






SCCMA is a professional association representing over 4,500 physicians in all specialties, practice types, and stages of their careers. We support physicians like you through a variety of practice management resources, coding and reimbursement help, training, and up to the minute news that could affect your practice. The Bulletin is our quarterly publication.

Santa Clara County Medical Association
SCCMA OFFICERS
President | Gloria Wu, MD
President-elect | Fahd Rahman Khan, MD
Secretary | Randal Pham, MD
Treasurer | Shahram Gholami, MD
Immediate Past President | Anlin Xu, MD
VP-Community Health | Santosh Pandipati, MD
VP-External Affairs | Christine Doyle, MD
VP-Member Services | Sam Wald, MD
VP-Professional Conduct | Lewis Osofsky, MD
SCCMA STAFF
CEO/Executive Director | Marc E. Chow, MS
Director of Membership & Programs | Angelica Cereno
Governance & Advocacy Associate | Emily Coren Facilities & IT Manager | Paul Moore
SCCMA COUNCILORS
El Camino Hospital of Los Gatos | Jaideep Iyengar, MD
El Camino Hospital – Mountain View | Carol A. Somersille, MD
Good Samaritan Hospital | CK Park, MD
Kaiser Foundation Hospital - San Jose | Veena Vanchinathan, MD
Kaiser Permanente Hospital | Reena Bhargava, MD
O’Connor Hospital | OPEN
Regional Medical Center | Raj Gupta, MD
Saint Louise Regional Hospital | Kevin Stuart, MD Santa Clara Valley Medical Center | Patricia Salmon, MD Stanford Health Care/Children’s Health | OPEN
Managing Editor | Emily Coren
Production Editor | Prime42 – Design | Market | Host
Opinions expressed by authors are their own, and not necessarily those of The Bulletin or SCCMA. The Bulletin reserves the right to edit all contributions for clarity and length, as well as to reject any material submitted in whole or in part. Acceptance of advertising in The Bulletin in no way constitutes approval or endorsement by SCCMA of products or services advertised. The Bulletin and SCCMA reserve the right to reject any advertising.
Address all editorial communication, reprint requests, and advertising to:
Emily Coren, Managing Editor
700 Empey Way
San Jose, CA 95128
408/998-8850
Fax: 408/289-1064
emily@sccma.org
 Gloria Wu, MD
SCCMA President
Gloria Wu, MD
SCCMA President
I am continuously inspired by the dedication, resilience, and unwavering commitment each of you demonstrates towards the noble cause of healthcare. This profession is more than a career; it is a calling that requires our utmost dedication, particularly during these unparalleled times. Rest assured, the Santa Clara County Medical Association (SCCMA) is dedicated to providing you with essential tools and resources. We encourage you to regularly visit our website and review our e-blasts, News Bytes, and Bulletin to stay informed about the numerous opportunities to engage with us throughout the year.
On February 10th, we embraced the virtual Interim Session of the California Medical Association (CMA) House of Delegates (HOD). It was a pleasure to see several of our District VII Council Members join us at SCCMA for a communal viewing. The session spotlighted three critical areas:
and Long Health. This event was a unique opportunity for learning and networking.
We are pleased that a number of you will be joining us on April 10th in Sacramento for the CMA 50th Legislative Advocacy Day. We anticipate joining more than 400 of our colleagues across the state to provide our elected officials with information about the opportunities and challenges that we face as physicians regarding the practice of medicine.
This profession is more than a career; it is a calling that requires our utmost dedication, particularly during these unparalleled times.
• Office of Health Care Affordability
• Consumer Health Tech and AI
• Climate Change
As pioneering physician leaders in the heart of Silicon Valley, we are enveloped in a culture of startups and healthcare innovation. Many of our members are actively integrating various healthcare technologies into their practice. In this spirit, on February 17th, SCCMA proudly hosted our first Hybrid AI, Healthcare, and Innovation event, featuring distinguished speakers from IBM, e-L ōvu, Blue Cross Blue Shield, Truss Health, Blink Pad,
SCCMA Environmental Health has been actively engaged in advocacy for issues related to climate change, air quality, water quality and toxics including sending several letters opposing the installation of artificial turf in public spaces across a variety of cities in Santa Clara County. We will be focusing on topics that fall into the category’s climate change, air quality, water quality and toxics moving forwards. Please email emily@sccma.org if you are interested in joining these efforts.
We will continue to engage with elected officials and a variety of county agencies to develop and strengthen SCCMA’s voice within our community.
With the success from last year, we are excited to be continuing our monthly series in providing additional insights to solo, small, and medium medical practices on a variety of key topics every third Wednesday of the month. The first Saving Private Practice (SPP) Webinar will be on Wednesday, March 20 with a presentation from the Presi-
We are in the process of launching the “Joy of Medicine” initiative, a renowned program designed to help physicians rediscover the joy in practicing medicine
dent of Practice and Liability Insurance, Debra Phairas, to speak on “How to Manage Your Manager (for Physicians).” The series is open to all physicians and their office managers! Please register online at sccma.org.
We are thrilled to offer our members ongoing access to our quarterly book club. We kicked off with our inaugural book on 09/06/23 with “Doctors and Friends” by Kimmery Martin, MD. Register for our next selection, “What Looks Like Bravery” by Laurel Braitman, PhD. “What Looks Like Bravery” is a hero’s journey for our times that teaches us that hope is in a form of courage. Book Club will meet in-person at the SCCMA Office on March 27 at 6:30 PM. The author will join in via Zoom to discuss the writing process and have discussion about the book. All registrants will receive a copy of the book for free. Please
register online at sccma.org.
Your well-being is paramount to maintaining the capacity to practice medicine and care for patients. This summer, we are excited to host our second annual Wellness Retreat. We are in the process of launching the “Joy of Medicine” initiative, a renowned program designed to help physicians rediscover the joy in practicing medicine. This program will offer access to a wealth of resources, including educational materials, advocacy, events, and services.
We eagerly anticipate engaging with you throughout the year. Whether you’re in private practice, corporate, or group practice, please know that we are here to support you in any way possible.


The Medical Board of California will review best practices for physician health programs, a move advocated by the California Medical Association (CMA) to better support physicians facing mental health challenges, burnout and substance abuse. CMA supports increasing physician wellbeing by reducing stigma to seeking care and increasing access to supportive, confidential services as being in the best interest of both patients and physicians.
The California Medical Association (CMA) Governance Reform Technical Advisory Committee (GTAC) is hosting two townhall-style meetings for all CMA members. These meetings are an opportunity to discuss upcoming changes to governance policies currently under development or consideration.
Whether you’re new to CMA and have never participated in governance activities or are a seasoned House of Delegates (HOD) veteran, your involvement will help steer the future of our organization. These townhalls are your chance to learn more about CMA’s governing structure, share your ideas and get answers to your questions.
CMA filed a lawsuit against the California Department of Managed Health Care (DMHC) for the agency’s failure to enforce California’s prompt payment regulations in implementing Senate Bill 510 (Pan). This legislation, sponsored by CMA in 2021, requires health plans and insurers to reimburse physicians and other health care providers for certain COVID-19 services retroactive to March 4, 2020. However, DMHC put out fundamentally flawed guidance that effectively relieved plans of some of their legal payment obligations, resulting in significant delays and reductions in reimbursement.

CMA is sponsoring the Physicians Make Decisions Act (SB 1120), which requires that physicians be the ones to make final decisions on what kind of treatments patients should receive, rather than artificial intelligence (AI).
In recent years, health plans have increasingly relied on AI to streamline the processing of claims and prior authorization requests. SB 1120—authored by Senator Josh Becker (D-Menlo Park)—requires licensed physicians to supervise treatment and coverage decisions made by algorithms.
While AI is becoming an important tool in diagnosing and treating patients, it should not be the only factor in determining if or what kind of health care a patient receives. The Physicians Make Decisions Act acknowledges that algorithms cannot replicate the nuanced decision-making process of a physician, ensuring that patients receive fair and appropriate coverage decisions. By reintroducing human oversight, SB 1120 seeks to uphold the integrity of the health care system and prioritize patients’ well-being above all else.
SCCMA celebrates all California Women Physicians, past and present, including our current president, Dr. Gloria Wu, and past president, Dr. Anlin Xu.
SCCMA has various committees such as Environmental Health, Bioethics, Physician Wellbeing, and Membership, that do focused work within the Association. If you want to get involved in one of these committees, please call Director of Membership and Programs, at (408) 998 – 8850 x3012.

Josh Markowitz, MD, RDMS, FACEP, SAIUM has been a member of the Santa Clara County Medical Association for more than eleven years. From 2019 to 2022 he also served on the SCCMA Board as the physician delegate from Kaiser Permanente’s Santa Clara Hospital and was a Delegate to CMA House of Delegates. Josh Markowitz joined Santa Clara Kaiser Permanente in 2012 as an Emergency Medicine physician.
Dr. Markowitz received his undergraduate and medical degrees from Brown University where he was elected to the Sigma Xi Honor Society and became the recipient of the Outstanding Student in Emergency Medicine Award from the Rhode Island Chapter of the American College of Emergency Physicians. He attended Yale New Haven Hospital for Residency in Emergency Medicine and completed his fellowship in Emergency Ultrasound at Drexel University College of Medicine. He then joined the faculty at the Albert Einstein Healthcare Network in Philadelphia where he oversaw Emergency Ultrasound education and eventually served as the Director of Emergency Ultrasound. After 3 years, he returned home to California and joined Kaiser Permanente.
At Santa Clara Kaiser, he now serves as the Assistant Lead for Disaster Medicine and serves on the Regional Emergency Management Group. He has also been the EMS Liaison for Santa Clara Kaiser Hospital for the last 8 years. During this time, to help improve performance and provide greater access to education for local EMS crew members, he started a regular free EMS class, which he continues to teach. This quarterly class has provided education to our local EMS, Fire and Police crews over the last 8 years. During this time, he has received 2 grants from Santa Clara County Emergency Medical Services to help purchase equipment for these classes, he has been highlighted in multiple Kaiser publications as well as in the Mercury News for his work, and he was awarded the 2022 Outstanding Contribution in Medical Education by the Santa Clara County Medical Association.
Despite his love for Emergency Medicine, Dr Markowitz acknowledges that the field is struggling. After the COVID-19 Pandemic, EM physicians are tired and over worked. Doctors are retiring early, hospitals are having trouble hiring new doc-
tors and EM Residencies are having trouble filling spots. With patients flocking to the ED because clinics are full and are experiencing increased wait times because hospitals are overloaded, it created a perfect storm for the field. This has also led to delays with ambulances, a process that he is trying to address currently with his hospital administration.
Despite its current issues, Emergency Medicine has provided Dr Markowitz with the opportunity to pursue many different interests. Through both of his roles in Disaster Medicine and Emergency Management, he has had the opportunity to work as a physician for the America Cup trials and finals in 2012 as well as working for the NFL Super Bowl 50 events throughout the Bay Area. He has participated multiple times in the Urban Shield full scale disaster exercises and served as an instructor for Ultrasound and Disaster Medicine at the 2018 Kaiser Permanente Emergency Medicine Conference. On the more academic side, he has also served as a journal reviewer for The Permanente Journal and WestJEM and was recognized in 2022 as a Change to High Quality Peer-Reviewer.

seen them many times in concert and have attended many DMB shows in the bay area with other Emergency Medicine friends from work.
When he leaves the hospital, Josh Markowitz enjoys being active and spending time with his family and friends. He enjoys playing basketball, ran his first half marathon a few years ago and will soon be trying for his 3rd degree blackbelt in TaeKwonDo. He loves skiing and sailing, when time permits. He loves to travel and spend time with his beautiful wife and 3 wonderful boys.
What do you love most about practicing in Emergency Medicine?
As an Emergency Medicine physician, I have the opportunity to constantly see and do new things. When I walk into the ED, I know that at any point, a patient could come through that door with some new diagnosis I have never seen before, an incredible story that is amazing to listen to or possibly a patient that is fighting between life and death. It has also given me the opportunity to be involved in areas outside of the ED, such as providing medical care during the America’s Cup Races, Gravity Games, Air Shows and for the NFL Super Bowl 50 Experience. I was always intrigued with radiology, EMS, Disaster Medicine and many other topics, and Emergency Medicine has provided me with the opportunity to include them all in my practice and to not just have to pick and choose.
If you weren’t a physician, what profession would you like to try?
Had I not chosen to enter medicine, I might have considered being an architect. I have always loved construction and building things with my own hands. I enjoy the process of designing and understanding the difference in the material used. I think it would be fascinating researching how to make them more energy efficient, designed for better access and with reduced waste.
What is your favorite music artist/band?
One of my favorite bands would have to be Dave Matthews Band. I remember seeing them for the first time in high school at Shoreline as part of the H.O.R.D.E. festival. The concert was great, and it started my interest in DMB. Since then, I have
What is the most important thing you learned in medical school or residency?
When I was 16 years old, my father died suddenly. While this was devastating, the interactions with our ED Physician that day made the situation even more difficult. From this, I became interested in medical ethics and how to interact with patients and families. As a medical student, I watched how other Residents and Attendings interacted with their patients and how patients responded to this. But it was in my third year of medical school, during my first rotation on medicine, with my very first patient, that I learned what to do. And it was not my colleagues or instructors who taught me, but my patient. She had a terminal illness and had come into the hospital to die comfortably. I requested her to be my patient and I spent the few days that she was with us, sitting with her, talking to her and listening to what she had to say. She did not need some expensive tests or a top-rated physician, she wanted someone to listen to her story. And from this patient, I truly learned that every patient has a story, every patient wants to be listened to and acknowledged. And from this woman, I learned that the medical care I was able to provide as a physician was only part of my duties, the rest was to hear what they had to say.
Why are you a SCCMA member?
I joined SCCMA because I joined Kaiser Permanente, and they pay the dues. Then I came to a meeting because a colleague and friend, Tom Dailey, invited me to do so. However, I became involved with SCCMA and joined the board because I saw how passionate they were and what they wanted to do for us. This organization works tirelessly to provide incredible educational opportunities for the community and the physicians it serves, while fighting to make changes to local and national policies. There are many members from the SCCMA who have gone on to serve in leadership roles for the CMA, AMA and other organizations. This group is passionate about what it does and that is why I have remained a member.
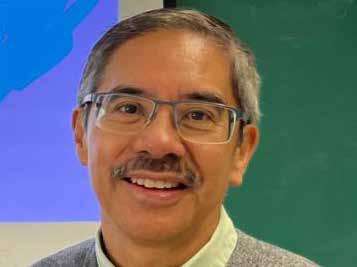
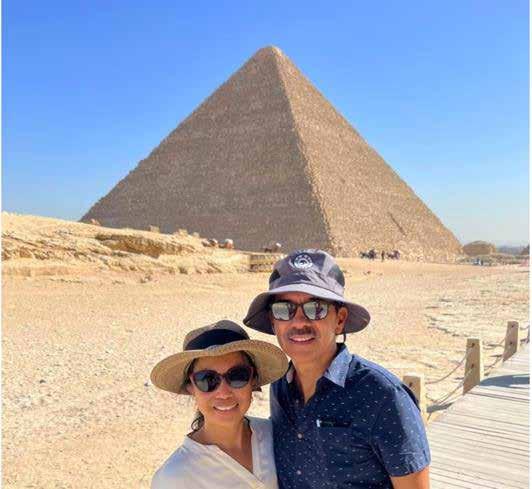
Thad Padua is a board-certified pediatrician who has been a member of the Santa Clara County Medical Association for 32 years. He and his wife, Rosemarie R. Padua, MD, also a pediatrician, share a private practice together. In addition, Dr. Padua teaches the Stanford Family Medicine Residents at O’Connor Hospital and cares for children at the Pediatric Center of Indian Health Center of Santa Clara Valley.
Dr. Padua was born and raised in San Francisco, received his Bachelor of Arts Degree in Social Welfare at UC Berkeley, and attended medical school at Far Eastern University in the Philippine. He completed his Pediatric Residency and Adolescent Medicine Fellowship at the Medical College of Pennsylvania in Philadelphia. He remained on faculty as an assistant professor before being recruited by O’Connor Hospital in San Jose to help start their hospital-based pediatric center in 1991. He served as the medical director for 24 years and helped develop a comprehensive pediatric primary care service for low-income families. The Pediatric Center for Life became one of the first primary care clinics to address the needs of the whole child by having health educator, social worker, nurses, and pediatricians caring for medical and psycho-social needs of families.
Dr. Padua was also the Chair of the Department of Pediatrics at O’Connor Hospital before Santa Clara County purchased the hospital in 2019. In 2020, he became medical director of Pediatrics and helped establish the O’Connor Pediatric Urgent Care Center, which helps address the urgent healthcare needs of children after pediatricians’ offices close.
Dr. Padua’s dedication and commitment to the health and well-being of children has been well-demonstrated by his advocacy and past service on various community boards, including O’Connor Hospital and Lucile Packard Foundation for Children’s Health. He currently serves as chair of the Santa Clara Family Health Plan Provider Advisory Council and is board member of
the Healthier Kids Foundation which helps school aged children get dental, vision, and hearing, and wellness screens.
As past president of the Philippine Medical Society of Northern California, Dr. Padua has helped lead medical missions in the Philippines. The organization has been performing annual medical missions since 1986. Dr. Padua finds volunteering to help the very poor to be truly rewarding.
He and his wife have been married for 38 years. They have two children who have followed in their footsteps as healthcare professionals: Ilyssa is a family nurse practitioner at Stanford Healthcare, and Irie is a Family Medicine physician who is completing his sports medicine fellowship at the University of California, Irvine. Thad and Rosemarie enjoy international travel, attending performing arts events, and volunteering for medical missions.
Why are you an SCCMA member?
To be able to connect with other physicians in our community, stay knowledgeable about the world of medicine, help advocate for independent physicians, and learn about health resources available for physicians.

Which SCCMA member resource is most helpful to you?
Practice Management Tools, Webinars, Legal Assistance, Billing Assistance.
What do you like to do when you’re not at work?
Travel with my spouse, volunteer at medical missions and community outreach programs, attend performing arts and athletic events.
What is the most important thing you learned in medical school or residency?
A child’s physical health is not only affected by good medical care but also affected by the environment he lives in.
What are some of the biggest opportunities or challenges you see in health care within the next five years?
The biggest challenge is the survival of independent prima-

ry care pediatricians. With low reimbursement and high practice expenses, private practice pediatricians will either retire or leave the area.
What do you love most about practicing [your specialty]?
As a pediatrician, I enjoy helping parents help their child stay healthy. The trusting relationship that I develop with families is so rewarding. I often feel a part of my patient’s family especially when they invite me to special family events such as birthday parties and graduations.
What is the best piece of advice you have been given throughout your career so far?
Helping to make positive change in the world requires perseverance and patience.
Who’s your favorite music artist/band?
Queen
What is your favorite restaurant in the Bay Area?
A Bellagio Italian Restaurant in Campbell
If you weren’t a physician, what profession would you like to try?
A college professor teaching about social justice.

Dr Veena Vanchinathan is a proud SCCMA member and Bay Area native! She was born in New Jersey but spent most of her childhood growing up in Fremont. She studied at Cornell University and dual majored in Neurobiology and Behavior and Comparative Literature. She enjoys finding a balance between arts/humanities and the sciences whenever feasible. Dr Vanchinathan went to medical school at the David Geffen School of Medicine at UCLA. She initially devoted the first two years of medical school on cardiology research, but later had a change of heart when she took a year off to help Dr Noah Craft, in his lab, and in the process, fell in love with the field of dermatology. She performed her internship in preliminary medicine at Santa Clara Valley Medical Center and her dermatology residency at Henry Ford Hospital in Detroit.
Dr Vanchinathan is an SCCMA member because it is incredibly important for her to give back to her local medical community and to volunteer time to advocacy in medicine and important issues that affect physician practices and the well-being of patients. She enjoys the SCCMA webinars and found Legislative Advocacy Day at the state capitol to be a very rewarding experience. Her absolute favorite SCCMA offering for 2023 was the 1440 Multiversity retreat in August, where she had a chance to forge connections with fellow healthcare providers and focus on optimizing their own health and wellness so they can bring their best selves to their own families and work.



Dr Vanchinathan loves the field of dermatology, she really enjoys being able to provide quick relief or improvement for her patients, because skin disorders often cause them significant distress and impact their quality of life. She can see patients of essentially any age, with thousands of different diagnoses, and help get them on the right treatment path by correctly identifying their dermatologic disorder. The most important thing that Dr Vanchinathan learned as an intern at Santa Clara Valley Medical Center, was from an attending physician, Dr Steve Roey. He taught her that “life is a battle against bad data.” In other words, to never use a lab test or biopsy result as a standalone value, but rather interpret it within the clinical context, and to always keep in mind that more data (e.g., more or repeat tests) might be needed for diagnostic confirmation. These words have helped her solve some elusive medical cases in her career over the past ten years and was some of the best advice

she ever received.
When Dr Vanchinathan is not at work, you can find her biking around beautiful Morgan Hill, painting, doing crafts and watching movies with her family. She loves spending time with her two children Ahana (age 9) and Ahvan (age 7) and their very spoiled cat (Bella). While she appreciates all the different restaurants the Bay Area has to offer, her favorite is Saravana Bhavan, (a vegetarian South Indian restaurant in Fremont). Her family hails from South India, and good Southern Indian restaurants are hard to find. Her favorite meal there is the butter masala dosa.


The physicians in Santa Clara County go above and beyond the role of their jobs to make the community a healthier and happier place to live. Here we are honoring just a few of the outstanding physician leaders that have made exceptional contributions to our community.
Barbi Phelps-Sandall, MD, Med, Graduate of UCLA school of Medicine, Graduate of the Andrew Weil, Integrative Medicine Fellowship, at the University of Arizona, Graduate of the Leadership in Integrative Medicine Program at Duke University (scholarship), Graduate of the Contemplative Medicine Fellowship, (inaugural class) New York Zen Center.
Dr. Phelps-Sandall has been selected as Chair of the Physician Wellness Committee at El Camino Hospital, where she is working on developing a Wellness Website for physicians, whose goal is to destigmatize mental health issues on our privileging applications, developing promotion of wellness resources in new physician orientation.


Dr. Phelps-Sandall serves as a preceptor for multiple students, has attended Stanford International Humanitarian Surgical Skills program, participated in the 13th Komen 3 Day/Avon 39 breast cancer walk to raise funds and awareness of breast cancer. She is an active member of the South Bay Chapter of AMWA, and of the Palo Alto Alumnae Association of Kappa Kappa Gamma Fraternity.
Outside of her profession, Dr Phelps-Sandall enjoys yoga and Pilates, studying history, reading, participating in book groups, and spending time with her puppy that she rescued in Mexico.


Fahd Khan, MD, MSE, MPH, is a General Neurosurgeon based in San Jose, with a subspecialty concentration in Stereotactic and Functional Neurosurgery. His expertise lies in employing deep brain stimulation techniques to address movement disorders, including Parkinson’s Disease and Essential Tremor, ultimately contributing to the enhancement of patients’ quality of life. Dr. Khan made history as the inaugural surgeon on the West Coast to utilize the cutting-edge Medtronic Stimulator Percept, yielding exceptional results. His reputation extends beyond Santa Clara County drawing patients from as far as the Oregon border. Apart from his clinical achievements, Dr. Khan holds noteworthy leadership positions, serving as the president-elect of the SCCMA (Santa Clara County Medical Association) and Chief of Staff Elect at Good Samaritan Hospital. Additionally, he recently attained a Masters Degree in Public Health (MPH) from UC Berkeley, complemented by a practicum project centered on educating healthcare professionals about the health impacts of climate change. Dr. Khan is committed to raising awareness on this critical issue and has delivered insightful grand rounds presentations to both physicians and nurses in Santa Clara County. His dedication to advancing medical knowledge and promoting environmental health underscores his diverse contributions to the field.

Cindy Lee Russell, MD, Plastic Surgery, PAMF, Past President and Co-Chair SCCMA Environmental Health Committee, as a breast reconstructive surgeon Dr. Russell witnessed the epidemic of breast cancer during her career. Learning that breast milk contains over a hundred known toxic chemicals which could act as endocrine disruptors and immune suppressants, contributing to cancer, spawned a passion for environmental issues and public health.
After completing her residency in plastic surgery at Stanford she began practice locally. Dr. Russell focused on toxins in the environment as Chair and now CoChair of the Santa Clara County Medical Association Environmental Health Committee for more than 20 years. During that time, she authored many policy resolutions related to reducing environmental toxicants at the California Medical Association House of Delegates, collaborating with colleagues within and outside the SCCMA Environmental Health Committee.
In 2001 she led the effort, with a community group, to pass the Santa Clara County Integrated Pest Management Ordinance to reduce pesticide exposure on County property. She is a Co-Founder and Executive Director of Physicians for Safe Technology, a non-profit group formed in 2016 to educate physicians and the public about the science, risks and safer use of wireless technology. Her 2018 publication, 5 G wireless Telecommunications Expansion: Public Health and Environmental Implications, has been cited over 100 times in the literature.
Last year the SCCMA Environmental Health Committee, in partnership with the SCVWD, created a special issue of the SCCMA Bulletin, Water and Health, The Coming Crisis and What We Can Do About It, which highlighted the need to reduce contaminants by regulating chemicals. Dr Russell maintains her commitment to a healthy sustainable environment, improved individual health and preventative public health issues, including climate change.
Robert M. Gould, MD President, San Francisco Bay Physicians for Social Responsibility (SFBPSR) North American Regional Vice-President, International Physicians for the Prevention of Nuclear War (IPPNW). Adjunct Assistant Professor, Program on Reproductive Health and the Environment, Department of Obstetrics, Gynecology and Reproductive Science, UCSF

Of his many accomplishments in 2023, Dr Gould has been happy to help lead SFBPSR in a variety of programs addressing climate change, especially those focused on highlighting equity considerations in our major regional work with EJ community partners on building electrification and related decarbonization efforts and supporting efforts to institute health-protective “setbacks” from toxic oil and gas operations. He also is continuing to connect our existential climate work with our continued core work on abolishing nuclear weapons, an example being my article “Let’s Heed Oppenheimer and End the Threat of Nuclear Weapons” published in San Francisco Marin Medicine, as well as participating in the terrific IPPNW World Congress held in Mombasa, Kenya in April.
Dr. Gould has also been very pleased partnering with University of New Mexico Project ECHO in developing a 6-week CME course for health professionals “Global Nuclear and Environmental Threats Critical to Climate Change and Human Health” starting March 2024, leading-off with talk “The Global Nuclear Threat and Nuclear Landscapes in the United States”.
Allison Collins, MD, is a pediatrician and a board-certified lifestyle medicine specialist. She is the director of Lifestyle and Culinary Medicine for the Kaiser Permanente Santa Clara Medical Center. She specializes in working with kids, teens, and families on lifestyle change to prevent, treat, and reverse chronic diseases.

In 2011, she founded the HEAL (Healthy Eating, Active Living) program at Kaiser Permanente Santa Clara in California. She works with a multidisciplinary team — including a pediatric nutritionist, pediatric physical therapist, pediatric psychologist, and clinical health educator — to run individual and group visits for kids and teens who struggle with weight and obesity, along with health issues such as prediabetes or diabetes, high cholesterol, hypertension, and other issues that put them at risk for future medical issues.
Dr. Collins also founded the Cook for Health culinary medicine program in 2017, initially with in-person cooking classes for kids and teens. Now, the classes have expanded to offer both adult as well as kids plantbased cooking classes several times a month to a larger group in the virtual setting for Kaiser Permanente Santa Clara patients. As part of that, she develops her own plant-based, family-approved recipes to teach in her classes.
Dr. Collins attended Tufts University in Boston where she earned her B.S. in psychology and biomedical engineering. After college, she received a Fulbright scholarship and conducted research on obesity in Indonesia. She received her medical education at University of California, San Diego and was awarded the American Nutrition Society Fellowship. Collins completed her residency training at Lucile Packard Children’s Hospital at Stanford and joined Kaiser Permanente in 2010. She became Board Certified in Lifestyle Medicine in 2018 and became a Certified Lifestyle Medicine Specialist in 2021.

Every year, medical students that near the end of their studies get matched to residency programs to begin their journey into the field of medicine. “Match Day” was established in 1952 by the National Residency Matching Program (NRMP), a private, non-profit organization that organizes an orderly and fair mechanism for matching medical students to residency programs. With the advancements of technology, NRMP provides a matching mechanism through the “Registration, Ranking, and Results (R3) System” where a mathematical algorithm matches the applicants to programs on their most preferred choices. The Match system allows applicants and program directors to consider each other and evaluate their options without pressure. It is a fair, efficient, transparent, and reliable system that eliminates common issues such as early offers.
Match Day is a pivotal day for medical students. The journey is full of anticipation. The 2023 Match Day process offered
residency positions to 40,375 medical students. (https://www. ama-assn.org/medical-students/preparing-residency/whenmatch-day-2024) With over ten residency programs throughout the hospital systems in Santa Clara County, 77 students got matched into residency programs in 2023. This year, Match Day will be on March 15 and matches can be made as early as March 11.
The early stages of anyone’s medical career are simultaneously fragile and exciting. SCCMA hopes to create a “hub” for all incoming Residents as an extra resource and create a community for young physicians in Santa Clara County. SCCMA recognizes emerging health professionals and the significance of The Future of Medicine. Residents have complimentary membership with CMA/SCCMA during their training and membership offers student loan discounts, a career center, and loan forgiveness.
If any residents are looking to getting involved in SCCMA or being a resident representative, please contact Director of Membership and Program, Angelica Cereno, at angelica@sccma.org

“Service, leadership and advocacy are the heart of medicine, and CMA is an essential part of being the kind of doctor that our communities and country needs.”
Oscar Echevarria, M.D. Resident Physician Intern 2016 Member
To help shape the future of medicine in California, CMA provides FREE membership for medical students, residents and fellows.
STUDENT LOAN DISCOUNTS: CMA members save an average of $27,000 when they refinance their student loans through our partner SoFi®.
CAREER CENTER: CMA’s California PhysicianTM Career Center provides job opportunities, career advice and helpful resources at careers.cmadocs.org.
PHYSICIAN WORKFORCE: CMA is committed to ensuring California is training enough physicians to meet current and future demand. Our CalMedForce GME grant program to date has allocated over $189 million to 143 GME programs across California to retain and expand residency programs in primary and emergency medicine.
LOAN FORGIVENESS: The CalHealthCares program provides loan repayment of up to $300,000 on educational debt for California physicians and dentists who provide care to Medi-Cal patients. To date, 1,077 California providers have received a combined total of $256 million to pay down student debt.
CMA also sponsored legislation that created the Steven M. Thompson Loan Repayment Program, which provides physicians with up to $105,000 to repay educational loans in exchange for a three-year service commitment in a medically underserved area of the state.
CMA provides many avenues for medical students and residents to strengthen their CVs, with federal, state and local opportunities.
Be an advocate and have a direct impact on public health and the future of medicine in California.
Connect, network and learn with physician colleagues from across the state.

ChatGPT is a free, large language model AI chatbot (OpenAI, San Francisco). It was launched on November 30, 2022. By April 2023, it has averaged over 60 million visits per day. ChatGPT has natural language processing capabilities to train in the auto-completion of sentences and ideas. For me, as an ophthalmologist, I would type the word “glaucoma”, and the response is quick. These models may predict the next word to be “open angle” or “angle closure” based on statistical parameters learned from prior training data sets. It gained traction due to its unprecedented ability to generate human-like language and respond to a massive range of inputs.
Of note, BARD launched in March 2023 and relaunched in August 2023, is catching up to ChatGPT in popularity as of this writing. ChatGPT and BARD both have approximately one million downloads a day. BARD is in 140 languages and ChatGPT is in 60 languages. Claude and Cohere’s Coral are

also LLMs but they are catering to the B2B market. Their chatbots are not as popular as ChatGPT and BARD.
One hundred thirty million Americans lack proficiency in literacy, reading below the equivalent of a sixth-grade level.1-3 The average American reads between 7th to 8th grade.4,5 Health literacy is a recognized problem for most Americans.4,5,6 For ChatGPT and patient users, health literacy may be a problem.1,2,3 ChatGPT types out text in fully formed paragraphs which may be difficult for our average patient, who have a 6th to 8th grade reading level.
During the COVID-19 pandemic, many patients resorted to self-isolation or hesitated to visit their doctors. Consequently, their family members turned to the Internet for patient information, which may be incorrect. The introduction of ChatGPT on November 30th, 2022 fulfilled an unmet need, drawing users from all parts of the world.
The medical literature has discussed the need for patient education in managing chronic conditions, such as diabetes, where certified diabetes educators play a crucial role.9 Some fields of medicine lack certified medical educators, instead, nurses are filling that role. However, with the nursing shortage, how can we leverage these chatbots to save money and time for us in the busy clinic?
Medical assistants and nurses are paid employees versus ChatGPT and BARD, which are free. ChatGPT and BING are similar since Microsoft bought a large share of OpenAI which created ChatGPT. These bots would achieve cost savings for our office budgets but they are not accurate as standalone solutions for complex scenarios in medicine. However, a new development since June 2023, both ChatGPT and BARD now start off with their response with “I am not a doctor, but…” This warning is a great beginning.
Although ChatGPT has the potential to contribute to patient education, it is improving every day because it is “learning” from our questions and our responses.
For example, when prompted with the term “glaucoma,” ChatGPT’s predictions are based on statistical parameters learned from prior training datasets, up to the year 2021 in the internet, potentially missing newer information related to innovative medications and techniques for glaucoma treatment. However, BARD which uses PaLM2, a slightly different algorithm, is taking its responses from the internet directly.
ChatGPT and BARD’s text responses requires reading comprehension at an 11th to 12th-grade reading level, whereas the average American reads at a 7th to 8th-grade level.3,4 This discrepancy poses a challenge for patients with lower health disease prevention. Improved adherence to medication regimens is closely associated with higher health literacy, socioeconomic status, and education level.10,11,12
However, you can ask ChatGPT and BARD to answer you as a fifth grader and the responses are much easier to comprehend for a lay person.
In conclusion, the availability of large language models like ChatGPT and BARD has opened a new era where physicians can leverage AI for clinical decision-making and general patient education.14,19,20 In the near future, residency and fellowship programs may utilize chatbots to enhance trainees’ clinical reasoning skills through generative case reports, similar to oral board examination questions. As physicians, we must be aware of the capabilities and limitations of AI-mediated chatbots, as they may
generate inaccurate or biased results.14,18,20,21 It is crucial for physicians to recognize the influence of their written “phrases,” and “word associations” as these are used in the training of chatbots by their software programmers. Frequent inclusion of the phrase “see a physician “ may be needed in the software codes of Medical websites and web journals, to ensure the inclusion of “physicians” in the AI vocabulary of AI-mediated chatbots.
1. Hirosawa T, Harada Y, Yokose M, et al. Diagnostic Accuracy of Differential-Diagnosis Lists Generated by Generative Pretrained Transformer 3 Chatbot for Clinical Vignettes with Common Chief Complaints: A Pilot Study. Int J Environ Res Public Health 2023; 20(4):3378.
2. Eysenbach G. The Role of ChatGPT, Generative Language Models, and Artificial Intelligence in Medical Education: A Conversation With ChatGPT and a Call for Papers. JMIR Med Educ 2023; 9:e46885. Accessed April 20, 2023.
3. Bader M, Zheng L, Rao D, et al. Towards a more patient-centered clinical trial process: A systematic review of interventions incorporating health literacy best practices. Contemp Clin Trials. 2022;116:106733.
4. Kutner, M., Greenberg, E., Jin, Y et al. Literacy in Everyday Life: Results from the 2003 National Assessment of Adult Literacy [U.S. Department of Education web site]. April 2007. Available at: https://nces.ed.gov/Pubs2007/2007480_1.pdf. Accessed April 20, 2023.
5. Camille LR. and Bauman K. Educational Attainment in the United States: 2015. [U.S. Census Bureau web site]. March 29, 2016. Available at: https://www.census.gov/library/publications/2016/demo/p20-578.html. Accessed April 21, 2023.
6. An L, Bacon E, Hawley S, et al. Relationship Between Coronavirus-Related eHealth Literacy and COVID-19 Knowledge, Attitudes, and Practices among US Adults: Web-Based Survey Study. J Med Internet Res 2021;23(3):e25042. Accessed April 26, 2023.
14. Crigger E, Reinbold K, Hanson C, Kao A, Blake K, Irons M. Trustworthy Augmented Intelligence in Health Care. J Med Syst 2022; 46(2):12. doi: 10.1007/s10916-021-01790-z. PMID: 35020064; PMCID: PMC8755670. Accessed April 27, 2023.
18. Erdem E, Kuyu M, Yagcioglu S, et al. Neural Language Generation: A Survey on Multilinguality, multimodality, controllability, and Learning. Journal of Artificial Intelligence Research 2022; 73: 1131-1207.
19. Ayers JW, Poliak A, Dredze M et al. Comparing Physician and Artificial Intelligence Chatbot Responses to Patient Questions Posted to a Public Social Media Forum. JAMA Intern Med, April 28, 2023, Accessed April 29, 2023. Published online April 28, 2023. doi:10.1001/jamainternmed.2023.1838. Accessed April 29, 2023.
20. Li R, Kumar A, Chen JH. How Chatbots and Large Language Model Artificial Intelligence Systems Will Reshape Modern Medicine: Fountain of Creativity or Pandora’s Box? JAMA Intern Med. Published online April 29, 2023. doi:10.1001/jamainternmed.2023.1835, Accessed April 29, 2023.
21. Brender TD. Medicine in the Era of Artificial Intelligence: Hey Chatbot, Write Me an H&P. JAMA Intern Med. Published online April 29, 2023. doi:10.1001/jamainternmed.2023.1832. Accessed April 29, 2023.
 BY GLORIA WU, MD
BY GLORIA WU, MD
Artificial Intelligence took the world by storm on November 30, 2022 when Open AI unleashed ChatGPt into the internet space. By January 2023, it had 100 million users. During 2023, ChatGPT dominated the newsrooms, newsfeeds and even the New England Journal of Medicine. I was particularly interested in this topic having written two papers in this area in Ophthalmology. Thus, at Santa Clara County Medical Association, we had our first educational seminar on Artificial Intelligence and Healthcare. The meeting was held from 7:30 to 10:00 am on February 17, 2024 at 700 Empey Way, the headquarters of Santa Clara County Medical Association.
I introduced the topic of AI for a 5-minute introduction. We saw that generative AI is not new and occupies the space of large language models such as ChatGPT, Bard, Cohere’s

Coral and Claude. In addition, AI now encompasses administrative startups, clinical data management, the organization of unstructured data into more targeted data sets to yield specific answers to questions. AI encompasses patient facing companies, physician facing companies and revenue management as well. Cybersecurity has an AI component as well.
At 8:10 am, the next speaker was Brian Grady, MD, a urologist from San Francisco who joined us by Zoom. He is part of Golden Gate Urology. He is the Past President of the San Francisco Marin Medical Society. He spoke about disparities in diagnosis for urological cancers among patients in minoritized populations. It was a compelling talk about the health disparities of medicine.

Dr. Demilade Adedinsewo MB, CH B, FACC joined us via a prerecorded Zoom. She is Assistant Professor of Medicine at the Mayo Clinic in Florida. She is a member of the Board of Direc-
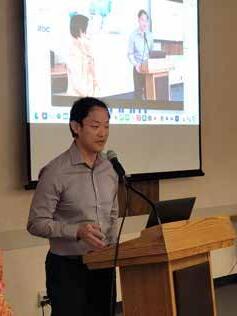


tors of the American College of Cardiology. In addition, she is the Berggren Innovation Scholar, Mayo Clinic College of Medicine and Science. She is a non-invasive cardiologist. Her topic was Pre-eclampsia and ECG Based Learning Model. It was an overview of pre-eclampsia and heart disease in African women and American women. The AI model could read the ECG with 100% accuracy.
At 8:20, we had the video from Japan. The author of this talk on Internet of Things was Professor Giulia Barbareschi. The presentation showed the use of robots in the healthcare and non-healthcare settings in Japan. Dr Barbareschi is a senior assistant professor at Keio University, Graduate School of Media Design. She is particularly interested in disability, innovation, assistive technology. She is from Italy but now resides in Japan. The video of the robots was inspirational.
At 8:37 am, we had a presentation by our own Santa Clara County Medical Association’s member, Santosh Pandipati MD, the founder of E-Lov-U, which has raised more than $4 million and has more than 20 hospital systems using its app for compliance and pre-natal care. It delivers pre-natal and post-natal care, and it is



covered by insurance. The platform is the first of its kind in the field of Obstetrics and Gynecology. This app is the brainchild of Dr Pandipati, an obstetrician gynecologist and a maternal and fetal medicine physician. Dr. Pandipati is also an active member of the Environmental health committee here at Santa Clara County Medical Association.
A highlight of the program was the presentation by Vice President, Blue Shield, Dr. Zoher Karu, PhD, he is Chief Data and Analytics Officer. He gave an outstanding talk about AI and big data and how it impacts insurance prediction models of disease. He liked the question-and-answer period with our audience. Dr. Karu obtained his PhD in Electrical Engineering and Computer Science from Massachusetts Institute of Technology. He has a BS in Electrical Engineering from Carnegie Mellon University. He has held executive positions at eBay, as Chief Data Officer and Vice President of Customer Optimization and Data.
After the Blue Shield presentation, Dr. Jianying Hu from IBM presented live from Yorktown Heights, New York via Zoom. She spoke about IBM’s efforts on developing AI technologies for accelerated discovery of therapeutics. Dr. Hu holds the prestigious title of IBM fellow, Director of Healthcare and Life Sciences Research, Global Science Leader, AI for Health. She is the Adjunct Professor at Icahn School of Medicine at Mount Sinai.


A break from AI was the video lecture by
AI encompasses patient facing companies, physician facing companies and revenue management as well. Cybersecurity has an AI component as well.

YouTube Producer for companies, Influencers with several million followers. He breaks down the Do’s and Don’ts of social media. He advises to do the following 3 things: 1) Don’t use social media to become famous but Publish Content with Value, 2) Publish Content with a Payoff→ does it entertain, does it give information, does it inspire you? 3) You need to know your target audience. He has been a YouTube producer helping influencers and brands to grow their Instagram and YouTube audience for ten years. He lives in Los Angeles. He was physically present for questions and answers at our Meeting
Francisco in January 2024. Priti Dugar has a background in mathematics and has been involved in previous startup ventures.


Next was the Startup Focus Section. First there was the video presentation of Long Health, a data exchange company to address the friction points of unequal data exchange by the patient and by the Doctor. No one was getting the referral letters and as a result, the patient has to have repeated blood tests or ECGs. Thus, Long Health connects with all EHRs to the doctors and to the California Data Exchange Framework, The National Care Quality Data Framework. The California law, AB 133, mandates bidirectional data exchange as of Jan 1, 2024 in large group practices (over 25 MDs) and will affect smaller MD practices as of Jan 1, 2026. Rohit Patil is the Founder and CEO. He came across this idea when his own mother was unable to obtain her medical records when she visited doctors. He is a computer science engineer with a decade of experience in data and data analytics at CISCO.
Next to present was Blinkpad’s founder and CEO, Priti Dugar. Blinkpad provides a service that facilitates precise connections between healthcare businesses and specialized individuals, each with certifications, licensures and specific language capabilities. She and her company presented at JP Morgan week in San

The last startup to present to our group was Truss Health. The presenter was Kadambari Beelwar, MBA, CEO. Truss Health is a remote patient monitoring platform. Its aim is to decrease surgical site infections by leveraging AI technology to monitor the patients’ health status. It has proprietary software and hardware to detect surgical site infections. Kad Beelwar, prior to joining Truss Health, was the Telehealth manager at Stanford’s Lucille Packard Children’s Hospital in Palo Alto. She is enthusiastic about telemedicine and remote patient monitoring.
References
Asch, DA. An Interview with ChatGPT About Health Care. New England Journal of Medicine Catalyst. April 4, 2023. https:// catalyst.nejm.org/doi/full/10.1056/CAT.23.0043, Accessed Feb. 29, 2024.
Wu, G., Lee, D. A., Zhao, W., Wong, A., & Sidhu, S. (2023). ChatGPT: Is it good for our glaucoma patients? Frontiers in Ophthalmology, 3, 1260415. https://doi.org/10.3389/ fopht.2023.1260415, Accessed Feb. 29, 2024.
Wu, G., Zhao, W., Wong, A., Lee, D.A. “Patients with floaters: Answers from virtual assistants and large language models.” Digital Health 10 (2024): 20552076241229933, Accessed Feb. 29, 2024.
 BY BRANDON CRAIG
BY BRANDON CRAIG
The Santa Clara County Medical Association is launching a new program to address physician wellness and burnout in 2024.
Practicing as a physician continuously gets more and more challenging as the years go by. Patient loads grow, administrative burdens expand, and the number of physician colleagues shrinks. Software is introduced to make the job easier but ends up complicating things further. These concerns aren’t new but were further exacerbated by the COVID-19 Pandemic, which highlighted every crack in the healthcare system. All these factors have worked together to create a difficult and demanding environment and burned-out thousands of physicians nationwide. On the macro level, this is a devastating detriment to patients’ access to care. On the micro level, this can mark significant tragedy as burnt-out physicians are significantly more likely to commit suicide.
SCCMA will address these concerns by adopting tried and true methods. These methods are being replicated from the highly-successful Joy of Medicine program run by our sister society – the Sierra Sacramento Valley Medical Society (SSVMS). SSVMS began Joy of Medicine in 2017 and has helped other medical societies at both the state and local levels launch their
own programs.
According to SSVMS, the Joy of Medicine “mitigates physician burnout both by alleviating the effects on physicians and by advocating for systemic changes to prevent burnout at the source.”
Accordingly, SCCMA will attack physician burnout using a two-pronged approach: by treating the individual physicians and by fostering systemic changes to address the root causes.
On the individual side, physician burnout is dangerous. This career is inherently physically demanding and emotionally taxing. No one ever entered the healthcare field with the understanding that it would be easy but that doesn’t mean that the role should become even more draining due to broken systems. As such, beginning in 2024, SCCMA will offer all physician members up to six lifetime virtual counselling sessions. These sessions are with vetted mental health professionals, including psychologists and life coaches, and are convenient, free, and anonymous. Neither SCCMA nor your employer will be permitted to know whether you access these sessions. Simply contact one of the participating providers and let them know you’re a member of SCCMA to get started. All sessions will be virtual, allowing you to access the program from the comfort of your own home. And, once again, these services are available to SCCMA members at no cost to them.

SSVMS members take advantage of
Physicians know that treating the symptoms isn’t enough; you must fix the root cause. To affect systemic changes, SCCMA will create a forum for the Chief Wellness Officers of our region to share their best practices to prevent physician burnout. In their program, SSVMS convenes the Joy of Medicine Advisory Committee, which includes the Chief Wellness Officer or equivalent from each of the Sacramento region’s integrated medical groups, as well as physicians in private practice, medical students, and residency program representatives, to collaboratively shape the goals and activities of the program to benefit all physicians and physicians in training. The Joy of Medicine Advisory Committee meets on a quarterly basis to share best practices, to provide guidance on program offerings, and to advise SSVMS on the direction and sustainability of the Joy of Medicine program. They perform original research to determine how significant burnout is for local physicians and to have accurate information on its most significant sources.
For example, SSVMS conducts biennial surveys of physicians creating benchmarks to evaluate how burnout has increased or decreased over time. They found that in 2018, burnout in their region was at 37%. That fell to 35% in 2020 and but, due to COVID19, rose to 44% in 2022. Nationally in 2022, the burnout rate for physicians was at 63%. This survey was turned into a whitepaper, “Joy of Medicine: Physician Wellness and Workforce,” which broke down the drivers of burnout into seven different categories (Organizational Culture and Values, Workload and Job Demands, Compensation, Social Support and Community Work, Efficiency and Resources, Work-Life Integration, and Control and Flexibility) and compared how respondents rate those over time. This data was then compiled into a dashboard for individual medical groups to consider how their burnout rates compare not only to themselves over time, but how it compared to the region as a whole. These dashboards include specific recommendations on changes the medical groups can make to better address burnout, such as prioritizing improving the electronic health record and allowing more flexibility in scheduling.
This survey also informs the medical society of arising issues that need to be addressed. For example, SSVMS included
questions about violence, abuse, and mistreatment from a variety of sources, including patients and their families, colleagues, nurses, leadership, and more. Responding physicians indicated that 39% overall had been mistreated in the prior twelve months and 31% had been mistreated specifically by patients and their families. Following this result, SSVMS addressed the necessary stakeholders and began drafting policy resolutions on physician mistreatment, compiling personal experiences into an article in their magazine to raise awareness, hosting educational sessions on communication and de-escalation techniques, and working with health systems and medical groups to craft best practices on patient codes of conduct, escalation prevention strategies, de-escalation policies and procedures, and post escalation protocols. Because they had solid data demonstrating the severity of the problem, SSVMS found there was little trouble in pulling workgroups together to address the epidemic.
September.
This new program will not completely solve burnout, by any means. The burnout rates will never reach zero. But the current rates are untenable and threatening the livelihood of physicians and risking access to quality care for patients. By focusing on healing the individual and improving the systems in place, SCCMA will harness our resources to create a healthier environment for physicians to practice. We’re going to work together to reduce the prevalence of burnout. Please stay tuned for more information regarding the program launch later this year and take advantage of the resources whenever you need.
Climate change is having a wide-ranging impact on human health, well-being, and livelihoods. Some of the key ways climate change affects humans include: heat-related illnesses, vector-borne diseases, extreme weather events, air quality and respiratory issues, water scarcity and contamination, food insecurity, mental health challenges and disruption of healthcare systems.
Existing health disparities and environmental injustice mean we need to pay special attention to historically disadvantaged groups as well as other vulnerable cohorts like the elderly, children, and those with pre-existing health conditions.
Physicians wield considerable influence in enhancing patient health and tackling climate change. Physicians are encouraged to engage in conversations with their patients about the interdependent relationship between individual health and the collective impact on climate change. Here are several recommended discussion points for engaging with patients:
1. Diet: Adopt a Plant-Based Diet:
Encourage patients to consume more plant-based foods and reduce their intake of red meat and processed foods. This lowers the environmental impact associated with livestock agriculture and is associated with a lower risk of chronic diseases, including heart disease, diabetes, and certain cancers. Processed foods on the other hand are high in added sugars, unhealthy fats and sodium and involve resource-intensive production with a loss of nutritional value of foods.
2. Support Local and Sustainable Agriculture:
Choose locally produced, sustainably sourced and seasonal foods. This not only supports local economies but also reduces the carbon footprint associated with transporting food over long distances. Encourage patients to be mindful of what and how they eat by paying attention to portion sizes, choosing nutrient-dense foods, and avoiding excessive packaging.
3. Encourage Sustainable Transportation Choices:
Promoting active transportation such as walking or cycling contributes to increased physical activity. Physicians can, for example, encourage patients to walk 10,000 steps per day by emphasizing the health benefits, setting realistic goals, and leveraging fitness trackers. Creating personalized walking plans, promoting accessibility, and celebrating milestones can further motivate patients to integrate walking into their daily routine for improved overall health.
4. Renewable Energy Sources:
Support the transition to renewable energy sources such as
LAYA KHAN High School Student, Khan Lab Schoolsolar, wind, and hydroelectric power. This helps reduce air pollution and mitigates climate change, while positively impacting respiratory and cardiovascular health. Recommend the use of energy-efficient vehicles, such as electric cars or hybrids, to reduce air pollution and dependence on fossil fuels. Public transportation and carpooling are also eco-friendly options.
5. Advise on Air Quality:
Discuss the importance of indoor and outdoor air quality for respiratory health. Physicians can provide guidance on avoiding exposure to pollutants, supporting clean air initiatives, and using air purifiers in indoor spaces. Physicians can encourage patients to check the Air Quality Index (AQI) with smartphone apps or websites that offer real-time AQI readings and advise them to modify outdoor activities or take preventive measures when the AQI levels are high.
6. Advocate for Spending Time in Nature:
Physicians can advise patients that spending time in nature has mental health benefits, including reduced stress and improved mood. Encouraging outdoor engagement can enhance overall health, providing opportunities for exercise, relaxation, and connection with the natural environment.
7. Improved Water Quality:
Access to clean and safe drinking water is crucial for preventing waterborne diseases and maintaining overall health. Educate patients on the importance of water conservation for personal and environmental health. Encourage practices such as fixing leaks, using water-efficient appliances, and promoting responsible water consumption habits.
8. Support Mental Health in a Changing Climate:
Acknowledge the mental health impacts of climate change, including anxiety and stress related to extreme weather events. Physicians can incorporate mental health support into their practice and advocate for broader mental health resources in the community.
As physicians we have a unique influential role in our society and can be charged with leading by example and demonstrating environmentally conscious practices within the healthcare setting. We can implement energy-efficient technologies, reduce waste, and adopt sustainable healthcare practices. This can inspire both staff and patients to follow suit. Finally, Physicians can advocate for policies that address both public health and climate change. This may include supporting initiatives for clean energy, sustainable transportation, and regulations that reduce pollution.



Global Nuclear and Environmental Threats Critical to Climate Change and Human Health
Wednesdays, March 6 – May 15 Bi-Weekly
11 a.m.-12 p.m. PT / 12 p.m.-1 p.m. MT / 2 p.m.-3 p.m. ET
Given the decades-long global threats of nuclear weapons and power, environmental health exposures from chemical solvents and superfund sites, and resulting environmental injustice, our bi-weekly sessions will be a primer for health professionals, public health officers, first responders, and community-based educators interested in learning from nationally and internationally known experts.
Medical Director – Joanna Katzman, MD, MSPH







March 6 The Global Nuclear Threat and Nuclear Landscapes in the United States
March 20 Health Impacts of Radiation
April 3
90 min
Environmental Justice and Nuclear Harms Panel
Facilitated by Robert M. Gould, MD and Ryan Edgington, PhD
Robert M. Gould, MD President, San Francisco Bay Physicians for Social Responsibility
Dan Hirsch
Retired Director of the Program on Environmental and Nuclear Policy at the University of California, Santa Cruz, and President of the Committee to Bridge the Gap, a nuclear policy NGO.
Douglas Brugge, PhD, MS
UCONN Health, Department of Public Health Sciences, environmental and occupational health.
April 17
Environmental Exposures and Nuclear Superfund Sites
May 1 Identifying the Source of Chemical Solvents and Their Health-Related Impacts
May 15
90 min
2.21.24
Environmental Justice and Environmental Toxicities Panel
Facilitated by Lesa Walker, MD, MPH and Joanna Katzman, MD, MSPH
Jacqueline Cabasso Executive Director, Western States Legal Foundation, Mayors for Peace
Tina Cordova, MSc, BSc
Trinity Downwinders, Cofounder of the Tularosa Basin Downwinders Consortium
Michelle Hunter, MS
NM Office of Engineers, New Mexico Department of Health
Michelle Hunter, MS
NM Office of Engineers, New Mexico Department of Health
Yohanna Barth-Rogers, MD
Chief Medical Officer, UMMA Community Clinic, Los Angeles, CA
Dino Chavarria
Tribal Superfund Working Group, Santa Clara Pueblo, NM
Ryan Edgington, PhD
Project ECHO Senior Program Manager – New Mexico Health Programs Team, University of New Mexico Health Sciences Center
Marylia Kelley Executive Director of the Livermore, CA based Tri-Valley CAREs (Communities Against a Radioactive Environment)
Myrriah Gomez, PhD Assistant Professor in the Honors College, University of New Mexico
Jackie Medcalf
Texas Health & Environment Alliance (THEA) Founder and Executive Director, Houston, TX










Tuberculosis (TB) is on the rise – and it doesn’t need to be.
Santa Clara County has one of the highest TB case rates in California and in the country. Data from 2023 show an almost 20 percent increase in new TB cases compared to the previous year.1 This follows a six percent increase in new TB diagnoses from 2021 to 2022.2 The increase in cases was not caused by any one large outbreak, and surprisingly few cases appear to be caused by recent transmission from one person to another. Instead, more than 80 percent of cases were caused by activation of a previously latent TB infection (LTBI). Most people infected with TB bacteria acquire it from a person with contagious TB disease and can then walk around for years with LTBI. Detecting and treating LTBI before it progresses is the key to ensuring people never have to endure active TB disease.
“Asian people born outside the US are diagnosed with TB at 50 times the rate of US-born White people, which far outstrips disparities by race and ethnicity noted in HIV, heart disease and diabetes” (CDPH).4 Those at highest risk of progressing from LTBI to TB disease include individuals with recent exposure to TB disease, children under five years of age, and individuals living with HIV or other immunosuppressing conditions.1 In Santa Clara County, 25 percent of TB patients have diabetes, the most common comorbidity for TB.5
Latent TB infections are more likely to progress to active TB infections when the immune system is compromised. The following are the most common symptoms of TB disease
• Cough lasting 3 weeks or longer
• Unexplained weight loss and / or fever
• Coughing up blood or sputum
Treatment for LTBI is very effective – it can decrease the risk of developing TB disease by over 90 percent when medications are taken as prescribed.5 There are now shorter rifamycin based treatment options for LTBI.7 Most LTBI regimens used in the US are now 3 to 4 months in duration.
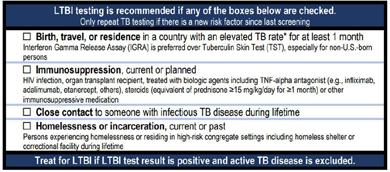
But if LTBI is asymptomatic, how should doctors know how to screen and treat it?
“The good news about LTBI is that it’s so easy to screen for,” says Dr. Ann Loeffler, Assistant Health Officer and TB Controller for the County of Santa Clara Public Health Department. “In every visit, ask some simple screening questions and, if the patient meets those criteria, order a single blood test. This disease is entirely preventable, and we should all be doing everything we can to put an end to it.”
What are those screening questions? The California Department of Public Health and California TB Controllers Association suggest:5
Anyone can become infected with TB, but testing is recommended for individuals who were born or have lived in a country where TB is common. This includes a large part of the world: Asia, Latin America, the Caribbean, Africa, and Eastern Europe.
• Weakness and fatigue
• Loss of appetite
Providers are required to report suspected and confirmed TB disease cases to the Public Health Department
Physicians are in a powerful position to stop the progression of TB and catch it while it’s still latent. This intervention is critical. In California half of individuals diagnosed with tuberculosis are hospitalized and 13% die before starting or during TB treatment. Santa Clara County Public Health is committed to achieving TB elimination.
To learn more about testing, treatment, and reporting of TB cases, in Santa Clara County, providers can visit sccphd.org/tb Resources for patients can be found at sccphd.org/TBInfo.
References:
1. California Department of Public Health, Tuberculosis Control Branch. California Tuberculosis Data Tables, 2022, 2021, 2019, 2017. Accessed February 23, 2024. https:// www.cdph.ca.gov/Programs/CID/DCDC/Pages/TB-Disease-Data.aspx
2. County of Santa Clara Public Health Department. In-
creased tuberculosis cases reported in Santa Clara County (2024). Published January 30, 2024. Accessed February 23, 2024. https://publichealth.sccgov.org/news/news-release/ increased-tuberculosis-cases-reported-santa-clara-county
3. California Department of Public Health. Substantial Increase in Tuberculosis in California: Recommendations for California Healthcare Providers. Published February 26, 2024. Accessed February 27, 2024. https://www. cdph.ca.gov/Programs/OPA/Pages/CAHAN/Substantial-Increase-in-Tuberculosis-in-California-Recommendations-for-California-Healthcare-Providers.aspx
4. California Department of Public Health. Costs and consequences of Tuberculosis in California. https://www.cdph. ca.gov/Programs/CID/DCDC/CDPH%20Document%20 Library/CostsandConsequencesofTBinCA.pdf
5. California Department of Public Health. Tuberculosis Control Branch. TB Risk Assessment Accessed February 23, 2024. https://www.cdph.ca.gov/Programs/CID/DCDC/ Pages/TB-Risk-Assessment.aspx
6. Shete PB, Tang AS, Flood J. Screening for Latent Tuberculosis Infection Among Non–US-Born Adults in the US: A Path Toward Elimination. JAMA. 2023;329(17):1457–1459. doi:10.1001/jama.2023.4967
7. Sterling TR. Guidelines for the Treatment of Latent Tuberculosis Infection: Recommendations from the National Tuberculosis Controllers Association and CDC, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 https://www.cdc.gov/ mmwr/volumes/69/rr/rr6901a1.htm


California Medical Association
Virtual Grand Rounds: New Weight Loss Medications – Panacea or Pandora’s Box
March 12, 2024 | Virtual | 12:00 PM – 1:00 PM
Santa Clara County Medical Association Book Club: What Looks Like Bravery by Laurel Braitman
Date: March 27, 2024 | In-Person – SCCMA Building (700 Empey Way, San Jose, CA 95128) | 6:30 PM - 8:00 PM

Obesity management began to shift dramatically starting in 2014 with the first FDA approval of a GLP-1 receptor agonist (RA) for weight loss. But things really took off in 2021 with the approval of another medication to this class, semaglutide. The weight loss with these medications is significant, but so are the side effects. It appears that patients are at high risk of regaining weight after discontinuing these medications. Combined with the high cost and patchy insurance coverage, equitable access is a concern. Carolyn Jasik, M.D., an adolescent medicine specialist with UCSF Benioff Children’s Hospitals, will join us to review the evidence and real-world data on this new class of obesity medications.
Santa Clara County Medical Association
Saving Private Practice Webinar: Managing Your Manager (For Physicians)
March 20, 2024 | Virtual | 12:15 PM – 1:15 PM

Saving Private Practice is a program designed to assist physician members from solo/small/medium medical practices. The webinar series are monthly educational sessions designed to assist with office operations, decision making, and practice management. Each one-hour session will be led by Debra Phairas, President of Practice & Liability Consultants, LLC. This webinar will teach how to effectively manage, evaluate and motivate your practice manager. An excellent practice manager can increase revenues, decrease practice overhead and manage staff to highest performance!
This quarter, SCCMA Book Club will read “What Looks Like Bravery” by Laurel Braitman, PhD. Laurel is a writer, teacher and secular, and clinical chaplain-in-training. She received her doctorate in History and Anthropology of Science from MIT and is the director of Writing and Storytelling at the Stanford School of Medicine’s Medical Humanities and the Arts Program where she helps clinical students, staff and physicians communicate more clearly and vulnerably for their own benefit and that of their patients. Laurel is also the founder of Writing Medicine, the global community of writing healthcare professionals. Her work has appeared in the New York Times, The Guardian, Wired, California Sunday, National Geographic, Radiolab, National Public Radio and many other places. She splits her time between rural Alaska and her family’s ranch in Southern California.
What Looks Like Bravery is a hero’s journey for our times. Laurel teaches us that hope is a form of courage, one that can work as an all-purpose key to the locked doors of your dreams.
California Medical Association
Legislative Advocacy Day
April 10, 2024 | Sacramento, CA
The CMA Legislative Advocacy Day is approaching fast! Sign up today! This is your chance to meet with your legislators and advocate for what you want to see in the practice of medicine. Come join us! We currently have meetings scheduled with Assemblymember Evan Low, Assemblymember Gail Pellerin, Senator Josh Becker, Assemblymember Marc Berman, Assemblymember Ash Kalra, Senator Dave Cortese, Senator Aisha Wahab and Staff members for Assemblymember Robert Rivas and Assemblymember Alex Lee.
We are offering free rides on a shuttle bus from the SCCMA office to Sacramento for the day. First come first served. To reserve your spot email emily@sccma.org.
Santa Clara County Medical Association
AI and Healthcare Session 2
May 11, 2024 | HYBRID – Zoom & SCCMA Office
Save the date! More details to come.



SCCMA would like to hear your input on content you would like to see featured in the Bulletin.
The first ten people to respond will get a $10 gift card to Starbucks.

OFFER ENDS APRIL 1ST, 2024
for Clean Air and Climate Action



Climate change is already harming our health, from worsened ozone pollution due to warmer temperatures, to more frequent and intense wildfires producing dangerous particle pollution. Medical and health voices are critical to raising awareness of the overwhelming health burden caused by air pollution and climate change. We are looking for physicians, nurses, public health workers, respiratory therapists and other health professionals to join our efforts and speak out for stronger climate action.
Visit Lung.org/ClimateChangesHealth to take part in our growing Health Professionals for Clean Air and Climate Action community, where you can:
• Sign up for the Health Professionals for Clean Air and Climate Action monthly newsletter
• Share your story about why addressing climate change is critical to protecting public health
• Read stories from other health professionals around the country
• Sign our letters to urge policymakers to clean up dangerous air pollutants For more information, please contact Elise Wallis, MPH, Manager, Health Partnerships, at Elise.Wallis@Lung.org.
