

COMMON SENSE VOICE OF THE AMERICAN ACADEMY OF EMERGENCY MEDICINE VOLUME 30, ISSUE 4 JULY/AUGUST 2023 Editor's Message: Health Systems Work 6 10 The Whole Physician: You're Not the Boss of Me! 16 Emergency Medical Services Section: What Every Emergency Medicine Doctor Should Know about EMS 31 AAEM/RSA Editor's Message: Introducing Your New AAEM/RSA Publications Chair 30 AAEM/RSA President's Message AAEM/RSA New Board President's Message Page 2
Officers
President
Jonathan S. Jones, MD FAAEM
President-Elect
Robert Frolichstein, MD FAAEM
Secretary-Treasurer
L.E. Gomez, MD MBA FAAEM
Immediate Past President
Lisa A. Moreno, MD MS MSCR FAAEM FIFEM
Past Presidents Council Representative
Tom Scaletta, MD MAAEM FAAEM
Board of Directors
Heidi Best, MD FAAEM
Laura J. Bontempo, MD MEd FAAEM
Kimberly M. Brown, MD MPH FAAEM
Phillip A. Dixon, MD MBA MPH FAAEM CHCQMPHYADV
Al O. Giwa, LLB MD MBA MBE FAAEM
Robert P. Lam, MD FAAEM
Bruce Lo, MD MBA RDMS FAAEM
Vicki Norton, MD FAAEM
Kraftin Schreyer, MD MBA FAAEM
YPS Director
Fred E. Kency, Jr., MD FAAEM
AAEM/RSA President
Leah Colucci, MD MS
Editor, JEM
Ex-Officio Board Member
Stephen R. Hayden, MD FAAEM
Editor, Common Sense
Ex-Officio Board Member
Edwin Leap II, MD FAAEM
Executive Director
Missy Zagroba, CAE
Executive Director Emeritus
Kay Whalen, MBA CAE
Common Sense Editors
Mehruba Anwar Parris, MD, Assistant Editor
Mel Ebeling, MS3, Resident Editor
Stephanie Burmeister, MLIS, Managing Editor
Articles appearing in Common Sense are intended for the individual use of AAEM members. Opinions expressed are those of the authors and do not necessarily represent the official views of AAEM or AAEM/RSA. Articles may not be duplicated or distributed without the explicit permission of AAEM. Permission is granted in some instances in the interest of public education. Requests for reprints should be directed to AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202, Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org
AAEM is a non-profit, professional organization. Our mailing list is private.
AAEM ANTITRUST COMPLIANCE PLAN:
As part of AAEM's antitrust compliance plan, we invite all readers of Common Sense to report any AAEM publication or activity which may restrain trade or limit competition. You may confidentially file a report at info@aaem.org or by calling 800-884-AAEM
Mission Statement
The American Academy of Emergency Medicine (AAEM) is the specialty society of emergency medicine. AAEM is a democratic organization committed to the following principles:
1. Every individual, regardless of race, ethnicity, sexual identity or orientation, religion, age, socioeconomic or immigration status, physical or mental disability must have unencumbered access to quality emergency care.
2. The practice of emergency medicine is best conducted by a physician who is board certified or eligible by either the American Board of Emergency Medicine (ABEM) or the American Osteopathic Board of Emergency Medicine (AOBEM).
3. The Academy is committed to the personal and professional well-being of every emergency physician which must include fair and equitable practice environments and due process.
4. The Academy supports residency programs and graduate medical education free of harassment or discrimination, which are essential to the continued enrichment of emergency medicine, and to ensure a high quality of care for the patient.
5. The Academy is committed to providing affordable high quality continuing medical education in emergency medicine for its members.
6. The Academy supports the establishment and recognition of emergency medicine internationally as an independent specialty and is committed to its role in the advancement of emergency medicine worldwide.
Membership Information
Fellow and Full Voting Member (FAAEM): $525* (Must be ABEM or AOBEM certified, or have recertified for 25 years or more in EM or Pediatric EM)
Associate: $150 (Limited to graduates of an ACGME or AOA approved emergency medicine program within their first year out of residency) or $250 (Limited to graduates of an ACGME or AOA approved emergency medicine program more than one year out of residency)
Fellow-in-Training Member: $75 (Must be graduates of an ACGME or AOA approved emergency medicine program and be enrolled in a fellowship)
Emeritus Member: $250 (Please visit www.aaem.org for special eligibility criteria)
International Member: $150 (Non-voting status)
Resident Member: $60 (voting in AAEM/RSA elections only)
Transitional Member: $60 (voting in AAEM/RSA elections only)
International Resident Member: $30 (voting in AAEM/RSA elections only)
Student Member: $40 (voting in AAEM/RSA elections only)
International Student Member: $30 (voting in AAEM/RSA elections only)
Pay dues online at www.aaem.org or send check or money order to:
AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202 Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org
Table of Contents COMMONSENSE AAEM-0623-427 TM Foundation Contributions 8 PAC Contributions 8 LEAD-EM Contributions 9 Upcoming Events 9 Academic Affairs: Dealing with Challenging Consultants 14 Emergency Medical Services Section: What Every Emergency Medicine Doctor Should Know about EMS: Scope of Practice 16 Operations Management Section: What is ED Operations? 18 CAL/AAEM: Dear Students .............................................................................................................20 Wellness Committee: Data-Driven Behavior Change: How Utilizing Metrics in Emergency Medicine Can Drive Physician Burnout 25 AAEM/RSA President’s Message: AAEM/RSA New Board 30 AAEM/RSA Editor’s Message: Introducing Your New AAEM/RSA Publications Chair 31 Opinion: Emergency Physicians Should Give Ketamine to Patients with Acute Suicidal Ideation 32 Wellness Committee: Beyond the Curriculum: Exploring Moral Injury in Emergency Medicine from the Medical Student Lens 34 Justice, Equity, Diversity, and Inclusion Section: Justice, Equity, Diversity, and Inclusion Section’s 2023 Medical Student Scholarship Awardee Highlight ...............................................36 AAEM Locum Tenens Section: Introduction of the AAEM Locum Tenens Section (LT-AAEM) 37 AAEM/RSA Resident Journal Review: Colchicine in Coronary Artery Disease 38 AAEM Job Bank 42
COMMON SENSE MAY/JUNE 2023
COMMONSENSE
2
President’s Message: What is Your Why?

10
**NEW COLUMN** The Whole Physician: You’re Not the Boss of Me! Understanding Agency and Psychological Reactance

19
Actually, I am the Doctor
Even though female representation in the workforce is increasing, “Actually, I am the Doctor” is something Dr. Albury finds herself repeating throughout her day. The cure? Having the whole care team reinforcing to the patient that she is, in fact, the doctor.
22
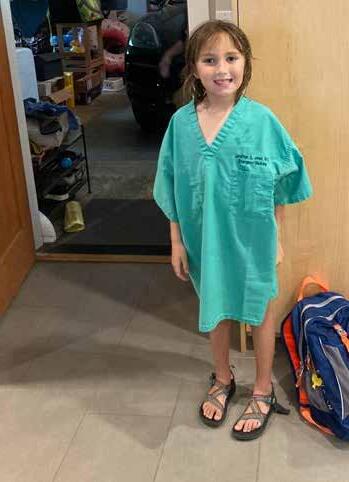
“Why do you have to work tonight? Why does it have to be you that helps them? Couldn’t someone else help them?” These are all valid questions from his seven-year-old daughter that AAEM President Dr. Jones has to answer. In his President’s Message, Dr. Jones answers the question of why he is an emergency physician and challenges you for your answer.
6
Editor’s Message: Health Systems Work
In this new Common Sense column, the Whole Physician Doctors discuss how Newton’s Third Law of Motion doesn’t just apply to physics, but applies to all aspects of human behavior—including EM docs.

12
Can Unions Empower Physicians

Operations Management
Section: QUEST: A Framework for Value-Based Care in Emergency Medicine
In his Editor’s Message, Dr. Leap discusses the proliferation of monopolistic tendencies that private equity and large health systems have on our health care system and how it impacts the ability of ER doctors to their own autonomy.
In this article, Dr. Pulliam argues that unions can be an important tool for EPs in their fight to regain some power over corporate medicine and a way to ensure that patients get the care that they deserve.

The authors of this article discuss the five components of QUEST and argue that QUEST will prepare EPs for the future of health care as it shifts from a fee-for-service system to a value-based care system.
27
Aging Well in Emergency Medicine Interest Group: The “Lowdown” on Wills and Testamentary Trusts
Do you think you don’t need a trust agreement? Think again, says Dr. Gaddis!
Featured Articles VOICE OF THE AMERICAN ACADEMY OF EMERGENCY MEDICINE VOLUME 30, ISSUE 4 JULY/AUGUST 2023
What is Your Why?
 Jonathan S. Jones, MD FAAEM
Jonathan S. Jones, MD FAAEM

“And now for something completely different.”
Maybe because it is the summer or maybe just because she is a bit older, my seven-year-old daughter has recently been asking me a lot about my work. While she asks multiple different questions about my work, to be honest, her main question, especially on evening or overnight shifts is, “Daddy, why do you have to work tonight?” While she knows that I am a doctor and work at the hospital and in the emergency department, I’m not sure she really knows what the ED is. I suppose this is a good thing as luckily, she has never experienced the ED. The way I usually explain why I must go to work is that sometimes people get sick or injured and someone must take care of them. Someone must help them.
This seems to make sense to her and often we start talking about completely different subjects. At other times, she poses some more difficult follow-up questions such as, “Why does it have to be you that helps them?” Or, “Why do you have to do it tonight?” Or, “Couldn’t someone else help them?” On the surface, these seem like simple questions, but the more I think about them, the more complex they can be.
Why does it have to be me that helps them? Couldn’t someone else help them?
I suppose it does not have to be me, but it happens to be me. Or rather, I like that it is me. I, hopefully like many of you, applied to medical school somewhat naive but also full of energy and hope. At least for me, one of the basic interview questions I faced at nearly every school was, “Why do you want to be a doctor?” One of my reasons, which I feel was and still is quite legitimate, is that I want to help people. And while of course there are many ways to help people and most of them do not require medical school, I think most would agree that doctoring does help people. We each had other reasons why we wanted to start the process of becoming a physician, maybe it was because
we liked the science or the research or the environment or a million other reasons. But hopefully, somewhere near the top of each of our lists was that we wanted to help.
So now when I explain to my daughter that I must go into work, instead of explaining that someone must help the sick and injured, I explain that I want to be that person who helps the sick and injured. At first that is a bit harder to explain as this implies that I would rather
couch in our living room. Laying on that couch answering questions such as “Why do you feel that way?” I realized that I didn’t need a counselor to help me figure out my inner thoughts. I had a mental health professional (I won’t use the term psychologist as that would be professional title misappropriation) right in my own home.
I will use this moment to encourage everyone to pay attention to their own mental health. I
help sick strangers than spend time with my family. It feels kind of rough explicitly stating this and even rougher documenting it on paper, but it must be true. Of course, there are limits and exceptions and I do place tremendous value on my time with family and friends, at some level, there is something in me and in all of us that makes us willing to sacrifice.
I’ll honestly admit that I hadn’t truly thought of the reasons I am a physician until forced to explain them. If you have not tried it, explaining your reason and logic to a seven-year-old is an incredibly useful exercise. They ask insightful questions and, perhaps more importantly, they don’t let you get away with vague non-answers. For example, when was the last time you verbalized your own reasons for doing what you do?
One time when my daughter and I were having this discussion I happened to be laying on a
have neglected mine at times and this has not been healthy for me, my family, or my patients. I do not mean to make light of the mental health crises by the above paragraph. Physician mental health is the most important challenge of our time. Please use professional resources as needed. Please also know that most (but not all) states no longer require reporting of mental health issues to the state medical board. Many inside and outside AAEM have worked on this issue and the Academy continues to be a leader in this space.
Why am I sharing all of this? It’s because I think we need to talk about our reasons for doing what we do more often and more openly. Why? Because we are often tired and we are burned out. We are managed and micromanaged by non-physicians. We are abused verbally and at times even physically. We are guilt tripped into taking one more shift or staying
>> AAEM PRESIDENT’S MESSAGE
COMMON SENSE JULY/AUGUST 2023 2
“Why does it have to be me that helps them? Couldn’t someone else help them?
later and later after a shift. We are vilified when we finally speak out about dangers in health care. We even lose our jobs for doing what we feel is best. So why do we continue to do this job? For me, thinking of and actually verbalizing the reasons I do this job, makes me feel less tired, less injured, more confident, and quite simply, happier.
I am an emergency physician because I am empathetic. Seeing someone suffer hurts me. Luckily, I have not suffered much in my life, but I sure know that it doesn’t feel good when I stub a toe. It feels horrible to have a GI bug. And I know that way back when I was a kid vomiting in a trash can, it sure felt a little better when my mother rubbed my back and brought a damp washcloth to wipe my mouth. It sure feels good to be comforted. And so, I want to be able to comfort people. And while I certainly want to be able to comfort my family, I also want to be able to comfort others, especially, once I outgrew childhood and realized that not everyone has a loving mother or other family member to comfort them. Some people have no one. I want to be that someone. A skeptic could say that I want to be that someone because it ultimately makes me feel good and well, it sure does. Yes, I receive a benefit by caring for others and I freely admit it. It also feels good to feel empathetic. It seems to me this is a classic win-win.
I am an emergency physician because I am curious. Life is amazing. To me biology is a complex interplay of two more basic sciences—chemistry and physics. And while I actually enjoyed studying both physics and chemistry more than biology, seeing the ultimate effect
each of these three sciences has on the human body is amazing. Figuring out how it works and why is exciting. Learning the different ways and reasons it stops working is interesting. Learning methods to fix those problems is rewarding. Realizing how little we understand about this whole thing is fascinating. While research is not a major part of my current career, I nonetheless enjoy reading about and utilizing new discoveries in medicine. While an overly technical paper may induce slumber, reading about most scientific discoveries energizes and excites me.
I am an emergency physician because I am capable. Or, what I actually think is, I am an emergency physician because this is an incredibly difficult job and I am incredibly talented and damn good at doing it. Sounds a bit egotistical sure, but I’m tired of the self-depreciation of physicians. It is an honorable attribute, self-depreciation, but it can be taken to extremes. I studied, I trained, I dedicated countless hours, and partially because of that or perhaps for some unknown mystery of the universe, but I excel at an incredibly difficult job. Most people cannot do what I do. Yes, one of the reasons I am an emergency physician is because I can be an emergency physician.
I am an emergency physician because I want to improve the human experience. Despite our differences, all of us humans, are in this together. The discoverer of a new star improves
humanity. The builder of a new public park improves humanity. The conserver of a fragile species improves humanity. And while the above paragraph may have sounded a bit brash, now I’ll say that I can’t do anything of these things which I just mentioned. I can’t and I’m fine with that. But I do what I can and I enjoy it. So, while I likely won’t be the first human to explore Mars, I may have just saved that person’s life.
I have no idea if any of those are reasons that you are an emergency physician. Maybe some are and some are not. But I do hope that I’ve helped you think of the reasons that you are an emergency physician. And I urge you to do more. Write down the reasons you do what you do. Tell your family or friends. It helps me to verbalize my reasons and it may help you. There have been nights when I returned from a difficult shift, my family was all in bed and I hugged my dog and told her why I am an emergency physician. She is an amazing listener by the way.
Maybe we each just need to do what one of my favorite philosophers of all time recommended. Look in the mirror and say, “I’m good enough, I’m smart enough, and dog gone it, people like me.”

>> AAEM PRESIDENT’S MESSAGE
“There have been nights when I returned from a difficult shift, my family was all in bed and I hugged my dog and told her why I am an emergency physician. She is an amazing listener by the way.”
COMMON SENSE JULY/AUGUST 2023 3
“I’ll honestly admit that I hadn’t truly thought of the reasons I am a physician until forced to explain them. If you have not tried it, explaining your reason and logic to a seven-year-old is an incredibly useful exercise.”
Have a great summer and enjoy life. And if you are so inclined, after writing your reasons for being an emergency physician, submit them to Common Sense using the QR code nearby. All submissions are anonymous. Let’s compile a list for the Academy and share. The more reasons the better and the wider those reasons are shared the better. I look forward to reading about what is meaningful for you. (Oh and I’ll buy a drink next SA for the first person who tells me the source of both my opening and closing quotes.)
Cheers and know that you are good enough, you are smart enough, and dog gone it, I like you. I also thank you. More importantly than that, your patients thank you. Humanity thanks you. You are special and you deserve to feel that way.
29th Annual SCIENTFIC ASSEMBLY








Preview of the AAEM23 5k Fun Run Results





Congratulations to Drs. Bryan Knoedler and Rohan Janwadkar for beating AAEM President Dr. Jones in the 5k Fun Run held during AAEM23 and for making donations to the AAEM Foundation. As promised, Dr. Jones has matched their contributions to the Foundation. Congratulations and thank you!

AAEM PRESIDENT’S MESSAGE
COMMON SENSE JULY/AUGUST 2023 4
How can you help?
Join your colleagues and make a gift or a pledge today.
Gifts at all levels can be paid in one year or pledged over two to five years. We encourage individuals, physician groups, and companies to help support the fight!
$50,000+ Champion Circle
$25,000 - $49,999 President’s Club
$10,000 - $24,999 Advocate
$5,000 - $9,999 Steward
$2,500 - $4,999 Ambassador
$1,000 - $2,499 Supporter
Up to $1,000 Friend
Donate Now
The AAEM Foundation
AAEM was established in 1993 to promote fair and equitable practice environments necessary to allow emergency physicians to deliver the highest quality of patient care. AAEM later established the AAEM Foundation to defend the rights of such care and the emergency physicians who provide it.
Recently, AAEM-Physician Group, a subsidiary of the American Academy of Emergency Medicine (AAEM), filed suit in the Superior Court of California against Envision Healthcare Corporation to avoid a takeover of an emergency department contract that was held by and independent group. Issues at stake include lay influence over the patient-physician relationship, control of the fees charged, prohibited remuneration for referrals, and unfair restraint of the practice of a profession.
Our specialty is in crisis. We cannot let these practices continue here and across the country.
AAEM is the only EM organization that speaks and acts against the harmful influences of the corporate practice of medicine.
Our Goal: $2.5 million by 2025
Gifts in Honor and Gifts in Memory
Gifts at all levels can be given In Honor Of or In Memory Of a program director, mentor, and/or colleague.
Notification of gifts made In Honor or In Memory will be sent to the honoree or their family and listed in our Annual Report.
Ways to Give
• Donate Online
• Scan QR Code
• Employer Matching Gift
• Return the Donation/Pledge Form
• Planned Giving
The AAEM Foundation gratefully accepts IRA distributions, contributions through donor-advised funds, planned gifts and bequests.
ACMS-0718-026
aaem.org/donate/aaem-foundation The AAEM Foundation is a 501(c)(3) non-profit organization. EIN: 20-2080841 American Academy of Emergency Medicine Foundation 555 East Wells Street, Suite 1100, Milwaukee, WI 53202 (414) 276-7390 • (800) 884-2236 • Fax: (414) 276-7390 25% 50% 75%
COMMON SENSE JULY/AUGUST 2023 5
Health Systems Work
Edwin Leap II, MD FAAEM

began my career in the golden days of emergency medicine, when independent, fee-for-service groups were still fairly common. I was fortunate to work for such a group for 20 years before embarking on an adventure in locums emergency medicine. In that group, Blue Ridge Emergency Physicians, we made decisions that were best for us, our families, and for our patients. We contributed to the function of the hospital as we saw fit. We negotiated with the hospital. We even discounted charts when we thought it was appropriate. It was glorious… while it lasted. Ultimately the hospital was purchased by a larger hospital nearby. We were promised it would never happen. Now it’s all in the rear-view mirror.

Looking back I can now see that one of the grand things about those fee-for-service groups was far more personal than the financials. It was that one could, without great difficulty, leave and change jobs within a region. A personality conflict, an unfavorable contract, a better job elsewhere, a change in family needs and it was possible to go a few counties over and still have a career in the same general area.
As we fast forward to 2023, things are different. Private equity owns huge segments of the emergency medicine market in many areas. If you find that your current job doesn’t work for you for any of a number of reasons, it can be very hard to stay in a particular area as you’ll have the same regional “boss,” with the much the same contract.
Run afoul of someone in the corporation and you might find yourself looking across regions, or across state lines, for work. You could be considered “persona non-grata” in hundreds of facilities across the country.
However, as easy as it may be to point fingers at private equity, there is another problem. That is the expansion and power of large health systems, including university centers.
IAs competing entities constantly try to grab up as much of the health care market as possible, I understand that it makes strategic sense for large corporate health systems and universities to try and out-compete one another. Still, it can feel like a great big game of medical Risk. The health care map changes as assorted groups acquire new hospitals—sometimes within the “territory” of another system. Occasionally I’ve laughed to myself that it almost seems like gang wars. I have half expected to hear of drive-by shootings at board meetings as systems struggle for new patients. But what it means for the individual physician is that because of large regional systems, our personal options are becoming more and more limited. As with private equity, if you’re unhappy in the job you may be out of luck. If you find yourself pushing back against practice patterns or speaking out about dangerous staffing or other problems within the system, you may be offered the door. And again, if you end up in conflict with someone of influence, then it’s “heave-ho and best wishes.” And no kind letter of reference ends up in your file.
I have known physicians who faced exactly this situation. When their contracts changed, when they lost money or time off, when their personal satisfaction dropped like a rock, when someone in the power structure seemed to have a grudge, there was simply no place to go without selling the house, uprooting the family, and exiting the stage.
Of course this can happen in any job. But medicine, like it or not, is increasingly monolithic.
It’s easy to imagine that a physician express a viewpoint at odds with “corporate compliance,” or with the dominant beliefs of a majority of the power-players in a hospital system.
This could easily result in a kind of banishment. And again, given the enormous financial weight and geographic spread of health care systems and private equity, the ability of a physician to speak what they believe is true might be severely curtailed.
If we learned anything from COVID, it’s that physicians are not all the same. For better or worse, we work and practice along a wide spectrum of ideas and viewpoints. And it isn’t as easy as some think to divide us into “scientists” and “science deniers.” Science can be a pretty fluid thing, and people we thought were completely off track occasionally turn out to have been right all along. A trip to a good conference every couple of years, like the incredible AAEM Scientific Assembly, should be enough for any honest physician to look at his or her practice and think “guess I’ve got to change some things!” The ability to disagree and question moves medicine forward, even when it’s uncomfortable.
This is equally true on social, cultural, and >>
EDITOR’S MESSAGE
COMMON SENSE JULY/AUGUST 2023 6
“ When their contracts changed, when they lost money or time off, when their personal satisfaction dropped like a rock, when someone in the power structure seemed to have a grudge, there was simply no place to go without selling the house, uprooting the family, and exiting the stage.”
political issues. Emergency medicine is made up of committed progressives and dyed-in-the wool conservatives and everything in between. And that’s exactly the right thing, since our patients cross a wide spectrum of attitudes, beliefs, and descriptors.

I am convinced that one of the best reasons for us to push back against the monopolistic tendencies of health care systems as well as private equity is simply this. To retain the ability to speak candidly (and professionally) about problems and also maintain ideological diversity.
Sometimes I long for the days of the old “trust busters” who recognized the inherent dangers of corporations having too much influence for the public good. I think, as the size and influence of health care systems grows to staggering levels, and as powerful health care concerns insinuate themselves into our lives more and more, it may be time for another politician with the temerity to do just that.
If only so physicians, like you and like me, can still be true to ourselves, true to the sick and suffering…and continue to keep our jobs without fear.
Preview of the 29th Annual SCIENTFIC ASSEMBLY

1st Place: Quoc Vinh Tran, DO
2nd Place: Deanna Margius, MD
3rd Place: Michael D. Zwank, MD FAAEM
CCMS-AAEM Breveloquent Competition

1st Place: Rebecca Raven, MD
2nd Place: Kimberly Pistell, DO
3rd Place: Amina Ramadan, MD
EDITOR’S MESSAGE
“Sometimes I long for the days of the old “trust busters” who recognized the inherent dangers of corporations having too much influence for the public good.”
AAEM23 Photo Competition Results
COMMON SENSE JULY/AUGUST 2023 7
Congratulations to the AAEM23 Photo and the CCMS-AAEM Breveloquent Competition Winners
AAEM Foundation Contributors – Thank You!
AAEM established its Foundation for the purposes of (1) studying and providing education relating to the access and availability of emergency medical care and (2) defending the rights of patients to receive such care and emergency physicians to provide such care. The latter purpose may include providing financial support for litigation to further these objectives. The Foundation will limit financial support to cases involving physician practice rights and cases involving a broad public interest. Contributions to the Foundation are tax deductible. Levels of recognition to those who donate to the AAEM Foundation have been established. The information below includes a list of the different levels of contributions. The Foundation would like to thank the individuals below who contributed from 1/1/2023 to 7/1/2023. Please note any donations made during the 2023 Scientific Assembly will be reflected in our next issue..
Contributions $1000 and above
Algis J. Baliunas, MD FAAEM
Babak Khazaeni, MD FAAEM
David W. Lawhorn, MD MAAEM
Jonathan S. Jones, MD FAAEM
Kathryn Getzewich, MD FAAEM
Oscar A. Marcilla, MD FAAEM
Thomas R. Tobin, MD MBA FAAEM
Contributions $500-$999
Fred Earl Kency, Jr., MD FAAEM
Pedro I. Perez, MD FAAEM
Robert A. Frolichstein, MD FAAEM
Ronald T. Genova, MD
Contributions $250-$499
Bradley Houts, MD FAAEM
David Thomas Williams, MD FAAEM
Eric D. Lucas, MD FAAEM
Floyd W. Hartsell, MD FAAEM
Jeffrey J. Thompson, MD FAAEM
Kenneth Scott Hickey, MD FAAEM FACEP
Laura Richey, MD FAAEM
Marc R. Houston, DO FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Ming-Jay Jeffrey Wu, MD FAAEM
Nayla M. Delgado Torres, FAAEM
Piotr Jurgielewicz, MD
Robert J. Feldman, MD FAAEM
Shane Coughlin, MD
Contributions $100-$249
Alexander Tsukerman, MD FAAEM
Andrew Thomas Larkin, DO FAAEM
Anisha Malhotra, MD FAAEM
Ann Loudermilk, MD FAAEM
Arnold Feltoon, MD FAAEM
Barry N. Heller, MD FAAEM
Brian J. Browne, MD FAAEM
Brian J. Cutcliffe, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Bruce E. Lohman, MD FAAEM
Bryan Knoedler, MD
Catherine V. Perry, MD FAAEM
Chaiya Laoteppitaks, MD FAAEM
D. Scott Moore, MS DO FAAEM
David R. Steinbruner, MD FAAEM
David Wang, MD FAAEM
Donald L. Slack, MD FAAEM
Douglas P. Slabaugh, DO FAAEM
Gary M. Gaddis, MD PhD MAAEM
FAAEM FIFEM
H. Samuel Ko, MD MBA FAAEM
Irene Tien, MD FAAEM
Jason M. Driggs, MD FAAEM
Jeffrey A. Rey, MD FAAEM
Jenna Otter, MD FAAEM
Jessica Moore, MD
Jonathon D. Palmer, MD FAAEM
Kathleen Hayward, MD FAAEM
Katrina Green, MD FAAEM
Katrina Kissman, MD FAAEM
Marc D. Squillante, DO FAAEM
Nancy Conroy, MD FAAEM
Neeharika Bhatnagar, MD FAAEM
Patrick B. Hinfey, MD FAAEM
Paul W. Gabriel, MD FAAEM
Philip Beattie, MD FAAEM
Renee Marie Nilan, MD FAAEM
Riley MW Williams, MD MBA
Robert Boyd Tober, MD FAAEM
Rohan Janwadkar, MD
Roland S. Waguespack III, MD MBA FAAEM
Sameer D. Mistry, MD MBA CPE FAAEM
Tim J. Carr, FAAEM
Timothy J. Durkin, DO FAAEM CAQSM
William E. Franklin, DO MBA FAAEM
Yeshvant Talati, MD
Contributions up to $99
Alexander J. Yeats, Jr., MD FAAEM
Alexander S. Maybury, MD FAAEM
Amie Rose
Benson Yeh, MD FAAEM
Brian Gacioch, FAAEM
Caitlin E. Sandman, DO FAAEM
David C. Crutchfield, MD FAAEM
Edward T. Grove, MD FAAEM MSPH
Eric M. Rudnick, MD FAAEM
AAEM PAC Contributors – Thank You!
Ernest H. Leber Jr., MD FAAEM
Erol Kohli, MD MPH FAAEM
Everett T. Fuller, MD FAAEM
James P. Alva, MD FAAEM
James R. Gardner, FAAEM
Jason J. Morris, DO FAAEM
Joanne Williams, MD MAAEM FAAEM
Jonathan Y. Lee, MD FAAEM
Jose G. Zavaleta, MD
Joseph M. Reardon, MD MPH FAAEM
Kelly Dougherty, MD
Kenneth T. Larsen, Jr., MD FAAEM
Kevin C. Reed, MD FAAEM
Linda Sanders, MD FAAEM
Marianne Haughey, MD FAAEM
Megan Crossman, MD FAAEM
Michael Lajeunesse, MD
Om Pathak, DO
Peter H. Hibberd, MD FACEP FAAEM
Peter M.C. DeBlieux, MD FAAEM
Peter Stueve, DO
Sachin J. Shah, MD FAAEM
Samuel M. Morris, MD
Scott Beaudoin, MD FAAEM
Stacy G. Hooks, MD
Tabitha Williams, FAAEM
Virgle O. Herrin Jr., MD FAAEM
AAEM PAC is the political action committee of the American Academy of Emergency Medicine. Through AAEM PAC, the Academy is able to support legislation and effect change on behalf of its members and with consideration to their unique concerns. Our dedicated efforts will help to improve the overall quality of health care in our country and to improve the lot of all emergency physicians.
All contributions are voluntary and the suggested amount of contribution is only a suggestion. The amount given by the contributor, or the refusal to give, will not benefit or disadvantage the person being solicited.
Levels of recognition to those who donate to the AAEM PAC have been established. The information below includes a list of the different levels of contributions. The PAC would like to thank the individuals below who contributed from 1/1/2023 to 7/1/2023. Please note any donations made during the 2023 Scientific Assembly will be reflected in our next issue.
Contributions $500-$999
Mark S. Penner, DO FAAEM
Ronald T. Genova, MD
Contributions $250-$499
Bradley Houts, MD FAAEM
Fred Earl Kency, Jr., MD FAAEM
Joseph T. Bleier, MD FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Michael L. Martino, MD FAAEM
Paul W. Gabriel, MD FAAEM
Thomas B. Ramirez, MD FAAEM
Tim J. Carr, FAAEM
Contributions $100-$249
Alexander S. Maybury, MD FAAEM
Alexander Tsukerman, MD FAAEM
Brian J. Cutcliffe, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Bruce E. Lohman, MD FAAEM
Catherine V. Perry, MD FAAEM
David W. Lawhorn, MD MAAEM
Donald L. Slack, MD FAAEM
Garrett Sterling, MD FAAEM
Gary M. Gaddis, MD PhD MAAEM
FAAEM FIFEM
Jeffrey A. Rey, MD FAAEM
Jeffrey J. Thompson, MD FAAEM
Joseph M. Reardon, MD MPH FAAEM
Katrina Green, MD FAAEM
Philip Beattie, MD FAAEM
R. Lee Chilton III, MD FAAEM
Raviraj J. Patel, MD FAAEM
Riley MW Williams, MD MBA
Robert Boyd Tober, MD FAAEM
Robert M. Esposito, DO FAAEM
Stewart Sanford, MD FAAEM
William E. Franklin, DO MBA FAAEM
Contributions up to $99
Alex Kaplan, MD FAAEM
Amie Rose
Brice Guy, DO
Chaiya Laoteppitaks, MD FAAEM
David L. Sincavage, Jr., MD FAAEM
David R. Steinbruner, MD FAAEM
Eric M. Rudnick, MD FAAEM
Erol Kohli, MD MPH FAAEM
James R. Gardner, FAAEM
Jason J. Morris, DO FAAEM
Kevin C. Reed, MD FAAEM
Laura M. Mory, MD FAAEM
Linda Sanders, MD FAAEM
Marc D. Squillante, DO FAAEM
Om Pathak, DO
Peter H. Hibberd, MD FACEP FAAEM
Peter Stueve, DO
Ruth P. Crider, MD FAAEM
Tabitha Williams, FAAEM
Virgle O. Herrin Jr., MD FAAEM
COMMON SENSE JULY/AUGUST 2023 8
LEAD-EM Contributors – Thank You!
The AAEM Institute for Leadership, Education & Advancement in the Development of Emergency Medicine, Inc. (LEAD-EM) was established after the tragic and unexpected death of AAEM president, Dr. Kevin G. Rodgers.
The Kevin G. Rodgers Fund and the Institute will LEAD-EM just like Dr. Rodgers did. The funds will support important projects such as development of leadership qualities, and clinical and operational knowledge of emergency physicians with a view toward improving and advancing the quality of medical care in emergency medicine, and public health, safety and well-being overall. LEAD-EM would like to thank the individuals below who contributed from 1/1/2023 to 5/1/2023. Please note any donations made during the 2023 Scientific Assembly will be reflected in our next issue
Contributions $1000 and above
Jonathan S. Jones, MD FAAEM
Contributions $500-$999
Fred Earl Kency, Jr., MD FAAEM
Contributions $250-$499
David W. Lawhorn, MD MAAEM
Dale S. Birenbaum, MD FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Mary Ann H. Trephan, MD FAAEM
Contributions $100-$249
Alexander S. Maybury, MD FAAEM
Ann Loudermilk, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Catherine V. Perry, MD FAAEM
Christopher Kang, MD FAAEM
David R. Steinbruner, MD FAAEM
Edward T. Grove, MD FAAEM MSPH
Gary M. Gaddis, MD PhD MAAEM
FAAEM FIFEM
Joseph M. Reardon, MD MPH FAAEM
Kathleen Hayward, MD FAAEM
Kevin C. Reed, MD FAAEM
Paul W. Gabriel, MD FAAEM
Roland S. Waguespack III, MD MBA
FAAEM
Contributions up to $99
Alicia J. Starr, DO
Erol Kohli, MD MPH FAAEM
Jose G. Zavaleta, MD
Marc D. Squillante, DO FAAEM
Om Pathak, DO
Richard G. Foutch, DO FAAEM
Samuel M. Morris, MD
Virgle O. Herrin Jr., MD FAAEM
Upcoming Events: AAEM Directly, Jointly Provided, & Recommended
AAEM is featuring the following upcoming conferences and activities for your consideration. For a complete listing of upcoming conferences and other meetings, please visit: aaem.org/education/events
AAEM Events
August 8, 2023
EMSS-AAEM: Mass Gathering Medicine
August 10, 2023
WiEM-AAEM: IMG Student Mentoring Webinar Series: Q&A About ERAS
August 22, 2023
WiEM-AAEM: The Whole Physician
August 24, 2023
JEDI-AAEM: Egg Freezing in Residency
September 13 & 14, 2023
Virtual Oral Board Review Courses aaem.org/education/events/oral-boards
7-10 September 2023
XIIth Mediterranean Emergency Medicine Congress (Rhodes, Greece) aaem.org/memc23/
November 29 & 30, 2023
Virtual Oral Board Review Courses aaem.org/education/events/oral-boards
April 27-May 1, 2024
30th Annual Scientific Assembly (Austin, TX) aaem.org/aaem24
Jointly Provided
Re-Occurring Monthly
Unmute Your Probe: Virtual Ultrasound Webinar Series
Jointly provided by EUS-AAEM aaem.org/get-involved/sections/eus/resources/unmute-your-probe/
Re-Occurring Monthly Spanish Education Series*
Jointly provided by the AAEM International Committee aaem.org/get-involved/committees/committee-groups/international/ spanish-education-series
September 19-23, 2023
UC Davis Emergency Medicine Hot Topics (Maui, HI)
Jointly provided by UC Davis ces-apps.ucdavis.edu/confreg/?confid=1257
October 16-20, 2023
Essential Emergency Medicine: Can’t Misses in EM - Cardiac Misfortunes, Environmental Misadventures, and Unfortunate Misdiagnoses (Lake George, NY)
Jointly provided by EssentialCME essentialcme.com/conferences
Recommended
Advances in Cancer ImmunotherapyTM: sitcancer.org/education/aci
• August 17, 2023 - A Focus on Cellular Therapies and T cell Engagers (Washington, DC and Virtual)
• October 19, 2023 - A Focus on Hematologic Malignancies (Virtual)
The Difficult Airway Course: Emergency™: theairwaysite.com/a-course/the-difficult-airway-course-emergency/
• September 22 - 24, 2023 - San Diego, CA
• October 20 - 22, 2023 - Washington, D.C.
• November 17 - 19, 2023 - New Orleans, LA
Online CME
• Recognizing Life-Threatening Emergencies in People with VEDS - thesullivangroup.com/TSG_UG/VEDSAAEM/
COMMON SENSE JULY/AUGUST 2023 9
You’re Not the Boss of Me! Understanding Agency and Psychological Reactance


 Laura Cazier, MD FAAEM, Amanda Dinsmore, MD FAAEM, and Kendra Morrison, DO
Laura Cazier, MD FAAEM, Amanda Dinsmore, MD FAAEM, and Kendra Morrison, DO
Hearken back with me to middle school science for a moment. Remember Newton’s Third Law of Motion? Of course, you do—that was the one that went like this: For every action, there is an equal and opposite reaction. In his book “Effortless,” author Greg McKeown describes this law as one based on an essential principle—what goes out comes back.1 Sound familiar? What goes around, comes around, karma, etc. As it turns out, Newton’s Third Law also applies to human behavior. Let’s explore.

Have you ever bristled when someone gave you unsolicited advice? Or had the instinct to say, “No!” when someone told you to do something—even if it was something you were just about to do?
Have you ever behaved in a toddler-like way in reaction to someone being bossy, or as we like to say at our house, “overly directive?”
*Raises hand sheepishly.*
Most likely, we all have had this experience (we were once all two-year-olds, after all). Are we just stubborn?
Many physicians self-identify as stubborn people—it’s part of what helps us survive our medical training. But is that all there is to it?
Let’s talk about psychological reactance and agency. Agency is the feeling of control over our actions and their consequences.2 Like another word for personal freedom. According to Self-Determination Theory, having a sense that our agency is intact is essential to our well-being as humans.3 Psychological “reactance is an unpleasant motivational arousal that emerges when people experience a threat to or loss of their free behaviors. It serves as a motivator to restore one’s freedom.”4
Reacting to perceived threats to our freedom is hard-wired in us. It’s why we don’t like unsolicited advice. It’s why we don’t like being “bossed around.” None of us likes it when a patient says, “You will order such and such test.” Oh, no sir (or ma’am). If such a test is clinically indicated, we might still not want to order it because of the disrespectful way the patient requested it, which isn’t good for anyone. Just as we don’t like to have our agency threatened, other people will react when they sense we are infringing on their personal freedom.
Example: A report was circulated around one department of an MD sternly telling a nurse to “check your orders—I ordered Percocet” when she asked how much intranasal fentanyl she should give a child in severe pain after being mauled by a dog. The physician’s psychological reactance to the nurse’s question is clear, but it begs the question—what is the result of his reactance? Is he better off in the long run for having reacted this way? Do the nurses now respect him more? Are they more likely to carry out his orders cheerfully and efficiently, or might they have some reactance of their own?
As we all well know, this little interchange did not increase the nurses’ respect for this physician, nor did it improve camaraderie, morale, or anything related to wellness in the department. It dropped an aliquot of toxicity into the milieu of an otherwise well-running and generally happy emergency department. While it’s true he had written an order for a different analgesic which the nurse had not seen, he might have had a more favorable outcome had he chosen to approach this situation with respect for the nurse and her personal agency, knowing that she doesn’t have to do anything. She doesn’t have to work in the emergency department. She could go work any number of other places—thank goodness for all the nurses who still come to work with us. Communicating patiently and kindly, with a respectful tone and curiosity about what the nurse thinks, goes a long way toward creating a healthy work environment for everyone. Seasoned EM docs know if we give respect, we get respect. We
>> THE WHOLE PHYSICIAN
COMMON SENSE JULY/AUGUST 2023 10
"Seasoned EM docs know if we give respect, we get respect. We don’t earn respect by saying, “I give the orders around here.”
don’t earn respect by saying, “I give the orders around here.”
Reactance shows up in our personal lives as well. We may know someone who gives us unsolicited advice. Someone who seems to know how we “should” be living, how we “should” raise our kids, what foods we “should” be eating, etc. That “should” word is a red flag that someone is making an attempt, consciously or subconsciously, to infringe on our agency. Likewise, if others are distancing themselves from us, examining our communication with them might reveal that we have violated their agency.
As it turns out, resistance to infringement on personal freedom is a natural response, not only in humans but in animals as well. It’s difficult to imagine an animal that, given the opportunity, would not attempt to escape its cage. Elephants don’t allow humans to ride them for their own enjoyment. They do it after being tortured into submission. The classic Seligman study of learned helplessness comes to mind. In this study, dogs were shocked either unavoidably, or with the opportunity to escape the shock. The dogs who had been shocked without ceasing were unable to recognize when the opportunity to get relief finally presented itself, and instead of getting off the shock plate, they lay down and whimpered.5
Let’s not be the “should”-er, but let’s also not be the dog on the shock plate. We all have agency—we get to choose how to live. We choose to work in the emergency department. We could decide to do something else entirely, but we don’t. Likewise, others get to choose how they live and experience life in their own way. Nobody likes to be bossed around. And what we send out will come back to us, just like Newton said.
Dr. Laura Cazier is an emergency physician practicing in Huntsville, Alabama, a certified physician wellness coach, and co-founder of Valley Leadership Academy, a K-12 hybrid school focused on emotional wellness and leadership development. Dr. Amanda Dinsmore is an emergency physician in Springfield, MO. She completed a fellowship in integrative medicine and is a certified physician wellness coach. Dr. Kendra Morrison is an emergency physician, the medical director of a freestanding ED in Springfield, MO, and clinical faculty at the Kansas City University College of Medicine. She has additional training in integrative medicine and wellness coaching. Together they founded The Whole Physician, an organization dedicated to optimizing physician well-being. Follow them on Facebook (facebook. com/thewholephysician), Instagram @thewholephysician, or Twitter @WholePhysician.
References
1. McKeown, G. (2021). Effortless. Currency.
2. Moore JW. What Is the Sense of Agency and Why Does it Matter? Front Psychol. 2016 Aug 29;7:1272. doi: 10.3389/fpsyg.2016.01272. PMID: 27621713; PMCID: PMC5002400.
3. Wehmeyer, M. L., Little, T. D., & Sergeant, J. (2009). Self-determination. In S. J. Lopez & C. R. Snyder (Eds.), Oxford handbook of positive psychology (pp. 357–366). Oxford University Press.
4. Steindl C, Jonas E, Sittenthaler S, Traut-Mattausch E, Greenberg J. Understanding Psychological Reactance: New Developments and Findings. Z Psychol. 2015;223(4):205-214. doi: 10.1027/2151-2604/ a000222. PMID: 27453805; PMCID: PMC4675534
5. Maier SF, Seligman ME. Learned helplessness at fifty: Insights from neuroscience. Psychol Rev. 2016 Jul;123(4):349-67. doi: 10.1037/ rev0000033. PMID: 27337390; PMCID: PMC4920136
HEART OF A DOCTOR
COMMON SENSE JULY/AUGUST 2023 11
"Many physicians self-identify as stubborn people—it’s part of what helps us survive our medical training."
Can Unions Empower Physicians and Protect Patients?
 Bryce Pulliam, MD FAAEM
Bryce Pulliam, MD FAAEM

AAEM has long championed physician owned practices, but for nearly two decades has also formally supported emergency physicians’ right to unionize.1 Until this year there were no unions exclusive to emergency department providers. That changed in April 2023 when my colleagues and I formed the Southern Oregon Providers Association (SOPA), the first U.S. union comprised exclusively of emergency physicians, nurse practitioners, and physician assistants. Now, more than ever, unions are becoming an important tool for emergency physicians looking to regain some power over corporate medicine and ensure their patients get the care they deserve.
In 1957 house staff at New York City’s public hospitals formed the Committee for Interns and Residents (CIR), the first physician union. In recent years the number of union residents has increased rapidly, with CIR membership nearly doubling in the past five years to 27,000 members.2,3 Attending physicians first unionized in 1972 with the Union of American Physicians and Dentists. However, physician union membership remains low, with only 5.9% of practicing doctors represented by unions.4
One reason for the slow adoption of physician unions may be that, historically, many physicians were not eligible to join unions. Union eligibility is determined by the National Labor Relations Board (NLRB), the federal agency charged to protect “the rights of private sector employees to join together, with or without a union, to improve their wages and working conditions.”5 The NLRB notes that self-employed physicians and independent contractors, sometimes referred to as “1099 employees,” are not eligible to unionize. Also, physicians considered managers are ineligible to unionize, including physician-owners of medical groups, tenured or tenure-track academic physicians, and those with significant authority to hire, fire, or discipline employees or direct day-to-day operations.6,7
Many physicians employed by hospital systems and corporations are W-2 employees, and therefore potentially eligible to unionize. Simply serving on hospital committees or writing orders executed by nurses have not been deemed to be management activities by the NLRB, and do not preclude otherwise eligible physicians from forming or joining a union.6,8
While in 1983, 73.8% of physicians were employed by physician owned groups, by 2022, an estimated 74% of physicians were employees of hospitals, health systems, or other corporate entities.9,10 This reflects years of consolidation by health systems and corporations that only accelerated during the COVID pandemic.4 This shift away from physician ownership not only creates a situation where providers feel a lack of autonomy and advocacy over patient care and safety, but also a general sense of disenfranchisement. However, it also means that an increasing
number of physicians have become eligible to unionize. Increasingly, physicians are unionizing to regain some of the power to advocate for themselves and their patients.
Unions are not a panacea. In an industry already burdened by layers of bureaucracy, unions can add yet another layer of complexity, and may actually impede interactions in groups with strong, well-functioning relationships with management. Furthermore, with unions come union dues. These typically range between 1-3% and come directly from member physicians’ pay. Unless members see tangible benefits from their union, these forgone wages may be a source of discontent. Also, in practices where each physician has negotiated their contract independently, standardization of compensation under a union contract may result in reduced pay for strong negotiators, while weaker negotiators may get a raise.6
One of the largest concerns many physicians have about unions is the threat of strikes, which, while exceedingly rare, especially for attending physicians, can be damaging to public relations and theoretically put patients at risk, though in at least one study, a physician strike actually resulted in a reduction in deaths.11 Strikes are a last resort of failed negotiations and if physicians strike to improve patient care, it is in the patients’ best interest that they do so. Physicians do not bear the responsibility for patient care alone, and while they should only strike if all other options have been exhausted and they believe patient harm will result
>>
COMMON SENSE JULY/AUGUST 2023 12
"While in 1983, 73.8% of physicians were employed by physician owned groups, by 2022, an estimated 74% of physicians were employees of hospitals, health systems, or other corporate entities."
from current or proposed conditions, institutions must also ensure that they uphold their responsibility to provide the resources and conditions to make appropriate care possible, while they benefit financially from the care that physicians provide.12
While unions certainly advocate for appropriate physician compensation, the benefits of organizing can be much more far reaching. For my colleagues and I, forming SOPA was primarily about addressing patient safety concerns. Specifically, we oppose expanding of our duties to include performing or supervising procedures on inpatients outside the ED, while the ED is left unattended, a position long supported by AAEM.13 To this end, union negotiations can also affect working conditions and have been used to mandate work hour restrictions for residents, ensure access to critical equipment such as bedside ultrasound, and increase nurse staffing.2 These changes can help ensure that we can provide the safe care our patients deserve. Family leave, including maternity and paternity leave benefits as well as other benefits can be negotiated under union contracts. Unions can also be used to ensure due process for disciplinary actions, something woefully lacking in many practice environments.14
authorizing a union vote, at least 30% of eligible members must sign union authorization cards and file a petition for union election, though it is worth noting that many unions will wish to see 70-80% support before agreeing to represent a potential bargaining group. If, upon the formal NLRB union election, 50% plus one of the votes are in favor of unionizing, the union is officially recognized and collective bargaining can begin.16
We, as emergency physicians and AAEM members, have a duty to ensure that we provide the best possible care to our patients. When possible, physician-owned groups help guarantee that the power to make patient care decisions rests with the physicians, but when physicians are employees of hospitals or health care organizations, unions can be a means to put patients before corporate interests and to ensure our own fair treatment. With the formation of SOPA, I hope the groundwork has been laid for other emergency physicians to explore how union representation may benefit them and their patients.
References
1. https://www.aaem.org/resources/statements/position/primaryresponsibility-of-the-emergency-physician-is-the-care-of-patients-withinthe-ed
2. https://acphospitalist.acponline.org/archives/2022/09/21/free/why-arephysicians-unionizing.htm
3. https://www.cirseiu.org
4. Bowling D, Richman BD, Schulman KA. The Rise and Potential of Physician Unions. JAMA.2022;328(7):617–618. doi:10.1001/ jama.2022.12835
5. https://www.nlrb.gov
6. https://www.ama-assn.org/system/files/advocacy-issue-brief-physicianunions.pdf
7. https://www.nlrb.gov/guidance/key-reference-materials/national-laborrelations-act
8. https://medicaljustice.com/can-doctors-form-a-union/
9. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/ premium/health-policy/prp-physician-practice-arrangements_0.pdf
In practices where working relationships between physicians and administration have ceased to function effectively, and physician concerns are disregarded or responded to only with platitudes and hand waving, unions give physicians the power to ensure they have a seat at the bargaining table, as the NLRB deems some issues “mandatory” subjects of bargaining, such as wages, benefits, and working conditions. Finally, unionizing is a protected activity under federal law and employers are barred from retaliating against employees for exploring unionizing or exercising their union rights.15
Emergency physicians interested in starting or joining a union should first begin speaking with their colleagues to gauge interest. If there is significant interest, speak to one or more unions to get more information. Ask about dues (as these can vary widely), the experience of other physicians represented by the union, and how the union expects to support its physician members. In order for the NLRB to start the process of
10. http://www.physiciansadvocacyinstitute.org/Portals/0/assets/docs/PAIResearch/PAI%20Avalere%20Physician%20Employment%20Trends%20 Study%202019-21%20Final.pdf
11. Thompson SL, Salmon JW. Strikes by Physicians: A Historical Perspective toward and Ethical Evaluation. International Journal of Health Services.2006;36(2):331-354. doi:10.2190/B5CX-UX69-45LY-2D6D
12. Howard D. What Should Physicians Consider Prior to Unionizing. AMA J Ethics.2020;22(3):E193-200. doi:10.1001/amajethics.2020.193
13. https://www.aaem.org/resources/statements/position/primaryresponsibility-of-the-emergency-physician-is-the-care-of-patients-withinthe-ed
14. Hubbell GP. Physician Unions and Work-Life Balance. Missouri Medicine.2022;119(5):406-407
15. https://www.nlrb.gov/about-nlrb/rights-we-protect/your-rights/employerunion-rights-and-obligations#:~:text=After%20employees%20choose%20 a%20union,practices%20and%20other%20mandatory%20subjects.
16. https://www.nlrb.gov/sites/default/files/attachments/pages/node-184/ steps-to-forming-a-union-final-412.pdf
CAN UNIONS EMPOWER PHYSICIANS AND PROTECT PATIENTS?
COMMON SENSE JULY/AUGUST 2023 13
"[W]hen physicians are employees of hospitals or health care organizations, unions can be a means to put patients before corporate interests and to ensure our own fair treatment."
Dealing with Challenging Consultants
Mary Claire O’Brien, MD FAAEM

Up front, verify you have the correct service and the appropriate person. Do this before you launch into long-winded details about the case. “Hi, thanks for answering my page. The web schedule says Orthopedics is on call for Hand this week. Are you the right person to speak to about an ED consult?”
Dear EM Attending,
The senior residents from a particular consult service insist on “stacking” their telephone calls to their on-call attendings, who do not like to be interrupted during the day or woken up at night. This is outrageous! It causes long delays in admission. To add insult to injury, the families are all barking at me—and so are you! Help!
Signed,| Beleaguered Emergency Medicine Resident
Dear Beleaguered,
Been there, understand that. Here are some suggestions for fostering goodwill among nations while you expedite the consultation process.
Don’t say, “Sorry to bother you.” The consultant is on call, and part of that responsibility includes answering pages, speaking with you on the phone, and seeing patients in the ED when formally requested. To apologize at the beginning of your interaction suggests that EM is “at fault” somehow for “bothering” them. Patient care is not an interruption of the consultant’s job. It *is* their job.
Be appreciative. “Thank you for coming to see the patient. Let me know if I can do anything to help you.”
Be helpful. If the consultant’s requests are reasonable—even if they are not part of your “EM work-up”—do what you can to make their life easier. “Of course. I will be glad to order an extra set of blood cultures (or an iron panel or a sedimentation rate).” “Hey, I put the plastics tray and the lidocaine at the bedside. What else do you need?” “Can we get the family from the waiting room for you?” “If you’re hungry, there’s cake in the back.” What goes around, comes around.
Develop rhinoceros skin. Don’t take umbrage when a consultant disagrees with you or points out a mistake. A tough hide is essential for the long-term practice of emergency medicine. Say, “Thank you. That’s helpful.” Remember, the “Ologist” should know more “Ology” than you do. If she did not—she wouldn’t be an “Ologist!” Nurture curiosity— you might learn something.

Develop standardized language.
“What are your thoughts on how best to handle this?”
“I’m not comfortable with that plan. My concerns are…”
“How would you suggest we resolve our differences? I know we both want to do the right thing for the patient.”
Be genuinely open to persuasion.
“I am open to persuasion, but am not yet persuaded.”
“Help me understand why yours is a better plan for the patient.”
Do not be defensive. Being defensive indicates that you are on the opposite side from the consultant. You are not! You are both on the same side, trying to do the right thing for the patient. It is possible to disagree courteously about what the “right” thing is.
ACADEMIC AFFAIRS COMMITTEE >> EM Attending Help!
Calm EM response: Actually, only 80% of patients with surgically proven appendicitis have leukocytosis. Leukocytosis is only 80% sensitive and 55% specific.
COMMON SENSE JULY/AUGUST 2023 14
Consultant pushback: He can’t have appendicitis, his white count is normal.
Be prepared with data and equanimity. Don’t be snarky.
Consultant pushback: “He can’t have appendicitis, his white count is normal.”
Calm EM response: Actually, only 80% of patients with surgically proven appendicitis have leukocytosis. Leukocytosis is only 80% sensitive and 55% specific.
Consultant pushback: “She can’t have pyelonephritis, she doesn’t have a fever.”
Calm EM Response: Well, classically patients with pyelonephritis do have fever. However, this patient is older and she is on immune suppressants. We would not expect her presentation to be classic.
Practice metacognition. In high-stress clinical environments, it is easy to be provoked. Be aware—and be wary—when you are tired, hungry, or in pain. You will be better able to address the needs of others if you first recognize your own needs.

Finally, focus on process, not personalities. “Dr. Consult Resident, I see you are very busy. Have you had a chance to speak with Dr. Consult Attending? The hospital guidelines mandate that consults are staffed within three hours so that patients have timely dispositions. My EM attending has offered to call Dr. Consult Attending herself, since you are tied up.”
EM attendings should set a good example by not throwing busy consult residents under the bus when contacting their supervising attendings. Remember, our consultants are beleaguered too.
Model the courtesy and professionalism that you expect to receive in return.
Consultant pushback: She can’t have pyelonephritis, she doesn’t have a fever.
ACADEMIC AFFAIRS COMMITTEE
the Code to Join the Academic Affairs Committee COMMON SENSE JULY/AUGUST 2023 15
Calm EM Response: Well, classically patients with pyelonephritis do have fever. However, this patient is older and she is on immune suppressants. We would not expect her presentation to be classic
Scan
What Every Emergency Medicine Doctor Should Know about EMS: Scope of Practice
Christopher W. Root, MD NRP,* Kyle Fratta, DO NRP, † and Bryan Everitt, MD NRP FAAEM ‡



Emergency physicians must possess a comprehensive knowledge of the EMS clinician’s knowledge base and clinical capabilities. It is imperative to understand the discrepancies between the various levels of EMS clinicians and the roles of nurse practitioners, PAs, and physicians in EMS systems.
Emergency Medical Responder (EMR)
EMS is an essential part of health care. It’s not just a means of transportation anymore. Modern EMS is vital in diagnosing, treating, and stabilizing patients who need emergency medical attention or need to be transferred to higher levels of care.

The National Highway Traffic Safety Administration oversees the development of nationally recommended educational standards; however, there is no national scope of practice for different levels of EMS providers. This harkens back to the founding of federally funded EMS systems in response to the landmark 1966 white paper “Accidental Death and Disability: The Neglected Disease of Modern Society,” which laid out the lack of standard equipment and minimum training contributing to deaths from trauma.
Most states define in code what the education expectations of the different levels of providers will be, with a significant exception being Texas, a delegated practice state. After initial training, the scope of practice in the field is dictated by protocols, educational standards, and quality metrics, which can be developed and implemented locally, regionally, or statewide. All EMS agencies will have a physician serving as medical director to provide clinical oversight and support the agency’s providers.
EMRs receive introductory training in CPR, AED, bleeding control, BVM ventilation, and other first-aid techniques. They play an essential role in volunteer EMS agencies that may not have the resources to train and retain more providers with advanced certifications. Generally dispatched as first responders, EMRs work alongside providers with higher levels of training to treat and transport patients to definitive care.
Emergency Medical Technician (EMT)
EMTs offer basic life support level care, which includes skills from the EMR scope, triage, basic airway adjuncts, and limited pharmacology. They can administer medications such as epinephrine auto-injectors, chewable aspirin, naloxone, and a few others, depending on local protocols. In some cases, EMTs may be trained in more advanced skills, such as the placement of supraglottic airways or acquisition and transmission of 12-lead EKGs, but these skills are not as common.
Advanced EMT
Advanced EMTs receive additional training after completing EMT basic training. This training covers IV access, basic cardiac monitoring, airway adjuncts, and pharmacology. As a result, they can administer epinephrine during cardiac arrest and initiate crystalloid infusions, such as dextrose solutions for hypoglycemia. Advanced EMTs are a less resource-intensive option for advanced care, similar to EMRs’ role in volunteer organizations.
Paramedic
In most EMS systems, paramedics are the top-level providers regulated by state legislation. After completing EMT training, they undergo additional training in anatomy, physiology, pharmacology, advanced airway management, and pathophysiology. They also have dedicated hospital rotations in various specialties. Paramedics can perform tasks like intubation, 12-lead EKG interpretation, needle thoracostomy, and administer medications like antiarrhythmics, analgesics, and steroids. Some states allow additional skills like blood component administration, surgical airways, and simple thoracostomies.
>>
EMERGENCY
SERVICES SECTION
MEDICAL
COMMON SENSE JULY/AUGUST 2023 16
"Modern EMS is vital in diagnosing, treating, and stabilizing patients who need emergency medical attention or need to be transferred to higher levels of care."
Advanced Paramedic Certifications
Paramedics can expand their education and obtain certifications to work in specialized practice settings. Although most states do not regulate these designations, EMS Medical Directors are responsible for credentialing these clinicians. Critical care paramedics receive additional training in critical care transport, including mechanical ventilation, invasive blood pressure monitoring, and mechanical circulatory support. Flight paramedics are trained in flight physiology, aircraft operations, and critical care transport. Community paramedics have specialized training in community health needs, interdisciplinary care, and sub-acute and chronic conditions. Lastly, wilderness paramedics have additional training in wilderness medicine and providing care in harsh environments.
EMS Nurse Practitioner/Physician Assistant
Advanced practice practitioners (APPs) are valuable members of certain EMS systems, assisting with medical direction, provider education, quality improvement, and clinical oversight. Coordination with a physician’s medical director is necessary for these tasks. Some EMS systems also employ APPs to provide field-response care for low-acuity conditions like uncomplicated infections, medication refills, and behavioral health issues. This approach can help avoid unnecessary ER visits and bring a higher level of care to the scene.
EMS Physician
In most states, physicians are legally required to provide medical direction and clinical oversight for EMS systems. However, certain states have
attempted to remove this requirement. EMS physicians are typically fellowship trained and are responsible for developing protocols for EMS providers, overseeing quality assurance and improvement efforts, and communicating with local, state, and national governments regarding EMS issues. Some EMS systems also have clinical EMS physicians who respond to scenes and provide telemedical evaluations to offer advanced skills and real-time teaching and reduce the burden on emergency rooms for less critical patients.
The system of EMS continues to grow and become more complex. We provide a vital service at the intersection of public safety, public health, and emergency medicine. Emergency medicine physicians must make efforts to understand the local capabilities and resources as they work with EMS clinicians to support and care for their communities.
References
*EMS Fellow, Department of Emergency Medicine, University of New Mexico Health Sciences Center
†Emergency Medicine Resident PGY-2, University of Pittsburgh Medical Center - Harrisburg Hospital

‡EMS Medical Director, Assistant Clinical Professor, University of Texas Health San Antonio, Department of Emergency Medicine
1. National Emergency Medical Services Education Standards. National Highway Traffic Safety Administration. Accessed June 1, 2023. https:// www.ems.gov/assets/EMS_Education-Standards_2021_FNL.pdf
skills plus triage, BLS airway adjuncts, assisting patient with own medications, some injectable and oral medications including epinephrine auto-injectors, naloxone, aspirin, albuterol
Hours EMT skills plus, supraglottic airways, IV access and crystalloid therapy, glucagon, and D50 for hypoglycemia
Paramedic
Hours
Advanced EMT Skills plus intubation, EKG interpretation, ACLS medications, additional IV medications, IO access, cardioversion, transcutaneous pacing, needle thoracostomy
Broadened scope of practice and pharmacology, mechanical ventilation, mechanical circulatory support, surgical airways, tube thoracostomy, etc
2023 Recipients of ABEM 30-year Certificate
AAEM would like to CONGRATULATE the following AAEM member who has achieved this honor but was not included in our previous issue:
Mark J. Tamsen, MD FAAEM
SOCIAL EM & POPULATION HEALTH COMMITTEE
CERTIFICATION INITIAL TRAINING SCOPE OF TRAINING EMR 40 hours Advanced first aid, CPR,
EMT 120 Hours EMR
EMT 300
and AED use
Advanced
1200
Care Paramedic,
Paramedic Variable
Critical
Flight Paramedic, Community
Figure 1. Table Describing EMS Levels of Certification1
COMMON SENSE JULY/AUGUST 2023 17
What is ED Operations?

 Algis Baliunas, MD FAAEM
Algis Baliunas, MD FAAEM
After single handedly trying to empty the city of New Orleans of its oyster supply at SA, I had a great time helping to man the booth for the Operations Management Committee (now the Operations Management Section). I recently graduated from the AAEM ED Operations Certificate course and I was a little nervous because I thought people would expect me to be an expert in ED ops. It turns out the most frequent question that I got was “What is ED operations?”
ED operations is about developing a systematic approach to solving problems. While it’s most useful for ED directors/assistant directors, everyone needs to know something about operations as it affects our ability to care for our patients. Most residents get some exposure to this subject in their last year of residency, where they are typically in charge of patient flow in the department and putting out the daily fires that inevitably occur. What most graduating residents don’t realize is that, over the span of their career, the greatest challenge will not be the medicine, but how to decompress your packed waiting room, handle patient complaints, keep administration happy, and maintaining healthy relationships with nursing and ancillary staff. Here are some examples of the problems we face daily.

Problem One
Your waiting room times have increased by 20% and left without being seen numbers have now topped 6%. Your administration wants to set up a meeting next week to deal with “the problem.” How do you respond? One way to respond would be to mention that hospital boarding times have increased, beds aren’t being cleaned due to labor shortages and your nurses are already stretched too thin. If the administration could solve these issues, do you think they would be coming to you for answers?
Instead, focus on what you can control, which is the ED itself. How should you look at the data? Perhaps create a value stream map of each process a patient goes through and see what actually adds value. Is your triage process too long? How about quick registration and a pull to full model where most triage occurs in a bed? Does that bed have to be an actual bed, could it be a chair or hallway? You might calculate the percentage of high acuity patients and adopt a split flow triage, where low acuity patients are evaluated and placed back in the waiting room
awaiting results. Maybe it’s your coverage. You calculate the patient arrivals by hour versus physician shifts and find that the 12a-12p shift should really be a 9a-9p shift.
Armed with this data, you go to the meeting and propose a split triage model with bedside registration and pull-to-full when beds are available along with adjusting physician coverage and propose to measure the outcome by tracking triage times, door to doc times, door to disposition times, and LWBS percentages.
Problem Two
You were just appointed ED director two years out of residency at your hospital, mainly because nobody else seemed willing to do the work. After two weeks on the job, your hospital CEO comes to you and says “Something needs to be done about Dr. Jones.” With a frightened look on your face, you ask what’s wrong, expecting some clinical deficiency. It turns out that Dr. Jones has been with the group for 15 years and is an excellent clinician, but administration over the past six months has received multiple complaints from nursing that he is belittling and frequently screams at staff when he perceives that they are not working fast enough. How do you approach someone that has been at your hospital far longer than you have?
This would be a good time to develop a formal plan for approaching these matters. This might include an initial information gathering where you talk to the people directly involved, you then formulate a plan and script prior to the meeting and you start with an informal conversation with the assistant director present as your witness. Your process then includes a period of monitoring and a formal letter if no improvement is made. If there is no response to the formal letter, you have either reviewed the medical staff policies on physician conduct or helped draft them yourself so that formal action can be taken.
Armed with this plan, you have a meeting with Dr. Jones and find out that he is in the middle of a divorce involving a bitter child custody battle. You suggest a peer coaching program offered by the hospital and he seems
OPERATIONS MANAGEMENT SECTION
"If the administration could solve these issues, do you think they would be coming to you for answers?"
Countinued on page 40 >> COMMON SENSE JULY/AUGUST 2023 18
"How do you approach someone that has been at your hospital far longer than you have?"
Actually, I Am the Doctor
Courtney Albury, DO
This is the sentence I find myself saying to many of my patients after walking in the room, even after introducing myself as the doctor a few seconds prior. Only my colleagues with this same lived experience can understand the extent of this never-ending frustration. Colleagues who do not struggle with the same issue wonder why it is a problem. Why is it so taxing to take 10 seconds to clarify with the patient or my team? Once or twice would not be a problem—it is constant, numerous times a day, every day, and comes with an emotional toll on the side.
Despite the growing number of female physicians in medicine in recent years, it is the assumption that if a female walks into the room, she will be the assumed nurse and the male in the room will be the assumed doctor. The thought behind this stereotype is rooted mainly in our patriarchal societal history. Females were seen to be nurturing, caring and subordinate—which many feel is more consistent with the nursing profession—whereas the doctors were seen as the authority figures. The doctor role was historically seen as a masculine role, and females were typically excluded from this role in early years. As a society in general, this obsolete mindset still has not caught up with the times.
According to the AAMC, the percentage of female physicians increased from 28% in 2007 to 36% in 2019. In addition, according to AAMC medical school enrollment reports, 2019 was the first year in which female medical students outnumbered males by 1%. This is why it is particularly important to discuss the emerging future of medicine with our patients and team. We have and will continue to have better female representation in the workforce. Our patients and our team need to recognize this and respect it.
It is already particularly difficult as a young female doctor to have patients take me seriously when I walk into a room. The first five minutes are usually encompassed by me proving that I am old enough and capable of being their doctor. This adds another obstacle to an

already-difficult career, and this obstacle is one that maybe only colleagues with the same lived experience can fully understand. I worked hard to get here, I care, and I do good work every day. I should not also have to be male.
With patients typically picturing physicians as older gentlemen, they are less inclined to trust my clinical decisions, as evidenced with their response, “Are you sure you’re old enough to be making these decisions?” This routinely comes from older individuals while they look at me with a facial expression that says, “Aww, that’s cute that you’re here playing doctor, what do you want to be when you grow up?” I have been told to take this as a compliment, but I believe this undermines the tone behind it. After 20 plus years of schooling, I am qualified to make these decisions. I dedicated my entire young adult life in school sacrificing time with friends and family, forfeiting much of the free time I could have spent having fun and enjoying my youth. Because of this, it never loses its sting when someone questions the validity of my credit— especially when this happens multiple times a day. Defending my qualifications and practicing medicine for every encounter makes it difficult to establish respectful rapport.
We have come a long way as a society, as evidenced by the fact that we let women into medical school now. We still have a big task at hand which is to gently but firmly educate patients that they are bound to be cared for by a female physician in the workforce nowadays. The whole team can help take on the burden by explaining and reinforcing the roles of all team members for the patient. For example, if a patient does not recall seeing the doctor (despite the female doctor already having been in the room), the rest of the team can reinform them that you are, in fact, the doctor and are the qualified, respected leader of the health care team. If we can help educate them on this
every time, they will no longer be in shock the next time a female physician walks into their room as the leader of the team caring for them.
If we introduce ourselves as “the doctor,” we are not kidding. We have earned this title through very hard work and sacrifice. If the whole team gently but persistently reinforces this for patients, it will help society catch up with the times.
References
1. Boyle P. Nation’s physician workforce evolves: more women, a bit older, and toward different specialties. AAMC News. February 2, 2021. Accessed May 29, 2023. https://www.aamc. org/news/nation-s-physician-workforceevolves-more-women-bit-older-and-towarddifferent-specialties.
2. Why is there a perception that nursing is a female occupation? Best Colleges Online. August 2, 2021. Accessed May 29, 2023. https://www.bestcollegesonline.org/faq/ why-is-there-a-perception-that-nursing-is-afemale-occupation/#:~:text=Rooted%20in%20 Patriarchy%20While%20the%20nursing%20 profession%20has,to%20the%20authority%20 figure%20of%20a%20medical%20doctor.

3. Takeshita J, Wang S, Loren AW, et al. Association of Racial/Ethnic and Gender Concordance Between Patients and Physicians With Patient Experience Ratings. JAMA Netw Open. 2020;3(11):e2024583. Published 2020 Nov 2. doi:10.1001/ jamanetworkopen.2020.24583


COMMON SENSE JULY/AUGUST 2023 19
“If we introduce ourselves as 'the doctor,' we are not kidding. We have earned this title through very hard work and sacrifice.”
Dear Students
Yusuke Kishimoto, MD

Although Match Day was supposed to be an exciting day for all of us to find out where we were going to start our new residency journeys, these were some of the words that stuck with me. It was upsetting to hear but I was more hurt and disappointed. It denies all the passion and dedication that my colleagues and I have for this field as well as the decades of hard work our mentors and predecessors have contributed to the history of emergency medicine. I’m sure that many of my colleagues will agree that all throughout clinical years, many of our attendings scoffed that we were even thinking about EM. What surprised me the most was some of those voices were from EM physicians themselves. Of the 14 people from my friend group who were initially interested in EM, only six ended up applying.
The reasons for the decreasing number of applicants are multifaceted but some are painstakingly clear: the expansion of scope of practice by non-physician practitioners (NPPs), the predatory practice of corporate medicine, and the negativity plaguing the internet.
I respect nurses and all the work they do. They are the cornerstone for supporting the emergency department. However, there is just no substitute for a licensed board-certified emergency physician. To begin with, the amount of clinical hours, education, training, licensing examinations, and standards are just incomparable. Alarmingly, an increased number of NP/PA programs have started to appropriate the term “fellowships/ residencies” and compete with resident’s for procedures.1 As is the case with other fields of practice, I believe there should be distinct differences, as seen between optometrists vs. ophthalmologists, paralegal vs. attorneys, and teachers-assistants (TAs) vs. professors. We wouldn’t want optometrists performing eye surgery, paralegals giving legal advice, or TAs leading courses.2,3 An unfortunate fact is that at least two of these things are currently happening as well. Optometrists are putting legislative pressure for approval to do surgical procedures such as LASIK and TAs are increasingly the de facto teachers for college courses. Some of the things we are seeing in EM are playing out in the ophthalmology world and college campuses. The common denominator: money interests working tirelessly to turn medicine, surgery, and education into consumer products, and the patient/students into consumers.
But as voiced by Dr. Rebekah Bernard from the American Medical Association (AMA), “It’s not an us-vs-them. This is a team-based approach.”4 Each position is vital in the functioning of the system, however, there should be clear borders on roles and functions of each, just as much as running a code. Thankfully in addition to AAEM, organizations such as AMA and Physicians for Patient Protection (PPP) have been actively focused on strongly lobbying against these issues with many successes and expecting more to come.
Private equity is parasitizing not just emergency medicine, but all fields
across medicine. They both simply operate by different principles. Maximizing profit and monetary gain should never be in the forefront of the patient-physician relationship. There are a multitude of concerns being voiced, even by people who work for these companies regarding issues of complacency, morality, greed, staffing, and safety. Many of my colleagues and I joined medicine to care for our patients, not to make money off vulnerable people coming to seek help.
“EM is a perfect back up specialty since they’ll take anyone.”
“It’s a saturated and dying field.”
A sad fact is that residents and NPPs are cheaper to hire. As seen in the recent years (2019-2023), over 40 new EM programs were accredited by the ACGME with many owned by private equity firms. They have also been making open moves to hire more NPPs rather than physicians. Fortunately, some students have been taking notes and many of the presoap unfilled spots were from these private equity programs. Through increase in open communication, education, and advocacy, I foresee this trend to continue and strengthen the fight against corporate medicine. We could only look forward to the ACGME revamping their requirements to slow the explosive growth of residencies. Other key victories recently include the judge’s decision to deny Envision’s motion to dismiss the AAEM-PG vs. Envision lawsuit and US Acute Care Solutions’ (USACS) losing their contract at Santa Clara Valley Medical Center to a local democratic group.5,6
The negativity surrounding emergency medicine through Reddit, Student Doctor Network, and Twitter was astounding. For example, just searching for the phrase “the future of EM” showed over 20 plus Reddit threads where people have been actively discussing topics such as the unprecedented increase in unfilled positions for the past three years and the corporate practice of medicine. Many posts and comments were from concerned medical students worrying if they should switch and jump ship to other specialties with a majority of attendings advising to stay clear. Despite this, I was glad to see that compared to 2021 the threads during 2023 have been slightly more positive talks about how “EM might make a comeback” or “the job market is improving” with a unified stance from residents and attendings alike on their negative view on private equity/ CMGs and their ill effects on health care. However, I rarely encountered comments or posts that encouraged becoming involved in organizations or societies to improve the current climate.
554 unfilled positions is an unprecedented and frightening number, but let’s break it down. In 2018 there were 220 EM programs (2278 positions) compared to 2023 with 287 EM program (3010 positions).7,8 Similarly in family medicine (FM) and internal medicine, categorical (IM) from 2018 to >>
CAL/AAEM
“It’s a dumpster fire. I don’t know why anyone would apply EM anymore.”
COMMON SENSE JULY/AUGUST 2023 20
"There were so many spots open this year. You don’t even need a SLOE to SOAP in.”
2023, there has been an explosive increase in programs seen by 557 FM Programs (3629 positions) to 773 (5088 positions) and 517 IM programs (7542) to 668 (9725 positions).7,8 Overshadowed by EM’s sudden numbers, this year’s match cycle saw colleagues in FM and IM unfilled by 557 and 380 positions respectively. Since 2014, the average number of new FM and IM programs were 10 and 15, with unfilled positions around 140 and 70 respectively. Though reasons are plenty, since 2018 there was a doubled rate of new programs that may have played a role with the gradual increase in unfilled positions in both FM and IM. Now, the spike in EM’s unfilled positions during 2022 with the aforementioned reasons may be coupled with the release and scare of the EM physician workforce projection for 2030 released a year previously suggesting a surplus of >7,800 EM physicians (see graph 3).9 However, through the release of this workforce study, the projections have vastly changed shown by the previous match cycle results.
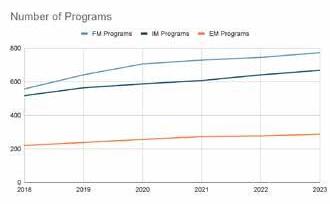
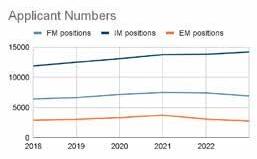
With a deeper analysis, this should be a wake-up call for larger underlying issues, the same issues that were mentioned multiple times: increase in NPPs in the department and growth of residency programs that are shifting the supply-demand curve. Some plausible solutions to mitigate

these issues would be to actively advocating against scope creep and independent practice of NPPs as well as raising the ACGME accreditations standards to slow the growth of new residency programs.
I’m still young, naïve, and inexperienced. I feel presumptuous to even borrow this platform to speak regarding these topics. But with the recent negativity and bleak mood surrounding emergency medicine, I wanted to take this opportunity to speak up. It’s slight, but positive steps are being made. We just have to push further with the current traction we have.
To our medical students, I urge you to be curious, stay involved, and ask questions. Have your EM interest group invite guest speakers to talk about current events or projects. Get a group of friends to attend a scientific assembly, EM symposium, or an advocacy conference. Knowing once you’re a resident is too late. Being unaware causes us to cyclically feed the problem. Don’t let your passion for the field die out on forums and tweets. If you don’t like the current direction or environment that emergency medicine is in, let’s change that.
We are the future of emergency medicine. Emergency medicine is not dead.
References
1. Phillips, A., Sites, J, Quenzer, F., & Lercher, D. (2023). Effects of NonPhysician Practitioners on Emergency Medicine Physician Resident Education. Western Journal of Emergency Medicine. 24(2), 224-230; https://doi.org/10.5811/westjem.58759
2. California State Legislature. (2018) AB-2336 Optometry: Certification to Perform Advanced Procedures. Retrieved from: https://leginfo.legislature. ca.gov/faces/billTextClient.xhtml?bill_id=202120220AB2236
3. California State Legislature. (n.d.). Business and Professions Code - BPC Division
3. Retrieved from: https:// leginfo.legislature.ca.gov/faces/codes_displayText.
xhtml?lawCode=BPC&division=3.&title=&part=&chapter=5.6.&article=
4. Bernard, R. (2022, August 23). Scope Creep and Patient Care. AMA. https://www.ama-assn.org/practice-management/scope-practice/rebekahbernard-md-im portance-physician-led-care
5. American Academy of Emergency Medicine Physician Group, INC v. Envision Healthcare Corporation, et al. 22-cv-00421-CRB (2022) https:// www.aaem.org/UserFiles/file/USDCDoc47.pdf
6. Geha, J. (2023, March 21). Santa Clara County Doctors Celebrate New Management. San Jose Spotlight.
7. https://sanjosespotlight.com/santa-clara-county-valley-medical-centerdoctors-celebrate- new-management-hospital-san-jose-health-care/
8. Results and Data: 2018 Main Residency Match. (April 2018). https://www. nrmp.org/wp-content/uploads/2021/07/Main-Match-Result-and-Data-2018.pdf
9. Advance Data Tables: 2023 Main Residency Match. (March 2023). https:// www.nrmp.org/wp-content/uploads/2023/04/Advance-Data-Tables-2023_ FINAL-2. pdf
10. Marco, C., Courtney, M., Ling , L., Salzburg, E., Reisdorff, E., Gallahue, F., Suter, R., Muelleman, R., Chappell, B., Evans, D., Vafaie, N., Richwine, C. (2021). The Emergency Medicine Physician Workforce: Projections for 2030. Annals of Emergency Medicine. 78(6), 726-737; https://doi. org/10.1016/j.annemergmed.2021.05.029
CAL/AAEM
COMMON SENSE JULY/AUGUST 2023 21
QUEST: A Framework for Value-Based Care in Emergency Medicine

 Tom Scaletta, MD MAAEM, Akiva Dym, MD FAAEM, and Anthony Rosania, MD MHA FAAEM
Tom Scaletta, MD MAAEM, Akiva Dym, MD FAAEM, and Anthony Rosania, MD MHA FAAEM
delivery. The hospital is increasingly viewed as a costly choice, and care models that remove care from within the four walls of our hospitals are gaining attention.
Value-based care (VBC) aims to improve patient outcomes while controlling health care costs. Since the emergency department (ED) is a gateway to most medical services, including inpatient hospital care, outpatient specialty care, and community resources, it behooves emergency physicians (EPs) to understand and embrace the concept.
VBC represents a departure from the conventional fee-for-service (FFS) model, where physicians are remunerated based on the number of patients and procedures performed, regardless of their effectiveness.

In recent years, Medicare Advantage has emerged as the VBC alternative to traditional Medicare, becoming the majority choice for enrollees in 2023. Consequently, many payers are now following suit to incentivize health care providers to deliver excellent care that emphasizes cost, quality, and outcomes. With this mind shift, the U.S. is poised for a paradigm shift after years of failed attempts.
According to a report by the American Hospital Association, as mega-corporations such as Amazon, CVS, United Health Group, Walgreens, and Walmart continue to assemble the necessary components, including brick-and-mortar care sites, prescription delivery, and chronic disease management, doctors and hospitals must prepare for increased competition in the health care marketplace.1 Additionally, tech giants like Apple and Google/Alphabet are creating platforms to facilitate health care
Success in this competitive landscape will be measured by value from the perspectives of patients, physicians, and payers. This value is defined as the benefit-cost ratio, with VBP benefits including quality, utilization, efficiency, satisfaction, and teamwork, all of which can be remembered by the acronym QUEST.2

To improve the experience of EPs and our patients, it is crucial to implement one or more components of QUEST, assuming the cost is reasonable. Cost represents any obstacle to achieving these goals, including financial barriers, time constraints, political capital, and competing priorities. Therefore, physicians and hospitals must prioritize VBC and remain vigilant in changing market dynamics.
Quality
Quality is the foremost goal in every ED, and evidence-based practice is the foundation for defining it. However, even the most competent nurses and physicians may make unintentional errors, so it is crucial to incorporate safety layers to prevent patient harm.
After ED discharge, patients may face three cardinal wellbeing issues: missed diagnoses, unanticipated worsening of a correctly diagnosed problem, or inadequate aftercare. Conducting wellbeing checks on discharged patients is essential to mitigate these issues and avoid potential legal claims. This can be achieved through nurse callbacks or issues screening technology, which helps identify quality breaches and facilitate timely interventions. By implementing a follow-up mechanism, EDs can improve care quality and ensure better patient outcomes.
Utilization
Utilization is a critical factor in the ED, and EPs make the costliest decision of admitting a patient approximately six times during each ED shift. Unnecessary admissions consume over 40 hours of inpatient staff time and contribute to ED boarding, impacting sicker patients’ care. To address this issue, health care providers must focus on safely avoiding admissions.
>>
OPERATIONS MANAGEMENT SECTION
COMMON SENSE JULY/AUGUST 2023 22
"This value is defined as the benefit-cost ratio, with VBP benefits including quality, utilization, efficiency, satisfaction, and teamwork, all of which can be remembered by the acronym QUEST."
Medicare incorporates the rate of observation status and hospital readmissions within 30 days into VBC reimbursement, highlighting the importance of reducing unnecessary admissions. ED case managers play a crucial role in cost reduction by providing a wide range of assistance, including arranging outpatient stress echocardiograms and placing medically fragile patients in skilled nursing facilities when acute care hospitalization can be avoided. By leveraging the expertise of ED case managers, EPs can improve utilization while also delivering better patient outcomes.

Efficiency
Efficiency is crucial in achieving optimal clinical area turnaround time, particularly for discharged patients. EPs should remain focused, avoid distractions, and make quick, informed decisions to ensure efficiency. They should consistently check test results and take immediate action when necessary.
The most efficient doctors constantly seek opportunities for parallel processing to increase productivity. For example, they may prepare aftercare instructions while a technician irrigates a laceration.
Satisfaction
Patient satisfaction is essential to health care as it reflects the patient’s perception of the quality of care they receive. Research shows that patients can accurately determine whether they received high-quality care, and this perception is strongly correlated with actual quality care.3
Moreover, satisfied patients trust their doctors more and adhere to aftercare plans better, improving clinical outcomes. They also file fewer malpractice claims, highlighting the importance of patient satisfaction in health care.
Teamwork
Effective teamwork involves collaboration among payers, doctors, and hospital administrators to achieve VBC goals. The team should work together to streamline operations workflows and identify opportunities for ongoing improvement in all aspects of the QUEST framework. Such collaborative environments facilitate excellent patient care and staff satisfaction.
The QUEST framework is a balanced scorecard considering patient experience, physician expectations, and payer requirements. Collecting data around these performance indicators is essential to measure the impact of any changes made to the QUEST items. For example, reducing staff hours to improve productivity may negatively impact patient satisfaction.
QUEST provides a structured approach to setting VBC goals and prepares us for the future of health care. It is crucial to foster collaboration among all stakeholders to achieve success, and EPs should strive to be early adopters as our health care system shifts from FFS to VBC.
References
1. https://www.aha.org/system/files/media/file/2023/02/The-Buzz-DisruptionOutlook-2023.pdf
2. https://www.medscape.com/viewarticle/893987
3. https://bmjopen.bmj.com/content/bmjopen/3/1/e001570.full.pdfw
OPERATIONS MANAGEMENT SECTION
COMMON SENSE JULY/AUGUST 2023 23
"QUEST provides a structured approach to setting VBC goals and prepares us for the future of health care."
I T C ’ s A d v a n c e s i n C a n c e r I m m u n o t h e r a p y

( A C I ) p r o g r a m s o f f e r f o c u s e d c l i n i c a l e d u c a t i o n o n a d i s e a s e s t a t e o r t o p i c a t n o c o s t t o t h e e m e r g e n c y c a r e t e a m . A t t e n d e e s o f t h e s e h a l f - d a y , i n n o v a t i v e p r o g r a m s g e t i n - d e p t h t r a i n i n g i n i m m u n o t h e r a p y t r e a t m e n t t h a t c a n b e d i r e c t l y a p p l i e d t o p a t i e n t s i n e m e r g e n c y c a r e .

2023 PROGRAMS
ACI: A Focus on Cellular Therapies & T Cell Engagers
Aug. 17 | Hybrid | Washington, DC & Virtual
Join SITC's panel of experts for an in-depth education on all aspects of cellular therapies & T cell engagers.


ACI: Online Courses




2 0 2 3 A C I : I n t r o d u c t i o n t o B i o m a r k e r s
ACI: A Focus on Hematologic Malignancies

Oct. 19 | Virtual | Zoom Webinar
Gain leading industry insights on the clinical implementation of immunotherapy for hematologic malignancies.
2 0 2 3 A C I : M e c h a n i s m s o f I m m u n e - r e l a t e d A d v e r s e E v e n t s ( i r A E s )
2 0 2 3 A C I : I n t r o d u c t i o n t o I m m u n o l o g y
2 0 2 3 A C I : B a s i c P r i n c i p l e s o f C a n c e r I m m u n o t h e r a p y U n d e r s t a n d b a s i c i m m u n o l o g y a n d i m m u n o t h e r a p y p r i n c i p l e s a n d m e c h a n i s m s w i t h C E a n d M O C - c e r t i f i e d o n l i n e c o u r s e s f r o m S I T C ' s A C I s e r i e s G a i n a n i n - d e p t h u n d e r s t a n d i n g o f h o w i r A E s f u n c t i o n a n d t h e k e y b i o m a r k e r s i n i m m u n o t h e r a p y t r e a t m e n t w h i l e e a r n i n g C E a n d M O C c r e d i t s
The 2023 ACI series is jointly provided by the Partners for Advancing Clinical Education and the Society for Immunotherapy of Cancer in collaboration with the Association of Community Cancer Centers, the Advanced Practitioner Society for Hematology and Oncology and the Hematology/Oncology Pharmacy Association. These programs are provided in collaboration with the American Academy of Emergency Medicine

I N - D E P T H E D U C A T I O N F O C U S E D O N Y O U R S P E C I A L T Y R e g i s t e r a t s i t c a n c e r o r g / a c i | # L e a r n A C I C L I N I C A L E D U C A T I O N P R O G R A M S F O R E M E R G E N C Y P H Y S I C I A N S F R E E F O R H E A L T H C A R E P R O F E S S I O N A L S , S T U D E N T S , P A T I E N T S A N D P A T I E N T A D V O C A T E S . C M E , C N E , C P E A N D M O C C R E D I T S A V A I L A B L E .
™
S
SCAN OR VISIT SITCANCER.ORG/ACI TO LEARN MORE & REGISTER
COMMON SENSE JULY/AUGUST 2023 24
Data-Driven Behavior Change: How Utilizing Metrics in Emergency Medicine Can Drive Physician Burnout

 Andrew Grock, MD* and Al’ai Alvarez, MD †
Andrew Grock, MD* and Al’ai Alvarez, MD †
Alegal dispute between Amazon and one warehouse’s unionized employees led to the release of shocking working conditions. The exposé, titled “2022 Internal Documents Show Amazon’s Dystopian System for Tracking Workers Every Minute of Their Shifts,” describes how Amazon tracks their workers’ productivity by recording every minute they spend “off task.”1 Amazon states the tracking program’s goal is to encourage employees to be more productive since they know they are being tracked. Employees who spend too much time “off task” may have to explain the occurrences to the boss, receive written disciplinary warnings, or even be fired. The report that Amazon employees urinated in bottles to avoid having their bathroom breaks documented as “off task” time was most appalling. After initially refuting this report, Amazon later admitted that this does happen regularly. This Orwellian oversight, terrifying as it may be, sounds unfortunately familiar to some of our emergency departments.
The rise in electronic health records has enabled tracking of every part of the patient, doctor, and department experience.2,3 This data can help identify critical systems problems that interfere with patient care. It can also serve as feedback to doctors on the efficiency of their care and help them streamline their practice. Data can also highlight inefficiencies in practice that prevent doctors from providing the care they are trained to do.
However, a dearth of literature exists describing whether or not this data’s use is ethical and within the purpose of helping doctors and patients. One example worth discussing is an EM staffing company that emails its entire physician staff a monthly spreadsheet with every physician’s non-anonymous metrics. What does this tell us about what this company values?

excellent features of care that EM physicians provide are ignored by these metrics. This monthly report card on “key performance indices” implies that all our work boils down to speed—and thus RVUs. This depersonalization of our work can lead to burnout.
Burnout consists of emotional exhaustion, depersonalization, and reduced personal accomplishment. Metrics directly depersonalize the work of physicians. Furthermore, non-anonymized report espouses name, blame, and shame. In quality improvement and patient safety work, we know systems and processes play important roles beyond teams and human factors impacting care turnaround times. Metric reports that pin physicians as the reason for inefficiencies and delays are dangerous and only add to burnout. Burnout, in turn, leads to further inefficiencies, higher cost of care, adverse patient outcomes, and attrition of doctors. Without care and context, these reports devalue all the incredible things we do in emergency medicine.
The Amazon report on workplace metrics serves as a wake-up call for physicians that data without context and care for the health care teams is dangerous. In 2007, the Institute of Healthcare Improvement released the Triple Aim: improving the health care experience, improving population health, and decreasing the per capita cost of health care. Understanding the role of the health care team, including their well-being, has led to the evolution of the Quintuple Aim to include Clinician Well-Being and Health Equity.4
What if instead of metrics, these emails included the great saves, examples of interpersonal connections that earned a patient’s trust that led to better care, excellent discharge instructions that prevented a bounceback, or an acknowledgment of the time spent clarifying goals of care that led to a patient dying with dignity? So many more consistently
During busy shifts, many of us struggle to find the time to fulfill the basic level of Maslow’s hierarchy of needs. The unintended consequences of our strategies should always be considered. Amazon’s policies resulted in numerous credible reports of employees urinating in bottles since they
>>
WELLNESS COMMITTEE WELLNESS COMMITTEE
COMMON SENSE JULY/AUGUST 2023 25
"Metric reports that pin physicians as the reason for inefficiencies and delays are dangerous and only add to burnout."
worried about the disciplinary implications of using the bathroom. This way of utilizing metrics would only compromise the physician’s basic needs and self-care.
We must balance our need for efficiency and the nature and meaning of our work as physicians and healers. Suppose we want to move the needle to minimize variations of practice. In that case, sending out individual emails with metrics compared to the group average would significantly reduce shame and competition. It seems too easy to include a brief message describing the purpose of the metrics in each email and acknowledging that they fall short in evaluating all that we do. Even better, instead of emailing the metrics, each physician is aware of trends individually during a regular evaluation and feedback session. These metrics are used as a jumping-off point to discuss the physician’s strengths and strategize areas of improvement.
Financial goals and rapidly evolving technology make tracking our every move easier. How might we use data to improve physician well-being and sense of fulfillment rather than harm them? How are you currently using data in your department that breaks physicians, and how might you change how it is delivered? We must do all we can to avoid creating an environment that fosters a dystopian, Amazon-like tracking system. Patients are not customers. Doctors are humans, too.
References
*UCLA Emergency Medicine Department, @AndyGrock
†Director of Well-Being, Stanford Emergency Medicine, @alvarezzzy
1. Internal Documents Show Amazon’s Dystopian System for Tracking Workers Every Minute of Their Shifts. Accessed June 1, 2023. https:// www.vice.com/en/article/5dgn73/internal-documents-show-amazonsdystopian-system-for-tracking-workers-every-minute-of-their-shifts
2. Welch SJ, Asplin BR, Stone-Griffith S, et al. Emergency department operational metrics, measures and definitions: results of the Second Performance Measures and Benchmarking Summit. Ann Emerg Med 2011;58(1):33-40. doi:10.1016/j.annemergmed.2010.08.040

3. Almasi S, Rabiei R, Moghaddasi H, Vahidi-Asl M. Emergency Department Quality Dashboard; a Systematic Review of Performance Indicators, Functionalities, and Challenges. Arch Acad Emerg Med. 2021;9(1):e47. doi:10.22037/aaem.v9i1.1230
4. Itchhaporia D. The Evolution of the Quintuple Aim. J Am Coll Cardiol 2021;78(22):2262-2264. doi:10.1016/j.jacc.2021.10.018
WELLNESS COMMITTEE
"How might we use data to improve physician well-being and sense of fulfillment rather than harm them?"
COMMON SENSE JULY/AUGUST 2023 26
The “Lowdown” on Wills and Testamentary Trusts
Gary M. Gaddis, MD PhD MAAEM FIFEM, Aging Well in Emergency Medicine Interest Group Co-Chair

ne of the goals of the Aging Well in Emergency Medicine Interest Group (AWIEMIG) is to serve as a form of institutional memory for others in our specialty. One aspect of institutional memory is for those of us a bit long in the tooth to tell less senior members of the profession some life tips to help them avoid some of the mistakes that we have seen others make, or that we have made ourselves.
Toward that end, this issue’s installment from our AWIEMIG concerns wills and testamentary trusts. Herein, we are not considering the trusts that those who sought to decrease the influence that the robber barons of industry enjoyed at the dawn of the 20th century. However, what will be covered are key types of trust agreements that can be created by emergency physicians early in their careers, near mid-career, or in late career to protect their financial interests, especially when the physician themselves cannot act in their own self-interest. Do you think you don’t need a trust agreement? Well, if you have a spouse and especially if you have children, think again!
For the purpose of this article, a trust is a legal tool which permits someone who owns something of value (which generally includes cash, investments such as mutual funds, stocks and bonds, property, and/or other things of financial value), to designate someone else or some other legal entity to be the director of how that asset is to be managed and distributed if the owner of those assets becomes incapable of performing that directive
Ofunction themselves. The person or entity that assumes this function is known as a trustee. Trustees are most often individuals or corporations. When the trustee is a corporation, the role of trustee is generally assumed by a trust officer or other employee of that organization.
If you are a high net worth individual, which in the parlance of many banks and investment companies means you have at least $500,000 or $1,000,000 of assets under management, then trustee services are often provided gratis by the institution with which you have investments. However, for those of you earlier in your careers who are not yet a high net worth individual or couple, you will probably have to pay a nominal fee to gain access to a trustee’s services. That small investment is definitely not something about which to be penny wise and pound foolish. Just as any emergency physician should have an attorney conversant in contract matters to review a proposed employment agreement before signing it, so emergency physicians should expect to pay a fee for a trustee’s potential services, should they become needed.
As to the type of trust that a trustee can administer, know that there are many different types of trusts, and this review will not discuss all

thirty types that exist. Rather, the focus here is upon the type of trust that is most important for many emergency physicians, a testamentary trust. Testament refers to one’s last will and testament. Which establishes that, before delving further into trusts, one must first consider whether one needs to work with an attorney to create a will.
No one, especially those early in their careers, likes to think about the prospects of their untimely death. However, death is a fact of life, and unfortunately, some who one would expect to be an early career physician becomes a former physician due to accidents or fatal illnesses. Personally, I know of a resident whom I helped train who died in a tragic bicycle crash before age 30, causing a probable neck injury that led to his drowning in water less than a foot deep, leaving a widow and two children. I also know of several colleagues who have died of medical illnesses before reaching age 50. Being a physician does not insure against an early death. When physicians meet a premature demise, if they have not created a will, all of their assets will be managed by probate court.
This outcome may not be such a disagreeable prospect for many single early career physicians, because they are likely (due to medical school debts) to have a negative net worth (one’s net worth is the sum of all of a person’s financial assets minus the sum of their financial liabilities). However, if such a physician dies with a negative net worth, their educational loan may or may not include a provision allowing the loaning institution to collect the remainder of the unpaid debt from
AGING WELL IN EMERGENCY MEDICINE INTEREST GROUP
>> COMMON SENSE JULY/AUGUST 2023 27
"Do you think you don’t need a trust agreement? Well, if you have a spouse and especially if you have children, think again! "
loan co-signers. Such co-signers are often the physician’s parent or parents. Thus, even unmarried young physicians may have a motivation to enable payment of their loans via proceeds from life insurance, and if there is life insurance covering the physician, they are wise to establish a will to direct how those proceeds are to be distributed.
However, once the physician marries, and especially when the physician has children, it is usual and proper to become concerned about the financial welfare of one’s dependents, in the event of the physician’s untimely death. Toward optimizing one’s dependents’ financial status in case such an event occurs, one can purchase life insurance, with a death benefit sufficiently large to meet the physician’s family’s perceived needs. Considerations that impact the size of one’s death benefit include whether one’s spouse is employed or employable in a high-wage occupation, and whether one hopes to finance their children’s post-secondary educations, and the like. A financial counselor can help a young physician consider the variables that will influence the size of the death benefit that they will choose.
I believe that most younger physicians are wisest to purchase term life insurance, because term insurance is the most economical way to gain a large death benefit for the welfare of their survivors. A reasonable rule of thumb is to insure one’s-self for at least five times their annual pre-tax income, but some may find that a death benefit in excess of this is more to their preference. The younger one’s age, the greater may be their need to provide a large sum for their survivors. Again, to have a financial counselor to guide the physician is a wise idea because a counselor can spend time with a physician and their spouse to learn their expectations and arrive at a reasonably-sized death benefit.
Once one has arranged to purchase life insurance, if the physician meets an early and
untimely demise, the death benefit from the insurance policy will convert the physician’s estate from having a negative net worth to having a positive net worth. Because the insurance proceeds will be substantial, and because those proceeds will enable the doctor to fulfill their wishes for their survivors, it is common to set up a testamentary trust. This type of trust becomes effective upon the need to activate the provisions of the physician’s will. Such a type of trust is an especially useful tool for younger physicians who have both a spouse and children.
If only the physician themselves dies unexpectedly, typically all life insurance proceeds would quickly flow (courtesy of the will) to the spouse, and there may be no need to execute a trust—the physician’s will may suffice as a testamentary trust typically names the spouse as the trustee if the spouse survives the deceased physician. On the other hand, those who die without a will (which is called being intestate) will have survivors who will not be pleased with the extra time required for a probate court to take final actions as regards one’s financial assets. Bottom line: Be sure you have executed a last will and testament to save your (potential) survivors a lot of headaches.
Moreover, if the physician and the spouse have children, in the event that the physician and the spouse die together, such as in a motor vehicle crash, then a testamentary trust is a crucial tool. It can be just the ticket to enable
the wishes of the physician and their spouse to be met. My wife and I established a testamentary trust upon the birth of our first child, while I was a first-year resident, and then periodically updated our trust agreement as life circumstances (such as the birth of a second child) dictated.
A testamentary trust typically names who will become the deceased couple’s children’s guardian(s), and will provide funds to that accrue to the guardian(s) to offset the expenses the guardian(s) encounter to provide for those children. The trust can also enable the trustee to disburse any remaining funds once the children reach certain ages or milestones. Among the options are to disperse all remaining funds at one point in time, or to disburse a portion of the funds at certain ages.
Most parents would probably not want their children to receive the entire sum of the assets of such a trust could enable to be distributed, upon a major life event such as graduation from a university or technical school. Testamentary trusts can provide for this, by directing the trustee to disburse, say, one-third of the remaining funds at age 21 or upon school graduation, then one-half of the then-remaining funds at some later age, such as 25 or 30, with the final disbursement occurring at a later age, such as 30 or 35. In this manner, if the child is a spendthrift in their young adulthood, they have a builtin second chance not to have squandered all of their inheritance.
A testamentary trust can also be a highly useful tool for a mid-career or late career physician, because the need to provide for the welfare of the couple’s children will persist, even as the physician ages, pays off their educational debts, and acquires a positive net worth. Many younger physicians who have had to utilize loans to pay for their educational expenses may not reach this point until age 40 or beyond, and others whose parents or other benefactors have offset their educational expenses may reach this point at an earlier age. However,
AGING WELL IN EMERGENCY MEDICINE INTEREST GROUP
>>
COMMON SENSE JULY/AUGUST 2023 28
"Thus, I believe that a testamentary trust is a crucial tool for any physician at any age, to enable their trustee to execute the physician’s financial wishes, beyond that provided in one’s will."
the physician or physician couple’s net worth may not have yet reached the value that the physician would hope to pass to their heirs until they reach their late 50s or early 60s. Thus, to continue to pay for term life insurance coverage is a reasonable consideration to enable proper estate planning.
An added wrinkle to mention here includes that to purchase term coverage, one must continue to be a good risk for the insurer. If one has acquired a chronic illness, and as one ages, term insurance can become prohibitively expensive. Furthermore, even if one ages in good health, term policy coverage premiums will naturally increase, and at an accelerating rate, because we all have an expiration date. Thus, for the physician to consider adding some other insurance product other than term insurance is a wise consideration, especially as one ages. A competent life insurance agent is part of a useful asset management strategy, because at some point in time, a physician may wish to assure insurability and lock in the ability to maintain life insurance coverage no matter what chronic illnesses may befall them. A mixed portfolio of term and whole life coverage can be a rational choice.
By competent life insurance agent, I am not specifying a life insurance agent who will try to use the fact that life insurance proceeds generally pass tax-free to one’s heirs as a hook to try to persuade the young physician to build a financial portfolio composed entirely or chiefly of life insurance cash values. Those large and impressive skyscrapers that most larger insurers have are the result of the large gap by which the company’s income exceeds
the company’s expenses. It is reasonable to purchase a mixture of whole life insurance (or a variant, which acquires cash value and insures future insurability) and term life insurance, with the plan that eventually, when the physician’s assets grow, the physician will stop funding the term policy, or will purchase a progressively smaller amount of term coverage over time.
Eventually, most physicians reach the happy point where their net worth can be sufficient to meet their perceived needs for the size of their estate, at which point they can stop purchasing term life insurance, and/or stop paying premiums on other life insurance tools that assure ongoing insurability and provide a cash value that grows with the number of years an insured maintains coverage.
At that point, their child or children may or may not have reached adulthood, and the physician’s perceived needs and wishes may have changed markedly from those of their earlier years. The need to periodically update one’s will and one’s trust agreement should be obvious.
The need to continue a testamentary trust may be less obvious. If one has remained married to their only partner for their entire life, there will probably be little reason to suspect the surviving spouse is likely to commit financial malfeasance. However, many physicians marry and divorce, and then re-marry. This can make the role of a testamentary trust crucial to the physician, who may wish to provide for their biological children and not the children of their second spouse. If the physician has had children with both spouses, the need for a clear document to enable execution of their wishes becomes even more obvious.
Thus, I believe that a testamentary trust is a crucial tool for any physician at any age, to enable their trustee to execute the physician’s financial wishes, beyond that provided in one’s will.
This article has only explored testamentary trusts. There exist numerous other types of trusts that some physicians may wish to execute. For example, a charitable trust can enable the funding of one’s philanthropic desires. However, such desires are typically one of the last things that early and mid-career physicians would consider, and thus they have not been covered here.
If one wishes to obtain a more comprehensive overview of trusts, then one is encouraged to consult directly with a trust officer of a reputable institution. The information provided above is not meant to be any form of official financial guidance, but it is intended to spur physicians into thinking about how they may wish to provide financially for their heirs, a goal shared by most high-net-worth individuals such as typical physicians eventually will become.
AGING WELL IN EMERGENCY MEDICINE INTEREST GROUP
Submit a Letter to the Editor Email your Letter to the Editor to: cseditor@aaem.org Scan the Code to Join the Aging Well in EM Interest Group COMMON SENSE JULY/AUGUST 2023 29
What stood out to you from this issue of Common Sense? Have a question, idea, or opinion? Edwin Leap II, MD FAAEM, editor of Common Sense, welcomes your comments and suggestions. Submit a letter to the editor and continue the conversation.
AAEM/RSA New Board
Leah Colucci, MD MS
It is that time of year where we welcome our new board! I will be staying on another year as your president. There were too many projects in the works that we were accomplishing, and I did not want to slow down our momentum. I am honored to serve this organization for another year and plan to be a part of AAEM for as long as I am a physician.
Before I introduce you to your new board, I would like to highlight what we have accomplished over the last year:
• We developed a URiM office hours for minority applicants and partnered with HBCUs. Every individual that sought help through our team was able to match this year.
• We revamped our mission, vision, and values statements. Our organization has a unique set of values that are driving us, and we wanted to highlight that we are the advocacy organization for emergency medicine.
• We developed our own unionization tool kit and then partnered with SAEM/RAMS and EMRA for panels and education at their respective conferences.
• We wrote a student loan letter to Joe Biden and the White House for specific requests and an explanation on why emergency medicine residents and physicians are unique in our struggles through the COVID-19 pandemic.
• We had a successful wellness fuel event where residencies from across the country shared what they do for wellness and fought to be the “most well” program.
• We hosted the Health Policy in Emergency Medicine course in Baton Rouge with our Louisiana lobbyists and learned how to get involved on a local level.
• We advocated to the FTC about ending non-competes and we increased education around AAEM’s mission and their progress in the lawsuit against Envision.
• We are creating a workforce toolkit with professional development to create curriculum that will educate on topics of importance for residents. These are topics like contract negotiations, working with NPPs, locums etc., that might not be in a traditional residency curriculum. Part of this toolkit is our locums webinar series with the AAEMLocums Group!
We have made amazing progress this year!
Without further ado, I am excited to be working with this team this year:
Vice President: Anantha Singarajah, DO
Secretary/Treasurer and Education Liaison: Matthew Carvey, MD FP-C


Publications Liaison: Robert Canning, MD

Membership & Awards and JEDI Liaison: Reba Gillis, MD
Wellness Liaison: Kasia Marciniec, DO

International Liaison: Taylor Smith, MD

Advocacy Liaison: Heath Spencer, DO

Medical Student Council Liaison: Mary Unanyan, DO

Medical Student Council Chair: Katy Wyszynski



Past President and YPS Liaison: Lauren Lamparter, MD
 AAEM/RSA PRESIDENT’S MESSAGE
AAEM/RSA PRESIDENT’S MESSAGE
COMMON SENSE JULY/AUGUST 2023 30
Introducing Your New AAEM/RSA Publications Chair
Mel Ebeling, MS3
Hello, AAEM! My name is Mel Ebeling, and I’m honored to introduce myself as the new Chair of the AAEM/RSA Publications and Social Medical Committee. In this brief letter, I intend to share with you more about who I am, my interests, and goals for the upcoming academic year. First, though, I want to thank our outgoing committee chair, Dr. Alessandra Della Porta, for nominating me for this position and wish to acknowledge her publication of several timely and important articles in Common Sense this past year.
Where to begin? Growing up in a small northern Alabama town, the “City of Southern Hospitality,” I am well-acquainted with tornadoes and scorching summers. Just when I thought I was going to get out of the South for college, I was accepted into the Early Medical School Acceptance Program at the University of Alabama at Birmingham. There, I earned my bachelor’s degree in neuroscience before matriculating into the Heersink School of Medicine, where I am now a third-year medical student. My passion for emergency medicine started in high school, where I had the opportunity to obtain my Emergency Medical Technician license from a local community college during my senior year. During college, I worked on an ambulance doing interfacility transfers for a short time before joining the volunteer staff of Fultondale Fire & Rescue, where I have been running 911 calls for the past six years. Through my affiliation with the fire service, I was able to capitalize on numerous training opportunities with the Department of Homeland Security which enabled me to become qualified as a Hazardous Materials Specialist.
Having these opportunities to travel across the country to receive practical training on incident response to chemical, biological, radiological,
nuclear, and explosive (CBRNE) and other mass casualty events shaped my professional and academic interests over the years. My current interests include counterterrorism/CBRNE medicine, event medicine, Emergency Medical Services, medical education (esp. simulation), and matters of diversity, equity, and inclusion in medicine. Outside of academics, I am a long-standing martial artist and consider myself a bit of an adrenaline junkie.
I am grateful to be a new voice for the AAEM/RSA and, through my role as Chair, look forward to utilizing my knowledge and interests to produce high-quality works on behalf of the organization over this next year. To further develop the voice of the humanities in emergency medicine, I also intend to develop a repository of narrative medicine resources for current and prospective writers. As the concurrent Vice Chair of the AAEM/RSA Medical Student Council, I hope to augment the student voice within the Publications and Social Media Committee as well. I encourage all AAEM and RSA members who want to develop their voice through publications and social media and who are interested in assisting with these goals to reach out to me directly so that we can continue to grow this essential element of AAEM/RSA. Again, I want to express my gratitude to Dr. Alessandra Della Porta and the AAEM/RSA for allowing me to step into this role, and I look forward to working with everyone this year!
Mel Ebeling Medical Student (MS3)

University of Alabama at Birmingham Heersink School of Medicine
Pronouns: they/them/theirs
Contact: mebeling@uab.edu

EDITOR’S MESSAGE
AAEM/RSA
"
COMMON SENSE JULY/AUGUST 2023 31
I encourage all AAEM and RSA members who want to develop their voice through publications and social media and who are interested in assisting with these goals to reach out to me directly so that we can continue to grow this essential element of AAEM/RSA."
Emergency Physicians Should Give Ketamine to Patients with Acute Suicidal Ideation
 Curtis Marino, DO PGY3
Curtis Marino, DO PGY3

Acute suicidal ideation (SI) represents about 1% of all adult emergency department (ED) visits in the U.S. and has increased over the past few decades, especially in the wake of the COVID19 pandemic.1 According to the CDC, ED visits have increased for suspected suicide attempts among adolescents and young adults since 2020.2 The ED is a frequently utilized health care resource for at risk mental health patients. Approximately 40% of patients who died by suicide had visited an ED within one year prior to death, according to retrospective studies in the UK.3,4 Outcomes could be improved if these patients received prompt treatment. Unfortunately, many community hospitals have limited mental health resources. Patients often endure long boarding times in the ED until they are assessed by a mental health worker, admitted to inpatient psychiatry, or transferred to an appropriate facility. On average, psychiatric patients are boarded in the ED for more than 11 hours and this increases to over 15 hours if a transfer is required.5
While waiting for care in the ED, these patients often experience mental distress while in solitude, and are rarely provided with anything to ameliorate their symptoms. Antidepressant medications, such as SSRIs and SNRIs, are most often used to manage symptoms linked to acute SI, but are ineffective in the acute setting.6 Antidepressants often require four to six weeks or longer to improve symptoms and many patients do not respond to the first trial of medication.7,8 The limited options to provide immediate relief can be burdensome for many emergency physicians when managing these patients, but maybe a familiar agent could be of benefit.
Ketamine, the Swiss army knife of ED medications, has increasingly garnered attention for its effectiveness in treating psychiatric disorders, including treatment-resistant depression, post-traumatic stress disorder, and suicidal ideation. Over the past decade, randomized control trials (RCTs) have shown ketamine’s efficacy in reduction of acute SI symptoms, but most of the research involving ketamine therapy for SI has been conducted in inpatient psychiatry settings. Dosing protocols ranged from 0.2 mg/kg to 0.5 mg/kg intravenously, but the most commonly utilized dose was 0.5 mg/kg in 100 mL normal saline infused over 40 minutes.11-16 A randomized control trial from 2017 demonstrated a statistically significant reduction in SI symptoms compared to midazolam.9 These effects were maintained for up to six weeks.9 Meta-analyses and systematic reviews demonstrated similar conclusions for the rapid reduction of SI symptoms after ketamine infusions.11-16 In one meta-analysis, after a
single-dose ketamine infusion, a significant reduction in SI symptoms was observed for up to seven days.11 Although most existing literature has emerged from the inpatient psychiatry setting, more recent studies suggest the evidence supports its use in the ED as well.
Over the past decade, there has been a growing body of research to investigate the efficacy of ketamine for acute SI in the ED setting. Kashani et al, a single-arm study with 49 enrolled patients reported a significant reduction of SI symptoms at 40 minutes post-infusion.17 However, the 0.2 mg/kg ketamine dose falls in the lower range of doses utilized in the
inpatient psychiatry studies. Burger et al, an RCT from 2016 (n=10), demonstrated a reduction of symptoms in the ketamine group at 240 minutes post-infusion that was comparable to the control group after receiving inpatient psychiatric treatment.18 Another RCT (n=16), Domany et al, used 0.5 mg/kg ketamine and reported a statistically significant reduction in symptoms in the ketamine group compared to placebo.19 There were two studies published in 2022. Gaither et al, a single-arm study that administered 0.5 mg/kg to patients in the ED waiting for admission to inpatient psychiatry and demonstrated significant reduction in symptoms at two hours post-infusion.20 The other, an RCT by Domany and McCullumsmith, randomized patients (n=30) to intranasal ketamine or placebo and resulted in SI remission in 80% of the ketamine group vs 33% of the control group.21 None of the studies reported serious adverse
OPINION
>> COMMON SENSE JULY/AUGUST 2023 32
"Ketamine, the Swiss army knife of ED medications, has increasingly garnered attention for its effectiveness in treating psychiatric disorders, including treatmentresistant depression, posttraumatic stress disorder, and suicidal ideation."
events. The degree of efficacy may be dose dependent, and larger RCTs with broader inclusion criteria would be beneficial to determine optimal dosing, infusion rate, and potential for ketamine to serve as a bridge to conventional therapy. Despite limited data from the ED, it largely trends with the inpatient psychiatry evidence: ketamine is an effective tool in providing rapid relief for these otherwise suffering patients.
Ketamine at a subanesthetic intravenous dose is well tolerated with minimal rates of serious adverse effects.22 If the evidence suggests that the benefit outweighs the risk, and there are no other feasible treatment options, why are we not regularly utilizing this tool? Considering the potentially severe mental distress these patients experience while waiting in the ED, there is a strong argument for emergency physicians to offer ketamine, especially in the context that there are no other effective immediate-acting medications except for one that is ubiquitously available.
Some may critique the small sample sizes of ED-based studies, but efficacy in symptom reduction has been sufficiently demonstrated in larger inpatient studies. There may also be criticism of the short-lived symptomatic relief, but from the perspective of the common use of analgesics, it makes sense. It would be unethical to withhold pain medication for a kidney stone or severe trauma using the rationale that it is unnecessary because the relief is temporary—that is expected.
While lacking evidence for reduction of SI in the long-term, the transient symptomatic reduction is a reasonable goal in the ED, in the same way morphine provides relief for severe physiologic pain. Insufficient evidence for reduction in long-term suicidality should not prevent patients from receiving relief in the acute setting. Hesitancy to make unorthodox choices should not override evidence in medical decision making, and there is adequate evidence to suggest benefit to the patient with minimal to no reported adverse effects. Emergency physicians are skilled in managing ketamine safely, especially at subanesthetic doses, and are in an ideal position to provide relief as the first physicians to assess these patients. I urge my colleagues to consider incorporating ketamine into the management of patients with acute SI.
References
1. Pamela, Owens, et al. “Statistical Brief #220Emergency Department Visits Related to Suicidal Ideation, 2006–2013.” National Center for Biotechnology Information, Healthcare Cost and Utilization Project, Jan. 2017, https://www.ncbi.nlm.nih.gov/books/NBK442036/.
2. Yard, Ellen, et al. “Emergency Department Visits for Suspected Suicide Attempts among Persons Aged 12–25 Years before and during the COVID-19 Pandemic - United States, January 2019–May 2021.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 17 June 2021, https://www.cdc.gov/mmwr/volumes/70/wr/ mm7024e1.htm.
3. Da Cruz D, Pearson A, Saini P, Miles C, While D, Swinson N, Williams A, Shaw J, Appleby L, Kapur N. Emergency department contact prior to suicide in mental health patients. Emerg Med J. 2011 Jun;28(6):467-71. doi: 10.1136/emj.2009.081869. Epub 2010 Jul 26. PMID: 20660941.
4. Gairin I, House A, Owens D. Attendance at the accident and emergency department in the year before suicide: retrospective study. Br J Psychiatry 2003 Jul;183:28-33. doi: 10.1192/bjp.183.1.28. PMID: 12835240.
5. Weiss AP, Chang G, Rauch SL, Smallwood JA, Schechter M, Kosowsky J, Hazen E, Haimovici F, Gitlin DF, Finn CT, Orav EJ. Patient- and practicerelated determinants of emergency department length of stay for patients with psychiatric illness. Ann Emerg Med. 2012 Aug;60(2):162-71.e5. doi: 10.1016/j.annemergmed.2012.01.037. Epub 2012 May 2. PMID: 22555337.
6. Dick C. Kuo, Mina Tran, Asim A. Shah, Anu Matorin, Depression and the Suicidal Patient, Emergency Medicine Clinics of North America, Volume 33, Issue 4, 2015, Pages 765-778, ISSN 0733-8627, ISBN 9780323416849, https://doi.org/10.1016/j.emc.2015.07.005.
7. Machado-Vieira R, Baumann J, Wheeler-Castillo C, Latov D, Henter ID, Salvadore G, Zarate CA. The Timing of Antidepressant Effects: A Comparison of Diverse Pharmacological and Somatic Treatments. Pharmaceuticals (Basel). 2010 Jan 6;3(1):19-41. doi: 10.3390/ ph3010019. PMID: 27713241; PMCID: PMC3991019.
8. Michael Browning, Jonathan Kingslake, Colin T. Dourish, Guy M. Goodwin, Catherine J Harmer, Gerard R. Dawson, Predicting treatment response to antidepressant medication using early changes in emotional processing, European Neuropsychopharmacology, Volume 29, Issue 1, 2019, Pages 66-75, ISSN 0924-977X, https://doi.org/10.1016/j. euroneuro.2018.11.1102.
9. Grunebaum, Michael F., et al. “Ketamine for Rapid Reduction of Suicidal Thoughts in Major Depression: A Midazolam-Controlled Randomized Clinical Trial.” American Journal of Psychiatry, vol. 175, no. 4, 2018, pp. 327–335., https://doi.org/10.1176/appi.ajp.2017.17060647.
10. Fan W, Yang H, Sun Y, Zhang J, Li G, Zheng Y, Liu Y. Ketamine rapidly relieves acute suicidal ideation in cancer patients: a randomized controlled clinical trial. Oncotarget. 2017 Jan 10;8(2):2356-2360. doi: 10.18632/oncotarget.13743. PMID: 27926528; PMCID: PMC5356805.
11. Wilkinson ST, Ballard ED, Bloch MH, Mathew SJ, Murrough JW, Feder A, Sos P, Wang G, Zarate CA Jr, Sanacora G. The Effect of a Single Dose of Intravenous Ketamine on Suicidal Ideation: A Systematic Review and Individual Participant Data Meta-Analysis. Am J Psychiatry. 2018 Feb 1;175(2):150-158. doi: 10.1176/appi.ajp.2017.17040472. Epub 2017 Oct 3. PMID: 28969441; PMCID: PMC5794524.
12. Siegel AN, Di Vincenzo JD, Brietzke E, Gill H, Rodrigues NB, Lui LMW, Teopiz KM, Ng J, Ho R, McIntyre RS, Rosenblat JD. Antisuicidal and antidepressant effects of ketamine and esketamine in patients with baseline suicidality: A systematic review. J Psychiatr Res. 2021 May;137:426-436. doi: 10.1016/j.jpsychires.2021.03.009. Epub 2021 Mar 16. PMID: 33774537.
13. Kritzer MD, Mischel NA, Young JR, Lai CS, Masand PS, Szabo ST, Mathew SJ. Ketamine for treatment of mood disorders and suicidality: A narrative review of recent progress. Ann Clin Psychiatry. 2022 Feb;34(1):33-43. doi: 10.12788/acp.0048. PMID: 35166663; PMCID: PMC9044467.
14. Dadiomov, David, and Kelly Lee. “The Effects of Ketamine on Suicidality across Various Formulations and Study Settings.” Mental Health Clinician, vol. 9, no. 1, 2019, pp. 48–60., https://doi.org/10.9740/mhc.2019.01.048.
15. Jollant F, Colle R, Nguyen TML, Corruble E, Gardier AM, Walter M, Abbar M, Wagner G. Ketamine and esketamine in suicidal thoughts and behaviors: a systematic review. Ther Adv Psychopharmacol. 2023 Feb 7;13:20451253231151327. doi: 10.1177/20451253231151327. PMID: 36776623; PMCID: PMC9912570.
16. Hochschild A, Grunebaum MF, Mann JJ. The rapid anti-suicidal ideation effect of ketamine: A systematic review. Prev Med. 2021 Nov;152(Pt 1):106524. doi: 10.1016/j.ypmed.2021.106524. Epub 2021 Sep 16. PMID: 34538369.
Countinued on page 35 >>
OPINION
COMMON SENSE JULY/AUGUST 2023 33
Beyond the Curriculum: Exploring Moral Injury in Emergency Medicine from the Medical Student Lens

 Will Zhu, MS4* and Aliza Siddiqui, MS4 †
Will Zhu, MS4* and Aliza Siddiqui, MS4 †
hether it be caring for those young and new to this world or those who are in their twilight years, medicine has always been a profession immersed in the full spectrum of the human experience. With the conclusion of the 2022-2023 Match cycle, a new class of almost 30,000 graduating physicians will join the health care workforce of the U.S.1 These new doctors will be with patients on their worst days and also become integral parts of communities and safety nets. At the same time, they will be facing the threat of burnout and moral injury which endangers both them and patients. Next year we will be following their footsteps as two fourth-year medical students applying to emergency medicine (EM) in this upcoming cycle. We have a unique chance to serve our community and explore fundamental issues within medicine.
Physicians are on the frontlines of responding to public health crises and pandemics. Policy failures to ensure our country’s health and safety will often be left to the health care system to clean up. Declining life expectancy,2 shrinking access to primary care,3 and rising drug4 and insurance prices5 create an increasingly adverse health care work environment. This all contributes to burnout and moral injury. This is especially true in EM, which according to the 2023 Match data has had a record amount of unmatched spots.6
As defined by the Department of Veteran Affairs, moral injury occurs when one “witnesses or fails to prevent an act that disobeys their own moral values or personal principles.”7 In other words, it feels like a betrayal on the part of an institution and oneself when continuously forced to perform actions that contradict our reasons for entering medicine and our core values. Although initially described in combat veterans, moral injury is also commonly observed among health care workers.8 Repeated instances of moral injury are distressing and contribute to burnout. Ultimately, burnout can result in early retirement, worsened patient care outcomes, and increased rates of depression.9
Our medical school experience in some ways mirror the above. The start of our medical education was unconventional in almost every way. We faced the challenge of learning medicine with resource constraints.
WInstead of traditional cadaver labs, we relied on iPad apps and recorded dissections. We even had to learn to conduct physical exams on ourselves through Zoom. Our faculty and educators in addition had the Herculean task of teaching and building connections with students who had never set foot into their lecture halls or office hours. Although many of the typical challenges of medical school persisted, we missed the support that previous classes had before the pandemic. As we start our fourth year of medical school, many students like us are applying to EM because this was the specialty that best aligned with our motivations to enter medicine, and it is here where we see ourselves finding our community and support. However, burnout and moral injury are increasingly prevalent within emergency medicine, with reports indicating that 65% of EM physicians experience burnout, the highest rates among all specialties.10
Nevertheless, there is something uniquely special about the ability to care for the populations that EM physicians serve. The U.S. medical system has failed many patients, leaving them without insurance coverage for life-saving measures. The emergency department becomes the primary refuge for these patients; the only place they can access the care they need. As a result, waiting rooms become crowded, and the demand for care exceeds the available beds. EM physicians are left to care for these populations with nowhere else to turn. At the same time this allows us to advocate for our patient from a position of first-hand knowledge and experience. This is an opportunity to show the public at large the excellence of our training and depth of our kindness.
Health care has increasingly become corporatized and profit-driven over the years.11 This is seen with the rise of corporate management groups and large acquisitions such as Amazon buying One Medical.12 Private practices are an increasingly rare sight, and prior authorizations are becoming routine. In the face of this, the emergency department is still a place where patients are treated according to each one’s greatest need. This is made possible in part by laws like EMTALA which limit the insurance involvement at the point of care, and it is one of the few medical specialties where we do not choose the patients we treat.13 EM remains strongly connected to our communities and has the privilege to address some of the most salient health issues in society, whether it be the opiate epidemic or gun violence.
WELLNESS COMMITTEE
>> COMMON SENSE JULY/AUGUST 2023 34
"[Moral injury] feels like a betrayal on the part of an institution and oneself when continuously forced to perform actions that contradict our reasons for entering medicine and our core values."
The emergency department was where we first started feeling at home in medicine and where we were able to best envision ourselves as physicians. The diversity of pathologies and patients present as well as the chance to do procedures make EM a versatile field. While we are thrilled to join the EM workforce and provide much-needed care within today’s health care system, there is also concern regarding the future of the specialty and our working conditions. We must strive for increased protection of the health and well-being of EM physicians to combat moral injury. To ensure the future resilience of the specialty, we must work to enhance the well-being of EM physicians. Only by prioritizing the whole person, which includes our mental health, can we sustain a community that will weather the challenges we are facing currently and those yet to come.
References
*MS4 at University of Maryland School of Medicine, @WiLLyZ109
†MS4 at Chicago Medical School at Rosalind Franklin University, @alizas_14
1. Total number of medical school graduates. KFF. (2022, May 4). https://www.kff.org/other/state-indicator/total-medical-schoolgraduates/?currentTimeframe=0
2. Centers for Disease Control and Prevention. (2022, August 31). Life expectancy in the U.S. dropped for the second year in a row in 2021 Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/ pressroom/nchs_press_releases/2022/20220831.htm#:~:text=Life%20 expectancy%20at%20birth%20in,its%20lowest%20level%20since%20 1996.
3. IHS Markit Ltd. (2021). The complexities of physician supply and demand: Projections ... - AAMC. Association of American Medical Colleges. https:// www.aamc.org/media/54681/download?attachment2034
4. Prescription drugs: Spending, use, and prices. Congressional Budget Office. (2022, January). https://www.cbo.gov/publication/57772
5. Telesford, I., Telesford, I., Rakshit, S., McGough, M., Twitter, E. W., &
OPINION
Countinued from page 33 >>
17. Kashani P, Yousefian S, Amini A, Heidari K, Younesian S, Hatamabadi HR. The Effect of Intravenous Ketamine in Suicidal Ideation of Emergency Department Patients. Emerg (Tehran). 2014 Winter;2(1):36-9. PMID: 26495340; PMCID: PMC4614623.
18. Burger, John, et al. “A Double-Blinded, Randomized, Placebo-Controlled Sub-Dissociative Dose Ketamine Pilot Study in the Treatment of Acute Depression and Suicidality in a Military Emergency Department Setting.” Military Medicine, vol. 181, no. 10, 2016, pp. 1195–1199., https://doi. org/10.7205/milmed-d-15-00431.
19. Domany Y, Shelton RC, McCullumsmith CB. Ketamine for acute suicidal ideation. An emergency department intervention: A randomized, doubleblind, placebo-controlled, proof-of-concept trial. Depress Anxiety. 2020 Mar;37(3):224-233. doi: 10.1002/da.22975. Epub 2019 Nov 16. PMID: 31733088.

Twitter, K. A. (2023, February 7). How has U.S. spending on healthcare changed over time?. Peterson-KFF Health System Tracker. https:// www.healthsystemtracker.org/chart-collection/u-s-spending-healthcarechanged-time/#Total%20national%20health%20expenditures,%20US%20 $%20Billions,%201970-2021
6. Christian Rose, A. I. L. (2023, March 17). Will there be any emergency doctors to see you in the future?. STAT. https://www.statnews. com/2023/03/20/emergency-medicine-residency-positions-unfilled-thematch/
7. Moral injury. DAV. (2022, December 7). https://www.dav.org/get-help-now/ veteran-topics-resources/moral-injury/
8. Avery, S. (2022, April 5). Indications of moral injury similar between combat veterans and covid-19 health care workers. Duke Health. https:// corporate.dukehealth.org/news/indications-moral-injury-similar-betweencombat-veterans-and-covid-19-health-care-workers
9. Stehman, C. R., Testo, Z., Gershaw, R. S., & Kellogg, A. R. (2019). Burnout, Drop Out, Suicide: Physician Loss in Emergency Medicine, Part I. The western journal of emergency medicine, 20(3), 485–494. https:// doi.org/10.5811/westjem.2019.4.40970
10. Carbajal, E. (2023, February 1). 29 physician specialties ranked by 2022 burnout rates. Becker’s Hospital Review. https://www. beckershospitalreview.com/hospital-physician-relationships/29-physicianspecialties-ranked-by-2022-burnout-rates.html
11. Abelson, R. (2023, May 8). Corporate Giants buy up primary care practices at Rapid Pace. The New York Times. https://www.nytimes. com/2023/05/08/health/primary-care-doctors-consolidation.html
12. One medical joins Amazon to make it easier for people to get and stay healthier. One Medical. (2023, February 22). https://www.onemedical. com/mediacenter/one-medical-joins-amazon/
13. Overview of the Emergency Medical Treatment and Active Labor Act (EMTALA) and Emergency Abortion Services. Congressional Research Service. (2023, March 21). https://crsreports.congress.gov/product/pdf/IF/ IF12355
20. Gaither, Rachel, et al. “A Feasibility Study of Low‐Dose Ketamine for Acute Management of Suicidal Ideation.” Journal of the American College of Emergency Physicians Open, vol. 3, no. 4, 2022, https://doi. org/10.1002/emp2.12790.
21. Domany, Yoav, and Cheryl B. McCullumsmith. “Single, Fixed-Dose Intranasal Ketamine for Alleviation of Acute Suicidal Ideation. an Emergency Department, Trans-Diagnostic Approach: A Randomized, Double-Blind, Placebo-Controlled, Proof-of-Concept Trial.” Archives of Suicide Research, vol. 26, no. 3, 2021, pp. 1250–1265., https://doi.org/10. 1080/13811118.2021.1878078.
22. Rodrigues NB, McIntyre RS, Lipsitz O, Lee Y, Cha DS, Nasri F, Gill H, Lui LMW, Subramaniapillai M, Kratiuk K, Lin K, Ho R, Mansur RB, Rosenblat JD. Safety and tolerability of IV ketamine in adults with major depressive or bipolar disorder: results from the Canadian rapid treatment center of excellence. Expert Opin Drug Saf. 2020 Aug;19(8):1031-1040. doi: 10.1080/14740338.2020.1776699. Epub 2020 Jun 15. Erratum in: Expert Opin Drug Saf. 2020 Jul 7;:1. PMID: 32539491.
WELLNESS COMMITTEE
"Only by prioritizing the whole person, which includes our mental health, can we sustain a community that will weather the challenges we are facing currently and those yet to come."
COMMON SENSE JULY/AUGUST 2023 35
Justice, Equity, Diversity, and Inclusion Section’s 2023 Medical Student Scholarship Awardee Highlight




 Jordan Vaughn, MD and Alyssa Eily, MD
Jordan Vaughn, MD and Alyssa Eily, MD
AAEM’s JEDI Section (Justice, Equity, Diversity, and Inclusion) is excited to announce the winners of our 2023 Medical Student Scholarship. JEDI was born out of a need for increasing support for those URiM including, but not limited to, BIPOC and LGBTQ EM physicians. Perhaps no specialty treats such a broad range of patients spanning across cultures, race, ethnicity, gender, and sexual identity as emergency medicine. Through JEDI, we are creating a pathway to not just diversify EM but also help medical students and residents develop into future leaders to champion inclusion. We had a competitive applicant pool this year with stellar applicants. This year, we had the honor of awarding five URiM medical students with $500 to help offset the often prohibitive cost of residency applications, interviews, etc. Each of these students has exemplified true leadership, compassion, and commitment to our core mission. It is our pleasure to highlight our 2023 JEDI Medical Student Scholarship Awardees.
Student Doctor Mahlaqa Butt
Hometown: Brooklyn, NY
Plans for next year: Starting EM intern year at Maimonides Med
Interest(s) within EM: Administration, pain management, peds EM
What does JEDI in emergency medicine mean to you: JEDI in EM allows individuals like myself to become a part of this amazing specialty that can advocate for immigrant patient populations.
Student Doctor Shawn Gibson
Hometown: Queens, NY
Plans for next year: Starting EM residency at SUNY Downstate/Kings County in Brooklyn, NY
Interest(s) within EM: Social EM, youth violence prevention, mentoring, medical education
What does JEDI in emergency medicine mean to you: JEDI in emergency medicine means providing an opportunity for students who don’t know their true potential to make impactful change. For many of us underrepresented minority students in medicine, a lack of seeing someone who looks like us and/or someone we can relate to culturally, may limit us from displaying our best selves. I am honored to be a recipient of this year’s JEDI’s Medical Student Scholarship Award and look forward to gaining mentorship and giving it back in the future years to ensure all students are comfortable and confident in embracing their best selves to serve all populations.
Student Doctor Deidre V Gubac
Hometown: Jackson, MS
Plans for next year: Resident at Alameda-Highlands Hospital in Oakland, CA
Interest(s) within EM: DEI and social EM with an emphasis on health equity
What does JEDI in emergency medicine mean to you: Unfortunately, not everyone in this country can afford specialty care, and many don’t even have a primary care provider, but emergency medicine has the unique opportunity to touch the lives of all generations, all cultures, and all walks of life. With that being said, it is our responsibility to provide equitable care acknowledging that it may look different for patients at different levels of social vulnerability. Emergency medicine is full of innovative thinkers and we must use all of our uniqueness to achieve the goal of dismantling these long-standing barriers in medicine and beyond.
Student Doctor Abigail Hecht
Hometown: Centerville, OH
Plans for next year: Emergency medicine residency at University of Washington
Interest(s) within EM: Social emergency medicine, climate change & health, ultrasound, medical education
What does JEDI in emergency medicine mean to you: Everything! Emergency medicine is a specialty defined by serving diverse populations—thus, prioritizing justice, equity, diversity, and inclusion in trainees and the workforce is vital to improving care for our patients. As a member of the LGBTQ+ community, I hope to contribute my unique perspective and experiences to my training program while also learning from my patients and colleagues.
Student Doctor Adetoriola Odetunde
Hometown: Toronto, Canada
Plans for next year: Starting residency at the University of Chicago
Interests within EM : Social EM, critical care, and administration
What does JEDI in emergency medicine mean to you? JEDI in emergency medicine means creating space for our patients and coworkers to be seen, heard, and cared for holistically. It means addressing systemic and individual issues affecting physical and mental health to create safe, equitable, and inclusive communities.
As we know diversity in our workforce is imperative to provide high quality care to our patients. We look forward to the next generation of emergency medicine physicians leading JEDI efforts and all that they will accomplish.
JUSTICE, EQUITY, DIVERSITY, AND INCLUSION SECTION
COMMON SENSE JULY/AUGUST 2023 36
Introduction of the AAEM Locum Tenens Section (LT-AAEM)
Pamela A. Ross, MD FAAEM FACEP FAAP
tenens staffing company that was transparent and willing to stand in full representation of my best interests as an emergency physician. The transition from academics to locum tenens left me with only one regret—that I hadn’t started locum tenens work several years prior.
the formation of the LT-AAEM Section. The AAEM Locum Tenens Section is the newest section of the Academy and we invite you to join for cutting edge resources and education for all things locum tenens related.
After 17 years of a dedicated academic career, I launched a second career as a locum tenens physician and took up traveling the world to learn about health and healing in other cultures. The path of my academic career included completion of a fellowship in Integrative Medicine at the University of Arizona Center for Integrative Medicine. So right along with my locum tenens practice, I launched a robust international travel agenda to study health and healing in other cultures. I started in Peru under the teachings of an Andean Shaman traditional healer and then on to Indonesia under the teachings of Balains, the traditional healers of Indonesia who work with divine energy to treat physical and mental illnesses. I launched a very limited concierge integrative medicine practice on a part-time basis in addition to my work in emergency medicine and pediatric emergency medicine. Locum tenens practice allowed me to shape my life and my practice of medicine to my highest personal ideal.
I have met many physicians along the way who have started both part-time and full-time locum tenens practices. I find that our reasons strike resonant chords of autonomy, scheduling control, more time with family, more shielding from burn out, etc. It also kept me connected to the space I value most as a physician—the sacred space of me and my patient together—engaging their stories, diagnosing, and treating their real and perceived life-threatening emergency conditions. Fortunately, I started with a locum
In the swell of a rapidly changing environment of the practice of emergency medicine, locum tenens has become an increasingly appealing option for physicians looking to transition away from practices that leave them feeling unfulfilled and questioning their decisions to practice emergency medicine altogether. The American Academy of Emergency Medicine strongly supports fair working practices for emergency physicians and recognizes the existence of many different emergency department business models. There are five pillars of excellence that AAEM believes are imperative for all emergency physicians:
• Partnership, political equity, and transparency
• Financial fairness and transparency
• Due process and post-employment fairness
• Commitment to the American Academy of Emergency Medicine
• Commitment to patients
AAEM formed the AAEM Locums Group with a mission to connect emergency physicians with reputable staffing companies who carry the ideals of workplace fairness for emergency physicians as well as create a pipeline of coverage options for private democratic groups who were seeking temporary solutions for covering temporary holes in the group practice schedule. The business model was subsequently revised to include the dissolution of the AAEM-LG and
Our Purpose
The AAEM Locum Tenens Section empowers emergency physicians to regain their professional and fiscal autonomy through the incorporation of independent contracting. We believe that educated, confident, and business savvy emergency physicians are vital to a healthy market. LT-AAEM feels that empowered physicians will in turn have greater ability to advocate for high quality, safe provision of care in healthy workplace environments.
Our Mission
The AAEM Locum Tenens Section was formed to address the unique needs of emergency physicians engaged or considering locum tenens work. The LT-AAEM will accomplish this through two main pillars: advocacy and education. Under the scope of education, the section will develop educational resources and tools. Under the scope of advocacy, the section will facilitate mentorship, network, and work/contract opportunities. As a section of the Academy, activities of the section will be in accordance with the standards established by the Academy. The purpose and mission statement of the Academy also extend to the Locum Tenens Section of AAEM.
If you have any desire to start a locum tenens practice, obtain locum tenens work, or simply enhance the locum tenens work you are already doing—this new section is for you.
AAEM LOCUM TENENS SECTION
COMMON SENSE JULY/AUGUST 2023 37
Colchicine in Coronary Artery Disease
Authors: Wesley Chan, MD, Christianna Sim, MD MPH, Christopher Kiang, MD, and Victoria Zaccone, MD
Editors: Donald Doukas, MD and Kami M. Hu, MD FAAEM
Introduction
The cornerstone of coronary artery disease (CAD) management includes slowing the progression of atherosclerosis. An inflammatory response plays a role in the initiation, progression, and thrombotic complications of atherosclerosis, leading to continued interest in the potential role of anti-inflammatory drugs in CAD management.1 Most commonly used in acute gout and acute pericarditis, colchicine is an easily accessible, inexpensive anti-inflammatory medication that works by inhibiting tubulin polymerization and hindering leukocyte response.2 Its proven efficacy as an anti-inflammatory agent has led to continued investigation into its potential role in the treatment of CAD.
Clinical Question: Does low-dose colchicine improve cardiovascular outcomes in patients with coronary artery disease?
Nidorf SM, Eikelboom JW, Budgeon CA, Thompson PL. Low-dose colchicine for secondary prevention of cardiovascular disease. Journal of the American College of Cardiology. 2013;61(4):404-410. doi:10.1016/j. jacc.2012.10.027 9 - LoDoCo
The potential cardioprotective effects of colchicine were first noted during a retrospective analysis of colchicine’s use for gout.3 The Low-Dose Colchicine (LoDoCo) trial investigators hypothesized that targeting the inflammatory pathway with colchicine, in addition to standard medical management, could modulate disease progression and improve outcomes in patients with stable coronary disease. They conducted a prospective, randomized, observer-blinded endpoint (PROBE) trial at a single center in Western Australia.
They enrolled 532 adults ages 35 to 85 years old with angiography-proven CAD that had been clinically stable for at least six years. Adults who had prior coronary artery bypass grafting (CABG) were included if surgery had taken place at least 10 years prior to enrollment or if they had proven graft failure or stenting. The treatment group (n=282) was given colchicine 0.5 milligrams per day, while the control group (n=250) received standard therapy only. Participants were followed for a minimum of two years. The primary composite outcome included acute coronary syndrome (ACS) defined as acute myocardial infarction or unstable angina, out-of-hospital cardiac arrest (OHCA), and non-cardioembolic ischemic stroke. Secondary outcomes were the individual components of the primary outcome and components of ACS unrelated to stent disease.
The investigators found that the composite outcome occurred at a significantly lower frequency in the treatment group (5.3%) than in the control group (16%), (Hazard Ratio [HR] 0.33; 95% Confidence Interval [CI] 0.18-0.59, p<0.0001). This reduction was driven primarily by the
decreased frequency of ACS, particularly non-stent-related ACS. There was no outcome benefit observed for OHCA or non-cardioembolic stroke. The reduction in the composite outcome varied across certain cohorts in subgroup analysis, with significant reduction, for example, in the composite outcomes for adults without prior CABG compared to adults with prior CABG.
The results suggest that low-dose colchicine may reduce cardiovascular events in patients with stable CAD. However, given that the reduction in cardiovascular events was driven by the decreased frequency of ACS and that there was no outcome benefit for the other two components of the composite outcome, it may only be beneficial in preventing ACS. The results also suggest that the underlying mechanism of this benefit may only be observed in de novo lesions and not stent-related lesions. Given the small sample size, single-center design, and lack of a placebo arm; it should only be considered as hypothesis-generating. Validation studies to confirm the benefit of colchicine need to be performed and further investigations into which subsets of patients may benefit the most should be conducted.
Nidorf SM, Fiolet ATL, Mosterd A, et al. Colchicine in patients with chronic coronary disease. New England Journal of Medicine. 2020;383(19):18381847. doi:10.1056/nejmoa2021372 - LoDoCo 2
In a follow-up to LoDoCo, LoDoCo2 investigated the effects of low-dose colchicine in patients with chronic CAD. It was a double-blind, event-driven, randomized controlled trial comparing colchicine 0.5 mg daily to placebo. Patients were enrolled if they had at least six months of clinically stable CAD evidenced by invasive coronary angiography, computed tomography angiography, or a coronary artery calcium score of at least 400 (Agatston method). Exclusion criteria included moderate to severe renal impairment, severe heart failure, severe valvular heart disease, and known side effects from colchicine. A total of 5,522 patients (2762 intervention, 2760 placebo) aged 35 to 82 years old were enrolled. The treatment and placebo arms were well-matched, and the participants’ chronic CAD was well-treated. The median follow-up time was 28.6 months. The primary composite endpoint included cardiovascular death, spontaneous (non-procedural) myocardial infarction, ischemic stroke, or ischemia-driven coronary revascularization. The secondary composite endpoint included cardiovascular death, spontaneous myocardial infarction, or ischemic stroke.
The investigators found that compared to the placebo group, the colchicine group had a 31% relative risk reduction in primary endpoint events (HR 0.67; 95% CI 0.57-0.83), translating to a composite endpoint
>>
AAEM/RSA RESIDENT JOURNAL REVIEW
COMMON SENSE JULY/AUGUST 2023 38
incidence rate of 2.5 events per 100 person-years in the colchicine group compared to 3.6 events per 100 person-years in the placebo group. They also found that compared to the placebo group, the colchicine group had a 2.8 percent relative risk reduction in secondary endpoint events (HR 0.72; 95% CI 0.57-0.92), or an incidence rate of 1.5 events per 100 person-years in the colchicine group compared to 2.1 events per 100 person-years in the placebo group. There was an additional slight, non-significant increase in non-cardiovascular deaths among patients who received colchicine compared to those who received placebo with incidence rates of 0.7 per 100 person-years and 0.5 events per 100 person-years (HR 1.51; 95% CI 0.99-2.31).
This was a well-designed, well-powered clinical trial that was also placebo-driven, unlike the first LoDoCo trial. This trial presents convincing evidence supporting the use of colchicine in chronic CAD for patients who are already receiving standard-of-care treatment for chronic coronary disease. It is important to note that patients with moderate-to-severe renal impairment, severe heart failure, or severe valvular disease were not eligible for this study. The authors also acknowledge that the percentage of women included in the study was much lower than the percentage of women with chronic CAD in the general population. Lastly, the tolerability of colchicine was a major barrier to the completion of colchicine during the trial and continuation of colchicine after the trial, limiting its potential efficacy in chronic CAD.
Tardif J-C, Kouz S, Waters DD, et al. Efficacy and safety of low-dose colchicine after myocardial infarction. New England Journal of Medicine. 2019;381(26):2497-2505. doi:10.1056/
nejmoa1912388 - COLCOT
While the results of LoDoCo suggested that colchicine may reduce cardiovascular events in patients with stable CAD, it did not account for the acute inflammatory response in patients with ACS. The investigators of the Colchicine Cardiovascular Outcomes Trial (COLCOT) conducted a randomized, controlled trial to explore the cardiovascular outcomes and safety profile of colchicine 0.5 mg daily versus placebo in patients who have recently had a myocardial infarction (MI).
The study enrolled 4745 patients who had an MI within 30 days as well as individuals who had completed planned percutaneous revascularization procedures. Patients with severe heart failure, left ventricular ejection fraction less than 35%, stroke in the last three months, type two MIs (demand ischemia), CABG recipients, history of cancer in the last three years, chronic diarrhea or inflammatory bowel disease, neuromuscular disease, significant hematologic abnormalities, severe renal or hepatic disease, drug or alcohol abuse, or planned long-term systemic glucocorticoid therapy were excluded. The primary composite endpoint was death from cardiovascular causes, resuscitated cardiac arrest, MI, stroke, or urgent hospitalizations related to angina leading to coronary revascularization. The secondary endpoints consisted of the components of the primary composite endpoint and total mortality in time-to-event analyses. Coronary revascularization, hospitalization for heart failure, atrial fibrillation, deep venous thrombosis or pulmonary embolus, change
in C-reactive protein (CRP) over six months, and change in white blood cell counts over 12 months were prespecified as exploratory endpoints.
There were 2366 patients in the intervention arm and 2379 in the control arm. Participants were followed for a mean of 22.6 months. The mean age of participants was 60.6 years old, and 19.2 percent were women. The primary endpoint was reached in 5.5 percent of patients in the colchicine group, compared with 7.1 percent of patients in the placebo group (HR 0.77; 95% CI 0.61 to 0.96; p=0.02). The hazard ratios for the components of the composite endpoint were 0.84 (95% CI 0.46 to 1.52) for death from cardiovascular causes, 0.83 (95% CI 0.25 to 2.73) for resuscitated cardiac arrest, 0.91 (95% CI 0.68 to 1.21) for myocardial infarction, 0.26 (95% CI 0.10 to 0.70) for stroke, and 0.50 (95% CI 0.31 to 0.81) for urgent hospitalization for angina leading to coronary revascularization. They also found that adverse events related to the active drug or placebo were 16% in the colchicine group and 15.8% in the placebo group. Nausea was reported in 1.8% of patients in the colchicine group and 1% of patients in the placebo group (p=0.03). Pneumonia was considered a significant clinical event and was reported as a serious adverse event in 0.9% of patients in the colchicine group compared to 0.4% of patients in the placebo group (p=0.03), raising concern that this could be due to impaired immune response in the colchicine group. Notably, the incidence of septic shock was not increased in the colchicine group, and there was also no serious event of myopathy despite the use of statins in 99% of patients. Diarrhea was reported in 9.7% of patients in the colchicine group, compared with 8.9% of patients in the placebo group (p=0.35). Out of the 207 participants in which inflammatory marker changes were evaluated, there were nonstatistically significant trends towards decreased CRP and white blood cells associated with colchicine use.
Overall, the results suggest that in patients with recent MI, low-dose colchicine led to a statistically significantly lower risk of cardiovascular events when compared to placebo, although with a borderline confidence interval. The investigators did find that colchicine was associated with a reduction in CRP and white blood cell counts—but this finding was not statistically significant. The investigators found the most common adverse events to be gastrointestinal complaints and the most severe adverse event to be pneumonia. This study is limited by its short duration and lack of generalizability given the specified population of patients who have had a myocardial infarction in the past 30 days.
Tong DC, Quinn S, Nasis A, et al. Colchicine in patients with acute coronary syndrome. Circulation. 2020;142(20):1890-1900. doi:10.1161/ circulationaha.120.050771 - COPS
Similar to the COLCOT trial, the investigators of the Colchicine in Patients with Acute Coronary Syndromes (COPS) trial sought to assess the safety and efficacy of colchicine in patients with recent acute coronary syndromes. It was a randomized, double-blind, placebo-controlled trial.
Across 17 hospitals in Australia, the trial enrolled 795 patients (n=795) aged 18-85 years old who presented with ACS and had angiographic
AAEM/RSA RESIDENT JOURNAL REVIEW >> COMMON SENSE JULY/AUGUST 2023 39
evidence of CAD and underwent percutaneous coronary intervention (PCI) or were medically managed. Patients were excluded if they required surgical revascularization, had pre-existing long-term colchicine or immunosuppressant therapy, had severe hepatic or renal insufficiency, or had known active malignancy. The intervention group received colchicine 0.5 mg twice daily for one month followed by 0.5 mg daily for 11 months. The control group received a matching placebo. Follow-up was conducted via structured telephone interviews at one, six, and 12 months and by review of primary and secondary care records. The primary outcome was the composite outcome of death from any cause, ACS, ischemic-driven urgent revascularization, and non-cardioembolic ischemic stroke. Secondary outcomes included the components of the primary composite outcome.
At 12 months, the primary outcome was 6.1% for the colchicine group and 9.5% for the placebo group (p=0.09). Post hoc analysis was performed after unblinding the trial. While cardiovascular deaths occurred less frequently in the colchicine group compared to the placebo group (5.0% versus 9.5%; HR 0.51; 95% CI, 0.29–0.89; p=0.019), the colchicine group had a greater incidence of death by any cause. There were eight patient deaths in the colchicine group compared to one patient death in the control group (p<0.05). Additionally, there were five patient deaths by non-cardiovascular cause in the colchicine group compared to zero patient deaths by non-cardiovascular cause in the control group (p=0.023).
The results suggest that colchicine does not improve one-year cardiovascular outcomes for patients presenting with ACS. It is worth noting the higher rate of total deaths, and particularly the higher rate of non-cardiovascular deaths, in participants receiving colchicine. The authors note that the study was limited by its small sample size from a single country, the risk of reporting bias introduced by telephone interviews, inconsistency in follow-up time, and the number of patients lost to follow-up in the presented mortality data. Larger studies assessing colchicine in ACS and other cardiovascular populations are required to definitively prove or disprove the utility and safety of colchicine.
Conclusion
LoDoCo1 and LoDoCo2 both demonstrated convincing evidence for the use of colchicine in secondary cardiovascular prevention for those with stable CAD. However, the tolerability of colchicine may be a major barrier to patient compliance with gastrointestinal symptoms being the most common side effect.
While COLCOT demonstrated a technically statistically-significant reduction in major adverse cardiovascular events (mainly in the reduction of stroke and coronary revascularization) with colchicine compared to placebo in patients presenting with ACS, the COPS trial showed that colchicine did not improve cardiovascular outcomes at 12 months in those suffering from recent ACS. Importantly, COLCOT reported pneumonia as an adverse event in the colchicine group compared to the placebo, while COPS reported a higher incidence of all-cause mortality in the colchicine group.
Clinical Question: Does low-dose colchicine improve cardiovascular outcomes in patients with coronary artery disease?
Answer: Although there is promising evidence that it may reduce cardiovascular deaths in patients with stable CAD, its utility in acute and recent ACS is less convincing, and its long-term safety and efficacy still need to be established before widespread use.
References
1. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105(9):1135-43.
2. Leung YY, Yao Hui LL, Kraus VB. Colchicine--Update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum. 2015;45(3):341-50.
3. Crittenden DB, Lehmann RA, Schneck L, et al. Colchicine Use Is Associated with Decreased Prevalence of Myocardial Infarction in Patients with Gout. J Rheumatol. 2012;39:1458-64.
OPERATIONS MANAGEMENT SECTION
Countinued from page 18 >>
surprisingly receptive. Six months later the CEO comes back to you and asks how you were able to change his behavior. The CEO is pleased that his problem is solved, Dr. Jones is again a happy and productive clinician and you are relieved that you were able to handle the situation.
These are some of the issues that ED operations focuses on. Want to learn more? Join the Operations Management Section.
AAEM/RSA RESIDENT JOURNAL REVIEW
COMMON SENSE JULY/AUGUST 2023 40

COMMON SENSE JULY/AUGUST 2023 41
AAEM Job Bank Service
Promote Your Open Position
To place an ad in the Job Bank: Equitable positions consistent with the Mission Statement of the American Academy of Emergency Medicine and absent of restrictive covenants, will be published (upon approval). All ads run for a six month period or until canceled and will appear in the AAEM member magazine Common Sense and online. For pricing and more information visit www.aaem.org/membership/benefits/ job-bank.
Complete a Job Bank registration form, along with the Criteria for Advertising Section, and submit payment. If you are an outside recruiting agent, the Job Bank Criteria for Advertising must be downloaded and completed by a representative from the recruiting hospital/group.
Direct all inquiries to: www.aaem.org/membership/benefits/job-bank or email info@aaem.org.
Positions Available
For further information on a particular listing, please use the contact information listed.
Section I: Positions in full compliance with AAEM’s job bank advertising criteria, meaning the practice is wholly-owned by its physicians, with no lay shareholders; the practice is equitable and democratic; due process is guaranteed after a probationary period of no more than one year; there are no post-employment restrictive covenants; and board certified emergency physicians are treated equally, whether they achieved ABEM/AOBEM/RCPSC certification via residency training or the practice track.
Section II: Positions that cannot be in full compliance with AAEM’s job bank criteria, because they are employee positions with hospitals or medical schools and the practice is not owned by its emergency physicians. Thus there may not be financial transparency or political equity.
Section III: Positions that cannot be in full compliance with AAEM’s job bank criteria, because they are government or military employee positions. The practice is not owned by its emergency physicians, and there may not be financial transparency or political equity.
Section IV: Position listings that are independent contractor positions rather than owner-partner or employee positions.
SECTION I: POSITIONS RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK CRITERIA
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA (Below are hospitals, non-profit or medical school employed positions.)
CONNECTICUT
Trinity Health Of New England seeks BC/BE EM Physicians to join our emergency medicine teams at Mercy Medical Center in Springfield, Massachusetts, Saint Francis Hospital and Medical Center in Hartford, Connecticut and Saint Mary’s Hospital in Waterbury, Connecticut. Our practice model empowers our physicians to work at their highest level, while allowing time for professional development and family life. Whether you are focused on providing outstanding patient-centered care or driven to grow into a leadership role, you will thrive at Trinity Health Of New England. To learn more, visit our provider portal at www. JoinTrinityNE.org (PA 1985)
Email: ndiehl@abccreative.com
Website: https://www.jointrinityne.org/Physicians
MayJun, JulAug, SepOct
LOUISIANA
Ochsner Health is seeking a board certified/board eligible physicians to join our Division of Pediatric Emergency Medicine at Ochsner Medical Center and Ochsner Hospital for Children. Opportunity Details: • Employed physician group that offers competitive fair market compensation plus benefits • In House pediatric intensivist and hospitalist attendings 24/7 to assist with streamlined pediatric admissions and patient care. • All facilities utilize Epic electronic health records integrating care across the system and facilitating seamless multi-hospital practice • All specialties available for consultation and easy one-call transfer from our community emergency departments to our main campus Interested physicians should apply to: https://ochsner. wd1.myworkdayjobs.com/OchsnerPhysician/job/New-Orleans--New-Orleans-Region---Louisiana/Pediatric-EmergencyMedicine_REQ_00158668 (PA 1991)
Email: courtney.lawhun@ochsner.org
Website: https://ochsner.wd1.myworkdayjobs.com/ OchsnerPhysician/job/New-Orleans---New-Orleans-Region--Louisiana/Pediatric-Emergency-Medicine_REQ_00158668
MayJun, JulAug, SepOct
MASSACHUSETTS
Emergency Medicine Physician Dartmouth Health The Department of Emergency Medicine at Dartmouth-Hitchcock Medical Center (DHMC) is seeking a BC/BE Emergency Medicine Physician to join our team of dedicated Emergency
Physicians. Responsibilities include supervision and teaching of medical students, off-service residents, and Emergency Medicine residents. Interested physicians are encouraged to apply online by submitting their CV and addressing their cover letter to: Scott Rodi, MD, MPH, FACEP Chair, Department of Emergency Medicine Emergency Medicine Regional Medical Director, Dartmouth Health Qualifications • Advanced clinical degree (MD or DO) • Post graduate training in Emergency Medicine residency program Apply link: https://careers. dhproviders.org/emergency-medicine-physician-lebanon-3-0 EOE. (PA 2000)
Email: Jacqueline.M.LaBelle@hitchcock.org
Website: https://careers.dhproviders.org/emergency-medicinephysician-lebanon-3-0
JulAug, SepOct, NovDec
MICHIGAN
Medical Director of Emergency Medicine Research Corewell Health William Beaumont University Hospital (previously Beaumont Royal Oak) The Department of Emergency Medicine is recruiting a Medical Director of Research to lead a nationally recognized research program. The successful candidate will be an ABEM certified emergency physician who works clinically at University Hospital with academic appointment at Oakland University William Beaumont School of Medicine. Preference will be given to candidates with a record of extramural funding, success mentoring colleagues, formal academic research training, and experience managing research. The institution is seeking a broad and diverse candidate pool. University Hospital is a 1,100-bed referral center that has been recognized by U.S. News and World Report as one of the “Best Hospitals” for the past 26 years. In 2022, it ranked second statewide. The Emergency Department is the busiest center in Michigan with an annual volume approaching 120,000 visits. It has had an EM residency program for 30+ years and has Emergency Geriatric, Pediatric, Ultrasound and Medical Education fellowships. In 2021, ED faculty published 50+ papers; extramural support totaled over $550,000. MD or DO (PA 1979)
Email: kimberly.andrews@beaumont.org
Website: https://providers.beaumont.org/physician-resources/ physician-careers
MayJun, JulAug, SepOct
NEW HAMPSHIRE
Dartmouth Health and The Geisel School of Medicine at Dartmouth are pleased to announce a national search for the Chair of the Department of Emergency Medicine. This is an opportunity to lead an exceptional clinical department known nationally for providing outstanding patient care, fostering the medical and biomedical education of the next generation, and supporting innovative research. In this leadership role, the Chair of the Department of Emergency Medicine will have primary responsibility and accountability for the overall direction, operation, and management of the Department in accordance with the mission and goals of Dartmouth Health and The Geisel School of Medicine at Dartmouth. Qualified candidates will: hold a medical degree (MD, MD/MPH, MD/MBA, MD/PhD) or equivalent degree(s); qualify for rank of Professor or Associate Professor at the Geisel School of Medicine; be American board certified; and be a New Hampshire licensed physician or should be eligible for licensure in the state of New Hampshire. The preferred candidate will have five or more years of experience as a strategic leader with the ability to manage a substantial, complex, and evolving organization. All application material should be submitted to: Elizabeth Homsy Senior Associate, Healthcare Practice Korn Ferry elizabeth.homsy@kornferry. com Dartmouth Health is an equal opportunity employer, and all qualified applicants will receive consideration for employment without regard to race, color, religion, sex, national origin, disability status, veteran status, gender identity or expression, or any other characteristic protected by law. (PA 1966)
Email: elizabeth.homsy@kornferry.com
Website: https://www.dartmouth-health.org/ MarApr, MayJun, JulAug
NEW JERSEY
Opportunity: Chairman, Department of Emergency Medicine, Capital Health Systems Licensing and Education Requirements: • Board certified in Emergency Medicine • 5-10 years of clinical experience (preferred) • 5 years of group leadership (preferred) Responsibilities for this position include, but are not limited to:
1. Provider Management: a. Manage recruitment and retention of provider staff b. Maintain regular reviews and evaluations of providers c. Interview provider candidates d. Participate in on-boarding of new providers to ensure they have a full

None Available at this time. 42
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
are hospitals, non-profit or medical school employed positions.)
understanding of operational procedures e. Monitor the overtime rate of providers across the system to ensure department goals are achieved f. Create routine schedule, call schedule, and staffing models for the Capital Health Emergency Department
2. Clinical Workflow & Operations: a. Be accountable for the optimal operating efficiency of staff and develop/maintain a patient-centered approach to clinical care b. Develop and maintain a process to review note closure rates and plan to mitigate deficiencies across the system c. Meet with Utilization Review and Medical team leadership to identify opportunities for proper bed assignment and level of care d. Lead the ED Operations, ED leadership and ED Documentation meetings. Participate in other required meetings such as OBS Operations and CHMG Inpatient Operations e. Assist with implementation of Surge management f. Analyze metrics and review analysis with Senior Capital leaders g. Review clinical variation of practice and promote best practices h. Provide new disease management oversight i. Work in conjunction with emergency management systems to ensure emergency preparedness
3. Quality a. Keep abreast of local, regional and national trends in science and education as related to emergency medicine and communicate this information to staff, faculty and administration b. Liaison to committees such as Sepsis, AMI/CPC, stroke accreditation and Patient Satisfaction, Neuro Operations, Resuscitation, Maternal/ child, and Radiology c. Appoint committees and leadership roles as needed to further the goals and functions of the Department d. Address reported safety events, participate in adverse event review, and work directly with providers to ensure continued performance improvement
4. Residency a. Teaching b. Oversee development in conjunction with the Residency Director (PA 1959)
Email: apatel@capitalhealth.org
Website: https://www.capitalhealth.org/ MarApr, MayJun, JulAug
NEW JERSEY
RWJBarnabas Health, the largest integrated healthcare system in NJ, is seeking a Pediatric Emergency Medicine Physician for a FT role at Monmouth Medical Center in Long Branch, NJ. As part of the Pediatric Emergency Medicine team, the candidate will work alongside an experienced team of physicians and the opportunity to work closely alongside MMC’s Pediatrics division. In the heart of the Jersey Shore, this practice is just moments away from the famous NJ beaches and shore attractions.
Requirements: • BE/BC in Pediatric Emergency Medicine • NJ licensed or eligible If you are interested in this position, contact Meghan.Ryan@rwjbh.org (PA 1997)
Email: Meghan.Ryan@rwjbh.org
Website: https://www.rwjbh.org/ JulAug, SepOct, NovDec
NEW YORK
Chair of the Department of Emergency Medicine at Glen Cove Hospital Glen Cove Hospital is a 216-bed community hospital with the resources to care for all types of patients. Glen Cove has a very supportive and pro-emergency medicine administration as well as a new ICU, CCU, Telemetry, and Brain Injury Unit. We also have a very active and supportive hospitalist program. As Emergency Medicine Chair, you’ll have complete operational and clinical oversight of the department. You’ll collaborate with our experienced service line leadership team in efforts such as recruiting, finance, business development, and more. You’ll also have the incredible opportunity to work with other healthcare professionals across Northwell Health’s extensive integrated network. Glen Cove Hospital has a full-service Emergency Medicine department. Some highlights include: • Approximately 20,000 annual visits • ED consists of 22 private rooms and 4 trauma/critical care beds • 18 ICU/CCU beds • Press Ganey Guardian of Excellence Award 2022 for patient experience • Our Geriatric Emergency Department has a Level 1 Accreditation from ACEP • Designated Primary Stroke Center by The Joint Commission • AHA/ASA Get with the Guidelines Stroke Gold Plus with Honor Roll Plus Award • ACEP Accreditation Bronze Level for PACED (Pain & Addiction Care in the ED) Submit your CV to: adaily@northwell.edu In addition to the listed responsibilities, this leader will promote a positive and inclusive organizational culture, play an essential role in creating and executing team member engagement initiatives, and champion and advance diversity, equity, and inclusion as central to the organization and its values system. (PA 1981)
Email: ppenso@northwell.edu
Website: https://jobs.northwell.edu/career-specialties/ physicians/ MayJun, JulAug, SepOct
NORTH CAROLINA
Emergency Medicine – Site Medical Director (MD/DO) Wake Forest Emergency Providers We are seeking candidates with proven experience in leadership and clinical practice. This is a unique opportunity to lead a dynamic Emergency Medicine team with the support and backing of a large, regional, nonprofit, academic health system. In addition to practicing clinically, the selected candidate will also provide leadership in staffing, financial management, performance improvement, and quality and safety initiatives for their site. We offer a highly innovative model wherein our physicians have tremendous influence in their practice. This includes access to transparent financials and performance metrics and the ability to influence practice plans. With a lean administrative model and responsible staffing, our physicians have abundant resources at their disposal to improve outcomes for patients and lead care innovations. While our Medical Directors have autonomy to manage their sites, they also enjoy great collaboration and support with experienced peers, a strong Regional Director and a supportive President. This is an employed position with Wake Forest Emergency Providers About Wake Forest Emergency Providers Affiliated with Atrium Health Wake Forest Baptist (www.wakehealth.edu), Wake Forest Emergency Providers is a nationally recognized, 501c3 non-profit, proudly providing health care for all! We are contracted with select, partner organizations to provide staffing for Hospital Emergency Departments, Free Standing Emergency Departments, and Urgent Cares throughout the North Central and Northwest regions of North Carolina. Location Outdoor activities abound in the area with unrivaled hiking, road/gravel/ mountain biking, fly fishing, kayaking/rafting and rock climbing easily accessible. Public schools are among the top ranked in the state and the community is close-knit and supportive. Position Requirements: • Qualified Candidates must be Board Certified (or eligible) by the American Board of Emergency Medicine or equivalent, and licensed (or eligible) to practice medicine in the state of North Carolina. What We Believe When you join Wake Forest Emergency Providers, you will be welcomed into an inclusive culture that celebrates and respects the contributions a diverse team can make together. Practice where your voice is valued, your passion for advancing medicine is rewarded, and you get the resources and support you need to thrive personally and professionally. In our organization, you can work alongside the most advanced minds in medicine to improve medicine, elevate hope and advance healing—for all. Interested
Candidates May Contact: Scott Dudley Atrium Health Wake Forest Baptist - Provider Recruitment 336-341-2631 sdudley@ wakehealth.edu (PA 1969)
Email: sdudley@wakehealth.edu
Website: http://www.wakehealth.edu
AprMar, MayJun, JulAug
NORTH CAROLINA
Duke Pediatrics is recruiting for a faculty member to join the Division of Pediatric Emergency Medicine. Duke Children’s is ranked among the nation’s finest for pediatric care and is #1 in NIH funding for pediatric clinical science departments. Ideal candidates will possess excellent clinical skills, a passion for education, and a demonstrated record of scholarly contributions. The Greater Triangle area of Raleigh, Durham and Chapel Hill is culturally diverse, economically resilient and nationally recognized as a great place to live and work. Interested candidates should submit CV and Letter of Interest via https:// pdc.dukehealth.org/physician-jobs (PA 1958)
Email: sherrod.basnight@duke.edu
Website: https://pdc.dukehealth.org/physician-jobs
MarApr, MayJun, JulAug
VERMONT
The Department of Emergency Medicine at The Larner College of Medicine (LCOM) at The University of Vermont (UVM) is seeking an Emergency Medicine Physician to fill the role of Associate Professor or Professor in the Clinical Scholar Pathway, commensurate with years of experience and accomplishments. The physician identified in this search will be provided the opportunity to serve as the Vice Chair of Academic Affairs (VCAA) of the Department of Emergency Medicine. The Department of EM provides clinical coverage at the seven clinical campuses of the University of Vermont Health Network in Vermont and upstate New York. Fifty academic faculty in the Department work with colleagues in community clinical practice to serve approximately 200,000 patient visits annually, and the Network hospitals serve a catchment of 40,000 square miles and 1.4M people. LCOM students and Emergency Medicine
residents train clinically in three of the network sites with elective rotations in multiple other sites. Our primary teaching campus is the University of Vermont Medical Center, the only level 1 trauma center in the greater region. The majority of academic faculty provide clinical coverage at multiple sites in Network, including our rural and critical access sites, underscoring our commitment to high quality rural acute care delivery. The Vice Chair of Academic Affairs (VCAA) will lead advancement of the academic components of the mission of the Department of EM. The VCAA will mentor faculty, fellows, and residents in their academic efforts and will lead the Promotions and Tenure Committee in advising the Chair on readiness for promotion. Recruitment and retention of faculty, fellows, and residents with a commitment to diversity, equity, and inclusion will remain a top priority. The VCAA will collaborate with colleagues locally at LCOM and nationally through organizations such as AAEM, SAEM, CORD, and the AAMC, providing networking opportunities, enhancing mentorship, incorporating innovative educational practices, and fostering faculty development. The VCAA will be provided with 30% nonclinical time to achieve the roles and responsibilities across the following domains: · Leadership and Strategic Planning · Faculty Development & Mentorship · Faculty Evaluation and Feedback · Diversity, Equity, and Inclusion · Faculty Recruitment, Retention, and Wellness · Scholarship Although all interested candidates are encouraged to apply, strong preference will be given to candidates with leadership experience in the educational, clinical, and research activities of academic emergency medicine. Consistent with all recruitments, we seek candidates that demonstrate empathy, humanism, and humility, and candidates must be comfortable with an environment that employs transparency to create faculty and leadership accountability. Candidates must commit to our core values of Professionalism at the Larner College of Medicine and are advised to review our Statement on Professionalism. Interested individuals should apply online at https://www.uvmjobs.com/postings/58864 (position number 00026358). Confidential inquiries to acquire further information about this position may be directed to Dr. Ramsey Herrington, Chair of the Department of Emergency Medicine at ramsey. herrington@uvmhealth.org (PA 1962)
Email: Ramsey.herrington@uvmhealth.org
Website: https://www.uvmjobs.com/postings/58864
MarApr, MayJun, JulAug
WEST VIRGINIA
The Department of Emergency Medicine at Charleston Area Medical Center is recruiting a pediatric emergency medicine physician to work at Women and Children’s Hospital located in Charleston, WV. This 120-bed dedicated Women and Children’s Hospital is a part of a large university-affiliated regional referral center with a drawing population of 562,000. We have in-house Neonatologist with 24/7 coverage in Level III NICU as well as a PICU with pediatric intensivists. Charleston Area Medical Center also sponsors an ACGME accredited emergency medicine residency program with 20 residents at present. Position Requirements: • MD or DO degree from an accredited university medical school • Completion of an Emergency Medicine Residency and a Pediatric Emergency Medicine Fellowship or completion of a Pediatric Residency and a Pediatric Emergency Medicine Fellowship • Board Certification or Board Eligible (ABEM or AOBEM) in Pediatric Emergency Medicine • Ability to achieve full and unrestricted hospitalist privileges at Charleston Area Medical Center • Eligibility for a West Virginia Medical License Benefits include: • Excellent benefits package • Competitive compensation • Affordable community • Extraordinary family environment • Unsurpassed recreational activities • Outstanding school systems About Charleston, West Virginia Charleston is the state capital and largest city in the state. We are proud of our diverse population, amazing outdoor activities, and excellent schools. We are centrally located to numerous major metropolitan areas in North Carolina, Ohio, Pennsylvania, Virginia and Washington, DC, and Yeager International Airport is just 5 miles from the hospital. In addition, Charleston offers a Downtown district filled with eclectic galleries, chic boutiques, and unique restaurants. The area boasts a vibrant academic and professional community that offers a balanced professional career and a fulfilling personal lifestyle. Come see what our community can offer you! (PA 1955)
Email: carol.wamsley@camc.org
Website: http://www.camc.org
MarApr, MayJun, JulAug
COMMON SENSE JULY/AUGUST 2023 43
(Below
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA, CONTINUED
(Below are hospitals, non-profit or medical school employed positions.)
WEST VIRGINIA
The Charleston Area Medical Center Institute for Academic Medicine is seeking Emergency Medicine clinicians for academic positions as Core Faculty and Clinical Core Faculty. This regional, tertiary medical center sponsors an ACGME accredited emergency medicine residency program with 20 residents at present. Serving a multi-county area, the four Emergency Departments see over 130,000 patients per year and the following locations: CAMC Memorial Hospital - 30 beds with
4 assessment beds CAMC General Hospital – Level 1 Trauma Center with 26 beds and additional fast flow areas CAMC Teays Valley Hospital – 10 beds with 2 assessment beds CAMC Women and Children’s Hospital – 20 beds · Mid-level coverage all sites · 24/7 Hospitalists Coverage · Complete specialty and surgical support · Strong Administrative Support (PA 1989)
Email: ryan.nagy@vandaliahealth.org
Website: https://www.camc.org/ MayJun, JulAug, SepOct
SECTION III: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
(Below are military/government employed positions.)
None Available at this time.
SECTION IV: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
CALIFORNIA
Join our independent, democratic, partnership Group in sunny southern California. Epic, Dragon, holiday and night shift differential as well as APP help. Please send CV in confidence or see our website https://www.scemg.org/ (PA 1994)
Email: smistry007@yahoo.com
Website: https://www.scemg.org/
JulAug, SepOct, NovDec
CALIFORNIA
Join our team in the San Francisco Bay Area with immediate and ongoing Emergency Medicine and Urgent Care positions! Recently awarded a 5-year contract with an option for a 5-year extension with Santa Clara County Health System. Emergency Physicians Associates (EPA) is a democratic group with absolutely zero private equity, public debt, venture capital involvement, or non-physician shareholders. Pay is productivity based. Average EP hourly in excess of $300.00/hour. Night shift stipend. Transparent 3-year partnership track. Scheduling is performed by a practicing Emergency Physician with a full understanding of typical ED scheduling patterns. Predominantly 9-hour shifts. Engaged and responsive ED leadership. Excellent relationships with hospital administration and nursing staff. EDs we staff: Santa Clara Valley Medical Center. High acuity county hospital. Level 1 trauma center. Regional burn center. STEMI and Stroke receiving center. EM residency host. O’Connor Hospital. Full-service county-owned community hospital. Saint Louise Regional Hospital. Rural county-owned community hospital. Currently in the planning stages for trauma designation. Onsite CalStar base for ease of transfer. Washington Hospital. Busy well, resourced full-service district-owned community hospital in Fremont, CA. Epic EMR at all facilities. Start date ASAP. Ongoing. Full-time or per-diem. Requirements: ABEM BC/BE, unrestricted CA License, unrestricted DEA. Contact EPA at careers@epamg.com with questions and to apply. (PA 1999) Email: daniel.nelson@epamg.com
JulAug, SepOct, NovDec
FLORIDA
International Emergency Medicine Fellowship Opening at Global Physician Network, at Sarasota Memorial Health Care System, Sarasota, Florida A two (2) Year Fellowship Track Position for an ACGME Accredited Emergency Medicine Board Eligible / Board
Certified Attending who will accomplish the Fellowship with a Fully Funded International Project Based Field Experience, MBA in Project Management, and Certification in Crisis Leadership. Located in Sarasota the Fellowship is home to the Florida State University College of Medicine Emergency Medicine Residency Program. Please contact forwarding a statement of interest and your curriculum vitae. Dr. Sagar Galwankar, International Emergency Medicine Fellowship Director Email: gcsagar@ yahoo.com (PA 1968)
Email: gcsagar@yahoo.com
Website: https://www.globalphysiciannetwork.com/ MarApr, MayJun, JulAug
FLORIDA
Join a democratic group in Cape Coral, FL established since 1985, partnered with Lee Health. An annual volume of 70k at a single community hospital site. Competitive pay and top-notch
benefits including CME reimbursement, medical, 401k. Equal shift distribution averaging 14 shifts per month, 8-10 hours each, with only a few overnight shifts annually. Patient load of 1.5-2 per hour, with 24-hour physician and APP coverage. Epic with Dragon dictation. Opportunity to teach residents due to a new internal medicine residency. Enjoy a sunny coastal location, perfect for outdoor enthusiasts and families. (PA 1976)
Email: tylerensley@gmail.com
Website: https://capecoralemergencyphysicians.com/ MayJun, JulAug, SepOct
MINNESOTA
Join Emergency Physicians Professional Association (EPPA)! -a physician-owned, independent, democratic group of over 220 physicians staffing multiple facilities throughout Minnesota. Currently staffing 7 Twin Cities metro hospitals, 1 central MN hospital, 5 regional/rural sites, and 3 Urgency Rooms. Patient volumes 9K-75K per year. Immediate openings for BC/BE, Emergency Medicine residency trained physicians in the St. Cloud, Wilmar, and Monticello, MN areas with significant financial advantages (Shareholder buy-in is waived). Shifts range from 8 hours (metro) to 12 hours (rural). Sites include Level 1-4 trauma centers in multiple hospital systems. EPIC EMR at all sites. Variable workload based on site, ranging from 1.2-2 patients per hour. W2 with multiple benefits: malpractice, health, dental, life, disability, personal umbrella insurance; 401k, pension and profit sharing. Competitive compensation for full-time contract (1600 hours/year) with average RVU productivity. Shareholder/ Ownership track available. Night, weekend, and holiday differentials. Nocturnist positions possible. (PA 1965)
Email: bleagjeld@eppahealth.com
Website: https://www.eppahealth.com
MarApr, MayJun, JulAug
NEW YORK
CityMD is a network of urgent care centers dedicated to setting an unprecedented standard of care for our patients and an edifying, intuitive work environment for our employees. We are looking for board-certified Emergency and Family Practice trained physicians who thrive in an environment surrounded by highly trained and motivated individuals and operate on one of the most advanced administrative systems in healthcare today. Your responsibilities will include the diagnosis and treatment of patients of all ages and interpreting and archiving medical information. We are hiring board-certified physicians who are Emergency Medicine or Family Medicine trained to work in our state-of-the-art urgent care centers. Our facilities are staffed with highly trained and motivated individuals who operate one of the most advanced administrative systems in healthcare today. Highlights • Scribes on staff. This allows you to focus your time on direct patient care. • Advanced imaging available on a routine and STAT basis, including CT, US and MRI. • Specialist consultation allows for 48 hour turn around and same day results for urgent cases. • State-of-the-art facilities, digital X-Ray, laboratory services with modern, clean and aesthetically designed work environments. • Dedicated physician led Aftercare team following up on all aspects of patient care. • Integrated Electronic Medical Records across all CityMD locations. Our commitment to our patients and employees, along with our state-of-the-art personalized healthcare delivery
system, has taken CityMD from one location on the Upper East Side to over 130 in the New York/New Jersey area including Northern/Central/Southern New Jersey and Manhattan, Brooklyn, Queens, Long Island, Rockland, and Westchester County. As a proud “People First” company, we are centered on the values of integrity, excellence, professionalism, and quality. Our Compensation package is broken down as follows: • Competitive hourly rate plus performance-based bonus • 4 weeks of paid time off • $3000 annually in CME • 401K match is up to 4% of your bi-weekly pay up to annual IRS limits • Full medical, dental and vision benefits, as well as short term and long term disability benefits and company paid life insurance • Medical Professional Liability Insurance Covered • Holiday Pay & Extended Hour Site Differentials up to $45/hour on top of base • $120 - $185 per hour The provided compensation range is based on industry standards and salary determinations will be made based on numerous factors including but not limited to years of experience, individual performance, quality measures and location of position. (PA 1961)
Email: slameira@summithealth.com
Website: http://www.citymd.com
MarApr, MayJun, JulAug
NORTH CAROLINA
More than 40 years strong, ECEP II, P. A. is seeking a full-time emergency medicine physician for our emergency medicine group serving the greater Wilmington, NC area. Our full-time physicians practice an average of 28 to 30 hours per week. Wilmington practice sites include New Hanover Regional Medical Center, a level II trauma center, treating an annual patient volume of 75,000, Orthopedic Hospital, a community hospital with an annual patient volume of 27,000, and Scotts Hill Emergency Department, a full-service standalone emergency department with an annual patient volume of 34,000. Our group also practices at Pender Memorial Hospital in Burgaw, a community hospital located just 25 minutes north of Wilmington with an annual patient volume of 17,000. ECEP offers competitive pay and an excellent benefits package. Live, practice and enjoy a great quality of life in an exceptional coastal community with beaches, golf, and a historic waterfront at your doorstep. (PA 1984)
Email: kskaggs@ecepnet.com
MayJun, JulAug, SepOct
WASHINGTON
Emergency Physicians of Mason County are recruiting to add 1-2 partners to our LLC. We are an independent democratic group that staff a rural critical access hospital in the south Puget Sound. We have held the contract for over 30 years. Mason General Hospital in Shelton, Washington has an ED that sees approximately 20k patients a year. We have three daily shifts, 1112 hours each. No midlevels, and everyone is ABEM certified. 13 Bed ED. Excellent nursing coverage, often with 5 RN’s. General surgery and OB/GYN backup. Benefits: Competitive salary, malpractice paid by hospital (occurrence), 401-K, group health plan. Beautiful place to live. 1 hour or less from Olympic National Park. 2 hours to skiing. 2 hours from Seattle and Portland. Email rgbelville @ runbox.com. (PA 1982)
Email: rgbelville@runbox.com
MayJun, JulAug, SepOct
(Below are independent contractor positions.)
COMMON SENSE JULY/AUGUST 2023 44
AAEM is the leader within our field in preserving the integrity of the physician-patient relationship by fighting for a future in which all patients have access to board certified emergency physicians and physician rights are protected.
Member Benefits
Publications
Free subscriptions to the Journal of Emergency Medicine and Common Sense
Education
Free registration to the Annual Scientific Assembly with refundable deposit and discounted registration for other AAEM events
Members-Only Section
Access the AAEM Job Bank, your Advanced Resuscitation Expertise Card (for Full Voting members), and other academic and career-based benefits
Learn more about these and other member benefits at www.aaem.org/membership/benefits
American Academy of Emergency Medicine 555 East Wells Street, Suite 1100, Milwaukee, WI 53202-3823 (800) 884-2236 info@aaem.org www.aaem.org
Membership Categories
Fellow and Full Voting – FAAEM
Dues: $525 Board certified in emergency medicine or pediatric emergency medicine
Associate
Dues: $250 Graduate of an ACGME or AOA approved emergency medicine training program and not yet taken or passed your EM board
Fellow-in-Training
Dues: $75 Graduate of an ACGME or AOA approved emergency medicine training program and currently enrolled in a fellowship
International Member
Dues: $150 Physicians with an interest in emergency medicine who practice outside of the United States or Canada

Emeritus Member
Dues: $250 Full voting member who has practiced emergency medicine for 30 or more years and has been a full voting member for a minimum of 10 years -or- at least 65 years of age and have been a full voting member for a minimum of 10 years
Special circumstances may lead to a request for emeritus membership and will be reviewed on a case-by-case basis. See www.aaem.org/membership for more information.
Learn more and join today at: www.aaem.org/membership
Group Membership
AAEM offers group memberships to allow hospitals/groups to pay for the memberships of all their EM board certified & board eligible physicians.
100% ED Group Membership
Criteria: All board certified and board eligible physicians at your hospital/ group must be members
Discount: 10% discount on membership dues
ED Group Membership
Criteria: Two-thirds of all board certified and board eligible physicians at your hospital/group must be members
Discount: 5% discount on membership dues
For group memberships, AAEM will invoice the group directly. If you are interested in learning more about the benefits of belonging to an AAEM ED group, please contact us at info@aaem.org or (800) 884-2236.
Join Today! www.aaem.org/membership 51 COMMON SENSE SEPTEMBER/OCTOBER 2021

COMMONSENSE 555 East Wells Street / Suite 1100 Milwaukee, WI 53202-3823 PRSRT STD U.S. POSTAGE PAID MILWAUKEE, WI PERMIT NO. 0188








 Jonathan S. Jones, MD FAAEM
Jonathan S. Jones, MD FAAEM

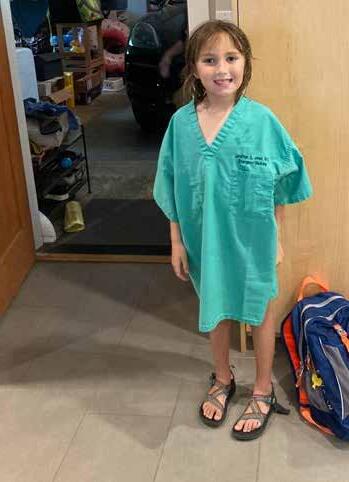









 Laura Cazier, MD FAAEM, Amanda Dinsmore, MD FAAEM, and Kendra Morrison, DO
Laura Cazier, MD FAAEM, Amanda Dinsmore, MD FAAEM, and Kendra Morrison, DO

 Bryce Pulliam, MD FAAEM
Bryce Pulliam, MD FAAEM










 Algis Baliunas, MD FAAEM
Algis Baliunas, MD FAAEM






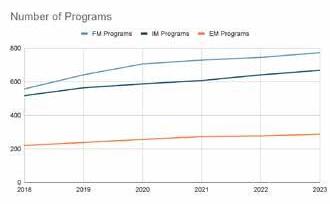
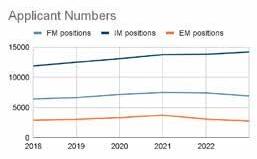


 Tom Scaletta, MD MAAEM, Akiva Dym, MD FAAEM, and Anthony Rosania, MD MHA FAAEM
Tom Scaletta, MD MAAEM, Akiva Dym, MD FAAEM, and Anthony Rosania, MD MHA FAAEM







 Andrew Grock, MD* and Al’ai Alvarez, MD †
Andrew Grock, MD* and Al’ai Alvarez, MD †














 AAEM/RSA PRESIDENT’S MESSAGE
AAEM/RSA PRESIDENT’S MESSAGE


 Curtis Marino, DO PGY3
Curtis Marino, DO PGY3


 Will Zhu, MS4* and Aliza Siddiqui, MS4 †
Will Zhu, MS4* and Aliza Siddiqui, MS4 †





 Jordan Vaughn, MD and Alyssa Eily, MD
Jordan Vaughn, MD and Alyssa Eily, MD



