
COMMON SENSE VOICE OF THE AMERICAN ACADEMY OF EMERGENCY MEDICINE VOLUME 30, ISSUE 2 MARCH/APRIL 2023 President's Message: Stay in the Fight 2 6 Editor's Message: The Personalities in Your Resuscitation Room 9 Heart of a Doctor: Trust 46 AAEM/RSA President’s Message: Not Even the Sky is The Limit for Emergency Medicine 45 Young Physicians Section: Keeping the Flame Lit Page 15 If You Died and Came Back, What Would Your Art Look Like? Page 22
Officers
President
Jonathan S. Jones, MD FAAEM
President-Elect
Robert Frolichstein, MD FAAEM
Secretary-Treasurer
L.E. Gomez, MD MBA FAAEM
Immediate Past President
Lisa A. Moreno, MD MS MSCR FAAEM FIFEM
Past Presidents Council Representative
William T. Durkin, Jr., MD MBA MAAEM FAAEM
Board of Directors
Kimberly M. Brown, MD MPH FAAEM
Phillip A. Dixon, MD MBA MPH FAAEM CHCQMPHYADV
Al O. Giwa, LLB MD MBA MBE FAAEM
Robert P. Lam, MD FAAEM
Bruce Lo, MD MBA RDMS FAAEM
Vicki Norton, MD FAAEM
Kraftin Schreyer, MD MBA FAAEM
YPS Director
Fred E. Kency, Jr., MD FAAEM
AAEM/RSA President
Leah Colucci, MD MS
Editor, JEM
Ex-Officio Board Member
Stephen R. Hayden, MD FAAEM
Editor, Common Sense
Ex-Officio Board Member
Andy Mayer, MD FAAEM
Executive Director
Missy Zagroba, CAE
Executive Director Emeritus
Kay Whalen, MBA CAE
Common Sense Editors
Mehruba Anwar Parris, MD, Assistant Editor
Alessandra Della Porta, MD, Resident Editor
Stephanie Burmeister, MLIS, Managing Editor
Articles appearing in Common Sense are intended for the individual use of AAEM members. Opinions expressed are those of the authors and do not necessarily represent the official views of AAEM or AAEM/RSA. Articles may not be duplicated or distributed without the explicit permission of AAEM. Permission is granted in some instances in the interest of public education. Requests for reprints should be directed to AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202, Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org
AAEM is a non-profit, professional organization. Our mailing list is private.
Mission Statement
The American Academy of Emergency Medicine (AAEM) is the specialty society of emergency medicine. AAEM is a democratic organization committed to the following principles:
1. Every individual, regardless of race, ethnicity, sexual identity or orientation, religion, age, socioeconomic or immigration status, physical or mental disability must have unencumbered access to quality emergency care.
2. The practice of emergency medicine is best conducted by a physician who is board certified or eligible by either the American Board of Emergency Medicine (ABEM) or the American Osteopathic Board of Emergency Medicine (AOBEM).
3. The Academy is committed to the personal and professional well-being of every emergency physician which must include fair and equitable practice environments and due process.
4. The Academy supports residency programs and graduate medical education free of harassment or discrimination, which are essential to the continued enrichment of emergency medicine, and to ensure a high quality of care for the patient.
5. The Academy is committed to providing affordable high quality continuing medical education in emergency medicine for its members.
6. The Academy supports the establishment and recognition of emergency medicine internationally as an independent specialty and is committed to its role in the advancement of emergency medicine worldwide.
Membership Information
Fellow and Full Voting Member (FAAEM): $525* (Must be ABEM or AOBEM certified, or have recertified for 25 years or more in EM or Pediatric EM)
Associate: $150 (Limited to graduates of an ACGME or AOA approved emergency medicine program within their first year out of residency) or $250 (Limited to graduates of an ACGME or AOA approved emergency medicine program more than one year out of residency)
Fellow-in-Training Member: $75 (Must be graduates of an ACGME or AOA approved emergency medicine program and be enrolled in a fellowship)
Emeritus Member: $250 (Please visit www.aaem.org for special eligibility criteria)
International Member: $150 (Non-voting status)
Resident Member: $60 (voting in AAEM/RSA elections only)
Transitional Member: $60 (voting in AAEM/RSA elections only)
International Resident Member: $30 (voting in AAEM/RSA elections only)
Student Member: $40 (voting in AAEM/RSA elections only)
International Student Member: $30 (voting in AAEM/RSA elections only)
Pay dues online at www.aaem.org or send check or money order to:
AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202 Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org
Table of Contents COMMONSENSE AAEM-0223-348
TM Upcoming Events 4 Foundation Contributions ................................................................................................................8 PAC Contributions ............................................................................................................................8 LEAD-EM Contributions 8 Aging Well in Emergency Medicine Interest Group: Caring for Aging Parents: Challenges and Skills 34 Operations Management Committee: Avoiding Emergency Department Admissions: The Why and How 35 Rural Medicine Interest Group: “If It Wasn’t For You, I Wouldn’t Be Here Today” 37 Palliative Care Committee: CPR is Not Resuscitation 39 Critical Care Medicine Section: Overcoming Obstacles to Bystander CPR 42 Emergency Ultrasound Section: An Argument for Ultrasound in Cardiac Arrest ..........................43 Academic Affairs Committee: Dragon Slayer ................................................................................44 Young Physicians Section: Keeping the Flame Lit 45 AAEM/RSA Editor’s Message: Care that Seeks to Affirm Life 47 Medical Student Council Chair’s Message: Emergency Medicine Fellowships 49 Early Management of Right Ventricular Dysfunction in the Emergency Department 52 Leveraging AMA and State Medical Society Memberships toward Advocacy for and by Physicians: Some Success Stories from the November 2022 Interim Meeting of the American Medical Association House of Delegates 55 AAEM/RSA Resident Journal Review: Utility of Haloperidol and Droperidol in Cannabinoid Hyperemesis Syndrome 58 Board of Directors Meeting Summary: February ..........................................................................61 AAEM Job Bank ..............................................................................................................................62
COMMON SENSE MARCH/APRIL 2023
COMMONSENSE
Featured Articles
2
President’s Message: Stay in the Fight
In his President’s Message, Dr. Jones discusses the FTC proposal to ban non-compete contract clauses and the ongoing role AAEM is playing in this potentially exciting change and encourages all AAEM members to continue fighting for changes to improve health care.
6
Editor’s Message: The Personalities in Your Resuscitation Room
When you walk into this room, along with the newest and sickest patient is a diverse group of individuals who all have a unique role and perspective. In this article, our Editor asks you to put yourself into the other participants’ shoes and see the resuscitation from their perspective.
9
Heart of a Doctor: Trust Pavitra Krishnamani pulled her patient, Lina back into the temporary patient evaluation room, she faltered. How was I going to deliver this news that may make her feel as though she been misled?
11
Board of Directors Candidate Statements
Please review the candidate statements from the 2023 Board of Directors candidates, then exercise your democratic right to vote and make your voice heard!
26
Wellness Committee: Mental Health Licensure Questions: Is Your State Good or Bad?
“Is there a map of good states and bad states?” Sigh. “It isn’t that easy.”
46
28
Preview of the 29th Annual Scientific Assembly
Come join AAEM for the annual Scientific Assembly occurring April 21-25 in New Orleans, LA. We look forward to seeing you!

22
If You Died and Came Back, What Would Your Art Look Like?
A new documentary featuring Dr. Matthew Wetschler has answered this question. Dr. Wetschler is a fellow emergency physician and artist who survived a catastrophic spinal cord injury and cardiac arrest while surfing and returned to both his career and artistry.

23
Social EM & Population Health: Climate Change, Social Justice, and the Future of Emergency Medicine: An Interview with Emily Sbrioli, MD
You’ve probably thought of how climate change effects emergency medicine physicians—we are the safety net for our communities. But have you ever thought of the oopposite—how are emergency physicians contributing to climate change?

38
AAEM/RSA President's Message: Not Even the Sky is the Limit for Emergency Medicine
How would you like to practice emergency medicine...IN SPACE! Former AAEM/RSA President Haig Aintablian shares his thoughts on the future outlook of practicing EM in space.
Ethics Committee: "First, Do No Harm"
We all remember standing in our graduation robes, hand raised, as we recited the Hippocratic Oath at our medical school graduations. It seemed very simple...at first.
VOICE OF THE AMERICAN ACADEMY OF EMERGENCY MEDICINE VOLUME 30, ISSUE 2 MARCH/APRIL 2023
COMMON SENSE MARCH/APRIL 2023 1
Stay in the Fight
Jonathan S. Jones, MD FAAEM

n the last month or so, I feel like I’ve spent nearly as much time talking with the Federal Trade Commission (FTC) and various reporters as I have with patients and consultants. I must admit that this did take a little getting used to and at times I was not entirely thrilled to receive word that yet another reporter with yet another news organization wanted an interview for their story on non-competes, and by the way, the deadline is in four hours. However, this is obviously great!
Imental health, boarding of patients, staffing levels, or truly any other issue, the single most difficult problem we face is getting our perspective into the public media. Now, at least in regards to non-competes, we have accomplished that.

Our strategy is not simply to comment on non-competes, but to parlay this newfound public interest in non-competes into wider awareness of the problem with lack of due process, among others.
AAEM is the clear expert on this issue amongst medical societies.
Then, in April 2022, when the FTC hosted a listening session on the influence of private equity and consolidation in health care, AAEM was well represented with multiple speakers on the topic. We obviously made an impact as in January of this year, the FTC contacted us and asked to arrange a specific follow-up conference to better understand the Academy’s concerns and our suggested interventions and resolutions.
We have continued to provide information and commentary since these meetings. Then in February of this year, I participated in an FTC sponsored listening session on their new proposed ban on non-competes. AAEM was the only emergency medicine organization officially represented on the call.
The Academy’s official response to the FTC proposal has been submitted and widely publicized to lawmakers and journalists. All information referenced above, including links to the FTC sessions, can be found by visiting our webpage or clicking on the QR code at the end of this article.
This is a sign of progress for the Academy. Ever since the founding of the Academy, the inappropriateness of non-compete clauses in emergency physician contracts has been core to our mission. Now non-physicians care too. It is exciting, energizing, and makes one optimistic. For decades, we have fought to bring issues vital to the sustained practice of emergency medicine into the public sphere.
During my time with the Academy, with nearly every discussion involving our core issues, weather it be non-competes, non-physician practitioners, due process, physician oversupply, lack of rigorous residency standards,
First, some background. While the FTC (and nearly every federal agency) is fairly secretive about the impetus behind their decisions, this non-compete decision didn’t just happen overnight. Way back in December 2020, AAEM, along with multiple other organizations, wrote a letter to President Biden encouraging him to consider opposition to non-compete clauses as a factor in choosing nominations to the FTC. AAEM was the only national medical organization to sign this letter. While I am sure that this one single letter did not influence his administration’s decision, it sure did not hurt. In addition, it also further cemented the fact that
Following the most recent FTC call, requests for interviews from journalists greatly increased. Many mentioned that AAEM seems to be a leader in opposing non-competes and that they had not previously heard some of our arguments. This is progress. For far too long, journalists simply went to the American Medical Association (which actually supports the presence of non-compete clauses in physician contracts) or to one of the larger subspeciality organizations.
At least in relation to emergency medicine, the media finally seem to be realizing that bigger does not necessarily mean better. Likewise, better funded does not mean better. Better means better. An unwavering devotion to both the patient and specialty physician, such as the
AAEM PRESIDENT’S MESSAGE
>>
[B]igger does not necessarily mean better… [B]etter funded does not mean better. Better means better.
COMMON SENSE MARCH/APRIL 2023 2
An unwavering devotion to both the patient and specialty physician, such as the mission of our Academy, means better.”
mission of our Academy, means better. Switching gears a little, I want discuss some concerns I have heard from members as well as non-physicians concerning the FTC proposal to ban non-competes as I think this could help us all communicate our concerns more succinctly.
First, many of our members (and some in Congress) have a general libertarian and/or free-market outlook. At first glance, the FTC rule would seem to run counter to these more general beliefs. Specifically, is it an overreach of executive authority? Is it increasing government interference in private business decisions? Does it simply enlarge the administrative state? Does any of this matter as long as the proposal is good for emergency medicine?
Well, of course it matters. We do not need to convince EM doctors that it matters, we need to convince the patients, media, politicians, and even hospitals that it matters.
Therefore, as to the concern that the FTC may be overstepping its constitutional authority in proposing a ban, this does not matter. This is a separate issue. It is certainly an important issue, but one on which AAEM cannot comment. We are not a constitutional law society. We are an emergency medicine society. It is premature to have that discussion and detracts from the pertinent issues related to the need for a ban. Other than acknowledging that the Supreme Court may well strike down any final FTC rule, no further discussion of this issue need take place at this time. Anyone pushing this angle is simply sidestepping the true concern which is the appropriateness, or lack thereof, of non-compete clauses, specifically in emergency physician contracts.
And by the way, this is one reason why the Academy is not simply communicating with the FTC, but with media and politicians as well. Even if the FTC ban is overturned, we are working to create enough public and political support so that critical portions of the rule will be pursued by Congress.
As to the argument that the rule is increasing government intervention in private business decisions. Well, if health care were truly a
free market system, then this rule may indeed be unnecessary. However, I can think of no industry in this country (perhaps save alcohol distribution), that is further from a true market economy than health care. Health care is essentially the only industry where the consumer has no idea of the actual cost of the product. The consumer also often has limited to no choice as to where to obtain the product. Likewise, the true supplier of the product is often obfuscated from the consumer. Finally, government price controls exist to cover a vast majority of the product. Those arguing against the FTC proposal because it would distort the market or that it is an over intrusive government intervention, have clearly flawed logic. There already is overly intrusive government intervention in health care.
While it feels odd and somewhat uncomfortable to refer to patients as consumers, and medicine as a product, I think some of the problems we face are due to not treating health care as a business. Yes, it is a unique business, but if we are to hold sway with the FTC and other agencies regulating business, then we must, at least in some respects, treat what we do as a simple business.
Much media attention has rightly been given to the fact that many service sector workers, specifically in fast food have non-compete clauses in their contracts. This is egregious and unwarranted. And while we are well compensated, in the grand scheme of things, at least in the business world, how is an emergency physician any different than a short order cook? I hold that we
are not. Just as the cook has no inside or proprietary knowledge concerning the restaurant, neither do we have proprietary knowledge of the hospital or of how to practice emergency medicine. It’s not like we know the recipe to the secret sauce. And just as the restaurant does not teach the cook how to cook, the hospital does not teach the doctor how to doctor. The cook and the doctor are both hired because we already possess the knowledge and skills needed for the job. The main difference is compensation.
This leads us to collaborations. It may seem odd at first, but to the ubiquitous Contract Management Group (CMGs), especially one run by private equity, we are simply labor. The CMG sees us as an expense, as a worker, as a provider.

Yes, I actually used the word provider. I hate it too, but that is what we are to CMGs. Incidentally, one CMG for which I work parttime seems to go out of their way to call physicians providers, even given an award to the physician with the highest patient satisfaction for the month, but the award is for the being an excellent “provider.”
If we are to vanquish our advisories, then we need to understand how they think. And so if they see us simply as an expendable and replacement labor expense, then it may well be time to examine the successful strategies of those also viewed as replaceable labor.
AAEM PRESIDENT’S MESSAGE
>>
COMMON SENSE MARCH/APRIL 2023 3
One repercussion of the [Covid] crisis is the public realization that the emergency medicine “safety net” has holes. Together with our like-minded partners in other specialties, similarly impacted workers in other fields, concerned patients, citizens, and politicians, we are starting to mend those holes.”
Is it time for collective bargaining? I don’t know, but it certainly seems that it is time for serious consideration. Maybe instead of collective bargaining, we need some trust busting. Maybe it’s time to realize that there is no market economy left in health care and so intervention, such as the recent FTC proposal are needed.
To address these questions, the Academy is communicating with multiple other specialties, specifically hospital based specialties, to organize a summit to address shared concerns and pursue meaningful action from either federal agencies or Congress. And we are partnering with allies outside of the house of medicine as
well. The American Academy of Emergency Medicine has been fighting for fair and equitable practice rights for decades. We are no longer fighting alone. Like all crises, the COVID crisis affected significant change, some for the better and some for the worse. One repercussion of the crisis is the public realization that the emergency medicine “safety net” has holes. Together with our like-minded partners in other specialties, similarly impacted workers in other fields, concerned patients, citizens, and politicians, we are starting to mend those holes. The prohibition of non-compete clauses is just the beginning.
This is an exciting time to practice emergency medicine. It is an even more exciting time to be fighting for changes to improve health care delivery in this country. That is what you, I, and every single member of the Academy is doing. Thank you for your support. Stay in the fight.
aaem.org/advocacy/noncompete
Upcoming Events: AAEM Directly, Jointly Provided, & Recommended
AAEM is featuring the following upcoming conferences and activities for your consideration. For a complete listing of upcoming conferences and other meetings, please visit: aaem.org/education/events

AAEM Events
April 21-25, 2023
29th Annual Scientific Assembly (New Orleans, LA) aaem.org/aaem23
April 22, 2023
ED Operations Certificate Course (Virtual and in-person at AAEM23) aaem.org/education/events/edocc
May 3 & 4, 2023
Virtual Oral Board Review Courses aaem.org/education/events/oral-boards
May 26-27, 2023
FLAAEM 2023 Scientific Assembly aaem.org/get-involved/chapter-divisions/flaaem/scientific-assembly
7-10 September 2023
XIIth Mediterranean Emergency Medicine Congress (Rhodes, Greece) aaem.org/memc23
September 13 & 14, 2023
Virtual Oral Board Review Courses aaem.org/education/events/oral-boards
November 29 & 30, 2023
Virtual Oral Board Review Courses aaem.org/education/events/oral-boards
Jointly Provided
Re-Occurring Monthly
Unmute Your Probe: Virtual Ultrasound Webinar Series Jointly provided by EUS-AAEM aaem.org/eus
Re-Occurring Monthly Spanish Education Series*
Jointly provided by the AAEM International Committee aaem.org/get-involved/committees/committee-groups/international/ spanish-education-series
July 10-12, 2023
Joy & Wholeness Summit (Park City, UT)
Jointly provided by the Coalition for Physician Well-Being forphysicianwellbeing.org/2023-coalition-annual-conference
Recommended
March 31, 2023
2023 ACMT Annual Scientific Meeting (San Diego, CA) education.acmt.net/products/2023-acmt-annual-scientific-meeting#tab-product_tab_overview
Advances in Cancer ImmunotherapyTM sitcancer.org/education/aci
April 24, 2023 - A Focus on Toxicity Management Part 1 (Chicago, IL and Virtual)
June 27, 2023 - A Focus on Toxicity Management Part 2 (Virtual)
Date/Time TBD - A Focus on Cellular Therapies and T cell Engagers (Washington, DC and Virtual)
October 19, 2023 - A Focus on Hematologic Malignancies (Virtual)
May 19-21, 2023
Take Medicine Back Summit 2023 (Asheville, NC and virtual) bit.ly/tmbsummit22
Online CME
Recognizing Life-Threatening Emergencies in People with VEDS thesullivangroup.com/TSG_UG/VEDSAAEM/
AAEM PRESIDENT’S MESSAGE
COMMON SENSE MARCH/APRIL 2023 4
How can you help?
Join your colleagues and make a gift or a pledge today.
Gifts at all levels can be paid in one year or pledged over two to five years. We encourage individuals, physician groups, and companies to help support the fight!
$50,000+ Champion Circle
$25,000 - $49,999 President’s Club
$10,000 - $24,999 Advocate
$5,000 - $9,999 Steward
$2,500 - $4,999 Ambassador
$1,000 - $2,499 Supporter
Up to $1,000 Friend
Donate Now
The AAEM Foundation
AAEM was established in 1993 to promote fair and equitable practice environments necessary to allow emergency physicians to deliver the highest quality of patient care. AAEM later established the AAEM Foundation to defend the rights of such care and the emergency physicians who provide it.
Recently, AAEM-Physician Group, a subsidiary of the American Academy of Emergency Medicine (AAEM), filed suit in the Superior Court of California against Envision Healthcare Corporation to avoid a takeover of an emergency department contract that was held by and independent group. Issues at stake include lay influence over the patient-physician relationship, control of the fees charged, prohibited remuneration for referrals, and unfair restraint of the practice of a profession.
Our specialty is in crisis. We cannot let these practices continue here and across the country.
AAEM is the only EM organization that speaks and acts against the harmful influences of the corporate practice of medicine.
Our Goal: $2.5 million by 2025
Gifts in Honor and Gifts in Memory
Gifts at all levels can be given In Honor Of or In Memory Of a program director, mentor, and/or colleague.
Notification of gifts made In Honor or In Memory will be sent to the honoree or their family and listed in our Annual Report.
Ways to Give
• Donate Online
• Scan QR Code
• Employer Matching Gift
• Return the Donation/Pledge Form
• Planned Giving
The AAEM Foundation gratefully accepts IRA distributions, contributions through donor-advised funds, planned gifts and bequests.
ACMS-0718-026
aaem.org/donate/aaem-foundation The AAEM Foundation is a 501(c)(3) non-profit organization. EIN: 20-2080841 American Academy of Emergency Medicine Foundation 555 East Wells Street, Suite 1100, Milwaukee, WI 53202 (414) 276-7390 • (800) 884-2236 • Fax: (414) 276-7390 25% 50% 75%
COMMON SENSE MARCH/APRIL 2023 5
The Personalities in Your Resuscitation Room
Andrew Mayer, MD FAAEM
alking into your emergency department’s resuscitation area usually causes each of us to heighten our senses. We become hyper alert so we can determine what we will need to do in the next few minutes. Sometimes we know something about an incoming patient via an EMS report but often you simply hear that you are needed in “trauma.” Almost all emergency physicians start at least as adrenaline junkies. We walk towards the sickest patients with the anticipation of a procedure or an interesting diagnosis or intervention. We have learned to walk into the room and focus on the patient. We have that first glance assessment of the sights, sounds, and smells of our newest and sickest patient. This is what we do and most of us keep up an interest in seeing these patients. When you walk into this room, along with the newest and sickest patient is a diverse group of individuals who all have a unique role and perspective.
In this article, I ask you to look around your resuscitation room and try and put yourself into the other participants’ shoes and see the resuscitation from their perspective. I want you also to consider the many personalities, goals, and expectations of the other people in the room and consider each of their goals and objectives. I find that many of the issues which arise out of difficult resuscitations have little to do with the medicine but more to arise from each member of the teams’ expectations and perceptions of what did, or what they think, should, or could have happened.


Let’s look at a few of the people in the room and wonder what they are thinking. First, consider the EMS crew who brought the patient. They may have just spent the last 30 minutes dragging a very large patient down stairs in front of a screaming family knowing that what they were doing was hopeless. A seasoned paramedic usually knows what is going to happen and has an expected timeline and outcome. However, the brand-new crew member
Wwith little experience on the street may be sur prised and disappointed when the emergency physician or resuscitation team is not excited and ends a code quickly. This young and enthusiastic EMS team member may have an ticipated a heroic and lifesaving procedure on the asystole code and walks away upset. He or she may have expected a more noble effort with a TV ending.
Look at your charge nurses’ eyes when they follow EMS into the room. See his or her thoughts spinning as they consider how this patient’s arrival will impact the function of the department. They may be realizing that you just filled up their last trauma bay stretcher and another sick EMS patient is inbound. They may be wondering how long you are going to “play around” with this hopeless case or even worse regain ROSC when there are no ICU beds in the hospital. They need the room and the nurses to keep flow going. Their eyes may roll when they hear the “seventh epi is going in.” Remember we all have our own priorities and expectations with any given situation.
Think about the resuscitation room nurse. Typically, they are one of your best nurses who know how to get things done. However, in today’s world they could be an agency nurse you have never worked with before. You may have no rapport with the nurse and do not know their strengths and abilities. Can they juggle three drips? Remember that they are busy and will have to deal with the physical and emotional mess which you have help create from the bloody sheet to the crying widow. They have to complete all of the paperwork and sit with the family when you leave the room after the notification. They also realize that they have not given the lovenox, zosyn, or whatever to their other patient in the next bed. They may be thinking that their other patient actually has a reasonable chance of survival while they were helping you with the latest code from the local nursing home. Their thoughts could be focused on why EMS bothered to transport this patient
or why you did not call the code on arrival. They may also be thinking that one of your colleagues may be disappointed at how long it took them to accomplish some task placed for them in the electronic record while they were focusing on your patient.
Consider the new ED tech who has never seen a code and is eager to perform CPR for the first time. In their mind, the ED saves lives and they want to be part of the team. Their mind is racing forward to years from now after they finish nursing or medical school to when they can really have a more important role and start “saving lives” for themselves. It truly is delightful when you see the wonder in their young and impressionable eyes the first time they see a patient go into ventricular fibrillation in front of them. They are amazed when the patient jerks and wakes up groaning when the defibrillator goes off just like on their favorite
>> EDITOR’S MESSAGE
COMMON SENSE MARCH/APRIL 2023 6
I ask you to look around your resuscitation room and try and put yourself into the other participants’ shoes and see the resuscitation from their perspective.
medical television series. However, also peek at them when that decubitus ridden contracted nursing home patient rolls in and see them trying to understand modern medicine and the futility and waste of some of the things which we are required to do. Their minds are trying to rationalize some of their new experiences with their expectations. The conflict in their eyes can be dramatic and can change their career goals and dreams.
The police officer who arrived with the latest shooting victim may be the battle-hardened homicide detective or a rookie cop. The role they play is different and unique. They want evidence and victim statements while still trying to figure out if the patient laying on the stretcher is really a victim or an assailant. They can show real sympathy or think this is a hardened criminal who has finally gotten his just rewards for his criminal life.
Your consultants are a mixed lot of perspectives. I work in a community hospital which has some residents. This is different from the team of consultants at a big urban trauma or tertiary referral hospital which has every type of resident in house. I can see a tired middle-aged surgeon walking in at 2:00am thinking he is too old to be on call. He or she is thinking about the five elective cases they have scheduled in the morning and what the case laying in front of them is going to do to their day. They may be grumpy and in “survival mode.” This consultant may just be considering if they still have the stamina to get it all done. Their surly attitude usually has little to do with you or your team and more about where their head is related to the case. In contrast, you can have some senior resident walk in and want to show off his superior clinical prowess and power. They may spout off ridiculous statements related to the resuscitation to boost their ego and stake their role as a leader. The perspectives and attitudes are as varied as can be. You have to navigate these turbulent waters to keep the room in balance.
The emergency medicine resident has their own perspective walking into the room. They want the procedure. Being able to practice at the top of their skill set while having a staff to watch over them can be wonderful to watch. You see the growing confidence and you know that they are ready to be on their own. They can be the one that the room looks to for calm and order. It can also can be disheartening to me when as the staff, I ask a resident what they want to do when faced with a critically ill patient and their answer is to do what I think is best. They are unable to commit. The fear of being in charge has to be overcome in that resuscitation room and faculty has to be willing to give them enough autonomy to start making the tough decisions. If a resident cannot make this transition then they will always struggle in emergency medicine and when I see one of these residents in the resuscitation room I feel for the resident as I know their road will be difficult.
Then there is you. How do you feel and more importantly, how do you act in this room? Who knows what you will see when you walk through those doors and pull back the curtain. Remember, it could be anything and you have to appear to be ready to take on the challenge no matter the situation. The whole tone of the resuscitation will be dictated by your composure and cadence. Everyone in the room can sense fear or uncertainty. All emergency physicians learn this early. The captain of the ship needs to act like they know what they are doing and exude confidence or the whole experience can sour for all of the participants. Your personal armor has to shine so you can personify confidence and skill even if you are thinking to yourself that you have no idea what to do next. I am not saying that you cannot ask for help but you need to establish the rhythm and tone of the resuscitation. If your team senses anxiety, then they too will be anxious. If you project ability and confidence, then your team will follow your lead even when it is a hopeless situation. You will also need to be able to process this
more importantly, how do you act in this room?
stress for the sake of your own wellness. In the end, remember the poor housekeeper. You simply walk away from an especially messy, smelly, or bloody resuscitation. You have to go speak to the family and complete your chart. Some housekeeper who had nothing to do with the resuscitation or any knowledge of health care has to walk into the shambles which you have created and clean it up. They have to watch for dropped needles and the various bodily fluids which are on the stretcher and floor. Remember that they are the ones to mop up your bloody footprints. These staff members need our thanks and respect as they keep us going. Often, the next deathly ill patient rolls into this area before the floor dries and the whole things starts again.
There are others in the room who I have not discussed. Think about all of them. Remember that as the leader of the team you need to help all of these individuals process the events in the room and the role that they played. Any one of them can grow and mature from being a participant in an especially difficult or emotionally charged resuscitation. However, try to notice anyone who is struggling or seems upset after the event is over. A kind word of reassurance or understanding can make all of the difference to this struggling team member. Witnessing a young nurse transform into a rock-solid trauma nurse or a junior resident who shows leadership ability and who has just realized that they can be a leader in the room is gratifying to watch.

Then there is you. How do you feel and
COMMON SENSE MARCH/APRIL 2023 7
AAEM Foundation Contributors – Thank You!
AAEM established its Foundation for the purposes of (1) studying and providing education relating to the access and availability of emergency medical care and (2) defending the rights of patients to receive such care and emergency physicians to provide such care. The latter purpose may include providing financial support for litigation to further these objectives. The Foundation will limit financial support to cases involving physician practice rights and cases involving a broad public interest. Contributions to the Foundation are tax deductible.
Levels of recognition to those who donate to the AAEM Foundation have been established. The information below includes a list of the different levels of contributions. The Foundation would like to thank the individuals below who contributed from 1/1/2023 to 2/28/2023
Contributions $1000
and above
David W. Lawhorn, MD MAAEM
Jonathan S. Jones, MD FAAEM
Thomas R. Tobin, MD MBA FAAEM
Contributions $500-$999
Fred Earl Kency, Jr., MD FAAEM
Ronald T. Genova, MD
Contributions $250-$499
David Thomas Williams, MD FAAEM
Eric D. Lucas, MD FAAEM
Floyd W. Hartsell, MD FAAEM
Jeffrey J. Thompson, MD FAAEM
Kenneth Scott Hickey, MD FAAEM FACEP
Ming-Jay Jeffrey Wu, MD FAAEM
Nayla M. Delgado Torres, FAAEM
Piotr Jurgielewicz, MD
Contributions $100-$249
Alexander Tsukerman, FAAEM
Andrew Thomas Larkin, DO FAAEM
Ann Loudermilk, MD FAAEM
Arnold Feltoon, MD FAAEM
Barry N. Heller, MD FAAEM
Brian J. Browne, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Bruce E. Lohman, MD FAAEM
Catherine V. Perry, MD FAAEM
D. Scott Moore, MS DO FAAEM
David Wang, MD FAAEM
Donald L. Slack, MD FAAEM
Gary M. Gaddis, MD PhD MAAEM
FAAEM FIFEM
H. Samuel Ko, MD MBA FAAEM
Jason M. Driggs, MD FAAEM
Jeffrey A. Rey, MD FAAEM
Jenna Otter, MD FAAEM
Jessica Moore, MD
Kathleen Hayward, MD FAAEM
Katrina Green, MD FAAEM
Marc D. Squillante, DO FAAEM
Nancy Conroy, MD FAAEM
Neeharika Bhatnagar, MD FAAEM
Paul W. Gabriel, MD FAAEM
Renee Marie Nilan, MD FAAEM
Robert Boyd Tober, MD FAAEM
Roland S. Waguespack III, MD MBA
FAAEM
Sameer D. Mistry, MD CPE FAAEM
Timothy J. Durkin, DO FAAEM CAQSM
William E. Franklin, DO MBA FAAEM
Yeshvant Talati, MD
AAEM PAC Contributors – Thank You!
Contributions up to $99
Alexander J. Yeats, Jr., MD FAAEM
Alexander S. Maybury, MD FAAEM
Benson Yeh, MD FAAEM
David C. Crutchfield, MD FAAEM
Edward T. Grove, MD FAAEM MSPH
Ernest H. Leber Jr., MD FAAEM
Erol Kohli, MD MPH FAAEM
Jason J. Morris, DO FAAEM
Joanne Williams, MD MAAEM FAAEM
Kelly Dougherty, MD
Kenneth T. Larsen, Jr., MD FAAEM
Kevin C. Reed, MD FAAEM
Linda Sanders, MD FAAEM
Marianne Haughey, MD FAAEM
Michael Lajeunesse, MD
Peter H. Hibberd, MD FACEP FAAEM
Peter M.C. DeBlieux, MD FAAEM
AAEM PAC is the political action committee of the American Academy of Emergency Medicine. Through AAEM PAC, the Academy is able to support legislation and effect change on behalf of its members and with consideration to their unique concerns. Our dedicated efforts will help to improve the overall quality of health care in our country and to improve the lot of all emergency physicians.
All contributions are voluntary and the suggested amount of contribution is only a suggestion. The amount given by the contributor, or the refusal to give, will not benefit or disadvantage the person being solicited.
Levels of recognition to those who donate to the AAEM PAC have been established. The information below includes a list of the different levels of contributions. The PAC would like to thank the individuals below who contributed from 1/1/2023 to 2/28/2023
Contributions $500-$999
Mark S. Penner, DO FAAEM
Ronald T. Genova, MD
Contributions $250-$499
Fred Earl Kency, Jr., MD FAAEM
Joseph T. Bleier, MD FAAEM
Michael L. Martino, MD FAAEM
Paul W. Gabriel, MD FAAEM
Thomas B. Ramirez, MD FAAEM
Contributions $100-$249
Alexander S. Maybury, MD FAAEM
Alexander Tsukerman, FAAEM
Brian R. Potts, MD MBA FAAEM
Bruce E. Lohman, MD FAAEM
Catherine V. Perry, MD FAAEM
David W. Lawhorn, MD MAAEM
Donald L. Slack, MD FAAEM
Garrett Sterling, MD FAAEM
Gary M. Gaddis, MD PhD MAAEM FAAEM FIFEM
Jeffrey A. Rey, MD FAAEM
Jeffrey J. Thompson, MD FAAEM
Katrina Green, MD FAAEM
R. Lee Chilton III, MD FAAEM
Robert Boyd Tober, MD FAAEM
Robert M. Esposito, DO FAAEM
William E. Franklin, DO MBA FAAEM
LEAD-EM Contributors – Thank You!
Contributions $1000 and above
Jonathan S. Jones, MD FAAEM
Contributions $500-$999
Fred Earl Kency, Jr., MD FAAEM
Contributions up to $99
Alex Kaplan, MD FAAEM
Erol Kohli, MD MPH FAAEM
Jason J. Morris, DO FAAEM
Kevin C. Reed, MD FAAEM
Linda Sanders, MD FAAEM
Marc D. Squillante, DO FAAEM
Peter H. Hibberd, MD FACEP FAAEM
The AAEM Institute for Leadership, Education & Advancement in the Development of Emergency Medicine, Inc. (LEAD-EM) was established after the tragic and unexpected death of AAEM president, Dr. Kevin G. Rodgers.
The Kevin G. Rodgers Fund and the Institute will LEAD-EM just like Dr. Rodgers did. The funds will support important projects such as development of leadership qualities, and clinical and operational knowledge of emergency physicians with a view toward improving and advancing the quality of medical care in emergency medicine, and public health, safety and well-being overall. LEAD-EM would like to thank the individuals below who contributed from 1/1/2023 to 2/28/2023
Contributions $250-$499
Dale S. Birenbaum, MD FAAEM
David W. Lawhorn, MD MAAEM
Mary Ann H. Trephan, MD FAAEM
Contributions $100-$249
Alexander S. Maybury, MD FAAEM
Ann Loudermilk, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Catherine V. Perry, MD FAAEM
Christopher Kang, MD FAAEM
Edward T. Grove, MD FAAEM MSPH
Gary M. Gaddis, MD PhD MAAEM FAAEM FIFEM
Kathleen Hayward, MD FAAEM
Kevin C. Reed, MD FAAEM
Paul W. Gabriel, MD FAAEM
Roland S. Waguespack III, MD MBA FAAEM
Contributions up to $99
Alicia J. Starr, DO
Erol Kohli, MD MPH FAAEM
Marc D. Squillante, DO FAAEM
COMMON SENSE MARCH/APRIL 2023 8
Pavitra P. Krishnamani, MD MS

Ayoung African-American woman barely thirty years of age walked into our emergency department one day. She appeared anxious, wincing while touching small lumps that had developed across her neck in the week before. She had a son, a long-term boyfriend, and a dream to build a family with them both in the future. But today, she was worried. What if she was truly ill? she had wondered to herself. WebMD had said the tender lumps in her neck could be from the common cold, but they could also be cancer. What’s more, her boyfriend had been losing so much weight lately—what if they were both ill? she feared.
The woman’s anxiety was palpable in the waiting room and it was perhaps the first thing I noticed about her as she silently stared off into the distance through her heavy-framed eyeglasses, lost in her own thoughts amidst of the chaos that surrounded her. I pulled her into a temporary exam room to talk more.
“Hi there Ms. Matthews, so nice to meet you. I’m Dr. Pavitra and I’ll be taking care of you today,” I said, introducing myself to the portly woman who sat across from me.
“Pleased to meet you as well, please call me Lina,” she offered. She was oddly silent, both wanting to seek help but reluctant to describe why or how. After some time and several questions, Lina expressed her worries and the circumstances that bothered her. “I just noticed this past week some of these tender little lumps on my neck,” she started, “and I don’t know, I’ve just been so achy and tired all week. I wake up with these hot flashes and my last period was just a week ago. There’s no way I’m pregnant and I’m too young for menopausal.” She fell silent once more. “Have you lost any weight recently or had any fevers?” I asked. “No, I’m right about where I have been with my weight, but my boyfriend…” she paused. “He has. I, I don’t know,” she stuttered, “He’s been acting somewhat strange recently. I don’t know what it is, but he’s more reserved, he just doesn’t seem as interested in me anymore, and he’s been losing a ton of weight for months now. I’m worried about him, but also worried about me and I just don’t know who I should be more worried about. And what if we’re both sick—what if my son just grows up with two sick parents…or worse, with none at all?”
“I see.” In front of me, I saw a woman who looked as if the weight of the world was on her shoulders, and recognized in her the struggle that many women have prioritizing their health above all else. It was the first of many times in my career I’d use the sentence I said next. “That’s a lot to worry about, but the good news is you’re here now and my job is to
shoulder some of those worries for you. Let’s work together to try and figure out if there’s something worth worrying about right here with your health first and then we can make a plan to tackle what we find out, okay?”
Lina looked somewhat relieved. “Yes, sure. You had asked about fevers,” she reminded me, “I haven’t had any, but I just feel awful. It’s like having the flu, but somehow worse.”
Lina had no recent travel or trips precipitating her symptoms. She had no family history or personal history of cancer or autoimmune diseases. When I asked Lina about her sexual history, I learned that she was monogamous with her boyfriend and was hoping that the two of them would be taking the next step in their relationship before he had started becoming aloof and secretive. They hadn’t used barrier protection in a long time because she trusted him, and she was adamant that he was monogamous with her as well. He was such a great role model for her son, she noted, and such a good partner too. Her facial features noticeably softened when talking about the two of them and the dreams she had to add more children to the family they’d make soon.
Along with some basic lab work, which came back normal, I tested her for infectious diseases. Her respiratory panel and flu tests were negative. Her sexually transmitted infection testing was positive for HIV. I stared at the result and refreshed the page a few times before confirming with Lina’s nurse that the sample sent was indeed hers. This, I knew would be a difficult discussion to have.
HIV is no longer the near-death sentence it was in the United States during the AIDS epidemic in the 1980s. Advances in pharmacology and prevention have allowed for those struggling with the illness to live long lives with undetectable viral loads. However, controlling the illness is not
HEART OF A DOCTOR Trust
>>
COMMON SENSE MARCH/APRIL 2023 9
[C]ontrolling the illness is not necessarily a cure and, having HIV is life changing for most individuals who contract it, particularly from partners who they had trusted to be monogamous.
necessarily a cure and, having HIV is life changing for most individuals who contract it, particularly from partners who they had trusted to be monogamous.
Though HIV prevention campaigns around the world originally included monogamy as a core tenet of their message, studies as early as 2008 showed that cultural factors play a large role in the success of monogamy as a preventive measure. One such study showed that lifetime monogamous women in Tanzania were still at high risk for HIV infection because such monogamy was limited to women, but not their partners. The study concluded that efforts to empower sexually active women with tools to protect themselves against contracting HIV would be important to prioritize alongside efforts in partner reduction.1 A qualitative study conducted around the same time in India showed that many women feared or felt unable to negotiate safe sex practices or barrier protection use with their partners, even when in a monogamous relationship.2
The United States is not immune to these factors, with a 2016 study showing that approximately a fifth of participants felt that a partner might not listen if asked to use barrier protection.3 Published around the same time, a qualitative study examining the high prevalence of HIV/AIDS in middle socioeconomic status African American women in the United States found that gendered relationship dynamics and trust levels in relationships may reduce some women’s ability to negotiate monogamy and condom use with male partners.4
Lina had found herself in a similar predicament: in believing her partner was monogamous and trustworthy, she hadn’t felt it necessary or comfortable to ask to use barrier protection. After all, this was a man she saw herself marrying—a man she believed would become a father figure to her son. As I pulled Lina back into the temporary patient evaluation room, I faltered. How was I going to deliver this news that may make her feel as though she been misled?
Once she settled into the room, she turned to me, “Anything?” she asked.
“Lina, your lab tests mostly looked alright, but there was one that was concerning. I know you had allowed us to screen you for sexually transmitted illnesses today and, unfortunately, your HIV test came back positive.” The room was so silent a pin drop would have resonated throughout it.
“Oh, I see.” Lina was visible shaken.
“The good news is, your symptoms are really those that people may experience early on in the illness and there have been so many advances that can allow folks with HIV to live normal full lives. I can connect you with our clinics and other resources to help you along this journey.”
Lina looked off into the distance once more, clearly troubled by the news. “So then, my boyfriend…” she started as she had a moment of realization. “He’s not on any medications that I know of. Oh my goodness,
his weight loss. Do you think it could be because of HIV or AIDS?” she turned to me and asked.
I held my breath, proceeding carefully. “I really wouldn’t be able to say since I haven’t examined him myself, but it may make sense for him to see his primary care doctor and discuss the possibility.”
“That son of a b**** probably already knows—he’s been so reserved for months. And I was worried about him. Did you know, he said he had seen a doctor about his weight loss and they said there was nothing wrong…”
“Oh, they had?” I was quickly interrupted.
“No. That’s what he told me. How could he lie to me about something like this. Something that changes everything???” Lina was appropriately distraught, and I walked over the cabinets to bring her a tissue. “I mean, my life…my whole life. I have had two relationships—my ex and him, and I was thinking about giving him children. Something like this, it affects me. And now, it could affect all of my future relationships and affect my future children. How can a partner just betray someone like that?” She looked shattered, wiping away her tears with tissue box in hand.
“I’m so sorry to have had to give you this news today.”
“You know what? I just want to go home. I just want to be with my son. And I never want to see him again. I’m just exhausted. I’m so tired. I want to go home.” Lina looked defeated, having mentally cycled through the seven stages of grief in a span of minutes.
“Okay, we can work on getting you home, but I want to make sure we have a plan together to get you through this too.”
“Get me through what? I have HIV. I have to live with HIV for the rest of my life. How does it matter if I get treated or not? It’s never going away.”
I pulled closer to Lina and held her hand. “You have a son,” I said, “who loves you and looks up to you, and needs you. And you have a life, a whole life ahead of you whether it’s with your boyfriend or not. You’re right in that HIV doesn’t really ever go away, but that doesn’t mean it has to kill you.”
“He betrayed me,” Lina said.
“Even if he did, are you willing to let what happened kill you?”
“But, how did I miss it? How did I misjudge him?” Lina asked the question that so many of us ask when we’ve feel cheated or lost in a relationship.
I took a deep breath. “Lina, I know I’ve only gotten to know you for a few minutes here, but in my experience, people are a bit too hard on themselves for misjudging someone. Most people have pulled together the whole set of experiences they’ve had with someone and formed an informed opinion of them. I’m sure you did the same. This isn’t your fault. It may now be your responsibility, but we are all here to help, okay?” Lina nodded and later left the emergency department with an outpatient appointment at a local HIV clinic. She was the youngest patient I had ever
Countinued on page 25 >>
HEART OF A DOCTOR
COMMON SENSE MARCH/APRIL 2023 10
Dear AAEM Member,
Enclosed are the candidate statements for the 2023 AAEM Board of Directors Election.
As you are aware, the call for nominations was sent to all voting members. Those AAEM members who appear on the enclosed ballot have indicated their willingness to serve on the AAEM board.
Statements from each of the candidates full listing of previous board service and awards as well as AAEM activities dating back five years (2018 and on) are on the following pages. Please review the enclosed information, then exercise your democratic right to vote for the representatives you would like to see serve as AAEM’s leaders. You can also view pre-recorded videos of each candidate online at aaem.org/about-us/leadership/ elections/candidate-statements or by scanning the QR code below. Remember, we have a one member, one vote system, so your voice counts. Please follow these instructions for casting your ballot in the 2023 election.
If You Will Attend the Scientific Assembly:
• We recommend that you do not complete your official ballot at this time. There will be a Candidates’ Forum held during the Scientific Assembly on Sunday, April 23, 2023, 5:30pm-6:30pm CST, where you can hear the candidates respond to direct questions from the voting membership. You will be asked to submit your ballot online at the conclusion of the Forum.
• If certain of your choices or unsure if you will attend the Forum, you may vote online at aaem.org/ elections. Voting will remain open until April 23, 2023 at 11:59pm CST.
If You Are Unable to Attend the Scientific Assembly:
• You may complete your official ballot online at aaem.org/elections. Online voting will remain open until April 23, 2023 at 11:59pm CST.
Balloting Procedure for 2023:
• Voting ballots will only be available online. Please visit aaem.org/elections to cast your vote electronically.

Thank you for your continued support of AAEM. Please call (800) 884-2236 with any questions you may have regarding the election procedure.
Sincerely,
Missy Zagroba, CAE Executive Director
PLATFORM STATEMENTS
COMMON SENSE MARCH/APRIL 2023 2023 11
Heidi Best, MD FAAEM
CANDIDATE FOR AT-LARGE BOARD MEMBER
Current Role/Employer: President, Emergency Physicians of Tidewater
Clinical EM Practice Employment Type: 75/25 academic/community
Clinical Hours in the ED per Month: 65
Nominated/Endorsed by: Bruce M. Lo, MD MBA RDMS FAAEM, Robert M. McNamara, MD MAAEM FAAEM, and Mark Reiter, MD MBA MAAEM FAAEM
Additional Leadership Roles: Chair, Emergency Medicine Business Coalition
Membership: 2005, 2021-2024
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
Capital Region (CR/AAEM) Chapter Division Member
AAEM Emergency Medicine Workforce Committee Member

WIEM-AAEM Section Member
Candidate Statement for At-Large Board Member
As the president of an independent democratic EM group, the importance of advocacy for our specialty and within our specialty is greater now than ever before. In the past five years as president of Emergency Physicians of Tidewater, I have modernized our practice, brought in valuable new administrative talent, and solidified camaraderie that had been waning just before my inauguration.
There are multiple threats to EM that AAEM is well suited to tackle. I have a solid understanding of the financial threats to EM, which includes payors using surprise billing legislation to tank reimbursement. Government payors (like that in my state of Virginia) are joining in by utilizing automatic chart downcodes despite the clear violation of the prudent layperson standard. Corporatization of EM and of medicine in general has contributed to burnout amongst physicians. As community faculty for the EM residents at Eastern Virginia Medical School, the importance of educating our upcoming leaders in the non-clinical side of Emergency Medicine is ever-growing.
My commitment to non-corporate physician practice extends beyond my own group as I fulfill my new role as the Chair of the Emergency Medicine Business Coalition. During the past two years as Chair-elect on the EMBC Board, I sought out ways to support independent physician EM groups in the current market. As an AAEM Board member, I would be able to expand AAEM’s reach to physicians and physician groups like my own.
I am encouraged by the work that AAEM is doing and am proud to continue to support the organization.
PLATFORM
STATEMENTS
COMMON SENSE MARCH/APRIL 2023 12
Laura J. Bontempo, MD MEd FAAEM

CANDIDATE FOR AT-LARGE BOARD MEMBER
Current Role/Employer: Faculty Development, University of Maryland
Clinical EM Practice Employment Type: Academic, urban, tertiary care, level 1 trauma center
Clinical Hours in the ED per Month: 80
Nominated/Endorsed by: Self-nomination
Additional Leadership Roles: N/A
Membership: 2003-2023
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
Education Committee
Scientific Assembly Planning Subcommittee Co-Chair
Breve Dulce Subcommittee Chair
Written Board Comprehensive Review Work Group Vice Lead
Scientific Assembly Planning Work Group Member
Breve Dulce Subcommittee Member
Scientific Assembly Speaker
Candidate Statement for At-Large Board Member
Written Board Review Course Speaker
Scientific Assembly Abstract Reviewer
WiEM-AAEM Section Member
Oral Board Review Course Examiner
Medical Student Ambassador Mentor
Speaker Development Group Mentor
Since my first contact with AAEM, I have been impressed by the educational offerings, advocacy, and, most importantly, the members with whom I have interacted.
As an At-Large Board Member, I will work to help AAEM maintain its relevance by reaching out to, and actively recruiting, residents and new residency graduates practicing in both academic and community settings. Advocating for members of these groups to join committees and workgroups and to participate in AAEM's educational offerings is an opportunity for continued growth within the Academy. A second, equally important, motivation for my candidacy is to maintain AAEM as a leader in EM education while working to extend high quality, relevant learning opportunities to all its members. After presenting a track talk at the Scientific Assembly in 2015, I became a member of the Scientific Assembly Planning Sub-Committee then a member of the Breve Dulce Work Group. Through my ongoing involvement, I became Chair of the Breve Dulce Work Group and then served as Cochair of the Scientific Assembly Planning Committee. I, along with my co-chairs, shepherded the AAEM Scientific Assembly through the turbulent years of the COVID pandemic with social distancing precautions and travel restrictions. This was a major challenge, however, both in-person and virtual attendees were able to enjoy the Scientific Assembly in St. Louis in 2021 and in Baltimore in 2022.
In 2015, I taught at the AAEM Written Board Review Course and subsequently advanced to become Vice-Chair of the work group, with the anticipated pathway of becoming the Chair. Through my participation, I was honored to receive the AAEM Written Board Review Course Top Speaker Award in 2020. I am an active member of the AAEM Education Committee, an AAEM Oral Board Examiner, a Mentor for the Medical Student Ambassador Program and a member of the Women in EM Section. Additionally, I have represented AAEM to the American Association of Otolaryngology in a guideline development group.
My background includes medical school then residency at Northwestern University. Thereafter, I was the Associate Program Director for the Harvard Affiliated Emergency Medicine Residency Program then the Program Director for the Yale-New Haven Hospital Emergency Medicine Residency Program. Currently I am an Associate Professor at the University of Maryland where I have developed educational programs for medical students and EM residents while also working in faculty development. I am passionate about EM education at all levels—student, resident, and practicing physicians.
Thank you for considering my candidacy. It will be an honor to represent you as a member of your AAEM Board of Directors.
PLATFORM STATEMENTS
COMMON SENSE MARCH/APRIL 2023 2023 13
PLATFORM STATEMENTS
Kimberly M. Brown, MD MPH FAAEM CANDIDATE FOR AT-LARGE BOARD MEMBER

Current Role/Employer: Brown EMP, PLLC (Locums)
Clinical EM Practice Employment Type: Locum Tenens/Community Practice
Clinical Hours in the ED per Month: 120
Nominated/Endorsed by: Liza Chopra, MD FAAEM, A. Antoine Kazzi, MD MAAEM FAAEM, Vicki Norton, MD FAAEM, and Joanne Williams, MD MAAEM FAAEM
Additional Leadership Roles: N/A
Membership: 2013-2023
Board Meeting Participation: 100%
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
AAEM Board of Directors
AAEM Foundation Board of Directors
AAEM LEAD-EM Board of Directors
Aging Well in Emergency Medicine Interest Group Board Liaison
Geriatric Committee Board Liaison
International Committee Board Liaison
The Ruby: Gender Diversity WiEM Award
Breve Dulce Work Group Member
Education Committee Member
Tennessee Chapter Division Member
Candidate Statement for At-Large Board Member
CCMS-AAEM Section Member
EUSS-AAEM Section Member
JEDI-AAEM Section and Work Group Lead
WiEM-AAEM Section Member
YPS-AAEM Section Member
Oral Board Review Course Examiner
MEMC Abstract Reviewer
Scientific Assembly Abstract Reviewer
Common Sense Author
JEDI-AAEM Inclusion Initiative Podcast Host
Thank you for your consideration and I would be honored to continue my board and organizational service as a Member at Large. During my brief service on the board, I have dedicated my time to serving on the Leadership Taskforce, revamping our Leadership Academy curriculum and experience. In addition to serving on the board, I also serve the Academy as a Virtual Oral Board Examiner, a judge for student presentations during Scientific Assembly, and as an active member of the Women in EM, Young Physicians, and JEDI sections. I host of JEDI’s new podcast, the Inclusion Initiative, featuring conversations with members about their lives, careers and passion for the mission of AAEM.
My continued devotion to AAEM comes from the relationships that I have made with you, the incredible members of this organization. I can always find a mentor, sponsor, or new connection within this dynamic organization. It is the passion of past-presidents, current and past section and committee leaders, residents, and medical students that encourages me to say yes to leadership.
I am excited to continue to bring my passion for emergency medicine and people to the board of the American Academy of Emergency Medicine. I am committed to continuing to work with the board and the membership to continue the Academy's mission. I believe that my leadership skills, strategic thinking, and passion for emergency medicine will make a valuable contribution to the board and the organization as a whole.
COMMON SENSE MARCH/APRIL 2023 14
Frank Christopher, MD FAAEM CANDIDATE FOR AT-LARGE BOARD MEMBER

Current Role/Employer: President/Locums Emergency Medicine Physician, Lugnut Medical Services PLLC
Clinical EM Practice Employment Type: Locums EM work at a variety of small facilities across North Carolina; concomitantly serve as Medical Director & Associate Professor at Pfeiffer University's Masters in Physician Assistant Studies program
Clinical Hours in the ED per Month: 72
Nominated/Endorsed by: Robert A. Frolichstein, MD FAAEM, David A. Farcy, MD MAAEM FAAEM FCCM, and Robert M. McNamara, MD MAAEM FAAEM
Additional Leadership Roles: N/A
Membership: 1999-2023
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
Joe Lex Educator of the Year Award Winner
Mitchell Goldman Service Award Winner
Oral Board Review Course National Course Director
Oral Board Review Course Vice Chair
Oral Board Review Course Regional Course Director (Orlando)
Oral Board Review Course Examiner
Candidate Statement for At-Large Board Member
Education Committee Member
Membership Committee Member
Scientific Assembly Moderator
Leadership Academy Participant
Common Sense Author
Dr. Bob McNamara came to my (military) PGY 2-4 residency program nearly 25 years ago and gave an inspiring talk to the faculty and residents, educating us on how the Academy was formed, what the Academy stands for, and why it was important for us to understand the economics, workforce, and potential of EM as a specialty. Immediately, our program became a 100% faculty and resident member program and I have remained engaged with the Academy ever since.
I am running for an AAEM Board At-Large position to continue to share this message, help drive change, and shape the work of our Academy to benefit our specialty and patients.
The future of our specialty is our colleagues. I am committed to growing AAEM membership and continuing to provide high quality continuing medical education to help the future generation of EM physicians proudly and confidently achieve and maintain board certification and professional excellence. After twenty plus years in the active Army, including administrative, operational, clinical, and command assignments both overseas and in the U.S., I retired as a Colonel and joined an independent democratic group. For a few years, I was one of the group’s recruiters and had the opportunity to review the CVs of potential colleagues both coming out of residency and from other practice environments. I usually skipped over the meat of the CV and looked immediately at the listed professional organization memberships. Far more often than not, AAEM was not listed. When I asked why, the responses frequently amazed me, and I learned that there is much work yet to accomplish.
When you get back to the roots of our founding, as Dr. McNamara told my residency program, you start with the WHY of the Academy. At a recent Membership Committee meeting, it was discussed that AAEM was largely considered “the advocacy society.” I take this as a compliment, as it nests within the Academy’s mission statement and our motto “Champion of the Emergency Physician.”
I’ve had the privilege of spending many years teaching the Oral Board Review Course and have used that platform to talk with new colleagues about the educational, legislative, policy, and personal growth and leadership opportunities the Academy provides to its members. The expansion of the Academy to include the Physician Group, Locums Group, various Chapter Divisions, Sections, Interest Groups, and Committee structures enable members to get inspired and work together to impact change and ultimately ensure the highest quality of care for our patients.
The Board serves the Academy via its bedrock—our members. We are only as strong as our collective voices. Less than 10% of the residency-trained, board-certified EM workforce are members of the Academy. If we can continue to look at the tenets of our founding, be the advocate, the Champion, we can serve that EM workforce even more robustly. I look forward to the opportunity to serve the Academy and its members to expand membership, enhance our role, and set a course for a strong future for our specialty.
PLATFORM STATEMENTS
COMMON SENSE MARCH/APRIL 2023 2023 15
PLATFORM STATEMENTS
Kevin Reed, MD FAAEM

CANDIDATE FOR AT-LARGE BOARD MEMBER
Current Role/Employer: Vice Chief, Department of Emergency Medicine, MedStar Georgetown University Hospital
Clinical EM Practice Employment Type: Emergency Medicine attending at a busy, urban, tertiary care hospital in Washington, D.C. Primary teaching site for 3-year Emergency Medicine Residency (30 total residents) and primary site for Georgetown Medical Students required EM clerkship.
Clinical Hours in the ED per Month: 80
Nominated/Endorsed by: William T. Durkin, Jr., MD MBA MAAEM FAAEM and Robert M McNamara, MD MAAEM FAAEM
Additional Leadership Roles: N/A
Membership: 2002-2022
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
Joe Lex Educator of the Year Award Winner
Education Committee Chair
Speaker Development Group Chair
Scientific Assembly Planning Work Group Advisor
Scientific Assembly Planning Work Group Member
Candidate Statement for At-Large Board Member
Education Committee Member
Scientific Assembly Speaker
Medical Student Ambassador Mentor
Written Board Comprehensive Review Committee
Leadership Academy Participant
I joined the Academy in 2002, shortly after completing an Emergency Medicine residency at the University of Maryland Medical System, excited about the opportunity to become part of an organization that shared many common values and ideals. In 2004, I was honored to become a Fellow of the Academy.
For over 15 years, it has been my privilege to work with truly outstanding educators across the country as a member of the Education Committee. In addition to helping plan many of AAEM’s incredible educational offerings, my particular focus has been on programming for the annual Scientific Assembly and helping to create the one-of-a-kind Speaker Development Group. I have enjoyed the opportunity to serve as both Vice-Chair and then Chair of the Education Committee. I was truly honored to be selected for the AAEM Joe Lex Educator of the Year Award in 2017.
Over the past 10 years, I have held multiple leadership roles within MedStar Health, a large, 10 hospital system in the Mid-Atlantic region. This includes serving as Vice-Chair and Chair at three very busy, high acuity Emergency Departments. These roles have provided me with the opportunity to better understand the multi-faceted challenges facing emergency medicine physicians on a daily basis. With ongoing effects from the COVID-19 pandemic, a rapidly changing work-force environment and a shortage of qualified clinical support staff, the challenges our specialty faces have never been greater.
I believe in the academy’s commitment to its members and to promoting an environment in which we as emergency medicine physicians can provide the highest quality care. I hope to apply a unique perspective gathered from over 20 years of clinical, educational, and administrative experience to help further advance the academy and serve you, its members and most vital asset, over the next three years. If elected, I promise to work with the AAEM Board to further advance our shared vision and goals. I will continue to advocate for the personal and professional well-being of every member, support our high quality continuing medical education offerings and provide ongoing support to international EM programs and societies.
I appreciate your consideration and look forward to speaking with many of you at the upcoming Candidates’ Forum at the Scientific Assembly in New Orleans.
COMMON SENSE MARCH/APRIL 2023 16
Scott Rineer, MD MPH FAAEM CANDIDATE FOR AT-LARGE BOARD MEMBER

Current Role/Employer: American Physician Partners (APP)
Clinical EM Practice Employment Type: Community based working for staffing company
Clinical Hours in the ED per Month: 120
Nominated/Endorsed by: Mark Reiter, MD MBA MAAEM FAAEM, Kevin Beier, MD FAAEM, and William T. Durkin, Jr., MD
MBA MAAEM FAAEM
Additional Leadership Roles: N/A
Membership: 1998-2025
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
Oral Board Review Course Examiner
Candidate Statement for At-Large Board Member
Greetings! My name is Scott Kain Rineer and I am a Tampa Bay emergency physician who has worked in a variety of settings. I remain passionate about our great specialty; past, present, and future. Please accept my apologies for not being able to attend New Orleans and yet another fantastic Scientific Assembly for the AAEM.
Over the past 30 years I have worked in large and small; military and civilian; academic and community settings. My employers have been small independent groups and large National contract organizations. What ties all of these together is our patients who rely on our joint abilities for take care of anyone, anytime, anywhere. Changes in our specialty have accelerated rapidly increased influence from Private Equity. Our specialty organization has been and continues to be on the front lines. I am honored to have been an active member for all into three decades, and it has been apparent to me that it is well past time to pay it forward and take my experiences to the board as an active, contributing member. Hope to convince you in my absence for my vote for AAEM At-Large Board of Director.
My personal tipping point has been in receiving a termination for cause three days before Christmas 2022 by a large National Contract group. To date, I have not been told the reason! I have retained counsel for my claim of wrongful termination and lack of due process; Regret that I am unable to share more at this time, but for clear reasons this is not possible.
As background, I graduated from the Uniformed Services University of the Health Sciences (USUHS) F. Edward Hebert School of Medicine in 1990; Operation 'Deep Freeze,’ Antarctica; earning the USN/USMC parachutist designation and Expeditionary Field Medical Badge (EFMB) were side benefits. Naval Hospital San Diego (NHSD) transitional internship (90-91) then preceded my time as assigned General Medical Officer and Flight Surgeon serving many world-wide deployments. Post-graduate Emergency Medicine residency at the Naval Medical Center San Diego (NMCSD) (5-98) included tactical emergency medicine; urban search and rescue teams (CA USAR TF-8); the USMC Chemical Biological Response Force (CBIRF) and serving as EMS medical director and EMT director at Camp Pendleton. After joining the reserves and serving as a Commanding Officer, I was mobilized back to active duty as Force Surgeon, US Marine Corps Forces Central Command.
Post-graduation Masters in Public Health (MPH) in Disaster Management and Humanitarian Assistance was followed by Aerospace Medicine Residency; completion of the USAF Critical Care Air Transport Team (CCAT) training and additional aeromedical training prior to reporting as the Senior Medical Officer aboard the USS Ronald Reagan (CVN-76).
As a Fellow of the American Academy of Emergency Medicine, who has years ago dropped being a Fellow, American Academy of Emergency Physicians, I am hopeful that these two professional organizations will continue to opine together on the needs of our members, specialty and most importance, our patients.
PLATFORM STATEMENTS
COMMON SENSE MARCH/APRIL 2023 2023 17
PLATFORM STATEMENTS
Anthony Rosania, MD FAAEM CANDIDATE FOR AT-LARGE BOARD MEMBER

Current Role/Employer: Vice-Chair for Clinical Operations, Associate Professor of Emergency Medicine and Medical Director for ED Observation, Rutgers - New Jersey Medical School.
Clinical EM Practice Employment Type: University employed, emergency physician and clinical informaticists at an academic medical center practicing in a public, urban, safety-net hospital.
Clinical Hours in the ED per Month: 48
Nominated/Endorsed by: Lewis S. Nelson, MD FAAEM
Additional Leadership Roles: Chair-Elect of ACEP Observation Medicine Section
Membership: 2018-2024
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
Delaware Valley Chapter Division Member
New York Chapter Division Member
Government and National Affairs Committee Vice Chair
Operations Management Committee Vice Chair
Observation Medicine Interest Group Chair
Leadership Academy Participant
Candidate Statement for At-Large Board Member
Medical Student Ambassador Mentor
CCMS-AAEM Section Member
JEDI-AAEM Section Member
WiEM-AAEM Section Member
Common Sense Author
I am honored to accept this nomination for a board of director position in the Academy. Since joining AAEM, I have been continually impressed by the mission and culture of the institution and its people. Emergency medicine relies upon relationships and communication. And more than any other professional society I am a member of, the members of AAEM are a family of people with whom I've been happy to have built relationships. From my very first days in the academy, I have felt welcomed, supported, mentored, and cared for. From members to presidents, in the Academy there is a sense of family and equality, and it is that culture, and a commitment to championing the cause of emergency medicine physicians and our patients, that makes our organization so great.
Since joining, I have been honored to be able to stand up the Observation Interest Group, which we recently brought under the umbrella of the Operations Management Committee. I most recently served as Vice-Chair of the Operations Management Committee and the Government and National Affairs Committee. As part of those responsibilities, I've been a regular contributor to Common Sense and working with the committee for PPH/Staffing ratios. At Scientific Assembly, I have made it a point to mentor students and to network with outstanding members of our organization. Most recently I have engaged my local program's leadership to support a larger presence from New Jersey Medical School at the AAEM Scientific Assembly.
The Academy stands for emergency physicians. We also stand for our patients. Moreover, we stand for the simple act of taking a stance. And at every turn, our stance has proven to be the correct one—for our specialty, our partners, and our patients. Health systems, and our other societies, have been forced to admit the “correctness” of that stance. Whether it be related to private equity, restrictive covenants, the importance of physician led teams, or the use of learners as a labor source—the AAEM has stood for clarity and common sense.
I believe that scope of practice and workforce issues, two of our most looming crises, go together. The commoditization of emergency medicine is a major threat to us, and the safety of our patients. I work with and supervise nurse practitioners, and there is a place for them on the emergency medicine team—a team that must be led and managed by a board-certified or board-eligible emergency physician. Moreover, we, emergency physicians, and no one else, must be the ones to decide how many team members we can supervise safely. If chosen for the board, I would focus part of my energy on addressing these pressing issues. More broadly, I would commit to doing what we do best in AAEM: being inclusive, welcoming and building great relationships, and importantly—taking a stance.
COMMON SENSE MARCH/APRIL 2023 18
Haig Aintablian, MD

CANDIDATE FOR YPS DIRECTOR
Current Role/Employer: Space Medicine Fellowship Founder, UCLA Health
Clinical EM Practice Employment Type: Full time academic emergency medicine and space medicine
Clinical Hours in the ED per Month: 120
Nominated/Endorsed by: Self-nomination
Additional Leadership Roles: Council Member, Space Medicine Fellowship Council
Membership: 2016-2023
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
AAEM Resident of the Year Award
AAEM/RSA Committee Member of the Year Award
AAEM Board of Directors
AAEM/RSA Board of Directors
CAL/AAEM Board of Directors
YPS-AAEM Council Member
AAEM/RSA Advocacy Committee
Candidate Statement for YPS Director
AAEM EM Workforce Committee Member
AAEM Leadership Academy Participant
MEMC Abstract Reviewer
Scientific Assembly Abstract Reviewer
Common Sense Author
I'm blessed to have been on the board of AAEM while president of AAEM/RSA for two years. During these two years, I grew to understand the complex environment and key players that influence our sacred specialty. With my board, I was able to publish numerous well-circulated position statements that helped put AAEM on the map, including on topics related to midlevel providers and CMGs opening up new residencies. Additionally, I helped organize the HPEM symposium for two years. These were two of the best years of my life. Now that I'm one year into working in the community and in academics, I have an even more enhanced understanding of the issues that plague us. I have found AAEM to be my home since I was in medical school, and I aim to be a member for life. As part of this membership, I know just how important it is to do more than just sit idly by. As I start to have more free time to dedicate to advocacy issues, I want to spend this time improving our specialty and fighting the good fight. With that, I'd love to continue to work with AAEM on the AAEM board of directors, bringing light to our incredible advocacy work and protection of emergency medicine physicians and patients. I humbly ask for your vote and look forward to giving this organization my undivided effort. Thank you!
PLATFORM STATEMENTS
COMMON SENSE MARCH/APRIL 2023 2023 19
PLATFORM STATEMENTS
Fred E. Kency, Jr., MD FAAEM CANDIDATE FOR YPS DIRECTOR

Current Role/Employer: Assistant Professor Emergency Medicine, University of Mississippi Medical Center, Jackson, MS; Baptist Medical Center, Jackson MS
Clinical EM Practice Employment Type: Community and Academic
Clinical Hours in the ED per Month: 140
Nominated/Endorsed by: Jonathan S. Jones, MD FAAEM and William T. Durkin, Jr., MD MBA MAAEM FAAEM
Additional Leadership Roles: MS-ACEP Councilor (2019-Present)
Membership: 2015-2023
Board Meeting Participation: 100%
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
AAEM Board of Directors
AAEM Foundation Board of Directors
AAEM LEAD-EM Board of Directors
AAEM/RSA Board of Directors
Scientific Assembly Abstract Reviewer
Oral Board Review Course Examiner
Common Sense Author
Candidate Statement for YPS Director
Clinical Practice Committee Board Liaison
Membership Committee Board Liaison
YPS-AAEM Council
JEDI-AAEM Section Member and Work Group Lead
WiEM-AAEM Section Member
Scientific Assembly Abstract Reviewer
Simulation Interest Group
It would be my honor to serve a third and final year as your Young Physicians Section (YPS) Director. As a member that has served on multiple boards/committees/sections within the American Academy of Emergency Medicine (AAEM) organization, I have a wealth of knowledge, key, to leading and directing the future of our specialty. In my opinion, young physicians have a unique set of challenges when stepping into the medical arena, of becoming an attending. Whether it is finances, board certification, job searches, malpractice, or geographical differences in practice, I stand ready to assist. It has been my pleasure to be the guiding light already for so many young physicians under my charge.
As a Military Veteran, I know the importance of being on the front lines to truly enact change and progress in any powerful organization. Continuing to serve as the AAEM YPS Director would give me that opportunity. Over the past two years the AAEM Board and YPS Board have worked hard to bring awareness and programming for our members. Whether it is helping increase membership, developing education tracks for conferences, brand development, or helping increase international awareness, I continually stand ready to help this organization move forward.
Educating fellow physicians and those in early medicine education training has always been a true passion of mine. From teaching a second-year medical student to write appropriate history and physicals to guiding a fourth-year medical students with placing their first central venous or arterial line, nothing brings me more joy than knowing I’m helping develop the skills and education of our next generation of physicians.
When I served as a Navy Physician in Africa, I had many opportunities to see international medicine first-hand. The opportunity to see the vast differences in practice and the opportunity to incorporate that into my own niche has been great. I seek the opportunity to continue to spread that passion though AAEM.
COMMON SENSE MARCH/APRIL 2023 20
Jennifer McGowan, MD FAAEM CANDIDATE FOR YPS DIRECTOR

Current Role/Employer: Assistant Professor of Emergency Medicine, Associate Residency Program DirectorUniversity of Louisville
Clinical EM Practice Employment Type: I have a hybrid position that allows me to work both clinically in a community ED setting and serve as a core faculty member for our residency program where I am an Associate Program Director
Clinical Hours in the ED per Month: 120
Nominated/Endorsed by: Self-nomination
Additional Leadership Roles: N/A
Membership: 2015-2017; 2022-2023
Disclosure: Nothing to disclose.
AAEM Activities (past five years)
WiEM-AAEM Section Member
YPS-AAEM Section Member
Candidate Statement for YPS Director
I write this letter in self-nomination to serve as an AAEM Young Physicians Section director. I completed my residency training at the University of Louisville in 2018 and have practiced clinically in the community of Louisville, KY since that time. As an Assistant Professor of Emergency Medicine, I now split my time between the community and academics, serving as an Associate Program Director for the ULSOM Department of Emergency Medicine Residency. I am also a Fellow in the Academy of Wilderness Medicine (FAWM). I am actively involved in both undergraduate and graduate medical education, serving as a faculty advisor for the undergraduate Wilderness Medicine Interest Group, an Advanced Wilderness Life Support (AWLS) lead instructor for medical students and residents, the rotation coordinator for both student and resident community EM rotations, the creator and supervising faculty for a resident wilderness medicine elective, and work in a teaching capacity with didactics, administration of mock oral exams, simulation training, and on shift supervision and teaching of students and residents.
I would add value as a YPS director as a young, enthusiastic voice that is far enough into my career to have a good grasp of the issues facing our specialty and our residents, but young enough to emphasize with residents and new attending physicians because I was recently in their position. As a female with a strong interest in mentorship of other young females in emergency medicine, this opportunity would enhance my connections to better serve my peers and the next generation. My residents and colleagues would describe me as dedicated to the specialty, outspoken to injustices, and a fierce advocate for patient care and proper medical education.
Many of my career and academic interests align with the services of the YPS. For several years, I have performed mock interviews with senior medical students pursuing an emergency medicine residency. With this service, I have provided them with feedback and assistance with their CVs and personal statements. I have applied to be an AAEM medical student mentor, and eagerly await my potential match(s). This is something I have found great personal satisfaction in during my opportunities to mentor medical students of all stages at our home institution.
I have chosen AAEM to be my professional representative organization of choice because I feel their values and mission most closely reflect my own. I was raised in a residency program that has always championed and supported democratic practice groups and is against the corporate practice of medicine. I am a part of a residency leadership team that is actively trying to incorporate DEI initiatives into our program. My program raised me to believe we all have a voice, and our voices will shape the future of medicine, our specialty, and good patient care. It would be an honor to serve as a YPS representative so my voice can be used to help make a difference.
PLATFORM STATEMENTS
COMMON SENSE MARCH/APRIL 2023 2023 21
If You Died and Came Back, What Would Your Art Look Like?
 Joelle Borhart, MD FAAEM FACEP
Joelle Borhart, MD FAAEM FACEP



Incredibly, Dr. Matthew Wetschler has answered this question. Dr. Wetschler is a fellow emergency physician and artist who survived a catastrophic spinal cord injury and cardiac arrest while surfing. You may remember Dr. Wetschler from his moving keynote address, “Water and Stars” at the 2019 AAEM Scientific Assembly in Las Vegas, NV. As co-chair for the 2019 Scientific Assembly Planning Committee, I was in the front row when he shared his inspiring story of recovery against all odds.
Since that keynote address, I have continued to think about Dr. Wetschler often, and was delighted to learn that a short documentary of his story was recently released. The movie begins on the beach just after the injury. Two strangers—one another doctor—resuscitate Dr. Wetschler after pulling him out of the water. Weeks of inpatient rehabilitation follows. While in the hospital, an art therapist works with Dr. Wetschler as he begins to process the significance of his harrowing death experience and learns to create art with his changed body, what he describes as “a beautiful opportunity.” Beautiful indeed—we watch as Dr. Wetschler creates gorgeous pieces using medical supplies such as betadine and gauze and only limited use of his right arm.
Another poignant moment takes place in a kitchen. Dr. Wetschler is preparing to return to work in the ED and a friend has set up mannequins to practice placing a central line and intubating. Prior to the accident, he had worked just a single shift as an attending at his hospital. Now 15 months have passed. Dr. Wetschler appreciates the high stakes of returning to work with no back up (“If I can’t get the procedure, no one can get the procedure”). Yet he approaches the situation with humility and levity joking with the mannequin that, “I need to place a big IV in your neck. Side note: I have no feeling or coordination in my hands.”
I have thought of Dr. Wetschler frequently since hearing him speak in Las Vegas. His story is a testament to the resiliency of the human spirit and to the miracles of modern medicine. I hope you will consider watching his inspiring documentary. Matthew Wetschler died and came back, and his art is beautiful.

vimeo.com/teamvessel/resurrectionartist
COMMON SENSE MARCH/APRIL 2023 22
Photo Permission by Scott Fitzloff
Climate Change, Social Justice, and the Future of Emergency Medicine: An Interview with Emily Sbrioli,
 Faith Quenzer, DO MPH FAAEM
Faith Quenzer, DO MPH FAAEM
Recently, climate change has been on the forefront of media attention. Our greater global and local communities are experiencing firsthand the direct effects of climate change through extreme weather events—increased frequency of flooding, storms, and heat. Additionally, climate change has been implicated in increasing the spread of novel infectious diseases on populations. Those who are most vulnerable to climate change are those who are socioeconomically disadvantaged. As emergency physicians, we often provide medical care to those who are also most vulnerable as these patients are most likely to suffer from the most severe complications such as dehydration, asthma/COPD exacerbations, birth complications, infectious diseases like COVID-19, cholera, and influenza to name a few of the many medical conditions impacted by climate change.
Though the Clinical Research Fellowship at UC San Diego, I have had the unique pleasure knowing and working alongside Dr. Emily Sbrioli. For our piece, I have had the unique and wonderful opportunity of interviewing Dr. Sbiroli who is a board-certified emergency medicine physician in San Diego, California and holds a diploma in Climate Medicine (DiCM) from the University of Colorado. Last year, she completed the National Physician Fellowship in Climate and Health Science Policy. Dr. Sbiroli finished her residency in 2021 at UC San Diego where she served as Chief Resident. She now practices emergency medicine at several community health care systems in the San Diego area including areas near the border serving at-risk populations. Her current focus includes health care sector decarbonization, the impacts of climate change on human health, and clinician education and engagement with climate and health issues.
Dr. Sbiroli has given numerous lectures, presentations, and participated in panels and podcasts for a wide variety of audiences, from high school students to graduate health professionals, practicing clinicians, and

 MD
MD
lay audiences on the topics of climate change health impacts and health care sector sustainability. She has developed and led curricula for medical students and physician training programs on climate and health, and participated in California state advocacy initiatives. She shared the stage at the Environmental Media Association Impact Summit, which was featured on a podcast with “At Home with Drew and Linda Scott,” and was also featured on UN Women. She has presented at Health Care Without Harm’s CleanMed annual conference, California’s American College of Emergency Physicians, and FemInEM. In 2019, she was awarded as an inaugural Emerging Physician Leader by Health Care Without Harm’s Physician Network. As a National Physician Fellow, she has partnered with Health Care Without Harm and the US Environmental Protection Agency Climate Science and Impacts Branch.
Faith Quenzer (FQ):* You have such a unique set of passions and skills. Tell me about your upbringing and how that shaped you into becoming the physician we see today.
Emily Sbiroli (ES): I grew up in New York splitting my time between Queens and Long Island. My mother was an immigrant from Italy so we spoke Italian in our household. My younger brother has severe autism so at a young age I was exposed to the health care system and the complexities of caring for someone who has different needs than the norm. I’m the first of my family to go to medical school in the U.S.
FQ: What inspired you to become an emergency medicine physician?
ES: In 2012, Hurricane Sandy hit New York and I, quite literally, found myself caught in the storm while evacuating my family and grandparents from their homes, which eventually flooded. I distinctly remember while driving
SOCIAL EM & POPULATION HEALTH COMMITTEE
>> COMMON SENSE MARCH/APRIL 2023 23
Interestingly, even though this question asks “how is climate change affecting emergency physicians” another important question is just the opposite: how are emergency physicians contributing to climate change?
through the storm and thinking, “Wow… I really need to become a doctor who can help anyone at any time, in any situation.” That was when I started to embrace emergency medicine as the specialty for me.
FQ: Tell me how you found the intersection between climate change and emergency medicine.
ES: I had always been interested in environmental sustainability even in my undergraduate years—it was actually my major during my undergraduate years. But in retrospect, it was again that same storm, Hurricane Sandy, that truly brought home for me the impacts of our changing climate on our health. It’s not just polar bears in the Arctic that are affected—the effects of climate are very much at our doorstep and affecting our daily lives. The polar bear narrative is over. In emergency medicine, we are on the front lines of caring for our communities in times of crisis. The effects of climate change on health are very much seen in our waiting rooms on a daily basis. Whether it manifests as an acute COPD exacerbation or asthma exacerbation on days with poor air quality, or heat-related illnesses, or GI illnesses from flooding and contaminated water sources, or direct injuries or loss of access to care from extreme weather events—these impacts on our health are very much there.
FQ: Tell me about the fellowship that you did. What did you learn?
ES: I finished residency in June 2021 and July 1st, 2021 I started the National Physician Fellowship in Climate and Health Science Policy with the University of Colorado, which I completed in June 2022. Through this fellowship, I worked with an organization called Health Care Without Harm, which is an organization leading the health care sector towards a net-zero carbon footprint. I also worked with the US EPA, specifically with the amazing team in the Climate Science and Impacts branch. I could write novels and talk for days about what I learned in the fellowship and with these two organizations, but in brief, I learned how to interpret current climate science data and pull out what is important to physicians regarding environmental impacts on human health. I then learned how to apply key facets of this to different settings, like medical education, policy making, or health care delivery including directly at the bedside with my patients. We like to call ourselves “climate docs.”
FQ: How do you see the effects of environmental justice in the ED and in the hospital?
ES: One of the most important lessons I learned in my fellowship is that even though climate change is a global problem, not all societal groups or regions are affected the same. Some groups bear more of a burden than other groups. For instance, urban, low-income areas tend to feel amplified effects of air pollution or extreme heat events. Rates of asthma in children are higher in inner cities, or areas with worse air pollution—Black children are particularly at risk compared to other groups. The elderly and the socially isolated, such as the homeless, are more vulnerable than other groups in extreme heat events as well. Pregnant
women experience higher rates of preterm labor or neonatal complications in areas more strongly affected by climate events and pollution. Women in general are also more likely to experience domestic abuse after an extreme weather event, such as what happened after Hurricane Katrina in Louisiana.
There is very important report published by the US EPA in 2021 that looked at social vulnerability in the US related to climate change and found that specific groups were more vulnerable than others when it came to health impacts.1 It found that Black/African American individuals over age 65 had the most disproportionate risk of living in an area with the highest projected increases in premature mortality related to air pollution. Latino individuals were more likely to live in areas with the highest projected labor hours lost and disruption to livelihoods. The impacts of climate change are not evenly distributed and vary across populations and exposure types, and some communities are less resilient than others in dealing with them. This leads to inevitable health disparities that will show up in our hospitals and emergency rooms.
FQ: How do you think climate change effects emergency medicine physicians?

ES: Climate change affects EM physicians the same way that the pandemic affects us. We are on the frontlines and will have to deal with its effects, whether we are ready or not. We are the safety net for our communities. The good thing is that there is nothing new in terms of what pathophysiology to expect when it comes to climate change. Do we know how to treat hyperthermia? Yes. Can we treat a severe asthma exacerbation? Yes. Can we treat trauma, whether it’s physical trauma from an injury, or a mental health crisis? Yes. Can we make a safe disposition for someone who can’t go home for whatever reason? Yes. We can treat whatever climate change throws at us. But where we really need to pay attention is are we doing enough to help alleviate the problem in the first place?
Interestingly, even though this question asks “how is climate change affecting emergency physicians” another important question is just the opposite: how are emergency physicians contributing to climate change? The very act of delivering health care contributes to the problem in a very real, measurable way. The United States health care sector is the largest contributor to the global health care carbon footprint at 27% of absolute emissions.2 Remember all that waste you see in the emergency
CLIMATE CHANGE, SOCIAL JUSTICE, AND THE FUTURE OF EMERGENCY MEDICINE
>> COMMON SENSE MARCH/APRIL 2023 24
It’s not just polar bears in the Arctic that are affected— the effects of climate are very much at our doorstep and affecting our daily lives. The polar bear narrative is over.
SOCIAL JUSTICE, AND THE FUTURE OF EMERGENCY MEDICINE department? All the energy used? The devices and products we use and the supply chain behind it? That’s all contributing to the problem. Frankly, I was tired of seeing all the waste generated in the emergency department so I joined the sustainability committee at my hospital to see if we could do something about it.
FQ: What can we do about the problem of climate change and social/ environmental justice in our settings?
ES: We have a very trusted voice, both inside and outside the hospital. What I have found is that just by sharing my stories of patients I see in the emergency department, sharing my expertise and concern, people will listen. Other leaders will listen, policy makers will listen, and in turn we can try to tackle this massive public health crisis that is climate change. The good news is that we have so many solutions out there already just waiting to be deployed. We know who is most vulnerable and where they are—we just need to advocate for them. One of the ways I like to educate my patients at the bedside if I think they are particularly at risk is I share some publicly available and user-friendly apps, like the EPA Air Now App or the Heat Index App by OSHA-NIOSH. I’ll just counsel them on avoiding going out or doing strenuous activities on days with poor air quality, or making sure they can keep their temperature-sensitive medications cool during a heatwave. I see the ED as a place where we can help with prevention in this way.
In our greater hospital setting, I think it’s important we advocate for sustainable practices and health care delivery, and we often do not need to reinvent the wheel with this one. There are many resources out there to help us with this, such as Practice Greenhealth. It also seems to be the case that practicing medicine mindfully and with best-practices also tends to be the most environmentally conscious way of delivering health care, such as not shot gunning full lab work-ups or imaging, and practicing a bit more mindfully.
Continued from page 10
HEART OF A DOCTOR
seen who was unknowingly infected with HIV by a supposedly monogamous partner.
Experiences in the emergency department can makes physicians strong, jaded, or fearful—some would argue a combination of all three arise with years of experience. That day, I left pensive about what Lina had wondered—How could a partner just betray someone like that? It was a legitimate question posed by a woman not far off in age from myself and it reminded me just how influential friends, family, and partnerships are in our lives. It reminded me how important it is to treasure those relationships worth treasuring while I have them.
References
1. Landman KZ, Ostermann J, Crump JA, Mgonja A, Mayhood MK, Itemba DK, Tribble AC, Ndosi EM, Chu HY, Shao JF, Bartlett JA, Thielman NM.
FQ: What is the one important thing we can learn as EM physicians from climate change?
ES: If we’re asked “what is one thing EM physicians can learn from climate change,”I would ask…well, what did we learn from the pandemic (another public health crisis)? Climate change is often labeled the greatest public health threat of the 21st century (but now some folks are changing it and saying it’s the greatest public health opportunity of the 21st century—which is also true, but I personally find that doesn’t convey the sense of urgency we really need). So given these public health crises, what did we learn? In the pandemic, I learned that prevention and preparation is key. The same is true for climate change in my opinion. When we are prepared, we can deal with whatever is thrown at us in the ED. Our hospital systems need to be able to withstand influxes of sick folks suffering from the effects of climate change. Our facilities can’t shut down with the rest of the community during an extreme weather event. Access to care needs to be reliable and ready. Ideally, we’d be participating in preventative actions in the meantime; we educate and look out for vulnerable patients, and we help decrease our carbon footprint. These are the key lessons I have learned as a climate doc.
FQ: Thank you for your time and your efforts as both an advocate for climate change and as a frontline emergency medicine physician. Our colleagues and patients are most fortunate to have you in these spaces.
References
*Interview on January 30, 2023
1. US EPA Climate Change and Social Vulnerability: A Focus on Six Impacts https://www.epa.gov/cira/social-vulnerability-report
2. Health Care’s Climate Footprint: https://noharm-global.org/sites/default/ files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf
Gender differences in the risk of HIV infection among persons reporting abstinence, monogamy, and multiple sexual partners in northern Tanzania. PLoS One. 2008 Aug 27;3(8):e3075. doi: 10.1371/journal. pone.0003075. PMID: 18728779; PMCID: PMC2516930.
2. Varma DS, Chandra PS, Callahan C, Reich W, Cottler LB. Perceptions of HIV risk among monogamous wives of alcoholic men in South India: a qualitative study. J Womens Health (Larchmt). 2010 Apr;19(4):815-21. doi: 10.1089/jwh.2008.0884. PMID: 20201705; PMCID: PMC2867557.
3. Farrington EM, Bell DC, DiBacco AE. Reasons People Give for Using (or Not Using) Condoms. AIDS Behav. 2016 Dec;20(12):2850-2862. doi: 10.1007/s10461-016-1352-7. PMID: 26969001; PMCID: PMC5720389.
4. Caldwell K, Mathews A. The Role of Relationship Type, Risk Perception, and Condom Use in Middle Socioeconomic Status Black Women's HIVprevention Strategies. J Black Sex Relatsh. 2015 Fall;2(2):91-120. doi: 10.1353/bsr.2016.0002. PMID: 29218311; PMCID: PMC5716635.
CLIMATE
CHANGE,
COMMON SENSE MARCH/APRIL 2023 25
Mental Health Licensure Questions: Is Your State Good or Bad?
Loice Swisher, MD MAAEM FAAEM and Alice Min Simpkins, MD FAAEM
"Is there a map of good states and bad states?”
Sigh. “It isn’t that easy.”
That was the reply of Mark Staz, the Federation of State Medical Boards’ (FSMB) Director of Continuing Professional Development, to my question back in the summer of 2017 when I started to look at mental health questions on state medical licensure applications. He explained that the FSMB was collating the variety of state licensure language and that it was not truly binary, i.e. good versus bad.

In the spring of 2016, the FSMB developed a Workgroup on Physician Wellness and Burnout to find strategies to combat physician burnout. Clearly, the fear of losing one’s medical license had been a barrier for physicians to seek mental health care—an issue over which the FSMB had influence but not total control as licensure language is in the purview of each individual state.

Previously there were no overarching recommendations regarding mental health questions on state licensure applications. The workgroup went to work to create recommendations to support help-seeking and, although not explicitly stated, comply with the American with Disabilities Act. An ultimate hope was to prevent physician suicide. The workgroup unveiled a document with 35 recommendations, 10 of which were specific to licensure, at the 2018 FSMB Annual Meeting in Charlotte, North Carolina. The recommendations were unanimously accepted by the delegation.1
The document and vote was just the start of change as each individual state medical board had to look at their own language, deciding whether to amend their verbiage and adopt the FSMB’s recommendations. Over the last five years, many states have wrestled with the recommendations and have made language
Image: amwa-doc.org/our-work/initiatives/physician-mental-health/ >>

WELLNESS
COMMITTEE
COMMON SENSE MARCH/APRIL 2023 26
changes to mental health questions on their applications. Unfortunately it can be extremely difficult to find up-to-date information. In many states, the licensure applications are not publicly visible, hidden behind portals on the internet. Articles on this topic are virtually certain to be inaccurate by the time they are published. Maps have also been developed but can be difficult to interpret as some only categorize states as binary “all or none,” meaning all the FSMB recommendations have been adopted, excluding many states that have made positive changes to their mental health questions even if all of the FSMB recommendations have not been met.2,3
When reviewing the licensure application language, we can organize them into five categories:
No mental health or substance use questions.

No mental health questions, but substance use questions are included.
Attestation statement .
Questions pertain to current impairment only.
Questions are overly broad or overly long in time frame (greater than two years) or posing hypothetical situations.
Only two states currently use an attestation statement—North Carolina and Mississippi. Mississippi’s medical license application uses this language:
Mississippi went from one of the worst states regarding licensure language to one of the best. Our own AAEM president, Dr. Jonathan Jones, was part of making that change.
Other state boards have also made positive changes—Idaho, Kansas, Montana, Florida, Minnesota, and many more. Many use questions that are commonly worded as: Are you currently suffering from any condition for which you are not being appropriately treated that impairs your judgment or that would otherwise adversely affect your ability to practice medicine in a competent, ethical and professional manner?
So is your state good or bad? The answer really depends on your point of view and personal concerns, and it is not clearly black and white. Get to know your own state’s current language. Don’t make assumptions—the landscape has significantly changed over the past five years. We hope that continued advocacy, visibility, and normalization of mental health treatment for physicians will lead to continued progress. This is the just one step towards destigmatizing mental health care and addressing the fear individual physicians face as they consider the impact of seeking mental health treatment on their career.
If you want to know more, come to Dr. Swisher’s presentation “The Changing Map: Licensure and Mental Health” at AAEM Scientific Assembly in New Orleans on Monday April 24th at 3:05pm.*
References
1. FSMB Efforts on Physician Wellness and Burnout. Arthur S. Hengerer, MD, FACS; Mark L. Staz, MA; Humayun J. Chaudhry, DO, MACP. Journal of Medical Regulation (2018) 104 (2): 14–16. https://doi. org/10.30770/2572-1852-104.2.14
2. https://www.amwa-doc.org/our-work/initiatives/physician-mental-health/
3. https://drlornabreen.org/removebarriers/
*For up-to-date program information, please visit: aaem.org/aaem23/ program
WELLNESS COMMITTEE COMMON SENSE MARCH/APRIL 2023 27
WELCOME TO BALTIMORE!
On behalf of the Scientific Planning Work Group of the American Academy of Emergency Medicine Education Committee, we are looking forward to welcoming you to AAEM23 Scientific Assembly and to New Orleans, Louisiana. This event is one of the most anticipated academic conferences of the year, with a focus on cutting edge clinical medicine as well as practical application to patient care. Networking opportunities are plentiful as well as open invitations to attend any committee, section, or interest group meetings.
AAEM’s Scientific Assembly will take an innovative and practical look at various topics within emergency medicine that shape our field of practice. We are excited to expand the conversation on the topics of toxicology, cardiology, critical care, infectious disease, and many more. By combining discussion from leading scholars with innovative medical nuances, we hope to provide a resource to enhance the understanding of our beloved specialty.
AAEM continues to feature several learning styles: 20-minute track talks; 7-minute, “short and sweet” Breve Dulce lectures; 45-minute plenaries; hands-on Small Group Clinics; and pre-conference courses. The Meeting of the Minds literature review panels are back by popular demand. The competitions at Scientific Assembly continue to grow: listen to oral abstract presentations, watch up-and-coming speakers at Open Mic, and browse the poster gallery for research posters and baffling case encounters in the Photo Competition. Many AAEM groups are planning social events to supplement your educational time with opportunities to meet new colleagues as well as socialize with cherished friends.
The planning work group has invested significant time and thought to ensure that every participant has an educational, enjoyable, and safe experience in New Orleans. We look forward to sharing these amazing topics and engaging presenters with you.
We look forward to seeing you in New Orleans!
SIX EM DOCS WALK INTO A SHIFT SHOW
Saturday, April 22, 2023 | 4:00pm – 5:50pm



"Six Docs" is a collaborative effort by the six AAEM Sections providing a fun, fresh take on a traditional lecture. Follow Dr. Calhoun as she works her way through a traumatic shift, taking care of a crashing pregnant patient, aided by her specialist colleagues. Each section will provide a "breakout" lecture on a topic related to the hot topic du jour—abortion care in the ED—meant to help Dr. Calhoun (and you) take better care of the patient at hand. While each section will speak on a topic closely related to their section goals, the content will be applicable to all EM docs taking care of pregnant patients, from pre-hospital care to final disposition and beyond.
MEETING OF THE MINDS
Watch as prominent EM practitioners debate the pros and cons of the latest practice-changing articles on the HINTS exam and the impact of the Justice, Equity, Diversity, and Inclusion movement in emergency medicine. Bring your questions for an audience Q&A with the experts.
BREVE DULCE
These ever-popular “short and sweet” sessions are seven-minute overviews and 25 slides packed full of information! Plan to catch a variety of Breve Dulce topics at AAEM23 to round out your educational experience. For the first time this year, the “Stacked Session” in Breve Dulce II on Monday, April 24 will feature back-to-back lectures on similar topics: Critical Care, Cardiology, Ultrasound, Pharmacology, Toxicology, and Pediatrics. Every 10 minutes there’s a new speaker!

Preview of the Preview of the
CO-LEAD Christopher Colbert, DO FAAEM CO-LEAD Molly K. Estes, MD FAAEM FACEP
CO-VICE LEAD Jason Hine, MD FAAEM
AAEM.ORG/AAEM23
CO-VICE LEAD Julie Vieth, MD FAAEM
VISIT THE AAEM23 WEBSITE FOR FULL EDUCATIONAL DETAILS INCLUDING THE SCIENTIFIC PROGRAM, HOTEL AND TRAVEL INFORMATION, AND MORE!
COMMON SENSE MARCH/APRIL 2023 28
COLLABORATE AND NETWORK WITH COLLEAGUES FROM AROUND THE WORLD.
COMPETITIONS
Plan to browse the poster displays or attend abstract presentations at AAEM23. The following competitions will be taking place during the conference.


• AAEM and Journal of Emergency Medicine Resident and Student Research Competition
• AAEM/RSA & Western Journal of Emergency Medicine Population Health Research Competition
• Photo Competition
• AAEM Young Physicians Section (YPS) Research Competition
• AAEM/RSA Resident Breve Dulce Competition
• AAEM/RSA & EUS-AAEM Sim Sono Sleuthing Case Challenge
• CCMS-AAEM Breveloquent Competition
• Open Mic Competition – Onsite sign-ups available!
Learn more at aaem.org/aaem23/program/competitions
RELAX & RECHARGE WITH WELLNESS EVENTS

SMALL GROUP CLINIC
These sessions provide personal and hands-on education. At AAEM23 25 slots will be filled with advanced registration and 5 slots will be avail able on a first-come, first served-basis.
Not only does AAEM23 offer enriching education, it is also a motivational retreat where you leave feeling a renewed passion for emergency medicine. Throughout the Assembly, stop by the Wellness Room for a sanctuary from the conference bustle. The AAEM Wellness Committee has also planned the following events to participate in: 5K Fun Run/Walk, F3 Wellness Meals, Early Risers Yoga, Airway at AAEM, Wellness Paint'N'Sip, and AAEM Wellness New Attendee Reception. Some events require pre-registration.
Learn more at aaem.org/aaem23/program/networking-events
AAEM/RSA RESIDENT TRACK AT AAEM23
AAEM/RSA RESIDENT TRACK AT AAEM23
April 24, 2023 | 10:15am – 5:50pm
The AAEM/RSA Resident Track programming is selected by residents for residents. The goal of the track is to prepare residents for their careers in emergency medicine by concentrating on clinical topics and lectures on career success. The session concludes with the AAEM/RSA Breve Dulce Competition, featuring five resident presentations on the theme of “Widen the Differential”: creating a framework to approach the undifferentiated patient.
RESIDENT UNIONIZATION DISCUSSION PANEL
April 24, 2023 | 3:45pm – 4:35pm
‘Resident Labor Rights: Are Residency Unions the Best Way to Advocate?’ is a panel discussion featuring residents, fellows, and attending physicians who will provide a neutral and objective overview of the issue of resident unionization. Attending physicians, especially those within an academic practice setting, are welcome and encouraged to attend this session within the RSA Track. Listen and learn how to advise your trainees about the pros, cons, and nuances of resident unionization.
NETWORK AT SOCIAL EVENTS
Join AAEM for networking and other fun activities throughout the Assembly. Kick off AAEM23 at our Opening Reception. Enjoy light hors d’oeurves and drinks while networking with colleagues and exhibitors. Spend time with the Women in EM Section at their Networking Lunch, YPS Financial Literacy, RSA party, and JEDI Social. Explore opportunities to get involved in AAEM with the Chapter Divisions and Sections Social. Attend Airway at AAEM for an evening which promises to showcase the great range of human experience—to enlighten minds, expose vulnerabilities, and quietly suggest ways to overcome the challenges we all face each day. Learn more at aaem.org/aaem23/program/networking-events
COMMON SENSE MARCH/APRIL 2023 2023 29
KEYNOTE SPEAKER
COMMUNITY VIOLENCE AND THE EMERGENCY PHYSICIAN






Monday, April 24, 2023 | 8:00am – 8:45am
Rob Gore, MD








PLENARY SPEAKERS
EMERGENCY CARDIOLOGY 2023: THE ARTICLES YOU'VE GOT TO KNOW!
Saturday, April 22, 2023 | 1:45pm – 2:30pm
Amal
MD FAAEM
ROOM 13 IS MISCARRYING, CAN WE PAGE A LAWYER?
Saturday, April 22, 2023 | 2:40pm – 3:25pm
RECENT IMPORTANT ARTICLES FOR EMS PHYSICIANS AND THE ED TOO
Sunday, April 23, 2023 | 8:55am – 9:40am
ADDICTION MEDICINE PANEL
Sunday, April 23, 2023 | 3:15pm – 4:00pm
RECENT UPDATES IN CRITICAL CARE & RESUSCITATION
Tuesday, April 25, 2023 | 8:00am – 8:45am
MEETING OF THE MINDS: TO HINTS OR NOT TO HINTS: A TALE OF 2 GUIDELINES
Tuesday, April 25, 2023 | 10:15am - 11:00am
THE IMPACT OF THE JUSTICE, EQUITY, DIVERSITY & INCLUSION MOVEMENT IN EMERGENCY MEDICINE
Monday, April 24, 2023 | 1:30pm – 2:15pm
PEM LITERATURE UPDATE
Sunday, April 23, 2023 | 8:00am – 8:45am
Ilene Claudius, MD FAAEM FAAP FACEP




BOOST YOUR CME BY COMING EARLY OR STAYING AFTER AAEM23 AND ADDING A PRE- OR POSTCONFERENCE COURSE.
Mimi Lu, MD FAAEM


Preview of the Preview of the
Mattu,
Brian Acunto, DO EJD
Kimberly Chernoby, MD JD
Corey M. Slovis, MD FAAEM FACP FACEP
Jack C. Perkins, Jr., MD FAAEM
Anne Ickes, DO
Kimberly Hunt, NPRSS RPRS
Redina Davis
Harman Gill, MD FAAEM
Cortlyn Brown, MD FAAEM
Italo M. Brown, MD MPH
Mohamed Hagahmed, MD FAAEM
Peter DeBlieux, MD FAAEM
Michael E. Winters, MD MBA FAAEM
Andrew W. Phillips, MD FAAEM
Danya Khoujah, MBBS MEHP FAAEM
Bruce M. Lo, MD MBA FAAEM
COMMON SENSE MARCH/APRIL 2023 30
AAEM23 SPEAKERS

Michael K. Abraham, MD FAAEM
John R. Acerra, M, MPH FAAEM
Brian Acunto, DO EJD FACOEP
FACEP FHELA
Jason Adler, MD
Afrah A. Ali, MBBS FAAEM
Al'ai Alvarez, MD FAAEM
Hala Ashraf, DO
Zeki Atesli, MD
Jerome Balbin, MD FAAEM
Kimberly Baldino, MD FACEP FAEMS
Alex Barbuto, MD FAAEM
Stacey Barnes, DO FAAEM
Katey Bettencourt, MD
Rahul G. Bhat, MD
Neha Bhatnagar, MD
Michael Billet, MD FAAEM
James Blum, MD MPP
Michael Bond, MD
Laura J. Bontempo, MD MEd FAAEM
Joelle C. Borhart, MD FAAEM
Joseph Bove, DO
William J. Brady, MD FAAEM
Courtney Briggs-Steinberg, DO
Cortlyn Brown, MD FAAEM
Italo M. Brown, MD MPH
Vonzella A. Bryant, MD FAAEM
Joshua Bucher, MD
Josh Bukowski, MD FAAEM
Katharine Burns, MD FAAEM
Christine Butts, MD FAAEM
Elisabeth Calhoun, MD MPH FAAEM
David J. Carlberg, MD FAAEM
Lena Carleton, MD
Jennifer Carnell, MD FAAEM
Tatiana Carrillo, DO
Matthew Carvey, MD
John Casey, DO MA FACEP FACOEP
Wan-Tsu W. Chang, MD FAAEM
Yash Chavda, DO FAAEM
Kimberly Chernoby, MD JD
Eric J. Chin, MD MBA FAAEM
Kene Chukwuanu, MD FAAEM
Ilene Claudius, MD
Christopher Colbert, DO FAAEM
Joseph S. Colla, MD
Leah Colucci, MD MS
Katherine L. Darr, MD
Suchismita Datta, MD
Redina Davis
Peter DeBlieux, MD FAAEM
Pierre G. Detiege, MD FAAEM
Christopher I. Doty, MD MAAEM
FAAEM FACEP
Luke J. Duncan, MD
Sean Dyer, MD
Brandon A. Elder, MD FAAEM FAWM
Molly K. Estes, MD FACEP FAAEM
Cheyenne Falat, MD
Jessica Fleischer-Black, MD FAAEM
Deborah Fletcher, MD FAAEM
Kristin E. Fontes, MD FAAEM
Manish Garg, MD FAAEM
Harman S. Gill, MD FAAEM
June Gordon, MD FAAEM
Katarzyna Gore, MD
Robert J. Gore, MD
Stephen R. Gore, MD
Michael Gottlieb, MD FAAEM
Karen Greenberg, DO FACOEP
FAAEM FAHA
John C. Greenwood, MD FAAEM
Tanner G. Greiving, MD
Bruce R. Gutierrez, DO
Joshua Guttman, MD FRCPC FAAEM
Mohamed Hagahmed, MD FAAEM
Michael A. Hayoun, MD FAAEM
Megan Healy, MD FAAEM
Matthew B Hoekstra
Beatrice Hoffmann, MD PhD FAAEM
Maite Huis in 't Veld, MD
Kimberly Hunt, NPRSS RPRS
Darren Hyams, MD
Mercy M. Hylton, MD MBA FAAEM
Anne Ickes, DO
Paul S. Jansson, MD MS FAAEM
Gregory N. Jasani, MD
Jordan Johnson, DO
Jonathan S. Jones, MD FAAEM
Jerry W. Jones, MD FAAEM
Lauren Kalodner, MD
Prianka K. Kandhal, MD
Ryan Kelly, MD, MSc
Danya Khoujah, MBBS MEHP FAAEM
Patrick G. Kishi, MD FAAEM
Adeola A. Kosoko, MD FAAEM FAAP
Rebecca Kreston, MD MSPH
Diana Ladkany, MD FAAEM
Michael J. Lambert, MD RDMS FAAEM
Lauren E. Lamparter, MD
Andrew S Langille, DO
Rachel Le, MD
Christopher J. Lemon, MD
Skyler Lentz, MD FAAEM FACEP
Nathaniel T. Leu, MD MS
Bruce M. Lo, MD MBA FAAEM
Michael Losak, MD
Spencer Lovegrove, MD
Bobbi-Jo Lowie, MD
Mimi Lu, MD
Phillip D. Magidson, MD MPH FACEP
FACP FAAEM
Amal Mattu, MD FAAEM
Nicole S. McCoin, MD
Mary E. McLean, MD
Alina Mitina, DO
Siamak Moayedi, MD FAAEM
Malia J. Moore, MD FAAEM
William Mundo, MD MPH
Melissa Myers, MD FAAEM
Robert K. Needleman, MD FAAEM
Kimberly Nordstrom, MD JD
Ava Omidvar, MPH FP-C
Brandon Oswald, MD
Michael Owens, DO MPH CEM FAAEM
Jessica Palmer, MD
Ryan Pappal, MD
Brian Parker, MD MS FAAEM
Daven Patel, MD MPH
Andrew Pellet, MD FAAEM
Jessica Pelletier, DO
John Perkins, MD
Andrew Phillips, MD FAAEM
Valerie A. Pierre, MD FAAEM
Elizabeth Pontius, MD FAAEM
Arthur Pope, MD PhD
Christina M. Powell, DO
D Brady Pregerson, MD
Amy Prescott, MD
Michael Pulia, MD PhD FAAEM
Margaret Putman, DO FAAEM
Steven A. Radloff, MD
Maria Ramos-Fernandez, MD
Mark Ramzy, DO
Renato Rapada, DO
Joe Ravera, MD
Angela Regina, DO
Zachary Repanshek, MD
Thomas W. Riney, MD FAAEM
Rebekah Riordan, MD
Max Rippe, MD
Andrew Rizzo, DO FAAEM
Anthony Rosania, MD MHA FAAEM
Jordan A. Rosenberg, DO
Shana EN Ross, DO MS FAAEM FACEP
Alexis Salerno, MD FPD-AEMUS FAAEM
Alan J. Sazama, MD FAAEM
Kraftin E. Schreyer, MD MBA FAAEM
Tara Shapiro, DO FAAEM
Joseph Shiber, MD FAAEM FACP
FCCM FNCS
Mari Siegel, MD FAAEM FACEP
Michael M Silverman, MD MBA FAAEM FACEP
Corey M. Slovis, MD
Kristyn J. Smith, DO
Ryan Spangler, MD FAAEM
Matthew J. Stampfl, MD
Eric Steinberg, DO MEHP FAAEM
Kathleen Stephanos, MD FAAEM
Sean Stuart, DO FAAEM FACEP
FAWM
Mark Sutherland, MD FAAEM
Loice A. Swisher, MD FAAEM MAAEM
Jordan Thiesen, DO
Joseph R. Twanmoh, MD MBA FAAEM
Julie T. Vieth, MD FAAEM FACEP
Kathryn Voss, MD
Elias E. Wan, MD FAAEM
Joseph Weber, MD FAAEM FAEMS
Jim Webley, MD FAAEM
Benjamin White, MD FAAEM
Anne Whitehead, MD FAAEM FACEP
Joanne Williams, MD MAAEM FAAEM
George Willis, MD FACEP FAAEM
Michael P. Wilson, MD PhD FAAEM
Mike Winters, MD MBA FAAEM
Carmen Wolfe, MD
Andrea Wolff, MD FAAEM FACEP
Joseph P. Wood, MD JD MAAEM FAAEM
Gregory Wu, MD FAAEM
Anna Yap, MD
Nicole Yuzuk, DO
Bassam Zahid, MD FAAEM
Allison Zanaboni, MD FAAEM
Mitchell Zekhtser, DO
Bob Zemple, MD MBA FAAEM
Matthew Zuckerman, MD VISIT
THE EXHIBIT
COMMON SENSE MARCH/APRIL 2023 2023 31
HALL TO MAKE NEW CONNECTIONS – EXHIBITING AND SPONSORSHIP OPPORTUNITIES ARE STILL AVAILABLE.
THANKS TO OUR 2023 INDUSTRY PARTNERS
AAEM extends its thanks and appreciation to the following industry partners who have funded activities at the 2023 AAEM Scientific Assembly.
GOLD SPONSOR – $20,000-$49,999 SUPPORT LEVEL
• Abbott, Point of Care
• Gilead Sciences
SILVER SPONSOR – $5,000-$19,000 SUPPORT LEVEL
• LogixHealth
IN-KIND SPONSOR
• EchoNous, Inc.
• FUJIFILM/Sonosite
• Gaumard Scientific
• Hamilton Medical, Inc.
• Intelligent Ultrasound
• Karl Storz Endoscopy – America, Inc.
• Verathon | Glidescope
AAEM23 EXHIBITORS – THANK YOU

Plan your visit to the exhibit hall in New Orleans to network with these exhibitors:
• Abbott, Point of Care
• ABEM
• Aspirus Health
• AstraZeneca, Inc.
• Auburn University Physicians Executive MBA Program
• Aya Locums
• Biodynamic Research Corporation
• Bioxcel Therapeutics
• Brault
• Care Pharma
• Change Healthcare
• Emergency Care Partners
• Emergency Medicine Specialists
• ER Doc Finance
• Gilead Sciences
• Hamilton Medical
• Hippo Education
• Indian Health Service
• Ivy Clinicians
• Janssen Pharmaceutical, Inc.
• Kaiser Permanente/The Permanente Medical Group
• LogixHealth
• Magill Medical Technologies
• Money Script Wealth Management
• Moonstone Nutrition
• NeurOptics, Inc.
• Nova Scotia Health Authority
• Omni-Stat Medical Inc.
Please visit aaem.org/aaem23/exhibit-sponsor for the most up-to-date list.
• OptoMed
• PEPID
• PracticeMatch
• Purdue Pharma
• Resolv Healthcare
• Rhino Medical Services
• Rosh Review
• SimKit
• TeamHealth
• The Whole Physician
• Ventra Health
• Vituity
• Washington Emergency Care Physicians
• WestJEM
• Zerowet, Inc.
Preview of the
COMMON SENSE MARCH/APRIL 2023 32


Register Now! aaem.org/aaem23 COMMON SENSE MARCH/APRIL 2023 33
Caring for Aging Parents: Challenges and Skills

 Isabel A. Barata, MS MD MBA
Isabel A. Barata, MS MD MBA
As I write this article, we are blessed that we just celebrated my mom’s 91st birthday on January 1, 2023, and my mom-in-law celebrated her 98th birthday October 2022. Reaching old age is something to be celebrated but it comes with its own set of challenges. My mom still lives independently in Florida and has a beautiful flower, fruit, and vegetable garden. She gives fruits and vegetables to all her much younger neighbors. However, she has become frail, has had some serious falls, and overall, we are finding managing on her own is becoming much harder. We are at the crossroad of deciding what to do next. My mom-in-law has dementia and has lived for several years now in assisted living.
Most older adults are probably like our moms that initially do not need much help and contribute to their families, communities, and workplaces. Eventually as people live into their 80s, 90s, and beyond, there comes a point when they do need assistance. As an older person starts to need help it is usually close family members that step in. Family members find themselves having to take on more and more eldercare assistance. At times it may be straightforward such as helping with shopping, household chores, and transportation. However, as an older person develops more complex medical issues, frailty, and loss of physical strength, people start encountering more complicated issues that they are not prepared to address. There are several domains to consider and areas to help with some of these challenges: activities of daily living (ADLs), instrumental activities of daily living (IADLs), housing, safety, medical, legal, and quality of life.
The needs of ADLs and IADLs determine what kind of living arrangements which in turn ties in with housing decisions such as age in place (you may be able to seek support to enable them to live more independently via programs that focus on balance, safety, mobility, and fitness, in addition to considering hiring a professional caregiver to help your loved one remain in their own home and ensure their needs are being met), move in with a family member, or assisted living, each choice carries their own financial and lifestyle implications. You need to understand how difficult it is for a person who has been independent for many
years and now needs the help of others. Support them in adjusting to their new environment. Maintain an open dialogue of what they need and how they are coping with the sudden change in their lifestyle.
In the domain of safety, major concerns are related to falls, driving, and financial vulnerability. Create a safe environment in which they receive support in tasks they are not capable of doing. Another important decision is retiring from driving. This carries significant consequences in terms of privacy and spontaneity for the person. It can bring in the fear of even more isolation. You need to prepare them for this difficult transition. Help them maintain a sense of dignity by engaging them to create a sense of purpose and respect. Even cognitively intact individuals may fall prey to financial exploitation and be vulnerable to scams and fraud, aid with day-to-day finances made more complicated by the fact that bill paying, and investing is done online now. Continue to help them to take control of their finances as long as possible. This can give them reassurance and security.
Medical issues are prevalent in older individuals due to chronic conditions, loss of ability to make health care decisions, and overall mental decline. It is often difficult to navigate the health care system and elderly people may see a lot of different medical professionals. You may need to help coordinate appointments, medication delivery, and medical supplies they may need. If possible, accompany them to the doctor to give them comfort as well as getting to know the treatment plan and medications. However, even when planning medical care where we may feel we are the experts we should check their preferences and make sure they are comfortable and do not have concerns. Legal concerns are to be considered and we need to prepare ahead for significant decisions in health care and other matters. You need to have conversations about end-of-life options, advance directives, palliative care, organ donation, the financial implications of their passing, and how they wish to be honored when they pass away.
Finally, quality of life is an important consideration and keep in mind their autonomy, need for connectedness, and dignity. Give them space
AGING WELL IN EMERGENCY MEDICINE INTEREST GROUP
Countinued on page 40 >> COMMON SENSE MARCH/APRIL 2023 34
As an older person develops more complex medical issues, frailty, and loss of physical strength, people start encountering more complicated issues that they are not prepared to address.
Avoiding Emergency Department Admissions: The Why and How
 Tom Scaletta, MD MAAEM, Akiva Dym, MD FAAEM, and Anthony Rosania MD MHA FAAEM
Tom Scaletta, MD MAAEM, Akiva Dym, MD FAAEM, and Anthony Rosania MD MHA FAAEM
In the United States, approximately 30% of adult emergency department (ED) patients are admitted, and three-quarters of all hospitalized patients originate in the ED. An emergency physician (EP) hospitalizes approximately six patients on an average shift. However, when one patient is safely discharged from the ED instead of being admitted, about 40 hours of inpatient human resources are conserved, which is especially important during this unprecedented nursing shortage.1 Furthermore, given the scarcity of staffed inpatient beds, reducing unnecessary admissions reduces ED boarding and thus improves overall ED throughput and performance. The opportunity cost of boarding can be high, and reducing unnecessary admissions can provide significant financial, operational, and human resource savings to the ED and the entire hospital system. More than half of Medicare patients are enrolled in Medicare Advantage, a program that shifts reimbursement from fee-for-service to capitation.2 With capitation, payment for health care services is based on value (high quality and low cost) rather than volume. It is expected that Blue Cross, Humana, Cigna, Aetna, Anthem, and United Healthcare will expand value-based payments across all their product lines. CVS, Walgreens, Amazon, and Walmart are currently evaluating capitated health care models.3 As such, it is thus critical to reduce unnecessary hospitalizations to prevent excess costs which may be preventable.

As a case study, ED visits were analyzed at the author’s large, suburban ED, with an annual volume of approximately 80,000 visits. During the fourth quarter of 2022, there were 20,341 ED encounters. A total of 4,668 cases were seen by a pediatric EP and excluded from this study. Of the 15,673 remaining encounters (92% adults), the average admission rate was 30.3%, with a range of 19.7%-41.9%. This data
is consistent with previously reported ranges of ED admission rates.4 The lowest admitter ordered 35.2% fewer advanced radiology studies, prescribed 49.1% fewer antibiotics, and 35.5% fewer opiates. He generated 11% more RVUs per hour and discharged patients 44 minutes faster. However, his patient satisfaction scores were lower as compared to his peers. No correlation was found between admission rate and the number of medical malpractice claims, cases referred for quality review, or rate of patient returns within three days of ED discharge.


Normalization of the ED emergency severity index (ESI) data was performed to exclude the practice of “cherry-picking” cases as a potential explanation for the wide admission rate range. The respective admit rates by ESI for the lowest and highest admitters were 40.0% versus 67.9% for ESI-2 cases (emergent), 11.8% versus 34.6% for ESI-3 (urgent) cases, and 0% versus 1.5% for ESI-4 (non-urgent) cases.
What is the impact of this wide range of admission rates on the ED and hospital?
If the EP with the highest admission rate shifted to the mean admission rate, it would translate into two fewer patients being admitted per shift worked. In addition to the significant cost and time savings of reduced admissions, judicious admitting also reduces hospital-acquired infections, episodes of sundown syndrome, mortality in older chest pain patients, and 30-day rehospitalizations, a metric of Medicare Advantage reimbursement.6 Additionally, it is intuitive that admissions that can be safely avoided are lower acuity. So a more conservative approach to admissions will positively impact a hospital’s case-mix index, or CMI, which can lead to increased Medicare reimbursement. Judicious admitting practices also reduce the chance that a recovery audit contractor (RAC) will report concerns to CMS. Such investigations occasionally force corrective action plans that disrupt business operations and hold back Medicare payments. Furthermore, patients should be informed of the risks associated with admission and participate in shared decision-making regarding their disposition, as most prefer to go home.
>> OPERATIONS MANAGEMENT COMMITTEE
COMMON SENSE MARCH/APRIL 2023 35
Patients should be informed of the risks associated with admission and participate in shared decision-making regarding their disposition, as most prefer to go home.
As noted above, it was found that EPs with the highest admission rates were also more prone to order more advanced imaging studies, supporting the notion that individuals have varying tolerances for uncertainty.7,8 This concept translates to some EPs being more confident in making decisions with limited, imperfect data. They more readily accept that a missed diagnosis or rapid worsening of an illness is possible, and they thus calibrate the acceptable level of risk at a higher level. They may also feel more comfortable with discharging patients home. Conversely, others may excessively worry about being sued for malpractice, which results in higher levels of stress and burnout.9 This may also translate into increased imaging and other diagnostic studies being performed, as well as increased ED admissions rates.
For example, consider a patient presenting with typical Bell’s palsy signs and symptoms. While some EPs may be comfortable with performing no imaging and discharging home, other EPs may need to obtain a “just in case” brain CT scan showing an incidental finding, which occurs in 10% of cases.10 The patient may receive a neurological consultation, a contrast MRI scan, and an overnight observation or hospital admission. This occurrence exponentially increases the cost with no improvement in outcome.
Now that we have identified the significant variability in EP admission rates, what are some effective strategies to help potentially reduce ED admissions among the so-called “high admitters”? Some tactics which have been identified include:
• Developing uniform practice habits among EPs within a practice. Examples include the management and disposition of those presenting after syncope or breakthrough seizure. By introducing uniform practice patterns, variability in clinical care, and thus in admissions, can likely be reduced.
• Collecting and sharing monthly performance metrics to make statistical outliers aware of their performance and motivate self-correction. Many high admitters may not be aware that they are admitting patients at rates well above the group mean and will be able to perform self-review to identify practice patterns leading to their admission rates.
• Searching for cases where a discharge opportunity may exist to coach outliers. For example, encourage those with more chest pain admissions to use the HEART score to identify those appropriate for outpatient stress testing versus inpatient admissions.
• Encouraging case managers to assert an alternate disposition to hospitalization (e.g., skilled nursing facility), provide more intensive help at home (e.g., visiting nurses), and participate in next-day wellbeing checks.

• Having hospitalists evaluate patients in the ED and identify those appropriate for immediate discharge.
• Developing a model for close patient follow-up, such as by contacting patients the day after an ED discharge, inquiring about their condition, and addressing any follow-up or medication management challenges.
• Monitoring and reviewing all ED returns within three days and re-admissions within 30 days.
As payment models continue to shift from fee-for-service to capitation, hospitals are more motivated to reduce ED admissions through intensive case management and to identify and coach excessive admitters. By identifying high-admitters within the ED and implementing strategies as noted above, preventable admissions may be reduced and thus provide significant savings to the entire health system.
References
1. https://www.ncbi.nlm.nih.gov/books/NBK493175/
2. https://www.kff.org/medicare/issue-brief/medicare-advantage-in-2022enrollment-update-and-key-trends/
3. https://www.fiercehealthcare.com/health-tech/healthcare-plays-cvswalgreens-and-amazon-will-drive-more-partnerships-tech-investment
4. https://www.sciencedirect.com/science/article/abs/pii/ S0196064413000383
5. https://epmonthly.com/article/finding-the-best-solution/
6. https://pubmed.ncbi.nlm.nih.gov/32732782/
7. https://www.sciencedirect.com/science/article/abs/pii/ S0735675708003690
8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7294596/
9. https://www.sciencedirect.com/science/article/abs/pii/ S0196064408021185
10. https://pubmed.ncbi.nlm.nih.gov/31256598/
Many high admitters may not be aware that they are admitting patients at rates well above the group mean and will be able to perform self-review to identify practice patterns leading to their admission rates.
OPERATIONS MANAGEMENT COMMITTEE COMMON SENSE MARCH/APRIL 2023 36
“If It Wasn't For You, I Wouldn't Be Here Today”
Robyn Hitchcock, MD FAAEM
A68-year-old woman presented to the emergency department towards the end of my shift yesterday with UTI symptoms.
When I went into the room to talk with her she expressed joy and recognition after hearing my name. She talked for some time about the heart attack she had in the summer and how appreciative she was of my care. She said over and over, “If it wasn't for you, I wouldn't be here today.”
I encouraged her to share her perception of what she remembered of her ER stay. The nurse had given me a heads up that the patient remembered me so I did dig into her chart and review her ED care from several months ago. She had an inferior STEMI, I thrombolysed her, and gave her aggressive fluid, nitrates, aspirin, etc—the usual—and the helicopter was flying that day so I got her down to the cath lab 70 miles away pretty quickly.
Her memory of her ED stay was rather sketchy but she filled me in on her tertiary hospital stay, the repeated cath, and other procedures she had, and how well she's doing now including getting her 10,000 steps every day, shoveling snow, and right back to her active healthy life style.

She pointed out that her husband had some cardiac issues and she feels like people dragged their feet and his care was not expedited like hers was. She was grateful and happy and we chatted for some time. This was a very much appreciated mental boost for me.
Like most weeks these days, this was a crappy week. The boarders we constantly have in the emergency department have no end in sight. This week, my long term boarders included a 79-year-old woman with a new brain tumor, probably metastases from her stage 4 colon cancer. She had a large amount of edema, shift, and mass effect. She boarded in the emergency department for three days on a hypertonic saline drip and decadron and I eventually sent her home because she can see a neurosurgeon as an outpatient for a discussion about removal versus palliative care. Right now, she can get into the office sooner than she could find a bed at a tertiary care facility. We had an 82-year-old NSTEMI that we
boarded for a week who we finally sent down for an “out and back” heart catheterization on day number seven of his boarding in the ED. We try to phone consult with the specialists who will talk with us, but unlike larger facilities, these patients have no hope of seeing or being evaluated by a consultant until they are transferred.
The frustration of small town medicine when there are never any beds at any higher level of care facility, and you are boarding these patients for days and literally just can't provide them the care you need is causing extreme moral injury and it escalates every day. On Tuesday of this week we had nine boarders in my ten bed emergency department. At one point there were 27 patients registered in the department. One doctor. One PA. Four nurses. Not good.
But the positives of small town medicine are very real. In a smaller place, you're much more likely to get follow up like the kind, grateful woman that I saw at the end of my shift yesterday. I was called to OB a couple of months ago for an expedited delivery because the family doctor with OB privileges couldn't make it in time to deliver the baby of the woman who came in ready to push. A month later I took care of her older son for an abdominal pain evaluation and got to follow up on the baby, and three weeks after that I took care of the baby himself when he came in with a cough and had RSV. He looked great and it was fun chatting with Mom and catching up.
There are many downsides of practicing in a location with limited resources. But it's important to remember the positives too. We are much more able to create relationships over time with the patients in our community. Sometimes, when I'm having difficult “goals of care” discussion with a family, there's extra trust because I took care of one of their family members with a broken arm or an anxiety attack. Sometimes you go to the grocery store or the local diner and your cashier or server thanks you for taking care of them or their family member. Grateful patients in small towns will occasionally send treats or snacks to be shared out in the break room. I haven't gotten a goat or chicken yet to pay for my medical care but it's probably just a matter of time.
Academic medicine frequently overlooks rural practice. Small town care poses unique challenges, but offers significant, heartwarming rewards.

RURAL MEDICINE INTEREST GROUP
COMMON SENSE MARCH/APRIL 2023 37
At one point there were 27 patients registered in the department. One doctor. One PA. Four nurses. Not good…But the positives of small town medicine are very real.”
ETHICS COMMITTEE “First, Do No Harm”
Melissa Myers, MD FAAEM and Al Giwa, MD FAAEM
difficil? I would say most practicing emergency physicians have written that prescription once, or perhaps many, times. It’s hard not to in the age of patient satisfaction scores. Holding this principle in mind may help us all to give our patients the care they need, even if it’s not exactly what they want.
e all remember standing in ourgraduation robes, hand raised, as we recited the Hippocratic Oath at our medical school graduations. The room would have filled with voices saying the famous phrase “First, Do No Harm.” It seemed very simple to me as a graduating medical student but as the years have passed this has proved to be a more difficult oath to keep than I first thought.
“First, Do No Harm” is the basis of the bioethical principle “non-maleficence.” This bioethical principle states that a physician should “act in such a way that he or she does no harm.”1
An obvious example of violating this ethical principle would be to come to work altered or intoxicated. In this case, the physician would be unable to provide medical care without harm to their patients due to their own incapacity. This is an extreme example that I think most of us can say we have either avoided during our careers or sought needed help.
There are more subtle kinds of harm, and times when a tradeoff must be made. The second part of this definition is “does no harm, even if her or his patient or client requests this.” Imagine a scenario we all face frequently—perhaps multiple times a shift. A patient presents to the ED with lower back pain, requesting narcotics for their pain. Do you write the prescription? Potentially, your prescription will lead to a narcotic addiction for the patient, surely a type of harm. Or the patient who presents with sinus pain and is requesting antibiotics for what is clearly a viral illness. Do you write the prescription? What if that patient returns with Steven-Johnson-Syndrome or clostridium
Closely related to this principle is that of beneficence, which states that not only must a physician not cause harm, but they should also act in a way the benefits their patient.2 As with non-maleficence this is more difficulty in practice than in theory. As physicians, we all believe that we are giving the best possible care to our patients with our extensive training and experience. I would argue that this ethical principle requires us to go farther and confront our own internal biases to improve our care for all
patients. Patients in the United States receive different care based on their race and gender with differences in pain control and maternal outcomes between white and minority patients.3,4 A patient recently arrived to a hospital I work at complaining of abdominal pain. The physician who initially saw the patient described her as “hysterical” and wanted to avoid giving pain medication. Another patient presented with arm pain, and was this time described as “histrionic.” The first patient was diagnosed with a high-grade small bowel obstruction, the second with a humeral fracture. The commonality in these cases was that both patients were women of color, whose race and gender meant that their pain was not taken seriously. To truly do good for our patients, we must avoid perpetuating these differences and learn to avoid our own implicit biases.
“Do No Harm” seemed much more straightforward I realized that I left the easy answers behind when I started intern year. Holding to the principles of non-maleficence and beneficence, trying to intentionally apply these principles to our patients on shift, can help us to be the physician we wanted to be as a student.
References
1. Schröder-Bäck P, Duncan P, Sherlaw W, Brall C, Czabanowska K. Teaching seven principles for public health ethics: towards a curriculum for a short course on ethics in public health programmes. BMC Medical Ethics. 2014;15(1):1-10.
2. Beauchamp TL. The ‘four principles’ approach to health care ethics. Principles of health care ethics. 2007;29:3-10.
3. Johnson TJ, Weaver MD, Borrero S, et al. Association of race and ethnicity with management of abdominal pain in the emergency department. Pediatrics. 2013;132(4):e851-e858.

4. Callaghan WM. Overview of maternal mortality in the United States. Elsevier; 2012:2-6.
COMMON SENSE MARCH/APRIL 2023 38
Do No Harm seemed very simple to me as a graduating medical student but as the years have passed this has proved to be a more difficult oath to keep than I first thought.
CPR is Not Resuscitation
Tara Shapiro, DO FAAEM
Do you want to be resuscitated? Should we really be saying this anymore? Is Cardiopulmonary Resuscitation (CPR) actually resuscitation if the survival rate is approximately 5% to 10% for out of hospital arrest and 24% for in hospital arrest?1
Resuscitation is the act of reviving someone from apparent death. CPR doesn’t really revive someone from apparent death very often. The general public believes CPR has a success rate of 53%-75%.2,3,4,5 Thank you, Hollywood! In medical dramas, return of spontaneous circulation occurred in 62% of patients. In addition, CPR on television does not adhere to published guidelines so individuals who watch these dramas regularly are more likely to have substandard knowledge of how to perform effective CPR.6
So what about the survivors of CPR? What does life really look like for the very few whose heart’s start again?

CPR is not resuscitation. All the other modality we do, such as IV fluids, defibrillation, antibiotics, IV pressures, and surgical procedures are all forms of resuscitation because they can actually change the course of a patient’s disease progression from badness or death towards improvement with a better chance than the mere 5-20% that CPR can. I encourage physicians to use more basic language that actually helps a patient or family make a well informed decision about their lives and health care.
Instead of asking, “Do you want to be resuscitated?” maybe try saying things like, “If your heart stops and you are dead, would you want us to do chest compressions?” This is more descriptive and allows a patient to ask questions and consider options. You also will have the opportunity to ask patients and families what they know about the success rates of CPR before you tell them the real truth.
So what about the survivors of CPR? What does life really look like for the very few whose heart’s start again? If patients survived hospitalization to discharge, some studies report the quality of life for survivors of CPR was generally acceptable. However, they also described survivors’ experience of anxiety, depression, post-traumatic stress and cognitive dysfunction.7,8 I wonder if we are preparing families with realistic outcomes since approximately one in three admitted to intensive care will survive out of hospital cardiac arrest, but many of whom will need intensive, tailored rehabilitation after discharge.9
CPR also becomes less effective as people age. In those over the age of 80, successful CPR is associated with a risk of substantial functional decline.10 People needed daily help with ADLs and could no longer live independently. However, most studies were inconsistent and did not have uniform endpoints. Most in hospital cardiac arrests, found an increased risk of poor neurologic function at discharge, but the variables measured were not the same.11 In many studies that show good quality of life for
survivors of CPR, cognitively impaired patients were not included in the data set and the review did not include a definition of QOL or what “good” or “acceptable” meant in relation to reported findings.12 Survivors of cardiac arrest might have sustained cognitive, emotional, and physical impairment which can reduce social participation, return to work, and adversely affect health-related quality of life.13
Again, I propose that CPR is not resuscitation. I believe we should stop asking the question, “Do you want to be resuscitated?” and replace this statement with questions that are more patient centered around their values while we give realistic expectations on what the road ahead will look like for an individual. Ask people what kind of lives they would value rather than asking “Do you want to be resuscitated?”
References
1. Vivian Lam, Cindy H Hsu. “Updates in Cardiac Arrest Resuscitation.” Emerg Med Clin North Am. 2020 Nov;38(4):755-769. doi: 10.1016/j. emc.2020.06.003.
2. Norkamari Shakira Bandolin, Weixiao Huang, Laurel Beckett, Garen Wintemute. “Perspectives of emergency department attendees on outcomes of resuscitation efforts: origins and impact on cardiopulmonary resuscitation preference.” Emerg Med J 2020 Oct;37(10):611-616. doi: 10.1136/emermed-2018-208084.

3. Lindsey Ouellette MPH, Amanda Puro MD, Jeffrey Weatherhead MD, Michael Shaheen MD, Todd Chassee MD, David Whalen MD, Jeffrey Jones MD. “Public knowledge and perceptions about cardiopulmonary resuscitation (CPR): Results of a multicenter survey.” Am J Emerg Med 2018 Oct;36(10):1900-1901. doi: 10.1016/j.ajem.2018.01.103.
4. Catherine A Marco, Gregory L Larkin. “Cardiopulmonary resuscitation: knowledge and opinions among the U.S. general public. State of the science-fiction.” Resuscitation 2008 Dec;79(3):490-8. doi: 10.1016/j. resuscitation.2008.07.013.
PALLIATIVE CARE COMMITTEE
>> COMMON SENSE MARCH/APRIL 2023 39
5. Shif Y., Doshi P., Almoosa K.F. “What CPR means to surrogate decision makers of ICU patients.” Resuscitation 2015; May;90:73-8. doi: 10.1016/j. resuscitation.2015.02.014.
6. Michael Colwill, Charlotte Somerville, Eric Lindberg, Caroline Williams, James Bryan,Ted Welman, Colwill M, et al.“Cardiopulmonary resuscitation on television: are we miseducating the public?” Postgrad Med J 2018;94:71–75. doi:10.1136/postgradmedj-2017-135122.
7. Gunilla Haydon, Pamela van der Riet, Jane Maguire. “Survivors' quality of life after cardiopulmonary resuscitation: an integrative review of the literature.” Scand J Caring Sci, 2017 Mar;31(1):6-26. doi: 10.1111/ scs.12323
8. M Schluep, H Endeman, B Y Gravesteijn, C Kuijs , M J Blans, B van den Bogaard, A W M M Koopman Van Gemert, C J Hukshorn, B J M van der Meer , A H M Knook,, T van Melsen, R Peters, K S Simons, G Spijkers, J W Vermeijden , E-J Wils , R J Stolker , S E Hoeks . “In-depth assessment of health-related quality of life after in-hospital cardiac arrest.” J Crit Care 2022 Apr;68:22-30. doi: 10.1016/j.jcrc.2021.11.008.
9. Gisela Lilja, Niklas Nielsen, John Bro-Jeppesen, Hannah Dunford, Hans Friberg, Caisa Hofgren, Janneke Horn, Angelo Insorsi, Jesper Kjaergaard, Fredrik Nilsson, Paolo Pelosi, Tineke Winters, Matt P. Wise and Tobias Cronberg. “Return to Work and Participation in Society After Out-of-Hospital Cardiac Arrest.” Circulation: Cardiovascular Quality and Outcomes. 2018;11:e003566. doi: 10.1161/ CIRCOUTCOMES.117.003566.
Continued from page 34
AGING WELL IN EMERGENCY MEDICINE INTEREST GROUP

and let them know that you are there to help them. It seems self-evident but spending quality time with them and helping them make connections with family and friends is essential to their wellbeing. Most of all take the time to talk to them, it helps with not feeling lonely. This connectedness is crucial to avoid losing their sense of purpose as mental health is strongly tied to physical health. Remaining socially involved is essential to maintain a sense of self-esteem and dignity while tapping into their experience and knowledge.
Caring for an elderly parent can be complicated and time consuming as many people must continue to tend to their jobs, children, and other
10. Daniel Kobewka, Tayler Young, Tolu Adewole, Dean Fergusson, Shannon Fernando, Tim Ramsay, Maren Kimura, Pete Wegierf. “Quality of life and functional outcomes after in-hospital cardiopulmonary resuscitation. A systematic review .” Resuscitation; 2022 Sep;178:45-54. doi: 10.1016/j. resuscitation.2022.07.011.5-54,
11. Gunilla Haydon, Pamela van der Riet, Jane Maguire. “Survivors’ quality of life after cardiopulmonary resuscitation: an integrative review of the literature.” Scand J Caring Sci; 2017 Mar;31(1):6-26. doi: 10.1111/ scs.12323.
12. Gavin D Perkins, Clifton W Callaway, Kirstie Haywood, Robert W Neumar, Gisela Lilja, Matthew J Rowland, Kelly N Sawyer, Markus B Skrifvars, Jerry P Nolan. “Brain injury after cardiac arrest.” The Lancet; 2021 October, 398: 1269-1278.DOI:https://doi.org/10.1016/S01406736(21)00953-3
13. Claudio Sandroni, Tobias Cronberg and Mypinder Sekhon. “Brain injury after cardiac arrest: pathophysiology, treatment, and prognosis.” Intensive Care Med (2021) 47:1393–1414. doi.org/10.1007/s00134-021-06548-2
responsibilities, as they also start trying to figure their new caregiving role. As much as it can be a rewarding experience it can become a source of stress as it changes family dynamics with siblings and others who may be involved. In addition, caregivers are potentially at an increased risk for adverse effects on their own wellbeing as far as their own health, quality of life, and economic implications. It can lead to exhaustion, feeling overwhelmed, and not having enough time for one’s own needs. The caregiver must be aware of self-care and learn to set boundaries, ask for help, and prioritize. It is important to try to maintain a balance between caregiving and tending to one’s own life.
PALLIATIVE CARE COMMITTEE
COMMON SENSE MARCH/APRIL 2023 40

COMMON SENSE MARCH/APRIL 2023 41
Overcoming Obstacles to Bystander CPR
Cara Gardner, MS* and David H. Gordon, MD †

ystander cardiopulmonary resuscitation (CPR) initiated in out-of-hospital cardiac arrest (OHCA) has shown to have tremendous benefits to neurologic function and survival. Bystander intervention with high quality chest compressions in the field have increased survival to hospital admission rates from 14.1% to 23%.1 Moreover, the number of patients who retained good neurologic function at hospital discharge following a OHCA nearly doubled from 8.7% to 16.8% with bystander CPR.1 This evidence supports the notion that bystander intervention plays a crucial role in successful resuscitation. Additionally, in a study comparing OHCA outcomes to those receiving mechanical circulatory support and those that did not, several patients survived neurologically intact with up to 120 minutes of low flow time when they were also put on ECMO.2
Roughly 75% of OHCA occur at home, compared to 25% in public. A recent analysis of the Cardiac Arrest Registry to Enhance Survival (CARES) database showed that 47.1% of arrests had CPR initiated by a lay person.3
The barriers to bystander CPR can be divided into patient level and rescuer level obstacles. First in regards to patient level obstacles, it was shown that patients who identified as Black and Hispanic were less likely than Caucasians patients to receive Bystander CPR.3 Other frequently reported barriers include patient being female sex, low socioeconomic status, and difficulty repositioning the patient.4
In regards to the rescuer level obstacles point of view, one main concern is the traumatizing experience bystanders endure during cardiac arrest— whether it be a loved one, neighbor, or stranger. Panic and hysteria are reported as one of the largest barriers for a bystander starting resuscitation efforts according to a study interviewing bystanders following a call to EMS dispatch. Results of another study showed 81.3% of bystanders delayed initiation of resuscitative efforts due to a perceived lack of knowledge and familiarity with how to perform CPR, including still believing that mouth to mouth is necessary.5 The average time for a bystander to confirm that there were no breaths during dispatcher-assisted CPR was 59 seconds shown by one study, which again may reflect bystander uncertainty
Bover who needs CPR.5 When seconds matter, the ability to recognize cardiac arrest and the confidence of the bystander in their ability to initiate resuscitation will save lives. With greater education we can overcome several of these barriers.

The International Liaison Committee on Resuscitation (ILCOR) has set a goal of 50% of cardiac arrests should get bystander CPR, as a result the world restart a heart day trained over 5.4 million people, but only 7900 of them in the U.S.6 Traditionally CPR has been taught in four hour Basic Life Support Classes. The time commitment itself can stop people from getting CPR education. However, hands only CPR and AED education can be only a minute away. The AHA and Red Cross have one to three minute long videos online for learning hands-only CPR and use of an AED.7,8,9 The American Heart Association (AHA) created an ultra-brief video lasting one minute that teaches hands-only CPR which was shown to participants in a research study. Individuals were significantly more likely to intervene as a bystander performing CPR immediately following the video, as well as individuals faced with simulated cardiac arrest two months later.10 These videos often do not go into and mollify the barriers to providing bystander CPR. Frequent exposures can mitigate the lack of familiarity that occurs as length of time from training increases. Use of brief repetitive educational CPR training videos in schools, workplaces, gas stations, airports, and even in the ED can break the above obstacles and barriers. These small changes will make a profound difference in the lives of our communities we save.
Countinued on page 50 >>
CRITICAL CARE MEDICINE SECTION
The barriers to bystander CPR can be divided into patient level and rescuer level obstacles.
COMMON SENSE MARCH/APRIL 2023 42
An Argument for Ultrasound in Cardiac Arrest
Melissa Myers, MD FAAEM and Kristine Jeffers, MD FAAEM

e all agree that a patientin cardiac arrest deserves the best possible treatment. If only we could all agree on what that treatment is. The role of ultrasound in cardiac arrest is controversial, with proponents citing the increased diagnostic accuracy and opponents the potential increase in pulse check time and thus a decrease in CPR effectiveness. We believe that point-of-care ultrasound (POCUS) should play a role in cardiac arrest, and thus disagree strongly with the recent International Liaison Committee on Resuscitation (ILCOR) recommendations against the routine use of ultrasound during cardiac arrest.1
The authors cite the valid concern of pulse check prolongation with the use of POCUS as a reason to avoid its use entirely. While initial studies did show increased pulse length with the use of POCUS, follow on research shown that with correct use POCUS can be used without prolonged interruption of CPR.2,3 With intentioned practice and planned evaluation it is possible to perform a full assessment without prolonging pulse checks.
The ILCOR recommendations are based on a systematic review which identified 12 studies of sufficient quality to be included a qualitative synthesis and none which they could include in a meta-analysis. The authors base their recommendations off these studies, which are extremely heterogenous and often not applicable in the ED. For example, one is a validation trial for a novel POCUS algorithm in cardiac arrest, an interesting paper which describes both potential harms and diagnostic benefits from ultrasound and does not attempt to make any definitive claims regarding the use of ultrasound in cardiac arrest.4 In addition, the exclusion criteria used excluded important
research in the field, including the landmark, multi-center REASON trial evaluating the use of ultrasound in cardiac arrest.5 The authors note in their discussion that POCUS does not have a high negative predictive value in cardiac arrest. They are correct but misunderstand the use of POCUS in this situation. Experts in POCUS agree that POCUS in cardiac arrest is often not
the full understanding of the limitations and the need to avoid increased pulse check time.7,8
a “rule out” exam, rather its utility is in finding evidence to support a potential diagnosis.
The utility of ultrasound in cardiac arrest is primarily to find a small group of patients which require interventions outside the usual algorithm. In the REASON trial, 34 patients out of a cohort of 793 patients were found to have a pericardial effusion, with 13 requiring a pericardiocentesis. This group, although small, had a significantly higher survival to hospital discharge than the rest of the cohort. In addition, the REASON trial demonstrate the utility of ultrasound in predicting outcomes in patients with cardiac standstill and avoiding futile resuscitation attempts.5 Ultrasound can be used to evaluate for right heart strain, which in the right clinical situation can direct early administration of thrombolytics.6 Experts in this field will argue for the use of ultrasound in cardiac arrest, with
The ILCOR recommendation against the routine use of ultrasound during cardiac arrest comes with a risk of missing intervenable causes of cardiac arrest with the potential to cause patient harm. When done by properly trained physicians with pre-prepared protocols POCUS in cardiac arrest can improve patient outcomes through the early diagnosis of reversible pathology and the avoidance of futile resuscitative outcomes.
References
1. Reynolds JC NT, O’Neil BJ, Drennan I, Issa M, Welsford M. Diagnostic Test Accuracy with Point-of-Care Ultrasound During Cardiopulmonary Resuscitation to Indicate the Etiology of Cardiac Arrest: Consensus on Science with Treatment Recommendations. Accessed January 28, 2023.
2. Gaspari R, Harvey J, DiCroce C, et al. Echocardiographic pre-pause imaging and identifying the acoustic window during CPR reduces CPR pause time during ACLS–A prospective Cohort Study. Resuscitation Plus 2021;6:100094.
Countinued on page 48 >> EMERGENCY ULTRASOUND SECTION
The ILCOR recommendation against the routine use of ultrasound during cardiac arrest comes with a risk of missing intervenable causes of cardiac arrest with the potential to cause patient harm.
COMMON SENSE MARCH/APRIL 2023 43
Dragon Slayer
Mary Claire O’Brien, MD FAAEM

Aresident confided to me that he is on a remediation plan.
“They say I am thinking too much,” he said. “I’m supposed to keep moving. Decide as soon as possible whether to admit or discharge. Push the consults! Be quicker about dispositions! Get the patients out of the ER! One way or the other, don’t think too much!”

This resident is a contemplative sort of guy. Telling him “not to think” is like telling him not to breathe.
“Hmm,” I said. “That’s not right. That makes you a glorified traffic cop.” The resident shook his head. “I don’t know,” he wavered. “It feels that way.”
“Listen,” I said. “I don’t walk into a patient’s room trying to decide right away whether or not they need to be admitted.
I’m
We Dragon Slayers have four weapons in the epic battle that is emergency medicine.
Weapon One: Discernment. I can tell, fast: is the patient sick or not sick? First I decide if the patient is really sick. I’d better slay that dragon before it eats the patient! I resuscitate. I can decide which dragon it is later. It is enough that I can tell it’s a dragon.
Weapon Two: Investigation. Ok, once the patient is stabilized, is the dragon known or not known? Do I recognize this pattern of illness? What exactly is going on? If they are not sick, I take a breath. I think! I think hard. What information do I need to figure this out, where is that information, and how do I get it?
Weapon Three: Skepticism. Are there any risk factors that would interfere with my ability to tell number one or number two? Extremes of age, immune suppression, mental illness, cognitive decline, substance use? Is it possible the patient or their family is lying, or withholding information? O’Brien’s Rule #2 of emergency medicine is “Watch your back.” Question everything.
Weapon Four: Integration. I am superb at putting it all together, in a hurry. So it’s not that I don’t think, it’s that I think fast. And I don’t mind re-thinking it all, when more information comes in that supportive or contradictory.
This is a one-on-one duel, friend, me, and the dragons, over and over, each patient, all day, every day. Be a Dragon Slayer.

ACADEMIC AFFAIRS COMMITTEE
We Dragon Slayers have four weapons in the epic battle that is emergency medicine.”
a dragon slayer, not a traffic cop. A Dragon Slayer.”
COMMON SENSE MARCH/APRIL 2023 44
PHYSICIANS SECTION Keeping the Flame Lit
Michelle Romeo, MD

Recently, the New York Times published an opinion essay, “Doctors Aren’t Burned Out From Overwork. We’re Demoralized by Our Health System.” It outlines what I presume many people would describe as burnout—this idea that we are losing a sense of purpose in our workplace and feeling that the work we do in actuality is not what we idealized it to be. The argument is that our demoralization stems from the systems we work in versus the conditions or patient care. The number of physicians suffering from some sort of burnout is staggering across the country and it forces us to take a lens to not only ourselves, but our departments and our country’s health care practices as a whole. I’ve always compared the emergency department to being the pulse of the community it is housed in. Moving to Philadelphia and starting my work as an attending in two Philadelphia neighborhoods where violence and drug use are some of the most common comorbidities of our patients has been quite the adjustment for me. There is the stress of being the one in charge, the stress of the continued shift work, the stress of learning new systems, and the stress of making a home in my new city. I find these stressors easily palatable. I love the energy of the ED, the hours allow my personal life the freedom I crave, the new systems to learn now are comfortable, and Philadelphia’s food and art scene swallowed me whole. What the unsavory part of my job entails are the discharges at 4:00am to the street because there is no social work on hours or intake shelter that is open 24 hours a day, the AMA of a patient who does not have health insurance and rather risk their life than be forced into an unmanageable hospital bill. The intolerable part is watching young people die by violence, directed at them or not, and hearing their families recount how guns have ruined their communities. It’s demoralizing to watch 20-year-olds come in with wounds so severe they end up with an auto amputation of their limb but leave the hospital before completing antibiotics because their withdrawals are a new degree of unmanageable.
My first year as an attending left me feeling anxious, uncertain, and overall depressed on the outlook of my ability to do this job for a long time. I was never trained on answers for housing insecurities, being uninsured, or managing family loss in the midst of a uniquely American gun problem. I knew I loved this work though, so I wasn’t going to let my flame burn out. I knew I had to find ways to keep it lit.
The first objective was taking care of myself. Seeing friends, family,

traveling, indulging in the art and food scene were all at the top of my list now that Covid has subsided, but so was restarting therapy, getting in a healthy workout and sleep routine, and incorporating meditation daily. Once I was in a space where I felt more whole and overall less anxious, I could do the work that I deemed necessary to help care for patients as much as I possibly could. I signed up to lead a lecture series for the second year residents. I dedicated the series to the social determinants of health with lectures devoted to understanding more about gun violence, the housing crisis, health of people suffering from homelessness, transgender health and more. There is no sense in being an advocate if you don’t understand what history has shaped where we are today. So along with the residents, I learn why some patients, some communities, and our nation may suffer uniquely compared to other societies. I connect with community experts, and not just those in Philadelphia. I look back at those I’ve met during my training: alumni, nurses, social workers and understand the work they are doing outside of the ED. Whether it be research to understand morbidity of living on the streets or setting up a van to help with needle exchange and laundry, learning more about their initiatives and real-world implementations allows me to figure out what holes in our system might be able to be filled and who we would need to talk to about it.
I’ve become more curious about politics than ever before. Understanding that politicians can control our state’s Medicaid dollars versus physicians or hospital systems was definitely an eye opener. Voting has never been more important to me, and advocating patients to vote and understand how it can affect their health has become entwined in my fall clinical days. I’ve learned that having an MD after your name makes your voice instantly a bit more credible, though we have seen how it can be abused. I’ve learned that being silent is no longer an option when it comes to my opinions on gun reform, public housing, and Medicare for all and writing has been not only a powerful outlet for my mental health but provides a message to the public of the reality we face in the emergency department.
I’m not suggesting you start submitting to the NYT or try to create new social initiatives overnight in your hospital, but I am asking you to examine your own “burnout” if you think you are experiencing it. What is demoralizing to you about the system? Is there a way to educate yourself and others about it? Find out what your city and hospital may be doing to assist in efforts to combat these issues. In doing this work, you may just find the spark that keeps you going.
YOUNG
COMMON SENSE MARCH/APRIL 2023 45
My first year as an attending left me feeling anxious, uncertain, and overall depressed on the outlook of my ability to do this job for a long time… I knew I loved this work though, so I wasn’t going to let my flame burn out.
Not Even the Sky is the Limit for Emergency Medicine
Leah Colucci, MD MS

ur former AAEM/RSA President, Haig Aintablian, is paving uncharted territory on a mission to bring emergency medicine to space! I did a brief interview with Haig to gather more information about the two year space medicine fellowship he is completing at UCLA.
Leah Colucci: Can you describe your career path to this point and what brought you to this fellowship?
Haig Aintablian: I have always been interested in space and space related things. Even as a child I would look at the stars through a telescope with my dad or go to the observatory. In medical school I would unwind by doing Milky Way photography in the deserts of Arizona. I also did a clerkship during the fourth year of medical school and continued to fall in love with space medicine. Things just aligned perfectly.
LC: What will you be doing long term in your career? What will the day to day look like?
HA: My primary goal will be to work clinical in the ED and first to always be as best a terrestrial physician as I can be. My other time will be spent advancing space medicine and the medical infrastructure to support expeditions for long duration space travel. Over the next 20 to 30 years as space travel increases, and the amount of people we send up with medical issues also increases, especially for private crews, I know that the role we have as physicians will increase exponentially.
OLC: What advice do you have for a medical student interested in this career path?
HA: I would suggest that you show your interest early and do whatever you can to get opportunities with our aerospace medical associations, and network. There is no clearcut easy path but with participation in these groups, opportunities will arise. Ultimately though you need to be a good terrestrial doctor first, so I suggest focusing on fine tuning your terrestrial clinical skills above all else.
LC: What other specialties could someone enter this career path from?
HA: Right now, our fellowship is only EM based, but there are preventative medicine pathways, that although different in their approach, do lead to physicians from different specialties in the space medicine world.
LC: What sort of medical problems are you preparing for in space?
HA: One of the biggest things that occurs in space is fluid shifts as the blood equilibrates instead of going to dependent areas. Overtime, that will cause structural changes to the body and create heart issues, vision issues, etc. Your immune system is weaker in space, so we have to be concerned for infections. Other
physiological changes might occur—for example, your appendix might not be in your RLQ so you might not experience pain in that area. Just like OBGYNs study disease during a unique physiological state of pregnancy we will do the same with the changes that occur with space travel. There will be similar things that we see on earth like vertigo, or things we rarely see like radiation exposure.
LC: How do you think this type of fellowship will impact our future workforce?
HA: It will open up even more opportunities for EM physicians and shows that we are a multi-talented physician that can do many things. We’re going to start seeing an explosion of this field in the next five to ten years as we start becoming multiplanetary. This field could be the piece that allows us to live on another planet, and it’s cool to see it being driven by EM.

LC: How could AAEM support this?
HA: AAEM can help recognize space medicine as a subspecialty. The principles of AAEM such as being led by a board certified physician are the same principles we have of space medicine. The creation and support of space medicine is beneficial to all subspecialties.
AAEM/RSA PRESIDENT’S MESSAGE
This field could be the piece that allows us to live on another planet, and it’s cool to see it being driven by EM.
COMMON SENSE MARCH/APRIL 2023 46
Care that Seeks to Affirm Life
 Alessandra Della Porta, MD*
Alessandra Della Porta, MD*

As a postgraduate year one (PGY-1) resident, every shift in the emergency department is still rife with “firsts.” The first time a patient codes, the first time pushing tPA, the first small bowel obstruction, the list goes on and on. One of the beauties of the intern year is that every shift, I have the opportunity to see a “first” that will shape my perception of an illness moving forward. One that is particularly memorable, is the first time I had a goals of care discussion with a patient and their family. A mid-sixties gentleman presented to our emergency department for chest pain. Unbeknownst to me at first contact, he had a history
Palliative care does not seek to hasten or prolong death, but to affirm life. Often misunderstood by patients and their families as a surrender to the disease process, or abandonment by medical care teams, palliative care engagement and referrals are often delayed to late stages of illness. When possible, referrals at time of diagnosis of a life limiting illness can offer patients significant comfort and improvement in quality of life, while supporting their families through death and bereavement. A study conducted in 2012 found that greater than 75% percent of patients visit an emergency room within the last six months of their lives. Whether for complications of their illness, or for management of associated symptoms, we have the opportunity to see terminally ill patients on a daily basis. Despite the frequency of their presentation, and our understanding of their disease course, emergency medicine physicians make up less than 5% of referrals to palliative care. There are several stated barriers to engaging in palliative care discussions in the emergency department, with the most commonly cited reasons including poor patient-provider rapport, inability to devote adequate time, and provider specific factors, such as discomfort with the topic or perceived knowledge deficits.
of aortic aneurysm with a chronic dissection. As any good intern would, after seeing his widened mediastinum on his chest radiograph and differing blood pressures in both arms, I ordered cross sectional imaging. Fast forward an hour or so, and I have a call out to cardiothoracic surgery, and am preparing myself to tell that patient about my concern and their likely need for emergent intervention. His simple response?
“I know.”
As it turns out, this patient had been seen prior at other hospitals for similar symptoms and been deemed a poor surgical candidate given their comorbidities. Despite the evidence of progression of their disease, my conversation with surgery ended with a surprising recommendation, “I would probably call palliative.” The discussion that followed is a first that had a meaningful impact on me and provided important insight into palliative care in the emergency department.
First, while it is undeniable that emergency medicine providers have limited interactions with patients compared to other specialties, I would argue that we have a unique ability to build rapport in the briefest of encounters. Furthermore, I would argue the rapport necessary to have an end of life discussion with a patient is no more than that of telling a loved one their family member has died, a practice which, while challenging, we all do. Second, we face the perception that the time it would take to devote to palliative care would be too great within the context of other clinical duties. A study of simulated ED based palliative care conversations found an average length of time for these discussions to be less than 12 minutes. I would, again, argue that this is likely no longer than the time we spend with families following a patient's death. While a fellowship trained hospice and palliative medicine physician, or those with similar specific training, will have broader and lengthier conversations with patients, they may not be available for referral at the time we evaluate a critically ill patient. Third, despite the fact that the American College of Emergency Physicians (ACEP) recognizes the identification of palliative care needs in ED patients as an important milestone in training, greater than a quarter of medical residents report that they do not feel comfortable having these discussions. Additionally, greater than 80% of residents agree that
AAEM/RSA EDITOR’S MESSAGE
Fast forward an hour or so, and I have a call out to cardiothoracic surgery, and am preparing myself to tell that patient about my concern and their likely need for emergent intervention. His simple response? “I know.
>> COMMON SENSE MARCH/APRIL 2023 47
knowledge of palliative care is a competency of emergency medicine and they would like to receive additional training in hospice and palliative care.
Finally, a provider's knowledge regarding identification of patients who would benefit from palliative care and the services available can be a challenge to engagement through the ED. Several ED-specific screening tools have been created to empower providers and bridge the aforementioned referral gap. A systematic review conducted in 2020 found 14 unique screening tools for identification of unmet palliative care needs in patients presenting to the ED. The most commonly utilized is termed “the surprise question” (i.e., would you be surprised if this patient died in the next 12 months?) which is a single question assessment to determine the need for referral. The surprise question has an ability to predict mortality at 12 months with a median sensitivity of 63% and a specificity of 75%. Despite these impressive test characteristics, validation studies have found that utilization of the surprise question alone may overestimate the number of patients needing referral. Furthermore, this test is binary and does not take into account the differing level of need that patients may have. Therefore, following a positive result, additional screening with other tools that take into account specific conditions and are symptom driven is reasonable. Two examples of such tools include P-CaRES (the Palliative Care and Rapid Emergency Screening) and SPEED (Screening for palliative needs in the emergency department).
In my case, we were ultimately able to have goals of care and code discussion with the patient and their loved ones at bedside. Our patient was able to be sent home with referrals for palliative care on an outpatient basis and medications aimed at providing comfort. While it is an unreasonable expectation for emergency providers to fulfill the role of palliative care, I would argue that we have the motivation, time, opportunity, and tool box to start end of life discussions and refer patients for the life affirming care they deserve.
Continued from page 43
EMERGENCY
3. Clattenburg EJ, Wroe PC, Gardner K, et al. Implementation of the Cardiac Arrest Sonographic Assessment (CASA) protocol for patients with cardiac arrest is associated with shorter CPR pulse checks. Resuscitation. 2018;131:69-73.
4. Lien W-C, Hsu S-H, Chong K-M, et al. US-CAB protocol for ultrasonographic evaluation during cardiopulmonary resuscitation: validation and potential impact. Resuscitation. 2018;127:125-131.
5. Gaspari R, Weekes A, Adhikari S, et al. Emergency department point-ofcare ultrasound in out-of-hospital and in-ED cardiac arrest. Resuscitation 2016;109:33-39.
6. Alerhand S, Sundaram T, Gottlieb M. What are the echocardiographic
References
*University of Cincinnati Medical Center - Emergency Medicine, PGY-1
1. Chang A, Espinosa J, Lucerna A, Parikh N. Palliative and end-of-life care in the emergency department. Clin Exp Emerg Med. 2022;9(3):253-256. doi:10.15441/ceem.22.341
2. Smith AK, McCarthy E, Weber E, et al. Half of older Americans seen in emergency department in last month of life; most admitted to hospital, and many die there [published correction appears in Health Aff (Millwood). 2012 Jul;31(7):1650]. Health Aff (Millwood). 2012;31(6):1277-1285. doi:10.1377/hlthaff.2011.0922
3. Shoenberger J, Lamba S, Goett R, et al. Development of Hospice and Palliative Medicine Knowledge and Skills for Emergency Medicine
Residents: Using the Accreditation Council for Graduate Medical Education Milestone Framework. AEM Educ Train. 2018;2(2):130-145. Published 2018 Mar 22. doi:10.1002/aet2.10088
4. George N, Bowman J, Aaronson E, Ouchi K. Past, present, and future of palliative care in emergency medicine in the USA. Acute Med Surg 2020;7(1):e497. Published 2020 Mar 18. doi:10.1002/ams2.497
5. Schmit JM, Meyer LE, Duff JM, Dai Y, Zou F, Close JL. Perspectives on death and dying: a study of resident comfort with End-of-life care. BMC Med Educ. 2016;16(1):297. Published 2016 Nov 21. doi:10.1186/s12909016-0819-6
6. Lamba S, Nagurka R, Zielinski A, Scott SR. Palliative care provision in the emergency department: barriers reported by emergency physicians. J Palliat Med. 2013;16(2):143-147. doi:10.1089/jpm.2012.0402
7. Lamba S, Pound A, Rella JG, Compton S. Emergency medicine resident education in palliative care: a needs assessment. J Palliat Med. 2012;15(5):516-520. doi:10.1089/jpm.2011.0457
8. Pajka SE, Hasdianda MA, George N, et al. Feasibility of a Brief Intervention to Facilitate Advance Care Planning Conversations for Patients with Life-Limiting Illness in the Emergency Department. J Palliat Med. 2021;24(1):31-39. doi:10.1089/jpm.2020.0067
9. Kirkland SW, Yang EH, Garrido Clua M, et al. Screening tools to identify patients with unmet palliative care needs in the emergency department: A systematic review. Acad Emerg Med. 2022;29(10):1229-1246. doi:10.1111/acem.14492
findings of acute right ventricular strain that suggest pulmonary embolism? Anaesthesia Critical Care & Pain Medicine 2021;40(2):100852.
7. Gottlieb M, Sundaram T, Olszynski P, Atkinson P. Just the facts: pointof-care ultrasound in cardiac arrest. Canadian Journal of Emergency Medicine. 2022;24(6):579-581.
8. Atkinson P, Bowra J, Milne J, et al. International Federation for Emergency Medicine Consensus Statement: Sonography in hypotension and cardiac arrest (SHoC): An international consensus on the use of point of care ultrasound for undifferentiated hypotension and during cardiac arrest. Canadian Journal of Emergency Medicine. 2017;19(6):459-470.
AAEM/RSA EDITOR’S MESSAGE
ULTRASOUND SECTION
COMMON SENSE MARCH/APRIL 2023 48
Emergency Medicine Fellowships
Mary Unanyan, OMSIV, AAEM/RSA Medical Student Council Chair

To do, or not to do a fellowship. That is the question you have already or will eventually ask yourself. Emergency medicine offers a variety of unique fellowship opportunities after residency. The decision to pursue a fellowship is often multifactorial—often depending on factors such as long-term career goals, family, financial, and more. Furthermore, it is a choice that residents should consider early in their training to better plot their career course. With so many fellowships to choose from, I thought it may be helpful to outline some of the popular emergency medicine fellowships available.

Administration
Administration fellowships train emergency physicians for department management and administration by helping them develop the administrative, quality, health policy, patient safety, research, and operational skills necessary to lead. These programs may be combined with a master’s in business administration or a master’s in medical management.
Critical Care and/or Trauma
Critical care and trauma fellowships are available to emergency medicine residents via multiple pathways such as through surgical, neurolical, internal medicine, or anesthesia. Each path may differ in where the majority of its focus is but generally those interested in critical care will be trained on how to better care for critically ill patients as well as how to better integrate critical care practices in the ED.
Emergency Medical Services (EMS)
These fellowships focus on the emergency medical services system including field care delivery, administrative oversight, offline and online medical direction, and disaster and event medicine training. The training can cover systems ranging from local to state to nation, and even to international. Furthermore, EMS fellowships differ significantly as they are catered to their environment and may have specific interests (e.g., disaster, tactical, search and rescue, etc.).
Hyperbaric and Undersea Medicine
This fellowship allows EM physicians to specialize in the operation of hyperbaric chambers, the use of hyperbaric oxygen therapies, and the medical aspects of deep sea diving.
Medical Education
Medical education fellowships will train emergency physicians with skills in curriculum design, education research, learning theory, excellent and innovative teaching, immersive learning, continuing medical education, and faculty development. Some programs combine medical education with a simulation component.
Pediatric Emergency Medicine
These fellowships train emergency physicians to better care for complicated and acutely ill pediatric patients.
Simulation
Medical simulation fellowships focus on building skills in simulation curriculum development and scenario design, development of debriefing and feedback skills, and exposure to procedural simulation training and education.
Social Emergency Medicine
Social EM fellowships focus on studying how social determinants of health impact patient’s ED presentation, with the goal of using that knowledge to improve the delivery of emergency care. Due to how broad the field of social EM is, each program varies in its specific area of focus.
Sports Medicine
A sports medicine fellowship focuses on the non-operative medical treatment of musculoskeletal injuries both on and off the athletic field. It can include performance of pre-participation evaluations and management of acute and chronic medical conditions in athletes.
Toxicology
Toxicology fellowships train EM physicians on the diagnosis, management, and prevention of poisonings. Examples include managing drug overdoses, envenomations, ingestions of plant toxins, chemical exposures, and drug withdrawal.
MEDICAL STUDENT COUNCIL CHAIR
>> COMMON SENSE MARCH/APRIL 2023 49
To do, or not to do a fellowship. That is the question…
Ultrasound
Ultrasound fellowships focus on the applicability and the teaching of ultrasound in the emergency department, while also exploring future facets of ultrasound in the ED. Fellows will learn how to perform and interpret basic and advanced ultrasound applications and apply them in clinical practice.
Wilderness Medicine
Wilderness medicine trains EM physicians to be able to provide care with limited resources in austere environments isolated from formal medical care. Programs can have specific foci such as hyperbaric and marine medicine, altitude related illnesses, orthopedics and wound care, tropical and travel medicine, hypothermia, and animal envenomations.
The above list is not exhaustive. Some other fellowships include: aerospace medicine, cardiovascular emergencies, forensics, geriatric, health policy, informatics, injury control, observation medicine, pain management, research, telemedicine, woman’s health, and more. With so many sub-specialties available, it is important for residents to explore their interests early on in their residency to better navigate what fellowship opportunities are available.
References
1. https://www.saem.org/about-saem/Services/fellowship-approval-program/
2. https://www.emra.org/books/fellowship-guide-book/i-title/
3. https://www.emra.org/embark/residents/fellowships/
References
* MS-III
†Attending Medstar- Washington Hospital Center
1. Cournoyer, Alexis, et al. “Clinical Outcomes Following Out-ofHospital Cardiac Arrest: The Minute-by-Minute Impact of Bystander Cardiopulmonary Resuscitation.” Resuscitation, Jan. 2023, p. 109693. DOI.org (Crossref), https://doi.org/10.1016/j.resuscitation.2023.109693
2. Mørk SR, Bøtker MT, Christensen S, Tang M, Terkelsen CJ. Survival and neurological outcome after out-of-hospital cardiac arrest treated with and without mechanical circulatory support. Resusc Plus. 2022 Apr 6;10:100230. doi: 10.1016/j.resplu.2022.100230. PMID: 35434669; PMCID: PMC9010695. https://pubmed.ncbi.nlm.nih.gov/35434669/
3. Garcia, R. A., Spertus, J. A., Girotra, S., Nallamothu, B. K., Kennedy, K. F., McNally, B. F., Breathett, K., Del Rios, M., Sasson, C., & Chan, P. S. (2022). Racial and ethnic differences in bystander CPR for witnessed cardiac arrest. New England Journal of Medicine, 387(17), 1569–1578. https://doi.org/10.1056/nejmoa2200798
4. Matsuyama, Tasuku, et al. “Willingness to Perform Bystander Cardiopulmonary Resuscitation: A Scoping Review.” Resuscitation Plus, vol. 4, Dec. 2020, p. 100043. DOI.org (Crossref), https://doi.org/10.1016/j. resplu.2020.100043
5. Clegg, G. R., Lyon, R. M., James, S., Branigan, H. P., Bard, E. G., & Egan, G. J. (2014). Dispatch-assisted CPR: Where are the hold-ups during calls to emergency dispatchers? A preliminary analysis of caller–dispatcher interactions during out-of-hospital cardiac arrest using a novel call transcription technique. Resuscitation, 85(1), 49–52. https://doi. org/10.1016/j.resuscitation.2013.08.018.
6. Böttiger BW, Lockey A, Aickin R, Carmona M, Cassan P, Castrén M, Chakra Rao S, De Caen A, Escalante R, Georgiou M, Hoover A, Kern KB, Khan AMS, Levi C, Lim SH, Nadkarni V, Nakagawa NV, Nation K, Neumar RW, Nolan JP, Mellin-Olsen J, Pagani J, Sales M, Semeraro F, Stanton D, Toporas C, van Grootven H, Wang TL, Wijesuriya N, Wong G, Perkins GD. Up to 206 Million People Reached and Over 5.4 Million Trained in
Cardiopulmonary Resuscitation Worldwide: The 2019 International Liaison Committee on Resuscitation World Restart a Heart Initiative. J Am Heart Assoc. 2020 Aug 4;9(15):e017230. doi: 10.1161/JAHA.120.017230. Epub 2020 Jul 30. Erratum in: J Am Heart Assoc. 2020 Dec 15;9(24):e014622. PMID: 32750297; PMCID: PMC7792236. https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC7792236/
7. https://www.youtube.com/watch?v=M4ACYp75mjU&ab_ channel=AmericanHeartAssociation
8. https://www.youtube.com/watch?v=-Yqk5cHXsko&ab_ channel=AmericanRedCross
9. https://www.youtube.com/watch?v=YWyU1IRaMGs&t=19s&ab_ channel=AmericanHeartAssociation
10. Bobrow, B. J., Vadeboncoeur, T. F., Spaite, D. W., Potts, J., Denninghoff, K., Chikani, V., Brazil, P. R., Ramsey, B., & Abella, B. S. (2011). The effectiveness of Ultrabrief and brief educational videos for training lay responders in hands-only cardiopulmonary resuscitation. Circulation: Cardiovascular Quality and Outcomes, 4(2), 220–226. https://doi. org/10.1161/circoutcomes.110.959353
11. Goyal, M., Dall, T., Tainsh, V., Konieczny, J., Garcia, O.E., Carlberg, D., A Teachable Moment: Clinically Stable Emergency Department Patients and Their Companions are Willing to Learn Compressiononly Cardiopulmonary Resuscitation. Abstract 18471. Circulation. 2015;132:A18471. https://doi.org/10.1161/circ.132.suppl_3.18471
12. Case, R., Cartledge, S., Siedenburg, J., Smith, K., Straney, L., Barger, B., Finn, J., & Bray, J. E. (2018). Identifying barriers to the provision of bystander cardiopulmonary resuscitation (CPR) in high-risk regions: A qualitative review of emergency calls. Resuscitation, 129, 43–47. https:// doi.org/10.1016/j.resuscitation.2018.06.001
13. Aldridge, E. S., Perera, N., Ball, S., Finn, J., & Bray, J. (2022). A scoping review to determine the barriers and facilitators to initiation and performance of bystander cardiopulmonary resuscitation during emergency calls. Resuscitation Plus, 11, 100290. https://doi.org/10.1016/j. resplu.2022.100290
MEDICAL STUDENT COUNCIL CHAIR
CRITICAL CARE MEDICINE SECTION
COMMON SENSE MARCH/APRIL 2023 50
Continued from page 42

COMMON SENSE MARCH/APRIL 2023 51
Early Management of Right Ventricular Dysfunction in the Emergency Department
Christine Yang, MD* and Pratik Doshi, MD †
Right ventricular dysfunction is important to recognize as early as possible, because routine resuscitative interventions that are a part of the emergency department (ED) course, such as early intravenous fluid administration for hypotension and emergent endotracheal intubation can cause rapid clinical deterioration in these patients.
Physical Exam
Physical exam findings that are suggestive of right sided ventricular involvement can be thought of the consequences of what would happen to the body if fluids were backed up from the right side of the heart. The lungs would be clear to auscultation with little evidence of pulmonary edema on chest x-ray, and the patient would not usually have escalating oxygen requirements. There may be peripheral edema such as bilateral lower extremity swelling, jugular venous distension, and abdominal ascites. However, keeping in mind that left sided heart failure is the most common cause of right sided heart failure and a mixed picture of all of the above symptoms in addition to pulmonary edema may also be seen. Pertinent laboratory findings may suggest congestive hepatopathy, as seen as elevated transaminases and bilirubin. Other laboratory values such as an elevated brain natriuretic peptide and elevated troponin may aid in diagnosis, however are not reliably the sole indicators of heart failure.
Pathophysiology
In order to think through the resuscitation of right ventricular dysfunction, it is important to recognize the key differences between the right and left ventricle. Just as the afterload of the left ventricle is equal to the systemic vascular resistance, the afterload of the right ventricle is equivalent to the pulmonary vascular resistance. The left ventricle has a thicker muscle wall compared to the right ventricle, and is able to tolerate a larger increase in systemic vascular resistance with only a minimal drop in stroke volume. The right ventricle is more sensitive to increased afterload, even a small increase in pulmonary vascular resistance can cause a large decline in right ventricle stroke volume and contractility.
The right ventricle is dependent on preload and therefore relies on adequate intravascular volume to maintain right sided filling pressures in order to sustain cardiac output. However, once volume reaches a point where an increase in RV volume results in a significant increase in right ventricle pressure, the highly compliant walls of the right ventricle can become overdistended.1
At this point, the right ventricle is unable to generate enough contractile force due to overstretching of the myocytes of the right ventricle. Tricuspid valve dilation can precipitate tricuspid regurgitation, causing worsening RV overdistension. This in turn eventually leads to interventricular septal shift that bows into the left ventricle, leading to reduced left ventricular preload and overall cardiac output. This is often referred to as the “right ventricle spiral of death.”
Precipitants of right ventricular failure can be divided into three categories: excessive preload (e.g. excessive volume administration, insufficient diuresis, etc.), excessive afterload (e.g. pulmonary hypertension, left ventricular dysfunction, pulmonary embolism, chronic obstructive lung disease, etc.), and depressed right ventricular contractility (sepsis, right sided myocardial infarction, etc.). Management of right ventricular failure should be directed towards correcting underlying reversible causes along with optimizing right sided filling pressures and reducing afterload.3
Optimizing Right Ventricular Preload
Fluid management in these patients must be given with consideration to the patient’s volume status. If low intravascular volume is suspected in the setting of normal pulmonary vascular resistance, fluid resuscitation is key to maintain adequate right sided filling pressures to maintain cardiac output. However, when right ventricular failure occurs in the setting of increased right ventricular afterload, the excess volume can result in displacement of the ventricular septum and impair left ventricular diastolic filling. Consider diuresing patients or dialysis as clinically warranted for removal of excess preload.3 In an acute decompensated heart failure the initial dose of diuretics depends if the patient is naive to diuretics or is on chronic diuretic therapy. If naive, beginning with intravenous 20-40 milligrams furosemide or its dosage equivalent twice daily is a reasonable first choice.6 If the patient is on chronic diuretic therapy, consider doubling the outpatient dose as the initial intravenous dose administered twice daily. Further dosing should be titrated according to the patient's urine output and reduction in symptoms. During diuresis, the patient's renal function and electrolytes should be closely monitored. Thiazide diuretics may also be used in conjunction with loop diuretics to overcome diuretic resistance. Patients with advanced kidney disease may require even higher doses of diuretics in order to achieve desired response. Patients who fail to respond to escalating diuretic therapy may require renal replacement therapy to mechanically remove intravascular volume.7 Point-of-care ultrasound is a quick and easy tool available in the emergency room that can be used to estimate right atrial pressure (RAP). An inferior vena cava (IVC) of less than or equal to 2.1cm and a collapsibility of greater than 50% indicates a normal RAP of 0-5mmHg. An IVC diameter of greater than 2.1cm and less than 50% inspiratory collapse indicates a high RAP of 10-20mmHg. However, these cutoffs cannot be applied to mechanically ventilated patients as the IVC will be dilated at baseline with no respiratory variations. Furthermore, the IVC ultrasound should be interpreted in conjunction with the overall clinical picture of the patient and should not be used as the sole indicator of fluid responsiveness.9
>>
COMMON SENSE MARCH/APRIL 2023 52
Optimizing Right Ventricular Afterload
Reducing right ventricular afterload should be aimed at identifying the reversible causes of increased pulmonary vascular resistance. Examples include initiating anticoagulants if pulmonary embolism is the source of right heart strain, administering bronchodilators if chronic obstructive lung disease is the cause, etc. Alveolar hypoxia induces pulmonary vasoconstriction and is worsened by hypercapnia and acidemia.3 Ideally, the SpO2 should be kept above 92% and PCO2 and pH are as close to physiologically normal as possible. Pulmonary vasodilators are typically reserved for primary pulmonary hypertension and no agents have yet been approved for treatment of right ventricular failure in a critically ill patient.3 Although not clearly evidence based, use of inhaled nitric oxide may be helpful in critically ill patients with right ventricle failure.
Optimizing Right Ventricular Contractility
Loss of contractile force of the right ventricle is primarily caused by three factors: overstretching of the myocytes of the right ventricle, derangements in cellular metabolism of myocytes, and insufficient oxygen delivery to myocytes of the right ventricle due to decreased coronary arterial perfusion such as in a right sided myocardial infarction. Fluid resuscitation can lead to acute right ventricular enlargement and lead to overdistension of the myocytes and further worsening of the distension as described above.1
To promote contractility of the right heart, the ideal vasopressor to use would be an agent that will increase the systemic arterial pressure without raising pulmonary vascular resistance. The goal of vasopressors is to increase contractility of the right ventricle and reduce right ventricular afterload, enhancing forward flow of blood in the ventricles.7 Norepinephrine acts on alpha-1 and beta-1 receptors, causing vasoconstriction and increase in myocardial contractility respectively. This is a reasonable first line choice in a hypotensive patient to restore mean arterial pressure.5 At low doses (less than 2mcg/min), norepinephrine has pronounced beta-1 effects and increases cardiac output. At higher doses (greater than 3mcg/min), this has pronounced alpha-1 effects and results in vasoconstriction with dose-dependent increases in systemic vascular resistance.10 Vasopressin stimulates V1 receptors on vascular smooth cells and at lower doses (0.01-0.03 U/min) can cause pulmonary vasodilation via stimulation of endothelial nitric oxide, however, at higher doses can induce pulmonary vasoconstriction.3 Epinephrine, a mixed alpha and beta agonist has also been shown to improve cardiac output without significant detrimental effects on pulmonary vascular resistance as well.3 Dobutamine is an inotrope that acts on beta-1 receptors to
improve myocardial contractility, however its stimulation of beta-2 can cause vasodilation and hypotension. Milrinone is a selective phosphodiesterase-3 (PDE-3) inhibitor that slows cyclic AMP metabolism that can increase inotropy and pulmonary vasodilation, however can also cause a drop in systemic vascular resistance. These last two agents are reasonable agents for a patient with normal blood pressures with concerns of impending cardiogenic shock.
Caution with Intubation
Spontaneous respirations causes decreased right ventricular afterload and higher preload ventricular preload, both which are helpful for improving forward flow in right ventricular failure. Positive pressure ventilation has the potential to cause an acute increase in right ventricle afterload, leading to dilation of the right ventricle and causing ventricular wall stress.4,8 Intubation can cause an acute drop in cardiac output, leading to peri-intubation hypotension and cardiac arrest. If possible, consider other noninvasive modalities and avoid intubation if at all possible.
References
*PGY-2 Louisiana State University Baton Rouge and Pratik Doshi †McGovern Medical School Associate Professor, Division of Critical Care
1. Crager SE, Humphreys C. Right ventricular failure and pulmonary hypertension. Emergency Medicine Clinics of North America. 2022;40(3):519-537.
2. Luecke T, Pelosi P. Clinical review: Positive end-expiratory pressure and cardiac output. Crit Care. 2005;9(6):607-621. doi:10.1186/cc3877
3. Ventetuolo CE, Klinger JR. Management of acute right ventricular failure in the intensive care unit. Ann Am Thorac Soc. 2014;11(5):811-822.
4. Wanner PM, Filipovic M. The right ventricle—you may forget it, but it will not forget you. J Clin Med. 2020;9(2):432.
5. Mandras SA, Desai S. Right heart failure. In: StatPearls. StatPearls Publishing; 2022.
6. Suri SS, Pamboukian SV. Optimal diuretic strategies in heart failure. Ann Transl Med. 2021;9(6):517-517.
7. Konstam MA, Kiernan MS, Bernstein D, et al. Evaluation and management of right-sided heart failure: a scientific statement from the american heart association. Circulation. 2018;137(20):e578-e622.
8. Alian AA, Shelley KH. Respiratory physiology and the impact of different modes of ventilation on the photoplethysmographic waveform. Sensors. 2012;12(2):2236-2254.
9. Argaiz ER, Koratala A, Reisinger N. Comprehensive assessment of fluid status by point-of-care ultrasonography. Kidney360. 2021;2(8):1326-1338.
10. Smith MD, Maani CV. Norepinephrine. In: StatPearls. StatPearls Publishing; 2022.
EARLY MANAGEMENT OF RIGHT VENTRICULAR DYSFUNCTION IN THE EMERGENCY DEPARTMENT
COMMON SENSE MARCH/APRIL 2023 53
The FDA approval of Nalmefene HCl Injection has given healthcare professionals an additional treatment option for the management of known or suspected opioid overdose . However, there is limited data on the use of Nalmefene HCl Injection in today’s op ioid overdose environment.
Proposals to be considered for this RFP should explore outcomes associated with the use of Nalmefene HCl Injection
Instructions for Submission of Research Proposals
Sponsor investigator applicants must submit their CV and a brief letter of intent (i.e., 1-2 pages) outlining the study concept via email to iitprogram@pharma.com by 5:00 PM ET April 30, 2023. The letter of intent should include:
» Sponsor/investigator CV
» Institutional affiliation/Study Site(s)
» Research Objective(s)
» Study design, methods
Proposal Review and Response
» Target population(s)
» Endpoints and intended analysis
» Estimated study duration and preliminary budget
» Anticipated drug supply required and any funding request
Applicant proposals will be evaluated by a medical and scientific review committee. Selection of proposals will be based on medical and scientific merit, feasibility, and investigator/site qualifications. Review focus will also be on innovation, cost -efficiency, and translatability to medical practice. Following initial Letter of Intent review, a selected set of applicants will be asked to submit a full study proposal which includes a line ‐item budget reflective of the fair market costs for executing the research
Financial support and/or drug supply will be issued based upon a fully executed agreement. All approved projects are expected to result in publication of findings in a peer‐reviewed journal.
Sponsor Investigators must be willing to assume regulatory responsibility for the research including obtaining an IND or exemptions granted by FDA as applicable.
Important Information A bout Nalmefene HCl Injection
Nalmefene HCl Injection, a sterile solution containing 2 mg/2 mL (1 mg/mL) in vial form for intravenous, intramuscular, and subcutaneous injection, was FDA approved in February 2022.
Indications and Usage : Nalmefene HCl Injection is an opioid antagonist indicated for the complete or partial reversal of opioid drug effects, including respiratory depression, induced by either natural or synthetic opioids. Nalmefene HCl Injection is indicated in the management of known or suspected opioid overdose. 1

Contraindications : Nalmefene HCl Inj ection is contraindicated in patients with a known hypersensitivity to the product. 1
Warnings and Precautions : Nalmefene HCl Injection is associated with the following Warnings and Precautions: Use of Nalmefene in Emergencies, Risk of Recurrent Respiratory Depression, Cardiovascular Risks with Narcotic Antagonists, Risk of Precipitated Withdrawal, Incomplete Reversal of Buprenorphine, and Use in Pediatric Patients. Patients treated with Nalmefene HCl Injection should be observed until, in the opi nion of the physician, there is no reasonable risk of recurrent respiratory depression.1
Adverse Events : The most common adverse reactions (>1%) reported in clinical trials with Nalmefene HCl Injection were nausea (18%), vomiting (9%), tachycardia (5%), h ypertension (5%), postoperative pain (4%), fever (3%), and dizziness (3%). 1
Please consult the Nalmefene HCl Injection Full Prescribing Information found here for complete product information . 1
Questions regarding the process/requirements for submitting may be sent to: iitprogram@pharma.com
Reference 1: Na lmefene HCl Injection [Full Prescribing Information]. Stamford, CT: Purdue Pharma L.P. MR-08293
COMMON SENSE MARCH/APRIL 2023 54
Leveraging AMA and State Medical Society Memberships toward Advocacy for and by Physicians: Some Success Stories from the November 2022 Interim Meeting of the American Medical Association House of Delegates
Gary M. Gaddis, MD PhD FIFEM MAAEM FAAEM
 The Advocacy Channel
The Advocacy Channel
Overview
I write to inform AAEM members of some recent and successful advocacy I have made within the House of Delegates (HOD) of the American Medical Association (AMA), chiefly regarding gaining the official support of the AMA to work toward the elimination of “waiver of due process” (WODP) clauses in health care worker employment agreements.
I also led advocacy concerning two other matters. One was to place the AMA more firmly and expansively on record in support of the need to eliminate asking doctors if they are receiving mental health care as a condition of licensure or credentialing. The other regards the wisdom of renewing and expanding efforts to mitigate violence in health care workplaces.
I believe this information will be favorably received by most AAEM members. As you read this narrative, I hope you will find that its words facilitate you to seek membership and involvement in your own state’s medical society, and in the AMA.
Waiver of Due Process Clauses in Employment Agreements
Many members of AAEM believe WODP clauses need to be eliminated or voided in all health care worker employment contracts. This position is consistent with the aspirations of our American Academy of Emergency Medicine (AAEM).
When one is burdened by a WODP in one’s employment agreement, one can be fired at will and without “cause” by one’s supervisor. Thus, the “truth” becomes whatever one’s supervisor says it is, whether or not that “truth” is factual! Doctors need due process protections to be able to confidently advocate for patients and other health care workers, without the fear of angering someone in the “C-Suite” and then being fired or “disappeared from the schedule.” This is so because doctors work at the patient care interface where problematic if not dangerous health care institution policies, procedures and practices can most rapidly be identified.
Acting on this belief, I accomplished successful advocacy in the form of a resolution I developed and wrote about this topic. My “Anti-WODP” Resolution was officially submitted, considered, and adopted during the November 2022 Interim Meeting (Interim) of the American Medical Association House of Delegates in Honolulu. My hope is that the AMA,
with a much larger public presence than our AAEM, may be more ideally poised to successfully advocate for the permanent elimination of these pernicious WODP clauses than is AAEM, now that this AMA resolution has been adopted as a “Directive to Take Action.”
This resolution directs the AMA to facilitate and enable federal legislation that would prohibit WODP clauses in future health care worker employment contracts, while voiding them in current agreements. This goal is consistent with legislation that was introduced in the 116th Congress, which ended in January of 2021. That proposed bill, the “ER Hero and Patient Safety Act”, also known as HR 6910 of the 116th Congress, did not gain a hearing after its introduction. However, with its adoption of the WODP resolution that I originated, the AMA is officially “on-board” as regards engaging actively in useful future advocacy on this matter. Further, as the proposed resolution was being debated, I was pleased to learn that the AMA has already been developing model legislation for future dissemination to legislative bodies regarding WODP clauses. Such legislative proposals, once enacted, would prohibit and void any such WODP language in physicians’ employment agreements.
The path to adoption of this resolution was typical for AMA processes. I had previously, formally and personally, presented this “WODP” resolution I authored to the Missouri State Medical Association (MSMA) at its annual meeting in April of 2022. After discussion, MSMA formally adopted my resolution exactly as I wrote it. Next, MSMA officially offered the resolution for consideration by the national AMA HOD. Once the HOD convened, the AMA Reference Committee (RefComm) “B,” the RefComm relevant to this resolution, heard testimony concerning it. That testimony was unanimously supportive. The RefComm considered this testimony and then recommended the resolution for adoption after a slight amendment of wording. Finally, on November 14th, the AMA HOD formalized its stance regarding the evils of WODP clauses. AMA formally adopted Resolution 205 not simply as a policy or as an opinion, but as a “directive to take action.”
Other Advocacy
The encouraging result regarding WODP matters was not the only useful matter I put before the HOD in 2022. I also authored two other Resolutions that received a favorable response.
Physicians and Mental Health
I created the original language of what became adopted by the AMA
>> COMMON SENSE MARCH/APRIL 2023 55
HOD as Resolution 228 “Requirements for Physician Self-reporting of Outpatient Mental Health Services, Treatments, or Medications to Credentialing Agencies and Insurers.” The path to the AMA’s HOD for this resolution proposal was via AMA’s Academic Physicians Section (APS), within which I have a leadership role. Here is how that came to pass.
I am a Past Chair of the Governing Council (GC) of APS, and I currently serve as APS’s Alternate Delegate to the AMA HOD. One of the useful changes I have been able to lead within APS (which contrary to the expectations or beliefs of many does not simply serve merely as a “Deans’ Club” within the AMA) is that APS should appropriately concern itself with the practice environments into which academic medical centers send their trainees. This is a new “expansion of our lane,” if you will, for APS, and an expansion for which I am chiefly responsible.
I submitted the first draft of Resolution 228 to APS, targeting it for eventual official submission by APS to the AMA HOD. Then, I led APS as it discussed, amended, and finally adopted language for what became Resolution 228. Once officially adopted by the APS, the resolution became eligible for forwarding to the full HOD for its consideration.
Resolution 228 advocates that most questions regarding a doctor’s receiving outpatient mental health services are not germane to credentialing processes, and should not be asked unless the goal is to reveal a mental health matter that represents a probable cause for a physician’s impairment. You may or may not know that it was already prior AMA policy to advocate that “incriminating” questions regarding the prior receipt of mental health care services without an impairing degree of severity, such as a current need for inpatient mental health care, should not be among the questions asked at the time of state medical licensure or re-licensure. Indeed, a slight majority of states have subsequently followed AMA’s suggestions in this matter.
The “Whereas” clauses that helped Resolution 228 gain support noted that physicians are humans, humans develop diseases, diseases are best borne if managed rather than if ignored, and some of those diseases that occur among health care workers are diseases of mental health. Most of these mental health matters can be successfully managed on an outpatient basis. Thus, the receipt of outpatient mental health services by a physician should not be considered as an impairment.
Indeed, to receive mental health care, if indicated, should be encouraged and not discouraged for those doctors who need that care. This is especially timely with the current pervasiveness of “burnout,” a condition which can pre-dispose to clinical depression, a manageable disease. Further, the American people have already demonstrated a formal interest in the matter via the passage of HR 1667 of the 117th Congress, the Lorna Breen Health Care Provider Protection Act. You probably recall the tragic death by suicide of Dr. Lorna Breen in the first half of 2020, in the time of peak burdens due to COVID-19 disease on the health care system. Approximately 300 American physicians die by suicide every year. The act enables useful changes as regards the mental health of
physicians and other health care workers.
Finally, it is arguable that to ask most mental health questions of physicians may not only be a violation of the Americans with Disabilities (ADA) Act, but they are also a form of discrimination. I will explain how these questions are discriminatory. A doctor who is a “brittle diabetic” may be unsuited to making medical decisions with a blood glucose of 40mg%. A doctor with a body mass index of 45 may not be able to move quickly and effectively through the hospital, or may crowd out others on the care team when providing care to a patient. Yet, no state singles out diabetes or obesity as a potentially impairing condition which must be revealed as a condition of licensure. There is no reason to use discriminatory and unscientific practices to make pariahs of the doctors who have had the wisdom and judgment to seek mental health care, when that care is indicated.
With these factors in mind, I was able to first persuade the AMA APS GC, and then the AMA HOD, of the following wording which gives AMA a “directive to take action.” That action is to extend its prior policy regarding the matter of requirements to reveal non-impairing conditions to state licensure boards more broadly to hospitals (via advocacy for a new requirement to be imposed upon hospitals by the Joint Commission), insurers, and specialty boards (via advocacy to them). Without broadening the advocacy, those irrelevant and counter-productive questions that stigmatize doctors who receive outpatient mental health services would be perpetuated, and doctors would continue to be actively discouraged from obtaining needed care.
As you will notice, the resolution also extends to discussion of matters of doctors who are under the supervision of a state’s “physician health program.” Here is the exact wording of this resolution:
RESOLVED, That our American Medical Association compile a report summarizing which states have implemented the suggestions that medical boards should not require disclosure of mental health conditions as a condition for re-licensure, as listed in Policy 35 H-275.945, “Self-Incriminating Questions on Applications for Licensure and Specialty Boards” (Directive to Take Action); and be if further
RESOLVED, That our AMA advocate to applicable organizations, such as the Federation of State Medical Boards and The Joint Commission, that state licensure boards, hospital credentialing committees, private and public health insurers and medical specialty boards refrain from asking whether physicians are currently receiving outpatient mental health care while continuing to ask whether they are currently impaired, as stated in AMA Policy H-295.858 (2), “Access to Confidential Health Services for Medical Students and Physicians” (Directive to Take Action); and be it further
RESOLVED, That our AMA advocate to applicable organizations, such as Federation of State Medical Boards and Joint Commission, that Substance Use Disorder (SUD) conditions currently managed with the assistance of a state’s Physicians’ Health Program (PHP) (or similar
SOME SUCCESS STORIES FROM THE NOVEMBER 2022 INTERIM MEETING OF THE AMERICAN MEDICAL ASSOCIATION HOUSE OF DELEGATES >> COMMON SENSE MARCH/APRIL 2023 56
entity) need not be reported on applications for re-credentialing by state licensure boards, hospital credentialing committees, private and public health insurers and medical specialty boards, because participation in a PHP ensures strict accountability on the part of physicians with a history of SUD, with this accountability enabling these physicians to such successfully and safely re-engage in the practice of medicine. (New HOD Policy)
The rationale for asking for involvement of the Joint Commission (JC) is that once we gain its support, the JC has the power to mandate useful, humane, and non-discriminatory credentialing practices by the health care organizations which it accredits. In this manner, any need for doctors and other health care workers to win victories slowly and haltingly regarding hospital credentialing practices, hospital system by hospital system, could be obviated. When I engage in controversial topics, I seek the most rapid means to eliminate the controversy, and this proposed path through the JC to each hospital is an example. Further, the JC is more likely to include influential members less likely to be subject to anti-mental health care prejudices that may characterize a hospital system’s lay public board members.
Workplace Violence
Finally, I presented a resolution concerning workplace violence, in response to the increasingly pervasive armed intruder violence that infiltrates health care institutions, which are designed for the purpose of healing. This violence was most tragically expressed during 2022 in the fatal shootings at Saint Frances Hospital in Tulsa, Oklahoma in June, and at a Labor and Delivery unit in Methodist Dallas Medical Center in Texas in October. These and other events led to the presentation of an Educational Forum during the AMA Interim Meeting, “Workplace Violence in Health Care Settings,” which was organized by the Surgical Section of the AMA.
Once I learned of this Educational Forum, I crafted a late resolution proposing an “AMA Study of Efficacy of Requirements for Metal Detection/ Weapons Interdiction Systems in Health Care Facilities.” My proposed resolution was debated, amended, and then adopted by APS of AMA, as another example of how APS feels comfortable “expanding its lane” and making advocacy not only for the students, residents, and fellows that we train, but indeed, for all health care workers and for all patients. The proposed resolution was then submitted to the HOD for its consideration. When APS shared the language of this proposed resolution, we encountered skeptics. One in particular noted that their home state, Texas, has an “open carry” law that would make uniform metal detection scanning of those who enter a hospital problematic to enforce.
That and other similar skepticism carried over to the larger group assembled at the RefComm hearing, which voted that it should be referred for further consideration. It was noted that the Council of Science and Public Health has studied this matter on two separate occasions. Both times their conclusions supported a local, tailored approach that considers local laws, jurisdictions, and risk factors. The Council did not find comfort
in advocating a blanket approach for every hospital and care setting. I am not content to leave this matter unresolved. Two factors weigh heavily in my decision.
The first factor is that even in states with open carry laws such as Texas, airports have uniformly retained the ability to utilize metal detection equipment for weapons interdiction. In other words, a national solution has been enabled and adopted to address a critical issue in a manner that overrides existing state laws. Airports are not the only places where a national solution to a weapons problem is indicated. Health care institutions are ripe for a similar national solution.
The second factor lies in the Constitution of the United States. The 10th Amendment, the “Supremacy Clause,” would enable a national solution. The “Supremacy Clause” helps adjudicate conflicts in which state laws contradict federal laws. In these cases, the federal law supervenes. Thus, if there were to be a federal law regarding this matter of how to make health care environments safer by outlawing the bringing of weapons into health care environments, the “Supremacy Clause” would enable the application of such a law in every state and territory, contradictory state laws notwithstanding.
I will raise this point to the Council of Science and Public Health between now and the June 2022 annual meeting of the AMA HOD, because it has apparently not been considered previously. The problem of firearms deaths being inflicted in hospitals is not new. The first of which I am aware is when a disgruntled patient entered the emergency department (ED) at the University of Kansas Hospital in Kansas City, KS and murdered a psychiatry resident and a member of the ED’s clerical staff. That tragedy occurred in the early 1980s, when I was a medical student. It seems that we should have had sufficient time to learn from prior oversights and remediate them in a useful fashion.
Another Item of Interest
Resolution 219, introduced by the delegates of the Mississippi State Medical Society, was titled, “Hold Accountable the Regulatory Bodies, Hospital Systems, Staffing Organizations, Medical Staff Groups, and Individual Physicians Supporting Systems of Care Promoting Direct Supervision of Emergency Departments by Nurse Practitioners.”
The proposed resolution was supportive of the goals inherent in its title. Its spirit and general goals received strong support from ACEP members when it was debated at RefComm B. No one spoke against the wisdom of advocating for physician-led care in emergency departments. However, AMA has no enforcement powers and thus cannot hold any one person or any group of people as accountable. It was also noted that current AMA policy already advocates that physicians should lead care teams, including emergency department care teams.
The RefComm that heard testimony thus recommended that Resolution 219 be adopted as amended by the RefComm before presenting it to the HOD. However, after debate and discussion on the floor of the HOD, the
SOME SUCCESS STORIES FROM THE NOVEMBER 2022 INTERIM MEETING OF THE AMERICAN MEDICAL ASSOCIATION HOUSE OF DELEGATES Countinued on page 60 >> COMMON SENSE MARCH/APRIL 2023 57
Utility of Haloperidol and Droperidol in Cannabinoid Hyperemesis Syndrome
Clinical Question: What is the evidence for use of haloperidol or droperidol as the primary therapy for management of cannabinoid hyperemesis syndrome?
Introduction
First described in 2004, cannabinoid hyperemesis syndrome (CHS) is a syndrome of cyclic vomiting related to chronic cannabis use.1 With no objective diagnostic test to diagnose CHS the difficulty in identifying this syndrome typically results in multiple ED visits with excessively high resource utilization.2-4 Long-term treatment of CHS is abstinence from cannabis, but acute symptomatic management has been a struggle for many clinicians, without any universally agreed-upon best treatment strategy.5 Antipsychotics, namely haloperidol, have been used successfully in the past as an antiemetic by both oncologists and general surgeons and has achieved recognition for their potential utility in treating CHS.
Wesley Chan, MD, Christianna Sim, MD MPH, Christopher Kiang, MD, and Victoria Zaccone, MD Editors: Donald Doukas, MD and Kami M. Hu, MD FAAEM patients, another with four. Another review of ED visits after cannabis described the use of various medications but did not provide treatment response rates. In the 12 case series, benzodiazepines (n=6), haloperidol (5), and topical capsaicin (5) were the most frequently reported as helpful, with olanzapine also reported once as efficacious. Out of the 44 case reports, benzodiazepines (5), metoclopramide (4), and haloperidol (4) were reported most frequently as effective. The authors note that hot showers or baths were mentioned across all of the case series and case reports as effective in managing CHS.
Overall, this article served primarily to highlight the lack of high-quality evidence in the management of CHS and was a descriptive look at therapies tried without the ability to offer much insight into efficacy. The authors noted the complexity of the endocannabinoid system and hypothalamic-pituitary-adrenal axis regulation. Various cannabinoid, GABA, dopamine, and serotonin receptors have their roles, which all the aforementioned medications modulate at some level.
Richards JR, Gordon BK, Danielson AR, Moulin AK. Pharmacologic Treatment of Cannabinoid Hyperemesis Syndrome: A Systematic Review. Pharmacotherapy. 2017;37(6):725-734.
Richards et al. sought to determine the most used pharmacologic therapies in the treatment of CHS. Their literature search included all human trials, case reports, and case series for the pharmacologic treatment of CHS. Data was pooled from a myriad of sources, including Medline, PsychINFO, Cochrane Library, CENTRAL, and DARE, while references of any relevant report were also hand-screened. Due to the limited number of relevant trials with a wide heterogeneity of pharmacologic therapies and study durations, the data was analyzed qualitatively and a meta-analysis was not performed.
A total of 1262 articles were reviewed with 63 meeting the inclusion criteria: four prospective trials, three retrospective case-control or cohort studies, 12 case series, and 44 case reports. One prospective study examined tricyclic antidepressant (TCA) therapy in the treatment of cyclic vomiting syndrome (CVS), including 34 patients with chronic cannabis use, 25 (74%) of which responded favorably to TCAs, although several also quit using cannabis, and it was not clear that TCAs were helpful in acute hyperemesis management. Another prospective study found that use of TCAs in CVS resulted in a decrease in symptoms and occurrence of hyperemesis at three months, with less success in the CHS cohort. For acute therapy in the ED, benzodiazepines were suggested as the most effective therapy without clear data given, and a separate study indicated that cannabis users responded to various antiemetics, lorazepam, and hydromorphone without much supplemental data.
The retrospective studies included few cannabis users, one with three
Witsil JC, Mycyk MB. Haloperidol, a Novel Treatment for Cannabinoid Hyperemesis Syndrome. Am J Ther. 2017;24(1):e64-e67.
In this single-center retrospective case series, the authors reviewed the use of haloperidol in cannabinoid hyperemesis syndrome. Data was collected over a three month period, and eligible subjects were identified by the documented chief complaint or final ED diagnosis. Patients were only included if they admitted to chronic long-term cannabis use and admitted to compulsive bathing habits, which the authors felt was diagnostic of CHS. Additional inclusion criteria included cyclical vomiting with failure of outpatient antiemetics, multiple ED visits without other identified cause, and receipt of haloperidol as a treatment specifically for cyclical vomiting.
Four patient cases met the inclusion criteria, all males, aged between 20-50 years old, with multiple ED visits. All were treated with a combination of IV hydration, ondansetron, metoclopramide, and chlorpromazine. All were discharged within eight hours of receiving haloperidol as the last therapy, and the authors noted that none of the cases needed a repeat dose of haloperidol.
The authors acknowledge the limitations of the small retrospective case series, and note the possibility of missed patients eligible during that study period because of potential medical coding errors. The medications given to patients prior to haloperidol were neither controlled nor blinded. Interestingly, the authors also hypothesized a role for a formal psychiatric evaluation to determine whether haloperidol’s pharmacologic benefits are related specifically to the organic treatment of hyperemesis
>>
AAEM/RSA RESIDENT JOURNAL REVIEW
COMMON SENSE MARCH/APRIL 2023 58
AAEM/RSA RESIDENT JOURNAL REVIEW
to the treatment of underlying psychiatric illness.
Lee C, Greene SL, Wong A. The utility of droperidol in the treatment of cannabinoid hyperemesis syndrome. Clin Toxicol (Phila). 2019;57(9):773-777. In this single-center, retrospective observational study conducted in Australia, where droperidol is more readily available, the authors sought to assess if the use of droperidol decreased the overall hospital length of stay in patients with CHS. Though 689 records were identified, only 76 met the criteria for CHS and were included in the study. Of these, 37 were treated with droperidol and 39 were not. The other medications used in both groups were reported including other antiemetics (e.g., metoclopramide, ondansetron), opiates (morphine, oxycodone), benzodiazepines (diazepam), and topical capsaicin cream.
Despite the small sample size, the authors found a statistically significant difference in the primary outcome, the median length of stay: 6.7 hours (IQR 4.7, 11.9) in the droperidol group versus 13.9 hours (IQR 5.2, 57.3) in the no-droperidol group (p=0.014). They also report significant differences in their secondary outcomes, which include the median length of time to discharge after final drug administration and total doses of antiemetics administered. The median length of time to discharge after final drug administration in the droperidol treatment group was 137 minutes (IQR 65, 203) versus 185 minutes (IQR 149, 403) in the no-droperidol treatment group (p=0.002). The median number of antiemetics used before droperidol was one (n=1, IQR 0, 1.5) versus zero after droperidol (n=0, IQR 0, 1) (p=0.02). There were no adverse cardiac events reported with use of droperidol, but there were two cases of drowsiness and one dystonic reaction which resolved with benztropine.
Limitations of this study include its single-center nature and very small sample size, as well as the fact that there was no standardization of treatment arms, all of which make it difficult to draw definitive conclusions. These issues aside, the results seem promising that droperidol may shorten the time to ED discharge while reducing the amount of medication required to improve symptoms.
Ruberto AJ, Sivilotti MLA, Forrester S, et al. Intravenous Haloperidol Versus Ondansetron for Cannabis Hyperemesis Syndrome (HaVOC): A Randomized, Controlled Trial. Ann Emerg Med. 2021;77(6):613-619.
The HaVOC trial examined the effectiveness of haloperidol compared to ondansetron in treating cannabis hyperemesis syndrome. The study randomized cannabis users presenting with presumed CHS in a triple-blind crossover trial to either IV ondansetron 8mg or IV haloperidol at a dose of either 0.05 or 0.1mg/kg. The primary outcome was the reduction from baseline abdominal pain and nausea at two hours after treatment, using the 10-cm visual analog scale (0=none, 10=worst), with 2cm difference as a widely-established threshold for meaningful symptom difference.
The study population included adults at least 18 years old who experienced three or more episodes of cyclic emesis separated by more than
one month during the preceding two years and near-daily to daily use of inhaled cannabis for six or more months. Additionally, patients were required to present with two or more hours of ongoing witnessed emesis or retching, and could not have received an IV antiemetic, antipsychotic, or anticholinergic medication other than up to 100mg of dimenhydrinate in the previous 24 hours. Pregnant patients were also excluded.
A total of 33 patients were randomized, with similar baseline demographic and physical characteristics between the haloperidol and ondansetron groups. The investigators found that haloperidol at either low or high dose resulted in greater symptom reduction at two hours than ondansetron for both abdominal pain and nausea (difference -2.3cm [95% CI 0.6 to 4.0cm]; P=0.01). Additionally, the haloperidol groups showed less use of rescue antiemetics (31% versus 59%; [95% CI -61% to 13%]) and shorter time to ED departure (3.1 hours [SD 1.7] versus 5.6 hours [SD 4.5]; [95% CI 0.1 to 5.0 hours]; P=0.03). Due to similar improvements between the two haloperidol doses, the authors favor the lower dose to prevent side effects such as akathisia and dystonia.
This trial did well in having a strong working diagnostic definition of cannabis hyperemesis syndrome. Part of the syndrome’s Rome IV diagnostic criteria includes improvement of symptoms with sustained cessation of cannabis. Given that many adults with other forms of cyclic vomiting syndrome self-medicate with cannabis, diagnostic uncertainty exists among the paper’s selected population. Its major limitations include its small enrollment size, which limits its generalizability, and the poor follow-up data at 24 and 48 hours after treatment. The study investigators also initially designed a three period crossover study, but due to its low crossover rate the study had to perform unmatched testing of its subjects. Lastly, the subjective nature of the 10-cm visual analog scale poses issues of outcome reliability.
In summary, the HaVOC trial offers strong evidence that haloperidol has a role in aborting cannabis hyperemesis syndrome when compared to ondansetron and should be considered in patients suffering from this syndrome. Future randomize controlled trials will help elucidate this claim.
Conclusion
Cannabinoid hyperemesis syndrome is an underdiagnosed illness.6 Acute episodes often necessitate an ED visit, and patients are often given a cocktail of different, unrelated medications to control symptoms with mixed results. The majority of existing literature is in case reports and case series, but recent evidence suggests that the antipsychotics haloperidol and droperidol may be used as first-line treatment. These studies showed a larger reduction in symptoms, medication redosing, and higher discharge rates. The exact mechanism of how haloperidol or droperidol works in CHS is unknown, but the symptomatic response should encourage physicians to reach for these medications as a potential first-line option.
Answer: The data behind haloperidol and droperidol for treatment of CHS is admittedly limited, but promising. Several case reports and recent RTCs have shown the utility of these drugs and as first-line options for
AAEM/RSA RESIDENT JOURNAL REVIEW >> COMMON SENSE MARCH/APRIL 2023 59
cannabinoid hyperemesis syndrome, although mechanism of action and appropriate dosing remains to be determined.
References
1. Lapoint J, Meyer S, Yu CK, et al. Cannabinoid Hyperemesis Syndrome: Public Health Implications and a Novel Model Treatment Guideline. West J Emerg Med. 2018;19(2):380-386. doi:10.5811/westjem.2017.11.36368
2. Sorensen CJ, DeSanto K, Borgelt L, Phillips KT, Monte AA. Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment-a Systematic Review. J Med Toxicol. 2017;13(1):71-87. doi:10.1007/s13181016-0595-z
3. Kim HS, Anderson JD, Saghafi O, Heard KJ, Monte AA. Cyclic vomiting presentations following marijuana liberalization in Colorado. Acad Emerg Med. 2015;22(6):694-699. doi:10.1111/acem.12655
Continued from page 57
4. Soriano-Co M, Batke M, Cappell MS. The cannabis hyperemesis syndrome characterized by persistent nausea and vomiting, abdominal pain, and compulsive bathing associated with chronic marijuana use: a report of eight cases in the United States. Dig Dis Sci. 2010;55(11):31133119. doi:10.1007/s10620-010-1131-7
5. Allen JH, de Moore GM, Heddle R, Twartz JC. Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut 2004;53(11):1566-1570. doi:10.1136/gut.2003.036350
6. Hernandez JM, Paty J, Price IM. Cannabinoid hyperemesis syndrome presentation to the emergency department: A two-year multicentre retrospective chart review in a major urban area. CJEM. 2018;20(4):550555. doi:10.1017/cem.2017.381
SOME SUCCESS STORIES FROM THE NOVEMBER 2022 INTERIM MEETING OF THE AMERICAN MEDICAL ASSOCIATION HOUSE OF DELEGATES
Resolution was “Referred”. This means that the language of Resolution 219 will undergo further study before final consideration at a future meeting of the AMA HOD.
Watch This Space
I have written another draft resolution which was adopted by APS of AMA, but which was adopted at a time too late for it to be submitted to the HOD for AMA-Interim in 2022. Thus, it will be submitted to the annual meeting of the AMA HOD in June 2023.
The resolution will ask AMA to remind physicians that they have the right to engage in nonviolent civil disobedience, even if that leads to arrest. The inspiration for this draft resolution included several “heavy-handed” law enforcement responses following the 2020 murder of Mr. George Floyd. One such response occurred in my home region of St. Louis, in which police “kettled” protesters. “Kettling” is accomplished by police when a cordon of tens (or more) officers surround peacefully protesting citizens and then arrest each one.
Additional considerations include an editorial in the August 24, 2022 New England Journal of Medicine. That editorial advocated that it is appropriate for physicians to engage in civil disobedience in the wake of the Dobbs decision that overturned Roe and left to the states the matter of whether or not to allow abortions of pregnancies, and how to define just what is meant by “abortion.” My colleague and former fellow member of the GC of the AMA APS, Dr. Ken Simons, has subsequently served with the Federation of State Medical Boards, and he has educated me as I wrote my draft resolution that it is a belief among the FSMB leadership
that to be arrested during nonviolent civil disobedience should not delay or complicate a physician’s licensure or re-licensure, and that the FSMB would weigh in on that matter if need be. (However, Dr. Simons also cautioned that medical licensure is a state-level function, and that the various states are free to adopt their own laws regarding licensure.)
Closing Comments: Get Involved!
It is hoped that some who read this will be heartened that a direct route toward usefully influencing AMA actions and policies is provided by becoming active and involved in AMA’s individual state societies, or within various sections. It is notable that AAEM has only one representative to the Emergency Medicine Section Council, former AAEM President, Dr. Joe Wood of Arizona.
However, state medical societies’ meetings are open to all who are members. To my view, the best path for younger physicians and students to become most rapidly involved in AMA is to become an active in their state’s medical society and/or to become a member of the AMA’s Medical Student Section, the Resident and Fellows Section, or the Young Physicians Section. Both at the state and the national level, older AMA members are receptive to input from students, residents, and younger physicians. After all, these are the future of medicine! Mid- and late-career doctors can gain rapid traction within the Organized Medical Staff Section or the Senior Physicians Section.
If you perceive that there is a need for advocacy by AMA toward a medically-related goal that it can influence, then you should become active in organized medicine!
AAEM/RSA RESIDENT JOURNAL REVIEW
COMMON SENSE MARCH/APRIL 2023 60
February Board of Directors Meeting Summary
February Board of Directors Meeting Summary



The members of the AAEM Board of Directors met in-person at in Dallas, TX, on February, 2023, to discuss current and future activities. The members of the board appreciate and value the work of AAEM committee, section, interest group, and chapter division members and chairs as they strive toward the AAEM mission and to be the specialty society of emergency medicine. Over the course of the meeting, a number of significant decisions and actions were made. Here are the highlights:
Presentations
President Jonathan S. Jones, MD FAAEM, presented his President’s report which highlighted the many activities that he and other leaders have been involved in including reviewing online comments submitted by members.


Treasurer L. E. Gomez, MD MBA, reported on AAEM and AAEM subsidiaries financial performance through December 31, 2022. He informed the Board that the annual AAEM Audit had begun.









Board Actions
The Board set forth the following actions during the meeting including:
• Approval of a partnership with the National Pediatric Readiness Project (NPRP).



• Approval of two additional Social EM Mini Grants.
• Approval of the updated CPC Statement “Do Steroids Improve Clinically Relevant Outcomes in Patients with Septic Shock?”
• Approval of the formation of the Locums Tenens Section.
Miscellaneous
2022-2023 Elected Board of Directors
The Board approved expanding the Chapter Division and Sections social at AAEM23 to include Committees and Interest Groups to provide attendees the ability to learn how to get more involved with AAEM. The Board also confirmed that there will be no virtual options available for the 2023 Scientific Assembly.
The Next Board of Directors Meeting
When April 21, 2023
Where
AAEM 2023 Scientific Assembly
New Orleans Marriott | New Orleans, LA
COMMON SENSE MARCH/APRIL 2023 61
AAEM Job Bank Service
Promote Your Open Position
To place an ad in the Job Bank: Equitable positions consistent with the Mission Statement of the American Academy of Emergency Medicine and absent of restrictive covenants, will be published (upon approval). All ads run for a six month period or until canceled and will appear in the AAEM member magazine Common Sense and online. For pricing and more information visit www.aaem.org/membership/benefits/ job-bank.
Complete a Job Bank registration form, along with the Criteria for Advertising Section, and submit payment. If you are an outside recruiting agent, the Job Bank Criteria for Advertising must be downloaded and completed by a representative from the recruiting hospital/group.
Direct all inquiries to: www.aaem.org/membership/benefits/job-bank or email info@aaem.org.
Positions Available
For further information on a particular listing, please use the contact information listed.
Section I: Positions in full compliance with AAEM’s job bank advertising criteria, meaning the practice is wholly-owned by its physicians, with no lay shareholders; the practice is equitable and democratic; due process is guaranteed after a probationary period of no more than one year; there are no post-employment restrictive covenants; and board certified emergency physicians are treated equally, whether they achieved ABEM/AOBEM/RCPSC certification via residency training or the practice track.
Section II: Positions that cannot be in full compliance with AAEM’s job bank criteria, because they are employee positions with hospitals or medical schools and the practice is not owned by its emergency physicians. Thus there may not be financial transparency or political equity.
Section III: Positions that cannot be in full compliance with AAEM’s job bank criteria, because they are government or military employee positions. The practice is not owned by its emergency physicians, and there may not be financial transparency or political equity.
Section IV: Position listings that are independent contractor positions rather than owner-partner or employee positions.

SECTION I: POSITIONS RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK CRITERIA
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA (Below are hospitals, non-profit or medical school employed positions.)
SECTION TWO COLORADO
The Emergency Medicine Residency at Denver Health Medical Center is recruiting for a Program Director to lead our Emergency Medicine Residency Program. The following position description outlines the specific duties of the Denver Health Residency in Emergency Medicine Program Director necessary to meet the requirements of the ACGME Next Accreditation System (NAS). The Program Director has authority and accountability for the operation of the program and has broad responsibilities that encompass every aspect of postgraduate medical education training. This includes oversight of: · Curriculum and evaluation as well as the learning environment · Faculty as teachers, coaches, mentors, advisors and role models · Supervision of residents and fellows, including duty hours, and · Program management (e.g., program evaluation and improvement, communications, ACGME accreditation, program resources). The Program Director must ensure continuing accreditation of the program by being familiar with and complying with the ACGME Institutional Requirements Common Program Requirements(CPR) and Emergency Medicine Program Requirements, as well as ACGME and Review Committee Policies and Procedures and the CU SOM GME Policies and Procedures. The Program Director should monitor his or her specialty Review Committee activities, and be familiar with the ACGME Program Directors’ “Virtual Handbook” Minimum Qualifications Experience: Minimum of 3-5 years of participation as a core faculty member in an ACGME-accredited emergency medicine residency program and graduate medical education administrative and leadership experience. Applicants should submit CV and cover letter/statement of interest to: Aaron Ortiz, Manager Provider Recruitment aaron.ortiz@dhha.org P: 303602-4992 (PA 1932)
Email: aaron.ortiz@dhha.org
Website: https://www.denverhealth.org/services/emergencymedicine
NovDec, JanFeb, MarApr
CONNECTICUT
Trinity Health Of New England seeks BC/BE EM Physicians to join our emergency medicine teams at Mercy Medical Center in Springfield, Massachusetts, Saint Francis Hospital and Medical Center in Hartford, Connecticut and Saint Mary’s Hospital in Waterbury, Connecticut. Our practice model empowers our physicians to work at their highest level, while allowing time for professional development and family life. Whether you are focused on providing outstanding patient-centered care or driven to grow into a leadership role, you will thrive at Trinity Health Of New England. To learn more visit our provider portal at www. JoinTrinityNE.org (PA 1939)
Email: dhowe@TrinityHealthofNE.org
Website: https://www.jointrinityne.org/Physicians
NovDec, JanFeb, MarApr
MISSOURI
Centerpoint Medical Center is seeking an Emergency Medicine Program Director for their new residency program in Independence, Missouri. Qualified Candidates: - Board certified in emergency medicine with a minimum of three years’ experience - Previous experience as an Associate Program Director, Core Faculty member, or Department Chair is requiredAvailable to begin work in spring 2023 - Ability to obtain Missouri licensure - Excellent interpersonal and communication skills Duties and Responsibilities: - Work on obtaining initial ACGME accreditation through submission of application. - Recruit and select candidates for the residency program through the National Residency Matching Program. - Provide accurate statistical and narrative information in accordance with the requirements of the ACGME and the ACGME’s Review Committee for Emergency Medicine. - Maintain current knowledge of the accreditation and operational requirements of the residency program, including monitoring current trends and anticipating changes. - Assure that faculty meet research and scholarly activity requirements of the program. Incentive/Benefits Package: - Competitive W2 compensation - Robust benefits include medical, dental, vision and 401k - A-rated professional liability insurance (PA 1947)
Email: amie.murphy@hcahealthcare.com
Website: https://careers.hcahealthcare.com/jobs/10681698emergency-medicine-residency-founding-program-directoropportunity-in-independence-missouri
JanFeb, MarApr, MayJun
NEW HAMPSHIRE
Dartmouth Health and The Geisel School of Medicine at Dartmouth are pleased to announce a national search for the Chair of the Department of Emergency Medicine. This is an opportunity to lead an exceptional clinical department known nationally for providing outstanding patient care, fostering the medical and biomedical education of the next generation, and supporting innovative research. In this leadership role, the Chair of the Department of Emergency Medicine will have primary responsibility and accountability for the overall direction, operation, and management of the Department in accordance with the mission and goals of Dartmouth Health and The Geisel School of Medicine at Dartmouth. Qualified candidates will: hold a medical degree (MD, MD/MPH, MD/MBA, MD/PhD) or equivalent degree(s); qualify for rank of Professor or Associate Professor at the Geisel School of Medicine; be American board certified; and be a New Hampshire licensed physician or should be eligible for licensure in the state of New Hampshire. The preferred candidate will have five or more years of experience as a strategic leader with the ability to manage a substantial, complex, and evolving organization. All application material should be submitted to: Elizabeth Homsy Senior Associate, Healthcare Practice Korn Ferry elizabeth.homsy@kornferry. com Dartmouth Health is an equal opportunity employer, and all qualified applicants will receive consideration for employment without regard to race, color, religion, sex, national origin, disability status, veteran status, gender identity or expression, or any other characteristic protected by law. (PA 1966)
Email: elizabeth.homsy@kornferry.com
Website: https://www.dartmouth-health.org/ MarApr, MayJun, JulAug
NEW JERSEY
Opportunity: Chairman, Department of Emergency Medicine, Capital Health Systems Licensing and Education Requirements:
• Board certified in Emergency Medicine
• 5-10 years of clinical experience (preferred) • 5 years of group leadership (preferred) Responsibilities for this position include, but are not limited to:
1. Provider Management: a. Manage recruitment and retention of provider staff b. Maintain regular reviews and evaluations of providers c. Interview provider candidates d. Participate in on-boarding of new providers to ensure they have a full understanding of operational procedures e. Monitor the overtime rate of providers across the system to ensure department goals
None Available at this time. 62
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
are achieved f. Create routine schedule, call schedule, and staffing models for the Capital Health Emergency Department 2. Clinical Workflow & Operations: a. Be accountable for the optimal operating efficiency of staff and develop/maintain a patient-centered approach to clinical care b. Develop and maintain a process to review note closure rates and plan to mitigate deficiencies across the system c. Meet with Utilization Review and Medical team leadership to identify opportunities for proper bed assignment and level of care d. Lead the ED Operations, ED leadership and ED Documentation meetings. Participate in other required meetings such as OBS Operations and CHMG Inpatient Operations e. Assist with implementation of Surge management f. Analyze metrics and review analysis with Senior Capital leaders g. Review clinical variation of practice and promote best practices h. Provide new disease management oversight i. Work in conjunction with emergency management systems to ensure emergency preparedness 3. Quality a. Keep abreast of local, regional and national trends in science and education as related to emergency medicine and communicate this information to staff, faculty and administration b. Liaison to committees such as Sepsis, AMI/CPC, stroke accreditation and Patient Satisfaction, Neuro Operations, Resuscitation, Maternal/ child, and Radiology c. Appoint committees and leadership roles as needed to further the goals and functions of the Department d. Address reported safety events, participate in adverse event review, and work directly with providers to ensure continued performance improvement 4. Residency a. Teaching b. Oversee development in conjunction with the Residency Director (PA 1959)
Email: apatel@capitalhealth.org
Website: https://www.capitalhealth.org/ MarApr, MayJun, JulAug
NEW YORK
Bon Secours Charity Medical Group has an excellent opportunity for a BC/BE emergency department Assistant Medical Director to provide administrative support and medical care to patients of all ages presenting to the Emergency Department. In this role, you will also develop short/long term plans for on-going improvement of the clinical, operational, and administrative quality of the department. In addition to current New York State license to practice medicine, active unrestricted DEA license to prescribe medications, ideal candidates will have: • Prior emergency medicine leadership experience or completion of fellowship training in emergency department administration. • Proficiency in all procedures, techniques and skills listed in the delineation of privileges for emergency department physicians. • Completion of at least three years of post-graduate training in emergency medicine. A great place to live and work. In addition to an excellent salary and comprehensive benefits package, the Hudson Valley offers magnificent scenery, historic mansions, cultural treasures, and unique attractions. From great restaurants to beautiful gardens and performing arts, creativity thrives amid inspiring landscapes. For your enjoyment, farm-totable cuisine is created at country inns and the world-famous Culinary Institute of America by legendary chefs. With abundant farmers markets, award-winning wineries, craft-breweries and food festivals, Hudson Valley dining is legendary. If great schools are top of mind, the Hudson Valley is the place to be. Good Samaritan Hospital in Suffern, NY, is a 286-bed hospital providing emergency, medical, surgical, obstetrical/gynecological, and acute-care services to residents of Rockland and southern Orange counties in New York; and northern Bergen County, NJ. The hospital is home to a recognized cardiovascular program, comprehensive cancer-treatment services, the area’s leading Wound and Hyperbaric Institute and outstanding maternal/ child services that includes a Children’s Diagnostic Center. Good Samaritan Hospital also provides social, psychiatric, and substance-abuse services and its certified home-care agency supports residents of the Hudson Valley and beyond. Bon Secours Charity Medical Group part of Bon Secours Charity Health Systems (BSCHS), a regional network of more than 120 primary care physicians and specialists from a broad array of medical specialties. BSCHS, a member of the Westchester Medical Center Health Network (WMCHealth), includes Good Samaritan Hospital in Suffern, NY, Bon Secours Community Hospital in Port Jervis, NY, and St. Anthony Community Hospital in Warwick, NY. WMCHealth is an Equal Opportunity Employer. It is the policy of Westchester Medical Center Health Network to provide equal employment opportunities without regard to race, color, religion, gender, national or ethnic origin, sex, sexual orientation, gender identity or expression, age (40 or older), marital status, genetic information or carrier status, disability
(mental or physical), citizenship status, pregnancy, military service or veteran status, arrest or criminal accusation, domestic violence victim status or any other status protected by federal, state, or local law. (PA 1946)
Email: claire@fusionideas.com
NovDec, JanFeb, MarApr
NORTH CAROLINA
Emergency Medicine – Site Medical Director (MD/DO) Wake Forest Emergency Providers We are seeking candidates with proven experience in leadership and clinical practice. This is a unique opportunity to lead a dynamic Emergency Medicine team with the support and backing of a large, regional, nonprofit, academic health system. In addition to practicing clinically, the selected candidate will also provide leadership in staffing, financial management, performance improvement, and quality and safety initiatives for their site. We offer a highly innovative model wherein our physicians have tremendous influence in their practice. This includes access to transparent financials and performance metrics and the ability to influence practice plans. With a lean administrative model and responsible staffing, our physicians have abundant resources at their disposal to improve outcomes for patients and lead care innovations. While our Medical Directors have autonomy to manage their sites, they also enjoy great collaboration and support with experienced peers, a strong Regional Director and a supportive President. This is an employed position with Wake Forest Emergency Providers About Wake Forest Emergency Providers Affiliated with Atrium Health Wake Forest Baptist (www.wakehealth.edu), Wake Forest Emergency Providers is a nationally recognized, 501c3 non-profit, proudly providing health care for all! We are contracted with select, partner organizations to provide staffing for Hospital Emergency Departments, Free Standing Emergency Departments, and Urgent Cares throughout the North Central and Northwest regions of North Carolina. Location Outdoor activities abound in the area with unrivaled hiking, road/gravel/ mountain biking, fly fishing, kayaking/rafting and rock climbing easily accessible. Public schools are among the top ranked in the state and the community is close-knit and supportive. Position Requirements: • Qualified Candidates must be Board Certified (or eligible) by the American Board of Emergency Medicine or equivalent, and licensed (or eligible) to practice medicine in the state of North Carolina. What We Believe When you join Wake Forest Emergency Providers, you will be welcomed into an inclusive culture that celebrates and respects the contributions a diverse team can make together. Practice where your voice is valued, your passion for advancing medicine is rewarded, and you get the resources and support you need to thrive personally and professionally. In our organization, you can work alongside the most advanced minds in medicine to improve medicine, elevate hope and advance healing—for all. Interested Candidates May Contact: Scott Dudley Atrium Health Wake Forest Baptist - Provider Recruitment 336-341-2631 sdudley@ wakehealth.edu (PA 1969)
Email: sdudley@wakehealth.edu
Website: http://www.wakehealth.edu
AprMar, MayJun, JulAug
NORTH CAROLINA
Wake Forest Emergency Providers is currently seeking to add to our team of exceptional patient-centered emergency physicians in the Blue Ridge Mountains due to our continued expansion and growth. We offer a unique employment model inclusive of salary, RVU based incentive, paid malpractice, benefits, CME allowance and relocation. Our physicians have local influence on practice decisions, and a strong provider voice in care delivery. These positions are located in Boone, North Carolina, a beautiful town in the Blue Ridge Mountains with a booming local economy, friendly people, thriving arts and food cultures and a wide variety of indoor and outdoor recreational activities in both the community and on the campus of Appalachian State University. Boone is 84 miles from Asheville, 100 miles to Charlotte and 87 miles to the Piedmont Triad. (PA 1941)
Email: michael.ginsberg@wakehealth.edu
Website: http://www.wakehealth.edu
NovDec, JanFeb, MarApr
NORTH CAROLINA
Wake Forest University School of Medicine’s Department of Emergency Medicine has a unique opportunity to join our faculty as an Assistant or Associate Professor with a scholarly focus on Diversity, Equity, and Inclusion. This position will be an integral part of our ongoing EM DEI initiatives. The successful candidate will have career development and leadership opportunities within
our active DEI committee. Our ED includes a Level 1 trauma center, accredited chest pain center, stroke center, and a burn centers. Our clinical affiliate physicians staff 18 EDs across the state, providing services to >500,000 patients annually, with patient acuity in the 95th percentile and an admission rate of 30 percent. In 2020, Wake Forest Baptist Health and Atrium Health joined together in a strategic partnership to operate as a single enterprise. As part of this new enterprise, Atrium Health has announced $3.4 billion in planned investments in our health system and the communities we serve. The growth of the school of medicine, including the building of a new medical school campus in Charlotte, will expand existing academic research capabilities and opportunities for clinical trials across a large, diverse market with some of the nation’s leading medical experts. (PA 1944)
Email: michael.ginsberg@wakehealth.edu
Website: http://www.wakehealth.edu
NovDec, JanFeb, MarApr
NORTH CAROLINA
Duke Pediatrics is recruiting for a faculty member to join the Division of Pediatric Emergency Medicine. Duke Children’s is ranked among the nation's finest for pediatric care and is #1 in NIH funding for pediatric clinical science departments. Ideal candidates will possess excellent clinical skills, a passion for education, and a demonstrated record of scholarly contributions. The Greater Triangle area of Raleigh, Durham and Chapel Hill is culturally diverse, economically resilient and nationally recognized as a great place to live and work. Interested candidates should submit CV and Letter of Interest via https:// pdc.dukehealth.org/physician-jobs (PA 1958)
Email: sherrod.basnight@duke.edu
Website: https://pdc.dukehealth.org/physician-jobs
MarApr, MayJun, JulAug
PENNSYLVANIA
WellSpan Health’s vision is to reimagine healthcare through the delivery of comprehensive, equitable health and wellness solutions throughout our continuum of care. As an integrated delivery system focused on leading in value-based care, we encompass nearly 1,900 employed providers, 220 locations, eight award-winning hospitals, home care and a behavioral health organization serving South Central Pennsylvania and northern Maryland. Our clinically integrated network of 2,600 aligned physicians and advanced practice providers provide the highest quality and safety, inspiring our patients and communities to be their healthiest. Position Highlights: Looking for a board certified/eligible emergency medicine physician for York, Pennsylvania This position is designed to have split responsibilities which would include 40% Clinical and 60% administrative Successful candidate will possess considerable clinical, resident teaching and leadership experience York Hospital (YH) is a Level 1 Regional Resource Trauma Center serving an annual volume of over 80,000+ visits per year York Hospital is designated as a Comprehensive Stroke Center Work with a team of physicians, advanced practice providers and 38 residents Support includes lab turnaround in an hour or less, a large hospitalist team to facilitate admissions, two digital imaging exam rooms & two 128 CT Scanners WellSpan Emergency department is a busy department seeing an average of 240 patients per day In 2017 a renovation was completed to incorporate WellSpan’s own helipad and branded helicopter
Our Commitment to You: Competitive Compensation Signing bonus 6 weeks of Scheduled Time Off Relocation Retirement Savings Plan Full Malpractice Coverage Including Tail About the Community: Conveniently situated within a short drive of major cities like Philadelphia, Baltimore and Washington, D.C., WellSpan Health’s service area is made up of a diverse mix of welcoming communities that you will love to call home. South Central Pennsylvania offers an idyllic blend of unique cities and towns including Lancaster, York, Gettysburg, Lebanon, Chambersburg and Waynesboro. For Confidential Consideration
Contact: Tammie Chute, Provider Recruitment WellSpan Health tchute@wellspan.org Office (717) 267-7780 (PA 1929)
Email: jsteffen4@wellspan.org
Website: https://www.joinwellspan.org/jobs/Emergency_ Medicine_-_Chair/York_Pennsylvania/100/290719/
NovDec, JanFeb, MarApr
VERMONT
The Department of Emergency Medicine at The Larner College of Medicine (LCOM) at The University of Vermont (UVM) is seeking an Emergency Medicine Physician to fill
COMMON SENSE MARCH/APRIL 2023 63
(Below
are hospitals, non-profit or medical school employed positions.)
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA, CONTINUED
the role of Associate Professor or Professor in the Clinical Scholar Pathway, commensurate with years of experience and accomplishments. The physician identified in this search will be provided the opportunity to serve as the Vice Chair of Academic Affairs (VCAA) of the Department of Emergency Medicine. The Department of EM provides clinical coverage at the seven clinical campuses of the University of Vermont Health Network in Vermont and upstate New York. Fifty academic faculty in the Department work with colleagues in community clinical practice to serve approximately 200,000 patient visits annually, and the Network hospitals serve a catchment of 40,000 square miles and 1.4M people. LCOM students and Emergency Medicine residents train clinically in three of the network sites with elective rotations in multiple other sites. Our primary teaching campus is the University of Vermont Medical Center, the only level 1 trauma center in the greater region. The majority of academic faculty provide clinical coverage at multiple sites in Network, including our rural and critical access sites, underscoring our commitment to high quality rural acute care delivery. The Vice Chair of Academic Affairs (VCAA) will lead advancement of the academic components of the mission of the Department of EM. The VCAA will mentor faculty, fellows, and residents in their academic efforts and will lead the Promotions and Tenure Committee in advising the Chair on readiness for promotion. Recruitment and retention of faculty, fellows, and residents with a commitment to diversity, equity, and inclusion will remain a top priority. The VCAA will collaborate with colleagues locally at LCOM and nationally through organizations such as AAEM, SAEM, CORD, and the AAMC, providing networking opportunities, enhancing mentorship, incorporating innovative educational practices, and fostering faculty development. The VCAA will be provided with 30% nonclinical time to achieve the roles and responsibilities across the following domains: ·
Leadership and Strategic Planning · Faculty Development & Mentorship · Faculty Evaluation and Feedback · Diversity, Equity, and Inclusion · Faculty Recruitment, Retention, and Wellness · Scholarship Although all interested candidates are encouraged to apply, strong preference will be given to candidates with leadership experience in the educational, clinical, and research activities of academic emergency medicine. Consistent with all recruitments, we seek candidates that demonstrate empathy, humanism, and humility, and candidates must be comfortable with an environment that employs transparency to create faculty and leadership accountability. Candidates must commit to our core values of Professionalism at the Larner College of Medicine and are advised to review our Statement on Professionalism. Interested individuals should apply online at https://www.uvmjobs.com/postings/58864 (position number 00026358). Confidential inquiries to acquire further information about this position may be directed to Dr. Ramsey Herrington, Chair of the Department of Emergency Medicine at ramsey. herrington@uvmhealth.org (PA 1962)
Email: Ramsey.herrington@uvmhealth.org
Website: https://www.uvmjobs.com/postings/58864
MarApr, MayJun, JulAug
VIRGINIA
Email: alana.aisthorpe@kornferry.com
The University of Virginia School of Medicine invites applications and nominations for the position of Chair, Department of Emergency Medicine. Founded in 1819 as just the 10th medical school in America, the University of Virginia School of Medicine (UVA School of Medicine) – with 21 clinical departments, 8 research departments, and 6 research centers – consistently attracts some of the nation’s most prominent researchers to develop breakthrough treatments to benefit patients around the world. Those research efforts are backed by more than $230 million in grant funding. UVA Health is a world-class academic medical center and health system with a level 1 trauma center, a NCI comprehensive cancer center, and UVA Children’s Hospital. Its footprint encompasses 4 hospitals and 2 physician groups with an integrated network of primary and specialty care clinics throughout Charlottesville, Culpeper, and Northern Virginia. In September of 2021, Dr. Melina Kibbe began her tenure as Dean of the School of Medicine and Chief Health Affairs Officer. With this new leadership, the UVA School of Medicine is poised to undertake new directions in all four missions, including clinical strategy and growth, expansion of research in collaboration with other UVA schools, the promotion of educational programs of the highest caliber, and developing partnerships within the community. Integral to the success of this vision will be the recruitment of a dynamic and aspirational leader to serve as Chair, Department of Emergency Medicine. The Chair of Emergency Medicine will be an outstanding leader, communicator, and skilled physician, widely recognized in the field with a strong track record of program building and innovation. The Chair will be responsible for clinical, academic, and administrative activities of the Department and therefore they must have a deep knowledge of clinical practice; a strong commitment to training and career development in research and clinical care; and demonstrated leadership and administrative ability in complex clinical enterprise. The Chair must bring vision to the task of drafting the Department’s future, coupled with an ability to communicate in a fashion that inspires others to follow. The Chair will be a consensus builder, while also capable of serving as an agent for change. The Chair will evaluate the current strengths of the Department, and identify areas for productive growth in clinical, educational, and research programs. From that assessment, they will establish a strategic overarching long-term plan for the Department. The Chair must demonstrate a passion for mentoring and development of faculty and fellows, including interpersonal skills that will assure successful relationship building with a variety of internal and external stakeholders. The Chair will work with leadership to foster a collective and collaborative culture within the Department and beyond, bringing together the multidisciplinary people and programs with a shared vision and purpose, and thereby enhancing faculty engagement and development. Korn Ferry is assisting the University of Virginia School of Medicine with this important search. Please forward, as soon as possible, applications or nominations of appropriate candidates, in confidence, to: c/o Alana Aisthorpe, Korn Ferry Email: alana. aisthorpe@kornferry.com (PA 1940)
Chair, Department of Emergency Medicine
Website: https://med.virginia.edu/
NovDec, JanFeb, MarApr
WEST VIRGINIA
The Department of Emergency Medicine at Charleston Area Medical Center is recruiting a pediatric emergency medicine physician to work at Women and Children’s Hospital located in Charleston, WV. This 120-bed dedicated Women and Children’s Hospital is a part of a large university-affiliated regional referral center with a drawing population of 562,000. We have in-house Neonatologist with 24/7 coverage in Level III NICU as well as a PICU with pediatric intensivists. Charleston Area Medical Center also sponsors an ACGME accredited emergency medicine residency program with 20 residents at present. Position Requirements: • MD or DO degree from an accredited university medical school • Completion of an Emergency Medicine Residency and a Pediatric Emergency Medicine Fellowship or completion of a Pediatric Residency and a Pediatric Emergency Medicine Fellowship • Board Certification or Board Eligible (ABEM or AOBEM) in Pediatric Emergency Medicine • Ability to achieve full and unrestricted hospitalist privileges at Charleston Area Medical Center • Eligibility for a West Virginia Medical License Benefits include: • Excellent benefits package • Competitive compensation • Affordable community • Extraordinary family environment • Unsurpassed recreational activities • Outstanding school systems About Charleston, West Virginia Charleston is the state capital and largest city in the state. We are proud of our diverse population, amazing outdoor activities, and excellent schools. We are centrally located to numerous major metropolitan areas in North Carolina, Ohio, Pennsylvania, Virginia and Washington, DC, and Yeager International Airport is just 5 miles from the hospital. In addition, Charleston offers a Downtown district filled with eclectic galleries, chic boutiques, and unique restaurants. The area boasts a vibrant academic and professional community that offers a balanced professional career and a fulfilling personal lifestyle. Come see what our community can offer you! (PA 1955)
Email: carol.wamsley@camc.org
Website: http://www.camc.org
MarApr, MayJun, JulAug
SECTION III: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
(Below are military/government employed positions.)
None Available at this time.
(Below are hospitals, non-profit or medical school employed positions.)
COMMON SENSE MARCH/APRIL 2023 64
CALIFORNIA
EMERGENCY MEDICINE PHYSICIANS Full-Time and Per Diem opportunities in Southern California Southern California Permanente Medical Group (SCPMG) is an organization with strong values, which provides our physicians with the resources and support systems to ensure they can focus on practicing medicine, connecting with one another, and providing the best possible care to their patients. In Southern California, you'll enjoy amazing recreational activities, spectacular natural sceneries, and an exceptional climate. SCPMG is proud to offer its physicians: • An organization that has served the communities of Southern California for more than 65 years • A physician-led practice that equally emphasizes professional autonomy and cross-specialty collaboration • Comprehensive administrative support • An environment that promotes excellent service to patients • A fully implemented electronic medical record system
Full-time: partnership eligibility after 3 years, malpractice insurance and tail coverage provided, comprehensive benefits package, and excellent salary. Contact Michael Truong at 800-541-7946 or Michael.V.Truong@kp.org. Per Diem: flexible schedule, malpractice insurance and tail coverage provided, and non-benefitted. Must have CA medical license and paid DEA certificate. Contact Quan Nguyen at 800-541-7946 or Quan.D.Nguyen@kp.org. For consideration or to apply, visit https://scpmgphysiciancareers.com/emergency-medicine/. We are an AAP/EEO employer. (PA 1943)
Email: Michael.V.Truong@kp.org
NovDec, JanFeb, MarApr
FLORIDA
International Emergency Medicine Fellowship Opening at Global Physician Network, at Sarasota Memorial Health Care System, Sarasota, Florida A two (2) Year Fellowship Track Position for an ACGME Accredited Emergency Medicine Board Eligible / Board
Certified Attending who will accomplish the Fellowship with a Fully Funded International Project Based Field Experience, MBA in Project Management, and Certification in Crisis Leadership. Located in Sarasota the Fellowship is home to the Florida State University College of Medicine Emergency Medicine Residency Program. Please contact forwarding a statement of interest and your curriculum vitae. Dr. Sagar Galwankar, International Emergency Medicine Fellowship Director Email: gcsagar@ yahoo.com (PA 1968)
Email: gcsagar@yahoo.com
Website: https://www.globalphysiciannetwork.com/ MarApr, MayJun, JulAug
MINNESOTA
Join Emergency Physicians Professional Association (EPPA)! -a physician-owned, independent, democratic group of over 220 physicians staffing multiple facilities throughout Minnesota. Currently staffing 7 Twin Cities metro hospitals, 1 central MN hospital, 5 regional/rural sites, and 3 Urgency Rooms. Patient volumes 9K-75K per year. Immediate openings for BC/BE, Emergency Medicine residency trained physicians in the St. Cloud, Wilmar, and Monticello, MN areas with significant financial advantages (Shareholder buy-in is waived). Shifts range from 8 hours (metro) to 12 hours (rural). Sites include Level 1-4 trauma centers in multiple hospital systems. EPIC EMR at all sites. Variable workload based on site, ranging from 1.2-2 patients per hour. W2 with multiple benefits: malpractice, health, dental, life, disability, personal umbrella insurance; 401k, pension and profit sharing. Competitive compensation for full-time contract (1600 hours/year) with average RVU productivity. Shareholder/ Ownership track available. Night, weekend, and holiday differentials. Nocturnist positions possible. (PA 1965)
Email: bleagjeld@eppahealth.com
Website: https://www.eppahealth.com
MarApr, MayJun, JulAug
NEW YORK
We are looking for board-certified Emergency and Family Practice trained physicians who thrive in an environment surrounded by highly trained and motivated individuals to deliver urgent care services of the highest quality. Your responsibilities
will include the diagnosis and treatment of patients of all ages, and interpreting and archiving medical information. Highlights: Scribes on staff. This allows you to focus your time on direct patient care. Advanced imaging available on a routine and STAT basis, including CT, US and MRI. Specialist consultation allows for 48 hour turn around and same day results for urgent cases. State-of-the-art facilities, digital X-Ray, laboratory services with modern, clean and aesthetically designed work environments. Dedicated physician led Aftercare team following up on all aspects of patient care. Integrated Electronic Medical Records across all CityMD locations. Current NY/NJ State Medical License required and at least 2 years post residency preferred. (PA 1938)
Email: slameira@summithealth.com
Website: https://citymd.com
NovDec, JanFeb, MarApr
NEW YORK
CityMD is a network of urgent care centers dedicated to setting an unprecedented standard of care for our patients and an edifying, intuitive work environment for our employees. We are looking for board-certified Emergency and Family Practice trained physicians who thrive in an environment surrounded by highly trained and motivated individuals and operate on one of the most advanced administrative systems in healthcare today. Your responsibilities will include the diagnosis and treatment of patients of all ages and interpreting and archiving medical information. We are hiring board-certified physicians who are Emergency Medicine or Family Medicine trained to work in our state-of-the-art urgent care centers. Our facilities are staffed with highly trained and motivated individuals who operate one of the most advanced administrative systems in healthcare today. Highlights • Scribes on staff. This allows you to focus your time on direct patient care. • Advanced imaging available on a routine and STAT basis, including CT, US and MRI. • Specialist consultation allows for 48 hour turn around and same day results for urgent cases. • State-of-the-art facilities, digital X-Ray, laboratory services with modern, clean and aesthetically designed work environments. • Dedicated physician led Aftercare team following up on all aspects of patient care. • Integrated Electronic Medical Records across all CityMD locations. Our commitment to our patients and employees, along with our state-of-the-art personalized healthcare delivery system, has taken CityMD from one location on the Upper East Side to over 130 in the New York/New Jersey area including Northern/Central/Southern New Jersey and Manhattan, Brooklyn, Queens, Long Island, Rockland, and Westchester County. As a proud “People First” company, we are centered on the values of integrity, excellence, professionalism, and quality. Our Compensation package is broken down as follows: • Competitive hourly rate plus performance-based bonus • 4 weeks of paid time off • $3000 annually in CME • 401K match is up to 4% of your bi-weekly pay up to annual IRS limits • Full medical, dental and vision benefits, as well as short term and long term disability benefits and company paid life insurance • Medical Professional Liability Insurance Covered • Holiday Pay & Extended Hour Site Differentials up to $45/hour on top of base • $120 - $185 per hour The provided compensation range is based on industry standards and salary determinations will be made based on numerous factors including but not limited to years of experience, individual performance, quality measures and location of position. (PA 1961)
Email: slameira@summithealth.com
Website: http://www.citymd.com MarApr, MayJun, JulAug
OREGON
We believe in giving physicians what they need to succeed! Summit Health is actively recruiting for an experienced board certified/board eligible Family Medicine, Internal Medicine or Emergency Medicine Physician to work with our dedicated team of Clinical professionals in our Urgent Care Centers. Summit Health includes more than 150 providers and 30 specialties and services providing care to over 50,000 attributed lives in Central Oregon and is launching the community’s first full spectrum
Accountable Care Organization (ACO) in 2022. Summit Health is Central Oregon’s largest multispecialty group and is a for-profit, physician led/professionally managed practice with multiple locations in Bend, Redmond, and Sisters. Health is committed to maintaining a full-service Urgent Care for our community in Central Oregon including Bend, Redmond, Mt. Bachelor (limited in scope during the ski season) and currently looking to expand into additional locations. Summit Health will further advance our group’s mission of lowering the total cost of care for all patients in Central Oregon by continuing to offer and expand outpatient services throughout the community. You will be joining a team of 150 Providers within Summit Health and a total catchment area of 250,000 people throughout four locations within the group. As part of our team, you’ll enjoy: Physician led and professionally managed medical group. Market competitive rates with high earning potential and a quality bonus program. Shareholder opportunity. Team based approach focused on patient centered care. An established and growing integrated multispecialty medical practice. Comprehensive administrative and clinical support. Easy access to resources. Located east of the Cascade Mountains, Bend enjoys 300 days of sunshine and a wonderful high desert climate. World class skiing, renowned fishing and amazing golf, water sports, cycling and trail running are all part of a quality lifestyle for Central Oregon residents. Our community also offers excellent schools, a variety of cultural activities, great food, and entertainment, and is noted as one of the best places to live for outdoor activity by Sunset Magazine, Bike Magazine, CNN, Newsweek, and Golf Magazine. We offer competitive compensation, comprehensive benefits package, and a dynamic practice experience. (PA 1937)
Email: slameira@summithealth.com
Website: https://smgoregon.com
NovDec, JanFeb, MarApr
TENNESSEE
Middle TN Emergency Physicians is a private, physician owned democratic group staffing seven hospitals of the Ascension St. Thomas Health system in middle Tennessee. After over 35 years staffing the core urban hospitals of Saint Thomas, the two premier private democratic emergency groups in the area merged with a shared vision of providing the highest quality emergency care in the dynamic middle Tennessee area centered around Nashville. Our success offered the ability to expand our vision to the four regional facilities further advancing opportunities for emergency physicians in the area. We are currently seeking motivated BC/ BE physicians to serve as independent contractors at the St. Thomas River Park, St. Thomas DeKalb, St. Thomas Highlands, St. Thomas Stones River and St. Thomas Westlawn hospitals. Highly competitive pay is commensurate with volume at each individual facility with a bonus of no state income tax. Send CV to MTEPJobs@gmail.com. (PA 1948)
Email: brad.w.russell@gmail.com
JanFeb, MarApr, MayJun
TEXAS
Victoria Emergency Associates (VEA) is an established private group of EM, PedsEM and HM physicians, servicing 19 hospital locations in South Texas. VEA is one of the few physician-owned and managed practices in TX. We have solid relationships and steady growth with our partner facilities, and achieve high physician retention by sustaining a culture reflective of our values: compassion, quality, community, accountability, and transparency. Our goal is to offer physicians a meaningful career, not just a job. We are seeking dedicated FT/PT BC EM and/or BC/FP/IM w/ED physicians for our San Antonio and surroundings areas. "Compassion Is Our Specialty" (PA 1942)
Email: april@victoriaemergency.com
Website: https://www.victoriaemergency.com/ NovDec, JanFeb, MarApr
SECTION IV: POSITIONS
NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA (Below are independent contractor positions.)
COMMON SENSE MARCH/APRIL 2023 65

555 East Wells Street / Suite 1100 Milwaukee, WI 53202-3823 PRSRT STD U.S. POSTAGE PAID MILWAUKEE, WI PERMIT NO. 0188
COMMONSENSE
























 Joelle Borhart, MD FAAEM FACEP
Joelle Borhart, MD FAAEM FACEP




 Faith Quenzer, DO MPH FAAEM
Faith Quenzer, DO MPH FAAEM

 MD
MD





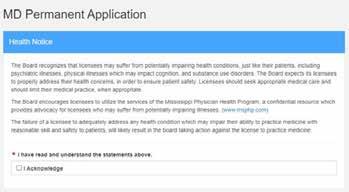































 Isabel A. Barata, MS MD MBA
Isabel A. Barata, MS MD MBA
 Tom Scaletta, MD MAAEM, Akiva Dym, MD FAAEM, and Anthony Rosania MD MHA FAAEM
Tom Scaletta, MD MAAEM, Akiva Dym, MD FAAEM, and Anthony Rosania MD MHA FAAEM





















 Alessandra Della Porta, MD*
Alessandra Della Porta, MD*





 The Advocacy Channel
The Advocacy Channel


















