in good bfohealth.com
March 2016 • Issue 17
No Reading Glasses Ephraim Atwal is one of the first eye doctors in NYS to use camera inlay to eliminate need for reading glasses. He shares his technique
MEN’S SPECIAL ISSUE
• More options to fight prostate cancer • Fat Dads = Fat Children
priceless
Buffalo & WNY’s Healthcare Newspaper
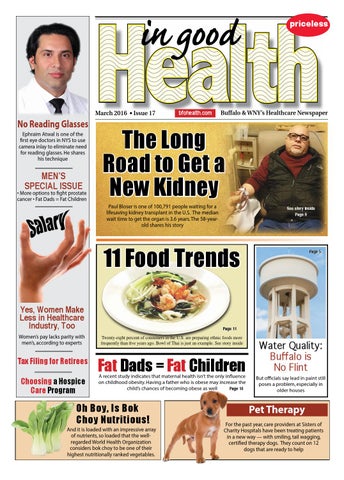
The Long Road to Get a New Kidney Paul Bloser is one of 100,791 people waiting for a lifesaving kidney transplant in the U.S. The median wait time to get the organ is 3.6 years. The 58-yearold shares his story
See story inside Page 9
11 Food Trends Yes, Women Make Less in Healthcare Industry, Too
Page 11
Women’s pay lacks parity with men’s, according to experts
Twenty-eight percent of consumers in the U.S. are preparing ethnic foods more frequently than five years ago. Bowl of Thai is just an example. See story inside
Tax Filing for Retirees
Fat Dads = Fat Children
Living Alone: Making Choosing a Hospice the Best of 2016 Care Program
Page 5
A recent study indicates that maternal health isn’t the only influence on childhood obesity. Having a father who is obese may increase the child’s chances of becoming obese as well Page 14
Oh Boy, Is Bok Choy Nutritious!
Water Quality: Buffalo is No Flint
But officials say lead in paint still poses a problem, especially in older houses
Pet Therapy For the past year, care providers at Sisters of Charity Hospitals have been treating patients in a new way — with smiling, tail wagging, certified therapy dogs. They count on 12 dogs that are ready to help
And it is loaded with an impressive array of nutrients, so loaded that the wellregarded World Health Organization considers bok choy to be one of their highest nutritionally ranked vegetables. March 2016 •
IN GOOD HEALTH – Buffalo & WNY’s Healthcare Newspaper
•
Page 1