The News Magazine of the American Association of Colleges of Pharmacy


The News Magazine of the American Association of Colleges of Pharmacy

New opportunities await future pharmacists as schools build a playbook for sports pharmacy in the curriculum. 16
The News Magazine of the American Association of Colleges of Pharmacy
Pharmacists Help People Live Healthier, Better Lives.
1400 Crystal Drive, Suite 300 P Arlington, VA 22202
703-739-2330 P www.aacp.org
Founded in 1900, the American Association of Colleges of Pharmacy is the national organization representing the interests of pharmacy education. AACP comprises all accredited colleges and schools of pharmacy, including more than 6,600 faculty, approximately 63,800 students enrolled in professional programs and 4,800 individuals pursuing graduate study.
We welcome your comments. Please submit all letters to the editor to communications@aacp.org.
Academic Pharmacy Now highlights the work of AACP member pharmacy schools and faculty. The magazine is published as a membership service.
For address changes, contact LaToya Casteel, Member Services Manager, at lcasteel@aacp.org. ©2024 by the American Association of Colleges of Pharmacy. All rights reserved. Content may not be reprinted without prior written permission.
For advertising information and rates, contact Elissa Brooks, Senior Director of Development, at ebrooks@aacp.org.

CEO & Publisher Lee Vermeulen



Editorial Director
Editorial Advisor

Managing Editor Jane E. Rooney

Editorial Assistant Kyle R. Bagin
Art Director

Freelance Writer Joseph Cantlupe

Freelance Writer Athena Ponushis
Freelance Writer
Emily Jacobs

community impact
What do pharmacy closures mean for public health, and how can schools help the profession build back? 5 8
Two University of Florida College of Pharmacy faculty members finally convinced the FDA that a widely used nasal decongestant does not work.
AACP’s debut Artificial Intelligence Institute drew a big audience looking for answers about the rapid changes that AI is bringing to the digital environment and what that means for pharmacy education.

campus connection
New opportunities await future pharmacists as schools build a playbook for sports pharmacy in the curriculum.

Pharmacy Education Heads Back to Boston
More than 2,000 pharmacy educators, practitioners and students will head to Boston, July 20–23, to gain new perspectives and skills at Pharmacy Education 2024.


Dear Colleagues:
In just a few short weeks more than 2,000 pharmacy faculty, staff, students, administrators and practitioners will descend on Boston for the can’t-miss event of our profession, Pharmacy Education 2024 , AACP’s Annual Meeting. Over four days of programming, attendees will learn, network and collaborate to share ideas, solve problems, and find solutions to critical issues facing pharmacy education and practice. My favorite parts of our Annual Meeting are reconnecting with friends and colleagues from across the Academy, making new connections, and creating new collaborations. The energy of this meeting recharges our batteries, and sends us home excited for the future.
In this second issue of Academic Pharmacy Now, articles address timely topics such as the future of artificial intelligence in healthcare, career opportunities for pharmacists in sports pharmacy, and the impact of pharmacy closures on community pharmacy practice. With more student pharmacists considering non-traditional career opportunities, this issue’s feature article, A Wide-Open Field, highlights one possible path that is gaining traction: sports pharmacy. Many schools offer courses that focus on anti-doping, but USC’s Alfred E. Mann School of Pharmacy has gone a step further and created a certificate program to train pharmacists to understand the unique needs of athletes.
Another timely article given the recent New York Times cover story about PBMs examines the impact of pharmacy closures on public health. Mapping a New Future outlines the efforts by the ACT Pharmacy Collaborative to map pharmacy closures across the country and bring attention to the need to strengthen community pharmacy practice.
With the success of AACP’s recent inaugural AI Institute, All Eyes on AI recaps some highlights from that event. Session speakers raised questions about the possible beneficial applications of AI in pharmacy education as well as the ethical implications to consider. The Institute offered plenty of food for thought as we witness AI’s rapid evolution.
It’s hard to believe that summer will be in the rearview mirror as we wrap up the Annual Meeting in late July. I hope you find time to relax and recharge before the new academic year begins, as I know many of AACP staff—myself included—will be doing so too.
Sincerely,

Lee Vermeulen, B.S.Pharm., M.S., FCCP, FFIP CEO and Publisher
Two University of Florida College of Pharmacy faculty members finally convinced the FDA that a widely used nasal decongestant does not work.
By Matt Splett
Phenylephrine is a popular ingredient found in more than 260 over-the-counter cold and allergy medicines. Drug makers have long contended that it helps clear nasal decongestion—but two professors from the University of Florida College of Pharmacy spent two decades refuting that claim. Backed by science, they finally convinced the FDA that the common nasal decongestant does not work.
In 2005, Dr. Randy Hatton was co-directing the Drug Information Center at UF Health Shands Hospital when questions about oral phenylephrine began flooding the phone lines. Pharmacists and physicians from around Florida were calling the center asking if oral phenylephrine worked and what dose to take.
A federal law enacted that year mandated retailers move pseudoephedrine products behind the counter to combat illicit methamphetamine production. Pharmaceutical manufacturers reformulated common cold and allergy medicines using phenylephrine instead of pseudoephedrine. Yet, skepticism emerged within the healthcare community regarding the effectiveness of oral phenylephrine. “The Drug Information Center fielded many similar calls questioning whether oral phenylephrine worked as a decongestant,” said Hatton, a clinical professor in the college. “The UF College of Pharmacy students and residents staffing the center would examine the literature to provide informed responses to the healthcare professionals. In the case of phenylephrine, they did not have to look far for an answer.”
In 1993, Dr. Leslie Hendeles, a professor of pharmacy in the UF College of Pharmacy, published a review paper in the journal Pharmacotherapy addressing the choice of decongestants and mentioned the ineffectiveness of oral phenylephrine. While the drug posed no safety risks, he referenced earlier unpublished studies suggesting phenylephrine’s resemblance to a placebo, with it being inactivated in the gut during the first pass through the liver resulting in little of the drug reaching the bloodstream.
1976: The monograph for over-the-counter nasal decongestants begins
1993 : Leslie Hendeles publishes a review suggesting oral phenylephrine is ineffective
1994: The over-the-counter nasal decongestant monography is completed. Phenylephrine is generally recognized as safe and effective
2005: The Combat Methamphetamine Epidemic Act requires pseudoephedrine to be moved behind the counter and oral phenylephrine use increases
2005: Randy Hatton and Leslie Hendeles begin researching oral phenylephrine’s effectiveness
2007: Hatton and Hendeles submit a Freedom of Information Act request for oral phenylephrine evidence
2007: The researchers’ systematic review and metaanalysis show oral phenylephrine is ineffective
2007: Hatton and Hendeles, along with Almut Winterstein from the UF College of Pharmacy and Jonathan Shuster from the UF College of Medicine, submit a citizen’s petition to the FDA to reevaluate the effective dose of phenylephrine
2015: Hatton and Hendeles submit a second citizen’s petition to the FDA to withdraw oral phenylephrine
2023: An in-depth internal FDA review concludes that oral phenylephrine is ineffective and the Nonprescription Drugs Advisory Committee votes unanimously that the evidence supports that oral phenylephrine is ineffective

Hendeles and Hatton met one day to discuss their suspicions about phenylephrine. As academic pharmacists, they prioritized evidence-based approaches to ensure the safety and efficacy of drug therapies for patients. They left the meeting with a mutual determination to investigate the inefficacy of oral phenylephrine and share the evidence with the FDA.
For almost 20 years, the endeavor to persuade the FDA of the inefficacy of oral phenylephrine encompassed extensive research, editorials, citizen petitions and advocacy efforts aimed at influencing policymakers and public sentiment. Hendeles and Hatton acknowledge they may have been a bit naïve at the beginning, believing the task would be straightforward. Nevertheless, as the journey unfolded, their commitment to the cause never wavered. “Every time new evidence emerged that supported our assumptions, it would reignite us,” said Hendeles, now a professor emeritus in the college. “We were committed to the issue and viewed our efforts as a public service.”
In 2006, Hendeles and Hatton published their first editorial in the Journal of Allergy and Clinical Immunology. They contested the FDA’s endorsement of the 10-milligram oral dosage approved in 1976, citing inconclusive evidence to support phenylephrine’s effectiveness in alleviating nasal congestion. A few months later, Hatton submitted a Freedom of Information Act request to the FDA. They sought all the available data employed by the agency in evaluating the safety and efficacy of oral phenylephrine.
“We were able to use all that information and do a systematic review and meta-analysis to support what Leslie had published in 1993 and what pharmacists were calling the Drug Information Center and reporting that oral phenylephrine did not work,” Hatton said.
Dr. Russell McKelvey, a pharmacy resident at the UF Drug Information Center, contributed to the systematic review and meta-analysis that was published in 2007. The same year, Hendeles and Hatton filed their first of two citizen petitions asking the FDA to reevaluate the dose of phenyleph-
“Every student who went through this college during our tenure was taught that oral phenylephrine was ineffective. It was gratifying to hear from former students expressing their excitement that tangible progress had finally been made with the FDA.”
—Dr. Leslie Hendeles
rine. They thought a higher dose might compensate for the poor absorption. The move spurred the FDA to form a Drug Advisory Committee to review phenylephrine’s effectiveness, but the panel ultimately decided more data was needed before a decision could be reached.
As the years passed, new studies contributed to the mounting evidence against oral phenylephrine. Despite persistent advocacy efforts from Hendeles and Hatton urging action from the FDA, progress seemed elusive. However, a significant turn of events occurred in 2023, when the FDA appointed a second drug advisory committee to review the issue. The 16-member committee evaluated the existing data and heard testimony from drug makers advocating for the efficacy of oral phenylephrine alongside experts like Hendeles and Hatton who advocated against its ongoing use—setting the stage for a momentous decision.
On Sept. 12, 2023, the FDA’s Nonprescription Drugs Advisory Committee voted unanimously that oral phenylephrine is ineffective. The decision came as no surprise to Hendeles and Hatton, who had dedicated a considerable part of their professional lives advocating against its use in cold remedies. “For the vote to be unanimous, that was a significant achievement,” Hatton said. “I was delighted when it happened, feeling vindicated for what we had been saying for a long time.”
The committee’s decision made immediate headlines across the country. Americans spend about $1.8 billion on cold medicines annually, so the idea that one of the key ingredients was deemed ineffective carried considerable implications. Hendeles and Hatton found themselves inundated with interview requests from many major media outlets ranging from the New York Times and Wall Street Journal to National Public Radio and CBS News. It seemed everyone wanted to hear from the two University of Florida pharmacists who had figured out that a key ingredient in cold and allergy remedies does not work. “The media attention was more than I expected,” Hendeles said. “If it wasn’t for the two of us and
recent studies with modern study designs, the FDA would have never addressed the oral phenylephrine issue.”
Headlines such as “The Two Scientists Taking Down Cold Medicines That Don’t Work” and “Florida Pharmacists Bring National Attention to Ineffective Drug” put the spotlight on the two decades of research and advocacy led by Hendeles and Hatton. They accepted as many media interview requests as their schedules allowed, as they aimed to inform the public about oral phenylephrine’s ineffectiveness.
Following the ruling, Hendeles and Hatton received messages from numerous colleagues and former students, including those who had been affiliated with the UF Drug Information Center or studied in the college’s Pharm.D. program. “Every student who went through this college during our tenure was taught that oral phenylephrine was ineffective,” Hendeles said. “It was gratifying to hear from former students expressing their excitement that tangible progress had finally been made with the FDA.”
Although the committee’s decision cleared a significant hurdle toward eliminating decongestants containing phenylephrine from shelves, the actual removal process is expected to take some time. The FDA must finalize its decision and allow for public commentary. Hatton anticipates that it may be another year before oral phenylephrine is completely phased out from cold medications. In the interim, he hopes that heightened public awareness about phenylephrine will encourage consumers to be more discerning in their cold and allergy medicine purchases.
“We are just two pharmacists looking out for the best interests of patients to ensure their cold medicines are safe and effective,” Hatton said. “Leslie and I have always been focused on helping the public get the most out of their drug therapy.” P
This article is reprinted with permission from the University of Florida College of Pharmacy. It appears in the latest issue of the college’s alumni magazine.
What do pharmacy closures mean for public health, and how can schools help the profession build back?
By Athena Ponushis
It was over a routine, focus group phone call, when three researchers—Sophia Herbert, Nicole Pezzino and Jennifer Bacci—decided to bring visibility to the drastic rate of pharmacy closures. Familiar with the community pharmacy landscape and working with independent pharmacy owners through the Academia-Community Transformation (ACT) Pharmacy Collaborative, they knew that pharmacies had been closing for years, but they also knew the rate of closures was going to continue to climb. Acknowledging this reality compelled them to action. “We need to do something,” Dr. Sophia Herbert, assistant professor at the University of Pittsburgh School of Pharmacy, remembers the three researchers affirming. “We need to put this message out there so people other than pharmacists realize what’s going on, and maybe will do something about it.”
The more they talked, the more their plan took root. They each had P4 students who would be joining them on rotation soon. They came up with a project: Their students would comb the media for pharmacy closures in every state, compile what they found into a map of locations, add a series of links to news stories reporting on closures and upload it all on the ACT Pharmacy Collaborative website.
The pharmacy closures map gained traction rather quickly, but the picture was not complete. Many pharmacies were closing that were not receiving attention from local media, so the team opened up a “report a closure” feature, inviting the public to submit news of more closures. Now the density and color of the pins on the map are hard to deny: Pharmacy closures are not an isolated problem, they are a nationwide occurrence. “Making that visual impact was really our goal with the map,” Herbert said, “to convey that message and point people toward action, whether it be spreading the message, participating in some legislative action, or supporting a local community pharmacy in any way. Times are certainly challenging right now and many pharmacies are struggling to keep their doors open.”
There have been many shifts in the community pharmacy marketplace, but the main driver impacting closures would be the decrease in reimbursement for drug products. That decrease varies from place to place, but as Herbert explained, “Nationally, the overall trend is reimbursement for drugs is tanking. And in some cases, pharmacies are even losing money dispensing a drug product. They are getting reimbursed less than what they paid to obtain that medication.”
Such losses do not make for a viable business model. There are different reasons for the diminishing returns, but the main culprits right now are pharmacy benefit managers (PBMs). Originally, the purpose of PBMs was to help pharmacies and health plans work together. Every pharmacy must have a contract with every health plan that it is billing and dispensing medications through, so the PBM was designed to serve as the middleman between the pharmacy and the health plan to orchestrate the contract. PBMs may have come out of a genuine need, but they have not been heavily regulated and the end result has been PBMs profiting while pharmacies are closing, ultimately leaving patients suffering. “This is not a situation of pharmacies wanting to make more money,” Herbert said. “They want transparency, they want to know they are going to be able to turn a modest profit, or at least break even, on the medications they are dispensing.” An unfair drug reimbursement system means that pharmacies cannot keep their doors open if they are relying on repayment.
Dr. Jennifer Bacci, associate professor at the University of Washington School of Pharmacy, said it’s no secret that pharmacies are closing. It’s happening in urban centers like Seattle and in rural communities. From independent to corporate community pharmacies, no pharmacy is immune from the effects of the marketplace.
“It’s an important time for us as a profession to own what happens next, because if we don’t step up to create the future

In April, Pennsylvania State Senator Judy Ward issued a statement urging reforms in order to lower prescription drug costs. In noting several pharmacy closures across the Pittsburgh region, Ward said, “We’re seeing this issue repeated across the commonwealth and the nation. The University of Pittsburgh has created a website (ActForPharmacy.com) that tracks community pharmacy closures and provides a sobering view of the challenges Pennsylvania community pharmacies face in staying open—and of Pennsylvanians who desperately need their prescriptions.” Read the full statement here: https://senatorjudyward.com/2024/04/26/reforms-needed-to-lower-prescription-costs-for-pennsylvania-pharmacies-families/
“It’s
an important time for us as
a profession to own
what happens next, because if we don’t step up to create the future for ourselves, then other people will. That’s the message I try to communicate to my students. There is an opportunity to come into community pharmacy and help create the future.”
—Dr.
Jennifer Bacci
for ourselves, then other people will,” Bacci said. She sees pharmacy closures as both a problem and an opportunity. “That’s the message I try to communicate to my students. There is an opportunity to come into community pharmacy and help create the future. It will not look the way it looks now, and that’s O.K. But we need to take ownership of what we want, we need to step up and make it be what we want it to be. That’s our opportunity.”
The public health impact cannot be understated. People need face-to-face interaction with pharmacists for their medications and medication-related services. When people lose the ability to go into a healthcare space embedded in their community and talk with a trusted healthcare provider, they lose a lot.
Dr. Nicole Pezzino, associate professor at Wilkes University Nesbitt School of Pharmacy, started working in a community pharmacy when she was 16 years old. The issue of pharmacy closures is personal to her. One pharmacy where she did a rotation has closed. Her mentor ran a diabetes clinic in a community pharmacy. His clinic had a collaborative practice agreement with 50 providers in the greater Pittsburgh area. There was a waitlist for new patients but he would find a way to
squeeze them in. She would follow up with them every week until they reached their goal. “I remember telling him when I was a student, ‘I’m going to take over for you. We’re going to be partners first, and when you’re ready to retire, I got you,’” Pezzino said. Her mentor passed away a few years back. Catching up with the pharmacy owner recently, she learned that the pharmacy had closed. Pezzino said it’s “saddening and frightening” to think of more pharmacies closing and patients losing out on those services.
Mail-order pharmacies come up in this discussion. “Mail order can certainly help some patients and I’m glad that it exists as an option, but we cannot rely on mail order to take care of everyone’s mediation-related needs,” Herbert said. “It’s not realistic.” Medication management, immunizations and other services that can be provided by an embedded pharmacist in a community is huge, and when that pharmacy closes, it all goes away.
Herbert believes that the profession will continue to feel the effects of closures and changes in the marketplace for some time, but there is still a great need for pharmacists in this country. “I think with this kind of crashing of a system, there’s going to be a rebirth of what community pharmacy looks like,” she said. She does not know a pharmacist working in a direct patient care setting who is not feeling the changes in the healthcare landscape in some way, but she does hold hope that these changes will bring a new era of pharmacy practice and a way that works better for the profession and the patients. The ones who will usher in this era will be students.
Faced with this reality, educators are having hard conversations—trying not to be dreary, finding ways to be encouraging—but they must involve students and show them the landscape they are entering while assuring them that they can impact the profession’s future. “We need to empower them to be part of the change,” Herbert said.
Pittsburgh’s School of Pharmacy takes its entire class of second-year students to legislative day, an event the Pennsylvania Pharmacists Association puts on every year at the capitol in Harrisburg. Faculty weave it into the course for students who are spending time at community pharmacies, seeing the impacts of drug reimbursement and hearing preceptors talk about it at their sites. This past year, they advocated for a bill that would regulate PBMs and support pharmacists, making cash flow transparent and giving means to fight back any acts of unfairness.
“Demonstrating that students can be involved in the advocacy for change, whether that be in a legislative way or a local way, at their own pharmacy, whatever it might be for them, I think is important.”
—Dr. Sophia Herbert
“Demonstrating that students can be involved in the advocacy for change, whether that be in a legislative way or a local way, at their own pharmacy, whatever it might be for them, I think is important,” Herbert noted.
It can be hard to conceptualize what pharmacy closures really mean, but the impact continues to spread. Herbert has family members and friends who rely on pharmacies for healthcare. “If they have a question about something related to their healthcare, they are not making an appointment with their primary care physician. They are going to the pharmacy to talk with a trusted professional,” she said. At legislative day, some of the legislators talked about closures in their districts that had affected them or someone they know personally. Legislators who had been touched by pharmacy closures were much more inclined to enact change to prevent further closures.
At Wilkes, Pezzino sees her students as inherent advocates. She teaches them to amplify their voices in their profession by sharing their personal stories. She asks her students, many of whom work in community pharmacy, to think about times when things went really well, or times when things didn’t go so well. They talk about the issues together, as a class, digging for root causes. Students naturally progress from sharing their stories in class to writing letters to legislators to posting stories on social media, strengthening their voices.
When Pezzino broaches the subject of PBMs, she uses a colleague’s method and puts unfair reimbursement in the context of grades: “Let’s say I tell you today that you are going to get an A on your transcript because you did everything you were supposed to do, you turned everything in, you did everything right,” she tells students. “In your mind, you are getting an A, but six months later, when you get your transcript, it says C.” She then explains, “That’s what it’s like. Some of our best performing pharmacies are hitting all the metrics but still losing money.”
Pezzino sees a difference in how students react to pharmacy closures depending on their academic year. Her younger students seem more excited about the opportunities. “But my newer grads are saying, ‘I signed with a store that just closed. What’s going to happen to my job?’” she said. “There might be a little bit of fear there, but when you have that, you are forced to innovate.”
As the pharmacy profession invests energy into remedying the drug reimbursement problem, they must also invest in ensuring that pharmacists are paid fairly for provision of services. “While we navigate this difficult time and extraordinary change in the marketplace, remember there are other ways for pharmacies to earn
revenue besides dispensing,” Herbert said. “While we fight against poor reimbursement and fight for regulating PBMs, we must also try to expand access to pharmacist-provided services, point-of-care testing, hormonal contraceptive prescribing, immunizations, diabetes education…there are so many services pharmacies can offer beyond dispensing of drug products.”
As far as the ACT Pharmacy Collaborative pharmacy closures map goes, Herbert, Pezzino and Bacci will keep updating it as long as it’s useful. There are other resources in the pipeline, including a recently released map of closures specifically linked to pharmacy claims that may show the effect on communities to a greater extent: https:// storymaps.arcgis.com/stories/21620f1e0 7c14d7f81adc4503faaf51e
“I truly believe there is great possibility for what we will be able to do in the community pharmacy space in the future,” Herbert said. “We’re just at this turning point, and unfortunately, I think it’s going to take this crashing and closing of many pharmacies for people to wake up to what’s going on. But we will be able to rebuild what the future looks like together.” A future where community pharmacies are seen as a hub of community health and community pharmacists are treated as healthcare providers. P
Athena Ponushis is a freelance writer based in Ft. Lauderdale, Florida.
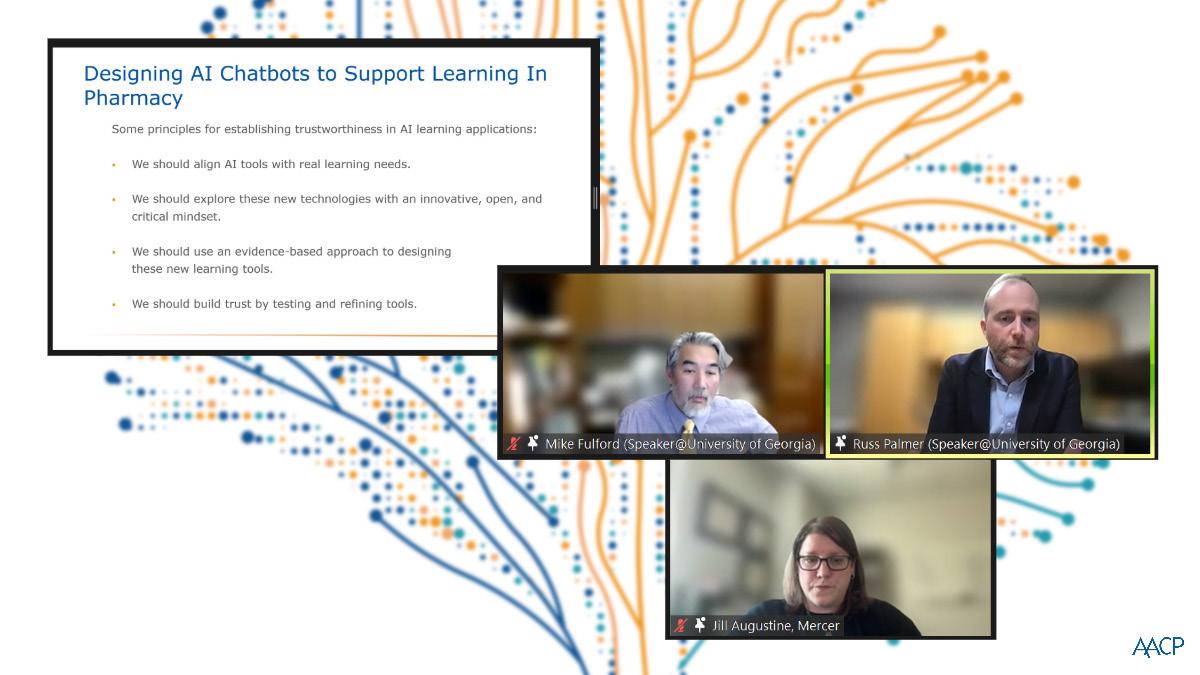
AACP’s debut Artificial Intelligence Institute drew a big audience looking for answers about the rapid changes that AI is bringing to the digital environment and what that means for pharmacy education.
By Joseph A. Cantlupe
As artificial intelligence bursts into day-to-day life, and increasingly into the healthcare sphere, pharmacy schools run the gamut from slowly testing the AI waters to diving right in. But nearly everyone agrees they must be prepared to confront the mushrooming reality of artificial intelligence now That was the message as AACP presented its inaugural Use of Artificial Intelligence in Pharmacy Education Institute, held virtually April 3-5. Some participants expressed deep concern about the prospects with AI, but most agreed that it will be a dominant issue in healthcare for years to come.
“I think everybody recognizes that AI is going to impact pretty much everything we do,” said Dr. Anne Lin, dean and professor at the College of Pharmacy and Health Sciences at St. John’s University and an AACP past president. “I heard from people who attended the Institute who felt that it was in some ways almost overwhelming. AI is moving so quickly and so fast that if we don’t stay on top of it, we will in fact fall behind.”
During the sessions, academic pharmacy leaders who welcome AI said it can overhaul instruction with dynamic efficiency and depth, in evaluations and assessments and in real-life decision making. AI-enhanced simulation technologies can create more realistic and diverse clinical scenarios, offering students the opportunity to practice in a wider range of situations. It also can monitor students’ techniques and provide immediate feedback on accuracy, safety and adherence to protocols, according to some who presented at the Institute.
College and university officials are beginning to determine how AI is integrated into curricula, including ways to expand the lessons for students. Student pharmacists are creatively integrating AI into their higher education. But some cautioned that there are ethical issues to overcome as well as the potential for misleading information that must be
monitored closely, as professors and students recognize AI’s limitations. Meanwhile, schools must confront challenges in the classroom as students use AI before clear guidelines have been established. Pharmacy schools are evaluating procedures and establishing protocols to keep pace with this fast-growing phenomenon.
The Institute was one of AACP’s most highly attended, said Dr. Sarah Shrader, senior director of academic programs and professional development at AACP. “We feel it was a success. We had the challenge of trying to figure out what the needs were in our Academy, and they are so varied,” she said. “Some people had never even opened any basic AI tools that are out there such as ChatGPT.”
After the sessions, Shrader said a poll of attendees suggested that many were skeptical or scared of AI. “You know that shows a lot of people obviously have a lot of work to do,” she said, adding that some were “caught off guard” by the approaching AI possibilities. On the other hand, “other people are using it every single day and have many sophisticated programs. We are trying to figure out how we can meet their needs, and this is a good first step.” Shrader anticipates a series of professional development sessions in future years. “It’s a very critical and rapidly changing topic; we will be diving deeper to address certain aspects with AI and taking a more specific approach in various areas.”
During the sessions, panelists explored AI’s origins when scientists began laying the groundwork in the early 1950s and later explored various medical applications in the 1970s. Moderating a panel on how AI is used in pharmacy practice today, Dr. Risa Vatanka, co-founder and CEO of Digital. Health, described the technology’s early days as being “characterized by algorithms and clinical decision support to
the evolution to machine learning—and now generative AI and other AI-based solutions.” In moderating a session on how student pharmacists are using AI, Dr. Mary K. Gurney, professor, department of pharmacy practice at Midwestern University College of Pharmacy, said, “Pharmacy students, the architects of tomorrow’s healthcare landscape, are creatively integrating AI into their higher education, revolutionizing workflow processes and unlocking myriad potential applications.”
Dr. Michael Fulford, assistant dean for institutional effectiveness and strategic initiatives and director of faculty affairs at the University of Georgia (UGA) College of Pharmacy, led the session “Revising Assessments in an AI World,” which provided insight into how AI can be used with assessment today and what may happen in the future. When it comes to the use of immersive technology and AI, “medicine is ahead
“Pharmacists are risk averse, and they should be in most cases, but when it comes to education and technology, we’re going to have to push a little bit out of the comfort zone to take that next big leap in regard to innovation and AI.”
—Dr. Michael Fulford

of where we are today,” Fulford said, comparing medical practice and education to pharmacy practice and education. “The pharmacy profession is playing catch up in this arena. We must be open to these changes in technology and embrace using them. However, pharmacists are risk averse, and they should be in most cases, but when it comes to education and technology, we’re going to have to push a little bit out of the comfort zone to take that next big leap in regard to innovation and AI.” He applauded AACP’s leadership for taking these first steps with AI initiatives including the Institute, programming at annual meetings and reaching out to new sponsors and partners who are working in immersive technology and AI.
At UGA, Fulford is leading an interdisciplinary presidential cluster hiring initiative focused on translational education research in the health professions. This initiative seeks to bring new faculty to UGA who will build bridges between innovations in practice and education using immersive technology
and AI. The College of Pharmacy is partnering with the College of Veterinary Medicine and the College of Education to build this faculty cluster so they can “create an immersive learning experience,” which includes AI, he said. One goal of the cluster is to bring a “transformative perspective to the experience in the classroom and the curriculum and better prepare future pharmacists to use immersive technology and AI in the practice of the future.”
While there are enormous possibilities with AI in pharmacy education, Fulford believes the curriculum should anchor to three key literacies identified by Joseph Aoun in his book, RobotProof: Higher Education in the Age of AI. Aoun posits that every student should learn three literacies as a part of their curriculum: technical literacy, data literacy and human literacy. Human literacy is especially important because “what AI and computers—as good as they can try to be—will never truly replicate is the concept of humanity and what we bring to healthcare and education,” Fulford noted.
He added that the biggest hurdle we face with AI in general, but especially in relation to assessment, is trust. “We can talk all we want about technology and AI and all the amazing stuff it can do, but really the first thing we must talk about is trust. Trust in someone or something else is developed through repeated behaviors and experiences, so until we spend time getting to know AI and build a ‘relationship’ with AI, we will continue not to trust it because it will remain a stranger to us.”
From the professor’s chair to the lab to the classroom, AI’s potential impact is formidable. Academic leaders are working to integrate the variations
of study, data and patient care possibilities into the curriculum. “We have started having those conversations to think about how you handle AI in the classroom settings,” said Shrader. “Our student pharmacists are going to be pharmacists who utilize these AI tools in the healthcare systems, and that’s a skill set they need to develop.” For many universities, the curricula have not been adjusted to incorporate AI learning.
Attendees and panelists examined a litany of possibly unsettling questions. Among them: What if a pharmacy school decided to incorporate AI into much of its coursework but was concerned that the institution became too reliant on AI assistance? And what about the impact on students’ critical thinking or clinical judgment? What if an instructor felt conflicted about a top student using AI to complete an assignment who previously had a clean academic record?
Sometimes, people use the AI tools but “are not recognizing the limitations because all tools have limitations,” said Lin, who led the session “Artificial Intelligence Competencies for Health Professions Education.” She added, “The questions themselves—the way they are worded—can result in prompts that determine the answers and determines what comes back to you.”
“There are guides now of how to write good question prompts; that’s a skill, how to recognize information that’s coming back that is not accurate,” Lin continued. A portion of an AI piece, for instance, “may sound plausible and real but there is no such article. How does a student learn how to evaluate these tools, about whether what they are reading is accurate? That’s a big part of it.”
Those are some of the questions St. John’s University is examining as it


takes significant steps to evaluate the use of AI in the classroom and the ethical implications. There is even discussion of prohibiting AI. The university’s artificial intelligence task force is “looking at what all this means for not just my school but the entire campus,” Lin said. “There are going to be guidelines on how to use these tools. You don’t want to put anything out that violates HIPAA regulations, so ethical uses in that sense also become important.”
Shrader noted that these conversations will be ongoing as schools wrestle with what the future holds now that AI is here to stay. Among the major concerns are not only the accuracy of some of the AI tools but the need to recognize their limitations and identify frauds. “The accurate verifying of information and potential bias of these systems is an important conversation moving forward. These are skills that we have to teach our student pharmacists to be able to navigate along with patients.” P
Joseph A. Cantlupe is a freelance writer based in Washington, D.C.


New opportunities await future pharmacists as schools build a playbook for sports pharmacy in the curriculum.
By Jane E. Rooney
As the world gears up for the Olympics this summer in Paris, the athletes are working nonstop to keep themselves in peak physical shape. Their efforts to maintain their physical fitness involve athletic trainers and coaches, certainly, but also physicians, dieticians and in some instances, pharmacists. Participants in the Olympics must pay particular attention to whether their medications are in compliance with the International Olympic Committee (IOC) regulations around performance-enhancing drugs. But athletes at all levels can benefit from a pharmacist’s knowledge, getting answers to questions ranging from how medications impact performance to what types of supplements are safe and might be helpful.

While the pharmacist’s role in sports is not a new concept, sports pharmacy is gaining traction as a career path that allows pharmacists to tailor their expertise to a unique demographic. “This is a patient population we’ve been missing and we can reach them from a medication standpoint,” said Dr. Athena Cannon, a clinical pharmacist affiliated with the University of Minnesota College of Pharmacy and founder and chair of the U.S. Sports Pharmacy Group. “More than half of athletes are taking a dietary supplement. Awareness and education [around that] is huge. That’s true for every level from middle school all the way up to professional athletes. Anyone can seek help with their performance, focus and general health. That’s a huge area for pharmacists.”
Cannon created the U.S. Sports Pharmacy Group in 2020 as an informal networking group for sports medicine professionals who were interested in how to get pharmacists more involved. An official nonprofit organization since 2022, the group now has 95 members including students, pharmacists and researchers who want to share their expertise and collaborate to support athletes’ health and safe medication use. Cannon has seen interest in the subject gain momentum in recent years.
“Internationally there are well-established curriculums out there, primarily around anti-doping and what medications are prohibited,” she noted. Many U.S. pharmacy schools devote at least one lecture course to medication abuse
“We’ve created an important consortium of expertise to lend to this certificate program that students can tap into and learn how to best excel in the area of sports pharmacy.”
—Dr. Kari Franson
or drugs that are prohibited by the U.S. Anti-Doping Agency. She would like to see universities support initiatives that will help pharmacists become a goto resource for athletes. “We need education that’s reliable and keeping up with the growing information about things like treatment for concussions or post-operative pain management. There’s a lot of research and a push from national organizations right now to keep up with those big changes. We already have faculty teaching some of these subjects.”
Dr. Hoai-An Truong, professor and director of public health, University of Maryland Eastern Shore School of Pharmacy & Health Professions, recently earned a Drugs in Sports Certificate from the IOC, making him one of about 200 individuals globally to receive the certification. Truong, who is also an atlarge board member for the U.S. Sports Pharmacy Group, conducts research regarding the role of the pharmacist in sports.
“The student athlete wants a pharmacist on sports teams to provide education on health, medication and pain management,” he said, adding that it is an area that lends itself to interprofessional collaboration. “There is a growing interest among students in nontraditional career pathways. Working conditions for pharmacists are not the best at this time. Students who have an interest in sports find there is a missing component [that pharmacists can fill] by teaching athletes about pain management.” Truong emphasized the need to raise awareness about how pharmacists can make a difference on these healthcare teams. He works with physical therapy faculty

and is developing a program to educate student athletes about alternative medicine and pain management. He also sees the regulatory area as a space where pharmacists can learn more and open doors to new career options.
“The conclusion we learned from our research is that it is important to have pharmacists on the sports team for consistency,” he continued. “Communication and collaboration can improve student athletes’ knowledge and performance outcome. It’s beneficial for pharmacy and physical therapy to collaborate regularly and consistently with student athletes and coaches to improve their health and optimize performance.”
The University of Southern California (USC) Alfred E. Mann School of Pharmacy and Pharmaceutical Sciences is one of a few pharmacy schools blazing a trail to integrate sports pharmacy in the curriculum and open up new career pathways to students.
This spring, USC announced the creation of a 12-credit certificate for licensed intern pharmacists and practicing pharmacists that will cover subjects including dietary supplements, physical assessments and drug management. Students will also be required to do rotations in interprofessional sports pharmacy ambulatory care and athlete-centric community pharmacy. The impetus for the program, according to Dr. Kari Franson, senior associate dean for academic & student affairs, and professor
of clinical pharmacy, was recognizing the need to train pharmacists to be more aware of the unique needs of an athlete.
“Our athletic department is an interprofessional group already, and they embrace the expertise that the pharmacist brings to the table,” Franson said, noting that USC is a major Olympic preparatory school. “A general therapeutics course covers how to manage medication in athletes and understanding anti-doping regulations. A physical assessment and drug management course teaches learners how to assess how an athlete is responding to treatment and how to measure the physical impact of medications.” The third required course covers supplements, which has become a $200 billion industry in the United States. “People are seeking ways in which these products can help them and optimize their performance, so we need to offer help in interpreting how to use them.”
The school hired Michael Kessler, a Mann Pharmacy School alumnus who holds a degree in exercise physiology and has worked with the Los Angeles
Chargers, to teach and be part of the interprofessional medical team. Rotations may involve working with a community-based pharmacy or partners connected with the L.A. Chargers and Rams. A physician who uses digital therapeutics and focuses on measuring drug responses will work with students on medical computing. “We’ve created an important consortium of expertise to lend to this certificate program that students can tap into and learn how to best excel in the area of sports pharmacy,” Franson said.
Kessler noted that there can be silos in sports medicine, leaving gaps in what physicians and providers know. “As pharmacists, we are the medication experts. We know the side effects and can educate the patient and staff or providers,” he pointed out. “We can serve as that third-party person to close the gap on what the medication is and how it will affect the athletes. The provider may not know what’s on the prohibited list. We can step in with our familiarity with what can cause a positive drug test. We can help ensure athlete safety, efficacy of treatment and what that looks like for different sports.”


Students who participated in the pilot program last spring shared positive feedback and an enthusiasm for the new possibilities this specialty offers. Alexis Brown, a rising P4 student at the school, shared that “the sports pharmacy elective courses helped show me how I can apply the clinical knowledge I’ve learned to better support athletes of all experience levels. It helped me to develop practical skills like knowing how to reference the USADA and NCAA anti-doping lists. I feel like my goal of becoming a sports pharmacist is much more attainable having taken these courses.”
As the program grows, the hope is to train more pharmacists to collaborate with physicians and athletic trainers to provide interventions that keep athletes safe. “The [pilot course] demonstrated that this is an area of entrepreneurial growth and excitement. People are craving this information,” Franson said. “We have current faculty lending their expertise. Our dean is an expert on steroids and lends that knowledge to the research contributing to sports pharmacy. More work is needed to understand things like how cannabis can impact
sports performance. We have an opportunity to have scientists and clinicians work together to generate more expertise.”
Given that sports medicine is a highly regulated area, particularly at the Olympic level, Franson said there is a strong need and desire for the kind of information that pharmacists can share. The school aims to become a hub for training and accrediting sports pharmacy specialists. “Our community pharmacies are a fantastic place for this training. The pharmacy has products in the aisles that the pharmacist should be able to adequately counsel the athlete on how to optimize utilization of something like a non-steroidal therapeutic,” she said. “Or understanding how something like CBD could be problematic, understanding the supplements and the steroids contained in those. Having that knowledge makes the pharmacist such an asset to their community. Combining the education, the clinical work and the research from the pharmacy perspective will be such a growth area for universities moving forward.”

The career opportunities for student pharmacists who have a passion for sports medicine may be slightly different than the traditional roles in pharmacy practice. Cannon, for instance, consults with an anti-doping organization to help code medications that athletes can and cannot take and helps navigate questions about the medications on the prohibited list. She believes these types of opportunities will expand as education around anti-doping continues to grow.
“I’d like to see pharmacists partnering with sports medicine practitioners so we can have a more collaborative approach to questions from athletes about medications and their dietary approach,” she said. “We need to educate universities about over-the-counter products and empowering students to make the right decisions when it comes to medications. Those are the big areas I already see becoming opportunities.” Other career options may include a pharmacist working directly with a school’s athletic department; some professional sports teams employ pharmacists as well.
Dr. Mitchell Howard, clinical assistant professor at the University of Toledo College of Pharmacy and Pharmaceutical Sciences, and vice chair of the U.S. Sports Pharmacy Group, has published research on sports medicine and the pharmacist’s role. He found that medication inventory is another growth area. “Sites that had a small pharmacy on hand that would order medications need someone to restock over-the-counter items and go-bags for travel teams,” explained Howard, who also earned the IOC’s Drugs in Sports Certificate. “Some athletic trainers identified adherence concerns with athletes. A pharmacist could make sure an athlete was sticking with an antibiotic after an infection, for example. Regard-

“It’s a collaborative effort to be working with the sports medicine physicians and other providers, helping with guidelines and possibly treating an existing disease state. A pharmacist on the team can help athletes control these things to perform at their best capabilities.”
—Dr. Mitchell Howard
ing supplements, there’s a lot of information out there that may or may not be true. Having someone who could work with athletes to answer those questions, review the literature and debunk myths about supplements…our pharmacotherapy background can help us provide education to a healthcare team.”
Pharmacists can also assist with interpreting lab results and recommending appropriate over-thecounter medications for athletes. “It’s a collaborative effort to be working with the sports medicine physicians and other providers, helping with guidelines and possibly treating an existing disease state,” he continued. “A pharmacist on the team can help athletes control these things to perform at their best capabilities.”
In the classroom, Howard said he will often integrate sports medicine into topics already being covered in the curriculum. “For example, I have given a case scenario with an athlete getting drug tested and it comes back positive for a banned substance. I have students look at a medication list to see what could be causing a potential false positive.”
The best advice for recent graduates who want to explore a career in sports pharmacy may be to keep an open mind. As Cannon pointed out, more professional teams may start to invest in hiring pharmacists to work with elite athletes. “There are jobs out there that might not be defined as sports pharmacy but a pharmacist could be involved,” Howard noted.
He referenced a job posting with the World AntiDoping Agency for a medical manager that monitors therapeutic use exemptions and reports to the chief medical officer. “Our graduates would be qualified to take on that role. The job titles don’t always have to say pharmacist. Thinking about our skill sets, it could be anything clinical, or maybe evaluating literature. It does not have to be just dispensing medication. It could be broader—something like getting involved with policymaking with organizations.”
Another way to get involved with sports pharmacy, he suggested, is through compounding. “One of our local pharmacies is the official compounding pharmacy for the Guardians. They have shipped and dispensed medications to other teams as well. A compounding pharmacy in California is marketing itself toward athletes. Some of the bigger health systems that are involved with major league athletics are also starting to open up to wellness pharmacy in general.”
Cannon sees further growth opportunities in ambulatory care. “I’m seeing a lot more pharmacists stepping into the role from a clinical perspective,” she said. “In Florida they do integrate pharmacists into the team setting. Community pharmacists see athletes all the time. We need more of them to step into those roles. And pharmacy schools can help this field begin to thrive.”P
Jane
E. Rooney is managing editor of Academic Pharmacy Now.
Get ready to connect and collaborate with colleagues from across the country and around the world to share ideas, solve problems, and find solutions to critical issues facing pharmacy education and the changing healthcare landscape.
Pharmacy Education 2024 , July 20-23, promises to deliver outstanding programming, opportunities for networking and renewing old friendships, and hopefully some time to take in the sights and sounds of Boston.
Check out some of the Pharmacy Education 2024 highlights:
• More than 150 micro-, mini- and special session formats, conversation world cafes and interactive workshops to meet your learning needs.
• Pre-conference sessions, including the Teachers’ Seminar, Mission Critical: Strategies to Promote Critical Thinking Across the Curriculum, the Admissions Workshop and the AFO SIG Program.
• A thought-provoking Opening General Session, Seeing Around Corners: Leveraging Leading Indicators, followed by a book signing with keynote speaker Dr. Rita McGrath.
• More than 400 posters displayed on two full days of the meeting.
• Timely session topics addressing the use of artificial intelligence in pharmacy education, practice and research; enhancing academic freedom at colleges and schools of pharmacy; developing best practices for incorporating, teaching, and assessing social determinants of health; and much more!
Up to 13.50 hours of CPE credit can be earned by attendees for Pharmacy Education 2024 , with up to 4.50 hours for the Teachers’ Seminar.


Can’t Miss Sessions
Opening General Session: Seeing Around Corners: Leveraging Leading Indicators
Sunday, July 21
8:00 a.m.-9:30 a.m.
Speaker: Rita McGrath, Ph.D.
Best-selling Author and Longtime Professor at Columbia Business School


In this talk, Rita McGrath will offer a way of thinking about future uncertainties and how we can prepare for them through the creation of an ‘early warnings’ system that provokes your mind into summoning ingenious and novel responses to different possible future states, allowing leaders to face uncertainty with greater confidence.

Clinical Science and Trials in Pharmacy–Preparing the Clinical Research and Drug Development Workforce
Monday, July 22
10:30 a.m.–Noon
Join us for a discussion on preparing the diverse, interdisciplinary, culturally competent workforce needed to translate scientific innovation into effective clinical care that reaches all patients. A panel of experts in clinical and translational science will provide a vision of the role of pharmacists in clinical research and how pharmacy schools can train the clinical research workforce. We will also celebrate the 2024 recipients of the Volwiler Research Award, Paul R. Dawson Award for Excellence in Patient Care and AFPE Mentor of the Year.
Argus Forecast Session
Monday, July 22
9:15 a.m.–10:15 a.m.
Members of the Argus Commission present and discuss the results of the 2023–24 Argus Commission Forecast Survey and Report. Copies of the report will be available onsite.


Be Social With Us!
Use the hashtag #PharmEd24 across your favorite social media platforms to engage with other attendees, and post your thoughts, highlights and reactions during and after sessions.
AACP greatly appreciates the support from our meeting sponsors, whose contributions make this event possible:
Certiphi Screening is a leader in student screening, creating and administering the AACP’s centralized criminal background check and drug screening program and helping individual schools and other fields of study build thorough, compliant student screening programs. Certiphi Screening is proud to be a platinum sponsor for the AACP Annual Meeting! www.Certiphi.com
At CVS Health, we share a clear purpose: helping people on their path to better health. Through our health services, plans and community pharmacists, we’re pioneering a bold new approach to total health. Making quality care more affordable, accessible, simple and seamless.
www.cvshealth.com
At Rite Aid, our mission is to improve the health and wellness of our communities through engaging experiences that provide our customers with the best products, services and advice to meet their unique wellness needs. www.riteaid.com
Walgreens’ more than 120-year heritage of caring for communities, is playing a greater role today as an independent partner of choice. Our trusted pharmacists provide a wide range of pharmacy and healthcare services that improve care, lower costs, and drive equitable access for some of the nation’s most underserved populations.
www.walgreens.com

CORE Higher Education Group offers innovative software solutions that empower institutions to manage clinical and experiential learning programs effectively. CORE’s solutions have evolved to support over 450 programs at more than 220 higher educational institutions, catering to their needs in clinical and experiential education, competency assessment, workforce readiness, recruiting, and e-portfolios.
corehighered.com
Through a powerful combination of technology and services, Liaison assists higher-ed institutions and students in making informed enrollment decisions. Our vision of fostering a more educated world fuels our passion for expanding access, simplifying experiences, and empowering decision-makers. With over 30 years of experience, we’ve served over 1,200 campuses and supported 40,000 programs globally, empowering individuals, partnering with institutions, and strengthening communities in the pursuit of knowledge and success.
www.liaisonedu.com


The NACDS Foundation aims to improve the health and well-being of communities in America by sustainably supporting groundbreaking research, education, and scholarship programs that enhance health outcomes, foster equity, strengthen access, and advance public health.
NACDSFoundation.org


Pharmacists Help People Live Healthier, Better Lives.
1400 Crystal Drive, Suite 300 P Arlington, VA 22202
703-739-2330 P www.aacp.org