TikTok, Facebook, Reddit, Twitter and other social



platforms may have good information, but when it comes to healthcare, check other sites



TikTok, Facebook, Reddit, Twitter and other social



platforms may have good information, but when it comes to healthcare, check other sites


Abrisk 11-minute daily walk can help you live longer, a new University of Cambridge study reports.

Researchers found that 75 minutes a week — 11 minutes daily — of moderate-intensity physical activity is enough to lower a person's risk of heart disease, stroke and cancer.
The investigators estimated that one in 10 early deaths could be prevented if everyone got that amount of exercise, which is half the level recommended by U.S. guidelines.
“If you are someone who finds the idea of 150 minutes of moderate-intensity physical activity a week a bit daunting, then our findings should be good news,” co-researcher physician Soren Brage, of the Medical Research Council at the University of Cambridge in the United Kingdom, said in a university news release.


“Doing some physical activity is better than doing none," he added. "This is also a good starting position — if you find that 75 minutes a week is manageable, then you could try stepping it up gradually to the full recommended amount.”
disease and stroke) were the leading causes of death worldwide, responsible for nearly 18 million deaths in 2019. Cancers were responsible for 9.6 million deaths in 2017.

To examine how much exercise could make a dent in those numbers, the researchers pooled and analyzed data from 94 large studies involving more than 30 million people.
The findings showed that two out of three people don't get their recommended 150 minutes per week of moderate-intensity exercise, and fewer than one in 10 managed more than 300 minutes of activity per week.
Broadly speaking, the researchers concluded that getting more than 150 minutes a week of exercise produces marginal benefits in terms of reduced risk of disease or death.
But even half that amount came with significant benefits, the team reported.
For example, 75 minutes per week of moderate-intensity exercise reduced risk of early death by 23%. It was also enough to reduce the risk of heart disease and stroke by 17% and cancer by 7%.
For some specific cancers, the reduction in risk was even greater. Getting that amount of exercise reduced the risk of head and neck, myeloid leukemia, myeloma and gastric cardia cancers between 14% and 26%.
The researchers calculated that if people get their recommended 150 minutes of exercise a week, around 16% of early deaths would be prevented. In addition, 11% of cardiovascular disease cases and 5% of cancer cases would be prevented.
But if folks manage at least 75 minutes per week of moderate-intensity physical activity, around 10% of early deaths would be prevented. And 5% of cardiovascular disease cases and 3% of cancer cases would be prevented.
Further, moderate-intensity exercise doesn't require you to run yourself ragged, the researchers noted. It raises your heart rate and makes you breathe faster, but you'd still be able to speak during the activity.
Other examples include dancing, riding a bike, playing tennis and hiking.
“Moderate activity doesn't have to involve what we normally think of exercise, such as sports or running,” co-researcher physician Leandro Garcia from Queens University Belfast explained.
“Sometimes, replacing some habits is all that is needed,” Garcia added. “For example, try to walk or cycle to your work or study place instead of using a car, or engage in active play with your kids or grand
kids. Doing activities that you enjoy and that are easy to include in your weekly routine is an excellent way to become more active.”
The findings were published Feb. 28 in the British Journal of Sports Medicine.

Renier Brentjens, MD, PhD Deputy Director

Q: You’re now the chairwoman of the department of family medicine in the Jacobs School of Medicine and Biomedical Sciences after having held it as an interim position. What made you want to take it on long-term?
A: We can start with why I wanted to be the chair. It’s a bit of a lifelong professional dream. I started my career at Buffalo medical school and my residency out in rural practice for a little while. I’ve also been faculty at the school of medicine in different roles, roles that included the design of medical student education curriculum and the evaluation of that curriculum — essentially being the director of medical student education in the department of family medicine and the director of residency education in the department of family medicine. I had a good, professional relationship with the chair at that time. He was very solid in the role. His name was Jeffrey Thomas Rosenthal. And
I was called by a recruiter to serve as family medicine department chair at SUNY Upstate in Syracuse. So in 2006 I went to Syracuse and led that department from 2006 through most of 2011. I got married and returned to Buffalo for family reasons. I felt like I left the Syracuse department in pretty good hands.
Q: What happened when you came back to Buffalo?
A: When I came back to Buffalo, there was still someone in the chairman role. So I served under the title of associate dean of student affairs. What that basically is is a guidance counselor of sorts for medical students, counseling students if they’ve had any economic difficulty and, more importantly, counseling students and helping them if they’ve had academic difficulty and, most importantly, helping them launch from medical school to a residency
program. I’d write what’s called a dean’s letter, which is an institutional transfer letter. I served in that role for 10 years, until the end of 2021. The chair of the department announced he was stepping away from the position after eight years in the role. So it was at that time, immediately post-pandemic, I said I’d be interested in the role, put together a proposal and was appointed the interim chair of the department of family medicine. A few months later the dean changed. I let her know I’d be happy to stay on permanently. There was so much influx in the medical school at the time that I think she was happy to have some stability. So that’s how I got here, long story. I have the experience of having been a chair even though the department in Syracuse is much smaller, but I also have a track record at Buffalo.
Q: Can you tell us some more about your curriculum development?
A: Approximately 24 years ago there was an effort to update the curriculum. There had been a course we might call, in a friendly way, Doctoring 101. It began in the second year of medical school. So I led the design of clinical skills course for first-year students. In other words, while they’re learning the hard sciences, at the same time they’re learning how to communicate with the patient, take medical history, do a physical examination. That was the goal of the first-year course. We weren’t teaching them how to differentiate between heart murmurs; we were making sure they knew how to put the stethoscope in the right place, to be able to conduct a physical examination on a healthy patient. The course incorporated some lectures, small group learning and working with standardized patients. These are people who are basically actors who are trained to act like patients. So the students and their colleagues could get together and practice their examination skills. And we took it farther in the assessment part of the course, which would happen in an examination room with faculty looking on and evaluating them.
Q: You have a background in caring for complex medical conditions. What kinds of things does that include?

A: That includes a complexity in any given individual. So it’s not a specific disease that’s complex but, for example, taking care of a senior citizen Medicare patient who has a long list of medical problems. I think the single most important thing in family medicine and primary care is to take a very patient-centered approach to care, taking care of the patient and their family within the context of their family and community.
Q: When it comes to preventive care, lifestyle changes always seem like the hardest to implement. Is there an effective strategy you’ve found for helping patients make those changes and getting results from them?
A: I think it’s respecting the patient, respecting their goals and their capacity and coaching and guiding them into a healthier life year over year. I’ve been known to say to people that I want to see that they’re healthier this year than they were last year. And maybe that’s medically healthier: their numbers are better. But it could also mean that they’re happier. That they’ve made some dietary changes. That they have a bit
more activity in their lives. Gaining a calendar year doesn’t necessarily mean that they’ve lost a year of health.
Q: The pandemic was a bit of a disaster when it came to managed conditions and screenings. How have you gone about getting people whose conditions have decompensated back to health?
A: So I can speak primarily for our private practices: we were up and running telehealth visits on patients within 10 days of closure. So although people might think that can’t work across a computer screen, but if you’ve known the patient for many years you can still do all the history taking and ask them questions like you could in office. On top of that, most of the patients had a smartphone and could hold their phone to their ankles to show me if they had swelling. They could hold the phone to a knee if they had an injury, to a rash. It was obviously imperfect when it came to listening to heart and lung sounds. It was very good for looking in the mouth. It was impossible to look into an ear or palpate a lymph node. But there was so much that you could do.
Q: Were there any surprises with telehealth?
A: A hidden and unexpected benefit was that you were making a pseudo-health call. You could get a sense of the patient’s living circumstances. I recall having a telehealth visit with a single mom who was working from home, had a child in a playpen, another in her arms. So it increased the understanding of home life and community life.
Q: As a physician, what can you do with that information?
A: The first thing is to be supportive. “It looks like things are stressful in your home right now, is there anything we could do to help you manage your work?” And then, in the long run, when you see them back in the office you remember what you saw and you have the context of those pseudo-health calls to their ongoing care. Yes, some people gained weight during the pandemic. Most people maintained their medications and prescriptions. Some people actually improved their health and started running for the first time, or were able to use the exercise bike in the next room on their breaks. Some of them may have started cooking for themselves for the first time instead of eating at restaurants. So it was a mixed bag.
Name: Andrea T. Manyon, M.D.
Positions: President of UBMD Family Medicine and chairwoman of the department of family medicine at the Jacobs School of Medicine and Biomedical Sciences at the University of Buffalo
Hometown: Williamsville
Education: University at Buffalo
Affiliations: Erie County Medical Center; Kaleida Health
Organizations: Society of Teachers of Family Medicine; Association of Departments of Family Medicine
Family: Married, blended family with eight children, three grandchildren
Hobbies: Activities at Greek Orthodox Church; sewing; cooking

Pedestrian deaths have surged on U.S. roads in recent years, and they are climbing again.
Pedestrian deaths hit a 40-year high in 2021, and numbers for the first half of 2022 were up about 5% over the same period in 2021, according to a new Governors Highway Safety Association (GHSA) analysis.
It cites a variety of contributors, including heavier vehicles that are more likely to injure or kill people on foot. Roads, meanwhile, are designed to prioritize fast-moving traffic over the slower speeds that are safer for pedestrians, according to the GHSA.
Many parts of the United States lack adequate sidewalks, crosswalks and lighting, the group noted.
In addition, dangerous driving surged at the start of the pandemic and has not abated.
“There is a pedestrian safety crisis on our roads, and it's only gotten worse since the start of the pandemic,” Jonathan Adkins, chief executive officer of GHSA, said in an association news release. “A single roadway death is tragic. But it's absolutely mind-boggling and heartbreaking that drivers are killing an average of 19 pedestrians every single day.”
GHSA's annual Spotlight on Highway Safety report is based on preliminary data from state highway safety offices.
GHSA said the increase is even more alarming compared to 2019, before the pandemic.
Between the first half of 2019 and 2022, pedestrian deaths surged 18%, the GHSA found. The numbers

showed 1.04 pedestrian deaths per 100,000 people in 2022, up from 0.9 per 100,000 in 2019.
There were 168 more deaths during the first half of 2022 compared to the first half of 2021, the findings showed.
“The only way to reverse this awful trend is to do more of everything that works — more and better designed infrastructure to keep people walking safe, equitable enforcement of traffic safety laws to stop dangerous driving and engaging more communities where the impacts of this crisis are felt the hardest,” Adkins said.
The GHSA said it supports a solution based on the safe system approach outlined in the U.S. Department of Transportation's national roadway safety strategy.
Its elements — safe road users, safe vehicles, safe speeds, safe roads and post-crash care — provide a multilayered safety net to protect people on foot as well as other road users, GHSA said.
The reported increases continue a decade-long trend.
In the first half of 2013, the United States recorded 2,141 pedestrian deaths — compared to 3,434 in the first half of last year. That's a 60% increase and nearly 1,300 more people killed.
The U.S. National Highway Traffic Safety Administration (NHTSA) reported that 2021 also saw the most roadway deaths since 2005, about 43,000.
Editor & Publisher: Wagner Dotto
Writers: Deborah J. Sergeant, Jim Miller, Gwenn Voelckers, Anne Palumbo, Brenda Alesii, Ernst Lamothe Jr., George Chapman, Christ Motola, Jane Schmitt


Advertising: Anne Westcott, Amy Gagliano, Pam Roe

Anew prevention-based, consultative service at Child Care Council Inc. will help ensure children with disabilities have access to quality child care.

Child Care Council’s special needs consultation service will equip caregivers with strategies and supports to reduce suspension and expulsion for young children with disabilities in child care. Built on relationship-based practices, the service is provided through observation, modeling and collaboration.
According to a 2018 article by the Center for American Progress, “Suspensions Are Not Support,” children with disabilities in early childhood settings represent about 13% of enrolled children but account for 75% of suspensions and expulsions.
Children with autism are the most likely to be suspended or expelled, according to Child Care
Council, which served 125 families who self-reported at least one child was diagnosed with autism spectrum disorders between January 2016 and December 2019.
Child Care Council’s team of special needs consultants will provide a caring, compassionate, responsive and effective service to meet each program and child’s unique needs. The special needs consultation service is funded by a $175,000 grant from the Mother Cabrini Health Foundation.
The service, which does not provide one-to-one care to children, is available in Monroe, Wayne and Livingston counties.

Child care providers interested in learning more about this service can contact Bethany Williams, special needs services supervisor, at 585-6541287 or b.williams@childcarecouncil. com.
Medical debt has become the No. 1 contributor to personal bankruptcy. Over 100 million of us have significant medical debt. The Consumer Financial Protection Board issued a letter to the IRS outlining its recommendations to give indebted consumers relief.

1. Debt resulting from necessary medical care kept off credit reports.
2. Ban hospitals from selling patient debt to collection agencies. 3. Require hospitals to increase their financial
assistance and charity care as they are tax exempt. 4. Establish standards for charity care. (NYS has a “bad debt and charity pool” that can compensate hospitals for charity care, but it is basically underfunded and pays only a fraction of charity care.) More than two-thirds of hospitals sue their patients or take other legal actions. The collection industry has pushed back saying these consumer protections will only hurt their provider clients.
infections further reducing the strain on overtaxed and understaffed hospitals. I understand while they are at it, they can help set up your TV.
In what is probably a sign of the times for the hospital industry, the Michigan-based 100 bed hospital system lost nearly $300 million in the second half of last year. St. Joseph’s in Syracuse and St. Peter’s in Albany are affiliates. The pandemic has created a “new normal” for hospitals, meaning inpatient revenues will continue to be a declining percentage of overall revenues. The innovative hospital-at-home program discussed above, born out of necessity, exemplifies the rapid transition to cheaper non-inpatient settings such as home care, ambulatory care, digital/virtual care, urgent care, remote monitoring and pharmacy care.
The pandemic has been debilitating impact on care givers. A recent survey of more than 9,000 physicians by Medscape revealed 25% of the respondents indicated they suffered from clinical depression and 9% indicated they had suicidal ideations (versus 5% of the general population). 40% of the docs surveyed admitted they have not shared their thoughts with anyone, let alone sought professional help. A legitimate fear of disclosure is the possibility of an untoward or punitive action by a medical board. Clearly, the pandemic has increased depression and anxiety in all of us. But when it severely impacts those who battle on the front lines, we are all in deeper trouble. Many of the respondents felt our fractured healthcare “system” continues to contribute to the depression and anxiety felt by patients and physicians alike.
They are typically located in isolated rural communities and underserved urban neighborhoods. Consequently, they serve a relatively higher percentage of patients with Medicaid insurance or no insurance at all. Consequently, these hospitals, so critical in providing care to underserved populations, receive “disproportionate share payments” to help them maintain fiscal viability. Congress is now threatening to cut $8 billion in DSP to these safety net hospitals. At least nine hospital and medical associations have petitioned congress to maintain the funding needed to keep these hospitals open. Still reeling from the negative impact of the pandemic, the $8 billion cut could not come at a worse time.
Industry analysts predict dozens of these hospitals, already on the brink of financial crisis, could close.
In what is certainly innovative, Atrium Health has partnered with Best Buy, (yes, Best Buy) to provide what they call “hospital-at-home” care. It was born out of the pandemic which undoubtedly strained inpatient care. According to Rasu Shrestha, the chief “innovation and commercialization” officer (yes, commercialization) the program has served more than 6,000 patients at home saving the insurer 25,000 inpatient days. Initially serving mostly patients suffering from COVID-19, they now treat chronic heart problems, COPD, pneumonia, asthma and
Thanks to the Inflation Reduction Act, effective Jan. 1, Medicare members with Part D (drug) coverage will pay no more than $35 a month for insulin. The rest of Medicare recipients, all of whom have Part B (physician) coverage, will pay not more than $35 a month effective July 1. 34 million of us, or one in 10, suffer from diabetes. Drug manufacturer Eli Lilly will voluntarily slash its price for insulin. Mark Cuban’s company will follow suit as well as nonprofit Utah based Civica. Diabetes is one of the fastest growing chronic conditions in younger Americans. The Inflation Reduction Act also permits Congress to negotiate the price of 10 selected drugs starting in 2026. That’s right. JUST 10 drugs. THREE years from now. But that “leaps” to 20 drugs SIX years from now. Cynics worry, and with good cause, drug manufactures will simply raise prices on the myriad other drugs where prices aren’t negotiated. Optimists hope the insulin price competition will infiltrate the industry and finally result in more price competition outside negotiations. It is estimated that 44% of us don’t fill prescriptions, or reduce dosages and cut pills, due to cost.
It is expected to be near depletion in just five years. This is a concern for all of us, both younger than and older than 65. Medicare taxes have been subtracted from our paychecks since we started collecting one. President Biden is proposing to raise the Medicare tax rate from 3.8% to 5% on those making more than $400,000 a year. Analysts believe that certainly will help, but not make Medicare totally solvent. Negotiating ALL drug prices immediately, not just 10 prices in 2026, will make Medicare solvent. It should be noted, Medicare (basically congress) SETS fees/reimbursement for physician and hospital services. While provider lobbyists can plead, there are NO formal negotiations.
George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.

According to a 2022 study commissioned by CharityRx of 2,000 U.S. adults, Americans turn to social media influencers for advice on anxiety (34%), weight loss (34%) and depression (33%), each of which represents the most common sources of information on these topics.
The study also relates that nearly 20% of Americans trust health influencers more than their local medical professionals and one in five rely on TikTok videos before seeing a doctor when they seek treatment for a health issue.
Karl Shallowhorn, credentialed alcoholism and substance abuse counselor and director of youth programs at Mental Health Advocates of Western New York in Buffalo, acknowledges that “there’s a lot of good information online, but is it an accurate source, or Joe’s blog or a TikTok video?” he said. “Is this person a credentialed individual with experience? A peer can provide good information, but when a person is talking about themselves, where is it coming from? It doesn’t necessarily mean that it’s scientifically based or research based. I encourage people to seek out resources to make sure there’s research behind it.”
The lack of accountability or verification with personal information make it less reliable and most likely based upon anecdotes than information from organizations and from professionals in that specialty. Add to that tendency the anecdotes offered by social media influencers and many people looking online — especially young people who are less experienced in research — may find false information. Random posters have no oversight or accountability.
Shallowhorn said that “contagion behaviors” such as self-harm is prevalent on social media, especially with young people.
It is also easy to get caught up in self-diagnosis for those exhibiting symptoms.
“If you know what you’re looking for, you’ll probably find it,” he said.
Oftentimes, patients research their symptoms online to self-diagnose before seeing a provider. Although research can help generate more in-depth questions if patients then see a provider, some people try home remedies or otherwise delay important care because of a false
diagnosis.
“It’s almost human nature,” Shallowhorn said of this tendency. “You can read into information however you want and find a way to identify yourself. It’s one of the dangers of the internet.”
Online quizzes can falsely lead participants to think that their unrelated symptoms add up to something serious. Although some healthcare providers may use an evidence-based questionnaire to help patients better express their symptoms and their severity, online quizzes about symptoms tend to ask too few questions and derive inaccurate conclusions.
Shallowhorn said that his organization provides an online screening tool for mental health operated through Mental Health America. But screening tools help participants consider reaching out to providers, not attempt diagnosis.
Shallowhorn recommends the websites of the National Institutes of Mental Health, American Psychological Association, and those of college and universities.
News articles from reputable organizations hold weight, as journalists are held to ethical and professional standards requiring finding reputable sources and quoting them accurately. Before publication, books and reputable periodicals fact check and ensure that the information is correct and up to date. Few such checks exist on social media.
TikTok’s content — along with a good share of other social media — is for entertainment purposes or at best anecdotal examples, not healthcare information that applies to the general population.
“As a general rule, don’t listen to people if they’re not famous for knowing about medicine,” said physician Steven Dubovsky, president of UBMD Psychiatry, professor and chair of the Department of Psychiatry at Jacobs School of Medicine and Biomedical Sciences at University at Buffalo.


Even when finding good sources, it is important to make sure it is upto-date and to interpret it correctly.
“If you don’t know how to interpret it, you can draw the wrong conclusions,” Dubovsky said. “On the CDC site, you may learn information about treatment for a condition, but not about do you have that or the best treatment.”
He does see merit in learning
about conditions to gain background information. However, the application of health information is best in the hands of medical providers.
Another provider who likes to see patients learn about their health is physician John Fudyma, who holds a master’s in public health and serves as interim division chief of General Internal Medicine at UBMD Internal Medicine and associate professor at Jacobs School of Medicine and Biomedical Sciences, University at Buffalo.
“I encourage patients to go and look for information on their own regarding their condition so they’re an educated patient. The key is finding sites that are reputable,” Fudyma said.
He recommends the Cleveland or Mayo clinic websites or similar, reputable institutions. Although research papers are widely available online, it can be difficult to determine what they mean. Fudyma said that these can even become stress and anxiety generating if they do not understand the science behind them. Some studies are based on small populations and groups of people who do not represent the person reading the study, which would reduce the likelihood that the information pertains to them.

“As always, the best thing to do is to discuss it with your primary care provider to better understand what you may have found on the web,” Fudyma said.

The following are reputable sources of healthcare information:

American Psychological Association www.apa.org
CDC www.cdc.gov
Cleveland Clinic
https://my.clevelandclinic.org

Food & Drug Administration www.fda.gov

Mayo Clinic
https://www.mayoclinic.org
National Institutes of Health www.nih.gov
Psychology Today psychologytoday.com

PubMed www.ncbi.nlm.nih.gov/pubmed WebMD www.webmd.com
World Health Organization www.who.int
It hasn’t been easy. Like many people, I’ve been reluctant to ask for help, not wanting to be a burden or inconvenience my family and friends.
But things have changed. Thankfully, for the better.
As I write this column, spring cleaning is tugging at my proverbial apron strings.
I need, I must, make sense of the boxes and bags of family photos, documents and items I inherited after losing my mother and father. I’ve procrastinated far too long. It’s time.
So ... I called my dear friend Carol and asked if she would help me begin the emotion-laden process of deciding what to keep, donate or throw away.
A self-described decluttering guru, Carol happily agreed to get me started. Among many helpful tips, she encouraged me to ask myself, “Does it have value? Does it bring me joy?”

I’m delighted to report that we made great progress. Her help was invaluable!
And we had a good time together, often laughing at the silly things I’ve held onto all these years. My grade school report cards come to mind. No need to be reminded that I “whispered too much.”
Below is an essay titled “Asking for Help” that I included in my book, “Alone and Content: Inspiring,
empowering essays to help divorced and widowed women feel whole and complete on their own.”
I hope it inspires you to reach out and ask for assistance if you need it.
A ride to the doctor’s office. Extra hands to move heavy furniture. An emergency dog-sitting request. Giving and receiving help from my friends and family has proved to be a wonderful way for me to strengthen bonds. I have learned time and again that asking for help brings blessings, not burdens.
Many people — and often those of us who need it most — find it hard to reach out and ask for help in times of need.
The reasons are numerous, but my experience tells me that lots of women and men who live alone avoid asking for help because they fear being seen as weak or vulnerable.
I know that after my divorce I was reluctant to ask for help. I
Fewer high school athletes are getting hurt playing sports, but those who do are more likely to suffer severe injuries that require surgery or a timeout from their chosen sport, new research shows.
Which teens are most at risk? Those who participate in football, girls' soccer and boys' wrestling, the study authors found. Knee and ankle sprains and strains, along with head injuries such as concussions, were the most common injuries seen.

Exactly why injuries are becoming more severe isn't fully understood, but having kids specialize in sports too early may play a role. That can lead to an increase in overuse injuries, overtraining and burnout, said study co-author Jordan Pizzarro, a medical student at George Wash-
ington University School of Medicine and Health Sciences, in Washington, D.C.
Still, the new data isn't a reason for kids to stop playing sports.
“Sports build endurance and stamina and help with growth and maturity,” Pizzarro said. Instead, parents should talk to the school or coach about pre-season training programs that may help stave off injuries among young athletes.
For the study, the researchers tapped into 2015 to 2019 injury data from 100 high schools. These schools have athletic trainers who report injuries for five boys' and four girls' sports.
Overall, there were 15,531 injuries that occurred during 6.8 million athletic exposures. (An athletic expo-
wanted to show the world that I was perfectly fine, thank you very much. I avoided asking anybody for anything, determined to muscle through on my own. It led to isolation and pointless hardships.
But the biggest shame? Not asking for support kept me distant from friends and family. I denied myself (and them) the chance to connect on a genuine and meaningful level. Looking back, it’s clear to me that my healing and personal growth came more slowly as a result.
I encourage you to let go of any excuses not to ask for help, in favor of being true to yourself and to those who love and want to support you.
How can you help yourself?
• Be honest. Take a moment to reflect on what keeps you from asking for assistance. Could it be pride? Do you think you’ll be seen as incapable or inadequate? Are you concerned about being a bother? Or, would asking for help force you to acknowledge that, indeed, you need it?
• Redefine what it means to be strong. Everyone needs outside support from time to time, and seeking help on your terms is not a weakness. In fact, the strongest people are often those who have the courage to admit they need reinforcements. I’ve always admired this quality in others. Real strength is knowing your personal limitations and having the confidence to recruit assistance when necessary.
• Have some faith. Believe that people truly want to help. Just think about how you’d respond if a friend, family member or co-worker asked for a helping hand. You likely wouldn’t hesitate; you might even feel slighted if not asked, especially if someone you cared about was having real difficulty. Know that others, too, want to be there for their friends and family in need.
• Take a chance. When you choose to open yourself up and expose your authentic self, you are taking a risk. That’s a good thing! When you are real like this, you have an amazing opportunity to cultivate deeper, more meaningful bonds with others.
• Make the request. First put some thought into where you could really use some support; then ask for help with one specific item. It could be something as simple as asking a neighbor for help raking out a garden bed to something as important as identifying a financial adviser.
If you think you’ll feel awkward making the request, you might start out by saying, “You know, I’m not very comfortable asking for favors, but I wonder if you might be able to help me with something?”
• Express your gratitude. You know this, of course. A heartfelt thank you in person or in writing will be warmly received by the person whose help you have accepted. No need to go overboard. Remember, people want to help others and don’t expect to be compensated for doing a good deed.
• Offer help in return. Because giving can be as gratifying as receiving, make it known that you are available to return the favor. Better yet, find opportunities to offer help. We all have gifts and can be of great assistance to one another.
So, take it from me ... life can be better, just for the asking.
Gwenn Voelckers is the founder and facilitator of Alone and Content, empowerment workshops for women and author of “Alone and Content,” a collection of inspiring essays for those who live alone. For information about her workshops, to purchase her book, or invite her to speak, visit www. aloneandcontent.com
sure is defined as one athlete participating in one practice or competition during which an injury could potentially occur.) This equals an overall rate of nearly 2.3 injuries per 1,000 athletic exposures, which can be extrapolated to 5.2 million sports-related injuries among high schoolers nationally.
Most injuries took place during games. Overall, the injury rate was higher in boys' sports compared to girls' sports, and 3.5% of all injuries were fractures, and these mainly occurred in boys' baseball, basketball and football. Overall, just over 6% of injuries — most often from wrestling, girls' basketball and boys' baseball — required surgery.
In total, 39% of sports injuries resulted in athletes taking less than one week off from their sport, while 34% of injuries required taking up to three weeks off to heal. Seven percent of injuries required athletes to take more than three weeks off to
heal, and nearly 21% of injuries led to medical disqualification for the season or career.
The new research was presented at the American Academy of Orthopaedic Surgeons (AAOS) annual meeting March 7 to 11. Research presented at medical conferences should be considered preliminary until published in a peer-reviewed journal.
"The majority of high school sports are recreational, so the players may be under-conditioned and not prepared for the grinds of organized sports, making them more prone to muscle strains and other soft tissue injuries,” said Sean Tabaie, an orthopedic surgeon at Children's National Hospital in Washington, D.C..
His advice? “Start early and introduce kids to a lot of different sports. Rotating the sports that kids play throughout the seasons is really important. Don't focus on one sport, as that will leave you prone to overuse of specific muscles,” Tabaie said.
It’s a condition that results in more than 454,000 hospitalizations in the United States each year. Even worse, the Centers for Disease Control and Prevention predict around 12.1 million people could be diagnosed with the ailment by 2031.
Atrial fibrillation — or a-fib — is an abnormal heart rhythm from the top chambers of the heart. This often causes the heart to beat irregularly and quickly. The risks of atrial fibrillation include stroke and, if the heart rate is fast, a weaken heart.

“Heart arrhythmia is more common than people believe and it is associated with an increased risk of stroke. The rate of the condition dramatically increases as someone gets older,” said physician Anne B. Curtis, distinguished professor of medicine at the University at Buffalo Jacobs School of Medicine & Biomedical Sciences.

She explains five things you should know about a-fib.
Atrial fibrillation often presents with racing heartbeats, irregular heartbeats and a lack of stamina. However, many patients have no symptoms, particularly those whose heart rates are not as fast when they are in atrial fibrillation. Other symptoms include lightheadedness, extreme fatigue, shortness of breath and chest pains. A normal heartbeat begins with one electrical impulse from the sinus node, a single point in the heart’s right atrium. A healthy person’s heart usually beats 60 to
150 beats per minute. With a-fib, electrical impulses fire from multiple sites in both atria. That can cause the atria to contract 400 or more times per minute. The ventricles become overwhelmed trying to keep up with the contractions.
“Patients will complain about palpitations, shortness of breath and fatigue, and when untreated, that can lead to heart failure,” said Curtis. “When your heart has to work harder than normal that affects your overall body and you simply feel exhausted. Sometimes my patients don’t even feel the palpitations so that is why it is essential to go to your regular physician visits to make sure everything is going well with your heart.”
A healthy lifestyle with regular aerobic exercise and a well-balanced diet helps reduce your risk of atrial fibrillation and other forms of heart disease. Exercise works like beta-blocker medication to slow the heart rate and lower blood pressure at rest and also when exercising. A combination of aerobic workouts — including walking, running, swimming — in combination with strength training, remains the ideal combination for great heart health. High blood pressure is a major risk factor for heart disease. In ad-
dition, experts recommend avoiding tobacco and smoking. Whether it’s your eating habits leading to diabetes or the way you handle your environment leading to stress and high blood pressure, she also suggests making sure to monitor those aspects of life.
“Many of the ways you can improve your life have to do with lifestyle. You are at a higher risk if you have high blood pressure, sleep apnea or have obesity issues,” said Curtis. “We recommend exercising appropriately because consistent movement and being in shape is ideal. We also recommend not over exercising. Many marathoners and elite athletes are at higher risk for a-fib than the general population so they have to watch their heart rates when they practice or compete.”
Episodes of atrial fibrillation may come and go, or they may be persistent. However, even though the condition isn’t always life-threatening it has the possibility of leading to more serious medical conditions that require proper treatment.
Family history may play a role in atrial fibrillation. Certain genes have been identified as associated with atrial fibrillation. If you have familial atrial fibrillation, you may get it earlier in life than do those without a family history of the condition.
“I would say it is very unusual that family history plays an issue. There have been studies that talk about some genetic correlation and ethnicity does play a factor,” she added.

Asian and Black populations see lower atrial fibrillation rates than those of European ancestry.
A common misconception about atrial fibrillation is that a pace-
maker is the first and best therapy. A pacemaker does not keep the heart beating regularly. It increases the heart rate.
“It’s very rare to have a specific gene lead to A-fib in a family, but it can occur. Much more often, obesity, hypertension and sleep apnea may run in a family, and those conditions make a-fib more likely,” Curtis said.
People with atrial fibrillation have three to five times greater risk for ischemic stroke. “The stroke risk is real and it is worth pointing out,” said Curtis. “If someone has diabetes and hypertension then they are at higher risk because sometimes you have blood thinning medication when you are diagnosed with a-fib to prevent a stroke.”
As the largest medical group in Western New York, with the most specialty and subspecialty care services, we’re with you at every step.
With a team of 550+ physicians offering primary, specialty and surgical care for all ages, UBMD Physicians’ Group is the one source for the life you lead.
If you are interested in the medical field and enjoy high adrenaline situations, working as an emergency medical technician might be for you.
Abby Harning, professor of emergency medical technology at SUNY Erie in Williamsville, felt initially drawn to EMT work as she wanted to enter the medical field.
“I heard you could do EMT work without a lot of education, so that’s what I decided to do,” she said.
Compared with that of a physician, it’s a much shorter academic career. EMT programs at community colleges or other schools last one semester (about 100-150 hours) and accept applicants as young as 17 (must be 18 upon completion). After successfully passing the exam, EMTs must complete 36 hours annually as a refresher and recertify every three years to maintain their credential.
In addition to the education, Harning said that candidates should be willing to work in inclement weather, possess patience and demonstrate an ability to cope with stress.

“Have some healthy hobbies to distract yourself when you’re away from work,” she said. “Have friendships away from emergency medical service. We’re great support to each
other, but having a life balance is important.”
The state requires that each person working as an EMT must be able to lift 125 pounds individually or 250 with assistance, read and speak English fluently, and carry a valid driver’s license. Individual agencies may also have additional requirements, such as a commercial driver’s license for a mobile stroke unit.

The role has significant turnover because of the entry-level nature of the work. Many people move on to working as a paramedic. Paramedic classes take one to two years to complete with an average of 1,000 hours of training and 800 hours of clinical time. Taking a National Registry EMT course and passing the associated exam can enable an EMT to work on cruise ships, oil derricks, in rural areas and internationally.
“There’s a community paramedicine which hasn’t caught on yet in New York, where we do a home visit of a patient to do telemedicine with a physician and provide a visit that prevents having to transport a person to the hospital,” Harning said. “They have the ability to draw blood, use a portable lab to analyze the blood, do ultrasound assessment, transmit EKGs
and do things like start IVs and administer medications. All of this helps keep the person at home.”
Managing mental stress is part of working as an EMT. Ray Hubert, second assistant chief with Tri-Community Ambulance Service, Inc. in Sanborn, learned this years ago. He currently volunteers with the service 20 hours weekly with the 100% volunteer company, which makes more than 2,300 calls annually. He had trained to become an EMT as a young adult and worked in the field from 1979 to 1982 but left the field for 16 years “because of the depression, PTSD and inappropriate coping mechanisms,” he said.
Eight years ago, his daughter wanted to become an EMT, so he joined her in training. He eventually went on to become a paramedic.
“I realized I had passion for this
again, “Hubert said. “I remembered why I did this in the first place: to make a difference.”
Now he teaches EMTs and paramedics. He believes that good candidates for this work should have an aptitude for helping others and a desire to continue to learn.
“We need people who are adaptable,” Hubert said. “We identify, improvise, adapt and overcome. You have to have a relatively stable mental capability. There’s a lot of stressors and mental health is a really big concern for us and overall. There’s a lot of alcoholism and drug addiction.”
Anyone interested in working as an EMT can advantage of opportunities at volunteer agencies that provide free classes for those who pass the exam.

Healthcare has so many high-paying opportunities for people with the right skills. You can learn those skills at Trocaire College and get a great-paying job in Medical Assisting, Digital Medical Sonography, Radiologic Technology and more.

We
committed to empowering people of all abilities






When I was a child, the only peas I ever ate were canned, and the only reaction I ever had was ick!
Mushy and tasteless, canned peas forced me to develop an important culinary survival skill: “food dispersion.”
These days, however, I couldn’t fathom leaving one pea behind!






What prompted my pea epiphany? Two discoveries: fresh and frozen. Make that three: a pea’s remarkable nutrition.

Much like other legumes, these tiny green globes carry quite a punch when it comes to fiber and protein, with a ½-cup portion delivering about 4 grams of each. Both nutrients slow the breakdown of carbohydrates, which means you are less likely to have sudden spikes in blood sugar after eating them. This slower digestion also promotes feelings of fullness, making it easier to resist snacks.
Peas are vitamin superstars, boasting impressive amounts of vitamins C, K, thiamine (B1) and folate (B9), many of which are antioxidants that help reduce inflammation. Multiple studies suggest that anti-inflammatory nutrients, such as these, may help protect against some chronic illnesses: heart disease, diabetes, autoimmune diseases, and more.
Concerned about your blood pressure? Peas teem with minerals that play a major role in blood pressure control: magnesium, potassium, and calcium. High blood pressure, which damages your arteries by making them less elastic, can lead to heart disease or even a deadly heart attack or stroke. In addition, the high fiber content of peas has been shown to lower total cholesterol and “bad” LDL cholesterol, both of which increase the risk of heart disease when elevated.

Eating peas regularly may reduce the risk of cancer. Karen Collins, RDN, nutrition adviser for the American Institute for Cancer Research, says peas contain phytochemicals that help support the body’s antioxidant defenses. Antioxidants disarm compounds that may cause the kind of cell damage that contributes to inflammation and an increased risk of diseases such as cancer.
Similar to other legumes, peas are a bit high in carbs, with ½ cup serving up around 11 grams. A few comparisons: ½ cup carrot slices, 6 grams; 1 medium tomato, 5 grams; and 1 stalk celery; 1.2 grams. However, because peas are nutrient dense, garnering the benefits of those nutrients tends to outweigh a pea’s carbs. Nonetheless, for those watching carbs, monitoring intake of
peas is often advised. Final pea perk? These bead-sized jewels are super low in fat, cholesterol, sodium, and relatively low in calories—only 60 per ½-cup serving.
If buying fresh peas, look for firm, plump pods that are a vibrant medium green. Unwashed, unshelled peas will last several days in the refrigerator. If buying processed peas, many recommend frozen over canned—for taste, texture, and nutrition. Steaming peas in as little water as possible helps to preserve the vitamin C.

2¼ cups water (or more if too thick)
1 13.5-oz. can fat-reduced coconut milk
1 16-oz. bag frozen peas (or 3¾ cups fresh)
Small handful of cilantro leaves (optional)
Warm the oil in a medium saucepan over medium-low heat. Add the onion and cook, stirring frequently for 6 minutes. Add the ginger, garlic, cumin, cayenne, salt, and pepper and cook 2 minutes more, stirring frequently.
Add the water and coconut milk and increase the heat to high. Once the mixture starts to boil, reduce the heat to low and add the peas. Cook just until the peas are bright green and tender, about 5 minutes.
Puree the soup using an immersion blender or a regular blender. Season the soup to taste with salt, ladle into bowls, top with cilantro leaves (optional) and serve.

Adapted from Better Homes & Gardens Serves 4-6
2 tablespoons canola or olive oil



1 small onion, diced

2 tablespoons minced ginger
2 garlic cloves, minced
½ teaspoon cumin


¼ teaspoon cayenne pepper
1 teaspoon kosher salt
¼ teaspoon coarse black pepper



Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.



When it comes to organ donation designations, New York could do better to meet the need.
According to the US Health Resources and Services Administration, 105,800 people nationwide are waiting for an organ donation. More than 8,500 of those are New Yorkers and about 500 of those will die before they receive a transplant Univera Healthcare report released in March 2022.
“These aren’t just statistics, but rather our loved ones, coworkers and neighbors,” said Lorna Fitzpatrick, vice president medical affairs and senior medical director at Univera Healthcare in a statement. “We can increase their odds for a successful donor match by increasing the number of people who register to be donors.”
On average, each donor can save eight lives and enhance 75 more.
Despite ranking as one of the highest states for donor need, only 49% of New Yorkers eligible to do-
nate have enrolled in the Donate Life Registry; 63% is the national average.
New York-Presbyterian, a healthcare system in New York City, stated that as of 2017, New York state ranks last in the nation for the number of enrollees.
Ten years ago, the New York state enrollment rate for donors was 29% but is nearly 50% now, which Ryan counts as an important increase. Ryan believes that increasing the number of methods for singing up for the NYS Donate Life Registry has helped the rate inch upward. Regardless of how or where a donor registers, it goes to the NYS Donate Life Registry.
Myths about medical care prevent some people from registering. For example, some people believe that their level of care will be compromised if they are admitted to the hospital and identified as a registered donor.
“That doesn’t make any sense,” said Jorge Ortiz, transplant surgeon with UBMD Surgery and professor
Jackie O’Lay, chief financial officer for UBMD Emergency Medicine, wasn’t a match for the intended recipient of her kidney. But she did save the life of a man to whom she subsequently donated her kidney.
In early 2022, O’Lay read about Elena DePaolo of Niagara Falls, a young mother who needed a kidney and posted about it on social media.
Her story drew O’Lay and prompted her to volunteer for testing to see if she could be a match for her.
DePaolo had survived acute lymphoblastic leukemia, but the chemotherapy and radiation had destroyed her kidneys. By 2017, she was diagnosed with kidney disease.

“I was touched by her story and everything she had been through
with chemo and surviving cancer,” O’Lay said.
DePaolo and her husband had struggled to have children and adopted a little boy. Shortly thereafter she learned she was in kidney failure. O’Lay saw images of the small child and did not want to imagine him growing up without his mother.
Despite O’Lay’s generous gesture, testing showed that she was not a match for DePaolo.
Eventually, another donor proved a match and DePaolo underwent a successful transplantation.
“It was a longshot anyway,” O’Lay said. “I was disappointed, but Erie County Medical Center had asked me pretty much immediately if I would consider someone else. I
in the department of surgery, Jacobs School of Medicine and Biomedical Sciences at University at BU. “Someone in Jonestown, Pennsylvania is not trying to get organs for Pittsburgh. No one wants to lose their license. That doesn’t make any sense.”
Plus, only donation experts have that access to who is registered and it is only accessed at the point of death. Doctors providing care to patients who are critically ill or injured are not the same as those who coordinate donor transplants.
The records in the NYS Donate Life Registry are secured in a database closed to medical personnel at hospitals and only accessible to organizations such as ConnectLife Registry, which serves Western New York. The organization provides the link in coordinating donation to recipients in transplant centers.
It’s also a myth that people in a coma are automatically considered for organ donation.
“If you’re in a coma, they cannot take your organs unless you’re brain dead or about to be brain dead and your family consents,” Ortiz said. “It’s against US federal law to buy and sell organs. The rich and famous do not get organs first. Popularity and finances are not considered. Your organs won’t be used for experimentation unless you designate them for a research institute.”
Some people resist signing up for organ donation as they assume that their family members would want to make that decision. Ortiz said that selecting registration in advance can provide comfort to family members who do not have to make that decision. However, they can override the decision. It can also help them feel that their loved one’s loss can at least benefit someone else.
Another myth is that ethnicity or sexual orientation makes a difference
in organ donation. Ortiz said that neither of these disqualifies potential organ donors.
“One problem among non-majority recipients is that there aren’t enough donors that would match them genetically,” Ortiz noted.
Some people believe it is costly to donate organs. Ortiz said that it is free for those donating. The recipient is responsible for paying medical expenses.
It’s a mistake to assume that one’s body is too old, ill or unusual to help others. Ortiz said that no medical information is gathered upon registration.
“History of mental illness, health and age are not contraindicated,” he said. “If you’re an organ donor, you can donate your body to research.”
He also said that many people assume that religion forbids organ donation. Most major world religions support organ and tissue donation. Any religious, cultural or familial beliefs should be discussed before deciding about organ donation.
Some think that organ donation causes problems with burial and funeral services.
“That’s not true; you can have an open casket service,” Ortiz said. “The way the incision is made, it’s not obvious donation has been made. Open casket is still viable.”
According to Health Resources & Services Administration, the most common transplants nationwide in 2021 were kidney (24,670, with 90,483 still waiting); liver (9,236, with 11,891 still waiting); heart (3,817, with 3,502 still waiting); lung (2,524 with 1,051 still waiting) and other (1,108, with 290 still waiting). The “other” category includes skin, face, hands and abdominal wall. Some things such as a kidney, bone marrow and part of the liver may be donated by living donors.
thought, there are 100,000 people nationwide on the transplant list whose stories I don’t know.”
One of those was a patient for whom O’Lay proved a match. On Feb. 28, 2022, she went under the knife at Erie County Medical Center to give one of her kidneys to a stranger for whom the surgery was successful. As for O’Lay, she returned to work about a week after the procedure, suffering only some discomfort and fatigue.
“ECMC goes through how your body will adjust to having one kidney,” O’Lay said. “They screen to make sure you can live a normal, active life with one kidney. They do look at blood pressure to make sure you don’t have high blood pressure or any kind of damage like if you had kidney stones.”
It took a few months of testing to confirm that she could donate.
As for drawbacks to donating her kidney, she cannot think of any.
O’Lay credited the surgical team at ECMC for “a smooth process. I can’t say enough about the transplant team. My experience was positive all the way through. I highly recommend it. It’s a process to start with but once the ball was rolling, it was quick and methodical, and the recovery was minimal. Considering you’re
saving someone’s life it was an easy choice for me.”
It took about six months after surgery for O’Lay to finally meet the patient whose life she saved.
“And we are still in touch,” O’Lay added.
In fact, they celebrated their oneyear transplant anniversary by going out to dinner.
“It’s such a small world but we have mutual friends and we didn’t know each other,” O’Lay said. “His wife knew someone I grew up with and he had a lot of mutual friends with my husband, Scott.”
Most people don’t think much about organ donation unless they or a loved one are waiting on an organ recipient list or they work in a role like Jorge Ortiz, transplant surgeon with UBMD Surgery and professor in the department of surgery, Jacobs School of Medicine and Biomedical Sciences at University at Buffalo.

“It’s a myth that there are not enough people waiting for organ donors to make it worthwhile,” he said.
Because so many New Yorkers wait for an organ donation, it is important to sign up as an organ donor. Unfortunately, too few people do so and as a result, 17 Americans die daily while waiting for a lifesaving transplant. Still more await transplants that could enhance their lives.
“It’s not difficult to become a donor,” Ortiz said. “You just have to say yes.”
Since relatives can override their deceased loved one’s consent, Ortiz said it is important to not only obtain designation as an organ donor, but tell loved ones about the decision.

“Theoretically, my wife can override what I wrote on my license,” he said. “Tell your loved ones. They’re the ones who will say it at that time.”
Obtaining designation as an organ donor is simple to do, but for some hard to think about.
“We live in a society where it is not so easy to think about our own demise,” said Nancy Ryan, director of development at Finger Lakes Donor Recovery Network, the federally designated, nonprofit liaison between donors and recipients awaiting donation. “We put off making wills until way too late. We put off thinking about our own death as long as we can. When something unexpected
happens to a middle-aged or younger person, the family is caught offguard. A 30-year-old doesn’t make end-of-life plans. Every day is a gift to every person. Being prepared with what you want is important.”
FLDRN serves 20 counties upstate facilitating organ, eye and tissue transplants.
Anyone 16 or older may sign up to become a donor. One means of designating as a donor is through the DMV when applying for or renewing a driver’s license. Ryan said that is the most common means. Potential donors can also sign up through the voting registration form. New York is the only state with this option available. New Yorkers applying for or renewing their health insurance benefits through the New York State of Health Insurance Exchange can register as a donor. Yet another is https://donatelife.ny.gov/register, where people can sign up. All methods are free.
Ryan said that FLDRN has been working to promote donation by making QR codes available in the community for people to scan and access the site.
“We’re getting our hospital partners to put this link in the patient-facing medical record systems,” Ryan said. “On those patient medical record accounts, many put the link to sign up as a donor in those systems, which is fantastic. It’s so relatable.”
When a person dies or is imminently about to, the medical providers are required by law to contact FLDRN. The organization’s organ procurement coordinators manage the medical side of patients and decedents to match donors with recipients. The family coordinators help honor the end-of-life designations
and speak with family members if the deceased have not registered.
Although donors can make their wishes known using documents such as a driver’s license, last will and testament or health care proxy, these documents may not be readily available when donation decisions are made. Ryan encourages donors to use the electronic registry and to also make family members aware of the designation decision.

“You want a determination about what will happen after you pass away,” she said. “If you don’t put it in writing and if your family doesn’t know if you wanted to be a donor, they’ll be asked by an organ or tissue agency staff member if they’ll be interested. What a difficult conversation that is.”
Donation does not always mean a deceased donor. Be the Match (https://bethematch.org/about-us) seeks registration for living donors for people to donate bone marrow but not organs. In Upstate New York, ECMC offers transplant programs for live donor and cadaver donor kidney
transplants.
To register for live donor kidney donation, visit National Kidney Registry (www.kidneyregistry.org), so people with end-stage kidney disease will not require a regimen of dialysis to survive. The average life expectancy of someone on dialysis is five to 10 years.
To promote more lifesaving and life improving organ donation, the New York Legislature passed the New York State Living Donor Support Act, which takes effect in April. The state’s health commissioner will set expenses covered for reimbursement. Funding from employee sick leave, the National Living Donor Assistance Program and other sources will first provide coverage and the state program picking up any remaining expenses.
“With expanded assistance for those inspired to become organ donors, I am confident this new law will help more New Yorkers give and receive the gift of life,” said State Sen. Gustavo Rivera (D-the Bronx) in a statement. Rivera sponsored the bill in his chamber.
According to the Finger Lakes Donor Recovery Network:
• Every nine minutes, someone is added to the national transplant waiting list.
• More than 5,000 people died in 2022 while waiting for an organ transplant.
• One donor can save up to eight lives through organ donation and could improve the lives of up to 75 more through tissue and cornea donation.
The number of people waiting for a life-saving organ transplant:
• Nationally: 104,000
• New York state: 8,125 (7,000 are waiting for a kidney)
Asingle nonprofit has what amounts to a monopoly over all organ transplants performed in the United States, but the federal government said that it plans to change that.
In 2022, a record 42,887 organ transplants were performed. Yet nearly 104,000 people remain on waiting lists for organs. About 22 people die each day while waiting, even as organs are discarded, damaged while being delivered or not collected, according to a new story published by the Washington Post.
The Health Resources and Services Administration (HRSA), which has contracted with the United Network for Organ Sharing (UNOS) to run the Organ Procurement and Transplantation Network for 37 years, announced in March it will invite organizations to bid for contracts for different parts of the transplant system’s functions.
“Every day, patients and families across the United States rely on the Organ Procurement and Transplantation Network [OPTN] to save the lives of their loved ones who experience organ failure,” HRSA Administrator Carole Johnson said in a news release announcing the change. “At HRSA, our stewardship and oversight of this vital work is a top priority. That is why we are taking action to both bring greater transparency to the system and to reform and modernize the OPTN.”
Among the plan’s many changes are steps to improve the technologies used by surgeons and transplant coordinators.
Network structure would also change, including adding a strong, independent board of directors. A new public dashboard should also make the donation and receipt process more transparent.
UNOS said in a statement it “supports HRSA’s plan to introduce additional reforms into the nation’s organ donation and transplantation system, and welcomed a competitive bidding process.”
“We believe we have the experience and expertise required to best serve the nation’s patients and to help implement HRSA’s proposed initiatives,” the statement said.
But the White House’s U.S. Digital Service called UNOS’s technological system archaic in a confidential 2021 assessment for HRSA. It also recommended breaking up UNOS’s monopoly over that technology, the Post reported.
“UNOS has allowed the organ donation system to become mismanaged, unsafe and self-enriching,” Greg Segal, founder and CEO of Organize, a nonprofit patient advocacy group, told the Post. “Today’s announcement that HHS will break up UNOS’s monopoly, and bring in competent and transparent new contractors, is a transformative and unequivocal win for patients.”
UNOS oversees a transplantation network that includes about 250 hospitals that perform transplants.
Iroquois Healthcare Alliance’s CEO seeks to get assistance from state for its members. “Our member hospitals are experiencing some of the worst financial and workforce challenges they’ve ever faced,” he says
 By Brenda Alesii
By Brenda Alesii
The New York state budget is a focal point every April, and this year Gary Fitzgerald is making a request that could impact thousands of hospital patients.
Fitzgerald, a Cornell University alumnus, is the CEO and president of the Iroquois Healthcare Alliance. The nonprofit alliance is a regional healthcare trade organization representing more than 50 hospitals and health systems, across 32 counties of Upstate New York. Its representation includes everything from rural facilities to so-called safety net providers to large, academic medical centers
in urban areas. Hospital size ranges from 10 beds to 500-plus. Advocacy, education and cost-savings efforts are among their shared objectives.
In Good Health spoke with Fitzgerald about his organization’s funding request in the final state budget.
Q: The Iroquois Healthcare Alliance serves a vast area, spanning more than 28,000 square miles. What is the connection with the Iroquois name?
A: Iroquois recognizes the history and collaboration of the Six Nations Iroquois Confederacy—a tribal alliance of Native Americans, which
serves as one of the first examples of organizations working together for the betterment of all. The vast geography of the consolidated region includes Central, Northeastern, Utica-Watertown, Southern Tier and the North Country, all of which were once part of the Iroquois lands.
Q: Do you have collaborations with hospitals and health-care facilities in Buffalo and Western New York?
A: Yes, we occasionally work with the Western New York Hospital Association, talking with leaders at the hospitals and exchanging ideas. While we are based in Upstate New York, anyone can join the alliance. We have members in Vermont and Pennsylvania. Our primary job is advocacy, that’s number one. It is important that all are treated fairly with reimbursements and overall regulations.
Q: Why should the state budget provide support for Upstate New York hospitals?
A: We want to convey to lawmakers that the needs of Upstate New York and rural hospitals are great. It’s no secret that health care has been in peril since the pandemic started, and as the infection rate and stories about heroic health care workers subside, it may seem as if we are returning to normalcy. The reality is wildly different. Our member hospitals are experiencing some of the worst financial and workforce challenges they’ve ever faced. Much of it has to do with lasting effects of the pandemic, the impact of wildly increased staffing agency costs, longstanding staffing shortages, and harmful, but well-meaning, regulations.
Q: What do you think of Gov. Hochul’s proposed 5% Medicaid rate increase?
A: We are calling for a Medicaid rate increase on the order of 25% as that demonstrates the magnitude of the challenges we are facing. That change is sorely needed in this new and developing landscape.
Q: Your organization recently conducted a staffing vacancy survey, which reflects how the shortage of workers remains unabated, continuing at rates two-and-a-half times higher than before the pandemic. How can the state help?
A: We commend Gov. Hochul for including measures in the budget to increase staffing agency practices transparency. These agencies charge exorbitant rates. We call on the state to invest in a permanent upstate healthcare workforce recruitment and retention fund, supporting education and pipeline programs to supply the next generation of workers.
Q: On your website, www.Iroquois. org, you have a section on the “Caring Gene.” What information is available there?
A: So many healthcare workers became burned out during the pandemic. Hospitals are now paying up to three times more than before the pandemic. Rather than working at McDonald’s, we encourage people who are looking for security and who enjoy caring for people to find fulfillment in a health care position. We have more than 300 positions available, including those for nurses, technicians, lab workers. The need is great; workforce is our biggest challenge.
ability to function as a result of what happened.
Obsessive compulsive disorder doesn’t always present as washing hands 20 times before leaving home every day as many people think. For some people, it can mean perfectionism regarding a task to the point where the job is never good enough — and never completed, making employment challenging. Misusing this term is often a lazy shorthand for a tendency for neatness, not doing something that interferes with work or school and interactions with other people.
“‘My OCD is kicking up’ or ‘my depression is kicking up’ it sounds like an old friend is visiting to explain why you’re doing or not doing things as opposed to ‘I’m a little freakish about things being neat,’” Dubvosky said.
“I just cleaned all my closets — I’m just so OCD.”
“I’m so depressed that I forgot to eat my takeout leftovers — again!”
“Ugh! Rain again?! I’m getting PTSD over the rotten weather lately.”
Posts such as these on social media may seem humorous to the posters, but they all misuse words associated with mental health terms, reducing the meaning of the words.
“A mental health issue is a condition with well-defined set of symptoms, and signs,” said Steven Dubovsky, president of UBMD Psychiatry, professor and chair of the Department of Psychiatry at Jacobs School of Medicine and Biomedical Sciences at University at Buffalo. “A sign is something you observe; a symptom is something the patient experiences. They have a recognized course and outcome and generally a recognized treatment.”
Typical spring cleaning, forgetting about leftovers or experiencing a rainy day are “natural consequences of human experience,” Dubovsky said, but typically do not disrupt activities of daily living for days and weeks and require treatment. Using mental health terms as part
of hyperbole can feel dismissive of the genuine struggles of people with these conditions.
In additional to minimization, using mental health diagnoses as shorthand for garden variety preferences and inconveniences also makes it seem as if a diagnosis defines those experiencing it, such as, “He’s a bipolar today.”
Misusing terms also often means defining them in an inaccurate way. Dubovsky used post-traumatic stress disorder as an example.
“It’s defined as either experiencing or being directly exposed to a type of trauma that either threatens your life or physical integrity,” he said. “It has a distinct likelihood of causing your death or bodily harm or witnessing someone else’s life. You hear politicians saying they have PTSD about the Jan. 6 demonstrations in the Capitol even though they were in a building six blocks away.
“Or if your parents took away your cell phone or a teacher was mean to you, that’s not PTSD. PTSD requires a life-threatening or severe trauma directly affecting you or you were there when it happened.”
In examples such as these, the individuals do not experience in-
Bipolar is another example of a mental condition with distinctive signs and symptoms.

“We hear people say, ‘My teenaged son went bipolar because I took away his cell phone,’” Dubovsky said. “No, he wasn’t. He had a temper tantrum. Everybody has mood swings. Bad things happen. People feel bad. Bipolar causes involuntary mood swings that affect the ability to think straight. It often runs in families and requires treatment.”
He thinks that the current-day premium placed on victimhood has exacerbated the problem of language misuse.
“You see a whole swath of the population, particularly those who are in the news a lot or political who are ‘victims’ on the grounds that it gets them elected or gets them out of trouble,” Dubovsky said. “This has promoted the trend of, ‘Of course I’m doing badly; I have clinical depression or panic disorder.’”
Throwing in the term “clinical” is meant to help their audience take them more seriously, which represents a disservice to those who are ill and must find ways to cope and carry on without the abundance of accommodations these public figures expect.

Experiencing a few quirks, traits or unpleasant circumstances does not a diagnosis make. A recent trend in social media is sharing a video revealing a “diagnosis” in what posters hope is a shocking fashion to gain

clicks and likes. However, without a provider’s actual diagnosis, it’s just guesswork. Most likely, it is incorrect. Unfortunately, some viewers believe it and form a misguided perspective on mental health issues, believing the most extreme “example” is typical.
Karl Shallowhorn, credentialed alcoholism and substance abuse counselor and director of youth orograms at Mental Health Advocates of Western New York in Buffalo, is involved with the Erie County Anti-stigmatizing Coalition. He believes that flippant use of mental health terms can add to stigma, especially since the most extreme elements or exaggerated symptoms are sometimes represented as typical of that issue. Or as noted before, everyday inconveniences and preferences are treated as mental health issues.
“We’re using a term to describe something denigratingly,” he said. “It’s about perception. We’ve found that stigma impacts relationships and people’s ability to seek help. When stigmatized, people may feel self-conscious and like they don’t want to be labeled for fear of losing their job. I have a friend who is a private businessperson and in long-term recovery and he said he was with a business partner who doesn’t know he’s in recovery. He keeps it a secret because of stigma. That’s a problem we have as a society.”
He believes that the keys to reducing stigma includes talking about mental health and using terms accurately and respectfully — not as insults or to describe non-mental health issues.

Misusing mental health language may also lead people to believe that nothing can help improve their mental health. If “everyone” is depressed, those experiencing real depression may think that there’s no point in seeking help. A person with a diagnosis may also feel like they are failing at recovery since they are not coping as well as the self-diagnosed who have no mental health issues.
“Anyone who has a stressful day may have a headache from stress and that’s a part of mental health,” Shallowhorn said. “When it becomes a problem, those symptoms are persisting longer than a couple weeks. That’s where you need to get some help.”
Integrative medicine will see a number of trends this year. We spoke with two practitioners. Here’s what they had to say:

• “Integrative medicine is moving more toward a non-pharmaceutical approach to different syndromes.
• “What I tell people to do who talk with me about integrative medicine is I have people focus on the basic pillars of primary and secondary prevention.
• “Once you’ve developed a chronic disease, we look at, ‘Is my diet the healthiest it can be?’ ‘How many servings of plant-based foods do I eat?’ ‘Am I eliminating processed foods like refined sugars?’ ‘Am I eating the right amount of calories per day?’ ‘How best can I use food as source of nutrients?’
• “Exercise is definitely being recognized as important for maintaining physical and cognitive
health. Exercise can reduce stress and anxiety. There are long-term benefits for reducing risk of cognitive impairment.
• “One thing we overlook is the importance of sleep and getting a good amount of total sleep and restful sleep. Impaired sleep is associated with impaired cognition and can have long-term effects on cardiovascular and cognitive health. I try to get people to focus on those. When we eat later in the day, and drink alcohol, it disrupts the sleep cycle. How can we decompress and shut off our brains? I have people focus on sleep hygiene and at least seven hours or restful sleep and work on shutting the brain down.
• “We’re recognizing the role of alcohol in health. More studies link it to certain cancers and cognitive issues later in life. The American Cancer Society recently came out with guidelines to limit alcohol to two per week. That’s my approach
Matters of the heart are what matter to Ronald P. Emerson, an interventional cardiologist who most recently was named medical director of the cardiac catheterization laboratory at Niagara Falls Memorial Medical Center.
Life-saving care is the goal of the lab, a joint venture for the hospital with Catholic Health System, Kaleida Health and Erie County Medical Center. In the top post, Emerson oversees the clinical performance, provides patient care and reports clinical outcomes to New York state and national data registries.
Heart care has been his professional pursuit, but for Emerson, who grew up in Orchard Park, it is highly personal, too.
“I knew early in my undergraduate education that cardiology would be my chosen field as my father had succumbed to a heart attack at age 42,” he said.
A keen interest in science as a youth led him to enter a pre-med program in college and go on to a career in medicine.
“I was guided by my parents, who provided me the opportunity, support and direction to be successful in school,” Emerson said.
He earned a master’s degree in health sciences at the University at Buffalo and completed his medical degree at St. George’s University of Medicine in Grenada, West Indies.
Then came a residency in internal medicine at UB. He completed a
for how best they can prevent illness and manage chronic conditions.
• “We all deal with stress, but we look at how we approach stress and reduce it. Stress is a killer that worsens cardiovascular conditions and sleep.
• “Meditation is something people should incorporate daily into their routines. I recommend yoga for people who want some type of more of a combination of mindfulness and flexibility exercise. There’s a host of things we can do to decompress.
Physician John Fudyma holds a master’s in public health and serves as interim division chief, general internal medicine at UBMD Internal Medicine, associate professor department of medicine at Jacobs School of Medicine and Biomedical Sciences, University at Buffalo.

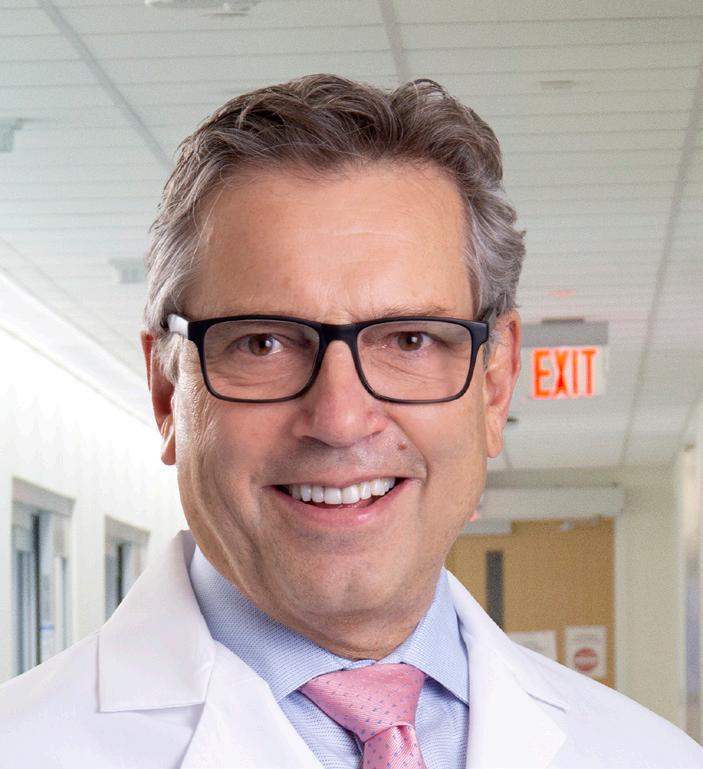

• “People are interested in immune support. Because of the pandemic, the number of public presentations I’ve been asked to give has dropped off but the last one was at the public library and I was asked to speak on immune system enhancement. Another one coming up, I was asked about immune system.
• “I don’t know as though there’s a trend, but since the pandemic, but I have a lot of patients coming with
cardiovascular disease fellowship at the University of Wisconsin in 1994 and a second fellowship at Sinai Samaritan Medical Center in Milwaukee in 1995.
The pull of family eventually brought him back to Buffalo.
“My mother still lives in Orchard Park and she always hoped that I might return home to Western New York to practice medicine,” Emerson said. “After three years on the faculty at the Sinai Samaritan Medical Center, I returned to Orchard Park to join a private practice with a colleague.”
He is affiliated with Empire Cardiology P.C. and is a longtime clinical assistant professor in the department of medicine at Jacobs School of Medicine and Biomedical Sciences at UB.
According to Emerson, the catheterization lab at Niagara Falls Memorial Medical Center provides a vital service in Niagara County. Its primary function is to visualize coronary arteries and heart muscle in order to diagnose heart disease for patients and assist in determining the most appropriate treatment strategy.
“We also have the capability to perform coronary angioplasty and stenting of arteries to improve blood flow that has been compromised by cholesterol plaques or acute thrombosis,” he said. “This is especially
symptoms consistent with thyroid disease. They want guidance.
• “Often, people have symptoms without a diagnosis. Physicians may have done a complete workup and have nothing else to give them. The patients may be frustrated with the number of pills they’re on.
• “The ones who come with an explicit goal of reducing medications is actually very few. I ask on the intake, ‘How did you learn of this practice? Why are you here today?’ And sometimes people write an essay, but generally it’s a few words as to symptoms or a diagnosis.
• “There are some people where their treatment is working and they want to get off medications, but most, conventional medicine has not offered anything to significantly improve their quality of life. A lot of patients want a pill for every ill but that’s not people who are seeking me.
• “I think over the past five years, there have been a number of nurse practitioners who have opened practices in integrative medicine. In terms of physicians, it’s myself and one more. There’s a smattering of nurse practitioners and some offer IV vitamins and IV treatments.”
important in patients who need this service emergently such as those sustaining a heart attack and re-establishing blood flow to the heart as soon as possible will result in less heart muscle damage and thus (improved) outcomes.”
The resiliency of patients who experience health emergencies continues to impress Emerson.
“When faced with life-threatening health challenges and direction, patients will make dedicated changes to their lives which can be physically and mentally challenging,” he said. “But they come to realize that they are making healthy choices for not only themselves but for those who love them.”

Dear Savvy Senior,
I am interested in possibly donating my body to science when I pass away. What can you tell me about this, and what would I need to do to set it up?

If you’re looking to help advance medical research, and in the process, eliminate your funeral and burial costs, donating your body to science is a great option to consider. Here’s what you should know.

Each year, it’s estimated that approximately 20,000 people donate their whole body after death, to medical facilities throughout the country to be used in medical research projects, anatomy lessons and surgical practice.
After using your body, these facilities will then provide free cremation and will either bury or scatter your ashes in a local cemetery or return them to your family, usually within a year.


And, just in case you’re wondering, your family cannot not be paid for the use of your body. Federal and state laws prohibit it.
Here are a few other things you need to know and check into, to help you determine whether whole-body donation is right for you:
• Donation denial: Most body donation programs will not accept bodies that are extremely obese or those that have infectious diseases like hepatitis, tuberculosis, H.I.V. or MRSA. Bodies that suffered extensive trauma won’t be accepted either.
• Organ donation: Most medical school programs require that you donate your whole body in its entirety. So, if you want to be an organ donor (with the exception of your eyes), you probably won’t qualify to be a whole-body donor too.
• Religious considerations: Most major religions permit individuals to donate both their full body and organs, and many even encourage it. If you are unsure, you should consult with your pastor or spiritual adviser.

• Special requests: Most programs will not allow you to donate your body for a specific purpose. You give them the body and they decide how to use it.
• Memorial options: Most programs require almost immediate transport of the body after death, so there’s no funeral. If your family wants a memorial service, they can have one without the body. Or, some programs offer memorial services at
their facility at a later date without the remains.
• Body transporting: Most programs will cover transporting your body to their facility within a certain distance. However, some may charge a fee.
If you think you want to donate your body, it’s best to make arrangements in advance with a body donation program in your area.
Most programs are offered through university-affiliated medical schools. To find one near you, the University of Florida maintains a list of U.S. programs and their contact information at Anatbd.acb.med.ufl. edu/usprograms. If you don’t have Internet access, you can get help by calling the whole-body donation referral service during business hours at 800-727-0700.
In addition to the medical schools, there are also private organizations like Science Care (ScienceCare.com) and Anatomy Gifts Registry (AnatomyGifts.org) that accept whole body donations too. Some of these organizations will even allow organ donation because they deal in body parts as well as whole cadavers.
Once you locate a program in your area, call and ask them to mail you an information/registration packet that will explain exactly how their program works.
To sign up, you’ll need to fill out a couple of forms and return them. But you can always change your mind by contacting the program and removing your name from their registration list. Some programs may ask that you make your withdrawal in writing.
After you’ve made arrangements, you’ll need to tell your family members so they will know what to do and who to call after your death. It’s also a good idea to tell your doctors, so they know your final wishes too.

Niagara Lutheran Health System (parent of The GreenFields Continuing Care Community), Schofield Care and Weinberg Campus have taken a significant step forward in their growing partnership.
The three nonprofit senior care providers announced recently that Weinberg Campus has joined the Lineage Care Group strategic alliance, which was first announced by Niagara Lutheran and Schofield Care in 2021.
This new entity will operate as a passive super parent organization to help oversee strategy and operations and create efficiencies, paving the way for an active parent arrangement.
The unique strategic alliance aims to strengthen all three organizations and position them for future growth. The partnership is rooted in an effort to improve the quality and clinical scope of senior care in Western New York.
“This innovative nonprofit affiliation model will ensure patient-focused care remains at the core of our collective mission, provided by individuals who live in, and are invested in, the local community, while maintaining decades of historic care by these organizations,” said Christopher Koenig, president & CEO of Niagara Lutheran Health System and Schofield Care, speaking on behalf of the three organizations.
Koenig said the affiliation will empower the partners of Lineage Care Group to deliver high-quality care more efficiently through the
Enjoy reading In Good Health newspaper? The paper is free to you but very expensive to produce and distribute. Keep the publication going. Consider supporting the publication. If you are a reader, please become a paid subscriber. If you’re a nonprofit, a medical practice or organization, consider advertising in the paper. You will get a great deal of exposure since the paper is everywhere for the entire month. We will even design your ad at no charge.
For more information, send an email to editor@bfohealth.com
— Type “Support” on the subject line.
sharing of clinical guidelines and professional expertise, optimization of human resources, maximization of Medicaid reimbursement, and the reduction of combined overhead costs.
The full continuum of services now provided by Lineage Care Group includes skilled nursing, certified and licensed home health care, adult day care, assisted living, memory care, independent senior housing, inpatient and outpatient rehabilitation, traumatic brain injuries, veterans’ care, hospice care, and palliative care.
“This nonprofit collaboration model provides greater benefits to the residents and community than the for-profit alternative,” said Weinberg Campus President/CEO Robert Mayer. “Free of the financial obligation to generate returns for investors, nonprofit senior care organizations are able to re-invest their profits into their operations and communities, leading to superior clinical outcomes, more satisfied employees, and enhanced patient and community welfare.”
Neighborhood Health Center is implementing a new program focused on improving health outcomes for pregnant patients and their newborn babies with support from a Univera Healthcare Health Equity Award.
Neighborhood Health Center serves communities that experience
disproportionate percentages of high-risk pregnancy outcomes, such as low birth weight, premature birth, and late or no entry to prenatal care.
This $20,000 grant will help fund a maternal-infant health community health worker and care coordination training program at Neighborhood. The program will offer Neighborhood community health workers and care coordinators specialized training in obstetrics and gynecology to assist patients with internal referrals to nutrition, behavioral health, pediatrics, and other services, as well as referrals to outside medical specialists and community resources for social support.
“In the Buffalo zip codes where our Neighborhood offices are located nearly 14% of births are premature compared to less than 12% on the county level,” said Neighborhood President and CEO Joanne Haefner. “These same zip codes also have higher instances of low birth weight and pregnant patients entering prenatal care late or not at all. We thank Univera for believing in our efforts to improve these health outcomes and care for our patients so they can lead healthier lives.”
The William R. Kenan, Jr. Charitable Trust has awarded $400,000 to Mental Health Advocates (MHA) for the expansion of the nonprofit’s Youth Peer Advocates (YPA) program. The two-year grant will allow
Erie County will host the first of many mental health first aid trainings in Buffalo this spring. The events will take place from 9 a.m.–5 p.m., Saturday, April 15, at Johnnie B. Wiley Stadium, and from 10 a.m.–6 p.m., Saturday, May 6, at the Frank E. Merriweather Library.
“Mental health first aid is a nationally recognized program that aims to make this important training as common as CPR,” said Office of Health Equity Director Kelly Wofford. “2022 was a stressful and traumatic year for our community. Our office decided to offer this valuable, effective training that gives an adult the tools they need to provide immediate and practical support to someone experiencing a mental health challenge.”
She continued, “We are making this happen here in Erie County. Several of our team have been trained to deliver this course as instructors, and we have already begun trainings for Erie County personnel.”
Co-instructors Arica Rouse and Eddie Payne from the Office of Health Equity will teach these two classes. Participants will learn to recognize the signs of mental health or substance use challenges in adults, how to offer and provide help, and how to guide a person towards appropriate care.
These trainings are open to the public. Registration is required. Call 716-858-2385, email healthequity@ erie.gov or visit the OHE web site.
The Office of Health Equity will also offer mental health first aid training to community groups, businesses and industry groups, faith organizations, non-profit agencies, schools and colleges; contact Arica Rouse at 716-858-2385 or healthequity@erie.gov to learn more.
MHA to expand the youth program into five additional schools and four community organizations, hire two more YPAs, and assist with retention efforts.
Youth peer advocates are trained individuals between the ages of 18-30 who self-identify as a person with first-hand experience receiving services in any one of the child-serving systems: mental health, addiction recovery, juvenile justice, child welfare, and special education. YPAs use their own lived experiences to connect with at-risk youth through peer-led support groups, educational trainings, and 1:1 non-crisis support for youth and young adults ages 9-26.
In 2022, MHA’s YPA program provided services to 62 schools and served 6781 students. The YPAs also provide support in four Western New York in-patient mental health facilities that treat youth: Erie County Medical Center, Brylin Hospital, OLV Human Services, and Western New York Children’s Psychiatric Center with support groups and 1:1 peer services.
“Because of their closeness in age, students are able to connect with a YPA in a way someone older may not,” explains Director of Youth Programs Karl Shallowhorn. “The goal is to improve mental health literacy and awareness while helping young people learn the skills needed to handle everyday stress and build positive mental health.”
YPAs are credentialed as New York State Youth Peer Advocates administered by Youth Power of Families Together in NYS.
The Kenmore Village Improvement Society (KVIS) is forming a wellness and weight loss group. The purpose of the group is to share individual’s wellness goals and offer support in accomplishing those goals. People with all kinds of wellness goals are welcome, it could be reducing stress, exercising more, eating healthier, etc. The group is open to all and free of charge. Meetings will take place at 7 p.m. on the third Monday of each month (April 17). The April meeting will take place online via Zoom, please email the KVIS at mail@villageofkenmore.com for the meeting link.
The KVIS is a group of volunteers celebrating 15 years of serving the community. It strives to help make the community as good as possible in as many ways as needed. Membership to the KVIS is free and open to all people living anywhere who care about Kenmore.
For more information, please contact KVIS President Melissa Foster at mail@villageofkenmore.com.





Erie County Medical Center announced that the new ECMC Center for Dental Care has opened at the People Inc. Health Services Building on Hertel Avenue in North Buffalo.
“Our brand new location offers access to all the same excellent dental care services provided at our Grider Street location and free, convenient parking,” said Maureen Sullivan, chief of ECMC’s department of dentistry. “Additionally, the new dental office was built with advanced equipment to support the complex dental health of special needs patients, from throughout Western New York. This practice will provide adult and pediatric dental care to the local community as well. We look forward to continuing to provide high-quality dentistry to patients at either our new location at 800 Hertel Avenue or at the ECMC Dental Center on the ECMC Campus.”
ECMC’s department of dentistry’s division of outpatient general





dentistry provides general (primary) dental health services for adults and their families. The division is the only large, accredited hospital-based dental residency program in Western New York. Identical to ECMC’s existing outpatient general dentistry service on its Grider Street Health Campus, this new center for dental care provides patients with access to dental care regardless of their insurance coverage including “straight” Medicaid, Medicaid managed care, FAP, DFAP and self-pay.
For more information or to schedule an appointment please contact: 716-898-3351(Grider Street location) or 716-218-7399 (Hertel Avenue location).




On Feb. 28 Tim Hortons franchise owners, managers and representatives presented to ECMC Corp. COO Andrew L. Davis (fifth from left) a check in the amount of $146,745. The funds were raised during the September 2022 Smile Cookie campaign to benefit ECMC frontline care services.

For a fifth consecutive year, Erie County Medical Center (ECMC) Corporation and Tim Hortons restaurants partnered to support the institution’s frontline care services.






“We are grateful to Tim Hortons and the thousands of Western New Yorkers who again supported the Smile Cookie campaign,” said Thomas J. Quatroche Jr., PhD, president and CEO of ECMC Corporation. “We greatly appreciate our partners at Tim Hortons for their commitment, and we are humbled and thankful to the residents of Western New York for their continued support of ECMC through efforts such as this.”

Children on the autism spectrum often struggle with social skills, academics, communication and other activities of daily living in varying degrees. Applied behavior analysis is a kind of therapy that uses observation, recordkeeping and positive reinforcement to find what triggers unwanted behaviors and what promotes desired behaviors.
Its goal is to help children achieve their potential for independence.
Psychologist Ole Ivar Lovaas developed ABA in the 1960s, based upon behaviorism. ABA doesn’t “cure” autism but helps children with autism better understand the rules and expectations of a world that oftentimes seems inconsistent, incoherent and frustrating to them. Caregivers and teachers at school and parents use ABA to help understand how to best support their children’s development.
Although early versions of ABA included negative reinforcement for unwanted behavior, the current version of ABA uses positive reinforcement to help foster desired behavior. ABA has garnered criticism for its intention to force children on the spectrum to behave in ways socially and academically acceptable rather than to consider autism an example of neurodiversity.
For some people, behaviors manifested by their autistic neurodiversity may hinder their ability to act upon and interact in their environment. That’s where ABA can prove helpful.
“Applied behavior analysis is a well-documented, evidence-based practice that teaches skills critical for maximizing a person’s independence,” said Marcus Thomeer, licensed psychologist and professor at Canisius College Institute for Autism Research.

For autistic individuals who are having trouble in their social/ social-communication and adaptive functioning, it is critical to identify skills that are needed to meet academic, adaptive, social or emotional demands of their environments. An ABA approach breaks down skills needed into its component steps and then teaches one step at a time. As the individual masters one step then each subsequent step is added and taught until mastery is achieved for completing the entire skill.
“It’s not about changing who a person is, but rather building skills that help them navigate the social environment,” Thomeer said.
One of the criticisms of ABA approach in working with autistic children is that it fails to follow the
child’s lead.
“In an ABA approach, the adult directs the instruction so that the child can acquire necessary skills to meet the demands of the child’s home and school environments,” Thomeer said. “As the child acquires the skills needed, an ABA approach works toward fading out their prompts and cues so that the autistic child initiates and functions as independently as possible for the specific child. Again, the goal is to
while hungry. Scheduling lunch earlier or serving a larger breakfast may represent ways to prevent the meltdown.
“ABA, when following protocols, is a good way to teach children with autism spectrum disorder discrete skills in controlled surroundings,” said Amy Nwora, Ph.D., and director of health professions education at D’Youville College. “Utilizing repetition and planned rewards allows many children to master each
maximize the child’s potential and level of independence. If a child were able to meet the demands of the environment they are faced with, then we would not have to provide instruction. For some children with limited cognitive and language abilities, we want to help build skills that enhance their lives.”
Typical children also must learn to follow directions, converse and abide by rules.
Autistic children are different because these social nuances and rules are not as intuitive or as easily learned. But they can learn with a few different strategies and tools.
Discovering the patterns of cause-and-effect aid parents in developing strategies that work. For example, if lunch is late on the days a child has a meltdown, it’s apparent that it’s tough for the child to cope
component of a skill, building to a larger task.
“Documentation in ABA clearly denotes any and all progress toward the prescribed outcome and ABA researchers are able to use this documentation for a strong research foundation that aids in evidence-based practice. Having documented proof in the form of peer-reviewed research is important both from a buy-in and a reimbursement standpoint.”
Although helpful, the data collection and strategy implementation for ABA can be time-consuming. Nwora said that this aspect can make it hard to use other effective strategies and techniques, like those that focus on sensory processing and occupational development.
“Additionally, because of the individualized presentation of ASD in children, ABA may not be effective
for all children on the spectrum,” Nwora said. “No one treatment fits all and children with ASD often benefit from a variety of treatments that can be limited when multiple hours per day are dedicated to ABA.”

One of the criticisms of ABA is that it includes a reward system typically related to favorite foods — not the type of reward a lot of parents want to give.
“Rewards help us establish importance to something a young child doesn’t think is important,” said Kathy Ralabate Doody, Ph.D., associate professor, associate chairwoman of graduate programs and coordinator of the Early Childhood Students with Disabilities Program at SUNY Buffalo. “It’s a token economy system. When you give someone something small relatively meaningless like a penny, check mark or sticker or mark with a bingo dauber on a chart, it’s like currency such as when you get 10, you can cash it in for a prize. We use that all the time. Schools even with children who are not on the spectrum use this.”
The difference is that autistic kids may receive this type of motivation for other skills that come easier to neurotypical children and their rewards may be for shorter term goals.
Another criticism of ABA is that the data collection can be laborious. Doody said that using phone apps or even paper on a clipboard-bound chart helps. The key is paying attention to the details in the environment so the therapist notices what preceded the behavior.
“Once we establish why it’s occurring, we can decrease or increase the behavior, depending upon what’s appropriate,” Doody said.