Heat and Health:



Heat Impacts on Health | Green Spaces Improve Air Quality Change Our Children’s Climate Future for the Better Health Care Professionals Must Address Climate Change
Ticket Prices: $85 early bird if purchased by November 15; $100 after November 15; Tables of 8 available for $680
Corporate Sponsorships are available!
Bronze: $1,000 Silver: $2,500
Gold: $5000 Platinum: $10,000
Presenting Sponsor: $15,000
The Santa Clara County Medical Association (SCCMA) is excited to announce the 45th Annual Awards Gala at The Westin Hotel in Downtown San Jose!


The SCCMA invites you to attend our 2023 Awards Gala which brings together SCCMA leadership, members, supporters, advocates, and partners to introduce our new president, Gloria Wu, MD, and to bid farewell to our outgoing president, Anlin Xu, MD. We will also honor those who are making a difference in medicine and made an impact to their community this past year.
Let’s reconnect and see friends and colleagues at this annual event. Members may bring a guest. Come to enjoy networking and dinner for our last social event of the year.

RSVP at www.sccma.org/awards2023

Questions? Contact Director of Membership and Programs, Angelica at angelica@sccma.org
For Sponsorship Opportunities, contact Erin Henke at erin@sccma.org
SCCMA is a professional association representing over 4,500 physicians in all specialties, practice types, and stages of their careers. We support physicians like you through a variety of practice management resources, coding and reimbursement help, training, and up to the minute news that could affect your practice. The Bulletin is our quarterly publication.
Santa Clara County Medical Association
SCCMA OFFICERS
President | Anlin Xu, MD
President-elect | Gloria Wu, MD
Secretary | Randal Pham, MD
Treasurer | Anh T. Nguyen, MD
Immediate Past President | Clifford Wang, MD
VP-Community Health | Ken Yew, MD
VP-External Affairs | Christine Doyle, MD
VP-Member Services | Sam Wald, MD
VP-Professional Conduct | Lewis Osofsky, MD
SCCMA STAFF
Interim Chief Executive Officer | Erin Henke, CAE
Director of Membership & Programs | Angelica Cereno
Governance & Advocacy Associate | Emily Coren
Facilities & IT Manager | Paul Moore
SCCMA COUNCILORS
El Camino Hospital of Los Gatos | Shahram S. Gholami, MD
El Camino Hospital – Mountain View | Fahd Khan, MD
Good Samaritan Hospital | CK Park, MD
Kaiser Foundation Hospital - San Jose | David Hensley, MD
Kaiser Permanente Hospital | Reena Bhargava, MD
O’Connor Hospital | David Cahn, MD
Regional Medical Center | Raj Gupta, MD
Saint Louise Regional Hospital | Kevin Stuart, MD
Santa Clara Valley Medical Center | Patricia Salmon, MD

Stanford Health Care/Children’s Health | Laurice Yang, MD
Managing Editor | Erin Henke
Production Editor | Prime42 – Design | Market | Host
Opinions expressed by authors are their own, and not necessarily those of The Bulletin or SCCMA. The Bulletin reserves the right to edit all contributions for clarity and length, as well as to reject any material submitted in whole or in part. Acceptance of advertising in The Bulletin in no way constitutes approval or endorsement by SCCMA of products or services advertised. The Bulletin and SCCMA reserve the right to reject any advertising.
Address all editorial communication, reprint requests, and advertising to: Erin
SCCMA has been busy this year. We started several new and exciting programs, such as Saving Private Practice for independent physician practices, Physician Wellness and Walk with a Doc. Our biggest and most time-consuming task this year was embarking on the search and selection of a new CEO for SCCMA.
We started planning the CEO search process early this year. Being one of the largest county medical associations in California, we had help from the CMA. We formed a CEO search committee led by me and Immediate Past President, Dr. Clifford Wang, as well as five members of the SCCMA Executive Committee and two SCCMA Councilors. CMA Vice President of Membership, Marketing and Component Relations, Mike Steenburgh, assisted with developing and posting the position profile, as well as screening and interviewing candidates. We received an overwhelmingly response with more than 450 applicants!
The selection process was thorough and thoughtful. Candidates were screened and the search committee was then tasked with ranking the top 40 screened candidates based on 20 characteristics. That ranking produced the top ten candidates. Six candidates were then invited for in-person interviews. In the second round of interviews, the final three candidates presented the search committee with their vision for their first 100 days as SCCMA CEO. It was an extensive, exhaustive, and meticulous process.
I’m pleased to share that the candidate that has been selected is Marc Chow. Mr. Chow comes from a family of physicians. His father is a primary care physician in San Francisco who has been
involved extensively in organized medicine, as a Board member and Past President of the San Francisco Medical Society, and as a CMA Trustee.
Mr. Chow is passionate about and very close to the healthcare system. He has a master’s degree in health administration and over 11 years managing a national organization of renal healthcare providers, including physicians. Mr. Chow was instrumental in organizing renal physician systems so that even smaller dialysis centers can be paid by Medicare. He is excited to contribute to a local physician organization and has a vision for how to improve SCCMA, grow our membership and enhance member services. We think he will be a great leader for SCCMA and look forward to him joining the organization on October 2nd.
There are so many great SCCMA events and programs between now and the end of the year. Personally, I’m really looking forward to the next Saving Private Practice webinar. I always enjoy them. I’m also looking forward to the Saving Private Practice Vendor Solutions event which will connect physicians with service providers who can enable them to provide better and more efficient care. I also look forward to the virtual SCCMA Annual Meeting and Election on November 14 where we elect our 2024 Councilors and Officers. And our Annual Awards Gala on December 8 will be a lot of fun, as we honor physician leaders who are the shining stars of our physician community. I hope to see you at one or all of our upcoming events!
Thank you to all our physician members whose participation makes SCCMA a truly vibrant organization.
There are so many great SCCMA events and programs between now and the end of the year.
the awards, outlined below, would be appreciated. Suggestions must be received by October 14, 2022. Thank you for your recommendations.
If you previously suggested a candidate who was not given an award, please feel free to resubmit that name.
Robert D. Burnett, MD Legacy Award For a physician member of the Medical Association who has demonstrated extraordinary visionary leadership, tireless effort, selfless long-term commitment, and success in challenging and advancing the health care community, the well-being of patients, and the most exalted goals of the medical profession.
Benjamin J. Cory, MD Award For a physician member of the Medical Association who has displayed forward-looking, pioneering ideas, enterprise, enthusiasm, and prolonged professional stature and ability.
Outstanding Achievement in Medicine For a physician member of the Medical Association who, during his/her medical career, has made unique contributions to the betterment of patient care, for which he/she has achieved widespread recognition. Consideration shall be given to research and/or the development of procedures, methods of treatment, pharmaceutical agents, or technological advances in the field of medicine.
Outstanding Contribution to the Medical Association For a physician member of the Medical Association who has exhibited sustained interest and participation in one or more activities of the Association over and above that expected of the membership at-large.
Outstanding Contribution in Medical Education For a physician member of the Medical Association who has exhibited sustained interest and participation in one or more medical education activities over and above that expected of the membership at-large.
Award for Outstanding Contribution in Community Service For a physician member of the Medical Association who has exhibited sustained interest and participation in one or more activities of the community over and above that expected of the membership at-large.
Citizen’s Award For an individual who is not a member of the Medical Association, who has achieved public recognition for a significant contribution in the health field. (This usually will be a non-physician, although physicians are not categorically excluded.)
William C. Parrish, Jr. Leadership in Healthcare Award This award is named after the beloved long-time executive director of the Santa Clara County Medical Association and recognizes an individual whose leadership, innovation, and dedication have resulted in profound improvement to healthcare in Santa Clara and has left a lasting impact on the physicians and patients of the County. William Parrish is the first recipient of this award (established in 2018).
CLICK HERE TO SUBMIT NOMINATIONS
For a complete list of ALL award recipients since 1978, please refer to www.sccma.org.


The Santa Clara County Medical Association (SCCMA) would like you to submit nominations for the 2023 Annual Awards Gala! Do you have a physician in mind that has gone above and beyond this year? Has a physician impressed you with their contribution to healthcare? Did an individual make significant contributions to the health field? Nominate a colleague to be recognized at this year’s Annual Awards Gala. Recipients are selected from among our outstanding members who have distinguished themselves with extraordinary service to medicine, the association, the community, and medical education. The nomination deadline is October 14, 2023. To nominate someone, visit https://www.surveymonkey.com/r/5DZZV6S.
The California Medical Association (CMA) and the Coalition to Protect Access to Care (https:// www.accesstohealthcareca.com/), a broad and diverse group of health care organizations, recently filed a statewide ballot initiative to expand access to health care for millions of Californians, with a goal of qualifying and then passing the measure on the November 2024 ballot. The “Protect Access to Healthcare Act” increases Medi-Cal provider rates, invests in the healthcare work and will be critical to ensuring the accessibility and affordability of health care services for all Californians, as well as recognizing the critical role that physicians play in achieving this vision. The initiative will continue the Managed Care Organization (MCO) tax agreement that will bring billions of dollars in federal funds to California each year and invest it in the Medi-Cal system and health care workforce priorities.
In the coming months, CMA will be working closely with the other members of the coalition to gather the hundreds of thousands of signatures needed for the initiative to be placed on the ballot. Your support and engagement will be invaluable in driving this initiative forward. You can view informational materials at www. cmadocs.org/access/initiative.




Recently, 28 SCCMA physicians and their guests attended an all-inclusive weekend wellness retreat at 1440 Multiversity that included private accommodations, locally sourced meals, wellness activities, and use of campus amenities such as hiking trails, fitness center and infinity-edge hot tub. Throughout the weekend, attendees interacted during signature sessions with facilitators that discussed topics such as moral injury, grief, and healing, and ended with wellness champion, Dr. John Chuck, speaking on hope, journey to joy, and growth. Attendees also had the option to participate in wellness activities such as nature walks, yoga, stick tai chi, meditation, and a sound journey.
Upcoming wellness events are listed in the SCCMA eNewsletter and Upcoming Events page on our website, www.sccma.org. We hope you can join us!


Reading has a way of bringing relaxation by slowing down your heart rate and getting lost in the words on a page. This year, SCCMA started a book club for our physician members. In September, SCCMA’s first book club gathered at the SCCMA office to socialize and talk about the medical fiction book, Doctors and Friends, by Kimmery Martin, MD, emergency medicine doctor-turned novelist. Dr. Martin joined the book group virtually to share her writing process and insights on character development. Written prior to Covid-19, Doctors and Friends provides a unique insider’s perspective into the world of medical professionals working to save lives during the most difficult situations of their careers.
If you are interested in joining SCCMA’s Book Club, please contact Director of Membership and Programs, Angelica, at angelica@sccma.org.



SCCMA recently teamed up with physicians and administrators from Bay Area Community Health (BACH) to advocate for legislation to address physician shortages and patient access to care. Dr. Christine Doyle, Dr. Clifford Wang, and Dr. Sydney Thomson represented the SCCMA team and Dr. Ramchandani, Chief Medical Officer, Dr. Zetti Page, CEO, and Wilfredo Lacro, Chief of Strategic Development represented the BACH team. Congressman Panetta attended with his field representative, Alyssa Garcia-Marquez. They met at the White Road office of the Bay Area Community Health facility, which served over 300 patients that day alone. The BACH staff gave Congressman Panetta a brief tour and then joined everyone for a lively discussion about how physician shortages impact patient care. During the visit, the physicians requested that Congressman Panetta cosponsor several bills that address physician shortages and patient access to care. Our collaborative efforts showcased our unity and strength, sending a clear and powerful message.
To get involved in SCCMA’s legislative advocacy efforts and External Affairs Committee, please contact Governance and Advocacy Associate, Emily Coren at emily@sccma.org.
ARE YOU TAKING ADVANTAGE OF YOUR CMA BENEFITS? HERE’S AN EXAMPLE OF HOW MUCH YOU COULD SAVE.
Purchase health insurance for your staff through CMA’s Insurance Brokerage Program.
SAVE $12,968
Call CMA’s legal information line and access CMA’s online health law library as your first step in getting the information you need.
SAVE $2,846
Select PatientPop’s all-in-one technology solution that’s proven to help physicians thrive in the digital age.
SAVE $2,354 OR MORE
Call CMA’s reimbursement helpline for help with problematic payors.
RECOVER $1,070
Refinance student loans with CMA partner SoFi, which offers a variety of programs.
SAVE $27,000
Purchase workers’ comp insurance through the Preferred Employers program.
SAVE $3,750
Participate in complimentary memberonly online webinars .
SAVE $318
Save up to 7% on your auto coverage and up to 23% by bundling your auto and home insurance through Mercury Insurance.
SAVE $671
TOTAL SAVINGS: $50,977+
CAN YOU AFFORD NOT TO BE A MEMBER?
Visit cmadocs.org/join today!
For more information, call the CMA Member Resource Center at (800) 786-4262.

The California Medical Association (CMA) recently won a significant NEW expansion in the federal Public Service Loan Forgiveness (PSLF) program that expands eligibility for California physicians who were previously barred from participating. If you still have student loans and provided services in a nonprofit hospital, clinic/office owned by a 1206(l) foundation or other nonprofit entity for an average of 30 hours per week, you may now qualify. Even if you work for a for-profit sole proprietorship, have a contract with a for-profit partnership or are employed by a for-profit medical group, you may still qualify if the services you provided were in a facility owned by a nonprofit.
CMA has published a guide – “ Public Service Loan Forgiveness: What California Physicians Need to Know ” – to help physicians determine whether they may qualify for hours worked back to 2007 or for future years of service. The guide also contains detailed instructions on the application form. To view the complete guide, visit bit.ly/pslf-guide.
CMA along with the California Hospital Association, Texas Medical Association, and Texas Hospital Association are cohosting a free webinar on the new PSLF rules. The one-hour webinar is Thursday, September 28, 2023, at 12:15 p.m., Pacific time. To register, visit cmadocs.org/events .
The webinar will provide specific instructions about how more California and Texas physicians can qualify for PSLF. It will also discuss how hospitals, foundations and other entities can serve as “qualifying employers” for purposes of PSLF, even though they are prohibited by state law from employing physicians.

The U.S. Department of Education will provide information about eligible qualifying loans and the new eligibility criteria. There will also be a legal presentation about the types of practices that qualify, the required written agreements between physicians and nonprofit entities, and suggestions for documenting the required work hours with time for your questions.
After the event, download the webinar by visiting CMA’s on-demand webinar library at cmadocs.org/webinars .
Marlene Sturm, MD, serves as Medical Director of the Children’s Advocacy Center (CAC) of Santa Clara County, our county’s program to provide comprehensive medical and forensic services for children and adolescents who have experienced all forms of maltreatment. The CAC provides medical services for children from birth to age 18 who have experienced physical abuse and neglect, sexual abuse and sexual assault (SAFE), emotional abuse, child abduction, and child trafficking (CSEC).
Dr. Sturm attended Brown University as an undergraduate and received a BA in Comparative Literature, magna cum laude. After college, she taught 9th grade math for two years at her high school alma mater in Los Angeles. Dr. Sturm attended Stanford Medical School, then completed a residency in pediatrics at Stanford Hospital. Following residency, Dr. Sturm worked as a general pediatrician at East Valley Clinic, a small clinic on the East side of San Jose, affiliated with Santa Clara Valley Medical Center (SCVMC). She loved the work and stayed at East Valley for over twenty-five years. During those years, Dr. Sturm raised her children and served as a member and then president of two Bay Area non-profit boards in the field of education.
In 2016, SCVMC administration asked Dr. Sturm to direct the County’s child abuse program. In 2018 and 2019, Dr. Sturm was a leading voice in the effort to establish a Children’s Advocacy Center (CAC) in Santa Clara County. CAC, located adjacent to O’Connor Hospital in San Jose, opened its doors two years ago, in April 2021. There are more than 900 CACs across the United States. Following the national model, the Children’s Advoca-

cy Center of Santa Clara County is a collaboration between all government and non-government agencies that help children and families disclose their experiences of trauma, seek justice, and begin to heal. The Children’s Advocacy Center is a collaboration between the District Attorney’s Office, Santa Clara Valley Medical Center, Social Services Agency (CPS), the thirteen law enforcement agencies in our county, and non-profit advocacy organizations, including Community Solutions and the YWCA.

Dr. Sturm is a member of
We have a 24-hour HOTLINE to answer all questions about the medical evaluation of child abuse. We can answer your questions about the case; discuss mandated reporting, authorization and consent; make appointments at the CAC; and refer you to other services or providers when appropriate. We have counseling services on site at the CAC, available to all our patients.




the Helfer Society, the national honor society of child abuse pediatricians. She currently serves as Chair of the Child Abuse Prevention Council of Santa Clara County, a commission of the Board of Supervisors. This spring, Dr. Sturm received the 2023 award for Outstanding Service from the California Chapter of the American Professional Society on the Abuse of Children (CAPSAC).
Dr. Sturm enjoys art projects, playing the piano, and spending time with her friends, two dogs, and three children.
If you see children and adolescents in your practice, please save these phone numbers:
CAC Medical HOTLINE: 1 (669) 299-8810 Staffed by CAC Medical staff 24/7/365
CPS HOTLINE: 1 (833) 722-5437 Staffed by Social Services 24/7/365 for mandated reporting.
Please note: For mandated reporters, calling the CAC Medical HOTLINE does not replace your responsibility to contact the CPS HOTLINE or to call the law enforcement agency where the alleged incident occurred.
WHEN CHILDREN FEEL SAFE, THEY CAN BEGIN TO TALK ABOUT WHAT HAPPENED TO THEM. AT THE CAC, WE ARE SO PROUD TO PROVIDE A PLACE WHERE CHILDREN FEEL SAFE AND UNDERSTOOD—AND WHERE THEY CAN BEGIN THE LONG PROCESS OF HEALING.
~MARLENE STURM, MD
The California Medical Association and the Coalition to Protect Access to Care have launched the Protect Access to Healthcare Act and are working to place it on the November 2024 ballot to ensure that millions of Californians have greater access to affordable, high-quality, life-saving health care.
+ Medi-Cal provides essential health coverage to one in three Californians and is foundational to the state’s health care delivery system and economy. In fact, 15 million Californians and nearly 50% of children get their health care through the Medi-Cal program, making it essential for preventive and routine care for California kids.
+ Medi-Cal provider rates have not increased in more than a decade, and for most physicians it’s been more than 25 years – leaving millions of patients insured, but without meaningful access to health care. Patients with Medi-Cal coverage routinely wait weeks or months for appointments, and oftentimes must travel long distances to receive care.
+ Historically, California has used the Managed Care Organization (MCO) Tax – a tax on health insurance companies – to draw down federal funding and help support the state’s General Fund. The last MCO Tax expired at the end of 2022.
+ Recognizing that we have a generational opportunity to improve health outcomes for millions of Californians, this ballot initiative will use MCO Tax revenue to make critical and meaningful investments in the Medi-Cal system.
The Protect Access to Healthcare Act will increase reimbursement rates for Medi-Cal providers – some of which have not been increased in decades – and expand our state’s graduate medical education and training to create more physician residency programs and funding for more residency positions within those programs. Additionally, there will be funding for loan repayment for physicians, dentists and other allied health professionals. These actions will bring more providers to areas across California where they are needed most.
Specifically, the initiative will:
+ Make the Medi-Cal provider rate increases that were included in the 2023-24 state budget permanent for generations to come
+ Expand access to health care for Medi-Cal patients, which will result in less use of emergency rooms and decrease wait times for all Californians Increase funding for mental health programs that care for children and Medi-Cal patients
+ Allow California to manufacture its own insulin and other prescription drugs for Californians at much lower prices than currently exist
In addition to funding Medi-Cal rate increases for primary care, specialty care, mental health care and emergency physician care, the measure will ensure that Medi-Cal patients have more access to preventive medicine, which will reduce expensive and timely emergency room usage, benefiting everyone.
The Protect Access to Healthcare Act will raise $4.3 billion in annual, ongoing revenue that will be distributed in the following areas:
+ Primary Care - 22%
+ Specialty Care - 22%
+ Emergency Department Access - 8.75%
+ Mental Health Facility Access - 7%
+ Outpatient and Clinic Access - 5.75%
+ Family Planning - 5.5%
+ Graduate Medical Education - 4.5%
+ Health Care Workforce - 4.5%
+ Improved Clinic Quality - 3.5%
+ Public Hospitals - 3.5%
+ Specialty Dental Services - 3.5%
+ Ground Emergency Transport - 3%
+ Emergency Room Physicians - 2.5%
+ Abortion Access - 1.25%
+ Advance Practice Cllinician and Allied Health Loan Repayment - .75%
+ CalHealthCares Physician and Dental Loan Repayment - .75
+ Community Health Care Workers - .75%
+ Affordable Prescription Drugs - .5%
+ The Coalition to Protect Access to Care consists of of physicians, dentists, health care workers, hospitals, community health centers, Planned Parenthood and emergency responders working together to support a ballot measure to permanently use dedicated funding to support Medi-Cal providers such as physicians, hospitals, women’s health, and community clinics and health centers.
+ The coalition’s goal is to ensure that Medi-Cal enrollees have the same access to care as those with commercial insurance, and that providers can afford to treat their communities as they present themselves – without worrying about the financial solvency of their practices.
9-8-23
cmadocs.org/access
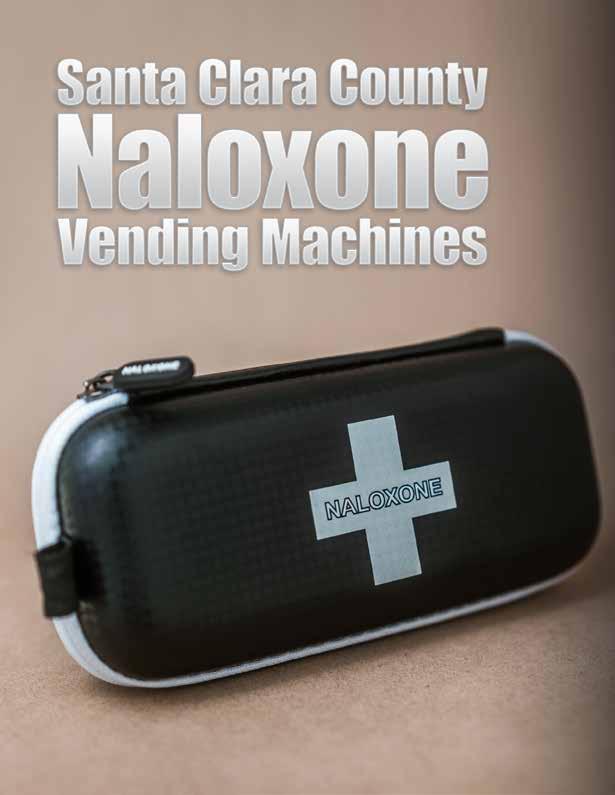
Illicit fentanyl-related overdose deaths for 2023 in Santa Clara County more than doubled at the end of May, with 41 deaths compared to 17 recorded deaths at the end of April 2023.
Naloxone is a medication used to reverse potentially lethal fentanyl and other opioid overdoses. The FDA granted approval for non-prescription naloxone.
The Naloxone Distribution Project (NDP) as funded by the Substance Abuse and Mental Health Services Administration (SAMHSA) is administered by the California Department of Health Care Services (DHCS) to combat opioid overdose-related deaths. The NDP aims to reduce opioid overdose deaths through the provision of free naloxone.

Public health vending machine (PHVM) programs are a promising strategy to increase naloxone access as well as safer injection kits.

In Ohio, registrants connected with a harm reduction coordinator (HRC) and can receive naloxone kits from a PHVM. In Nevada, naloxone dispensation by PHVMS was associated with a short-term reduction in opioid overdose fatalities.
Installing a PHVM outside can facilitate around the clock access. Outdoor PHVMs may require temperature control to protect their contents.
A PHVM may contain only naloxone or it can dispense other items such as fentanyl test strip and sterile syringes.
A PHVM may require that participants swipe a card or enter a PIN number received after registering with a HRC to allow for public health data collection. Other PHVMs dispense items without swiping a card/submitting personal information resulting in less data collection.
Last November, the Santa Clara County Behavioral Health Services Department (BHSD) Addiction Medicine Division started a PHVM program. Five vending machines are presently located at Santa Clara County jails including Elmwood and Juvenile Hall. The approximately nine-thousand-dollar cost of each machine was funded by opioid settlement funds, and Substance Abuse Prevention and Treatment Block Grant (SABG) programs. The NDP is providing all the naloxone kits.
Each machine contains 150 naloxone kits. Restockingsupplies is at least once per week. Anyone is eligible to use the machines. One can simply push a button and get a kit containing two 4mg naloxone nasal spray doses. There is no cost to use the machine. No user information is collected at the present time. Each kit contains directions for use. There is a scannable QRS code that provides a link to an instructional video. The machines are accessible to the public during the business hours of the building housing the machine. The agency responsible for the building housing a machine is responsible for maintenance and re -
stocking the naloxone kits.
While PHVMs appear to be a novel approach in coping with opioid overdoses, there remains limited evidence for their effectiveness. Research is needed to evaluate whether PHVMs reduce overdose deaths or can establish a connection to opioid use disorder treatment.
References:
Wagner NM, Kempe A, Barnard JG, Rinehart DJ, Havranek EP, Glasgow RE, Blum J, Morris MA. Qualitative exploration of public health vending machines in young adults who misuse opioids: A promising strategy to increase naloxone access in a high risk underserved population. Drug Alcohol Depend Rep. 2022 Dec;5:100094. doi: 10.1016/j.dadr.2022.100094. Epub 2022 Sep 8. PMID: 36687307.
Stewart RE, Cardamone NC, Loscalzo E, French R, Lovelace C, Mowenn WK, Tarhini A, Lalley-Chareczko L, Brady KA, Mandell DS. “There’s absolutely no downside to this, I mean, except community opposition:” A qualitative study of the acceptability of vending machines for harm reduction. Harm Reduct J. 2023 Feb 28;20(1):25. doi: 10.1186/s12954-023-00747-4. PMID: 36855064; PMCID: PMC9971672.
Russell, E., Johnson, J., Kosinski, Z. et al. A scoping review of implementation considerations for harm reduction vending machines. Harm Reduct J 20, 33 (2023). https:// doi.org/10.1186/s12954-023-00765-2
Arendt D. Expanding the accessibility of harm reduction services in the United States: Measuring the impact of an automated harm reduction dispensing machine. J Am Pharm Assoc (2003). 2023 Jan-Feb;63(1):309-316.
Allen ST, O’Rourke A, Johnson JA, Cheatom C, Zhang Y, Delise B, Watkins K, Reich K, Reich R, Lockett C. Evaluating the impact of naloxone dispensation at public health vending machines in Clark County, Nevada. Ann Med. 2022 Dec;54(1):2692-2700.
https://www.songforcharlie.org/college-toolkit
Heat harms health. Heat is the leading cause1 of weather-related deaths in the United States though heat impacts are also increasing globally.2 In the U.S., 326 million people, around 97% of the population, experienced at least one summer day with temperatures made at least 2x more likely due to human-caused climate change. Exposure to extreme heat makes it difficult for our bodies to cool off, resulting in heat-related illnesses3 including heat cramps, heat exhaustion, and even fatal medical emergencies such as heat stroke. Heat can also worsen air quality4 by trapping harmful pollutants in the air we breathe. These pollutants can exacerbate respiratory health issues in people with asthma and other lung diseases. Heat harms mental health5 as well as physical health. It increases irritability, symptoms of depression and rates of suicide. It affects behavior, contributing to increased aggression and incidence of domestic violence and increased substance use. These challenges provide opportunities for public health improvements6 such as increasing urban green space.7

Extreme heat events are an ongoing health concern in Santa Clara and are increasing in frequency 8 as result of climate change. Local examples include this Advisory Issued for Excessive Heat Wave in Santa Clara County on August 13, 20209, and this issued heat advisory from July 2023.10 The FEMA National Risk Index score for Santa Clara County11 is very high with a score of 99.8 with heat waves being listed as the third highest risk factor. Health impacts aren’t the only direct consequences of heat events, the losses to the community have financial impacts too, such as the Expected Annual Loss (EAL) for a heat wave event in Santa Clara is listed as $4,149,888. The CDC Heat and Health Tracker12 provides local heat and health information so communities can better prepare for and respond to extreme heat events. These extreme heat events are going to continue to get worse and will remain a persistent impact to healthcare in Santa Clara County.


Climate change is a human caused shift in the Earth’s climate due to overreliance since the industrial revolution on fossil fuels as energy sources. Adaptation opportunities such as increasing greenspaces and lowering surface albedos will improve public health outcomes in Santa Clara by keeping surface temperatures cooler. These adaptation measures improve the safety of community members in already hot places. However, extreme weather events are increasing in frequency and severity as a result of climate change and adaptation measures alone are not enough. Mitigation efforts are how we can reduce the severity of heat events in the future by pulling down carbon use. Mitigation includes strategies such as transitions to renewable energy sources and increasing electrification infrastructure. Electrification is currently the best energy option available to us and a rapid transition to electrification is already underway. Programs like Rewiring America13 and the American Council for an Energy-Efficient Economy (ACEEE) Building Electrification Programs14 and the now year-old Inflation Reduction Act (IRA) of 202215 which makes the single largest investment in climate and energy in American history, increasing domestic clean energy manufacturing and infrastructure.
While it is essential that we make these changes, and fast, some irreversible damage has already been done. One of the regional consequences is that Santa Clara is getting hotter. We must reduce carbon emissions by transitioning to a carbon neutral economy to mitigate what could still be the worst of the regional impacts to Santa Clara. We need to use both adaptation and

• Extreme heat results in excess death and illness through heat stroke, heat exhaustion and exacerbations of chronic illness. Heat stress and associated dehydration can exacerbate existing renal disease and may be linked to new epidemics of chronic kidney disease among individuals without other traditional risk factors. Heat increases ozone levels, exacerbating asthma, other respiratory disease, and cardiovascular disease. Some medications inhibit sweating or reduce the ability to sense overheating, increasing the risk of heat illness.
• Heat causes more deaths than any other type of natural disaster. From 1999-2010, 7,415 people died from heat-related illness in the U.S., an average of 618 per year. The 2006 California heat wave resulted in 655 excess deaths, over 16,000 additional emergency room visits, and a 10-fold increase in admissions for heat-related illness.
• Heat waves and concurrent drought contribute to crop and livestock loss, resulting in rising food prices and increased food insecurity. In 2015 the California drought resulted in $900 million in crop revenue loss, $350 million in livestock and dairy loss, tens of thousands of lost jobs, and a total economic impact estimated to be $2.7 billion.
Excerpt from the Public Health Institute toolkit on Extreme Heat, Climate Change and Health available at https://climatehealthconnect.org/wp-content/uploads/2016/09/ExtremeHeat.pdf.
These heat events are not a one-time occurrence. They will get worse in magnitude and frequency for the foreseeable future as a result of climate change.
mitigation actions to improve heat safety in Santa Clara County.
Urban heat islands are areas in a community with dense urban areas, fewer trees, less green space, more buildings, higher energy use, and more impervious asphalt and concrete. These characteristics create areas where nighttime temperatures may be as much as 22°F higher than surrounding areas. The areas that get the hottest have the highest albedo surface temperatures, such as concrete and asphalt. Concrete and cement are hotter than the living systems such as green spaces because they absorb and retain heat and energy. Plants and greenspaces reduce heat impacts by both having a lower surface albedo and through the evapotranspiration of their respiration. In cities and other urban environments these heat impacts are worse.
These heat impacts are not evenly distributed. Extreme heat can affect everyone, but some face greater risks of heat-related illness than others. These vulnerabilities map onto areas of historical residential segregation. Low income and communities of color are more likely to be located in urban heat islands. Additionally, children, adults over 65, pregnant people, and people with preexisting medical conditions are more vulnerable to heat related illnesses. Outdoor workers and athletes are also at elevated risk16 due to work- and recreation-related exposure to extreme heat. Cooling centers17 are already being set-up around the county during extreme heat events, however these programs fail to address the structural changes needed to reduce heat island effects and eliminate fossil fuel use.
Individuals trying to reduce the immediate consequences of heat can increase the shade around their homes, plant trees, replace asphalt with cooler surfaces and reducing energy use by installing energy-efficient appliances. However, to appropriately address the municipal impacts, we need to also address policy level decisions. Planting trees and other vegetation18 lowers
References
1. https://www.weather.gov/hazstat/
2. https://www.who.int/news-room/fact-sheets/detail/climatechange-heat-and-health
3. https://www.heat.gov/pages/planning-and-preparing
4. https://www.climatecentral.org/climate-ma`ers/stagnant-air
5. https://www.psychiatry.org/news-room/apa-blogs/extremeheat-can-take-a-toll-on-mental-health
6. https://www.niehs.nih.gov/research/programs/climatechange/ health_impacts/heat/index.cfm
7. https://storymaps.arcgis.com/stories/1a4413e0ca1e48c5973ca87d6d59fdfc
8. https://abc7news.com/extreme-heat-hot-weather-bay-area-climate-change-weathering-tomorrow/13659905/
9. https://www.sanjoseinside.com/news/advisory-issued-for-excessive-heat-wave-in-santa-clara-county/
10. https://www.santaclaraca.gov/Home/Components/News/ News/44602/3171
11. https://hazards.fema.gov/nri/report/viewer?dataLOD=CounD -
surface and air temperatures by providing shade and cooling through evapotranspiration. Trees and vegetation that directly shade your home can decrease the need for air conditioning, making your home more comfortable and reducing your energy bill. Trees also protect your family’s health by improving air quality, by providing cooling shade for outdoor activities, and reducing exposure to harmful UV radiation. Cool or reflective surfaces help to reflect sunlight and heat away from your home, reducing roof temperatures. This allows for your home to stay cooler, reducing the amount of air conditioning needed during hot days. Using efficient appliances and equipment in your home can help to lighten the load on the electric grid during heat waves, thus ensuring a more reliable supply of electricity to your community.
Physicians can help shape policy decisions by speaking with their representatives and advocating for policy decisions that reduce carbon emissions (mitigation), such as electrification and renewable energy, and adaptation policies including urban greening and building with lower albedo surfaces. In these examples it is helpful to provide specific examples of how heat has harmed the health of your patients.
The Public Health Institute has written a Physician’s Guide to Climate Change, Health and Equity19 as a resource to strengthen and inform your voice as a trusted health professional on climate change, health and equity including a guide and posters20. Within these resources, the Extreme Heat, Climate Change and Health states that, “Extreme heat has direct effects on health, and heat kills more people than any other extreme weather event. In this brief, we focus on the health impacts of climate change and heat in the U.S.” Bay Area physicians are already speaking up advocating for policies that reduce these health harms, such as Dr. Lisa Patel who works at a small community hospital in the East Bay, advocating for green spaces in city schools20.
es&dataIDs=C06085
12. https://ephtracking.cdc.gov/ApplicaDons/heatTracker/
13. https://www.rewiringamerica.org/
14. https://www.aceee.org/research-report/b2201
15. https://www.energy.gov/lpo/arDcles/transforming-clean-energy-financing-and-supply-chains-united-states-lpo- one-yearajer
16. https://www.heat.gov/pages/who-is-at-risk-to-extreme-heat
17. https://news.sccgov.org/excessive-heat-advisory-santa-clara-county-through-labor-day-weekend
18. https://www.epa.gov/heaDslands/using-trees-and-vegetaDon-reduce-heat-islands
19. https://climatehealthconnect.org/resources/physicians-guide-climate-change-health-equity
20. https://www.phi.org/about/impacts/empowering-physiciansto-speak-out-on-climate-change/ https://localnewsma`ers.org/2023/07/30/going-to-extremesschools-ditching-asphalt-playgrounds-to-protect- kids-fromrising-heat/

Policy makers need to make rapid adjustments to reduce the severity of extreme heat events in Santa Clara County.
The SCCMA Environmental Health Committee has examined the issue of artificial turf and recommends that the Saratoga High School Board of Trustees replace the artificial turf with natural living grass, as have other cities, for the health and safety of both the students and the environment. Although in the past artificial turf seemed to be the best alternative due to reduced costs, reduced water usage, and lower maintenance, newer information has come to light regarding the direct and indirect environmental and health impacts of synthetic grass, including full life cycle analysis.
August 6, 2023
We understand that you are planning to replace older artificial turf on your playing field with new artificial turf. The SCCMA Environmental Health Committee has examined this issue and recommends that you replace the artificial turf with natural living grass, as have other cities, for the health and safety of both your students and the environment. Although in the past artificial turf seemed to be the best alternative due to reduced costs, reduced water usage, and lower maintenance, newer information has come to light regarding the direct and indirect environmental and health impacts of synthetic grass, including full life cycle analysis. This is a global problem (Armada 2022).
The cost of a natural field is less than synthetic fields in the long run. Daviscourt (2017) performed a complete life cycle analysis comparing artificial turn versus natural turf over an 8-year period with turf replacements and revealed that the cost savings significantly favored natural turf grass. The University of Arkansas in came to a similar conclusion when looking at maintenance costs, which include mowing, cleaning, chemical applications, replacement costs, and water use. The additional costs for synthetic turf are described below and can be quite significant.
The creation of local heat islands are known problem on artificial fields. Temperatures can be significantly higher even under normal weather conditions due to their solar absorption and lack of evaporative cooling that natural grass has. This poses risks of burns, heat stroke and heat exhaustion, making the fields unusable in certain conditions. With climate change this will be more of an issue for athletes and children.
There is also data showing increased risks of sports injuries on artificial turf, particularly in football and soccer, as well as the promotion of antibiotic resistant bacterial infections.
Artificial turf contains hazardous chemicals and heavy metals as discussed below. Children are more vulnerable to all toxic exposures due to their immature biological systems. On an artificial sport field children and athletes are routinely in contact with the surface, especially with soccer and football; therefore, they more readily inhale, ingest, and come in dermal contact with dust and chemicals emitted from the fields. Thus, it is reasonable to expect that these synthetic turf fields can pose an increased health risk to children. Precaution is thus imperative.
In addition, sports fields will last 8 to 20 years before disposal. Plastic waste is an ongoing challenge at the end of their lifetime. Typical sports fields are about 80,000 square feet and contain about 40,000 pounds of “grass” turf along with 240,000 ± 720,000 pounds of infill according to the Synthetic Turf Council. This complex mixture of compounds is not recyclable and is usually sent to the landfill with continued leaching of chemicals.

As awareness of all of these factors increase, more cities, such as Boston, are banning artificial turf in parks and on sports fields. In addition, governments in the US and abroad are restricting the use of artificial fields with crumb rubber or certain hazardous plasticizers (EU and California) due to environmental bio-accumulation of toxic chemicals.
Artificial turf is composed of a plastic backing, plastic “blades of grass” and cushioning infill. Typically tire crumb rubber is used for infill. All of these components are derived from petroleum products. These components contain microplastics as well as chemicals acknowledged as being hazardous such as polycyclic aromatic hydrocarbons (PAHs), bio-accumulative (“forever”) per- and polyfluoroalkyl substances (PFAS), phthalates, silica (silica sand infill), polychlorinated biphenyls (PCBs), carbon black and metals such as lead, mercury, cadmium, chromium, cobalt, and arsenic. In addition, pesticides and biocides are used on artificial fields to reduce bacteria, viruses and weeds, which could cause adverse reactions and skin sensitization.
These chemicals can potentially contaminate water supplies through runoff, as well as leaching into groundwater and soil, persisting in the environment. Children can be exposed via inhalation of off-gassing compounds or ingestion of infill components. The crushed tire rubber infill adheres to skin, shoes and clothing then enter cars and homes. Based upon the presence of known toxic substances in tire rubber and the lack of comprehensive safety studies, The Children’s Environmental Health Center of the Icahn School of Medicine urged a moratorium on the use artificial turf generated from recycled rubber tires. The US Environmental Protection Agency states in their assessment that “the existing studies do not comprehensively evaluate the concerns about health risks from exposure to tire crumb.” (Marsili 2014).
PFAS are found in all samples of artificial turf. They are used in processing to enhance smoothness and reduce friction. PFAS
in plastics are especially problematic because they are a category of chemicals that contain multiple fluorine atoms bonded to a chain of carbon atoms which makes them resistant to breakdown. They are typically used for water resistance, stain resistance and non-stick cookware. This group of chemicals bioaccumulates in the food chain and has contaminated water supplies throughout the nation.
Human health risks include endocrine disruption, adverse effects on the liver and thyroid, as well as metabolic effects, developmental effects, neurotoxicity, and immunotoxicity.
The Mindaroo-Monaco Commission on Plastics and Human Health Report 2023 concludes: “It is now clear that current patterns of plastic production, use, and disposal are not sustainable and are responsible for significant harms to human health, the environment, and the economy as well as for deep societal injustices…The thousands of chemicals in plastics—monomers, additives, processing agents, and non-intentionally added substances—include amongst their number known human carcinogens, endocrine disruptors, neurotoxicants, and persistent organic pollutants. These chemicals are responsible for many of plastics’ known harms to human and planetary health. The chemicals leach out of plastics, enter the environment, cause pollution, and result in human exposure and disease. All efforts to reduce plastics’ hazards must address the hazards of plastic-associated chemicals…to protect human and planetary health, especially the health of vulnerable and at-risk populations, and put the world on track to end plastic pollution by 2040. This Commission supports urgent adoption by the world’s nations of a strong and comprehensive Global Plastics Treaty in accord with the mandate set forth in the March 2022 resolution of the United Nations Environment Assembly (UNEA).” (Landrigan 2023)
Ford and Monsanto Industries joined efforts to make the first artificial turf in 1964 called Chemgrass which was first installed in the Astrodome when the grass died due to issues with the plastic covering of the dome. By the 1980’s athletes were complaining that the turf was harder and caused more injuries. A poll by the National Football League in 1995 revealed that 95% of players believed that synthetic turf increased their risk of injuries (Claudio 2008). There is both anecdotal and scientific evidence of higher rates of injuries on artificial fields.
A 2019 study from Case Western Reserve University and the
University Hospital Sports Medicine Institute analyzed data collected by 26 high school athletic trainers during the 2017-2018 athletic seasons. The authors found, “athletes were 58 percent more likely to sustain an injury during athletic activity on artificial turf. Injury rates were significantly higher for football, girls and boys soccer, and rugby athletes. Lower extremity, upper extremity, and torso injuries were also found to occur with a higher incidence on artificial turf.” (Voos 2019)
A 2005 high school football study noted that during higher temperatures there were reported higher incidences of noncontact injuries, surface/epidermal injuries, and muscle-related trauma, reported on artificial fields (Meyer). Other surveys of high school and collegiate trainers have shown more serious concussions when athletes play on artificial fields that have a concrete foundation (Guskiewicz; Naunheim). Natural grass better absorbs physical impacts.
Methicillin-resistant Staphylococcus aureus (MRSA) has been recognized as a significant skin infection in the athletic population, causing minor to serious infections. MRSA is responsible for 33% of infectious outbreaks reported among competitive high school and collegiate athletes.
Cutaneous manifestations included abscess (70%), cellulitis (16%), folliculitis, impetigo, and necrotizing fasciitis. Of the infections, 90% underwent surgical drainage, whereas 27% received intravenous antibiotics.” The most common areas for infections were in the extremities: elbow, knee and forearm (Bowers 2008).
It is notable that high school football players have a fourfold increase in MRSA infections than that of the general student-athlete population. While locker room surfaces can harbor MRSA, artificial turf can as well.

The abrasive nature of synthetic turf along with sheltered MRSA in the turf and infill can make athletes and kids more vulnerable (Keller 2020). Synthetic turf requires bacteriocidal chemicals to reduce bacterial growth on fields and infections in players. These liquid turf cleaners can be toxic and may pose risks to the health of workers, children, and surrounding ecosystems. Bacteriocides have been shown to act as skin sensitizers (Hahn 2010).
Working in the tire industry exposes workers to some 50 chemicals many of which are toxic. Occupational studies in-
dicate an association of working in the manufacture of tires to bladder cancer, emphysema, esophageal cancer, larynx cancer, leukemia, liver cancer, lung cancer, multiple myeloma, pancreatic cancer, prostate cancer and stomach cancer. Most chronic diseases caused by occupational toxins don’t appear until 10 to 40 years after first exposure.
Also, if crystalline silica is used as infill, then athletes can inhale fine dust from the breakdown of this substance. The occupational literature is consistent in showing an association of silica inhalation with lung cancer and other lung diseases. Chronic silicosis, an inflammatory lung disease, can occur after 10 or more years of exposure to inhaled crystalline silica. This particular infill has not yet been tested for safety.
Cancer is another concern for athletes and children playing on artificial turf. Although there are no studies to date associating an increased risk of cancer to artificial turf, many questions remain about exposure to carcinogens on these fields.
Artificial sports fields significantly exceed temperatures of natural turf, at times 40 to 60 degrees higher than living grass. Even with moderate air temperatures, artificial sports fields become heat islands, even with moderate air temperatures, due to increased solar absorption and energy retention, as well as a lack of cooling water evaporation that natural grass provides. These higher temperatures can cause heat stroke, heat exhaustion, poor athletic performance and skin burns, making these fields potentially unusable under certain weather conditions. Irrigating the fields with water reduces temperatures, an effect that lasts for less than 20 minutes, according to research performed by Penn State Center for Sports Surface Research (Abraham 2019; Claudio 2008; NPRA 2019).
Attempts to alter turf materials to reduce surface temperatures have not been successful to date. Games can be cancelled if temperatures are too high. After an athlete suffered a heat burn from artificial turf in Utah, Brigham Young University performed a study on the artificial turf and found that the artificial turf temperature was 87°F hotter than natural grass (Williams and Pulley 2002). A temperature recorded on an artificial turf was 200°F, well above that which would cause a skin burn. Buskirk (2002) measured temperatures for 24 days on artificial turf, natural grass and in air and recorded turf temperatures that were 50°F higher than natural grass temperatures and reached 70°F higher than the air temperatures.
A University of Missouri study showed “elevated air temperatures (138°F) and elevated turf temperatures (173°F) – while adjacent natural turf temperatures were 105°F and local air temperatures were 98°F.” (Abraham 2019)
Public schools have developed heat guidelines for playing on synthetic sports fields (National Recreation and Park Association (NRPA) 2019). As global temperatures rise with climate change, the heat effects of artificial turf is an ever-increasing concern.
There are over 16,000 artificial playing turfs in the US and about 1,500 are added yearly. The synthetic turf industry recycles about one-twelfth of the 300 million auto tires that are withdrawn from use each year. An average soccer field of 80,000 square feet can use 27,000 crushed tires for infill at 4-15 pounds per square foot, equivalent to 320,000 to 1 million pounds of infill along with 40,000 pounds of plastic (Claudio 2008). Synthetic turf fields have a lifespan of 10 to 12 years. Thereafter, the material must be disposed of and typically it is landfilled.

While the narrative has been that artificial turf costs less, an analysis of the entire life cycle of artificial turf versus natural grass confirmed that using natural grass was cheaper in the long run (Daviscourt 2017). This 2017 study noted, “The results of this case study support what has previously been estimated in the literature: synthetic fields cost more to install than natural turfgrass fields… The average cost of the life-cycle analysis for natural grass was $821,000 and for synthetic infill was $1,767,000.” The University of Arkansas came to the same conclusion noting increased maintenance costs of artificial turf. The costs for artificial fields included:
• Installation Costs: More extensive subgrade work for artificial fields.
• Annual Maintenance: Additional infill, irrigation for high temperatures, chemical disinfectants, sprays to reduce static cling and odors removal of organic matter, erasing and repainting temporary lines, irrigation because of unacceptably high temperatures on warm-sunny days.
• Replacement Costs of synthetic turf vs grass.
• Disposal costs: Due to complex plastic components a special disposal fee is often needed.
Use of synthetic fields displaces natural green spaces which are also important to the health, development and wellbeing of children. The tactile and sensory benefits of real grass are lost with artificial turf. Natural green spaces can reduce stress and improve wellbeing. (Zhang 2020) notes, “It is evident that time spent in, or exposure to, green space can improve positive mood and emotions, provide a retreat from daily hassles, and reduce the risk of psychological and physiological stress in adolescents. There is also evidence of lasting mental health benefits of green space exposure in childhood.”
“Today’s children largely grow up in synthetic, indoor environments. Now, with the growing popularity of synthetic turf fields, their experience with nature will be less than ever.” (Claudio 2008) Athletes by far prefer playing on real grass (Owen 2016).
The concerns for harmful plasticizers and microplastics in artificial turn, long term effects on children’s health as well as life cycle analysis have led to policies to ban artificial turf altogether as well as ban specific toxic components. Zucarro (2022) reviewed policies on synthetic turf and wrote, “While nearly every country acknowledges the potential health risks posed by heavy metals, microplastics, PAHs, and PFAS chemicals, very few have actually implemented artificial turf and crumb rubber infill regulations and/or established adequate surveillance measures to protect those regularly exposed to the fields.”
Westport, Connecticut banned crumb rubber in 2017 and passed an “ordinance prohibiting the application of synthetic infill material on playing fields on town property.” David Brown, a Westport resident with a doctorate in toxicology from Harvard University, formerly headed up a toxicology group at the state health department. He testified in favor of the synthetic infill ban and stated, “The primary problem with turf is the off-gas from particles that contain toxic and carcinogenic chemicals. When people ingest the crumb rubber, the toxic chemicals are released in their body.”
In 2021 the European Union (EU) expanded the scope of restriction of the eight polycyclic aromatic hydrocarbons (PAHs) in infill material in synthetic turf use on playgrounds or sports fields.

Boston banned artificial turf in parks due to toxic ‘forever’ chemicals in 2022.
Holland is banning crumb rubber infill on artificial turf fields due to soil pollution under the turf.
California AB 1423 is moving through the 2023 legislature process. The bill proposed will ban the manufacturing and sale of artificial turf containing some hazardous PFAS compounds.
Turfgrass is a living organism and thus can provide environmental benefits (STMA). They cool the surrounding areas, including homes, and can help control soil erosion and run off. Carbon sequestration is another benefit. It is estimated that net carbon sequestration rates in urban lawns are between 200 and 1,800 lbs of carbon per acre per year. Research modeling of carbon sequestration by lawns indicates “lawns in the United States alone can sequester between 12.5 million and 95 million tons of atmospheric carbon dioxide per year. That’s equivalent to the annual emissions of between 2.4 million and 18 million typical passenger vehicles.” Sports fields compared to lawns or parks are not a carbon sink due to higher maintenance and operations. The University of Oregon has been researching this and recommends several management practices for irrigation, fertilization, and mowing which can help transform them into a neutral or carbon sink while also maintaining healthy turf.
There has been no proof of safety for artificial playing fields and many data gaps. There is growing evidence that the health and safety risks outweigh the benefits of artificial fields. It appears that natural grass is less expensive when a full life cycle analysis is performed. Considering that studies on the risks of long-term health have not been performed, along with absence of comprehensive data on the hazardous chemical components of artificial fields we recommend 1) not to place artificial turf on playing fields and 2) should artificial turf already be present, to replace this with natural grass.
Thank you for your consideration in this matter.
A full list of article references can be found at https://bit.ly/3LunVoL.
There is an increasing interest in green space as an intervention to improve public health. Green spaces integrated into cities provide health benefits including the abatement of air pollution and the reducing urban heat island effects. Plants are good for our health1 with both indirect effects and physical benefits. Plants need to be kept close to where people are acting as physical barriers between high emitting air pollution sources, such as traffic lanes and industry, and ideally are comprised of native vegetation.



Green spaces have positive health benefits2 and improve community wellness, “Urban green space, such as parks, playgrounds, and residential greenery, can promote mental and physical health and reduce morbidity and mortality in urban residents by providing psychological relaxation and stress alleviation, stimulating social cohesion, supporting physical activity, and reducing exposure to air pollutants, noise and excessive heat.” Urban green space improves human health3 generally.
Susan Prescott, a Professor of Pediatrics at the University of Western Australia, says that, “The evidence of the value of greenspace for health is overwhelming. From immune, psychological, physicality, microbiome, activity, social cohesion4, and even reducing crime5 in neighborhoods. It is so important for child health and development. New studies indicate it has benefits for health behavior including healthier food choices6.”
Green space exposure improves microbiome health. Exposure to urban green spaces can increase skin and nasal microbial diversity7 suggesting exposure to diverse outdoor environments may increase the microbial diversity for positive health outcomes. Green walls8 installed in office rooms in a two-week intervention increased skin Proteobacteria and Gammaproteobacteria with associated immunomodulatory effects compared with control subjects, suggesting the health benefits of green infrastructure. In the first trial with greening in daycare setting 9 , urban environmental biodiversity had demonstrated effects on the commensal microbiome and immunoregulation in children.
Increasing green spaces generally improve community health outcomes, including mental health10, “a variety of green spaces, rather than a standard configuration of a single type of green space and/or higher concentrations of a certain green space type or quality, may meet the needs of various types of green space users, especially in highly diverse and dynamic urban and peri-urban settings, and while facing the consequences of climate change.”
In one of the most famous papers on urban green space11, the researchers used mobile electroencephalography (EEG) recorders to measure participants taking a 25 min walk through three different areas of Edinburgh. In the paper, they showed evidence of systematic differences in EEG recordings and “lower frustration, engagement and arousal, and higher meditation when moving into the green space zone; and higher engagement when moving out of it”. The study provides strong
physical evidence for promoting urban green space for improving happiness.
Green space removes many types of air pollutants and can be one tool in a toolbox for managing air quality. The filtration that plants provide varies by the types of vegetation, the size of the leaves, and the age of the plants. So, it’s good to select a range of plants. Combinations of species are more supportive than monocultures as plants filter pollutants differently and can be active at different times during the year.
David Rojas-Rueda an Assistant Professor in Epidemiology at Colorado State University advises to, “Choose a variety of plants, of different species and put them in places where they require less maintenance. Choose plants with larger leaves and less pollen. Select for native plants that are specific to the region that you’re in. Put them in close proximity to people. Where people move, live, and work is where you need green spaces. Everyone needs easy access to vegetation, not on a hill far away.”
Plants need to be specific to the region that you are putting them in. Try to avoid exotic plants. Local organizations such as universities and native plant societies can provide guidance on which native plants are appropriate for your specific location. Native plant societies such as these examples, from North America12, South Africa13, and Australia14 can help you select native plants for your urban design planning. Some ornamental plants look beautiful but have lots of pollen, so selecting native plants that have low pollen can help avoid plants that can add to respiratory irritants later.
Plants in urban areas need to be integrated into the city, near people, as much as possible. For example, communities that are installing physical barriers between car lanes and either bike lanes or pedestrian pathways can substitute plant barriers for plastic or concrete barriers. In addition to filtering pollutants directly, plants also provide cover over asphalt that lowers air temperature and indirectly reduces air pollution.
Make substitutions by swapping higher polluting spaces for green spaces. You can swap cars, parking spaces, or traffic lanes for trees. Supposing you have a large flat parking lot in a city, the heat index from asphalt is high contributing to urban heat island effects and the cars increase particulate matter contributing to air pollution. If you swap every third or fourth parking space for a tree,
then you cool the space and add air filtration. Specific design characteristics for creating effective roadside vegetation barriers15 to reduce air pollution along transportation routes are that, “generally, a vegetation barrier along a high-volume highway should be tall, thick, and dense to achieve greater reductions in downwind pollutant concentrations.”
Vegetation barriers will only be effective at reducing air pollution in urban areas with limited space for planting if there’s full coverage from the ground to top of the canopy.
Whenever feasible, native species should be considered for implementing the roadside barrier. Native species will usually be more robust and resistant to local climatic conditions. Yet, there are several barriers. Tree maintenance can be expensive and sometimes it can be hard to know where to put them.
• Select native and local plants that do not need a lot of water or fertilizer. Not all cities need the same trees. Vegetation should be adapted to where you are on the planet which will reduce water, fertilizer, and maintenance costs.

• Create small parks in pockets wherever is available, such as transforming vacant lots and parking lots into green spaces.
• Incorporate green roofs and green walls wherever they’re available as a barrier between cars and transportation lanes. Substitute plastic or metal traffic barriers for plant barriers.

• Transportation rain trams have rocks in alleys, swap them for plants.
• Add plants to yards, facades, and windows. This can be supported at both a policy level and through individual contributions. Cities can support residents and industry landscaping who would like to participate in these efforts by providing urban green space plans with easy
1. https://apps.who.int/iris/handle/10665/345751
2. https://link.springer.com/chapter/10.1007/978-3-319-56091-5_11
3. https://pubmed.ncbi.nlm.nih.gov/29510520/
4. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2688343
5. https://pubmed.ncbi.nlm.nih.gov/22871378/
6. https://pubmed.ncbi.nlm.nih.gov/35382562/
7. https://pubmed.ncbi.nlm.nih.gov/32977191/
8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9021224/
9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7556828/
10. https://apps.who.int/iris/bitstream/hand le/10665/342931/9789289055666-eng.pdf
access to native plant guidance, free plants and incentives for landscaping transitions.
Stakeholders should be using green space as a tool in their toolbox to improve air quality, tools such as GreenUR and iTree can help determine where and how much green space to include in your city planning. GreenUR16 is a tool that helps quantify the health benefits of green spaces to guide policy decisions. You can use the GreenUR tool to map out green spaces in your city as a planning tool for where to add more green spaces. Policy17 is used as a driver to help invest in cities for example deciding where to increase future urban tree canopy and by how much. GreenUR can collect data to help identify where to put plants. It can also be used to quantify the health impacts of the greenspaces you currently have.
iTree18 provides peer-reviewed tree benefits estimation science from the USDA Forest Service to all types of users with free tools and support. Developed by USDA Forest Service, iTree is designed to set priorities for more effective green space decision-making19. There are substantial health benefits for communities in increasing green spaces in improving livability, health, and equity with the potential to improve biodiversity and climate resilience both now and in the future.
This article is reprinted with permission from the BreatheLife Campaign, which is jointly funded by the World Health Organization, the Climate and Clean Air Coalition, the United Nations Environment Programme and the World Bank. You may view the article online at https:// breathelife2030.org/news/green-spaces-improve-air-quality/
11. https://pubmed.ncbi.nlm.nih.gov/23467965/
12. https://nanps.org/native-plant-societies/
13. https://botanicalsociety.org.za/
14. https://anpsa.org.au/
15. https://www.researchgate.net/publication/315634025_Roadside_vegetation_design_characteristics_that_can_improve_loc al_near-road_air_quality
16. https://www.who.int/initiatives/urban-health-initiative/guidance-and-tools
17. https://www.who.int/europe/home?v=welcome
18. https://www.itreetools.org/
19. https://static1.squarespace.com/static/5bbd32d6e66669016a6af7e2/t/5eff3f4065a3745ddd0cdfdf/1593786185681/Nowak+ Feature.pdf
ClimaHealth manages a global open-access platform that was developed by the World Health Organization (WHO) and World Meteorological Organization (WMO) to serve as a technical reference point for users of interdisciplinary health, environmental, and climate science. The site represents the public face of the WHO-WMO Joint Technical Programme, bringing together the expertise and science of both organizations for the first time.
This living platform will be enhanced with new content and dynamic features in the coming months and years, with an eye towards expanding its offerings to meet the needs of users on
all sides of the climate – environment – health interface.
ClimaHealth is managed and maintained by the WHO / WMO Joint Office for Climate and Health in Geneva, Switzerland, and is supported by funding from the Wellcome Trust. Research articles are compiled and curated by the US National Institute of Environmental Health Sciences (NIEHS).
The platform may be accessed by visiting www.climahealth. info.

As students and educators in California begin the transition from summer’s end to the return to school, we health professionals and our allies are celebrating a hard-earned moment of hope that they can look forward to a future of better health and better educational outcomes. A bill, SB394 (Gonzalez) - Master Plan for Healthy, Sustainable, and Climate Resilient Schools SB-394, has passed both the Assembly and the Senate and now sits on the desk of Governor Newsom to either sign or veto. SB-394 would require the California Energy Commission to collaborate with various state agencies, and education stakeholders, to develop a Master Plan for Healthy, Sustainable, and Climate-Resilient Schools, including a baseline statewide assessment of our school facilities’ vulnerability to climate threats, their sustainability, and their contribution to harmful emissions and a policy roadmap for our schools moving forward.
That “healthy” is the first descriptor of the Master Plan is no accident. As documented by the Climate Resilient Schools Report1, climate change poses a grave threat to children’s health and that health is the pathway to learning.
These threats include:
• Extreme heat, specifically more frequent, intense, and sustained heat waves, results in illness as well as decreased cognitive function and poorer academic performance.2
• Children’s asthma is associated with 1.6 million school days lost per year from respiratory illness.3
• Wildfire smoke is up to 10x more toxic than other forms of air pollution.4
• In 2018-2019, more than 1,911 schools in California had nearly 3,893 total closure days due to wildfires, impacting 20% of all K-12 students in the state.5
• 77% of students affected by wildfires experienced stress, anxiety, and depression as obstacles to learning.6
• Children are at risk for thermal burns or heat-related illnesses from unshaded playgrounds. On a 100°F day, playground surfaces can reach over 170°F.7
Beyond these immediate threats, the Report points out that schools themselves, with their large footprint across the state, are themselves an important source of planet-warming pollution that threatens their future health. It states, “California will neither achieve nor sustain carbon neutrality unless our elementary and secondary schools are transformed into sites of climate mitigation and energy efficiency. Covering 125,000 acres of ground and encompassing 730 million square feet of buildings, the schools are a main part of the State’s infrastructure that must be activated as part of our climate solution.”
SB-394 lays out an investment strategy and a roadmap that can make every new school facilities project an opportunity to both immediately protect students and teachers from the health harms and disruptions of climate-related health hazards and protect their health longer term by reducing heat-trapping pollution from schools. Specific facilities projects include:
• Install solar and storage to ensure schools can stay open during power outages.
• Install, upgrade, maintain HVACS to improve indoor air
quality when outdoor air quality is poor.

• Reduce concrete and blacktop surfaces to reduce the “heat island” effect. Greener schoolyards improve children’s mental health.
• Transition the school bus fleet to electric to decrease toxic exhaust and decrease fossil fuel usage and greenhouse gas emissions.
• Improve the quality of school meals and thereby benefit local regenerative food systems.
• Fully staff schools with climate literate health professionals ready to respond to children’s climate anxiety.

Lisa Patel: When I was asked if I could write a report on how schools can prepare for climate change, I had two opposing reactions. My first reaction was immediate enthusiasm. As a mother and pediatrician, I had sent my daughter to a wildfire-smoked classroom in a school that had no HVAC system. As the leader of the Medical Society Consortium on Climate and Health8, I know that the voice of health professionals can make a difference, especially now that wildfires, heat waves, floods and droughts have catapulted health concerns to the center of the climate conversation. My second reaction was the paralyzing realization that I knew next to nothing about how schools can best prepare for what climate change is bringing! I realized at that moment that I needed to invite anyone who cared about this issue to write the report together. The result was a large working group of teachers, students, health professionals, engineers and others who could help build a combined vision for what a climate resilient school would look like.
The Climate Resilient Schools Report was created, and with it a coalition to shape and advance SB-394, the legislation that would transform its recommendations into action initially led by Undaunted K129 and Ten Strands10. That’s when I reached out to Climate Health Now to see if this was an issue their health professional advocate network would like to take on.
Amanda Millstein: Climate Health Now is the California state nonprofit group affiliated with the Medical Society Consortium on Climate and Health. When Lisa reached out about the report, we were excited to join this large and diverse coalition that has grown to 19 organizations. We used the Report as a centerpiece for setting up meetings to educate policymakers, marshaling support with sign-on letters to frame school resiliency as a critical health issue and overcoming legislative hurdles.
We activated our members’ voices in advocacy as part of the broader coalition working to advance the bill. Close to 170 CHN members signed a letter to Governor Newsom asking for a budget allocation of $10 million for the Master Plan and generated 60 emails to the Chair of the Assembly Appropriations Committee. Members also attended legislative visits with the offices of key Senators and Assemblymembers to speak to the importance of the bill for protecting health and promoting equity. One member, Dr. Mike Harris, a general pediatrician, contributed to a press release about the importance of the bill11
We see a number of key aspects of the report itself, and the process of its creation, as key to its positive influence on state policymakers and SB-394’s success. These seven “success factors” can be helpful in guiding other climate and health advocacy efforts in CA as well as other school-focused efforts in other states.
1. Focus on Children’s Current and Future Health. When we health professionals talk about children’s health, we are talking as professionals about our work, of course, but we are often also talking about our own children. Not only does this resonate with our deeply-held feeling of responsibility for looking out for our children, but also the unavoidable reality that our children will inherit the impacts of whatever future climate we create. Moreover, even with the increase in extreme weather events afflicting our state, we know that framing climate as a health issue also shifts thinking about climate from an abstract future to the here and now.
2. Facts Matter. What makes the climate and health movement strong is not just the implicit trust that policymakers and the public place in health professionals, but also their assumption that health professionals can support their assertions and recommendations with facts. The Asserting that there are health harms of climate change that our children are suffering now may be intuitive, but buttressing those assertions about that reality with authoritative studies and transparent methodologies is what creates confidence and increased buy-in from all stakeholders.
3. Teams Win Together. Improving health outcomes for children is the big thing everyone cares about, but it’s not the only thing people care about. School superintendents care about educational outcomes and ensuring that they have the trained personnel and other resources to translate policy demands into achievements. Environmental advocates care about ensuring that students and teachers have the level of eco-literacy they will need to carry into a future where dealing with climate will inevitably move toward the center of our economic, social and political lives. Community leaders care about setting priorities that account for schools that have been chronically under-resourced by traditional funding mechanisms. Legislative champions care about getting credit for what they’ve already done and being able to explain the economic and social ROIs for their communities. All of these stakeholders must be included in preparing the report and in advocating in coalition to state legislators for passing the bill that can make its recommendations real.
4. Lead with a Positive Vision. The title of the Report was not “A Master Plan to Address the Dire Climate Health
1. https://static1.squarespace.com/static/635dbc6808cab54e82a25127/t/640f57089a49a966b5803dcb/ 1678726934033/ Climate-Resilient+California+Schools
2. https://forhealth.org/Harvard.Schools_For_Health.Foundations_for_Student_Success.pdf
3. https://www.cdc.gov/pcd/issues/2012/11_0312.htm

4. https://publications.aap.org/pediatrics/article/147/4/ e2020027128/180791? autologincheck=redirected
5. https://disasterdays.calmatters.org/california-school-closures
Threat to Our Children.” It was “Climate Resilient California Schools.” Its first pages illustrated, in concrete terms, how a resilient school would effectively deal with the reality of the climate threat. Schools, powered by renewable energy generated and stored on site, will remain open when extreme weather forces cuts in power. School ventilations and filtration systems will provide clean cool air to students and their families when wildfire smoke fouls the air. Children will be able to play on tree-sheltered school yards with permeable, heat-deflecting surfaces even when temperatures soared. Students will be given the education they need to cope with an uncertain future.
5. Create A Cog, Not A New Wheel. California has already made a number of investments in clean energy and other programs to achieve its ambitious goals for net-neutrality by 2045, both in schools and in communities. The report was careful to celebrate these investments and programmatic achievements and point to how the master planning process investments would act to augment and align these programs, not duplicate or ignore them.
6. Don’t Shy Away From What’s Needed. On the other hand, the report makes a brutally honest assessment of an aging school infrastructure that was constructed for a milder, cooler climate. An incremental, piecemeal or one-time booster-shot approach to funding might be seen as politically more feasible, but fundamentally dishonest in the face of the challenge and, frankly, in the timeline already set for achieving net neutrality. The report makes clear that clear that there will be a need for substantial new investments and for scaling up current investments, if the goals are to be achieved.
7. Map Out the Key Steps. Social change experts have long noted that, especially when change is hard, it’s important to clearly map the immediate and short-term steps to help people and organizations move from accepting an idea to taking action. Moveover, since all good planning involves priority setting, goal setting and milestone tracking, the lack of many key state-wide infrastructure status benchmarks is called out as an immediate priority to address. The good news is that these first-step planning recommendations and measurement priorities were included in SB-394.
If you’ve read this story to its conclusion and have taken its message to heart, please know that we welcome you to join Climate Health Now by visiting our website www.climatehealthnow.org. None of us can do everything but each of us can do something – and Climate Health Now is here to help you find your place in helping to solve the climate health crisis in order to protect all those we love. This is just the beginning. We have much more to get done!
6. YouthTruth (2021)
7. https://www.sciencedirect.com/science/article/pii/ S0360132322007314?via%3Dihub
8. https://medsocietiesforclimatehealth.org/
9. https://www.undauntedk12.org/
10. https://tenstrands.org/
11. https://tenstrands.org/press-releases/as-extreme-weather-wreaks-havoc-for-students-california- advocates-call-for-amaster-plan-for-climate-resilient-schools/
Have you ever wondered how city policies impact the health of your patients?
The County of Santa Clara Public Health Department tracks this! Cities are critical to health. Their design plays an integral role in overall wellness, including nutrition, safe spaces to play and be active, access to healthcare services and resources, and how much or how little people are exposed to smoke, pollution, and harmful chemicals.
In November 2016, the County of Santa Clara Public Health Department launched its Healthy Cities Program1 to encourage policies that help prevent and address conditions that increase risk for chronic disease and injury. As you know, chronic diseases affect quality of life, increase healthcare costs, and increase risks for negative outcomes of other illnesses.
A key feature of the Healthy Cities Program is the annual release of its dashboards, recognizing cities for their actions to improve the health of their residents, and your patients. This dashboard, which you can view at sccphd.org/healthycities displays the status of each of the county’s 15 cities and towns in adopting plans and policies across nine categories focused supporting physical activity, access to healthy foods and beverages, preventing and reducing exposure and access to tobacco products, violence prevention, housing and built environment, advancing racial equity, and climate change mitigation and adaptation.
Initially there was some trepidation in having a County program evaluating its city partners. Elected officials and staff ultimately expressed appreciation for the ability to inform their decision making and policy planning, and to tout the public health policies they had implemented. Public Health consults with cities and community partners to assess new recognition opportunities and encourage the adoption of new promising public health policies.
new construction.
• Adopt and implement Climate Action Plans (CAPs) with measures to address racial inequities.
• Adopt hazard mitigation plans and prioritize the needs of vulnerable populations.
• Adopt plans to identify—with resident input— community facilities for use during climate events (like wildfires, poor air quality, and extreme heat).
• Adopt urban forestry plans.
What does this mean for a city’s status on the dashboard? Public Health’s Healthy Cities and Climate and Health programs3 set aside funding from the Centers for Disease Control4 to support nonprofit and community-based organizations and cities to implement projects and policies furthering climate change adaptation and readiness. Cities awarded funding can see their status as it improves! Work on funded projects and policies will begin in 2024 and continue throughout the year.
If you’d like to be involved or kept informed of Healthy Cities updates and Public Health efforts, scan the QR code and sign up for our mailing list.

You can always find more information on the Health Cities program by visiting www.sccphd.org/healthycities or emailing Teddy Daligga at edward.daligga@phd.sccgov.org.
Climate change mitigation and adaptation is one of the recent additions, encouraging cities to:
• Adopt Transportation Demand Management2 strategies.
• Allow for telework of eligible employees.
• Adopt ordinances to reduce and eliminate use of natural gas in
The Healthy Cities Dashboard (pictured below) awards medals to cities across nine categories, based on criteria outlined on the Healthy Cities webpage. 1.
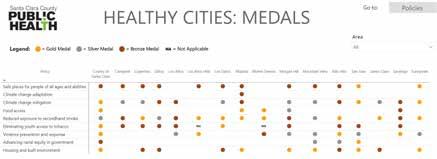
The World Health Organization has declared climate change “the single biggest health threat facing humanity” (World Health Organization, 2021). The health risks of climate change are and will be felt disproportionately by the most vulnerable and disadvantaged in society including women, children, ethnic minorities, poor communities, migrants and displaced persons, older populations and those with underlying health conditions. In June 2022 the American Medical Association (AMA) adopted a new policy declaring climate change a public health crisis (AMA Adopts New Policy Declaring Climate Change a Public Health Crisis, 2022). The AMA additionally called for rapid implementation and incentivization of clean energy solutions and significant investments in climate resilience through a climate justice lens.
In 2021, over 200 medical journals released an unprecedented joint statement urging world leaders to cut heat-trapping emissions in order to avoid “catastrophic harm to health that will be impossible to reverse” (Sommer, 2021). An editorial in the New England Journal of Medicine encouraged health professionals to
aid in the transition to a sustainable, fairer, resilient and healthier world (Atwoli et al., 2021).
Climate change is affecting human health in a variety of methods detailed below:
Extreme Heat: can directly lead to hyperthermia and heat stroke as well as worsening preexisting conditions such as heart and lung disease, diabetes, asthma and kidney problems;
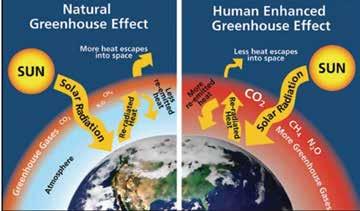
and is associated with increased visits to the emergency room. Can also lead to flare ups of migraines, rosacea, lupus, rheumatoid arthritis, hypertension and multiple sclerosis. Additionally patients taking diuretics, beta blockers, antipsychotic drugs, anxiolytics and antidepressants may have impaired resistance to heat stress and may interfere with heat regulation. Medications meant to be stored at cooler temperatures may become unstable during heat waves. Studies have also found a relationship between increased temperature being associated with aggression, violent crime and accidental injuries.
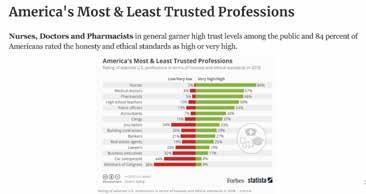
Reduced Air Quality: is known to increase the incidence of respiratory illness including asthma, bronchitis, chronic obstructive pulmonary disease (COPD) and pneumonia. Ozone pollution is also worse in hotter temperatures. In fact air pollution kills 10 million people per year, which is more than smoking. Majority of those deaths are particulates causing cardiovascular disease – heart attacks and stroke (Milne, 2019). In fact, fossil fuel air pollution is responsible for 1 in 5 deaths worldwide, especially in developing countries such as Indonesia, China, Pakistan and India (Fuller et al., 2022).
Drought: results in reduced water quantity and quality and damages yields of crucial crops such as wheat, corn and soy. Drought directly impacts 55 million people every year.
Wildfires: can directly cause burns and traumatic injury as well as asthma/COPD exacerbations. Smoke from wildfires in California has been shown to infiltrate the lungs and bloodstreams of people as far away as Ohio and Texas. We will likely see longer and worse wildfire seasons in the future.
Vector Borne Diseases: mosquitos, ticks, fleas and rodents all exhibit sensitivities to weather and we are already seeing
higher rates of Dengue, Yellow Fever West Nile Virus and Valley fever cases due to climate change. In addition, studies have shown a higher rate of surgical site infection with warmer weather (Anthony et al., 2017).
Extreme Events: Due to climate change we are experiencing an increased frequency and intensity of extreme weather events such as hurricanes, large storms, extreme cold which all can lead to increased incidences of direct trauma, drowning due to flooding, hypothermia and frostbite.

Increased Allergens: as heavier rain has become more frequent and winter more milder with less frost, pollen season has lengthened resulting in increased frequency and severity of allergic illness and asthma complications. Additionally, elevated carbon dioxide increases growth of allergen-producing ragweed, grasses, trees and fungi. Heavy rainfall and flooding also causes home dampness leading to indoor mold and fungal growth.
Mental Health: although sometimes overlooked, climate change including extreme weather events can lead to shock, PTSD, anxiety, stress, depression and suicide ideation. Heat can directly fuel mood and anxiety disorders, schizophrenia, interpersonal aggression and violence. Air pollution has also been linked to increased anxiety, lower happiness and life satisfaction as well as use of mental health services (Clayton et al., 2021).
Effects on Food Supply: hotter temperatures increase risks of bacterial growth on crops during growth, transport, handling and storage. Fish and seafood are more likely to become contaminated by marine water with higher bacterial growth and harmful algae bloom. Higher carbon dioxide levels also reduce the nutritional value of many staple crops such as wheat, rice and potatoes by decreasing protein content and micronutrients such as calcium, zinc and iron. Drought will also reduce arable land. Beef production is notoriously associated with food-related emission of greenhouse gasses.

The elderly population is more sensitive to extreme temperatures and are at a much greater risk of dying during heat waves. Pre-existing health conditions also make the elderly more susceptible to cardiac and respiratory impacts triggered by air pollution. Additionally, the elderly may be least able to evacuate during emergency situations.
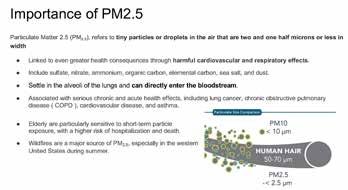
According to UNICEF, up to one billion children are at an extremely high risk from climate change (Frost, 2022). Children are in a constant state of growth and development and are: 1 –physically more vulnerable to floods, drought, severe weather and heatwaves; 2 – physiologically more vulnerable to toxins such as from air pollution; 3 – more at risk of death from diseases exacerbated by climate change such as malaria and dengue; and 4 – climate and environmental degradation exposure at a young age can result in a lifetime of lost opportunity.
Additionally, infants are less able to regulate their temperatures and are at higher risk of death from heatstroke. If it is too hot to play outdoors and exercise, there is an increased risk of being overweight and obese. Extreme heat can also make learning harder and increased pollen can limit productivity at school due to allergies.
Exposure to heat during pregnancy increases the risk of infants born with congenital heart disease, preterm birth, low birth weight and infant mortality. Pregnant women are also at higher risk of dehydration (Rudolph et al., 2016).
Marginalized communities are disproportionately affected by climate change due to a lack of resources and poverty. This is despite wealthier people having a per carbon footprint 25% higher than low-income residents (Tummala, 2020). Black individuals are 2.5 times more likely to experience health related mortality compared to their White counterparts. Both Black and Latinx communities have been found to breathe air that is 46% and 39% more polluted than Whites. Formerly redlined neighborhoods are on average 2.6 degree Celsius hotter than non-redlined neighborhoods (United States Global Research Program, 2016).
Additionally, outdoor and migrant farm workers exposed
to higher temperatures are at higher risk of heat-related injury and occupational traumatic injuries in addition to exposure to pesticides and other farm chemicals that lead to cancer and other physical ailments. Heat also leads to decreased productivity of those who work outdoors.

A survey in 2021 reported that 78% of adults in the US are either very (48%) or somewhat (31%) concerned about climate change (Clayton et al., 2021). 67% of adults aged 18-23 are concerned about the impact of climate change on their mental health and people of color express equal or greater concern about climate change than White individuals.
Most people perceive themselves, their families, and people in their community to be at less risk from climate change than people who are spatially (e.g., in developing countries) or temporally distant (e.g., future generations). Despite present, serious and growing impacts of climate change on health, most Americans do not accurately assess these risks, especially for themselves, their families, and people in their community. Only 27% of Americans can accurately name one or more specific type of health harm caused by climate change, and only 25% can identify any disproportionately affected populations (Kotcher et al., 2021).
There is a growing realization of the impacts of climate change among health professionals and Americans report that they trust health professionals more than any other source of information which presents a rare opportunity. Healthcare professionals are uniquely positioned to advance the message that climate solutions are a health priority and will provide enormous health benefits. In 2021, 68% of adults in the United States said they trust health professionals as a source of climate change information (Krygsman & Speiser, 2016).
Medical professionals have unparalleled assets in terms of their knowledge, skills, credibility, and access to important audiences—including policy makers, government officials, educators, patients, and the general public—both in and beyond their own community. They are aware of and concerned about the health impacts of climate change and have called for integrating climate advocacy as part of their professional responsibility.
Health professionals have a duty to help the public prepare for the health risks posed by our changing climate and to promote climate solutions that also deliver health benefits for patients, their children and future generations as well as those disenfranchised. When health professionals take the lead, patients will gain a better understanding of the significance of climate change when considering our health.
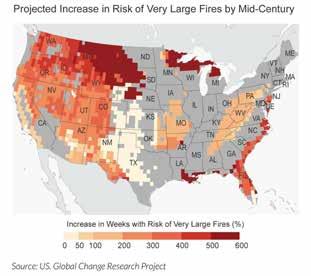
1. Encourage patients to walk and cycleUsing “green” transportation methods benefit both the patient’s cardiovascular health and the quality of the air they breathe.
2. Reduce meat consumption - Both farming and meat production are major contributors to global warming and reducing consumption will benefit cardiovascular health as well.

3. Encourage air conditioning - Sheltering in cool places like a cooling center or air conditioned shopping center or public building to reduce risk of heat-related health consequences.
4. Stay hydrated - Drinking plenty of cool water and avoiding dehydrating drinks such as alcohol and caffeinated beverages can help patients keep their bodies cool. Using cool water for showers and baths can also help.
5. Never leave vulnerable persons unattended - Children, elderly people, and pets can suffer fatalities when alone in homes without air conditioning and particularly in vehicles, even if the windows are ‘cracked’.
6. Inform patients about the risks of some medications and heat Some medications increase the risk of heat illness, such as psychotropic medications, diuretics,
tranquilizers, and some medications for Parkinson’s disease. Other medications, such as insulin, may lose their effectiveness with very high temperatures.
7. Encourage individuals to check in on neighbors, friends and relatives - During extreme heat events encourage patients to make sure they have a “heat buddy” who will check in on them.
8. Advise patients with pre-existing respiratory illness - Patients predisposed with asthma or COPD should be checking air quality levels during extreme heat events and limiting outdoor air exposure when air quality is poor.
9. Connect patients to resources - financial support is available for coping with heat.
10. Become aware of local ‘green’ grants

Especially informing those who are struggling financially. Patients can stay alert for grants for home insulation or bus passes in their area.
How health professionals can address sustainability with their patients and as individuals:
• Choose a fuel-efficient or electric vehicle and keep your car well maintained, including properly inflated tires.
• Decrease the amount you drive by using public transportation, riding a bike, walking, or telecommuting.
• Ask your electricity supplier about options for purchasing energy from renewable sources.
• When purchasing appliances, look for the Energy Star label and choose the most energy efficient model. Energy Star light bulbs use ~90% less energy than standard bulbs, last 15 times longer, and save ~$55 in electricity costs over their lifetimes.
• Space heating is the largest use of household energy (32%). Ensure that your house is properly sealed by reducing air leaks, installing the recommended level of insulation, and choosing Energy Star windows.
• Become a champion within your own health system for the White House-HHS Climate Sector pledge with a commitment to lowering greenhouse gas emissions and building more climate resilient infrastructure.
• Advocate local, state and federal governments for policies and legislation promoting climate health. Physicians can meet with their legislators, write policy relevant media and testify at hearings to benefit public health.
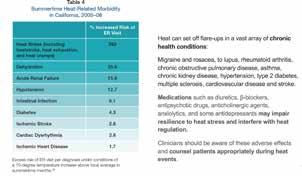
Greenhouse gas emission reduction policies include improved respiratory health from better air quality and reduced heart disease from walking and using other environmentally friendly active transportation. One study estimated that increasing safe active transport and use of lower-emission vehicles in London could reduce heart disease burden by 10-19%, cerebrovascular disease burden by 10-18%, dementia by 7-8%, and depression by 4-6% (Crowley, 2016). Additionally, there are many actions
that individuals can take to reduce their greenhouse gas emissions; many involve energy conservation and also save money.
Climate change is a genuine, human-caused concern. It is essential that we recognize the impact of climate change on our patients’ health. Unless aggressive, concerted efforts are made to curb greenhouse gas emissions, irrevocable damage could be done, including negative effects on human health, such as elevated risk for cardiovascular and respiratory diseases, food and water insecurity, infectious disease, and compromised mental health.
Physicians, both collectively and individually, are encouraged to take action by adopting lifestyle changes that reduce environmental impact, increasing the environmental sustainability of their practice and the broader health system in which they work, educating the public on the potential effects and health consequences of climate change, and advocating for policies in their own countries and globally to reduce greenhouse gas emissions and address the health effects of climate change We need to start taking action now to protect the health of our community’s most vulnerable members—including children, seniors, people with chronic illnesses, and the poor—because our climate is already causing physical and mental harm.
This is a potential “win-win” situation since dealing with climate change will benefit our health and the environment. By informing patients and the public of the human health threat

posed by climate change, physicians can help depoliticize the issue and encourage cooperation in the development of necessary adaptation and mitigation strategies.
Climate change–related coursework should be incorporated into medical school and CME coursework so that physicians can accurately articulate the immediacy of climate change and its potential effects on human health. The issue of climate change is often positioned as a purely environmental, economic, or political one; however, climate change will have severe consequences for human health and physicians can play an important role in raising awareness.
For a full list of references, visit www.sccma.org.
CMA House of Delegates Meeting
October 21-22 | LA Live, Los Angeles
Information available at www.cmadocs.org/hod-2023
This year’s California Medical Association (CMA) House of Delegates (HOD) meeting will take place on October 21-22, 2023 at JW Marriott LA Live. Major issues selected for this year’s agenda include Consumer Health Technology/Artificial Intelligence, Office of Health Care Affordability, and Climate Change. We look forward to this year’s lively debate as physicians continue to advocate to improve the practice of medicine.
SCCMA Annual Meeting & Election

Tuesday, November 14 | 6:30-8:00pm | Virtual Register at https://bit.ly/3Zr1hDN
Join us for the SCCMA Virtual Annual Meeting & Ratification of 2024 Council Slate of Candidates as we elect our 2024 SCCMA Officers and Councilors.
SCCMA Annual Awards Gala
Friday, December 8 | 6:00-9:00pm | The Westin Hotel San Jose Register at https://bit.ly/3PJhQr0
SCCMA invites you to attend our 2023 Awards Gala which brings together SCCMA leadership, members, supporters, advocates, and partners to introduce our new president, Gloria Wu, MD, and celebrate our outgoing president, Anlin Xu, MD. We will also honor those who are making a difference in medicine and the community. Join us to reconnect and see friends and colleagues at this annual event. Members may bring a guest. Come to enjoy networking and dinner for our last social event of the year.
Questions? Contact Angelica@sccma.org
For sponsorship inquiries or to purchase a full table(s), please email Erin@sccma.org

If you are a health professional, please take part in the American Lung Association’s Health Professionals for Clean Air and Climate Action community and sign up for our monthly newsletter at Lung.org/climatechangeshealth
98% of Californians live in areas with unhealthy air
Medical and healthcare voices are critical when calling for stronger policies to address air pollution and climate change.




