
IN PARTNERSHIP WITH: TITLE SPONSOR:
& Ending
DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT
Understanding
Health Disparities
THE WASHINGTON INFORMER NEWSPAPER (ISSN#0741-9414) is pub lished weekly on each Thursday. Periodi cals postage paid at Washington, D.C. and additional mailing offices. News and ad vertising deadline is Monday prior to pub lication. Announcements must be received two weeks prior to event. Copyright 2016 by The Washington Informer. All rights reserved. POSTMASTER: Send change of addresses to The Washington Inform er, 3117 Martin Luther King, Jr. Ave., S.E. Washington, D.C. 20032. No part of this publication may be reproduced without written permission from the publisher. The Informer Newspaper cannot guarantee the return of photographs. Subscription rates are $55 per year, two years $70. Papers will be received not more than a week after pub lication. Make checks payable to:
THE WASHINGTON INFORMER 3117 Martin Luther King, Jr. Ave., S.E Washington, D.C. 20032 Phone: 202 561-4100 Fax: 202 574-3785 news@washingtoninformer.com www.washingtoninformer.com
PUBLISHER

Denise Rolark Barnes
STAFF
Ron Burke, Advertising/Marketing Director


Shevry Lassiter, Photo Editor
Lafayette Barnes, IV, Editor, WI Bridge DC
Jamila Bey, Digital Content Editor
Austin Cooper, Our House Editor
Desmond Barnes, Social Media Stategist
ZebraDesigns.net, Design & Layout

Mable Neville, Bookkeeper
Angie Johnson, Office Mgr./Circulation
Angel Johnson, Admin. Asst.
REPORTERS
Kayla Benjamin, (Environmental Justice Reporter) Stacy Brown (Senior Writer), Sam P.K. Collins, Curtis Knowles, Brenda Siler, Lindiwe Vilakazi, Sarafina Wright, James Wright

PHOTOGRAPHERS
Shevry Lassiter, Photo Editor, Roy Lewis, Jr., Robert R. Roberts, Anthony Tilghman, Abdula Konte, Ja’Mon Jackson
Disrupting Disparities by Shaking off Fears
 Dr. Shantella Y. Sherman WI Special Edition Editor
Dr. Shantella Y. Sherman WI Special Edition Editor
At the close of each year insurance companies and health care providers give patients an opportunity to change their coverage through “open enrollment.” Open enrollment coincides with the personal goals of many to improve their health by cutting out harmful habits and taking measure of their overall health through annual assessments and tests. Increasingly, this end-of-the-year ritual fosters a level of dread or anxiety for those who do not trust or feel intimidated by health systems. Many of the health dispar ities facing the African American community have roots in a distrust of physicians or the lack of quality care they believe they are receiving (real or perceived) based on race.
Much of this fear surrounding healthcare has been squarely documented across racial, ethnic, and socioeconomic lines. For instance, a 2017 Mayo Clinic report found that millions of Americans suffer through “hostage bargaining syndrome” in the company of doctors. Hostage bargaining syndrome is a form of fear and anxiety in the presence of healthcare professionals that leads patients to mask symptoms, attempt to ingratiate themselves to those who must care for them, or remain silent when they need assistance to avoid “bothering” or “upsetting” nursing or hospital staff.
One study respondent gave this example, which is considered a textbook example: “Immediately after undergoing major abdominal surgery, I overheard a nurse label me as “difficult” when I refused an attempted blood sample draw until I felt that my pain was more adequately controlled. I sat, wordless, as the surgical team she summoned interro gated me about my home pain regimen (there was none). I felt hopeless as they attributed my pain to an imagined tolerance to opioids. In that bed, in pain, I felt terribly, frighteningly vulnerable, dependent on strangers for my most basic needs in addition to their complex care. I felt powerless in a way that is impossible to imagine when one is in a privileged position of wholeness and well-being. I know this because after that comment, I pathetically tried to ingratiate myself to the care team,” the respondent noted. “I suppressed my fear and sadness, and attempted to make small talk with people who just moments earlier had made me feel belittled and somehow ashamed. I offered compliments and commiserated about burdensome charting responsibilities and unwieldy patient assignments. I believed that I needed to make them like me in order to receive their best care—in effect, to earn pain control through good behavior. I felt I had to prove to them that I was deserving.”
While the relationship between patient and physician requires open communication, it also demands an embrace of the Hippocratic oath to “do no harm,” as well as a bedside manner that recognizes that a person experiencing illness is vulnerable and weak.


Delia Lunger, a retired orthopedic surgeon said that she always found ways of making her patients feel com fortable and took extra time to ask about their sleeping habits, fears, and worries, to ensure they were comfortable enough to discuss their health in detail.
“We have other people’s lives in our hands and they are depending on us to not only do the job, but to be caring and loving in our engagements. With managed care, physicians are encouraged to see a set number of patients in a given time period; that is not always tenable,” Lunger said.
She said she often ran over scheduled appointments and worked into the late evenings to ensure every patient was seen and felt comfortable with the quality of care they received.
“When selecting a new physician, it is important to ask around about the doctor’s bedside manner – how much time do they spend with patients? Do they listen intently to the needs of the patient or are they overtalking them or assessing and writing prescriptions without a full picture? The other side of the coin, which is very important, is that patients must be open, honest, and persistent with having their health needs addressed. You cannot leave a physician’s office without a satisfactory treatment pro gram or care solution.”
This Washington Informer health supplement encour ages readers to find the help they need and address the fears they may have in seeking treatment. Being the best “you” possible requires taking charge and disrupting dis parities.
Read, Learn & Grow Dr. Shantella Sherman


HS-2 www.washingtoninformer.com / DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT
In Memoriam Dr. Calvin W. Rolark, Sr. Wilhelmina J. Rolark NEWSPAPER READING IS A HABIT DON’T BREAK THE HABIT! 202-561-4100 For advertising contact Ron Burke at rburke@washingtoninformer.com ...Informing you everyday in every way READ THE WASHINGTON INFORMER YOUR WAY: n In Print – feel the ink between your fingers of our Award Winning Print Edition n On the Web – www.washingtoninformer.com updated throughout the day, every day n On your tablet n On your smartphone n Facebook n Twitter n Weekly Email Blast – sign up at www.washingtoninformer.com
5 Dr. Shantella Sherman (Photo by India Kea)
African American Health Disparities
 By Lee Ross WI Staff Writer
By Lee Ross WI Staff Writer

One possible contributing factor: The Centers for Disease Control and Prevention (CDC) says African Americans are more likely to die at early ages for all causes, as young African Ameri cans are living with diseases that are typically more common at older ages for other races.

Black patients represent as much of a third of all patients in the U.S. receiv ing dialysis for kidney failure, though they don’t represent anywhere near that proportion of the U.S. popula tion, they added. Individuals who are black alone, the Office of Minority Health says, make up 12.7 percent of the U.S. population.
Another area of health care where there is disparity is renal dis ease. African Americans can suffer from kidney failure at as much as 3 times the rate of Caucasians, according to the National Kidney Foundation.

whites, affect African Americans at younger ages: unemployment, living in poverty, not owning a home, cost-prohibitive effects of trying to see an MD, smoking, inactive lifestyle, or obesity.

Diabetes is common in 10 percent of blacks aged 35-49 compared to 6 percent of whites.

Stroke is present in 0.7 percent of blacks aged 18-34 compared to 0.4 percent of whites the same age.
Stroke is common in 2 percent of African Amer icans compared to 1 percent of whites aged 35-49 and 7 percent vs. 4 percent , respectively, in those aged 50-64.
High blood pressure is common in 12 percent vs. 10 percent of blacks vs. whites aged 18-34 years, respectively. High blood pressure is common in 33 percent vs. 22 percent of those aged 35-49 years, respectively.

A white paper from Cigna went further, acknowl edging mental health disparities between African Americans and white patients. They noted blacks are 20 percent more likely to report psychologi cal distress and 50 percent less likely to receive counseling or mental health treatment due to the aforementioned underlying socioeconomic factors.

H-3 DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT / www.washingtoninformer.com HS-3
Learn more about our free online classes, cook-alongs and more at giantfood.com/healthyliving Scan the QR code to register! Join our Healthy Living Team for a free, virtual series that starts 2023 with your wellness goals in mind. Join online classes live or watch recorded sessions whenever works best for you! LEARN
• Organizing and Planning for the New Year • A Mindful Approach for the New Year • Healthy Habits to Support Fitness Goals • Food as Preventive Medicine • Expanding & Balancing your Plate HEALTHIER Together VIRTUAL
The series begins
ALL ABOUT...
S eries
the week of January 16!
ALANNAH, Nutritionist on the Healthy Living Team
Eugenia’s Story: Why Flu Vaccines are Important

Submitted by Amerigroup Maryland
It was the Holiday season and school was out, so Eugenia had the opportunity to visit and spend qual ity time with her grandchildren. Her youngest, who was five years old and on break from kindergarten, had what seemed to be a mild case of the sniffles, but she was Eugenia’s favorite and that was not going to stop her from hugging, snuggling and spend ing time together. Almost a week af ter that visit, Eugenia started to feel under the weather. She thought that she might have caught a bug that the kids brought home from school, but it wouldn’t be the first time and thought it would pass. Eugenia hadn’t gotten
around to getting her flu vaccine yet that year, and she had type 2 diabetes – a disease that is all too familiar to the Black community. As the days passed, it became obvious that Eugenia had the flu, and she was struggling to con trol her glucose levels. She knew how much insulin she was supposed to take as well as what she should and should not be eating, but she didn’t know that when a person is sick, their body man ufactures additional glucose to provide energy to fight infection, and that the body releases stress hormones that can reduce the effectiveness of insulin. After not being able to get her glu cose levels under control, Eugenia’s next visit was to a hospital. She ex perienced diabetic ketoacidosis, then pneumonia, then kidney failure and finally multiple organ failure. Eugenia didn’t make it home from the hospi tal, and her family was left wonder ing what if she had gotten vaccinated against the flu before visiting the kids? What if all the grandchildren and the entire family had been vaccinated against the flu?
Eugenia was one of 42.9 million people in the U.S. who caught the flu that year, and one of approximately 52,000 people who died. A dispropor tionate number of these deaths were among adults who were Black, and there could be a number of reasons for this disparity. Black adults have lower rates of immunizations against the flu than white adults. The CDC reports that less than 43 percent of Black men and women were vaccinated during the 2021-2022 flu season. Addition ally, people who have chronic disease are more likely to suffer complications, be hospitalized and die from the flu. Black adults have higher rates of heart disease and diabetes than their white counterparts, and during the 20212022 flu season, flu hospitalization rates were 80 percent higher among Black adults than white adults.
Many people miss opportunities to vaccinate, and many times it turns out to be regrettable, but misinformation and vaccine distrust should never be the reason a person loses their life to the flu. The flu vaccine has been prov en to be safe for most people over the age of six months. There are even safe alternatives for children and adults
with certain allergies and sensitivities. Flu vaccines are easily accessible via pharmacies, shopping super centers, at doctor’s offices and clinics, and they are available at no cost to people with health insurance. Most importantly, decisions to vaccinate should always be based on credible information: https:// www.cdc.gov/vaccinesafety/vaccines/ flu-vaccine.html.
Amerigroup Maryland is a huge supporter of flu vaccination and offers assistance to people who need help accessing vaccines or information. Amerigroup offers a website where members or guests can search for care providers who administer vaccines: https://findcare.amerigroup.com/ search-providers. Amerigroup also of fers its member help by phone: 1-800600-4441 (TTY 711). Additionally, Amerigroup members may be eligible for gift card rewards – just for getting vaccinated against the flu. To read more about Amerigroup Maryland’s Healthy Rewards, visit https://www. myamerigroup.com/md/benefits/ medicaid-healthchoice-benefits.html.
Thousands of lives can be saved if individuals and their families get vacci nated against the flu. Eugenia’s family will always wonder how things could have been different if their entire fam ily had been vaccinated. Take action today to catch up on your vaccines, so your family doesn’t have to experience the tragedy Eugenia’s did – or be left wondering.
AMERIGROUP MARYLAND UPDATES AND REMINDERS:

On January 1, 2023, Amerigroup Community Care, also known as Amerigroup Maryland, will begin operating as Wellpoint. There will be no change to members’ coverage as a result of this name change. Until Jan uary 1, 2023, members can continue to use their Amerigroup ID cards to access benefits as they always have.
Amerigroup members should expect to receive updated materials and more information about this change by ear ly December 2022. Learn more by visiting: https://www.myamerigroup. com/md/mdmd_caid_faqwellpoin trebrand.pdf. WI

HS-4 www.washingtoninformer.com / DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT PGANECDM12822012/801 8 YTT( 1444-006-00 7 )11 m /moc.puorgiremay m d D detacide y.htlaeh ruo D detacide y.ytinummoc tnemtrapeD.htlaeHH
Black Americans’ Views of Health Disparities Uncovered in Pew Research
By Lee Ross WI Staff Writer


In a recent study from Pew Re search, African Americans provided a mixed assessment of the progress that has been made improving health out comes for Black people. Roughly 47 percent said health outcomes for Black people have gotten better over the past 20 years, while 31 percent say they’ve stayed about the same and 20 percent think they’ve gotten worse.

Less access to quality medical care is the top reason Black Americans see contributing to generally worse health outcomes for Black people in the U.S. Large numbers also believe environmental quality problems in Black communities, and hospitals and medical centers giving lower priority to the well-being of Black people also play vital roles in health inequity.
“The pandemic has been a stark reminder of the disparate health out comes Black Americans face. It was essential for the survey to be able to speak to health and medical experi ences. The health and medical care system is one of the primary ways people encounter science in their daily lives,” said Cary Funk, director of the Pew Research Center’s science and society research. “There are ongoing efforts to address systematic bias in the medical care system, as well as ef forts to improve trust between Black Americans and the broader science, medical science, and public health communities. And while this research was in the works before the coronavi rus outbreak, the pandemic has been a stark reminder of the disparate health outcomes Black Americans face. It was essential for the survey to be able to speak to health and medical expe riences.”
Funk said that one of the chief aims of the study is to gain insight into the potential barriers and opportunities to deepen engagement with science among Black Americans. More im portantly, the research highlighted the impact of discrimination – real or perceived – in how African Americans sought care, from whom, and to what extent healthcare advice was followed.
The experiences of younger Black women in the medical system, for instance, showed that a large majority of Black women ages 18 to 49 report ed having experienced at least one of
seven negative health care experiences. They are also more likely than other Black adults to say they would prefer a Black health care provider for routine care and to say a Black doctor or other health care provider would do a better job than medical professionals of other races and ethnicities at providing them with quality medical care.

Such was the case with Charleesa Graham, 32, a graduate student liv ing in D.C.’s Petworth neighborhood, who recently relocated from Florida. After developing asthma while living near Coral Gables, she said she could not get a grasp on the condition or even a proper diagnosis because the physicians had such a poor bedside manner or treated her disrespectfully.
“The attitudes of the hospital work ers was very curt and direct, there was no compassion or empathy even though it was clear I was having trou ble breathing. They seemed more interested in whether I was taking il legal drugs,” Graham said. “I left the hospital and returned to my apart ment where a neighbor recognized my symptoms as a potential asthma attack and took me to a local botanica for an herbal tincture.”
Graham said since then, she choos es only doctors with cultural compe tencies of the Black community or naturopathic physicians who treat holistically. She said that while natu ral medicine is not for everyone, every person should feel comfortable in the care of the doctors who are paid to treat them.
The complexities of public trust were found to drive the breakdown in communication between health systems and physicians and the people they serve. Pew also found that Black Americans expressed a wariness about medical researchers’ trustworthiness when it comes to admitting their mistakes and taking responsibility for them when they happen – with 61 percent of Black adults noting that medical research misconduct is just as likely to occur today as it was in the past. With historical injustices including the Henrietta Lacks (HeLa cell) abuses and those of the Tuskegee Syphilis experiment ever-looming, Af rican Americans readily reject the idea that safeguards are in place today to prevent serious cases of research mis conduct.
“This is not about bad doctors; it
is about finding the right fit to ensure we get the best care possible. It is also important that Black people keep up with those preventative healthcare appointments and adhere to the com mon-sense guidelines that they are given. This cannot happen if we do not trust the doctors, or the doctors have a not-so-hidden bias.” Graham said. WI

H-5 DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT / www.washingtoninformer.com HS-5
MENTION THIS AD FOR 15% OFF YOUR FIRST PURCHASE! CurbsideGroceries.org FRESH PRODUCE. FRESHER PRICES. SHOP FOR YOUR GROCERY ESSENTIALS CLOSE TO HOME WEEKLY STOPS IN DC AND PRINCE GEORGE’S COUNTY
Funk said that one of the chief aims of the study is to gain insight into the potential barriers and opportunities to deepen engagement with science among Black Americans.
Recovery Is Possible
Submitted by DC Department of Behavioral Health (DBH)
Opioid-related overdose deaths in the District have risen steadi ly in recent years and the pan demic exacerbated the problem, with lockdowns initially making it harder to access addiction ser vices. In addition, a large portion of drugs — including heroin, co caine, MDMA and methamphet amine — are now being laced with fentanyl, a synthetic opioid that is 50 to 100 times more po tent than morphine.
Last year, there were 427 opi oid-related overdose deaths in the District. According to the Office of the Chief Medical Examiner, 95% of those deaths included the presence of fentanyl.
DC’s Department of Behavioral Health (DBH) and its communi ty partners have announced the continued expansion of its nal oxone distribution program and the launch of a new campaign to encourage treatment for those suf


fering from addiction. Both initia tives are part of LIVE.LONG.DC.










2.0, the District’s strategic plan to reduce opioid use, misuse, and re lated deaths.
DBH makes naloxone, a life-saving medication used to re verse an opioid-related overdose, widely available and easy to get for free, without a prescription or ID required in pharmacies and at community sites. The program has grown from a handful of ini tial distribution sites to nearly 40 pharmacy locations and over 120 community organizations in all eight Wards.
In addition, in 2020, DBH launched a unique naloxone dis tribution service. By texting the words LiveLongDC to 888-811, District residents get a message back with a link to a map of the locations where they can pick up naloxone. Recently, an option for free home delivery and mail deliv ery was added to the service.
“Naloxone should be near at hand like any lifesaving medica
tion. Family, friends, and others in the community can use naloxone to save someone who is overdos ing,” said Dr. Barbara J. Bazron, Director of the Department of Be havioral Health. “We want all Dis trict residents to be ready to save a life and carry naloxone.”
Recognizing that a substance use disorder is a disease and that users often must seek treatment multi ple times as part of their recovery journey, DBH has launched a new public education campaign de signed to encourage users to try again at treatment with the hope that “this time can be different.” The campaign highlights DBH’s comprehensive set of treatment supports, including:
• Free substance use disorder treatment, available seven days a week at sites across the District;
• Three medications (metha done, buprenorphine and naltrex one) proven effective at treating the disease of addiction;



• Enhanced care coordination so that individuals receive compre






hensive care;



• Peer counselors who have been there, and can support an individual through treatment and recovery; and




• Transportation, recovery housing and other support ser vices.

“We need DC residents with substance use disorders to know that DBH has the services and supports to help them succeed,” said Bazron. “We know that treat ment works, and recovery is pos sible.”
Information about the District’s recovery services is available online at MyRecoveryDC.org or by call ing the 24-hour Access Helpline at 1-888-793-4357 (7WE-HELP). WI
meth cocaine pills heroin
HS-6 www.washingtoninformer.com / DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT
LIVE
lives from the opioid epidemic
LONG DC Saving
Scan to find naloxone near you.




H-7 DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT / www.washingtoninformer.com HS-7 � Free substance use disorder treatment available 7 days a week � Three medications to help � Better coordinated treatment services � Peer counselors who have been there � Transportation, recovery housing, and more “This time, it’s different.” TREATMENT WORKS. RECOVERY IS POSSIBLE. When you are ready to try again, you can start right now Text READY to 888-811 for a list of treatment sites that are open. LIVE LONG DC Saving lives from the opioid epidemic
How to Make Eating More Dark Leafy Greens a Habit that Sticks!
 By Elaine Magee MPH, RD, Safeway Corporate Dietitian (@therecipedoctor and author of 25 books)
By Elaine Magee MPH, RD, Safeway Corporate Dietitian (@therecipedoctor and author of 25 books)
If someone were to ask me what’s one of the best food habits they could make…I would en courage them to enjoy dark leafy greens each and every day! Dark leafy greens are just one of those super food categories that nutri tionally cross all the “T” s and dot all the “I” s. As a group, these veg gies boost your intake of several powerful plant compounds with antioxidant and anti-inflammato ry action, and are also tops in vita min C and E, potassium, calcium, magnesium and of course, fiber.
the three “R” s: Reminders, Rep etition and Rewards.
As you are forming this new habit, you need reminders that you are committed to including them every day. Then to really solidify it as a habit, you need the repetition so eventually it’s some thing you just do without even thinking about it. And along the way you need plenty of rewards as you are building this new awe some habit. Rewards can be as simple as writing a checkmark on your calendar with a fun green pen or patting yourself on the back because your new habit is de creasing your risk of heart disease and some cancers, to noticing that your intestines seem happier. You might even observe you feel fuller
a serving of dark leafy greens ev ery day. Within several months, it became a habit that stuck. I approached it similarly to when I made flossing my teeth at night a habit (albeit several decades ago). My reminder back then was sim ply keeping a container of floss right near my sink where I got ready for bed every night. Eventu ally it was an automatic part of my routine and the floss could then move to the upper drawer where I kept the toothpaste. The rewards were the way my teeth and gums felt after flossing and of course the praise from my dental hygienist when she noticed a difference!
Here are some of my favorite tips to inspire you to make eating dark leafy greens a habit that sticks

refrigerator so you are reminded that they are there for you to use every time you open the refriger ator door.
A picture is worth a thousand words. Inspire yourself to include them in your meals by placing a beautiful picture of dark leafy greens in your kitchen where you can see it.
dark leafy greens to whatever egg dish I was making (from omelets to scrambled eggs and quiche!
It’s a wrap!
It all starts at the supermarket! You have to buy it first, to have it on hand in order to enjoy them each day (so focus first on grab bing them at the supermarket). I like to buy bags and clam shells of triple washed greens so they are su
Out of sight, out of mind when it comes to dark leafy greens, so keep them front and center in your

REPETITION
Challenge yourself and your family and think about some of your favorite weekly meals that you can easily add dark leafy greens to every time you make them. With this repetition, it will become a healthy habit. For me this started with egg dishes. We have eggs several times a week so I got in the habit of always adding

Each time you make a sand wich or wrap, include some kale, spinach, arugula, for example. It will add a burst of color and fresh flavor and texture to your wrap. You can even add sautéed greens to grilled cheeses and quesadillas. It only takes a couple of minutes to sauté them up with a drizzle of extra virgin olive oil, and a sprinkle of your favorite low sodium sea soning blend, before adding them in. I usually add a huge handful of greens per person I am cooking for (because they tend to shrink up when they cook).
Toss a salad.
Ready-to-grab bags or clam shells of triple washed dark leafy greens (like spinach, super greens, kale, arugula) make salads a quick fix for lunch or dinner. If you are using a thicker green (like kale) for your salad, soften it up just by massaging some extra virgin olive oil in with clean hands. You can also cut the kale into shreds and add it to coleslaw type dishes!
Elevate salad kits during the week for easy lunches or din ners using what you have on hand! I have gotten into a habit of grab bing a couple of salad kits each shopping trip as a fun fill-in for meals where I don’t have anything planned. These are my favorite ways to elevate salad kits:
• Add shredded Kale to Caesar Salad kits!
HS-8 / DECEMBER 2022 HEALTH WELLNESS
NUTRITION SUPPLEMENT
&
Ever since I wrote the book, FOOD SYNERGY (Rodale, 2008), I was determined to enjoy a serving of dark leafy greens every day. Within several months, it became a habit that stuck. CONTINUED ON PAGE HS-9
might want to avoid the stronger flavored greens like arugula and spring mix. You definitely want to keep your smoothie green not brown, so avoid adding anything red (and avoid berries) to your green smoothie. Think yellow like banana and mango!

Passionate about pesto!
Have you discovered pesto yet? It’s one of my favorite sauces and condiments and comes in handy not just with pasta but with piz zas and sandwiches/wraps, dips and as a condiment for eggs, meat, veggies, bread and potatoes! I like going 50/50 with fresh basil and a green like spinach, kale, arugula or beet greens when making my pe
Dark
Leafy Greens are Freezer Friendly.
One way to make sure you are setting yourself up for success to make enjoying eating dark leafy greens a habit that sticks is to al ways have them in your kitchen. That’s where the freezer comes in handy. I always have a bag of fro zen chopped spinach or kale in my freezer just in case. And if you are

leaving on a trip and you have some fresh dark leafy greens you want to save for later, don’t waste


H-9 DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT / www.washingtoninformer.com HS-9
GL00181271_SWY_1208_WashingtonInformer_HalfPg The pro in produce We pick and pack maximum freshness. shop now at Safeway.com
Caring for Your Mental Health
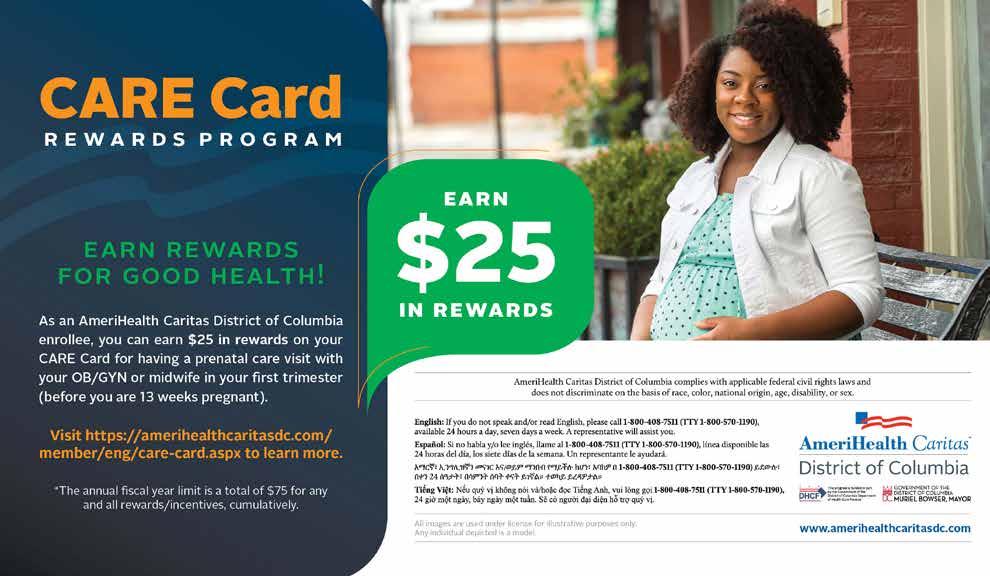
Submitted by AmeriHealth Caritas District of Columbia
THERE’S
A NEW NUMBER TO CALL WHEN YOU’RE EXPERIENCING
A MENTAL HEALTH CRISIS: 988.
If you or someone you love is experiencing a suicidal crisis or emotional distress, it can be diffi cult to know what to do. Before 2020, it was best to dial 911 for the help you needed. Today, you can call or text 988 at any time to access mental health services.
The 988 Suicide & Crisis Life line is nationwide. It provides services for those experienc ing thoughts of suicide, mental health–related distress, a substance

use crisis, or any other kind of emotional distress.1 Once you are on the line, a crisis counselor lis tens to you, works to understand how your problem is affecting you, provides support, and directs you to the best resources to help you address the problem. In addition, 988 is available if you are worried about a loved one who may need crisis support.
The counselors at the 988 Sui cide & Crisis Lifeline are trained and will use their expertise to sup port callers experiencing urgent mental health crises. Callers will be routed to the local Lifeline net work crisis center based on their area code.
HOW DOES 988 DIFFER FROM 911?
The mental health services pro vided when you call 988 will be different from those you will re ceive if you call 911.2 Dialing 988 offers easier access to crisis resourc es, as opposed to the public safety purposes of 911, which focuses on sending emergency medical services, the fire department, and police officers as needed. In ad dition, 911 responses to mental health emergencies have often led to harmful consequences for those
who simply needed mental health support.3 A small number of 988 Lifeline calls require 911-related services only when there is an im mediate risk to someone’s life that cannot be addressed during a 988 call.4
ADDITIONAL MENTAL HEALTH RESOURCES
In addition to the 988 Suicide & Crisis Lifeline, other options and resources are available:
• Department of Behavioral Health (DBH) Access HelpLine. The 24/7 HelpLine will connect you to services provided by a DBH-certified, community-based service provider and pair you with a case manager who can help coor dinate your care. You can contact the DBH Access HelpLine in two ways:

Call 1-888-793-4357. Visit https://dbh.dc.gov/ service/access-helpline.
• MyRecoveryDC. MyRecov eryDC is a District of Colum
bia Department of Health (DC Health) program. Many resourc es to help those starting recovery journeys are available at https:// myrecoverydc.org, including the following:
Stories of people who have faced addiction and whose experiences highlight their treat ment and recovery journeys Information on how treat ment and recovery processes work, why they work, and where to seek treatment and recovery services near you
Assistance finding a “peer.” Peers are people who have lived through addiction and recov ery. MyRecoveryDC’s Certified DC Peers are ready to help people find their path to recovery and will support them along the way.
• School-based services. If your child is a student at a DC public school or public charter school, they can receive counsel ing from a school-based mental health provider. Visit https://

dbh.dc.gov/node/1500291 to find contact information for the provider assigned to your child’s school.
• Help for veterans. When you call the Suicide & Crisis Lifeline, press “1” after dialing 988 to get connected directly to the Veter ans Crisis Line, which serves our nation’s veterans, service mem bers, National Guard and Reserve members, and those who support them. For texts, continue to text the Veterans Crisis Line short code: 838255.
The information in this article is intended to help you learn more about this topic. It is not meant to take the place of speaking with your health care provider. If you have questions, talk with your health care provider. If you think you need to see your health care provider because of something you have read in this ar ticle, please contact your health care
HS-10
DECEMBER
SUPPLEMENT
www.washingtoninformer.com /
2022 HEALTH WELLNESS & NUTRITION
CONTINUED ON PAGE HS-11
The counselors at the 988 Suicide & Crisis Lifeline are trained and will use their expertise to support callers experiencing urgent mental health crises.
CONTINUED FROM PAGE HS-10
provider. Never stop or wait to get medical attention because of some thing you have read in this material.
Sources
1. “988 Suicide & Crisis Lifeline,” Federal Communications Commission, https://www.fcc.gov/sites/ default/files/988-factsheet.pdf
2. “How Is 988 Different Than 911?” Substance Abuse and Men tal Health Services Adminis tration, https://www.samhsa.gov/findhelp/988/faqs#about-988-basics
3. “Deaths of People with Mental Illness During Interactions with Law Enforcement” Interna tional Journal of Law and Psychi atry, https://perma.cc/826F-AKG8
4. “988 Frequently asked
questions”, Substance Abuse and Mental Health Services Administra tion
https://www.samhsa.gov/findhelp/988/faqs
All images are used under license for illustrative purposes only. Any in dividual depicted is a model WI
#BestMe Corner
AmeriHealth Caritas District of Columbia (DC) has many mental health resources available for enrollees.
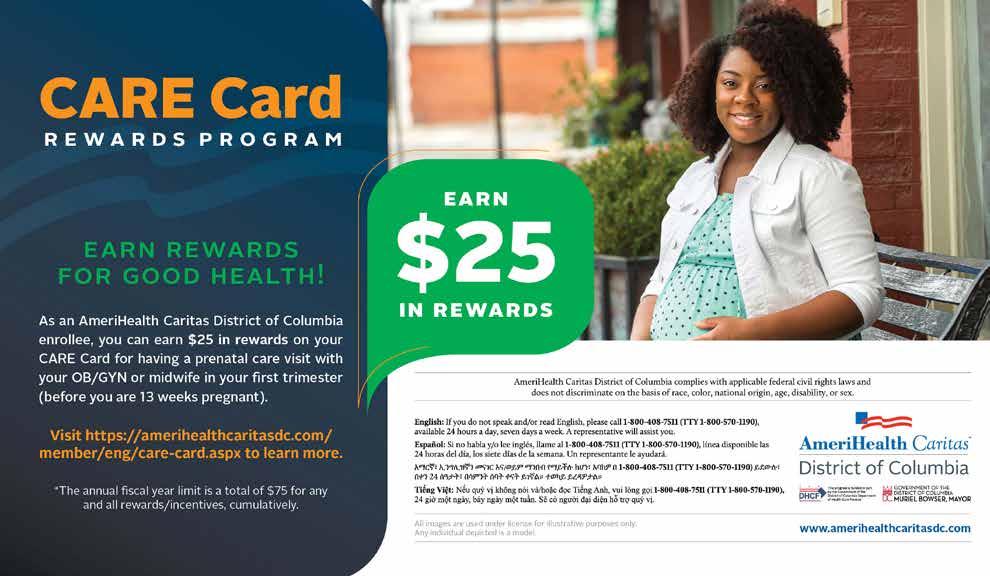
Behavioral health providers. You may benefit from speaking with an experienced, trained behavioral health provider if you have a problem that makes you feel overwhelmed or interferes

Visit www.amerihealthcaritasdc.com to find the Provider Directory or call Enrollee Ser vices at 1-800-408-7511 to get help with finding a behavioral health care provider.
Ginger Emotional Support app. The Ginger Emotional Support app offers 24/7 support tailored to your mental health needs. Text with a coach every day for quality care for every indi

If you are age 21 or older, download the Ginger app from the Google Play™ store or Apple App Store® to text with an emotional support coach. (Standard messaging and data fees may apply.)
MindRight. MindRight is an app that specializes in providing 24/7 emotional support for teens and young adults. You can text with a coach every day and access the support you need straight from your smartphone.
Enrollees ages 13 to 20 can text “hello” to 886-886 and use referral code “AmeriHealth” during enrollment to start texting with a MindRight support coach. (Standard messaging and data fees may apply.)
H-11 DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT / www.washingtoninformer.com HS-11
us
Twitter at www.twitter.com/amerihealthdc. / Find us on Facebook at www.facebook.com/AmeriHealthCaritasDC. / Find us
at
Find
on
on Instagram
www.instagram.com/amerihealthcaritasdc.
Celebrating SHIRE’s 25 Years: Past, Present, and Future
Ruth T. Perot Executive Director/CEO rperot@shireinc.org

On December 8th, 2022, Sum mit Health Institute for Research and Education, Inc. (SHIRE) cel ebrates our Silver Anniversary in Washington, DC. We will be com memorating 25 years of service, advocacy, and community engage ment in pursuit of health justice, equity, and empowerment for Afri can Americans and other people of color.
Since 1997, SHIRE has main tained a rock-solid commitment to help eradicate racial/ethnic health disparities and to promote optimal health and wellness for the com munities we serve. For example, the impact of our cutting-edge policy research focused on racial/ethnic data collection is reflected in the Af fordable Care Act. Our leadership

and advocacy aimed at the inclusion of people of color, with respect to health information technology, has served as a catalyst for federal and state policies and programs. The convening of people of color under the banner of Out of Many One has been a model for multicultural collaboration. Our refurbished web site www.shireinc.org features more information about these and other
activities.
At the same time, SHIRE has become a highly respected partner with numerous community orga nizations and has engaged thou sands of residents in the District of Columbia in wellness initiatives.

The Early Childhood Obesity Pre vention Collaborative convened over 100 stakeholders, including parents, educators, government representatives, and members from community organizations, univer sities, corporations, and the media who develop creative policies and programs. Another childhood obe sity prevention effort was SCOOP, SHIRE’s Childhood Obesity and Overweight Prevention program, that engaged young children and their teachers in activities promoting movement using music and drama created for that purpose. Our Pass port for Youth Program, conducted in partnership with the YMCA, has served as a model for encour aging middle school youth to become involved in physi cal activities, such as swimming, that were new to them. We have trained and involved over 50 in dividuals as health coaches and peer educators who have
spread the message of health and wellness throughout 5 DC wards.
Over 1500 men and women have participated in SHIRE’s Wellness Circles to date. They have acquired tools and strategies to improve their health outcomes and make lasting lifestyle changes—taking charge of their health and their lives.
The COVID-19 pandemic, which has revealed the urgent need for fundamental change in our healthcare systems, also offers an opportunity to think differently about health and wellness. SHIRE offers a compelling answer to this challenge. We have equipped com munity residents with the informa tion and tools they need to demand respect, high quality treatment, and promote changes in the healthcare systems that serve them. Although we are aware of the influence of so cial determinants, we firmly believe that fostering self-determination and empowerment is a powerful strategy for meaningful change. This is the mission that we carry into our next 25 years.
In 2023, we will vigorously promote our Wellness Circle pro gram as a concept applicable to new groups and health challenges. For example, we will seek partners and sponsors to advance improved maternal health, which has been greatly impacted by the recent Su
preme Court decision. Building on past experience, SHIRE will seek to involve youth in Wellness Cir cles—particularly those impacted by violence to aid their develop ment as self-empowered health am bassadors. Our approach is to equip individuals with the tools they need—accurate information, skills and experiences, encouragement and motivational group support— which can be applied to many challenges facing community resi dents. Lastly, we will build on the success of Wellness Circles focused on chronic health conditions by of fering this program to providers of health services and health insurance agencies in the District of Columbia and surrounding jurisdictions.
Indeed, there are many reasons to celebrate SHIRE’s past, present, and future. Over the past 25 years, SHIRE has continued to thrive and with the support of the community our collective success is assured. WI
www.washingtoninformer.com
HS-12
/ DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT
OUR 25TH ANNIVERSARY WHY WE CELEBRATE 1. SHIRE commemorates 25 years of service, advocacy, and community engagement for people of color. 2. SHIRE maintains a rock-solid commitment to eradicate health dispari ties and to promote health and wellness for communities of color. 3. SHIRE is a highly respected community partner and engages hundreds of the residents in the District of Columbia in their Wellness Circle pro grams. 4. SHIRE empowers people of color with health information and the tools to improve their health outcomes and make lasting lifestyle changes. 5. SHIRE trains community residents as health coaches and peer educa tors to spread the message about health and wellness among DC residents of color. 6. SHIRE has influenced policies that support health equity and justice at the national level. For more about SHIRE’s Silver Anniversary
Recent & Recommended Books About Black Health
 By Lee Ross / WI Staff Writer
By Lee Ross / WI Staff Writer
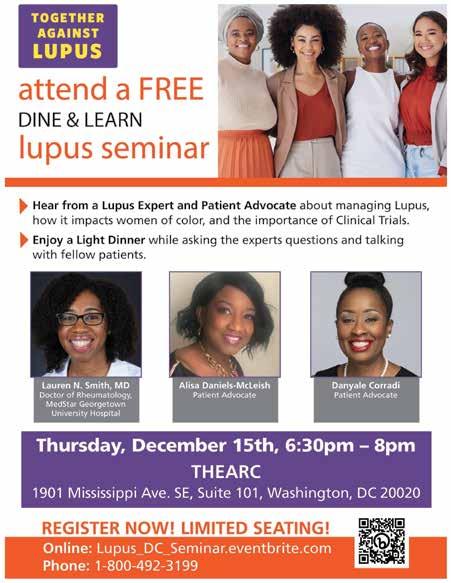
Sickening: Anti-Black Racism and Health Disparities in the United States
 By Anne Pollock
By Anne Pollock
From the spike in chronic disease after Hur ricane Katrina to the lack of protection for Black residents during the Flint water crisis--and even the life-threatening childbirth experience for tennis star Serena Williams--author Anne Pollock takes read ers on a journey through the diversity of anti-Black racism operating in healthcare. She goes beneath the surface to deconstruct the structures that make these events possible, including mass incarceration, police brutality, and the hypervisibility of Black athletes’ bodies. Ultimately, Sickening shows what these shocking events reveal about the everyday racialization of health in the United States. Concluding with a vital examination of racialized healthcare during the COVID pandem ic and the Black Lives Matter rebellions of 2020, Sickening cuts through the mind-numbing statistics to vividly portray healthcare inequalities. In a gripping and passionate style, Pollock shows the devastating reality and consequences of systemic racism on the lives and health of Black Americans.
We’ll Fight It Out Here: A History of the Ongoing Struggle for Health Equity

David Chanoff, Louis W. Sullivan Racism in the U.S. health care system has been deliberately undermining Black health care profes sionals and exacerbating health disparities among Black Americans for centuries. These health dispar ities only became a mainstream issue on the agenda of US health leaders and policy makers because a group of health professions schools at Historically Black Colleges and Universities banded together to fight for health equity. We’ll Fight It Out Here tells the story of how the Association of Minority Health Professions Schools (AMHPS) was founded by this coalition and the hard-won influence it built in American politics and health care. David Cha noff and Louis W. Sullivan, former secretary of health & human services, detail how the struggle for equity has been fought in the field of health care, where bias and disparities continue to be volatile national issues.
Black Man in a White Coat: A Doctor’s Reflections on Race and Medicine
 By Damon Tweedy
By Damon Tweedy
When Damon Tweedy begins medical school, he envisions a bright future where his segregated, working-class background will become largely irrelevant. Instead, he finds that he has joined a new world where race is front and center and black bodies are considered pathological and in herently diseased. Black Man in a White Coat examines the complex ways in which both black doctors and patients must navigate the difficult and often contradictory terrain of race and med icine. Tweedy discovers how often race influences his encounters with pa tients, and e illustrates the complex social, cultural, and economic factors at the root of many health problems in the Black community. Tweedy explores the challenges confronting black doctors, and the disproportionate health burdens faced by black patients, ultimately seeking a way forward to better treatment and more compassionate care.
Body and Soul: The Black Panther Party and the Fight Against Medical Discrimination
 By Alondra Nelson
By Alondra Nelson
Between its founding in 1966 and its formal end in 1980, the Black Panther Party blazed a distinctive trail in American political culture, touting revolutionary rhetoric and militant action. Alondra Nelson, however, uncovers an indispensable but lesser-known aspect of the organization’s broader struggle for social justice: health care. The Black Panther Party’s health activism—its network of free health clinics, its campaign to raise awareness about genetic dis ease, and its challenges to medical discrimination—was an expression of its founding political philosophy and also a recognition that poor blacks were both underserved by mainstream medicine and overexposed to its harms. In 1971, the party launched a campaign to address sickle-cell anemia. In addition to establishing screening programs and educational outreach efforts, it exposed the racial biases of the medical system that had largely ignored sickle-cell anemia, a disease that predom inantly affected people of African descent.
Black and Blue: The Origins and Consequences of Medical Racism
By J. Hoberman
Black & Blue is the first systematic description of how American doctors think about racial differences and how this kind of thinking affects the treatment of their black patients. The standard studies of medical racism examine past medical abuses of black people and do not address the racially motivated thinking and behaviors of physicians practicing medicine today. Black & Blue penetrates the physician’s private sphere where racial fantasies and mis information distort diagnoses and treatments. Doctors have imposed white or black racial identities upon every organ system of the human body, along with racial interpretations of black children, the black elderly, the black athlete, black musicality, black pain thresholds, and other aspects of black minds and bodies. WI

H-13 DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT / www.washingtoninformer.com HS-13
Did You Know? Results of Pew Disparities Research
By Lee Ross WI Staff Writer
The health care system is also seen as contributing to the prob lem: 49 percent say a major reason why Black people generally have worse health outcomes is because health care providers are less likely to give Black people the most advanced medical care.
Large majorities of Black postgraduates (78 percent) and college graduates (76 percent) say less access to quality medical care is a ma jor reason Black people have worse health outcomes than other adults in the U.S., compared with 67 percent of those with some college experience and 51 percent of Black adults with a high school diploma or less education.
Younger Black adults are more likely than older adults to cite actions from hospitals and medical centers: 50 percent of those un der age 50 say hospitals and medical centers giving lower priority to their well-being is a major reason why Black people have worse health outcomes; 43 percent of Black adults 50 and older say the same.
Overall, 47 percent think health outcomes for Black people have gotten a lot or a little better over the last 20 years. Still, 31 percent say they have stayed about the same and 20 percent think they have gotten a lot or a little worse.
A majority of Black Americans give positive ratings of their re cent health care, but can also point to negative experiences in the past. A majority (61 percent) rate the quality of care they’ve received from doctors or other health care providers recently as excellent (25 percent) or very good (36 percent). A quarter describe the quality as good, while just 11 percent say it was fair and only 3 percent describe the quality of care they’ve received most recently as poor.
A majority of Black adults report at least one negative interaction with doctors and other health care providers at some point in the past – that was 56 percent who say they’ve had at least one of several negative experiences with doctors or other health care providers at some point in their lives.

One focus group respondent described their experience this way: “I had a situation where I had to go through about two differ ent doctors until I was able to get the results that I was requesting, because they did not believe that the issues that I had were valid, or that they were as serious as I made them out to be. It’s kind of been an ongoing thing, so I’m always leery when I’m talking to physicians. I don’t trust them just because they are doctors. I know they have the Hippocratic Oath, but it feels like it’s a little different when they deal with African American patients. And I don’t care if it’s an African American physician or White physicians.” – Black woman, 25-39
About three-in-ten Black adults (32 percent) say they’ve felt rushed by their health care provider and 29 percent say they’ve felt they were treated with less respect than other patients, either recently or in past experiences with doctors and other health care providers. Similarly, 29 percent say they’ve felt they’ve received lower quality medical care at some point; 70 percent of Black adults say this has not happened to them. WI
HS-14 www.washingtoninformer.com / DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT Give yourself and your loved ones the gift of high quality, affordable health insurance PREMIUMS AS LOW AS $11/MONTH It’s the Season of Giving! 10th Anniversary • Many plans to meet your needs and budget • Standard plans with no deductible for essential care • FREE expert enrollment support OPEN ENROLLMENT NOVEMBER 1 - JANUARY 31 Enroll by December 15 for Coverage Beginning January 1 DCHealthLink.com/residents (855) 532-5465 / TTY: 711












H-15 DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT / www.washingtoninformer.com HS-15 The pro in produce. We pick and pack maximum freshness. shop now at Safeway.com GL00181271_SWY_1208_WashingtonInformer_FullPg




HS-16 www.washingtoninformer.com / DECEMBER 2022 HEALTH WELLNESS & NUTRITION SUPPLEMENT
time, it’s TREATMENT WORKS. LIVE LONG DC Saving lives from the opioid epidemic When you are ready to try again, you can start right now Text READY to 888-811 for a list of treatment sites that are open.
“This









 Dr. Shantella Y. Sherman WI Special Edition Editor
Dr. Shantella Y. Sherman WI Special Edition Editor









































 By Elaine Magee MPH, RD, Safeway Corporate Dietitian (@therecipedoctor and author of 25 books)
By Elaine Magee MPH, RD, Safeway Corporate Dietitian (@therecipedoctor and author of 25 books)












 By Anne Pollock
By Anne Pollock

 By Damon Tweedy
By Damon Tweedy
 By Alondra Nelson
By Alondra Nelson