16 minute read
Chapter 7: How does Covid affect the organs long-term?
CHAPTER 7
How does Covid affect the organs longterm?
AcuteSARS-CoV-2infectionmayresultinshortorlong-term damage to critical organs. This section will include organ damageasafeatureofLongCovidinordertoacknowledgethe lastingdisabilitythatcanoccur. Fortreatmentandreimbursementpurposes,aslongasthereis clear and specific organ damage, the condition will not be classifiedasLongCovidbutratherinjurytothatspecificorgan (e.g.kidneydisease,notLongCovidkidneydisease).LongCovid is a diagnosis of exclusion, meaning there is no other clear medicalevidencesuchasmeasurabledamagetoaspecificorgan or tissue. Patients will be diagnosed with Long Covid for the purposeofmedicaltreatmentonlyiftheunderlyingcauseofthe symptomscannotbedirectlypinpointed.98
Can acute SARS-CoV-2 infection cause long-term lung damage?
SARS-CoV-2infectioncanaffectthelungs,causingcomplications such as pneumonia, sepsis (infection that spreads through the bloodstream),andbronchitis.Itcantakemonthstoayearforthe lungstorecovertopre-Covidlevels.99 Thisisespeciallytruefor
98 Recognizing the Clinical Sequelae of COVID-19 in Adults: COVID-19 LongHaulers -PMC 99 COVID-19 Lung Damage | Johns Hopkins Medicine
more severe Covid-19 cases, in which the damage to the lungs takesmonthstoheal.100
Covid-19lungfibrosis,orscarring,developsasaresultofsevere lunginflammation.Acuteinfectioncausesthelung’sairsacsto scarandthicken,leavingthempermanentlyunabletooxygenate blood.101 This is often seen when Covid-19 pneumonia progresses to Acute Respiratory Distress Syndrome (ARDS), a typeoflungfailure.Otherscarringriskfactorsincludesmoking, advancedage,comorbiditiessuchasdiabetes,hypertensionand coronary artery disease, and prolonged ICU stay/mechanical ventilationforCovid-19.102 Lungfibrosisisirreversibleandcan cause lasting impacts on breathing and exercise beyond acute SARS-CoV-2infection.
Commonlungsymptomsincludeshortnessofbreath/difficulty breathing (dyspnea), cough, chest pain and/or fatigue.103 Difficulty breathing, especially during exercise, and fatigue in particularareoftenreportedinpeoplewithLongCovid.104
How can I assess lung damage caused by Covid-19?
ClinicalprofessorAlejandroComellasrecommendsrequestinga computed tomography (CT) scan to look for small-airway abnormalities; a standard breathing capacity test is unlikely to detectanythingunusualforthosewithLongCovid,butaCTscan might.105 Treatment plans would focus on treating symptoms andrehabilitatinglungfunction.
100 COVID-19 Lung Damage | Johns Hopkins Medicine 101 Treatment for pulmonary fibrosis | Asthma + Lung UK 102 Post covid 19 pulmonary fibrosis. Is it real threat?
103 Long COVID or Post-COVID Conditions | CDC 104 Phenotyping long COVID | European Respiratory Society 105 Long COVID May Bring Long-Term Lung Damage | Health News | US News
Can acute SARS-CoV-2 infection cause long-term Kidney damage?
SARS-CoV-2 can cause long-term kidney damage. The kidneys are a direct target for the Covid-19 virus, which can invade highlyspecializedkidneycellscalledpodocytes.106Kidneyinjury canalsooccurasaconsequenceofinflammationinotherparts ofthebodyafterviralexposure,oralackofoxygenintheblood asaresultofCovid-relatedpneumonia.107 Thelong-termresult of such damage is kidney disease and/or kidney failure. More information can be found on Covid-19 and podocytes in the article, Targets for Infection: How SARS-CoV-2 Damages the Kidneys. ContractingCovid-19increasesthelikelihoodofkidneydamage no matter the severity of one’s symptoms. People who were hospitalized or went to the ICU for SARS-CoV-2 infection have the highest risk—about 30% for those hospitalized, and more than 50% for those in ICU.108 People with severe cases should takespecialprecautions.109KidneyimpactmaychangeasCovid19variantscontinuetoevolve,asexpertsbelievenewervariants maybelesscapableofinfectingkidneycells.110 About90%ofpeoplewithkidneyinjurydonotexperiencepain orothertellingsymptoms.111 Itisimportanttodetectandtreat earlyon.112Severekidneydamagecanleadtokidneyfailure,and
106 Frontiers | SARS-CoV-2 Employ BSG/CD147 and ACE2 Receptors to Directly Infect Human Induced Pluripotent Stem Cell-Derived Kidney Podocytes 107 COVID-19 can directly infect and damage human kidney cells --ScienceDaily 108 Coronavirus: Kidney Damage Caused by COVID-19 | Johns Hopkins Medicine 109 Kidney Outcomes in Long COVID | American Society of Nephrology 110 COVID-19 can directly infect and damage human kidney cells --ScienceDaily 111 COVID-19 long-haulers at risk of developing kidney damage, disease 112 Kidney Disease: The Basics
the only treatment options at that stage are dialysis or kidney transplantsurgery.113
How can I assess kidney damage caused by Covid-19?
After catching Covid-19, the best course of action is to request tests which identify kidney damage: an Albumin-Creatinine Ratio (ACR) urine test and a glomerular filtration rate (GFR) blood test. If kidney damage is detected early, a doctor can prescribetreatmentstokeepthekidneysfunctioningforaslong aspossible.114 Lifestylechangestodietandexercisemayalsobe recommended, especially if that person has other risk factors suchasdiabetesandhypertension.
Can acute SARS-CoV-2 infection cause long-term heart damage?
Covid-19canhavelong-lastingimpactsontheheart.TheSARSCoV-2virusdamagestheheart’sbloodvesselswithoutinfecting thecellsdirectly.115 Thedysfunctiontothesecells—pericytes— seeminglyaccountsforCovid-19’svascularcomplications.More onCovid-19damagetoheartpericytescanbefoundinthearticle Pericyte Damage: Surprising Cause of Covid-Related Myocarditis. Covid-19infectionincreasestheriskofseveralheartissues.This includes blood clots (thrombosis), heart inflammation (myocarditis or pericarditis), irregular heartbeat (dysrhythmias),heartattacks(myocardialinfarction),andheart
113 Choosing A Treatment For Kidney Failure 114 Early Kidney Disease Treatment in Baltimore | University of Maryland Medical Center 115 The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147 receptor-mediated signalling: a potential noninfective mechanism of COVID-19 microvascular disease
failure.116 ThiscouldbecausedbyCovid-19damagingtheright sideoftheheart.117
Contracting any form of Covid-19—be it severe, mild or asymptomatic—increases risk of heart complications. People who did not have heart problems or pre-existing conditions to begin withstillexperience thisheightenedrisk.118 Cardiologist SaurabhRajpaldescribesCovid-19itselfasariskfactorforheart disease,asonewouldobesityordiabetes.119 LingeringCovid-19-relatedheartissuesmanifestthroughchest pain, shortness of breath (dyspnea), fatigue, palpitations, arrhythmias (irregular heartbeats), fainting (syncope), and others.120 Elevated blood pressure is also possible.121 These issues can cause problems with exercise ability and general mental/physical well being.Current data suggeststhese heartrelatedsymptomsmaypersistformorethanayear.122 TreatmentforCovid-19-relatedheartcomplicationsdependson an individual’s type of heart disease. For example, those suffering with rare Covid-19-related myocarditis may receive immunosuppressive drugs (e.g. corticosteroids) and be
116 Long Covid: post-acute sequelae of COVID-19 with a cardiovascular focus | European Heart Journal | Oxford Academic 117 Right ventricular dysfunction in patients with COVID‐19 pneumonitis whose lungs are mechanically ventilated: a multicentre prospective cohort study McCall --Anaesthesia -Wiley Online Library 118 Long-term cardiovascular outcomes of COVID-19 | Nature Medicine 119 Five months post-covid, Nicole Murphy's heart rate is still doing strange things 120 Long Covid: post-acute sequelae of COVID-19 with a cardiovascular focus | European Heart Journal | Oxford Academic 121 2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults: Myocarditis and Other Myocardial Involvement, PostAcute Sequelae of SARS-CoV-2 Infection, and Return to Play 122 Long-term cardiovascular outcomes of COVID-19 | Nature Medicine
monitored to prevent worsening symptoms.123 Athletes with myocarditis will likely abstain from training for three to six months.124 Other possible heart diseases include cardiomyopathy (heart muscle disease) and ischemic heart disease(heartdiseasecausedbynarrowedheartarteries). Some people may experience cardiovascular syndrome rather thanheartdisease.125 Inthesecases,itisdifficulttopinpointthe exact cause of the issues experienced. Evaluation and management will address the most prominent symptoms instead. People suffering from exercise intolerance or a rapid heartratemaybeadvisedtoslowallactivitiesinfavorofrest,or toreplaceallstandingexerciseswithlyingexercises(i.e.rowing, swimmingorcycling).126 Eachpersonshoulddiscusstheircase andtailortheiroptionswithamedicalpractitioner.
1232022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults: Myocarditis and Other Myocardial Involvement, PostAcute Sequelae of SARS-CoV-2 Infection, and Return to Play 124 ACC Issues Clinical Guidance on CV Consequences of COVID-19 -American College of Cardiology. 125 3 tips for doctors trying to manage long COVID's cardiac symptoms | American Medical Association 126 ACC Issues Clinical Guidance on CV Consequences of COVID-19 -American College of Cardiology.
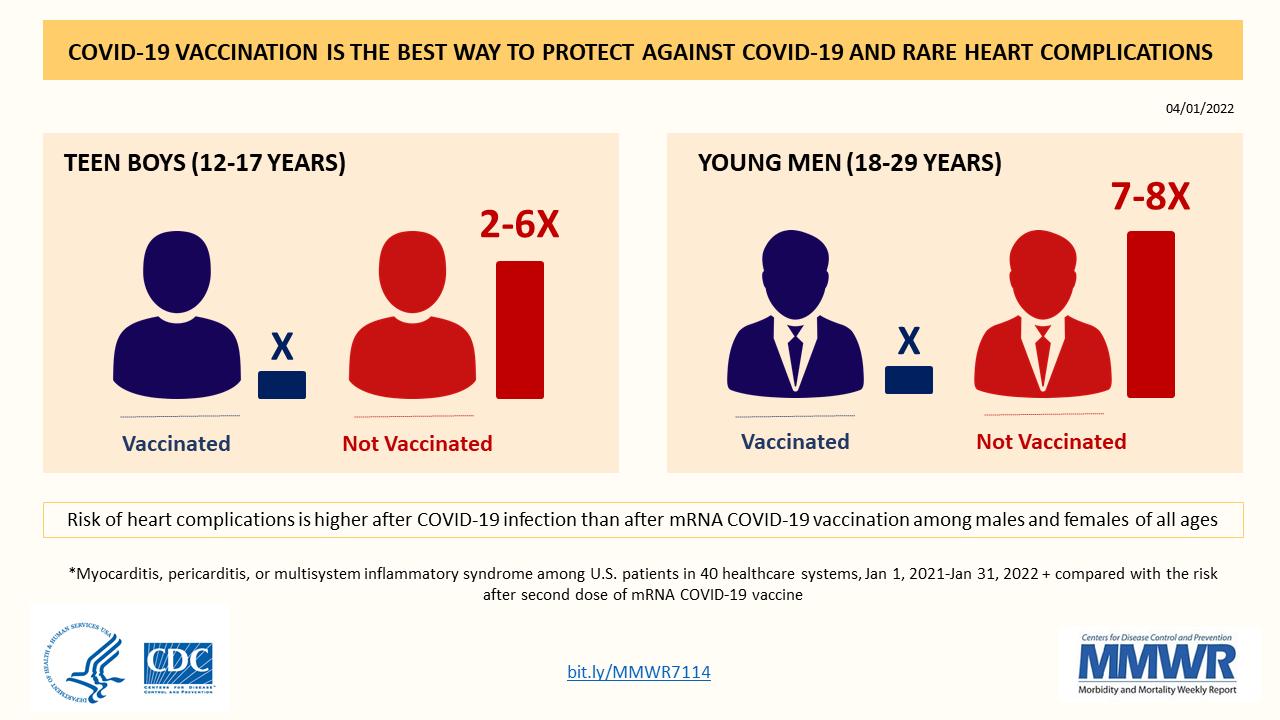
Source:CardiacComplicationsAfterSARS-CoV-2InfectionandmRNA COVID-19Vaccination—PCORnet,UnitedStates,January2021–January2022
Does Covid-19 cause blood clots?
Acute SARS-CoV-2 inflammation can lead to abnormal blood clotting in the body—in the lungs, legs, brain, kidneys and peripheral blood vessels.127 This is seen most often in people hospitalized for Covid-19, but obesity, diabetes and heart diseasecanincreasethisrisk.128
While the body naturally dissolves some clotting, issues arise when the clots form faster than the body can dissolve them. Serious hypercoagulation to the lungs (pulmonary embolism) can cause shortness of breath, chest pain, lightheadedness and more.Aministrokeorstrokeoccursifclotsblockvesselsinthe brain, heart attack if blood flow is reduced in the heart. An uncommonsymptomcausedbybloodclottingis“Covidtoe”:an
127 Long COVID-19 Exercise Capacity Linked to Abnormal Blood Clotting Markers -Hematology.org 128 Coronavirus and Blood Clots: Risks, Complications, Prevention
itchy, reddish-purple rash around the toes that resembles frostbite.129
The risk for blood clots can persist for months after the acute phase for both mild and severe cases. Bleeding events can last for up to two months, blood clots in the leg (deep vein thrombosis)uptothreemonths,andpulmonaryembolismupto sixmonths.130
Do blood clots associated with acute infection contribute to Long Covid?
Newstudiessuggestthatmicroclots—bloodclotswhichcanonly be seen under a microscope—could create the common symptoms of Long Covid and worsen them.131 Microclotting duringtheacutephasewhichusuallynormalizesdoesnotsettle and develops into Long Covid microclots. The clots circulate, reducingoxygenandbloodcellflowthroughoutthebody.This mechanismmaycontributetoLongCovidbrainfogandfatigue. When left untreated, severe microclotting could cause irreparablecelldamagetoorgansliketheheartorbrain. Typically,bloodthinnermedicationisprescribedtoslowdown clotproduction.132 HELPapheresisisanotheralternativewhich filtersoutmicroclotsinadialysis-styletreatment.133Thehopeis to implement blood-clotting therapies early in treatment to
129 Are COVID Toes and Rashes Common Symptoms of the Coronavirus?. 130 Post-COVID Risk for Blood Clot Lasts at Least 6 Months 131 A central role for amyloid fibrin microclots in long COVID/PASC: origins and therapeutic implications | Biochemical Journal | Portland Press 132 Combined triple treatment of fibrin amyloid microclots and platelet pathology in individuals with Long COVID/ Post-Acute Sequelae of COVID-19 (PASC) can resolve their persistent symptoms 133 Could microclots help explain the mystery of long Covid? | Resia Pretorius | The Guardian
alleviateLongCovidsymptoms.NotethatthistypeofLongCovid treatmentisnew,andmaybedifficulttoacquire.
How can I assess damage caused by Long Covid microclots?
People with Long Covid will have a hard time confirming if microclotsarecausingtheirmaladies.Thesymptomscouldbea resultofseveralcomplicationsbesidesmicroclotting,andthere are currently no standard blood tests readily available at hospitalsorlaboratories.134
Can acute SARS-CoV-2 infection lead to lasting thyroid complications?
Covid-19-relatedthyroiditisoftencreateshormoneimbalances thatimpactbodyfunctions.Between15and30%ofpeoplewith Covid-19 develop thyroid problems after infection, with some having issues for 12 months or more.135 Thyroiditis is the inflammation of the thyroid gland, which regulates hormone productionthatimpactsthemetabolismandothermajororgans. TwocommonthyroiddysfunctionsfollowingCovid-19infection include hypothyroidismandthyrotoxicosis.136 Hypothyroidism iswherethethyroiddoesnotcreateandreleaseenoughthyroid hormone into the bloodstream. Thyrotoxicosis is where excessive levels of thyroid hormone circulate in the bloodstream. Both dysfunctions cause serious damage to the host.
Covid-19-related thyroid complications are treatable in most cases. Hypothyroidism is treated with synthetic thyroid
134 Could Microclots Be a Hidden Cause of Long COVID Symptoms? 135 How does COVID-19 impact the thyroid? 136 Thyroid and COVID-19: a review on pathophysiological, clinical and organizational aspects
hormone levothyroxine. Thyrotoxicosis is treated with antithyroiddrugssuchasmethimazoleandpropylthiouracil,as wellasradioactiveiodine.
Thebiggestconcernforpeoplewiththyroid-relatedLongCovid isthyroiditis.Thetypicaltreatmentforthyroidinflammationis aspirin and rest, or steroids in prolonged cases. If thyroid dysfunctions continue for months after infection, contact a specialist to discuss the best approach, as rest and aspirin are likelynotenough.
Can acute SARS-CoV-2 infection lead to lasting gastrointestinal issues?
Persistent infection of the gastrointestinal tract may cause at leastsomefractionofLongCovid.Increasingevidencesuggests thevirusmaypersistinthegutundetectedthatcouldgiverise tosystemicdamage. Some of the most common Covid-19 symptoms are gastrointestinal, including nausea, vomiting, and diarrhea. Roughly one third of people with Covid-19 report gastrointestinal complaints. One study found that 17.6% of peoplewithCovid-19experiencegastrointestinalsymptoms.137 Diarrheaisthemostcommon,affecting11.5%. Those with severe Covid-19 are in danger of a wide range of gastrointestinal issues. These include, but are not limited to, elevated liver transaminases, acute cholecystitis, acute pancreatitis, ileus and feeding intolerance, and mesenteric ischemia. The mortality rate for people with mesenteric ischemiaisashighas40%.Thisisanarteryblockagethatcuts
137 COVID Long-Haulers: Gastrointestinal System | The Coronavirus Visualization Team
bloodflowtotheintestines,damagingrelatedorgansandoften resultinginorganfailure. One study found that 44% of those with Covid-19 report gastrointestinal symptoms 90 days after Covid-19 hospitalization.Themostcommonsymptomwaslossofappetite (24%),butothersymptomsincludednausea(18%),acidreflux (18%), diarrhea (15%), abdominal distension (14%), and abdominalpain(7%). The typical recommendations for these symptoms are rest, drinking plenty of fluids, eating certain fiber-rich foods (e.g. bananas), and over-the-counter medications such as laxatives. However, if these symptoms extend several weeks or months afterinfection,pleasecontactaspecialistaboutnextsteps.
Can acute SARS-CoV-2 infection lead to lasting brain damage?
Many of the most common Long Covid symptoms relate to the brain. Between 50 to 90% of hospitalized Covid-19 patients develop at least one type of cognitive or functional impairment.138,139 Impairment can last up to 12 months after initial infection, and likely beyond. Persistence of cognitive issuesthreemonthsafterinfectioniscorrelatedwithanincrease in depression one year on. Cognitive issues have also been
138 Trajectory of cognitive impairments over 1 year after COVID‐19 hospitalisation: Pattern, severity, and functional implications 139 A prospective study of long-term outcomes among hospitalized COVID-19 patients with and without neurological complications
recorded in patients with only mild infections that did not requirehospitalization.140,141 Cerebrospinal fluid (CSF) helps cushion the brain from injury and helps provide it with vital nutrients. Inflammation of the brain can change the protein content of cerebrospinal fluid. In many Covid-19 patients, the cerebrospinal fluid is filled with inflammatoryproteins.142 Thepresenceofsuchmarkersinthe brainiscorrelatedwithalossofgraymatter,meaningthebrain shrinks. Such shrinkage has been observed in the brains of people with Covid-19 no matter the severity of infection.143 Whetherthisdamageispermanentisnotyetknown. Thelossofbrainsizeinthosewhorequiredhospitalizationfor theirCovid-19mirrorsthelossinsizeseenbetweentheagesof 50and70.Thisisroughlyequivalent tolosing10IQ points.144 The area of the brain responsible for memory is particularly strongly affected, with a reduction of brain mass ranging from 0.2% to 2%. Middle aged adults and beyond lose only around 0.2%to0.3%ofbrainvolumeayear. There are currently no specific treatment options for the cognitiveimpairmentcausedbyCovid-19.
Can acute SARS-CoV-2 infection lead to lasting liver damage?
140 Frequent neurocognitive deficits after recovery from mild COVID-19 | Brain Communications | Oxford Academic 141 Persistent COVID-19-associated neurocognitive symptoms in nonhospitalized patients | SpringerLink 142 Brain cortical changes are related to inflammatory biomarkers in hospitalized SARS-CoV-2 patients with neurological symptoms | medRxiv 143 SARS-CoV-2 is associated with changes in brain structure in UK Biobank | Nature 144 Lasting brain impacts of severe COVID-19 equivalent to 20 years of ageing | Imperial News
Liver damage has been reported in hospitalized Covid-19 patients with a rate of incidence ranging from 10.6 to 69%.145 Abnormal liver function manifests itself as elevated aspartate aminotransaminase(AST),alanineaminotransferase(ALT),and bilirubin levels. Although more common in severe cases of Covid-19,liverdamagecanstilloccurinmildcases.146,147 LiverdamageinCovid-19patientsisusuallymildtomoderate, and returns to normal after recovery from acute infection without the need of any special treatment.148, 149 Severe liver damage is rare, and usually lasts only a short period of time; patients can be given drugs such as L-ornithine-L-aspartate to helpwithrecovery.150 Researchisongoingtounderstandthepediatricimplicationsof Covid-19-relatedliverdamage.Acasestudyreportsthedelayed development of hepatitis in children who had mild/asymptomatic Covid-19.151 The mechanism is not yet understood, but the authors speculate the cause to be a postinfection immune reaction (similar to MIS-C). Another alternative explanation is that SARS-CoV-2 infection causes
145 Liver injury in COVID-19: clinical features and treatment management | Virology Journal | Full Text 146 Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis -The Lancet Gastroenterology & Hepatology 147 Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis 148 Potential Effects of Coronaviruses onthe Liver: An Update | Medicine 149 Liver injury in critically ill patients with COVID-19: a case series | Critical Care | Full Text 150 Etiology and management of liver injury in patients with COVID-19 151 Long COVID-19 Liver Manifestation in Children
immune dysregulation, leaving the body vulnerable to other infectiousagentsthatcausehepatitis.
Can acute SARS-CoV-2 infection lead to lasting pancreatic damage?
In rare cases, SARS-CoV-2 can damage the pancreas.152, 153, 154 This is evidenced by raised amylase and lipase levels, both of which are biomarkers for pancreatic damage. Generally, this damagemanifestsasacutepancreatitis—aconditionwherethe pancreas becomes inflamed for a short period of time. Symptomsofacutepancreatitisinclude:nausea,vomiting,fever, andthesuddenonsetofextremeabdominalpain.Mostpatients recoverfullyfromacutepancreatitiswithinaweek.155 Preliminary evidence suggests SARS-CoV-2-induced damage to thepancreasmayalsoleadtohighbloodsugar(hyperglycemia), alteredglucosemetabolism,and,insomecases,theonsetoftype 1diabetes.156,157,158 Onsetoftype1diabeteswasnotassociated withanypre-existingriskfactorssuchasobesity,pre-diabetes, orrecentadministrationofcorticosteroids.Furtherresearchis requiredtoconfirmthesefindings.
152Frontiers | Emerging Clinical Features of COVID-19 Related Pancreatitis: Case Reports and Review of the Literature 153Pancreatic damage in COVID‐19: Why? How? -Bacaksız -2021 -International Journal of Clinical Practice -Wiley Online Library 154 COVID-19 induced acute pancreatitis after resolution of the infection ScienceDirect 155 Acute pancreatitis -NHS. 156 Consequences of COVID-19 for the Pancreas | HTML 157 SARS-CoV-2 infects and replicates in cells of the human endocrine and exocrine pancreas | Nature Metabolism 158 New-Onset Diabetes in COVID-19: Time to Frame Its Fearful Symmetry | SpringerLink
Ifyouareexperiencingasuddenonsetofsymptomsthatmirror type 1 diabetes following Covid-19, reach out to a healthcare provider.Ifnecessary,theymayreferyoutoanendocrinologist.
What’s the relation between Long Covid and the vagus nerve?
There hasn’t been sufficient research on the impact of SARSCoV-2 on the vagus nerve to establish whether it may be contributingtoLongCovidsymptoms. There is only one study—still unpublished and yet to undergo peer-review—thatsuggestsSARS-CoV-2maybeabletodamage the vagus nerve.159 The authors note: “In this pilot evaluation, most Long Covid subjects with vagus nerve dysfunction symptoms had a range of significant, clinically-relevant, structural and/or functional alterations in their vagus nerve, includingnerve thickening,trouble swallowing, and symptoms of impaired breathing. Our findings so far thus point at vagus nerve dysfunction as a central pathophysiological feature of LongCovid.” Untilmoreresearchisconductedinthisfieldandadditionaldata gathered,itremainsuncleartowhatextentdamagetothevagus nerve plays a part in Long Covid. It is possible, but currently thereisapaucityofevidence.
Can acute SARS-CoV-2 infection lead to lasting eye damage? Mostlikely,no.TheCovid-19virusdoesaffecttheeyesin11to 32% of cases. Studies suggest the SARS-CoV-2 virus can infect cellsintheeyeandrapidlyreplicatewithinthefirst42hoursof
159 Pilot study suggests long COVID could be linked to the effects of SARS-CoV-2 on the vagus nerve
infection.However,after72hoursvirus-causedplaquesettlesto levelsseenatthe24hourtimepoint.160 Thisprocessisfurther explained in the article In the Eye of the Storm: How Covid-19 Impacts the Eye. Thesymptomscausedbythisprocessseemto be short term and normally do not cause visual impairment. Some short-lived ocular symptoms include soreness, dryness, itchiness, tearing, a foreign body sensation, and blurred vision.161 162
Conjunctivitis—typically known as pink eye—is the most common eye disease associated with post-Covid infection.163 This eye inflammation occurs in 1 to 3% of Covid-19 cases164 , manifesting as redness in one or both eyes days—or weeks— after initial infection.165 Avoid touching the discharge from a pinkeye;thiscancontaminatesurfacesandeventuallyspreadit toothers.166Therednessshouldsubsidewithdoctor-prescribed eyelubricantsandpreservative-freeeyedrops. In rare cases, Covid-19 infection may increase the risk of developing blood clots in the eye (retinal vein occlusion) in a similar way the virus does to other blood vessels in the body; thiscouldbefromtheinfectionitself,orasideeffectfromlack
160SARS-CoV-2 infects and replicates in photoreceptor and retinal ganglion cells of human retinal organoids 161Sore eyes as the most significant ocular symptom experienced by people with COVID-19 162 Ocular Manifestations of COVID-19: A Systematic Review and Meta-analysis -PMC 163Prevalence of and Short-term Changes in Conjunctival Manifestations Among Patients With SARS-CoV-2 Infection | External Eye Disease | JAMA Network Open 164 Conjunctivitis and COVID‐19: A meta-analysis -Loffredo -2020 -Journal of Medical Virology -Wiley Online Library 165 COVID-19 and Eye: A Review of Ophthalmic Manifestations of C... : Indian Journal of Ophthalmology 166 Eye Care During COVID-19: Masks, Vaccines and Procedures - American Academy of Ophthalmology
ofphysicalactivityorworseningsystemicbloodpressure.Preexisting conditions such as diabetes, hypertension or hyperlipidemia may further this risk.167 Generally, vein blockages in the eye can increase blood pressure in the eye or causefluidtoleakthere,leadingtodiseaseswhichdistortvision: glaucomaandmacularedemarespectively.168 Inthesecases,an ophthalmologist might prescribe anti-VEGF to lessen the swelling.169
How does Covid-19 contribute to hair loss?
HairlossisnotadirectsymptomofCovid-19.170 However,inthe months following severe fever, noticeable hair loss is often reported.FeverisoneofthemostcommonsymptomsofCovid19,meaningmanysevereCovid-19casesmayleadtosomehair loss.
Hair typically begins to shed two to three months after illness ends. This occurs due to a higher than average amount of hair enteringthesheddingphaseatthesametime,whichisforcedby fever.Hairlosscouldcontinueuptoninemonthsafteritbegins, however almost all instances of Covid-19-related hair loss will concludeandhairvolumewillreturntonormalinduecourse.
Hairlosscanalsobetriggeredbyphysicalandemotionalstress, which is common in those with Covid-19. However, if you believeyourhairlossisnotrelatedtofeverorstress,consulta dermatologistforpotentialtreatment.
167 Changes in the Incidence of Retinal Vascular Occlusions After COVID-19 Diagnosis | Ophthalmology 168 Retinal vein occlusion: MedlinePlus Medical Encyclopedia 169 Practical Guidelines for RVO Management -Retina Today 170 Can COVID-19 cause hair loss?
Can acute SARS-CoV-2 infection cause bone damage?
InfectionwithSARS-CoV-2cancausequickandsignificantbone loss in severe and even mild cases. One study using mouse models observed a 25% decrease in bone mass within two weeks of infection and a 63% increase in osteoclasts.171 This suggests the disease also leads to increased chance of osteoporosis, causing brittle and weak bones. This puts the elderlyathighriskastheyareleastlikelytonaturallyregenerate lostbonematter.
AmorerecentstudyonSyrianhamsterscorroboratesthemouse findings.172 The Syrian hamsters showed similar decreases of bonemassandincreasesofosteoporosisindicators.
How does Covid-19 affect sense of smell?
A hallmarkCovid-19symptomisthe lossof smellandtaste.In mostcases,thesenseofsmellrestoresitselfafterafewweeks, but 12% of people continue to report complete loss of smell monthsaftertheinitialinfection.173
Olfactory cells are a major factor in taste recognition, but researchshowsthattheSARS-CoV-2virusbindstoanddepletes sustentacularsupportcells,whichsurroundolfactoryreceptors in the epithelium.174 Unlike receptor neurons, sustentacular cellsexpressACE-2andTmPRSS2membraneproteinsthatthe SARS-CoV-2 uses to attach to and invade cells. Despite the fact
171 IU School of Medicine researchers discover ties between COVID-19 and bone loss 172 SARS-CoV-2 infection induces inflammatory bone loss in golden Syrian hamsters | Nature Communications 173 Losing the Sense of Smell: How Covid-19 Infection Induces LongLasting Symptoms 174 Mechanism Revealed Behind Loss of Smell with COVID-19
thatolfactoryreceptorsarenotdirectlyinfected,theydosustain significantdamagefromtheinfectionofneighboringcells.
Can Covid-19 cause long-term damage to the female reproductive system?
One study suggests that SARS-CoV-2 infection can increase the risk of placenta complications in unvaccinated pregnant women.175 SARS-CoV-2placentitischangestheplacenta,making it difficult to deliver oxygen and nutrients to the baby.176 The asphyxiationcausedcanleadtohigherchancesofstillbirths.The CDCstatesthat,althoughrare,contractingCovid-19canelevate theriskforstillbirths(notablyduringtheDeltawave).177
Can Covid-19 cause long-term damage to the male reproductive system?
Themalereproductivetractisatriskofinfectionanddamageby SARS-CoV-2.178, 179 This damage can be long lasting, persisting upto4monthsafterinitialinfection. Theconsequencesofinfectiontothemalereproductivetractare notlimitedtoonesingletissue.Instead,damagecanspanacross four major areas: the testes, the prostate, the penis, and the pampiniformplexus.
175 New research shows impacts of COVID-19 on reproductive health 176 Placental Tissue Destruction and Insufficiency From COVID-19 Causes Stillbirth and Neonatal Death From Hypoxic-Ischemic Injury | Archives of Pathology & Laboratory Medicine 177 Risk for Stillbirth Among Women With and WithoutCOVID-19 at Delivery Hospitalization —United States, March 2020–September 2021 178 An immunoPET probe to SARS-CoV-2 reveals early infection of the male genital tract in rhesus macaques | bioRxiv 179 Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection by Intranasal or Intratesticular Route Induces Testicular Damage | Clinical Infectious Diseases | Oxford Academic
Testosterone levels can drop following SARS-CoV-2 infection, leading to significant testicular shrinkage, a decrease in sperm qualityandquantity,andadecreaseinoverallfertility.180, 181 In the prostate, there is a noticeable increase in prostate-specific antigen(PSA),aproteinassociatedwithprostatecancer.Covid19-induced damage to the prostate can also decrease sperm quality. Infection of the penis can lead to erectile dysfunction andPeyronie’sdisease.Infectionofthepampiniformplexus—a massofsmallveinsthathelpsregulatetesticulartemperature— canleadtotheformationofbloodclots,chronictesticularpain, andtesticularatrophy. Preliminary evidence suggests vaccination may help protect fromlastingdamagetothemalereproductivetract.
180Implications of testicular ACE2 and the renin–angiotensin system for SARSCoV-2 on testis function | Nature Reviews Urology 181Review Article Impact of COVID-19 on Male Fertility




