RISK FACTORS & MANAGEMENT STRATEGIES FOR SEATING

ALSO INSIDE

TOOL-LESS ADJUSTMENT


ANATOMICAL PIVOT POINT
MAINTAINS SECONDARY POSITIONING


SCAN


RISK FACTORS & MANAGEMENT STRATEGIES FOR SEATING

ALSO INSIDE

TOOL-LESS ADJUSTMENT


ANATOMICAL PIVOT POINT
MAINTAINS SECONDARY POSITIONING


SCAN

In September, the industry marked the third anniversary of asking the Centers for Medicare & Medicaid Services (CMS) to fund power standing for Medicare beneficiaries.
And while justifiably celebrating the agency’s decision to fund power seat elevation — a huge win, no question — we cannot forget that power standing still has no timeline, three years after the ITEM Coalition formally requested a reconsideration of the existing National Coverage Determination.
Thus the fact that power standing reconsideration was the first of our three “asks” during the Sept. 13 CRT (Complex Rehab Technology) Virtual Fly-In, hosted by NCART and NRRTS.

Between you and me, I’m a bit puzzled by the lag on power standing. I’m not a clinician, but to me it seems that the “medically necessary” argument for standing is even more of a slam dunk than it was for seat elevation. From range of motion to respiration, from digestion to bowel and bladder management, from bone density and weight bearing to pressure relief and improved reach with less strain on the neck and shoulders, standing would seem to be the gold standard for repositioning.
I know it’s contraindicated for some wheelchair riders, but that’s true of any seating intervention, right? For what seems to be the majority of wheelchair riders, a standing assessment seems wise. And Medicare funding for power standing is long overdue.
Whenever I think about power standing, I recall queuing one Saturday at my local bank. In front of me were a dad and his teenage son; the kid was in a power chair. A family friend of theirs happened to walk in, and as adults do, she marveled over how the boy had grown. His dad volunteered that the night before, his son had gone to his first school dance. He’d moved into standing mode and asked a girl to dance. She said yes, and off they went. Dad showed photos.
The family friend squealed. The kid hissed, “Dad! Dad, stop it!” I tried to pretend I wasn’t listening.
Asking a classmate to dance isn’t a mobility-related activity of daily living by Medicare standards. But I can almost guarantee that dancing with the girl he liked got that kid’s heart racing. Surely, therapists would argue the benefits of social and emotional growth, as well.

Standing is seating, CMS, and standing is life. Please open the reconsideration process so we can tell you all about it. m
September/October 2023
mobilitymgmt.com
CO-FOUNDER & CEO, WTWH MEDIA Scott McCafferty
EDITORIAL EVP OF HEALTHCARE George Yedinak

MANAGING EDITORS Bob Holly Tim Mullaney
EDITOR Laurie Watanabe lwatanabe@wtwhmedia.com
ART VP, CREATIVE DIRECTOR Matt Claney mclaney@wtwhmedia.com


SALES VP OF SALES Sean Donohue
Mobility Management (ISSN 1558-6731) is published 5 times a year, March/April, May/ June, July/August, September/ October, and November/December, by WTWH Media, LLC., 1111 Superior Avenue, 26th Floor, Cleveland, OH 44114.

© Copyright 2023 by WTWH Media, LLC. All rights reserved. Reproductions in whole or part prohibited except by written permission. Mail requests to “Permissions Editor,” c/o Mobility Management, 1111 Superior Avenue, 26th Floor, Cleveland, OH 44114.
The information in this magazine has not undergone any formal testing by WTWH Media, LLC, and is distributed without any warranty expressed or implied. Implementation or use of any information contained herein is the reader’s sole responsibility. While the information has been reviewed for accuracy, there is no guarantee that the same or similar results may be achieved in all environments. Technical inaccuracies may result from printing errors and/or new developments in the industry.
Corporate Headquarters: WTWH Media, LLC 1111 Superior Avenue, 26th Floor Cleveland, OH 44114 https://marketing.wtwhmedia.com/





Media Kits: Direct requests to George Yedinak, 312-248-1716 (phone), gyedinak@wtwhmedia.com.
Reprints: For more information, please contact Laurie Watanabe, lwatanabe@wtwhmedia.com.
Laurie Watanabe, Editor lwatanabe@wtwhmedia.com @CRTeditorComplex Seating. Simplified.
www.symmetric-designs.com
Fit a custom molded back in one appointment
Single tool adjustment
Completely ventilated custom seating
HCPCS Coded E2617 and E2609
Demos available
StimuLITE ®
Beat the heat with for fully ventilated custom seating!
Back Kits available with a full range of sizes, shapes, padding/covers and mounting options.

Pressure wounds. Friction. Shear. These are three common words in the seating and mobility world that are a persistent threat plaguing the wheelchair community.
Pressure is defined as the continuous physical force exerted on or against an object by something in contact with it.
Friction is the resistance that one surface or object encounters when moving over another.
And shear is the strain in the structure of a substance produced by pressure when its layers laterally shift in relation to each other.
When a client is referred to a seating clinic due to a wound issue, our first instinct is to look at the cushion. While much of the time the cushion does play a significant role, there are other not-so-obvious sources of pressure injuries that may be contributing to skin breakdown. There are also numerous risk factors that contribute to the risk for compromised skin integrity.
Over a three-part series, we’ll discuss these risk factors, including the seat cushion and other identified factors, to highlight some of the areas that can be addressed to minimize wheelchair clients’ risk of potential skin breakdown and/or prolonged wound healing time.
Factors that increase risk for compromised skin run the gamut over multiple body systems.
For clients using a wheelchair, “a number of contributing or compounding factors are associated with pressure injuries; the primary of which is impaired mobility.”1

• Bony prominences — most notably the ischial tuberosities, but this group can also include the sacrum, coccyx, greater trochanters, and lateral malleoli — are at greater risk of breakdown, as less tissue is present between the bone and the skin.
• A client who is underweight is more likely to be very bony, with malnutrition also slowing the healing process.
• Another risk factor is impaired muscle tone . Friction and shear forces can occur with increased tone and spasticity. On the contrary, the lower muscle mass associated with low muscle tone increases pressure injury risk, particularly over bony prominences.
The same can occur in people with muscle atrophy secondary to spinal cord injury or degenerative conditions such as amyotrophic lateral sclerosis (ALS).

•
Individuals who cannot effectively communicate their needs due to impaired cognition or communication are at higher risk for skin breakdown.
• Sensory deficits are a risk factor, for someone who cannot feel discomfort or numbness will not move in response. The client also may not be able to feel a wound, and if skin checks are not done consistently, a wound may develop prior to discovery.
• During the aging process, skin naturally becomes thinner and loses elasticity. The reduced vascularization associated with aging is another risk for prolonged healing and skin breakdown.
• Skin may be compromised when sitting is prolonged and static , and when weight shifts are not performed. Individuals who cannot perform weight shifts independently must rely on a competent caregiver to do so or face a greatly increased risk of pressure injury. The ability to continuously move in one’s wheelchair is an essential part of preventing skin breakdown.
Now that we’ve established a better understanding of when and why compromised skin risk factors are present, let’s take a deeper dive into the more specific culprits of skin breakdown.
The wheelchair seat cushion probably seems like the most obvious reason for seated surface pressure, and it’s the one cause that clients and clinicians gravitate towards most often.

While the seat cushion can frequently be an issue, it may not be the only issue; other factors may also be contributing. Cushions, particularly ones with a foam base, can have a limited lifespan. There is no actual time frame of how long a cushion should last; however, some factors may predict a quicker degradation, including moisture, extreme temperatures — both high and low — and even the number of daily transfers the wheelchair rider performs. Depending on how “bony” one’s ischial tuberosities
are, depressions within the cushion may be accelerated.
All of these reasons can contribute to a rapid decline in the integrity of seat cushions, particularly those with foam bases. While the cushion aging process may not be preventable, if the
to unnecessary pressure and shear forces. During initial cushion inspection, clients coming in for a seating assessment, including pressure mapping, have been found to be sitting on the abductor, which is supposed to be in the front of the cushion.
cushion has been successful in terms of providing pressure relief, it may be better to caution a user to be on the lookout for breakdown in the foam and look to have it replaced if that breakdown is indicated. Cushions can be replaced every two to three years through insurance if this degradation occurs.
Incorrect cushion orientation has played a role in abnormal pressure mapping results and has contributed
How does this occur? Maybe the cushion was laundered by a caregiver and returned to the wheelchair incorrectly.
Many of our clients have sensory deficits or are unable to communicate their discomfort due to cognitive deficits. This could result in excess pressures and could cause increased shear, as they attempt to accommodate for the disoriented cushion. Often, the simple act of labeling the cushion and cushion cover — front and rear, top and bottom — can prevent this error from recurring in the future.
Friction and shear forces can occur with increased tone and spasticity. On the contrary, the lower muscle mass associated with low muscle tone increases pressure injury risk, particularly over bony prominences
The revolutionary ProGrip™ 6-wheel active suspension senses and responds to driving terrain keeping all six wheels on the ground. When decelerating quickly, the suspension automatically stiffens, ensuring outstanding stability. Over bumps and cracks, ProGrip softens, delivering maximum traction and a smooth riding experience.
Discover ultimate performance and comfort with the Q700® M and its cutting-edge ProGrip suspension. The best support for any terrain!

Many clients with pressure issues claim they were not provided with sitting restrictions while their wounds were healing. While there are no definitive parameters regarding sitting restrictions, protocols that occur within rehabilitation settings and gradually allow increased sitting time make sense and are quite effective.

Whether it be 30 minutes twice per day or two hours twice per day, it is important to emphasize the importance of consistent pressure relief to clients. This can be in the form of weight shifts or use of power positioning systems, if the client is in a power wheelchair.
Experience has shown that forward and lateral weight shifting can effectively reduce and even eliminate pressure on the coccyx and ischial tuberosities. Studies have shown that maintaining certain tilt and recline positions for two to three minutes and performing these actions every 20 to 30 minutes can be effective pressure relief. 2
If a client is using power seating functions, it is important to sequence those functions correctly — tilt, then elevating legrests, then recline. Then the sequence should be reversed when returning upright to be sure to avoid unnecessary forces.
Everyday life can interfere with these sitting restrictions when convalescing at home or trying to maintain a work/life balance. If this is the case, balancing between sitting and full pressure relief should be prioritized, and if possible, built into the client’s everyday schedule.
Jillian Cacopardo, MPT, ATP/SMS, is a Physical Therapist at Gaylord Specialty Healthcare. Read parts two and three of this series in upcoming Mobility Management issues.
1. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline, Published by European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance, 2019.
2. Jan, yih-Kuen, et al. “Effect of Durations of Wheelchair Tilt-in-Space and Recline on Skin Perfusion Over the Ischial Tuberosity in People with Spinal Cord Injury.” Archives of Physical Medicine and Rehabilitation 94.(2013): 667-672. m
Incorrect cushion orientation has played a role in abnormal pressure mapping results and has contributed to unnecessary pressure and shear forcesDAPPER GENTLEMAN: ISTOCKPHOTO.COM | YOURPHOTOSTOCK







Even those outside of healthcare are likely to have some knowledge of pressure injuries, which they might refer to as bedsores or pressure ulcers. Possibly they’ve had an older relative who was bedridden and developed a pressure injury on a heel or back of the head. That’s what happens when people in bed aren’t turned often enough, they might say.
But they’ll likely know less about shear, even if you provide the hint that shear can occur, for example, during wellintentioned efforts to reposition someone in bed
“It’s harder to conceptualize [than pressure is],” said Cole Carson, PE, Director of Business Development for Tamarack Habilitation Technologies. “It’s also harder to measure when you’ve got pressure mapping that helps to visualize these spots of high and low pressure. Shear has just been a lot trickier of a characteristic to measure.”
Ironically, while shear can be tough to visualize, it’s also pervasive in the seating world. “It can be at the surface, it can be deep tissue, it can be anywhere across that spectrum,”

Carson said. “Shear is a three-dimensional concept when you’re discussing human anatomy, and soft tissue, and whatnot. It’s not a 2D thing, like pressure is.”
“The most basic definition of shear,” Carson said, “is that it’s a strain in the structure of a substance produced by a pressure, when its layers are laterally shifted in relation to each other. In the context of Complex Rehab and soft tissue in the human body, shear stress is inextricably linked to pressure. One doesn’t happen without the other.”
One of the challenges in understanding shear is that while pressure can produce some visible effects — such as the non-blanchable redness of a stage 1 pressure injury, according to the National Pressure Injury Advisory Panel — the internal location of shear can produce fewer outwardly noticeable signs.
In a classic example of pressure, Carson noted, “ You talk about sitting still for long periods of time without moving, or
Discover the ultimate mobility experience with Dynarex. From wheelchairs to walkers, canes to crutches, our products are built to enhance your independence and improve your quality of life. Built for performance and designed to make life easier, Dynarex mobility equipment features quality craftmanship, ergonomic design, and meticulous attention to detail.
Take your mobility to the next level. Upgrade to Dynarex premium mobility equipment today!

 LEARN MORE!
LEARN MORE!
without lifting up and redistributing your weight.” But pressure isn’t the only force at work. Carson said, “There is shear still occurring within your soft tissue as your bony prominences are pressing down upon those parts of your body. It’s just not as a result of sliding or moving from side to side for long periods of time without moving, or without lifting up and redistributing your weight.”
Therein lies the challenge of managing shear. Even when someone sits still, pressure is present. When that person moves, even just slightly to weight shift, “You’re creating more shear,” Carson said. “You already have some that is acting upon the soft tissue immediately around the bones that are distributing your weight. When you move, you cause more.”
So, shear occurs because of pressure?
“Yes, exactly,” Carson said. “Pressure is present. In fact, you could say pressure is present non-uniformly.”
Remember learning in school about tectonic plates? Carson said, “In an earthquake, you’ve got a static shear, where two surfaces are trying to slide against or across each other. They’re not [doing that] until the pressure is so great that it overcomes that static shear, that friction. Then you’ve got that lurch of material that creates an earthquake, until the friction stops it again.”
And that all happens because pressure was present.
While pressure is ubiquitous and often thought of as the enemy, it can actually be harnessed to, for example, keep us stably positioned while seated. The case is similar for shear, Carson said. “You can have safe levels and unsafe levels of shear. What we are trying to do when we try to manage shear in seating or other instances is to keep it below that damaging threshold.”
Carson noted as well that there are different types of shear. “At Tamarack, I’d say we separate shear into three different types of events or loading events,” he said. “We identify them as quasi-static, high impact, and repetitive.
“High-impact shear would be the situation that occurs during transfers, or when there’s a reclining back [on a wheelchair] or in the reclining bed. These are exceptionally high levels of shear stress that immediately fracture the skin and soft tissue and usually occurs at the surface level. There’s a reason that’s the first thing that people think of or is most quickly associated with shear or shear injuries.”

The next most relevant and very important type, Carson said, “is quasistatic. That’s where the skin is left in a distorted position for extended periods of time without relief when you’re sitting, when you’ve transferred into your chair or bed, and you haven’t lifted up to let your skin go back into its natural position around your skeleton. What’s happening there is that the shear forces are slowly cutting off blood flow to the capillaries. That, in turn, is slowly killing the cells.
“This is the type of shear that leads to the pressure injuries or decubitus ulcers in wheelchair users and patients in beds.”
Ever recall plunking into your airline seat quickly to get out of the way of other passengers behind you? Then, maybe without even thinking about it, you likely repositioned yourself in that seat to get more comfortable.
But many wheelchair riders lack the ability to feel that uncomfortable sensation and therefore quickly reposition
themselves to prevent the damage that prolonged shear and pressure can cause.
“There is this built-in default for people with sensation to periodically reposition themselves sitting, or standing, or how they walk, so that they are keeping that shear from reaching a damaging level or duration,” Carson said, adding that shear can happen as the result of even the slightest, seemingly innocuous actions. “That type of skin distortion can happen even when you’re leaning over in your chair and don’t reposition after that.
“It’s not just when you’re in a reclined position, although that’s definitely kind of a worst-case place for that to happen. Really, anytime your skeleton and bony prominences are shifting relative to your skin, and your skin and soft tissue are unable to just naturally follow that change in direction or movement, is when you start getting the buildup of shear forces that are damaging.”
Finally, the third kind of shear is repetitive shear, Carson said: “That’s when the skin is repeatedly exposed to smaller shear forces in relatively quick frequency, such as when running, shoveling, or in sports activities, and that causes blisters.
“Left untreated, the blisters will eventually progress into ulcers, and can eventually reach deep tissue if they’re untreated for long enough. Again, you

go back to that sensation point: Most of us have this built-in warning system in our skin that tells us, ‘Hey, this is painful. You’ve got to stop moving this way. You’ve got to stop walking or shoveling. You’ve got to either change how you do those things, or stop altogether.’”
Even very active and fit wheelchair riders, he added, can be at risk for shear injuries. Wheelchair athletes, for example “are just being really aggressive in their movements. Also, with sports you tend to sweat, and sweating impacts the durability of your skin. It’s easier to break down your skin in the presence of moisture. With wheelchair athletes, their bodies take an absolute pummeling during their seasons. Oftentimes, they spend their off season healing, they get ready for the next season. They just push themselves so hard and play through injuries.
Repetitive shear is a common concern for people with diabetes, Carson added: “They lose sensation in their feet, and they walk around and do activities. They can’t feel that they’re having that rubbing, and after a day of walking at the fair, or doing something fun with their grandkids, they take off their shoes, and they see a super-bloody sock. That’s because they didn’t have the sensation to tell them that they were rubbing their skin in a way that it couldn’t handle.”
A major risk factor for shear injuries is the inability for wheelchair riders to discern when they’re in danger of being injured or have already been injured. That can be the case for people with impaired sensation, and for people unable to understand that they’ve been injured or unable to communicate that fact to caregivers who could help.
But there are other risk factors as well, such as when skin changes as part of the normal aging process.
“I’d say there’s three factors that fit in that category,” Carson said. “One would be just the age of the skin, losing its elasticity as we age. The second would be the amount of soft tissue that’s in between the bony prominence in the skin. When you have more soft tissue, it can handle greater amounts of displacement, I guess you could say, of the bone relative to the skin surface before damage is occurring.
“Then the third instance would be scar tissue, once a wound has happened and you have scar tissue.”
Scar tissue has different properties than healthy skin. As David T. Corr and David A. Hart wrote in their 2013 research Biomechanics of Scar Tissue and Uninjured Skin, “Compared with uninjured skin, scar tissue demonstrates similar high-load stiffness, greatly reduced resistance to failure, reduced low-load compliance, and altered material directionality.” Basically, scar tissue is starting at a deficit compared to normal skin.
“That’s why there’s such prevalence of wound recurrence for people after they already have a pressure injury,” Carson said. Not the only reason, but it’s a primary reason. Once a pressure injury has happened, you are immediately at much greater risk to have recurrence because of the scar tissue, and perhaps even adhesion of scar tissue to the bone.”
“I would just say that shear is present basically all the time, and so much more than people realize. With the loss of sensation, the inability to have the warning system telling you to reposition or stop what you’re doing, or to do it differently, that puts [the wheelchair user] in immediate risk for just letting damaging levels of shear develop.”
Therefore, shear, like pressure, must be managed.
“We at Tamarack like to use the term strategic friction management or strategic shear management, where you’re offloading shear in the same analogous concept of offloading pressure to other parts of the body that can handle it,” Carson said. “You still need friction and shear to keep yourself positioned and have postural control. If you had an entire seat surface made of something that’s slippery, and you slid, you’d slip all over the place, slide out of your chair, fall off the side.
“It still is important to have [friction/shear]. It’s just got to be distributed and offloaded in the way that pressure is distributed to different parts of the body that can handle it, and keep it within safe ranges.”
He referenced two Tamarack products that create lowerfriction surfaces to manage shear: “The one that’s most relevant to Complex Rehab is GlideWear. It’s a two-layer material that creates a really low-friction surface that can be sewn into any areas that are at risk for someone that needs to wear it, whether it’s a wheelchair user or someone that’s confined to a bed.
“We sew it into different sections of wheelchair cushion covers, primarily under the ITs [ischial tuberosities], the back two thirds of a seat cushion, leaving the front third or half to be a regular highfriction material that helps to provide the positioning, stability, and postural control to stay in the seat. We sew it into socks, into underwear, but we don’t make socks or underwear or cushion covers completely out of it, just in areas that are at risk.”
As for what we still misunderstand about shear, Carson said, “The greatest misunderstanding from my perspective is that people keep saying we need to know or learn more about shear before implementing solutions. Tamarack believes Complex Rehab already knows more than enough to begin strategically managing and lowering friction and shear in at-risk areas, and that we as a community can’t justify not doing anything. It’s such an epidemic. Waiting to conduct more clinical studies and learn more — it’s valuable, but we can start implementing solutions based on what research and science say about it already.” m
Shear is basically present all the time, and so much more than people realize
ROHO cushions are one of the most trusted names in complex rehab and this year we’re golden! That’s right. ROHO’s air-filled cushions have been providing protection, positioning, stability, and peace of mind for 50 years!


Our team is dedicated to the research, engineering, and manufacturing of these clinically tested cushions, and over a million ROHO cushions are used worldwide each day.
As we celebrate this big milestone, we want to thank our employees, clinicians, providers, and end users for their ongoing support and trust. You’ve helped us become the world leader in skin protection and positioning products.

Complex Rehab Technology (CRT) is medically necessary; the seating team must provide medical justification with the insurance claim being filed. But should seating do more than meet immediate needs?

Jennifer Gray, MOT, OTR/L, Territory Sales Manager, Permobil, believes so. “I do think it’s so huge to not only think about today and tomorrow, but where is this client going to be a year from now?” she said. “And making sure that we’re taking all of that into account. Pressure injury prevention is a huge part of that. The decision to choose manual or power [mobility] sometimes comes into play with pressure injuries, prevention, and things like that. So I think it should be at the forefront of decision making when it comes to seating clinic, as far as prevention of things such as skin breakdown.”
Given documentation requirements — not to mention the time crunches of seating clinic — how can seating teams balance
what’s justifiable today with what could be needed tomorrow?
“I will say it’s a challenge,” Gray acknowledged. “And of course, that client’s function and independence are huge factors as well. Being a clinician, you get this idea of anatomically what someone should sit or look like. What is proper posture? What is upright posture? How should that look?
“Over time, you realize what is normal. But there is a standard, an anatomical position that the body should be in. And I think it’s a challenge when you have the seating and positioning and complex needs that some of these clients have. You’re trying to balance. You’re thinking, ‘I want you to be upright.’ However, if I’m going to limit your function or your independence trying to put you in this position, then we need to figure out goals.”
That means the goals of multiple people. “What are your desires?” Gray said she asked clients. “What are your caregiver’s desires?”
And while that’s a lot to discuss and process, Gray added, “All those things have to factor in. In thinking of the future, these
Numotion is committed to improving the lives of people with disabilities by enabling them to actively participate in everyday life. Our team receives the tools and resources needed to be successful, including support, flexibility and continuing education.



Open positions include:
• Assistive Technology Professionals (ATPs)
• Service Technicians
• Seating Technicians
• Specialty Account Managers
• Customer Care Coordinators
are conversations that need to be had early on. Be honest about it, and make the client and the family or caregivers aware of what the potential is: ‘If we don’t stop [a seating issue] now, if we don’t provide you some support to eliminate the potential for this to get worse, we are going to be in a worse state.’ Sometimes you have the client on board, sometimes you don’t, if you’re potentially suggesting something that might be out of their realm or something different than what they have been doing.”
Discussing the future can be difficult, Gray admitted: “It can be a challenging conversation, especially if someone has a progressive disease. They don’t want to know how bad it’s going to get. But you do need to broach these things, like with ALS [amyotrophic lateral sclerosis], for instance. You know that they’re going to need more assistance down the road, whether it’s in drive controls or postural support. Providing a seating system that has the capability to work with them and progress with them and support them as they need throughout the time that they have is really important.
“I think it’s about having open conversations about that and using your judgment,” she said. “It’s knowing your client and
presenting it in a way that works for them as best you can. It needs to be discussed because these seating systems are so important for their ability to be functional and independent and be able to tolerate being up in the chair. But it’s also to prevent future challenges and issues as best as possible.”
Some of these conversations happen over time, as clients return to clinic; in other cases, Gray said, clients are discharged from in-patient rehab, and another therapist will take over.
“It’s doing what you can with the time that you have, and then some of this will happen over time, because it is a challenge,” she said. “No one wants to hear that they’re going to get worse when they’re already dealing with something that can be very tragic or traumatic or depressing. No one wants to hear that it’s getting worse. But being an OT, I think I was presenting it in a way so that function was at the forefront all the time.
“I want to continuously provide you with equipment that can help you be as independent as possible, with whatever function you have. That’s where my focus is. If you get better, wonderful. I would absolutely love that. But if you don’t, I want you to have what you need to be functional. As functional as possible.” m

Mobility Management: You’re a clinician who also works for a manufacturer. How do researchers’ pressure injury findings potentially impact your work — your product recommendations, or product development and design, for example?
Jessica Presperin, OTD, MBA, ATP/SMS: Researchers’ pressure injury findings are extremely valuable in product development, design, and clinical recommendations. The research and clinical findings have demonstrated how various techniques such as immersion, envelopment, off-loading, anti-shear, and three points of control assist in relieving pressure and promoting desired postures. For instance, the RESNA position paper on the application of tilt, recline, and elevating legrests provides evidence in their statements on how various seat functions work. We used those findings pertaining to the optimal angles of tilt and recline for pressure relief when developing tilt and recline power and manual wheelchairs to ensure we meet those criteria. The shapes of some of our cushions, combined with JAY fluid, air, or foam, are specifically designed to provide pressure distribution and postural support based on research findings.
MM: Pressure injury research focuses on prevention, on how to prevent future injuries. When you’re seating a complex client, do you think of products that not only are appropriate today, but could also prevent or slow progression of, for example, an asymmetrical posture?
JP: We do have evidence from Europe that demonstrates that if a child with cerebral palsy is provided with 24-hour postural support starting at a young age, there is significantly less bony deformity as they age. A seating system, promoting a neutral pelvis and spine; a standing device, advocating for alignment at the hip; and a sleep product, preventing asymmetrical posturing are highly recommended to decrease the potential for scoliosis, hip dislocation, and other postural deformities. When Leckey designed the Squiggles+ Stander, abduction up to 60° was added in response to evidence from Pountney, which demonstrated that abduction of the hips in standing for children 0-5 can assist in the development of the femoral head and the acetabular joint.
MM: While Complex Rehab Technology (CRT) is medically necessary by definition, should we also think of it as preventive?
JP: Absolutely. Part of the evaluation looks at sensation, postural control, postural tendencies, and tonal influence on the body. These findings, as well as the diagnosis, especially if it is progressive, will determine the cushion and back support recommendations. If an individual has a spinal cord injury, our recommendations will include providing a supportive back to promote stability of the spinal curves and a seat cushion that will distribute pressure and stabilize the pelvis. The immediate goal is to promote functional posture. The future goal is to prevent pressure sores or posterior pelvic tilt and kyphosis. m

Amylior’s mid-wheel-drive M3 and pediatric P3 power chairs are available in a narrower base configuration. The N2221 boasts a base width of 21" with GP22 batteries (2 3/8" narrower than standard size), either with full-size 14" or 12.5" drive wheels and 6" front casters. With a 300-lb. weight capacity, this configuration supports Amylior’s full line of power positioning: 50° of tilt, 160° of recline, ALTA Power Seat Elevation, and independent elevating legrests or a power articulating center mount foot platform. This narrow option has patented dual-action suspension to provide stability, performance on uneven terrain, and comfort.



Amylior
(888) 453-0311
amylior.com
The Dynamic Arm Support’s three points of contact limit shoulder pain and subluxation by providing properly positioned support at the elbow, forearm, and hand, allowing for a return of upper-extremity function. The arm support can be mounted on a height-adjustable armrest to ensure proper support. The innovative hand block allows fingers to flex while encouraging the hand to return to a neutral position once muscle tension releases. The pivot plate allows independent range-of-motion (ROM) exercises and ROM in the shoulder for ADLs such as dressing and hygiene. A quick-release tab allows for easy transfers with caregiver assistance.

Bodypoint
(800) 547-5716
bodypoint.com
The Dynarex Bari+Max Wheelchair with Elevating Legrests provides reliable support and improved mobility for larger users. The heavy-duty steel frame with dual cross brace for extra support allows patients to feel secure and stable. The wheelchair is equipped with tool-free adjustable elevating legrests with padded calf pads, detachable arms with padded armrests, and black, padded, double-embossed vinyl upholstery. The Bari+Max wheelchair is available in sizes 22x18" and 24x18", with a 500-lb. weight capacity.
Dynarex (888) 396-2739
www.dynarex.com
Building upon the industry-leading innovation and features of the Zing multi-position stander, the new Zing Portable stander is a leap forward in product design. This new early-intervention stander is the first “right-sized” product for standing children as young as possible (fits children from infancy to 36" and up to 36 pounds). Typically developing children will usually begin the processes of learning to stand between 9 and 13 months. Pivot points are in line with the hips, promoting proper alignment in the hips, knees, and feet. Abduction can be adjusted and used throughout the entire positioning range.
EasyStand
(800) 342-8968
zingstanders.com
The PC Proform Head Support with singlelatch EZ-Clamp Bracket has a screw-less design requiring minimal dexterity and is easily adjustable. It’s a perfect complement to Avid power wheelchairs. The PC ProForm Head Support features a 6" hardware stem; a full range of adjustability without removing the cover; two removable hardware options (midline or multi-axis); a stainless-steel gear system for secure positioning; a multi-layer foam headrest pad for comfort and support; and an EZ-Clamp Bracket, single-latch system for quick release.


Merits Health Products
(239) 772-0579
meritsusa.com
The company’s newest addition to power standing, the M Corpus VS offers the same cutting-edge technology, ergonomic design, and customizable standing Permobil is known for, but with the maneuverability of a mid-wheel-drive base. The front and rear caster swing-arm positions maximize stability, while minimizing the footprint for a compact 22" turning radius. The new DualLink suspension system optimizes stability in standing, along with superb low-end torque. New swing-away knee supports are 75-percent lighter than the original single-post design and include convenient on-chair storage.
Permobil
(800) 736-0925
permobil.com
Ride Designs takes a potentially more effective approach (orthotic and prosthetic) to address postural care, mobility, and skin protection. We support university-level, ongoing research to inform best practices for wheelchair seating and mobility.

Explore the recent studies here...
https://www.ridedesigns.com/research
TRU-Balance 4 Power Positioning promotes a change in position, enhances functional activities, facilitates physiological functioning, and improves a user’s visual field. It provides 10°, 20°, or 30° of anterior tilt, which facilitates an anterior pelvic position, placing the user in a partial weight-bearing stance. With TRU-Balance 4, users may find it easier to perform mobility-related activities of daily living, such as meal preparation and doing laundry. In addition, users may enjoy improved upper-extremity function and increased access under and over tables and other surfaces. TB4 is available on the Edge 3 Stretto, Edge 3, and 4Front 2 power chairs.
Quantum Rehab
(800) 800-8586
www.quantumrehab.com


The Custom Back provides exacting support for the widest range of needs. It is the better solution for those considering traditional custom wheelchair seating and also an ideal match for the growing, active user. The shape capture process allows the Custom Back to be made to fit virtually any size and contour. Custom Back shapes are captured using the bead bag and vacuum system. Skip the plaster step and use the RideWorks app to quickly and accurately scan a 3D image of the shape. Ride Custom Backs are now manufactured utilizing the latest in 3D printing technology.
Ride Designs
(866) 781-1633
www.ridedesigns.com
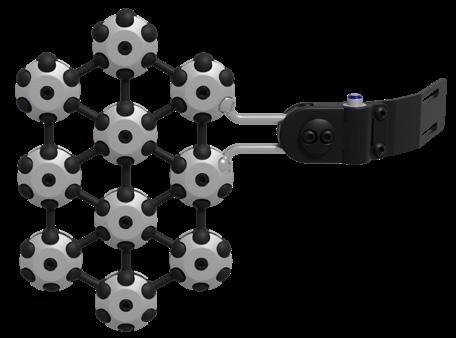
EPiC Seating is a postural management system allowing clinicians to introduce movement into a wheelchair seating environment. The system provides the ability to change positions for function while maintaining control of the pelvis, mitigating the opportunity to introduce shear. Features include an anatomical pivot point that originates from the client, not the frame, so the back moves from the waist up, not from the seat. Daily-routine relief adjustments can be made on demand, with no tools required: Just unlock, adjust and lock. The client can relax and return to a neutral position without a caregiver once the system is unlocked.


Stealth Products
(800) 965 9229
www.stealthproducts.com
The MyWay+ gait trainer has an open design that effectively assists children in maintaining an upright posture, enhancing their walking abilities, and optimizing their chances for engaging in exploration, social interaction, and active participation. It’s tailored to meet the needs of nearly all children (ages 1-16) who require additional trunk support, thanks to its wide range of adjustments and accessories. The gait trainer’s robust, multi-functional casters offer excellent indoor and outdoor performance. One standout feature is the corset-like harness, meticulously engineered to provide 360° wraparound support to the trunk.

Sunrise Medical
(800) 333-4000
www.sunrisemedical.com
Respira Back Supports feature both active (lithium-ion fan) and passive ventilation to create an ultralightweight back support system. The unique ball-joint mounting hardware provides extensive positioning range. Silver thread covers act to eliminate fungi, bacteria, and viruses. As the back medium, choose from cooling, gel-infused and perforated memory foam or Stimulite honeycomb. With two trim levels, a range of sizes, and unique features such as Stimulite padding, Respira Back Supports are the lightest and coolest back supports in the industry.
Symmetric Designs
(800) 537-1724
symmetric-designs.com/respira-back
The Lateral Upper Body Support system (L.U.B.S.) from Symmetric Designs is a new approach to supporting wheelchair users. The swing-away hardware can be mounted to either a wheelchair back support or wheelchair cane and offers depth, height and angle adjustment. The home locking position can be adjusted to ensure a perfect fit. Two lateral pad options are available in a variety of sizes. Free Form pads offer custom-contoured support, and the planar pads offer 360° of angle adjustment.
Symmetric Designs
(800) 537-1724
symmetric-designs.com