opening.
REF: p. 226 a. Presence of end tidal CO2 one breath after intubation b. Pulse oximetry > 88% c. Presence of end tidal CO2 five breaths after intubation d. Presence of vapor in the ETT
10. How should the therapist confirm proper placement of an endotracheal tube?
ANS: C
The presence of vapor in the ETT is not an accurate test for proper ETT placement. Proper endotracheal, and not esophageal, placement of the endotracheal tube is confirmed with sustained presence of end tidal CO2. Capnography via a monitor is preferred over a single-use end tidal device (Pedi-Cap; Nellcor, Boulder, Colorado). End tidal CO2 should be monitored for at least five breaths after intubation. Even endotracheal tubes placed in the esophagus may have transient detection of CO2 due to the presence of CO2 in the stomach (which can occur due to bag-mask ventilations).
REF: p. 226 a. 8 cm at the lip b. 9 cm at the lip c. 10 cm at the lip d. 12 cm at the lip
11. Where should the therapist secure a 4.0-mm endotracheal tube after the intubation procedure?
ANS: D
The proper depth of the endotracheal tube can be estimated based on the size of the endotracheal tube used. Multiply the internal diameter of the endotracheal tube by three and tape the ETT at that centimeter mark at the lip (e.g., a 4.0-mm ETT should be taped at 12 cm at the lip). The proper length of the endotracheal tube can be estimated in premature infants according to their weight: add 6 to their weight in kg (e.g., in a 1-kg baby the ETT should be taped at 7). This formula cannot be used in children weighing more than 3 kg.
REF: p. 226 a. Advance the ETT until breath sounds are not heard over the stomach. b. Pull the ETT at least 4 cm until breath sounds are not heard over the stomach. c. Leave it in place because breath sounds over the stomach are simply transmitted from the lungs. d. Pull the ETT because it is most probably in the esophagus.
12. The therapist is trying to confirm the proper placement of an endotracheal tube of an infant. Auscultation reveals breath sounds over both the stomach and the chest wall. What should the therapist do?
ANS: D
The chest is auscultated after intubation as a method for assessing whether the ETT is in the trachea. Breath sounds should be heard bilaterally over the lateral chest wall. If breath sounds are auscultated over both the stomach and the chest wall, the ETT is in the esophagus and should be pulled. It should be noted that auscultation is not the most accurate method of assessing proper ETT placement.
REF: p. 226
13. Which of the following conditions are considered contraindications for nasotracheal intubation?
I. Bleeding diathesis
II. Facial trauma
III. Temporal skull fractureIV. Choanal atresia a. I and II only b. I, II, and IV only c. I, III, and IV only d. II, III, and IV only
ANS: B
The major contraindications to nasotracheal intubation are a bleeding diathesis, such as thrombocytopenia, abnormal clotting times, facial trauma, suspected basilar skull fracture, and abnormal anatomy such as choanal atresia.
REF: p. 228 b. The upper airway in the laryngeal area is smaller in an infant. c. The cricoid cartilage in an infant acts as a partial airway obstruction. d. The upper airway structures in an infant are more pliable and compliant.
14. Which of the following anatomic differences between the larynx of an infant and that of an adult makes blind nasal intubation of the infant more difficult? a. The larynx of an infant is more cephalad and anterior.
ANS: A
The larynx of an infant or small child is anterior and cephalad, making intubation more difficult in general. This anatomic difference between adults and children makes attempts at blind nasal intubation almost uniformly unsuccessful. Wisdom dictates that attempts at a blind nasal intubation be vigorously discouraged because of the potential for damaging the airway. Mechanically generated damage and subsequent bleeding would make further intervention and attempts at intubation more difficult and dangerous.
REF: p. 228 a. Postextubation atelectasis among very low–birth weight infants b. Pressure necrosis of the nares c. Deformation of the nasal turbinates d. Olfactory nerve damage
15. Which of the following conditions is considered a disadvantage of nasotracheal intubation in neonates?
ANS: B
Disadvantages to nasal intubation include a predisposition to sinusitis, pressure necrosis of the nares, and bleeding complications associated with passing the ETT through the nares and upper airway.
REF: p. 228 a. Nasotracheal intubation b. Routine orotracheal intubation c. Fiberoptic laryngoscopy d. Finger intubation of the trachea
16. Which of the following techniques should be considered when intubating neonates with Pierre Robin syndrome?
ANS: C
Children with craniofacial syndromes (e.g., Treacher Collins syndrome or Pierre Robin syndrome) are assumed to have a difficult airway, even if they have undergone jaw advancement. Acquired causes of a difficult airway include limited mouth opening due to decreased temporomandibular joint mobility (as may occur in rheumatoid arthritis or muscular dystrophy), orofacial trauma, trauma to the neck, hematoma of the neck, and infections either of the anterior neck or the epiglottis. Patients with a history of burns or radiation to the face or neck are very difficult to intubate. The clinician should always have additional options available to secure the airway in the event that orotracheal intubation is not successful. An LMA should be readily available during intubation attempts. The Glidescope is a fiberoptic laryngoscope that greatly facilitates intubation of patients with a difficult airway. It is best to learn how to use the Glidescope on patients with a normal airway prior to using this device on patients with an abnormal airway.
REF: p. 228 b. A tracheotomy needs to be performed in the emergency department. c. The child is in urgent need of transport to the operating room to be intubated. d. Nebulized 2.2% racemic epinephrine needs to be given via face mask every 10 minutes.
17. A 5-year-old child is brought to the emergency department in severe respiratory distress with a diagnosis of epiglottitis. What measures must be performed to secure the child’s airway? a. The child should be immediately intubated orally in the emergency department.
ANS: C
The child with clinical manifestations of epiglottitis (drooling, stridor, and respiratory distress) should not undergo a visual examination in the emergency department. The child should not be stimulated and should be kept as calm as possible. If the patient is stable, a soft tissue lateral neck radiograph (refer to Figure 13-8 in the textbook) can be performed. Radiologic findings include thickening of the epiglottis and aryepiglottic folds and the classic "thumbprint" sign. If the patient is not stable or if the diagnosis of epiglottitis has been made, the patient should be immediately transported to the operating room to be managed by an ENT surgeon and an anesthesiologist.
REF: pp. 228-229 a. The therapist should recommend that a tracheotomy be performed. b. The therapist needs to insert an oral ETT smaller than the one in place. c. The therapist must insert an oral ETT large enough to stop the leak. d. The therapist should do nothing because this situation is acceptable for this type of patient.
18. A child orally intubated because of laryngotracheal stenosis has an air leak at 25 cm H2O. What action does the therapist take now?
ANS: B
Children with laryngotracheal stenosis who do not have a tracheotomy may require intubation. The severity of the stenosis may dictate the approach used to access the airway. Plain magnified soft tissue radiographs may show subglottic narrowing or long-segment tracheal stenosis. In cases of mild subglottic stenosis, the patient may be intubated orally, but it would be essential to start with an endotracheal tube size at least one smaller than the ageappropriate tube, and air leakage must be checked. A leak between 10 and 20 cm H2O during the time of intubation is necessary so that further damage is not incurred. If the air leak is greater than 20 cm H2O, a smaller tube should be placed. In cases of severe laryngotracheal stenosis, an LMA may be used, or occasionally an emergency tracheotomy may be performed as an alternative.
REF: p. 229
19. The therapist is measuring the intracuff pressure of a pediatric ETT. Where should the pressure be maintained to avoid complications? a. 5 to 10 cm H2O b. 10 to 20 cm H2O c. 20 to 25 cm H2O d. Not greater than 30 cm H2O
ANS: C
Positive pressure applied through the ETT should produce an audible escape of air, or leak, at less than or equal to 20 cm H2O. The larynx should be auscultated to confirm the leak. Intracuff pressures are maintained at less than 20 to 25 cm H2O because higher pressures are associated with ischemia and necrosis of the tracheal mucosa and can lead to tracheal stenosis.
REF: p. 229 a. An oxygen saturation > 95% b. A respiratory rate < 35 breaths per minute c. A cuff leak < 25 cm H2O d. A successful spontaneous breathing trial
20. What is considered the best predictor of a successful extubation?
ANS: D
The best predictor of successful extubation is a successful spontaneous breathing trial. Successful extubation appears to be inversely related to the duration of the intubation period.
REF: p. 230
21. Prolonged exposure to increased tracheostomy cuff pressure may cause which of the following disorders? a. Tracheomegaly b. Tracheomalacia c. Tracheal granulomatosis d. Tracheal bleeding
ANS: A
Prolonged exposure to increased pressure can lead to tracheal dilation, or tracheomegaly. Careful management of the tube size and cuff may prevent this complication. Cuff pressure should be checked regularly and adjusted as needed.
REF: p. 233 a. Between the second and fourth tracheal rings b. Between the fourth and fifth tracheal rings c. Between the cricoid and the thyroid cartilage d. Between the first and second tracheal rings
22. Where is the tracheostomy tube usually placed in children?
ANS: A
The tracheotomy tube is usually placed between the second and fourth tracheal rings, depending on ease of exposure and size of the trachea and tube to be placed.
REF: p. 233 a. Hemorrhage b. Sepsis/infection c. Significant leaks d. Mucous plugging
23. What are the most common causes of death in tracheotomy-dependent children?
ANS: D
The two most common reasons for death of a tracheotomy-dependent child include plugging of the tube with mucus and accidental decannulation. Plugging with mucus occurs when thick, viscous mucus obstructs the lumen of the tracheotomy tube. Several factors that lead to this problem include dehydration, infection, and lack of humidity.
REF: p. 235
24. Ideally, how many hours after last feeding should a therapist consider before changing a tracheostomy tube to minimize the risk of vomiting and aspiration? a. At least 2 hours b. At least 4 hours c. At least 6 hours d. At least 12 hours
ANS: A
Ideally, at least 2 hours should have passed after the last feeding before the tracheostomy tube is changed to minimize the risk of vomiting or aspiration during the tracheostomy tube change.
REF: p. 237
25. What conditions should be met before considering decannulation?
I. Original indication for tracheostomy has resolved
II. Tolerance of a Passey-Muir valve most of the day
III. No need for suctioning
IV. Absence of fever a. I, II, and III only b. I and III only c. III and IV only d. I, II, III, and IV
ANS: A
A patient may be considered for decannulation or removal of the tracheostomy when the following conditions have been met: The original indication for the tracheostomy tube has resolved or been corrected. The patient should be either tolerating a cap during most or all of their waking hours or tolerating a Passey-Muir valve most of the day. The patient should not require removal of either for suctioning or respiratory complaints. If these conditions have not been met, the patient should at a minimum tolerate downsizing of their tracheostomy tube.
REF: p. 237
Chapter 14: Surfactant Replacement Test Bank
Multiple Choice
1. According to Laplace’s law the pressure required to open an alveoli in the lung is: a. Directly proportional to the radius b. Inversely proportional to the length of the airway c. Directly proportional to the surface tension d. Indirectly proportional to the viscosity of the gas in the airway
ANS: C
In his theory of capillary action Laplace described the relationship of trans-surface pressure and surface tension at a gas–fluid interface in a sphere as P = 2 ST/R (where P is the transsurface or distending pressure, ST is surface tension, and R is the radius of the sphere).
REF: pp. 245-246 a. Large alveoli would empty into smaller ones at the end of exhalation. b. Every exhalation would demand ventilatory muscle activity. c. Every breath would require a considerable amount of pressure to expand the lung with each inspiration. d. Some alveoli would collapse during exhalation.
2. Which of the following physiologic consequences would develop if the liquid–gas interface were without surfactant?
ANS: C
The lung can be thought of as a large number of interconnected bubbles that form the interface between the gaseous environment and the wet alveolar surface. If this interface were devoid of surfactant, two consequences would ensue: (1) every breath would take a considerable amount of pressure to expand the lung, comparable to the 80 to 90 cm H2O of pressure required for a newborn’s first breath, and (2) the lung would rapidly collapse during exhalation.
REF: p. 246 a. Pulmonary compliance decreases. b. Uniform gas distribution during expiration occurs. c. The functional residual capacity is maintained. d. Pulmonary perfusion matches alveolar ventilation.
3. Which of the following physiologic conditions result from the presence of normal amounts of pulmonary surfactant in the lung?
ANS: C
Functionally, surfactant increases lung compliance, promotes homogeneous gas distribution during inhalation, and allows a residual volume of gas to be evenly distributed throughout the lung during exhalation that is, it maintains functional residual capacity. In the absence of surfactant, distribution of ventilation becomes uneven, the lungs become stiff, and atelectasis ensues during exhalation. The result is increased work of breathing, hypoxia, and respiratory failure, the clinical picture exemplified by preterm infants with respiratory distress syndrome (RDS). Surfactant functions are summarized in Box 14-1 in the textbook.
REF: pp. 246-247
4. Which of the following is the most important component of pulmonary surfactant?
I. Dipalmitoyl phosphatidylcholine
II. Phosphatidylglycerine
III. PhosphatidylinositolIV. Sphingomyelin a. I only b. I and IV only c. I, II, and IV only d. II, III, and IV only
ANS: A
Surfactant composition is fairly constant among mammalian species. Surfactant is composed of approximately 90% lipids (of which 80% to 85% are phospholipids) and approximately 10% proteins (see Table 14-1 in the textbook). Phosphatidylcholine (PC) is the most abundant phospholipid (75% to 80%) and is mostly saturated (40% to 55%) in the form of dipalmitoyl phosphatidylcholine (DPPC). DPPC is the most important surfactant component in reducing surface tension; it consists of two molecules of palmitic acid and one molecule of phosphatidylcholine attached to a glycerol backbone. DPPC has a hydrophobic end (fatty acids) and a hydrophilic end (nitrogenous base) and aligns itself in the air–liquid interface with the hydrophobic end toward the gas phase and the hydrophilic end toward the liquid phase.
REF: pp. 247-248
5. What is the role of SP-D in human pulmonary surfactant?
I. Suppresses proinflammatory responses
II. Enhances phagocytosis
III. Enhances killing of microbesIV. Functions as an opsonin for bacteria a. II and III only b. III and IV only c. I, II, and III only d. I, III, and IV only
ANS: C
SP-D is also a collectin and enhances binding, phagocytosis, and killing of microbes by alveolar macrophages. In addition, SP-D has a role in the suppression of proinflammatory responses. Lack of SP-D in transgenic mice leads to emphysema, macrophage activation, accumulation of oxygen-reactive species, and increased surfactant alveolar pools. SP-D also plays a key role in surfactant homeostasis.
REF: p. 250 a. Magnesium sulfate b. Terbutaline c. Systemic corticosteroids d. Lecithin
6. A pregnant woman believed to be at 26 weeks gestation has been admitted for premature labor. What should be administered to this woman to decrease the risk of RDS if the infant is delivered prematurely?
ANS: C
Antenatal steroids have been extensively studied and have been shown to decrease RDS in infants between 24 and 34 weeks of gestation. There is no increased infection risk with rupture of membranes including prolonged rupture of membranes or chorioamnionitis. A single course of corticosteroids is currently recommended by the American College of Obstetricians and Gynecologists (ACOG) for pregnant women between 24 weeks and 34 weeks of gestation who are at risk of preterm delivery within 7 days. This course may consist of betamethasone (2 doses, 24 hours apart) or dexamethasone (4 doses, 12 hours apart). A single rescue course may be considered if first course was given more than 2 weeks prior in women < 32 weeks’ gestation likely to deliver within the next week.
REF: p. 251 a. Phosphatidylglycerol (PG) and phosphatidylcholine (lecithin) increase while sphingomyelin decreases during gestation. b. PG increases and lecithin and sphingomyelin decrease during gestation. c. PG and lecithin decrease while sphingomyelin increases during gestation. d. PG and lecithin increase while sphingomyelin decreases during gestation.
7. Which of the following relationships is correct regarding the analysis of amniotic fluid to determine fetal lung maturity?
ANS: D
Measurement of phospholipids in the amniotic fluid can be used to determine fetal lung maturity because PG and phosphatidylcholine (lecithin) increase while sphingomyelin decreases during gestation.
REF: p. 251 a. Inactivation by proteins b. Altered surfactant metabolism c. Altered surfactant pool d. Altered surfactant composition
8. Which of the following is the most common form of surfactant abnormality associated with acute lung injury?
ANS: A
Inactivation by proteins is the most common surfactant abnormality seen in acute lung injury. These proteins competitively displace surfactant phospholipids from the alveolar monolayer and are less surface-active molecules than surfactant. Consequently, the result is a decreased capacity for reducing surface tension.
REF: p. 252
9. What appears to be the benefit of administering prophylactic surfactant replacement therapy to preterm infants?
I. Decreased risk of mortality
II. Reduced threat of pneumothorax
III. Decreased incidence of diaphragmatic hernia
IV. Reduced risk of developing pulmonary interstitial emphysemaa. I and II only b. II and IV only c. I, II, and IV only d. II, III, and IV only
ANS: C
Prophylactic surfactant is administered after initial stabilization in the first 15 minutes after birth, compared with 1.5 to 7.4 hours in rescue strategies. Initial studies comparing prophylactic to rescue surfactant favored the former, with noted decrease in mortality, pneumothorax, and pulmonary interstitial emphysema.
REF: p. 254 a. Synthetic surfactants contain exclusively SP-A, SP-B, SP-C, and SP-D. b. Synthetic surfactants contain only SP-A. c. Bovine surfactants contain SP-B and SP-C, and synthetic surfactants contain SP-A and SP-D. d. Bovine surfactants contain SP-A and SP-D, and synthetic surfactants contain SP-B and SP-C.
10. How do synthetic surfactants compare with bovine surfactants?
ANS: C
The bovine surfactants contain SP-B and SP-C, but not SP-A. Infasurf contains much more SP-B and SP-C than does Survanta. The synthetic surfactants contain no proteins.
REF: p. 256 a. Pause the procedure and administer PPV until vital signs are stable. b. Rapidly infuse the rest of the dose and reconnect the patient to the mechanical ventilator. c. Extubate the patient and administer nasal CPAP until stable. d. Continue administration of the surfactant while administering PPV.
11. The respiratory therapist administering surfactant to a premature newborn notices a significant deterioration in vital signs. What should be done at this time?
ANS: A
Surfactant delivery should be paused until vital signs recover and ETT clears of visible surfactant. Infant may need to be repositioned prone and positive pressure ventilation increased for lung inflation.
REF: p. 256 a. 1-antitrypsin deficiency b. Vitamin B deficiency c. SP-A deficiency d. SP-D deficiency
12. A full-term infant received surfactant as rescue therapy for RDS. Despite redosing, the infant has not been able to be extubated during the first 2 weeks of life. What should this neonate be evaluated for?
ANS: A
Full-term infants with RDS, surfactant nonresponders, and infants who cannot be extubated in the first weeks of life because of a respiratory condition should be evaluated for SP-B deficiency, alveolar capillary dysplasia, and 1-antitrypsin deficiency.
REF: p. 258
13. Which of the following clinical conditions should be suspected in a neonate unresponsive to surfactant due to its inactivation? a. Pulmonary hypertension b. Pulmonary hemorrhage c. Pneumonia d. Methemoglobinemia
ANS: B
Blood is a strong inactivator of surfactant, with several of its components such as hemoglobin, fibrin, fibrinogen, red blood cell membrane lipids, immunoglobulins, and plasma proteins contributing to this process. Inactivation can occur as a result of pulmonary hemorrhage, hemorrhagic edema, or blood aspiration during birth or trauma.
REF: p. 258 a. Switch to a pressure-limited mode b. High-frequency chest oscillation c. ECMO d. Administer surfactant
14. A term baby with meconium aspiration syndrome is receiving mechanical ventilation per protocol. On the third day, the therapist observes that the FiO2 requirement is increasing and both lung compliance and oxygenation index are worsening. What should be suggested at this time?
ANS: D
A meta-analysis confirmed that surfactant replacement for MAS decreases the need for ECMO with a number needed to treat of 6.
REF: p. 258
Chapter 15: Non-invasive Mechanical Ventilation and Continuous Positive Pressure of the Neonate Test Bank
Multiple Choice
1. Which of the following therapeutic interventions would be appropriate for a neonate with a respiratory rate of 65 breaths/minute while displaying paradoxical chest wall movement with suprasternal and substernal retractions, grunting, nasal flaring, and cyanosis, along with the following blood gas data: pH 7.30; arterial partial pressure of carbon dioxide (PaCO2), 50 mm Hg; arterial partial pressure of oxygen (PaO2), 60 mm Hg? a. Intubation and mechanical ventilation b. High flow nasal cannula c. Extracorporeal membrane oxygenation d. Continuous positive airway pressure (CPAP)
ANS: D
According to American Association for Respiratory Care (AARC) clinical practice guidelines, neonates presenting with a respiratory rate greater than 30% of normal and paradoxical chest wall movement with suprasternal and substernal retractions, grunting, nasal flaring, and cyanosis should be considered for placement on CPAP as long as they are able to demonstrate adequate ventilation as defined by PaCO2 less than 60 mm Hg and pH greater than 7.25.
REF: pp. 269-270
2. Which of the following conditions are contraindications for nasal CPAP?
I. Pneumonia
II. Tracheoesophageal fistula
III. Choanal atresia
IV. Atelectasis a. I and II only b. II and III only c. III and IV only d. I, II, and III only
ANS: B
Infants with persistent apneic episodes who are unable to maintain PaCO2 less than 60 mm Hg and pH greater than 7.25 should not be given CPAP. If they are already receiving CPAP, mechanical ventilation is indicated. Infants with congenital anomalies such as choanal atresia, cleft palate, tracheoesophageal fistula, or preoperative diaphragmatic hernia should not receive CPAP. CPAP is contraindicated in infants with neural muscular disorders, infants receiving CNS depressants, and infants with central apnea or frequent apneic episodes resulting in desaturation and/or bradycardia. In addition, severe cardiorespiratory instability and poor respiratory drive is also a contraindication to the initiation of CPAP.
REF: p. 270 a. Pulmonary hypertension b. Pneumothorax c. Atelectasis d. Diaphragmatic hernia
3. Which of the following complications of CPAP can develop when an infant experiences inadvertent positive end-expiratory pressure (PEEP) from gas trapping resulting from tachypnea?
ANS: B
CPAP is associated with some of the same hazards and complications that are frequently associated with mechanical ventilation. Pneumothorax is a complication occasionally reported in infants receiving CPAP. This is a result of inadvertent positive end-expiratory pressure related to gas trapping when infants are tachypneic and do not have a sufficient expiratory time. This may also occur after surfactant replacement therapy, when pulmonary compliance improves and the infant has not been weaned appropriately and, thus, is exposed to excessive airway and hence alveolar pressure.
REF: p. 270
4. What is considered the most effective interface option for delivering CPAP to infants? a. Binasal prongs b. Nasal mask c. Nasal pillows d. Oronasal mask
ANS: A
Today, CPAP is most often administered through short binasal prongs, and this method is considered the most effective interface option for delivering CPAP to infants.
REF: p. 271 a. B-CPAP b. IF-CPAP c. Single probe CPAP d. V-CPAP
5. A preterm infant in respiratory distress is a candidate for CPAP. To minimize the work of breathing, which device should be used?
ANS: B
IF-CPAP has been shown to significantly reduce inspiratory WOB in preterm infants.
REF: p. 272
6. Which of the following features are often components of CPAP systems incorporated within infant ventilators?
I. Highly responsive demand flow systems
II. Apnea backup breaths
III. FiO2 compensation mechanisms IV. Leak compensation capabilities a. I and II only b. II and III only c. III and IV only d. I, II, and IV only
ANS: D
Today, a number of commercially available microprocessor-controlled infant ventilators allow non-invasive application of V-CPAP. In these systems CPAP is maintained with a variable demand–flow system. Flow rate and airway pressure are regulated by servo-controlling the aperture size of the exhalation valve. These ventilators also include the following: (1) highly responsive demand flow systems, (2) leak compensation, (3) airway graphics monitoring, and (4) apnea backup breaths.
REF: p. 273 a. The therapist dials the desired CPAP level directly on the ventilator. b. The therapist immerses the distal end of the expiratory limb a certain distance below the water surface. c. The CPAP level is established by stacking adaptors with weighted balls to the distal opening of the expiratory limb. d. The positive pressure is achieved by tightening a screw clamp attached to the expiratory limb until the desired pressure is achieved.
7. How is the positive pressure level established in a bubble CPAP system?
ANS: B
A measuring tape is attached to the outside of the water column. The CPAP level is maintained by submerging the distal end of the expiratory circuit straight down into the fluid from the surface of the water line to a measured depth in centimeters, thus creating the amount of CPAP in centimeters of water. If a higher level of CPAP is needed, the tube can be advanced farther down into the fluid column.
REF: p. 273
8. In order to rinse the system of exhaled CO2 and meet the inspiratory flow rate requirements of infants placed on B-CPAP, the flow rate of humidified gas should be set at: a. 6 to10 L/minute b. 11 to 15 L/minute c. 16 to 20 L/minute d. at least 15 L/minute
ANS: A
The flow rate of humidified gas (6 to10 L/min) is set to meet the inspiratory flow rate requirements of the patient, maintain the CPAP level, and rinse the system of exhaled carbon dioxide.
REF: p. 273 a. The amount of CPAP is excessive for this age group. b. The flow rate is very high and the CPAP measured at the nasal prongs is probably > 4 cm H2O. c. The cannula is probably too large for the infant and causes inadvertent CPAP. d. The chest X-ray finding is consistent with the amount of CPAP set at the water chamber.
9. A bubble CPAP has been set up on an infant at 12 L/min and the water column is reading 4 cm H2O. A chest X-ray reveals mild lung overdistention. What is the most feasible explanation for this finding?
ANS: B
The pressure measured at the nasal prong could be slightly higher than the submersion depth of the expiratory tubing below the water surface when higher flow rates are used; therefore, airway pressure should always be monitored at the nasal prong to ensure proper CPAP levels.
REF: p. 274 a. Anywhere along the exhalation limb b. Anywhere along the inspiratory limb c. Inside the ventilator d. As close to the patient’s airway as possible
10. Where in the CPAP delivery system should the pressure-relief/pop-off valve be placed to detect circuit occlusion?
ANS: D
A high-pressure pop-off can be placed as close to the patient as possible should the expiratory limb become occluded.
REF: p. 274 a. IF-CPAP (infant flow CPAP) b. MV-CPAP (mechanical ventilator CPAP) c. B-CPAP (bubble CPAP) d. V-CPAP (ventilator-derived CPAP)
11. Which form of CPAP has been associated with a “thoracic wiggle”?
ANS: C
Subjective accounts of a visible “thoracic wiggle” from bubbles are often reported by clinicians caring for infants receiving B-CPAP. The use of higher flows can result in more vigorous bubbling and higher pressure fluctuations in the delivery system. However, higher flows do not appear to improve gas exchange.
REF: p. 274 a. B-CPAP b. MV-CPAP c. V-CPAP d. IF-CPAP
12. Which of the following CPAP systems delivers a more consistent pressure, lowers work of breathing (WOB), is less sensitive to leaks, and is more effective at alveolar recruitment compared with other forms of CPAP?
ANS: D
The IF-CPAP system has been shown to deliver a more consistent pressure, to lower WOB, to be less sensitive to leaks, and to be more effective at alveolar recruitment compared with other forms of CPAP.
REF: p. 275 a. Tragus b. Philtrum c. Sphenoid axis d. Lower lip
13. Which of the following anatomic structures should be closely evaluated when using nasal masks in the administration of IF-CPAP?
ANS: B
Nasal prongs have been shown to result in nasal and septal wall skin breakdown, whereas nasal masks have been associated with breakdown low on the septum or at the base of the philtrum.
REF: pp. 275-276
14. When nasal cannulas are used in infants at high flows, which factors determine the amount of pressure to the airways?
I. Flow rate
II. Size of the leak around the cannula
III. Degree of the mouth opening
IV. FiO2 a. I and II only b. III and IV only c. II, III, and IV only d. I, II, and III only
ANS: D
When the pressures delivered with this technique measured are highly variable, depend on the flow rate, the size of leak around the cannula, and the degree of mouth opening.
REF: p. 276
15. Which of the following outcomes are advantages of CPAP over mechanical ventilation in infants?
I. Lower risk of sepsis
II. Lower incidence of lung injury
III. Fewer cases of chronic lung diseaseIV. Lower incidence of renal failure a. I and III only b. II and IV only c. I, II, and III only d. II, III, and IV only
ANS: C
Mechanical ventilation in preterm infants is associated with increased risk of sepsis, lung injury, arrested lung development, and chronic lung disease.
REF: p. 276 b. The CPAP level was not raised enough. c. The CPAP level was raised too high. d. A problem with the interface has likely developed.
16. After increasing the level of CPAP delivered to an infant, the therapist notices that the neonate’s PaCO2 rises and the PaO2 falls. What may have caused this situation? a. The FiO2 was not increased sufficiently.
ANS: C
A rise in PaCO2 or fall in PaO2 soon after the CPAP pressure has been increased may indicate that the optimal CPAP level has been exceeded. An increase in mean airway pressure can result in increased alveolar dead space because of mechanical compression of the pulmonary microvasculature. If gas exchange worsens in a patient who appeared to be improving, the CPAP pressure can first be reduced. If the patient’s situation does not improve, endotracheal intubation and mechanical ventilation may be indicated.
REF: pp. 277-278 a. The FiO2 was not increased sufficiently. b. The CPAP level was not raised enough. c. The flow through the CPAP system is too low. d. A problem with the interface has likely developed.
17. After initiating B-CPAP in an infant at 6 cm H2O, the therapist notices that, although “bubbling” is present, the pressure in the manometer fluctuates between 2 and 5 cm H2O. What may have caused this situation?
ANS: C
Small fluctuations in pressure are common because of the frequency and amplitude of the bubbles; however, if large fluctuations are noted and coincide with the inspiratory phase of the infant, additional flow should be added to the system.
REF: pp. 278-279 a. Correct the leak by placing a chin trap. b. Change to a smaller cannula. c. Increase the flow through the CPAP system. d. Change the flow generator.
18. After initiating IF-CPAP in an infant at 8 cm H2O, the therapist notices a low-pressure alarm. What should be done to correct this situation?
ANS: A
In the IF-CPAP and mechanical ventilator CPAP systems, low-pressure alarms usually indicate a leak caused by nasal prongs that are too small or an excessive oropharyngeal leak. The oropharynx acts as a safety valve, preventing excessive accumulation of pressure in the airway. Oropharyngeal leaks are more common when using CPAP levels exceeding 8 to 10 cm H2O. A chin strap or pacifier can be helpful at gently sealing the leak and reestablishing the CPAP level.
REF: p. 279 a. The prongs should occlude only 50% of the external nares diameter. b. The prongs should occlude at least 75% of the external nares diameter. c. The prongs should occlude 100% of the external nares diameter with minimal blanching. d. The prongs should occlude 100% of the external nares diameter without blanching.
19. How should a therapist determine the size of the nasal prongs to effectively administer CPAP to infants?
ANS: D
The prongs should fill the entire nares without blanching the external nares. Selecting prongs that are too small can result in increased resistance and WOB, prong displacement, and excessive leaks.
REF: p. 279




