









People wanting to keep wrinkles at bay will soon have a new option now that the U.S. Food and Drug Administration has ap proved the first competitor for Botox in decades.
Daxxify, made by Revance Ther apeutics Inc. in Nashville, Tennessee, is injected into the face along worry lines. It lasts longer than Botox, with about 80% of users seeing no or mild facial lines at four months after injec tion. For half of users, the treatment lasted six months, the company said
in a statement.
“Users do not have to go once every three months,” physician Balaji Prasad, who covers specialty phar maceuticals as an analyst for Barclays Investment Bank, told the New York Times. “In a world where time is of the essence, having a product with a long duration factor is extremely useful.”

The new drug now enters the $3 billion field of facial injection drugs. It is also a neuromuscular blocking agent and a botulinum toxin, like
Abbvie’s Botox.
“It also opens up the door for what we can do with therapeutics,” said Revance CEO Mark Foley, told the Times. “If you think of migraines, cervical dystonia [a neurological condition that affects the muscles in the neck and shoulders], overactive bladder, there’s a huge medical op portunity as well.”
The company has begun testing the drug on these other medical is sues, Foley said. While the company had been trying to create a product that needed no needle, it instead discovered a way to use peptide tech nology to keep the product stable. Typically, animal protein or human serum is used.
Botox is also used for more than just wrinkles. It has been an FDA-ap proved treatment for chronic mi graines since 2010.
Users of Daxxify in the Revance studies included some who expe rienced side effects. About 2% of people developed a drooping eyelid, while about 6% experienced head ache, the company said.
Toxin-based treatment can carry the potential for other side effects, such as general muscle weakness or breathing difficulties, the FDA cau tioned. Daxxify study participants showed none of those symptoms.
Revance had initially hoped for approval of its product in November 2020, but plans were postponed be cause of pandemic travel restrictions, the Times reported. An inspection finally conducted in June 2021 found problems with the quality control process and the company’s working cell bank, which contain the drug’s active ingredient. Those concerns were resolved, the Times reported.

matters who reads
you’re a woman 40 or older, you need an annual mammogram. Schedule your mammogram with the experts who know cancer best.
breast cancer in their lifetime, and the best fighting chance against breast cancer is regular screening mammograms. Most mammograms are normal … but if yours isn’t, Roswell Park is where you want to be. NO PRESCRIPTION OR REFERRAL NEEDED.


at the door who were either shot or stabbed. At the same time I had a patient who was crashing and had to be intubated and put on a ventilator. And I had a demented patient who was trying to escape. It was one of the craziest nights I’ve ever had. The good news is the shift always ends. That one went quickly. But it was definitely a crazy day.
Q: COVID-19 complicated ER situ ations over the last couple years. How is COVID-19 being handled now? Are things more or less back to normal?

Q: As an emergency medicine physician, what does your typical day look like?
about a lot of things, as opposed to a specialist who knows a lot about one specific area. Compared to prima ry care, I’d say our focus is more procedural-based. We do things like intubations, drain abscesses, put tem porary casts on patients. With prima ry care you’re monitoring health and wellness over a long period of time. We’re more looking at acute illness.
Your
dog may like to lick your hand or face, but if you’re using a chemother apy cream that treats certain skin conditions, you should not allow it, the U.S. Food and Drug Administration advises.
The medication fluorouracil is fatal to dogs when ingested. People who keep the cream on a nightstand or counter should put it out of reach of their dogs, who may ingest it if they chew the container, the FDA advised.
The agency has received reports involving dogs that were exposed to the cream; all the dogs have died.
Although the FDA has not yet received any reports of fluorouracil poisoning in cats or other pets, it recommends that this drug be kept away from all pets.
The cream is used to treat some types of skin cancers and a condition called actinic keratosis, which can lead to skin cancer. It may also be used to treat warts in children. Occasionally it is used to treat certain cancers in horses.
It can be dispersed as an in jection, or as a topical cream or a topical solution that’s applied on the skin. Brand names include Efudex, Carac, Tolak and Fluo roplex.
Pets who ingest fluorouracil may show signs of poisoning within 30 minutes. These signs can include vomiting, shaking, seizures, difficulty breathing and diarrhea.
Affected dogs can die in as little as six to 12 hours.
If you suspect your pet has consumed fluorouracil, imme diately get veterinary care and bring the container of cream with you. Also contact your vet or an emergency vet hospital immediately even if your pet just licks the area where you applied fluorouracil, and definitely call if your pet chews the container and consumes some of the fluo rouracil.
A: I’m an emergency room phy sician at DeGraff Hospital. I work for UBMD and work at Suburban and Eastern Niagara at Lockport. I’m also a physician liaison for all the physician assistants in our group, so I supervise all of the advance prac tice providers in our group. During a typical day at DeGraff, I usually work 7 a.m. to 7 p.m. A PA [physician assistant] usually comes in to assist me with work around 11 o’clock. I may or may not have a resident with me who I supervise. I typically see whatever walks in through the door: kids, adults, elderly people. Anything from lacerations to heart attacks, strokes, abdominal pain. We see just about everything at DeGraff.
Q: Emergency room physicians generally have to be broad in their skill set, not unlike primary care physicians, but the specialties are still pretty different. What would you say some of the key differences are with regard to training and competencies?
A: In emergency medicine we’re obviously there to treat acute emer gency issues, but we do also treat long-term conditions. We have to act a little more quickly than someone in prima ry care, although both of us are similar in that we know a little
Q: What got you interested in emergency medicine?
A: A few things. I liked that you never knew what your day was go ing to be like. You never knew what your schedule would be. You can’t predict what patients and conditions will walk through the door. I like that I’ve been doing this for 18 years and I still learn something new every day, whether from a patient, a nurse or another provider. I’m always getting educated. It’s also shift work. You come in, put in your time and then you go home. You’re not usually on call. I also like that I basically get to wear pajamas to work every day; I get to wear scrubs. That’s another thing that drew me to the field. I like the camaraderie with the nurs es. We’re in close proximity to the nursing station and we work closely with them. It has more of a family feel. Not that you wouldn’t get that in the office, I think it just happens more easily. I like the variety of the schedule. Sometimes I work on the weekend and holidays, but it also gives me some sched ule flexibility, which makes it easier to have a family with kids and make events.
Q: What’s the cra ziest day you’ve had?
A: I lived and worked in Chicago for about 15 years. I had a shift there that was probably the craziest shift I’d ever had. It was an overnight shift and I was pretty new at the time, pret ty fresh out of residency. And I was working alongside a doctor who had gotten sick and had to go home. I had three patients get dropped off
A: I think in the ER things didn’t change all that much. We’re prob ably the only part of medicine that didn’t. We saw patients all through COVID-19 pretty much as normal, other than the precautions we took and are still taking with regard to gowning up, masks and gloves. Most surgical procedures are back to normal. Some doctor’s offices are still a little bit reluctant to see patients with COVID-19, so they get sent to us, which increases our volume. But for us in the ER, it’s pretty much business as usual. We see everyone, whether or not you have COVID-19. Each room at DeGraff is separate since our remodel, so we’re in good shape for containing patients if we need to and keeping them and staff safe.
Q: Are you still seeing a lot of patients with COVID-19 compared to a year ago?
A: We are seeing patients with COVID-19, but the numbers have definitely decreased; the symptoms and severity of illness has decreased as well.

Q: You mentioned working 12hour days. Are you on a few days then off a few days?
A: Well, for me personally, I work three to four days a week. Sometimes five if I pick up extra hours. Most of the shifts at my group are 12 hours, but there are some 11- and 10-hour shifts. I prefer 12-hour shifts, because if I’m already there, what’s two more hours? The flexibility of the schedule is nice. Some weeks I work a little heavier, some weeks I work a little lighter.
Q: How would you sell emergency medicine to a medical student who wasn’t sure what they wanted to do yet?
A: I think the fact that it encom passes so much of medicine. You see OB-GYN, you see cardiology, you see psychiatry, you see dermatology, you see trauma. I liked it all in medical school, so I gravitated to the specialty where I could do it all. So I think it’s actually a great field for someone who is undecided. It’s also good for people who like to work with their hands or interact with people a lot. And if you don’t like getting dressed up for work, it’s a great choice.
Name: Melissa M. DeSantis, M.D. Position: Emergency medicine physician at DeGraff Hospital
Hometown: Niagara Falls Education: University of Buffalo
Affiliations: Millard Fillmore Suburban Hospital; Eastern Niagara Hospital
Family: Three children, two stepchildren
Hobbies: Watching her kids play sports, exercise, skiing, Bills football
Never a dull moment at the hospital’s ER: ‘We see just about everything,’ says DeGraff Hospital physician who works 12-hour shifts at the emergency department
At ECMC, each of us—from doctors, nurses, support staff, and specialists—is focused on not just healing the community but supporting each other at every turn. Our commitment to our employees starts with a rewarding work environment and continues through to our professional development programs. Whether you’re just starting out or you’re a seasoned healthcare professional, ECMC is the perfect fit to further your career.


caregivers at ECMC.EDU/CAREERS

$7,050 in 2022, you enter catastrophic coverage but are still responsible for 5% of your prescription drug costs, with no limit.
But in 2024, people with Part D coverage will no longer be responsi ble for any out-of-pocket drug costs once they enter catastrophic cover age. This is significant for seniors who use expensive medications for conditions like cancer or multiple sclerosis.
drugs will be capped at $2,000 per year. This will be a major savings for the more than 1.5 million beneficia ries who currently spend more than $2,000 out-of-pocket each year.
The
climate, tax and health care bill known as the Inflation Reduction Act that was passed by Congress and signed into law by President Biden in August includes significant improvements to the Medicare program that will kick in over the next few years.
These changes will lower pre scription drug prices for millions of seniors by allowing the government to negotiate drug prices for the first time and capping seniors’ out-ofpocket drug costs at $2,000 annually. Some other popular changes will include free vaccinations, lower insu lin costs and expanded subsidies for lower income seniors.
Here is a breakdown of the changes to expect in Medicare and when they will roll out.
2023
Starting this January, all vac cines covered under Medicare Part D, including the shingles vaccine, will be free to beneficiaries. And the skyrocketing cost of insulin will be capped at $35 per month. This will be a significant saving for the more than 3 million Medicare enrollees who currently use insulin to control their diabetes.
Also starting in 2023, drug mak ers will be penalized in the form of rebates that they would be forced to pay to the government if they impose price increases that exceed general inflation.
Cost sharing for catastrophic coverage in Part D will be eliminat ed. Under the current Part D benefit, once your out-of-pocket costs reach
Also starting in 2024 through 2029, Part D premiums will not be allowed to grow faster than 6% per year.
And for lower-income Medicare beneficiaries, eligibility for the Part D Low Income Subsidy (also known as Extra Help) will be expanded to 150% of the federal poverty level, from today’s limit of 135%. This change will mean about 500,000 more seniors will qualify for financial assistance to help pay some or all of their prescription drug premiums and deductibles.
One of the biggest cost reduction measures for Medicare beneficiaries will begin in 2025 when out-of-pock et spending on Part D prescription
When Medicare’s Part D pro gram was enacted in 2003, negotiat ing lower drug prices was forbidden. But because of the Inflation Reduc tion Act, starting in 2026 Medicare will be empowered to begin nego tiating prices with drug companies for 10 of the most expensive drugs covered under Part D. In 2027 and 2028, 15 drugs would be eligible for negotiations and in 2029 and sub sequent years, 20 drugs would be chosen.
And, in addition to all the Medi care improvements, the Inflation Re duction Act also extends the Afford able Care Act (Obamacare) premium subsidies for three years that have helped millions of Americans gain coverage before they’re eligible for Medicare.
Jim Miller is the author of Savvy Senior column, which runs every month in In Good Health newspaper.
After slowly climbing back from the devastation caused by the pandemic, July median hospital operating margins plunged a staggering 64% from June op erating margins, according to industry consultants Kaufman Hall.
Its survey of 900 hospitals revealed an average year-to-date margin of negative 1%.
KH attributes this trend to lower outpatient volumes, more acute and expensive inpatient cases and an end to COVID-19 relief and PPP from the federal government.
Financial services company Fitch Ratings has reduced its hospital out look from “neutral” to “deteriorat ing.” Shaky finances are the driving force behind hospital mergers and
Typically, an ACO is a partner ship between physicians and one or more hospitals to participate in the Medicare Shared Savings Program (MSSP). The goal is to cooperate in exceeding quality benchmarks and reducing per capita cost benchmarks established in advance by Medicare. ACOs submit their bills, physician and hospital, to Medicare per usual. ACOs that reduce per capita costs will share in the savings with Medi care. If ACO costs per capita go up, the ACO must return money to Medicare. The MSSP is designed to encourage and reward the delivery of care by a cooperative of physicians
acquisitions. Not price fixing as skep tics have speculated. To survive and deliver care to their respective com munities, hospitals must be allowed to freely explore opportunities to increase fragile operating margins via shared over head, operating savings, and improved credit without onerous regulato ry oversight. At stake, in many cases, is the survival of smaller rural hospitals. While mergers might save hospitals, there could be a point where there are diminishing returns. For example, the 20-hospital Cleve land Clinic lost just over $1 billion the first half of 2022. While $628 million is attributed to investment losses, the system still lost close to $400 million on operations.
and hospitals working as a team to exceed common goals. An “every man for himself” model won’t work. And it never has. Medicare has learned that the more primary care physicians in the ACO, the better at reducing per capita costs. This makes sense. Effective primary care deliv ery can reduce illness, unnecessary referrals to specialists and overall hospitalization. Last year, 99% of ACOs beat quality benchmarks and 58% beat per capita costs. ACOs beat per capita costs benchmarks by $3.6 billion.
In 2018, the FDA approved the
Apple watch for EKGs. Who would have thought? Now, the NIH has granted $37 million to researchers at Northwestern and Johns Hopkins (and others) to study it. By moni toring atrial fibrillation, the watch can prevent strokes and reduce the amount of expensive blood thinners patients with Afib are receiving. Afib affects 2.5 million to 5 million of us. That is predicted to be 12 million by 2030. The seven-year study will involve 5,400 people with Afib. Some in the study will continue to receive the standard regimen of continuous expensive blood thinners to prevent strokes. Others will have their Afib monitored by the watch and receive targeted blood thinner therapy only when at risk of a stroke.
Congress has discontinued fund ing the government’s COVID-19 vac cine program effective next year. That means it will no longer purchase the vaccine from manufacturers and distribute it for free. It has turned the keys over to Big Pharma. Pfizer and Moderna must be licking their chops. (Is this what it took for Big Pharma to finally agree to negotiate some drug prices?) The government has already dropped free home testing due to lack of funds. Both drug giants claim that with the feds out of the way, they can be “more competitive” in an open market versus a govern ment-controlled contract market. Both also claim they can now focus on “branded education” which is in their area of expertise. It remains to be seen if Medicare and commercial insurers will charge for the vaccine or make it available for free.
The Biden administration and Congress has approved close to $100
million in funding for ACA naviga tors who help people select an insur ance that fits their needs and budget. The increased funding should add 1,500 new navigators. The ACA has been a widely successful program now insuring more than 36 million people. The uninsured rate is at an all-time low below 8%. Open enroll ment begins Nov. 1. To hamstring the ACA, the Trump administration slashed navigator funding to $10 million.

Just about half of all Medicare beneficiaries, or 28 million, are now covered by a commercially operated advantage plan. Sixty-six percent of the beneficiaries are individually covered; 18% are insured via employ er or union; and 16% are enrolled through special programs. Market shares for the largest carriers are Humana 28%; United 18%; and BCBS 14%. Cigna, Centene and Kaiser com bine for 24% market share.
Advantage plans are Part C Medicare. They draw members away from traditional Medicare by offering perks such as dental, vision, OTC drugs, transportation and even meals. Unlike traditional indemnity Medicare, most advantage plans require preauthorization for certain procedures.
George W. Chapman is a healthcare busi ness consultant who works exclusively with physicians, hos pitals and healthcare organizations. He op erates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapman consulting.com.

There’s
an easy way to reduce your risk for dementia, heart disease and cancer: Start walk ing.
Getting in those recommended 10,000 steps a day makes a real differ ence, new research affirms, but even fewer will pay big dividends. No matter how many you log, however, step up your pace for the biggest benefit.

For every 2,000 steps you log, up to about 10,000 a day, your risk of early death drops by between 8% and 11%, researchers found.
“So, 10,000 steps maximizes the chances of getting all these benefits, but also for inactive people who can’t engage in so many steps — any steps have benefits — every step counts,” said lead researcher Borja del Pozo Cruz of the Center for Active and Healthy Aging at the University of Southern Denmark in Odense.
And, he added, it’s never too late to get going.
“The range of participants that we had in the study went from 40 to 79,” Cruz said. “That means that any person can actually get the benefits.”
This study, however, doesn’t prove that walking 10,000 steps a day has a health benefit, only that number of steps is associated with a reduction in heart disease, cancer, dementia and early death.
Cruz said that the power of the study lies in its large size and in researchers’ ability to isolate walking from other exercises.
For the greatest health benefit, the sweet spot was 9,800 steps a day, which slashed dementia risk by 40%. But just 3,800 steps lowered it by 25%, the investigators found.
Over and above the number of steps, walking at a brisker pace — about 80 steps a minute — brought the greatest reduction in dementia, heart disease, cancer and premature death, Cruz noted.
But all that walking doesn’t have to happen all at once. It can be spread out during the day, the researchers said.
The study drew from data from 78,500 adults in the United Kingdom who were followed for a median sev en years, meaning half were followed even longer. They wore wrist sensors that measured their physical activity over seven days.
Cruz said that wearable devices like Apple watches and Fitbits that track steps can be useful if you use them faithfully.
“What we know about those devices is in the beginning people take them very seriously, but after a while,” use tapers off, he said. “We also know that you need to create the habit.”
A monthly newspaper published by Local News, Inc. Distribution: 25,500 copies throughout more than 1,500 high-traffic locations.
In Good Health is published 12 times a year by Local News, Inc.
© 2022 by Local News, Inc. All rights reserved. P.O. Box 550, Amherst, NY 14226
Phone: 716-332-0640 • Fax: 716-332-0779 • Email: editor@bfohealth.com
Editor & Publisher: Wagner Dotto
Writers: Deborah J. Sergeant, Jim Miller, Gwenn Voelckers, Anne Palumbo, Brenda Alesii, Amanda Jowsey, Ernst Lamothe Jr. • Advertising: Anne Westcott, Amy Gagliano
• Layout & Design: Angel Campos-Toro • Office Manager: Ahme Cruz
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement—not to take the place of—the recommendations of your health provider. Consult your physician before making major changes in your lifestyle or health care regimen.
It takes a lot to provide excellence in emergency care. It takes quick and easy access to care, state-of-the-art technology, and most importantly, it takes physicians who have dedicated themselves to achieving excellence every single day. Physicians who have seen it all and know how to handle essentially anything.

That excellence can be found at the Emergency Center at DeGraff Medical Park (formerly DeGraff Memorial Hospital). Our physicians are second to none and combined with our highly-trained nurses and staff, they all share one goal– to provide patients with outstanding medical care. In fact, they’re the same physicians who provide emergency care at Millard Fillmore Suburban Hospital.


Where excellence is.
DeGraffEmergency.org
Fall is such a special time of year. For me, it means all good things: relaxing in front of a cozy fire, making pumpkin soup on Sunday afternoons, donning my well-worn leather jacket for long walks and turning my attention to all those inside projects I neglected over the summer.
The brilliant colors, autumnal aromas and industriousness that arrive with the falling leaves really appeal to me. But this hasn’t always been the case.
After my divorce, the month of October left me feeling melancholy. I missed sharing the beauty of the season with a special someone. And I missed the sunshine as daylight waned.
Nostalgia and wistfulness would creep in, and I just wanted to retreat into myself. For those who live alone, the month of October has unique challenges.
Not one to wallow in a “poor is me” state of mind, I began to develop and employ some strategies to rekin dle my love of the fall season. It can be a great time to mix it up, get busy and expand your horizons.
Below are elements of my annual fall game plan. Take a look and see if one or more of these suggestions might not add a little color to your life palette this fall:
■ Tackle indoor projects. Fall is a great time to accomplish all those
nagging in door projects on your to-do list. I have a long list and I keep it right in front of me — a daily reminder that I have plen ty of home improvements to tackle, both large and small.
Too much idle time is not a friend at any time of year, but it can become downright unfriendly when gray clouds appear and the tempera ture drops. Now is the time to get busy: organize your storage space, do some touch-up painting, update your wardrobe, or clean the garage.
There’s nothing like being pro ductive to beat the autumn blues.
Don’t I know it. I just finished coating my flat-roof porch with a sticky tar sealant. Confession: it was messier than it was fun, but still ... I’m proud of my accomplishment. It lifted my spirits.
■ Get up and get going. Staying ac tive when there’s a chill in the air can be difficult. I can remember many a cold morning when all I wanted to do was hit the snooze button, pull up the covers, and stay in bed.
As nice as sleeping in can be
from time to time, I don’t recom mend it as a steady diet.
In my experience, there’s no better way to start your day than to wake up early. In the early morning’s peace and quiet, there is glorious time to reflect and feel gratitude. I use this important “me time” to meditate and set my intentions for my day.
As the morning brightens, my energy grows, as does my apprecia tion for the precious day ahead me.
■ Start moving and enjoy the great outdoors. Fresh air, sunlight and even a gentle rain can be invigorating first thing in the morning. I find a sunrise walk boosts my energy and kickstarts my day. Do I feel like layering up and taking a walk every morning? No. Do I feel better after I make the effort? Yes, without fail.
I love a long solitary walk to clear my head and be mindful. But I also love a walk with my sister Anne or good friend Kate to enjoy their company and avoid the siren’s song of isolation as the days grow short and get colder.
■ Learn something new. Going back to school and fall go hand-inhand. Who among us isn’t reminded of the nervous excitement associated with returning to school in the fall? It’s a great time to expand your intel lectual horizons.
Each fall I identify a new skill or subject to learn. Last year, I re searched how to divide and relocate perennials (my irises and peonies); this fall, I’m signing up to learn French on Duolingo, the free lan guage-learning app.
Continuing education opportuni ties are abundant in this community and online. Check out colleges and universities, community centers, arts and cultural institutions, your local library, and workshop listings for class and workshop offerings.
■ Invite people in. Over the years,
I’ve discovered a few simple and manageable ways to bring people into my world and into my home. One way is to organize a gathering around a TV show or series — yes, around the TV, as odd as that might sound.
For years, I invited my single friends over to watch “Downton Abbey” with me on Sunday nights. I provided the soup and salad; they provided the good company.
So, what’s your pleasure? Wheth er it’s football, a favorite weekly sitcom, or “Ted Lasso” on Apple TV+ — all of these and other TV shows can become reasons to bring friends and family together. The benefits? You’ll hone your cooking skills (boy, do I now have some great soup reci pes!) and you’ll connect with people you care about.
What better way to enjoy a nice fall evening.
There are so many wonderful and meaningful strategies to enjoy the fall season and to ward off the blues that can sometimes emerge during this changing time of year. But these strategies require effort –conscious, creative effort.
If you are feeling sluggish, lonely, or isolated, try a few of the strategies above. They have stood me in good stead and have reinvigorated my love for the fall season.
If you, too, are ready to turn over a new leaf, October is the perfect time!
Gwenn Voelckers is the founder and facilitator of Alone and Content, empowerment workshops for women and author of “Alone and Content,” a collection of inspiring essays for those who live alone. For information about her workshops, to purchase her book, or invite her to speak, visit www. aloneandcontent.com

sleep outcomes, researchers said.
Many
teens look at screens at bedtime, but some apps are more likely to keep them awake than others, leading to sleep problems.
That’s the upshot of a new study in which researchers found YouTube fans experienced consistent and neg ative effects on sleep. Surprisingly, traditional TV was associated with earlier bedtimes.
“We’ve been seeing teenagers who have sleep problems in our clin ic,” said co-author Michael Gradisar, head of sleep science at Sleep Cycle in Adelaide, Australia. “A lot of them have tried refraining from using technology, and clearly that hasn’t worked for them. Many of them mentioned that they would watch YouTube as they try to fall asleep. They find it entertaining without it
being overly stimulating.”
While many studies have been done on devices, little research has looked at the effects of specific apps on sleep, he said.
“We wanted to learn if there were specific apps that people should avoid, so that they could continue using their devices in a healthy way that didn’t affect sleep,” Gradisar said.
For the study, the researchers asked more than 700 12- to 18-yearolds how much time they spent using technology. That included mobile phones, gaming consoles and TV, as well as apps before going bed and in bed before falling sleeping.
While the study looked at the streaming service Netflix as well as YouTube, YouTube was the only app consistently and negatively related to
For every 15 minutes teens spent watching YouTube, they had a 24% greater chance of getting fewer than seven hours of shuteye. Watching YouTube and using gaming consoles both were associated with greater odds of getting insufficient sleep.
Contrary to the classic advice to keep TV out of the bedroom, tradi tional TV was associated with earlier bedtimes.
Gradisar said that might be because teens don’t interact with a TV in the same way they do with a phone. Instead, they just sit back and watch.
A half-hour in bed using phones, laptops, tablets and watching You Tube delayed lights out by seven to 13 minutes.

The issue with YouTube in partic ular may be that it’s so easy to finish
one video and click on a related one, said physician Alon Avidan, director of the UCLA Sleep Disorders Center.
Even homework done on screens late at night can be harmful, added Avidan, who reviewed the findings.
Watching Netflix was also asso ciated with greater sleepiness during the day.
Gradisar said one takeaway for parents is that not all technology use before bed is bad for their teen. Mom and Dad can also apply the findings to their own sleep health, he said.
“We often recommend that people do their own experiments with their tech use before sleep,” Gradisar said. “Find something that’s enjoyable so you don’t develop a bad relationship with your bed or bed room. The tech you’re using should be relaxing, but also be aware if it’s controlling your bedtime.”
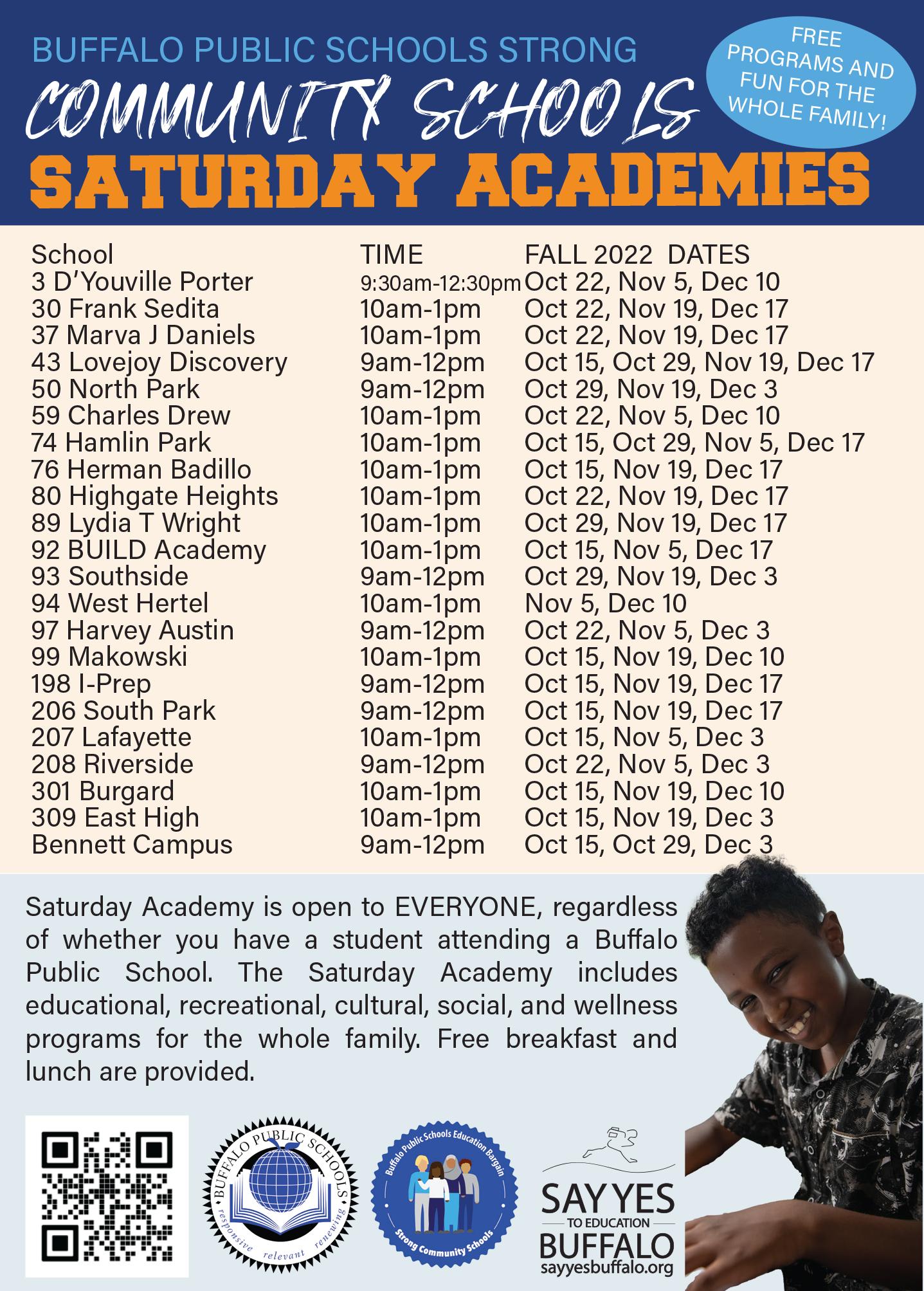
Practical tips, advice and hope for those who live aloneSay Yes Buffalo CEO and founding executive director discusses how the program works, its recently expansion in East Buffalo and how it has helped nearly 5,000 local students so far
By Brenda AlesiiWhat do you think is the cor rect answer to this question: Should barriers to educational and economic attain ment, workforce participation, and economic mobility for students in public and charter schools in Buffalo be removed?
The obvious answer? Say Yes!
Say Yes Buffalo is much more than just an answer to an obvious need for kids who need support to further their education through the use of locally funded tuition scholar ships.
With a strong focus on racial equity and inclusion, Say Yes Buffa lo’s mission is to provide a post-sec ondary tuition promise for all eligible charter and public school students in the city. This education-based ini
tiative is a multipronged partnership involving the Buffalo Public School District, parents, government repre sentatives, as well as business and philanthropic organizations, all in an effort to offer year-round support to students throughout their K-12 years and beyond.
In Good Health—Western New York Health Newspaper recently spoke with Say Yes Buffalo CEO and founding Executive Director David Rust, a St. Bonaventure alumnus, who recently announced the open ing of a new office in the heart of the Cold Spring business corridor on Jefferson Avenue.

Q. What are the minimum application requirements for students to achieve the dream of post-secondary education?


A. Our minimum requirements: students must live in Buffalo, attend eligible charter or public schools from grades 9 through 12, and apply for financial aid programs — TAP and Pell grants. In addition, students must enroll in our program within one year of graduation.
Q. Since the inception of Say Yes Buffalo some 10 years ago, how many students made it to college and what are some of the types of programs offered?
A. We have well over 2,000 stu dents who have benefited from our program, with another 2,400 in the higher education pipeline. A number of disciplines are offered: certificates, two-year degrees, or four-year de grees. Along with tremendous public support, we have a high level of par ticipation in our nationally renowned project. I expect growth to continue from year to year.
Q. With so many colleges and universities located in this region, do a lot of students stay local?
A. There are 21 colleges in our area, 85-90% end up staying local, attending schools we’re all familiar with — UB, Buffalo State, SUNY Erie, Villa Maria, Medaille, etc. Some of our students attend schools outside of Western New York, including Ivy League institutions.
Q. New York State Assembly Majority Leader Crystal Peoples-Stokes secured a $1 million capital grant to cover construction costs of your new location. She noted that race, zip code, income and other socioeconomic factors should not hinder furthering one’s education. Why was opening on Jefferson and Southampton in East Buffalo significant?
A. This simply would not have been possible without the invest ment and vision of Majority Lead er Peoples-Stokes. Thanks to her leadership, this beautiful office space will serve the entire city for years to come. Our mission is centered on investing in undervalued resources to make our community stronger, so opening up in a place that has seen so much disinvestment is meaningful for our entire team. We also want ed to invest in a neighborhood that represents the individuals we serve. That sentiment is more important than ever in light of the devastation following the massacre at Tops on May 14.
Q. How is Say Yes Buffalo funded?
A. We’ve had a number of angel investors working to build our scholarship endowment, largely supported by foundations, individ uals, businesses, and the state who believe in our work. These generous contributors recognize that a well-ed ucated populace with access to good jobs will improve the Buffalo Niagara area and help the region thrive.
Our programs are primarily funded by the Buffalo Public Schools, Erie County, the City of Buffalo, Medicaid and foundations (RCW JF, CFGB, JROF, Gates, HFWCNY, Cullen), and many others. These generous partners invest in public school-based supports, preparing students to access the scholarship upon graduation.
Q. With such a successful model, do you get approached by people in other cities who may want to use Say Yes Buffalo as a model for their community?
A. Yes, regularly, but Buffalo is our only focus.
Don’t miss the next issue of In Good Health. Some of the stories we’re working on:
■ Free online hearing tests you can take at home ■ Mistakes to avoid when choosing a Medicare plan ■
Top senior discounts to improve good health ■ Home sharing: A growing trend among baby noomers ■ Vistion awareness — How to stay sharp

To advertise in this special issue of In Good Health, please call 716-3320640 or send an email to editor@bfohealth.com


 By Deborah Jeanne Sergeant
By Deborah Jeanne Sergeant

Vegetarians may be at higher risk for hip fractures. A Uni versity of Leeds research paper compared the rate of hip fracture among 26,318 women who occasion ally eat meat; pescatarians, people who eat fish but not meat; and vege tarians.


Even after adjusting for factors like smoking and age, vegetarians evidenced a 33% greater risk of hip fracture in the median 22.3-years the women were followed for the study.
Because pescatarian and vegetar ian diets limit animal products, it can be challenging to get certain nutri ents in sufficient amounts for main taining bone health. The Leeds study was conducted in the UK where the fluid milk supply is not fortified with vitamin D. Most Americans who drink milk consume vitamin D-forti fied milk, which aids in calcium ab sorption. Few foods contain sufficient levels of vitamin D. The body gener ates vitamin D through sun exposure, which is limited in northern climates. Because vegans and some vegetari ans do not drink milk, they need to take vitamin D supplements or find other sources of vitamin D.

Mary Jo Parker, registered dieti tian in private practice in Williams ville, encourages vegetarians to look for alternative sources of calcium and vitamin D-fortified milk such


as dairy alternatives “such as soy milk and some almond and other milks (check labels for amounts and if fortified), tofu (it is packed in a calcium brine), and greens and green vegetables like broccoli, kale and spinach. Other vegetables, like Brussels sprouts and cabbage are not only sources of calcium, but vitamin K, which helps with bone density as well.”

She added that minerals like cal cium are not as available to the body when sourced from plants.


Adding supplements may be warranted. Parker also said that prunes, which are rich in vitamin K, can help increase bone density.
“Eating six per day were shown to improve density in studies,” Park er said.












Vitamin B-12 can be tough for vegans to obtain, as its main dietary




sources are from meat, such as beef liver (2,977 daily value per serving), tuna (385), and ground beef (100), although 2% milk (54) and eggs (19) offer B-12. Tempe (fermented soy beans) and shiitake mushrooms rep resent low-level sources of vitamin B-12. Non-meat eaters or minimal meat eaters may need to supplement with B-12.



Nuts and seeds are rich in miner als like magnesium, which also aid in absorbing calcium.
Although some foods may represent good sources of import ant nutrients, it is vital to not label some “super foods” while ignoring many other healthful foods. Justine Hays, registered dietitian and senior Snap-Ed nutritionist with Cornell Cooperative Extension in Niagara County, likes to see clients consume a wide array of foods to support good health.

“For all folks, we recommend a variety of calcium-rich foods, such as dark green leafy vegetables, fortified




juices, dairy and non dairy milks, and if a healthcare professional rec ommends, a calcium supplement,” she said.

A balanced, healthful diet can aid in avoiding hip fractures. However, building and maintain bone health also relies upon fitness to avoid falls. Practicing balance-dependent activities can help keep that sense sharp into later life. Strength training can also help build bone, as it stress es the areas where bone and muscle connect. More muscle mass also can provide more cushion to bones in case of a fall.
“Weight bearing exercise, such as walking, jumping, dancing, and using hand weights can also help strengthen bones,” Parker said.






Anyone who feels unsteady while standing or walking should seek a care provider’s recommenda tion in finding a balance class.





 Mary Jo Parker is a registered dietitian in private practice in Williamsville.
Justine Hays is a registered dietitian and senior Snap-Ed nutritionist with Cornell Cooperative Extension in Niagara County.
Mary Jo Parker is a registered dietitian in private practice in Williamsville.
Justine Hays is a registered dietitian and senior Snap-Ed nutritionist with Cornell Cooperative Extension in Niagara County.
To get the most out of ap ples, leave the skin on, as it con tains half the fiber and most of the polyphenols. Eat them raw, if possible, since cooking can deplete some nutrients. Wash all apples (including organic) before preparing or eating. Apples stored in the refrigerator can last six to eight weeks. Kept at room temperature, apples last about a week.
my kids were young, I used to call all fruit “na ture’s candy.” The nickname won them over, especially when it came to apples. As a family, we de voured apples by the bushelful!
Although the kids are long gone, apples continue to be my go-to fruit and here’s why: they’re delicious; they’re always available; they last forever in the fridge; and they’re loaded — absolutely, positively load ed — with powerful health benefits. Let’s begin with apple’s most bountiful nutrient: fiber.
Apples are a good source of both soluble and insoluble fiber, with one medium apple providing about 20% of our daily needs. Soluble fiber protects against heart disease by lowering bad cholesterol, while insoluble fiber keeps us regular and feeling full. Both fibers, along with an apple’s high-water content, help with weight control, which further benefits the heart by lowering the risk of high blood pressure.
Apples are packed with polyphenols, an import ant group of antioxidants that might help prevent cancer. Antiox idants protect our bodies from disease and accelerated aging by

neutralizing free radicals — harmful by-products of daily living— that can wreak havoc with healthy tissues.
Many studies suggest that eating an apple a day (or more) is associated with a reduced risk of certain can cers, including colorectal, oral, lung, prostate and breast cancers. Al though the results so far look prom ising, researchers point out that more studies are needed.
Eating apples may also reduce your risk of Type 2 diabetes, a chron ic condition that results in too much sugar circulating in the blood stream. Even though apples taste sweet, they have a low glycemic index, which means your blood sugar levels don’t spike when you eat them. Research ers at Tufts University found that people who ate one or more apples a day had up to a 23% lower risk of Type 2 diabetes than non-apple eat ers. Experts say the fruit’s fiber helps stabilize blood sugar, along with its high concen tration of antioxi dants.
Just under 100 calories, nutrient-rich apples are also a decent source of im mune-boost ing vitamin C and have no fat, cholesterol or sodium.
Dieters who believe that eating a big breakfast followed by a small dinner is the surest way to lose weight will likely be very dis appointed by the findings of a new, small study.

What did the researchers dis cover? Eating the largest meal early in the day is unlikely to make any difference.
“The notion of timing of eating to influence health has been around for a long time,” said study author Alexandra Johnstone, a registered nutritionist and professor in the school of medicine, medical sciences and nutrition with the Rowett Insti tute at the University of Aberdeen in Scotland.
Johnstone acknowledged that the advice to “breakfast like a king and dine like a pauper” has plenty of adherents.
And prior research has in fact “suggested that eating earlier in the day enhanced weight loss, affecting energy metabolism, compared to
eating later in the day,” she noted.
Still, “chrono-nutrition” — the relationship between food intake and time of day — “is a relatively young science,” Johnstone cautioned.
To try to separate myth from fact, she and her colleagues decided to conduct a diet test involving 16 men and 14 women. For a month, each participant was randomly assigned to follow a morning-heavy diet or an evening-heavy diet, the study authors explained.
All meals were based on a 30% protein, 35% carbs and 35% fat break down, while total daily calorie intake was fixed.
But those on the morning-heavy diet consumed 45% of their daily calories at breakfast, followed by 35% and 20% at lunch and dinner, respec tively.
In contrast, those on the eve ning-heavy diet followed a 20%, 35% and 45% daily calorie split.
At the end of the month, all participants took a one-week break,
Adapted from twopeasandtheirpod.com
Serves 4-6
Maple-mustard dressing:
¼ cup olive oil
1 tablespoon fresh lemon juice
2 tablespoons apple cider vinegar
½-1 tablespoon pure maple syrup
2 teaspoons Dijon mustard
1 clove garlic, minced Kosher salt and black pepper, to taste
Apple quinoa salad:

2/3 cup quinoa, rinsed
1¼ cups water
4 cups mixed greens
2 cups chopped apples
½ cup dried cranberries
½ cup crumbled goat, feta or Gor gonzola cheese
½ cup chopped walnuts Kosher salt and black pepper, to taste
which was then followed by a switch: for the following month all the morning-heavy eaters became eve ning-heavy eaters, and vice versa.
The result: “We found weight loss was similar with both diets,” Johnstone said.
All participants did lose a nota ble amount of weight, with an aver age loss of about 7 pounds during each of the one-month periods. It’s just that neither dietary pattern prompted more weight loss.
However, Johnstone and her colleagues did identify one big differ ence between the two styles of eating: diminished hunger among those on the morning-heavy diet.
While “there was no impact on energy expenditure,” she noted, “there was a positive influence of big breakfast to control appetite through out the day, with less hunger.”
And that could give a morn ing-heavy diet a leg up in the long run, she said.
“Hunger is one of the main reasons that people fail to comply to a weight-loss or calorie-restricted diet,” said Johnstone. “So if we have diet strategies that can help control hunger, then it would be beneficial in the real world.”
Johnstone and her team also
First, make the quinoa. Combine the quinoa and water in a medium pot. Bring to a boil, cover, reduce the heat and simmer for 15 minutes. Remove from the heat and let it sit, covered for 10 more minutes. Fluff with a fork.
While quinoa is cooking, make the maple-mustard dressing. In a small bowl, whisk together all the dressing ingredients. Set aside.
In a large bowl, add the mixed greens, cooked quinoa, apples, dried cranberries, crumbled cheese, and walnuts. Toss until the salad is combined. Then, drizzle with dressing (add the amount that suits you) and toss again. Season to taste with more salt and pepper, if needed.
Anne Palumbo is a lifestyle colum nist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

stressed that there is unlikely to be a one-size-fits-all approach to how dietary planning affects metabolism. Yet broadly speaking, “our work sug gests that the distribution of calories throughout the day does not influ ence energy metabolism or weight loss,” she said.
The findings were published online Sept. 9 in the journal Cell Metabolism.

DENT Neurologic Institute recently found that medical cannabis shows promising results as an effective treatment for Parkinson’s disease.
CannaBuff, a new magazine about the current and future industry of recreational and medical marijua na in Buffalo, recently published an article by Laszlo L. Mechtler, medical director of DENT Neurologic Insti tute Headache Center, Neuro-Oncol ogy Center and Cannabis Clinic.
Mechtler is also the chief of neu ro-oncology at Roswell Park Cancer Institute.
In the article, Mechtler explained about PD and the research so far on medical marijuana as an additional treatment option for patients.
PD affects around a million peo ple in the US. There are 60,000 new cases diagnosed each year. There is no cure and its underlying causes are not yet fully understood. It primarily affects those older than 55. It current ly costs the healthcare industry $52 billion a year and is projected to cost $79 billion per year by 2037 in the US alone.
“PD is classified as a common chronic neurodegenerative disorder characterized by motor dysfunction including bradykinesia (slowness of movement), rigidity, tremor, dyskine sia (involuntary muscle movements) and dystonia (involuntary muscle contractions),” Mechtler said.
In one DENT study, 87% of patients with a diagnosis of PD due to secondary conditions observed im provement in at least one symptom after initiating MC therapy. The three symptoms that demonstrated the most improvement were pain (61%), spasticity (58%) and tremor (48%).
Another study found a 22.2% reduction “in total on-period dys kinesia after receiving a synthetic cannabinoid similar to THC.”
THC (tetrahydrocannabinol) and
CBD (cannabidiol) are the two main cannabinoids in marijuana. Another study with patients receiving only CBD found significant improvements in sleep, hallucinations and illusions and delusions.
“A survey assessing the impact of MC on 47 PD patients found over all symptomatic improvement in 82% of patients, including improvement in tremors, muscle stiffness, pain, insomnia and/or mood,” he said.
Another survey-based study including nine PD patients who used cannabis “found patient-reported improvements in mood, sleep, motor symptoms and quality of life.”
DENT also found an additional benefit to medical marijuana: it helps patients reduce or end their reliance on opioid medications. In those patients with PD due to secondary conditions, “50% of patients using opioid pain medications were able to reduce their dose or discontinue treatment” using MC.
PD is caused by “a degenera tion” in the substantia nigra, a part of the brain responsible for producing dopamine. It affects many aspects of the central nervous system, including movement, cognitive executive func tion, and the fight or flight response.
Most of the PD medications used currently are to replenish this dopa mine and improve symptoms like rigidity and tremor.
“The problem is it’s not a cure. It’s like giving insulin to a diabetic to maintain their sugar control,” Mecht ler said.
These medications are also not without their side effects.
When used as an additional treatment, medical marijuana signifi cantly improves patients’ quality of life.
“[MC] helps not to cure the disease but helps with the symp tomatology. Most patients tolerated it extremely well and most came
back and said, ‘My quality of life has improved.’ And at the end of the day, when you’re a physician, and you hear these words: ‘I feel better. I sleep better. I have less anxiety, less stiffness. Then that’s a win-win situ ation,” Mechtler said. “Any time you treat a neurodegenerative disorder, a disorder that is progressive in nature, quality of life becomes of paramount importance.”
Experts are divided on its effi cacy; but Mechtler emphasized the importance of continuing studies like the ones being done at DENT.
He would like to do prospec tive, randomized studies on MC and other chronic diseases, but the legal restrictions placed on cannabis present what feel, in today’s day and age, like unnecessary roadblocks to life-changing information.

“As with most MC research, the overall number of studies evaluating its effects on Parkinson’s patients remains relatively low, due in part to cannabis’ classification as a schedule 1 controlled substance under fed eral law,” he said. “There is a need for large, randomized placebo-con trolled, clinical trials to fully under stand the efficacy and long-term effects of MC on PD before it can be officially validated as a treatment option.”
37 states have legalized medical marijuana. Medical marijuana has been legal in New York since 2014. As of 2021, New York joined the list of the 19 others that have legalized recreational marijuana. Its federal classification still lays out numerous barriers for clinical studies.
“For that reason, cannabis has not been accepted in the medical community because of the lack of quality research and that needs to change. I’m surprised it hasn’t changed.” Mechtler said.
These studies would help pave the way for additional research on medical marijuana, the benefits of which extend far beyond helping just those with Parkinson’s.
“Cannabis is not a treatment for all disorders,” Mechtler said, but the facts are there, and the numbers don’t lie.
“Does it improve quality of life? Unequivocally. Does it improve anxiety, sleeping patterns, pain and chronic inflammation? Yes,” he added.
The fact that it has shown a significant decrease in the reliance on opioids, in an opioid epidemic, is also a gift.
“Then you look at the other side of the coin: side effects. The side effects [of medicinal marijuana] be come minimal compared to the usual medications we take on a daily basis, which have a laundry list of side effects that are real,” Mechtler said.
In his experience, Mechtler has seen significant improvement in pa tients’ symptoms, not just in Parkin son’s, but in those who suffer from chronic illnesses like fibromyalgia, chronic migraines and even irritable bowel syndrome.
Mechtler continues to explore research under a hypothesis called endocannabinoid deficiency syn drome, studied by Ethan B. Russo, a board-certified neurologist, psycho pharmacology researcher and author.
The endocannabinoid system ex ists naturally in everyone’s body and, from a very basic standpoint, serves to stabilize stressors from life and maintain emotional, physical and mental homeostasis. The CED hy pothesis suggests that deficiencies in this system can cause several chronic, “treatment-resistant” diseases, as described in one of Russo’s studies.
By taking the cannabinoids from the marijuana plant and using them medicinally to supplement this de ficiency, symptoms improve great ly, the same way that Parkinson’s medications are used to supplement dopamine.
Mechtler hopes that this con tinued research will help to further legitimize marijuana in the medical community so that its benefits can be fully understood and utilized in addition to traditional treatments offered.
Laszlo L. Mechtler is medical director of DENT Neurologic Institute Headache Center, Neuro-Oncology Center and Cannabis Clinic. He is also the chief of neuro-oncology at Roswell Park Cancer Institute. Presented by:About80 autoimmune disor ders exist, depending upon how these conditions are classified.
Although affecting different areas and systems of the body, this group of disorders possess a few similarities.
Some share a few core symp toms, such as fatigue, body aches, fever, swelling, difficulty in focusing, weight fluctuation, and skin changes.
Most autoimmune conditions present with other specific issues. Some inexplicably go into remission and flare up later, but in most cases are lifelong upon onset. Medical care and good self-care can usually make living with an autoimmune condition much more comfortable. No cures exist for autoimmune conditions.
“The effects of having an auto immune disease extend beyond the physical symptoms, as depression and anxiety frequently co-exist with autoimmune disease,” said Molly Murray, president and CEO of the Autoimmune Association in Clinton Township, Michigan. “Autoim mune patients can feel stressed from navigating healthcare coverage and treatments, having to go to frequent medical appointments, and trying to balance their condition with other life responsibilities. They can feel isolated and misunderstood and can grieve the lifestyle they had before their diagnosis. Autoimmune patients should know they are not alone. Mental health providers can
provide coping tools and we encour age everyone to share their stories and connect with other patients.”
Some autoimmune conditions are “invisible” and can be mini mized by outsiders. Crohn’s disease and colitis cause diarrhea, urgency, abdominal pain/cramping, bloody stool, fatigue and weight loss and “it is not just ‘tummy pain’ or diarrhea,” said Becky Johnson Rescola, vice president of Education and Commu nity Engagement at the Crohn’s & Colitis Foundation in New York City. “Many people don’t understand the fatigue, chronic pain, and day-today accommodations that are part of coping with these diseases.”
The organization operates a chapter in Rochester that serves all of Western and Central New York.
Celiac disease is another example of an autoimmune condition. Joanne Hameister, a retiree in East Aurora, was diagnosed in 1985. She found ed WNY Gluten Free Diet Support Group (www.glutenfreeinwny.com).
“I had all the symptoms 30 years,” Hameister said.
These include abdominal cramping, amenorrhea (absence of menstruation), anemia, bloating and distention, brain fog and inability to concentrate, canker sores, constipa tion, dental abnormalities, diarrhea, edema and swelling, electrolyte im balance, fatigue, headaches, pain in bones and joints, vitamin and miner al deficiencies, vomiting and weight loss or gain. Celiac disease damages
the villi in the small intestine when ever gluten is consumed. Gluten is a protein naturally occurring in wheat and rye that is harmless to most people.
She tried eight gastroenterolo gists, one of whom accused her of being a hypochondriac and sent her to a psychiatrist. A biopsy—not the current blood test—finally uncov ered the truth when she was in the hospital on an IV after a 40-pound weight loss.
“My doctor said, ‘I have good news and bad news. The good news is, we know what you have, celiac disease. The bad news is, I have no idea what that is,’” she said.
A dietitian helped her better un derstand how she could avoid foods with gluten and how that affects her health.
At first, eating out and finding safe foods was very difficult, as few people understood how sensitive Hameister is to gluten. For example, using the same utensils for foods containing gluten and her gluten-free goods can cause contamination. Even while taking this level of precaution, she lost all the villi in her small in testine in 1992 and nearly died. For a year, she had to receive IV nutrition.
She said that for a time, she felt like her body betrayed her by not do ing what it should. Initially, she was treated like a “fussy eater” because she could tell what foods tended to bother her. For years as a young adult, she kept three sizes of clothing in her closet—4, 6, and 8—for her fluctuating weight.
“I’m so used to it now,” she said. “You have to be careful. Right now, my whole kitchen, except dog food, is gluten-free.”
By eliminating gluten from her diet, she can control her condition.
“I feel pretty good now,” Ham eister said.

• Rheumatoid arthritis, in which the immune system destroys the joints, followed by the organs.
• Psoriasis/psoriatic arthritis causes skin cells to build up and form inflamed scales on the skin. About one-third of people with psoriasis also have psoriatic arthritis.
• Multiple sclerosis attacks the myelin sheath which surrounds the central nervous system’s nerve cells, slowing impulses from the brain to the body, resulting in difficulty in movement.
• Systemic lupus erythematosus causes joint pain, severe body fatigue and skin rashes.
• Inflammatory bowel dis eases include Crohn’s disease, inflaming any portion of the GI tract and ulcerative colitis, which affects the colon and rectum.
• Addison’s disease affects the how much hormones the adrenal glands produce, which regulates how the body uses and stores carbohydrates and regulates sodium in the blood stream.
• Although in different ways, Graves’ disease and Hashimoto’s thyroiditis affect the thyroid, a gland important for controlling the metabolism.
• Sjögren’s syndrome attacks the glands that produce saliva and tears, meaning the patient experiences dry eyes and a dry mouth.
• Celiac disease causes the immune system to attack and inflame the small intestine whenever the patient eats foods containing gluten, a naturally occurring protein in wheat and rye. Gluten is not harmful to people without celi ac disease or sensitivity. Gluten sensitivity is not an autoim mune disease.
Joanne Hameister is a retiree in East Aurora who was diagnosed with Celiac disease in 1985. She founded WNY Gluten Free Diet Support Group.Tal said 60% of people stop their breastfeeding journey sooner than planned. There are multiple reasons that this happens.
Breastfeeding
is one of the most healthy things a mother can do for her newborn baby. It helps create a deeper connection between mother and child and provides chil dren the vital nutrients they need for surviv al and growth. It’s also something that doesn’t always come natural to everyone and can provide stress for a new mother if her intention was to breastfeed. Nearly two out of three infants are not exclusively breast fed for the initial recommended six months, according to the World Health Organization.
“Breastfeeding is one of the best things you can do for your baby. It sets up the baby and mother in so many ways,” said Elana Tal, an ob stetrician-gynecologist at University at Buffalo Jacobs School of Medicine & Biomedical Sciences.

Tal discusses five aspects of breastfeeding information.
When it comes to breastfeed ing, myths run rampant. Common ones include the notion that breast feeding hurts and a laundry list of certain foods to avoid while breast feeding.
“Mothers are concerned that it is going to be difficult, time consum ing and painful,” said Tal. “That is a myth we want to dispel because a
good and healthy latch should not be painful. It may have challenges, but that is why there are many good resources and lactation consultants that can help.”
Another myth she wants to dis pel occurs about breast milk produc tion and nourishment.
“There is also a worry that de pending on their breast shape or size, they won’t be able to provide enough milk and nutrition. However, breast milk can provide the full nutrition that is necessary for the baby,” she said.
There are many benefits of breastfeeding, for both the lactating parent and infant. Breastfeeding can help protect babies against some short- and long-term illnesses and diseases. Maternal health benefits of breastfeeding include reduced risk of breast and ovarian cancer, Type 2 diabetes, and cardiovascular disease. Recovery from childbirth can be quicker and with less risk of heavy postpartum bleeding.
“Breastfeeding lowers a baby’s risk for common health problems such as ear infection, respiratory issues and non infections such as asthma, obesity and sudden infant death syndrome,” said Tal. “For the mother, it can also lower chances of stroke, diabetes and depression.”

“Anything from not having a supporting workplace environment that allows you to pump to not asking for help early in the hospital or a lactation consultant if it becomes challenging after you leave the hos pital. You can’t be afraid to ask for help. We also tell mothers you need to identify people in your life that can give you support at home if it be comes challenging and help encour age you,” said Tal. “I want to sup port anyone who wants to achieve breastfeeding. But if for whatever reason you can not breastfeed there are alternatives. Nothing competes with having parents who love and support their child so it is important not to pass judgment either way.”
Current evidence suggests that breast milk is not likely to spread the virus to babies. If you have COVID-19, wash your hands before breastfeeding and always wear a mask within six feet of your infant. Get a lot of rest and take good care of yourself. Follow CDC recommenda tions regarding isolation from others.
“It is safe to continue to breast feed. We recommend the mother wear a mask and wash their hands before and after handling the baby,” she said.
If you do not develop symptoms, get tested at least five days after you last had close contact with someone with COVID-19.
The World Health Organi zation and the American Academy of Pediatrics recommend infants are exclusively fed breast milk for the first six months of life, then continue breastfeeding along with introducing appropriate complementary foods for up to 2 years of age or longer.
“Breast milk is the best nutrition for babies especially in the first six months of their lives,” said Tal. “In those first six months, they don’t need any other food or water because it provides everything they need to grow in developmental ways. The data we are getting on the benefits is why health experts are recommend ing breastfeeding longer as much as two years.”
study hands parents what seems like a miraculous gift: A simple, free technique that takes just 13 minutes to put wailing infants to sleep.
Researchers in Japan found that walking around while carry ing infants for five minutes calmed the newborns, while another eight minutes of sitting while holding the sleeping babies quietly made the transfer to a crib a smooth one.
The team studied the calming process using a baby ECG machine and video cameras to compare changes in heart rate and behavior as 21 mothers performed some activities that are common for calming infants. These included carrying the babies, pushing them in a stroller and hold ing them while sitting.
The researchers were able to record detailed data from babies who were crying, awake and calm, or sleeping. The idea was to track changes in both behavior and physi ology with great precision.
The team found that “walking for five minutes promoted sleep, but
only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” said study author, physician Kumi Kuro da, from the RIKEN Center for Brain Science in Saitama, Japan.
Regardless, all the babies in the study had stopped crying by the end of the five-minute walk and had lowered heart rates. About half were asleep.
The study found that babies were extremely sensitive to all move ments by their mothers, their heart rates changing when their mothers stopped walking or just turned. The most significant event that disturbed the sleeping infants happened just when they became separated from their mothers, pinpointing the prob lem of having a sleeping baby wake just as the infant is put down.
“Although we did not predict it, the key parameter for successful lay down of sleeping infants was the la tency from sleep onset,” Kuroda said in a RIKEN news release.
Specifically, babies often woke up if they were put down before they
got about eight minutes of sleep.
To fix the issue, Kuroda suggests mothers should carry a crying baby steadily for about five minutes with few abrupt movements, followed by about eight minutes of sitting before laying them down for sleep.
The study does not address why some babies cry excessively and can not sleep, but it does offer a solution that can help parents.
The findings were published Sept. 13 in Current Biology.
Elana Tal is an obstetrician-gynecologist at University at Buffalo Jacobs School of Medicine & Biomedical Sciences. “Breastfeeding is one of the best things you can do for your baby,” she says.TheFDA announced in June its approval of baricitinib (brand name Oluminant, among oth ers) to treat alopecia areata. Many people experience hair thinning and loss related to aging or medication.
Alopecia areata is different.
The autoimmune disease causes sudden, round patches of hair loss all over the head. The patches may grow in size and come and go in different areas over weeks and months. Alo pecia totalis means that all of the hair on the patient’s head falls out and al opecia universalis refers to complete bodily hair loss.
About 6.8 million Americans have alopecia areata.
“Patients seem to really like the
option of this medication if they’ve had this condition for a while and we’ve tried different treatments with them, like topical and intralesional steroids,” said Melissa Vaughn, nurse practitioner with Neiman Dermatol ogy in Buffalo. “Baricitinib is a great option. We’ve seen from the studies; it has good results.”
As with any medication, the office discusses with patients the side effects and their health history. As a janus kinase inhibitor, baricitinib affects the immune system. This class of medication requires an initial tuberculosis test and routine lab monitoring.
Side effects may include higher risk of infection, increased risk of
death for those 50 and older who al ready have one or more heart disease risk factors, possibly life-threatening blood clots and higher risk of cancer, especially for past or current smok ers.

Along with King, Louis J. Papa, primary care physician at University of Rochester Medical Cener (URMC), and Sherry Schaefer, founder of My Wig Coach in Penfield, Thea Chas sin, founder of Scarborough-based Bald Girls Do Lunch, appeared on Joan Lunden’s Second Opinion show airing on public television stations nationwide March 28, 2022.
Diagnosed in 1997, Chassin, founded awareness and support group Bald Girls Do Lunch, Inc. She decided that baricitinib is not right for her, but she can also understand why many women with alopecia areata feel eager to try it.

“The stigma of female hair loss is very big in our culture,” Chassin said. “Women feel less feminine and have concerns about their looks and acceptance should they choose to go without supplemental hair. There’s
a lot of worry about feeling normal and feeling they fit in. Our society prizes hair, not just in the US. Hair is a defining part of a woman in most cultures. A lack of hair is a very big deal. It affects self confidence and self-esteem.”
While Chassin appeared on Lunden’s program with her bare pate exposed, she knows that many wom en do not feel that is the right choice for them.
Beyond appearance, a lack of hair otherwise affects health. Without eyebrows and eyelashes, dust and sweat get into the eyes easier and mucus flows readily out of the nose without hairs to stop it. Chassin said that some people with alopecia areata have painfully brittle fingernails.

She views wearing wigs, scarves, hats, turbans or nothing at all on one’s head as daily choices that wom en with alopecia areata can make, depending on their situation or pref erence. Chassin’s hair fell out slowly in patches and in overall thinning for three decades. Eventually, it had fallen out to the point where it “was hair, but not a hairdo,” she said.
She likened her appearance then to Bozo the clown.
“When I shaved it off, I felt like a huge weight had been lifted off me,” she said. “It was truly a step forward to self-acceptance.”
She also felt a powerful sense of control over a situation which had previously spun out of control for years.
For women interested in medi cation, Chassin views baricitinib as “a game-changer. There are many people who have been waiting for a medication that they can try. Pre viously, the options were limited. It’s an opportunity for people to try something if they’re not contra indicated. It doesn’t work 100% in everybody, but for those who want to try it, it’s FDA-approved.”
 Thea Chassin, founder of Bald Girls Do Lunch in Westchester County, and Brett King, dermatologist with Yale School of Medicine. “The stigma of female hair loss is very big in our culture,” Chassin says.
Thea Chassin, founder of Bald Girls Do Lunch in Westchester County, and Brett King, dermatologist with Yale School of Medicine. “The stigma of female hair loss is very big in our culture,” Chassin says.
‘Patients seem to really like the option of this medication if they’ve had this condition for a while.’
Melissa Vaughn, nurse practitioner with Neiman Dermatology in Buffalo.
 By Deborah Jeanne Sergeant
By Deborah Jeanne Sergeant
Anyone who has received a clean bill of health after cancer treatments wants to maintain their good health.
Although nothing can guarantee cancer won’t come back, people in remission can certainly increase their chances of good healthy by taking a few steps.
“Survivorship is a key part of cancer care,” said Arnold Baskies, chairman of the Global Health Ad visory Council and past chairman of the board of directors, American Cancer Society, Inc. “The Commis sion on Cancer has recommended that all hospitals and providers pro vide a survivorship plan to patients. The American Cancer Society also recommends it. It includes informa tion on the treatment rendered and what should be done in terms of follow-up and surveillance.”
Since 14 million people in the US have survived cancer—and Baskies estimates it will likely swell to 20 million in the next five to 10 years— developing survivorship plans will only increase in importance.
“The specific recommendations are relative to the type of cancer and treatment rendered,” Baskies said. “A specific survivorship care plan should be personalized.”

For example, a colon cancer survivor may have scheduled colo noscopy and blood tests or for lung surgery, CT scans and other tests. General recommendations typically include healthful diet, exercise, stress management and smoking cessation.
Baskies noted that any time sur vivors change providers outside their health system, “they need to take with them the information of what
treatment they had and what needs to be done going forward.”
Mary Jo Parker, registered dieti tian in private practice in Williams ville, recommends that survivors focus on fruits and vegetables, whole grains, healthful sources of fat and lean protein sources.
“Limit sugars and processed and packaged foods,” she said. “The best eating styles are traditional Mediter ranean, DASH or MIND diets.”
One of her easiest tricks for ramping up the produce intake and eating a more balanced diet is to load half the plate at a meal with fruits and vegetables, fill one-quarter of it with a lean protein and fill the remaining quarter with a whole grain or starchy vegetable.
She also likes clients to drink at least 64 ounces of water and only healthful, non-sugar or artificially sweetened beverages like seltzers, tea or coffee but limited alcohol.
In addition to a healthful diet low in processed foods, red meats and dairy, Jennifer Wojcik, physician assistant and Survivorship Program director at Great Lakes Cancer Care in Williamsville, encourages clients to exercise.
“Get 150 minutes of moderate ac tivity a week with cardiovascular and weight bearing exercise,” she said. “Weight-bearing exercise is good for bone health, which can be an issue with a lot of cancer survivors as some treatments affect bones.”
Some cancers are hormonally driven. To help mitigate this effect, Wojcik said to maintain a healthful weight, as fat cells store hormones.
As a breast cancer survivor herself, Pamela Paplham of Getzville
speaks from firsthand experience with her patients. She is a doctor of nursing practice and advanced oncol ogy certified nurse practitioner and associate dean for clinical programs at UB.
“One of the biggest things I found to keep myself health is get ting a good night’s sleep,” Paplham said. “It’s underrated as far as how it contributes to people’s health. If I don’t get a good night’s sleep, I don’t have a good day the rest of the day.”
Since her experience with caner, she has become more conscious of exercising, reading food labels and monitoring her diet and watching her water intake. She likes journaling in a food diary where she can track what she eats and her fluids.
She encourages people who have recently completed treatments to “set small goals and reach that bar. They’ll feel much better about themselves. A lot of times, sometimes patients set goals that were great but a little too much for them. When they’d first go home after treatments rather than saying, ‘I’m going to walk to the end of the street,’ may be the first day, go to the end of the
driveway and maybe do that a few days; and then, three houses down. If they overshoot, they’ll feel lousy and down on themselves.”
Prostate cancer survivor Bill Krellner leads the Western New York chapter of Us Too, a prostate cancer support group. He encourag es any cancer survivor to faithfully follow through on all recommended checkups. For Krellner, that means having his PSA level checked, even though “I’m nervous about it,” he said. “Even after 17 years, I get con cerned. You’re never really out of the woods.”

That is why he believes it is so vital to join a support group and to find hobbies and interests that promote good mental health. He vol unteers at the VA two days a week, serves on a consortium at Roswell Park Comprehensive Cancer Center and leads Us Too. He also likes going for walks and boating and fishing at his cottage on Honeoye Lake.
“If you keep busy, those prob lems seem to disappear,” he added. “But helping other people is what really helps me. I get a lot of enjoy ment from it.”
Arnold Baskies, chairman of the Global Health Advisory Council and past chair of the board of directors, American Cancer Society, Inc. Bill Krellner leads the Western New York chapter of Us Too, a prostate cancer support group.Anew “WNY Cancer Snapshot: 2022” conducted by Roswell Park Comprehensive Cancer Center reports that while cancer incidence generally remains higher in this region than in the state and nationwide, both diagnoses of latestage cancer and deaths from cancer are decreasing as a whole.
The report cites effective out reach, education and access to cancer screening and treatment as factors.
“Education and outreach aimed at reducing cancer’s impact on our community is a hugely important part of what Roswell Park offers as a comprehensive cancer center,” says Roswell Park President, CEO and M&T Bank Presidential Chair in Leadership Candace S. Johnson, PhD. “We closely track statistics on how cancer impacts our community — and how it impacts distinct com munities differently — because that intelligence guides our strategies for advancing health equity and improv ing public health. And today we are proud to share this information with
our community.”
Johnson revealed the new re source at a recent press at Roswell Park with three public-health experts who helped compile and analyze the data.
“We’re encouraged by the overall picture we see from the data,” says Elizabeth Bouchard, Ph.D., senior vice president and associate director for community outreach and engage ment at Roswell Park. “Data like these help us understand where we are seeing improvement, and high light high-priority opportunities to save lives and improve the health of communities across Western New York.”
“WNY Cancer Snapshot” is based on publicly reported data, pri marily newly available information through 2019 from the NYS Cancer Registry, a resource maintained by the New York State Department of Health. Roswell Park’s analysis of the data shows that:
• Overall cancer incidence in WNY decreased by 1.1% between
Cancersurvivors all have a different story, as everyone’s journey in life and cancer is unique.
Nonetheless, most say their experience has given them a new perspective on life after undergoing the devastation of their diagnosis, the struggle to select their next step, their treatment and their recovery.
The support of family, friends and their medical team helped in ways they never expected.
In 2006, Mike Ameroso, now 81, received his prostate cancer diagno sis.
“I had no inkling I had any kind of cancer because I felt good,” the Amherst resident said. “He laid it on me, right out of the blue, ‘You’ve got cancer.’ My first thought was ‘How long have I got to live? When will I die?”
He received a second opinion at Roswell, where he also received his biopsies and eventually chose surgery. Attending meetings at Us Too, a support group for men with prostate cancer, helped arm him with information to proceed with prosta tectomy in 2007 at Roswell Park.
“My father had prostate cancer and the statistics show that it was in your family, chances are, you’ll have it worse,” Ameroso said. “My think ing was it won’t get better, so I had it
taken out.”
His surgery went well and he said that he experienced no pain and an easy recovery. Every three months, he has his PSA checked. It is slowly increasing, but he said that his providers chalk that up to his age and are not concerned because the number is moving so slowly.
Ameroso advises anyone newly diagnosed to get a second opinion from an expert in that type of cancer.
“Don’t just go by what your pri mary care provider is telling you,” he said. “Then, definitely educate your self on procedures and the different treatments such as being in a support group where you can meet a number of people who’ve been through this.”
Physician Steve Lipshultz, president of UBMD Pediatrics and chairman of pediatrics at UB, is a cancer survivor and a physician who pioneered the field of pediatric car dio-oncology.

His team studied the long-term effects of cancer-fighting drugs. Some of these drugs caused 10% to 15% of the children taking them to develop heart failure as adolescents or young adults. Lipshultz helped develop medication to prevent this side effect.
After decades of taking care of young cancer patients’ hearts, Lipshultz received a lymphoma diagnosis in 2000. He endured che
2014 and 2019, meaning that about 92 fewer people were diagnosed with cancer each year.
• Overall cancer deaths in WNY decreased by 8.8% between 2014 and 2019, meaning that about 246 fewer people in WNY died from cancer each year.
• Death rates from three of the four most common cancers in this re gion declined from 2010 to 2019: lung cancer declined by nearly 18%, from 52.4% to 42.9%; breast cancer from 22.9% to 20.6%; and colorectal cancer from 14.1% to 12.7%.
• Black Western New Yorkers are more likely to die from lung, breast, prostate, and colorectal cancer — per sistent disparities that remain despite the region’s overall improvement in cancer.
• From 2015-2019, across all races and ethnicities, incidence of the 10 most common cancers and deaths from nine out of the 10 most deadly cancers were higher in Western New York than in the state and/or nation wide.
Roswell Park has dedicated additional resources to cancer outreach and education over the past five years, and now has a staff of 33 specifically dedicated to improving access to cancer information, screening and pro active care across our region.
Over the last five years, Roswell Park’s outreach teams reached over 49,000 commu nity members through evi dence-based efforts — purpose ful outreach that is crucial for increasing access to prevention and early detection resources.
Roswell Park screens more than 10,000 people for cancer every year. Through its programs targeted to the most at-risk com munities, including the Witness Project, Esperanza y Vida and the CICR, Roswell Park also navi gates even more area residents to recommended screenings — with 4,400 people navigated to ser vices provided by whatever their provider of choice is since 2018.
“WNY Cancer Snapshot: 2022” is available for download on the Roswell Park website, www.roswellpark.org, then type “wny cancer snapshot” in the search menu.
motherapy, radiation, bone marrow transplant and three relapses. Despite these experiences, he said, “I was one of the lucky ones; God was watch ing over me” because at one point, he was told he had a less than 20% chance of survival.

Although many people have told him to take it easy, he said he has never worked harder as he wants to improve the care of his patients.
“I circled the drain but didn’t go down,” he said.
The brush with death reinforced to him how cancer devastates fami lies on so many levels.
“You never forget the families,” he said. “Every day is an anniver sary of a child lost to cancer from a family.”
Lipshultz feels that like any other cancer patient, he is a different per
son on the other side.
“The privilege of being able to serve I think to me enabled me not to dwell on it,” he said. “This interview is the most I’ve talked about it. I’ve dealt with the greatest modern mir acles in history and also stories you don’t wish on anyone.”
He has remained in good health since 2001.
Lipshultz encourages anyone newly diagnosed to build a good support system and to trust their medical team.
“Be able to be the patient and honestly share what you feel,” he said. “It’s appropriate to be scared and have uncertainty. You do your best as your doctors are treating your cancer to work to have the best other aspects of what you comfortably can do.”
In 2006, Mike Ameroso of Amherst, now 81, received his prostate cancer diagnosis. Steve Lipshultz, president of UBMD Pediatrics and chairman of pediatrics at UB, is a cancer survivor.


Can you recommend any services that check in on elder ly seniors who live alone? I live about 200 miles from my 82-yearold mother and worry about her falling or getting ill and not being able to call for help.
— Worrywart DaughterThere are actually several differ ent types of check-in services, along with some simple technology devices that can help keep your mom safe at home while providing you some peace of mind. Here are some top options to look into.
• Check-in app: If your mom uses a smartphone, a great solution to help ensure her safety is Snug (SnugSafe.com), a free app that would check in on her every day to confirm she’s OK. This app is used by thousands of elderly seniors who live alone and want to make sure that if something happens to them, their loved ones will be notified quickly so they can receive help in minutes, rather than days.
Here’s how it works. After downloading the app, your mom will choose what time(s) throughout the day she’d like for Snug to check in. Snug will send a push notification at those times asking your mom to check in by tapping the big green check button on her smartphone screen. If she doesn’t check in within 10 minutes or respond after multiple pings, Snug will notify her emergen cy contacts and share her last known location so that she can receive fast help.
For extra peace of mind, your mom can purchase Snug’s premi um plan ($10 per month) where in addition to notifying her emergency contacts, Snug will request an in-per son wellness check by a police officer who will visit her house to confirm she’s OK and provide assistance as needed. The app works with iPhone and Android smartphones.
• Check-in calls: If your mom doesn’t use a smartphone, another option to help ensure her safety is a daily check-in call service program. These are telephone reassurance programs usually run by police or sheriff’s departments in hundreds of counties across the country and are usually provided free of charge.
Here’s how they work. A com puter automated phone system would call your mom at a designated
time each day to check in. If she an swers, the system will assume every thing is OK. But if she didn’t pick up or if the call goes to voice mail after repeated tries, you (or whoever her designee is) would get a notification call. If you are not reachable, calls are then made to backup people who’ve also agreed to check on your mom if necessary.
The fallback is if no one can be reached, the police or other emergen cy services personnel will be dis patched to her home.
To find out if this service is avail able in your mom’s community, call her local police department’s none mergency number. You should also check with the local county office of the aging in your mom’s area — call 800-677-1116 for contact information.
If, however, her community doesn’t have a call check-in pro gram, there are businesses like CARE (Call-Reassurance.com) and IAmFine (Iamfine.com) that offer similar ser vices for under $15 per month.
• Technology devices: You may also want to invest in some simple technology aids to keep your mom safe. One of the most commonly used devices for this is a medical alert sys tem that cost about $1 per day. These systems come with a wearable “help button” that would allow her to call for help 24/7.

Another option that’s becoming increasingly popular is smart speak ers, like Amazon Alexa or Google Home. These devices work with third-party applications — AskMy Buddy.net and MySOSFamily.com — that would let your mom to call multiple emergency contacts with a simple verbal command.
And be sure to check out Ama zon’s Alexa Together (Amazon.com/ AlexaTogether), a new $20 month ly subscription service that helps families support and keep tabs on their older loved ones who live alone through an Alexa-enabled device.
Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.


The team at Roswell Park Com prehensive Cancer Center continues to grow, with three accomplished healthcare executives recruited to oversee key clinical and operational areas.
• Ronald Andro was promoted
and caregivers and adept at translat ing that focus into our services and workflows.”
Erie County Medical Center (ECMC) Corporation officials recent ly learned that the Uniform Data System for Medical Rehabilitation has ranked ECMC’s medical rehabil itation unit above the top 20 national trauma programs for case complexity and patient outcomes.
Ronald Andro
to chief clinical operations officer. He began his healthcare career as a registered nurse in the 1980s, spending the last three decades in executive-level leadership. He joined Roswell Park in January as interim chief clinical operations officer and has been appointed to the role perma nently following a national search. In this position, Andro provides over sight for numerous patient-care services, ensuring quality and safety at the highest levels. He holds a bach elor’s degree from Winona State University and master’s degrees from Rush University and the University of Alabama.
• Catherine Cowan has joined
The functional assessment spe cialists at the Uniform Data System recently issued the “Custom Report for M150.” The “Comparison of ECMC and Peers-Trauma-Related Cases,” Jan. 1, 2021 – Dec. 31, 2021, includes data for 884 medical rehabil itation unit (MRU) facilities in North America.
Mark A. LiVecchi, chief of ser vice, physical medicine and rehabili tation at ECMC, said, “This achieve ment reflects favorably on ECMC as an organization, along with several disciplines and individuals. Trauma services, emergency services, nurs ing, therapy, and administration have all played integral roles in achieving this accomplishment. This type of consistent achievement only occurs in the presence of true teamwork.” ECMC’s Center for Rehabilitation Services consists of a team of physi cians, nurses, psychologists, social workers, speech-language patholo gists, and occupational and physical therapists. Rehabilitation services at ECMC are provided at several levels of care to ensure that each patient receives the specific support they require to achieve better outcomes, whether recovery from trauma or im proved mobility after a minor injury.
ucation, where she served as fellow and senior vice for chapter program ming; the Erie County Department of Mental Health; and Niagara Falls Medical Center, where she was CEO.

Catherine Cowan
as vice president of payer rela tions. Partnering closely with the chief financial officer, Cowan will develop relationships with health plans and partners and lead negotiations on managed care contracts. Cowan brings over three decades of experience to Roswell Park, serving in several executive healthcare roles across Arizona, Texas and Oklahoma. She holds a master’s degree from the University of Texas Medical Branch.
• John Kuhns has been appoint
ECMC has cared for the high est percentage of complex trauma patients in its MRU for the eighth consecutive year. When compared with the top 20 MRU trauma pro grams in the “Comparison of Facility Characteristics and Outcomes–Trau matic Spinal Cord Injury (TSCI) January-December 2021 ECMC and Peers,” ECMC’s patient mix included 56.7% trauma patients, whereas the next closest facility included only 39.3% trauma cases. Further, for the TBI population, the values for the “Change in Self-Care Obs/Exp Ratio” and the “Change in Mobility Obs/Exp Ratio” indicate that on average the TBI patients at ECMC exceed the amount of change ex pected. Any value over 100% on the “Obs/Exp Ratio” measures indicates outcomes are better than expected.
“The national, third-party data confirms that ECMC’s rehabilitation team continues to deliver exceptional results in the care of complex pa tients,” said Thomas J. Quatroche Jr., Ph.D., ECMC’s president and chief executive officer.


After nearly three decades of
In this new role, Grant will oversee the Roswell Park CARES Program, which provides volunteers, financial support and project man agement to help area organizations meet community needs. Much of her work will focus on expanding op portunities for minority and women business enterprises (MWBE) and service-disabled veteran-owned busi nesses (SDVOB). She will also help to build and enhance partnerships with organizations and educators from underrepresented communi ties toward the goals of promoting sustainability, building health equity, supporting those who are marginal ized or economically disadvantaged and encouraging learners from un derrepresented groups to engage in STEM (science, technology, engineer ing and math) fields.
“We are so fortunate to have Dr. Grant leading our work in these critically important areas,” says Candace S. Johnson, Ph.D., president, CEO and M&T Bank Presidential Chair in Leadership at Roswell Park. “Her perspectives on healthcare, education and sustainable growth will be an incredible resource as we work to ensure that every Roswell Park program and initiative purpose fully supports diversity, equity and inclusion both within and outside of our center.”
John Kuhns
ed senior execu tive director of ambulatory services. Kuhns is responsible for both ambulatory clinics as well as locations in Amherst and Niagara Falls, ensuring the highest care for our patients at the downtown campus and beyond. He comes to Roswell Park with extensive knowl edge in employee leadership and management, and recently served in leadership roles in emergency and family medicine in the Boston area. He is a graduate of Northeastern University and the University of New Hampshire.
“This is an accomplished group of health care visionaries,” says Errol Douglas, Ph.D., chief human resourc es officer at Roswell Park. “Ron, Catherine, and John are great addi tions to our team because they are attuned to the needs of our patients
Roswell Park Comprehensive Cancer Center recently opened
The 11 Day Power Play Cancer Resource Center. The newly renovat ed space is located on the first floor of the main hospital and is a place where patients and their families can find information, support, comfort and connection at Roswell Park.

Services in the new space include patient education, wellness activities,
Ellen Grant
service-focused work in the fields of education, government, education and nursing, Ellen Grant, Ph.D., is returning to healthcare, joining Roswell Park Comprehen sive Cancer Center in the newly created role of executive director for corpo rate social responsibility and commu nity education.
A Buffalo native, Grant began her career as a nurse, and most recently worked as deputy mayor of Buffalo. Her previous experience includes leadership roles with Say Yes to Ed
Grant has made history in both her professional and her volunteer work. During her time with the Erie County Department of Health, she became the first African American appointed as the county’s commis sioner of mental health and the first African American elected as presi dent of the New York State Associa tion of Counties. Grant has received awards at the local and state level, including the Western New York Women’s Hall of Fame.
ty is amazing,” said Martha Hickey, manager of the resource center. “And knowing it is made possible by support from the community is even better.”
self-care and materials for entertain ment and comfort. This resource is possible thanks to donations to Roswell Park from The 11 Day Power Play organization.
To accommodate for the grow ing patient population and need for the services available in the resource center, Roswell Park expanded its footprint, also opening the Elevate Salon earlier this year. The 11 Day Power Play Cancer Resource Center will work in conjunction with the salon to offer wig and hair coverings to cancer patients experiencing hair loss due to treatment. In both spac es, visitors will feel the warmth and knowledge of our compassionate staff and volunteers.
“On behalf of The 11 Day Power Play organization and its supporters, we know this beautiful new space will provide the necessary respite, hope and resources cancer patients and their families need,” said Amy Lesakowski, co-founder and exec utive director of The 11 Day Power Play organization. “We are proud and honored to have it bear The 11 Day Power Play name.”
October 2022 • IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper • Page 19 Health News “Knowing our patients and their loved ones have a dedicated area at Roswell Park to seek relief, have a quiet moment, educate themselves on what’s ahead and connect with other people in the cancer communi
Wearable health technology is one way that people are beginning to take their health and wellness into their own hands—or eventually their ears and feet and every other part of the body imaginable.
These devices can increase lon gevity by improving health and pre venting disease, improve communi cation between doctors and patients and provide peace of mind. Incor porating them into our daily lives is a great way to track poor habits and begin and follow better ones.
They can increase productivity, boost self-esteem and facilitate a grounding sense of purpose.
Here are the latest trends in wearable health technology:
Apple Watch Series 8
This is the most comprehensive wearable device currently available when it comes to overall health. It covers sleep, menstrual cycles, blood pressure, emergency situations and more.
It can act as a sleep tracker, re cording time spent in different sleep stages. These stages are key to un derstanding and getting better sleep. It can help to keep a sleep diary as well, which is one of the first steps to practicing healthy sleeping habits.
A new temperature sensor re cords your temperature while users sleep, so users can see patterns over time. “Cycle tracking uses this data to provide a retrospective estimate of when you likely ovulated, which can be helpful for family planning. When combined with your heart rate and logged cycle data, you’ll get a de tailed view of your menstrual cycle,” Apple said.
With a blood oxygen monitor and electrocardiogram app, users can also stay on top of their heart health. Heart disease is the leading cause of death in the United States. Ad ditional features include crash and fall detection and other emergency services that give unparalleled peace of mind to users.
The Oura Ring focuses primarily on sleep health. It is a more discreet and lightweight option than the Apple watch.
Referred to as “a sleep lab on your finger,” this ring tracks your sleep quality and all four sleep stag es: Deep sleep (physically restorative stage), REM sleep (mentally restor ative stage), light sleep and awake periods. A daily “sleep score” is then provided based on personalized, re al-time data points: total sleep, REM sleep, deep sleep, timing, movement, heart rate, heart rate variability and more.
But how do knowing these things lead to better sleep and even tually better health? By learning a person’s unique sleep patterns, the app then shares personalized guid ance and reminders on how to get the best sleep every day. It might recom mend when to start winding down for bed, or what to avoid during that day, for example. It creates a person alized sleep routine based on what your body is already doing.
It allows you to keep track of daily and nightly activities or food and drinks you’ve had before bed to see how these things may impact you over time. It offers sleep sounds and stories for relaxation before bed and remembers those that may have helped someone fall asleep faster so it can be used again.
Quality sleep boosts immunity, helps with weight management, de creases the risk for heart disease and brain diseases like dementia, helps to manage stress and improves memory and productivity.
Fitbits by Google are wearable trackers that can help users stay on top of their fitness goals, monitor overall health and even manage stress. They track health metrics like respiration, blood oxygen levels and skin temperature “to uncover trends

and changes in your daily well-be ing,” Google said.
They can help detect and indi cate illness or hormone fluctuations, stress and fatigue. They provide a daily readiness score based on activity, sleep and heart rate, and will base exercise recommendations on a person’s daily readiness so that they can work with their body rather than against it.
Studies show that devices like Fitbit do motivate individuals to ex ercise more frequently and improve overall health. The American Medical Association said adults who take 8,000 or more steps each day have a lower risk of death from numerous diseases than those who take fewer than 4,000. The average American takes 3,000 to 4,000 steps per day.
Jessie Adamski, a close friend and fitness fan from Buffalo, is one of the first people I know who started using a Fitbit in 2016 when she stared her health journey. She still uses it today.
“It motivated me to live a health ier lifestyle,” she said. “I definitely saw an improvement in my overall health.”
She used the Fitbit in conjunc tion with a food diary app to track calories and make healthier food choices. “At one point I was able to lose 40 pounds in a year by tracking everything,” she added. “It kept me accountable for reaching my goals. My cholesterol levels improved as well as my energy levels. I wanted to get out and be more active.”
“I even got my dog, Ellie, a ‘Fit bark,’ which is basically a Fitbit for dogs. For the first couple years I had her, I made sure both of us reached our goals as much as possible by go ing on walks, to dog parks and play ing. I thought it was a cool thing to have and helped us both be healthy together. Even if people thought I was nuts,” she laughed.

There are currently medical technology companies working on designing smart clothing with sen sors attached to fabric or woven in
Jessie Adamski, a fitness fan from Buffalo, started using a Fitbit in 2016 when she stared her health journey. She still uses it today. “It motivated me to live a healthier lifestyle,” she says. “I definitely saw an improvement in my overall health.”
and even implantable and injectable devices. There is infinite potential for medical wearables in the future.
Eventually, they can detect and prevent medical emergencies and even directly communicate with hos pitals and doctor’s offices.
People should always consult a healthcare professional before making medical decisions and not rely solely on these devices. Ulti mately, health wearables bring peace of mind, inspire us to learn and love ourselves more and let us take control of the things that make us feel better.
Apple Watch: Prices, models and options range from $300-$800

Oura Ring: Starting at $300
Fitbit: Prices, models and options range from $70-$300