Digitallyenabledsupplychainasastrategic assetfortheCOVID-19responseinAlberta
AnneSnowdon,PhD1 ;andAlexandraWright,MPA2
Abstract
HealthcareManagementForum 2022,Vol.35(2)90–98 ©2022TheCanadianCollegeof HealthLeaders.Allrightsreserved.
Articlereuseguidelines: sagepub.com/journals-permissions DOI:10.1177/08404704211057525 journals.sagepub.com/home/hmf
Thisprovincialcasestudy,oneofsevenconductedaspartofanationalresearchprogramonhealthcaresupplychainmanagement duringCOVID-19,focusesonAlberta.Withahistoryofemergencypreparedness,Alberta’suniquecontext,onethatincludeshaving analreadyestablished,centralized,anddigitalhealthcaresupplychainstrategy,setsthiscaseapartfromtheothersintermsofpandemic responses.AkeychallengenavigatedbyAlbertawastheinadequaciesoftraditionalsourcingandprocurementapproachestomeet surgesinproductdemand,whichwasovercomebytheimplementationofuniqueprocurementstrategies.OpportunitiesforAlberta includedtheintegrationofsupplychainteamsintoseniorleadershipstructures,whichenabledaccesstodatatoinformpublichealth decision-making.ThiscasedemonstratedhowAlberta’shealthcaresupplychainassets itssupplychaininfrastructure,data,and leadershipexpertise,especially contributedtoresilientsupplychaincapacityacrosstheprovince.
Introductionandreviewoftheliterature
TheCOVID-19pandemichasshoneabrightlightonthecritical importanceofhealthcaresupplychainasastrategicassetthat enablessafeworkenvironmentsforthehealthworkforceand qualitycaredeliveryforCanadians.Supplychainandlogistics infrastructureisastrategicassetinhealthsystemsthatmakesit possibletorespondtounexpectedevents,suchassurgein demandforcareduringapandemic,toensurethathealthcare workershavetheproductsandequipmentnecessarytodeliver careduringsurgeeventstoachievethebestpossibleoutcomesfor patients.Supplychaininhealthsystemsincludesthesourcingand distributionofproductsthatensureshealthcareteamshaveaccess totherightproductsattherighttime,inordertodeliversafeand effectivepatientcare.1 Inhealthsystems,supplychainteams sourceacomplexanddiversearrayofproductsandequipment, fromventilatorsandintravenouspumps,tomedications, vaccines,andPersonalProtectiveEquipment(PPE).
Supplychaindisruptionscanoccurduetonaturaldisasters andpublichealthcrises,resultinginsevereconsequencesthat puthealthworkersandpatientsatsignificantrisk.Forexample, duringHurricaneMariain2017,electricalgridswerewipedout inPuertoRico,whichimpactedtheproductionofIVbags manufacturedbyBaxter.2 Theresultingshortageinsupplyof IVbagsskyrocketedglobally,causinganincreaseincostby 600%.2 Similarly,a floodin2012impactedSanofi Pasteur,the supplierofthecancerdrugImmuCyst.Theresultwassignificant delaysincancertreatmenttopatientsasmanufacturerscouldnot increaseproductionofthedrugrapidlyenoughtomeetthe demand.3 Publichealthcrises,suchastheSARSepidemic,also putpressureonhealthsystemsupplychains,duetoincreasein demandforcriticalproductstokeephealthworkersandpatients safe.Thesecrisesputthephysicalhealthofessentialworkersat risk threeofthe44CanadianswhodiedfromSARSwere healthcareworkers,4 andemergingevidenceidentifies significantimpactonthementalhealthoftheworkforce
whenrealorperceivedsupplyshortagesoccurduringthese publichealthevents.TheinadequatesupplyofPPEandthe uncertaintythesesupplyshortagescreateamongCanada’s healthcareworkforcedirectlyimpactedtheirmentalhealth duringtheCOVID-19pandemic.5
Healthcaresupplychainmanagementandinfrastructurelag significantlybehindthewell-developedsupplychainsinother businesssectors.6-8 Supplychainandlogisticshavebeenwell researchedanddevelopedintheprivatesector;however, significantgapsinresearchstillexistinthehealthcare sector.9-12 Onereasonforthepaucityofresearchinthissector isthefactthattherearefeaturesthatareuniquetohealthcare supplychainthatdonotapplyacrosssectors.Healthcaresupplychainsinvolvemanymorestakeholdergroupscompared withotherbusinesssectors,includingpatients,clinicians,suppliers,healthcareorganizations,grouppurchasingorganizations,distributors,andinsurers,makingthemhighlycomplex systems.13,14 Boththerangeandcomplexityofproductsin healthcaresupplychainarealsouniquewhencomparedwith othersectors.Uniquefeaturesofthehealthcaresupplychain makeitparticularlycomplex,13 limitingtheapplicabilityof supplychainresearchfromothersectorstohealthcare.10 Of mostsignificanceperhapsiswhenthehealthcaresupplychain breaksdown,theresultisadirectimpactonhumanlife.15-17
TheCOVID-19pandemichashighlightedtheurgentneedfor healthcaresupplychainspecificresearch,tofurtherunderstand thenuancesevidentinthissector.
Thispaperreportsoncasestudyresearchoftheprovinceof Alberta’sresponsetotheCOVID-19pandemic,revealing
1 UniversityofWindsor,Windsor,Ontario,Canada.
2 UniversityofToronto,Toronto,Ontario,Canada.
Correspondingauthor:
AnneW.Snowdon,UniversityofWindsor,Windsor,Ontario,Canada.
E-mail: anne.snowdon@uwindsor.ca
empiricalevidenceofsupplychainprocessesandinfrastructure withinandacrosstheprovincialhealthsystem,duringthe firsttwo wavesofthepandemic.ThiscasestudyofAlbertaisoneofseven conductedtoexaminehealthsupplychaincapacityandinfrastructure acrossCanada,the firstnationalstudyofhealthsupplychain,funded byCIHR(Ref.VR5#172669).Thefollowingcasestudyexamines supplychainprocessesandinfrastructureandtheimpactofsupply chaincapacityonhealthcaredeliveryinAlberta,andhowit contributedtoCOVID-19outcomes.Thefollowingresearch questionswereexamined:
• Whatarethesupplychainprocessesandinfrastructure requiredtooptimizeeffectiveandtimelyhealthservices deliveryforthecurrentandfuturephasesoftheCOVID19pandemic?
• Whatprocurementmodels,approaches,andpolicy frameworksoffersecuresourcingofproductstomeet thesurgeindemandforcarebyCOVID-19patients?
• Whatisthedigitalmaturityofsupplychaininfrastructure (andprocesses)inAlberta,that,ifstrengthened,could optimizemanagementofCOVID-19?
• Whatarethedatainfrastructureandanalyticsstrategies neededtostrengthentheeffectivenessofhealthsystem supplychainprocessestosupportCOVID-19management?
• Whatistheinfluenceoffederalgovernmentinitiatives, fromtheperspectiveofprovincialstakeholders,on provincialhealthsystemcapacitytomanageCOVID-19?
Methods
Acasestudyresearchapproachwasemployedtoexaminethe capacityofhealthcaresupplychaininAlberta,giventhedearth ofresearchonhealthcaresupplychaininCanadatodate.The UniversityofWindsor ’sResearchEthicsBoardprovided approvalforthisproject.Thiscasewasoneofseven,aspart ofanationalCIHRRapidResearchprogram(CIHRRef.#VR5 172669)entitled “DevelopmentofanImplementation FrameworktoAdvanceProvincialandNationalHealth SystemSupplyChainManagementofCOVID-19 ” Acase studyapproachwasusedtounderstandAlberta ’shealthcare supplychainresponseinCOVID-19.Casestudiesofferawayto exploreandinvestigatereal-lifephenomenonthrough analyzingthecontextofeventsandtherelationshipsbetween them.18 Theprimarydatasourceforthisstudycamefrom13 semi-structuredinterviewsofhealthsystemstakeholdersaswell ascriticalreviewofpublicdocumentsandreports.Data collectionwasguidedbyasemi-structuredinterviewguide examiningsupplychaincapacityandprocessesandtheir relationshiptodecisionsandmanagementofthepandemic, completedfollowingthesecondwaveoftheCOVID-19 pandemic.Keyparticipantswhorepresentedvaried perspectivesandexpertiseincludingleadersinsupplychain, procurement,clinicianleaders(e.g.,physicians,nurses, pharmacists,andprimarycare),healthexecutives,union leaders,industryleaders,andgovernmentwereselectedusing purposivesamplinginitiallyandthensnowballsamplingas
leadersidentifiedinformantstobeapproachedtoparticipatein thestudy.Semi-structuredinterviewsdocumentedtheexperiences, perspectives,andviewsofhowsupplychaininfrastructureand processeswereoperationalizedduringtheearlywavesofthe pandemic,theimpactofleadershipdecisionsonsupplychain management,howsupplychaincapacityinfluencedleadership decisionsandCOVID-19healthsystemoutcomes,andhowand whichchallenges,solutions,andgapsinsupplychaininfrastructure contributedtoCOVID-19outcomes.Interviewswereconducted untilsuchtimeastheoreticalsaturationwasachieved.Codingof interviewsproceededasdatawascollected,wherebyresearchers wereabletoidentifyemergingthemesandconceptstoenable reflexivityasinterviewdatawerecollectedandanalyzed. Interviewswereaudio-recordedusingMicrosoftTeamsand transcribedverbatimbyanindependenttranscriptionist.The analysisincludeddetailedandmultiplereviewoftranscriptsto identifyinitialconcepts,followedbycoding,andcategorizingtext excerptstoidentifyconceptualpatternsacrosstranscriptsthatwere developedintothemes,usingN-Vivosoftwaretoassistwith organizationofdata.Thethemeswerethendefined,andare describedinthefollowingsections.
Provincialcontext
LocatedinWesternCanada,theprovinceofAlbertahas apopulationofover4millionpeople,withamajorityclustered aroundthemajorurbancentresofCalgaryandEdmonton.Alberta HealthServices(AHS)isCanada’s firstandlargestprovince-wide, integratedhealthcaresystem,providinghealthcareservicestoover 4.4millionpeople.19 In2008,Albertaamalgamatedallofitshealth regionsintooneprovincialorganization,AHS.AlbertaHealth Servicesisresponsibleforallhospitalservicesandhealthservices inanumberofhealthorganizationsincludingpalliativecare, mentalhealthandcontinuingcare,andsomelong-termcare organizations.20 Theconsolidationofallregionalhealth authoritiesintooneentitycreatedan “integratedhealthcare system” thatallowedAHStoshareinformationandprovide standardizedcareacrossmanyhealthcareorganizations.20,21 Currently,AHShas106acutecarehospitals,caredelivery programsat850facilities,27,774continuingcarebeds,256 communitypalliativeandhospicebeds,and2,785addiction andmentalhealthbeds.19 Thegoalofamorecentralizedhealth systemwasthereductioninduplicationofservicesandfunctions acrossthemanyhealthregionsandagencies(e.g.,supplychain andprocurementprocesses,policyandaccountabilityprocesses, HR,and finance).Aconsolidatedmanagementstructurehas enabledAlbertatoadvanceaprovince-widedatainfrastructure bothwithinandacrosshealthorganizationsinallregionsofthe province.Alberta’sprovince-widegovernancemodeland centralizeddatainfrastructuremeasurehealthsystem performanceacrosstheprovince.
WhenAHSwascreated,andprovincialhealthcarewas centralized,Albertamadeasignificantinvestmentinits enterpriseresourceplanninginfrastructure,whichenabled digitalsupplychaininfrastructureandvisibilityofproduct utilizationforallhospitalsacrosstheprovince.Thisdata
infrastructureenablestrackingandtraceabilityofproduct utilizationfrommanufacturerstopatientcareunitsineach hospital,includingtheadoptionofglobalstandardsto supportaccuracyofproductidentificationandproduct attributes.23
AlbertaHealthServiceshasestablishedtheContracting, Procurement,andSupplyManagement(CPSM)teamto manageallsupplychainprocessesacrosstheprovince.The CPSMteamisresponsibleforthecontracting,purchasing, inventorymanagement,warehousing,anddistributionofsupplies,products,andequipment.24 Themandateofthisteamis tomanagesupplychainservicesforallAHSorganizations, includingsourcing,procuringproducts,trackingutilization, integratingcliniciansintosupplychainteams,andmanaging supplychaindata.24 PriortotheCOVID-19pandemic,the CPSMsupplychainteam,andAHSmorebroadly,had reportedsignificantgainsincostsavingsforsuppliesby streamliningsupplyprocesses,trackingutilizationand productinventory,andreducingcostsduetoproductwaste. Allsourcing,contracts,andprocurementaremanagedbythe CPSMteam,ensuringeveryhospitalandcareteamhavethe productsneededtodelivercare.
COVID-19inAlberta
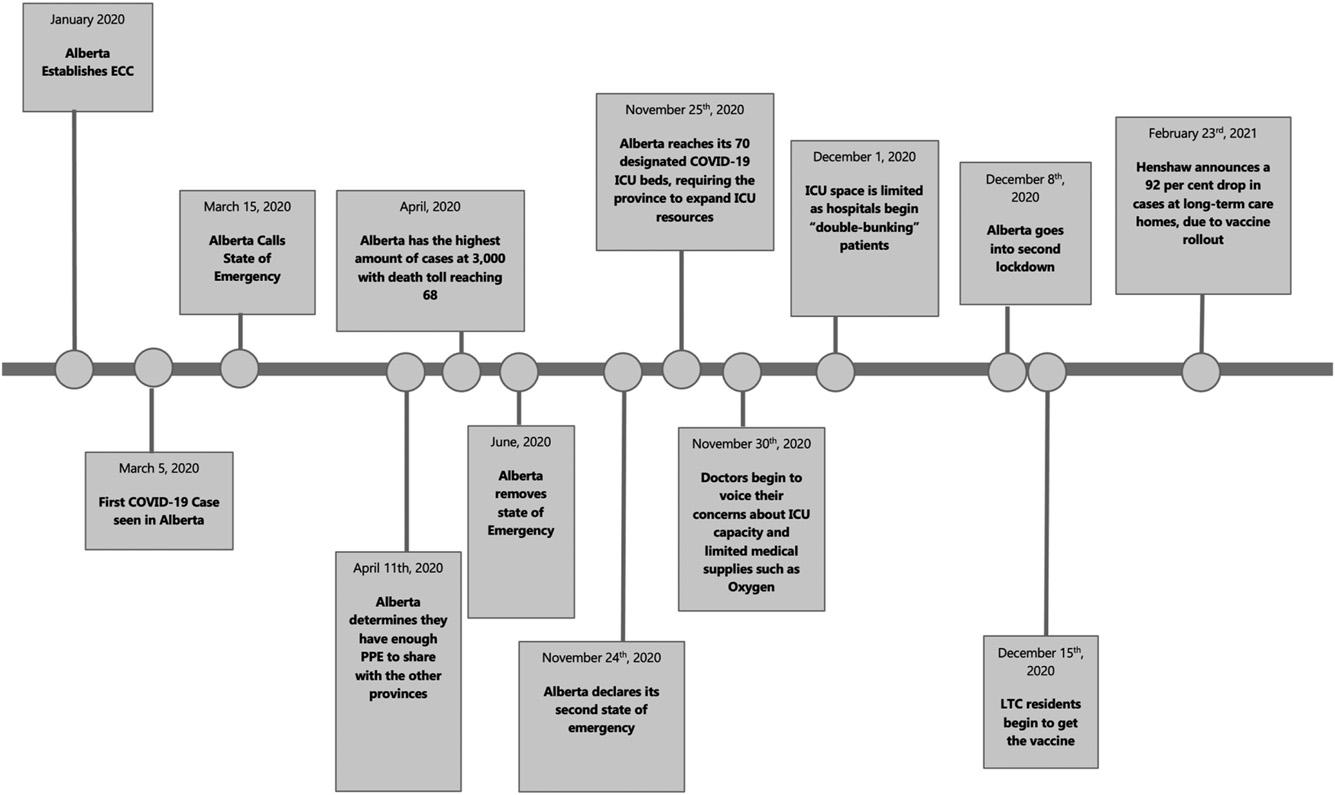
The firstCanadiancaseofCOVID-19wasreportedJanuary26, 2020inToronto,Ontario,withcasesrapidlyspreadingacross thecountryinthefollowingmonths.25 OnJanuary30,2020,the provinceofAlbertaEmergencyCoordinationCentre(ECC)was establishedtomanagethepandemicresponseacrossthe province.OnMarch5,2020,Albertareportedits firstcaseof COVID-19andpublichealthmeasureswerequicklyestablished tocontainthespreadofthevirus.Albertarespondedquicklyto the firstwaveofthepandemic,announcingastateofemergency onMarch15,2020andimplementedthenecessarypublichealth restrictions.25 Duringthe firstwaveofCOVID-19,casesin Albertapeakedat3,138onOctober19,2020.26 InMay2020, theprovincesawadeclineinnewinfections,andrestrictive publichealthmeasureswereeased.InNovember2020,things againbegantochangeascasecountsbegantorise.Inthesecond wave,caseshitapeakof20,500activecases.27 Therapidrisein casenumbersofCOVID-19overwhelmedAlberta’scontact tracingsystem,whichhadlimitedhumanresourcescapacityto keepupwiththedemandsforlabtestingservices.28 Asthe secondwaveunfolded,thegovernmentdelayedimplementation ofadditionalrestrictionsorpublichealthinitiatives,particularly lockdowns,despiterisingcasecounts.29 Cliniciansbeganto voicetheirconcernsaboutthecapacityofthehealthsystemto meetdemandsforcare,includingconcernsforthelimitedhealth workforceresourcesandcriticalsupplies,suchasoxygen,to adequatelysupportpatientcare.30 Fieldhospitalswerecreatedto increasehospitalcapacity,andseveralintensivecareunitswere requiredto “double-bunk,” puttingtwopatientsineachroomto managetheincreasingnumbersofcriticallyillpatientsinfected withCOVID-19.31 Astheprovincereached1,500newcasesa day,AlbertareachedouttotheFederalGovernmentandRed
Crossforsupportofthe fieldhospitals.32 Albertaenteredits secondlockdownonDecember8,2020,asvaccination programsbeganinlong-termcareorganizations. DecembersawthehighestnumberofcasesofCOVID-19 amonglong-termcareresidents,with776casesreported, andtwooutofthreeCOVID-19deathswereresidentsof long-termcare. 33 Toreducetheimpactonlong-termcare, Albertabegantoprioritizethevaccinationoflong-termcare residents.Justtwomonthslater,onFebruary23,2021,the ChiefMedicalOffi cerofHealthannouncedthattherehadbeen a92%dropincasesatlong-term carehomes,attributedtothe vaccineroll-out.34 Thesequenceofkeyeventsissummarized in Figure1 .Thekeythemesemergingfromanalysesprofi led thecriticalroleofleadershipandgovernancestructuresthat supportedleaderdecision-makingapproachestomanagethe pandemic.
Leadership,governancestructure,anddecision-making
TheMinisterofHealthandPremierofAlbertaweretheprimary decision-makersforAlberta’sCOVID-19response,informed andadvisedbypublichealthandAHSleadership,describedby onekeyinformant:
“Policydecisionsaremadebygovernmentcabinetandwedeliver wehaveanabilitytoinfluence,butgovernmentisowning everything.” (HealthSystemLeader)
Findingsrevealedadecision-makingstrategythatwas centralizedintheAlbertagovernmentwherebyAHSleadershipprovidedinformationtoinformdecisions,describedby onekeyinformant:
“Whatgovernmentdidearlyonwastheysetupsomethingcalled theemergencymanagementcabinetcommittee.Thisemergency managementcabinetcommittee,wecallitEMCC,atonepointwas meetingthreetimesaweek.AHSwouldbethereprobablyabout80%of thetime.(Supplychainleaders)wouldbepresent.Itwaschairedbythe Premier,andthatwaswherealotofthedecisionsweremadeabout shuttingdownschools,socialdistancing,visitationguidelines,soalot oftheoperationalpieces.TheywantedreportingfromAHS,andyou know,PPEwaspartofthat.” (SupplyChainLeader)
AlbertaHealthServicesprovidedsupplychaindataand informationtothecabinetcommitteeinordertoprovidesupply chainexpertisetogovernment.Akeyinformantdescribedhow supplychaindatainformedgovernmentdecisions:
“…theemergencymanagementcommitteeofthecabinetwas presentedwiththeoptionsinourmodelwhichbasicallysaid,you know,inaprobablescenariothisiswhatyou’regoingtoneed.In eachscenario,hewasprovidedwithinformationonwhat(supplies) wereavailabletoday,andtheprojectedburnrate,andhowmany dayswasthatgoingtolast.” (HealthSystemLeader)
Albertahadpreviousexperiencewithemergencies,suchas wildfires(e.g.,FortMcMurray)andsevere floods(Calgary),which meantthatemergencymanagementplans,communication,and governancestructureswerewellestablishedinAlberta,wellbefore
Figure1. SequenceofeventsinAlberta.
theCOVID-19pandemic.Keyinformantsidentifiedthat experiencewiththehistoryofcrisesinAlbertahadestablished theemergencymanagementstructuresnecessarytorespondtothe COVID-19crisis.Akeyinformantdescribedthisas “organizationalresilience,” inthefollowing:
“Youhavetothinkaboutthefactthatit’snotjustaboutpersonal resilience.It’severybodyhasgottohavetheirpersonalresiliency builtup,butit’salsoaboutorganizationalresiliency.So,ifyouasan organizationareresilientwithyour,youknow,forexamplebeing abletohaveagoodemergencydisastermanagementsysteminplace, makingsureyou’vegotbusinesscontinuity,makingsureyou’vegot theworkforce.ThatorganizationalresiliencyisIthinkwhat’sbeen key,Ithink,tokeepingpeoplefunctioning.” (HealthSystemLeader)
AlthoughAlbertawasfamiliarwithcrisismanagement,the pandemicrequiredleadershiptoadapttotherapidlychanging events.Akeyinformantdescribestheleadership’sabilityto learnandadapttotherapidlychangingpandemicscenarios:
“Wewereatsomepointchangingpolicyeveryweekoreverytwo weeks.Ithinkjustthereallyrapidlychangingenvironment.You knowwealsolearnedprettyquicklythatthebestwaytodealwith issues,withPPE,wedidaPPEtaskforce.Thatmanagement organizationmodel,wehadtochangeouremergencycoordinatingcentermodeltosomethingthatwasmoreadaptablefor theenvironmentthatwe’rein Weputthesetaskforcestogether, bringalltheexpertsacrosstheprovinceandthenweweremuchmore nimbleatapproachingthings.” (HealthSystemLeader)
Ataskforcestrategy,suchasthePPEtaskforce,wascreated tomobilizeexpertiseacrosstheprovincetofurtherinform leadershipdecisionstomanagethepandemic.TheAlberta StrategicClinicalNetworks(SCNs)wereengagedtoinform decisionsastheSCN’swerestructuredtointegrateclinical expertise,researchcapacity,patientperspectives,andpolicymakers thatwereaccessedtogenerateevidenceinformtaskforcedecisions, describedbyakeyinformant:
“InAlbertayouknow,wealwaystookaprovinciallensandeven beforepandemichit,severalofour(StrategicClinical)networks wereinvolvedinpullingtogetherprovincialgroupstostartto organizeourselvesprovinciallyaroundwhatwethoughtwe wouldneedtododuringCOVID19 TherewasaPPEtask forcethatwassetup,sohowdowethinkaboutmakingsurewehave PPE,andnotonlydowehaveit,canwebuildaproductionmodelso thatwecananticipateourneedsovertime.” (HealthSystem Leader)
Pandemicresponseandmanagementwereledbygovernment cabinet,informedbyAHSdata,information,andleaderexpert advice.TheroleofAHSleadershipwastooperationalize governmentdecisionstomanagethepandemic.Theprovincewideleadershipstructurereachedacrossclinicianleaders, academicleaders,andpatientsbymobilizingexistingSCNs acrosstheprovince.Theexistingleadershipinfrastructureof AHSsupportedahighlyintegratedandcentralizedprovincial pandemicresponse,ledbygovernmentdecisionmakers.
Supplychainvisibilityandprovincialcapacity
AlbertaHealthServiceshadanestablishedsupplychaindigital infrastructureattheonsetofthepandemic,whichenabled trackingandtraceabilityofcriticalsuppliesandequipment frommanufacturerorsuppliertohospitalcaresettings. Implementationofaprovince-wideElectronicMedicalRecord (EMR)wasunderwayatthetimethepandemicunfoldedin Alberta.However,untiltheEMRinstallationwascompleted, traceabilityofproductswasvisibleonlytoclinicalcareunits. Pointofcarecaptureofproductutilizationwasnotyetpossible, whichprecludedvisibilityofproductutilizationatthepointof care.However,theexistingdigitalinfrastructureenabledAlberta leaderstotracksupplyutilizationratesforeveryhospitalcare settingintheprovince:
“Weknewthatpre-COVIDourburnratewasabout33,000aday.At kindofthepeakofCOVIDwhenwehadthehighestnumberof cases,wewererunningthrough760,000aday.” (SupplyChain Leader)
TheAlbertateamhadmemberswithcloserelationshipsin China,whichofferedearlyinsightsintotheunfoldingpandemic wellbeforeCOVID-19caseswereevidentinNorthAmerica, describedinthefollowing:
“Ithink,itwasprobablyDecember,thatwehadstartedhavingsome discussiononwhattheimpact[ofCOVID-19]wouldbe.Itwas mostlybecausewehadpeoplewhoworkwithuswhoareChinese andarestillverywellconnectedbackhome .Whatwediddoat thatpointintimewasreviewwhatourstockpilewas,ofcoursenever anticipatingthatthedemandwasgoingtobesosignificant,and basicallymadearequesttopurchaseabout$2.3milliondollars’ worthofinventoryofsomeofthebasicneeds,likeatthattimewe thoughtweshouldorderN95s.” (HealthSystemLeader)
Theglobalshortageofcriticalsuppliesquicklyescalated. Albertahadtheadvantageofaccurateutilizationdata,described asthe “burnrate,” whichinformedpreparationsonmanaging productshortages,particularlyPPE.Asthepandemicprogressed,theCPSMteambegantoexperienceincreaseddifficulty procuringsuppliesaseveryglobalhealthsystemcompetedfor suppliesincriticalshortage.Akeyinformantdescribesthe limitationsofthesupplychainstrategies,whichprioritized lowestcost,ratherthansupplydiversityandcapacity:
“Ithinkfailingofthesupplychaininhealthcaresystemsisbecause oftherealfocusonreducedcostsandthereforeyouknow, streamliningthesupplychainchannelsandyouknow,those typesofthings,we’realsotiedintothesecontractswithGPOs.” (HealthSystemLeader)
Traditionalprocurementstrategies,suchasbulkpurchasing throughgrouppurchasingorganizations(GPOs),wereunableto respondtothemassivesurgeindemandforproductsgiven limitedmanufacturingcapacitytoscaleproduction,andthe limitedinventoryreservesavailable.The “just-in-timemodel” ledtoconservationstrategiesbyGPOs,whereAHSwasputon “allocation” meaningtheGPOwasunabletoprocureadditional
supplyvolumesbeyondthenormalcontractedvolumesof products.Insomeinstances,supplierswereunabletodeliver theirnormalcontractedvolumes.Theconservationmeasures reliedonallocationformulaethatprescribedthesupplyvolumes availabletoAHS,despitethesignificantsurgeindemandof patientsandtheurgentneedforcriticalsuppliesinmuchhigher volumesthannormal,describedinthefollowing:
“
Theotherpieceisthat[GPOname]says,wellmymanufacturers can ’tsupplyittoyou.[They]canactuallysaythatandgetawaywith thatbecausetheyareavirtualentity.IfIamthedistributorfor Alberta,Iactuallycan’tgotoAlbertaandsaysorry,toughluck,you don’tgetmasks.” (HealthSystemLeader)
“Thefunnythingthathappenedwasallthesedistributorscame backtousandsaidyouknowwhat,weactuallycan’thelpyou,we havenoproduct.We’reputtingyouonallocation.Everyvendoris onallocation.” (HealthSystemLeader)
AlbertaHealthserviceshadconsiderablestrengthsina centralizedsupplychainmanagementfortheprovincethat wasdigitallyenabledtocreatetransparencyandhighly accuratedataonsupplyutilizationanddemands.However, theglobalshortagesofsuppliesrapidlyescalated,resultingin havingnoalternativebutto findnewsourcesofproductsin ordertomeetthesurgeindemandforcriticalproductstosupport capacityforcaredeliveryacrosstheprovince.
Sourcingandprocurementstrategies
TheCPSMteamdesignedthreestrategiesto findalternative sourcesofcriticalsuppliesinordertomanagethemassive increaseindemandforcare:(i)establishingcontractsdirectly withmanufacturers;(ii)diversifyingsuppliersources;and(iii) engagingcompaniesinAlbertaasdomesticsuppliers.Notlong aftertheonsetofthe firstwaveofthepandemic,thescopeofthe mandateofAHSincreasedtosupplyPPEtoallhealth organizationsandteams(e.g.,primarycare,long-termcare,and privatepracticesettings),as wellasanumberofcommunity agenciesandessentialworkenvironments(e.g.,bordersand airports).Thisexpandedscopewasdesignedtofurther strengthenthepandemicresponseacrosstheprovince;however, itplacedadditionalpressureontheCPSMteamtoensurecritical supplieswereavailabletoallwhoneededthem.Eachofthethree strategiesengagedtosourceproductsaredescribed.
(i) Contractswithmanufacturers: The firststrategy implementedto findalternativesourceswastomobilizerelationshipsbetweenindividualsinAlberta andtheirnetworkinChina,wherethemajorityof manufacturersofPPEwerelocated.TheCPSMteam contractedwithprocurementspecialistsbasedin ChinatoleverageprocurementexpertiseinChinato identifymanufacturerstohe lpsourcedirectcontract relationshipswithmanufact urers.TheCPSMstrategy focusedonprocuringmanufa cturercapacity,rather thanlimitprocurementeffortstopurchasingsupplies, described:
“
Wedidmanufacturerdirectcontractsthroughanintermediary whereby,wehavecontractswithtwoleadingmanufacturersin China weactuallyhavetohaveasourcethatisgoingtogiveus committedproductiontime,andproductionquantitiesforaboutan 18–24-monthperiodsothatwecanseewherethemarketisgoingto endup.” (SupplyChainLeader)
TheCPSMteamshiftedtheirsupplysourcingeffortstofocus onmanufacturingcapacity,ratherthancompetewithevery globalhealthsystemforpurchasingsupplies.
(ii)
Dataanddigitalsupplychaininfrastructureinform decisionsandoutcomes
Leadersanddecision-makersinAlbertahadtheadvantageof accesstoreal-timesupplydatatoaccuratelytracksupply utilizationvolumesacrosstheprovince.Thesedataalso offeredsubstantialvalueintrackingtheoutcomesunfolding acrosstheprovince.Oneinformantsharedtheuseofsupply chaindatatotracktheeffectivenessofpublichealthmeasures, suchastransmissionofthevirusamongthehealthworkforce, describedinthefollowing:
“
Diversifyingsuppliers:
Thesecondstrategywasthe shiftfromsinglegeographicsuppliersourcingtomultiple geographysupplierssourcingtoofferabalancedsupplier networktomitigateriskofsupplyinterruptions.Diversity insuppliersourcingofferedredundancyinsupplysources sothatintheeventoffurthersupplyshortagesor disruptions,Albertacouldsourceproductfrommultiple andvariedjurisdictions,describedinthefollowing:
IthinkforsomeitemswewereveryNorthAmericancentric.For thoseitems,IthinkwenowhaveamixofprobablyAsiaandNorth America.IfIlookatN95sforexample,wearenowChinaandUS wealsowereabletoget3Mmasksreleasedthroughthe3Mfactory outofThailandforexample.Andthen,ifyoulookatprocedure masks,IthinkthatlandscapehasshiftedfromChinatoveryNorth Americancentric,right.Gloves,Ithink,hasshiftedfroma predominantlyMalaysiamarket.” (SupplyChainLeader)
(iii) Mobilizationofdomesticsuppliers:
Asthesecond waveunfolded,theCPSMteamlookedfornewsources ofdomesticmanufacturerstoofferfurthersourcesof criticalsupplywhich,overcomedistributionlogistics fromoffshoremanufacturers.Sourcingofproductfrom manufacturersinChinahadresultedinsomeshipments beingdefective,orinadequateforuseduetopoorquality (e.g.,unusualodourofmasks).Domesticsuppliersoffered theopportunitytoworkcloselywithmanufacturersto ensureproductqualitycouldbeassessedlocallytoensure productwouldbeacceptableforuse.Asupplychain leaderdescribesthisstrategy:
“Thesecondwavealsogaveusanopportunitybecauseinthe firstwaveit was,youknow,tryand findthebestsupplypossibleandworkwithlocalto seeifwecangetsomethingdone.Weactuallystartedworkingwithalocal manufacturerformasksforexample,andwesaid ‘well,ifyoucancome upwithamaskworkingwithus,wewouldcommittobuyingacertain numberofmasks’...Wenowhavealocalmanufacturerofmasksin Alberta,startedoffwithavolumeoffourmillionamonth,scaleditallthe wayupto10million(permonth)rightnow.” (HealthSystemLeader)
Sourcingandprocurementapproachesrapidlyshiftedaway fromthetraditionalfocusonlowestcost(e.g.,purchasingthrough GPOcontractstoleverageeconomiesofscaletoachievelowest cost)andmovedtowardmorediversesourcingstrategyfocused oncontractswithmanufacturers,bothlocalandglobal,toreduce theriskofexperiencingcriticalsupplyshortagesinfuture.
“ForthePPEupdateswewerelookingatourdatafromworkplace healthandsafety,likehowmanyofourworkershadbeeninfected andwhereweretheygettinginfected,becausethey(Decision makers)wantedtoknowwhethertheguidelinesforwearingPPE shouldbedifferentindifferentunits.Thisisaboutsupplychaindata informingdecisionsonoutcomes,inthiscaseinfectionratesrelative touseofPPE.” (HealthSystemLeader)
Thedigitally-enabledsupplychaininfrastructureenabled integrationofdatainnearrealtimetoprovideinsightsinto pandemicoutcomesassociated withsupplyutilizationaligned withpublichealthmeasurestocontainthespreadofinfection. Thistransparencyprovidedleaderswithsupplychaindataon useofPPEmeasures,relativetooutcomessuchasthe capacityofhospitalbeds,ICUcapacity,andCOVID transmissionoutcomes.Theimportanceofdata-driven decisionsisdescribedinthefollowing:
“Imeanwereallyusedthedatatoactuallyguideusastowhatwe weredoing.Thathelpedussetthetarget.Ithinkeverythingthatwe decidedintermsofthetargetsandthenumberswerebasedon evidence.ItwasalwaysbasedondataandevidenceandthePremier wasverystrongaboutthat.” (HealthSystemLeader)
DatainfrastructureenabledleaderstotrackCOVID-19 outcomes(e.g.,ratesoftransmissionofthevirus,hospitalization rates,anddemandsonsupplyinventorytosupportcareteamsand publichealthmeasures)relativetowarehousingandinventory levelsofcriticalproducts.Theabilitytoaccessthedatainrealtime allowedforpredictiveanalyticsandmodellingtoinform procurementteamsonsourcingprioritiesregardingspeci fi c suppliesneeded,productvolumesrequiredtosupportcare delivery,andhowsupplydistributionisprioritized.Thedigital infrastructureinAlbertaenabledleaderstomakeproactive,datadrivendecisionsonsupplyprocurementandutilization,which resultedinsufficientsupplyinventorythatmadeitpossibleforthe Albertagovernmenttosharesupplieswithotherprovinces experiencingcriticalshortages:
“ThePremierreallywantedtomakesurethatwesupportedthe otherprovincesandthatwaswhenwegavesomePPEtoOntario, Quebec,andactuallytoBC.Sothatwaskindofthestoryaround that,butasIsaid,there’snowaythatwewouldhavebeenabletodo thatwithoutthedataandthemodellingtoknowhowmuchwe need.” (SupplyChainLeader)
Digitally-enabledsupplychaininfrastructurewasastrategic assetfortheprovinceofAlbertathatenabledleaderstomake data-drivendecisions,informedbytransparencyofsupply inventories,trackaccurate “burnrate” orsupplyutilization, andtracktheoutcomesofpublichealthmeasures(e.g.,mask mandates)tomitigatetherisksoftransmissionofthevirus, particularlyamongthehealthworkforce.Dataemergingfrom supplychaininfrastructureoffertheuniqueopportunityto proactivelysourceandprocureproductstoensurehealth organizationshavethecapacitytoeffectivelyandsafety respondtorapidlychangingeventsthroughoutpandemics.
Conclusionandimplicationsforhealthleaders
ThepandemicresponseinAlbertawasuniquetoallother provinces,primarilyasAlbertaistheonlycentralized, province-widehealthsystemparticipatinginthisstudy,and alsoduetothemostadvanceddigitallyenabledsupplychain strategy,whichwaswell-establishedpriortotheonsetofthe pandemic.Thehistoryofemergencypreparedness,provincially organizednetworksofclinicianleaders,andproactivestrategies tosourceandprocurenewmodelsofsupplysourcingfocusedon manufacturingcapacity,arekeystrengthsthatcontributedto Alberta’scapacitytoeffectivelyrespondtothepandemic. Leadershipstrategiesinthiscasestudyhighlightimportant implicationsforleadersofhealthsystemsandarealigned withkeydimensionsoftheLEADSinaCaringEnvironment framework,whichembodiesthekeyskills,behaviours,abilities, andknowledgerequiredtoleadinallsectorsoftheeconomyand typesoforganizations.35 The findingsfromthiscasestudy reflectleadershipcapacityalignedwithfourdimensionsof theLEADSframework:Achievingresults,Engagingothers, Developcoalitions,andSystemtransformation.35
Achievingresults. Albertaleaderswereabletodemonstrate impressiveresults,byleveragingsupplychaindatatoinform decisionsonpandemicmanagementthatproactivelyengaged newsourcesofPPE,andenabledtraceabilityofoutcomesand progressofCOVID-19casesacrosstheprovince.Data-driven decisionswerealsocriticalforaccuratemodellingandforecasting ofsupplyvolumedemandsthatmadeitpossibleforAlbertato supplyotherprovinceswithPPE.Finally,datawereusedascritical evidencetoevaluatetheeffectivenessofPPEpolicyrelativetothe ratesoftransmissionofthevirustotheworkforce.Data-driven decisions,informedbyadigitally-enabledsupplychain infrastructure,wasastrategicassetAlbertausedtoevaluatethe effectivenessandimpactofpandemicresponseefforts.
Engagingothers. ThiswasevidentintheAlbertacasestudy. Albertaleadersestablishedanemergencymanagement infrastructurewellbeforethe firstcasewasdiagnosedin Alberta,andengagedawiderangeofexpertiseacrossthe provinceleveragingtheSCNsofleadersthatincludedclinical, academia,andcitizendomainsofknowledgetoinformdecisionmaking.TheSCN’sandAHSleaderswereabletoeffectively mobilizeknowledgeandprovincialnetworksofleaderstoinform
pandemicmanagementstrategies,particularlyintheearlywavesof COVID-19.Leadershipdecisionswereledbygovernment(e.g., cabinetcommittee),informedbysupplychaindatafromacrossthe provincethatenabledrapidexpansionofsupplysourcingstrategies toensuremosteveryorganizationintheprovincehadaccessto PPEtomitigatetheriskoftransmissionofthevirus.
Developcoalitions. Alberta findingsrevealthatthisprovincehad existingcoalitions(e.g.,networks)ofexpertsintheSCNs.The SCNsweremobilizedearlyinAlberta’spandemicresponseand servedanimportantroleinmobilizingintelligence,expert knowledge,andevidencetosupportandinformdecisions,as wellassupportandenableimp lementationofpandemicstrategies.
Systemtransformation. ThisisahallmarkfeatureofAlberta’s healthsystemdatingbackto2009whenallregionsandhospitals wereconsolidatedintoasingleprovincialhealthsystemunder oneadministration,AHS,alongwithimplementationofa digitally-enabledsupplychaininfrastructure,whichassumed acriticalroleindata-drivenleadershipdecisionstosupport pandemicmanagement.ThesuccessofAlberta’spandemic strategywasfurtherevidencedbyitscapacitytoshare inventoriesofsupplieswithotherprovincesincriticalneed duetoinabilitytoprocurecriticalsuppliesfastenoughtomeet thesurgeindemand.
TheimplicationsoftheAlbertacasestudyforhealthleaders are:
• Investinginarobusthealthcaresupplychaindigital infrastructureenablesleadershipdecision-makingthatis groundedinreal-timedatatoachieveproactiveresponses toeventscausingdisruptioninsupply,andtoinform decisionsthatareabletoproactivelymanagepandemic supplyinventories.
• Data-drivendecisionsthatareabletoevaluateandtrack theeffectivenessofdecisions,suchaspublichealth decisionstopreventtransmissionofthevirus,were centrallyimportanttothesuccessofthisprovincein managingthepandemicearlyinwavesoneandtwo.
• Developingsustained,strategiccoalitions,ornetworksof multisectoralexperts,includingclinicalandhealthcare supplychain,enablesthemobilizationandmultidisciplinary understandingofevidencetosupportsounddecision-making.
• Albertasupplychainleadershipwasabletopivotand adjusttheirsupplychainpractices,movingawayfrom traditionalsupplychaintodevelopstrategiesthatappear tobemoreresilienttofuturedisruption.They useddomestic suppliers,contractswithmanufactures,anddiversified suppliersasameanstochangeandimprovetheirapproach.
• Duetoitscentralizednature,therewasa “singlesourceof truth” thatcreatedclear,concisecommunicationand provideddirectionacrossthesystem.Theclear approachmitigatedconfusionandallowedfordirect linesofaccountability,withclearlinesofaction,tobe issuedacrosstheprovince.Theleadforpandemic managementdecisionswasthePremierandcabinet,
withpublichealthassuminganadvisoryrole.Thereis evidencethatdecisionsofpoliticalleadersinmanaging thepandemicareinfluencedbypoliticalpartyvalues ratherthanbeingdirectlyinformedbyevidenceandpublic healthexpertise.
Collectively,thestrengthsofAlberta ’ssupplychain infrastructureaffordedandenableddata-drivendecisionsbased onevidence,whichacceleratedeffortstostrengthendiverse suppliersourcingandmobilizedomesticmanufacturing. Achievingresults,engagingothersandmobilizingexisting coalitionsofexpertise,andleveragingarobustdigitallyenabled supplychaininfrastructurewereexamplesofprovincialleadership dimensions,whichcontributedtoveryresilientsupplychain capacityacrosstheprovince.
Funding
ThisprojectwasfundedbyCanadianInstitutesofHealthResearch (GrantNo.VR5172669).
ORCIDiD
AnneW.Snowdon https://orcid.org/0000-0003-4640-6842
References
1.SnowdonA,AlessiC. Visibility:TheNewValueProposition forHealthSystems.Windsor,ON:WorldHealthInnovation Network;2016.Availableat: https://scanhealth.ca/explore-projectsresources/view-all-articles/89-visibility-the-new-value-propositionfor-health-systems-condensed-version
2.WongJC.HospitalsfacecriticalshortageofIVbagsduetoPuerto Ricohurricane. TheGuardian;2018. https://www.theguardian. com/usnews/2018/jan/10/hurricane-maria-puerto-rico-iv-bagshortage-hospitals .
3.Mosta fi dAH,PalouRedortaJ,SylvesterR,WitjesJA. Therapeuticoptionsinhigh-risknon-muscle-invasivebladdercancerduringthecurrentworldwideshortageofbacille Calmette-Guerin. EurUrol .2015;67(3):359-360.doi: 10.1016/j. eururo.2014.11.031
4.LowDE.SARS:lessonsfromToronto.In:KnoblerS,MahmoudA, LemonS,MackA,SivitzL,OberholtzerK,eds Learningfrom SARS:PreparingfortheNextDiseaseOutbreak:Workshop Summary.Washington,DC:NationalAcademiesPress;2004:63-83.
5.SmithPM,OudykJ,PotterG,MustardC.Theassociationbetween theperceivedadequacyofworkplaceinfectioncontrolprocedures andpersonalprotectiveequipmentwithmentalhealthsymptoms:a cross-sectionalsurveyofCanadianhealth-careworkersduringthe COVID-19pandemic. CanJPsychiatry.2021;66(1):17-24.doi: 10.1177/0706743720961729
6.RicklesH. TheMysteriousCaseofHealthcareLogistics,AHRMM AnnualConference.SanFrancisco:SettingtheStandard;1999.
7.EbelT,GeorgeK,LarsenE,ShahK,UngermanD. BuildingaNew StrengthintheHealthcareSupplyChain.NewYork,NY: McKinsey&Company;2013.
8.KwonI-WG,KimS-H,MartinDG.Healthcaresupplychain management;strategicareasforqualityand financialimprovement. TechnolForecastSocChange.2016;113(partB):422-428.
9.DixitA,RoutroyS,DubeySK.Asystematicliteraturereviewof healthcaresupplychainandimplicationsoffutureresearch. IntJ PharmHealthcMark.2019;13(4):405-435.doi:10.1108/IJPHM05-2018-0028
10.GendyAWA,LahmarA.Reviewonhealthcaresupplychain [conferencepaper].In:2019IEEE/ACS16thInternational ConferenceonComputerSystemsandApplications(AICCSA). November3-7,2019;AbuDhabi,UnitedArabEmirates:1-10.doi: 10.1109/AICCSA47632.2019.9035234
11.KumarS,BlairJT.Healthcare fix:leveragingthelessonsfromthe foodsupplychain. TechnolHealthCare.2013;21(2):125-141.doi: 10.3233/THC-130715
12.ArshoffL,HenshallC,JuzwishinD,RacetteR.Procurement changeinCanada:anopportunityforimprovingsystem performance. HealthcManageForum .2012;25(2):66-69. doi: 10.1016/j.hcmf.2012.03.002
13.AbdulsalamY,GopalakrishnanM,MaltzA,SchnellerE.Health carematters:supplychainsinandofthehealthsector. JBusLogist 2015;36(4):335-339.doi:10.1111/jbl.12111
14.LandryS,BeaulieuM.Thechallengesofhospitalsupplychain management,fromcentralstorestonursingunits.In:DentonB,ed. HandbookofHealthcareOperationsManagement.NewYork, NY:Springer;2013;184:465-482.doi:10.1007/978-1-4614-58852_18.
15.MandalS.Theinfluenceoforganizationalcultureonhealthcare supplychainresilience:moderatingroleoftechnologyorientation. JBusIndMark.2017;32(8):1021-1037.
16.AldrighettiR,ZennaroI,FincoS,BattiniD.Healthcaresupply chainsimulationwithdisruptionconsiderations:acasestudyfrom NorthernItaly. GlobJFlexSystManag.2019;20(1):81-102.doi: 10.1007/s40171-019-00223-8
17.SnowdonA,SaundersM.COVID-19,workforceautonomyand thehealthsupplychain. HealthcQ.2021;24(2):16-26.
18.YinRK. CaseStudyResearch:DesignandMethods.4thed.. ThousandOaks,CA:Sage;2009.
19.AlbertaHealthServices. AboutAHS.AlbertaHealthServices; 2021.Availablefrom: https://www.albertahealthservices.ca/about/ about.aspx
20.DonaldsonC.Fire,aimready?Alberta’sBigBangapproachto healthcaredisintegration. HealthcPolicy.2010;6(1):22-31.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2929894/.
21.VeitchD.Oneprovince,onehealthcaresystem:adecadeof healthcaretransformationinAlberta. HealthcManageForum 2018;31(5):167-171.doi:10.1177/0840470418794272.Epub2018 Aug22.
22.AlbertaHealthServices. ReporttotheCommunity:Whoweare AlbertaHealthServices;2019.Availablefrom: https://www. albertahealthservices.ca/assets/about/publications/ahs-ar-2020/whowe-are.html
23.SnowdonA,WrightA.Casestudy:supplychaintransformationin albertahealthservices. HealthcQ.2018;21(3):34-36.doi:10. 12927/hcq.2018.25703
24.AlbertaHealthServices. VendorGuidetoDoingBusinesswith AlbertaHealthServices.AlbertaHealthServices;2012.Available from: https://www.albertahealthservices.ca/assets/about/org/ahs-orgcpsm-guide-doing-business-with-ahs.pdf
25.SlackJ. 2020LookBack:Alberta’spandemicResponse Edmonton,AB:CTVNewsEdmonton;2020.Availablefrom: https://edmonton.citynews.ca/2020/12/24/2020-look-back-albertaspandemic-response/
26.FletcherR. AlbertaHitsNewPandemicPeakforCOVID-19 Cases.Toronto,ON:CBCNews;2020.Availablefrom: https:// www.cbc.ca/news/canada/edmonton/alberta-covid-19-coronavirusactive-cases-pandemic-1.5768458
27.AlbertaHealthServices. COVID-19AlbertaStatistics Edmonton,Alberta:AlbertaHeal thServices;2021.Available from: https://www.alberta.ca/stats/ covid-19-alberta-statistics. htm#total-cases
28.AlbertaHealthServices. AHSEngagingAlbertansinClose ContactNotification.Edmonton,Alberta:AlbertaHealth Services;2021.Availablefrom: https://www.albertahealthservices. ca/news/Page15694.aspx.
29.FedorT. ArehealthRestrictionsandLockdownsaViolationofthe CharterofRights? Calgary,AB:CTVNewsCalgary;2020. Availablefrom: https://calgary.ctvnews.ca/are-health-restrictionsand-lockdowns-a-violation-of-the-charter-of-rights-1.5204571
30.MoslehO. ‘We’reinbigtrouble’:Albertadouble-bunkinginICUs, limitingoxygenduetosurgeinhospitalizations. TorontoStar; 2020.Availablefrom: https://www.thestar.com/news/canada/2020/
12/01/were-in-big-trouble-alberta-double-bunking-in-icus-limitingoxygen-due-to-surge-in-hospitalizations.html
31.RossT,MasonK. AlbertaReachingOuttoRedCross,Feds AboutPossibleFieldHospitals.660News;2020.Availablefrom: https://www.660citynews.com/2020/12/03/alberta-reaching-outto-red-cross-feds-about-possible-field-hospitals/.
32.CochraneD. AlbertaAsksFederalGovernment,RedCrossfor FieldHospitalsasCOVIDSpreads.Toronto,ON:CBCNews; 2020.Availablefrom https://www.cbc.ca/news/canada/calgary/ alberta-field-hospitals-red-cross-1.5825439
33.JefferyA. Optimism,ReliefasAlberta’sLong-TermCareCentres seeSignificantDropinCOVID-19Cases.Toronto,ON:CBC News;2021.Availablefrom: https://www.cbc.ca/news/canada/ edmonton/optimism-relief-as-alberta-s-long-term-care-centres-seesigni ficant-drop-in-covid-19-cases-1.5925376.
34.HerringJ. Alberta’sCOVIDrateisthehighestinCanada.Howdid thethirdwavegetsobadhere?CalgaryHerald;2021.Available from: https://calgaryherald.com/news/local-news/albertas-activecase-rate-is-more-than-twice-the-canadian-average-how-did-theprovinces-third-wave-get-so-bad
35.DicksonG,ThollB.Bringingleadershiptolifeinhealth:LEADS inacaringenvironment.In: PuttingLEADStoWork.2nded.New York,NY:Springer;2020.doi:10.1007/978-3-030-38536-1
