COMMON SENSE VOICE OF THE AMERICAN ACADEMY OF EMERGENCY MEDICINE VOLUME 30, ISSUE 5 SEPTEMBER/OCTOBER 2023 President’s Message “Why Me?” 2 4 Editor’s Message Lessons Learned When I Was a Medical Director 10 Government and National Affairs Committee An Update on Due Process 24 AAEM/RSA Editor's Message: To Be a “They/Them” in Medicine: A Call for Active Allyship 23 AAEM/RSA President's Message Partnerships! Your Financial Health: Considerations for Each Stage of Your Career Page 8
Officers President
Jonathan S. Jones, MD FAAEM
President-Elect
Robert Frolichstein, MD FAAEM
Secretary-Treasurer
L.E. Gomez, MD MBA FAAEM
Immediate Past President
Lisa A. Moreno, MD MS MSCR FAAEM FIFEM
Past Presidents Council Representative
Tom Scaletta, MD MAAEM FAAEM
Board of Directors
Heidi Best, MD FAAEM
Laura J. Bontempo, MD MEd FAAEM
Kimberly M. Brown, MD MPH FAAEM
Phillip A. Dixon, MD MBA MPH FAAEM CHCQMPHYADV
Al O. Giwa, LLB MD MBA MBE FAAEM
Robert P. Lam, MD FAAEM
Bruce Lo, MD MBA RDMS FAAEM
Vicki Norton, MD FAAEM
Kraftin Schreyer, MD MBA FAAEM
YPS Director
Fred E. Kency, Jr., MD FAAEM
AAEM/RSA President
Leah Colucci, MD MS
Editor, JEM
Ex-Officio Board Member
Stephen R. Hayden, MD FAAEM
Editor, Common Sense
Ex-Officio Board Member
Edwin Leap II, MD FAAEM
Executive Director
Missy Zagroba, CAE
Executive Director Emeritus
Kay Whalen, MBA CAE
Common Sense Editors
Mehruba Anwar Parris, MD, Assistant Editor
Mel Ebeling, MS3, Resident Editor
Stephanie Burmeister, MLIS, Managing Editor
Articles appearing in Common Sense are intended for the individual use of AAEM members. Opinions expressed are those of the authors and do not necessarily represent the official views of AAEM or AAEM/RSA. Articles may not be duplicated or distributed without the explicit permission of AAEM. Permission is granted in some instances in the interest of public education. Requests for reprints should be directed to AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202, Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org
AAEM is a non-profit, professional organization. Our mailing list is private.
AAEM ANTITRUST COMPLIANCE PLAN:
As part of AAEM's antitrust compliance plan, we invite all readers of Common Sense to report any AAEM publication or activity which may restrain trade or limit competition. You may confidentially file a report at info@aaem.org or by calling 800-884-AAEM
Mission Statement
The American Academy of Emergency Medicine (AAEM) is the specialty society of emergency medicine. AAEM is a democratic organization committed to the following principles:
1. Every individual, regardless of race, ethnicity, sexual identity or orientation, religion, age, socioeconomic or immigration status, physical or mental disability must have unencumbered access to quality emergency care.
2. The practice of emergency medicine is best conducted by a physician who is board certified or eligible by either the American Board of Emergency Medicine (ABEM) or the American Osteopathic Board of Emergency Medicine (AOBEM).
3. The Academy is committed to the personal and professional well-being of every emergency physician which must include fair and equitable practice environments and due process.
4. The Academy supports residency programs and graduate medical education free of harassment or discrimination, which are essential to the continued enrichment of emergency medicine, and to ensure a high quality of care for the patient.
5. The Academy is committed to providing affordable high quality continuing medical education in emergency medicine for its members.
6. The Academy supports the establishment and recognition of emergency medicine internationally as an independent specialty and is committed to its role in the advancement of emergency medicine worldwide.
Membership Information
Fellow and Full Voting Member (FAAEM): $525* (Must be ABEM or AOBEM certified, or have recertified for 25 years or more in EM or Pediatric EM)
Associate: $150 (Limited to graduates of an ACGME or AOA approved emergency medicine program within their first year out of residency) or $250 (Limited to graduates of an ACGME or AOA approved emergency medicine program more than one year out of residency)
Fellow-in-Training Member: $75 (Must be graduates of an ACGME or AOA approved emergency medicine program and be enrolled in a fellowship)
Emeritus Member: $250 (Please visit www.aaem.org for special eligibility criteria)
International Member: $150 (Non-voting status)
Resident Member: $60 (voting in AAEM/RSA elections only)
Transitional Member: $60 (voting in AAEM/RSA elections only)
International Resident Member: $30 (voting in AAEM/RSA elections only)
Student Member: $40 (voting in AAEM/RSA elections only)
International Student Member: $30 (voting in AAEM/RSA elections only)
Pay dues online at www.aaem.org or send check or money order to:
AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202 Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org
Table of Contents COMMONSENSE AAEM-0823-310 TM Foundation Contributions 6 PAC Contributions .......................................................................................................................... 6 LEAD-EM Contributions 7 Upcoming Events 7 Government and National Affairs Committee: An Update on Due Process 10 Young Physicians Section: YPS: Empowering Physician Advocacy and Fostering Resources for Young Emergency Medicine Physicians 14 Wellness Committee: Introducing the Mental Health Action Plan 17 Academic Affairs Committee and Wellness Committee: Breaking Burnout with an Emergency Department Debrief 21 AAEM/RSA President’s Message: Partnerships ...........................................................................23 Emergency Ultrasound Section: EFAST: Essential or Overrated 31 “Rebranding” Emergency Medicine 33 The Double Bullet Sign: Identification of Esophageal Intubation Using Point-of-Care Ultrasound 37 Opinion: Dobbs Decision 39 AAEM/RSA Resident Journal Review: Restrictive versus Liberal Fluid Resuscitation in Septic Shock 40 AAEM Job Bank 46
COMMON SENSE MAY/JUNE 2023
COMMONSENSE
Featured Articles

2
President’s Message: “Why Me?”
8
**NEW COLUMN**
Financial Wellness: Your Financial Health: Considerations for Each Stage of Your Career

15
Aging Well in Emergency Medicine Interest Group: Telemedicine: Enhance Your Career and Wellness
In this article, Dr. Hoyer discusses the benefits that telemedicine has on physicians, highlighting the flexible work hours, cost and climate savings, and the gratitude the telemedicine patients express.
Dr. Dr. Jones discusses Imposter Syndrome and how it effects emergency physicians. He admits that while Imposter Syndrome is not directly caused by an individual, we can all try to effect change one colleague at a time.
4
Editor’s Message: Lessons Learned When I Was a Medical Director
In this new Common Sense column, Dr. Chris McNeil, an emergency phrsician who transitioned his career to from medicine to finance, shares financial strategies for doctors in each stage of their career.
11
Social Media Committee: Paging Dr. TikTok
24
RSA Editor’s Message: To Be a “They/Them” in Medicine: A Call for Active Allyship
In his Editor’s Message, Dr. Leap discusses the 18 months he’s served as a medical director and comes to the conclusion that his strength is not management. With this experience and his experience as a “directee” for most of his career, he has seen both good and bad leaders and has learned lessons along the way.
In this article, the medical student authors discuss the transformative potential of TikTok in revolutionizing how doctors can connect with the public and disseminate medical information in a way that resonates with a diverse and global audience. Not only that, TikTok can also lend a hand in increasing medical students’ engagement with emergency medicine.
You may be asking yourself, “How can I make medicine more hospitable for my fellow gender diverse faculty and trainees?” Mel Ebeling, MS3 and a transgender/nonbinary person, shares a few high-yield actionable steps you can take in your department.
26
Legal Committee: Duty to Rescue: A Healthcare Perspective
As emergency physicians, what responsibility do we have to help others when we are removed from our hospital or other care services location? The “duty to rescue” legal doctrine is complex and varies throughout the U.S. it can be difficult to impossible to determine where the physician’s legal and moral duty lay.

VOICE OF THE AMERICAN ACADEMY OF EMERGENCY MEDICINE VOLUME 30, ISSUE 5 SEPTEMBER/OCTOBER 2023
“Why Me?”
S.
“Will the real highly educated, hardworking, self-sacrificing, altruistic, and supremely qualified doctor please stand up?”
Have you ever felt that you didn’t quite belong? Or that you were not fully prepared for the role you serve? Or maybe not the absolute best clinician for the patient in front of you? Or maybe not published enough for the promotion? Or not qualified for election? Or not expert enough to give a lecture?
While I wish this was a more interactive publication, alas, it is not, so instead of waiting for your reply, I will provide my answers. And my answers are: yes, without a doubt, clearly, certainly, every time, and absolutely.
any type of international emergency medicine. Heck, I don’t even like spicy food. I did think about my Indian roommate from medical school, my Indian friends, and the fact that my daughter had an absolute blast celebrating Diwali last year with some of her friends. But those really aren’t qualifications, so, I hesitated and declined, suggesting others who may be more appropriate.
I mostly forgot about the invitation and went back to my regular work…you know, the mundane task of helping people when they are most vulnerable. Time passed and after a few weeks I received a repeat invitation to the conference which was soon followed by a call. As I started to respectfully decline again and explain all the reasons I was not qualified to speak at the
ended, I immediately felt conflicted. I was excited but nervous. I was honored but apprehensive. I felt like a charlatan, an imposter.
OK, this column isn’t about me or India, but I needed some type of prologue.* I want to actually discuss Imposter Syndrome.
Webster defines Imposter Syndrome as: a psychological condition that is characterized by persistent doubt concerning one’s abilities or accomplishments accompanied by the fear of being exposed as a fraud despite evidence of one’s ongoing success.
About a year ago, research was published on the incidence and effects of Imposter Syndrome among physicians. The conclusions are straightforward and sadly not very surprising. Physicians have an increased incidence of Imposter Syndrome compared to other similar professions. Worse yet is that experiencing Imposter Syndrome is also associated with increased burnout, lower professional satisfaction, and even increased suicidal ideation.1

I was recently asked to speak and represent AAEM at EMIndia23 in Pune, India. I’d never been to India, but it certainly was a place I wanted to see. The invitation excited me, but after the first few minutes of excitement, I thought, “Why me?”

As mentioned, I’d never been to India. I did not know that much about Indian health care or emergency medicine. I’m not even an expert on
conference, I was politely interrupted and told, “No, we want you. We have plenty of experts on Indian emergency medicine, and they’re already invited too, but we want you. You are a leader in emergency medicine in the United States and we want your perspective.” (Perhaps that’s not an exact quote, but it’s fairly close.)
Somewhat reluctantly, I acquiesced and finally accepted the invitation. When the conversation
While Imposter Syndrome is the phrase most commonly used to describe this situation, more accurately, we should actually discuss Imposter Phenomena (IP) as it is a continuum. The above study was quite detailed and revealed many interesting findings but I want to touch on two. First, of all the medical specialties, emergency medicine has the second (technically third) highest imposter phenomenon score (highest is pediatric subspecialties, second highest is general pediatrics) which is perhaps not entirely surprising, at least given the way I feel when a sick kid presents to the ED. The second finding I want to point out is that female physicians have a higher score than male physicians (and while the n for other genders is incredibly small, “other” has an incredibly high imposter score, over 50% higher than the already high score for males). Somewhat surprisingly race and ethnicity were not categorized.
While overly simplistic, the first thing these findings make me think about is that we need to do more to support each other. We all need
>> AAEM PRESIDENT’S MESSAGE
Jonathan
Jones, MD FAAEM
COMMON SENSE SEPTEMBER/OCTOBER 2023 2
There are winners and losers and not every lecture is great. Not every effort deserves praise, but how many that do never receive it?
support and encouragement. The second comment I would like to make on the findings is that they state a fact, they describe a situation. While the discussion section raises some possible causes of increased IP in physicians, there is no clear cause and effect. To which I would like to add another simplistic statement of my own. IP is not a deficit of the physician experiencing it. IP is also not directly caused by the actions of one, two, or a handful of people. Rather, high IP scores among physicians are due to the system which has been created for us, shaped by us, and propagated by us. But while this unfortunate situation is more of a systems problem rather than an individual problem, it will require individuals to solve it. I am a firm believer in free will as well as our own ability to effect change. Which leads me off on a tangent, but I think it’ll work itself out.
I’m often made fun of by various others at work when I bring my metal water bottle from home instead of grabbing a bottled water from the work fridge. Similarly, I receive odd stares when I crush my can of sparkling water to bring back home so I can recycle it. Why do I do this? Because I happen to like our planet and the outdoor activities it provides me and I want that for others, not least of whom is my daughter. And because I believe that reducing, reusing, and recycling can actually help preserve that which I like. Sure, I burn fossil fuels and at times run my AC a little too much. I’m not perfect and I know that my act of recycling one aluminum bottle won’t make any difference in the world. But just because I am not perfect and just because my actions may not have a profound influence on the earth, it doesn’t mean that I shouldn’t try. And I view our battle with IP the same way.
I’ve witnessed numerous amazing lectures and then left the room to pursue my next goal without ever thanking the speaker. I’ve seen
tremendous work done by members of this Academy on committees and outside of committees and I have failed to thank them. I have seen the call for award nominations and have failed to nominate. I’m far from perfect and possibly far from good, but I try (at times). I also don’t think that I am alone. Could one small conversation from me or nomination by me help a colleague who may be struggling with Imposter Syndrome? I don’t know, but I think it could. It sure seems like it would be worth a try.
Which brings me to reflecting on an excellent recent lecture I had the pleasure to observe at MEMC23 in Rhodes by Molly Estes, MD. Ironically, I had this article partially written but was struggling with it when I attended her talk on…Imposter Syndrome. Hers was part of the Wellness II Session which included additional fascinating talks by Edward Ullman, MD, Michael Sperandeo, MD, Tim Cowan, MBBS, and Marianne Haughey, MD. Each of these physicians is a clear subject matter expert and also displayed excellent presentation skills.
It was a fascinating session and well planned. The various talks perfectly complemented each other and led into a conversation about both career and personal fulfillment, satisfaction, and accomplishment. While I thanked the speakers in private, I want to thank and praise them in public too.

I don’t want this to be interpreted as equivalent to every little league player getting a trophy or scores not being kept in soccer matches. No, this is real life. In fact, we practice in real life and death. There are winners and losers and not every lecture is great. Not every effort deserves praise, but how many that do never receive it?

I have no idea if any of the lecturers or the planners of this session have high IP scores or not. I do know that none of them are imposters. I also don’t know how many Common Sense readers have high IP scores. I do know that some do and as mentioned, I sure know that at least one Common Sense author does. While not every physician and not even every Academy member deserves praise and recognition, they are the outliers.
You are a board certified (or soon will be) emergency physician. Congratulations. This was not easy and you are already highly accomplished. You have dedicated you career to help others. You have volunteered your free time to be part of a professional academy dedicated to improving emergency care for all patients. Ignore those naysayers and negative influences. Now let’s all try to effect change one colleague at a time. That colleague whom you appreciate, the one with the knack for procedures, the one great with rashes, the one that is always willing to trade shifts—next time you see that one, tell them what you think of them. Maybe that one colleague has an IP score of zero and your interaction won’t make any difference whatsoever. Or maybe it will.
AAEM PRESIDENT’S MESSAGE
9
COMMON SENSE SEPTEMBER/OCTOBER 2023 3
“High [Imposter Phenomena] scores among physicians are due to the system which has been created for us, shaped by us, and propagated by us. But while this unfortunate situation is more of a systems problem rather than an individual problem, it will require individuals to solve it.”
Countinued on page
>>
Lessons Learned When I Was a Medical Director
Edwin Leap II, MD FAAEM
Ihave been a medical director for a total of 18 months. Spread, that is, over the course of my entire career. Basically I was director in a rural ED for one year and ‘co-director’ in another for about six months.
I learned a few things during those times. I realized, most powerfully, that my strength is not management. This is in no large part because I really don’t like confrontation. I also discovered that there is enormous inertia in any health care organization. People just don’t like change. The most common, and frustrating thing I heard was “well the thing is doc, we’ve always done it this way.”
I was a little surprised to discover that one of the hardest things to do is to cull out bad physicians. Even when everyone knows they’re bad, people feel sympathy and just hate to see them go or hate to offend them.
And I banged my head against the wall, over and over, when my hospital CEO (in my first directorship situation) asked me to improve staffing, with highly qualified physicians, but without any increase in pay to market levels.
However, I can share a few lessons I’ve contemplated that are relevant to people who are actually skilled directors and gifted managers. Because I have not only been a director, I have been mostly a “directee” for most of my career. Between the two I’ve seen both good and bad leaders.
If I were a director now, either a clinical director, or a hospital CEO or CMO, I would look at the difficulties of modern emergency medicine and I would focus first, and foremost, on my physicians. I would consider them the center of the clinical universe.
I would walk through the emergency department at least once a week, but hopefully more often. I would do it during the day and sometimes during the night. Not with an eye to criticism but encouragement. I would say “is there anything you need me to know? Is there anything we need to do from the administration side? What struggles are you facing?” I would not wait until the tidy, sterile department meetings which everyone wants to finish, but would do it in the place and at the time that my physicians were struggling.
I would not punctuate it with donuts, pizza, or Friday afternoon candy bars. Those are fine but can seem too much like gifts for toddlers who behaved well enough during the week.
If I were a director now, I would pay attention to difficult situations. When there were problematic consultants, transfers or call schedules, insufficient beds, disasters, power failures, EMR crashes, anything interrupting patient care, I would go to the department and say, “how can I help you right now?”
I would also recognize a much neglected point. We are taught to be sensitive to the complex emotional, cultural, and physical needs of our patients. And yet, our physicians are also complex. Our physicians, especially in emergency medicine, struggle with physical fatigue and pain, professional requirements, debt, toxic interactions, and horribly traumatic situations, all the while manage their own emotional issues and family dramas. I would try to be kind. As the old saying goes, “Be kind, for everyone you meet is fighting a great battle.”
It is a critical realization that physicians are not automatons, not financial problems to be solved, not puzzle pieces in the schedule, but human beings with their own unique struggles. This understanding can make it easier to face even the most difficult, or troubled physician. Along the same lines, I would keep a list of every physician’s birthday and anniversary, and a file with their successes, their triumphs, their good cases, their complimentary letters from patients and staff. I would honor them when such things occurred, and do it publicly.
And because physicians are typically representative of a family, I would send cards to their spouses, I would offer aid when their children were ill, I would celebrate their family triumphs and mourn their losses.
Many years ago my director interviewed my wife and me for my first job out of residency. He looked at Jan and said “I know your husband is qualified. What I want to know is what I can


EDITOR’S MESSAGE
>>
COMMON SENSE SEPTEMBER/OCTOBER 2023 4
“We are taught to be sensitive to the complex emotional, cultural, and physical needs of our patients. And yet, our physicians are also complex.”
do to make you happy.” Jan never forgot the way he made her feel both welcome and relevant.
He held quarterly group dinner meetings with spouses invited. It became a wonderful time of fellowship and also opened the door to discussions and dialogue. The reality is that the best director may miss a red flag, and a spouse who feels welcomed might be able to offer insights. Furthermore, if you want to motivate a physician to do things to increase billing and reimbursement, ask that physician’s spouse for help. They often write the checks and take care of the finances and they will get things done.
When COVID was unfolding, I was constantly stricken by the way that plans and protocols fell apart. Even more, I was amazed at the way physicians were given unrealistic expectations and demands to “find everyone a bed, transfer the sickest, hold them in the ED,” etc. All the while administrators were notoriously absent, and unable to suggest ways to

make those things happen. Worst of all, they just didn’t come by to see how things were going in person and to comfort and encourage their front-line physicians.
The way management treats physicians has more than emotional value. The job market is changing. I see advertisements every day for both employed and locums positions. The cost of filling those positions is rising as both new and seasoned physicians leave the specialty in frustration.
Retaining physicians will be key to the future. Treating physicians as valued and respected members of the team, and not as children or mere hired hands, will increase satisfaction and loyalty. And hopefully will result in more physicians staying in one job for 20 or 30 years, working happily and engaged in the community.
It is unlikely I will ever be an ED director again. (Although the schedule part is easy because my wife enjoys doing them as a kind of logic puzzle!)
But I will always watch and remember the way that directors manage not only the business and clinical care, but the human beings who see the sick, make the money, and give their all. Anyone who ignores that will lose my respect. Anyone who recognizes it will have my unwavering devotion.
PS: If you would like to submit a column, here are some suggestions:

1) Highlight your hobby. Tell us why you love it and how it helps you cope.
2) Discuss the way your personal philosophy or religious faith impacts your work. Atheists welcome!
3) Taken a cool trip? Write a travelogue and tell us why we should do the same trip!

“It is a critical realization that physicians are not automatons, not financial problems to be solved, not puzzle pieces in the schedule, but human beings with their own unique struggles.”
EDITOR’S MESSAGE
COMMON SENSE SEPTEMBER/OCTOBER 2023 5
AAEM Foundation Contributors – Thank You!
AAEM established its Foundation for the purposes of (1) studying and providing education relating to the access and availability of emergency medical care and (2) defending the rights of patients to receive such care and emergency physicians to provide such care. The latter purpose may include providing financial support for litigation to further these objectives. The Foundation will limit financial support to cases involving physician practice rights and cases involving a broad public interest. Contributions to the Foundation are tax deductible.
Levels of recognition to those who donate to the AAEM Foundation have been established. The information below includes a list of the different levels of contributions. The Foundation would like to thank the individuals below who contributed from 1/1/2023 to 9/1/2023.
Contributions $1000 and above
Algis J. Baliunas, MD FAAEM
Babak Khazaeni, MD FAAEM
David W. Lawhorn, MD MAAEM
Jonathan S. Jones, MD FAAEM
Kathryn Getzewich, MD FAAEM
Laura J. Bontempo, MD MEd FAAEM
Mark Reiter, MD MBA MAAEM FAAEM
Oscar A. Marcilla, MD FAAEM
Thomas R. Tobin, MD MBA FAAEM
Contributions $500-$999
Fred Earl Kency, Jr., MD FAAEM
Pedro I. Perez, MD FAAEM
Robert A. Frolichstein, MD FAAEM
Ronald T. Genova, MD
Timothy J. Titchner, MD FAAEM
Contributions $250-$499
Bradley Houts, MD FAAEM
David Thomas Williams, MD FAAEM
Eric D. Lucas, MD FAAEM
Floyd W. Hartsell, MD FAAEM
Jeffrey J. Thompson, MD FAAEM
Kenneth Scott Hickey, MD FAAEM FACEP
Laura Richey, MD FAAEM
Marc R. Houston, DO FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Ming-Jay Jeffrey Wu, MD FAAEM
Nayla M. Delgado Torres, FAAEM
Piotr Jurgielewicz, MD
Robert J. Feldman, MD FAAEM
Shane Coughlin, MD
Travis J. Maiers, MD FAAEM
Contributions $100-$249
Adam C. Benzing, MD MPH
Alexander Tsukerman, MD FAAEM
Andrew Thomas Larkin, DO FAAEM
Anisha Malhotra, MD FAAEM
Ann Loudermilk, MD FAAEM
Arnold Feltoon, MD FAAEM
Barry N. Heller, MD FAAEM
Brian J. Browne, MD FAAEM
Brian J. Cutcliffe, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Bruce E. Lohman, MD FAAEM
Bryan Knoedler, MD
Catherine V. Perry, MD FAAEM
Chaiya Laoteppitaks, MD FAAEM
D. Scott Moore, MS DO FAAEM
David R. Steinbruner, MD FAAEM
David Wang, MD FAAEM
Denis J. Dollard, MD FAAEM
Donald L. Slack, MD FAAEM
Douglas P. Slabaugh, DO FAAEM
Gary M. Gaddis, MD PhD MAAEM
FAAEM FIFEM
H. Samuel Ko, MD MBA FAAEM
Irene Tien, MD FAAEM
Jason M. Driggs, MD FAAEM
Jeffrey A. Rey, MD FAAEM
Jenna Otter, MD FAAEM
Jessica Moore, MD
Jonathon D. Palmer, MD FAAEM
Kathleen Hayward, MD FAAEM
Katrina Green, MD FAAEM
Katrina Kissman, MD FAAEM
Marc D. Squillante, DO FAAEM
Nancy Conroy, MD FAAEM
Neeharika Bhatnagar, MD FAAEM
Patrick B. Hinfey, MD FAAEM
Paul W. Gabriel, MD FAAEM
Philip Beattie, MD FAAEM
Renee Marie Nilan, MD FAAEM
Riley MW Williams, MD MBA
Robert Boyd Tober, MD FAAEM
Rohan Janwadkar, MD
Roland S. Waguespack III, MD MBA FAAEM
Sameer D. Mistry, MD MBA CPE FAAEM
Tim J. Carr, FAAEM
Timothy J. Durkin, DO FAAEM CAQSM
William E. Franklin, DO MBA FAAEM
Yeshvant Talati, MD
Contributions up to $99
Alexander J. Yeats, Jr., MD FAAEM
Alexander S. Maybury, MD FAAEM
Amie Rose, MD
Andrew J. Bleinberger, MD
Benson Yeh, MD FAAEM
Brian Gacioch, FAAEM
Caitlin E. Sandman, DO FAAEM
Christopher Laugier
David C. Crutchfield, MD FAAEM
Edward T. Grove, MD FAAEM MSPH
Eric M. Rudnick, MD FAAEM
Ernest H. Leber Jr., MD FAAEM
AAEM PAC Contributors – Thank You!
Contributions $500-$999
Mark S. Penner, DO FAAEM
Ronald T. Genova, MD
Contributions $250-$499
Bradley Houts, MD FAAEM
Fred Earl Kency, Jr., MD FAAEM
Joseph T. Bleier, MD FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Michael L. Martino, MD FAAEM
Paul W. Gabriel, MD FAAEM
Thomas B. Ramirez, MD FAAEM
Tim J. Carr, FAAEM
Travis J. Maiers, MD FAAEM
Contributions $100-$249
Alexander S. Maybury, MD FAAEM
Erol Kohli, MD MPH FAAEM
Everett T. Fuller, MD FAAEM
James P. Alva, MD FAAEM
James R. Gardner, FAAEM
Jason J. Morris, DO FAAEM
Joanne Williams, MD MAAEM FAAEM
Jonathan Y. Lee, MD FAAEM
Jose G. Zavaleta, MD
Joseph M. Reardon, MD MPH FAAEM
Kelly Dougherty, MD
Kenneth T. Larsen, Jr., MD FAAEM
Kevin C. Reed, MD FAAEM
Linda Sanders, MD FAAEM
Marianne Haughey, MD FAAEM
Matthew Mosko Mass, DO
Megan Crossman, MD FAAEM
Michael Lajeunesse, MD
Michael Timothy Schultz, MD FAAEM
Michael West
Neal Handly, MD
Om Pathak, DO
Peter H. Hibberd, MD FACEP FAAEM
Peter M.C. DeBlieux, MD FAAEM
Peter Stueve, DO
Sachin J. Shah, MD FAAEM
Samuel M. Morris, MD
Scott Beaudoin, MD FAAEM
Stacy G. Hooks, MD
Tabitha Williams, FAAEM
Virgle O. Herrin Jr., MD FAAEM
AAEM PAC is the political action committee of the American Academy of Emergency Medicine. Through AAEM PAC, the Academy is able to support legislation and effect change on behalf of its members and with consideration to their unique concerns. Our dedicated efforts will help to improve the overall quality of health care in our country and to improve the lot of all emergency physicians.
All contributions are voluntary and the suggested amount of contribution is only a suggestion. The amount given by the contributor, or the refusal to give, will not benefit or disadvantage the person being solicited.
Levels of recognition to those who donate to the AAEM PAC have been established. The information below includes a list of the different levels of contributions. The PAC would like to thank the individuals below who contributed from 1/1/2023 to 9/1/2023.
Alexander Tsukerman, MD FAAEM
Brian J. Cutcliffe, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Bruce E. Lohman, MD FAAEM
Catherine V. Perry, MD FAAEM
David W. Lawhorn, MD MAAEM
Donald L. Slack, MD FAAEM
Garrett Sterling, MD FAAEM
Gary M. Gaddis, MD PhD MAAEM
FAAEM FIFEM
Jeffrey A. Rey, MD FAAEM
Jeffrey J. Thompson, MD FAAEM
Joseph M. Reardon, MD MPH FAAEM
Katrina Green, MD FAAEM
Nicole M. Braxley, MD MPH FAAEM
Philip Beattie, MD FAAEM
R. Lee Chilton III, MD FAAEM
Raviraj J. Patel, MD FAAEM
Riley MW Williams, MD MBA
Robert Boyd Tober, MD FAAEM
Robert M. Esposito, DO FAAEM
Stewart Sanford, MD FAAEM
William E. Franklin, DO MBA FAAEM
Contributions up to $99
Alex Kaplan, MD FAAEM
Amie Rose, MD
Andrew J. Bleinberger, MD
Brice Guy, DO
Chaiya Laoteppitaks, MD FAAEM
David L. Sincavage, Jr., MD FAAEM
David R. Steinbruner, MD FAAEM
Eric M. Rudnick, MD FAAEM
Erol Kohli, MD MPH FAAEM
James R. Gardner, FAAEM
Jason J. Morris, DO FAAEM
Kevin C. Reed, MD FAAEM
Laura M. Mory, MD FAAEM
Linda Sanders, MD FAAEM
Marc D. Squillante, DO FAAEM
Om Pathak, DO
Peter H. Hibberd, MD FACEP FAAEM
Peter Stueve, DO
Ruth P. Crider, MD FAAEM
Tabitha Williams, FAAEM
Virgle O. Herrin Jr., MD FAAEM
COMMON SENSE SEPTEMBER/OCTOBER 2023 6
LEAD-EM Contributors – Thank You!
The AAEM Institute for Leadership, Education & Advancement in the Development of Emergency Medicine, Inc. (LEAD-EM) was established after the tragic and unexpected death of AAEM president, Dr. Kevin G. Rodgers.
The Kevin G. Rodgers Fund and the Institute will LEAD-EM just like Dr. Rodgers did. The funds will support important projects such as development of leadership qualities, and clinical and operational knowledge of emergency physicians with a view toward improving and advancing the quality of medical care in emergency medicine, and public health, safety and well-being overall. LEAD-EM would like to thank the individuals below who contributed from 1/1/2023 to 9/1/2023.
Contributions $1000 and above
Jonathan S. Jones, MD FAAEM
Contributions $500-$999
Fred Earl Kency, Jr., MD FAAEM
Mark Reiter, MD MBA MAAEM FAAEM
Contributions $250-$499
David W. Lawhorn, MD MAAEM
Dale S. Birenbaum, MD FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Mary Ann H. Trephan, MD FAAEM
Contributions $100-$249
Alexander S. Maybury, MD FAAEM
Ann Loudermilk, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Catherine V. Perry, MD FAAEM
Christopher Kang, MD FAAEM
David R. Steinbruner, MD FAAEM
Edward T. Grove, MD FAAEM MSPH
Gary M. Gaddis, MD PhD MAAEM
FAAEM FIFEM
Joseph M. Reardon, MD MPH FAAEM
Kathleen Hayward, MD FAAEM
Kevin C. Reed, MD FAAEM
Paul W. Gabriel, MD FAAEM
Roland S. Waguespack III, MD MBA
FAAEM
Contributions up to $99
Alicia J. Starr, DO
Erol Kohli, MD MPH FAAEM
Jose G. Zavaleta, MD
Marc D. Squillante, DO FAAEM
Om Pathak, DO
Richard G. Foutch, DO FAAEM
Samantha Abramovich
Samuel M. Morris, MD
Virgle O. Herrin Jr., MD FAAEM
Upcoming Events: AAEM Directly, Jointly Provided, & Recommended
AAEM is featuring the following upcoming conferences and activities for your consideration. For a complete listing of upcoming conferences and other meetings, please visit: aaem.org/education/events
AAEM Events
October 25, 2023
AAEMLa Annual Education Symposium
October 26, 2023
GLAAEM Virtual Annual Education Symposium
November 29 & 30, 2023
Oral Board Review Courses aaem.org/education/events/oral-boards
March 6, 2024
DVAAEM Annual Residents’ Day Save the Date!
April 27-May 1, 2024
30th Annual Scientific Assembly (Austin, TX) aaem.org/aaem24
Jointly Provided
Re-Occurring Monthly
Unmute Your Probe: Virtual Ultrasound Webinar Series
Jointly provided by EUS-AAEM aaem.org/get-involved/sections/eus/resources/unmute-your-probe/
Re-Occurring Monthly
Spanish Education Series*
Jointly provided by the AAEM International Committee aaem.org/get-involved/committees/committee-groups/international/ spanish-education-series
September 19-23, 2023
UC Davis Emergency Medicine Hot Topics (Maui, HI)
Jointly provided by UC Davis ces-apps.ucdavis.edu/confreg/?confid=1257
October 16-20, 2023
Essential Emergency Medicine: Can’t Misses in EM - Cardiac Misfortunes, Environmental Misadventures, and Unfortunate Misdiagnoses (Lake George, NY)
Jointly provided by EssentialCME essentialcme.com/conferences
Recommended
Advances in Cancer ImmunotherapyTM: sitcancer.org/education/aci
• August 17, 2023 - A Focus on Cellular Therapies and T cell Engagers (Washington, DC and Virtual)
• October 19, 2023 - A Focus on Hematologic Malignancies (Virtual)
The Difficult Airway Course: Emergency™: theairwaysite.com/a-course/the-difficult-airway-course-emergency/
• September 22 - 24, 2023 - San Diego, CA
• October 20 - 22, 2023 - Washington, D.C.
• November 17 - 19, 2023 - New Orleans, LA
Online CME
• Recognizing Life-Threatening Emergencies in People with VEDS thesullivangroup.com/TSG_UG/VEDSAAEM/
COMMON SENSE SEPTEMBER/OCTOBER 2023 7
Your Financial Health: Considerations for Each Stage of Your Career
 Chris McNeil, MD
Chris McNeil, MD
Dr. Edwin Leap and AAEM asked that I contribute some financial wellness topics to this outstanding publication, and I am ecstatic to join AAEM’s group of esteemed authors. After much deliberation, I have decided to open my post by sharing some observations from my own life and my clients that you may find helpful, particularly if you are beginning your career.
Like many of you, I am an emergency physician. I have practiced in the military, academics, the community, and through various global health projects. I’m old enough to know well that most of us never had formal training during medical school or residency on financial planning, investments, or business management. When beginning to pad my own retirement and investment accounts several years ago, I decided to learn more about the nitty-gritty of finance. I found I enjoy teaching other physicians about all aspects of financial planning. Hence, I obtained a securities license and transitioned my career as a physician to a partner in a financial planning firm.
As an introduction to this learning corner, I will focus on broad financial strategies for those in different career stages. In future articles, I may discuss specific investment strategies, financial planning topics, or anything you prefer. This issue, I want to share some practical observations I have seen working with physicians who enter my new office setting. Knowing what is coming around the corner can be helpful for everyone.
Early Career
Early in our careers, we are excited to finally start making money and working independently. This also is when many of us start families, buy homes, and are pulled in many directions, with life unfolding very quickly. Falling behind or procrastinating in caring for our financial lives is common. At this early career stage, most of us have been bombarded by those trying to sell us life or disability insurance, so we know the need to consider savings. Most also quickly learn that managing debts (student loans), contributing as much as possible to retirement accounts, starting an emergency fund, and attempting to live within our means are essential. However, making these goals a reality is often easier said than done.
This is typically the point when someone comes to my office with a multitude of questions. The basics are nearly covered—now what? At this point, there are typically four things that have been overlooked:
• Establishing liquidity
• Setting up a will and other legal documents
• Thinking about an ideal career path
• What type of investor are we?
Establishing liquidity early on provides enormous flexibility in our lives. This is accomplished by starting to invest outside of your retirement accounts. I encourage opening and investing in a taxable brokerage account as soon as possible. You can use this money for anything without the strings attached to retirement accounts. Early in our careers, we tend to change jobs more frequently and move more often. Things come up. If we throw all of our extra money towards our student loans, we can’t reborrow it to use when we have to move our family because the first job we took turned out not to be the most ideal. Accumulating investments outside of our retirement accounts provides us with options when life throws a curveball.
Setting up a will is pretty straightforward and just needs to be done, especially if you have children.
Another often overlooked item is establishing career goals. How much we need to save and what types of investment returns we are looking for is based on how we will ultimately use the money. Do we want to work full-time until retirement? Is that age 65? Or 70? Might we want to switch careers at some point? Night shifts don’t get easier. At the beginning of our careers, we can plan appropriately to financially support the career(s) we want. I often meet people early in their careers who plan to decrease their work hours in their mid-50s and hope to work part-time for as long as they are professionally satisfied. Do you have a similar plan?
FINANCIAL WELLNESS
COMMON SENSE SEPTEMBER/OCTOBER 2023 8
“Early in our careers, we are excited to finally start making money and working independently…Falling behind or procrastinating in caring for our financial lives is common.”
>>
Lastly, this is the time in your career to determine what type of investor you are and what your risk tolerance is. Each of our situations is unique. Our personal history with money, our relationship with savings, our exposure to money growing up, and our specific goals help us decide the type of investment risk we are willing to accept to reach our goals. The longer we have until we need the money, such as retirement, which is 30 years away, the more growth-oriented our investments should be. This generally refers to our exposure to stocks in our portfolios. I know many people desire YOLO options, meme stocks, and Bitcoin. Those are all fine in the proper proportions. Just remember, you didn’t finish residency to be a day trader. You completed training to have a long and fulfilling career in emergency medicine. There is no shame in obtaining help with a savings plan.
Mid-Career
Once night shifts start to hurt more than you remember from residency, you have officially transitioned to a mid-career investor. You are now closer to retirement than to graduating from medical school. In our mid-careers, if things work out, we often have much more sizable financial accounts than when we finished residency. We all know the stock market can be volatile, but we still need our investments to grow in our mid-career. The typical 10-15% market corrections each year feel much different when your accounts are more considerable, even though the percentage drawdown is the same. Sleeping at night when your account is down $10K is easier than when you’re down $400K. Psychologically preparing for this reality and frequently revisiting your risk tolerance and goals is extremely important.
Mid-career physicians often have a couple of other unique issues to consider. This is typically the time when our parents start to have health problems, and we may need to provide financial assistance. Planning ahead and discussing end-of-life issues with our parents is vital to avoid this blind spot in our financial plans. Life happens fast, and one day you wake up after a night shift and your kids are leaving for college. You have spent the last 15-20 years focusing on being an extraordinary physician and parent. Life happens to us all. It is common to feel a little behind in your savings and unprepared for the future. It is not quite panic time, but clearly, a time to reassess your situation and develop a solid game plan.
Later Career
Wealth preservation and income generation are paramount as we near retirement or move into post-retirement. We begin transitioning our investment strategies to support efficient withdrawals to cover our cost of living. By this time, if we have saved well, we are used to adding to our accounts and watching them grow. It can be disconcerting to start withdrawing money and watch the funds diminish. Dollar-cost averaging out of your retirement accounts is much different than systematically adding to them, and often people need help developing a plan for this strategy.
Near retirement is when many start to think about legacy planning as well. Finally, this is when the reality of savings shortfalls causes extreme dyspepsia. The world is not ending if you are behind in your savings at this stage, but you must begin creatively thinking outside the box if you find yourself in a shortfall. This is when retirement planning is most valuable, even if you have just started at this stage. How much cash flow do you need to be satisfied with your retirement life? Are there alternative ways to generate cash flow besides seeing the next back pain at 3:00am?
In conclusion, financial planning at each stage of our careers is constructive and somewhat unique. There are distinctive issues at each stage and things you may have yet to consider. I highly recommend working with someone you trust. A financial advisor with a fresh set of eyes can help identify your blind spots, navigate the different stages of your financial life, and serve as your accountability partner to routinely ensure you are making progress toward your goals.
Dr. Chris McNeil is an emergency physician and former emergency medicine residency program director who transitioned his career to finance. He owns a registered investment advisory firm, VitalStone Financial, LLC, and specializes in financial planning for physicians.
References
* I had a wonderful visit to India and was quite impressed with the EMIndia Conference. The Academy and our colleagues in India share very similar opinions about EM and we have numerous opportunities for future collaboration. I made many new friends and cannot say enough about how wonderful an experience it was. I want to congratulate the organizers on an amazing conference and thank them for their hospitality.
FINANCIAL WELLNESS
“How much cash flow do you need to be satisfied with your retirement life? Are there alternative ways to generate cash flow besides seeing the next back pain at 3:00am?”
1. Shanafelt TD, Dyrbye LN, Sinsky C, Trockel M, Makowski MS, Tutty M, Wang H, Carlasare LE, West CP. Imposter Phenomenon in US Physicians Relative to the US Working Population. Mayo Clin Proc. 2022 Nov;97(11):1981-1993. doi: 10.1016/j.mayocp.2022.06.021. Epub 2022 Sep 15. PMID: 36116974.
COMMON SENSE SEPTEMBER/OCTOBER 2023 9
AAEM PRESIDENT’S MESSAGE Countinued from page 3 >>
An Update on Due Process
Gregory Jasani, MD FAAEM, Government and National Affairs Committee Co-Chair

Due process is the right to appeal a termination through a hearing before a committee of members of the hospital staff. It is a right that every emergency medicine physician should have. Unfortunately, many of us do not. Many contracts, especially those offered by Corporate Medical Groups, force us to waive those rights. As emergency medicine physicians, we have a duty to advocate for our patients, many of whom are disadvantaged and vulnerable. Yet, advocating for ourselves and our patients can create friction with hospital and CMG leadership. Without due process protection, we may be forced to choose between protecting our patients and protecting our livelihoods.
Fortunately, the issue of enshrining due process protections for emergency medicine physicians has reached our legislators in Congress. During a previous session, Reps. Ruiz (D-CA) and Marshall (R-KS), both physicians themselves, introduced a bill to make it illegal for hospitals or CMGs to force physicians to waive their due process protections as a condition of employment. Sadly, as with many bills introduced in Congress, this one never made it to the floor for a vote.
AAEM is committed to ensuring this legislation ultimately passes. The Board of Directors and our lobbyists are working with supportive members of Congress to determine the best path forward for this bill. Most likely, the due process legislation will be added on as an amendment to another bill that is already on the floor for a vote.

Although bipartisanship may seem increasingly rare these days, this issue actually enjoys a fair amount of it. Currently, our lobbyists have identified Democrats and Republicans in the House who would be willing to sponsor the bill (either as its own bill or as an amendment). In the Senate, we have Republicans who are willing to sponsor this legislation. However, we do not currently have a Democratic senator who has committed to supporting this legislation.
Finding a supportive Democratic senator is currently our biggest need on this issue. Having bicameral support across the aisle will not only facilitate the legislation’s passage but will also send a strong message that our government supports our right to fair employment practices.
On behalf of the Government and National Affairs Committee, I am asking all of you to write to your senators and congressmen and women to tell them how important this issue is to you. Certainly, if you live in a state with a Democratic senator, please let him or her know how vital this issue is to your ability to advocate for your patients (see the list of Democratic senators on page 22). However, even if your state does not have a Democratic senator, still write! Your members need to hear from you on this issue. If you are having writer’s block, the Government and National Affairs Committee will be circulating a form letter you can use.
We are physicians but we are also advocates for our patients. To properly do either job, we can’t be worried that we can be arbitrarily fired. Due process is a right but a right many of us are sadly denied. We can change that. Let your legislators know that this issue is a significant issue for you. Hopefully, this will be the last Congressional Session where AAEM has to lobby for it.
GOVERNMENT AND NATIONAL AFFAIRS COMMITTEE
COMMON SENSE SEPTEMBER/OCTOBER 2023 10
“The issue of enshrining due process protections for EM physicians has reached our legislators in Congress… Sadly, as with many bills introduced in Congress, this one never made it to the floor for a vote”
Paging Dr. TikTok
Tai Donovan, MS4 and Mel Ebeling, MS3

APlatform for the People


Imagine opening your TikTok app, scrolling through an endless arrangement of entertaining content when, amongst the dance routines, comedic skits, and viral challenges, a particular video captures your attention. In this video, an eager doctor takes you through the breakdown of the symptoms associated with a potentially life-threatening medical emergency and gives advice on when you should go to the emergency room. The doctor—through engaging storytelling and a trending beat—can convey vital knowledge that you would have never known or even thought to ask. This information could possibly make a difference in recognizing and responding to the situation promptly. Everyone in the comment section feels the same way you do and expresses the desire to learn
education methods in effectively reaching underserved communities, social media, like TikTok have emerged as a valuable tool.2 It effectively bridges the information gap by presenting complex medical concepts in a visually stimulating and easily comprehensible format, resulting in crucial information becoming more accessible and engaging for the audience. With its massive user base and global reach, Tik Tok provides medical pro-

SOCIAL MEDIA COMMITTEE
COMMON SENSE SEPTEMBER/OCTOBER 2023 11
significant responsibility and influence that the platform holds when using it as


networking, authorship, and project involvement on a national scale. However,

SOCIAL MEDIA COMMITTEE
>> COMMON SENSE SEPTEMBER/OCTOBER 2023 12
from residents and attendings can bring

COMMON SENSE SEPTEMBER/OCTOBER 2023 13
YPS: Empowering Physician Advocacy and Fostering Resources for Young Emergency Medicine Physicians
 Moiz Qureshi, MD MBA
Moiz Qureshi, MD MBA

AAEM has long been a vanguard in championing physician advocacy and supporting the development of young emergency medicine physicians. As the premier professional organization for emergency medicine physicians in the United States, AAEM’s unwavering commitment to advancing the interests of its members and advocating for the highest standards of patient care sets it apart. This year, the Young Physicians Section (YPS) is looking to make substantial strides to focus its efforts on physician advocacy and bolster resources dedicated to nurturing the next generation of emergency medicine physicians.
At the core of AAEM’s mission lies in a strong belief in the value of physician advocacy: recognizing that the collective voice of emergency medicine physicians holds the potential to drive meaningful change in the health care landscape. Now, more than ever that advocacy is needed. With the recent news of multiple contract management groups declaring bankruptcy or ceasing operations, many emergency docs, both young and seasoned, find themselves in a terrible predicament. Some unpaid, some without reassuring malpractice coverage, and many without their next source of sustenance. For young physicians who have not had sufficient time to build a sound savings or investment account, this period is especially difficult.
YPS-AAEM stands at the forefront of physician advocacy and reiterates its unwavering support for young emergency medicine physicians. As

this year of change progresses, the YPS board aims to cultivate a generation of physicians who are not only skilled in their craft but also adept at advocating for their profession and patients alike. With this in mind, YPS is diligently working to develop comprehensive resources that cater specifically to the needs of young physicians. Ranging from mentorship and networking opportunities to building a virtual toolkit of professional advocacy resources and “life after residency” tips, YPS wants to ensure that young physicians are equipped with the knowledge and support necessary to thrive both personally and professionally.
As the general emergency medicine landscape treads into uncharted territory, young emergency medicine physicians will undoubtedly carry the torch for their patients and the specialty alike. By empowering young physicians to advocate for our profession and fostering a nurturing environment for new talent, AAEM and YPS are sowing the seeds for a brighter future for the practice of emergency medicine and stand at the forefront of positive change, driving innovation, and embracing the challenges of the healthcare industry with resilience and determination.
YOUNG PHYSICIANS SECTION
COMMON SENSE SEPTEMBER/OCTOBER 2023 14
“As the general emergency medicine landscape treads into uncharted territory, young emergency medicine physicians will undoubtedly carry the torch for their patients and the specialty alike.”
Telemedicine: Enhance Your Career and Wellness
David Hoyer, MD FAAEM

Telemedicine is a true game-changer in that many of the common diseases that afflict patients can be dealt with virtually. Of course that means physicians can now bypass the health care industrial complex (HIC), with its physician burnout and high costs for patients.

The list of manageable telemedicine chief complaints includes (but is not limited to) UTI, sore throat, COVID, cough, sinusitis, vomiting and diarrhea, rash, hay fever, anxiety, depression, nontraumatic back pain, and pink eye.
Starting with UTI, adult women with dysuria, urgency, and frequency without back pain or vaginal discharge have a 96% probability of uncomplicated UTI and can be treated empirically without any lab work.1 Many women have multiple UTIs per year and are very grateful when they can log on to their computer and within an hour have prescriptions sent electronically to their pharmacy instead of waiting to see their doctor.
especially valuable in treating COVID as the medications like Paxlovid generally need to be started ASAP and usually within five days of symptom onset. By the time patients have a positive COVID test it is often two to three days into the illness and by then, with the shortage of primary care doctors, it may not be possible to otherwise get the care they need without generating an expensive bill.
Cough, sinusitis, vomiting and diarrhea, rash, hay fever, nontraumatic back pain, and pink eye usually do not need tests in the ER and so, can generally be managed virtually. For anxiety, the GAD7 is a useful tool to see if a patient warrants psych referral, with breathing exercises and perhaps a short prescription for a benzo in the interim.3 Depression can be screened for with the InSADCAGES mnemonic.4 Patients who screen positive and who are not suicidal can be started on an SSRI (like sertraline 50mg/day or citalopram 20mg/day) provided they can follow-up within a couple weeks.5
For sore throat the Centor criteria can be used to decide between antibiotics or symptomatic treatment.2 Centor gives one point each for pharyngeal exudates, fever, absence of cough, tender cervical adenopathy, and patient age under 15 (-1 for age over 44). With a total of four to five points you can treat empirically with antibiotics. A score of two to three warrants referral to the PCP in two to three days. Centor, which has been widely used in the British National Health System for years, has the advantage over Rapid Strep in that it will allow antibiotic treatment of Fusobacterium Necrophorum and other non-strep bacterial causes of pharyngitis.
Obviously certain problems like chest pain, dyspnea of unknown etiology, abdominal pain, and ear pain are generally outside the scope of telemedicine. Ear pain may come off that list once the kiosks that allow photos of patients’ tympanic membranes become more widely available. Fortunately, EMTALA does not apply to telemedicine (outside of emergency departments), so you can decline any patient that makes you uncomfortable with a reason like “needs in person exam” or “needs to go to the ER.” Also, patients are generally good at self-triaging more serious illnesses away from telemedicine. I always document vital signs
AGING WELL IN EMERGENCY MEDICINE INTEREST GROUP
>>
COMMON SENSE SEPTEMBER/OCTOBER 2023 15
“Telemedicine allows one to work as much or as little as wanted and still do what many of us love, which is taking care of patients based upon evidencebased medicine without HIC nuisances like PressGaney scores.”
including a pulse as part of my physical exam to ensure I am not missing something. Patients almost always either have an Apple watch that gives a heart rate, or they can count their radial pulse while I time them. Of course, like in the ER, I always discuss when, why, and where I want the patient to follow-up. And there is invariably time for that discussion as I am rarely pressed for time doing telemedicine.
The health care cost savings with telemedicine could be enormous. There is almost no overhead with telemedicine and physicians can see any patient in their state of licensure, which should help with patients’ lack of access to health care as well. If I see four patients on telemedicine, anecdotally one would have gone to the ER, one to urgent care, one to their PCP, and one would have stayed home in the past.6 If those three patients I see each pay a customary $50 for their visit, I don’t think I need to do the math for the reader to see what the savings could be to our patients over time. Health insurance companies are realizing the potential; United Healthcare will be waiving co-pays for telemedicine as 25% of their patients’ ER visits could be handled virtually.7 Since our HIC is the most expensive in the world, leaving many patients with poor access, crushing medical debt, and even bankruptcies, telemedicine can truly be a game-changing benefit.
Telemedicine should benefit our climate, which is warming at least in part due to human activities. The HIC is a contributor, from employees and patients driving to and from sites, large facility power needs and much unrecyclable waste.8
References
1. Roberts JR. An Update on Routine Urinalysis: Microscopy. Emergency Medicine News. 42(11): 12-13, November 2020.
2. MDCalc. Mobile app. Available from: Apple App Store. Accessed 25 July 2023.
3. US Preventive Services Task Force. Screening for Anxiety Disorders in Adults. JAMA. 2023; 329(24): 2163-2170.
4. Hoyer D. Screening for Depression in Emergency Department Patients. The Journal of Emergency Medicine. 2012; 43(5): 786-789.
5. Hoyer D. Depression in the Emergency Department’. In: Zun L.S. (ed.), Behavioral Emergencies for Healthcare Providers. Springer, Cham. 89-93.
Telemedicine is not for everyone. The biggest losers should be the private equity plutocrats on Wall Street and the countless administrators who all have been taking over health care and raising costs for patients.9 Not all physicians will be interested as incomes would be less for most. However physicians deprived of income either voluntarily or involuntarily by the HIC can do telemedicine while they go through the onerous months long credentialing process of new employment. It would behoove any physician who does not have tenure or due process to get credentialed at one of the national telemedicine providers like Amwell, Teladoc, or MDLive as an employment “safety net.” The other category of physicians who can greatly benefit are those at the end of their careers.10 Physicians are prone to hang on past when they no longer need or enjoy working, for many reasons. Telemedicine allows one to work as much or as little as wanted and still do what many of us love, which is taking care of patients based upon evidence-based medicine without HIC nuisances like Press-Ganey scores.
A final note, telemedicine has the best patients I have seen in my 42 years of practice. These patients are seen in the comfort of their own home and so are not saddled with the ER hostility generators of a strange, disease laden facility with long waits and the fear that a large bill is in the works. That also means that telemedicine patients tend to be actually grateful for your time and expertise and generally are happy when they do not need to leave home to get a prescription, which can do wonders for a physician’s wellness.
6. Haleem A, Javaid M, Singh RP, Suman R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int. 2021; 2:100117.
7. Gilyard B. “United Healthcare drops out-of-pocket charge for telehealth”. Houston Chronicle, 6 July 2023, Page B12.
8. Patel KB, Gonzalez BD, Turner K, et al. Estimated Carbon Emissions Savings With Shifts From In-Person Visits to Telemedicine for Patients With Cancer. JAMA Netw Open. 2023; 6(1): e2253788.
9. Whoriskey P. “Private equity firms drive surge in U.S. medical prices”. Houston Chronicle, 11 July 2023, Page B9.
10. Leap E. Extend Your Career with Telemedicine. Emergency Medicine News, 42(7): p 14, July 2020.

AGING WELL IN EMERGENCY MEDICINE INTEREST GROUP
COMMON SENSE SEPTEMBER/OCTOBER 2023 16
Introducing the Mental Health Action Plan

The mental health of health care workers remains a constant challenge, exacerbated not only by the demanding nature of our work but also by the stigma and limitations we face when seeking mental health care. Emergency physicians faced mental health challenges even before the pandemic due to constant exposure to vicarious trauma and moral injury.1 Additionally, physicians encounter added barriers and potential licensing ramifications when they seek mental health care. When Dr. Lorna Breen, an emergency physician in New York City, tragically died by suicide during the height of the pandemic, it sparked multiple advocacy efforts towards receiving mental health care that have had a promising impact in raising awareness and legislation. The resulting Dr. Lorna Breen Health Care Provider Protection Act aims to reduce the stigma of seeking mental health assistance among health care professionals.2 The Dr. Lorna Breen Heroes’ Foundation and the #StopTheStigmaEM campaign have also worked diligently to increase awareness of the stigma surrounding mental health care.3,4 Though such admirable efforts have been made on a broader community scale, we need to pay more attention to our own individual mental health needs.
Indeed, a significant obstacle that continues to hinder progress in supporting physicians’ mental health is the mistaken notion that mental health care is exclusively meant for individuals with mental health disorders. Overcoming this misconception is crucial to providing better support for medical professionals. While we have well-studied and evidence-based algorithms, protocols, and contingency plans for our patients and their conditions, we often fall short when it comes to taking care of ourselves. In fact, a shift towards proactive and preventative mental health maintenance is essential, rather than solely focusing on addressing crises after they have already begun. Encouraging regular check-ins and implementing such measures can help physicians cope with the challenges we face in our demanding roles.
To that end, we propose a Mental Health Action Plan, comprising two components: promotion of self-awareness of your mental health state and pre-planned proactive measures executed according to that state. Considering the busy schedules of medical professionals and trainees, we must be mindful that additional wellness modules, tasks, and workshops may impinge upon much-needed self-care time. Recognizing that different strategies work for different people, we aim to provide manageable resources and ideas to avoid overwhelming individuals.
“[A] significant obstacle that continues to hinder progress in supporting physicians’ mental health is the mistaken notion that mental health care is exclusively meant for individuals with mental health disorders ”

Think for a moment when someone asks you what you do to relax or reset. What ideas come to you first? How would your answers change if you had a particularly challenging day? What happens to your relaxation ideas when you notice yourself feeling angry, frustrated, and in need of a break? Do you currently have a plan in place to actively navigate through those states of mind and get yourself back to a place of peace? It is immensely more difficult to find your bearings in the middle of the storm; let us instead devise the plan before the storm even hits us.
Similar to planning for surge crises like mass casualty events or natural disasters in the emergency department, our proposal addresses mental health needs at different urgency levels. In interacting with the mental health sector, fourth-year medical student Kelly Kossen noticed a gap in mental health care planning: it seemed to be focused on suicide and




COMMITTEE
WELLNESS
Theresa Adams, MS4,* Kelly Kossen, MS4, † Neha Bhatnagar, MD FAAEM, ‡ Al’ai Alvarez, MD FAAEM, § and Robyn Hitchcock MD FAAEM
>> COMMON SENSE SEPTEMBER/OCTOBER 2023 17

WELLNESS COMMITTEE >> COMMON SENSE SEPTEMBER/OCTOBER 2023 18
The Mental Health Action Plan:
Green = Go. Preventative daily measures, self-check-ins, keeping our wellness tank full.
Yellow/Orange = Caution. When your tank is running low, what are some things you can do to refresh, reach out, and refuel? Choose from this pre-planned list instead of having to think about a plan when you are already feeling run down.
Red = Danger. Recognize when you are in crisis or your tank is running on fumes. Use these resources for help, whether from loved ones or from mental health professionals/resources such as crisis helplines.
Example Actions for a Mental Health Action Plan
GREEN YELLOW RED
• Express a Gratitude7
• Affirmations
• Drink water
• Sunlight, outdoor air
• Text a loved one
• Movement: exercise, dance, walk, stretch
• Self-care: hygiene routine
• Savoring
• Awe8
• Humor and Laughter
Yoga9
• Reading
• Call a loved one
• Nap
• Self-care: long shower or bath, lotion, gentle stretching, facial
• Creative outlets: art, music, dance
• Longer meditation session
• Raise your “Beauty to Death Ratio” as Dr. Levitan says10
• Box Breathing11
• Grounding
• See a loved one in person or virtually
• Mental health professionals
• NPSA hotline12
• Sleep
• Avoid substances
• Safe venting activity: Rage Room, axe throwing, vigorous physical activity13,14
• Journaling
• Sunshine files or other visualization exercises that create mental space to visit to remember your purpose, priorities, and successes15
• Comfort Food: preplanned and portion controlled
• Podcast
References
*UQ-Ochsner Clinical School, @tessacatie
WELLNESS COMMITTEE
COMMON SENSE SEPTEMBER/OCTOBER 2023 19
mental health crises rather than on prevention. Therefore, we seek to implement a Mental Health Action Plan (MHAP). This plan includes daily mental health maintenance exercises and clear strategies for recognizing worsening symptoms and handling emergencies. On September 17, we observe National Physician Suicide Awareness Day. Building on that initiative’s Personal Crisis Management Plan, which lays out a structure for personal support in times of crisis, our MHAP endeavors to delineate actions that can be taken to bolster mental wellbeing in moderately stressful times, or even in times of low stress.5 It is essential to distinguish such mental health maintenance from mental health illness
In implementing a MHAP, we suggest you organize activities and resources based on their frequency of use: daily, occasional, or during crises. Additionally, you may incorporate Mental Health Vital Signs to proactively monitor your current mental state and remind you of pre-planned activities that you assigned for various states.6 Develop a protocol to triage yourself: Did you feel your patience slipping today? How is your appetite? How have you been sleeping? Are you enjoying your breaks or have you forgotten to even take them? Have you talked out loud about what is running through your head? It may be hard to notice how taxed we have become because we are so accustomed to dealing with unimaginable
References
†UQ-Ochsner Clinical School
‡Jefferson New Jersey, @nbhatnagar_md
§Stanford University, @alvarezzzy
¶Providence Mount Carmel hospital, stethoscopesuitcasemd.wordpress.com
1. Jacobs, BB. An alternate explanation for the 2023 Match: Emergency medicine physicians endure repeated workplace moral distress and our students are watching. Acad Emerg Med. 2023; 00: 1- 3. doi:10.1111/ acem.14761
2. H.R.1667 - 117th Congress (2021-2022): Dr. Lorna Breen Health Care Provider Protection Act. (2022, March 18). https://www.congress.gov/ bill/117th-congress/house-bill/1667
3. About the foundation | Dr. Lorna Breen Heroes Foundation. (n.d.). https:// drlornabreen.org/about-the-foundation/
4. Stop the Stigma EM- A Toolkit for Individuals, Educators & Institutions. (n.d.). Default. https://www.saem.org/education/saem-online-academicresources/wellness-and-resilience/StopTheStigmaEM
5. NPSA Personal Crisis Management Plan. (n.d.) https://npsaday.org/wpcontent/uploads/2022/09/Prepare-Before-a-Moment-of-Crisis.pdf
6. PAMQ. (2022, February 1). Tools and resources - PAMQ. https://www. pamq.org/en/tools-resources/ and https://www.pamq.org/wp-content/ uploads/2021/08/checking-our-mental-health-vital-signs.pdf
7. App Store. (2018, August 1). Delightful: Gratitude Journal. https://apps. apple.com/us/app/delightful-gratitude-journal/id1414957610
8. Awe Research | The Awe Project. (n.d.). The Awe Project. https:// www.5daysofawe.com/aweresearch
9. Busby, M. (2022, October 9). Why the health benefits of laughter yoga will make you smile. The Guardian. https://www.theguardian.com/ lifeandstyle/2022/oct/09/why-the-health-benefits-of-laughter-yoga-willmake-you-smile
stressors on a daily basis. With these regular conscious self-check-in’s, you can keep your reservoir full and course correct before you get to the crisis zone. This MHAP encourages creativity in determining actions that would be enjoyable and rejuvenating yet practical and accessible. Actions would thus be tailored to the needs of each emergency physician in maintaining their own mental well-being. See below for an example of what such a MHAP would look like and a few examples of activities from our own personal lists. To be clear, we have no affiliations or financial disclosures related to the activities or sites listed. Please share your ideas with the AAEM Wellness Section on social media and at the next Scientific Assembly in Austin, TX!
Emergency medicine is a challenging specialty, but you are not alone. Support is available to help you through the experience. The first step is awareness, and we encourage continuous learning about proactive mental health maintenance. In October, AAEM and national emergency medicine organizations observe #StopTheStigmaEM month, promoting awareness, advocating for mental health, and removing barriers to seeking care. Together, we can foster a healthier and more supportive environment for all. We wish you well in developing your own Mental Health Action Plan.
10. Acadia Airway and Sedation Course | Airway Cam. (n.d.). Airway Cam. https://www.airwaycam.com/acadia
11. WebMD Editorial Contributors. (2021, April 9). What is box breathing? WebMD. https://www.webmd.com/balance/what-is-box-breathing
12. https://npsaday.org/toolkit/
13. Rage Room Austin, TX | United States | www.TheBreakingPointAustin. com. (n.d.). The Breaking Point. https://www.thebreakingpointaustin.com/
14. https://batlgrounds.com/axe-throwing-nashville/
15. https://positivepsychology.com/visualization-techniques/
16. Wellness Committee - AAEM/RSA. (2023, June 30). AAEM/RSA. https:// www.aaemrsa.org/get-involved/committees/wellness/
17. AMA Steps Forward: Transform your Practice. (n.d.). https://edhub.amaassn.org/steps-forward
18. AMA Steps Forward Podcast - Compassion as a tool for burnout. (n.d.). https://edhub.ama-assn.org/steps-forward/audio-player/18796567
19. Kevin. (2023, February 14). The invisible graveyard of every physician’s career: Why every doctor needs a “badness” plan. KevinMD.com. https:// www.kevinmd.com/2023/03/the-invisible-graveyard-of-every-physicianscareer-why-every-doctor-needs-a-badness-plan.html
20. Chen, A. (2019). A personal Crisis management plan for residents. https:// escholarship.org/uc/item/1v91z16g
21. Mulholland, H. (2018, January 22). Alys Cole-King: ‘Suicide is a tragedy – particularly when it is a doctor or nurse.’ The Guardian. https://www. theguardian.com/society/2018/jan/16/alys-cole-king-suicide-nhs-doctorsnurses-winter-crisis
22. MIMS Learning. (n.d.). https://www.mimslearning.co.uk/courses/safetyplanning-to-mitigate-against-the-effects-of-stress
23. Sutton, J., PhD. (2022). Visualization in Therapy: 16 Simple Techniques & Tools. PositivePsychology.com. https://positivepsychology.com/ visualization-techniques/
WELLNESS COMMITTEE COMMON SENSE SEPTEMBER/OCTOBER 2023 20
Breaking Burnout with an Emergency Department Debrief
Allison Lane, MD and Lisa Stoneking, MD

The Emergency Department (ED) is a high-stress environment where staffing shortages, legal documentation requirements, and high acuity medical presentations, among other stressors, can all quickly lead to an exhaustive or even hazardous work environment.1 Functioning at its best, the ED operates with a certain level of organized chaos, drawing many thrill-seeking professionals to the field. However, the slightest disturbance in the workflow can drastically alter the operating environment of the ED, and over time, if left uncorrected, can contribute to burnout. Many programs and facilities have begun to utilize post-event, real-time debriefing exercises to combat this stress and reduce staff burnout.
Burnout is multifactorial and different from person to person, but themes that remain consistent in most health care professionals include emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment.2 While it may initially sound like a physician’s problem, burnout is a public health issue in that it leads to two times the risk of medical errors.1 Depersonalization and compassion fatigue carry the potential of resultant carelessness, placing both the patient and physician at risk of harm. And as expected, physician burnout in the post-COVID era is on the rise. Emergency medicine has seen the most significant increase in burnout, which has steadily increased from 45% in 2018 to 65% in 2022, according to the “Medscape Physician Burnout & Depression Reports.”3 With burnout comes the exodus of physicians from the field in effort to find more fulfilling or less stressful ways of earning income. This exodus leaves gaps in ED staffing which delays patient turnover, further congests the system, and contributes to the compounding cycle of stress within the ED.
Debriefs offer a way out of the cycle for many departments and can increase physician longevity. The benefits of debriefs expand beyond that of the individual physician. Interdisciplinary debriefs benefit all personnel involved in the patient encounter and should not be restricted to physicians, residents, or even nursing staff. In one study analyzing the behaviors of first responders who completed a debrief following an adverse or traumatic patient encounter,
Debriefing Card
inhibiting or biasing the discussion. Other team members may not feel welcome or willing to contribute or participate. In addition, there are studies showing lack of utilization by attending physicians. In response, some departments are choosing nurse initiated or led debriefings to increase the frequency and quality of the debriefing session. Regardless of the system used, guidelines must be established, including who initiates and leads the debrief, what is
Charge Nurse please read statements below prior to starting
1) “The purpose of debriefing is for education, quality improvement, and emotional processing; it is not a blaming session. Everyone’s participation is welcome and encouraged.”
2) “These debriefings usually take several minutes and if you have urgent issues to attend to you are welcome to leave at any time.”
3) “We will briefly review the patient’s summary. Then as an entire team, we can discuss what went well and what could have gone better. Please feel free to ask any questions.”
there were statistically significant reductions in alcohol use post-event compared to control groups who did not complete a debrief.4 Apart from the psychological benefits of debriefs, studies have demonstrated improved clinical outcomes with utilization of debriefs as well, including improved rate of return of spontaneous circulation, neurologic outcomes, hands-off compression times, and time delay to first compression following post-event debriefs in clinical cardiopulmonary resuscitation events.5 With benefits including improvement in quality of care expanding to improvement in quality of life and/or work atmosphere, debriefs appear to be a necessary, but underutilized, tool within the health care system.
Most ED debriefs involve the entire patient care team and are typically physician led. There is some data, however, that cautions against having an authority figure leading for fear of

discussed, where the debrief occurs, and the allotted time for these discussions to succeed. The debriefing should occur as soon as possible after the event, occur over a maximum of 10 to 15 minutes, and all members should be encouraged to give feedback or ask questions.6
An example would be a charge nurse initiated debrief paged out to all involved staff to meet in the doc box for a 10-minute post event
ACADEMIC AFFAIRS COMMITTEE AND WELLNESS COMMITTEE
Figure 1
“Debriefs offer a way out of the cycle for many departments and can increase physician longevity.”
>> COMMON SENSE SEPTEMBER/OCTOBER 2023 21
discussion. The charge nurse would state that the purpose of the debrief is for education, quality improvement, and emotional processing and that it is not a blaming session. Participation is encouraged, followed by a brief summary and discussion of what went well and what could have gone better. (See Figure 1 for a sample debrief card that can be used to facilitate an ED debrief.)
Debriefs allow for individualized and collaborative mindful reflection following adverse or traumatic events. This brief pause fosters a supportive environment and can help to reduce staff stress and burnout, leading to healthier work environments, higher productivity, and improved quality of life for ED employees. Given the multifactorial aspect of burnout, debriefs
References
1. Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and Medical Errors Among American Surgeons. Ann Surg. 2010;251(6):995-1000. doi:10.1097/SLA.0b013e3181bfdab3
2. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516-529. doi:10.1111/joim.12752
3. Kane, L.; (2022, January 21). Physician Burnout & Depression Report 2022: Stress, Anxiety and Anger. Medscape.
4. Tuckey MR, Scott JE; Group Critical Incident Stress Debriefing with Emergency Services Personnel: A Randomized Controlled Trial. Anxiety Stress Coping. 2014 Jan;27(1):38-54. doi: 10.1080/10615806.2013.809421
5. Nadir NA, Bentley S, Papanagnou D, Bajaj K, Rinnert S, Sinert R. Characteristics of real-time, non-critical incident debriefing practices in the emergency department. West J Emerg Med. 2017;18(1):146-151. doi:10.5811/westjem.2016.10.31467
List of Democratic Senators by State
Senator Tammy Baldwin (D-WI)
Senator Michael Bennett (D-CO)
Senator Richard Blumenthal (D-CT)
Senator Cory Booker (D-NJ)
Senator Sherrod Brown (D-OH)
Senator Maria Cantwell (D-WA)
Senator Ben Cardin (D-MD)
Senator Tom Carper (D-DE)
Senator Bob Casey (D-PA)
Senator Chris Coons (D-DE)
Senator Catherine Cortez Masto (D-NV)
Senator Tammy Duckworth (D-IL)
Senator Dick Durbin (D-IL)
Senator Dianne Feinstein (D-CA)
Senator John Fetterman (D-PA)
Senator Kirsten Gillibrand (D-NY)
Senator Maggie Hassan (D-NH)
can only partially absolve this issue. It will not change some contributing factors such as the bureaucratic tasks like charting, understaffing, government regulations, nor hours or pay. However, it may help with staff and colleague communication and respect.3 While the most commonly stated primary barrier to debriefing is time constraint, even short debriefs lasting under five minutes have been reported to be successful.5,7 The option to debrief or not debrief relies on several factors unique to each ED. However, in performing a cost risk analysis, it is essential to consider the immediate time expense necessary to complete a debrief alongside the long-term expense of not completing a debrief.
6. Lane, AD.; Bryce, E; Milbrandt, MR.; and Stoneking, LR; Who Leads the Emergency Department Debrief? Journal of Wellness. 2022. Vol. 4: Iss. 2, Article 3. DOI: https://doi.org/10.55504/2578-9333.1166
7. Dubash R, Govindasamy LS, Bertenshaw C, Ho JH. Debriefing in the Emergency Department. Emerg Med Australas. 2021;33(5):922-924. doi:10.1111/1742-6723.13855
8. Brazil V, Symon B, Twigg S. Clinical debriefing in the emergency department. Emerg Med Australas. 2021;33(5):778-779. doi:10.1111/1742-6723.13834
9. Holleman WL, Cofta-Woerpel LM, Gritz ER. Stress and Morale of Academic Biomedical Scientists. Academic Medicine. 2015; 90 (5): 562564. doi: 10.1097/ACM.0000000000000533.
Senator Martin Heinrich (D-NM)
Senator John Hickenlooper (D-CO)
Senator Mazie Hirono (D-HI)
Senator Tim Kaine (D-VA)
Senator Mark Kelly (D-AZ)
Senator Angus King (I-MI)
Senator Amy Klobuchar (D-MN)
Senator Ben Ray Lujan (D-NM)
Senator Joe Manchin (D-WV)
Senator Ed Markey (D-MA)
Senator Bob Menendez (D-NJ)
Senator Jeff Merkley (D-OR)
Senator Chris Murphy (D-CT)
Senator Patty Murphy (D-WA)
Senator Jon Ossof (D-GA)
Senator Alex Padilla (D-CA)
Senator Gary Peters (D-MI)
Senator Jack Reed (D-RI)
Senator Jacky Rosen (D-NV)
Senator Bernie Sanders (I-VT)
Senator Brian Schatz (D-HI)
Senator Chuck Schumer (D-NY)
Senator Jeanne Shaheen (D-NH)
Senator Krysten Sinema (I-AZ)
Senator Tina Smith (D-MN)
Senator Debbie Stabenow (D-MI)
Senator Jon Tester (D-MO)
Senator Christ Van Hollen (D-MD)
Senator Mark Warner (D-VA)
Senator Raphael Warnock (D-GA)
Senator Elizabeth Warren (D-MA)
Senator Peter Welch (D-VT)
Senator Sheldon Whitehouse (D-RI)
Senator Ron Wyden (D-OR)
ACADEMIC AFFAIRS COMMITTEE AND WELLNESS COMMITTEE
COMMON SENSE SEPTEMBER/OCTOBER 2023 22
Partnerships!
Leah Colucci, MD MS

AAEM/RSA is working on increasing sponsorships and partnerships! Two that I would love to highlight this month are the EMS/EIIC and The Laceration Course.
EMSC/EIIC: Emergency Medical Services for Children Innovation and Improvement Center

This group focuses on pediatric readiness and is currently conducting the National Pediatric Readiness Project and the Prehospital Pediatric Readiness Project. Children have unique characteristics that require specialized emergency care. Pediatric Readiness is ensuring that every EMS agency and emergency department has the pediatric-specific champions, competencies, policies, equipment, and other resources needed to provide high-quality emergency care for children. If you are wanting support in equipping your ED to become pediatric ready you can join a hands-on collaborative for quality improvement. If your focus is helping your EMS colleagues become more situated for children there are toolkits and checklists available for your local agencies.
Find more information here: emscimprovement.center
The Laceration Course

This course is lead with Dr. Patrick O’Malley and EB Medicine. There are 13 modules of online videos that cover simple to complex wounds with step-by-step guidance and demonstrations. Facial wounds, vermillion borders, bites, jagged edges, and even topics on medicolegal are covered. Laceration repairs are the leading causes of medical malpractice so this course will teach you not just how to repair with the best cosmetic outcome but also how to properly document. Through RSA you receive a significant discount to this course as well as a practice suture kit with a silicone pad that includes lips. Additionally with this partnership you also get free access to Emergency Medicine Practice (EMP) and Pediatric Emergency Medicine Practice (PEMP).

Dr. O’Malley is putting on webinars for RSA and is also seeking a resident interested in laceration repair research! Keep an eye out for these opportunities.
We are excited about these expanding partnerships. If there are other organizations you know of that have similar values to AAEM/RSA, please reach out to president@ aaemrsa.org so we can pursue a relationship!
AAEM/RSA PRESIDENT’S MESSAGE
COMMON SENSE SEPTEMBER/OCTOBER 2023 23
To Be a “They/Them” in Medicine: A Call for Active Allyship
 Mel Ebeling, MS3
Mel Ebeling, MS3
Fist clenched, wrist extended, arm raised, and knuckles just inches away from the door, I see it and pause. A sizable, laminated sign on the entrance to the patient’s room reads “FEMALE PROVIDERS PREFERRED.” To enter or not to enter? My arm drops limply to my side. I look over my shoulder and usher my fellow medical student, the pinnacle of femininity, into the room. I am transgender nonbinary.
Alone in the hallway, I ponder my decision. What matters more—that I am biologically female, that I once knew what it meant to be a “woman” despite my best wishes, or that I am now just a shade of gray between the extremes of pink and blue? What is included in “female”? What does the patient really want? Would any of it even matter if I didn’t have an undercut? I will never know.
Further complicating my predicament are the variable perceptions imposed on me by residents and attendings, their treatment of me in constant flux. The “they/them/theirs” badge buddy, a second pronoun pin, and the pride flag pin on my white coat—what I jokingly call the “triple threat”—are useless. Whether I am introduced to patients as a “he,” “she,” or “they” is a roll of the dice. Often, I am more than one of these in a single patient encounter (interestingly, the patients tend to get it right more often). Some of this is my own fault. When I transition to a different subrotation every one to two weeks, I feel unmotivated to insert my pronouns in my introductions to team members, as this is usually ineffective anyway. I like to rely on the “signage” adorning my uniform and the ambiguity of my appearance to get me through. And if they get it wrong? Water off a duck’s back; I will be on a new service soon enough.
But what happens when I start residency or my career as an attending and finally start working in one environment with a more stable group of colleagues? Then it will be more important to me that my team acknowledges and respects my identity. I imagine that this sentiment is shared by other gender diverse physicians. Unfortunately, many transgender and nonbinary physicians have experienced hearing derogatory remarks about their gender identity and have had to censor themselves to avoid disclosure of their identity out of fear of discrimination.1
In a time where anti-trans legislation is rising across the country, being an ally is more important than ever and requires more than not just hating someone for who they are. If you are a cisgender ally, you may be asking yourself at this point, “How can I make medicine more hospitable for my fellow gender diverse faculty and trainees?” I am so glad you asked.
Albeit just one transgender trainee’s perspective, here are few high-yield actionable steps you can take:
Make it commonplace to display pronouns. If your hospital system does not automatically print pronouns on official badges, encourage your department to use pronoun stickers on their badge or pins on their lanyard. Even better, supply one of these items to make it more standardized and normalized.

Put effort into using correct pronouns but do not over-apologize. We understand that slip-ups happen—it is okay! You are likely not the first, nor last, person to make that mistake. However, over-apologizing makes the situation uncomfortable and places an unfair burden on us to provide consolation for guilt. A simple, brief apology before moving onto the next topic of conversation will suffice.
Educate yourself. If you have a gender diverse colleague on your team, it
may be tempting to punt all questions regarding medical care for similar patients to them. However, while we may have some insight, just being gender diverse does not qualify us as subject matter experts on gender affirming care or LGBTQ+ health. The WPATH Standards of Care exist for a reason. Seek out opportunities for continuing medical education so that we can all be better for our patients and colleagues.
Never assume. You know what Oscar Wilde said about assuming! In casual conversations with any colleague, try to keep language neutral and never assume. For example, “Do you have a spouse/partner?” is better than “Do you have a husband/wife?”
AAEM/RSA EDITOR’S MESSAGE
>>
COMMON SENSE SEPTEMBER/OCTOBER 2023 24
“You may be asking yourself at this point, ‘How can I make medicine more hospitable for my fellow gender diverse faculty and trainees?’ I am so glad you asked.”
Do not ask us if we have had gender-affirming surgery or what kind. It should not have to be said, but this is inappropriate to ask unless the gender diverse person in question has clearly opened that topic up for discussion. It is like if a colleague randomly asked you if you had a vasectomy/breast implants/etc. Additionally, if caring for a gender diverse patient, this conversation is only justified if the knowledge obtained is relevant to their current care (i.e., if the chief complaint is a sinus infection, this is not the situation to be asking the patient what kind of genitalia they have).
Speak up. Allyship requires standing with us in the face of prejudice and discrimination. All too often, it seems that those who call themselves allies become silent when the assaults start. Your support in helping us fight against mistreatment is important!
Despite not being an exhaustive list, practicing these simple measures are important in helping transform the workplace into one where gender diverse trainees and physicians can thrive. Remember, it is when medicine becomes more diverse and inclusive through conscious effort that we can better identify and meet the unique health needs of every patient.

References
1. Dimant OE, Cook TE, Greene RE, Radix AE. Experiences of Transgender and Gender Nonbinary Medical Students and Physicians. Transgend Health. 2019;4(1):209-216. Published 2019 Sep 23. doi:10.1089/ trgh.2019.0021

AAEM/RSA EDITOR’S MESSAGE
COMMON SENSE SEPTEMBER/OCTOBER 2023 25
“Remember, it is when medicine becomes more diverse and inclusive through conscious effort that we can better identify and meet the unique health needs of every patient.”
Duty to Rescue: A Health Care Perspective
Richard I. Suarez, JM and Tessa Haspil-Corgan, MD
Introduction
As a medical practitioner, the concept of providing your services and expertise to care for others is engrained in the training and functioning of the day-to-day happenings of being in the field. Physicians and other level practitioners consider what needs to be accomplished in order to help an individual in need, such as what parts of the physical exam should be focused on, what diagnostic studies are needed, what labs should be ordered, and what is needed to manage this condition(s), among many others. However, when the medical personnel are removed from the context of the hospital, clinic, or other care services location, what responsibility is there to help others? Specifically, what duty is owed to rescue? This question strikes deep into the sense of morality and empathy shared in a society, but assumingly more so in a profession dedicated to the care of others.
A “duty to rescue” is a legal doctrine found (or rather absent) in the American tort law system. A “duty” is a matter of a policy determination in which the judge makes the decision of including the case or class of cases within tort liability or not. Therefore, a duty can be seen as the responsibility to act (or not), promoting an idea of connection to the existence of an obligation. In general, when it comes to strangers, there is no duty to rescue because strangers have no connection/relationship/obligation to one another, despite the fact that the lack of action when someone could help without endangering their lives may be seen as wrongful or unreasonable, regardless. However, do medical doctors and other practitioners not have an obligation to help all those in need based on the oaths and responsibilities set forth by their profession? The big questions rest in the context, and whether individuals who swear their time and lives to protecting and serving people must serve and protect at all times.
The idea of the force, scope, and justification of this duty and its application in the medical arena has been considered by bioethicists.1 Specifically, it has been proposed that clinicians encounter these scenarios frequently within the clinical context and beyond, such as the discovery of incidental findings and their subsequent care, the participation in research, and the allocation of resources for research and development, among others.2-5 In addition, current statutes, like Good (and “Bad”)
Samaritan laws, and common law, such as the Tarasoff decision, promote this idea of rescue for practitioners. When we consider the role that the foundational principles of medical ethics—beneficence, non-maleficence, justice, and autonomy—play in the actions and moral obligations of practitioners, there is an argument for this “duty to rescue” being an unnamed fifth principle interweaved amongst the others.

Though there has been legal analysis into the basis of the tort doctrine, as well as medical specialists’ commentary on the place this doctrine has within (and outside) the clinical context, there are few comprehensive integrations of the two disciplines surrounding the idea of rescue. In this article, we will describe what is the “duty to rescue” and the legal arguments that support its inclusion in modern day tort law, alongside the byproducts that have arisen because of it (Good Samaritan statutes). We will then discuss how this doctrine plays into the medical landscape and impacts, directly and indirectly, the processes of clinicians. Finally, we will incorporate the two arenas into one encompassing the idea of the “duty to rescue” in a combined, ample, multi-disciplinary approach. Overall, we aim to explain one of the many interactions of these two fields of study and demonstrate the importance of this analytic exercise in an effort to better understand the overlapping nature of these two distinct yet intertwined academic spheres.
A Duty to Rescue: Legal Analysis
When we consider the morality of a society, it appears immoral to not help others in need when one is able to do so. However, bystanders have no obligation, with few exceptions, to provide aid, even when reasonably feasible without harm to self. This is due to the rule of no “duty to rescue” set forth within the American tort law system. In this section, we will explore what is this tenet, why it exists in the modern-day legal system and derivatives of its establishment, specifically, “Good Samaritan” laws.
What is the “Duty to Rescue”?
Before we can discuss this duty (or lack thereof), it is important to provide a foundational understanding of legal principles. This doctrine is part of the general American tort system. A tort is defined as “an act or omission
>>
LEGAL COMMITTEE
COMMON SENSE SEPTEMBER/OCTOBER 2023 26
"The big questions rest in the context, and whether individuals who swear their time and lives to protecting and serving people must serve and protect at all times.”
that gives rise to injury or harm to another and amounts to a civil wrong for which courts impose liability…”injury” describes the invasion of any legal right, whereas “harm” describes a loss or detriment in fact that an individual suffers.”6 With this in mind, the inclusion of this no-duty within this framework is logical as it relates to the actions or lack of actions that an individual partakes in that subsequently could change the outlook of someone who is in need of rescue. Moreover, tort law can be further subdivided into intentional, negligent, and strict, with the former two taking into account the degree of care the defendant had, and the latter focuses on specific instances.6 The idea of negligence implies the idea of reasonability, which is the basis for this doctrine, manifesting a “nearly pervasive duty to act with at least reasonable care regarding other persons and their property.”7
A “reasonable” action is defined by the “industry standard,” which demonstrates what most people with the same or similar circumstances would have done and this comparison is used to determine whether an action was done negligently.8 For example, a neurosurgeon who makes a mistake during surgery and results in harm to a patient will be evaluated by what other neurosurgeons posed with similar circumstances would have done. Now, an industry standard may not always exist, or it may be challenged, which introduces another mechanism of defining reasonableness, known as the “Learned Hand Formula.”9,10 Essentially, this formula looks at cost of precautions to avoid harm versus the cost of the harm that could have been avoided had precautions been used/followed. Overall, the idea of negligence is critical to understanding the no-duty to rescue because essentially this doctrine exists in this zone between where the reasonability of an omission of action and/or related precautions necessary to ensure care and prevent harm is irrelevant as no duty to be reasonable manifested itself in the first place.
Therefore, what is the no-duty to rescue? Within the tort system, there is no legal duty to affirmatively act to aid a stranger in peril, no matter how reasonable a readily available affirmative act might be.7 For instance, if one was walking in Central Park and happened to see a random individual drowning in one of the ponds, and one was say an Olympic swimmer whom could easily maintain themselves in the water while saving this person, one would have no legal obligation to save them. Although morally unrighteous, within the law, there is no need to reasonably act in this circumstance or others when strangers are in peril.
Now, an important element of this rule is in essence the lack of an existence of a relationship between the involved parties, which would skew the line of stranger and bystander. Exceptions to this rule usually arise due to the blurring of these distinct roles within society. One exception is found if the harm towards the stranger was caused by the bystander, such as if a someone was skating through Central Park and in order to get through the crowd had to be less than graceful to the other pedestrians and through these actions one of these strangers fell in the pond. Another exception would be if a bystander begins to save the stranger and then stops. For example, if one sees someone drowning in one of the ponds in Central Park and goes into save the individual but while
doing so realizes they cannot swim when holding the person and then stops rendering aid, that bystander is no longer protected under this rule. In general, this doctrine exists within the legal context of tort—and more specifically negligence—and despite its exceptions, covers a wide variety of scenarios that protect inaction no matter the consequences.
Why do we still have the No-Duty to Rescue?
This no-duty to rescue appears to be a stain on the idea of morality and the perception that the law is intended to protect people from a multitude of harms through the gaze of justice. Yet, a doctrine such as not helping strangers in peril robustly exists within it and provides protections for these omissions of action. The question becomes why would the American tort system preserve such a rule? Legal scholars have debated this idea and have identified seven arguments that support its continued inclusion in the tort arena (Table 1).7
Table 1:
Rationales Supporting the No-Duty to Rescue
Slight benefit to coercive (verus uncoercive) rule
Reluctant rescuers
Discounted altruism
Intrusiveness of negligence law’s duty to reasonable care
Harm to the rescuer
Disincentive to cooperate with future investigations
Deter providing delayed aid
The brief discussion surrounding these seven arguments is adapted from previous legal analysis in the field.7
Slight benefit to coercive (versus uncoercive) rule: Due to the innate morality widely accepted by society to help others, this argument poses the question: why make a rule that coerces action when many others already act without the fear of litigation? Thus, the assumption is that there is no need to make a normal instinct a rule that implies legal action if not taken for only a small benefit.
Reluctant rescuers: In the opposite vein to the above, those who would not aid strangers in peril with the current no-duty are likely to still not change their behavior because of the new ruling. This can be related to the idea of likelihood of identification of the non-responder, which diminishes the practicality of the rule.
Discounted altruism: By requiring that others help those in peril, rather than allowing individuals to do so in an altruistic nature, this would foster compliance but devalue the beauty of an act of assistance without reward or personal benefit. Similarly, those who would not help without this duty will likely produce a lower “quality” of rescue, which furthers the idea of mere compliance rather than moral righteousness.
LEGAL COMMITTEE
>> COMMON SENSE SEPTEMBER/OCTOBER 2023 27
Intrusiveness of negligence law’s duty to reasonable care: Within the realm of negligence lies the “industry standard” and the Learned Hand formula, creations of the system that enforce oversight and regulation in the current legal schema. The development of a duty to rescue obliterates this gray zone that exists for this no-duty within negligence which would intrude on every aspect of individual choices and judgements due to fear of litigation.
Harm to the rescuer: Rescue is not always without harm. Though the current no-duty does not only apply to those circumstances that would be dangerous for the rescuer, the implementation of a duty to rescue would undeniably place individuals at risk of harm by forcing salvage in all cases. Consequently, by imposing this rule to attempt to generate as many successful outcomes for those in peril as possible, more victims may be the outcome.
Disincentive to cooperate with future investigations:
As it stands, bystanders, because they face no legal liability to assist those in peril, have no reasons preventing them from cooperating with investigations related to the situations. However, if this became a mandated duty, those who failed to render aid in the event would be less likely to provide details surrounding the circumstances because the liability that would fall upon them for their inaction.
Deter providing delayed aid: A duty would discourage those who may not have intervened at first from offering their aid later. This is because by returning, the delayed rescuer risks identification and realization of their initial failure to help, which could be used against them for legal liability.
All in all, the arguments for the preservation of the current non-duty are grounded in the ideas of limited overall benefit and increased cost (morally and financially), which offers important insight into the functioning of this doctrine within the modern American tort system.
Brief Overview of Good Samaritan Laws
Based on the ideas of tort liability, negligence there within and the idea of no “duty to rescue,” there is an implication of how this doctrine may have an influence outside of their established parameters. With this in mind, it is plausible to see the “Good Samaritan” laws as a direct result of this lack of duty, essentially a means of creating a “duty to rescue” (with limits).
“Good Samaritan” laws were developed under the premise of a favorable public policy initiative that sought to encourage intervention to help others without the promise of compensation and limited (if any) liability for the events that transpired during the aid.11 Originally aimed at promoting physicians and other health care professionals to respond to medical emergencies outside of the clinical setting, these statutes are meant to provide general protections from claims of negligence when care is provided and there is no expectation of exchange of money. Of note, these laws do not protect against all negligence, rather only “ordinary” negligence, defined as a “failure to act as a reasonably prudent person… failure to exercise such care as the great mass of humanity ordinarily applies under the same or similar circumstances.”11 Similarly, when we consider physicians and other practitioners, there must be no existing relationship (i.e., no existing duty to treat). Thus, the concept of the “Good Samaritan” is not meant to allow any and all actions amongst any and all people to be protected from legal liability, rather simply those related to emergency aid not rendered maliciously to strangers.
In the United States, every state, and the District of Columbia (D.C.) have their own “Good Samaritan” statutes with variability across state lines, but with the same general foundation. However, certain states have created “Bad Samaritan” laws, meant to establish a duty to aid (Minnesota, Rhode Island, Vermont) or at a minimal, a duty to report (Hawaii, Washington, Wisconsin).11 In addition, there have been modified versions of the “Good Samaritan” statutes that cover drug overdoses—known as “911 Good Samaritan” which provides some immunity for drug users and witnesses of overdoses who call for help—as well as ones that include AED usage.11 The implications on medical professionals and effectiveness of these statues will be explored later in this paper. An overview of the different types of laws are outlined in Figure 1.
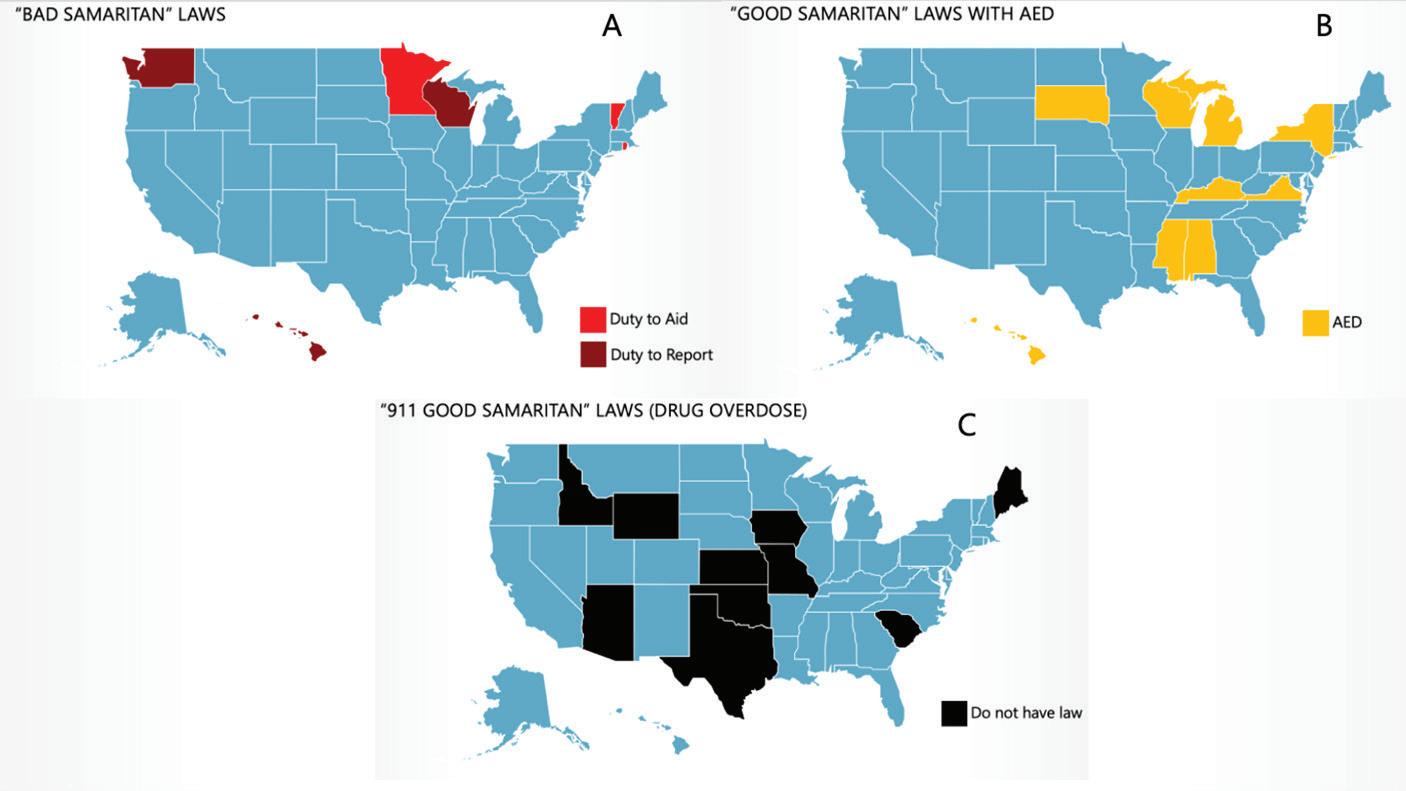
LEGAL COMMITTEE
>>
COMMON SENSE SEPTEMBER/OCTOBER 2023 28
Figure 1: Samaritan Laws by State. All 50 states have a “Good Samaritan” law. (A) States with “Bad Samaritan” laws. Duty to Aid: Minnesota, Vermont, Rhode Island. Duty to Report: Hawaii, Washington, Wisconsin. (B) States with “Good Samaritan” laws including AED: Alabama, Hawaii, Kentucky, Michigan, Mississippi, New York, South Dakota, Virginia, Wisconsin. (C) States who do not have “911 Good Samaritan” Laws (covering drug overdose): Arizona, Idaho, Iowa, Kansas, Maine, Missouri, Oklahoma, South Carolina, Texas, Wyoming.
Overall, the idea of rescuing thy neighbor is not a foreign concept in the legal realm, which helps highlight the inferences that this no-duty to rescue has on the structure of the law, as well as the practice of medical professionals even outside of the context of clinical settings.
A Duty to Rescue: Health Care Insight
When we consider the role of the medical practitioner, we often picture individuals willing to make strides and sacrifices toward the betterment of their patients. Though many do so due to the care, passion, and empathy they feel for those they treat, the professional obligations associated with their oaths—and their salaries—cannot be overlooked. Thus, when we remove the duties set forth by the place of employment, and the ethereal contracts within the doctor-patient relationship, what are we left with?
What remains are the main ethical principles that provide the framework for the promises health care workers make to society; however, how does this relate to their willingness to go the extra mile for a stranger in peril, when their checking account is not binging with monetary transfers? In this section, we will briefly discuss the ethical principles that outline the practice of medicine and explore the relations of the no-duty to rescue in the context of practitioners.
Outline of the Ethical Principles of Medicine
To better understand the possible motivations for why doctors and other medical personnel may—or may not—aid a stranger in peril and the ways that the law has attempted to circumvent this no-duty, it is important to briefly describe the four ethical tenets that flow throughout the care that is rendered.
As has been engrained in all people’s minds of the backbone of medicine, one of the central elements of the Hippocratic oath is to “do no harm,” which relates to the principle of non-maleficence. Though this sounds like a rather simple statement, it stands to support multiple morally righteous rules, including “do not kill, do not cause pain or suffering, do not incapacitate, do not cause offense, and do not deprive others of the goods of life.”12 Applied in practice, this represents the obligation of the practitioner to ensure that the benefits of this procedure, treatment, etc., outweigh the risks to support a net positive impact. Similarly, the principle of beneficence is one that promotes the welfare of the patient, always. Here, the moral rules are “protect and defend the right of others, prevent harm, remove conditions that will cause harm, help persons with disabilities, and rescue persons in danger.”12 The major distinction between these two tenets is that the former describes what shall not do, and the latter presents what shall be done, both in the service of the patient.
Furthermore, the concept of autonomy in the practice of medicine is critical as it emphasizes the role that patients, not just clinicians, play in their care, fortifying the ideas of the doctor-patient relationship and patient-centered care. As stated by Justice Cardozo “every human being of adult years and sound mind has a right to determine what shall be done with his own body.”13 Lastly, we have social justice, which relates to the equitable and proper usage of scarce medical resources. In general, these four principles help to highlight the underlying foundation of the
practice of medicine and drive the motivations of practitioners’ choices as they care for patients.
However, how does this transfer over to the no-duty rule of rescue?
Despite the protections allotted within the tort law doctrine, are physicians not held to a different standard considering their oaths, obligations, and unique skill set? This idea has been argued and there appears to be a more “stringent duty” when we are concerned with physicians and other health care workers. For example, the American Medical Association Code of Ethics implies that physicians “must” offer emergency medical assistance, even when not on the job. Moreover, bioethicists state that this is “uncontroversial” as it is “grounded in the profession’s history, an implicit contract with society, and voluntary assumption of the role by the individual professionals.”1 This more inflexible interpretation is maintained by the scope of their practice. For instance, Rulli and Millum state the following: “Doctors have more demanding duties to rescue the sick and injured than people who are drowning…Lifeguards have an increased duty to rescue swimmers, though they don’t have an increased duty to rescue people trapped in burning buildings; the latter is the professional domain of firefighters.”1 Thus, it is not simply the ethical foundations of the training of the individual, but also the scope of their practice, which takes into account their expertise and societal contract. Overall, the more medically focused arenas tend to lean more towards this added responsibility when it comes to professionals, especially when we consider the rescue of a stranger; however, this begs the question: why laws were needed to be set in place (i.e., “Good Samaritan” laws) to encourage it?
Circumvention of the Legal No-Duty to Rescue Imposed on Medical Professionals
The need for laws to encourage rescue of strangers by medical professionals implies that though the tort system offers protection via this no-duty, the legal system wanted—and/or needed—a way to bypass this process. With this in mind, we will discuss two examples of this, one at the state level and one at the federal level.
As described previously, “Good Samaritan” laws were developed to encourage intervention, specifically from doctors and other practitioners, to help others without the promise of compensation and limited (if any) liability for the events that transpired during the aid.11 The idea was that with no to little liability, people with expertise in saving lives would be more willing to do so. However, have these been as successful as intended? Certain research demonstrates that the knowledge of practitioners of protection from liability encourages these actions.
For instance, in a survey given to residents and fellows, most of them stated that they would provide emergency aid if needed, but the study made it clear that education about state statutes was critical to this decision.14 Though about half reported they would render aid, this significantly increased after they received guidance on the “Good Samaritan” statutes for their respective state, emphasizing the need to provide better coverage of these statues in medical education.14 Moreover, in a survey of over 5,700 clinicians, most (69%) conveyed their willingness to help
LEGAL COMMITTEE >> COMMON SENSE SEPTEMBER/OCTOBER 2023 29
in an emergency outside of the clinical setting, with general surgery and emergency medicine leading the wave.15 The hesitations were related to not having the proper equipment or feeling that they did not have enough experience.15 In general, these two surveys reveal that medical personnel are willing to rescue thy neighbor when they are a bystander, but in order to maximize this likelihood they first require education on what their protections are, implying an overall success of these statutes state to state.
Another example of this sidestepping of the no-duty to rescue can be found at the federal level, specifically with the Aviation Medical Assistance Act (AMAA) of 1998. It can be seen as the federal “Good Samaritan” equivalent law particularly concerned with in flight emergencies. With this law, the Federal Aviation Association (FAA) required all aircrafts with at least one flight attendant to have AEDs and an enhanced
References
1. Rulli, T., & Millum, J. (2016). Rescuing the duty to rescue. Journal of Medical Ethics, 42(4), 260-264.
2. Harris, J. (2005). Scientific research is a moral duty. Journal of medical ethics, 31(4), 242-248.
3. Miller, F. G., Mello, M. M., & Joffe, S. (2008). Incidental findings in human subjects research: what do investigators owe research participants?. The Journal of Law, Medicine & Ethics, 36(2), 271-279.
4. Merritt, M. W., Taylor, H. A., & Mullany, L. C. (2010). Ancillary care in community-based public health intervention research. American Journal of Public Health, 100(2), 211-216.
5. Largent, E. A., & Pearson, S. D. (2012). Which orphans will find a home? The rule of rescue in resource allocation for rare diseases. Hastings Center Report, 42(1), 27-34.
6. Restatement (Second) of Torts § 7
7. Scordato, 2008
8. Restatement (Second) of Torts § 295A
9. McCarty v. Pheasant Run, Inc., 826 E2d 1554, 1556-57 (7th Cir. 1987)
10. United States v. Carroll Towing Co., 159 E2d 169, 173, 1947 AMC 35, 41-42 (2d Cir. 1947).
11. West B., & Varacello, M. (2019). Good Samaritan Laws, StatsPearls https://www.ncbi.nlm.nih.gov/books/NBK542176/
medical kit.16 This also provided liability protection for health care professionals while attending to medical emergencies.17 Overall, similar to state-based statutes, the AMAA intends to encourage professionals to rescue those in need, particularly while in the air, but education on what their protections would be more likely to urge action.
These two examples outline how the legal arena aimed at overcoming the no-duty rule within the tort system to encourage emergency intervention by medical professionals. It appears that though these laws are not necessarily needed to promote this type of specialized rescue, they strongly increase the likelihood of its occurrence. Therefore, despite the general protection allocated under the law, the elements that surround the medical profession (ethics of the profession, societal contract, and assumption of the role via expertise and scope of practice) lend itself to rescue thy neighbor.
12. Varkey, B. (2021). Principles of clinical ethics and their application to practice. Medical Principles and Practice, 30(1), 17-28.
13. Schlendorff vs the Society of the New York Hospital, 211 NY 125 (1914).
14. Adusumalli, J., Benkhadra, K., & Murad, M. H. (2018). Good Samaritan laws and graduate medical education: a tristate survey. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 2(4), 336-341.
15. Tessier, M. Poll of 5,700 Clinicians: Would you Provide Care in an Emergency Situation Outside of the Workplace? Op-Med Doximity (January 31, 2023). https://opmed.doximity.com/articles/poll-of-5-700clinicians-would-you-provide-care-in-an-emergency-situation-outside-ofthe-workplace
16. Jordan, J. L. Jon Jordan - The Aviation Medical Assistance Act - Federal Air Surgeon’s Medical Bulletin. Federal Aviation Administration (May 8, 2017). https://www.faa.gov/other_visit/aviation_industry/designees_ delegations/designee_types/ame/fasmb/editorials_jj/assistanceact
17. Tunson, J. (2014). What Does the Law Say to Good Samaritans? A Review of Good Samaritan Statutes in 50 States and on US Airlines.: Stewart PH, Agin WS, Douglas SP. Chest 2013; 143: 1774–83. Journal of Emergency Medicine, 46(1), 153.
18. Code of Medical Ethics. American Medical Association. http://www. ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medicalethics/principles-medical-ethics.page
LEGAL COMMITTEE
COMMON SENSE SEPTEMBER/OCTOBER 2023 30
The E-FAST Exam is Essential Alexis Salerno, MD FAAEM


The Focused Assessment with Sonography in Trauma (FAST) protocol was introduced in the United States in the 1990s. This exam was developed to evaluate for hemoperitoneum and hemopericardium in patients who presented to the emergency department for traumatic injuries.1 Prior to the incorporation of the FAST exam, physicians would perform a diagnostic peritoneal lavage, an invasive procedure, to evaluate for hemoperitoneum. Today, the non-invasive and easily repeatable FAST exam has essentially replaced the diagnostic peritoneal lavage. The FAST exam has revolutionized the initial trauma assessment and many institutions have now incorporated it into their initial trauma algorithm.1
I can understand why some may feel that the FAST exam may be overrated. With a pooled sensitivity at 74%, if the FAST exam is negative, additional testing should still be performed on the patient.2 In my own practice, even if the FAST exam is positive, most patients will undergo a CT scan for surgical planning while the staff prepares the operating room. However, I firmly believe that the FAST exam is essential to the evaluation of the critically ill trauma patient. If positive, this noninvasive, three minute exam can expedite care for trauma and non-trauma patients alike. Here are three reasons, along with examples of clinical scenarios, where a positive FAST exam changed the patient’s clinical course.
Reason One
Including the FAST exam as part of our standard trauma evaluation ensures that we don’t miss obvious internal injuries. For instance, there was a middle-aged male with a history of housing instability who was reportedly hit by a car the day before presenting to our emergency department. Bystanders contacted EMS twice, but the patient refused transport. EMS was dispatched a third time and the patient finally consented to transport. Upon arrival, the patient had reassuring vital signs. Although the initial trauma assessment showed no significant findings except for mild abdominal pain and leg pain, we performed a FAST exam due to the reported history of trauma. To our surprise, the exam revealed a large amount of intraperitoneal blood in the abdomen with distortion of the splenic architecture. We immediately consulted surgery, and the patient was taken to CT scan where there was a confirmed splenic injury. The patient’s time to the OR decreased dramatically due to our diligence in performing a FAST exam for any patient with reported trauma.
Reason Two
Performing the FAST exam can lead to unexpected diagnoses. A female in her late 40s presented to the emergency department with abdominal pain, nausea, and vomiting after working overnight. Initially, I was concerned for cholecystitis and performed a POCUS biliary exam. However, to my surprise, the patient had a collection of blood near the tip of her liver. Continuing with the FAST exam, I noticed more fluid in her pelvis. She was immediately taken to CT and found to have a ruptured ectopic pregnancy. Her time to OR was significantly reduced. I have encountered a few patients with a diagnosis of ruptured ectopic pregnancy where the FAST exam dramatically decreased their disposition time.
Reason Three
The FAST exam may change your differential diagnosis. A middle-aged male presented to the emergency department in acute distress, experiencing vomiting and diaphoresis after attending a wedding. The immediate concern was for acute coronary syndrome, but the patient had a normal ECG. We then attempted to perform a POCUS cardiac exam. While performing the examination, we had poor visualization of the heart using the parasternal views. Continuing to the subxiphoid region, we evaluated both the heart and the abdominal aorta, and both exams yielded negative results. Therefore, we continued evaluating the patient using the FAST exam. To our amazement, we discovered an anechoic fluid collection with air bubbles near the tip of the liver. Surgery was consulted, the patient was transported immediately to the CT scanner, and they were diagnosed with Booerheaver’s syndrome.3 Performing the FAST exam significantly reduced the time to diagnosis for this patient.
In conclusion, I agree that most of the time the FAST exam will be negative, and you will need continued work up. However, sometimes the FAST exam can save a life and for those rare occasions it is worth it.
EFAST: Essential or Overrated
EMERGENCY ULTRASOUND SECTION
>> COMMON SENSE SEPTEMBER/OCTOBER 2023 31
Pro side: “Most of the time the FAST exam will be negative, and you will need continued work up… sometimes the FAST exam can save a life and for those rare occasions it is worth it.”
Potential Harm Associated with the E-FAST Exam
 Melissa Myers, MD FAAEM
Melissa Myers, MD FAAEM
The Extended Focused Assessment in Trauma (the E-FAST) is an undeniably useful exam in the setting of a critically ill trauma patient. However, a misunderstanding of what this exam can and can’t do, and the population it is intended for, means that this exam can cause more harm than good when used incorrectly.
Many emergency physicians overestimate the ability of the E-FAST to detect intra-peritoneal free fluid. One 2021 article on the EFAST states, “True negative E-FAST exams, rule out potential causes of rapid deterioration in trauma patients, such as abdominal hemorrhage or pericardial tamponade.” The E-FAST is a useful triage and “rule in” exam but should not be used as a “rule out” exam for intra-peritoneal bleeding. The E-FAST has a sensitivity for intra-peritoneal free fluid of 22-74%.4,5 The wide range and relatively low sensitivity leaves a reasonable chance for a false negative, even with good technique. This most commonly occurs if there is a low volume of hemoperitoneum, there is no bleeding outside the capsule of an organ, a penetrating injury to the bowel, or a retroperitoneal bleed, all serious injuries which cannot be missed.
The sensitivity of the E-FAST exam varies depending on the patient population and operator experience. Rising rates of obesity among Americans will likely decrease the overall sensitivity further in years to come.6 Furthermore, the E-FAST is often performed with inadequate training or oversight. A medical student or resident performing the
References
1. Bloom BA, Gibbons RC. Focused Assessment With Sonography for Trauma. [Updated 2023
Feb 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.https://www.ncbi.nlm.nih.gov/books/ NBK470479/
2. Netherton S, Milenkovic V, Taylor M, Davis PJ. Diagnostic accuracy of eFAST in the trauma patient: a systematic review and metaanalysis. CJEM. 2019 Nov;21(6):727-738. doi: 10.1017/cem.2019.381.
3. Felipe N, King SA, Salerno A. ‘Diagnosis of Boerhaave’s Syndrome With Aid of Bedside Ultrasound. J Emerg Med 2021 Nov;61(5):568-573. doi: 10.1016/j. jemermed.2021.05.017.
E-FAST should be directly supervised until fully trained. A minimum of 10 exams with feedback are required for minimal competence, with 50 exams a more reasonable goal for independent performance.7 Emergency physicians who finished training prior to the advent of ultrasound training during residency may have difficulty performing these practice exams and receiving feedback on their exams.
Physicians can easily misinterpret the images on the EFAST on a correctly performed exam.8 Common errors include misinterpreting perinephric fat or pericardial fat pad as free fluid. Physiologic free fluid in the pelvis can confound the exam and lead to a “false” positive with the physiologic free fluid difficulty to differentiate from blood. In one level one trauma center, a third of exams were incomplete with missing or unsaved images and incomplete documentation which leads to difficulty identifying false negatives.8
In conclusion, the EFAST is a useful exam that is often misunderstood and misused. Increased awareness of the effect of operator experience on exam sensitivity and the pathology which the EFAST can and cannot diagnose will lead to better utilization of this modality.
4. Netherton S, Milenkovic V, Taylor M, Davis PJ. Diagnostic accuracy of eFAST in the trauma patient: a systematic review and metaanalysis. Canadian Journal of Emergency Medicine. 2019;21(6):727-738.
5. Carter JW, Falco MH, Chopko MS, Flynn Jr WJ, Wiles III CE, Guo WA. Do we really rely on fast for decision-making in the management of blunt abdominal trauma? Injury. 2015;46(5):817-821.
6. Leichtle S, Lucas JW, Kim WC, Aboutanos M. Decreasing accuracy of the eFAST examination—another challenge due to morbid obesity. The American Surgeon 2019;85(8):923-926.
7. Jang T, Kryder G, Sineff S, Naunheim R, Aubin C, Kaji AH. The technical errors of physicians learning to perform focused assessment with sonography in trauma. Academic Emergency Medicine. 2012;19(1):98-101.
8. Khosravian K, Boniface K, Dearing E, et al. eFAST exam errors at a level 1 trauma center: A retrospective cohort study. The American Journal of Emergency Medicine 2021;49:393-398.
EMERGENCY ULTRASOUND SECTION
Con side: “Misunderstanding of what this exam can and can’t do, and the population it is intended for, means that this exam can cause more harm than good when used incorrectly.”
COMMON SENSE SEPTEMBER/OCTOBER 2023 32
“Rebranding” Emergency Medicine
Gary Gaddis, MD PhD MAAEM FIFEM

Emergency Medicine: A specialty that deserves “re-branding” because it enables large financial savings! (This may seem counter-intuitive, but it’s true.)
Introduction
Emergency departments are costly to maintain. They remain open every hour of the year to provide care for those who need it, when they need it. Therefore, emergency departments are a crucial resource for any modern society. No sensible person would want to close them, despite their cost.
However, the common perception that the care provided in an emergency department is excessively costly is just plain wrong. When our doctors’ and our specialty’s performance is viewed objectively, it becomes clear that emergency physicians have become crucial agents of cost savings. Therefore, EPs have earned the right to proudly rebrand themselves not as high-cost care options, but as indispensable, money-saving agents in any nation’s health care enterprise. If you don’t believe that, continue reading this commentary.
Role and Availability of Emergency Departments

Those who allege that our care is too costly and should in most cases be provided in a doctor’s office overlook at least four critical facts:
First, much of the emergency care we provide could not be provided in an office. Could you imagine treating a polytrauma patient, a cerebrovascular accident (stroke) patient, or acute S-T elevation myocardial infarction (STEMI) patient in a doctor’s office? Of course not!
Second, most urgent and emergent medical problems don’t happen on weekdays while the sun is in the sky. Patients often wish to access medical care when doctors’ offices are closed. If a doctor’s office remains open from 9:00am until 5:00pm on weekdays, even if the clinicians in that office are able to accommodate a few “urgent” appointment requests, that office is open for only 40 hours, or 23.8%, of a 168-hour week.
Third, we have implemented research findings to safely decrease costs of care via processes which did not exist when I entered emergency medicine residency training in 1986. This implementation of research findings saves considerable sums of money.
Fourth, the public’s need for inpatient care ebbs and flows, and when a hospital is operating “above capacity,” the emergency department is
typically where that care is provided. Provision of inpatient-level care in an emergency department is less expensive than would be the case if a hospital spent money to add sufficient inpatient capacity to enable that happy day when ED boarding of patients never had to occur.
Points number one, two, and especially four, should all be obvious, yet are sometimes not overtly acknowledged. They will not be further discussed, except for asking you, the readers, to imagine the cost to a hospital system, if it expanded its inpatient census averaged less than 80-85% of the hospital’s capacity, with the addition of numerous ICU beds, such that ED boarding of to-be-admitted patients was rarely required! Our boarding of patients saves hospital systems untold millions of dollars every month!
We Leverage Research Findings to Save Money
Regarding the third point, the leveraging of research findings, an important development that can easily be taken for granted, here are some illustrative examples demonstrating how EPs save health care systems money every day, when 1986 (the year I entered my emergency medicine residency) is compared to 2023.
In 1986, all acute pyelonephritis patients were admitted for several days of inpatient intravenous (IV) antibiotic therapy. Now, many acute pyelonephritis patients receive one dose of an IV antibiotic, plus analgesia and an antiemetic, in the ED. Once they demonstrate that their nausea and vomiting is controlled, most of these patients are then prescribed oral antibiotics, analgesics and antiemetics, and discharged. Acute
>>
COMMON SENSE SEPTEMBER/OCTOBER 2023 33
“However, the common perception that the care provided in an emergency department is excessively costly is just plain wrong.”
pyelonephritis has become a disease for which emergency physicians can contribute cost savings, because less expensive outpatient management is often feasible and appropriate.1
In 1986, most patients with Pelvic Inflammatory Disease (PID) were admitted for several days of IV antibiotics, under the now-disproven dogma that IV antibiotics decreased the scarring of the fallopian tubes and enhanced the patient’s future fertility. Now, many PID patients are treated and released after ED administration of appropriate antibiotics to eradicate possible infection by Neisseria gonorrhea and Chlamydia trachomatis, often with added treatment for anaerobic microbes, and an oral antibiotic upon home going. Female upper genital tract disease has been transformed to another disease for which emergency physicians can contribute cost savings, because less expensive outpatient management is often feasible and appropriate.2
In 1986 all patients diagnosed with the venous thromboembolic (VTE) diseases of deep venous thrombosis (DVT) or acute pulmonary embolism (PE) were admitted for several days of inpatient care to enable therapy with intravenous heparin as a bridge to oral warfarin. Warfarin pills are inexpensive, but the associated care is not. Warfarin is a drug highly prone to drug-drug and drug-food interactions.3 Further, warfarin dosing requires regular monitoring of the International Normalized Ratio (INR), both a cost and an inconvenience to patients. Fortunately, we first learned we could safely treat most DVT patients as outpatients by prescribing direct oral anticoagulants (DOACs) such as Factor Xa Inhibitors. Subsequently, we also learned that PE patients without hypoxia or evidence of right heart failure can safely be discharged with DOAC prescriptions. DVT and PE have been transformed to diseases for which emergency physicians can contribute cost savings, because they usually can implement feasible and appropriate outpatient management.4
In 1986, chest pain patients without an S-T elevation acute myocardial infarction (STEMI), whose pain was suspected to be cardiac in nature, became inpatients for sequential monitoring of their lactate dehydrogenase (LDH) and creatine kinase (CK) isozyme profiles. This process required at least a full day and an overnight inpatient stay. Now, for selected patients, EPs can leverage low and non-rising high sensitivity troponin values and a low “HEART score” to safely implement outpatient follow-up plans, within hours, sparing an inpatient admission. Chest pain has been transformed to a chief complaint for which emergency physicians can contribute cost savings, because outpatient management can be feasible and appropriate.5
In 1986, a complete workup of many other diseases also required several days of inpatient care. Thanks to improved systems of care and
better implementation of medical evidence, patients who used to be admitted for their multi-day workup can occasionally be treated and released. For example, a hospital at which I had worked in the past had a dedicated fast track pathway for patients diagnosed with transient ischemic attacks (TIA). Most of our TIA patients who did not need an urgent vascular procedure to protect them against a near-term stroke were treated and released from the ED Observation Area within 12 hours of their arrival. This expedites hospital throughput and saves significant sums of money.
A further benefit of all of these examples is that patients with these diseases can be returned to work much more quickly than in past years, enhancing overall workforce productivity in a nation’s economy. This has a huge and favorable impact toward financial efficiency.
Further Improvements are Possible
We could do even better at implementing cost savings, if only our patients would permit it. We already know how to apply validated and highly reliable clinical decision rules (CDR) such as the Ottawa Ankle Rules,6 the Ottawa Knee Rules,7 the NEXUS8 and Canadian C Spine9 Rules, and the PECARN10 (for children) and Canadian Head CT11 (for adults) Rules. All perform with high accuracy and validity. However, we know that patients often expect radiographs that these CDRs would establish as contraindicated.
Our collective experience is that there is a significantly long time required to explain these CDRs to patients, so it becomes more cost and time effective to simply obtain the non-indicated imaging.
Consider this idea for the future: Create educational modules that present advocacy to patients to allow doctors to implement these CDRs. This education could be efficiently accomplished if patients were enabled to view effective bedside “plug and play” teaching tools, explaining those CDRs. Such resources could dissuade patients of their false beliefs and persuade them to agree that omission of the contraindicated radiographs, tests which they believed they needed upon their ED arrival, represents appropriate care. This would both save money and shorten the patient’s ED stay. Added benefit would accrue when a pediatric patient has a head CT avoided by decreasing their risk for a subsequent cancer.12
To enable this vision and further enhance our role toward cost savings will require emergency medicine researchers to complement validated CDRs with the creation, testing and validation of accurate and persuasive patient education tools, sufficient to dissuade most patients of their dogmatic and erroneous beliefs regarding radiographs. EPs have
“REBRANDING” EMERGENCY MEDICINE
>>
COMMON SENSE SEPTEMBER/OCTOBER 2023 34
“Hopefully, you are now convinced that as EPs, we deserve to be valued not only for being available 24/7/365, but also for the numerous cost savings that our training permits us to enable.”
exploded incorrect dogmas before. For instance, consider the well-deserved death at the hands of academic EPs of the previous dogmatic belief that no abdominal pain patient can be administered an opiate until they have been examined by a surgeon.13 Hopefully, patients’ dogmatic beliefs regarding radiographs can also become consigned to the dustbin of history.
Certain Myths need to Die
In rebranding ourselves, we should also work to explode other dogmatic myths that plague us, by refuting certain misleading beliefs that cause the public to wrongly conclude that ED care is a larger source of health care expenditures than is the case.
Consider the myth of Medicaid expenditures in the United States. Medicaid, contrary to popular belief, is not health insurance. It is government welfare program. It provides a payment mechanism for low-income individuals to obtain health care, at no cost to them, while shielding them from the costs and charges for that care. If it were insurance, there would be premiums to be paid by the insured.
When I ask my friends and neighbors what percentage of a state’s Medicaid budget is spent for emergency department care of persons living in poverty, most of my contacts that number to be about 50%.
In truth, 52% of Medicaid spending goes for managed care organizations (MCOs) and health plans, 20% pays for fee-for service acute care, and 19% is spent for long term care (e.g., nursing homes) (see Figure 1).14 Spending for ED care is not large enough to merit its own share of that pie!
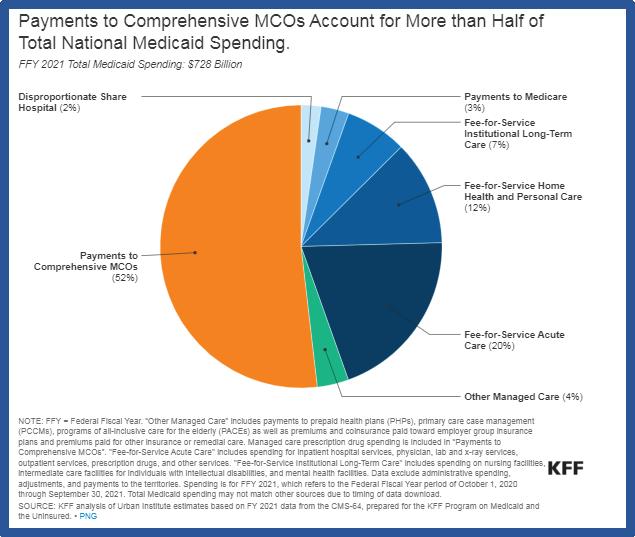
Further, in our country, patients who ideally would be receiving their medical care in an inpatient department often receive much of that care in an emergency department, when surges in patient demand occur. By pitching in and providing inpatient-type care to boarders in the emergency department, we help the hospital system avoid the considerable expense of expanding their inpatient capacity in such a manner that the hospital’s percent occupancy would fall, while enabling them to better accommodate occasional surges in demand for inpatient medical care.
The Take Away
In summary, rather than serving as a repeated whipping boy in the court of public opinion for our provision of what can be perceived to be highcost medical care, EPs should proudly call attention to the numerous ways by which EPs and EDs in which they work help save their nations and patients significant sums of money.
Hopefully, you are now convinced that as EPs, we deserve to be valued not only for being available 24/7/365, but also for the numerous cost savings that our training permits us to enable.
Brian Zink captured a wonderful initial vision statement for our specialty with the title of his book documenting the history of our specialty, “Anyone, Anything, Anytime,” first released in 2006. However, in 2023, it is time to move beyond that title. We need a new vision statement to rebrand EM in a manner that captures how EPs help not only save lives, but also save significant sums of money, 24/7/365.
I offer for consideration, “Emergency Medicine: Saving not only lives, money, by delivering life-saving, life-enhancing evidence-based medical care quickly, efficiently, and effectively”.
Emergency physicians should deservedly take pride in the numerous ways that they help save their nations money, via application of their tools and their training, as they accurately and expeditiously work up patients and implement therapy plans that were unthinkable when I entered my emergency medicine residency in 1986.
As our citizens and politicians learn of this story, perhaps a few words of their words of praise could somewhat offset the burnout that plagues many of us.
Now that you know the story that justifies the claim that emergency medicine should be rebranded as a cost-saving specialty, it becomes up to all of us to adopt and spread this message.
Countinued on page 44 >>
“REBRANDING” EMERGENCY MEDICINE
Figure 1
COMMON SENSE SEPTEMBER/OCTOBER 2023 35
I N - D E P T H E D U C A T I O N F O C U S E D O N Y O U R S P E C I A L T Y . R e g i s t e r a t s i t c a n c e r o r g / a c i | # L e a r n A C I
S I T C ’ s A d v a n c e s i n C a n c e r I m m u n o t h e r a p y ™ ( A C I ) p r o g r a m s o f f e r f o c u s e d c l i n i c a l e d u c a t i o n o n a d i s e a s e s t a t
2 0 2 3 P R O G R A M S
Scan or visit sitcancer.org/aci to learn more & register


ACI: A Focus on Hematologic Malignancies


Oct. 19, 2023 | 3-7 pm EDT | Live Via Zoom Webinar
Join SITC for an afternoon of in-depth education and gain leading industry insights from a panel of experts on the clinical implementation of immunotherapy for hematologic malignancies.


ACI: Online Courses



The ACI 2023 interactive eLearning modules are designed to cover the foundational and basic immunology principles and the mechanisms and clinical applications of immunotherapy.
2023 ACI: Introduction to Biomarkers
2023 ACI: Mechanisms of Immune-related Adverse Events (irAEs)
2023 ACI: Introduction to Immunology
2023 ACI: Basic Principles of Cancer Immunotherapy
ACI: Combination Therapies in Combating Cancer
Understand basic immunology and immunotherapy principles and mechanisms with CE and MOC-certified online courses from SITC's ACI series. Gain an in-depth understanding of how irAEs function and the key biomarkers in immunotherapy treatment while earning CE and MOC credits.
.

C L I N I C A L E D U C A T I O N P R O G R A M S F O R E M E R G E N C Y P H Y S I C I A N S F R E E F O R H E A L T H C A R E P R O F E S S I O N A L S , S T U D E N T S , P A T I E N T S A N D P A T I E N T A D V O C A T E S . C M E , C N E , C P E A N D M O C C R E D I T S A V A I L A B L E
e o r t o p i c a t n o c o s t t o t h e e m e r g e n c y c a r e t e a m . A t t e n d e e s o f t h e s e h a l f - d a y , i n n o v a t i v e p r o g r a m s g e t i n - d e p t h t r a i n i n g i n i m m u n o t h e r a p y t r e a t m e n t t h a t c a n b e d i r e c t l y a p p l i e d t o p a t i e n t s i n e m e r g e n c y c a r e .
The 2023 ACI series is jointly provided by the Partners for Advancing Clinical Education and the Society for Immunotherapy of Cancer in collaboration with the Association of Community Cancer Centers, the Advanced Practitioner Society for Hematology and Oncology and the Hematology/Oncology Pharmacy Association. These programs are provided in collaboration with the American Academy of Emergency Medicine.
COMMON SENSE SEPTEMBER/OCTOBER 2023 36
The 2023 Advances in Cancer Immunotherapy™ educational series is supported, in part, through independent medical education grants from AstraZeneca, Bristol Myers Squibb, Exelixis, GSK, Merck Sharp & Dohme, Corp., a subsidiary of Merck & Co., Inc. (MSD) and Novartis Pharmaceuticals Corporation.
The Double Bullet Sign: Identification of Esophageal Intubation Using Point-of-Care Ultrasound
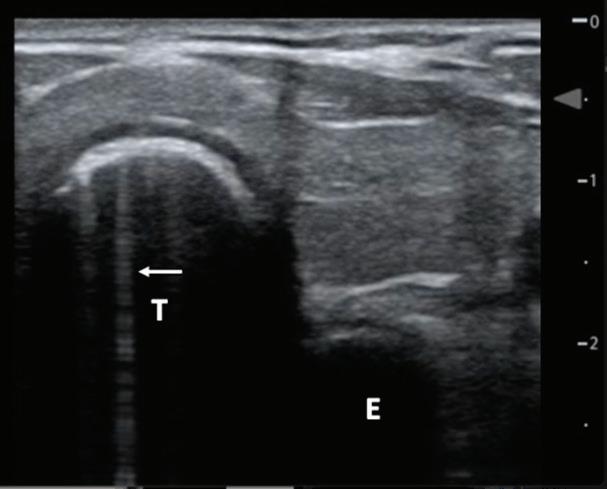
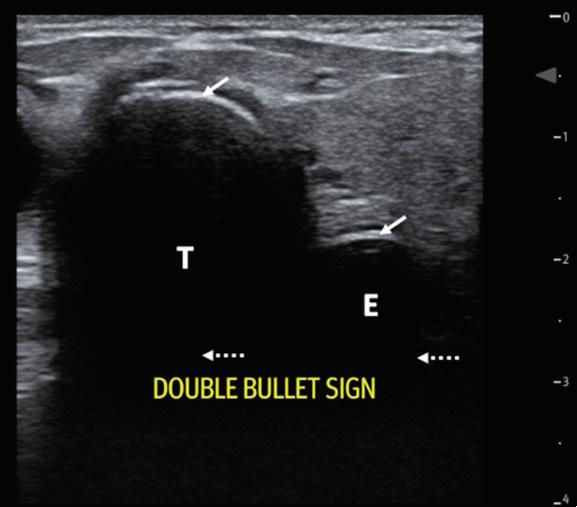 Bailey Balouch, MD,* Wesley Goodman-O’Leary, MD MPH, † Raghav Sahni, DO, † and James Longenbach, MD †
Bailey Balouch, MD,* Wesley Goodman-O’Leary, MD MPH, † Raghav Sahni, DO, † and James Longenbach, MD †
Introduction
Esophageal intubation is an unfortunately common occurrence, particularly during resuscitation or in the prehospital setting. Esophageal intubation may lead to detrimental hypoxia and hypercarbia and is associated with a high risk of morbidity and mortality if not detected early.1-4 Previous studies have shown that outside of the operating room, one in ten intubations are difficult airways and thus require three attempts or more to successfully intubate the patient.5 Furthermore, in a study of 21,000 emergency department (ED) intubations performed by both attendings and trainees, the success rate of first-pass intubations was as low as 72%, and the authors reported a 3.3% incidence of esophageal intubations.6 Thus, the need for real time confirmation of endotracheal tube (ETT) placement is hugely important in ED patients. In this report, we describe the case of a patient who presented to the ED following esophageal intubation in the field and discuss the utility of point-of-care ultrasound (POCUS) for rapid and convenient identification of ETT misplacement and subsequent correction.
Case
A 44-year-old female with a medical history of cirrhosis, functional quadriplegia secondary to previous stroke, chronic obstructive pulmonary disease (COPD), hyperlipidemia, and anemia, was brought to the ED by emergency medical services (EMS) having been intubated due to
worsening hypoxia despite duonebs, steroids, and CPAP. On arrival, the patient had a GCS of 3T, was hypoxic to 74% with bag valve mask, heart rate of 144, and a blood pressure of 91/61. POCUS was performed and transtracheal ultrasonography (TUS) showed a “double bullet sign” suggesting esophageal intubation (Figure 1). The patient was then reintubated successfully with confirmation of tracheal intubation via POCUS, end-tidal CO2 detection, and chest x-ray.
Although oxygen saturation quickly improved, she subsequently lost pulses and several rounds of CPR were performed. Return of spontaneous circulation (ROSC) was achieved and vasopressors were initiated due to hypotension. Subsequent laboratory tests, CT scans, EKG, and ABGs indicated hypercarbic acidosis respiratory failure of likely multifactorial etiology as the cause of the patient’s decline. She remained a GCS of 3T but otherwise stable in the ED and was admitted to the intensive care unit (ICU). She expired two weeks later when family decided to pursue palliative extubation.
Discussion
Standard techniques used for confirmation of correct ETT placement include vocal fold visualization during intubation, end-tidal CO2, chest radiography, lung auscultation, and observation of chest rise, among
Figure 2: Double bullet sign with comet tails. Trachea (T) identified by a hyperechoic air-mucosa interface with posterior shadowing. Comet tails (solid arrow) are seen posteriorly from the air-mucosa interface. The esophagus with ETT (E) is adjacent to the trachea.
COMMON SENSE SEPTEMBER/OCTOBER 2023 37
Figure 1: Double bullet sign. The trachea (T) is identified by a hyperechoic airmucosa interface (solid arrow) with posterior shadowing that causes obliteration of the posterior wall (dashed arrow). The presence of a non-collapsed esophagus (E), appearing as an adjacent air-mucosa interface (solid arrow) confirms esophageal endotracheal tube placement. Posterior wall obliteration is noted due to posterior shadowing (dashed arrow).
others.1,2 Measurement of end-tidal CO2 by capnography is considered the gold standard for ETT placement confirmation.2 However, these confirmation techniques may have limitations in the ED due to difficult anatomy, airway edema or obstruction, patients lacking sufficient pulmonary blood flow for reliable end-tidal CO2 measurement, and those who may require chest compressions.1-3 Quantitative waveform capnography only showed 65% to 68% sensitivity for confirming correct ETT placement.7 Furthermore, patients undergoing resuscitation, transportation, or repositioning may also be at risk for ETT dislodgement from the trachea.1
Transesophageal ultrasound has recently emerged as a useful adjunct to confirm ETT placement, identify ETT misplacement, and provide dynamic airway assessment in the emergency department.1-3 One recent meta-analysis demonstrated that sensitivity and specificity of TUS for confirmation of ETT placement to be 98.7% sensitive (95% CI 97.8 to 99.2%) and 97.1% specific (95% CI 92.4% to 99.0%).7 The mean time required to confirm placement was only 13.0 seconds.7 Another systematic review found sensitivity and specificity of TUS in pediatric patients to be 92-100% and 100%, respectively.8 POCUS is readily available in most emergency departments, is noninvasive, and may be faster than other methods for confirmation of ETT placement, such as a chest radiograph which may take up to 20 minutes to perform and interpret.1,4
To confirm ETT placement with POCUS, a linear transducer is placed in a transverse plane at the level of the suprasternal notch.4 The trachea can be rapidly identified as a hyperechoic air-mucosa interface overlying an anechoic lumen. When tracheal intubation is correctly performed, a single anechoic lumen and air-mucosa interface is present, and the
References
1. *Division of Otolaryngology – Head and Neck Surgery, Cooper University Hospital (corresponding author)
2. †Department of Emergency Medicine, Crozer-Chester Medical Center
3. White-Dzuro GA, Gibson LE, Berra L, Bittner EA, Chang MG. Portable Handheld Point-of-Care Ultrasound for Detecting Unrecognized Esophageal Intubations. Respir Care. 2022;67(5):607-612. doi:10.4187/ respcare.09239
4. Chou HC, Chong KM, Sim SS, et al. Real-time tracheal ultrasonography for confirmation of endotracheal tube placement during cardiopulmonary resuscitation. Resuscitation. 2013;84(12):1708-1712. doi:10.1016/j. resuscitation.2013.06.018
5. Sahu AK, Bhoi S, Aggarwal P, et al. Endotracheal Tube Placement Confirmation by Ultrasonography: A Systematic Review and MetaAnalysis of more than 2500 Patients. J Emerg Med. 2020;59(2):254-264. doi:10.1016/j.jemermed.2020.04.040
6. Gottlieb M, Holladay D, Burns KM, Nakitende D, Bailitz J. Ultrasound for airway management: An evidence-based review for the emergency clinician. Am J Emerg Med. 2020;38(5):1007-1013. doi:10.1016/j. ajem.2019.12.019
esophagus will remain collapsed as it is only a potential space as long as there is no substance within it. However, when an ETT is placed into the esophagus, the ETT creates a second anechoic lumen with an overlying air-mucosa interface adjacent to the trachea. The trachea will remain visible as it is non-compressible due to the cartilaginous rings. Like the trachea, the posterior wall of the esophagus is obliterated due to posterior shadowing (Figure 1). Comet tails may also be seen as the result of reverberation artifact (Figure 2). POCUS confirmation of ETT placement can be performed easily and rapidly and may facilitate early recognition of esophageal intubation, thus enabling prompt intervention.
Conclusion
Transtracheal ultrasound is a convenient, noninvasive, and rapid method for airway assessment and confirmation of ETT placement, with excellent sensitivity and specificity. TUS confirmation is useful in a variety of emergent settings such as during ongoing CPR, in a supervisory role of physicians in-training who are attempting intubation, and even perhaps even one day in the prehospital setting. There are numerous other applications of airway assessment with POCUS, including locating proper anatomy for cricothyroidotomy, predicting ETT size and measuring ETT depth.4 However, knowledge of the utility of TUS specifically for ETT confirmation may reduce time to recognition of ETT misplacement and does not require the cumbersome machinery of a chest x-ray and dependence on other members of the health care team to arrive at the bedside. This may drastically decrease periods of hypoxia, gastric distention, and aspiration pneumonitis and improve patient outcomes.7
7. Mort TC. Unplanned tracheal extubation outside the operating room: a quality improvement audit of hemodynamic and tracheal airway complications associated with emergency tracheal reintubation. Anesth Analg. 1998;86(6):1171-1176. doi:10.1097/00000539-199806000-00006
8. Brown CA 3rd, Bair AE, Pallin DJ, Walls RM; NEAR III Investigators. Techniques, success, and adverse events of emergency department adult intubations [published correction appears in Ann Emerg Med. 2017 May;69(5):540]. Ann Emerg Med. 2015;65(4):363-370.e1. doi:10.1016/j. annemergmed.2014.10.036
9. Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the Confirmation of Endotracheal Tube Intubation: A Systematic Review and MetaAnalysis. Ann Emerg Med. 2018;72(6):627-636. doi:10.1016/j. annemergmed.2018.06.024
10. Lin MJ, Gurley K, Hoffmann B. Bedside Ultrasound for Tracheal Tube Verification in Pediatric Emergency Department and ICU Patients: A Systematic Review. Pediatr Crit Care Med. 2016;17(10):e469-e476. doi:10.1097/PCC.0000000000000907
THE DOUBLE BULLET SIGN: IDENTIFICATION
OF ESOPHAGEAL INTUBATION USING POINT-OF-CARE ULTRASOUND
COMMON SENSE SEPTEMBER/OCTOBER 2023 38
Dobbs Decision
Jeremy Wilber, MD
As of June 24, 2023, a year has passed since the Supreme Court ruled to overturn Roe v. Wade via the Dobbs v. Jackson case. While this has been controversial, it is important for us to understand what this means. This decision outlines that “the Constitution does not confer a right to abortion.” This does not mean abortion is banned, it simply removes federal authority over the matter. As of June 2023, at least 15 states have ceased nearly all abortion services, according to an ABC News tally. Though blue states have seen an uptick in abortions due to laws in neighboring states, new data suggests roughly 25,000 abortions have been prevented nationwide since the Dobbs decision according to lifenews.com.
More importantly, this is a move towards proper function of the judicial branch. The judiciary was not created to make laws as they did in Roe v. Wade, but only to interpret the law. It should remain the burden of Congress to enact and amend federal statutes. If we allow government bureaucracy including an overreaching judicial branch to decide matters of health care such as abortion, it likely will not be long before they are deciding end of life care for us as well (exemplified by the death panels of Obamacare). Learn more Are Medical Death Panels Coming To America? (forbes.com)
While the Dobbs v. Jackson ruling seems to be a small loss for abortion providers like Planned Parenthood, this is a big win for Americans’ freedom to choose whether they would like to have looser or stricter abortion laws. I believe there are logical and moral reasons for providing strict abortion laws.
According to Abortion Risks - Students For Life of America, “new studies have shown that women who have abortions are 81% more likely to experience subsequent mental health problems.” In a study by the Journal of American Physicians and Surgeons 2017 noted “Remarkably few studies have addressed the extent to which freely available abortion services enhance women’s emotional well-being.” In 2013, Fergusson et al.16 published a review examining abortion-related beneficial outcomes through reduction in the mental health risks of unwanted or unintended pregnancy. The authors concluded that there is no available evidence that abortion has therapeutic effects. On the flip side, numerous studies have considered women’s adverse psychological consequences of abortion. There are also multiple post-abortion surveys which highlight many women’s pressure into a decision along with regret and depression. So let us at least have the courage to face the truth—abortion is for the perceived benefit of society, not to enhance a woman’s wellbeing.
I recall seeing a patient in the ER in her 20s—she was on her tenth abortion. Clearly, she was using abortion as birth control instead of contraception or abstinence. Fortunately, this is uncommon, but still a travesty.
Another instance, I recall seeing a distraught boyfriend in the ER—he was upset because his girlfriend decided to abort his first child in order to spite him. Certainly, there is evidence abortions should be banned in the later trimesters, if nothing else due to twice the complication rate (see below).
These two instances highlight the reality that abortion is not health care, but rather convenience care. If you can’t afford an abortion, why not just have an adoption? According to Adoption agencies.com there are often financial resources available. “Adoption agencies understand that—in addition to rent, utilities and groceries—you will likely need help with medical expenses as well. The adoption agency and the adoptive family that you choose will work to cover all of your medical expenses, including prenatal visits and the delivery of the baby for you.”
One of the other big issues for abortion is the issue of informed consent. If abortion is state (taxpayer) funded, it should be mandatory to provide risks and benefits. You should be offered an ultrasound and you should be aware of the risks. According to Foundations of Life. org “Abortion also carries the risk of significant complications such as bleeding, infection, and damage to organs. Serious complications occur in less than 1 out of 100 early abortions and in about 1 out of every 50 later abortions. Complications may include: Heavy Bleeding, Infection, Incomplete Abortion, Damage to the Cervix, Scarring of the Uterine Lining, Perforation of the Uterus, Damage to Internal Organs, Death, Abortion and Preterm Birth for future pregnancies, Links to Abortion and Breast Cancer.”
In my opinion, taxpayer funding should not be used for abortion care except in the case of threatened life of the mother. Since the Supreme Court banned Christian education in public schools, for that same reason, public funds should not be used to subsidize what amounts to an atheistic form of health care. State funded abortion care is essentially child sacrifice to the god of convenience.
References
1. https://adoptionagencies.com/pregnant/placing-for-adoption/get-paid-foradoption/#:~:text=Yes.%20Adoption%20agencies%20understand%20 that%20%E2%80%94%20in%20addition,and%20the%20delivery%20 of%20the%20baby%20for%20you
OPINION
COMMON SENSE SEPTEMBER/OCTOBER 2023 39
Restrictive versus Liberal Fluid Resuscitation in Septic Shock
Authors: Zachary R. Wynne, MD, Michael D. Sullivan, MD, Kyle A. Glose, MD, and Jonathan Hurst, MD
Editors: Kami M. Hu, MD FAAEM and Donald Doukas, MD
Clinical Question: Does a restrictive fluid resuscitation strategy lead to a lower mortality rate than standard fluid resuscitation in septic shock?
Introduction
Early Goal-Directed Therapy (EGDT), the first formal hemodynamically-based resuscitation strategy for sepsis, was pioneered in 2001 and included a prescription of intravenous fluids (IVF), vasopressors, and inotropes to maximize oxygen delivery to tissues.1 Later research noted an increase in mortality associated with aggressive fluid resuscitation and positive fluid balance when analyzed separately,2,3 while mounting evidence supports the early use of vasopressors in septic shock.4,5 Additionally, there is evidence that for diseases such as acute respiratory distress syndrome (ARDS), a restrictive fluid strategy reduces the risk of lung injury, potentially decreasing ICU stay and ventilation days.6-8 The purpose of this review is to determine if the existing literature indicates a difference in mortality with a restrictive fluid strategy compared to a more liberal fluid strategy in patients with septic shock.
Hjortrup PB, Haase N, Bundgaard H, et al. Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallelgroup, multicentre feasibility trial. Intensive Care Med. 2016;42(11):1695-1705.
CLASSIC is a randomized, parallel-group, multicenter feasibility trial that enrolled 151 adult patients with septic shock in nine intensive care units in Denmark and Finland. Patients were randomized 1:1 to a restrictive fluid group or a standard care group. Eligible patients were 18 years or older in an ICU, met criteria for sepsis, and had evidence of severe circulatory impairment (systolic blood pressure (SBP) below 90mmHg, lactate >4mmol/L, or use of vasopressors), received 30mL/kg of crystalloid, and had evidence of ongoing shock.
Both groups were required to maintain a MAP of at least 65. In the standard care group, isotonic crystalloids could be given if markers of hemodynamics improved with their use. In the fluid restriction group, isotonic crystalloid boluses could only be given for lactate >4mmol/L, MAP below 50mmHg despite norepinephrine infusion, mottling beyond the edge of the kneecap, or oliguria. In either group, reassessment was performed 30 minutes after the fluid bolus. The use of colloid solutions was considered a protocol violation.
Primary outcomes included the total volume of resuscitative fluid given after randomization as well as over the first five days. Secondary outcomes included cumulative fluid input at day five and for the total ICU
stay, the number of patients violating fluid resuscitation protocol, and rates of serious adverse reactions associated with crystalloid and/or norepinephrine infusion. Exploratory outcomes included 90-day mortality, time to death, days alive without mechanical ventilation or renal replacement therapy within 90 days, ischemic events during ICU stay, maximum change in serum creatinine, and number of patients with worsening acute kidney injury (AKI).
151 patients were randomized, 75 into the fluid restriction group and 76 into the standard care group. Baseline characteristics were overall similar between both groups. In the fluid restriction group, 73% of patients received resuscitation fluid compared to 92% in the standard care group (p=0.003). Cumulative fluid volumes given by day five and the entire ICU stay were statistically significantly lower in the fluid restriction group (mean differences -1.2L and -1.4L, respectively, p<0.001). Secondary outcomes of total fluid inputs and balances did not differ between groups, with no differences in the occurrence of adverse reactions to fluids or norepinephrine between groups. Exploratory outcomes only demonstrated a significantly higher incidence of worsened acute kidney injury during the 90-day period in the standard care group (17% higher, p=0.03).
This trial was unblinded and insufficiently powered to find a difference between secondary outcomes. Additionally, there were many protocol violations, including the administration of fluids to patients who did not meet criteria, as well as resuscitation with albumin and other colloids. The results of this pilot trial did, however, demonstrate that a restrictive fluid protocol could be used successfully in the ICU setting, serving as a critical foundation for the randomized control trial of the CLASSIC study group discussed later in this article.
Macdonald SPJ, Keijzers G, Taylor DM, et al.
Restricted fluid resuscitation in suspected sepsis associated hypotension (REFRESH): a pilot randomised controlled trial. Intensive Care Med. 2018;44(12):2070-8.
The REFRESH trial was a prospective, randomized, open-label clinical trial conducted at eight Australian hospitals comparing restrictive fluids resuscitation plus early vasopressor initiation to usual care (fluids alone) in patients presenting to the emergency department (ED) with suspected sepsis. The focus of the study was to investigate whether a protocol of early vasopressor initiation could reduce the IVF volume received by individual patients compared to standard practice. A secondary focus was to develop data that could be used to design a future trial appropriately powered to investigate this question with regard to patient-centered outcomes.
>>
AAEM/RSA RESIDENT JOURNAL REVIEW
COMMON SENSE SEPTEMBER/OCTOBER 2023 40
Patients were enrolled if they presented to the ED with a suspected infection treated with IV antibiotics and an SBP less than 100mmHg refractory to one liter of isotonic crystalloid over one hour. Patients were randomized in a site-stratified fashion in a 1:1 ratio using a webbased service.
In both groups, apart from fluid resuscitation, patients were treated according to the standard of care guidelines published by the Surviving Sepsis Campaign (SCC), including early initiation of broad-spectrum antibiotics, decisions regarding source control, invasive hemodynamic monitoring, ventilatory support, blood transfusion, and renal replacement therapy (RRT)—all decisions made at the discretion of the treating team. After randomization, patients in the usual care group received an additional one liter fluid bolus and could receive additional boluses of 500mL hourly at the treating clinician’s discretion. If MAP was persistently below 65mmHg, vasopressors were initiated to meet a MAP goal ≥ 65mmHg. For patients in the restricted fluid group, vasopressors were started immediately if the MAP was below 65mmHg; they could also receive hourly250 mL boluses at the discretion of the treating clinician. The trial interventions were carried out for six hours from patient presentation before reverting to usual care per the primary team.
104 patients were randomized, 50 to the usual care group and 54 to the restricted volume protocol. Overall, the usual care group received more fluids than the restricted volume arm (a median 43mL/kg vs 30mL/kg IV, p<0.001) within the first six hours of treatment. The restricted-volume group experienced a significant decrease in the median time from randomization to vasopressor initiation compared to the usual care group (34 min vs 150 min, p=0.001), although there was no difference in the proportion receiving vasopressors at 24 hours. There was no difference in fluid volumes between six and 24 hours. There was initially a difference in 28-day mortality (2% in restrictive versus 6% in usual care), but this difference was not maintained at 90 days (8% versus 6%). There was no difference in the number of hospital, vasopressor, ventilator, or RRT-free days.
This study found no evidence of harm with a restricted volume/early vasopressor protocol; however, the authors observed that the mortality rate in the study population (7%) was lower than expected based on other research on sepsis. They also noted that although patients in the restricted volume arm of the trial did receive 30% less fluid relative to the usual care group, the absolute difference in volume was less than one liter, casting uncertainty on whether this difference is clinically significant.
Corl KA, Prodromou M, Merchant RC, et al. The Restrictive IV Fluid Trial in Severe Sepsis and Septic Shock (RIFTS): A Randomized Pilot Study. Crit Care Med. 2019;47(7):951-9.
The RIFTS trial was a prospective randomized pilot study based in EDs and ICUs at two United States hospitals. Patients included were nonpregnant adult patients suspected by the treating physician of having severe sepsis or septic shock. Patients had to have hypotension or lactate ≥4mmol/L after one liter of IV fluids to be enrolled. Exclusion criteria
included alternative primary diagnosis other than sepsis, a “fluid wasting condition,” need for immediate surgery or extracorporeal membrane oxygenation (ECMO), or having received more than 60mL/kg of IVF prior to randomization. Patients were then randomized to either the restrictive or usual care groups. The restrictive fluid group could use up to 60mL/ kg crystalloid in the first 72 hours of enrollment to target a MAP goal of 65mmHg. The usual care group had no restrictions on the amount of fluid that could be used. Administration of albumin, blood products, and/ or vasopressors was not restricted in either group.
The primary outcome was 30-day all-cause mortality. Secondary outcomes included 60-day all-cause mortality, hospital length of stay, new onset organ failure, vasopressor-free days, ventilator-free days, ventilation hours, electrolyte abnormalities, and adverse events.
A total of 109 patients were included in the final analysis, with 55 patients assigned to the restrictive fluid group and 54 patients assigned to usual care. The groups were well-matched, with the exception of a higher percentage of chronic kidney disease in the restrictive fluid group (36% vs 11%). Patients in both groups received similar amounts of fluid resuscitation prior to randomization (approximately 35mL/kg). There was significantly less fluid administered in the restrictive group in the first 24 hours after randomization (7.8mL/kg versus 16.6mL/kg, p=0.02), which led to a difference in total resuscitative fluids over 72 hours as well (47.1mL/kg versus 61.1mL/kg, p=0.01). There was no difference in the volume of albumin, blood products, or use of stress dose steroids. No difference was found in 30-day (21.8% versus 22.2%, p>0.99) or 60-day mortality (27.3% versus 27.8%, p>0.99). There were fewer hours requiring mechanical ventilation in the restrictive fluid group compared to the usual care group (16.8 hours versus 37.8 hours, p=0.02). There were no differences in secondary outcomes of organ failure, vasopressor-free or ventilator-free days, ICU or hospital length of stay, electrolyte measurements, or adverse events.
The RIFTS pilot trial suggests that more conservative fluid resuscitation may be beneficial compared to aggressive fluid resuscitation. It should be noted, however, that the restrictive fluid group did have a larger percentage of CKD patients who, given the similar mortality outcomes, may have benefitted from the more cautious fluid resuscitation strategy. Additionally, it was noted that the trial effectively reduced the amount of fluid resuscitation in both groups compared to volumes administered to patients in the months before the study (75mL/kg pretrial to 35mL/kg during the trial), consistent with a possible Hawthorne effect. The outcome of fewer ventilator hours was consistent with existing data that excess fluid resuscitation can be detrimental in lung injury but did not carry over to a length of stay or mortality benefit.7-8
This study was not powered to find small statistically significant differences. Due to the nature of fluid resuscitation, the study could not blind patients or providers. Additionally, the study excluded patients who received greater than two liters of fluid resuscitation prior to enrollment and may have been more critically ill, causing a possible selection bias. Lastly, the
AAEM/RSA RESIDENT JOURNAL REVIEW >> COMMON SENSE SEPTEMBER/OCTOBER 2023 41
exclusion of “fluid wasting condition(s)” likely led to the exclusion of certain types of infections (gastrointestinal etiologies), potentially limiting the generalizability of the data.
Meyhoff TS, Hjortrup PB, Wetterslev J, et al. Restriction of Intravenous Fluid in ICU Patients with Septic Shock. N Engl J Med. 2022;386(26):2459-70.
This CLASSIC follow-up study is an international, open-label, randomized clinical trial that enrolled ICU patients with septic shock who had received at least one liter of IVFs in the 24 hours before screening. Patients were then randomized in a 1:1 fashion to either receive restrictive intravenous fluid therapy or standard intravenous fluid therapy. As in the pilot trial, the restrictive group could only receive additional fluid boluses for evidence of severe hypoperfusion, correction of documented fluid losses, correction of dehydration or electrolyte imbalance, and ensuring a total daily fluid intake of one liter per day. For the standard fluids group, additional fluids were given for the replacement of observed losses, electrolyte imbalances, or maintenance fluids at a rate determined by the clinical team. The primary outcome was death within 90 days of randomization. Secondary outcomes included serious adverse events, the number of days alive without life support, and the number of days alive out of the hospital at day 90.
A total of 1554 patients were randomized, with 770 patients assigned to the restrictive-fluid group and 784 to the standard-fluid group. At 90 days, the median cumulative fluid volume, excluding fluids with medication and nutrition, was 1798mL in the restrictive-fluid group and 3811mL in the standard-fluid group, while the median of all fluids given was 10,433mL in the restrictive-fluid group and 12,747mL in the standard-fluid group. There was no difference in 90-day mortality between groups (42.3% restrictive versus 42.1% standard, p=0.96) and no difference in the rate of serious adverse events (29.4% restrictive versus 30.8% standard, p=0.46), number of days without support, or number of days outside the hospital after 90 days. There was a trend towards benefit with a restrictive strategy in patients requiring respiratory support (-5.1% mortality difference, 95% CI [-11.3,1.6], p=0.03).
Strengths of this study included the large sample size, completeness of data, and generalizability of results. Patient characteristics and fluid volumes used in the study groups were similar to other recent trials looking at intravenous fluid management in ICU patients. This study does have several limitations, including the inability to blind patients and providers to treatment arms. Also, patients were randomized after receiving an initial fluid bolus though this was similar between groups at baseline. Additionally, violations of the IV fluid protocol occurred in 21% of the restrictive group and 13% of the standard group, which may have confounded the results, and the study was not powered to detect a difference between subgroups.
Jessen MK, Andersen LW, Thomson MH, et al. Restrictive fluids versus standard care in adults with sepsis in the emergency department (REFACED): A multicenter, randomized feasibility trial. Acad Emerg Med. 2022;29(10):1172-84.
The REFACED trial was a multicenter, randomized, open-label feasibility trial that sought to assess if ED patients with a diagnosis of “sepsis without shock” can receive a restrictive IVF protocol to decrease the volume of IVFs administered compared to standard care. Patients were included if their ED visit was unplanned, they were ≥18 years old, had a diagnosis of sepsis, and had an expected hospital stay of greater than 24 hours. Patients were excluded if they received more than 500mL of fluid prior to enrollment, had vasopressors or invasive ventilation started prior to screening, had known or suspected severe bleeding, pregnancy, if they were not expected to survive the next 24 hours, or were unable to provide informed consent.
Eligible patients were randomized in a 1:1 ratio to a restrictive fluid or standard care group. Patients in the restrictive fluid group only had fluids administered if there was a lactate of ≥4mmol/L, SBP <90mmHg, mottling beyond the edge of the kneecap, or if they had severe oliguria. If these criteria were met, a patient in the restrictive fluid group could receive a 250mL crystalloid bolus. In the standard care group, fluids were administered per the treating physician’s choice. Oral fluid intake was not restricted in either group.
The primary outcome was the total volume of crystalloids administered during the first 24 hours. Secondary outcomes included feasibility measures (number of protocol violations, time to inclusion, lost to follow-up rate, screened-to-included ratio), serious adverse events, death in-hospital, as well as death at 30 and 90 days.
124 patients were enrolled, with 62 patients in each group. At 24 hours, the fluid-restricted group received a mean of 562mL of IVF, while the standard-of-care group received a mean of 1370mL (Difference of -801mL, (p=0.001). In the restricted fluid group, 34% (21/61) had IVF administered outside of the restrictive protocol—most frequently (7/61 patients) due to elevated creatinine. There were no significant differences between groups in secondary outcomes, including mechanical ventilation or vasopressor use, new onset kidney failure at seven days, length of stay, or in-hospital, 30-day, or 90-day mortality. There were a similar number of adverse events between groups (17 in the restrictive, 18 in the standard), with similar rates of hypervolemia and acute kidney injury.
The mean difference between trial groups at the 24-hour mark was 801mL, representing a 58% relative reduction—almost doubling the relative fluid reduction from the REFRESH trial. Overall, 62% of patients in the restrictive group did not receive crystalloid fluids unless as a carrier for medication, to correct fluid loss, or to replace electrolytes, leading the authors to believe that clinicians are able to restrict fluid administration in a sizable proportion of septic patients.
>>
AAEM/RSA RESIDENT JOURNAL REVIEW COMMON SENSE SEPTEMBER/OCTOBER 2023 42
The trial was limited by sample size and was therefore inadequate to assess mortality. While the trial was able to recruit 124 patients, any patient who received more than 500mL of fluid prior to enrollment was excluded; thus, any patients who were given empiric fluid for soft blood pressures in the pre-hospital or peri-triage environment were eliminated. 19 patients were excluded from this trial, given that they were unable to provide informed, written consent. Considering this criterion, there could have been a selection bias against more critically ill patients. While the study did not show differences in adverse events, the study was not powered to do so.
The REFACED trial supported the feasibility of protocolizing and restricting initial 24-hour IV fluid administration in septic patients without shock in emergency departments. While this trial was not able to conclude that restrictive IV fluid provides a benefit in sepsis, it does provide a foundation for how a large-scale trial could be performed to assess clinical outcomes such as mortality.
Shapiro NI, Douglas IS, Brower RG, et al. Early Restrictive or Liberal Fluid Management for Sepsis-Induced Hypotension. N Engl J Med. 2023;10.1056/NEJMoa2212663.
The CLOVERS trial was an unblinded, multicenter superiority trial in which the investigators sought to compare the effects of a restrictive fluid, early vasopressor strategy versus a liberal fluid, late vasopressor strategy. It included patients 18 years and older with a suspected or confirmed infection and presumed sepsis-induced hypotension after receiving one or more liters of intravenous fluid. Patients were excluded if they received more than three liters of fluid prior to enrollment, if there was a clear alternative cause of hypotension, if more than four hours had passed between meeting study criteria and enrollment, or if more than 24 hours had passed since hospital presentation.
Patients were centrally randomized with stratification across sites in a 1:1 ratio to either a restrictive or a liberal fluid strategy. In both groups, the protocol was followed for 24 hours. In the restrictive fluid group, patients would receive at least one liter of fluid and could receive up to two liters of total IV fluid at the discretion of the clinical team. If the patient developed hypotension with a MAP of less than 65mmHg, patients would have norepinephrine and/or additional vasopressors added and adjusted for a goal MAP ≥65mmHg. Patients could receive a 500mL rescue bolus if they had the following conditions: severe hypotension with MAP <50mmHg, refractory hypotension with norepinephrine doses reaching 20µg/min or an equivalent dose of another vasopressor, lactate >4mmol/L and increasing after two hours of therapy, sinus tachycardia with rates above 130 for longer than 15 minutes, echocardiographic evidence of hypovolemia, or if the clinical team believed it was medically necessary. In the liberal fluid group, patients were given an additional one to two liters of crystalloid IVF at randomization in addition to up to three liters of fluid received prior to randomization. If the patient developed hypotension, lactate >4mmol/L, decreased urinary output, receipt of vasopressors to maintain MAP of 65, or clinical assessment suggesting
under-resuscitation, they would receive an additional 500mL bolus and be reassessed. Vasopressors could be initiated for severe hypotension, lactate >4mmol/L refractory to fluid boluses, clinical manifestations of fluid overload, or at the clinician’s discretion.
The primary outcome was death from any cause before discharge home by day 90. Secondary outcomes included days free from renal-replacement therapy, days without vasopressor use, days out of the ICU, and days out of the hospital.
The trial estimated they would need 2320 patients to have sufficient power to detect an absolute mortality difference of 4.5%. The trial enrolled 1563 patients at 60 different U.S. centers prior to being halted for futility given the lack of differences in the primary and secondary outcomes. In the first six hours after randomization, the restrictive group had a median of 500mL of IVF administered (95% CI [130,1097]), whereas the liberal fluid group had a median of 2300mL (95% CI [2000-3000]). Vasopressors were more common in the fluid-restricted group (59%) compared to the liberal fluid group (37%). The total mean fluid administration (including pre-enrollment fluids) was 3300mL in the restrictive group and 5400mL in the liberal fluid group. Protocol adherence was 97% and 96% in the restrictive and liberal fluid groups, respectively. Death before discharge home in the restrictive group was 14.0%, and 14.9% in the liberal fluid group (difference -0.9%, 95% CI [-4.4, -2.6]). The number of serious adverse events was similar between groups. There were no statistically significant differences in the primary or secondary outcomes, although there was a trend towards a mortality benefit to a restrictive strategy in patients with end-stage renal disease (27.3% restrictive versus 47.5% liberal, 95% CI [-41.9,1.5]).
In contrast to the CLASSIC trial, the CLOVERS trial almost exclusively enrolled patients with a primary presentation to an emergency department with sepsis. The results suggest that similar outcomes can be achieved with either liberal or restrictive fluid resuscitation in septic patients.
A limitation of this study included the difficulty of blinding a study on fluid administration, leading to potential bias. As clinician approval was required for trial enrollment, subgroups of patients with extremes of volume overload or depletion may not have been included. Alternatively, there may be subgroups of patients who benefit more from one strategy compared to another; those subgroups were not elucidated in this trial. The authors did not include an unstructured treatment group, making it difficult to assess how outcomes would compare to a “standard care” group. It is also worth noting that this study population’s mortality rate was relatively low at 14%, with only 60% of the restrictive—early vasopressor—group actually requiring the administration of vasopressors, potentially indicating that the patient population had less severe illness overall. Finally, while there was no demonstrated difference in outcomes with the trial’s 24-hour protocol, it may be that specific strategies over a longer study period would reveal differences in outcomes.
AAEM/RSA RESIDENT JOURNAL REVIEW >> COMMON SENSE SEPTEMBER/OCTOBER 2023 43
Conclusion
These trials support that there is no significant difference in mortality or adverse outcomes between restrictive and liberal or “usual care” fluid resuscitation strategies in sepsis and septic shock. Many of these studies used a similar fluid resuscitation protocol to the CLASSIC pilot study, making it methodically appropriate to compare and synthesize the results as done here. While well-designed, the limitations in CLASSIC and CLOVERS randomized trials may have resulted in overestimating the ability to detect a mortality difference between groups. Continued focus should be paid to the signals found for possible benefits to restrictive fluid strategies in specific subpopulations, with data thus far supporting the need to tailor fluid resuscitation to the individual patient rather than a fixed volume.
Clinical Question: Does a restrictive fluid resuscitation strategy lead to a lower mortality rate than the standard of care fluid resuscitation strategy in septic shock?
Answer: Current literature has not found a significant mortality difference between a restrictive fluid and liberal fluid resuscitation strategy in patients with sepsis-induced hypotension or septic shock.
References
1. Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001;345(19):1368-77. doi:10.1056/NEJMoa010307
2. Micek ST, McEvoy C, McKenzie M, et al. Fluid balance and cardiac function in septic shock as predictors of hospital mortality. Crit Care 2013;17(5):R246.
3. Marik PE, Linde-Zwirble WT, Bittner EA, et al. Fluid administration in severe sepsis and septic shock, patterns and outcomes: an analysis of a large national database. Intensive Care Med. 2017;43(5):625-32.
4. Bai X, Yu W, Ji W, et al. Early versus delayed administration of norepinephrine in patients with septic shock. Crit Care. 2014;18(5):532.
5. Permpikul C, Tongyoo S, Viarasilpa T, et al. Early Use of Norepinephrine in Septic Shock Resuscitation (CENSER). A Randomized Trial. Am J Respir Crit Care Med. 2019;199(9):1097-1105.
6. Lee J, Corl K, Levy MM. Fluid Therapy and Acute Respiratory Distress Syndrome. Crit Care Clin. 2021;37(4):867-75.
7. Murphy CV, Schramm GE, Doherty JA, et al. The importance of fluid management in acute lung injury secondary to septic shock. Chest 2009;136(1):102-9.
8. Silversides JA, Major E, Ferguson AJ, et al. Conservative fluid management or deresuscitation for patients with sepsis or acute respiratory distress syndrome following the resuscitation phase of critical illness: a systematic review and meta-analysis. Intensive Care Med 2017;43(2):155-70.
Countinued from page 35 >>
References
1. Herness J, Buttolph A, Hammer NC. Acute pyelonephritis in adults. A review. Am Fam Physician 2020;102:173-180. https://www.aafp.org/pubs/ afp/issues/2020/0801/p173.html Accessed February 23, 2023.
2. Centers for Disease Control and Prevention. Pelvic inflammatory disease (PID). CDC Sexually transmitted disease guidelines 2021. https://www. cdc.gov/std/treatment-guidelines/pid.htm Accessed February 23, 2023.
3. Mayo Clinic Staff. Warfarin side effects. Watch for interactions. The Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/deepvein-thrombosis/in-depth/warfarin-side-effects/art-20047592 Accessed February 23, 2023
4. Stubblefield WB, Kline JA. Outpatient treatment of emergency department patients diagnosed with venous thromboembolism. Postgrad Med 2021;133(Supp 1):11-19. https://pubmed.ncbi.nlm.nih.gov/33840338/ Accessed February 23, 2023.
5. Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/ SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78:e187-e285.
6. Stiell IG, Greenberg GH, McKnight RD et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA 1993; 269:1127-32.
7. Stiell IG, Greenberg GH, Wells GA et al. Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA 1996;275:611-5.
8. Hoffman JR, Mower WR, Wolfson AB et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343:94-9.
9. Stiell IG, Clement CM, McKnight RD et al. The Canadian c-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med 2003;349:2510-8.
10. Schonfeld D, Bressan S, DaDalt L, et al. Pediatric Emergency Care Applied Research Network head injury clinical prediction rules are reliable in practice. Arch Dis Child. 2014;99:427-31.
11. Stiell IG, Clement CM, Rowe BH et al. Comparison of the Canadian CT head rule and the New Orleans criteria in patients with minor head injury. JAMA 2005;294:1511-8.
12. Sheppard JP, Nguyen T, Alkhalid Y, et al. Risk of brain tumor induction from pediatric head CT procedures. A systematic literature review. Brain Tumor Res Treat. 2018;6:1-7.
13. Brewster GS, Herbert ME, Hoffman JR. Medical myth: Analgesia should not be given to patients with an acute abdomen because it obscures the diagnosis. West J Med. 2000;172:209-10.
14. Williams E, Rudowitz R, Hinton E et al. Medicaid financing. The basics. Kaiser Family Foundation, April 13, 2023. https://www.kff.org/medicaid/ issue-brief/medicaid-financing-the-basics/ Accessed July 31, 2023
AAEM/RSA RESIDENT JOURNAL REVIEW
“REBRANDING” EMERGENCY MEDICINE
COMMON SENSE SEPTEMBER/OCTOBER 2023 44

COMMON SENSE SEPTEMBER/OCTOBER 2023 45
AAEM Job Bank Service
Promote Your Open Position

To place an ad in the Job Bank: Equitable positions consistent with the Mission Statement of the American Academy of Emergency Medicine and absent of restrictive covenants, will be published (upon approval). All ads run for a six month period or until canceled and will appear in the AAEM member magazine Common Sense and online. For pricing and more information visit www.aaem.org/membership/benefits/ job-bank.
Complete a Job Bank registration form, along with the Criteria for Advertising Section, and submit payment. If you are an outside recruiting agent, the Job Bank Criteria for Advertising must be downloaded and completed by a representative from the recruiting hospital/group.
Direct all inquiries to: www.aaem.org/membership/benefits/job-bank or email info@aaem.org.
Positions Available
For further information on a particular listing, please use the contact information listed.
Section I: Positions in full compliance with AAEM’s job bank advertising criteria, meaning the practice is wholly-owned by its physicians, with no lay shareholders; the practice is equitable and democratic; due process is guaranteed after a probationary period of no more than one year; there are no post-employment restrictive covenants; and board certified emergency physicians are treated equally, whether they achieved ABEM/AOBEM/RCPSC certification via residency training or the practice track.
Section II: Positions that cannot be in full compliance with AAEM’s job bank criteria, because they are employee positions with hospitals or medical schools and the practice is not owned by its emergency physicians. Thus there may not be financial transparency or political equity.
Section III: Positions that cannot be in full compliance with AAEM’s job bank criteria, because they are government or military employee positions. The practice is not owned by its emergency physicians, and there may not be financial transparency or political equity.
Section IV: Position listings that are independent contractor positions rather than owner-partner or employee positions.
SECTION I: POSITIONS RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK CRITERIA
VIRGINIA
DEMOCRATIC GROUP TOP TIER COMPENSATION EQUAL PARTNERSHIP Fredericksburg Emergency Medical Alliance (FEMA) in Fredericksburg, Virginia. We are a small democratic group located an hour south of Washington DC currently staffing 3 EDs in the Mary Washington Health Care system. We are looking to hire several new partners after a couple of recent retirements and the addition of a new freestanding ED, anticipated opening in 2024. Mary Washington ED is a level 2 trauma center with annual volumes of ~65k. Stafford is a community hospital ED that sees ~40k. Our Lee’s Hill FSED is
on track to see ~35k this year. We use EPIC EMR, are supported by FEMA-employed APPs and scribes, and offer equitable scheduling from day one. We operate under a fee for service payment model. Top tier compensation. Please upload CVs to www.femainc.com or send directly to Cheema.samia1@gmail. com Feel free to reach out if you have any questions! (PA 2005)
Email: aalvarezfema@gmail.com
Website: https://www.femainc.com/
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
(Below are hospitals, non-profit or medical school employed positions.)
CONNECTICUT
Trinity Health Of New England seeks BC/BE EM Physicians to join our emergency medicine teams at Mercy Medical Center in Springfield, Massachusetts, Saint Francis Hospital and Medical Center in Hartford, Connecticut and Saint Mary’s Hospital in Waterbury, Connecticut. Our practice model empowers our physicians to work at their highest level, while allowing time for professional development and family life. Whether you are focused on providing outstanding patient-centered care or driven to grow into a leadership role, you will thrive at Trinity Health Of New England. To learn more, visit our provider portal at www. JoinTrinityNE.org (PA 1985)
Email: ndiehl@abccreative.com
Website: https://www.jointrinityne.org/Physicians
FLORIDA
The Schmidt College of Medicine at Florida Atlantic University is seeking an Assistant Program Director to join its Emergency Medicine Residency Program. This position is intended for faculty with experience in teaching, leadership, innovation and clinical service in an emergency medicine residency program. All applicants must apply electronically on the FAU Office of Human Resources’ career website (https://fau.edu/jobs) by completing the required online employment application. When completing the online application, please upload the required cover letter and curriculum vitae. To review the full minimum qualifications and requirements and to apply, visit www.fau.edu/jobs and go to Apply Now (REQ16576). (PA 2010)
Website: https://fau.wd1.myworkdayjobs.com/en-US/FAU/job/ Clinical---Off-Campus-Location-COM-use-only/AssociateProgram-Director--Emergency-Medicine-Residency--AssistantAssociate-Professor-_REQ16576?q=REQ16576
LOUISIANA
Ochsner Health is seeking a board certified/board eligible physicians to join our Division of Pediatric Emergency Medicine at Ochsner Medical Center and Ochsner Hospital for Children. Opportunity Details: • Employed physician group that offers competitive fair market compensation plus benefits • In House pediatric intensivist and hospitalist attendings 24/7 to assist with streamlined pediatric admissions and patient care. • All facilities utilize Epic electronic health records integrating care across the system and facilitating seamless multi-hospital practice • All specialties available for consultation and easy one-call transfer from our community emergency departments to our main campus Interested physicians should apply to: https://ochsner. wd1.myworkdayjobs.com/OchsnerPhysician/job/New-Orleans--New-Orleans-Region---Louisiana/Pediatric-EmergencyMedicine_REQ_00158668 (PA 1991)
Email: courtney.lawhun@ochsner.org
Website: https://ochsner.wd1.myworkdayjobs.com/ OchsnerPhysician/job/New-Orleans---New-Orleans-Region--Louisiana/Pediatric-Emergency-Medicine_REQ_00158668
MASSACHUSETTS
Emergency Medicine Physician Dartmouth Health The Department of Emergency Medicine at Dartmouth-Hitchcock Medical Center (DHMC) is seeking a BC/BE Emergency Medicine Physician to join our team of dedicated Emergency Physicians. Responsibilities include supervision and teaching of medical students, off-service residents, and Emergency Medicine residents. Interested physicians are encouraged to apply online by submitting their CV and addressing their cover letter to: Scott Rodi, MD, MPH, FACEP Chair, Department of Emergency Medicine Emergency Medicine Regional Medical Director, Dartmouth Health Qualifications • Advanced clinical
degree (MD or DO) • Post graduate training in Emergency Medicine residency program Apply link: https://careers. dhproviders.org/emergency-medicine-physician-lebanon-3-0 EOE. (PA 2000)
Email: Jacqueline.M.LaBelle@hitchcock.org
Website: https://careers.dhproviders.org/emergency-medicinephysician-lebanon-3-0
MICHIGAN
Medical Director of Emergency Medicine Research Corewell Health William Beaumont University Hospital (previously Beaumont Royal Oak) The Department of Emergency Medicine is recruiting a Medical Director of Research to lead a nationally recognized research program. The successful candidate will be an ABEM certified emergency physician who works clinically at University Hospital with academic appointment at Oakland University William Beaumont School of Medicine. Preference will be given to candidates with a record of extramural funding, success mentoring colleagues, formal academic research training, and experience managing research. The institution is seeking a broad and diverse candidate pool. University Hospital is a 1,100-bed referral center that has been recognized by U.S. News and World Report as one of the “Best Hospitals” for the past 26 years. In 2022, it ranked second statewide. The Emergency Department is the busiest center in Michigan with an annual volume approaching 120,000 visits. It has had an EM residency program for 30+ years and has Emergency Geriatric, Pediatric, Ultrasound and Medical Education fellowships. In 2021, ED faculty published 50+ papers; extramural support totaled over $550,000. MD or DO (PA 1979)
Email: kimberly.andrews@beaumont.org
Website: https://providers.beaumont.org/physician-resources/ physician-careers
46
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
(Below
MINNESOTA
Mayo Clinic is seeking board-certified and board-eligible Emergency Medicine Physicians to join our world-class clinical and academic communities throughout the country. You can choose from opportunities at our large medical centers in Minnesota, Arizona, and Florida, or a community-based practice within Mayo Clinic Health System locations across Minnesota, Iowa, and Wisconsin. Ranked as the #1 hospital in the nation by U.S. News & World Report in 2022-2023, Mayo Clinic physicians deliver excellence in patient care through active engagement in clinical care, teaching, research, and leadership.
A Mayo Clinic Career Offers: •Competitive Compensation •Comprehensive Benefit Package (https://jobs.mayoclinic.org/ benefits) •Funded CME and travel days •Generous Relocation Assistance •Malpractice covered by Mayo Clinic To view and apply to current opportunities, please visit jobs.mayoclinic.org/ emergencymedicine. (PA 2003)
Email: hooks.aaron@mayo.edu
Website: https://jobs.mayoclinic.org/emergencymedicine
NEW JERSEY
RWJBarnabas Health, the largest integrated healthcare system in NJ, is seeking a Pediatric Emergency Medicine Physician for a FT role at Monmouth Medical Center in Long Branch, NJ. As part of the Pediatric Emergency Medicine team, the candidate will work alongside an experienced team of physicians and the opportunity to work closely alongside MMC’s Pediatrics division. In the heart of the Jersey Shore, this practice is just moments away from the famous NJ beaches and shore attractions.
Requirements: • BE/BC in Pediatric Emergency Medicine • NJ licensed or eligible If you are interested in this position, contact Meghan.Ryan@rwjbh.org (PA 1997)
Email: Meghan.Ryan@rwjbh.org
Website: https://www.rwjbh.org/
NEW YORK
Chair of the Department of Emergency Medicine at Glen Cove Hospital Glen Cove Hospital is a 216-bed community hospital with the resources to care for all types of patients. Glen Cove has a very supportive and pro-emergency medicine administration as well as a new ICU, CCU, Telemetry, and Brain Injury Unit. We also have a very active and supportive hospitalist program. As Emergency Medicine Chair, you’ll have complete operational and clinical oversight of the department. You’ll collaborate with our experienced service line leadership team in efforts such as recruiting, finance, business development, and more. You’ll also have the incredible opportunity to work with other healthcare professionals across Northwell Health’s extensive integrated network. Glen Cove Hospital has a full-service Emergency Medicine department. Some highlights include: • Approximately 20,000 annual visits • ED consists of 22 private rooms and 4 trauma/critical care beds • 18 ICU/CCU beds • Press Ganey Guardian of Excellence Award 2022 for patient experience • Our Geriatric Emergency Department has a Level 1 Accreditation from ACEP • Designated Primary Stroke Center by The Joint Commission • AHA/ASA Get with the Guidelines Stroke Gold Plus with Honor Roll Plus Award • ACEP Accreditation Bronze Level for PACED (Pain & Addiction Care in the ED) Submit your CV to: adaily@northwell.edu In addition to the listed responsibilities, this leader will promote a positive and inclusive organizational culture, play an essential role in creating and executing team member engagement initiatives, and champion and advance diversity, equity, and inclusion as central to the organization and its values system. (PA 1981)
Email: ppenso@northwell.edu
Website: https://jobs.northwell.edu/career-specialties/ physicians/
ONTARIO, CANADA
Located in beautiful Windsor, Ontario, Canada, our client, Windsor Regional Hospital (WRH), is situated directly across the border from Detroit, Michigan. WRH is the regional provider of advanced care in complex trauma, renal dialysis, cardiac care, stroke, neurosurgery, intensive care and acute mental health. WRH is seeking a Chief, Department of Emergency Medicine who will provide strong leadership across the Department and Program for service delivery, resource utilization and metrics driven performance management. CPSO Pathway licensure is easily available for U.S. Board Certified Physicians. Please forward a CV and cover letter in confidence to: Marcy SaxeBraithwaite, E-mail: msaxe-braithwaite@medfall.com (PA 2004)
Email: msaxe-braithwaite@medfall.com
Website: https://www.medfall.com/
WEST VIRGINIA
The Charleston Area Medical Center Institute for Academic Medicine is seeking Emergency Medicine clinicians for academic positions as Core Faculty and Clinical Core Faculty. This regional, tertiary medical center sponsors an ACGME accredited emergency medicine residency program with 20 residents at present. Serving a multi-county area, the four Emergency Departments see over 130,000 patients per year and the following locations: CAMC Memorial Hospital - 30 beds with 4 assessment beds CAMC General Hospital – Level 1 Trauma Center with 26 beds and additional fast flow areas CAMC Teays Valley Hospital – 10 beds with 2 assessment beds CAMC Women and Children’s Hospital – 20 beds · Mid-level coverage all sites · 24/7 Hospitalists Coverage · Complete specialty and surgical support · Strong Administrative Support (PA 1989)
Email: ryan.nagy@vandaliahealth.org
Website: https://www.camc.org/
SECTION III: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
(Below are military/government employed positions.)
None Available at this time.
SECTION IV: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
CALIFORNIA
Join our independent, democratic, partnership Group in sunny southern California. Epic, Dragon, holiday and night shift differential as well as APP help. Please send CV in confidence or see our website https://www.scemg.org/ (PA 1994)
Email: smistry007@yahoo.com
Website: https://www.scemg.org/
CALIFORNIA
Join our team in the San Francisco Bay Area with immediate and ongoing Emergency Medicine and Urgent Care positions!
Recently awarded a 5-year contract with an option for a 5-year extension with Santa Clara County Health System. Emergency Physicians Associates (EPA) is a democratic group with absolutely zero private equity, public debt, venture capital involvement, or non-physician shareholders. Pay is productivity based. Average EP hourly in excess of $300.00/hour. Night shift stipend. Transparent 3-year partnership track. Scheduling is performed by a practicing Emergency Physician with a full understanding of typical ED scheduling patterns. Predominantly 9-hour shifts. Engaged and responsive ED leadership. Excellent relationships with hospital administration and nursing staff. EDs we staff: Santa Clara Valley Medical Center. High acuity county hospital. Level 1 trauma center. Regional burn center. STEMI and Stroke receiving center. EM residency host. O’Connor Hospital. Full-service county-owned community hospital. Saint Louise Regional Hospital. Rural county-owned community hospital. Currently in the planning stages for trauma designation. Onsite CalStar base for ease of transfer. Washington Hospital. Busy well, resourced full-service district-owned community hospital in Fremont, CA. Epic EMR at all facilities. Start date ASAP. Ongoing. Full-time or per-diem. Requirements: ABEM BC/BE, unrestricted CA License, unrestricted DEA. Contact EPA at careers@epamg.com with questions and to apply. (PA 1999)
Email: daniel.nelson@epamg.com
FLORIDA
Join a democratic group in Cape Coral, FL established since 1985, partnered with Lee Health. An annual volume of 70k at a single community hospital site. Competitive pay and top-notch benefits including CME reimbursement, medical, 401k. Equal shift distribution averaging 14 shifts per month, 8-10 hours each, with only a few overnight shifts annually. Patient load of 1.5-2 per hour, with 24-hour physician and APP coverage. Epic with Dragon dictation. Opportunity to teach residents due to a new internal medicine residency. Enjoy a sunny coastal location, perfect for outdoor enthusiasts and families. (PA 1976)
Email: tylerensley@gmail.com
Website: https://capecoralemergencyphysicians.com/
KENTUCKY
Full-time Emergency Department physician positions available summer of 2024. Looking for emergency medicine residency trained physicians ABEM eligible or certified. Compass Emergency Physicians is a democratic group located in Northern Kentucky. We staff the six hospitals owned by St. Elizabeth Healthcare. Five of the hospitals are in Northern Kentucky and one of the hospitals is in southeastern Indiana. Our group consists of 54 ABEM certified physicians and 40 APPs. (PA 2007)
Email: rgeers@compassemergencyphysicians.com
Website: http://compassemergencyphysicians.com
NORTH CAROLINA
More than 40 years strong, ECEP II, P. A. is seeking a full-time emergency medicine physician for our emergency medicine group serving the greater Wilmington, NC area. Our full-time physicians practice an average of 28 to 30 hours per week. Wilmington practice sites include New Hanover Regional Medical Center, a level II trauma center, treating an annual patient volume of 75,000, Orthopedic Hospital, a community hospital with an annual patient volume of 27,000, and Scotts Hill Emergency Department, a full-service standalone emergency department with an annual patient volume of 34,000. Our group also
practices at Pender Memorial Hospital in Burgaw, a community hospital located just 25 minutes north of Wilmington with an annual patient volume of 17,000. ECEP offers competitive pay and an excellent benefits package. Live, practice and enjoy a great quality of life in an exceptional coastal community with beaches, golf, and a historic waterfront at your doorstep. (PA 1984)
Email: kskaggs@ecepnet.com
OREGON
Northwest Acute Care Specialists, P.C. (NACS) is an independent, democratic emergency medicine group. We are seeking BC/BE Emergency Physicians who are collaborative team players with excellent interpersonal skills. NACS contracts exclusively with Legacy Health to provide emergency medical services in Portland, Oregon and the surrounding areas. We are recruiting for multiple sites with different practice opportunities. Please see our posting for full job description and to apply: https://emnacs.bamboohr.com/careers/26 (PA 2001)
Email: aflora@emnacs.com
WASHINGTON
Emergency Physicians of Mason County are recruiting to add 1-2 partners to our LLC. We are an independent democratic group that staff a rural critical access hospital in the south Puget Sound. We have held the contract for over 30 years. Mason General Hospital in Shelton, Washington has an ED that sees approximately 20k patients a year. We have three daily shifts, 1112 hours each. No midlevels, and everyone is ABEM certified. 13 Bed ED. Excellent nursing coverage, often with 5 RN’s. General surgery and OB/GYN backup. Benefits: Competitive salary, malpractice paid by hospital (occurrence), 401-K, group health plan. Beautiful place to live. 1 hour or less from Olympic National Park. 2 hours to skiing. 2 hours from Seattle and Portland. Email rgbelville @ runbox.com. (PA 1982)
Email: rgbelville@runbox.com
are hospitals, non-profit
or medical school employed positions.)
are independent
(Below
contractor positions.)
COMMON SENSE SEPTEMBER/OCTOBER 2023 47
AAEM is the leader within our field in preserving the integrity of the physician-patient relationship by fighting for a future in which all patients have access to board certified emergency physicians and physician rights are protected.
Member Benefits
Publications
Free subscriptions to the Journal of Emergency Medicine and Common Sense
Education
Discounted registration to the Annual Scientific Assembly and other AAEM events throughout the year
Members-Only Section
Access the AAEM Job Bank, your Advanced Resuscitation Expertise Card (for Full Voting members), and other academic and career-based benefits
Learn more about these and other member benefits at www.aaem.org/membership/benefits
American Academy of Emergency Medicine 555 East Wells Street, Suite 1100, Milwaukee, WI 53202-3823 (800) 884-2236 info@aaem.org www.aaem.org
Membership Categories
Fellow and Full Voting – FAAEM
Dues: $525 Board certified in emergency medicine or pediatric emergency medicine
Associate
Dues: $250 Graduate of an ACGME or AOA approved emergency medicine training program and not yet taken or passed your EM board
Fellow-in-Training
Dues: $75 Graduate of an ACGME or AOA approved emergency medicine training program and currently enrolled in a fellowship
International Member
Dues: $150 Physicians with an interest in emergency medicine who practice outside of the United States or Canada

Emeritus Member
Dues: $250 Full voting member who has practiced emergency medicine for 30 or more years and has been a full voting member for a minimum of 10 years -or- at least 65 years of age and have been a full voting member for a minimum of 10 years
Special circumstances may lead to a request for emeritus membership and will be reviewed on a case-by-case basis. See www.aaem.org/membership for more information.
Learn more and join today at: www.aaem.org/membership
Group Membership
AAEM offers group memberships to allow hospitals/groups to pay for the memberships of all their EM board certified & board eligible physicians.
100% ED Group Membership
Criteria: All board certified and board eligible physicians at your hospital/ group must be members
Discount: 10% discount on membership dues
ED Group Membership
Criteria: Two-thirds of all board certified and board eligible physicians at your hospital/group must be members
Discount: 5% discount on membership dues
For group memberships, AAEM will invoice the group directly. If you are interested in learning more about the benefits of belonging to an AAEM ED group, please contact us at info@aaem.org or (800) 884-2236.
Join Today! www.aaem.org/membership AAEM-0823-310 COMMON SENSE SEPTEMBER/OCTOBER 2023 48
Life-changing, lifesaving careers in Emergency Medicine

Join

When you work within Emergency Medicine at Mayo Clinic, you’re part of a collaborative, multidisciplinary team that’s delivering lifesaving care to those who need it most. Whether you’re based in an academic or community setting, you’ll get the full support of Mayo Clinic to put the needs of the patient first, all while growing your professional skills and experience. Take on a life-changing, lifesaving career with Mayo Clinic. jobs.mayoclinic.org/emergencymedicine Our Emergency Medicine Team

SENSE 555 East Wells Street / Suite 1100 Milwaukee, WI 53202-3823 PRSRT STD U.S. POSTAGE PAID MILWAUKEE, WI PERMIT NO. 0188
COMMON














 Chris McNeil, MD
Chris McNeil, MD










 Moiz Qureshi, MD MBA
Moiz Qureshi, MD MBA


















 Mel Ebeling, MS3
Mel Ebeling, MS3




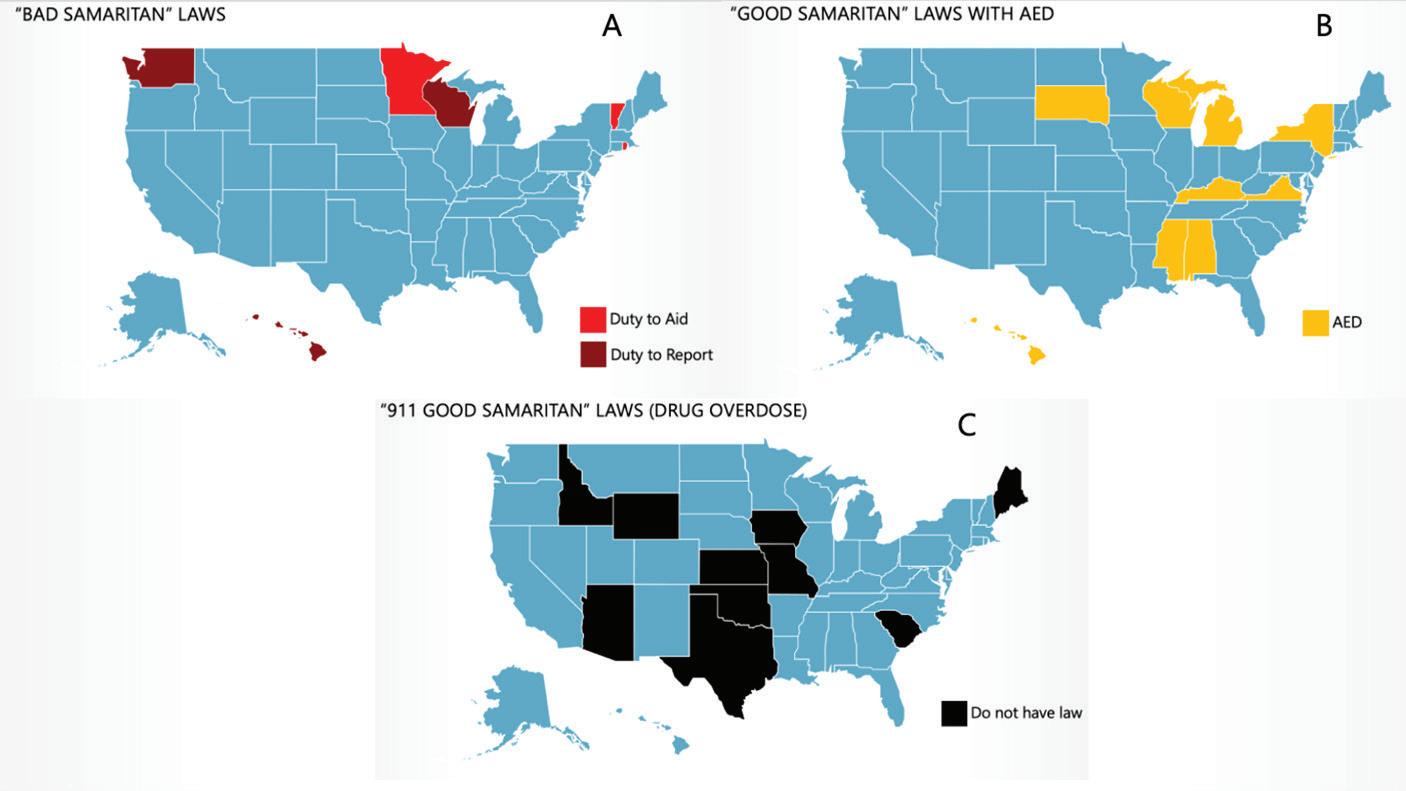


 Melissa Myers, MD FAAEM
Melissa Myers, MD FAAEM


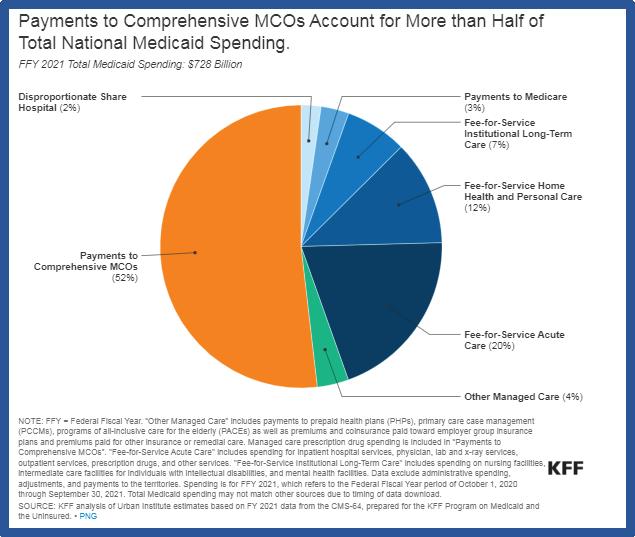










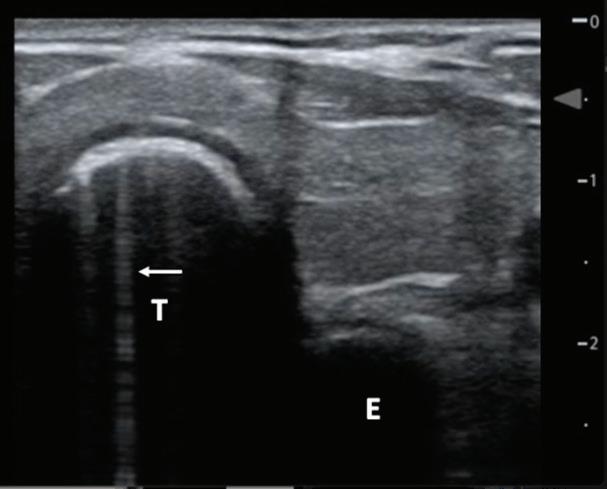
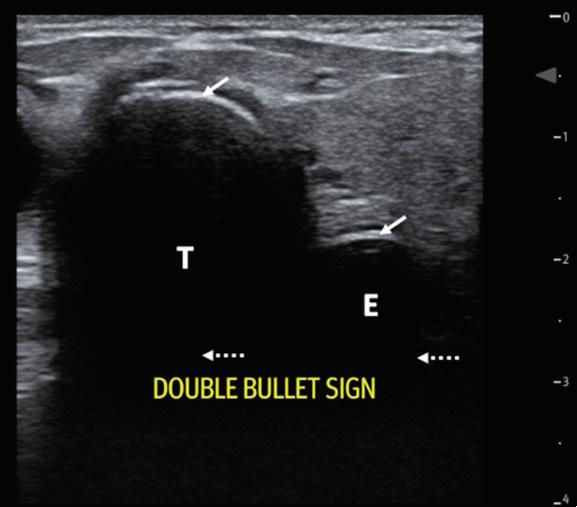 Bailey Balouch, MD,* Wesley Goodman-O’Leary, MD MPH, † Raghav Sahni, DO, † and James Longenbach, MD †
Bailey Balouch, MD,* Wesley Goodman-O’Leary, MD MPH, † Raghav Sahni, DO, † and James Longenbach, MD †