healthiersleepmag.com Winter 2022-23 | Artificial Intelligence Issue Introduction to Artificial Intelligence Sleep Tracking Devices New Feature: Clinician as Advocate Five Questions with Dr. Azizi Seixas Better Sleep for All: Expanding Acccess to Sleep Health for Underserved and Diverse Populations
Healthier Sleep
A publication of World Sleep Society
Your Trusted Source for Improving Sleep
Publisher
World Sleep Society
Editor
Karen Kilpatrick
Issue Reviewers
Melissa C. Lipford, MD
Maya Ramagopal, MD
Robert J. Thomas, MD
Sales Manager
healthiersleep@worldsleepsociety.org
Designer Brook Lanz
Contributing Writers
Matteo Cesari, PhD
Colin Espie, PhD, DSc
Lindsay Jesteadt, PhD
Rosei Skipper, MD
Haoqi Sun, PhD

Jessica Thomas, MPH
Robert J. Thomas, MD
Alexander Wachter, MSc
For advertising or editorial contact information, email healthiersleep@worldsleepsociety.org or visit healthiersleepmag.com for current rates.
Healthier Sleep is published up to five times per year by World Sleep Society, 3270 19th Street NW, Suite 109, Rochester, MN 55901 and distributed to sleep medicine and research professionals as well as the public. No part of this publication may be reprinted or reproduced without written permission.
Healthier Sleep does not necessarily endorse the claims or content of advertising or editorial materials. All advertisements and editorial material included represents the opinions of the respective authors.

World Sleep Society/Healthier Sleep Magazine does not provide or offer medical advice. All content within the magazine, such as text, graphics, information obtained from sleep experts, and other material, is for informational purposes only. The content is not intended to be a substitute for medical diagnosis, advice or treatment. Relying on information provided by World Sleep Society and/or any of its employees, experts within the material, or other writers is solely at your own risk.

©2022 World Sleep Society. All rights reserved. ABOUT


3 | healthiersleepmag.com CONTENTS Winter 2022-23 | Artificial Intelligence Issue 07 Can Your Digital Twin Heal You? 14 Sleep Stage Scoring with Artificial Intelligence 20 Two Challenges of Digital Therapeutics 22 Patient Organization Highlight: Sleep Consortium 24 Artificial Intelligence Applications in Sleep Medicine | 04 | Introduction to AI |08 | Sleep Tracking Devices | 18 | Dealing with the Data In Every Issue Page 23 Your latest buzzword is Brain Age The BuZZZ About Sleep Bedtime Reads Page 11 When Brains Dream Right Now in Sleep Science Page 17 Detecting Parkinson's Disease through Sleep Clinician as Advocate Page 12 Five Questions with Dr. Azizi Seixas Ask the Sleep Experts Page 29 Your questions answered by sleep professionals Harmony Biosciences through an unrestricted educational grant has supported the ‘Clinician as Advocate’ article. On the Cover Azizi Seixas, PhD, Director of The Media and Innovation Lab and Associate Director of the Center for Translational Sleep and Circadian Sciences at the University of Miami
Introduction to Artificial Intelligence
By Jessica Thomas, MPH
When most people think about artificial intelligence (AI) and its applications, they tend not to think about its link to sleep and sleep health. The truth is, though, that AI is at the forefront of providing insights into what is and isn’t working for humans and their sleep. During an interview with Dr. Thomas Penzel, Chair of the Sleep Medicine Lab in Berlin, we uncovered the role of artificial intelligence in sleep medicine, its history, and what’s expected in the future.
The History of Artificial Intelligence in Sleep
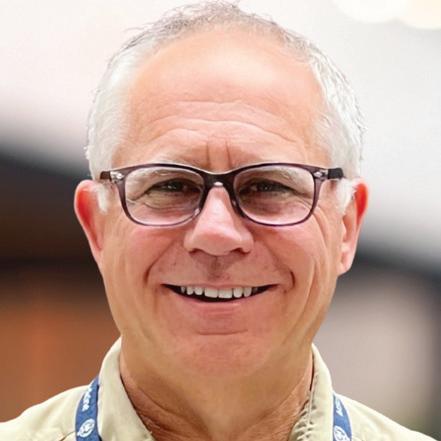
Dr. Penzel has forty years of top-notch medical and scientific expertise and has been at the forefront of sleep medicine research for the last 15 years. During his extensive career, he has seen a transformation in how artificial intelligence has been used to generate meaningful sleep insights.

Early in Dr. Penzel’s career, AI was primarily used to diagnose sleep stages and then provide scores to these various stages. Over the years, AI has progressed to find extensive information about sleep disruption events like sleep apnea and leg cramps. These sleep events have the potential to negatively affect the quality of sleep for millions of people around the world.
More recently, there has been a move towards passive and nondisruptive data collection. This means that what happens in the sleep lab more closely mirrors what happens in the real world. According to Dr. Penzel, being equipped with more accurate information about what is disrupting sleep helps doctors to implement meaningful treatment programs.
4 | Winter 2022-23 | Artificial Intelligence Issue
The Different Types of AI
Dr. Penzel acknowledges that AI is focused on the broad goal of looking at challenging issues and regularly updating information and expectations to determine the likelihood of an event occurring. Yet despite these broad similarities, he notes that it is crucial to recognize that there is a wide range of different AI tools. For instance, there is machine learning, big data analysis, and data trees. Due to technological innovations, though, machine learning tends to make up a disproportionate share of AI innovations. In fact, many people use the terms AI and machine learning interchangeably.
The Terminology Used in AI
The Limitations of AI Data

One of the most significant controversies in the field of AI, as it relates to sleep, is what happens when a human who is reading a sleep study and an AI tool disagree about a sleep event. Dr. Penzel highlighted that in past years there was a tendency to try to determine which of the two was wrong: the person or the machine. It was seen as a binary choice.
Today, he notes that there is more of a willingness to see these events as shades of gray. For example, it’s possible that AI technology may be better suited to identify certain sleep apnea symptoms. In comparison, a human with years of clinical experience may be better skilled at picking up on different types of subtleties. In the real world, these shades of gray and nuance are positive and will ultimately generate better patient care than in the previous black-andwhite world.
During the interview, Dr. Penzel mentioned that consumers often use “artificial intelligence” as a broad umbrella term. However, there are important terms that both patients and doctors should be aware of. One of the most important terms is trustworthy AI. According to Dr. Penzel and others, trustworthy AI is AI where we have faith in the generated outcomes and can use it to inform patient care. This does not mean that we blindly trust AI conclusions, however. Human verification is still a necessary component. Intro to AI continued on page 6 >
5 | healthiersleepmag.com
Dr. Penzel also noted another significant limitation of AI: it tries to smooth the average. This means that AI may not be as well-equipped to deal with a unique patient or an outlier. These rare cases would then also have to be excluded from system updates. Simply put, AI does well with things that are within the bounds of what has been seen before but struggles with the unusual or one-offs.
The Importance of Data Quality in AI
Today, artificial intelligence is being used in an ever-increasing number of medical situations. Dr. Penzel highlighted how critical it could be to guide treatment protocols in intensive care units. For example, AI can quickly analyze bloodwork and urine results more objectively than traditional doctors’ analyses.

However, Dr. Penzel also notes that an information gap exists. People do not understand exactly what AI is, and they are concerned about whether the information generated by AI is trustworthy. Dr. Penzel contends that AI is largely trustworthy, but it hinges on the quality of the inputs. Poor quality inputs will never generate strong outcomes, no matter how good the technological tool is.
It’s more important now than ever before that the data used in AI is accurate and consistent. Poor data inputs will not provide the precise information needed to learn more about sleep and improve health outcomes.
The Future: Where Sleep and AI Intersect
The future of medicine, according to Dr. Penzel, is a future that will incorporate AI into a wide variety of specialties, ranging from oncology to sleep medicine. This is primarily because of how fast AI is. It can create a tremendous amount of information quickly, and it also controls for and mitigates the impact of human errors.
But AI is not perfect. It also has numerous downsides, based on Dr. Penzel’s analysis, including a lack of understanding of what AI really is. This means that the best medical solutions will happen when AI cutting-edge technology is combined with the input of highly skilled medical professionals
To learn more about sleep medicine from a trusted source for improving sleep, visit healthiersleepmag.com
Jessica Thomas is a public health professional, health & wellness writer, and entrepreneur. She enjoys learning about and educating others on healthy living and observing how technology is changing the healthcare space.
References
University of Copenhagen Faculty of Science. Artificial intelligence enhances efficacy of sleep disorder treatments. ScienceDaily. 8 June 2021. www.sciencedaily.com/ releases/2021/06/210608113257.htm
Ducharme J. A Third of Americans Are Sleep-Deprived. This Technology Could Help Them Rest Easier. Time. January 25, 2019. https://time.com/5494363/sleep-artificial-intelligence/
Goldstein CA, Berry RB, Kent DT, et al. Artificial intelligence in sleep medicine: background and implications for clinicians. J Clin Sleep Med. 2020;16(4):609-618. doi:10.5664/jcsm.8388
6 | Winter 2022-23 | Artificial Intelligence Issue
Intro to AI continued from page 5
Dr. Thomas Penzel
Can Your Digital Twin Heal You?

Researchers at the University of Miami Miller School of Medicine are using an innovative approach to address sleep health issues in underserved communities. The project, called the Media and Innovation Lab (MIL) Box, delivers wearable and nearable technology devices to a patient’s home. The devices include smart watches, smart rings, blood pressure monitors, air quality devices, smart phones, and more. Data is captured 24 hours a day for seven days and uploaded to the cloud. Once the data is received, researchers use AI machine learning to identify diseases and create new ways of understanding health and wellness. Dr. Azizi Seixas, Founding Director of the MIL, says the technology is “geared towards understanding the potential barriers and facilitators to people getting good sleep.”

Once a person’s data is collected, researchers can create a biometric algorithm that represents that person’s “digital twin.” According to Dr. Seixas, the digital twin is a significant step towards personalized medicine. Instead of choosing a treatment or medication based on what has worked in a similar demographic group, the digital twin can be used to select the approach that will work best for the individual. “Instead of doing trial and error types of treatments, we will know already the solutions that will work best,” said Dr Seixas.
The data infrastructure can also be used to better understand why some people get a certain illness and others do not. Dr. Seixas said the research could also identify new early warning signs of health problems, catching issues before they become a major health concern. It might sound like science fiction, but Dr. Seixas says, “your digital twin will heal you!”
Dr. Azizi Seixas
7 | healthiersleepmag.com
Sleep Tracking Devices
By Jessica Thomas, MPH
In recent years, there has been a dramatic increase in the purchase of devices that monitor sleep quality and quantity. This is driven by increased marketing efforts and a heightened understanding by consumers of the importance of sleep for overall health. To gain more knowledge on these devices, we interviewed Dr. Timothy Morgenthaler, the Director of the Center for Sleep Medicine at Mayo Clinic in Rochester, Minnesota. Drawing on his 25 years of professional experience, he enlightened us on wearables and "nearables" and their role in sleep medicine.
Wearables and Nearables: Understanding What They Are
No matter what type of device a person decides to buy, it’s important to remember that all devices have the same fundamental goal: to collect information and offer insight into the amount of sleep a person gets and the quality of their sleep.
Wearables are the category of devices that you are likely most familiar with. They come into direct contact or touch with the person using
them. In fact, you’ve probably heard of some of the more common wearable devices like Apple Watches and FitBits. Many devices commonly considered smartwatches and activity trackers now include sleep tracking technology.
"Nearables" are devices that, as the name suggests, come near a user without directly touching them. Dr. Morgenthaler mentioned that these could be sensors or pads placed directly under a person’s mattress. While some devices are clearly placed very near to the user, Dr. Morgenthaler cautioned not to put too much emphasis on the near part of nearables. He noted that as technology improves, these devices can likely be placed farther and farther from the individual.

8 | Winter 2022-23 | Artificial Intelligence Issue
Not All Products Are Created Equally
There has been an explosion of new products available in the wearable and nearable markets in recent years. Many consumers struggle to separate the good devices from the not-sogood. Dr. Morgenthaler noted that this could be challenging even for medical providers since there is a lack of peer-reviewed studies that compare products. Even when studies do exist, they are often based on earlier generations of the device since technology is evolving so quickly.
activity as their baseline. This information is then used to create conclusions based on various algorithms. The algorithms vary dramatically from company to company, which can also play a role in quality differences.
Next Generation Data Collection Offers More Information

Movement-based measurements are typical in many wearables. Newer models, however, also collect other information, such as heart rate. Changes in heart rate and/or pulse rate can give insight into whether a person’s sleep is disrupted or not. It can also provide information, at least to a limited degree, on which sleep stage a person is in.
Nearables also collect data based on a person’s movement. For example, sensors placed under a person’s mattress can measure whether a person is tossing and turning during the night based on subtle pressure changes in the mattress. This tossing and turning can be a sign of disrupted or low-quality sleep. The sensors in under-mattress nearables are usually finely calibrated and can detect even slight pressure changes, such as those that could result from snoring.
Not all nearables collect information based on movement or activity, though. Some nearables use infrasonic sound waves to collect information about heart rate and breathing rate, as well as other physiological data. Other, simpler nearables use a microphone to detect sounds during the night, including snoring.
Numerous factors may explain the quality differences between devices. One driving factor is that different devices use different technology to collect patients’ data. Dr. Morgenthaler noted that wrist-based wearables tend to focus on Devices continued on page
9 | healthiersleepmag.com
>
14
No matter what type of device a person decides to buy, it’s important to remember that all devices have the same fundamental goal: to collect information and offer insight into the amount of sleep a patient gets and the quality of their sleep.
The Challenges of Nearables and Wearables
While nearables offer invaluable information about sleep quality and quantity, they are not perfect, according to Dr. Morgenthaler. For example, they may detect noises that another person in the room (not the device user) is making. They may also pick up background noise that is entirely unrelated to a person’s sleep. It’s a careful balancing act to get the sensitivity of sensors precisely right.
There are also potential problems that affect the quality of information from wearables. Some wearables may have too sensitive of a threshold that records everything as a movement, even if it is not really a movement. At the same time, other wearables may lack sufficient sensitivity and movement may be missed.
Problems also occur when the algorithms for the collected information incorrectly evaluate the data. Many companies have worked to improve their algorithms and correct the errors, but it’s not always perfect. Updating algorithms can also take extensive time. Some companies seem to be better at this process than others, based on Dr. Morgenthaler’s evaluation.
Final Words of Wisdom from Dr. Morgenthaler
When asked for his conclusions about wearable and nearable devices, Dr. Morgenthaler described them as the ultimate double-edged sword for both medical providers and users. People who use these devices often come to doctors with lots of data from their devices. Although this data can be helpful in starting conversations, it can also take time to sort out what information is truly meaningful.
The good news is that most devices available on the mass market do a relatively good job of estimating how much a person is sleeping each night and when they are falling asleep. Information about the total amount of sleep is one of the most important pieces of evidence that a provider may need to start treating sleep disturbances. The information generated from these at-home devices often closely mirrors what doctors find from inpatient sleep studies. Currently, though, overnight tests, such as sleep studies, are undoubtedly more scientifically rigorous
Consider This Cautionary Note
Dr. Morgenthaler underscored that wearables are much less accurate at determining sleep stages. For instance, some users might be concerned when their wearable tells them that they are not getting enough REM sleep. It’s important to consider that this conclusion may not be correct since it hinges on differentiating heart rate variability from stage to stage.
Reassuringly though, sleep stage information is frequently not integral in driving treatment protocols, according to Dr. Morgenthaler. However, it may be challenging to communicate this limitation to wearable users, who are often quite attached to the data they receive from their devices.
The most important thing that Dr. Morgenthaler wants wearable and nearable users to know is that these devices can be great starting points. At this point, however, they should never replace a thorough clinical evaluation from a skilled sleep practitioner. He also cautions that buyers need to carefully sort through the large variety of available options and focus (when possible) on buying a device that has been independently scientifically tested

10 | Winter 2022-23 | Artificial Intelligence Issue Devices continued from page 13
Dr. Timothy Morgenthaler
Jessica Thomas is a public health professional, health & wellness writer, and entrepreneur. She enjoys learning about and educating others on healthy living and observing how technology is changing the healthcare space.
Bedtime Reads
When Brains Dream
 by Antonio Zadra and Robert Stickgold
by Antonio Zadra and Robert Stickgold
Questions on the origins and meaning of dreams are as old as humankind and as confounding and exciting today as when nineteenth-century scientists first attempted to unravel them. Why do we dream? Do dreams hold psychological meaning or are they merely the reflection of random brain activity? What purpose do dreams serve?
When Brains Dream addresses these core questions about dreams while illuminating the most up-to-date science in the field. Written by two world-renowned sleep and dream researchers, it debunks common myths that we only dream in REM sleep, for example – while acknowledging the mysteries that persist around both the science and experience of dreaming.

11 | healthiersleepmag.com Looking to learn even more? Each issue, we highlight a book about sleep.
US-NAR-2200140/Sep
Find Real Personal Stories at KnowNarcolepsy.com Hear Their Stories Now Website is intended for US residents only.
Know Narcolepsy is a registered trademark of Harmony Biosciences. Harmony Biosciences name and logo are registered trademarks. © 2022 Harmony Biosciences. All rights reserved.
2022
Clinician as Advocate
Five Questions with Dr. Azizi Seixas, PhD
Dr Azizi Seixas, PhD is an Associate Professor of Psychiatry and Behavioral Sciences and an Associate Director of the Center for Translational Sleep and Circadian Sciences at the University of Miami Miller School of Medicine. He is also the Founding Director of The Media and Innovation Laboratory, where they have implemented an initiative that uses wearable and nearable monitoring technology to analyze the sleep of individuals from traditionally underserved communities.

12 | Winter 2022-23 | Artificial Intelligence Issue
Harmony Biosciences is the sponsor of this ‘Clinician as Advocate’ article.
What led you to work in sleep medicine?
My journey into sleep really is both fortuitous and serendipitous. I applied for a training program at NYU school of medicine and got in; it’s fortuitous because the deadline to apply was in two days and I found it at 2 am and obviously as a sleep person, you should be sleeping. I felt like it was fate in the sense that I struggle with sleep issues myself. I’m coming from a lived experience perspective and I know the struggles that people go through that prevent them from getting sufficient sleep or good sleep. Me-search is research, so that’s how I’ve ended up in sleep and it has catapulted me to do something greater than just contributing to sleep but also to other areas as well.
Why is patient advocacy important to you?

Advocacy is critical because it increases awareness about a health condition or a particular health behavior that may impact a certain subgroup of individuals. In the case of sleep, it impacts everyone. Advocacy also helps to increase access to care and access to providers who can treat sleep health issues. It also increases prevention and avoidance policies. I think advocacy is also very critical to help us with increasing the affordability of different types of health services.
How are you using artificial intelligence and technology in your work?
It pervades throughout everything we do at the Media and Innovation Lab (MIL). We have several funded projects that have some element of sleep; not all of them have elements of sleep, but everything that we do is fundamentally trying to make healthcare and getting healthy and staying healthy easier. Technology in its truest definition is really making complex things simple, so anything that we do is technological because it is striving to reduce complex things and make them easier.
You’re on a mission to make healthcare more equitable. Tell us more about that. We don’t have a well-codified plan of how to do it because it’s complex, but we have a bold vision and we have the conviction and the will to accomplish those things in partnership with others. We have created the MIL Box as a starting point; we’re pitching the MIL Box as solving the issue for the uninsured and the underinsured and the folks who have insurance but don’t really use it.
We need to demystify healthcare and engage and focus on wellness. With the MIL box we can say “you own this, this is your personal history, let’s get benchmarks, let’s learn, let’s do quick checkups, let’s see how you’re progressing.” We can use machine learning or AI to say these are the types of food you need to eat to lower your risk, this is the level of stress management you need, this is the amount of physical activity and the type of exercise that you need to do and when to confer the best health benefits from those. It has to be an adaptive, personalized type of recommendation as opposed to a one-size fits all. Our science needs to reflect the lived experience of people.
What
are you most excited about with your work?
I’m excited because of the team we have; this is not a one-person show at all. I couldn’t do what I do without them. We’re excited about where our imagination takes us. We’re also doing some really cool things in technology, particularly around Web3 types of technology. With Web3, you have your own health data and you travel with your own data. Instead of going to different hospitals and having them request your documents, you travel with it. It also allows for you to have a distributed ledger and say, “I’m going to put my fitbit data in it, my blood pressure data, my apple health data,” and you can leverage that data to have lower premiums in your insurance. I think that’s where health is going and that’s what we’re trying to push as well.
We can use machine learning or AI —
It has to be an adaptive, personalized type of recommendation as opposed to a one-size fits all. Our science needs to reflect the lived experience of people.
Sleep Stage Scoring with Artificial Intelligence
By Matteo Cesari, PhD and Alexander Wachter, MSc
Sleep stage scoring is a fundamental task when objectively evaluating sleep with polysomnography (PSG), the gold standard method for sleep assessment. The current rules for sleep stage scoring are defined in the Manual for Scoring Sleep and Related Events, which is regularly updated by the American Academy of Sleep Medicine (AASM). Using these rules, sleep experts and technicians manually score the PSG recordings, labeling each 30-second period of sleep (also called an “epoch”) as wakefulness,

rapid eye movement (REM) sleep, or one of the three non-REM sleep stages. Manual sleep stage scoring is time-consuming and can be inconsistent because the rules for scoring sleep stages are prone to subjective interpretation. When a PSG recording is given to two different technicians, they tend to agree on only 8590% of the epochs. The agreement decreases significantly for recordings of patients with neurodegenerative diseases.
Automatic methods would be highly beneficial in this field. Algorithms are faster and provide consistent and objective scoring, overcoming both problems of time consumption and subjective interpretation of PSG recordings. The first attempts to automatically score sleep stages began in the 1960s when simple rule-based algorithms were proposed. Such algorithms consisted in a series of human-defined rules to try to mimic manual scoring. However, due to their simplistic approach and the many exceptions that could not be foreseen by the rules, the algorithms did not perform as well as human scoring.
Artificial intelligence (AI) is a branch of computer science in which, to complete the required task,
14 | Winter 2022-23 | Artificial Intelligence Issue
the computer captures the patterns between the data and the desired output on its own without explicitly defined rules from a programmer. In the context of sleep stage scoring, the computers are given a set of thousands of sleep epochs previously scored by humans to learn the relationship between the data and the expected sleep stage. Once the learning is complete, the AI algorithms are tested on new unseen epochs and compared with human scoring to understand whether the algorithm performs as well as humans. In recent years, different research groups have proposed new AI algorithms, which reached the same accuracy as human experts in scoring sleep stages. These achievements are due to the increased computational power of computers as well as to the availability of large datasets, which allow computers to learn even the most difficult and rare patterns.
The results recently achieved by AI algorithms are promising in the sense of making AI-based sleep scoring a routine process in sleep labs around the world. This would allow sleep labs to evaluate PSGs faster and make it possible to record more patients and/or to reduce the costs related
to PSGs as well as increase the consistency between different sleep labs, making evaluation more standardized. Thanks to the increasing development of more portable at-home PSG systems, AI-based sleep stage scoring has the potential to record even more sleep studies and make waiting times for PSGs significantly shorter.
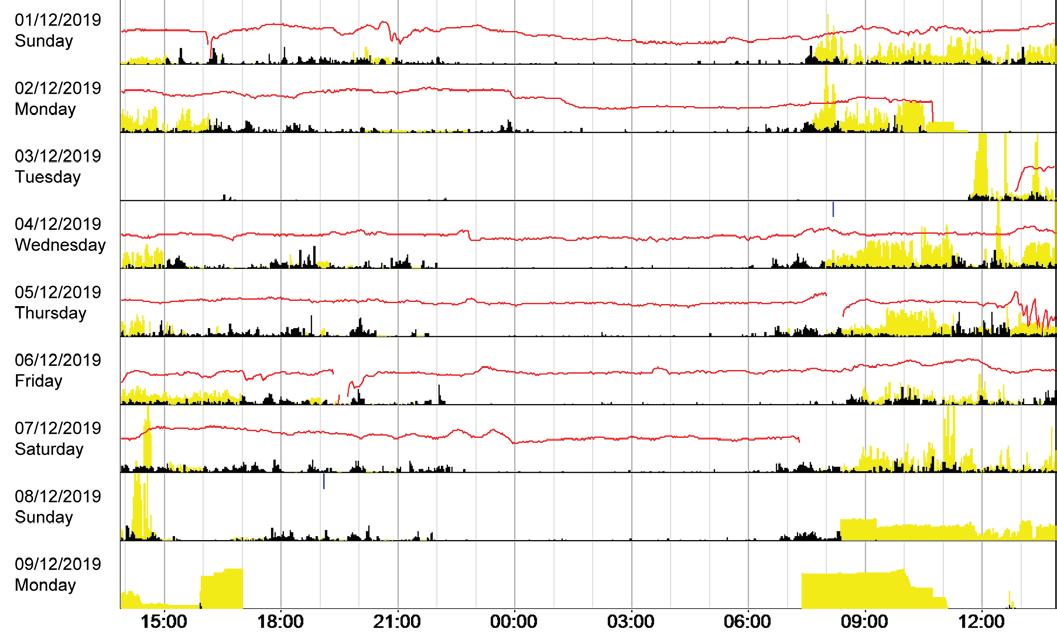
In addition to scoring PSGs, research studies show that AI-based sleep stage scoring might provide new information. AI algorithms not only provide the sleep stage for each sleep epoch but also estimate the probability of such stage, which is useful to better understand the transition between different stages and the stability of sleep structure. Research shows that the instability measures derived from these probabilities might be useful for improved diagnosis of narcolepsy type 1. Furthermore, since sleep is a continuous and dynamic process, automatic AI-based scoring could be adapted to score sleep epochs shorter than 30 seconds. This is better suited to capture the underlying information rather than simplifying it to 30-second epochs, which is a rudiment dating from the time sleep was scored on paper.
Scoring continued on page 18

15 | healthiersleepmag.com
>
Recent evidence shows that AI-based sleep stage scoring could potentially be used in clinics and, in the not so distant future, to improve the diagnosis of sleep disorders. The integration of AI in sleep medicine, however, requires clear guidelines to build trust in these automatic procedures. The AASM is actively working in this direction with a dedicated taskforce. To certify the reliability of AI-based sleep stage scoring algorithms, the AASM is developing a certification program in which AI algorithms for sleep stage scoring will be tested on unseen recordings owned by AASM and scored by several scorers. Based on the agreement with the human scorings, AI algorithms will receive a certification ensuring their reliability.
The time for moving from manual to AI-based sleep stage scoring is approaching, and clinics and sleep centers need to be prepared for this shift, which will reshape their organizational structure as well as the approach with patients
*Citations available on healthiersleepmag.com
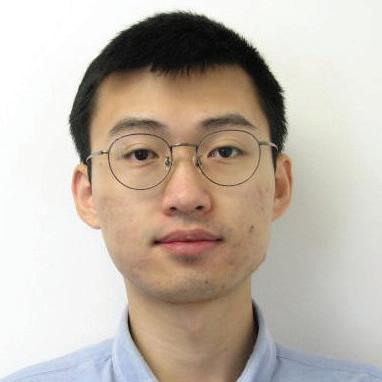
Matteo Cesari, PhD has been working in the field of sleep medicine & research since 2016. Dr. Cesari is currently Postdoc Fellow at the Sleep Disorders Unit, Department of Neurology, Medical University of Innsbruck in Austria. Alexander Wachter, MSc has been in the field of computer science since 2020. He is currently PhD student at the Sleep Disorders Unit, Department of Neurology, Medical University of Innsbruck in Austria.


The CG Fund
In his memory, World Sleep Foundation, a nonprofit 501c(3) organization, created an endowment in honor of Dr. Guilleminault. The CG Fund awards travel grants to young investigators in sleep medicine and research to encourage and enable their participation in the scientific sleep community.








CG Award Applications
Applications for the CG Award are accepted year-round and reviewed three times per year. The deadlines are: April 30 | August 31 | December 31
Christian Guilleminault “CG”
1938 – 2019
Dr. Christian Guilleminault (known as “CG” among colleagues) devoted his career to the development and advancement of sleep medicine and research. His groundbreaking research in the areas of sleep apnea, pediatric sleep disorders, and narcolepsy made him a leader in the field of sleep medicine and research. Throughout his career, Dr. Guilleminault mentored hundreds of physicians and scientists.
Get Involved!
• Contribute to the CG Fund
• Share the CG Award application with colleagues
Scan the QR code with your phone camera or visit worldsleep.info/yi for more information.
16 | Winter 2022-23 | Artificial Intelligence Issue
Matteo Cesari, PhD
Scoring continued from page 17
Alexander Wachter, MSc
Right Now in Sleep Science
Detecting Parkinson's Disease through Sleep
Researchers in the United States have discovered a way to use artificial intelligence (AI) to evaluate Parkinson's disease (PD), a neurological disease that affects more than 10 million people worldwide.

PD is a progressive disorder that does not have a specific diagnostic test. PD is typically diagnosed based on patient reports of symptoms like tremors in the hand muscles or stiff arms or legs. However, these symptoms usually do not show up until several years after the disease has started, leading to late diagnosis and missed opportunities for early treatment.
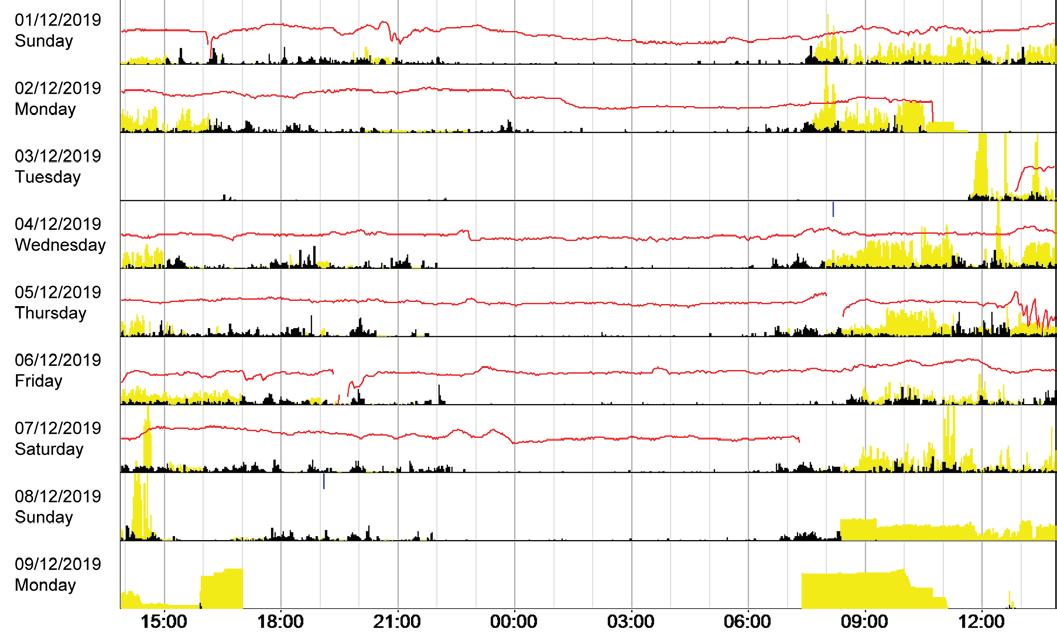
There is a link between PD and breathing, though, and sleep breathing disorders often present years before PD symptoms. In the study, researchers used an AI-based system to look for abnormal nighttime breathing patterns in a set of data with over 7,500 people and nearly 12,000 nights. The breathing signals were collected using either a wearable device (in this case, a breathing belt worn on the person’s chest or abdomen) or nearable device (a bedside radio signal transmitter).
Researchers found that for patients using the wearable device for one night, the AI system was about 80% accurate in identifying PD. For patients who used the nearable device for several nights, the accuracy was even higher.
The researchers from the study are hoping the AI-based system can lead to earlier diagnosis and treatment of PD. Using wearable or nearable technology could also be easier and less expensive for patients, both in diagnosing the disease and tracking its progression.
References
Yang Y, Yuan Y, Zhang G, et al. Artificial intelligence-enabled detection and assessment of Parkinson’s disease using nocturnal breathing signals. Nature Medicine. 2022; 28: 2207–2215 doi: https://doi.org/10.1038/ s41591-022-01932-x
https://www.nature.com/articles/s41591-022-01932-x#authorinformation
17 | healthiersleepmag.com
These days you can use technology to track almost anything in your life – including your sleep! You may have noticed that a watch or device that you already own records sleep data, or maybe you’ve purchased a specific tracker just for that purpose. Over the past few years these devices have become very popular.
Whether you choose to use a watch, a bracelet, your phone, or other device, what do you do with the data once you get it? Can it help you improve your overall health? We spoke with sleep expert Massimiliano de Zambotti, PhD about how these trackers work and what to do with the information they provide.
Dealing with the Data
By Rosei Skipper
According to Dr. de Zambotti, sleep trackers can record data such as sleep timings, how long you sleep, and nighttime awakenings. The newer generation of sleep trackers can also measure heart rate and its variability, blood oxygen levels, breathing patterns, and even stages of sleep. The data from the device sensors are processed by the manufacturer’s algorithms, then the data are combined and presented to the user through an app or website.
For a tracker to be most helpful, it must record accurate and reliable data and it should also provide the right contextualization and information to interpret it. Dr. de Zambotti says that at this time, consumer devices can’t be used to diagnose specific sleep disorders, and it’s still
18 | Winter 2022 | Restless Legs Syndrome
unclear how helpful the data can be from a clinical standpoint. The devices can help individuals be more aware of their sleep and may even help users to improve their sleep habits over time. However, while reaching the magic 10,000 steps per day for activity is under one’s control, achieving a specific sleep target is not so straightforward.
Some devices generate a “nightly sleep score” or a “grade” of the previous night’s sleep. Dr. de Zambotti explained that the goal of the sleep score is to take the data collected overnight and turn it into a number that reflects the quality of sleep of the user. It is still unclear, however, what this number truly represents. For example, you might wake up feeling refreshed and energetic, but your sleep score is lower than usual. Because scientists don’t have a full understanding of what goes into the sleep scores for different devices, Dr. de Zambotti said to pay more attention to how you feel and to other standard values these devices provide that have more actionable insights. Dr. de Zambotti suggests focusing on objective numbers like what time you go to bed and wake up.
While some people benefit from tracking their sleep over weeks or months, others might find
themselves getting overly invested with the information. Some users can get competitive about improving their sleep score or even feel anxiety about the data. It’s important for each person to note whether they feel a tracker and the data it generates are helpful to them as an individual.
The bottom line? If you think a sleep tracker might be helpful to you, try it out! There are many options, so make sure to research various devices and pick one that matches your individual lifestyle and budget. And as always if you have concerns about your sleep or health, be sure to contact your health care team.
Rosei Skipper, MD completed her Psychiatry residency and Child fellowship at the Mayo Clinic in Rochester, MN. She is currently pursuing further training in psychoanalytic therapy.
Massimiliano de Zambotti, PhD is a sleep neuroscientist serving as the Lead of the Translational Sleep Technology Unit, Human Sleep Research Program at SRI International in Menlo Park, California. He is also the Cofounder and Chief Scientific Officer of Lisa Health Inc.

19 | healthiersleepmag.com
For a tracker to be most helpful, it must record accurate and reliable data and it should also provide the right contextualization and information to interpret it.
Dr. Massimiliano de Zambotti
Two Challenges of Digital Therapeutics
And Solutions for How We Can Overcome Them
By Colin Espie, PhD, DSc
For more than a generation, international guidelines have recognized that cognitive behavioral therapy (CBT) is the recommended initial treatment for chronic insomnia in adults of any age, and that this is a recommendation clinicians should follow under most circumstances. From young people to the elderly, from those who are otherwise healthy to those with medical or psychiatric comorbidities or even with another sleep problem, CBT offers the promise of improved quality of sleep for patients with chronic insomnia.
Unfortunately, we will never have enough therapists to treat everyone who seeks CBT for insomnia relief. How can we scale CBT to fit this need? The obvious answer is mental health digital treatments, or digital therapeutics, which can deliver CBT through mobile apps to millions of people instantly and simultaneously.
Digital therapeutics raise suspicious eyebrows among sleep professionals – for good reason. This is a massively capitalized industry, valued at $3.5 billion and projected to reach $22 billion within 10 years, so it’s an understandable concern that apps can be products of consumerism and smart marketing and not methods of treatment. Some are.
Yet chronic insomnia is a healthcare crisis in need of an immediate solution and no solution holds more promise than digital CBT to meet this need. How can we address and overcome the two primary challenges of digital therapeutics to deliver CBT? Here are my ideas:
Challenge Apps for mental health problems have highly variable standards of evidence.
Solution
Digital therapeutics must be required to pass rigorous testing.
All mental health digital treatments are not created equally. The best apps are evidencebased, having undergone substantial randomized controlled trials with safety and effectiveness data further verified in real-world settings. Other apps use the loose standard of evidenceinformed, meaning the product has CBT content but has not undergone any trials to prove its safety or effectiveness. This approach can lead to untested apps which prioritize marketing over science. Indeed, I don’t believe that insomnia treatment apps should even be made available until they are specifically trialed for clinical benefit. We wouldn’t contemplate that for a pharmaceutical!
20 | Winter 2022-23 | Artificial Intelligence Issue
the Professor
From
To be considered a digital therapeutic, the product must undergo the same rigorous testing as any approved medication. We absolutely must not lower the bar because the purpose is no less than to deliver CBT as first-line treatment for insomnia worldwide. High-quality digital therapeutics can cross this threshold, and a few already have.
Challenge
It’s hard to know which CBT apps are evidence-based, which compromises faith in all of them.
Solution
Build patient trust, and clearly differentiate digital therapeutics as a new category of treatment.
In an app store, apps can all look alike – just as a pill that’s an approved medicine, for example, can look like a pill that’s a homeopathic drug. Labels, however, clearly distinguish one from the other.
Digital therapeutics that meet high standards of testing need to be clearly labeled as proven treatments. While wellness apps hold potential in promoting relaxation, they can’t be confused with evidence-based therapies and effective digital treatments. We need a system that clearly communicates whether an app is akin to an approved treatment or the mere equivalent of a discretionary spend item like a homeopathic remedy.
It’s hard to make a pill look attractive or interesting, but it is possible to dress apps up to be more engaging. Strong evidence of efficacy, clear labeling on the app, and listing on a digital formulary should help us determine which apps are credible and which are not.
Although analogies to drugs may be imperfect, it is important to apply the same standards, if not even higher, to the digital therapeutics clinical research pipeline. Some may say that the emergence of a new approach like digital therapeutics presents the opportunity to “break
the mold.” However, the counterbalance to that is that the greater the novelty, the greater the need for caution.
A Matter of Urgency
Insomnia is associated with cascading costs, not just in sleep itself but also relating to heart disease, high blood pressure, and diabetes. It’s linked to reduced work productivity and missed work. It’s hard to comprehend how much we sacrifice, on an individual and societal level, when we don’t get good quality sleep, yet have a treatable insomnia problem! Few people understand this more than the readers of this publication.
People already turn to their phones or to the internet for insomnia relief; during the first five months of the pandemic in 2020, Google had 58% more searches for “insomnia” than in the same period over the previous three years. Without the leadership of sleep scientists, wellness apps and digital therapeutics will continue to mingle as look-alikes. With our leadership, digital therapeutics can offer millions a proven insomnia treatment in a responsible manner that protects our patients, upholds our standards, provides CBT as per clinical guidelines, and enables medications to adopt the position of second-line treatments as per recommended care.
References available on healthiersleepmag.com
Colin Espie, PhD, DSc is Co-Founder & Chief Scientist at Big Health and Professor of Sleep Medicine at the Nuffield Department of Clinical Neurosciences, University of Oxford
21 | healthiersleepmag.com
Dr. Colin Espie
Sleep Consortium
Founded in 2021, Sleep Consortium is a nonprofit organization created to accelerate next-generation research, disease understanding, and therapy development for those living with central disorders of hypersomnolence (CDoH) and other related sleep disorders. These disorders of hypersomnolence include narcolepsy, idiopathic hypersomnia, and Kleine-Levin syndrome.

Cofounders Lindsay Jesteadt and Claire Crisp note that “Sleep Consortium was designed to serve at the intersection of the various roles that support the broader sleep ecosystem” (e.g., industry, researchers, patients, clinicians, patient organizations). Their goal is to accelerate knowledge development through effective patient-owned data collection, data connection, and community pooling of data, with a responsible and respectful structure to enable the entire network to thrive. Jesteadt expresses that “this type of precompetitive collaboration brings together multiple stakeholders to overcome a common barrier or develop a solution that allows them all to benefit, just as a rising tide lifts all boats.”
“The Sleep Consortium takes a bold new approach to sleep research putting the patient in the center of its efforts. This initiative demands that the patient be the driver of new research considerations, have ownership of their own data, and serve as an invaluable partner to researchers internationally."
sleep medicine by collecting, interconnecting, and federating data. Supported by leading researchers, industry partners, and patient advocacy groups, the patient data collection portal will launch in early 2023 and will allow patients and family members to assist in accelerating research by sharing their data. This patient-reported data will also live alongside other consented, robust data sets from registries and academic and clinical institutions globally. At present, patientreported outcomes measures are insufficient and detailed registry data is lacking. It will take a collaborative effort to create a sleep ecosystem that is abundant in meaningful data.
– Anne Marie Morse, Director of Child Neurology and Pediatric Sleep Medicine, Geisinger, Janet Weis Children’s Hospital
Patients will be able to share their consented data with global researchers, clinicians, and drug developers to advance research in CDoH and accelerate the development of new targeted therapies in this precompetitive space. The data collection portal will also serve to connect interested patients with qualifying clinical trials and studies to accelerate knowledge and future treatment options.
Partnering with RARE-X, a collaborative platform for global data sharing and analysis, Sleep Consortium is working to unburden patients while making the task of data collection easy and accessible for the sleep community. Through ethical data-sharing practices, leveraging artificial intelligence (AI) and machine learning, Sleep Consortium is reimagining data collection in
Jesteadt ends by adding, “We are empowering patient communities as the patient is indeed the expert when it comes to their symptoms and they should play an active role in identifying meaningful benefit…Perhaps, what is meaningful to the patients cannot be represented in numbers from current scales alone.”
For more information visit: sleepconsortium.org
22 | Winter 2022-23 | Artificial Intelligence Issue Patient Organization Highlight
The BuZZZ about Sleep
Your Latest Buzzword is Brain Age: A marker that quantifies brain health/aging from sleep
By Haoqi Sun, PhD
Some 60-year-old people are good at cognitively demanding tasks, while others suffer from poor memory and impaired cognition, problems that are uncommon until older ages. How can we quantify deviations from a normal brain-aging trajectory? One possibility is by measuring sleep.

Sleep patterns change with age and sleep tends to be shorter and lighter as people get older. The brain’s electrical activity during sleep also changes with age. For example, the height of “slow waves” during deep sleep – electrical brain waves that repeat fewer than four times per second – decreases more and more the older we get. This and many other changes in brain waves can be summarized into an age-like number: sleep-based “brain age.”
If a 60-year-old person has a brain age of 70, their sleeping brain waves resemble those of a 70-year-old person who is aging normally. This may be cause for concern in a 60-year-old person. Conversely, an older person may have a younger-looking sleeping brain, which is probably a good thing. The difference between brain age and actual age is correlated with multiple conditions including dementia, hypertension, diabetes, and HIV infection, as well as life expectancy. A marker like brain age can help sleep doctors get an objective and repeatable sense of brain health from sleep. Eventually, brain age may become a key piece of information to guide treatments to preserve and improve brain health.
Scientific Perspectives
Artificial Intelligence Applications in Sleep Medicine
By Robert Thomas, MD and Haoqi Sun, PhD
The measurement of sleep produces a large amount of data. Imagine – hours and hours of measurements from different parts of the sleeping brain and body. While complicated enough in health, there are so many changes at different ages, and of course, in sleep disorders. Some “rules” to help keep all this information under some order are required. Sleep medicine has largely used “rules-based” measurements from its inception – with specific criteria for different measurements such as brain wave and breathing. These rules are relatively rigid and –while convenient – tend to “lump” physiology, pathology, and indeed, individuals. Thus, two or more persons who are actually quite different may look similar. Though useful to convert large amounts of data into digestible bits, much of the information content is lost from this simplification.
Data in sleep medicine are intrinsically “big,” in terms of the large number of people suffering from sleep disorders, the multiple signal modalities collected during sleep through polysomnography (PSG), the possibility of nearly endless recordings from the same individual, and the rich information contained in PSGs. Therefore, sleep medicine is an important venue for data-driven approaches, especially artificial intelligence (AI), and AI has become an important technology in sleep medicine and vice
versa. In the AI approach, various computational methods and “architectures,” or types of connections in computers, which talk to each other in interconnected layers of information transfer and manipulation are able to establish and extract obvious and non-obvious patterns in data.
It would seem that sleep data are made for AI! AI can be applied to improve sleep in various modes. Here we summarize the applications into three levels: (1) improving the efficiency of existing sleep scoring, sleep disorder diagnosis, and treatment management; (2) new metrics of health biomarkers and interventions which are difficult to be implemented in a rule-based approach; and (3) predicting future incidence of outcomes for identifying people with high risk in advance.
To be fair to the rule-based approach, the initial training of AI sleep analytics systems often uses rules as the foundation (a supervised or semi-supervised approach), but AI can also be entirely unsupervised. When the AI system is unsupervised, the system is allowed to “see what is going on with its own eyes” without constraints. Nothing prevents a mutually beneficial interaction – where AI outputs could change rules which in turn could change the parameters of the AI analysis, and repeat. Applications continued on page 10
25 | healthiersleepmag.com
>
1) Improving Efficiency
The job of a sleep technologist who mostly scores sleep studies – a long tradition in sleep medicine – is surely at risk.
AI-assisted sleep scoring is becoming more commonly accepted. Instead of manually determining the sleep stages for more than 800 pages of sleep recording per night, sleep stages are automatically determined by an AI algorithm. The accuracy of AI-based sleep staging has reached the same level as the accuracy of human sleep scorers.
These algorithms also make the same types of errors humans do! After all, the training material is human.
In addition to the conventional sleep stages (hypnogram), the probability of being one of the five sleep stages can also be reported (hypnodensity graph) quantitatively reflecting the uncertainty in transitional stages. Transitions and fuzziness of rapid eye movement (REM) sleep or dream sleep, nonREM sleep, and wake states are common in disease states. Other important events including abnormal breathing, very brief (few seconds) awakenings from sleep movement of the legs, etc., are also automated. Automated sleep scoring improves the efficiency and reproducibility of a doctor’s diagnosis, such as sleep apnea (bad breathing during sleep), insomnia (taking too long to fall asleep, waking up too early, or waking up too many times), and narcolepsy (a condition causing extreme sleepiness in the daytime). Both single and multiple sources of information can be analyzed using AI, including data from wearable and non-touch devices, as these come into the medical mainstream.
2) New Metrics of Sleep
AI can be used to extract new information from sleep that cannot be explicitly expressed as rules. For example, sleep quality is a nonspecific term that could either mean the subjective feeling of refreshment when getting up, the objective percentage of deep sleep, or the association with cognition and unfavorable outcomes which is clinically more relevant. One example is sleep-based “brain age.” Many sleep patterns change with age; therefore, sleep patterns resemble sleep from a different age when the brain deviates from normal aging. In essence, if your sleep “looks” older than your calendar age, you are in trouble! AI is used to summarize the age-related changes in sleep into an age-like number. Older brain age has been associated with dementia and higher mortality. Another example is predicting cardiovascular diseases (CVD). AI is used to estimate the likelihood of CVD using oxygen and heart rate fluctuations during sleep. When it comes to sleep apnea, analysis at the borderland of rules and AI is used to classify four “endotypes,” or mechanisms of disease, of obstructive sleep apnea (OSA) using PSG, which then enables personalized OSA treatment plans. In brief, bad breathing during sleep can be caused by more than one problem. For instance, breathing may be “wobbly” because its control is not precise, or one might wake up too easily from small changes in breathing. Using a rules-based approach may not differentiate these types of bad breathing during sleep, and thus, treatments are not aimed properly at the cause. Thus, not just opening the airway, but also targeting breathing control or even sleep itself can enable “precision and personalized” sleep apnea care.
26 | Winter 2022-23 | Artificial Intelligence Issue
Applications continued from page 9
3) Predicting the Future
The most common sleep disorder, obstructive sleep apnea, can be effectively treated by using a continuous positive airway pressure (CPAP) mask. However, only 50% of patients are still using theirs after 12 months. One important AI application is to predict who will, or will not, give up. Sleep also contains information about future risk of unfavorable outcomes such as death, abnormal brain development including autism, and dementia (like Alzheimer’s disease, with loss of memory), which can be extracted using AI. These methods are still in development. In fact, sleep can be considered a window into the health of numerous biological systems, including the brain, heart, and lungs. Sleep also is a general marker of health, in that sleep becomes light and fragmented when one is sick – cancer, infection, and so on. Sleep then can be used as a way to track overall health, not just as a state with its own disorders which need treatment.
Future of AI in Sleep Medicine
The important limitations, and hence important future work for AI in sleep medicine, include its inability to interpret the results for some AI methods (the machines never say “I do not know!”), the lack of confidence measures (“how correct is the machine?”), biases in accuracy (performing better in some instances than others, but in an unpredictable way) due to lack of heterogeneity in the dataset (the data used for training is not representative of the data the machine is asked to analyze), and lack of standard certifications for validating AI algorithms for clinical use (most researchers create their own methods and think their method is the best!). If nothing else, the prospect of financial savings will drive integration of AI into sleep medicine practice but blind acceptance without healthy skepticism is foolish

Robert J. Thomas, MD is a Professor of Medicine at Harvard Medical School, Division of Pulmonary, Critical Care & Sleep Medicine, Department of Medicine, Beth Israel Deaconess Medical Center. He has been working in the field of sleep medicine and research for nearly 30 years.
Haoqi Sun, PhD is an Instructor of Neurology at Harvard Medical School and Department of Neurology, Beth Israel Deaconess Medical Center. He comes with a background of Artificial Intelligence (AI) and has been working to bring AI into sleep research for 5 years.
References
Bandyopadhyay, A. and Goldstein, C., 2022. Clinical applications of artificial intelligence in sleep medicine: a sleep clinician’s perspective. Sleep and Breathing, pp.1-17.
Stephansen, J.B., Olesen, A.N., Olsen, M., Ambati, A., Leary, E.B., Moore, H.E., Carrillo, O., Lin, L., Han, F., Yan, H. and Sun, Y.L., 2018. Neural network analysis of sleep stages enables efficient diagnosis of narcolepsy. Nature communications, 9(1), pp.1-15.
Sun, H., Paixao, L., Oliva, J.T., Goparaju, B., Carvalho, D.Z., van Leeuwen, K.G., Akeju, O., Thomas, R.J., Cash, S.S., Bianchi, M.T. and Westover, M.B., 2019. Brain age from the electroencephalogram of sleep. Neurobiology of aging, 74, pp.112-120.
Ye, E., Sun, H., Leone, M.J., Paixao, L., Thomas, R.J., Lam, A.D. and Westover, M.B., 2020. Association of sleep electroencephalography-based brain age index with dementia. JAMA network open, 3(9), pp.e2017357-e2017357.
Blanchard, M., Feuilloy, M., Gervès-Pinquié, C., Trzepizur, W., Meslier, N., Goupil, F., Pigeanne, T., Racineux, J.L., Balusson, F., Oger, E. and Gagnadoux, F., 2021. Cardiovascular risk and mortality prediction in patients suspected of sleep apnea: a model based on an artificial intelligence system. Physiological Measurement, 42(10), p.105010
Eguchi, K., Yabuuchi, T., Nambu, M., Takeyama, H., Azuma, S., Chin, K. and Kuroda, T., 2022. Investigation on factors related to poor CPAP adherence using machine learning: a pilot study. Scientific Reports, 12(1), pp.1-9.
27 | healthiersleepmag.com
..............................................................................................
Dr. Robert J. Thomas
Dr. Haoqi Sun


28 | Winter 2022-23 | Artificial Intelligence Issue WSO.fullpage.11-20 1 23/11/2020 11:23
Ask the Sleep Experts

As answered by our issue reviewers
Question: Can light therapy help me sleep better? How does it work?
Dr. Ramagopal: Light therapy can help if you have a circadian rhythm disorder, insomnia, seasonal affective disorder, or depression. Exposure to bright light suppresses the production of melatonin, the hormone that induces sleep. It helps to realign the body clock with that of the sun, so you are alert during the day and tired towards the evening.


There are different tools to deliver light therapy, including light therapy glasses and light boxes. A light box should have an intensity of about 10,000 lux to be effective. The light is full spectrum or only blue light. Ideally it should be placed 18-24 inches away; exposure for 15-30 minutes is sufficient. Lower intensity lights will need a longer exposure to be effective. Although light therapy is a safe treatment, there can be mild side effects like headache and irritability which will likely decrease with time.
Ask
experts continued on page 30 >
29 | healthiersleepmag.com
Maya Ramagopal, MD
Melissa C. Lipford, MD
Robert J. Thomas, MD
the
Dr. Thomas:
Light therapy likely would not help an average sleeper under average common sense lighting conditions such as turning down the lights around 8:00pm, turning lights on around 6:00am, and keeping it dark while sleeping. Therapeutic light can be used for bothersome delay (morning light) or advance (evening light) of internal circadian rhythms.
Dr. Lipford:
Bright light therapy can be used to manage circadian rhythm sleep disorders. These are disorders in which people have a sleeping pattern that falls outside of what is considered the social norm. A sleep specialist will carefully work with the person to decide on the optimal timing and duration of light exposure depending on the symptoms. Light therapy can help shift a person’s “internal clock” and facilitate sleeping during a more acceptable timeframe. Light therapy can also be used for other sleep and mood disorders. It is important to work with your medical provider to ensure it is right for you and is delivered in the right way.
Is it okay to use an e-reader before bed?

Dr. Ramagopal:
Reading using an e-reader or a tablet before bed is a popular way to "wind down." E-readers use e-ink screens, which emit less blue light than tablets, but they still use blue light spectrum for back lighting. Newer versions of
e-readers have better blue light filters but it is not completely absent. Exposure to blue light can prolong sleep onset, interrupt melatonin secretion, and disrupt the circadian rhythm. Some e-readers have night mode and dark mode features, which block blue light. This has a positive effect on the circadian rhythm and decreases eye strain.
Dr. Thomas:
With the light intensity at the lowest level, it is probably okay. A light meter phone app can be used to measure the lighting level; the light at the eye should be less than 10 lux. Reading cognitively engaging or disturbing material may be unwise.
Dr. Lipford:
The honest answer is maybe. For some, reading before bed is a relaxing activity which helps disengage the mind and leads to falling asleep more quickly. For others, reading is a stimulating activity and may make falling asleep more difficult. If you like to read in bed, consider choosing content that is interesting, but you can still put the book or device down when it is time to go to sleep. An exciting murder mystery
may not be the best choice before bed!
E-readers and other electronic devices have the added stimulating effect of light, which can make it harder to fall asleep. Many of the newer devices have settings which reduce blue light and have adjustable backlighting which can help.
30 | Winter 2022-23 | Artificial Intelligence Issue
Ask the experts continued from page 29
Exposure to blue light can prolong sleep onset, interrupt melatonin secretion, and disrupt the circadian rhythm.
How can I tell if I’m sleeping well?
Dr. Ramagopal:
The following are qualities of good sleep: the ability to fall asleep within 30 minutes of lying in bed, waking up not more than once during the night, and getting the age-appropriate amount of sleep. In adults, the recommended nightly amount of sleep is at least 7 hours. School-aged children should get at least 9-12 hours per 24 hours and teens 8-10 hours per 24 hours. Additionally, you should feel refreshed upon waking up and not be sleepy during the day. The need for a nap during the day could indicate that there is a problem with nighttime sleep.
Dr. Thomas:
Some clues that all is not well in the land of sleep include waking up very tired, being unable to stay awake in quiet daytime conditions, taking more than 15-20 minutes to fall asleep, waking up more than 2-3 brief times or for more than 30 minutes at night, waking up gasping for breath, having trouble waking up in the morning (multiple snooze button hits), having bedsheets that look like a war zone, or having a partner who is alarmed at your sleep behaviors or breathing patterns.
Dr. Lipford:
Most individuals need 7-9 hours of sleep nightly. If you are obtaining sufficient sleep on a regular schedule, you wake up feeling rested and refreshed, and you have good energy levels during the day, you are likely sleeping well.
My sleep tracking app says I’m not getting enough deep sleep. How do I improve it?
Dr. Ramagopal:
In addition to sleep hygiene recommendations, tips to improve deep sleep start with changes to the daytime routine. Moderate aerobic exercise, even for 30 minutes a day, can improve sleep quality. Exposure to sunlight helps reset the body’s circadian clock and promotes better sleep. Strenuous exercise within 1-2 hours of desired bedtime is not recommended because it can prolong the time to fall asleep. Eating a heavy meal too close to bedtime can also prolong sleep onset and sleep quality. Avoiding caffeine after 3pm is generally advised. The effect of alcohol on sleep depends on individual factors like age, gender, and body type; less than one glass of wine in women and less than two glasses of wine in men can decrease sleep quality.
Dr. Thomas:
The estimation of deep versus light sleep through consumer apps is not particularly reliable in people who need it the most: those with abnormal sleep. Trying to get to a "number" is not wise, outside of average sleep behaviors. For example, reducing your time in bed will likely increase "deep" sleep but that might cause you to be sleep-deprived. Apps are best for those who generally sleep well but put their sleep under stressors of various types; longitudinal tracking is probably the best use. Apps are useful in the sleep clinic, where the doctor knows what part of the output to use and how.
a question for the sleep experts? Submit your questions by email to healthiersleep@worldsleepsociety.org .
Have
Questions are selected based on space and applicability.
31 | healthiersleepmag.com





Healthier Sleep Magazine 3270 19th Street NW, Suite 109 Rochester, MN 55901 USA Healthier Sleep is a public awareness magazine that acts as a trusted source for information regarding sleep health, disorders, and research. Published four times per year, Healthier Sleep highlights a different topic in sleep with each issue. Issue Topics • Sleep Apnea • Healthy Sleep • Sleep Disorders • Insomnia • Daytime Sleepiness • Restless Legs Syndrome (RLS) • Artificial Intelligence Your Trusted Source for Improving Sleep In Every Issue Clinician as Advocate Bedtime Reads The BuZZZ About Sleep Ask the Sleep Experts Right Now in Sleep Science healthiersleepmag.com May/June2021|SleepDisordersIssue healthiersleepmag.com July/August 2021 | Insomnia Issue healthiersleepmag.com Winter 2022-23 Artificial Intelligence Issue Introduction to Artificial Intelligence Sleep Tracking Devices New Feature: Clinician as Advocate Five Questions with Dr. Azizi Seixas Better Sleep for All: Expanding Acccess to Sleep Health for Underserved and Diverse Populations For more information, visit healthiersleepmag.com For questions, contact healthiersleep@worldsleepsociety.org Subscribe to Healthier Sleep Today! Scan the code to subscribe to Healthier Sleep















 by Antonio Zadra and Robert Stickgold
by Antonio Zadra and Robert Stickgold