
6 minute read
Robotic Technology Brings Greater Accuracy, Safety to Spine Surgery
Randi Minetor
John Pollina, Jr., MD, FACS
Advertisement
As recently as a few years ago, a patient who needed spinal surgery probably received the news with anxiety, fear, and dread. Would the procedure work, or would it make things worse? Patients wondered if they should simply accept the fact of their pain or disability and learn to live with it, rather than risk a surgery that could just as easily fail as succeed.
They had reason to be nervous. A 2010 study from the Global Burden of Disease determined that 60 to 80 percent of the world’s population suffers from low back pain at some point in their lives, with ten percent of patients experiencing continued pain for more than three months. A paper published in the British Journal of Pain in 2013 reviewed patient data and determined that as many as 46 percent of spinal
surgeries performed from 1998 to 2008 resulted in “failed back surgery syndrome,” or a lack of positive impact on the patient’s pain. This, combined with anecdotes from countless patients who had undergone surgery that did not help, made a recommendation of a spinal procedure a scary proposition indeed.
As surgeons became less reliant on X-rays and turned to more sophisticated imaging technology like computed tomography (CT), outcomes improved significantly—but once the patient and surgical team were in the operating room, the planned procedure relied entirely on the surgeon’s skill. “We had very limited technology available in the operating room to help either plan or perform the surgery,” said John Pollina, Jr., MD, FACS, director of comprehensive spine surgery and associate professor of surgery at University at Buffalo Neurosurgery, and director, spine, at the Advanced Orthopedic/Spine Center at Kaleida Health. “So it was done in a
freehand technique. This is where surgical skill comes in—you use the limited amount of information you have to perform the surgery. That was all we had available.”
Dr. Pollina specializes in treatment of disorders of the cervical, thoracic, and lumbar spine, including low back and neck pain, herniated disc, spinal stenosis, scoliosis, spinal instability, spinal tumor and infection, carpal and cubital tunnel syndrome, and intracranial pathology—a wide range of surgeries that have the ability to end pain and increase mobility. He also conducts research in motion sparing and preserving technology of the spine and spine surgery outcomes, fields he has pursued since his neurosurgical residency at UB in the 1990s.
So when he heard about the work of an Israeli company, Mazor Robotics, in the development of robotic technology for spine surgery, he moved quickly to get involved. “I was able to see its true potential from a vision standpoint,” he said. “I approached the company about being involved in its further development and advancement.”
No stranger to the field of spine surgery, Mazor received approval from the US Food and Drug Administration for the first robotic device for the spine, the Mazor SpineAssist robot, in 2004. Surgeons used this device to guide the placement of pedicle screws in the vertebrae, and to decrease the amount of X-ray radiation used during surgery to place the screws accurately. With nearly five million spinal surgeries performed around the world every year—1.34 million in the US alone, according to the market research firm Researchmoz—Mazor saw the opportunity to take its robotic technology to the next level.
But the company needed the expertise and insight of a top spine surgeon to perfect a robotic system with many additional capabilities, so Dr. Pollina invited the development team
into his operating room. “We would have all these Israeli engineers in the OR collecting information and data,” he said. “It was a collaborative effort—we worked on workflow as well
as technology.”
The result is the Mazor X Stealth EditionTM Robotic Guidance System for Spinal Surgery, which provides preoperative planning, precise intra-operative execution, and real-time visualization of the implant throughout the procedure.
“Robotic-assisted spine surgery creates a more reproduceable, more accurate and safer environment for the patient when we’re performing these surgeries,” said Dr. Pollina. “It has eliminated or reduced greatly the variability between surgeries and surgeons, so every patient who has the same problem will have the same outcome with the same surgery.”
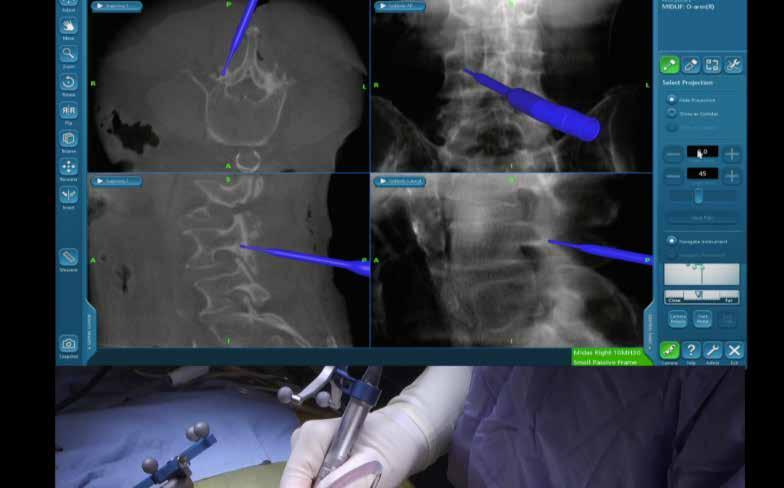
Familiar to spine surgeons worldwide, the well-established Mazor X platform uses a guidance system with a touchscreen workstation, a table-mounted robotic arm, a second control panel for the sterile area, and a navigation camera and instruments.
Central to its mission is its extensive surgical planning function, which “goes beyond individual pedicles to enable the benefits of an entire construct design,” according to the system’s website. The ability to plan the surgery in advance using the patient’s CT scan makes the surgery more accurate and effective in improving patient outcomes, said Dr. Pollina. “We can perform surgery in a much more reproduceable and reliable way that we have in the past,” he noted.
Accurate pre-planning means that incisions can be smaller, as the Mazor robotic system knows exactly where to make the incision to accomplish the surgery’s goal. “This means quicker recovery, shorter hospitalization, and fewer complications,” Dr. Pollina said.
Mazor’s Stealth navigation technology, embedded in the system, provides functions including customizable implant selection and 3D analytics, with precision registration to position screws, implants, and other surgical hardware at exactly the optimal angle. The bed-mounted robotic arm and the patient become fixated in a closed-loop system as the surgery begins, ensuring the accuracy of each step in the surgery.
“The robotic technology has created a situation in which the patient outcomes are improved because of improved accuracy and reproducibility,” said Dr. Pollina. “We know ahead of time what we want to do, and we instruct the robot to perform this, and it does it every time. You put the same data in, you get the same response out.”
The system can be used in all spinal surgery, he said. “Patients with degenerative spinal disease, scoliotic deformity, fractures, and tumors—this technology can be used for all of these patients. Whatever we operated on before, the robot can operate on now. It really crosses all boundaries.”
Dr. Pollina sees the future of robotic technology expanding to include even more procedures. “This is in the really early phase of its development—in the future, it will become a complete solution for patients’ spinal surgery. We’ll have preoperative implants that are unique to the patient.”
Implants to replace damaged or diseased bone are already produced using 3D printing technology, he noted, allowing the implant to be customized to the patient’s unique anatomy. As the robotic technology develops further, these implants will become even more precise as the system provides imaging and measurement to the printer. “For removing portions of the spine, the vision is for the robot to be involved in the preoperative planning, to execute from start to finish,” Dr. Pollina added. “So every aspect of spinal surgery will be part of that process.”
He continues to be involved in developing new capabilities for the Mazor X system, “We’re getting ready to launch technology to remove diseased parts of the spine with the robots,” he said. “That’s why I wanted to get involved. It’s really the next generation. It creates an extremely valuable tool.”










